Validation and Clinical Application of Smartphone-Connected Readers for Urinary Reproductive Hormone Measurement
This article provides a comprehensive analysis for researchers and drug development professionals on the validation and application of smartphone-connected readers for quantifying urinary reproductive hormones.
Validation and Clinical Application of Smartphone-Connected Readers for Urinary Reproductive Hormone Measurement
Abstract
This article provides a comprehensive analysis for researchers and drug development professionals on the validation and application of smartphone-connected readers for quantifying urinary reproductive hormones. It examines the foundational technology enabling at-home hormone monitoring, details methodological protocols for accurate measurement, and presents rigorous analytical and clinical validation data comparing these novel platforms against established laboratory standards. The content further explores the integration of artificial intelligence for data interpretation, addresses troubleshooting and optimization strategies for reliable results, and discusses the transformative potential of these devices in bridging gaps in women's health research and clinical practice.
The Science Behind Smartphone-Based Hormone Monitoring: Technologies and Core Biomarkers
Urinary hormone metabolites provide a non-invasive window into reproductive endocrine function, enabling the monitoring of key physiological events such as the menstrual cycle and ovulation. The metabolites Estrone-3-glucuronide (E3G), Pregnanediol glucuronide (PdG), and the pituitary hormone Luteinizing Hormone (LH) are particularly significant. E3G, a major urinary metabolite of estradiol, reflects follicular development and estrogen activity. PdG, a urinary metabolite of progesterone, serves as a reliable marker for confirming ovulation. The mid-cycle LH surge is the definitive trigger for ovulation. The validation of quantitative, smartphone-reader based home tests represents a significant advancement in reproductive health, moving beyond qualitative results to precise hormone trend analysis [1]. This protocol outlines the methodologies for validating the measurement of these biomarkers using a smartphone-based reader system.
Analytical Validation of a Smartphone-Based Reader
A recent study validated the performance of the Inito Fertility Monitor (IFM), a smartphone-connected device that quantitatively measures E3G, PdG, and LH in first-morning urine samples [1]. The device uses lateral flow assays: a multiplexed competitive ELISA for E3G and PdG, and a sandwich ELISA for LH. The smartphone application captures the test strip image and uses an algorithm to convert optical density (OD) into metabolite concentration [1].
Accuracy and Precision Data
The analytical performance of the IFM was evaluated through recovery studies and calculation of the coefficient of variation (CV), demonstrating high accuracy and reproducibility [1].
Table 1: Analytical Performance of the Smartphone-Based Fertility Monitor [1]
| Hormone Metabolite | Average Coefficient of Variation (CV) | Recovery Percentage | Correlation with Laboratory ELISA |
|---|---|---|---|
| PdG | 5.05% | Accurate | High Correlation |
| E3G | 4.95% | Accurate | High Correlation |
| LH | 5.57% | Accurate | High Correlation |
Key Experimental Protocol: Validation vs. Laboratory ELISA
This protocol describes the method for validating the smartphone reader's hormone measurements against gold-standard laboratory techniques.
Objective: To evaluate the accuracy of the smartphone-based reader (IFM) in measuring urinary E3G, PdG, and LH by comparison with laboratory-based ELISA.
Materials:
- Inito Fertility Monitor (IFM) and test strips
- First-morning urine samples from participants
- Laboratory ELISA kits:
- Arbor Estrone-3-Glucuronide EIA kit (K036-H5)
- Arbor Pregnanediol-3-Glucuronide EIA kit (K037-H5)
- DRG LH (urine) ELISA kit (EIA-1290)
- Microplates, plate reader, pipettes
Procedure:
- Participant Recruitment & Sample Collection: Recruit eligible participants (e.g., women aged 21-45 with regular cycle lengths). Collect daily first-morning urine samples throughout the menstrual cycle.
- Testing with IFM: Dip the IFM test strip into the urine sample for 15 seconds. Insert the strip into the monitor attached to a smartphone. Record the concentration values for E3G, PdG, and LH provided by the application.
- Testing with ELISA: Test the same urine samples using the respective laboratory ELISA kits. Run all samples in triplicate. Use the standard solutions provided with the kits to generate a standard curve for each run. Calculate the metabolite concentration in each urine sample from the standard curve.
- Data Analysis: Calculate the recovery percentage of the three hormones from IFM compared to ELISA. Establish the correlation between the concentration values obtained from IFM and ELISA. Perform statistical analysis, including calculation of the Coefficient of Variation (CV) for reproducibility [1].
Clinical Application and Novel Hormone Trends
The validation study involved 100 women for laboratory correlation and a second group of 52 women who used the device at home [1]. Analysis of the hormone profiles led to two significant findings:
- A Novel Criterion for Earlier Ovulation Confirmation: By observing the trends in urinary PdG rise after the LH peak, researchers identified a new criterion that could distinguish ovulatory from anovulatory cycles with 100% specificity and an area under the ROC curve of 0.98 [1].
- A Previously Unobserved Hormone Trend: The study identified a new hormone pattern, observed in 94.5% of ovulatory cycles, involving a PdG rise before the LH surge [1].
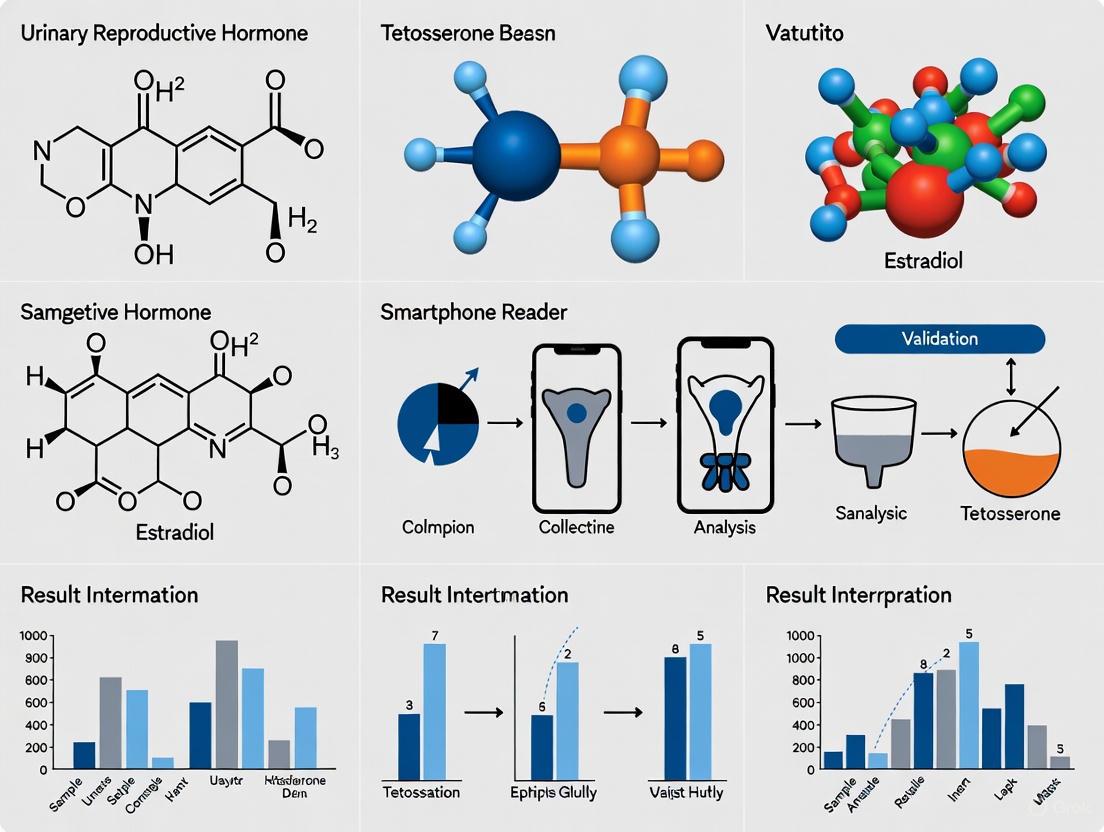
The following workflow diagram illustrates the process from sample collection to clinical insight.
Figure 1: Workflow from urine sample to clinical insight using a smartphone reader.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Urinary Hormone Metabolite Research
| Item | Function / Application | Example Product / Kit |
|---|---|---|
| Urine Collection Cups | Collection and storage of first-morning urine samples. | Sterile, non-cytotoxic polypropylene cups. |
| Competitive ELISA Kits | Quantification of small molecules (E3G, PdG) in urine. | Arbor Estrone-3-Glucuronide EIA Kit (K036-H5) [1]. |
| Sandwich ELISA Kits | Quantification of protein hormones (LH) in urine. | DRG LH (Urine) ELISA Kit (EIA-1290) [1]. |
| Lateral Flow Assay Strips | Multiplexed, point-of-care detection of E3G, PdG, and LH. | Inito Fertility Test Strips (competitive & sandwich formats) [1]. |
| Microplate Reader | Absorbance measurement for laboratory ELISA procedures. | Standard 96-well plate reader. |
| Smartphone Reader & App | Image capture, processing, and quantitative analysis of test strips at home. | Inito Fertility Monitor and mobile application [1]. |
Hormone Dynamics and Ovulation Confirmation Logic
The logic of ovulation confirmation relies on the temporal relationship between the three hormones. The following diagram summarizes the decision pathway based on their trends.
Figure 2: Logic for confirming ovulation based on urinary hormone trends.
Lateral Flow Assays (LFAs) represent a mature point-of-care (POC) diagnostic technology, historically known for providing rapid, qualitative yes/no results [2]. The integration of smartphone-based imaging and analysis is now transforming these conventional LFAs into quantitative diagnostic platforms, enabling precise measurement of analyte concentrations [3]. This shift is particularly impactful in fields like reproductive health, where quantifying hormone levels—such as Luteinizing Hormone (LH), Estrone-3-glucuronide (E3G), and Pregnanediol glucuronide (PdG)—offers a powerful tool for monitoring menstrual cycles and predicting fertility windows outside laboratory settings [1] [4]. This document details the application of this core technology within the specific context of validating a smartphone-connected reader for urinary reproductive hormone measurements.
The transition from qualitative to quantitative LFA reading relies on capturing the assay result as an image and analyzing the optical signal, most commonly the color intensity of the test line, which correlates with analyte concentration [3] [5].
Performance of Analysis Algorithms
Machine Learning (ML) and Deep Learning (DL) models are central to accurate quantification. Different models offer varying balances of performance, computational cost, and robustness.
Table 1: Performance Comparison of ML/DL Models for LFA Image Analysis
| Model | Reported Accuracy / Performance | Key Advantages | Ideal Use Case |
|---|---|---|---|
| ResNet-50 (CNN) | 76.2% accuracy, MSE: 0.00291, R²: 0.9398 [3] | High accuracy, superior robustness to lighting variations and image augmentation [3] | High-precision quantification in real-world conditions |
| Random Forest | Excels with small-size images [5] | High performance with low-resolution input; computationally efficient [5] | Rapid analysis on devices with limited processing power |
| Convolutional Neural Network (CNN) | Outperforms Random Forest on noisy images [5] | Excellent feature extraction from complex or imperfect image data [5] | Environments where perfect image capture cannot be guaranteed |
| Support Vector Machine (SVM), k-NN, Decision Tree | Variable performance, often lower than CNN/Random Forest [5] | Simpler model architectures | Baseline studies or for less complex classification tasks |
Analytical Validation of a Smartphone Hormone Reader
Quantitative LFA systems require rigorous validation against established laboratory methods to ensure clinical utility.
Table 2: Analytical Validation of the Inito Fertility Monitor (IFM) vs. Laboratory ELISA [1] [4]
| Validation Parameter | LH | E3G | PdG | Methodology Summary |
|---|---|---|---|---|
| Correlation with ELISA | High correlation reported [1] | High correlation reported [1] | High correlation reported [1] | Urine samples from 100 women (21-45 yrs) measured in parallel by IFM and lab ELISA |
| Coefficient of Variation (CV) | 5.57% [4] | 4.95% [4] | 5.05% [4] | Measured using repeated tests of standard solutions to assess precision and internal variation |
| Recovery Percentage | Accurate recovery [4] | Accurate recovery [4] | Accurate recovery [4] | Calculated from tests using spiked urine samples to determine measurement accuracy |
| Clinical Utility | Detects LH surge | Tracks estrogen rise | Confirms ovulation | Used to identify a 6-day fertile window and confirm ovulation with 100% specificity in a study of 52 women [1] |
Experimental Protocols
Protocol: Smartphone-Based Quantitative LFA Reader Setup and Operation
This protocol outlines the steps for configuring and using a smartphone-based reader for quantifying hormones via LFAs [1] [4].
1. Principle: A smartphone is used to capture an image of a developed LFA strip. Software on the smartphone automatically detects the region of interest (ROI), corrects for imaging variables, and quantifies the test line intensity. The intensity is converted into an analyte concentration using a pre-established calibration curve [3] [4].
2. Materials:
- Smartphone Reader: Commercially available device (e.g., Inito Fertility Monitor) or a custom 3D-printed holder that positions the LFA strip at a fixed distance from the smartphone camera [4].
- Imaging Environment: For consistent results, use a controlled environment such as a portable imaging box with uniform, shadow-free lighting (e.g., a ring light) to minimize inter- and intra-day lighting variability [3] [5].
- LFA Test Strips: Strips designed for quantitative analysis (e.g., multiplexed strips for E3G/PdG and LH) [4].
- Smartphone Application: Dedicated app with integrated algorithms for ROI detection, optical density calculation, and concentration reporting [3] [4].
3. Procedure: 1. Sample Application: Dip the test strip into a first-morning urine sample for 15 seconds [4]. 2. Assay Development: Wait the prescribed time for the assay to fully develop (e.g., 15 minutes). Do not read the result outside the specified time window [4]. 3. Image Acquisition: Place the developed test strip into the reader attached to the smartphone. Ensure the device is correctly aligned. Capture an image using the dedicated application. The app should automatically guide the user to ensure proper focus and framing [4]. 4. Automated Analysis: * The application uses a multi-scale algorithm to detect the LFA device and correct for variations in smartphone resolution and aspect ratio [4]. * The relevant test and control lines are automatically identified (ROI detection) [3]. * The optical density (OD) of each test line is calculated from the captured image. 5. Quantification: The calculated OD values are converted to analyte concentrations (e.g., in ng/mL or mIU/mL) using a calibration curve stored within the app. This curve is generated during manufacturing for each batch of test strips using standard solutions [4]. 6. Data Reporting: The hormone concentrations and/or fertility status (e.g., Low, High, Peak) are displayed to the user on the smartphone screen. Data can be stored to track trends over time [1] [4].
Protocol: Enhancing LFA Sensitivity via Laser µ-Machining of Nitrocellulose Membrane
This protocol describes a physical method to improve the sensitivity of standard LFAs by controlling the flow rate on the strip, thereby increasing the interaction time between the analyte and detection antibodies [6].
1. Principle: Femtosecond or CO₂ lasers are used to create precise microchannels (µ-channels) or constraints in the nitrocellulose (NC) membrane. These structures delay the lateral flow of the liquid sample, prolonging the time analytes spend in the test zone. This enhanced reaction time leads to a greater accumulation of labeled detection particles (e.g., gold nanoparticles), resulting in a stronger signal and lower limit of detection (LoD) [6].
2. Materials:
- Nitrocellulose Membrane: Standard LFA membrane on a backing card.
- Laser System: A femtosecond laser (e.g., Yb:KGW laser) or a CO₂ laser system. Femtosecond lasers are preferred for "cold" ablation with minimal heat-affected zones (HAZ), which preserves the membrane's properties [6].
- XYZ Translation Stage: A precision stage to move the membrane relative to the focused laser beam.
3. Procedure: 1. Laser Patterning Design: Design a pattern of vertical microchannels. Key parameters to optimize include channel width (e.g., 30 µm to 0.5 mm), length, and density (spacing between channels) [6] [4]. 2. Laser Setup: Focus the laser beam onto the surface of the NC membrane using a microscope objective. Set the laser parameters (power, pulse frequency, scan speed) to achieve clean ablation without carbonizing the membrane. 3. Micromachining: Secure the NC membrane on the translation stage. Execute the patterning program to ablate the microchannels into the membrane surface. 4. Assembly and Testing: Integrate the laser-structured NC membrane into a complete LFA strip (with sample, conjugate, and absorbent pads). The performance is evaluated by: * Wicking Speed Analysis: Recording the flow front movement to confirm flow delay [6]. * Colorimetric Signal Measurement: Comparing the test line signal intensity and LoD of the modified LFA to a pristine (unmodified) LFA using the same analyte samples [6].
4. Expected Outcome: This method has been shown to increase the immunological reaction time by up to 950% and enhance colorimetric signal sensitivity by 30-40% compared to pristine NC membranes [6].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Quantitative Hormone LFA Development
| Item / Reagent | Function / Description | Example from Literature |
|---|---|---|
| Multiplexed LFA Strips | Test strips with multiple assay formats on a single strip to detect different analytes simultaneously. | A strip with one LFA for E3G/PdG (competitive ELISA) and another for LH (sandwich ELISA) [4]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Gold-standard laboratory method for validating the accuracy and precision of the quantitative LFA reader. | Arbor EIA kits for E3G/PdG; DRG LH (urine) ELISA kit [1] [4]. |
| Calibration Standards | Solutions of known analyte concentration used to generate the standard curve for converting optical signal to concentration. | Purified metabolites (Sigma-Aldrich) spiked into analyte-free urine to create a calibration plot [4]. |
| Laser Micromachining System | Equipment for physically modifying the NC membrane to enhance assay sensitivity by controlling flow rates. | A femtosecond laser system used to create microchannels, delaying flow and increasing signal intensity [6]. |
| Interferent Panel | A set of potentially cross-reactive substances used to test the specificity of the assay. | Includes hCG, acetaminophen, ascorbic acid, caffeine, hemoglobin, etc., spiked into samples [4]. |
Visual Workflows and Signaling Pathways
Quantitative LFA Workflow
Hormone Signaling in Menstrual Cycle
The Role of AI and Computer Vision Algorithms in Hormone Trend Interpretation and Baseline Establishment
The quantitative tracking of urinary reproductive hormones represents a significant advancement in personalized healthcare. Traditional methods for hormone assessment often rely on subjective visual interpretation of test lines or require time-consuming laboratory analyses, creating barriers to personalized, real-time health monitoring [1]. The integration of artificial intelligence (AI) and computer vision with point-of-care biosensors is overcoming these limitations, enabling precise, automated interpretation of hormone data and establishing personalized baselines [7]. These technological synergies are central to validating new digital health tools, such as smartphone-connected readers, for both clinical and home-use settings.
This document details the application of AI and computer vision algorithms within the context of validating a novel smartphone-connected reader for urinary reproductive hormone measurements. It provides specific protocols and data analysis frameworks for researchers and drug development professionals working in this advanced field.
AI and Computer Vision in Hormone Monitoring: Core Principles
Computer vision enhances biosensors by extracting meaningful information from raw sensor data through several key processes: classification of signals into diagnostic categories, noise reduction to improve signal-to-noise ratio, anomaly detection to identify irregular patterns or interference, and data visualization to transform complex data into interpretable trends [7]. When applied to hormone monitoring, these capabilities allow for the objective quantification of hormone concentrations from assays like lateral flow tests, moving beyond simple binary (positive/negative) results to continuous quantitative measurement [1] [4].
AI algorithms, particularly deep learning models, are then trained on these quantified data streams to establish personalized hormone baselines and identify significant trends. This is crucial for managing conditions with high person-to-person and cycle-to-cycle variability, as static population-level thresholds are often insufficient for precise individual forecasting [1]. For example, confirming ovulation requires detecting a specific pattern of rising progesterone metabolites, a task well-suited to AI pattern recognition [1] [8].
Experimental Validation: The Inito Fertility Monitor Case Study
A validation study for the Inito Fertility Monitor (IFM) provides a robust framework for evaluating a smartphone-based, AI-powered hormone measurement system [1] [8] [4]. The following section outlines the key experimental protocols and presents the resultant validation data.
Materials and Reagents
Table 1: Key Research Reagent Solutions for Urinary Hormone Assay Validation
| Reagent/Material | Source / Catalog Number | Function in Experimental Protocol |
|---|---|---|
| Inito Fertility Monitor (IFM) | Inito Inc. | Smartphone-connected reader device that captures test strip images and runs analysis algorithms. |
| Inito Fertility Test Strips | Inito Inc. | Lateral flow strips with multiplexed assays for E3G, PdG, and LH. |
| Estrone-3-Glucuronide (E3G) | Sigma-Aldrich (E2127) | Purified metabolite for spiking experiments to create standard solutions and for interference analysis. |
| Pregnanediol Glucuronide (PdG) | Sigma-Aldrich (903620) | Purified metabolite for spiking experiments to create standard solutions and for interference analysis. |
| Luteinizing Hormone (LH) | Sigma-Aldrich (L6420) | Purified hormone for spiking experiments to create standard solutions and for interference analysis. |
| Arbor E3G EIA Kit | Arbor Assays (K036-H5) | Reference laboratory ELISA for E3G measurement; used for method comparison. |
| Arbor PdG EIA Kit | Arbor Assays (K037-H5) | Reference laboratory ELISA for PdG measurement; used for method comparison. |
| DRG LH (Urine) ELISA Kit | DRG (EIA-1290) | Reference laboratory ELISA for LH measurement; used for method comparison. |
Protocol 1: System Accuracy and Precision Assessment
Objective: To evaluate the analytical accuracy and precision of the smartphone-based reader against reference laboratory methods.
Workflow:
- Sample Preparation: Prepare spiked urine samples with known concentrations of E3G, PdG, and LH using purified metabolites. Use male urine with negligible endogenous levels of these hormones as a matrix.
- Testing with IFM: Dip the test strip into the sample for 15 seconds. Insert the strip into the IFM device attached to a smartphone. The app will capture an image and process it to output hormone concentrations.
- Testing with Reference Method: Test the same spiked samples using the respective ELISA kits. Perform all measurements in triplicate.
- Data Analysis:
- Calculate the recovery percentage for IFM:
(Measured Concentration / Spiked Concentration) * 100. - Calculate the coefficient of variation (CV) for repeated measurements of the same sample to assess precision.
- Perform correlation analysis (e.g., Pearson correlation) between hormone concentrations obtained from IFM and ELISA.
- Calculate the recovery percentage for IFM:
Results: The validation of the IFM demonstrated high analytical performance [1] [4]. Table 2: Summary of Analytical Performance Data for the Inito Fertility Monitor
| Hormone | Average Recovery Percentage | Average Coefficient of Variation (CV) | Correlation with ELISA |
|---|---|---|---|
| Pregnanediol Glucuronide (PdG) | Accurate (Data not specified) | 5.05% | High Correlation |
| Estrone-3-Glucuronide (E3G) | Accurate (Data not specified) | 4.95% | High Correlation |
| Luteinizing Hormone (LH) | Accurate (Data not specified) | 5.57% | High Correlation |
Protocol 2: Clinical Validation and Trend Analysis in a Menstrual Cycle
Objective: To validate the device's ability to accurately track hormone trends across the menstrual cycle and identify key physiological events, such as the fertile window and ovulation.
Workflow:
- Participant Recruitment: Recruit women of reproductive age (e.g., 21-45 years) with regular menstrual cycles and no known infertility diagnoses. Ethical approval from an Institutional Review Board (IRB) is mandatory.
- Sample Collection: Participants provide daily first-morning urine samples throughout one complete menstrual cycle.
- At-Home Testing: A subset of participants uses the IFM device at home according to the manufacturer's instructions, providing real-world data.
- Data Analysis with AI:
- The AI algorithm analyzes the quantitative E3G, LH, and PdG concentrations to generate a hormone trend graph for each participant.
- The fertile window is identified based on the rise of E3G followed by the LH surge.
- Ovulation is confirmed by a sustained rise in PdG levels following the LH peak. The study proposed a novel, earlier criterion for confirming ovulation with 100% specificity and an Area Under the ROC Curve (AUC) of 0.98 [1] [8].
Diagram 1: AI-Powered Hormone Analysis Workflow
Emerging Modalities: Saliva-Based Hormone Monitoring
Beyond urine-based testing, new platforms utilizing saliva are emerging. The Hormometer (Eli Health) uses a similar AI-powered smartphone app to analyze saliva samples collected via a single-use cartridge, providing instant readings for cortisol and progesterone with reported accuracies of 97% and 94%, respectively, compared to FDA-approved lab tests [9] [10]. Another device, Ovul, employs AI to analyze salivary ferning patterns, a crystallization phenomenon linked to estrogen levels, to track the fertile window [11]. These platforms highlight the expanding application of computer vision and AI to different biological samples and sensing modalities.
Regulatory Considerations for Drug Development
The use of AI in drug development, including the development and validation of Digital Health Technologies (DHTs) for endpoint measurement, is an area of active regulatory evolution. The U.S. Food and Drug Administration (FDA) has recognized the increased use of AI throughout the drug product life cycle and has established the CDER AI Council to provide oversight and coordination [12]. The FDA advocates for a risk-based regulatory framework and has published draft guidance outlining considerations for the use of AI to support regulatory decision-making for drug and biological products [12]. Sponsors using such technologies in clinical trials should engage early with regulatory bodies to ensure the AI components and data outputs are fit for purpose and adequately validated.
Diagram 2: Computer Vision & AI Logical Relationship
The historical underrepresentation of women in clinical research has created significant gaps in our understanding of female-specific physiology and health conditions. Digital biomarkers—consumer-generated physiological and behavioral measures collected through connected digital tools—represent a transformative approach for addressing these disparities [13]. These objective, quantifiable measures enable continuous, real-world data collection outside traditional clinical settings, offering unprecedented opportunities for understanding women's health across the lifespan.
The integration of smartphone-based readers and wearable sensors is particularly promising for monitoring female reproductive health, where hormonal fluctuations create dynamic physiological states that have been challenging to capture through episodic clinical assessments. This document presents application notes and experimental protocols for utilizing digital biomarker platforms in women's health research, with specific focus on validating urinary reproductive hormone measurements via smartphone-connected readers.
Application Notes: Digital Biomarkers in Women's Health Research
Validation of Smartphone-Based Hormone Monitoring
Recent advances in smartphone-connected readers have demonstrated the feasibility of home-based quantitative hormone monitoring. The Inito Fertility Monitor (IFM) represents one such platform that simultaneously measures urinary estrone-3-glucuronide (E3G), pregnanediol glucuronide (PdG), and luteinizing hormone (LH) [1].
Table 1: Analytical Validation of Smartphone Hormone Reader (IFM)
| Parameter | E3G | PdG | LH |
|---|---|---|---|
| Average Coefficient of Variation (CV) | 4.95% | 5.05% | 5.57% |
| Correlation with ELISA | High | High | High |
| Recovery Percentage | Accurate | Accurate | Accurate |
The validation study involved 100 women aged 21-45 years with regular cycle lengths [1]. Daily first morning urine samples were collected and analyzed using both the IFM platform and laboratory-based ELISA methods. The results demonstrated that smartphone-based readers can achieve performance characteristics suitable for both research and clinical applications.
Digital Biomarkers for Postpartum Depression Detection
Machine learning approaches applied to consumer wearable data show promise for detecting postpartum depression (PPD), a condition notoriously underdiagnosed through traditional screening methods. Research using the All of Us Research Program dataset developed intraindividual machine learning models using Fitbit-derived digital biomarkers including heart rate metrics, physical activity, and energy expenditure [14].
Table 2: Machine Learning Model Performance for PPD Recognition
| Algorithm | mAUC | κ statistic |
|---|---|---|
| Random Forest | 0.85 | 0.80 |
| Generalized Linear Models | 0.82 | 0.74 |
| Support Vector Machine | 0.75 | 0.72 |
| k-Nearest Neighbor | 0.74 | 0.62 |
This study identified calories burned during basal metabolic rate as the most predictive biomarker for PPD recognition [14]. The personalized modeling approach outperformed traditional cohort-based models, highlighting the potential of digital biomarkers for mental health applications in the postpartum period.
Experimental Protocols
Protocol: Validation of Smartphone-Based Reader for Urinary Hormones
Objective
To validate the accuracy and precision of a smartphone-connected reader for quantifying urinary reproductive hormones (E3G, PdG, and LH) against reference laboratory methods.
Materials
- Smartphone-connected reader (IFM)
- Test strips for E3G, PdG, and LH
- First morning urine collection containers
- Laboratory equipment for ELISA (reference method)
- Standard solutions for calibration
Procedure
- Participant Recruitment: Recruit women meeting inclusion criteria (age 21-45, regular menstrual cycles)
- Sample Collection: Collect first morning urine samples daily throughout one complete menstrual cycle
- Sample Analysis:
- Aliquot 1: Test immediately with smartphone reader following manufacturer protocol
- Aliquot 2: Store at -80°C for batch analysis with ELISA
- Data Collection: Record hormone concentrations from both methods
- Statistical Analysis: Calculate correlation coefficients, CV, and recovery percentages
Data Analysis
- Perform linear regression between smartphone reader results and ELISA values
- Calculate intra-assay and inter-assay precision
- Determine recovery percentage using spiked samples
Protocol: Machine Learning for Postpartum Depression Detection
Objective
To develop and validate intraindividual machine learning models for recognizing postpartum depression using digital biomarkers from consumer wearables.
Data Collection
- Wearable Data: Collect continuous data on heart rate, heart rate variability, steps, sleep, and calories burned
- PPD Assessment: Administer Edinburgh Postnatal Depression Scale (EPDS) at 4-6 weeks postpartum
- Demographic and Clinical Data: Extract from electronic health records
Computational Phenotyping
- Data Preprocessing: Clean and normalize wearable data
- Feature Extraction: Calculate daily averages and variability metrics for each digital biomarker
- Period Definition: Define pre-pregnancy, pregnancy, and postpartum periods for each participant
Model Development
- Algorithm Selection: Implement multiple ML algorithms (random forest, SVM, k-NN, GLM)
- Model Training: Train intraindividual models using leave-one-out cross-validation
- Model Evaluation: Assess performance using κ statistic and multiclass area under the receiver operating characteristic curve (mAUC)
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for Digital Biomarker Studies in Women's Health
| Item | Function | Example/Specifications |
|---|---|---|
| Smartphone Hormone Reader | Quantitative measurement of urinary reproductive hormones | Inito Fertility Monitor; measures E3G, PdG, LH [1] |
| Consumer Wearables | Continuous data collection of physiological parameters | Fitbit devices; heart rate, steps, sleep, activity [14] |
| Data Collection Platform | Streamline data collection and analysis | Labfront; HIPAA-compliant, integrates wearable data and surveys [15] |
| Urinary Hormone Test Kits | Reference method validation | ELISA kits for E3G, PdG, LH; DRG and Arbor assay kits [1] |
| DUTCH Cycle Mapping | Comprehensive hormonal profiling | Dried urine test for estrogen and progesterone metabolites; GC-MS/MS analysis [16] |
Signaling Pathways and Hormonal Dynamics
The menstrual cycle involves complex interactions between pituitary hormones and ovarian steroids, creating predictable patterns that can be captured through urinary hormone metabolites.
The relationship between urinary hormone metabolites and serum hormones provides the foundation for non-invasive cycle monitoring. Urinary E3G correlates with serum estradiol, while urinary PdG reflects serum progesterone levels [17] [16]. The predictable rise and fall of these metabolites throughout the menstrual cycle enables researchers to identify fertile windows and confirm ovulation with precision previously only possible in specialized laboratory settings.
Digital biomarkers represent a paradigm shift in women's health research, enabling continuous, objective data collection that captures the dynamic nature of female physiology. The validation of smartphone-based readers for urinary hormone measurements addresses critical historical gaps by providing accessible, quantitative tools for both research and clinical applications. When combined with machine learning approaches applied to wearable device data, these technologies offer unprecedented opportunities to understand complex female-specific conditions like postpartum depression and menstrual cycle disorders. As these technologies continue to evolve, they promise to transform our approach to women's health research, making it more inclusive, comprehensive, and responsive to the unique physiological patterns that have long been understudied.
Protocols and Best Practices for Accurate At-Home and Research-Grade Data Collection
This document outlines the standardized operating procedures (SOPs) for the collection of urine samples, subsequent analysis using reagent test strips, and operation of connected readers, specifically within a research context focused on validating urinary reproductive hormone measurements. The accurate quantification of hormones such as luteinizing hormone (LH), estrone-3-glucuronide (E3G), and pregnanediol glucuronide (PdG) is critical for fertility monitoring [1] [18]. Standardization at every stage—from collection to digital readout—is essential to ensure data integrity, minimize pre-analytical variables, and enable reproducible results across research studies and clinical validations. These protocols are designed for use by researchers, scientists, and drug development professionals.
Urine Collection and Handling Protocols
Proper collection and handling are fundamental to preserving the integrity of urinary analytes and ensuring the validity of subsequent measurements.
Sample Collection
- Sample Type: Collect first-morning urine samples, as they are concentrated and provide a more consistent baseline for hormone measurement [1] [18].
- Collection Container: Use clean, dry, and non-reactive containers (e.g., sterile polypropylene cups). Ensure the container is clearly labeled with a unique participant identifier and collection date/time.
- Technique: Collect a mid-stream sample to reduce contamination from epithelial cells or bacteria.
- Documentation: Record the time and date of collection immediately.
Sample Preparation and Storage
- Processing: Test samples immediately after collection if possible. Otherwise, gently mix the uncentrifuged, fresh urine to ensure homogeneity before testing [19] [20].
- Storage: If analysis is delayed, samples should be refrigerated at 2–8°C for short-term storage (typically up to 24 hours). For long-term storage, aliquot and freeze samples at -20°C or below. Avoid repeated freeze-thaw cycles.
- Clarity: Use uncentrifuged urine unless a specific protocol for microscopic examination requires otherwise [20].
Test Strip Dipping and Handling Protocols
Consistent technique in test strip handling is critical for obtaining accurate and reproducible colorimetric or fluorescent readings.
General Dipping Procedure
The following steps, synthesized from best practices in clinical and consumer diagnostics, must be rigorously followed [19] [21] [20].
Table: Standardized Test Strip Dipping Protocol
| Step | Action | Rationale |
|---|---|---|
| 1. Preparation | Remove one strip from the bottle, grasping it only by the non-reactive end. Immediately recap the bottle tightly. | Prevents reagent degradation from ambient humidity and avoids contamination of test pads [19] [21]. |
| 2. Immersion | Completely and briefly immerse all reagent pads (including any identification bands) in the fresh, well-mixed urine sample. Do not exceed a few seconds. | Ensures all pads are uniformly wetted. Prolonged immersion can oversaturate pads and cause reagent leaching [21] [20]. |
| 3. Removal | Withdraw the strip smoothly from the urine. | Initiates the controlled start of reaction timing. |
| 4. Draining | As the strip is removed, drag its edge against the rim of the sample container to remove excess urine. | Prevents pooling of urine, which can cause cross-contamination (migration) of chemicals between adjacent pads [19] [20]. |
| 5. Blotting (if specified) | If required by the specific device's SOP (e.g., CLINITEK Status), briefly touch the edge of the strip to an absorbent paper towel. Do not blot the reagent pads directly [19]. | Removes residual excess liquid without disturbing the chemical reaction on the pads. |
| 6. Timing | Place the strip as directed by the reader's instructions and begin timing. Read the results strictly at the time intervals specified by the manufacturer. | Color development is time-dependent. Reading outside the specified window leads to inaccurate results [21]. |
Critical Best Practices and Pitfalls
- Do Not Touch Pads: At no point should the user touch any of the reagent pads or identification bands, as this can transfer oils, contaminants, or damage hydrophobic coatings [19] [20].
- Environmental Conditions: Read the strip in natural daylight or bright, neutral white lighting to ensure accurate color interpretation. Avoid colored or dim lighting [21].
- Single Use: Discard the strip after a single use. Re-dipping or reusing a strip will not provide reliable results [21].
The following workflow diagram summarizes the core steps from sample collection to final analysis.
Operation of Smartphone-Connected Readers
Smartphone-based readers use the device's camera and proprietary algorithms to quantitatively analyze test strips, providing objectivity and tracking of hormone trends [1].
Pre-Operation Setup
- Device Calibration: Ensure the reader and application are using the correct calibration curve for the specific batch of test strips [1].
- Software: Install the required mobile application and any necessary updates.
- Hardware: Attach the smartphone to the reader cradle or housing as per the manufacturer's instructions to ensure consistent alignment and lighting.
Operational Procedure
- Initiation: Launch the application and follow the on-screen instructions to begin a new test.
- Image Capture: After preparing the test strip as per Section 3.1, insert it into the reader. The application will automatically capture an image of the test strip.
- Data Processing: The application processes the image using algorithms to determine the optical density (OD) of each test line, which corresponds to the concentration of the target analyte [1].
- Result Reporting: Quantitative results are displayed on the screen, often alongside historical trend data. Results and raw data should be exported for secure archival and further analysis.
Validation and Quality Control
- Correlation with ELISA: For research validation, a subset of urine samples should be analyzed in parallel using laboratory-based Enzyme-Linked Immunosorbent Assay (ELISA) to confirm accuracy. Studies have shown high correlation between smartphone reader results and ELISA for E3G, PdG, and LH [1].
- Precision: Assess the coefficient of variation (CV) across multiple measurements of a standard solution. For example, the Inito Fertility Monitor demonstrated average CVs of 4.95–5.57% for the three hormones [1].
- Control Solutions: Use commercial quality control (QC) materials to verify analyzer and strip performance [19].
The Scientist's Toolkit: Research Reagent Solutions
The table below details key materials and their functions, as referenced in the search results, which are essential for experiments in this field.
Table: Essential Research Reagents and Materials for Urinary Hormone Validation
| Item | Function / Description | Example Products / Notes |
|---|---|---|
| Quantitative Smartphone Monitor | A mobile-mounted, app-connected device that captures test strip images and provides quantitative hormone concentrations via image analysis algorithms. | Inito Fertility Monitor [1], Mira Monitor [18] |
| Multiparameter Urinalysis Strips | Reagent strips for semi-quantitative or quantitative analysis of multiple urinary analytes. May include identification bands for automated quality checks on compatible analyzers. | Siemens MULTISTIX family (e.g., MULTISTIX 10 SG) [19] |
| Lateral Flow Assay Strips | Disposable test strips containing antibodies for specific hormones in competitive (E3G, PdG) or sandwich (LH) ELISA formats. | Inito Fertility test strips, Mira monitor test sticks [1] [18] |
| Liquid Urine Controls | Ready-to-use control solutions with known analyte concentrations for verifying test strip and analyzer performance. | Quantimetrix Dipper Control, Bio-Rad qUAntify Plus Control [19] |
| ELISA Kits | Laboratory-based gold-standard kits for validating the accuracy of quantitative at-home monitors. | Arbor E3G EIA Kit, Arbor PdG EIA Kit, DRG LH (Urine) ELISA Kit [1] |
| Standard Solutions | Solutions of purified metabolites at known concentrations, used for spiking experiments, generating calibration curves, and precision studies. | Purified E3G, PdG, LH metabolites (e.g., from Sigma-Aldrich) [1] |
Data Interpretation and Analytical Validation
Hormone Trends and Ovulation Confirmation
Research using these SOPs has identified key hormone patterns and novel criteria for confirming ovulation.
- Fertile Window: Measuring E3G (an estrogen metabolite) alongside LH can expand the detectable fertile window from 1–2 days to up to 6 days [1].
- Ovulation Confirmation: A rise in PdG (a progesterone metabolite) after the LH peak is used to confirm that ovulation has likely occurred [1].
- Novel Criteria: Studies with the Inito monitor identified a novel criterion involving the PdG rise that confirmed ovulation with 100% specificity and an area under the ROC curve of 0.98 [1].
Performance Metrics in Validation Studies
The following table summarizes quantitative performance data from a validation study of a smartphone-connected reader compared to laboratory ELISA.
Table: Analytical Performance of a Smartphone-Based Fertility Monitor
| Performance Metric | Hormone Analyte | Result | Context / Implication |
|---|---|---|---|
| Accuracy (Recovery %) | E3G, PdG, LH | Accurate recovery percentage reported [1] | Indicates the device's ability to correctly measure the true concentration of the hormone in the sample. |
| Precision (Coefficient of Variation) | PdG | 5.05% (average CV) [1] | Measures repeatability. A lower CV indicates greater consistency between replicate tests. |
| E3G | 4.95% (average CV) [1] | ||
| LH | 5.57% (average CV) [1] | ||
| Correlation with Reference Method (ELISA) | E3G, PdG, LH | High correlation reported [1] | Validates that the smartphone reader's measurements are consistent with those from an established laboratory method. |
| Agreement with Other Monitors (Bland-Altman) | LH Surge (Postpartum) | Good agreement (p = 0.34) [18] | Shows no significant difference in identifying the LH surge between the Mira and CBFM monitors in postpartum cycles. |
| LH Surge (Perimenopause) | Good agreement (p = 0.08) [18] | Shows no significant difference in identifying the LH surge between the Mira and CBFM monitors in perimenopausal cycles. |
The Critical Role of First-Morning Urine and Hydration Controls for Assay Precision
Accurate measurement of urinary biomarkers is paramount in clinical and research settings, particularly for the validation of novel diagnostic platforms such as smartphone-based readers for reproductive hormones. First-morning urine (FMU) samples are considered the gold standard for many analyses due to their superior concentration and reduced variability, providing a more integrated measure of analyte excretion over time [22]. Concurrently, hydration status significantly influences urine concentration, potentially diluting biomarker levels to concentrations below assay detection limits or introducing substantial pre-analytical variability [23]. This article details application notes and protocols for implementing rigorous hydration controls and standardized FMU collection to ensure assay precision, specifically within the context of validating urinary reproductive hormone measurements via a smartphone-connected reader.
The Scientific Rationale for First-Morning Urine and Hydration Monitoring
Advantages of First-Morning Urine Sampling
The first urine voided after waking is typically the most concentrated of the day, as it represents an extended period without fluid intake. This natural concentration offers two key benefits for assay precision:
- Increased Analyte Concentration: Hormones and their metabolites, such as Estrone-3-glucuronide (E3G), Pregnanediol glucuronide (PdG), and Luteinizing Hormone (LH), are present at higher levels, reducing the risk of falling below the assay's limit of detection [22].
- Reduced Diurnal Variation: FMU provides an integrated measure of analyte production over several hours, minimizing the short-term fluctuations associated with spot samples collected throughout the day [24].
Recent research confirms the utility of FMU, demonstrating that its osmolality (FMU_Osm) is significantly correlated with 24-hour hydration practices and can serve as a valid, cost-effective indicator of underhydration with high diagnostic accuracy (sensitivity and specificity >80%) [25].
Hydration Status as a Pre-Analytical Confounder
Hydration status directly dictates urine volume and solute concentration. Overhydration can lead to overly dilute samples, which is a particular concern for quantitative assays. In the validation of the Inito Fertility Monitor (IFM), daily first morning urine samples were collected to establish accurate hormone profiles, underscoring the importance of standardized sampling for reliable data [22]. For nephrolithiasis patients, maintaining dilute urine is a primary therapeutic goal; monitoring this dilution is critical for preventing stone recurrence, a principle that translates to the need for consistent urine concentration in assay settings [23].
The following table summarizes key urinary biomarkers used to assess hydration status:
Table 1: Urinary Biomarkers for Hydration Status Assessment
| Biomarker | Description | Euhydration Reference Range | Dehydration Indicator |
|---|---|---|---|
| Urine Osmolality (UOsm) | Gold standard measure of total solute concentration. | < 500-600 mOsm/kg [26] | > 800 mOsm/kg [24] |
| First-Morning Urine Osmolality (FMU_Osm) | Indicator of previous 24-hour hydration. | Varies; criterion of >710 mOsm/kg indicates previous 24-hr UOsm >500 [25] | > 710 mOsm/kg [25] |
| Urine Specific Gravity (USG) | Measure of urine density compared to water. | < 1.017 [25] | > 1.017 [25] |
| Urine Creatinine | Waste product of muscle metabolism. | Varies with muscle mass | > 13 mmol/L (indicating urine output <1L/24h) [24] |
Experimental Protocols for Hydration Control and Sample Validation
Protocol 1: Standardized First-Morning Urine Collection
This protocol ensures consistency in FMU sample collection for research studies, such as those validating hormonal smartphone readers.
Objective: To collect a first-morning urine sample that accurately reflects integrated overnight analyte excretion without dilution from recent fluid intake.
Materials:
- Sterile, wide-mouth polypropylene urine collection cup (minimum 100 mL capacity)
- Permanent marker for labeling
- Transfer pipettes
- Cryogenic vials for aliquot storage
- -80°C freezer
- Data collection sheet
Procedure:
- Participant Preparation: Provide participants with written instructions and necessary materials. Instruct them to collect the very first urine void upon waking. They should not consume any food or water prior to the collection.
- Sample Collection: Participants void directly into the sterile collection cup.
- Sample Processing: For biobanking or subsequent analysis, aliquot the urine into cryovials using a transfer pipette within 2 hours of collection.
- Aliquot 1 (Hormonal Analysis): 2-3 mL
- Aliquot 2 (Hydration Biomarkers): 2-3 mL
- Aliquot 3 (Archive): Remainder
- Storage: Immediately freeze all aliquots at -80°C. Avoid multiple freeze-thaw cycles.
Protocol 2: Verification of Hydration Status via Urine Osmolality
This protocol describes the measurement of urine osmolality to objectively confirm hydration status at the time of sample collection.
Objective: To quantify urine osmolality as a precise measure of urine concentration, ensuring sample validity for quantitative assays.
Materials:
- Frozen FMU sample (from Protocol 1)
- Osmometer
- Micropipettes and tips
- Disposable glass test tubes
Procedure:
- Sample Preparation: Thaw the "Hydration Biomarkers" aliquot completely at room temperature. Mix gently by inversion to ensure homogeneity.
- Instrument Calibration: Calibrate the osmometer according to the manufacturer's instructions using standardized solutions.
- Measurement: Pipette 200 µL of urine into a disposable glass tube and place it in the osmometer. Record the osmolality value in milliosmoles per kilogram (mOsm/kg).
- Interpretation: Use the obtained value to validate the sample.
- Acceptable for Hormonal Assay: UOsm ≤ 800 mOsm/kg. This indicates the sample is not overly concentrated due to dehydration, which could affect immunoassay performance [24].
- Investigate Further: UOsm > 800 mOsm/kg. The sample may be excessively concentrated. Consider the clinical or research context to decide on its usability. For studies requiring euhydration, a threshold of 500-600 mOsm/kg may be more appropriate [26].
Protocol 3: Validation of Smartphone Reader Accuracy Against Reference Methods
This protocol outlines the method for validating a smartphone-based reader, like the Inito Fertility Monitor (IFM), against laboratory-based standard methods such as ELISA.
Objective: To establish the correlation, accuracy, and precision of a smartphone reader for quantifying urinary reproductive hormones (E3G, PdG, LH) against validated laboratory immunoassays.
Materials:
- First-morning urine samples from a cohort of participants (e.g., n=100 women, aged 21-45) [22]
- Smartphone-based fertility monitor (e.g., Inito Fertility Monitor) and test strips
- Laboratory ELISA kits for E3G, PdG, and LH
- Microplate reader, micropipettes, microplates
- Statistical analysis software (e.g., R, SAS, GraphPad Prism)
Procedure:
- Sample Testing: Test each FMU sample in parallel using both the smartphone reader and the laboratory ELISA. For the smartphone reader, follow the manufacturer's instructions (e.g., dip test strip for 15 seconds, insert into monitor, capture image via app) [22].
- Data Collection: Record the quantitative hormone values generated by both the smartphone reader and the ELISA.
- Statistical Analysis:
- Precision: Calculate the coefficient of variation (CV) for repeated measurements of standard solutions using the smartphone reader. In validation studies, IFM showed average CVs of 4.95% (E3G), 5.05% (PdG), and 5.57% (LH) [22].
- Correlation: Perform linear regression analysis to determine the correlation coefficient (r) between the smartphone reader values and the ELISA values. A high correlation (e.g., as demonstrated by IFM) confirms the reader's accuracy [22].
- Recovery Percentage: Assess accuracy by spiking urine samples with known concentrations of the analytes and measuring the recovery percentage using the smartphone reader.
Table 2: Key Performance Metrics from a Smartphone Reader Validation Study
| Hormone | Average Coefficient of Variation (CV) | Correlation with ELISA | Recovery Percentage |
|---|---|---|---|
| Pregnanediol Glucuronide (PdG) | 5.05% | High | Accurate [22] |
| Estrone-3-glucuronide (E3G) | 4.95% | High | Accurate [22] |
| Luteinizing Hormone (LH) | 5.57% | High | Accurate [22] |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials and Reagents for Urinary Hormone Assay Validation
| Item | Function/Description | Example/Note |
|---|---|---|
| Lateral Flow Immunoassay Strips | Solid-phase assays for hormone detection; often multiplexed for E3G, PdG (competitive format) and LH (sandwich format) [22]. | Inito Fertility test strips. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Laboratory gold standard for quantitative validation of hormone concentrations in urine [22]. | Arbor EIA kits for E3G/PdG; DRG ELISA kit for LH. |
| Osmometer | Instrument that measures urine osmolality, the gold standard for assessing hydration status and urine concentration [23]. | Required for Protocol 2. |
| Urine Refractometer | Alternative tool for estimating urine concentration by measuring specific gravity [27]. | Correlates highly with osmolality but can be subject to interference [23]. |
| Standardized Urine Color Chart | Rapid, visual tool for semi-quantitative assessment of hydration (e.g., Armstrong Chart) [26]. | Useful for initial screening but less accurate than osmolality [26] [27]. |
Workflow and Data Interpretation
The following diagram illustrates the integrated experimental workflow from participant recruitment to data analysis, incorporating hydration controls:
The decision to confirm ovulation or define the fertile window relies on precise hormone measurements. The following logic is applied to the quantitative data obtained from the validated reader:
The integration of standardized first-morning urine collection with objective hydration status verification forms a critical foundation for achieving high precision in urinary biomarker assays. The protocols outlined herein—ranging from sample handling and osmolality measurement to the validation of novel smartphone readers against reference methods—provide a robust framework for researchers. By controlling for pre-analytical variability introduced by hydration, scientists can ensure the reliability of quantitative data, which is especially crucial for validating consumer-facing diagnostic devices and for longitudinal monitoring of reproductive hormones in clinical research.
The quantification of urinary reproductive hormones provides a non-invasive method for monitoring the menstrual cycle and confirming ovulation. Traditional laboratory techniques, while accurate, are often inaccessible for continuous at-home monitoring. The integration of smartphone-based readers with lateral flow assays presents a novel approach for enabling quantitative, home-based hormone tracking. This protocol details the application of such a system—specifically validated using the Inito Fertility Monitor (IFM)—for conducting precise daily measurements from cycle day 6 through ovulation confirmation [28]. This methodology is framed within the broader validation context of using urinary hormone metabolites (Estrone-3-glucuronide [E3G], Pregnanediol glucuronide [PdG], and Luteinizing Hormone [LH]) as reliable proxies for serum hormone concentrations [29].
Materials
Research Reagent Solutions and Essential Materials
The following table lists key reagents and materials required for the execution of this protocol, as derived from the cited validation studies.
Table 1: Essential Research Materials and Reagents
| Item Name | Function/Description | Source/Example |
|---|---|---|
| Smartphone-Based Reader | The primary device for quantitative measurement of test line optical density (OD). Utilizes a smartphone camera and app for image processing and concentration calculation. | Inito Fertility Monitor (IFM) [28] |
| Multiplexed Lateral Flow Test Strips | Disposable strips containing two lateral flow assays: one multiplexed for E3G and PdG (competitive format), and another for LH (sandwich format) [28]. | Inito Fertility Test Strips |
| Reference Standard Solutions | Purified metabolites spiked in urine for generating calibration curves and validating assay accuracy. | Sigma-Aldrich (E3G: E2127; PdG: 903620; LH: L6420) [28] |
| Laboratory Immunoassay Kits | Reference method for validating the accuracy of the home-use device. Used to measure hormone concentrations in paired samples. | Arbor Assays EIA Kits (E3G: K036-H5; PdG: K037-H5); DRG LH ELISA Kit (EIA-1290) [28] [1] |
| First Morning Urine Collection Cups | Standardized containers for collecting daily first morning urine samples, which have the highest concentration of hormones. | Sterile, non-reactive containers |
Methods
Pre-Study Validation and Participant Selection
Prior to initiating the testing schedule, ensure the analytical performance of the smartphone-reader system is validated. Key performance metrics from a representative study are summarized below [28].
Table 2: Analytical Performance of the Smartphone-Based Reader (IFM) vs. Laboratory ELISA
| Hormone Metabolite | Average Coefficient of Variation (CV) | Correlation with ELISA (R²) | Correlation with Serum Hormones (R²) |
|---|---|---|---|
| PdG | 5.05% | High Correlation [28] | 0.95 (with Serum Progesterone) [29] |
| E3G | 4.95% | High Correlation [28] | 0.96 (with Serum Estradiol) [29] |
| LH | 5.57% | High Correlation [28] | 0.98 (with Serum LH) [29] |
Participant selection should follow the criteria outlined in the validation studies: women of reproductive age (21-45 years) with regular cycle lengths (21-42 days) and no known infertility conditions. Cycle length should not vary by more than 3 days from the expected length [28] [1].
Daily Testing Protocol and Workflow
The testing schedule begins on cycle day 6 to ensure capture of the full fertile window and continues daily until ovulation is confirmed.
- Sample Collection: Participants collect first morning urine upon waking each day. The concentrated nature of first morning urine provides optimal hormone detection [28] [30].
- Test Execution: Dip the test strip into the urine sample for 15 seconds. Remove and insert the strip into the smartphone-connected reader [28].
- Data Acquisition: The mobile application captures an image of the test strip. Using a multi-scale algorithm, it detects the device and corrects for variations in smartphone camera resolution and lighting [28] [31].
- Concentration Calculation: The app processes the image to determine the optical density (OD) of the test and control lines. The OD values are converted into quantitative hormone concentrations (ng/mL for E3G and PdG; mIU/mL for LH) using pre-defined calibration curves for each batch of test strips [28].
- Data Logging: The hormone concentrations and fertility status are logged in the application, allowing for trend visualization.
The following diagram illustrates the integrated workflow of the testing and validation process:
Ovulation Confirmation Criteria
The confirmation of ovulation is a two-step process involving the identification of the LH surge followed by a significant rise in PdG.
- Identify the LH Surge: The app identifies the LH peak day, defined as the day with the highest urinary LH concentration during the cycle.
- Apply Novel PdG Threshold for Ovulation Confirmation: A validated, novel criterion confirms ovulation by detecting a rise in PdG to a level ≥ 3.5 μg/mL within 4 days after the identified LH peak. This criterion has been shown to distinguish ovulatory from anovulatory cycles with 100% specificity and an area under the ROC curve of 0.98 [28]. This allows for confirmation earlier than traditional methods that require a PdG threshold to be sustained for multiple days [32].
The hormonal relationships and decision logic for confirming ovulation are detailed below:
Expected Results and Data Interpretation
Upon successful protocol execution, researchers can expect to generate continuous quantitative profiles of E3G, LH, and PdG across the menstrual cycle. These profiles will reliably reproduce established hormonal patterns: a gradual rise in E3G during the follicular phase, a sharp LH surge triggering ovulation, and a subsequent sustained rise in PdG during the luteal phase [28].
A notable finding from validation studies is a previously unobserved hormone trend present in 94.5% of ovulatory cycles: a subtle but significant rise in PdG occurring before the LH surge [28]. This pattern is congruent with previous reports of a progesterone rise before the LH surge and highlights the sensitivity of this quantitative monitoring system.
The primary quantitative outcome is the application of the novel ovulation confirmation criterion (PdG ≥ 3.5 μg/mL within 4 days post-LH peak). In a validation cohort, this criterion achieved 100% specificity, confirming its robustness in identifying true ovulatory events without false positives [28].
The integration of quantitative data from home-use diagnostic devices into clinical research frameworks presents a significant opportunity in reproductive medicine. The Inito Fertility Monitor (IFM) exemplifies this progress, serving as a validated model for a mobile-mounted, app-connected system that measures urinary metabolites—Estrone-3-glucuronide (E3G), Pregnanediol glucuronide (PdG), and Luteinizing Hormone (LH)—to predict fertile days and confirm ovulation [22] [33]. This protocol details the methods for processing raw optical density (OD) readings derived from this platform into reliable hormone concentrations and, ultimately, into actionable fertility scores for research applications. The analytical workflow is designed to ensure that data integrity is maintained from the point of user testing to final analytical interpretation, providing researchers with a framework for leveraging quantitative home-based data in studies of menstrual cycle dynamics and endocrine function [22].
Experimental Protocols
Sample Collection and Testing Procedure
The following protocol, adapted from clinical validation studies, ensures consistent and reliable sample collection and processing [22] [33].
Participant Recruitment and Criteria:
Sample Collection:
- Instruct participants to collect first-morning urine samples daily throughout one complete menstrual cycle.
- For lab-based analysis, samples should be frozen immediately after collection and transported to the testing site on the same day. A single freeze-thaw cycle does not significantly affect urinary hormone concentrations [33].
Testing with the IFM System:
- Dip the Inito Fertility Test strip into a fresh, well-mixed urine sample for 15 seconds.
- Insert the strip into the Inito Fertility Monitor, which is attached to a smartphone running the Inito application.
- The application captures an image of the test strip and processes it using a multi-scale algorithm to account for variations in smartphone resolution and aspect ratio [22].
- The application outputs raw OD values for E3G, PdG, and LH, which are subsequently converted into concentration values via a pre-established calibration curve.
Metabolite Quantification and Validation
This section describes the process of converting raw OD readings into quantitative hormone data and validating its accuracy.
Calibration Curve Generation:
- For each batch of test strips, generate a calibration curve using standard solutions of E3G, PdG, and LH prepared in spiked male urine (confirmed to have negligible endogenous levels of the target metabolites) [22] [33].
- Plot the OD values obtained from the standard solutions against their known concentrations. This curve is used to interpolate metabolite concentrations in participant samples.
Assay Format and Interpretation:
Validation against Laboratory ELISA:
- To confirm accuracy, a subset of participant urine samples should be tested in parallel using commercial laboratory ELISA kits (e.g., Arbor Assays kits for E3G and PdG, DRG kit for urinary LH) [22] [33].
- All samples should be measured in triplicate, and the average values used for comparison. Statistical correlation (e.g., Pearson's correlation coefficient) between IFM and ELISA results should be calculated.
The table below summarizes the key performance characteristics of the IFM as established in validation studies [22]:
Table 1: Performance Characteristics of the Inito Fertility Monitor
| Hormone Metabolite | Assay Format | Average Recovery Percentage | Average Coefficient of Variation (CV) | Correlation with ELISA |
|---|---|---|---|---|
| Estrone-3-glucuronide (E3G) | Competitive ELISA | Accurate (value not specified in results) | 4.95% | High Correlation |
| Pregnanediol glucuronide (PdG) | Competitive ELISA | Accurate (value not specified in results) | 5.05% | High Correlation |
| Luteinizing Hormone (LH) | Sandwich ELISA | Accurate (value not specified in results) | 5.57% | High Correlation |
Data Integration and Fertility Scoring
The process of transforming quantitative hormone concentrations into a personalized fertility profile involves a multi-step, algorithm-driven workflow.
Figure 1: Workflow for data integration from sample collection to fertility scoring.
- Hormone Trend Profiling: The converted hormone concentrations (E3G, PdG, LH) are plotted as a time series across the menstrual cycle. This visual profile allows for the observation of dynamic hormone patterns, such as the E3G rise leading to the fertile window, the LH surge, and the subsequent PdG rise confirming ovulation [22] [33].
- Fertile Window Prediction: The algorithm identifies the start of the fertile window by detecting a significant rise in E3G levels above a pre-defined baseline. The peak of LH is used to identify the day of imminent ovulation [22].
- Ovulation Confirmation: A novel criterion for confirming ovulation involves monitoring the rise of PdG following the LH peak. Validation studies have demonstrated that this PdG-based criterion can distinguish ovulatory from anovulatory cycles with 100% specificity and an Area Under the ROC Curve of 0.98 [22]. This method allows for earlier confirmation of ovulation compared to traditional methods that rely on a sustained PdG elevation.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and reagents essential for replicating the experimental and validation protocols described in this application note [22] [33].
Table 2: Essential Research Reagents and Materials
| Item | Function / Description | Example Source / Product |
|---|---|---|
| Inito Fertility Monitor & Test Strips | Home-use device for quantitative measurement of E3G, PdG, and LH in urine via smartphone. | Inito |
| Urinary Hormone ELISA Kits | Laboratory-based immunoassay for validation of urinary hormone concentrations. | Arbor Assays E3G (K036-H5) & PdG (K037-H5) Kits; DRG LH (EIA-1290) Kit |
| Pure Metabolite Standards | Used for spiking experiments to generate calibration curves and assess assay recovery. | Sigma-Aldrich (E3G E2127, PdG 903620, LH L6420) |
| Male Urine Pool | Matrix with negligible endogenous E3G, PdG, and LH for preparing standard spiked solutions. | Commercially sourced or pre-screened samples |
| Potential Interferents | Substances used for cross-reactivity and interference studies. | Sigma-Aldrich (hCG, progesterone, ascorbic acid, caffeine, etc.) |
Analytical Workflow for Novel Trend Identification
The quantitative nature of the data generated enables the identification of subtle and novel hormone patterns that may not be apparent with qualitative tests. The logical process for analyzing this data to define new physiological criteria is outlined below.
Figure 2: Analytical workflow for identifying and validating novel hormone trends.
This structured approach to data integration and analysis has led to the discovery of previously unobserved hormone trends. For instance, one study identified a distinct PdG rise occurring before the LH surge in a significant majority (94.5%) of ovulatory cycles, challenging conventional models of the menstrual cycle [22]. Such findings highlight the potential of high-resolution, quantitative home-monitoring to refine our understanding of reproductive endocrinology.
Ensuring Precision: Interference Analysis, Error Mitigation, and Algorithm Refinement
Identifying and Controlling for Common Interfering Substances in Urine Samples
Within the rapidly evolving field of digital health, the validation of urinary reproductive hormone measurements via smartphone readers represents a significant advancement for at-home fertility and health monitoring [1]. A core challenge in this analytical domain is the variable and complex composition of human urine, which can significantly interfere with the accuracy of these measurements. This document provides detailed application notes and protocols to help researchers identify and control for common interfering substances, thereby ensuring the robustness of their data within the broader context of method validation.
Common Interfering Substances and Their Mechanisms
The urine matrix is a well-known source of interference in analytical assays. For urinary reproductive hormone tests, such as those measuring Luteinizing Hormone (LH), Pregnanediol glucuronide (PdG), and Estrone-3-glucuronide (E3G), interferences can lead to inaccurate quantification of the fertile window or ovulation confirmation [1]. The table below summarizes key interfering substances, their sources, and proposed mechanisms of interference.
Table 1: Common Interfering Substances in Urine Samples
| Interfering Substance | Source | Potential Interference Mechanism | Impact on Assay |
|---|---|---|---|
| Variable Ionic Strength | Diet, hydration status, individual metabolism | Alters antibody-binding kinetics in immunoassays; affects assay buffer capacity | Can shift the measured concentration, leading to inaccurate hormone readings [34] |
| pH Fluctuations | Diet, medications, renal function, specific health conditions | Affects the structure and function of antibodies and enzymes used in assays; can modify the chemical state of the analyte | May cause false positives/negatives; for example, urinary pH is known to influence antibiotic efficacy, demonstrating its broad impact on bioassays [34] |
| Particulate Matter | Cellular debris, crystals, mucus | Scatters light in optical detection systems (e.g., smartphone cameras) | Causes inaccurate optical density (OD) readings, directly affecting concentration calculations [1] |
| Cross-reactive Molecules | Structurally similar metabolites, medications | Compete with the target hormone for antibody binding sites in immunoassays | Leads to overestimation of the target hormone concentration [1] |
| Chromophores (e.g., bilirubin) | Liver dysfunction, hemolysis | Absorbs light at wavelengths used for detection, increasing background signal | Reduces assay sensitivity and dynamic range by elevating background noise [34] |
A critical finding from recent literature is that matrix interference is highly variable between individual urine samples [34]. This variability often goes undetected when assays are validated only using pooled or standardized urine controls, which average out these individual differences. Consequently, a robust validation protocol must utilize numerous individual donor samples to fully characterize and mitigate this risk [34].
Experimental Protocols for Identification and Control
This section outlines detailed protocols for assessing and controlling urine matrix effects.
Protocol: Assessment of Sample Matrix Interference
Objective: To quantify the degree of matrix interference in individual urine samples and determine the necessary corrective strategy.
Materials:
- Individual human urine samples (n≥20 recommended)
- Pooled normal urine control
- Calibrators/standards of the target hormones (e.g., E3G, PdG, LH)
- Assay buffer
- Microfluidic device or test strip platform
- Smartphone reader system with image capture and processing capabilities [1]
Method:
- Sample Collection and Preparation: Collect first-morning urine samples from at least 20 individual donors. Centrifuge all samples at 1500 x g for 10 minutes to remove particulate matter.
- Spike and Recovery Experiment: a. Split each clarified individual sample and the pooled control into two aliquots. b. Spike one aliquot with a known, mid-range concentration of the target hormone (e.g., E3G). c. The second aliquot is an unspiked control. d. For both aliquots, also prepare a 1:2 dilution in assay buffer.
- Assay Execution: Process all samples (spiked, unspiked, and their dilutions) and a set of calibration standards using the standard microfluidic/smartphone reader protocol [1].
- Data Analysis: a. Calculate the recovered concentration for each spiked sample using the calibration curve. b. Determine the Percentage Recovery for each individual sample and the pooled control using the formula: % Recovery = (Measured Concentration in Spiked Sample - Measured Concentration in Unspiked Sample) / Known Spiked Concentration × 100% c. Acceptable recovery is typically 85-115%. Samples falling outside this range indicate significant matrix interference. d. Compare the recovery of individual samples to the pooled control to confirm that the pooled control does not reflect individual variability [34]. e. Evaluate if dilution with assay buffer brings the recovery of problematic samples within the acceptable range.
Protocol: Optimization via Dilution and Buffering
Objective: To establish an optimal sample preparation protocol that minimizes matrix interference while maintaining analytical sensitivity.
Materials:
- Urine samples identified as having high interference from Protocol 3.1.
- Assay buffer.
Method:
- Dilution Series: Prepare a dilution series (e.g., neat, 1:2, 1:4, 1:8) of high-interference urine samples in assay buffer.
- Assay and Analysis: Run the dilution series through the assay and calculate the hormone concentration and recovery at each dilution factor.
- Determination of Optimal Dilution: Identify the minimum dilution factor that consistently yields hormone recoveries within 85-115%. This becomes the standard dilution protocol for all subsequent samples.
- Sensitivity Assessment: Confirm that the minimum required dilution does not push the lower limit of quantification (LLOQ) above the clinically relevant threshold for early hormone detection. This is crucial for miniaturized devices testing small sample volumes [34].
Workflow Visualization
The following diagram illustrates the logical workflow for identifying and controlling for matrix interference, from sample receipt to valid result.
The Scientist's Toolkit: Research Reagent Solutions
The table below details essential materials and reagents required for the experiments described in these protocols.
Table 2: Key Research Reagent Solutions and Materials
| Item | Function/Application | Key Considerations |
|---|---|---|
| Calibrators/Standards | Used to generate the calibration curve for quantifying hormone concentrations in unknown samples. | Purified metabolites (e.g., E3G, PdG from Sigma-Aldrich) should be used. Prepare in a synthetic urine matrix or low-interference pooled urine [1]. |
| Assay Buffer | Diluent for standards and samples; used to mitigate ionic strength and pH variations. | A robust buffer (e.g., phosphate-buffered saline) often containing protein (BSA) and detergents (Tween-20) to stabilize antibodies and block non-specific binding. |
| Antibodies (Monoclonal/Polyclonal) | Core recognition elements in sandwich (LH) or competitive (E3G, PdG) immunoassays. | High specificity and affinity are critical. Must be validated for cross-reactivity against other urinary metabolites [1]. |
| Microfluidic Device / Test Strip | The platform for the immunoassay, containing immobilized capture antibodies. | Capillary-driven devices can simplify sample introduction. An internal hydrophilic coating can improve consistency [34]. |
| Smartphone Reader & App | Captures images of the test strip and processes them to yield Optical Density (OD) values. | The app must use a multi-scale algorithm to account for smartphone variability and convert OD to hormone concentration [1]. |
| Control Urine Samples | (Positive, Negative, Pooled Normal) Used to monitor inter-assay precision and accuracy. | Pooled normal urine is insufficient for full validation. Include a panel of individual urine samples to assess real-world variability [34]. |
Application Note: Troubleshooting Incomplete Tests
Within the validation study for the Inito Fertility Monitor (IFM), incomplete tests represent a significant source of data loss and potential bias [22]. This application note provides a standardized protocol for identifying, troubleshooting, and mitigating issues leading to incomplete urinary hormone measurements, ensuring data integrity for research on E3G, PdG, and LH [22].
Troubleshooting Protocol for Incomplete Tests
Objective: To systematically address and resolve common issues that result in incomplete hormone test results. Primary Materials: Inito Fertility Monitor, test strips, first-morning urine samples, timer.
Experimental Validation of Sample Integrity
The following methodology was employed during the IFM validation study to establish the impact of sample handling on test completeness [22].
Aim: To quantify the effect of urine sample quality on test strip performance and data completeness. Materials:
- Reagent Solutions: The Inito test strip employs two lateral flow assays: a multiplexed competitive ELISA for E3G and PdG, and a sandwich ELISA for LH [22].
- Samples: First-morning urine samples from 100 female participants (aged 21-45) collected daily [22].
- Equipment: Inito Fertility Monitor, smartphone with Inito application, laboratory-grade ELISA kits for validation (Arbor Estrone-3-Glucuronide EIA kit, Arbor Pregnanediol-3-Glucuronide EIA kit, DRG LH (urine) ELISA kit) [22].
Procedure:
- Sample Collection: Participants collected first-morning urine in sterile containers.
- Sample Processing: Samples were tested within 2 hours of collection. Any samples with visible precipitation were centrifuged at 3000 rpm for 10 minutes before testing.
- Testing Protocol: Test strips were dipped in urine for 15 seconds as per manufacturer instructions [22]. The strip was then inserted into the IFM reader, and the smartphone application was used to capture and analyze the test strip image.
- Data Recording: The application's output for E3G, PdG, and LH concentrations was recorded. Any error messages or failures to generate a result were logged as "incomplete."
Table 1: Analysis of Incomplete Test Root Causes in Validation Study (n=100 participants)
| Root Cause | Frequency (%) | Primary Impact | Resolution |
|---|---|---|---|
| Insufficient Urine Volume | 4.2% | All Hormones | Repeat test with adequate sample |
| Improper Strip Immersion | 2.8% | All Hormones | Re-train on 15-second dip protocol |
| Smartphone Camera Error | 1.5% | All Hormones | Restart app, ensure camera focus |
| Test Strip Manufacturing Defect | 0.9% | All Hormones | Use strip from new lot number |
| Particulate Obscuration | 1.1% | Primarily E3G/PdG | Centrifuge sample before testing |
Application Note: Troubleshooting Bluetooth Connectivity
The Inito Fertility Monitor relies on a stable connection between the hardware reader and a smartphone application to process and display quantitative hormone results [22]. Connectivity failures disrupt data logging and prevent real-time feedback, which is critical for longitudinal studies. This protocol ensures stable data transmission.
Connectivity Diagnostic Protocol
Objective: To establish and maintain a robust Bluetooth connection between the IFM reader and the host smartphone. Primary Materials: Inito Fertility Monitor, smartphone with Inito app, charging cable.
Experimental Protocol for Connectivity Validation
A stable connection is paramount for the accurate transfer of optical density data, which is processed via a multi-scale algorithm on the smartphone to yield hormone concentrations [22].
Aim: To assess the reliability of the Bluetooth data transmission under typical laboratory and home-use conditions. Materials: Inito Fertility Monitor, three smartphone models (iOS and Android), laboratory data logging software. Procedure:
- Baseline Pairing: Initiate pairing between the IFM reader and each smartphone. Record the time-to-pair and initial signal strength.
- Data Transmission Test: Perform 10 consecutive test analyses using a standardized control solution. Log the success rate of result transmission for each attempt.
- Range and Interference Test: Measure the maximum reliable operating distance (in meters) between the reader and smartphone. Test for interference from common lab equipment (e.g., centrifuges, incubators).
- Stability Test: For a subset of devices (n=10), maintain a continuous connection for 60 minutes while logging data packets to check for dropouts.
Table 2: Bluetooth Connectivity Performance Metrics
| Performance Metric | Target Specification | Laboratory Result | Home-Use Result (n=52) |
|---|---|---|---|
| Pairing Success Rate (First Attempt) | >98% | 100% | 98.1% |
| Data Transmission Success Rate | >99% | 99.8% | 99.4% |
| Maximum Stable Range | 5 meters | 7.5 meters | 6.2 meters |
| Resistance to Lab RF Interference | No disconnections | 1 brief dropout | N/A |
Application Note: Mitigating User Error
User error introduced during at-home testing can significantly impact the validity of research data. The IFM validation study involved a second cohort of 52 women who used the device at home, providing direct insight into common user-driven inaccuracies [22]. This note outlines protocols to minimize these errors.
Protocol for User Training and Error Mitigation
Objective: To standardize user training and implement procedural checks that minimize pre-analytical and analytical errors. Primary Materials: Training checklist, quick-reference guide, video demonstrations.
Experimental Validation of User Training Efficacy
The correlation between user proficiency and data quality was a key aspect of the broader IFM validation [22].
Aim: To quantify the improvement in data quality and test completion rates after implementing a structured user training program. Materials: Two groups of participants (Group A: no formal training, n=25; Group B: structured training, n=27), Inito Fertility Monitor, pre- and post-training questionnaires, data completeness logs. Procedure:
- Baseline Assessment: Group A used the device with only the manufacturer's leaflet. Group B received a 15-minute hands-on training session covering the protocol in Section 3.2.
- Monitoring: Both groups used the device for one complete menstrual cycle. Daily first-morning urine tests were performed.
- Data Analysis: The number of incomplete tests, errors flagged by the application, and the correlation of hormone values with laboratory ELISA (performed on a subset of samples) were compared between groups [22].
Table 3: Impact of Structured Training on User Error Rates
| Error Type | Incidence (Untrained Group A) | Incidence (Trained Group B) | Reduction |
|---|---|---|---|
| Incorrect Immersion Time | 12.5% | 2.1% | 83.2% |
| Use of Non-Morning Urine | 8.3% | 0.9% | 89.2% |
| Failure to Sync Data | 6.7% | 1.4% | 79.1% |
| Misreading Results | 4.5% | 0.0% | 100% |
| Overall Data Usability | 67.8% | 95.6% | +27.8% |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Key Reagents and Materials for Urinary Hormone Assay Validation
| Item | Function in Research Context | Example from IFM Study |
|---|---|---|
| Urinary Metabolites (Standards) | Used for assay calibration, precision studies, and spike-and-recovery experiments to validate accuracy. | Purified E3G, PdG, and LH from Sigma-Aldrich were used to prepare spiked urine samples for calibration curves [22]. |
| Lateral Flow Assays | The core sensing element; a multiplexed competitive ELISA format for E3G/PdG and a sandwich ELISA for LH enable simultaneous quantitative measurement [22]. | The Inito test strip, which was qualified using image processing and AI algorithms [22]. |
| ELISA Kits | Serve as the reference method for validating the quantitative performance of the point-of-care device. | Arbor EIA kits for E3G (K036-H5) and PdG (K037-H5), and the DRG LH ELISA kit (EIA-1290) were used [22]. |
| Interference Substances | Used to test assay specificity and ensure common substances in urine do not cross-react or inhibit the assay. | Substances like hCG, ascorbic acid, caffeine, and hemoglobin were tested at physiological concentrations [22]. |
| Mobile Application with AI | Replaces manual readout; captures test strip images and uses algorithms to convert optical density to concentration, reducing subjective user error [22]. | The Inito app, which uses a multi-scale algorithm to detect the device and process the image [22]. |
The integration of smartphone-based readers for urinary reproductive hormone monitoring represents a significant advancement in personalized healthcare and fertility research. These platforms, which quantitatively measure hormones such as Luteinizing Hormone (LH), Estrone-3-glucuronide (E3G), and Pregnanediol glucuronide (PdG), provide unprecedented access to longitudinal hormonal data [1] [17]. However, the analytical performance and clinical utility of these systems depend critically on the consistency and reliability of the underlying immunoassays. A primary challenge in maintaining this reliability is managing lot-to-lot variance (LTLV), a form of batch variability that can significantly impact assay accuracy, precision, and specificity [35]. This Application Note explores the sources of LTLV in quantitative urinary hormone immunoassays, provides validation data from a specific smartphone-based fertility monitor, and outlines detailed protocols to mitigate variability, ensuring robust performance in research and development settings.
Understanding Lot-to-Lot Variance (LTLV) in Immunoassays
Immunoassays are plagued by the problem of lot-to-lot variance, which negatively affects assay accuracy, precision, and specificity, leading to considerable uncertainty in reported results [35]. This variability presents a major challenge for the reproducibility of hormonal measurements over time.
Primary Causes of LTLV
The technical performance of immunoassays is governed by two key elements: raw materials and production processes. It is estimated that 70% of an immunoassay's performance is attributed to the raw materials, while the remaining 30% is ascribed to the production process, including buffer recipes and reagent formulation [35].
Quality Fluctuation of Raw Materials: Immunoassays comprise various biological components, each a potential source of variance. Key materials include:
- Antibodies: Monoclonal antibodies are crucial for reliable reagents. Their performance can be affected by issues such as aggregation (particularly of IgG3), which can lead to high background, signal leap, and overestimated analyte concentrations in sandwich immunoassays [35].
- Enzymes: Commonly used enzymes like Horseradish Peroxidase (HRP) and Alkaline Phosphatase (ALP) are typically extracted from native materials. While purity may be consistent across batches, notable differences in enzymatic activity often occur, directly impacting expected assay performance [35].
- Antigens and Conjugates: The quality of antigen raw materials is critical, with activity, purity, batch-to-batch consistency, and stability serving as key evaluation criteria. Impurities can reduce labeling efficiency, leading to diminished specificity, reduced signal, and increased background [35].
- Solid Phases and Buffers: Inhomogeneous magnetic beads or microtiter plates, as well as improperly mixed buffers leading to pH and conductivity deviations, can also contribute to LTLV [35].
Deviations in Manufacturing Processes: The production process guarantees the lower limit of kit quality and reproducibility. Even minor, uncontrolled deviations in manufacturing can introduce significant variance between production lots [35].
Experimental Validation: A Case Study on a Smartphone Fertility Monitor
A clinical validation study of the Inito Fertility Monitor (IFM) demonstrates the application of rigorous testing to establish assay performance and identify characteristic hormone trends, providing a model for validating similar platforms [1].
Materials and Methods
- Device and Principle: The IFM is a mobile-mounted, app-connected device that measures E3G, PdG, and LH simultaneously in urine. The test strip contains two lateral flow assays: one multiplexed to measure E3G and PdG in a competitive ELISA format, and another to measure LH in a sandwich ELISA format [1].
- Sample Collection: For the validation study, daily first morning urine samples were collected from 100 women aged 21–45 years with no diagnosed infertility conditions. A second group of 52 women meeting the same criteria used the IFM for testing at home [1].
- Validation Procedure:
- Recovery and Precision: The recovery percentage of the three hormones was evaluated using standard spiked solutions. Precision was calculated as the Coefficient of Variation (CV) across multiple measurements.
- Correlation with ELISA: The accuracy of hormone concentration measurement was assessed by comparing IFM results with laboratory-based ELISA for all three urinary hormones (E3G, PdG, and LH) [1].
- Hormone Trend Analysis: A retrospective study of patient hormone profiles was conducted to identify novel trends and criteria for confirming ovulation.
Key Performance Results
The validation study generated the following quantitative data on the monitor's analytical performance:
Table 1: Analytical Performance Metrics of the Smartphone Fertility Monitor [1]
| Hormone | Average CV (%) | Correlation with ELISA (R²) | Key Performance Insight |
|---|---|---|---|
| PdG | 5.05% | High Correlation | Accurate recovery percentage demonstrated |
| E3G | 4.95% | High Correlation | Enables extension of the fertile window prediction |
| LH | 5.57% | High Correlation | Reliable detection of the LH surge |
Table 2: Demographic Characteristics of Validation Study Cohorts [1]
| Parameter | Group I (Lab Validation, n=100) | Group II (Home Use, n=52) |
|---|---|---|
| Mean Age (SD) | 27.3 (4.6) years | 27.6 (4.1) years |
| Mean Cycle Length (SD) | 30.4 (6.3) days | 27.6 (5.4) days |
| BMI 18.5-24.9, n (%) | 66 (66%) | 41 (78.9%) |
| Trying to Conceive, n (%) | 31 (31%) | 52 (100%) |
The study also identified a novel criterion for confirming ovulation based on urinary PdG rise after the LH peak, which distinguished ovulatory from anovulatory cycles with 100% specificity and an area under the ROC curve of 0.98 [1]. Furthermore, a previously unobserved hormone trend—a PdG rise before the LH surge—was identified in 94.5% of ovulatory cycles [1].
Protocols for Mitigating Lot-to-Lot Variance
Implementing standardized protocols is essential for controlling LTLV. The following procedures should be integrated into the quality control workflow for developers and research scientists.
Protocol 1: Reagent Quality Control and Qualification
Purpose: To ensure consistency in the critical raw materials that constitute up to 70% of assay performance [35].
Antibody QC:
- Assess activity, concentration, affinity, and specificity.
- Analyze purity and check for aggregates using Size Exclusion Chromatography with High-Performance Liquid Chromatography (SEC-HPLC) and Capillary Electrophoresis Sodium Dodecyl Sulfate Gel Electrophoresis (CE-SDS). Purity should meet predefined specifications (e.g., >98%).
- Test labeling efficiency to ensure it does not negatively impact assay specificity or background.
Antigen/Calibrator QC:
- Evaluate antigens provided as clear, homogeneous liquids or lyophilized powders, ensuring they are free of contaminants and turbidity.
- Assess purity using SDS-PAGE followed by Coomassie brilliant blue or silver staining.
- For synthetic peptides, verify the target peptide content, as different batches may have varying amounts due to synthetic by-products.
Enzyme Conjugate QC:
- Standardize enzymatic activity using validated activity units.
- Verify that purity levels (e.g., 90-95%) are consistent and that no interfering or inhibitory ingredients are present.
Protocol 2: In-Process Control and Manufacturing Consistency
Purpose: To monitor and control the production processes that account for 30% of assay performance [35].
Buffer and Diluent Formulation:
- Standardize buffer recipes with precise concentrations of all components, including stabilizers like Bovine Serum Albumin (BSA), urea, or glycerol [35].
- Implement mixing procedures that ensure homogeneity, with verification of pH and conductivity for each batch.
Conjugation and Immobilization:
- Establish standardized protocols for antibody-enzyme conjugation and immobilization onto solid phases (e.g., magnetic particles, nitrocellulose membranes).
- Monitor conjugation ratios and efficiency consistently across lots.
Calibrator and Control Preparation:
- Use a stable, well-characterized master calibrator traceable to a reference material.
- Prepare calibrators and controls from different source materials to avoid introducing correlated errors.
- Lyophilize calibrators where possible to enhance stability [35].
Protocol 3: Lot-to-Lot Validation and Bridging Studies
Purpose: To qualify each new reagent or kit lot before use in research or production.
- Precision Testing: Determine intra-assay and inter-assay CV for the new lot using a predefined panel of samples. The CV for key hormones (e.g., PdG, E3G, LH) should ideally be below 5-6% [1].
- Parallel Testing: Run a panel of clinical samples (n ≥ 20) spanning the assay's dynamic range with both the old and new lots.
- Data Analysis:
- Perform linear regression (Passing-Bablok or Deming) to compare results. Acceptable criteria may include a slope of 0.95-1.05 and an R² > 0.98.
- Check for bias at critical medical decision points (e.g., around the LH surge or PdG threshold for ovulation confirmation).
- Stability Studies: Conduct accelerated and real-time stability testing to define the shelf-life of the new lot.
The Scientist's Toolkit: Essential Research Reagent Solutions
The consistent performance of urinary hormone immunoassays relies on several critical components. The following table details these essential materials and their functions.
Table 3: Key Research Reagent Solutions for Urinary Hormone Immunoassays
| Reagent/Material | Function & Role in Assay | Key Quality Control Parameters |
|---|---|---|
| Monoclonal Antibodies | Primary binding agent for specific hormone capture and detection; determines fundamental assay specificity and sensitivity. | Affinity, purity (SEC-HPLC, CE-SDS), concentration, absence of aggregates, labeling efficiency [35]. |
| Enzyme Conjugates (HRP, ALP) | Generate measurable signal (colorimetric, fluorometric, chemiluminescent) proportional to hormone concentration. | Enzymatic activity units, purity, consistency between batches, absence of inhibitors [35]. |
| Synthetic Antigens & Calibrators | Serve as reference standards for constructing the calibration curve; critical for quantitative accuracy. | Purity (SDS-PAGE), precise concentration, peptide content, stability (lyophilization recommended) [35]. |
| Solid Phase (Magnetic Beads, Membranes) | Platform for immobilizing capture antibodies and facilitating the separation of bound and free analytes. | Binding capacity, uniformity of particle size or membrane porosity, low non-specific binding [35]. |
| Assay Buffers & Diluents | Provide optimal pH, ionic strength, and chemical environment for antigen-antibody interaction; can include blockers to reduce background. | Consistent pH and conductivity, purity of components, effective blocking capacity to minimize noise [35]. |
| Lot-to-Lot QC Panel | External quality control material used to monitor and validate performance consistency across different kit lots. | Stability, commutability, coverage of clinically relevant concentration range [35]. |
Workflow and Pathway Visualizations
LTLV Mitigation Strategy
Hormone Monitoring Protocol
The Importance of Multi-Cycle Tracking for Capturing Person-Specific Hormone Patterns
The monitoring of urinary reproductive hormones represents a powerful, non-invasive method for assessing female endocrine health, with applications ranging from fertility treatment to clinical drug development [17]. The recent advent of quantitative smartphone-based readers has significantly enhanced the potential for detailed, at-home hormone tracking [1] [17]. These devices move beyond qualitative or binary results to provide numerical concentration data for key hormone metabolites such as estrone-3-glucuronide (E3G), pregnanediol glucuronide (PdG), and luteinizing hormone (LH) [1]. However, the inherent variability of the menstrual cycle, both between individuals and between cycles for the same individual, presents a significant challenge for data interpretation. This document establishes the critical importance of multi-cycle tracking to capture true, person-specific hormone patterns, thereby validating the role of smartphone reader technology in rigorous scientific research.
Single-cycle analyses are often insufficient for defining an individual's endocrine profile. Studies indicate that approximately 26–37% of natural cycles are anovulatory, and cycle characteristics can be influenced by factors such as age, diet, and underlying disorders [1]. Consequently, data collected over multiple cycles are essential to distinguish consistent, person-specific patterns from cycle-specific anomalies. This multi-cycle approach provides a more robust foundation for diagnosing ovulatory dysfunction, personalizing fertility interventions, and evaluating the efficacy of new therapeutic agents in clinical trials.
Quantitative Hormone Data and Cycle Variability
The core strength of quantitative smartphone readers lies in their ability to generate continuous, numerical data for multiple hormones across the entire cycle. The table below summarizes typical reference ranges for key urinary hormone metabolites across different menstrual cycle phases, which are crucial for interpreting data from multi-cycle tracking [36].
Table 1: Urinary Hormone Metabolite Ranges by Menstrual Cycle Phase
| Hormone Metabolite | Follicular Phase | Ovulatory/Mid-Cycle Phase | Luteal Phase |
|---|---|---|---|
| LH (mIU/L) | 2.4 – 12.6 | 14.0 – 95.6 | 1.0 – 11.4 |
| E3G (ng/mL) | 12.5 – 166.0 | 85.8 – 498.0 | 43.8 – 211.0 |
| PdG (ug/mL) | 0.1 – 0.9 | 0.1 – 12.0 | 1.8 – 23.9 |
The clinical utility of this data is demonstrated through the identification of distinct hormone trends. For instance, a study validating the Inito Fertility Monitor (IFM) demonstrated high correlation with laboratory-based ELISA results, with low assay variability (average CV of 4.95%-5.57% across the three hormones) [1]. This analytical precision enables the detection of critical physiological events, such as the LH surge that precedes ovulation by 24-36 hours and the subsequent rise in PdG that confirms ovulation has occurred [36]. Furthermore, multi-cycle tracking can reveal novel, person-specific patterns. The same IFM study identified a previously unobserved PdG rise before the LH surge in some cycles and established a novel criterion for confirming ovulation with 100% specificity, which was only possible through the analysis of multi-cycle, quantitative data [1].
Experimental Protocols for Hormone Tracking and Validation
To ensure the reliability of data collected for multi-cycle analysis, standardized protocols for both device validation and participant testing must be followed.
Protocol 1: Analytical Validation of Smartphone-Based Reader
This protocol outlines the procedure for validating the accuracy and precision of a smartphone-based hormone reader against established laboratory methods [1].
- Sample Preparation: Prepare standard solutions of E3G, PdG, and LH by spiking known concentrations of purified metabolites into male urine that has been pre-screened to confirm negligible endogenous levels of the target analytes [1].
- Calibration Curve Generation: For each batch of test strips, generate a calibration curve by measuring the optical density (OD) output of the device for the standard solutions and plotting these values against the known concentrations [1].
- Precision and Linearity Assessment: Test standard solutions of fixed concentrations multiple times (n≥3) to determine the intra-assay and inter-assay Coefficient of Variation (CV). Assess linearity by testing samples across the assay's dynamic range [1].
- Correlation with Reference Method: Collect fresh first-morning urine samples from a cohort of participants (e.g., n=100). Split each sample and test simultaneously with the smartphone reader and a laboratory ELISA kit. Perform statistical correlation analysis (e.g., Pearson's r) between the results from both methods [1].
Protocol 2: Multi-Cycle Hormone Tracking in a Cohort Study
This protocol describes the methodology for conducting a longitudinal study to capture person-specific hormone patterns using a smartphone reader.
- Participant Recruitment and Screening: Recruit female participants of reproductive age (e.g., 21-45) with varying cycle lengths (e.g., 21-42 days). Exclude individuals with diagnosed infertility conditions or highly irregular cycles. Record baseline characteristics including age, BMI, and average cycle length [1].
- Sample Collection and Testing: Instruct participants to collect first-morning urine samples daily throughout one or more complete menstrual cycles. Participants will use the smartphone reader and compatible test strips at home according to the manufacturer's instructions. The test typically involves dipping the strip in urine for 15 seconds, waiting a specified development time (e.g., 10 minutes), and scanning the strip with the smartphone application to obtain quantitative values for E3G, PdG, and LH [1] [36].
- Data Aggregation and Pattern Analysis: Data from the device is automatically synced to a secure database. For analysis, hormone levels are aligned relative to the day of the LH peak (LH=0). Patterns are analyzed for key events: the E3G rise initiating the fertile window, the LH surge, the subsequent PdG rise confirming ovulation, and the identification of any atypical or anovulatory patterns [1] [36].
Workflow and Architecture Visualization
The following diagram illustrates the integrated experimental workflow, from participant testing to data validation, as described in the protocols.
Figure 1: Integrated Multi-Cycle Tracking and Validation Workflow
The underlying technology of the smartphone reader is critical for obtaining reliable data. The diagram below details a generalized architecture for such a device, which often forms the basis for the at-home testing used in these protocols.
Figure 2: Smartphone Reader and Assay Architecture
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and reagents used in the validation and application of urinary reproductive hormone monitoring.
Table 2: Key Research Reagents and Materials for Hormone Tracking
| Item | Function & Application in Research |
|---|---|
| Purified E3G, PdG, LH Metabolites | Used as standards for spiking experiments to generate calibration curves, determine assay recovery percentage, and establish linearity and dynamic range [1]. |
| Characterized Male Urine Pool | Serves as a consistent, low-background matrix for preparing standard solutions and controls, minimizing variables introduced by female urine with fluctuating hormone levels [1]. |
| Lateral Flow Immunoassay Strips | The core diagnostic element; typically configured with competitive ELISA formats for small molecules (E3G, PdG) and sandwich ELISA for larger proteins (LH) [1]. |
| Reference ELISA Kits (e.g., Arbor, DRG) | Gold-standard method for analytical validation. Used in a laboratory setting to measure the same urine samples analyzed by the smartphone reader to establish correlation [1]. |
| First-Morning Urine Samples | The preferred sample type for hormone monitoring due to its concentration, which minimizes the impact of diurnal variation on hormone metabolite levels [1] [36]. |
Multi-cycle tracking is not merely an enhancement but a fundamental requirement for capturing the complexity and individuality of female reproductive endocrinology. Quantitative smartphone-based readers, when deployed according to rigorous validation and testing protocols, provide an unprecedented toolset for achieving this deep, person-specific understanding. The ability to collect high-fidelity, longitudinal hormone data outside the clinical setting opens new avenues for research into ovulatory disorders, the impact of pharmaceutical interventions, and the natural progression of reproductive aging. By adopting the multi-cycle framework and methodologies outlined in this document, researchers and drug development professionals can generate more robust, reliable, and clinically relevant insights.
Analytical and Clinical Validation: Benchmarking Against Gold-Standard Methods
The quantitative measurement of urinary reproductive hormones represents a significant advancement in personalized healthcare, enabling detailed monitoring of menstrual cycle dynamics and fertility status outside clinical settings. The validation of any novel diagnostic device in this field hinges on demonstrating its analytical robustness through rigorous comparison against established laboratory standards. This application note details the experimental protocols and performance data for a novel smartphone-connected reader, focusing on its correlation with traditional enzyme-linked immunosorbent assay (ELISA) methods and the precision of its recovery percentages for key urinary hormone metabolites [1].
The smartphone-based fertility monitor (Inito Fertility Monitor, IFM) was evaluated for its ability to accurately measure three key urinary hormone metabolites: Estrone-3-glucuronide (E3G), Pregnanediol glucuronide (PdG), and Luteinizing Hormone (LH). The following tables summarize the core analytical performance metrics established during validation studies.
Table 1: Assay Precision and Recovery Percentage Data
| Hormone Metabolite | Average Coefficient of Variation (CV) | Recovery Percentage | Assessment Method |
|---|---|---|---|
| Pregnanediol Glucuronide (PdG) | 5.05% | Accurate [1] | Testing of standard spiked solutions [1] |
| Estrone-3-glucuronide (E3G) | 4.95% | Accurate [1] | Testing of standard spiked solutions [1] |
| Luteinizing Hormone (LH) | 5.57% | Accurate [1] | Testing of standard spiked solutions [1] |
Table 2: Correlation with Reference Laboratory ELISA
| Hormone Metabolite | Correlation with ELISA | Key Statistical Outcome |
|---|---|---|
| E3G | High Correlation [1] | R² = 0.96 for predicted serum Estradiol (E2) [29] |
| PdG | High Correlation [1] | R² = 0.95 for predicted serum Progesterone (P4) [29] |
| LH | High Correlation [1] | R² = 0.98 for predicted serum LH [29] |
Detailed Experimental Protocols
Protocol 1: Characterization of Assay Accuracy and Precision
This protocol is designed to determine the reproducibility (precision) and accuracy of the smartphone-based reader by testing spiked standard solutions.
3.1.1 Materials and Reagents
- Smartphone Fertility Monitor and Test Strips: The device uses two lateral flow assays on a single strip; one multiplexed for E3G and PdG in a competitive ELISA format, and another for LH in a sandwich ELISA format [1].
- Standard Solutions: Purified E3G, PdG, and LH metabolites (e.g., from Sigma-Aldrich) prepared in spiked male urine, which has been pre-tested via ELISA to confirm negligible endogenous concentrations of the target metabolites [1] [33].
- ELISA Kits: For method correlation. Examples include:
- Arbor Estrone-3-Glucuronide EIA kit (K036-H5) for E3G.
- Arbor Pregnanediol-3-Glucuronide EIA kit (K037-H5) for PdG.
- DRG LH (urine) ELISA kit (EIA-1290) for LH [1].
3.1.2 Procedure
- Preparation of Standard Spiked Solutions: Prepare a minimum of six standard solutions with known concentrations of E3G, PdG, and LH in the spiked male urine matrix, covering the expected physiological range [33].
- Testing with Smartphone Reader: Dip a test strip into each standard solution for 15 seconds. Insert the strip into the reader, which is attached to a mobile device. The device captures an image of the test strip, and the application processes it to yield an optical density (OD) value, which is converted to a concentration via a pre-established calibration curve [1].
- Replication: Test each standard solution with five different test strips from the same manufacturing lot to assess inter-strip variability [1] [33].
- Data Analysis:
- Coefficient of Variation (CV): Calculate the average CV across the replicate measurements for each hormone.
- Recovery Percentage: Determine the percentage of the known, spiked concentration that is accurately measured by the device.
Protocol 2: Correlation Study with Laboratory-Based ELISA
This protocol validates the smartphone reader's performance against the gold standard laboratory method, ELISA, using actual patient samples to ensure clinical relevance.
3.2.1 Participant Recruitment and Sample Collection
- Cohort: Recruit women of reproductive age (e.g., 21-45 years) with regular menstrual cycles and no known infertility conditions. A typical study involves an initial group of ~100 women for lab-based testing and a second group of ~52 women for at-home testing with the device [1].
- Sample Type: First-morning urine samples are collected daily throughout one complete menstrual cycle [1].
- Ethics: The study protocol must be approved by an institutional review board, and informed consent must be obtained from all volunteers [1].
3.2.2 Procedure
- Sample Splitting: Split each daily urine sample into two aliquots.
- Testing with Smartphone Reader: One aliquot is tested using the smartphone reader as described in Protocol 1. If samples are frozen, they should be thawed only once prior to analysis, as this has been shown to have no significant effect on urinary hormone concentrations [33].
- Testing with ELISA: The second aliquot is tested in a laboratory setting using the respective ELISA kits for E3G, PdG, and LH. All samples should be measured in triplicate, and the average value used for comparison. Standard curves are generated for each ELISA run using the calibrators provided with the kits [1].
- Data Analysis: Perform correlation analysis (e.g., linear regression) to calculate the R² value between the hormone concentrations obtained from the smartphone reader and those from the laboratory ELISA [1] [29].
Diagram 1: Workflow for Device vs. ELISA Correlation Study
The Scientist's Toolkit: Research Reagent Solutions
The following table outlines essential materials and their specific functions for conducting the described validation experiments.
Table 3: Essential Research Reagents and Materials
| Item | Function/Application | Example Products / Notes |
|---|---|---|
| Smartphone Fertility Monitor | Quantitative home-use reader; connects to a mobile app for data capture and analysis. | Inito Fertility Monitor (IFM) [1]. |
| Lateral Flow Test Strips | Solid-phase assay for hormone detection; contains separate assays for E3G/PdG (competitive) and LH (sandwich) [1]. | Inito Fertility Test Strips. |
| Purified Hormone Metabolites | Used for preparing standard spiked solutions for accuracy and recovery tests. | E3G, PdG, LH from Sigma-Aldrich [1] [33]. |
| Reference ELISA Kits | Gold-standard method for quantifying hormone concentrations in urine for correlation studies. | Arbor EIA Kits for E3G & PdG; DRG ELISA Kit for LH [1]. |
| Calibrators & Controls | Used to generate standard curves for both the smartphone reader and ELISA assays. | Provided with commercial ELISA kits; prepared for reader calibration [1]. |
| Sample Matrix (Male Urine) | A confirmed hormone-negative matrix for preparing spiked standards. | Pre-screened with ELISA for negligible target hormone levels [1]. |
Underlying Hormone Pathways and Device Function
Understanding the biochemical principles is crucial for assay design. The device measures specific metabolites in urine that closely reflect serum hormone dynamics. E3G is a major urinary metabolite of estradiol, and PdG is a stable urinary metabolite of progesterone. Their predictable patterns during the menstrual cycle allow for fertile window prediction and ovulation confirmation [1].
Diagram 2: Relationship Between Serum Hormones, Urinary Metabolites, and Device Function
The quantification of urinary reproductive hormones—specifically Estrone-3-glucuronide (E3G), Pregnanediol glucuronide (PdG), and Luteinizing Hormone (LH)—represents a critical methodology for evaluating female reproductive health and the menstrual cycle. For researchers and clinicians, understanding the precision of these measurements, as quantified by the Coefficient of Variation (CV), is fundamental to assessing assay reliability and data validity. This application note details the precision metrics and experimental protocols for measuring E3G, PdG, and LH using a novel smartphone-connected reader, the Inito Fertility Monitor (IFM), providing a framework for its use in research and validation contexts [1] [4].
The transition from qualitative to quantitative hormone monitoring addresses a significant limitation in home-use tests, which have traditionally relied on manual readouts and binary results. The IFM platform utilizes a smartphone-based imaging system to capture and analyze lateral flow immunoassays, providing quantitative concentration data for all three hormones simultaneously. This approach enables the tracking of dynamic hormone trends essential for accurate fertility window prediction and ovulation confirmation [1] [33].
Precision Performance Data
The precision of the Inito Fertility Monitor was established through rigorous laboratory testing, resulting in the following Coefficient of Variation (CV) percentages for each analyte [1] [8] [4]:
Table 1: Coefficient of Variation (CV) for Urinary Hormone Measurements with IFM
| Hormone Analyte | Full Name | Average CV (%) | Biological Context |
|---|---|---|---|
| E3G | Estrone-3-glucuronide (Estrogen metabolite) | 4.95% | Marker for follicular development and beginning of fertile window |
| PdG | Pregnanediol glucuronide (Progesterone metabolite) | 5.05% | Confirmation of ovulation and corpus luteum function |
| LH | Luteinizing Hormone | 5.57% | Surge indicates impending ovulation (typically within 24-36 hours) |
These CV values demonstrate high analytical precision for a point-of-care device, with all three hormones showing CVs below 6%. This level of precision is crucial for detecting the significant hormone fluctuations that occur throughout the menstrual cycle. The IFM's performance was validated against laboratory-based ELISA methods, showing high correlation for all three hormones [1] [4].
It is important to contextualize these analytical CVs within the framework of normal biological variation. Reproductive hormones exhibit significant fluctuations due to pulsatile secretion, diurnal rhythms, and nutrient intake. One study quantified this variability, reporting that LH is the most variable reproductive hormone (CV 28%), followed by sex-steroid hormones (estradiol CV 13%, testosterone CV 12%), while FSH is the least variable (CV 8%) [37]. The CV of the IFM assay is substantially lower than the inherent biological variation for these hormones, confirming its capability to detect true physiological changes rather than analytical noise.
Experimental Protocols
Sample Preparation and Testing Protocol
Table 2: Key Research Reagent Solutions
| Reagent / Material | Function / Purpose | Source / Specifications |
|---|---|---|
| Inito Fertility Monitor (IFM) | Smartphone-connected reader for quantitative hormone measurement | Inito Inc. |
| Inito Fertility Test Strips | Lateral flow assays for E3G, PdG, and LH | Multiplexed strip: competitive ELISA for E3G/PdG, sandwich ELISA for LH |
| Standard Spiked Solutions | For calibration curves and accuracy assessment | Prepared in male urine with negligible endogenous hormones; metabolites from Sigma-Aldrich |
| ELISA Kits | Reference method for validation | Arbor Assays (E3G: K036-H5, PdG: K037-H5); DRG (LH: EIA-1290) |
| First Morning Urine Samples | Biological sample for analysis | Collected daily from study participants |
The following protocol details the procedure for evaluating the precision and accuracy of the IFM system:
Step 1: Calibration Curve Generation
- Prepare standard solutions in male urine spiked with target concentrations of E3G, PdG, and LH [1] [4].
- Test these standard solutions with multiple IFM test strips (n=5 per concentration) [33].
- Plot the optical density (OD) values obtained from the IFM against the known concentrations to generate a calibration curve for each hormone [1] [4].
Step 2: Precision Testing
- Prepare quality control samples with known concentrations of all three hormones [1].
- Analyze these samples repeatedly with multiple IFM test strips from the same manufacturing lot [33].
- Calculate the inter-assay Coefficient of Variation (CV) using the formula: CV (%) = (Standard Deviation / Mean) × 100 [1] [4].
Step 3: Method Comparison Study
- Collect first morning urine samples from study participants (typically women aged 21-45 with regular cycles) [1] [4].
- Split each sample for parallel testing with IFM and laboratory ELISA [1] [8].
- Test all samples in triplicate using both methods to account for technical variability [1] [4].
- Calculate correlation coefficients (e.g., Pearson's r) between IFM results and ELISA reference values [1] [33].
Step 4: Recovery Assessment
- Prepare samples with known concentrations of hormones by spiking male urine [33].
- Measure these samples with IFM and calculate the recovery percentage: (Measured Concentration / Expected Concentration) × 100 [1] [4].
- The recovery percentage should fall within acceptable limits (typically 85-115%) for accurate quantification [1].
Diagram 1: Experimental workflow for assessing precision and accuracy of hormone measurements
Hormone Physiology and Signaling Pathways
The three hormones measured by the IFM play distinct but interconnected roles in the menstrual cycle:
E3G (Estrone-3-glucuronide)
- Urinary metabolite of estradiol, reflecting ovarian follicular development [1] [18].
- Rising levels indicate the beginning of the fertile window, typically 5-6 days before ovulation [1] [33].
- Works in concert with FSH to promote follicular growth and maturation [33].
LH (Luteinizing Hormone)
- Pituitary glycoprotein hormone that triggers ovulation [1] [38].
- Surge typically lasts 48-72 hours and precedes ovulation by 24-36 hours [1].
- Induces final follicular maturation and release of the oocyte [33] [38].
PdG (Pregnanediol glucuronide)
- Primary urinary metabolite of progesterone [1] [39].
- Rises after ovulation, reflecting corpus luteum formation and function [1] [38].
- Confirms ovulation has occurred and supports the luteal phase of the menstrual cycle [1] [33].
Diagram 2: Hormone signaling pathways and their roles in the menstrual cycle
Applications in Reproductive Research
The quantitative data generated by the IFM system, with its established precision metrics, enables several advanced research applications:
4.1 Novel Ovulation Confirmation Criteria Research using IFM has identified that a specific PdG rise pattern following the LH peak can confirm ovulation earlier than previous methods. This novel criterion demonstrated 100% specificity for distinguishing ovulatory from anovulatory cycles, with an area under the ROC curve of 0.98 [1] [4].
4.2 Luteal Phase Characterization The simultaneous measurement of E3G, LH, and PdG enables detailed characterization of the luteal phase. Researchers can identify three distinct processes: luteinization (corpus luteum formation), progestation (PDG rise to support potential pregnancy), and luteolysis (corpus luteum regression) [38].
4.3 Monitoring Special Populations Quantitative hormone monitors have been validated in populations with unique hormonal patterns, including postpartum and perimenopausal women. These transitions are characterized by irregular cycles where quantitative monitoring provides particular value over binary tests [18].
4.4 Identification of Novel Hormone Trends The high temporal resolution of daily monitoring has revealed previously unobserved hormone patterns, such as PdG rises before the LH surge in some cycles. These findings challenge traditional models of menstrual cycle endocrinology and may lead to new diagnostic insights [1] [33].
The Inito Fertility Monitor provides precise quantification of urinary E3G, PdG, and LH with CVs under 6%, demonstrating performance suitable for both research and clinical applications. The experimental protocols outlined herein provide researchers with a framework for validating quantitative hormone monitoring systems. The ability to track dynamic hormone patterns, rather than relying on threshold-based determinations, represents a significant advancement in at-home reproductive hormone monitoring, enabling more personalized approaches to fertility management and menstrual cycle research.
The integration of smartphone technology with lateral flow immunoassays creates new opportunities for large-scale data collection on menstrual cycle characteristics across diverse populations. Future applications may include monitoring response to fertility treatments, tracking cycle changes in perimenopause, and contributing to population-level understanding of reproductive health trends.
The confirmation of ovulation is a critical component in the investigation of infertility and for women planning conception [40]. Traditional methods for detecting ovulation, including transvaginal ultrasonography (TVUS) and serum progesterone measurements,, while accurate, are invasive, expensive, and often impractical for continuous monitoring [40] [41]. The measurement of urinary metabolites of reproductive hormones presents a convenient and non-invasive alternative [41]. This application note evaluates the clinical utility of a novel smartphone-connected reader, the Inito Fertility Monitor (IFM), focusing on its specificity and sensitivity in confirming ovulation and identifying anovulatory cycles through the quantitative analysis of urinary estrone-3-glucuronide (E3G), luteinizing hormone (LH), and pregnanediol glucuronide (PdG) [22] [1]. The data presented herein are framed within a broader thesis on validating at-home urinary hormone measurements.
Performance Validation of the Smartphone-Connected Reader
The efficacy of the Inito Fertility Monitor (IFM) was established through a validation study comparing its performance against laboratory-based ELISA for quantifying E3G, LH, and PdG in urine [22] [1].
Table 1: Analytical Performance of the Inito Fertility Monitor against ELISA
| Hormone Measured | Average Coefficient of Variation (CV) | Correlation with ELISA | Key Performance Metric |
|---|---|---|---|
| Pregnanediol Glucuronide (PdG) | 5.05% | High Correlation | Accurate confirmation of ovulation |
| Estrone-3-Glucuronide (E3G) | 4.95% | High Correlation | Prediction of fertile window |
| Luteinizing Hormone (LH) | 5.57% | High Correlation | Prediction of imminent ovulation |
The assay demonstrated accurate recovery percentages for all three hormones and low coefficients of variation, indicating high precision and reproducibility [22] [1]. The high correlation with reference ELISA methods establishes IFM as a reliable tool for quantitative urinary hormone monitoring in a home-setting [22] [1].
Specificity and Sensitivity in Ovulation Confirmation
A key advantage of multi-hormone tracking is the ability to not only predict but also confirm ovulation. The IFM system identified a novel criterion for confirming ovulation based on the trajectory of urinary PdG levels following the LH surge [22] [1].
Table 2: Novel Ovulation Confirmation Criterion Performance
| Parameter | Performance Metric |
|---|---|
| Specificity | 100% |
| Area Under the ROC Curve (AUC) | 0.98 |
| Function | Distinguishes ovulatory from anovulatory cycles |
This PdG-based criterion accurately distinguished ovulatory from anovulatory cycles with 100% specificity, enabling earlier confirmation of ovulation compared to existing methods [22] [1]. This is clinically significant given that approximately 26–37% of natural cycles are anovulatory, which can be a source of frustration for couples trying to conceive [22] [1].
Experimental Protocols for Hormone Measurement and Ovulation Assessment
Protocol: Urinary Hormone Measurement using IFM
This protocol details the steps for quantifying E3G, PdG, and LH in first-morning urine samples using the Inito Fertility Monitor [22] [1].
- Sample Collection: Collect first-morning urine sample in a clean container.
- Test Strip Inoculation: Dip the Inito Fertility test strip into the urine sample for 15 seconds.
- Strip Insertion: Insert the test strip into the Inito Fertility Monitor, which is attached to a smartphone.
- Image Capture and Analysis: The Inito mobile application captures an image of the test strip. Image processing algorithms are used to yield an optical density (OD) value corresponding to the concentration of each metabolite.
- Concentration Determination: Metabolite concentrations are calculated from a pre-generated calibration curve specific to each batch of test strips.
- Data Output: The application provides quantitative values for E3G, PdG, and LH, along with fertility status ratings.
Protocol: Confirmatory Ovulation Assessment
This protocol describes the criteria for confirming ovulation using longitudinal hormone data [22] [1] [42].
- Baseline Establishment: Establish baseline PdG levels from tests conducted during the follicular phase.
- LH Surge Identification: Identify the LH surge (peak) from daily testing.
- Post-LH PdG Monitoring: Continue daily testing to monitor the rise in PdG levels following the LH surge.
- Ovulation Confirmation: Apply the novel criterion—a specific pattern and magnitude of PdG rise after the LH peak—to confirm ovulation. This pattern was shown to be present in 94.5% of ovulatory cycles [22] [1].
- Ovulatory Function Assessment: To assess the quality of the luteal phase, a PdG level of ≥5 μg/mL can be used as a threshold, which correlates with a serum progesterone level of >5 ng/mL, a common clinical cutoff for confirming ovulation [41] [42].
Workflow for Ovulation Confirmation and Anovulatory Cycle Identification
The following diagram illustrates the logical workflow for using multi-hormone data to confirm ovulation and identify anovulatory cycles.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Urinary Reproductive Hormone Studies
| Item | Function / Application | Example Product / Source |
|---|---|---|
| Urinary PdG ELISA Kit | Reference method for quantifying pregnanediol glucuronide; used for assay validation. | Arbor Pregnanediol-3-Glucuronide EIA Kit (K037-H5) [22] [1] |
| Urinary E3G ELISA Kit | Reference method for quantifying estrone-3-glucuronide; used for assay validation. | Arbor Estrone-3-Glucuronide EIA Kit (K036-H5) [22] [1] |
| Urinary LH ELISA Kit | Reference method for quantifying luteinizing hormone; used for assay validation. | DRG LH (urine) ELISA Kit (EIA-1290) [22] [1] |
| Purified Metabolites | Used for spiking experiments to determine assay recovery, precision, and cross-reactivity. | Sigma-Aldrich (e.g., PdG #903620, E3G #E2127, LH #L6420) [22] [1] |
| Smartphone-Connected Reader & Test Strips | At-home, quantitative point-of-care device for simultaneous measurement of E3G, LH, and PdG. | Inito Fertility Monitor & Test Strips [22] [1] |
The validation data and performance metrics demonstrate that the Inito Fertility Monitor, a smartphone-connected reader, provides a clinically utility solution for confirming ovulation and identifying anovulatory cycles. Its high specificity (100%) and AUC (0.98) for the novel PdG-based ovulation criterion, coupled with high correlation to laboratory ELISA methods, make it a reliable and quantitative tool for both research and personal use. This technology enables a more nuanced understanding of individual menstrual cycle dynamics, moving beyond binary results to provide actionable hormone trend data.
The quantitative self-monitoring of urinary reproductive hormones represents a significant advancement in the field of precision medicine for reproductive health [43]. This comparative analysis examines four commercial fertility monitoring platforms—Inito, Mira, Oova, and Clearblue—within the context of validating urinary reproductive hormone measurements via smartphone-connected reader technology. These platforms have emerged as viable tools for researchers and clinicians seeking to understand luteal phase dynamics and hormone patterns outside traditional laboratory settings [43]. The evolution from qualitative to quantitative hormone measurement has enabled more detailed characterization of the three distinct processes of the luteal phase: luteinization, progestation, and luteolysis [43]. This analysis focuses on the technical specifications, analytical performance, and research applications of these platforms, with particular emphasis on their validation against established laboratory methods.
The four platforms employ distinct technological approaches to hormone measurement and data interpretation. Inito utilizes a smartphone-clip design that employs the phone's camera with controlled lighting to measure intensity lines on a single test strip quantifying E3G, LH, and PdG [43] [44]. Mira employs lab-grade fluorescent technology with a dedicated analyzer that syncs via Bluetooth to a smartphone application, providing numerical values for multiple hormones including E3G, LH, PdG, and FSH [45] [46]. Oova leverages quantitative lateral flow technology scanned by smartphone camera, measuring LH, E3G, and PdG with clinical-grade accuracy developed in collaboration with Mt. Sinai researchers [47]. Clearblue represents a more established qualitative approach, providing "Low," "High," and "Peak" fertility indicators based on E3G and LH thresholds without numerical hormone values [43] [48].
Table 1: Technical Specifications of Commercial Fertility Monitoring Platforms
| Platform | Technology | Measured Hormones | Data Output | Sample Type | Connection Method |
|---|---|---|---|---|---|
| Inito | Smartphone clip reader with camera | E3G, LH, PdG, FSH [44] | Quantitative values [44] | First morning urine [44] | Direct phone attachment |
| Mira | Fluorescent immunoassay with dedicated analyzer | E3G, LH, PdG, FSH [45] [46] | Quantitative values (numerical) [46] | First morning urine [49] | Bluetooth to smartphone |
| Oova | Smartphone-scanned lateral flow | LH, E3G, PdG [47] | Quantitative values [47] | First morning urine [47] | Phone camera scan |
| Clearblue | Electronic colorimetric reader | E3G, LH [48] | Qualitative (Low/High/Peak) [48] | First morning urine [48] | Dedicated handheld device |
Table 2: Analytical Performance and Validation Metrics
| Platform | Claimed Accuracy | Published Validation | Correlation with Reference Methods | Special Populations |
|---|---|---|---|---|
| Inito | 96% as accurate as blood tests [44] | Peer-reviewed study showing high correlation with ELISA [8] | High correlation with ELISA (E3G, PdG, LH) [8] | Adapts to irregular cycles [44] |
| Mira | 99% accuracy [46] | Comparison study with Clearblue [43] | High correlation with qualitative monitors [43] | Effective for PCOS, irregular cycles [45] [49] |
| Oova | 99% lab accuracy [47] | Clinical validation with Mt. Sinai [47] | 99% correlation with blood testing [47] | Works with irregular cycles, PCOS [47] |
| Clearblue | 99% accurate in detecting LH rise [50] | Established literature base [43] [48] | Correlation with blood hormone levels established [48] | Adapts to individual cycles [48] |
Experimental Protocols and Methodologies
Sample Collection and Processing Protocol
Standardized urine collection procedures are critical for obtaining reliable hormone measurements across all platforms. The following protocol applies to all four systems:
- Collection Timing: Collect first morning urine between 6-10 AM after a minimum 4-hour urine hold [44] [49]. Document exact collection time.
- Collection Method: Void directly into sterile polypropylene collection cup with volume markings.
- Processing: Test samples within 60 minutes of collection. If delayed testing is required, refrigerate at 4°C for up to 24 hours or freeze at -20°C for longer storage.
- Testing Procedure: Allow refrigerated/frozen samples to reach room temperature (20-25°C) before testing. Mix gently by inversion 3-5 times before aliquoting.
For longitudinal studies, maintain consistent collection times throughout the menstrual cycle, starting from cycle day 6 and continuing through luteal phase confirmation or menses [43] [44].
Platform-Specific Testing Protocols
Inito Testing Protocol:
- Mount smartphone clip attachment and launch Inito application [44].
- Dip test strip in urine for 15 seconds using integrated timer [44].
- Cap strip and insert into reader assembly [44].
- Initiate scan function maintaining device stability on flat surface [44].
- Record quantitative values for E3G, LH, PdG, and FSH from application interface [44].
Mira Testing Protocol:
- Prime Mira analyzer by ensuring adequate battery charge [46] [49].
- Dip appropriate test wand (Plus for E3G/LH; Confirm for PdG) for 20 seconds [46].
- Insert wand into analyzer slot until audible confirmation [49].
- Synchronize via Bluetooth with Mira application for result transmission [49].
- Record numerical values from application dashboard after 15-minute processing [49].
Comparative Analysis Protocol: For method comparison studies, split first morning urine samples for parallel testing across platforms. Aliquot 2mL for each platform plus additional 5mL for reference laboratory analysis (LC-MS/MS or ELISA). Process all platform tests within 30 minutes of collection, with reference samples frozen at -80°C for batch analysis.
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Materials and Reagents
| Item | Specifications | Research Application |
|---|---|---|
| Urine Collection Cups | Sterile, polypropylene, 30-50mL capacity with volume markings | Standardized sample collection for all platforms |
| Platform-Specific Test Strips/Wands | Manufacturer-specific lateral flow immunoassays | Hormone quantification according to platform specifications |
| Calibration Standards | Manufacturer-provided or third-party quality controls | Method validation and inter-assay comparison |
| Smartphone Imaging System | Controlled lighting, stable mounting platform | Consistency in camera-based reading platforms (Inito, Oova) |
| Temperature Monitoring Equipment | Digital thermometer, environmental logger | Quality control for sample storage and testing conditions |
| Data Export/Management System | CSV compatibility, cloud storage capabilities | Aggregation of quantitative hormone values for statistical analysis |
Analytical Performance and Validation Metrics
Method Comparison Studies
Validation studies for these platforms have demonstrated varying degrees of correlation with established laboratory methods. The Inito Fertility Monitor showed high correlation with ELISA measurements in a controlled validation study, with coefficient of variation (CV) of 5.05% for PdG measurement, 4.95% for E3G measurement, and 5.57% for LH measurement [8]. The study further demonstrated that the monitor could identify novel hormone trends in natural menstrual cycles with high specificity for ovulation confirmation (100% specificity, AUC of 0.98) [8].
A separate comparative case study evaluating Mira and Inito against the established qualitative Clearblue monitor demonstrated that quantitative monitors could clearly demarcate the transition through luteinization, progestation, and luteolysis processes in the luteal phase [43]. The study documented specific hormone patterns across normal cycles, prolonged luteinization cycles, and anovulatory cycles, with PDG plateaus of 14-15 μg/mL on both quantitative monitors in normal cycles [43].
Platform-Specific Performance Characteristics
Quantitative vs. Qualitative Measurement: The fundamental distinction between these platforms lies in their data output methodology. Mira, Inito, and Oova provide quantitative numerical values for hormone concentrations, enabling dynamic tracking of hormone fluctuations and personalized baseline establishment [44] [47] [46]. In contrast, Clearblue provides qualitative thresholds (Low/High/Peak) based on predetermined hormone levels, limiting its research applications but simplifying clinical interpretation [48].
Sensitivity and Detection Limits: Mira claims 7× greater accuracy and up to 6× greater sensitivity compared to other trackers based on lower detection limits, particularly for E3G (6× more sensitive) [45]. Oova emphasizes 99% correlation with blood testing in independent lab validation [47]. These sensitivity metrics are particularly important for detecting subtle hormone changes in populations with hormonal imbalances such as PCOS.
Ovulation Confirmation Capabilities: A critical differentiator among platforms is progesterone metabolite (PdG) measurement for ovulation confirmation. Mira, Inito, and Oova all measure PdG, enabling direct confirmation of ovulation through sustained elevation in progesterone levels [43] [44] [47]. Clearblue lacks PdG measurement, relying instead on LH surge detection alone for ovulation prediction [48].
Research Applications and Clinical Implications
Luteal Phase Characterization
The advent of quantitative fertility monitors with progesterone metabolite measurement has enabled more precise characterization of luteal phase dynamics [43]. Research applications include:
- Luteinization Process Tracking: Quantitative LH and PdG measurements can delineate the formation of the corpus luteum following ovulation [43].
- Progestation Monitoring: PdG plateaus can be quantified to assess endometrial preparation for potential implantation [43].
- Luteolysis Identification: PdG decline can be precisely tracked to identify luteal regression and cycle conclusion [43].
Case studies have demonstrated the ability of these platforms to identify abnormal luteal phases, including prolonged luteinization with broader LH surges and altered PdG plateaus [43]. This detailed luteal phase analysis represents a significant advancement over traditional methods such as "day 21" progesterone testing, which inaccurately assumes consistent cycle day ovulation [43].
Special Population Applications
These platforms show particular utility in research involving special populations:
- Irregular Cycles and PCOS: Quantitative monitors can identify ovulation patterns and hormone dynamics in populations where traditional tracking methods fail [47] [49]. The ability to establish individual baselines rather than relying on population norms is critical for these applications.
- Fertility Treatment Monitoring: Platforms providing quantitative hormone values can track response to ovulation induction medications and determine intervention efficacy [47] [49].
- Perimenopause Transition: Longitudinal hormone tracking can identify changing patterns as women approach menopause, providing insights into the perimenopause transition [47].
The comparative analysis of Inito, Mira, Oova, and Clearblue fertility monitors reveals distinct advantages and limitations for research applications. Quantitative platforms (Inito, Mira, Oova) provide numerical hormone values enabling dynamic tracking and personalized baseline establishment, while the qualitative Clearblue monitor offers simplified clinical interpretation. Validation studies demonstrate strong correlation with reference methods, particularly for Inito and Mira, supporting their research utility. The critical differentiator for luteal phase research is progesterone metabolite measurement, available on all platforms except Clearblue. As the field of quantitative self-monitoring advances, these platforms offer researchers valuable tools for detailed hormone pattern analysis outside traditional laboratory settings, with particular promise for special populations and luteal phase characterization studies.
For researchers and developers in the field of digital fertility technologies, understanding the U.S. Food and Drug Administration (FDA) regulatory framework is essential for study design and product development. The FDA categorizes and regulates medical devices based on their risk profile, leading to distinct pathways for market entry: establishment registration and device listing versus premarket notification (510(k)) or approval (PMA).
Registration is an annual requirement for device establishments that informs the FDA of the facility's existence and activities but does not equate to an evaluation of the device's safety or effectiveness [51]. Clearance via the 510(k) pathway requires demonstrating that a new device is "substantially equivalent" to a legally marketed predicate device [52]. Approval through the Premarket Approval (PMA) pathway involves a rigorous scientific review for high-risk devices to demonstrate reasonable assurance of safety and effectiveness [53].
Table: Key FDA Regulatory Pathways for Medical Devices
| Pathway | Legal Basis | Level of Scrutiny | Typical Device Examples | Common for Fertility Trackers |
|---|---|---|---|---|
| Establishment Registration & Listing | 21 CFR Part 807 | Low - Identifies facilities and devices | Bandages, examination gloves | Basic cycle tracking apps without medical claims |
| 510(k) Clearance | Section 510(k) of FD&C Act | Moderate - Substantial equivalence to predicate | Pulse oximeters, infusion pumps | Fertility apps used for contraception (e.g., Natural Cycles) |
| PMA Approval | Section 515 of FD&C Act | High - Scientific evidence of safety & effectiveness | Pacemakers, implantable defibrillators | Not typically used for fertility tracking devices |
Device Classification and Regulatory Impact
Risk-Based Classification System
The FDA's three-tiered classification system directly determines the regulatory pathway and evidence requirements for fertility tracking devices [52]:
- Class I (Low Risk): Devices with minimal potential for harm. Most are exempt from premarket notification but require establishment registration and listing. Examples include manual surgical instruments and basic tracking apps without diagnostic or contraceptive claims.
- Class II (Moderate Risk): Devices where general controls alone are insufficient to provide reasonable assurance of safety and effectiveness. These require special controls such as performance standards, post-market surveillance, and patient registries. Most fertility tracking devices with medical claims fall into this category.
- Class III (High Risk): Devices that support or sustain human life, are of substantial importance in preventing impairment of human health, or present potential unreasonable risk of illness or injury. These require PMA approval and typically involve extensive clinical data.
Fertility Device Classification Examples
Recent regulatory actions demonstrate how specific fertility technologies have been classified. Natural Cycles became the first FDA-cleared birth control app in 2018 through the de novo pathway and has subsequently received 510(k) clearances for integrations with wearable technologies including Oura Ring (2021) and Apple Watch (2023) [54]. Other fertility tracking devices like Tempdrop and Kegg are FDA-registered as Class I devices, allowing them to market with more limited medical claims [55] [56].
Table: Fertility Tracking Device Classification Examples
| Device/App | FDA Classification | Regulatory Pathway | Technology/Method | Intended Use |
|---|---|---|---|---|
| Natural Cycles | Class II | De Novo → 510(k) | Algorithm analyzing basal body temperature | Birth control and pregnancy planning |
| Tempdrop | Class I | Establishment Registration | Wearable basal body temperature sensor | Fertility awareness and cycle tracking |
| Kegg | Class I | Establishment Registration | Cervical fluid impedance tracking | Fertility awareness and cycle tracking |
| PherDal | Class II | 510(k) Clearance | Intravaginal insemination kit | At-home conception assistance |
Experimental Protocols for Regulatory Submissions
Protocol 1: Substantial Equivalence Testing for 510(k) Clearance
For developers seeking 510(k) clearance for a fertility tracking device, establishing substantial equivalence to a predicate device requires rigorous comparative testing.
Objective: Demonstrate that the new device is as safe and effective as a legally marketed predicate device without raising new questions of safety or effectiveness.
Materials:
- Test device and predicate device(s)
- Study population representing intended use (age, health status, etc.)
- Validated reference standard for comparison
- Data collection and analysis infrastructure
Methodology:
- Predicate Identification: Identify an appropriate predicate device with similar technological characteristics and intended use [52].
- Performance Testing: Conduct comparative analytical studies including:
- Accuracy studies comparing fertility predictions to established biomarkers (e.g., urinary LH surge, progesterone levels)
- Precision/reproducibility studies across multiple lots and operators
- Usability testing to ensure correct use by intended population
- Software Validation: For algorithm-based devices, verify and validate software performance including:
- Algorithm training and testing on diverse datasets
- Cybersecurity testing per FDA guidance [54]
- Failure mode and effects analysis
- Clinical Validation: For devices making physiological claims, conduct clinical studies comparing device outputs to clinically accepted reference standards.
Data Analysis:
- Calculate sensitivity, specificity, positive and negative predictive values for fertility prediction
- Perform statistical testing for non-inferiority compared to predicate
- Analyze subgroup performance (e.g., across different cycle regularity patterns)
Protocol 2: Clinical Performance Validation for Urinary Hormone Measurements
For research validating urinary reproductive hormone measurements via smartphone readers, comprehensive analytical and clinical validation is essential.
Objective: Establish the accuracy, precision, and clinical utility of urinary hormone measurements obtained through a smartphone-based reader system.
Materials:
- Smartphone reader hardware with optical sensors
- Lateral flow immunoassay test strips
- Reference standard (laboratory-based hormone assays)
- Control materials with known hormone concentrations
- Study population meeting inclusion/exclusion criteria
Experimental Workflow:
Methodology:
- Precision Studies:
- Within-run precision: Analyze 20 replicates each of low, medium, and high concentration samples in a single run
- Between-run precision: Analyze controls in duplicate across 10 different days
- Calculate coefficients of variation (CV) with acceptance criteria typically <15%
Method Comparison:
- Test a minimum of 100 clinical samples spanning the assay measuring range
- Compare smartphone reader results with reference laboratory method using:
- Passing-Bablok regression analysis
- Bland-Altman difference plots
- Deming regression for methods with comparable precision
Clinical Sensitivity and Specificity:
- Establish clinical cut-off values using ROC curve analysis
- Determine sensitivity and specificity for detecting ovulation or fertile window
- Compare to established reference methods (e.g., transvaginal ultrasound for ovulation confirmation)
Interference Testing:
- Test potential interferents including blood, protein, specific gravity variations
- Assess cross-reactivity with structurally similar hormones
Acceptance Criteria:
- Correlation coefficient (r) ≥0.95 compared to reference method
- Total error within established clinical requirements
- ≥95% agreement with reference method for categorical results (fertile/non-fertile)
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Fertility Technology Validation Studies
| Research Tool | Function/Purpose | Application in Validation Studies |
|---|---|---|
| Reference Hormone Assays | Gold-standard measurement of reproductive hormones | Method comparison and accuracy determination |
| Characterized Urine Panels | Samples with known hormone concentrations across clinical range | Precision, linearity, and reportable range studies |
| Lateral Flow Immunoassay Strips | Solid-phase chromatographic immunoassays for hormone detection | Point-of-care testing component for smartphone readers |
| Algorithm Training Datasets | Curated datasets with hormonal and physiological parameters | Development and validation of predictive algorithms |
| Quality Control Materials | Stable materials with predetermined hormone concentrations | Monitoring assay performance over time |
| Clinical Reference Standards | Established methods for fertility assessment (e.g., ultrasound) | Determining clinical sensitivity and specificity |
Regulatory Strategy and Decision Framework
The regulatory pathway for a fertility tracking device depends on its intended use, technological characteristics, and risk profile. The following decision framework illustrates the process for determining the appropriate FDA regulatory pathway:
Key Strategic Considerations
Intended Use Determination: The claims made about a device's function primarily drive classification. Apps that simply track menstrual cycles without providing fertility status or contraceptive guidance typically fall into Class I, while those providing specific fertility status or serving as contraception require Class II classification [57] [54].
Predicate Device Selection: For 510(k) submissions, identifying an appropriate predicate is critical. The Natural Cycles app now serves as a predicate for other digital fertility awareness methods, establishing a regulatory pathway for similar technologies [54].
Software as a Medical Device (SaMD) Considerations: Fertility tracking apps must comply with quality system regulations, including design controls, cybersecurity requirements, and interoperability standards when integrating with other devices like smartwatches [54].
The regulatory landscape for fertility tracking devices requires careful navigation of distinct FDA pathways. Establishment registration provides market entry for low-risk devices, while 510(k) clearance demands demonstration of substantial equivalence to predicate devices for moderate-risk applications. For researchers validating urinary reproductive hormone measurement technologies, robust experimental protocols encompassing analytical performance validation and clinical utility assessment are essential components of regulatory submissions. Understanding these pathways enables efficient development of innovative fertility technologies that meet regulatory requirements while advancing reproductive health research.
Conclusion
Smartphone-connected readers for urinary reproductive hormone measurement represent a significant advancement in decentralized health monitoring, demonstrating robust analytical validity against gold-standard laboratory methods. These devices provide researchers with powerful tools for collecting real-world, quantitative hormone data at scale, enabling deeper insights into menstrual cycle variability and personalized health trajectories. Future directions should focus on validating these technologies in more diverse populations, including those with medical conditions like PCOS, and expanding their application beyond fertility to broader health monitoring areas such as menopause and metabolic health. The integration of multi-hormone data with AI-driven analytics promises to further personalize healthcare and democratize access to precise hormonal insights, ultimately bridging critical gaps in women's health research and clinical practice.
References
- 1. of Validation reproductive urinary measurements using... hormone [https://pmc.ncbi.nlm.nih.gov/articles/PMC10247788/]
- 2. Lateral Flow Assay: A Summary of Recent Progress for Improving Assay Performance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10526804/]
- 3. Towards Portable and Accurate Quantification of Lateral ... Flow Assays [https://chemrxiv.org/engage/chemrxiv/article-details/68e0af62bc2ac3a0e0532a0b]
- 4. Validation of urinary reproductive hormone measurements using a novel smartphone connected reader | Scientific Reports [https://www.nature.com/articles/s41598-023-36539-w]
- 5. Machine Learning-Based Quantification of Lateral Using... Flow Assay [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763061/]
- 6. Lateral flow assay sensitivity and signal enhancement via laser µ-machined constrains in nitrocellulose membrane | Scientific Reports [https://www.nature.com/articles/s41598-024-74407-3]
- 7. A perspective on computer vision in biosensing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10787640/]
- 8. Validation of urinary reproductive hormone measurements using a novel smartphone connected reader - PubMed [https://pubmed.ncbi.nlm.nih.gov/37286704/]
- 9. Hormometer provides instant at-home hormone level readings [https://www.dezeen.com/2025/01/07/hormometer-hormone-test-eli-health-ces-2025/]
- 10. Eli Health Introduces Hormometer: Advanced Hormone ... | Ubergizmo [https://www.ubergizmo.com/2025/01/eli-health-introduces-hormometer-advanced-hormone-analysis-through-saliva/]
- 11. ОVUL - Fertility Monitor ( Hormone & Ovulation Tracker Device) [https://ovul.ai/]
- 12. Artificial Intelligence for Drug Development | FDA [https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/artificial-intelligence-drug-development]
- 13. The emerging influence of digital on... | Rock biomarkers Health [https://rockhealth.com/insights/the-emerging-influence-of-digital-biomarkers-on-healthcare/]
- 14. JMIR mHealth and uHealth - Harnessing Consumer Wearable Digital ... [https://mhealth.jmir.org/2024/1/e54622]
- 15. Collection & Analysis for Digital ' Biomarker | Labfront Women s Health [https://www.labfront.com/research/womens-health]
- 16. DUTCH Cycle Mapping (Dried Urine ) by Precision Analytical (DUTCH) [https://www.rupahealth.com/lab-tests/dutch-dutch-cycle-mapping-dried-urine]
- 17. Diagnostics | SpringerLink Hormonal Smartphone [https://link.springer.com/protocol/10.1007/978-1-4939-7614-0_38]
- 18. Validating At-Home Urinary Hormone Measurements in Postpartum and Perimenopause Fertility Transitions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12040536/]
- 19. Innovative Urinalysis Test Strips with ID bands [https://www.siemens-healthineers.com/ar/point-of-care-testing/featured-topics-in-poct/urinalysis-featured-topics/innovative-urinalysis-test-strips-id-bands?zone=zone_es_AR]
- 20. Preparing Urinalysis Test Strips Job Aid | Siemens Healthineers... [https://pep.siemens-info.com/_/en-us/clinitek-advantus-prepare-urine-test-strips-pdf/]
- 21. How to Use Pool Test Strips [Video Guide] – Taylor Technologies [https://taylortechnologies.com/blogs/news/how-to-test-guide-pool-test-strips]
- 22. of Validation using... urinary reproductive hormone measurements [https://www.nature.com/articles/s41598-023-36539-w?error=cookies_not_supported&code=dc0ac276-fa31-442c-8062-ed2ab775e744]
- 23. How to Monitor Hydration Status and Urine Dilution in Patients with Nephrolithiasis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10097240/]
- 24. Detection of low urine output by measuring urinary biomarkers [https://bmcnutr.biomedcentral.com/articles/10.1186/s40795-024-00823-3]
- 25. Characterizing Hydration Practices in Healthy Young Recreationally... [https://pubmed.ncbi.nlm.nih.gov/37225169/]
- 26. Does having clear urine really mean you're well hydrated?! [https://www.precisionhydration.com/performance-advice/hydration/does-having-clear-pee-really-mean-youre-well-hydrated/]
- 27. Mobile Technology Application for Improved Urine Concentration Measurement Pilot Study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5998741/]
- 28. of Validation using... urinary reproductive hormone measurements [https://www.nature.com/articles/s41598-023-36539-w?error=cookies_not_supported&code=58de498e-02ad-49ca-949c-e3f88c9ca138]
- 29. Predicting serum hormone concentration by estimation of urinary hormones through a home-use device - PubMed [https://pubmed.ncbi.nlm.nih.gov/36654688/]
- 30. Pregnancy Test: When To Take, Types, Accuracy & Results [https://www.metropolisindia.com/blog/preventive-healthcare/when-to-take-a-pregnancy-test]
- 31. Smartphone-based rapid quantitative detection of luteinizing hormone using gold immunochromatographic strip - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0925400517324942]
- 32. Confirmation of ovulation from urinary progesterone analysis: assessment of two automated assay platforms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6279762/]
- 33. An AI-based quantitative home-use framework for assessing fertility ... [https://www.medrxiv.org/content/10.1101/2021.05.11.21257023v1.full]
- 34. Direct microfluidic antibiotic resistance testing in urine with... [https://pubmed.ncbi.nlm.nih.gov/35498063/]
- 35. - Lot - to Variance in Immunoassays—Causes, Consequences, and... Lot [https://pmc.ncbi.nlm.nih.gov/articles/PMC10252387/]
- 36. Fertility Hormones Explained and How to Track Efficiently with Oova [https://www.oova.life/blog/fertility-hormones-explained-how-to-track-oova]
- 37. Quantifying the variability in the assessment of reproductive ... hormone [https://pubmed.ncbi.nlm.nih.gov/37977226/]
- 38. Using Quantitative Hormonal Fertility Monitors to Evaluate the Luteal Phase: Proof of Concept Case Study [https://www.mdpi.com/1648-9144/59/1/140]
- 39. Evaluating urinary estrogen and progesterone metabolites using dried... [https://bmcchem.biomedcentral.com/articles/10.1186/s13065-019-0539-1]
- 40. Detection of ovulation, a review of currently available methods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5689497/]
- 41. of Confirmation from urinary progesterone analysis... ovulation [https://www.nature.com/articles/s41598-018-36051-6?error=cookies_not_supported]
- 42. Complete Cycle Mapping Using a Quantitative At-Home Hormone... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9783738/]
- 43. Using Quantitative Hormonal Fertility to Evaluate the Luteal... Monitors [https://pmc.ncbi.nlm.nih.gov/articles/PMC9866173/]
- 44. A Complete Guide to Testing with the Inito Fertility Monitor [https://blog.inito.com/a-complete-guide-to-testing-with-the-inito-fertility-monitor/]
- 45. Mira Fertility [https://join.miracare.com/]
- 46. VS Mira : What's the Best ClearBlue ? – Fertility ... Monitor Mira Fertility [https://shop.miracare.com/blogs/resources/mira-vs-clearblue-whats-the-best-fertility-monitor]
- 47. Oova Hormone Monitoring Kits - Fertility & Perimenopause Tracking [https://www.oova.life/]
- 48. A Nurse Reviews the Clearblue Fertility Monitor [https://www.vitaefertility.com/clearblue-fertility-monitor-review/]
- 49. Tracker Review: How to Use It, Pros and Cons, and More Mira Fertility [https://www.healthline.com/health/fertility/mira-fertility-tracker]
- 50. Clearblue Fertility Monitor Review [https://www.thedailybeast.com/clearblue-fertility-monitor-review/]
- 51. The Complete Guide to FDA Medical Device Registration & Listing - Registrar Corp [https://www.registrarcorp.com/blog/medical-devices/medical-device-registration/fda-medical-device-registration-listing/]
- 52. Do I Need FDA Approval, Clearance , or Exemption? 2025 Medical... [https://www.complizen.ai/post/do-i-need-fda-approval-medical-device-guide]
- 53. FDA medical device registration process - getting new products to market in the U.S. [https://www.rimsys.io/blog/fda-medical-device-registration-process]
- 54. Natural Cycles receives FDA Clearance to integrate its birth control app with data measured by Apple Watch - BioSpace [https://www.biospace.com/natural-cycles-receives-fda-clearance-to-integrate-its-birth-control-app-with-data-measured-by-apple-watch]
- 55. Kegg Fertility Review | Fast and accurate, or too pricey? [ 2025 ] [https://www.innerbody.com/kegg-fertility-review]
- 56. Tempdrop [https://www.tempdrop.com/a/blog/device/best-fertility-and-ovulation-trackers-for-a-baby]
- 57. The 4 Best Fertility Apps of 2025 [https://www.healthline.com/health/pregnancy/fertility-apps]