Strategies for Managing Breakthrough Puberty During Hormone Suppression Therapy: Mechanisms, Monitoring, and Clinical Interventions
This article provides a comprehensive analysis of breakthrough puberty during gonadotropin-releasing hormone agonist (GnRHa) therapy, a significant clinical challenge across multiple therapeutic areas including precocious puberty, transgender care, and oncology.
Strategies for Managing Breakthrough Puberty During Hormone Suppression Therapy: Mechanisms, Monitoring, and Clinical Interventions
Abstract
This article provides a comprehensive analysis of breakthrough puberty during gonadotropin-releasing hormone agonist (GnRHa) therapy, a significant clinical challenge across multiple therapeutic areas including precocious puberty, transgender care, and oncology. We examine the underlying mechanisms of incomplete ovarian and testicular suppression, explore incidence rates ranging from 3.6% to 50% depending on diagnostic thresholds and patient populations, and identify key risk factors including young age, high BMI, and specific drug formulations. The review synthesizes current evidence on monitoring protocols, treatment optimization strategies, and comparative effectiveness of therapeutic approaches. For researchers and drug development professionals, we highlight critical knowledge gaps and future directions for developing next-generation suppression therapies with improved efficacy and safety profiles.
Understanding Breakthrough Puberty: Mechanisms and Clinical Significance in Hormone Suppression Therapy
Within research on hormone suppression therapies, incomplete puberty suppression—also termed breakthrough puberty—presents a significant challenge. It refers to the insufficient suppression of the hypothalamic-pituitary-gonadal (HPG) axis, allowing for the progression of puberty despite therapeutic intervention. This phenomenon is critically relevant for studies on central precocious puberty (CPP) and gender-affirming care in adolescents. For researchers and drug development professionals, accurately defining and monitoring this state is essential for assessing therapeutic efficacy, optimizing dosing regimens, and evaluating long-term outcomes. This technical guide outlines the clinical parameters, hormonal thresholds, and troubleshooting methodologies essential for identifying and managing breakthrough puberty in a research setting.
FAQ: Core Concepts for Researchers
Q1: What defines incomplete puberty suppression in a clinical trial context? Incomplete suppression is a biochemical state where gonadotropin-releasing hormone agonist (GnRHa) therapy fails to adequately suppress the HPG axis to prepubertal levels, potentially allowing for the progression of secondary sexual characteristics. It is defined by specific hormonal and clinical parameters, detailed in Section 4.
Q2: Which hormonal parameter is more reliable for detecting breakthrough activity? The GnRH stimulation test is the gold standard for confirming suppression. A stimulated luteinizing hormone (LH) peak >3.1 - 5.0 IU/L is often used as a threshold indicating insufficient suppression [1]. Basal LH concentrations are not a reliable proxy. One study found that 87.8% of girls with adequately suppressed CPP had pubertal basal LH (≥0.3 IU/L) at least once during treatment, and the specificity of basal LH for predicting non-suppression was only 12.0% [1].
Q3: What are the primary clinical consequences of incomplete suppression? The main consequences include advancement of bone age (BA), accelerated growth velocity, and progression of secondary sexual characteristics (e.g., breast development or testicular growth) [2]. In transgender and gender-diverse youth research, a key consequence is the potential worsening of gender dysphoria and its associated psychological comorbidity [3] [2].
Q4: What are the key limitations in the current evidence base? Robust evidence is lacking. A 2024 systematic review concluded that existing studies are "inadequate in number, small in size, uncontrolled and relatively short-term," making it difficult to draw firm conclusions on efficacy and safety [4]. Large, long-term randomized controlled trials are needed [2].
Troubleshooting Guide: Managing Breakthrough Puberty
When incomplete suppression is suspected in a study cohort, follow this systematic troubleshooting guide.
| Suspected Issue | Diagnostic Action | Potential Corrective Action |
|---|---|---|
| Insufficient Dosing / Wrong Interval | Perform a GnRH stimulation test. Review injection records and formulation. | Shorten the interval between injections (e.g., from 4-week to 3-week cycles) [1]. Consider a higher-dose formulation. |
| Poor Drug Delivery/Compliance | Verify administration technique for subcutaneous implants/injections. Monitor adherence. | Re-train personnel on administration protocols. Implement stricter compliance monitoring. |
| Individual Pharmacokinetic Variability | Measure pre-injection (trough) and post-injection hormone levels. | Perform therapeutic drug monitoring to establish individual clearance patterns and optimize dosing. |
| Advanced Puberty at Treatment Initiation | Record Tanner stage and bone age at baseline. | Recognize that suppression may be less complete if treatment begins at later Tanner stages (e.g., IV-V) [2]. |
Quantitative Parameters and Thresholds
Researchers should monitor the following multi-modal parameters to definitively assess suppression status. The following table synthesizes key quantitative findings from recent literature.
Table 1: Clinical and Hormonal Parameters for Assessing Puberty Suppression
| Parameter | Definition of Suppression | Threshold for Incomplete Suppression | Key Evidence |
|---|---|---|---|
| GnRH-Stimulated LH | Suppressed peak LH post-stimulation | Peak LH >3.1 - 5.0 IU/L | In a study of 74 girls, a repeat GnRH test was the gold standard; none with a stimulated LH >3.1 IU/L showed clinical progression [1]. |
| Basal LH | Not a reliable standalone marker | Pre-injection basal LH ≥0.3 IU/L is common and does not alone indicate failure. | 53.5% of all pre-injection blood samples had basal LH ≥0.3 IU/L in a fully suppressed cohort [1]. |
| Bone Age (BA) Advance | BA advancement slows to align with chronological age | Significant advancement of BA over chronological age (BA/CA >1) during treatment. | Treatment aims to reduce bone age advance; its persistence indicates poor control [1] [2]. |
| Growth Velocity | Decrease in height standard deviation score (SDS) | Persistence of elevated, pubertal growth velocity. | A significant reduction in height SDS is expected with effective suppression (p<0.001) [1]. |
| Physical Exam (Tanner Staging) | Halting of pubertal progression | Any progression of breast (girls) or testicular (boys) development. | Lack of breast tissue development was a key clinical sign of effective suppression despite elevated basal LH [1]. |
| Bone Mineral Density (BMD) | Stable or increasing BMD Z-scores | Decreasing BMD Z-scores during treatment. | A 2-year treatment with GnRHa may result in bone mass accrual retardation [4] [2]. |
Essential Experimental Protocols
Protocol: GnRH Stimulation Test
This protocol is critical for definitively diagnosing incomplete suppression [1].
Objective: To assess the degree of HPG axis suppression by measuring the pituitary release of LH and FSH in response to a GnRH stimulus. Reagents:
- Gonadorelin (0.1 mg) or Leuprolide.
- Supplies for intravenous access and blood collection. Methodology:
- Insert an intravenous (IV) line.
- Administer Gonadorelin (0.1 mg) intravenously as a bolus.
- Collect blood samples for LH and FSH measurement at time points -5, 0, 30, and 60 minutes post-injection.
- Process serum samples immediately and freeze at -20°C until analysis via electro-chemiluminescence immunoassay or similar. Interpretation: A peak stimulated LH level below 3.1 IU/L (or <5.0 IU/L, depending on the assay and institutional cutoff) is typically indicative of adequate suppression. Levels above this threshold suggest breakthrough pubertal activity.
Protocol: Multi-Modal Clinical Assessment
This overarching protocol ensures a comprehensive evaluation of pubertal status.
Objective: To integrate biochemical, radiological, and clinical data to evaluate therapeutic efficacy. Methodology:
- Clinical Examination: Every 3-6 months, a trained clinician should assess Tanner staging for breast/genitalia and pubic hair.
- Auxology: Measure height and weight every 3-6 months. Calculate Height Standard Deviation Score (SDS) and Body Mass Index (BMI) SDS based on population references.
- Radiography: Obtain a bone age X-ray of the left hand and wrist every 12 months. Assess according to Greulich & Pyle or Tanner-Whitehouse methods.
- Biochemistry:
- Regular monitoring: Measure pre-injection basal LH, FSH, and sex steroids (estradiol/testosterone) every 3-6 months.
- Confirmatory testing: Perform a GnRH stimulation test if clinical (progression of Tanner stage, elevated growth velocity) or biochemical (consistent elevation of basal LH or sex steroids) signs suggest breakthrough puberty.
- Bone Health Monitoring: Conduct dual-energy X-ray absorptiometry (DXA) scans annually to monitor BMD.
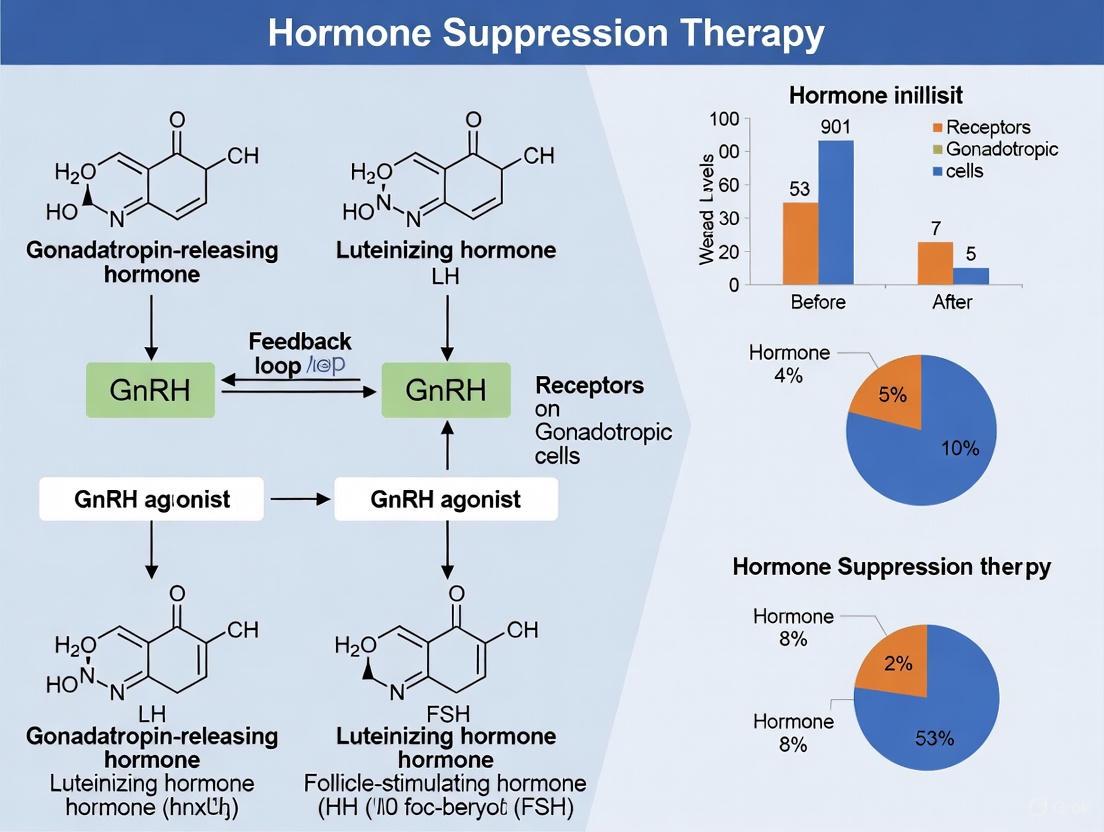
Signaling Pathways and Experimental Workflow
HPG Axis and GnRHa Suppression Mechanism
The following diagram illustrates the physiological HPG axis and the mechanism of action of GnRHa therapy.
Diagnostic Workflow for Breakthrough Puberty
This workflow provides a logical algorithm for identifying and managing incomplete suppression in a research cohort.
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Research Reagents and Materials
| Reagent / Material | Function in Research | Example Products / Assays |
|---|---|---|
| GnRH Agonists (GnRHa) | The primary intervention to suppress the HPG axis. Different formulations allow for testing of dosing and delivery. | Leuprorelin, Triptorelin, Goserelin, Histrelin [2]. |
| Immunoassay Kits | Quantifying hormone levels (LH, FSH, Estradiol, Testosterone) in serum/plasma. Critical for defining biochemical endpoints. | Electro-chemiluminescence immunoassays (e.g., Roche-Cobas) [1]. |
| GnRH (for stimulation test) | Diagnostic agent used in the gold-standard test to challenge the pituitary and assess suppression. | Gonadorelin [1]. |
| Bone Age Assessment Software | Objective and quantitative analysis of bone age from hand radiographs, a key efficacy parameter. | BoneExpert Software (Visiana Aps) [1]. |
| DXA Scanner | Monitoring bone mineral density (BMD) as a key safety parameter, tracking potential side effects of suppression. | Various commercial systems. |
Diagnostic Protocols for Breakthrough Puberty
Q: What diagnostic tests confirm breakthrough puberty during hormone suppression therapy?
A: Breakthrough puberty, characterized by the progression of pubertal development despite suppressive therapy, is confirmed through a combination of biochemical and imaging studies. The key diagnostic methodology is the Gonadotropin-Releasing Hormone (GnRH) Stimulation Test [5]. This test involves obtaining a baseline blood sample, administering a shot of GnRH hormone, and then taking repeated blood samples over time to measure the response of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). A significant rise in these gonadotropins after stimulation indicates central activation of the hypothalamic-pituitary-gonadal (HPG) axis, diagnostic of central precocious puberty (CPP) or breakthrough CPP during therapy [5] [6]. Additional essential diagnostics include:
- Bone Age X-ray: An X-ray of the left hand and wrist to assess bone maturation. Accelerated bone age advancement beyond chronological age is a hallmark of active sex steroid effect and a key indicator of treatment failure [5] [6].
- Hormone Assays: Baseline blood tests to measure LH, FSH, estradiol (in females), and testosterone (in males) [5] [6].
- Pelvic/Testicular Ultrasound: Used particularly when peripheral precocious puberty is suspected, to identify estrogen or testosterone-secreting cysts or tumors [5].
- Brain MRI: Recommended to rule out central nervous system abnormalities, such as hypothalamic hamartomas or other tumors, that may be driving the HPG axis reactivation, especially in younger patients or boys [5] [6].
Q: What is the detailed experimental protocol for the GnRH stimulation test?
A: The GnRH stimulation test is the gold-standard biochemical assay for confirming HPG axis activation [5].
Materials:
- GnRH agonist (e.g., leuprorelin)
- Sterile syringes and needles for injection and blood collection
- Blood collection tubes (serum)
- Centrifuge
- Access to a clinical laboratory with capabilities for chemiluminescence or immunoassay for LH and FSH
Methodology:
- Pre-test Preparation: Schedule the test in the morning. Fasting is not required.
- Baseline Sample: Draw a venous blood sample for baseline LH and FSH levels.
- GnRH Administration: Administer a subcutaneous or intravenous injection of the GnRH agonist (e.g., 100 mcg of leuprorelin).
- Post-Stimulation Samples: Draw subsequent blood samples at timed intervals, typically at 30 and 60 minutes post-injection. Some protocols may extend to 120 minutes.
- Sample Processing: Allow blood to clot, centrifuge, and aliquot serum for immediate analysis or frozen storage.
- Data Interpretation: A peak LH response greater than 5-8 IU/L (depending on the specific assay and protocol) is generally considered diagnostic of central precocious puberty activation, indicating a pubertal response of the pituitary gland [5].
Quantitative Data on Pubertal Timing and Treatment
Table 1: Normative and Diagnostic Age Ranges for Pubertal Onset
| Population / Condition | Typical Age of Onset | Definition of Precocious Puberty | Definition of Delayed Puberty |
|---|---|---|---|
| Females (General Population) | 8 to 13 years [7] | Before 7.5 - 8 years [5] [8] [6] | No breast development by 13 years or no menarche by 16 years [9] |
| Males (General Population) | 9 to 14 years [7] | Before 9 years [5] [8] [6] | No testicular enlargement by 14 years [9] |
| Transgender Youth (GnRHa Treatment) | Varies; treatment starts after pubertal onset (Tanner stage 2-3) [10] | N/A | N/A |
Table 2: Documented Outcomes of Puberty Suppression Therapy
| Outcome Measure | Findings in Transgender Youth | Findings in Central Precocious Puberty |
|---|---|---|
| Mental Health Impact | 67% lower odds of lifetime suicidal ideation in those who received wanted pubertal suppression vs. those who did not [11]. | Treatment aims to reduce emotional distress and social difficulties associated with early development [5] [6]. |
| Physical Efficacy | Effective suppression of unwanted pubertal development [10]. | Arrests progression of secondary sexual characteristics; slows accelerated bone age advancement [5] [12]. |
| Key Monitoring Parameters | Bone density, body composition, psychological wellbeing [10] [13]. | Growth velocity, breast/testicular size, bone age, GnRH-stimulated LH levels [12]. |
Troubleshooting Breakthrough Puberty in Research Settings
Q: A research subject on GnRH agonist therapy shows signs of progressive breast development and accelerated growth velocity. What is the systematic troubleshooting workflow?
A: This clinical scenario suggests potential breakthrough puberty and warrants a structured investigation. Adherence to this diagnostic workflow is critical for identifying the etiology.
Q: Following the workflow, what are the specific experimental protocols for investigating suspected peripheral causes?
A: If suppressed LH/FSH point to a peripheral (gonadotropin-independent) source of sex steroids, the investigation focuses on identifying autonomous hormone-producing tissue [5] [6].
Objective: To locate and characterize sources of ectopic or autonomous estrogen or testosterone production.
Materials:
- High-resolution ultrasonography system
- Blood collection equipment
- Test kits for hormone immunoassays (estradiol, testosterone, DHEAS, hCG)
Methodology:
- Pelvic/Testicular Ultrasound:
- For assigned females: Conduct a transabdominal pelvic ultrasound with a full bladder. Carefully examine the ovaries for cysts (e.g., McCune-Albright syndrome) or rare tumors. Measure uterine size and endometrial stripe thickness; a pubertal uterus indicates significant estrogen exposure.
- For assigned males: Perform a scrotal ultrasound to assess testicular volume and architecture. Look for testicular masses, such as Leydig cell tumors, which can secrete testosterone independently of LH.
Adrenal Hormone Panel: Draw blood for dehydroepiandrosterone sulfate (DHEAS), 17-hydroxyprogesterone, and testosterone. Elevated adrenal androgens may suggest congenital adrenal hyperplasia or adrenal tumors.
Human Chorionic Gonadotropin (hCG) Measurement: Particularly in males, measure serum hCG, as it can stimulate testicular testosterone production. hCG-secreting tumors (e.g., germinomas) are a rare but important cause.
Research Reagent Solutions for Key Experiments
Table 3: Essential Reagents and Materials for Puberty Research Protocols
| Research Reagent / Material | Primary Function in Experiment | Exemplary Use Case |
|---|---|---|
| GnRH Agonist (e.g., Leuprolide) | Stimulates pituitary gonadotrophs in a diagnostic test; chronically desensitizes GnRH receptor for treatment. | GnRH stimulation test; long-acting depot formulations for therapeutic suppression [5] [11] [10]. |
| LH & FSH Immunoassay Kits | Quantify gonadotropin levels in serum/plasma via chemiluminescence or ELISA. | Measuring baseline and post-stimulation LH/FSH to confirm HPG axis activation [5] [6]. |
| Estradiol/Testosterone Assays | Measure sex steroid levels in serum/plasma via highly sensitive LC-MS/MS or immunoassay. | Assessing biochemical efficacy of suppression; investigating peripheral precocious puberty [5] [6]. |
| Bone Age Atlas (e.g., Greulich-Pyle) | Standard reference for comparing hand/wrist radiographs to assign skeletal maturity. | Determining bone age to monitor tempo of maturation and predict adult height [5] [9]. |
Advanced Research Considerations and Monitoring Protocols
Q: What are the critical long-term parameters to monitor in subjects receiving prolonged pubertal suppression, and what are the associated research methodologies?
A: Long-term suppression therapy requires meticulous monitoring of several physiological systems beyond the HPG axis. Key parameters and their assessment methodologies are outlined in the following research workflow.
Q: What is the specific protocol for monitoring bone health in these subjects?
A: Bone density is a primary concern during prolonged sex steroid suppression [10] [13].
Objective: To track changes in bone mineral density (BMD) and bone metabolism over the course of treatment.
Materials:
- Dual-energy X-ray absorptiometry (DEXA) scanner
- Phantoms for calibration
- Blood collection equipment
- Assays for bone turnover markers (e.g., P1NP for formation, CTX for resorption)
Methodology:
- Baseline Assessment: Perform a DEXA scan (lumbar spine and total body less head) and obtain a bone age X-ray prior to or at the initiation of therapy. Draw blood for bone turnover markers and 25-hydroxyvitamin D.
- Longitudinal Monitoring:
- DEXA Scans: Conduct annually or biennially. Results should be reported as Z-scores (standard deviation scores compared to age- and sex-matched controls), not T-scores.
- Bone Age Annually: Essential to correlate bone density with skeletal maturation.
- Biochemical Markers: Measure bone turnover markers every 6-12 months to assess the dynamic state of bone remodeling. Expect an initial decline in markers with successful suppression.
- Adjunctive Therapy: Ensure adequate daily intake of calcium (1000-1300 mg) and vitamin D (600-1000 IU), with supplementation if necessary, to support bone mineral acquisition.
Molecular Mechanisms of GnRHa Action and Treatment Failure
FAQs: Understanding GnRHa Mechanisms and Failure
What is the primary molecular mechanism by which GnRHa suppresses puberty? Gonadotropin-releasing hormone agonists (GnRHa) are synthetic analogs of the natural GnRH decapeptide that possess greater potency and are resistant to enzymatic degradation [14]. They act by binding to GnRH receptors (GnRHR) on pituitary gonadotrope cells [15]. These receptors are G-protein coupled receptors (GPCRs) that primarily signal through Gαq/11 proteins [16]. Under normal physiological conditions, pulsatile GnRH release leads to the synthesis and secretion of gonadotropins (LH and FSH) [15]. However, continuous stimulation by GnRHa causes prolonged activation of GnRHR, leading to desensitization and down-regulation of these receptors [14] [16]. This results in suppression of gonadotropin secretion and subsequent reduction of gonadal sex hormones to pre-pubertal levels [14].
Why might GnRHa treatment fail to suppress puberty in some patients? Several factors can contribute to treatment failure:
- Insufficient dosing: The dose required for gonadal suppression varies, with higher doses (e.g., leuprolide 7.5-15 mg/28 days) sometimes needed, particularly in heavier patients [14].
- Individual variation in drug metabolism: Genetic factors affecting drug metabolism or receptor sensitivity can influence treatment response [14].
- Advanced bone age at initiation: GnRHa is most effective for improving final adult height when initiated in younger children (<6 years) with significant bone age advancement [14].
- Poor adherence to injection schedule: Missing doses or extended intervals between administrations can allow recovery of pituitary-gonadal axis activity [14].
What are the key signaling pathways activated by GnRHR? GnRHR activation triggers multiple interconnected signaling pathways [16]:
- Gq/11-PLC pathway: Primary pathway leading to activation of phospholipase C (PLC), which hydrolyzes PIP2 to generate IP3 and DAG [15] [16].
- Calcium mobilization: IP3 stimulates calcium release from endoplasmic reticulum [17] [16].
- Protein Kinase C activation: DAG activates PKC isoforms, which phosphorylate downstream targets [17] [16].
- MAPK pathway: Both ERK1/2 activation through PKC-dependent and potentially arrestin-dependent mechanisms [16].
- Cyclic nucleotide modulation: GnRHR can also influence cAMP and cGMP levels through cross-talk with other signaling systems [16].
How can researchers troubleshoot inadequate hormone suppression in experimental models?
- Verify receptor binding affinity: Test different GnRHa analogs (leuprolide, triptorelin, goserelin) with varying receptor affinities [14].
- Optimize administration frequency: Consider shorter intervals between doses (21-26 days instead of 28 days) for some patients [14].
- Monitor suppression criteria: Ensure luteinizing hormone (LH) suppresses to <3 mIU/mL after stimulation testing [14].
- Check for antibody formation: In rare cases, neutralizing antibodies might develop against specific analogs [18].
What cellular adaptations contribute to GnRHa resistance?
- Receptor desensitization patterns: The mammalian type I GnRHR lacks an intracellular C-terminal tail, making it resistant to rapid desensitization compared to other GPCRs [16].
- Altered pulsatility recovery: If GnRHa concentrations fluctuate, the pituitary may resume pulsatile response patterns [15].
- Post-receptor signaling adaptations: Changes in downstream signaling components like protein kinase C isoforms or calcium handling proteins [17] [16].
Table 1: Incidence of Significant Adverse Drug Reactions to GnRHa Therapy
| Adverse Reaction | Incidence | Clinical Management |
|---|---|---|
| Sterile abscess formation | 0.6% of patients (4 events in 3 of 621 patients) [18] | Switch to different GnRHa formulation; change injection site; symptomatic care [18] |
| Anaphylaxis | 0.16% of patients (1 of 621 patients) [18] | Immediate emergency care; discontinuation of triggering agent [18] |
| Slipped capital femoral epiphysis (SCFE) | 0.16% of patients (1 of 621 patients) [18] | Orthopedic consultation; surgical intervention [18] |
| Headaches, hot flushes, mood swings | Commonly reported but not quantified [14] | Supportive care; typically transient [14] |
Table 2: Efficacy of GnRHa Monotherapy vs. Combination Therapy on Growth Outcomes
| Outcome Measure | GnRHa Monotherapy | GnRHa + GH Combination Therapy | Treatment Effect (WMD) |
|---|---|---|---|
| Final Height (FH) | Baseline reference | No significant improvement (WMD = 0.14 cm, 95% CI: -1.66 to 1.94) [19] | P = 0.88 |
| Final Height minus Target Height (FH-TH) | Baseline reference | Significant improvement (WMD = 1.01 cm, 95% CI: 0.28 to 1.73) [19] | P = 0.006 |
| Predicted Adult Height (PAH) | Baseline reference | Significant improvement (WMD = 4.27 cm, 95% CI: 3.47 to 5.08) [19] | P < 0.0001 |
| Height Gain | Baseline reference | Significant improvement (WMD = 3.45 cm, 95% CI: 1.73 to 5.17) [19] | P < 0.0001 |
| Growth Velocity | Baseline reference | Significant improvement (WMD = 1.40 cm/year, 95% CI: 0.90 to 1.91) [19] | P < 0.0001 |
| Bone Maturation (ΔBA/ΔCA) | Baseline reference | No significant effect (WMD = 0.01, 95% CI: -0.05 to 0.07) [19] | P = 0.77 |
Experimental Protocols
Protocol 1: Assessing GnRHa-Induced Suppression of the HPG Axis
Objective: Evaluate the efficacy of GnRHa in suppressing the hypothalamic-pituitary-gonadal (HPG) axis in experimental models.
Materials:
- GnRHa (leuprolide, triptorelin, or goserelin)
- Animal model (typically peripubertal rodents) or primary pituitary cell culture
- ELISA kits for LH, FSH, and sex steroids
- GnRH receptor binding assay components
- Real-time PCR reagents for gonadotropin subunit mRNA quantification
Methodology:
- Administration: Administer GnRHa via subcutaneous or intramuscular injection at appropriate doses (e.g., 60-120 μg/kg for triptorelin) [14].
- Blood sampling: Collect serial blood samples at predetermined intervals (0, 30, 60, 120 minutes post-injection) for hormone measurement.
- Stimulation testing: Perform GnRH stimulation tests (using native GnRH) at baseline and after treatment to assess pituitary suppression.
- Tissue collection: Harvest pituitary glands for receptor quantification and mRNA analysis.
- Hormone assays: Measure LH, FSH, and sex steroid levels using validated ELISA or RIA.
- Receptor analysis: Assess GnRHR density and binding affinity using radioligand binding assays.
- Gene expression: Quantify mRNA levels for gonadotropin subunits (α, LHβ, FSHβ) using real-time PCR.
Interpretation: Effective suppression is demonstrated by reduced basal and GnRH-stimulated gonadotropin levels, decreased gonadotropin subunit mRNA, and downregulation of GnRHR.
Protocol 2: Investigating Signaling Pathways in GnRHa Action
Objective: Elucidate the molecular mechanisms of GnRHa action and potential sites of treatment failure.
Materials:
- Alpha T3-1 gonadotrope cell line
- GnRHa ([D-Trp6]GnRH)
- Pharmacological inhibitors (PKC inhibitors: staurosporine, GF 109203X; calcium chelators)
- Calcium imaging dyes (Fura-2, Fluo-4)
- Western blot reagents for phospho-proteins
- siRNA for specific signaling components
Methodology:
- Cell culture: Maintain Alpha T3-1 cells under standard conditions.
- Stimulation experiments: Treat cells with GnRHa (10 nM) for varying durations (30 min to 24 hours) [17].
- Inhibition studies: Pre-treat cells with specific inhibitors (e.g., PKC inhibitors, calcium chelators) before GnRHa stimulation.
- Calcium imaging: Monitor intracellular calcium fluxes using ratiometric dyes.
- Protein analysis: Extract proteins at designated time points and analyze phosphorylation of ERK1/2, PKC substrates, and other signaling intermediates by Western blot.
- Gene silencing: Transfect cells with siRNA targeting specific signaling components (G-proteins, PKC isoforms) to assess their necessity.
- mRNA quantification: Measure gonadotropin subunit mRNA levels using real-time PCR [17].
Interpretation: Key signaling pathways are identified by inhibitor sensitivity patterns and phosphorylation kinetics. Treatment failure mechanisms may involve altered regulation of these pathways.
Signaling Pathway Diagrams
Research Reagent Solutions
Table 3: Essential Research Reagents for GnRHa Mechanism Studies
| Reagent | Function/Specificity | Example Applications |
|---|---|---|
| GnRHa Agonists (Leuprolide, Triptorelin, Goserelin) | Synthetic analogs with greater receptor affinity and enzymatic resistance than native GnRH [14] | In vivo suppression studies; continuous receptor activation models [14] |
| GnRH Antagonists (Cetrorelix, Ganirelix) | Competitive receptor blockers that provide immediate suppression [16] | Control experiments; distinguishing receptor-dependent effects [16] |
| PKC Inhibitors (Staurosporine, GF 109203X) | Inhibit protein kinase C signaling downstream of GnRHR [17] | Pathway dissection; determining PKC-dependent effects [17] |
| Calcium Chelators (BAPTA-AM, EGTA) | Sequester intracellular or extracellular calcium [17] | Assessing calcium-dependent signaling components [17] |
| Alpha T3-1 Cell Line | Murine pituitary gonadotrope progenitor model [17] | In vitro studies of GnRHR signaling and gene regulation [17] |
| LHRH Antibodies | Detect and quantify GnRHR expression | Receptor localization and quantification studies |
| Phospho-Specific Antibodies (pERK, pCREB) | Detect activated signaling intermediates | Monitoring pathway activation dynamics [16] |
| Gonadotropin ELISA Kits | Quantify LH and FSH protein levels | Assessing functional suppression of HPG axis [14] |
The following table synthesizes the primary risk factors for incomplete suppression or breakthrough puberty during hormone suppression therapy, as identified in current clinical literature.
Table 1: Summary of Key Risk Factors for Incomplete Suppression
| Risk Factor | Impact on Suppression Efficacy | Supporting Evidence |
|---|---|---|
| Young Age(at treatment start) | Increased risk of incomplete ovarian function suppression (OFS); younger patients show higher escape rates. [20] | Incidence of incomplete OFS is higher in younger premenopausal breast cancer patients. [20] |
| High Body Mass Index (BMI) | Positive correlation with increased risk of incomplete suppression. [20] | Identified as a significant risk factor for ovarian function escape. [20] |
| Drug Formulation(e.g., 1-month vs. 3-month) | 3-month Leuprolide Acetate (11.25 mg) shows effective suppression, reducing injection burden. [21] | 94% of CPP patients showed peak LH suppression (<3 IU/L) at 6 months with the 3-month formulation. [21] |
| No Prior Chemotherapy | Associated with a higher risk of incomplete ovarian suppression. [20] | Patients without prior chemotherapy had a greater incidence of ovarian escape. [20] |
Troubleshooting Guide: FAQs on Breakthrough Puberty
This section addresses specific challenges researchers might encounter when studying hormone suppression therapy and managing breakthrough events.
FAQ 1: What are the established risk factors for incomplete hormone suppression in study participants?
The key patient-related risk factors for incomplete suppression are young age, high body mass index (BMI), and no history of prior chemotherapy. [20] These factors should be carefully recorded and stratified in study populations to control for their confounding effects. The diagram below illustrates the logical relationship between these risk factors and the clinical outcome of incomplete suppression.
FAQ 2: How is "incomplete suppression" defined and quantitatively measured in clinical trials?
There is no single universal definition, but it is typically quantified by measuring serum hormone levels against specific thresholds after a predefined treatment period.
- Luteinizing Hormone (LH) Suppression: In Central Precocious Puberty (CPP) research, a peak stimulated LH level of <3 - 4 IU/L is often used as a criterion for successful suppression. [21]
- Estradiol (E2) Suppression: In ovarian function suppression studies, various E2 thresholds indicate incomplete suppression, including >2.72 pg/mL, >10 pg/mL, >20 pg/mL, or >30 pg/mL. [20] The incidence rate of incomplete suppression varies significantly (from 5% to 50%) depending on the chosen E2 threshold. [20]
Table 2: Key Biomarkers for Monitoring Suppression Efficacy
| Biomarker | Target Level for Suppression | Clinical/Research Context | Notes |
|---|---|---|---|
| Luteinizing Hormone (LH) | Peak stimulated < 3 - 4 IU/L [21] | Central Precocious Puberty (CPP) | Measured via stimulation test. |
| Follicle-Stimulating Hormone (FSH) | Suppressed to prepubertal levels [21] | Central Precocious Puberty (CPP) | — |
| Estradiol (E2) | Thresholds vary: <30 pg/mL is a common benchmark [20] | Ovarian Function Suppression | Different thresholds (2.72-30 pg/mL) yield different incidence rates. [20] |
| Testosterone | ≤ 30 ng/dl (equivalent to 1.04 nmole/L) in boys [21] | Central Precocious Puberty (CPP) | — |
FAQ 3: Which drug formulations are available, and how does formulation impact treatment adherence?
The formulation and dosing frequency of GnRH agonists are critical for long-term efficacy.
- 1-Month Formulations: Well-established (e.g., LA 3.75 mg, 7.5 mg). [21]
- 3-Month Formulations: Leuprolide Acetate (LA) 11.25 mg is a 3-month depot formulation. It demonstrates comparable efficacy to monthly formulations in suppressing gonadotropins and sex steroids. [21] The primary advantage is a reduced injection frequency, which is a key factor in improving treatment adherence and quality of life in long-term studies. [21]
FAQ 4: What are the recommended experimental protocols for monitoring hormone levels?
Robust monitoring is essential for accurately capturing suppression efficacy and breakthrough events.
- Protocol for LH/FSH in CPP: After administering a 3-month LA formulation (11.25 mg), mean stimulated LH levels decreased from baseline to 1.90 IU/L at 3 months and further to 0.70 IU/L at 6 months. [21] A gonadotropin-releasing hormone (GnRH) stimulation test is the standard method for assessing the hypothalamic-pituitary-gonadal (HPG) axis.
- Protocol for Estradiol Monitoring: Regular monitoring of E2 levels is recommended, especially in patients with high-risk factors for incomplete suppression. [20] The method of detection (e.g., immunoassay vs. mass spectrometry) can influence the measured values and must be consistent throughout a study. [20]
FAQ 5: What methodologies are used to assess long-term efficacy beyond hormone levels?
Beyond direct hormone measurement, several auxological and radiological parameters are used.
- Bone Age (BA) to Chronological Age (CA) Ratio: Effective treatment slows bone maturation. In CPP, the BA/CA ratio decreased by -0.30 at 12 months and -1.10 at 3 years post-treatment with LA 11.25 mg. [21]
- Growth Velocity (GV): Suppression reduces growth velocity to a more typical, prepubertal rate. GV decreased from 6.11 cm/year at 6 months to 3.60 cm/year at 12 months post-treatment. [21]
- Final Adult Height (FH): This is a critical long-term endpoint. Pharmacologic intervention, particularly when started before 8 years of age, has been shown to improve final height in girls with CPP. [22]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Methods for Hormone Suppression Research
| Item / Reagent | Function / Application in Research |
|---|---|
| Leuprolide Acetate (LA) | A Gonadotropin-Releasing Hormone Agonist (GnRHa); the core intervention for suppressing the HPG axis. Available in 1-month (3.75 mg, 7.5 mg) and 3-month (11.25 mg) depot formulations. [21] |
| GnRH (for stimulation tests) | Used to perform diagnostic stimulation tests to assess the functional suppression of the pituitary gland's response. [21] |
| Estradiol (E2) Immunoassays | Kit-based systems for measuring serum E2 levels to confirm biochemical suppression. Critical for defining incomplete OFS. [20] |
| LH & FSH Immunoassays | Kit-based systems for measuring basal and stimulated levels of gonadotropins to quantify pituitary suppression. [21] |
| Recombinant Human Growth Hormone (rhGH) | An adjunctive therapy sometimes investigated in combination with GnRHa to mitigate potential treatment-related reductions in growth velocity and final height in CPP studies. [22] |
| X-ray for Bone Age Assessment | Standard method for evaluating skeletal maturation (bone age) as a key indicator of treatment efficacy on pubertal progression. [21] |
Frequently Asked Questions (FAQs)
FAQ 1: What defines "breakthrough puberty" in a research context? Breakthrough puberty during hormone suppression therapy refers to the progression of pubertal development despite treatment with GnRH agonists (GnRHa). In a clinical setting, this is monitored by tracking physical signs such as testicular enlargement in boys or breast development in girls, alongside biochemical markers like a rise in luteinizing hormone (LH) or sex steroids (testosterone or estradiol) above prepubertal levels [12].
FAQ 2: What are the primary clinical consequences of breakthrough puberty? The primary consequence is the potential for compromised treatment efficacy. This can manifest as [23]:
- Reduced Final Adult Height: Continued advancement of bone age can lead to premature growth plate fusion.
- Progression of Unwanted Secondary Sexual Characteristics: This undermines the primary goal of puberty suppression, particularly in gender-affirming care or for preventing distress in central precocious puberty (CPP) [10].
- Decreased Bone Mineral Density (BMD): While BMD often recovers after treatment cessation, breakthrough puberty may disrupt the expected trajectory of bone mineral accretion [23].
FAQ 3: Which patient factors most significantly influence treatment outcomes? The stage of pubertal development at the initiation of suppression therapy is a critical factor. Research shows that the effects of GnRHa and subsequent gender-affirming hormones on body composition are more pronounced in adolescents who are in early to mid-puberty (Tanner stages 2-3) compared to those completing puberty (Tanner stages 4-5) [24].
FAQ 4: What are the key experimental protocols for monitoring treatment efficacy? Standard monitoring involves a multi-faceted approach [12]:
- Clinical Assessment: Regular evaluation (every 4-6 months) of growth velocity and Tanner staging to ensure progression has arrested.
- Biochemical Testing: Conducting a GnRH stimulation test about 4 months after treatment initiation to confirm suppression of gonadotropin levels. In boys, a serum testosterone level falling below 20 ng/dL is a good indicator of efficacy.
- Radiological Evaluation: Annual bone age assessment to confirm that the rapid advancement seen prior to treatment has slowed.
Troubleshooting Guides
Issue 1: Inadequate Pubertal Suppression
Problem: During routine monitoring, a subject shows signs of continued pubertal progression (e.g., testicular growth, breast development, or accelerated linear growth).
Investigation & Resolution Protocol:
- Verify Compliance and Drug Administration: First, confirm the subject's adherence to the treatment regimen and the correct storage and administration of the GnRHa.
- Biochemical Confirmation: Perform a GnRH stimulation test and measure serum LH, FSH, and sex steroid levels. A pubertal-level LH response confirms breakthrough puberty [12].
- Assess Bone Age: Obtain a bone age X-ray to quantify the advancement since the last assessment [23].
- Corrective Actions:
- Dosage Adjustment: Consider increasing the dose of the GnRHa in accordance with the study protocol.
- Formulation Switch: Explore switching from a monthly to a longer-acting (e.g., 3-month) formulation to ensure more stable serum levels.
- Evaluate for Non-Compliance: Implement more frequent check-ins or dosing supervision if non-compliance is suspected.
Issue 2: Decline in Bone Mineral Density (BMD)
Problem: DEXA scans indicate a decrease in age-matched Z-scores for BMD during GnRHa therapy.
Investigation & Resolution Protocol:
- Establish Baseline and Monitor: Ensure a baseline DEXA scan was performed and that follow-up scans are conducted at standardized intervals (e.g., annually) [23].
- Evaluate Nutritional Status: Assess dietary intake of calcium and vitamin D. Multiple studies indicate that supplementation with calcium and vitamin D can mitigate BMD loss during treatment [23].
- Re-evaluate Treatment Necessity: For research subjects, consider the duration of GnRHa therapy. The decrease in BMD is often reversible after treatment cessation, with studies showing spontaneous restoration of bone mass 2-3 years after therapy ends [23].
Issue 3: Suboptimal Response to Subsequent Hormone Therapy
Problem: Subjects transitioning from puberty suppression to gender-affirming hormone therapy (e.g., testosterone or estrogen) show a blunted anthropometric or body composition response.
Investigation & Resolution Protocol:
- Analyze by Pubertal Stage Cohort: Stratify subject data based on their Tanner stage at the initiation of GnRHa treatment. A study found that "in puberty" trans boys (Tanner 2-3) had a significantly greater increase in lean and muscle mass during testosterone therapy compared to "completing puberty" (Tanner 4-5) individuals [24].
- Review Hormone Dosing and Levels: Ensure that the dosing of gender-affirming hormones is appropriate and that serum levels are within the target therapeutic range.
- Adjust Expectations and Protocols: Incorporate the baseline pubertal stage into the statistical analysis plan. This finding suggests that the timing of intervention is a key variable affecting study outcomes for body composition [24].
Data Presentation
Table 1: Impact of Pubertal Stage on Body Composition Changes During Hormone Therapy [24]
| Affirmed Gender | Pubertal Stage at GnRHa Start | Key Change during GAHT | Mean Change (kg, 95% CI) |
|---|---|---|---|
| Trans Boys | 'In Puberty' (Tanner 2-3) | Increase in Total Lean Mass | 6.28 kg (3.54; 9.02) |
| Trans Boys | 'In Puberty' (Tanner 2-3) | Increase in Muscle Mass | 6.08 kg (3.64; 8.51) |
| Trans Boys | 'Completing Puberty' (Tanner 4-5) | Increase in Total Lean Mass | Data not specified |
| Trans Girls | All Stages | Changes in Body Composition | Slight (No substantial changes) |
Table 2: Long-Term Health Outcomes Associated with Pubertal Timing and Suppression [25] [23]
| Health Outcome | Association with Early/Precocious Puberty | Association with Delayed Puberty | Effect of GnRHa Treatment |
|---|---|---|---|
| Final Adult Height | Short stature without treatment | Conflicting data on achieving genetic potential | Improves adult height, especially if started early [23] |
| Bone Mineral Density | — | Lower BMD in some adults [25] | Temporary decrease during treatment; recovers post-therapy [23] |
| Reproductive Health | Higher risk of early menopause [23] | Protective against breast/testicular cancer [25] | No negative effect on menstrual regularity [23] |
| Metabolic Health | Increased risk of obesity, T2DM [23] | Higher risk of metabolic/CVD disorders [25] | — |
| Mental Health | Increased risk of depression, anxiety [23] | Negative psychosocial effects [25] | Reduces depression, anxiety, suicidality [10] |
Experimental Protocols
Protocol 1: Monitoring Efficacy of Puberty Suppression Therapy
Objective: To quantitatively assess the suppression of the hypothalamic-pituitary-gonadal (HPG) axis in research subjects undergoing GnRHa therapy.
Methodology:
- Clinical Visits: Schedule subjects for follow-up every 4-6 months [12].
- Anthropometric Measurements: Record height, weight, and calculate BMI at each visit.
- Physical Examination: Perform Tanner staging by a trained clinician to assess breast (girls), genital (boys), and pubic hair development [12].
- Biochemical Testing:
- Baseline: Conduct a GnRH stimulation test prior to treatment initiation.
- On-Treatment: Perform a GnRH test ~4 months after starting GnRHa. Administer standard-dose GnRH (e.g., 100 mcg) and measure LH and FSH at 0, 30, and 60 minutes. Suppression is confirmed by a peak LH level falling to the prepubertal range [12].
- Alternative for Males: Measure serum testosterone; a level <20 ng/dL indicates adequate suppression [12].
- Radiological Assessment: Obtain a left hand and wrist X-ray for bone age assessment annually, using the Greulich and Pyle or Tanner-Whitehouse methods [12].
Protocol 2: Assessing Body Composition Changes
Objective: To evaluate the changes in fat, lean, and muscle mass in subjects undergoing puberty suppression and subsequent hormone therapy.
Methodology:
- Equipment: Use a calibrated bioelectrical impedance analyzer (BIA) or DEXA scanner for higher precision [24].
- Timing: Conduct body composition analysis at baseline (pre-treatment), every 6-12 months during GnRHa therapy, and at 3, 6, and 12 months after initiating gender-affirming hormone therapy [24].
- Data Collection: Record total fat mass (FM), lean body mass (LBM), and muscle mass (MM). Calculate Z-scores where appropriate for age and sex.
- Data Analysis: Stratify subjects based on their Tanner stage at the start of GnRHa therapy (e.g., Tanner 2-3 vs. Tanner 4-5) to analyze the differential treatment effect [24].
Signaling Pathways and Workflows
HPG Axis and GnRHa Action
Breakthrough Puberty Assessment
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Hormone Suppression Research
| Reagent / Material | Primary Function in Research | Key Considerations |
|---|---|---|
| GnRH Agonists (GnRHa)(e.g., Leuprolide, Triptorelin) | The primary intervention to suppress the HPG axis. Mimics native GnRH, causing receptor downregulation and desensitization [10] [12]. | Available in various depot formulations (e.g., 1, 3, 6-month). Choice affects dosing schedule and subject compliance. |
| Immunoassay Kits(for LH, FSH, Testosterone, Estradiol) | To quantitatively measure hormone levels in serum/plasma for monitoring HPG axis suppression and breakthrough [12]. | Ensure assays are sensitive enough to detect low, prepubertal hormone levels. |
| Bone Age Atlas(e.g., Greulich & Pyle) | The standardized reference for assessing skeletal maturation from hand/wrist radiographs, a key efficacy endpoint [12] [23]. | Requires a trained radiologist or endocrinologist for accurate interpretation. |
| Bioelectrical Impedance (BIA)or DEXA Scanner | To objectively measure body composition parameters (fat mass, lean mass) as secondary outcomes of treatment efficacy [24]. | DEXA is the gold standard but more expensive. BIA is more accessible but slightly less precise. |
| Calcium & Vitamin D Supplements | Used in studies to mitigate the known side effect of reduced bone mineral density during GnRHa treatment [23]. | Dosage should be standardized across the study cohort for consistent results. |
Monitoring Protocols and Detection Methods for Breakthrough Events
Estradiol monitoring is a critical component of research involving hormone suppression therapies. Accurate measurement is essential for verifying therapeutic efficacy, managing side effects, and understanding treatment resistance. This guide provides detailed protocols for monitoring estradiol levels, troubleshooting common assay issues, and interpreting results within the context of hormone suppression research.
Key Monitoring Principle: Estradiol levels exhibit substantial interindividual variation even at standardized doses. Research indicates that up to 25% of subjects may have subtherapeutic levels despite using the highest licensed transdermal doses, a phenomenon often termed "poor absorption" [26].
Quantitative Data & Target Thresholds
Therapeutic & Physiological Ranges
The table below summarizes estradiol reference ranges for various physiological states and therapeutic targets, which are crucial for assessing the efficacy of hormone suppression [26] [27] [28].
Table 1: Estradiol Reference Ranges Across Conditions
| Condition / Objective | Target or Typical Range | Notes & Context |
|---|---|---|
| Optimal Therapeutic Range (Postmenopausal HRT) | 220 - 550 pmol/L (~60 - 150 pg/mL) | Relieves vasomotor symptoms and prevents bone resorption [26]. |
| Bone Protection Threshold | >200 pmol/L | Suggested minimum for optimal osteoporosis prevention with HRT [26] [27]. |
| Pre-menopausal (Early Follicular Phase) | ~110 - 1285 pmol/L | Levels fluctuate significantly during the menstrual cycle [27]. |
| Post-menopausal (Untreated) | <73 pmol/L | Baseline level after ovarian function ceases [27]. |
| IVF Cycle (Follicular Development) | See Table 2 | Levels rise with follicular growth; used to monitor response [28]. |
Estradiol Levels During Ovarian Stimulation (IVF Context)
In protocols involving ovarian stimulation, estradiol levels provide a key metric for follicular development. The following table outlines typical values, though significant inter-individual variation occurs [28].
Table 2: Typical Estradiol Values During an IVF Stimulation Cycle
| Day of Stimulation | Typical Estradiol Range (pg/mL) | Approximate Conversion (pmol/L) |
|---|---|---|
| 1 | 25 - 75 | ~92 - 275 |
| 3 | 100 - 200 | ~367 - 734 |
| 5 | 400 - 800 | ~1468 - 2936 |
| 7 | 1000 - 1600 | ~3670 - 5872 |
| 9 | 1600 - 2400 | ~5872 - 8808 |
| 11 | 2400 - 4000 | ~8808 - 14680 |
Experimental Protocols & Methodologies
Protocol for Serum Estradiol Measurement in Transdermal Therapy Research
Application: This protocol is designed for obtaining reliable serum estradiol measurements in subjects using transdermal formulations, which is critical for assessing the pharmacokinetics of hormone suppression therapies [26] [27].
Workflow Diagram: Blood Collection for Transdermal Estradiol Monitoring
Detailed Methodology:
- Subject Preparation: Subjects should be on a stable, documented dose of transdermal estradiol for a minimum of 3 months prior to sampling to ensure steady-state levels [26].
- Blood Draw Timing:
- Site-Specific Collection:
- Sample Processing: Serum samples should be processed according to the specific requirements of the chosen immunoassay. The use of a consistent laboratory and assay method (e.g., the Atellica IM Enhanced Estradiol assay) across a study is recommended to minimize inter-assay variability [26].
- Data Interpretation: Compare results against target thresholds (Table 1), noting that a wide interindividual range is normal. Results should be correlated with clinical symptoms and research endpoints.
Protocol for Investigating Assay Interference ("Hook Effect")
Application: This protocol is used when falsely low estradiol results are suspected in the presence of very high analyte concentrations, which can occur in certain research models like ovarian hyperstimulation [29].
Mechanism Diagram: Immunoassay Hook Effect
Detailed Methodology:
- Suspicion Point: Suspect the "hook effect" when estradiol levels are unexpectedly low or normal in a research subject with clinical or other biochemical markers suggesting very high estrogen levels (e.g., numerous large follicles on ultrasound during an IVF cycle) [29].
- Serial Dilution Test:
- Prepare a series of dilutions (e.g., 1:10, 1:100) of the original serum sample using the appropriate diluent specified by the assay manufacturer [29].
- Re-run the estradiol assay on each of the diluted samples.
- Interpretation: If the measured estradiol concentration increases significantly with dilution (e.g., the result from the 1:100 sample is >100 times higher than the undiluted result), the hook effect is confirmed. The result from the diluted sample falling within the assay's linear range should be reported as the valid concentration.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Estradiol Monitoring Research
| Item | Function & Application in Research |
|---|---|
| Transdermal Estradiol (Gel/Spray/Patch) | Research intervention; used to study absorption pharmacokinetics and dose-response relationships in hormone suppression [26]. |
| Serum Separation Tubes | Collection of blood samples for subsequent analysis of serum hormone levels. |
| Enhanced Estradiol Immunoassay (e.g., Atellica IM) | Quantifies serum estradiol concentration. Critical for PK/PD studies. Note potential for interference [26] [29]. |
| PEG Precipitation Reagents | Used to investigate macroprolactinemia, a cause of falsely elevated prolactin, which can be a confounder in endocrine research [29]. |
| Assay-Specific Diluent | Required for performing serial dilutions to investigate and overcome the "hook effect" in immunoassays [29]. |
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: Why do estradiol levels vary so widely between research subjects using the same transdermal dose? A: This is due to substantial interindividual variation in absorption. Factors include skin thickness, local blood flow, skin temperature, and the specific application site. Research shows that interindividual variation is a primary reason why therapeutic drug monitoring is necessary, as a "one-size-fits-all" dose does not exist [26] [27].
Q2: When is the optimal time to collect blood for estradiol measurement in subjects using transdermal formulations? A:
- Gels/Sprays: Draw blood at least 4 hours after application.
- Patches: Draw blood the day before the patch is scheduled to be changed. Always draw blood from the arm not used for application to avoid contamination and artificially high readings [27].
Q3: What are the primary sources of error in estradiol immunoassays and how can they be mitigated? A:
- Hook Effect: Causes falsely low results when hormone levels are extremely high. Mitigation: Perform serial dilution of samples with unexpectedly low results in the context of high clinical suspicion [29].
- Heterophile Antibodies: Can cause either falsely high or low results. Mitigation: Use proprietary blocking reagents, re-assay with alternative methods, or use tandem mass spectrometry (LC-MS/MS) for confirmation [29].
- Biotin Interference: High doses of biotin supplements can interfere with some assay systems. Mitigation: Have subjects withhold biotin supplements for at least 48 hours prior to blood collection [29].
Q4: In the context of puberty suppression research, what estradiol level indicates "breakthrough" puberty or suboptimal suppression? A: While specific thresholds for puberty suppression are not defined in the general literature, the principle is to suppress estradiol to a level that prevents the development of secondary sexual characteristics and the progression of bone age. This typically requires suppression to pre-pubertal levels, which are very low. Researchers should establish baseline pre-treatment levels and define a target suppression threshold (e.g., <50 pmol/L or lower) as a study endpoint, monitoring for any consistent rise that may indicate escape from suppression.
Troubleshooting Guides
Guide 1: Addressing Immunoassay Interferences
Problem: Unexpected or clinically discordant analyte results.
Solution: Follow this systematic algorithm to identify and resolve common immunoassay interferences [30].
Detailed Investigation Protocol:
Confirm Preanalytical Integrity [30]
- Verify patient identification matches request form
- Confirm correct anticoagulant tube used (e.g., EDTA for ACTH)
- Check tube filling adequacy, especially for citrate tubes
- Inspect for clots, hemolysis, icteria, or lipemia
Rule Out Exogenous Analytical Errors [30]
- Review internal quality control (IQC) data for shifts
- Check external quality assurance (EQA) performance
- Verify reagent lot numbers and calibration dates
- Confirm automated analyzer error logs
Investigate Specific Interference Types:
- Heterophile Antibodies/ [31] Suspect when results are clinically inconsistent. Test by:
- Re-measurement with heterophile blocking tubes
- Serial dilution to check for non-linearity
- Method comparison with alternative platform
- Autoantibody Interference [31] (e.g., in thyroglobulin assays):
- Use polyethylene glycol (PEG) precipitation
- Employ alternative method (e.g., LC-MS/MS)
- Check for endogenous antibody presence
- Hook Effect [31] Suspect with very high analyte concentrations:
- Perform sample dilution and re-assay
- Typical for prolactin, TSH, tumor markers
- Look for saturation pattern in dose-response
- Heterophile Antibodies/ [31] Suspect when results are clinically inconsistent. Test by:
Guide 2: Managing LC-MS/MS Method Validation
Problem: Inconsistent performance of laboratory-developed LC-MS/MS tests.
Solution: Implement comprehensive quality assurance addressing technology-specific pitfalls [32].
Quality Assurance Protocol:
Address Pre-Analytical Variables
- Validate sample collection tubes for adsorption issues
- Establish stability conditions for each analyte
- Standardize processing protocols across sites
Control Analytical Phase
- Use stable isotope-labeled internal standards
- Implement ion ratio monitoring for confirmation
- Establish matrix effect evaluation protocols
- Monitor chromatographic performance metrics
Post-Analytical Quality Measures
- Review internal standard recovery rates
- Verify calibration curve fitting
- Implement data review criteria for technical staff
Frequently Asked Questions
What are the primary advantages of LC-MS/MS over immunoassays for hormone monitoring in puberty suppression research?
A: LC-MS/MS offers several critical advantages for monitoring low-level hormones in puberty suppression research [33] [34]:
- Superior Specificity: Measures analytes based on mass/charge ratio rather than antibody cross-reactivity
- Better Sensitivity: Lower limits of detection for steroids like estradiol and testosterone
- Multiplexing Capability: Simultaneous measurement of multiple analytes from small sample volumes
- Reduced Interference: Not affected by heterophile antibodies or autoantibodies
- Standardization Potential: Better alignment with reference methods and materials
How significant is inter-platform variability in immunoassays, and how does it impact longitudinal studies?
A: Inter-platform variability is substantial and clinically significant [31]. For example:
- TSH measurements across 6 platforms showed differences that could alter treatment decisions
- CA 19-9 results varied across 5 platforms, potentially leading to false cancer recurrence diagnosis
- This variability stems from different antibody epitopes, calibration materials, and detection methods
- Impact: Patients moving between healthcare systems may show apparent clinical changes due solely to methodological differences, compromising research data integrity
What practical strategies can minimize immunoassay interference in clinical research?
A: Implement a multi-layered approach [31] [30]:
- Sample Pre-treatment: Use heterophile blocking tubes, PEG precipitation
- Method Verification: Perform serial dilutions, spike recovery studies
- Result Corroboration: Compare with clinical picture, alternative methods
- Documentation: Maintain detailed interference testing protocols
- Staff Training: Educate technicians on interference recognition patterns
Comparative Performance Data
Table 1: Method Comparison for Key Analytes in Endocrine Research
| Analyte | Immunoassay CV | LC-MS/MS CV | Major Interferences | Clinical Impact |
|---|---|---|---|---|
| Testosterone | 4.5-6.7% [34] | 6.1% [34] | SHBG, heterophile antibodies [31] | False elevation/ suppression affecting diagnosis |
| Cortisol | 3.9-8.0% [34] | 6.8% [34] | Binding proteins, cross-reactants [32] | Misdiagnosis of Cushing's/ Addison's |
| 25OH-Vitamin D | 7.5-18.3% [34] | 4.7% [34] | Lipid content, metabolites [32] | Incorrect supplementation |
| Thyroglobulin | 10-25% (with autoantibodies) [31] | 8-12% [31] | Autoantibodies (25% of thyroid cancer) [31] | Missed cancer recurrence |
Table 2: Interference Frequency and Resolution Tactics
| Interference Type | Frequency | Typical Effect | Resolution Methods |
|---|---|---|---|
| Heterophile Antibodies | 0.4-4.0% of samples [30] | False elevation (sandwich), false decrease (competitive) | Blocking reagents, platform switching, dilution studies [31] |
| Autoantibodies | Target-dependent (up to 25% in thyroid cancer) [31] | Steric hindrance in immunometric assays | PEG precipitation, LC-MS/MS alternative [31] |
| Hook Effect | Rare but significant [31] | Falsely low at high concentrations | Sample dilution, method awareness [31] |
| Matrix Effects | Common in LC-MS/MS [32] | Ion suppression/enhancement | Stable isotope IS, efficient extraction [32] |
The Scientist's Toolkit
Research Reagent Solutions for Hormone Assessment
| Reagent/Category | Function | Application Notes |
|---|---|---|
| Stable Isotope-Labeled Internal Standards | Compensates for matrix effects & recovery variations in LC-MS/MS [32] | Use ( ^{13}C ) or ( ^{15}N )-labeled versions; avoid deuterium labels prone to exchange [32] |
| Heterophile Blocking Reagents | Neutralizes interfering human antibodies against reagent immunoglobulins [31] [30] | Use as additive in diluent; effective for 80-90% of heterophile interference cases [30] |
| Anti-Idiotype Antibodies | Recognizes and neutralizes specific autoantibodies in immunoassays [31] | Particularly important for thyroglobulin and insulin assays [31] |
| Solid Phase Extraction Cartridges | Pre-concentrates analytes and removes matrix components prior to LC-MS/MS [32] | Select sorbent chemistry based on analyte polarity; essential for low-concentration steroids [32] |
| Multi-analyte Calibrators | Provides traceable calibration for LC-MS/MS methods [34] | Use commutable materials with value assignment by reference methods [34] |
Experimental Workflow Visualization
Figure 2: LC-MS/MS Method Development Workflow
FAQs: Troubleshooting Breakthrough Puberty in Research Settings
Q1: What are the key biochemical parameters for confirming adequate hormone suppression in research subjects?
The primary parameter for confirming suppression of the hypothalamic-pituitary-gonadal (HPG) axis is the measurement of luteinizing hormone (LH) levels [35].
- Basal LH Level: A basal LH level of < 0.6 IU/L is a strong predictor of adequate suppression. This basal level can predict suppression escape, with a cutoff of ≥ 0.6 IU/L identifying 70% of those failing suppression [35].
- Peak-Stimulated LH Level: The gold-standard methodology is the peak gonadotropin-releasing hormone agonist (GnRHa) stimulated LH test. Effective suppression is confirmed when mean peak-stimulated LH levels remain below 4 IU/L [35].
Q2: What constitutes a "red-flag" symptom indicating potential breakthrough puberty or treatment failure?
"Red-flag" symptoms are warning signs of a more serious underlying issue, such as breakthrough puberty [36]. In this context, they are physical signs indicating that hormone suppression is inadequate.
- Key Red Flags:
- Progressing Secondary Sex Characteristics: Any new or progressing development, such as breast bud development in assigned females at birth or testicular growth in assigned males at birth.
- Resumed Menstruation: The return of menses in assigned females at birth.
- Rapid Growth Velocity: A significant increase in growth rate, indicating a pubertal growth spurt.
- Biochemical Escape: A basal LH measurement ≥ 0.6 IU/L or a stimulated LH level ≥ 4 IU/L [35].
- Considerations: The duration of the symptom and the age of the subject are critical contextual factors. A symptom that persists or progresses over time is of greater concern [36].
Q3: What is the recommended protocol for monitoring bone health in long-term suppression studies?
The use of GnRH analogues can have long-term effects on bone density, necessitating regular monitoring [37].
- Annual Monitoring: Yearly bone density and bone age tests are recommended [37].
- Auxiliary Support: To support bone health, research subjects may need to take calcium and vitamin D supplements [37].
- Height Checks: Height should be checked every few months to monitor growth patterns [37].
Q4: How should researchers manage the transition from 1-month to 3-month GnRHa formulations in a study protocol?
When transitioning from 1-month to 3-month leuprolide acetate (LA) formulations, the effectiveness and safety are not influenced by previous CPP therapies [35].
- Continuation of Suppression: Pretreatment with any 1-month formulation (7.5 mg, 11.25 mg, or 15 mg) for the most part does not affect the continuation of suppression after transitioning to a 3-month formulation (11.25 mg or 30 mg) [35].
- Monitoring Post-Transition: Basal and/or peak-stimulated LH levels should be measured at scheduled intervals (e.g., weeks 0, 4, 8, and 12) after the transition to confirm sustained suppression [35].
Experimental Protocols & Methodologies
Protocol for HPG Axis Suppression Testing
This protocol details the methodology for assessing the suppression of the HPG axis using a GnRH agonist stimulation test, which is critical for identifying breakthrough puberty [35].
Methodology:
- Administration: Administer a standard dose of GnRH agonist (e.g., leuprolide acetate).
- Blood Sampling: Collect blood samples at baseline and at a standardized post-administration time point (e.g., 30-40 minutes) to measure the peak LH response.
- Analysis: Measure serum LH levels via immunoassay.
Interpretation:
- Adequate Suppression: Peak-stimulated LH level < 4 IU/L [35].
- Inadequate Suppression / Breakthrough: Peak-stimulated LH level ≥ 4 IU/L [35].
Protocol for Monitoring Physical Signs of Puberty
This methodology provides a systematic approach for tracking the progression of secondary sex characteristics, which are key physical signs of breakthrough puberty.
Tools: Tanner Staging illustrations and guides, orchidometer, anthropometric tape. Procedure:
- Schedule: Conduct physical examinations at baseline and every 3-6 months.
- Staging: Document Tanner Stage for breast (in females), genital (in males), and pubic hair development.
- Measurements:
- Testicular Volume: Measure using a Prader orchidometer in males. A volume > 3 mL indicates the onset of puberty.
- Menstrual History: Record the onset and frequency of menses in females.
- Growth Velocity: Calculate height velocity (cm/year) from regular height measurements.
Data Presentation: Monitoring Parameters
Table 1: Biochemical and Physical Monitoring Parameters for Breakthrough Puberty
| Parameter | Method of Assessment | Frequency of Assessment | Interpretation Guidelines | Associated Risk |
|---|---|---|---|---|
| LH Suppression (Gold Standard) | GnRHa-stimulated test [35] | Pre-dose, then every 3-6 months or as clinically indicated [35] | Adequate Suppression: Peak LH < 4 IU/L [35] | Treatment failure, disease progression |
| Basal LH Level | Immunoassay from serum sample [35] | Can be used more frequently for monitoring; at weeks 0, 4, 8, 12 in clinical trials [35] | Concerning: Basal LH ≥ 0.6 IU/L (predicts 70% of suppression failures) [35] | Early indicator of breakthrough |
| Secondary Sex Characteristics | Tanner Staging by trained clinician | Every 3-6 months | Red Flag: Advancement of Tanner Stage | Inadequate suppression, need for dose adjustment |
| Bone Density | Dual-Energy X-ray Absorptiometry (DEXA) scan [37] | Annually [37] | Below expected range for age/sex | Long-term bone health compromise [37] |
| Bone Age | X-ray of left hand and wrist [37] | Annually [37] | Advancement over chronological age | Risk for reduced final adult height |
Table 2: Research Reagent Solutions for Key Experiments
| Research Reagent | Function/Application in Monitoring | Brief Protocol Explanation |
|---|---|---|
| GnRH Agonist (e.g., Leuprolide Acetate) | Stimulation agent for the definitive test of HPG axis suppression [35]. | Administered subcutaneously or intramuscularly to stimulate LH release from the pituitary; peak LH response is measured to assess suppression status [35]. |
| LH Immunoassay Kit | Quantitative measurement of Luteinizing Hormone (LH) in serum/plasma [35]. | Used to analyze basal and stimulated blood samples; results determine the adequacy of pituitary suppression [35]. |
| DEXA Phantom Calibration Standard | Ensures accuracy and precision of bone mineral density measurements over time [37]. | Scanned alongside the subject or during daily quality control procedures to calibrate the DEXA instrument, ensuring longitudinal data reliability [37]. |
| Tanner Staging Atlas | Standardized visual reference for classifying stages of pubertal development. | Used by clinicians during physical examinations to assign consistent and objective stages to the development of breasts, genitals, and pubic hair. |
Visualizations: Signaling Pathways and Workflows
Breakthrough Puberty Monitoring Workflow
Symptom Recognition & Research Escalation
For researchers developing strategies to manage breakthrough puberty during hormone suppression therapy, reliable biomarkers are crucial for assessing therapeutic impact and ovarian function. Anti-Müllerian Hormone (AMH), a glycoprotein produced by granulosa cells of preantral and small antral follicles, has emerged as a key biomarker of ovarian reserve. Its integration into clinical research protocols provides a sensitive, non-invasive method for monitoring ovarian activity and predicting pubertal outcomes in the context of endocrine therapies, offering critical insights for fertility counseling and treatment timing [38].
FAQs: AMH in Hormone Suppression Research
What is the primary clinical utility of AMH in pediatric endocrine research? AMH serves as a key quantitative biomarker for assessing ovarian reserve. It is used to evaluate the pool of growing follicles, providing researchers with a sensitive and non-invasive means to monitor ovarian function and its response to therapeutic interventions, such as gonadotropin-releasing hormone analogues (GnRHa) [38].
How does AMH inform studies on breakthrough puberty during hormone suppression? Detectable serum AMH levels correlate strongly with the capacity for spontaneous pubertal development. In research settings, tracking AMH in subjects undergoing hormone suppression therapy can help predict the risk of breakthrough puberty. A significant decline in AMH may indicate successful suppression of the hypothalamic-pituitary-ovarian axis, while persistent or rising levels could signal potential breakthrough events [38].
What are the key methodological considerations for AMH assay in clinical trials? Standardization of the AMH assay method is critical. Researchers should note that ELISA-based methods can detect low but clinically relevant AMH levels. Variability between different commercial assays can impact results, so using the same method and laboratory throughout a study is essential for data consistency. Incorporating this into a validated bioanalytical method is a best practice [38] [39].
What does recent evidence say about the impact of GnRHa on AMH levels in adolescents? A 2025 study of transgender male adolescents found that AMH levels did not show significant changes in the first 18 months after initiating GnRHa for pubertal suppression. This suggests that short-term use of puberty blockers may not drastically impact this specific marker of ovarian reserve, a vital finding for fertility preservation research [40].
Key Experimental Data and Protocols
Table 1: Key Quantitative Findings on AMH from Recent Systematic Reviews
| Population | Finding | Statistical Significance | Clinical/Research Implication |
|---|---|---|---|
| Turner Syndrome (TS) vs. Healthy Controls | Weighted Mean Difference (WMD): -3.04 ng/mL [38] | 95% CI: -3.26 to -2.83; p < 0.001 [38] | Confirms severely diminished ovarian reserve in TS. |
| TS with Spontaneous Puberty | Odds Ratio (OR): 5.12 for detectable AMH [38] | 95% CI: 2.87–9.12 [38] | AMH is a strong predictor of spontaneous pubertal onset. |
| Trans Boys on GnRHa (18-month study) | No significant change in AMH levels [40] | p-value: 0.347 [40] | Suggests short-term pubertal suppression may not diminish ovarian reserve. |
Detailed Protocol: Longitudinal AMH Monitoring in Intervention Studies
This protocol is designed for monitoring AMH in clinical trials involving hormone suppression.
1. Objective: To serially measure serum AMH levels to assess the impact of an intervention (e.g., GnRHa) on ovarian reserve over time.
2. Materials: Table 2: Essential Research Reagent Solutions
| Item | Function/Description |
|---|---|
| AMH ELISA Kit | For quantitative measurement of human AMH in serum/plasma. |
| GnRH Agonist/Analogue | e.g., Leuprolide, Triptorelin; for experimental puberty suppression. |
| Control Serum Pools | Quality control for assay validation and run-to-run precision. |
| Venous Blood Collection Tubes | Serum-separating tubes for sample acquisition. |
| -80°C Freezer | For long-term storage of serum samples at stable temperature. |
3. Methodology:
- Subject Enrollment & Baseline: Recruit subjects meeting predefined criteria (e.g., specific Tanner stage, karyotype). Obtain informed consent. Collect baseline venous blood sample (≥ 2 mL) prior to intervention initiation.
- Sample Processing: Allow blood to clot at room temperature (15-30 minutes). Centrifuge at 2000-3000 RCF for 10 minutes. Aliquot serum into cryovials and store at -80°C until batch analysis.
- Intervention & Follow-up: Initiate the study intervention (e.g., first dose of GnRHa). Schedule subsequent blood draws at regular intervals (e.g., 3, 6, 12, and 18 months post-baseline). Process and store all follow-up samples identically to baseline samples.
- AMH Quantification: Analyze all samples from a single subject in the same assay batch to minimize variability. Perform the AMH immunoassay according to the manufacturer's instructions. Include appropriate standards, controls, and blanks in each run.
- Data Analysis: Report AMH values in consistent units (e.g., ng/mL or pmol/L). Use non-parametric statistical tests (e.g., Wilcoxon signed-rank test) to compare longitudinal changes from baseline within the cohort, as AMH levels are often not normally distributed [40].
AMH Signaling and Experimental Workflow
Troubleshooting Common Experimental Issues
Issue: Inconsistent AMH values between assay batches.
- Solution: Implement a rigorous sample management protocol. Store all samples from a longitudinal study at -80°C and analyze all timepoints for a single subject within the same assay batch to control for inter-assay variability [38].
Issue: How to interpret low or undetectable AMH levels in a study subject.
- Solution: In the context of pediatric endocrinology, a low or undetectable AMH is strongly indicative of diminished ovarian reserve. This can be used as a predictive biomarker for absent spontaneous puberty or a positive response to suppression therapy, depending on the study objective. Correlate with other endocrine markers like FSH and estradiol for a comprehensive picture [38].
Issue: Designing a trial to assess the impact of a novel agent on puberty.
- Solution: The recently announced UK "Pathways Trial" provides a contemporary model. It is a randomized controlled trial where participants are assigned to either immediate intervention or a 12-month delayed start group. The primary outcomes focus on quality of life, mental health, gender/body distress, and physical health, with careful monitoring over 24 months [41] [42].
Troubleshooting Guides and FAQs
FAQ: What is the recommended frequency for monitoring bone health in adolescents undergoing puberty suppression? Answer: Longitudinal monitoring at a minimum of three time points is the consensus for capturing bone density changes. Research indicates that puberty blockers can cause reductions in bone density, making it a key parameter to track [43] [10]. The table below summarizes the core monitoring domains and their rationale.
| Monitoring Domain | Rationale for Standardized Tracking | Potential Risk if Unmonitored |
|---|---|---|
| Bone Density | Pubertal suppression is associated with reductions in bone density [10]. | Increased long-term risk of osteoporosis and fractures [10]. |
| Executive Function & Cognitive Control | Puberty is a period of significant brain maturation; blocking hormones may impact this development [43]. | Potential disruption to the development of abstraction, logical thinking, and cognitive control [43]. |
| Mental Health | Treatment aims to reduce gender dysphoria and improve psychological wellbeing [43] [10]. | Failure to identify and address anxiety, depression, or suicidal ideation [10]. |
| Social Awareness & Functioning | Adolescent neurodevelopment includes maturation of the "social brain" network [43]. | Potential impacts on social competence and peer interactions [43]. |
FAQ: Our study involves longitudinal assessment. What is the evidence-based minimum for assessment time points? Answer: An international Delphi consensus of experts recommends a study design with a minimum of three measurement time points [43]. This approach allows for the statistical modeling of developmental trajectories and is crucial for distinguishing treatment effects from normal developmental variation.
FAQ: How should we structure comparison groups to isolate the effect of puberty blockers from typical development? Answer: Expert consensus recommends using multiple comparison groups to minimize the limitations of any single group [43]. The recommended groups are:
- Untreated transgender youth matched on pubertal stage (e.g., Tanner stages 2-3) at baseline [43].
- Cisgender youth matched on pubertal stage at baseline [43].
- An independent sample from a large-scale youth development database for normative comparison [43].
FAQ: What is the evidence for the reversibility of effects after discontinuing puberty blockers? Answer: Preclinical evidence from animal models indicates that the effects on reproductive organ development are reversible after medication withdrawal. A 2024 study on female rats found that while puberty blockers delayed uterine and ovarian development, these organs showed normal development four weeks after treatment stopped. Reproductive function also recovered, though pregnancy occurred later and with fewer pups per litter [44]. The translational relevance to humans requires further study.
Troubleshooting Guide: Managing Breakthrough Puberty During Hormone Suppression Therapy
| Problem | Possible Cause | Evidence-Based Solution |
|---|---|---|
| Breakthrough pubertal development | Inadequate dosing or non-adherence to medication regimen. | Verify dosing and adherence. Re-evaluate pubertal stage (Tanner staging). Consider checking serum hormone levels (e.g., testosterone or estradiol) to confirm suppression [43]. |
| Significant drop in working memory scores | Potential neurocognitive impact of hormone suppression. | Implement the consensus-recommended assessment for executive function/cognitive control [43]. This finding is supported by a case study where working memory dropped over half a standard deviation after 22 months of treatment [43]. |
| High participant attrition | Burden of frequent or lengthy assessments. | Implement a schedule with a minimum of three time points but optimize interim follow-up (e.g., brief check-ins). Expert consensus emphasizes the need for statistical methods that account for heterogeneity and missing data [43]. |
Experimental Protocols for Key Studies
Detailed Methodology: Delphi Consensus Procedure on Neurodevelopment This protocol established research priorities for studying the neurocognitive impact of pubertal suppression [43].
- Objective: To leverage international expertise and identify priority research methodologies to assess whether pubertal suppression treatment is associated with real-world neurocognitive sequelae [43].
- Expert Panel: Comprised 24 international experts in neurodevelopment, gender development, puberty/adolescence, neuroendocrinology, and statistics/psychometrics [43].
- Procedure: A two-round, anonymous Delphi procedure was employed.
- Round 1: Experts were presented with the key research question and provided initial recommendations. The study team combined and organized 160 initial recommendations [43].
- Round 2: Experts rated each proposed statement. Recommendations that reached a pre-specified consensus threshold of 80% agreement were included in the final consensus parameter [43].
- Outcome: 44 recommendations achieved final consensus, covering optimal study design, comparison groups, and core assessment domains [43].
Detailed Methodology: Rat Model of Puberty Blocker Reversibility This preclinical protocol investigated the reversibility of GnRHa effects on reproductive development [44].
- Objective: To determine if the effects of puberty-blocking medication (GnRHa) on the development of female reproductive organs are reversible after treatment withdrawal [44].
- Subjects: Pre-pubescent female rats [44].
- Intervention: Rats were administered either GnRHa or a saline control for a period of four weeks, after which the treatment was stopped [44].
- Assessment Timepoints: Researchers assessed changes in the rats' reproductive organs at various timepoints during and after the treatment period [44].
- Functional Outcome: After treatment withdrawal, a subset of rats was paired with a male rat to track pregnancy rates and litter characteristics [44].
- Key Findings:
- Rats given GnRHa showed delayed development of the uterus and ovaries during treatment [44].
- Four weeks after stopping treatment, the reproductive organs showed normal development [44].
- Treated rats became pregnant significantly later than controls but showed no difference in overall pregnancy rate [44].
- Treated rats had significantly fewer pups per litter [44].
Visualizing Research Frameworks
Research Framework for Puberty Suppression Studies
Troubleshooting Breakthrough Puberty
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Research Context |
|---|---|
| Gonadotropin-Releasing Hormone Agonists (GnRHa) | The primary class of drugs used for pubertal suppression. They suppress the production of sex hormones (estrogen and testosterone) by acting on the pituitary gland [43] [10] [44]. |
| Tanner Staging Criteria | A standardized system for classifying the stages of pubertal development. Essential for ensuring a homogeneous study population at baseline (typically stages 2-3) and for monitoring for breakthrough development [43]. |
| Dual-Energy X-ray Absorptiometry (DEXA) | The gold-standard technology for monitoring bone mineral density (BMD). Used to track the known side effect of bone density reduction in youth undergoing puberty suppression [10]. |
| Standardized Neuropsychological Batteries | Validated test sets for assessing consensus domains such as executive function/cognitive control (e.g., working memory, task switching) and social awareness/functioning [43]. |
| Validated Mental Health Questionnaires | Instruments to measure psychological outcomes like depression, anxiety, and suicidality. Critical for evaluating the primary psychosocial benefits of treatment [43] [10]. |
Clinical Management Strategies for Incomplete Suppression
Dosage Optimization and Administration Interval Adjustments
This technical support center provides troubleshooting guides and FAQs for researchers investigating the management of breakthrough puberty during hormone suppression therapy.
∿ Frequently Asked Questions (FAQs)
Q1: What are the primary hormonal agents used to suppress puberty in research, and what are their typical administration intervals? Gonadotropin-releasing hormone analogues (GnRHa) are the standard agents for suppressing the hypothalamic-pituitary-gonadal (HPG) axis [45] [46]. They are considered the gold-standard treatment for central precocious puberty (CPP) [45]. Numerous preparations with a range of delivery systems and durations of action are commercially available [45]. The administration intervals can vary significantly based on the specific formulation, ranging from daily to monthly injections or long-acting implants.
Q2: What defines "breakthrough puberty" in the context of GnRHa suppression therapy? Breakthrough puberty refers to the occurrence of pubertal progression despite ongoing suppression therapy. Key indicators include [45]:
- Clinical Signs: Resumption or progression of secondary sexual characteristics, such as breast development in girls or testicular enlargement in boys.
- Biochemical Signs: A rise in basal or stimulated luteinizing hormone (LH) levels. A peak stimulated LH of >5 IU/L after GnRHa stimulation is often considered indicative of HPG axis reactivation [45].
- Auxological Signs: An unexpected acceleration in growth velocity or bone age advancement.
Q3: What are the recommended troubleshooting steps if breakthrough puberty is suspected in a subject?
- Verify Adherence: Confirm proper administration and adherence to the treatment regimen, especially with patient-administered formulations.
- Reassess Biochemical Suppression: Conduct a GnRH stimulation test to measure peak LH and FSH levels. Inadequate suppression may indicate an insufficient dosage or administration interval that is too long [45].
- Evaluate Bone Age: Obtain a bone age X-ray to assess if skeletal maturation is progressing faster than expected.
- Review Dosage and Interval: Consider increasing the GnRHa dosage or shortening the interval between administrations based on the subject's weight and the formulation's pharmacokinetics.
- Check Formulation and Storage: Ensure the drug has been stored and reconstituted correctly, as improper handling can affect efficacy.
Q4: When is combination therapy with Growth Hormone (GH) considered, and what is its intended effect? Combination therapy with GH may be considered for subjects with a poor growth prognosis, such as those with significantly compromised predicted adult height (PAH) or poor growth velocity after GnRHa initiation [46]. The goal is to augment height potential by promoting longitudinal bone growth through the stimulation of insulin-like growth factor-1 (IGF-1), which can offset the growth deceleration sometimes seen with GnRHa therapy [46].
∿ Experimental Protocols for Efficacy Evaluation
Protocol 1: Assessing HPG Axis Suppression
Objective: To biochemically confirm the suppression of the HPG axis and monitor for breakthrough puberty during GnRHa therapy.
Methodology:
- GnRH Stimulation Test: Administer a standard dose of GnRH or GnRHa (e.g., Leuprolide acetate 20 mcg/kg subcutaneously) [45].
- Blood Sampling: Collect blood samples at baseline and at 30, 45, and 60 minutes post-injection.
- Hormone Assay: Measure serum LH and FSH levels using an ultrasensitive immunoassay.
- Interpretation: Successful suppression is typically indicated by a peak stimulated LH level [45].<="" around="" breakthrough="" inadequate="" iu="" l="" l,="" lh="" li="" may="" often="" or="" peak="" specific="" suggests="" suppression="" target="" though="" thresholds="" value,="" vary.="">
Protocol 2: Evaluating the Efficacy of Combination GnRHa and GH Therapy
Objective: To determine the additive effect of GH on growth outcomes in subjects undergoing GnRH suppression [46].
Methodology:
- Subject Stratification: Stratify subjects into pre-pubertal and pubertal groups to account for developmental differences in treatment response [47].
- Intervention Groups:
- Control Group: Receive GnRHa monotherapy.
- Combination Group: Receive GnRHa plus GH (e.g., PEG-rhGH at individualized doses).
- Dose Titration: In the combination group, adjust the GH dose based on the subject's IGF-1 levels and annual growth velocity. For example, a 10-20% dose increase may be applied for suboptimal annual growth (<7 cm/year) or IGF-1 levels outside the target range [47].
- Outcome Measures: Track primary outcomes including final height (FH), final height minus target height (FH-TH), and predicted adult height (PAH). Secondary outcomes include growth velocity (cm/year) and bone maturation ratio (ΔBA/ΔCA) [46].
- Monitoring: Assess clinical pubertal development every 3-6 months and laboratory parameters (e.g., IGF-1, LH, FSH) every 6-12 months [47].
∿ Quantitative Data on Therapeutic Regimens
Table 1: Growth Hormone Dose-Response Data in Pediatric Subjects
| Pubertal Status | PEG-rhGH Dose (mg/kg/week) | Growth Velocity (cm/year, Mean ± SD) | Statistical Significance (p-value) | Source |
|---|---|---|---|---|
| Pre-pubertal | ≤0.200 | 0.87 ± 0.23 | [47] | |
| Pre-pubertal | ≥0.220 | 1.10 ± 0.24 | 0.048 | [47] |
| Pubertal | ≤0.200 | 0.80 ± 0.20 | [47] | |
| Pubertal | ≥0.220 | 0.99 ± 0.38 | 0.017 | [47] |
Table 2: Efficacy Outcomes of GnRHa Monotherapy vs. Combination Therapy in Girls with CPP
| Outcome Measure | GnRHa Monotherapy | GnRHa + GH Combination | Weighted Mean Difference (WMD) | Source |
|---|---|---|---|---|
| Final Height (FH) | Baseline | Baseline | 0.14 cm (NS) | [46] |
| FH - Target Height | Baseline | Baseline | 1.01 cm | [46] |
| Predicted Adult Height (PAH) | Baseline | Baseline | 4.27 cm | [46] |
| Growth Velocity | Baseline | Baseline | 1.40 cm/year | [46] |
∿ Signaling Pathways and Experimental Workflows
Diagram 1: HPG Axis and GnRHa Suppression Mechanism. This diagram illustrates the hormonal cascade of puberty and the pivotal point where GnRHa acts to suppress the axis by desensitizing the pituitary gland, thereby inhibiting the release of LH and FSH.
Diagram 2: Therapy Management and Titration Workflow. This flowchart outlines the logical decision-making process for managing subjects on suppression therapy, from initial assessment through to the consideration of combination therapy.
∿ Research Reagent Solutions
Table 3: Essential Reagents and Materials for Puberty Suppression Research
| Item | Function/Application | Example Use Case |
|---|---|---|
| GnRH Analogues(e.g., Leuprolide, Triptorelin) | Suppress the HPG axis by downregulating GnRH receptors in the pituitary. | The gold-standard treatment for inducing and maintaining pubertal suppression in Central Precocious Puberty (CPP) [45]. |
| Long-acting GH Formulations(e.g., PEG-rhGH) | Promote longitudinal bone growth; once-weekly dosing improves adherence. | Used in combination therapy studies to improve growth velocity and height outcomes in subjects with a poor growth prognosis [47] [46]. |
| Ultrasensitive LH/FSH Immunoassays | Precisely measure low, pre-pubertal levels of gonadotropins in serum. | Critical for performing GnRH stimulation tests to diagnose CPP and confirm biochemical suppression during therapy [45]. |
| IGF-1 Immunoassays | Monitor the biological activity and safety profile of GH therapy. | Used for titrating the GH dose in combination therapy regimens to maintain levels within a target range [47]. |
| Bone Age Assessment Kit(X-ray & Atlas/Software) | Assess skeletal maturation by evaluating epiphyseal development in the hand and wrist. | A key tool for diagnosing CPP (bone age is typically advanced) and for monitoring the efficacy of treatment in delaying bone age progression [45]. |
What is the primary purpose of developing long-acting depot formulations for hormone suppression therapy? Long-acting depot formulations are designed to enhance patient compliance and therapeutic outcomes by providing sustained drug release over extended periods, thereby reducing the frequency of injections. In the context of hormone suppression therapy, such as managing central precocious puberty (CPP), these formulations maintain stable therapeutic hormone levels, which is crucial for preventing breakthrough puberty. The shift from daily injections to monthly or three-month depot formulations represents a significant advancement in patient-centric care, reducing the treatment burden and improving quality of life [48] [49].
How do depot formulations align with the broader strategy for managing breakthrough puberty? The overarching strategy for managing breakthrough puberty involves maintaining consistent suppression of the hypothalamic-pituitary-gonadal (HPG) axis. Depot formulations are integral to this strategy as they provide continuous drug release, minimizing hormone level fluctuations that could lead to breakthrough events. The development of these formulations requires careful balancing of drug potency, release kinetics, and safety profiles to ensure effective long-term suppression [49].
Key Formulation Characteristics: Monthly vs. Three-Month Depots
Table 1: Comparative Analysis of Monthly and Three-Month Depot Formulations
| Characteristic | Monthly Depot Formulations | Three-Month Depot Formulations |
|---|---|---|
| Administration Frequency | Every 1-3 months (typically 1 month) [48] | Every 3 months [49] |
| Typical Injection Volume | 1.5 mL (IM) [49] | 1 mL (IM) [49] |
| Drug Loading Requirement | Lower | Higher |
| Polymer Degradation Profile | Faster degradation kinetics | Slower, more controlled degradation |
| Peak-Trough Fluctuations | Moderate | Potentially higher |
| Risk of Breakthrough Puberty | Lower due to more frequent monitoring | Higher, requiring more robust formulation |
| Patient Adherence | Good | Excellent |
| Clinical Monitoring Needs | Quarterly to semi-annual | Less frequent |
Table 2: Administration Route Considerations for Depot Formulations
| Parameter | Intramuscular (IM) | Subcutaneous (SC) |
|---|---|---|
| Typical Volume | 2-5 mL [50] | 1-2 mL [50] |
| Onset of Action | Moderate (15-30 minutes) [50] | Slower (30 minutes to several hours) [50] |
| Bioavailability | High, slightly lower than IV [50] | High but variable [50] |
| Tissue Environment | Higher vascularization | Lower blood flow, lymphatic absorption |
| Patient Self-Administration | More challenging | More feasible |
| Formulation Requirements | Must be well-tolerated in muscle tissue | Must minimize local irritation |
Troubleshooting Guide: Common Technical Challenges and Solutions
FAQ 1: How can we address the high drug loading requirements for three-month depot formulations while maintaining injectability?
Challenge: Developing three-month depot formulations requires incorporating a significantly higher drug load into a similarly sized delivery system while maintaining acceptable viscosity for injection.
Solution:
- API Concentration: Increase the concentration of the Active Pharmaceutical Ingredient (API) while using viscosity-reducing excipients [50].
- Advanced Delivery Systems: Consider micro-emulsions, liposomal encapsulation, or nanoparticle carriers to enhance drug solubility and reduce injection volume [50].
- Permeation Enhancers: Utilize enzyme-based permeation enhancers like recombinant hyaluronidase to facilitate diffusion of larger molecules through tissues [50].
Experimental Protocol: Viscosity and Injectability Testing
- Prepare formulations with varying API concentrations (e.g., 100 mg/mL, 150 mg/mL, 200 mg/mL).
- Measure viscosity using a rheometer at shear rates representative of injection (100-1000 s⁻¹).
- Assess injectability forces using a texture analyzer or force gauge with standard syringes and needles.
- Determine maximum acceptable viscosity (typically <50 cP for easy injection through fine needles).
- Correlate viscosity results with in vitro release profiles to ensure target release kinetics are maintained.
FAQ 2: What strategies can prevent the initial burst release and ensure consistent drug release over extended periods?
Challenge: Excessive initial burst release can lead to adverse effects, while insufficient release may result in subtherapeutic levels and breakthrough puberty.
Solution:
- Polymer Blending: Combine PLGA polymers with different molecular weights and lactide:glycolide ratios to achieve desired release profiles [48].
- Core-Shell Particles: Develop multilayer microparticles where the outer layer acts as a diffusion barrier.
- Excipient Optimization: Incorporate additives like trehalose to stabilize the protein structure and control release kinetics [50].
Experimental Protocol: Burst Release Optimization
- Prepare microparticles using double emulsion solvent evaporation technique.
- Vary the PLGA molecular weight (10-100 kDa) and lactide:glycolide ratio (50:50 to 85:15).
- Characterize particle size distribution using laser diffraction.
- Conduct in vitro release studies in PBS (pH 7.4) at 37°C with continuous agitation.
- Sample at predetermined time points (1, 4, 8, 24, 48, 72 hours, then weekly up to 3 months).
- Analyze drug content using HPLC and calculate cumulative release.
- Target: <15% burst release in first 24 hours with consistent linear release thereafter.
FAQ 3: How can we mitigate the negative impact on bone mineral density in long-term hormone suppression therapy?
Challenge: Prolonged use of gonadotropin-releasing hormone (GnRH) analogues like leuprolide in depot formulations has been associated with decreased bone mineral density in some patients [51].
Solution:
- Co-therapy Considerations: Evaluate calcium and vitamin D supplementation as adjunct therapy.
- Drug Holidays: Consider intermittent dosing schedules for certain patient populations.
- Formulation Approaches: Explore incorporating bone-sparing agents directly into the depot system.
- Monitoring Protocols: Implement regular bone density scanning for patients on long-term therapy.
Experimental Protocol: Bone Safety Assessment in Preclinical Models
- Utilize appropriate animal models (e.g., juvenile rats or non-human primates).
- Administer monthly and three-month depot formulations at therapeutic doses.
- Include control groups receiving vehicle or standard care.
- Monitor serum biomarkers of bone turnover (e.g., CTX for resorption, P1NP for formation).
- Conduct DEXA scans at baseline, 3, 6, and 12 months to assess bone mineral density.
- Perform histological analysis of bone tissues at study termination.
- Compare results between monthly and three-month formulation groups to assess differential effects.
Experimental Design and Methodologies
Critical Experiments for Formulation Development
Table 3: Essential Experiments for Depot Formulation Development
| Experiment Type | Key Parameters Measured | Significance for Formulation Selection |
|---|---|---|
| In Vitro Release Testing | Release kinetics, burst effect, completeness of release | Predicts in vivo performance and guides formulation optimization |
| Stability Studies | Physical and chemical stability under stress conditions | Determines shelf life and storage requirements |
| Pharmacokinetic Profiling | Cmax, Tmax, AUC, half-life, fluctuation index | Establishes bioequivalence and dosing regimen |
| Tissue Tolerance | Injection site reactions, histopathology | Assesses local tolerability and safety |
| Bone Density Monitoring | DEXA scans, bone turnover markers | Evaluates long-term safety of hormone suppression |
Detailed Methodology: Accelerated Stability Testing for Depot Formulations
- Prepare three batches of each formulation (monthly and three-month).
- Store samples under ICH guidelines conditions:
- Long-term: 5°C ± 3°C
- Accelerated: 25°C ± 2°C/60% RH ± 5% RH
- Stress testing: 40°C ± 2°C/75% RH ± 5% RH
- Withdraw samples at predetermined time points (0, 1, 3, 6 months).
- Evaluate:
- Physical characteristics (appearance, particle size, viscosity)
- Drug content and related substances by HPLC
- In vitro release profile comparison to initial time point
- Polymer molecular weight changes by GPC
- Establish acceptance criteria: ≥90% drug potency, consistent release profile, no significant particle aggregation.
Visualization of Key Concepts
Diagram 1: Drug Release Mechanisms from Depot Formulations
Diagram 2: Depot Formulation Development Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Depot Formulation Research
| Reagent/Material | Function/Application | Technical Considerations |
|---|---|---|
| PLGA Polymers | Biodegradable matrix for controlled release | Varying lactide:glycolide ratios (50:50, 75:25, 85:15) and molecular weights control degradation rate [48] |
| Dichloromethane (DCM) | Solvent for oil phase in microencapsulation | Residual solvent limits must be controlled per ICH guidelines |
| Polyvinyl Alcohol (PVA) | Stabilizer in emulsion systems | Concentration and molecular weight affect particle size and distribution |
| Trehalose | Stabilizer for protein therapeutics | Protects against aggregation during fabrication and storage [50] |
| Hyaluronidase | Permeation enhancer for SC administration | Facilitates diffusion of larger molecules through subcutaneous tissue [50] |
| Tonicity Adjusting Agents | Osmolarity regulation | Mannitol, sucrose, or sodium chloride to match physiological osmolarity |
| Antioxidants | Prevention of API degradation | Methionine, ascorbic acid for oxidation-prone compounds |
Regulatory and Clinical Translation Considerations
What are the key regulatory requirements for transitioning from monthly to three-month depot formulations?
Bridging Studies Strategy: Regulatory authorities require robust evidence demonstrating comparable safety and efficacy between different depot formulations. For extending release duration from one to three months, comprehensive pharmacokinetic (PK) studies are essential [50].
Critical PK/PD Parameters for Bridging Studies:
- Peak-Trough Fluctuation: ≤30% difference between formulations
- AUC Comparison: 90% confidence interval of 80-125% for bioequivalence
- Dose Proportionality: Linear relationship between administered dose and exposure
- Accumulation Factor: ≤2.0 for safe long-term use
Clinical Trial Design Considerations:
- Patient Population: Include sufficient numbers across relevant age groups and pubertal stages
- Breakthrough Monitoring: Regular assessment of HPG axis hormones (LH, FSH, testosterone/estradiol)
- Safety Endpoints: Bone density scans, injection site reactions, systemic adverse events
- Long-term Follow-up: Minimum 12-month safety data for three-month formulations
The development of monthly versus three-month depot formulations represents a critical optimization challenge in hormone suppression therapy. The selection between these approaches must balance patient convenience with therapeutic consistency, particularly in preventing breakthrough puberty. Current evidence suggests that three-month formulations offer significant adherence benefits but require more sophisticated formulation strategies to ensure consistent release and minimize long-term safety concerns. As research in this field advances, particularly with ongoing clinical trials [52] [53], the understanding of optimal formulation approaches continues to evolve, promising improved outcomes for patients requiring long-term hormone suppression therapy.
FAQ: Troubleshooting Breakthrough Puberty in Preclinical Models
Q1: In our rodent model of central precocious puberty (CPP), monotherapy with a GnRH agonist (GnRHa) is failing to fully suppress testosterone. What are the primary mechanisms for this failure?
Breakthrough puberty during GnRHa therapy can occur due to several key mechanisms. A primary cause is the development of peripheral precocious puberty (PPP), which is GnRH-independent. This is characterized by elevated sex steroids (estradiol or testosterone) alongside suppressed luteinizing hormone (LH) and follicle-stimulating hormone (FSH) levels [54]. This condition can be driven by activating mutations in genes such as GNAS1 (as seen in McCune-Albright Syndrome) or the LH receptor gene (in Familial Male-Limited Precocious Puberty), leading to autonomous gonadal sex hormone production that bypasses the hypothalamic-pituitary-gonadal (HPG) axis [54]. Another mechanism is incomplete HPG axis suppression, where the chosen GnRHa formulation or dosing regimen is insufficient to fully downregulate pituitary receptors [55].
Q2: What adjuvant drug classes can be combined with GnRHa to overcome resistance, and how do their mechanisms of action differ?
When GnRHa monotherapy is insufficient, several adjuvant drug classes can be introduced to target the problem at different levels. The table below summarizes the primary options.
Table 1: Adjuvant Drug Classes for Combination Therapy with GnRHa
| Adjuvant Drug Class | Specific Examples | Mechanism of Action | Primary Target |
|---|---|---|---|
| Aromatase Inhibitors | Letrozole, Anastrozole, Testolactone [54] | Inhibits the aromatase enzyme, blocking the conversion of androgens to estrogens [54]. | Reduces estrogen levels in PPP. |
| Steroidogenesis Inhibitors | Ketoconazole [54] | Broadly inhibits cytochrome P450 enzymes involved in steroid hormone synthesis [54]. | Reduces production of both androgens and estrogens. |
| Selective Estrogen Receptor Modulators (SERMs) | Tamoxifen [54] | Blocks estrogen receptors in certain tissues, preventing estrogen from signaling [54]. | Mitigates estrogenic effects despite high estrogen levels. |
| Pure Estrogen Receptor Blockers | Fulvestrant [54] | Downregulates and degrades estrogen receptors [54]. | Completely blocks estrogen signaling. |
Q3: What is a detailed experimental protocol for testing a GnRHa + Aromatase Inhibitor combination in a preclinical PPP model?
Objective: To evaluate the efficacy of a GnRHa (Leuprolide) and Aromatase Inhibitor (Letrozole) combination therapy in a murine model of McCune-Albright Syndrome (MAS) with PPP.
Materials:
- Animal Model: Female mice with a postzygotic activating mutation in the GNAS gene [54].
- Test Compounds: Leuprolide acetate (GnRHa), Letrozole (Aromatase Inhibitor), and appropriate vehicle controls.
- Reagents: Assay kits for serum 17β-Estradiol (E2), Luteinizing Hormone (LH), and Follicle-Stimulating Hormone (FSH). Reagents for bone age analysis via X-ray.
Methodology:
- Group Allocation: Randomize pre-pubertal female MAS mice into four groups (n=10/group):
- Dosing & Monitoring: Administer treatments for 12 weeks. Monitor vaginal opening and estrus cyclicity daily as markers of puberty. Record body weight weekly.
- Terminal Analysis (Week 12):
- Blood Collection: Collect terminal blood samples. Analyze serum for E2 (LC/MS preferred for sensitivity), LH, and FSH via immunoassay [55].
- Tissue Harvest: Collect and weigh ovaries and uteri. Perform histopathological analysis on ovaries to characterize cysts.
- Bone Age Analysis: Perform X-ray on hind limbs. Determine bone age by assessing epiphyseal plate closure and comparing to a known standard [54].
Expected Outcomes: The combination therapy group should demonstrate significantly lower uterine weights, reduced ovarian cyst formation, and a normalized bone age/chronological age ratio compared to monotherapy or control groups, indicating superior suppression of estrogenic effects.
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Investigating Puberty Suppression Therapies
| Reagent / Material | Function in Experimental Protocol |
|---|---|
| GnRH Agonists (Leuprolide, Histrelin) [55] [2] | To suppress the central HPG axis and establish a baseline model of central puberty suppression. |
| Aromatase Inhibitors (Letrozole, Anastrozole) [54] | To test combination strategies for overcoming GnRH-independent, estrogen-driven PPP in models like MAS. |
| Liquid Chromatography/Mass Spectrometry (LC/MS) [55] | For the highly sensitive and accurate quantification of low, prepubertal levels of sex steroids like estradiol and testosterone. |
| Immunoassay Kits (LH, FSH) [55] | To measure gonadotropin levels and confirm the state of the HPG axis (suppressed vs. active). |
| Bone Age X-Ray Analysis System | To quantitatively assess one of the most critical long-term outcomes of precocious puberty: skeletal maturation and its attenuation by therapy [54]. |
Visualizing Signaling Pathways and Experimental Logic
HPG Axis and Drug Targets
This diagram illustrates the hypothalamic-pituitary-gonadal (HPG) axis, the target of GnRHa therapy, and the peripheral pathways targeted by adjuvant therapies in cases of breakthrough puberty.
Combination Therapy Experimental Workflow
This flowchart outlines the logical decision-making process and experimental workflow for investigating and troubleshooting combination therapies for breakthrough puberty.
FAQs on Managing Breakthrough Puberty in Research
What defines treatment failure in hormone suppression therapy research? Treatment failure, or breakthrough puberty, is the progressive development of secondary sexual characteristics despite ongoing GnRH agonist therapy. Key indicators include a confirmed rise in serum Luteinizing Hormone (LH) >0.3 IU/L and testosterone >50 ng/dL in males or estradiol >20 pg/mL in females, alongside a sustained increase in testicular volume >4 mL in males or progression in breast development in females over a 3-6 month period [56].
What are the first-line investigative steps following suspected treatment failure? The initial investigation should prioritize confirming treatment adherence and proper drug administration to rule out pseudo-failure. The subsequent diagnostic workflow involves simultaneous biochemical and clinical monitoring [56].
When should researchers consider switching to a second-generation GnRH analog? Consider switching upon confirmation of true treatment failure with an approved first-line GnRH analog (e.g., leuprolide, triptorelin). Emerging research suggests second-generation analogs (e.g, degarelix) or higher-dose formulations may overcome failure, particularly in cases with advanced puberty at therapy initiation (bone age >12 years in girls, >14 years in boys) or in subjects with high BMI [57] [56].
What rescue strategies exist for candidates with confirmed GnRH analog failure? Rescue strategies involve combination therapy or surgical intervention. The choice depends on the research context, ethical approvals, and subject characteristics [10] [56].
- Additive Combination Therapy: Introducing an anti-androgen (e.g., spironolactone, bicalutamide) or aromatase inhibitor (e.g., letrozole) alongside the GnRH analog to block the peripheral action or synthesis of sex hormones.
- Surgical Intervention (Gonadectomy): A last-resort option in extreme cases, exclusively within approved clinical trial frameworks. It definitively eliminates endogenous sex hormone production.
Troubleshooting Guide: Breakthrough Puberty
Problem: Incomplete Puberty Suppression
| Symptom | Possible Cause | Investigation | Immediate Action |
|---|---|---|---|
| Rising LH/testosterone or LH/estradiol levels | Inadequate dosing, poor adherence, compromised drug storage | Verify administration records, dosing schedule, storage conditions | Review and correct dosing protocol; ensure proper handling |
| Progressing Tanner stage, rising hormone levels | True pharmacological resistance | GnRH stimulation test; check for neutralizing antibodies | Document failure; prepare for agent switch |
| Advanced bone age, virilization/feminization | Late therapy initiation (post-mid-puberty) | Compare bone age to chronological age | Consider more aggressive rescue therapy |
Problem: Hormonal Escape After Initial Suppression
| Symptom | Possible Cause | Investigation | Immediate Action |
|---|---|---|---|
| Hormone levels rise after >6 months of suppression | Antibody development against therapeutic agent | Assay for anti-drug antibodies | Switch to a different GnRH analog molecule |
| Central precocious puberty re-activation | Underlying CNS pathology progression | Repeat brain MRI (if clinically indicated) | Address underlying cause; consider neurosurgical consult |
Experimental Protocols for Efficacy Assessment
Protocol 1: Confirmatory Testing for Treatment Failure
Objective: To biochemically confirm suspected treatment failure in a research subject.
- Pre-test Preparation: Subject to fast for 4 hours prior to blood draw. Document the exact time of the last GnRH analog dose.
- Blood Sampling: Draw venous blood for:
- Baseline LH, FSH
- Testosterone (in males) or Estradiol (in females)
- Sample Processing: Centrifuge at 3000 rpm for 10 minutes within 30 minutes of collection. Store serum at -80°C if not assayed immediately.
- GnRH Stimulation Test:
- Administer a standard dose of synthetic GnRH (e.g., 100 µg intravenously).
- Draw post-stimulation blood samples at 30, 45, and 60 minutes for LH/FSH measurement.
- Interpretation: A peak LH response >5-8 IU/L is diagnostic of central puberty activation and confirms failure of suppression [56].
Protocol 2: Evaluating Rescue Therapy with Combination Regimens
Objective: To assess the efficacy of an anti-androgen as a rescue therapy in males with breakthrough puberty on GnRH analogs.
- Subject Selection: Males with confirmed treatment failure (as per Protocol 1).
- Study Design: Open-label, add-on trial. Continue the current GnRH analog.
- Intervention: Administer oral bicalutamide (50 mg/m²/day, max 100 mg/day) or spironolactone (start 1-2 mg/kg/day BID).
- Monitoring Schedule:
- Bi-weekly for Month 1: Serum testosterone, LH, FSH, liver function tests (LFTs).
- Monthly for Months 2-6: Hormone levels, Tanner staging, testicular volume, LFTs, bone age at 6 months.
- Success Criteria: Testosterone reduction to <30 ng/dL and halting of pubertal progression over 3 months.
Key Signaling Pathways in Treatment Failure
The pathway below outlines the physiological mechanism of puberty and the points of intervention for therapies, helping to identify potential mechanisms of treatment failure [56] [58].
Research Reagent Solutions
| Reagent / Material | Function in Protocol | Key Considerations |
|---|---|---|
| GnRH Agonists(Leuprolide, Triptorelin) | First-line pubertal suppression | Different salts/esters have varying release kinetics; document lot numbers. |
| Second-gen GnRH Analogs(e.g., Degarelix) | Rescue therapy for failure | Primarily used in prostate cancer research; off-label use requires rigorous IRB approval [57]. |
| Anti-Androgens(Bicalutamide, Spironolactone) | Blocks androgen receptors in rescue therapy | Monitor for hepatotoxicity (bicalutamide) and electrolyte imbalance (spironolactone). |
| Aromatase Inhibitors(Letrozole, Anastrozole) | Reduces estrogen synthesis in rescue therapy | More applicable in peripheral precocious puberty or estrogen-driven progression [59]. |
| ELISA Kits(for LH, FSH, Testosterone, Estradiol) | Biochemical monitoring of therapy efficacy | Ensure kits are calibrated to CDC-defined standards; use same kit batch for longitudinal studies. |
| GnRH for Stimulation Test | Diagnostic tool to confirm central puberty | Source from certified pharmaceutical suppliers; requires immediate use after reconstitution. |
Patient-Specific Dosing Algorithms Based on Risk Stratification
Patient-specific dosing algorithms represent a paradigm shift in therapeutic development, moving away from a "one-size-fits-all" approach to precision medicine. These algorithms integrate patient-specific factors—including genetic makeup, clinical characteristics, and biomarkers—to determine optimal dosing regimens that maximize efficacy while minimizing adverse effects. Within hormone suppression therapy research, particularly for conditions like central precocious puberty (CPP), these advanced dosing strategies are essential for managing complex endocrine pathways and ensuring sustained therapeutic effects. This technical support center provides researchers with practical guidance for implementing these sophisticated algorithms in experimental settings, with a specific focus on managing breakthrough puberty during hormone suppression studies.
Fundamentals of Risk Stratification in Dosing Algorithms
Risk stratification forms the foundational framework for developing patient-specific dosing algorithms. In clinical practice, this involves categorizing patients based on their susceptibility to specific outcomes, which directly informs therapeutic decisions. [60]
Key Concepts:
- Risk Stratification: The process of categorizing patients into distinct groups based on their probability of experiencing specific health outcomes or responding to treatments
- Patient-Specific Dosing: The customization of medication dosages based on individual patient characteristics rather than population averages
- Algorithm Adjudication: The process where clinicians review and adjust algorithm-generated recommendations based on nuanced patient factors not captured in automated models [60]
Modern risk stratification approaches often combine automated algorithms with clinical expertise. Studies demonstrate that provider adjudication of risk scores significantly improves prediction models for adverse outcomes compared to algorithms alone, with one study showing c-statistics improving from 0.649 to 0.663 for hospital admissions and from 0.721 to 0.753 for mortality. [60] This hybrid approach is particularly valuable for capturing complex patient factors like disease severity, self-management capabilities, and behavioral health considerations that may not be fully represented in structured electronic health record data. [60]
Troubleshooting Guides for Research Scenarios
Managing Breakthrough Puberty During Hormone Suppression Therapy
Problem: Resumption of pubertal development despite ongoing gonadotropin-releasing hormone analog (GnRHa) therapy.
Diagnostic Steps:
- Verify HPG Axis Suppression: Conduct a GnRH stimulation test to measure luteinizing hormone (LH) and follicle-stimulating hormone (FSH) responses. Inadequate suppression indicates insufficient dosing. [5]
- Assess Bone Age Progression: Obtain annual left hand and wrist radiographs. Accelerated bone age advancement (>1 year per chronological year) suggests incomplete puberty suppression. [12]
- Review Medication Administration: Confirm proper injection technique for depot formulations and check implant placement and integrity for subcutaneous delivery systems. [61]
- Evaluate Compliance: Document administration dates and verify adherence to the prescribed dosing schedule.
Solutions:
- Dose Adjustment: Increase GnRHa frequency or dosage following confirmation of inadequate suppression. [61]
- Formulation Change: Switch from 3-month to 1-month formulations for more consistent suppression, or consider a histrelin implant for sustained release. [61]
- Combination Therapy: For patients with significantly advanced bone age and growth deceleration, consider adding growth hormone adjunctively to improve adult height outcomes. [12]
Unexplained Variation in Drug Response
Problem: Significant inter-individual variability in treatment response not explained by standard demographic factors.
Diagnostic Steps:
- Pharmacogenetic Testing: Identify polymorphisms in drug-metabolizing enzymes (e.g., CYP450 family) and drug targets. [62]
- Therapeutic Drug Monitoring: Measure drug and metabolite levels at trough and peak periods.
- Evaluate Non-Genetic Factors: Assess liver and kidney function, concomitant medications, body composition, and timing of administration.
Solutions:
- Algorithm Refinement: Incorporate pharmacogenetic and clinical factors into dosing algorithms. For example, warfarin dosing algorithms that include CYP2C9 and VKORC1 genotypes plus clinical factors (age, weight, concomitant medications) improve predictive accuracy. [62]
- Bayesian Forecasting: Use Bayesian methods to individualize dosing based on prior doses and observed responses, particularly for drugs with narrow therapeutic windows. [63]
Algorithm Performance Issues
Problem: Dosing algorithms demonstrate declining performance when applied to new patient populations.
Diagnostic Steps:
- External Validation: Test algorithm performance in diverse demographic groups and clinical settings.
- Feature Analysis: Identify predictor variables with significantly different distributions between development and application cohorts.
- Bias Assessment: Evaluate algorithmic fairness across sex, race, age, and socioeconomic groups.
Solutions:
- Algorithm Retraining: Fine-tune models using transfer learning approaches with local data.
- Ensemble Methods: Combine multiple algorithms to improve robustness and generalizability.
- Continuous Learning: Implement systems for ongoing algorithm performance monitoring and periodic recalibration.
Frequently Asked Questions (FAQs)
Q1: What are the key components of an effective patient-specific dosing algorithm? Effective dosing algorithms integrate multiple data types: genetic variants affecting drug metabolism (pharmacogenetics), clinical biomarkers, demographic factors, and real-time treatment response data. The most successful algorithms combine these elements using appropriate statistical models (e.g., machine learning, Bayesian methods) and allow for clinician oversight and adjustment. [63] [62]
Q2: How can we validate a new dosing algorithm before implementation in clinical trials? Use rigorous internal validation (cross-validation, bootstrap methods) followed by external validation in independent datasets. Assess both discrimination (AUC-ROC) and calibration (observed vs. predicted response). For critical applications, consider prospective validation in limited pilot studies before full trial implementation. [64]
Q3: What distinguishes clinician-initiated data from non-clinician-initiated data in risk stratification models? Clinician-initiated data reflects clinical decision-making (test orders, prescriptions, procedures) and may incorporate clinician intuition and suspicion. Non-clinician-initiated data includes routine orders and direct physiological measurements. Models relying heavily on clinician-initiated data may be "looking over the clinician's shoulder" rather than providing truly novel insights. [65]
Q4: How should we handle missing data in algorithm development? Establish a missing data protocol before algorithm development. Options include complete-case analysis, multiple imputation, or using algorithms that handle missing data natively (e.g., XGBoost). The approach should be guided by the missing data mechanism and proportion. [64]
Q5: What are the ethical considerations in risk-stratified dosing? Key considerations include transparency in algorithm development, validation across diverse populations, addressing potential health disparities, ensuring clinician oversight, and maintaining patient autonomy in decision-making. Algorithms should be tools to enhance, not replace, clinical judgment. [60]
Quantitative Data on Algorithm Performance
Table 1: Performance Metrics of Risk Stratification Models for Healthcare Outcomes
| Model Type | Application Context | Outcome Predicted | Performance (AUC) | Reference |
|---|---|---|---|---|
| Machine Learning (XGBoost) | ICU patients with heart failure | In-hospital mortality | 0.831 | [64] |
| Adjudicated Risk Model | Primary care population | Emergency department visits | 0.689 | [60] |
| Adjudicated Risk Model | Primary care population | Hospital admissions | 0.663 | [60] |
| Adjudicated Risk Model | Primary care population | Death | 0.753 | [60] |
| Commercial Algorithm | Primary care population | Hospital admissions | 0.649 | [60] |
| Deep Learning (Charges Data) | General inpatient population | In-hospital mortality | 0.89 | [65] |
| Deep Learning (Charges Data) | General inpatient population | 30-day readmission | 0.71 | [65] |
| Deep Learning (Charges Data) | General inpatient population | Prolonged length of stay | 0.82 | [65] |
Table 2: GnRHa Formulations for Central Precocious Puberty
| Generic Name | Brand Name | Route | Available Doses | Duration of Action | Efficacy Notes |
|---|---|---|---|---|---|
| 3-monthly leuprolide | Lupron Depot-PED 3mo | Intramuscular | 11.25 mg, 30 mg | 3 months | <100% HPG-axis suppression in some studies [61] |
| 6-monthly triptorelin | Triptodur | Intramuscular | 22.5 mg | 6 months | 93% suppression at 6 months, 97.7% at 12 months [61] |
| Histrelin | Supprelin LA | Subcutaneous implant | 50 mg | ≥2 years | Profound suppression within 1 month; lasts beyond 1 year [61] |
Experimental Protocols
Protocol 1: Development and Validation of a Patient-Specific Dosing Algorithm
Objective: To create and validate a dosing algorithm that personalizes medication dosage based on genetic, clinical, and demographic factors.
Materials:
- Patient dataset with outcome measures
- Statistical software (R, Python)
- Genotyping platform (for pharmacogenetic algorithms)
Methodology:
- Cohort Selection: Define inclusion/exclusion criteria. Ensure adequate sample size for development and validation cohorts.
- Predictor Selection: Identify candidate predictors (demographic, clinical, genetic, behavioral).
- Model Building:
- For continuous outcomes: Use linear regression with regularization (LASSO, ridge)
- For binary outcomes: Use logistic regression or machine learning classifiers (XGBoost, random forests)
- For time-to-event outcomes: Use Cox proportional hazards models
- Internal Validation: Use bootstrapping or cross-validation to assess optimism and adjust performance estimates.
- External Validation: Test the algorithm in an independent dataset from a different population or setting.
- Clinical Implementation: Develop user-friendly tools for algorithm application in clinical settings.
Analysis: Evaluate algorithm performance using discrimination (C-statistic, AUC-ROC), calibration (plots, statistics), and clinical utility (decision curve analysis). [64] [62]
Protocol 2: Monitoring Hormone Suppression Therapy Efficacy
Objective: To assess the effectiveness of GnRHa therapy in suppressing the hypothalamic-pituitary-gonadal (HPG) axis.
Materials:
- GnRHa preparation (depot injection or implant)
- Equipment for venipuncture and blood sample processing
- GnRH for stimulation testing
- LH and FSH assays
- X-ray equipment for bone age assessment
Methodology:
- Baseline Assessment:
- Record Tanner staging, growth velocity, and physical examination
- Obtain bone age radiograph (left hand and wrist)
- Measure baseline LH, FSH, and sex hormones
- GnRH Stimulation Test:
- Administer GnRH (typically 100 μg intravenous)
- Measure LH and FSH at 0, 30, 60 minutes post-administration
- Interpret results: Prepubertal response if peak LH <3-5 mIU/mL (assay-dependent)
- Therapy Initiation: Administer appropriate GnRHa formulation based on risk stratification.
- Follow-up Monitoring:
- Conduct GnRH stimulation test 4-6 months after initiation
- Monitor growth velocity every 3-6 months
- Assess bone age annually
- Evaluate for pubertal progression every 6 months
Interpretation: Adequate suppression is confirmed by prepubertal LH response to GnRH stimulation, deceleration of growth velocity to prepubertal rates, and reduction in bone age advancement. [12] [5] [61]
Signaling Pathways and Workflows
Algorithm Development Workflow
Hormone Suppression Monitoring Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for Dosing Algorithm Studies
| Research Reagent | Manufacturer/Source | Application in Dosing Research | Key Considerations |
|---|---|---|---|
| GnRHa Formulations (leuprolide, triptorelin, histrelin) | Multiple pharmaceutical companies | Hormone suppression therapy; PK/PD studies | Consider duration of action, route of administration, and dose equivalencies [61] |
| LH/FSH Immunoassays | Various diagnostic companies | HPG axis suppression monitoring | Validate assay-specific cutoffs for pubertal vs. prepubertal levels [5] |
| Genotyping Platforms (e.g., CYP450 arrays) | Thermo Fisher, Illumina, others | Pharmacogenetic profiling | Select platforms that cover clinically relevant variants with known functional impact [62] |
| Bone Age Atlas Software | Multiple providers | Skeletal maturation assessment | Use consistent methodology across study; Greulich-Pyle or Tanner-Whitehouse methods [12] |
| Statistical Software (R, Python with scikit-learn) | Open source or commercial | Algorithm development and validation | Ensure reproducibility through version control and code sharing [64] |
| Electronic Health Record Data Extraction Tools | Institution-specific | Real-world data collection for validation | Address missing data, data quality, and harmonization across sources [60] [65] |
Therapeutic Efficacy Assessment and Comparative Outcomes Analysis
Within strategies for managing breakthrough puberty during hormone suppression therapy research, defining and measuring "efficacy" is a dual-faceted concept. Efficacy is evaluated through two primary, complementary lenses: hormonal suppression (the biochemical process) and clinical outcomes (the physical and psychological results). Hormonal suppression refers to the direct measurement of reduced gonadotropin and sex steroid levels, serving as an immediate, objective biomarker for treatment effectiveness. Clinical outcomes encompass the tangible physical prevention of unwanted pubertal development and the subsequent improvement in psychological well-being. Understanding the relationship between these two metrics is fundamental for researchers developing and optimizing puberty suppression protocols, particularly when troubleshooting cases of incomplete suppression or unexpected clinical progression.
Quantitative Efficacy Data
The efficacy of Gonadotropin-Releasing Hormone Agonists (GnRHa) is consistently demonstrated through the suppression of key hormonal levels. The tables below summarize quantitative data from clinical studies, providing a reference for expected outcomes.
Table 1: Hormonal Suppression with GnRHa in Transgender and CPP Adolescents after 2-12 Months of Treatment [55]
| Hormone / Group | Baseline Level (Mean ± SD) | Post-Treatment Level (Mean ± SD) |
|---|---|---|
| LH (mIU/mL) | ||
| • CPP Males / Transgender AMAB | 2.9 ± 1.6 | 0.4 ± 0.4 |
| • Transgender AMAB | 1.8 ± 1.4 | 0.6 ± 0.8 |
| FSH (mIU/mL) | ||
| • CPP Males / Transgender AMAB | 8.0 ± 9.1 | 0.4 ± 0.2 |
| • Transgender AMAB | 2.9 ± 1.9 | 0.5 ± 0.3 |
| Testosterone (ng/dL) | ||
| • CPP Males / Transgender AMAB | 180.8 ± 112.7 | Data Incomplete |
| • Transgender AMAB | 282.3 ± 224.7 | Data Incomplete |
| Estradiol (pg/mL) | ||
| • CPP Females / Transgender AFAB | 27.5 ± 20.8 | 1.8 ± 1.8 |
| • Transgender AFAB | 38.6 ± 27.1 | 9.4 ± 9.7 |
Table 2: Efficacy of Leuprolide Acetate 11.25 mg 3-Month Formulation in CPP [21]
| Efficacy Metric | Baseline | 3 Months Post-Treatment | 6 Months Post-Treatment |
|---|---|---|---|
| Stimulated LH (IU/L) | Not Specified | 1.90 | 0.70 |
| Proportion with Peak LH < 4 IU/L | Not Applicable | Not Specified | 94% |
| Growth Velocity (cm/year) | Not Specified | Not Specified | 6.11 |
| Bone Age/Chronological Age Ratio | Baseline | -0.04 change at 6mo | -0.30 change at 12mo |
Table 3: Biochemical Suppression Rates of Leuprolide Formulations in TGD Youth [66]
| Formulation | Administration Route | Biochemical Suppression Rate | Clinical Suppression Rate |
|---|---|---|---|
| Eligard | Subcutaneous | 90% | 100% |
| Lupron | Intramuscular | 69% | 100% |
Troubleshooting Guide: Managing Breakthrough Puberty
FAQ 1: What defines "breakthrough puberty" in a research context? Breakthrough puberty refers to the unexpected progression of pubertal development or an insufficient suppression of sex hormones following the initiation of GnRHa therapy. In a clinical trial or experimental setting, this is typically identified by [55] [66]:
- Biochemically: A stimulated LH level > 3-4 IU/L or sex steroid levels (testosterone or estradiol) failing to drop to prepubertal ranges after the initial suppression period.
- Clinically: Self-reported or physician-observed signs of continued pubertal progression, such as testicular growth, menstruation, or breast development.
FAQ 2: Our data shows suppressed LH but elevated estradiol in AFAB participants. Is this a treatment failure? Not necessarily. Research has shown that estradiol levels can remain higher in transgender youth assigned female at birth (AFAB) compared to those with central precocious puberty (CPP) despite similar LH and FSH suppression (e.g., 9.4 ± 9.7 pg/mL vs. 1.8 ± 1.8 pg/mL) [55]. This discrepancy may be related to the extragonadal production of estrogens or other non-pituitary factors. The critical metric is the clinical suppression of pubertal progression. If clinical progression is halted, the treatment may still be considered effective for its primary goal.
FAQ 3: A subject in our trial has unsuppressed post-injection hormone levels. What are the potential causes? This requires a systematic investigation. Potential causes and actions are outlined in the following diagnostic workflow.
FAQ 4: How do we measure and report "clinical puberty suppression" as a primary outcome? Robust measurement of clinical outcomes requires a multi-modal approach beyond just hormone levels. Key metrics include [67] [68]:
- Physical Examination: Tanner Staging by a trained clinician to document stability or regression of secondary sexual characteristics.
- Patient-Reported Outcomes (PROs): Use of validated scales to track changes in gender dysphoria, body image, and psychological functioning.
- Psychosocial Metrics: Assessment of anxiety, depression, and overall quality of life through standardized questionnaires.
- Documentation of Pubertal Events: Tracking specific events, such as the absence of menses in AFAB individuals after menarche.
Experimental Protocols for Efficacy Evaluation
Protocol: Biochemical Suppression Assay
This protocol details the methodology for assessing hormonal suppression, a core metric in GnRHa research [55] [66].
- Objective: To quantify the suppression of the hypothalamic-pituitary-gonadal (HPG) axis by measuring serum levels of LH, FSH, and sex steroids (Testosterone or Estradiol) following GnRHa administration.
- Materials:
- Blood Collection: Serum separator tubes.
- Assay Kits: Immunoassay (IA) for LH and FSH; Liquid Chromatography/Mass Spectrometry (LC/MS) for total Testosterone and Estradiol (recommended for higher accuracy) [55].
- GnRHa Stimulus: Leuprolide acetate injection (Eligard or Lupron).
- Procedure:
- Baseline Measurement: Obtain baseline (unstimulated) levels of LH, FSH, and the relevant sex steroid.
- Administer GnRHa: Administer the standard research dose of the GnRHa (e.g., Leuprolide 22.5 mg IM or SC).
- Post-Injection Sampling: Draw blood for hormone level measurement 1 hour after the injection (1hrPost). This timing is critical for detecting an initial agonist-stimulated rise, which indicates proper delivery and bioavailability [66].
- Trough Monitoring: For long-term studies, also measure hormone levels immediately before the next scheduled dose (trough level) to ensure continuous suppression.
- Analysis: Compare pre- and post-treatment levels. Effective suppression is typically defined by a stimulated LH level < 3-4 IU/L and sex steroids in the prepubertal range.
Protocol: Longitudinal Assessment of Clinical and Psychological Outcomes
This protocol outlines the long-term tracking of clinical efficacy, which is the ultimate goal of therapy [67] [68].
- Objective: To evaluate the physical and psychological impact of puberty suppression over time.
- Materials:
- Clinical Assessment Forms: Standardized Tanner Stage assessment sheets.
- Validated Questionnaires:
- Gender Dysphoria scales.
- Beck Depression Inventory (BDI) and Beck Anxiety Inventory (BAI).
- Youth Quality of Life instruments.
- Anthropometric Tools: Stadiometer, scale, and calipers for growth and BMI tracking.
- Imaging: Radiographs for bone age assessment (e.g., left hand and wrist).
- Procedure:
- Baseline Assessment (T0): Conduct at treatment initiation. Record Tanner Stage, bone age, height, weight, and administer all psychological questionnaires.
- On-Treatment Assessment (T1): Conduct at 6 and 12 months, then annually. Repeat all T0 measurements. Specifically document any signs of clinical puberty progression (e.g., testicular volume increase, breakthrough bleeding).
- Long-Term Follow-up (T2): Conduct after subsequent treatments (e.g., after cross-sex hormones and surgery) to assess long-term psychological well-being and satisfaction [67].
- Data Analysis: Use paired statistical tests (e.g., paired t-tests) to compare changes from baseline in quantitative scores (e.g., depression scores). Correlate improvements in psychological functioning with postsurgical subjective well-being.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 4: Essential Materials for Puberty Suppression Research
| Item | Function in Research | Example Products & Notes |
|---|---|---|
| GnRH Agonists | The primary intervention to suppress the HPG axis. | Leuprolide (Lupron, Eligard), Triptorelin (Triptodur), Histrelin (Supprelin LA implant). Note different formulations (1-mo, 3-mo, 6-mo, yearly implant) for dosing schedule studies [21] [69]. |
| LH/FSH Immunoassay | To measure gonadotropin levels for biochemical efficacy. | Various commercial IA kits. Ensure consistent use across study timepoints for reliable data [55]. |
| LC-MS/MS | Gold standard for accurate measurement of sex steroids (Testosterone, Estradiol). | Recommended over immunoassay for its higher specificity and accuracy, especially at low/prepubertal levels [55]. |
| Tanner Stage Criteria | Standardized tool for objective clinical assessment of pubertal development. | Requires training for reliable application. A key non-invasive clinical endpoint [55] [68]. |
| Validated PRO Scales | To quantify psychological outcomes (gender dysphoria, quality of life, mental health). | Scales for gender dysphoria, Beck's Depression/Anxiety Inventory, Youth QoL tools. Critical for demonstrating clinical benefit [67] [68]. |
Troubleshooting Guide: Frequently Asked Questions
FAQ 1: What are the key differences in the adverse event (AE) profiles of triptorelin, leuprolide, and goserelin in real-world settings?
Real-world data from the US Food and Drug Administration Adverse Event Reporting System (FAERS) highlights significant differences in the safety profiles of these GnRHa formulations [70].
- Goserelin has been associated with a significantly higher reported mortality rate (29.3%) compared to other agents, though this reporting bias may reflect its more frequent use in advanced cancer populations rather than a direct causal effect [70].
- Leuprolide and goserelin are more frequently reported in older patient populations (61-80 years), primarily for prostate cancer management, which influences the type of adverse events observed [70].
- Triptorelin adverse events are reported in a larger proportion of patients under 18 years of age [70].
- General Safety: All five long-acting GnRHa medications (including triptorelin, leuprolide, and goserelin) carry an elevated risk of significant medical events. This risk is notably lower in pediatric patients (<18 years) compared to adult populations (≥18 years) [70].
Table 1: Comparative Analysis of Long-Acting GnRHa Formulations [70]
| Parameter | Triptorelin | Leuprolide | Goserelin |
|---|---|---|---|
| Commonly Reported Indications | Central Precocious Puberty (CPP), Prostate Cancer | Prostate Cancer, Endometriosis, Uterine Leiomyomas | Prostate Cancer, Breast Cancer |
| Prominent AE Categories | Reproductive & breast disorders | Reproductive & breast disorders | Reproductive & breast disorders |
| Notable Patient Demographics | Higher proportion of reports in patients ≤18 years | Higher proportion of reports in patients 61-80 years | Higher proportion of reports in patients 61-80 years |
| Serious Outcome: Mortality | Lower reported mortality | Lower reported mortality | Higher reported mortality (29.3%) |
FAQ 2: How do I monitor and manage the risk of bone density loss in subjects receiving long-term GnRH agonist therapy?
Bone density loss is a recognized long-term effect of GnRHa therapy due to the induced hypoestrogenic or hypoandrogenic state [37].
- Monitoring Protocol: It is recommended that individuals taking GnRHa have their height checked every few months. Annual bone density and bone age tests are also advised [37].
- Preventive Strategy: To support bone health, patients may need to take calcium and vitamin D supplements. The addition of "add-back therapy" (estrogen or progestin) is a established clinical strategy to mitigate bone loss while maintaining the primary therapeutic benefit in adults [71].
FAQ 3: One of our research subjects is experiencing a suspected "breakthrough puberty" event. What are the potential causes and investigative steps?
Breakthrough puberty refers to the unsuppressed activation of the hypothalamic-pituitary-gonadal (HPG) axis during intended suppression therapy.
- Verify HPG Axis Suppression: The gold standard for assessing the effectiveness of puberty suppression is the measurement of blood levels of luteinizing hormone (LH), follicle-stimulating hormone (FSH), and the relevant sex hormone (testosterone or estradiol) [55]. Effective suppression results in low, pre-pubertal levels of these hormones.
- Confirm Medication Adherence and Formulation: For monthly injections, ensure the dosing schedule has been maintained. For implants (e.g., histrelin), confirm the device is still in place and has not been prematurely expelled or exhausted [55].
- Investigate Pharmacological Failure: Consider the possibility of inadequate drug delivery or individual variations in drug metabolism.
Experimental Protocols for Efficacy Assessment
Protocol 1: Assessing HPG Axis Suppression in Clinical Research
This protocol is based on standardized methodologies used to evaluate the biochemical effectiveness of GnRHa [55].
Objective: To verify the suppression of the HPG axis following administration of triptorelin, leuprolide, or goserelin. Materials:
- Research-grade GnRHa formulation (Triptorelin, Leuprolide, or Goserelin)
- Phlebotomy supplies
- Access to LC/MS or immunoassay platforms for hormone testing (LH, FSH, Testosterone, Estradiol)
Workflow:
- Baseline Blood Draw: Collect pre-treatment blood samples for baseline LH, FSH, and sex hormone (testosterone for AMAB subjects, estradiol for AFAB subjects) levels.
- Administer GnRHa: Administer the designated GnRHa according to the study protocol (e.g., intramuscular injection, subcutaneous implant).
- Follow-up Blood Draw: Collect follow-up blood samples 2-3 months after treatment initiation or as per the specific drug's pharmacodynamic profile.
- Analysis: Analyze hormone levels. Successful suppression is indicated by [55]:
- LH and FSH levels typically dropping to <1.0 mIU/mL.
- Testosterone levels in AMAB subjects dropping to castrate levels.
- Estradiol levels in AFAB subjects dropping to post-menopausal levels (though note, one study found estradiol levels may be higher in transgender AFAB patients compared to females with CPP despite similar LH/FSH suppression) [55].
Diagram Title: HPG Axis Suppression Verification Workflow
Protocol 2: In Vitro Assessment of GnRHa Receptor Binding and Activation
Objective: To compare the binding affinity and functional activity of different GnRHa formulations on the GnRH receptor. Materials:
- Cell line expressing human GnRH receptor (e.g., HEK293-GnRHR)
- GnRHa analogs (Triptorelin, Leuprolide, Goserelin)
- Radiolabeled or fluorescently tagged GnRH antagonist
- IP3 or Ca2+ detection kit for signaling output
Workflow:
- Cell Preparation: Culture cells in appropriate medium and plate for experimentation.
- Binding Assay: Incubate cells with a constant concentration of tagged antagonist and increasing concentrations of each unlabeled GnRHa. Measure the displacement of the antagonist to determine IC50 values.
- Signaling Assay: Stimulate cells with a range of concentrations of each GnRHa. Measure downstream second messengers (e.g., IP3 accumulation or intracellular Ca2+ flux) to determine EC50 and efficacy.
- Data Analysis: Compare the potency (IC50, EC50) and efficacy of the different analogs.
Underlying Signaling Pathways
Gonadotropin-Releasing Hormone analogs function by modulating the hypothalamic-pituitary-gonadal (HPG) axis.
Diagram Title: GnRHa Mechanism on the HPG Axis
The initial administration of a GnRHa causes a surge in LH and FSH secretion (the "flare" effect). However, continuous, non-pulsatile stimulation leads to downregulation and desensitization of pituitary GnRH receptors. This results in a profound suppression of LH and FSH release, which in turn drastically reduces the production of sex steroids from the gonads [71].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for GnRHa Research
| Research Reagent / Material | Function in Experimentation |
|---|---|
| Long-Acting GnRHa Formulations (Triptorelin, Leuprolide, Goserelin depot injections) | The primary investigational products used to induce and maintain suppression of the HPG axis in in vivo models or clinical research [70]. |
| GnRH Receptor Expressing Cell Lines (e.g., HEK293-GnRHR) | In vitro models for studying receptor binding affinity, functional activity, and downstream signaling pathways of different GnRHa analogs. |
| Hormone Assay Kits (for LH, FSH, Testosterone, Estradiol) | Essential for quantifying the biochemical efficacy of GnRHa therapy by measuring baseline and post-treatment hormone levels in serum or plasma [55]. |
| Add-Back Therapy (e.g., Estradiol, Norethindrone Acetate) | Used in research models to investigate strategies for mitigating hypoestrogenic side effects (e.g., bone density loss) while maintaining the primary therapeutic benefit of GnRHa [71]. |
| Kisspeptin Peptides | Research tool for investigating the upstream regulation of GnRH neurons and the central mechanisms controlling the HPG axis, which can provide context for breakthrough events [72]. |
FAQs: Managing Breakthrough Puberty in Hormone Suppression Research
What is the evidence for the long-term sustainability of puberty suppression? Long-term follow-up data primarily come from studies on Gonadotropin-Releasing Hormone Agonists (GnRHa) used for Central Precocious Puberty (CPP). Evidence indicates that treatment is effective at suspending pubertal development during the administration period. Key findings on sustainability include:
- Reproductive Function Recovery: Puberty typically recommences, and menarche occurs, within approximately 1 year (ranging from 0.9 to 1.5 years) after treatment discontinuation [73]. A 2024 animal study bolstered these findings, showing that while GnRHa treatment in pre-pubescent female rats delayed the development of reproductive organs, normal development was restored four weeks after treatment stopped, and reproductive function was largely recovered [44].
- Bone Mineral Density (BMD): A known effect of GnRHa treatment is a decrease in BMD during the treatment period. However, long-term follow-up studies into adulthood show that BMD recovers to normal levels after treatment is ceased, and the formation of peak bone mass is not adversely affected [73].
What are the primary risks or challenges to sustained suppression? The main challenges are not related to the failure of the drug mechanism but to managing the side effects that can arise during the period of sustained suppression.
- Bone Health: The suppression of sex hormones during a critical period for bone accretion leads to a measurable decrease in Bone Mineral Density. This requires monitoring and management, though the effect appears reversible [10] [73].
- Potential Impact on Brain Development: The effect of puberty blockers on cognitive development remains an area of ongoing investigation. While their use for early-onset puberty has not shown negative impacts on cognitive function, studies specific to transgender adolescents are ongoing [10].
- Breakthrough Puberty: True "breakthrough" (i.e., the drug failing to suppress puberty) is not commonly reported in the literature for GnRHa. The greater clinical challenge is determining the optimal duration of suppression, as treatment beyond a certain bone age (e.g., >12-12.5 years) may not provide additional benefit for final adult height and could unnecessarily prolong exposure to low-sex-hormone states [73].
How is treatment efficacy and sustainability monitored in long-term studies? Long-term studies use a combination of physiological and biochemical markers to track the sustainability of suppression and its after-effects. The table below summarizes the key outcomes measured in long-term follow-up studies.
Table 1: Key Long-Term Follow-Up Metrics for Puberty Suppression Sustainability
| Outcome Category | Specific Metrics | Typical Findings from Long-Term Follow-Up |
|---|---|---|
| Reproductive Function | Time to menarche after treatment cessation, regular menstrual cycles, pregnancy rates | Menarche at ~12.6-13.6 years chronologic age; normal reproductive function in adulthood [73] |
| Growth & Skeletal Maturation | Final Adult Height (FH), Bone Age (BA) progression, Predicted Adult Height (PAH) | FH gain of ~4-7 cm compared to pre-treatment predictions; benefit is greatest with earlier treatment initiation [73] |
| Bone Health | Bone Mineral Density (BMD) Z-scores | Transient decrease during treatment; recovery to normal range after treatment cessation [73] |
| Body Composition | Body Mass Index (BMI) | CPP patients often have higher BMI at diagnosis; GnRHa treatment does not appear to aggravate obesity [73] |
Experimental Protocols for Key Long-Term Studies
Protocol 1: Assessing Reversibility of Puberty Suppression (Animal Model)
This protocol is based on a 2024 study designed to evaluate the recovery of reproductive organs and function after the withdrawal of GnRHa treatment [44].
- Objective: To determine if the effects of short-term puberty-blocking treatment are reversible upon treatment withdrawal.
- Subjects: Pre-pubescent female rats.
- Intervention: Administration of GnRHa or saline (control) for four weeks.
- Withdrawal & Recovery: Treatment is stopped. Subjects are monitored during a post-withdrawal period.
- Assessment Timepoints: Measurements are taken at baseline, end of treatment, and at various timepoints post-withdrawal (e.g., 4 weeks).
- Key Outcome Measures:
- Organ Morphology: Histological analysis of uterine lining thickness and ovarian follicle development.
- Functional Recovery: Pregnancy rates, time to pregnancy, and litter size in subjects paired with males.
- Conclusion of Source Study: The developmental delay of the uterus and ovaries was reversible, with a majority of reproductive function recovering after treatment withdrawal [44].
Protocol 2: Long-Term Follow-Up of CPP Patients into Adulthood
This protocol summarizes the methodology used in multiple long-term observational studies that track individuals with CPP treated with GnRHa into adulthood [73].
- Objective: To evaluate the long-term safety and efficacy of GnRHa treatment, focusing on adult health outcomes.
- Cohort: Female patients diagnosed with and treated for CPP in childhood.
- Design: Retrospective and/or prospective longitudinal follow-up study.
- Follow-Up Duration: Ranges from several years post-treatment to full adulthood (e.g., 16-32 years old).
- Key Outcome Measures:
- Final Height: Compared to pre-treatment Predicted Adult Height and genetic Target Height.
- Reproductive History: Age at menarche, regularity of cycles, fertility outcomes.
- Bone Health: Dual-energy X-ray absorptiometry (DXA) scans to measure BMD.
- Metabolic and Psychological Health: Assessment of BMI, incidence of PCOS, and psychosocial wellbeing.
Signaling Pathway and Experimental Workflow
Diagram: Mechanism of Action and Research Assessment of GnRHa
Diagram: Long-Term Follow-Up Workflow for Sustainability Research
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Puberty Suppression Sustainability Research
| Research Reagent / Material | Function in Experimental Context |
|---|---|
| Gonadotropin-Releasing Hormone Agonists (GnRHa) | The primary interventional agent used to suppress the hypothalamic-pituitary-gonadal (HPG) axis and induce a reversible state of paused puberty. Examples include leuprolide, triptorelin, or histrelin [44] [73]. |
| ELISA/Kits for LH, FSH, Estradiol, Testosterone | Essential for biochemical verification of HPG axis suppression (low levels during treatment) and recovery (return to normal levels post-withdrawal) [73]. |
| Dual-Energy X-ray Absorptiometry (DXA) | The gold-standard technology for longitudinal, non-invasive monitoring of Bone Mineral Density (BMD) to assess bone health during and after suppression therapy [73]. |
| Histology Reagents | Used for morphological analysis of reproductive tissues (e.g., uterus, ovaries, testes) in pre-clinical models to assess the impact of suppression and subsequent recovery on organ structure [44]. |
| Validated Psychometric Scales | Tools to assess psychosocial functioning, quality of life, and gender dysphoria, which are critical for evaluating the holistic impact of treatment sustainability [10] [74]. |
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary bone health concern in research on puberty suppression? The primary concern is the negative impact of long-term puberty suppression on bone mineral density (BMD), particularly at the lumbar spine. Puberty is a critical period for bone mass accrual, driven by increasing concentrations of sex steroids. Suppressing these hormones defers this natural process, which can lead to lower BMD and potentially increase future fracture risk. The effects are more pronounced in trans girls (AMAB) than in trans boys (AFAB) [75] [76].
FAQ 2: Are the effects of puberty suppression on bone mineral density reversible? Research indicates that the decline in BMD during the puberty suppression phase is only partially restored after the initiation of gender-affirming hormones (testosterone or estradiol). While BMD improves with subsequent hormone therapy, it may not fully catch up to the trajectory expected without a prolonged period of suppression [75] [76].
FAQ 3: What are the key monitoring protocols for bone health in study participants undergoing hormone suppression? Clinical guidelines suggest the following monitoring regimen [77] [75]:
- Clinical Pubertal Development: Assess every 3 to 6 months.
- Laboratory Parameters: Monitor every 6 to 12 months.
- Bone Mineral Density: Obtain baseline DXA scans and follow-up measurements as indicated. More frequent monitoring is advised for individuals with additional risk factors for bone loss.
FAQ 4: Which behavioral interventions are recommended to support bone health in study cohorts? Behavioral health measures are strongly recommended to promote bone mineralization. These include [78] [75]:
- Ensuring adequate intake of calcium and vitamin D.
- Encouraging regular weight-bearing exercise.
- Maintaining a healthy lifestyle, avoiding smoking, and limiting alcohol.
FAQ 5: At what age is it considered appropriate to initiate gender-affirming hormones following suppression? According to Endocrine Society guidelines, sex hormone treatment can be initiated after a multidisciplinary team confirms the persistence of gender dysphoria and the individual has sufficient mental capacity to give informed consent, which most adolescents have by age 16 years. There may be compelling reasons to start treatment earlier in some adolescents, but this should be managed by an expert multidisciplinary team [77].
Troubleshooting Guides
Guide 1: Addressing Low Bone Mineral Density in Research Participants
Problem: A study participant undergoing long-term puberty suppression shows a declining Z-score in bone mineral density.
Recommended Actions:
- Review Treatment Duration: Evaluate the length of time on puberty-delaying medication. A longer duration is directly associated with lower BMD Z-scores. Discuss with the research and clinical team the optimal timing for introducing gender-affirming hormones [76].
- Optimize Non-Pharmacological Interventions: Reinforce and verify adherence to bone-healthy behaviors. Ensure the participant is meeting recommended daily intake of calcium (1,200 mg for postmenopausal women) and vitamin D (200-600 IU daily), and is engaging in regular weight-bearing physical activity [78] [75].
- Consider Hormonal Intervention: Per protocol, plan for the timely initiation of gender-affirming hormones (testosterone or estradiol). Evidence shows that BMD values improve after starting these hormones [76].
- Rule Out Secondary Causes: Conduct an evaluation for potential secondary causes of bone loss, such as other medical conditions or medications that can harm bone [78].
- Enhance Monitoring: Increase the frequency of BMD monitoring via DXA scans to track the response to interventions more closely [77].
Guide 2: Managing Variability in Response to Gender-Affirming Hormones
Problem: Significant variability is observed in BMD recovery among participants after initiating gender-affirming hormone therapy.
Recommended Actions:
- Verify Hormone Levels: Measure serum sex steroid levels to ensure that endogenous hormones are adequately suppressed and that administered hormones are maintained within the normal physiologic range for the affirmed gender. Dosing may need adjustment [77].
- Stratify by Birth-Assigned Sex: Analyze data separately for AMAB and AFAB participants. Trans girls (AMAB) are more vulnerable to compromised bone health and may show different recovery trajectories, particularly at the lumbar spine [75] [79].
- Control for Lifestyle Factors: Statistically account for variables such as physical activity levels, dietary calcium/vitamin D, and BMI in your analysis, as these significantly influence bone mineralization [78] [75].
- Standardize Protocols: Ensure consistent hormonal formulations, doses, and administration routes across the study cohort to reduce protocol-induced variability [79].
The following tables summarize quantitative findings from recent research on bone health in the context of gender-affirming hormone therapies.
Table 1: Impact of Puberty Suppression and Gender-Affirming Hormones on Bone Mineral Density
| Study Focus | Key Finding | Quantitative Summary | Reference |
|---|---|---|---|
| Puberty Suppression (GnRHa) | Longer treatment duration associated with lower BMD. | A longer duration of GnRHa therapy was correlated with a lower bone mineral density Z-score [76]. | |
| Puberty Suppression (GnRHa) | Negative impact on lumbar spine BMD. | Long-term puberty suppression has a negative impact on BMD, especially at the lumbar spine [75]. | |
| Cross-Sex Hormone Therapy (CSHT) in Adults | Neutral effect on BMD in trans men (AFAB). | In transgender men, mean BMD difference compared to natal women was not significant at any site (femoral neck, total femur, lumbar spine) [79]. | |
| Cross-Sex Hormone Therapy (CSHT) in Adults | Effect on lumbar spine BMD in trans women (AMAB). | In transgender women, before-after studies reported a slight but significant increase in lumbar spine BMD after 12 and ≥24 months of estrogen treatment [79]. |
Table 2: Essential Monitoring Parameters for Bone Health
| Parameter | Recommended Monitoring Frequency | Notes / Rationale |
|---|---|---|
| Clinical Pubertal Development | Every 3 to 6 months | Track physical changes of puberty during suppression and after hormone initiation [77]. |
| Laboratory Parameters | Every 6 to 12 months | Includes sex steroid levels, prolactin (for trans females on estrogen), and metabolic panels [77] [75]. |
| Bone Mineral Density (DXA) | As indicated by risk; baseline and periodic follow-up | Critical for those with prolonged suppression, after gonadectomy, or with other risk factors for osteoporosis [77] [80]. |
| Calcium & Vitamin D Intake | Ongoing assessment | Ensure daily intake of 1,200 mg calcium and 200-600 IU vitamin D; supplementation often required [78]. |
Experimental Protocols
Detailed Methodology for Longitudinal Bone Health Assessment
Objective: To systematically evaluate the impact of puberty-suppressing medication and subsequent gender-affirming hormone therapy on bone mineral density and architecture in transgender youth.
Population: Adolescents with persistent gender dysphoria, initiating treatment at the early stages of puberty (Tanner stage 2-3) [77] [75].
Interventions:
- Puberty Suppression: Administration of GnRH analogues (e.g., leuprolide, triptorelin) to suppress endogenous gonadal hormone production. Initiation occurs after the first physical changes of puberty are observed [77] [75].
- Gender-Affirming Hormones: After a multidisciplinary assessment and confirmation of persistent gender dysphoria, introduction of testosterone (for trans boys) or estradiol (for trans girls) using a gradually increasing dose schedule. This typically occurs around age 16 but can be earlier based on individual circumstances [77].
Primary Outcome Measure:
- Change in areal bone mineral density (aBMD) Z-score at the lumbar spine and femoral neck, as measured by dual-energy X-ray absorptiometry (DXA) [75] [79] [76].
Secondary Outcome Measures:
- Serum levels of testosterone or estradiol, LH, FSH.
- Markers of bone turnover (e.g., P1NP, CTX).
- Serum 25-hydroxyvitamin D, calcium, and PTH levels.
- Volumetric BMD (vBMD) and bone geometry, if assessed by quantitative computed tomography (QCT) [75].
Assessment Schedule:
- Baseline: Prior to initiation of any treatment.
- During Puberty Suppression: Every 12 months.
- After Initiating Gender-Affirming Hormones: At 6, 12, and 24 months.
Statistical Analysis: Use linear mixed-effects models to analyze longitudinal changes in BMD Z-scores, adjusting for covariates such as age, BMI, physical activity, and calcium/vitamin D intake.
Signaling Pathways and Workflows
Bone Health Intervention Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Bone Health Research in Hormone Therapy Studies
| Item | Function / Application in Research |
|---|---|
| Dual-Energy X-ray Absorptiometry (DXA) | The gold-standard clinical tool for non-invasive measurement of areal bone mineral density (aBMD) at key sites like the lumbar spine and femoral neck [79]. |
| GnRH Agonists (e.g., Leuprolide) | Research-grade compounds used to induce medical puberty suppression by downregulating the hypothalamic-pituitary-gonadal axis, creating a hypogonadal state for study [77] [75]. |
| Immunoassay Kits | For precise quantification of serum hormone levels (estradiol, testosterone, LH, FSH) and bone turnover markers (P1NP, CTX) to correlate with BMD changes [77] [75]. |
| High-Resolution pQCT | Provides 3D imaging to assess volumetric BMD (vBMD) and bone geometry, offering insights beyond the 2D projection of DXA [81]. |
| Validated Questionnaires | Tools to reliably collect data on covariates such as dietary calcium intake, physical activity levels, and sun exposure (for vitamin D synthesis) [78] [75]. |
Bone Health Study Workflow
Patient-Reported Outcomes and Quality of Life Measures
Frequently Asked Questions (FAQs)
1. What are Patient-Reported Outcomes (PROs) and why are they important in clinical research? Patient-Reported Outcomes (PROs) are reports that come directly from the patient about their health status without interpretation by a clinician or anyone else. They cover aspects like pain levels, fatigue, emotional well-being, and ability to perform daily activities [82]. In the context of research on breakthrough puberty, they are crucial because they provide a window into the patient's day-to-day health and quality of life that clinical tests alone cannot capture. They center the patient voice, helping researchers understand the true impact of hormone suppression therapy and any subsequent breakthrough puberty on an adolescent's life [82].
2. How do I select the right PRO instrument for a study on puberty suppression? The choice of a PRO should be justified based on its measurement properties, including validity (does it measure what it intends to), reliability (does it produce consistent results), and responsiveness (is it sensitive to change over time). Evidence supporting the instrument’s properties should be provided, ideally from the target population of transgender adolescents [83]. For studies on breakthrough puberty, you should select tools that are appropriate for an adolescent population and that measure domains relevant to the experience, such as physical function, emotional distress, or body image.
3. What is the recommended method for collecting PRO data to ensure high-quality results? The method of data collection (e.g., paper, electronic, telephone) should be explicitly stated [83]. A transition to digital Patient-Reported Outcome Measures is recommended. Using secure web portals or mobile apps allows data to flow directly into electronic health records (EHRs), improving efficiency and data integrity. Computer adaptive testing (CAT) can further enhance data collection by tailoring questions to the individual, reducing the number of questions while improving precision [82].
4. How should missing PRO data be handled in the statistical analysis? Missing data in PROMs is common and can introduce bias. The statistical approach for dealing with missing data should be explicitly stated in the study protocol. Common methods include imputation techniques or sensitivity analyses to understand the potential impact of the missing data [83].
5. How can I determine if a change in a PRO score is clinically meaningful? Statistical significance does not automatically mean a result is meaningful to a patient. Authors should use established interpretive thresholds, such as the Minimum Clinically Important Difference (MCID), to determine whether changes are clinically relevant. It is important to report both the average change in PROM scores and the proportion of patients who meet or exceed the MCID. The source of the MCID threshold used should be cited [83].
Troubleshooting Guide
| Problem | Possible Cause | Solution |
|---|---|---|
| Low Patient Response/Completion Rates | High respondent burden; complex or lengthy questionnaires; integration not into clinical workflow. | Use standardized, efficient tools like PROMIS with Computer Adaptive Testing (CAT) to reduce questions [82]. Integrate PRO collection seamlessly into clinical workflows via EHRs [82]. |
| Missing PRO Data | Patient dropout; accidental skipping of questions; administrative errors. | State the statistical approach for handling missing data (e.g., imputation methods) explicitly in the analysis plan. Perform sensitivity analyses to assess the potential impact of missing data [83]. |
| Inconsistent PRO Administration | Lack of standardization; different staff using different procedures. | Provide a brief description of the PROM(s) used, including information on structure and scoring. Explicitly state and standardize the method of data collection (paper, electronic, etc.) across all study sites [83]. |
| Unclear Clinical Significance of Results | Relying solely on statistical p-values; lack of predefined criteria for meaningful change. | Interpret results using established thresholds like the MCID or Patient Acceptable Symptom State (PASS). Report the proportion of patients achieving these benchmarks, not just group mean scores [83]. |
| Poor Integration of PRO Data with Clinical Outcomes | PRO data is siloed and not readily available for clinical decision-making. | Use digital platforms that integrate directly with Electronic Health Records (EHRs). This places PRO results directly within the clinician’s workflow, making them actionable for treatment decisions [82]. |
Standardized PRO Domains and Their Application
The following table illustrates how standardized PRO domains can be applied across different clinical scenarios, ensuring consistent and comparable data collection [82].
| Standardized Domain | Application in Chronic Conditions | Example in Breakthrough Puberty Research |
|---|---|---|
| Physical Function | Measures ability to perform daily tasks for patients with multiple sclerosis, arthritis, or post-surgery recovery. | Assess impact of breakthrough puberty changes (e.g., growth spurts) on ability to participate in sports or physical activities. |
| Pain Interference | Assesses how pain affects daily life for individuals with chronic back pain, cancer, or fibromyalgia. | Evaluate how pain associated with rapid bone growth or other physical changes interferes with schoolwork or social life. |
| Emotional Distress/Depression | Screens for and monitors depressive symptoms in patients with diabetes, heart disease, or during cancer care. | Monitor for anxiety or depression related to body image changes or distress from experiencing unwanted pubertal development. |
Key Methodological Reporting Criteria for PROs
For transparent and rigorous reporting of PROs in clinical studies, the following criteria should be addressed, as aligned with guidelines like the CONSORT PRO extension [83].
| Reporting Item | Description & Application |
|---|---|
| Identification & Rationale | Explicitly identify the PROM as a primary or secondary outcome. Justify its use and state a hypothesis involving the PROM, including the relevant domain and a clinically important difference (e.g., a specific change on a pain scale) [83]. |
| PROM Description | Provide a brief description of the PROM's structure (number of items, subscales) and scoring (score range, interpretation). Describe and justify any modifications to the original instrument [83]. |
| Sample Size Consideration | When a PROM is the primary outcome, provide a sample size calculation based on the established MCID for that PROM to ensure adequate statistical power [83]. |
| Handling Multiple Outcomes | Pre-specify a single primary outcome to limit Type I error. For multiple secondary outcomes, apply appropriate statistical corrections (e.g., Bonferroni) and label them as exploratory [83]. |
Experimental Protocols
Protocol 1: Integrating PROs into Clinical Workflow for Longitudinal Monitoring
Objective: To seamlessly collect and utilize PRO data at every clinical visit for adolescents on hormone suppression therapy to monitor for changes in quality of life and potential signs of breakthrough puberty distress.
Methodology:
- Tool Selection: Adopt widely-validated, standardized tools like the Patient-Reported Outcomes Measurement Information System (PROMIS). PROMIS provides precise tools for measuring physical, mental, and social well-being and is built on item response theory, allowing for efficient computer adaptive testing (CAT) [82].
- Digital Infrastructure: Implement a digital PRO platform (e.g., OutcomeMD) that integrates with the institution's Electronic Health Record (EHR). The platform should allow for automated data collection via patient portals or mobile apps [82].
- Administration Protocol: Prior to each clinic visit, patients are automatically sent standardized PROMIS assessments for key domains (e.g., physical function, pain interference, emotional distress). CAT is used to minimize the number of questions [82].
- Data Presentation: PRO results are automatically filed in the patient's EHR and presented in a visual, trended format (e.g., graphs over time) within the clinician's workflow for easy review during the consultation [82].
- Actionable Thresholds: Pre-defined clinical decision support rules can flag scores that fall outside normal ranges or show significant decline, prompting clinician action [83].
Protocol 2: Assessing the Impact of Breakthrough Puberty on Health-Related Quality of Life
Objective: To quantitatively evaluate the effect of breakthrough puberty on specific quality-of-life domains in a research cohort.
Methodology:
- Study Design: Prospective observational cohort or clinical trial.
- Primary Outcome Measure: A validated, disease-specific or generic PROM identified as the primary outcome. Example: The PROMIS Pediatric Profile-25, which covers domains like pain, fatigue, and peer relationships.
- Hypothesis & Sample Size: Pre-define a hypothesis stating the expected change in the PROM score (e.g., "Adolescents experiencing breakthrough puberty will report a ≥ X-point decrease in physical function compared to those with stable suppression"). Perform a sample size calculation based on the MCID for the chosen PROM [83].
- Data Collection Points: Collect PRO data at baseline (start of therapy) and at regular, pre-specified intervals (e.g., every 6 months). Concurrently, collect clinical data on pubertal staging (Tanner scale) and hormone levels.
- Statistical Analysis:
- Summarize baseline PRO data for each group.
- Report the number of participants contributing data at each time point.
- For the primary outcome, report the estimated effect size (e.g., mean difference between groups) and its precision (95% Confidence Interval) at each time point.
- Use established MCID thresholds to determine the clinical relevance of the findings, reporting the proportion of patients in each group who experienced a clinically important change [83].
Signaling Pathways and Workflows
PRO Implementation and Analysis Workflow
PROs in Breakthrough Puberty Monitoring
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application in PRO Research |
|---|---|
| PROMIS (Patient-Reported Outcomes Measurement Information System) | A publicly available system of highly reliable, precise tools for measuring physical, mental, and social well-being. Its item banks and CAT methodology allow for efficient, standardized assessment across diverse populations and conditions [82]. |
| Computer Adaptive Testing (CAT) Platform | A digital testing system that uses algorithms to select questions based on a patient's previous answers. It reduces respondent burden and improves measurement precision compared to fixed-length surveys [82]. |
| Electronic Health Record (EHR)-Integrated PRO Platform | A digital solution (e.g., OutcomeMD) that automatically collects PRO data via patient portals and files results directly into the EHR. This makes PRO data a visible part of the clinical record and workflow [82]. |
| Minimum Clinically Important Difference (MCID) | A pre-established threshold that defines the smallest change in a PRO score that patients perceive as beneficial or important. It is essential for interpreting the clinical relevance of study results, beyond statistical significance [83]. |
| CONSORT-PRO Extension Guidelines | A reporting guideline that promotes transparent and comprehensive reporting of PRO results in clinical trials. Following these guidelines is critical for the methodological rigor and interpretability of studies using PROMs [83]. |
Conclusion
Breakthrough puberty during hormone suppression therapy represents a significant clinical challenge with incidence rates varying widely based on population characteristics and monitoring thresholds. Effective management requires comprehensive understanding of risk factors, particularly young age and high BMI, coupled with rigorous monitoring protocols that include regular estradiol assessment. Current evidence supports treatment optimization through dosage adjustment, formulation switching, and combination therapies when incomplete suppression occurs. Critical research gaps remain in standardizing diagnostic criteria, developing predictive biomarkers, and creating personalized dosing regimens. Future directions should focus on next-generation suppression agents with improved efficacy profiles, standardized monitoring protocols across therapeutic areas, and long-term studies evaluating the impact of breakthrough events on ultimate treatment goals. For researchers and drug development professionals, these findings highlight the urgent need for more predictable suppression therapies and evidence-based management algorithms to address this clinically significant phenomenon.
References
- 1. Elevated Pre-injection Basal Luteinizing Hormone Concentrations are... [https://www.jcrpe.org/articles/elevated-pre-injection-basal-luteinizing-hormone-concentrations-are-common-in-girls-treated-for-central-precocious-puberty/jcrpe.galenos.2020.2020.0210]
- 2. Puberty suppression in adolescents with gender dysphoria [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1309904/full]
- 3. Use of Hormone Blockers in Transgender Teenagers [https://pmc.ncbi.nlm.nih.gov/articles/PMC11676889/]
- 4. Interventions to suppress in adolescents experiencing gender... puberty [https://pubmed.ncbi.nlm.nih.gov/38594047/]
- 5. Precocious puberty - Diagnosis and treatment [https://www.mayoclinic.org/diseases-conditions/precocious-puberty/diagnosis-treatment/drc-20351817]
- 6. Precocious Early Puberty [https://www.childrenshospital.org/conditions/precocious-early-puberty]
- 7. Puberty: An ultimate guide for parents [https://health.choc.org/puberty-an-ultimate-guide-for-parents/]
- 8. Precocious Puberty [https://www.endocrine.org/patient-engagement/endocrine-library/precocious-puberty]
- 9. Delayed Puberty - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK544322/]
- 10. What are puberty blockers? What are the benefits and risks ... [https://www.mcri.edu.au/news/insights-and-opinions/what-are-puberty-blockers]
- 11. Pubertal Suppression for Transgender Youth and Risk of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7073269/]
- 12. Precocious Puberty Treatment & Management [https://emedicine.medscape.com/article/924002-treatment]
- 13. Clinical pharmacology in adolescent transgender medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC12185136/]
- 14. Long-term effects and significant adverse drug reactions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7233750/]
- 15. Physiology, Gonadotropin-Releasing Hormone - StatPearls [https://www.ncbi.nlm.nih.gov/books/NBK558992/]
- 16. Molecular Mechanisms of Gonadotropin-Releasing ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2013.00180/full]
- 17. of Mechanism of gonadotropin-releasing hormone upon... action [https://pubmed.ncbi.nlm.nih.gov/7542447/]
- 18. Significant adverse reactions to long-acting gonadotropin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4208261/]
- 19. Efficacy of combined gonadotropin-releasing hormone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537404/]
- 20. Incomplete ovarian function suppression in ... [https://www.sciencedirect.com/science/article/abs/pii/S0305737225000015]
- 21. The Effect of Leuprolide Acetate 11.25 mg 3-Month ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579711/]
- 22. Pharmacotherapy for children with central precocious puberty ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12323909/]
- 23. Long-term health consequences of central precocious/early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10734238/]
- 24. Effect of puberty suppression and gender affirming ... [https://pubmed.ncbi.nlm.nih.gov/40820509/]
- 25. Adult Consequences of Self-Limited Delayed Puberty [https://pmc.ncbi.nlm.nih.gov/articles/PMC8579478/]
- 26. The range and variation in serum estradiol concentration in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12147738/]
- 27. Oestrogens and blood testing [https://www.mymenopausecentre.com/gp-resources/oestrogens-and-blood-testing/]
- 28. Unlocking the Mystery of Estradiol Levels: A Guide to Their ... [https://theluckyegg.com/2023/04/20/unlocking-the-mystery-of-estradiol-levels-a-guide-to-their-role-in-ttc-and-ivf-success/]
- 29. Common Pitfalls in the Interpretation of Endocrine Tests - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8453144/]
- 30. Interferences in immunoassays: review and practical algor... [https://www.degruyterbrill.com/document/doi/10.1515/cclm-2021-1288/html?lang=en&srsltid=AfmBOopwgRQACaGSNR6DnASkSOvPFMY0LnGtLaJxV87BmPg_bD99ojyn]
- 31. The Fundamental Flaws of Immunoassays and Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2720067/]
- 32. Mass Spectrometry in the Clinical Laboratory—Challenges ... [https://www.spectroscopyonline.com/view/mass-spectrometry-clinical-laboratory-challenges-quality-assurance]
- 33. Comparing immunoassay and mass spectrometry ... [https://www.sciencedirect.com/science/article/pii/S0306453025001027]
- 34. LC-MS/MS in clinical chemistry: Did it live up to its promise? [https://www.sciencedirect.com/science/article/abs/pii/S0009898123001936]
- 35. Monitoring treatment of central precocious puberty using basal... [https://pubmed.ncbi.nlm.nih.gov/27740929/]
- 36. How to identify red-flag symptoms and refer patients ... [https://pharmaceutical-journal.com/article/ld/how-to-identify-red-flag-symptoms-and-refer-patients-appropriately]
- 37. blockers for transgender and gender-diverse youth - Mayo Clinic Puberty [https://www.mayoclinic.org/diseases-conditions/gender-dysphoria/in-depth/pubertal-blockers/art-20459075]
- 38. Anti-Müllerian hormone as a biomarker of ovarian function ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1640583/full]
- 39. FDA Guidance for Industry on Bioanalytical Method ... [https://labs.iqvia.com/blog/fda-guidance-bioanalytical-method-validation-biomarkers]
- 40. Anti mullerian trends after aGnRH initiation in trans boys ... [https://www.endocrine-abstracts.org/ea/0110/ea0110ep1359]
- 41. Two UK clinical trials to assess impact of puberty blockers ... [https://www.theguardian.com/science/2025/nov/22/two-uk-clinical-trials-to-assess-impact-of-puberty-blockers-in-young-people]
- 42. NHS England commissions study on effects of puberty ... [https://pharmaceutical-journal.com/article/news/nhs-england-commissions-study-on-effects-of-puberty-blockers]
- 43. Consensus Parameter: Research Methodologies to Evaluate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7759272/]
- 44. Study Bolsters Evidence that Effects of Puberty Blockers ... [https://www.physiology.org/detail/news/2024/04/05/study-bolsters-evidence-that-effects-of-puberty-blockers-are-reversible]
- 45. Central Precocious Puberty: Update on Diagnosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5870137/]
- 46. Efficacy of combined gonadotropin-releasing hormone ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1662808/full]
- 47. Dose optimization of PEG-rhGH therapy to improve growth ... [https://www.sciencedirect.com/science/article/abs/pii/S1096637425000280]
- 48. An Overview of Clinical and Commercial Impact of Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4142089/]
- 49. insights for applications in HIV therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC4935562/]
- 50. Key Considerations For SC and IM Formulation Development [https://pci.com/resources/transforming-parenteral-delivery-key-considerations-for-sc-and-im-formulation-development/]
- 51. Lupron, used to halt puberty in children, may cause lasting ... [https://www.statnews.com/2017/02/02/lupron-puberty-children-health-problems/]
- 52. Puberty blockers: Can a drug trial solve the big debate? [https://www.bbc.com/news/articles/clyd2qe5kkjo]
- 53. Puberty blocker trial expected to begin in early 2025 [https://www.the-independent.com/news/uk/nhs-england-children-nhs-england-wales-b2592533.html]
- 54. Treatment of Peripheral Precocious Puberty - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5345994/]
- 55. Effectiveness of Puberty Suppression with Gonadotropin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7891223/]
- 56. Precocious Puberty - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK544313/]
- 57. Predictors of early androgen deprivation treatment failure in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4799954/]
- 58. The teen gene: Switching on puberty [https://www.newscientist.com/article/mg19125611-400-the-teen-gene-switching-on-puberty/]
- 59. Success Rate of Hormone Therapy for Breast Cancer [https://oncodaily.com/oncolibrary/hormone-therapy-for-breast-cancer]
- 60. Risk Stratification in Primary Care: Value-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8858376/]
- 61. Treatment of Central Precocious Puberty - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6486823/]
- 62. Pharmacogenetic-guided algorithms to estimate ... [https://www.sciencedirect.com/science/article/abs/pii/S2186495015000127]
- 63. Risk-Group-Specific Dose Finding Based on an Average ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4570736/]
- 64. A machine learning-based risk stratification tool for in-hospital ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-022-03340-8]
- 65. Machine learning for patient risk stratification [https://www.nature.com/articles/s41746-021-00426-3]
- 66. Leuprolide Acetate for Puberty Suppression in ... [https://www.sciencedirect.com/science/article/abs/pii/S1054139X22006863]
- 67. Young adult psychological outcome after puberty ... [https://pubmed.ncbi.nlm.nih.gov/25201798/]
- 68. Puberty suppression in adolescents with gender dysphoria [https://pmc.ncbi.nlm.nih.gov/articles/PMC11235884/]
- 69. Precocious Puberty Medication: Gonadotropin-Releasing ... [https://emedicine.medscape.com/article/924002-medication]
- 70. Adverse event profile differences among long-acting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12250665/]
- 71. Current approaches to overcome the side effects of GnRH ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8940613/]
- 72. Central Mechanism Controlling Pubertal Onset in Mammals [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2019.00312/full]
- 73. Long-term effects of gonadotropin-releasing hormone analogs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4342775/]
- 74. Psychological and Physical Health Outcomes Associated with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294553/]
- 75. Impact of gender-affirming treatment on bone health in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9578106/]
- 76. Longer treatment with puberty-delaying medication in ... [https://www.endocrine.org/news-and-advocacy/news-room/2022/longer-treatment-with-puberty-delaying-medication-leads-to-lower-bone-mineral-density]
- 77. Gender Dysphoria/Gender Incongruence Guideline ... [https://www.endocrine.org/clinical-practice-guidelines/gender-dysphoria-gender-incongruence]
- 78. Prevention and Treatment for Those Who Have Bone Diseases [https://www.ncbi.nlm.nih.gov/books/NBK45501/]
- 79. Bone Mass Effects of Cross-Sex Hormone Therapy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6469959/]
- 80. In breakthrough study, researchers map converging ... [https://www.sciencedaily.com/releases/2023/10/231031111440.htm]
- 81. Hormonal Control of Bone Architecture Throughout the ... [https://www.sciencedirect.com/science/article/pii/S1530891X24004968]
- 82. Scaling Patient-Reported Outcomes: Health Systems in 2025 [https://outcomemd.com/scaling-patient-reported-outcomes-health-systems-in-2025/]
- 83. A Short Primer on the Reporting of Patient-Reported Outcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12344331/]