Recent Insights into Hormonal Regulation of Development and Function: From Molecular Mechanisms to Therapeutic Innovation
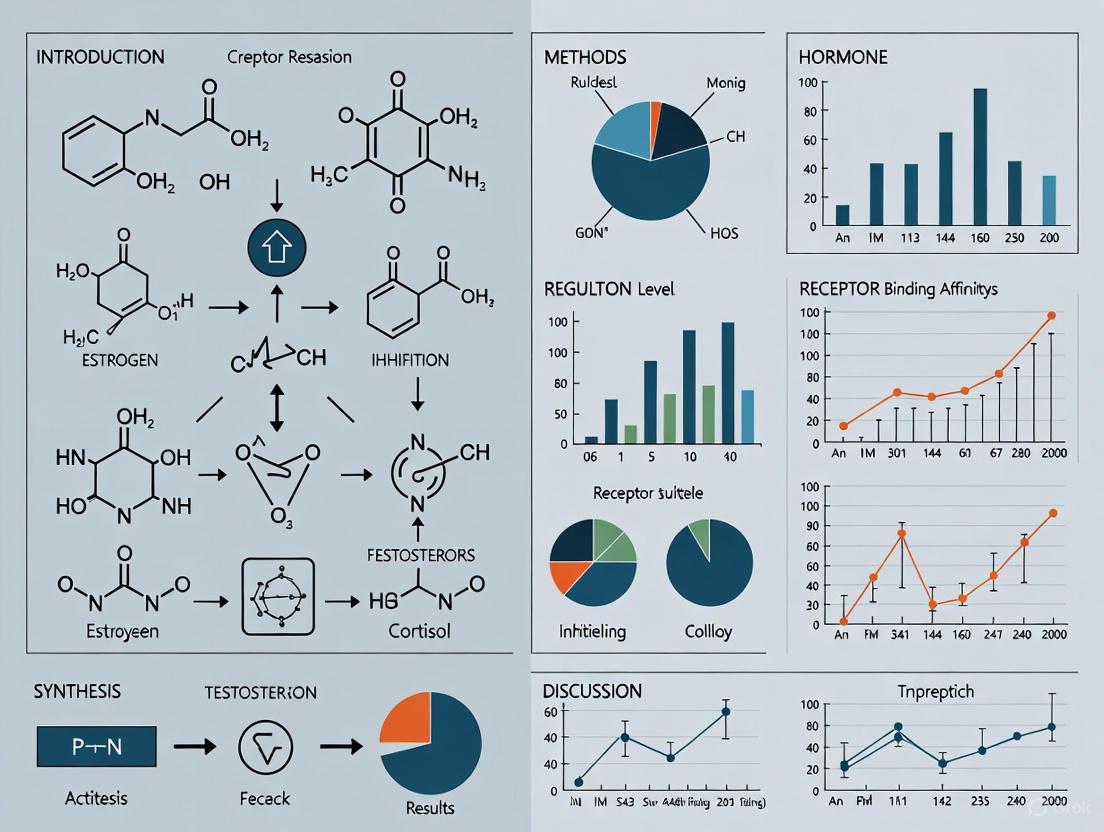
This article synthesizes recent advances in understanding the role of hormones during development and their functional regulation, tailored for researchers, scientists, and drug development professionals.
Recent Insights into Hormonal Regulation of Development and Function: From Molecular Mechanisms to Therapeutic Innovation
Abstract
This article synthesizes recent advances in understanding the role of hormones during development and their functional regulation, tailored for researchers, scientists, and drug development professionals. It explores foundational principles of hormone signaling and feedback mechanisms, examines cutting-edge methodological approaches like single-cell RNA sequencing and CRISPR/Cas9, and investigates troubleshooting for challenges such as sex-based differences in drug metabolism and hormonal disorder modeling. The content also covers the validation of novel hormonal pathways and comparative analyses of endocrine networks across species, highlighting the translation of basic research into targeted therapies for metabolic, inflammatory, and neuroendocrine disorders.
Core Principles and Emerging Discoveries in Hormonal Signaling
Hormones as Pivotal Signaling Molecules in Development and Homeostasis
Hormones, functioning as classic endocrine signals, travel through the bloodstream to coordinate development and maintain physiological stability from conception to adulthood. These signaling molecules are produced in one part of the body and regulate functions in distant target cells and tissues, acting as fundamental orchestrators of biological processes [1]. The hypothalamic-pituitary-gonadal (HPG) axis, along with other endocrine axes, creates an integrated communication network that guides the developmental trajectory while dynamically responding to internal and external environmental changes [2]. Recent research has significantly advanced our understanding of how hormonal signaling pathways maintain homeostasis through complex feedback mechanisms and crosstalk between different systems. This whitepaper examines the mechanistic roles of hormonal signaling in development and homeostasis, with emphasis on emerging research technologies and therapeutic applications relevant to drug development professionals and basic science researchers.
Hormonal Orchestration of Developmental Processes
Developmental Timeline and Key Hormonal Regulators
Hormonal signaling guides development through precise temporal and spatial regulation, with distinct endocrine actors assuming stage-specific dominance throughout the human lifespan. The following table summarizes the primary hormones and their functional roles during key developmental periods:
Table 1: Key Hormonal Regulators in Human Development
| Developmental Stage | Primary Hormonal Regulators | Core Functions | Clinical Significance |
|---|---|---|---|
| Fetal Development | hCS/hPL, hGH-V, IGFs (1, 2, 3), Placental Estrogen, Cortisol, AMH | Nutrient delivery, tissue proliferation, sexual differentiation, organ maturation | Fetal programming, birth weight determination, sexual differentiation disorders [2] |
| Childhood Growth | GH, IGF-1, Thyroid Hormone, Adrenal Androgens | Linear growth, metabolic regulation, neurodevelopment | GH deficiency/short stature, thyroid disorders, congenital adrenal hyperplasia [2] |
| Puberty | GnRH, FSH, LH, Sex Steroids (Estrogen, Testosterone) | Sexual maturation, growth spurt, brain remodeling | Precocious/delayed puberty, gender-affirming care, fertility preservation [2] |
| Adulthood | Sex Steroids, GH/IGF-1, Gastrointestinal Hormones | Metabolic maintenance, reproductive function, tissue repair | Age-related decline, infertility, metabolic syndrome, hormonal therapies [2] [3] |
Signaling Pathways in Developmental Hormone Action
The mechanistic actions of developmental hormones involve sophisticated intracellular pathways that translate endocrine signals into phenotypic outcomes:
Growth Hormone (GH) and Insulin-like Growth Factors (IGFs): The GH-IGF axis represents a pivotal signaling pathway for somatic growth and organ development. GH directly activates the JAK-STAT signaling cascade while simultaneously stimulating IGF production, which subsequently promotes cell proliferation, survival, and differentiation through PI3K-Akt and MAPK pathways [2]. Recent research has elucidated GH's role in ovarian function, where it improves follicular development and hormone secretion through multiple pathways, with novel biomaterial-based delivery systems enhancing its bioavailability for assisted reproductive technologies [4].
Thyroid Hormone (TH): Critical for neurologic development and metabolic regulation, TH acts through nuclear receptors (TRα and TRβ) that function as ligand-dependent transcription factors. The TR-RXR heterodimer binds to thyroid hormone response elements (TREs) in target genes, regulating neuronal migration, myelination, and metabolic rate [2]. Stress-induced inflammation can alter the hypothalamic-pituitary-thyroid (HPT) axis, potentially contributing to thyroid dysfunction and related developmental pathologies [2].
Anti-Müllerian Hormone (AMH): This transforming growth factor-beta (TGF-β) family member causes regression of Müllerian ducts in male fetal development through type II serine/threonine kinase receptors. AMH has gained clinical importance as a biomarker for polycystic ovarian syndrome (PCOS), with significantly elevated levels in affected women [2]. Current investigations explore its role as a tumor marker and potential therapeutic target for gynecological malignancies expressing AMH-specific receptors [2].
Hormonal Regulation of Homeostatic Processes
The Gut-Brain Axis: Metabolic Homeostasis
The gut-brain axis has emerged as a crucial signaling system in metabolic homeostasis, with gastrointestinal hormones communicating nutrient status to central regulatory centers:
Glucagon-like Peptide-1 (GLP-1): This 36-37 amino acid peptide, produced by intestinal L cells, stimulates insulin secretion, enhances insulin sensitivity, delays gastric emptying, and suppresses appetite via central mechanisms [3]. GLP-1 activates the cAMP-PKA pathway in glucose-sensitive neurons in the dorsomedial nucleus (DMN), inhibiting delayed rectifier potassium channels and lowering blood glucose levels [3]. Additionally, in the paraventricular nucleus (PVN), GLP-1 influences feeding behavior through PKA-mediated phosphorylation of serine 845 on the GluA1 subunit of AMPA receptors, enhancing postsynaptic excitability [3].
Peptide YY (PYY) and Ghrelin: These hormones function as antagonistic regulators of energy balance. PYY exerts anorexigenic effects while ghrelin stimulates appetite through GHS-R1a receptors, creating a dynamic equilibrium that maintains energy homeostasis [3]. Bariatric surgery significantly alters the expression patterns of these hormones, contributing to its metabolic benefits through mechanisms involving FXR/TGR5 signaling pathways [3].
Table 2: Key Gastrointestinal Hormones in Metabolic Homeostasis
| Hormone | Site of Production | Primary Receptors | Physiological Functions | Signaling Pathways |
|---|---|---|---|---|
| GLP-1 | Intestinal L cells | GLP-1R | Insulin secretion, appetite suppression, gastric emptying delay | cAMP-PKA, PLC-PKC [3] |
| GLP-2 | Intestinal L cells, Brain neurons | GLP-2R | Intestinal mucosal growth, glucose homeostasis | PI3K-Akt-FoxO1 [3] |
| PYY | Intestinal L cells | Y2 receptor | Appetite suppression, ileal brake mechanism | Inhibition of NPY/AgRP neurons [3] |
| Ghrelin | Gastric fundus cells | GHS-R1a | Appetite stimulation, GH release | Calcium mobilization, CREB activation [3] |
Sex Hormones: Neural Circuit Homeostasis
Sex hormones, including estrogens, progesterone, and androgens, exert powerful organizational and activational effects on neural circuits that govern behavior, cognition, and emotional states [5]. Recent systems-level approaches have revealed that these hormones promote behavioral persistence and reduce behavioral variability through several mechanisms:
Estrogen-mediated synaptic plasticity: Estrogen facilitates synaptic potentiation across various brain regions, strengthening recurrent connectivity in neural circuits that support persistent behavioral states [5]. This underlies the observation that higher estrogen states are associated with reduced behavioral variability and increased persistence in both reproductive and non-reproductive contexts.
Computational frameworks: Hormones appear to implement stability in neural population codes, reducing "representational drift" in hormone-sensitive brain regions. This creates attractor-like states in neural dynamics that maintain consistent behavioral outputs despite variable inputs [5].
Circuit-level communication: Hormones alter fundamental properties of neural communication, including shifts in functional connectivity between distributed brain networks. These changes modulate how information flows through social behavior circuits, influencing perception, decision-making, and action selection [5].
The mechanistic understanding of hormonal regulation of brain function has significant implications for developing novel therapeutics for neuropsychiatric conditions, optimizing hormonal formulations for gender-affirming care, and understanding the neural basis of mood disorders that exhibit gender disparities [5].
Experimental Approaches and Research Methodologies
Signaling Pathway Analysis: FERONIA as a Model System
The plant receptor kinase FERONIA (FER) provides an excellent model for studying complex hormone crosstalk mechanisms with relevance to mammalian systems. The experimental approaches used to elucidate FER signaling offer a methodological framework for hormone research:
Table 3: Research Reagent Solutions for Hormone Signaling Studies
| Reagent/Category | Specific Examples | Research Functions | Experimental Applications |
|---|---|---|---|
| Ligands/Peptides | RALF peptides, RALF1 | Receptor binding, signaling activation | Study of FER-mediated signaling crosstalk [6] |
| Hormone Analogs | Liraglutide (GLP-1 RA) | Receptor activation, pathway dissection | In vivo electrophysiology, feeding behavior studies [3] |
| Ion Channel Modulators | TRPC5 channel agents, K_ATP modulators | Neuronal excitability regulation | Mechanism of GLP-1 effects on POMC and AgRP neurons [3] |
| Novel Formulations | Biomaterial-based GH delivery systems | Enhanced bioavailability, targeted delivery | Assisted reproductive technology innovation [4] |
| Monitoring Technologies | Wearable sensors (Apple, Garmin, Fitbit) | Real-time physiological data collection | Pregnancy monitoring, hormone-physiology correlation [7] |
Protocol: Investigating FERONIA-Hormone Crosstalk
- Genetic Manipulation: Utilize FER mutant plants and transgenic complementation lines to establish baseline phenotypes related to growth, development, and stress responses.
- Hormone Treatment: Apply controlled concentrations of abscisic acid, auxin, brassinosteroids, or jasmonic acid to wild-type and mutant lines, monitoring transcriptional and post-translational responses.
- Transcriptional Analysis: Quantify expression of FER and RALF genes via qRT-PCR following hormone treatments to identify regulatory relationships.
- Protein-Protein Interaction: Employ co-immunoprecipitation and bimolecular fluorescence complementation to characterize interactions between FER and hormone signaling components.
- Phenotypic Characterization: Document physiological responses including root growth, stomatal aperture, and alkaline resistance under different hormone conditions.
Wearable Technology for Hormonal-Physiological Correlation
Recent advances in continuous monitoring technologies have enabled novel approaches to studying hormone-physiology relationships in real-world settings:
Protocol: Wearable Sensor Correlation with Hormonal States
- Participant Recruitment: Enroll eligible participants through digital platforms (e.g., PowerMom bilingual research platform), obtaining informed consent for data sharing [7].
- Device Integration: Collect data from commercial wearable devices (Apple, Garmin, Fitbit) capturing resting heart rate (RHR), physical activity, and sleep patterns [7].
- Longitudinal Tracking: Monitor physiological signals from pre-pregnancy through postpartum periods (approximately 18-month total duration) to establish baseline and track changes [7].
- Hormonal Correlation: Analyze RHR patterns in relation to expected hormonal fluctuations during pregnancy, using statistical modeling (e.g., R² calculation) to quantify associations [7].
- Outcome Stratification: Compare physiological patterns between normal pregnancies and those with adverse outcomes to identify predictive signatures [7].
This methodology has demonstrated a strong correlation (R² = 0.93) between RHR fluctuations and pregnancy-induced hormonal changes, highlighting the potential of wearable technology for non-invasive hormone-related monitoring [7].
Visualization of Key Signaling Pathways
GLP-1 Central Signaling Pathway
Diagram 1: GLP-1 Central Glucose Regulation (76 characters)
Hormonal Crosstalk in Plant Development
Diagram 2: FERONIA Hormone Crosstalk Network (77 characters)
GLP-2 Central Signaling Mechanism
Diagram 3: GLP-2 Central Signaling Pathway (76 characters)
Emerging Research Technologies and Clinical Applications
Innovative Monitoring and Therapeutic Platforms
The field of hormone research is being transformed by technological advances that enable unprecedented resolution in monitoring and intervention:
Continuous Hormone Monitoring Systems: The market for continuous hormone monitoring is projected to grow from USD 325.7 million in 2025 to USD 716.2 million by 2035, representing a CAGR of 8.2% [8]. These systems utilize non-invasive sampling methods (81% urine-based in 2025) and direct-to-consumer sales channels (62.7% market share in 2025) to make hormone tracking more accessible [8]. Innovations include DNA-based biosensors in wearable patches (Level Zero Health) and smartphone-integrated saliva analyzers (Eli Health's Hormometer) that provide real-time data on cortisol, progesterone, and other hormones [8].
Advanced Hormone Delivery Systems: Traditional hormone therapies face limitations in bioavailability and targeting. Novel biomaterial-based delivery systems for growth hormone and other therapeutic hormones enhance pharmacokinetic properties and tissue-specific delivery [4]. These innovations are particularly impactful in assisted reproductive technology, where GH formulations improve ovarian response and treatment outcomes [4].
Digital Phenotyping Integration: The correlation between wearable sensor data (resting heart rate, sleep patterns, activity) and hormonal states creates opportunities for digital biomarkers of endocrine function [7]. This approach has demonstrated utility in pregnancy monitoring, where specific RHR patterns strongly correlate with hormonal changes (R² = 0.93) and differ in pregnancies with adverse outcomes [7].
Future Research Directions
Several emerging areas represent promising frontiers for hormone research and therapeutic development:
Molecular Mechanism Elucidation: Despite rapid progress, comprehensive understanding of hormone signaling crosstalk remains incomplete. For example, while FERONIA is known to functionally connect with multiple plant hormones, the precise mechanisms of this interplay require further characterization [6]. Similarly, the exact signaling pathways by which GLP-1 activates POMC neurons and suppresses NPY/AgRP neurons in the arcuate nucleus remain poorly understood [3].
Hormone-Brain-Behavior Relationships: The computational and algorithmic frameworks linking hormonal states to neural population coding and behavioral persistence represent a transformative approach to understanding how hormones shape cognition and emotion [5]. Future research must disentangle causal effects from correlations and map the diversity of hormone-sensitive gene expression to neural functioning.
Personalized Hormone Therapeutics: The development of tailored hormone formulations based on individual genetic, metabolic, and lifestyle factors represents the future of endocrine medicine. This requires better understanding of how multiple hormones with different time-varying processes operate synergistically to change neural computation and behavior [5].
Hormones function as pivotal signaling molecules that coordinate development and maintain homeostasis through complex, interconnected pathways that operate across multiple biological scales—from molecular interactions to systemic regulation. Recent research has illuminated the sophisticated crosstalk between hormonal systems, the computational principles underlying hormone-brain interactions, and the potential of emerging technologies to monitor and modulate endocrine function with unprecedented precision. As the field advances, the integration of continuous monitoring platforms, targeted delivery systems, and computational modeling approaches will enable more effective interventions for hormonal disorders across the lifespan. These developments hold particular promise for addressing persistent challenges in reproductive health, metabolic disease, and neuroendocrine disorders, ultimately advancing both basic science understanding and clinical applications in endocrine research.
Novel Hormone Actions in Disease Development and Physiological Processes
The traditional understanding of hormones as simple chemical messengers regulating classic physiological processes like growth, metabolism, and reproduction has undergone a significant paradigm shift. Novel hormone actions extend beyond these conventional roles to include sophisticated regulation of cellular fate, immune modulation, cancer progression, and neural plasticity through mechanisms that are only beginning to be understood. These newly discovered functions operate through complex signaling pathways, often involving non-genomic actions and crosstalk with other regulatory systems, revealing an intricate network of hormonal influence on health and disease [2] [9].
The framework for understanding these novel actions is firmly rooted in the context of recent insights into hormonal roles during development and functional regulation. Hormones orchestrate developmental processes from conception through adulthood, with deviations from standard physiological levels leading to pathological states affecting the normal developmental trajectory [2]. This whitepaper examines the cutting-edge discoveries of unconventional hormone actions, their mechanisms, and their implications for therapeutic interventions, providing researchers and drug development professionals with a comprehensive technical resource.
Nuclear Receptor Signaling: Beyond Conventional Paradigms
Structural and Functional Complexity of Nuclear Receptors
Nuclear receptors (NRs) represent a major class of ligand-activated transcription factors that mediate the effects of steroid hormones, thyroid hormones, vitamins, and other lipid-soluble signaling molecules. The human genome encodes 48 nuclear receptors that sense hydrophobic ligand molecules and directly modulate gene expression, bypassing the need for cytoplasmic signal cascades [9].
Table 1: Classification of Nuclear Receptor Subfamilies and Their Ligands
| Receptor Type | Family Members | Endogenous Ligands | Primary Physiological Roles |
|---|---|---|---|
| Type I (Steroid Receptors) | ER, AR, PR, MR, GR | Sex hormones, Glucocorticoids, Mineralocorticoids | Reproduction, Stress response, Electrolyte balance |
| Type II (Non-steroid Receptors) | TRα/β, RARα/β/γ, VDR, PPARα/β/γ | Thyroid hormone, Retinoic acid, Vitamin D, Fatty acids | Metabolism, Development, Cell differentiation |
| Type III (Orphan Receptors) | Testicular receptor, Germ cell nuclear factor | Unknown (or no ligand) | Development, Metabolic regulation |
The typical NR structure consists of several functional domains: an N-terminal transcription activation domain (NTD), a highly conserved DNA-binding domain (DBD), a hinge region, and a C-terminal ligand-binding domain (LBD) [9]. The NTD contains the first of two transactivation regions (AF-1) and possesses transcriptional activator functions, while the DBD features two zinc fingers that dock the hormone-receptor complex to hexanucleotide response elements within NR-regulated promoters [9].
Novel Signaling Mechanisms and Pathological Implications
Beyond the classical genomic actions, NRs exhibit several novel mechanisms with significant implications for disease development:
Ligand-Independent Activation: Several NRs can be activated by growth factor signaling pathways through phosphorylation cascades, even in the absence of their canonical ligands, contributing to hormone-resistant cancer progression [9].
Non-Genomic Signaling: Membrane-associated NRs can rapidly activate intracellular kinase cascades (e.g., MAPK, PI3K/Akt) without directly regulating transcription, influencing processes such as cell migration and apoptosis within minutes [9].
Circadian Regulation: Certain NRs, including REV-ERB and ROR families, serve as core components of the molecular clock machinery, integrating metabolic signals with circadian rhythms [9].
These novel mechanisms are implicated in various pathological conditions. In prostate cancer, multiple nuclear receptors have been shown to inhibit tumor growth, proliferation, and metastasis, leading to significant interest in targeting these receptors as therapeutic strategies [9]. Dysfunction of NRs has also been associated with specific diseases, including infertility, obesity, and diabetes [9].
Novel Hormone Actions in Development and Disease
Developmental Trajectories and Hormonal Programming
Recent research has revealed sophisticated hormonal actions throughout the developmental continuum, from fetal stages to adulthood. During fetal development, the interplay between endogenous hormone production and the maternal endocrine system shapes developmental outcomes [2]. The placenta serves as a crucial endocrine organ producing peptide and steroid hormones, each with distinct mechanisms influencing fetal programming with long-term health consequences.
Anti-Müllerian hormone (AMH), a member of the TGF-β family, exemplifies novel hormonal actions beyond its classical role in Müllerian duct regression. AMH is now recognized as a significant factor in polycystic ovarian syndrome (PCOS), with levels significantly higher in women with PCOS compared to those without this condition [2]. During fetal development, AMH has also been implicated as a potential cause of spontaneous abortion by inhibiting placental aromatase and increasing fetal exposure to estradiol and progesterone [2]. Current studies are investigating the importance of AMH in predicting live birth and its influence on sexual differentiation disorders [2].
The gut microbiome has emerged as a novel modulator of hormonal activity, particularly in metabolic and pubertal timing regulation. Research on causes and treatment of precocious puberty has examined the role of microorganisms, suggesting that microbiota passed from mother to child influences both metabolism and the production of certain hormones [2].
Hormonal Variability and Its Clinical Implications
Quantitative assessments of hormonal dynamics have revealed significant variability in reproductive hormones due to pulsatile secretion, diurnal variation, and nutrient intake, with important implications for clinical assessment and research methodologies.
Table 2: Variability Parameters of Key Reproductive Hormones
| Hormone | Coefficient of Variation (CV) | Morning to Daily Mean Decrease | Key Modulating Factors |
|---|---|---|---|
| Luteinizing Hormone (LH) | 28% | 18.4% | Pulsatile secretion, Circadian rhythm |
| Follicle-Stimulating Hormone (FSH) | 8% | 9.7% | Minimal diurnal variation |
| Testosterone | 12% | 9.2% | Meal consumption, Circadian rhythm |
| Estradiol | 13% | 2.1% | Menstrual cycle phase |
Research has demonstrated that testosterone levels in healthy men fall between 9:00 am and 5:00 pm by 14.9% (95% CI 4.2, 25.5%), though morning levels correlate with late afternoon levels in the same individual (r² = 0.53, P<.0001) [10]. Testosterone levels were reduced more substantially after a mixed meal (by 34.3%) than during ad libitum feeding (9.5%), after an oral glucose load (6.0%), or an intravenous glucose load (7.4%) [10]. These findings have crucial implications for the timing and interpretation of hormonal assays in both clinical and research settings.
Experimental Approaches and Methodologies
Advanced Hormone Monitoring Technologies
The emergence of digital health technologies has revolutionized hormonal assessment, enabling precise, at-home quantitative tracking of multiple hormones simultaneously. These platforms utilize sophisticated detection methods that provide unprecedented insights into hormonal dynamics:
Quantitative Urine Hormone Monitoring: Systems like the MIRA monitor use immunochromatography with fluorescence labeling of urine assays, measuring estrone-3-glucuronide (E3G), luteinizing hormone (LH), follicle-stimulating hormone (FSH), and pregnanediol glucuronide (PdG) with results connected to smartphone applications via Bluetooth technology [11].
Lateral Flow Immunoassay with Computer Vision: Platforms such as Oova employ test cartridges using nanotechnology that adjusts for pH, normalizes hydration levels, and filters out non-specific binding. The system utilizes innovative computer vision algorithms to adjust for effects from lighting, shadows, and movement to ensure accurate image capture for analysis [12].
Machine Learning for Baseline Determination: Advanced algorithms report each user's unique hormone baseline levels, with daily fluctuations compared to the user's personalized baseline instead of population-based norms, enabling more precise detection of individual hormonal patterns [12].
These technologies have revealed previously unappreciated aspects of hormonal physiology. For instance, research using these platforms has determined that calculated cycle lengths tend to be shorter than user-reported cycle lengths, and significant differences exist in cycle phase lengths between age groups, indicating that follicular phase length declines with age while luteal phase length increases [12].
Molecular Techniques for Hormone Action Elucidation
Cutting-edge molecular biology techniques have enabled unprecedented insights into the mechanisms of novel hormone actions:
CRISPR/Cas9 Screening: Gene knockout studies using the CRISPR/Cas9 system have elucidated the functions of specific hormone receptors. For example, investigation of melanocortin-3 and -4 receptors (MC3R and MC4R) in red crucian carp revealed that mc4r+/- fish had better growth performance and more visceral fat mass while mc3r+/- fish showed no significant differences compared to wild type fish [13].
Co-immunoprecipitation and Luciferase Assays: These techniques have been employed to explore genetic interactions in hormonal pathways. Research on ecdysone signaling in crustaceans utilized co-immunoprecipitation to confirm interaction between EcR and RXR receptors, while dual-luciferase assays demonstrated that their heterodimer complex strongly activated transcription of the ecdysone pathway's key gene E75 [13].
RNA Sequencing for Pathway Analysis: Transcriptomic analyses have identified hormonal regulation of diverse physiological processes. RNA-seq in melanocortin receptor knockout models showed that pathways related to lipid accumulation and growth were changed in mc3r+/- and mc4r+/- fishes [13].
Diagram 1: Experimental Workflow for Comprehensive Hormone Analysis. This flowchart outlines the key steps in modern hormone assessment, from sample collection through clinical interpretation, highlighting the integrated approach required for accurate hormonal profiling.
Signaling Pathways and Molecular Mechanisms
Nuclear Receptor Activation and Gene Regulation
The molecular mechanisms through which nuclear receptors regulate gene expression involve a sophisticated multi-step process with several regulatory checkpoints:
Diagram 2: Nuclear Receptor Signaling Pathway. This diagram illustrates the sequential process of nuclear receptor activation, from ligand binding through gene expression regulation, culminating in physiological effects on development and metabolism.
Upon ligand binding, nuclear receptors undergo conformational changes that facilitate their interaction with transcriptional cofactors and specific DNA sequences called hormone response elements (HREs) in the promoter or enhancer regions of target genes [9]. The HREs are composed of two hexanucleotide sequences separated by a variable number of spacer sequences, with sequence variations determining receptor specificity [9].
Several posttranslational modifications, including phosphorylation, ubiquitination, and SUMOylation, finely modulate NR activities, adding layers of regulation to hormonal signaling [9]. Additionally, NRs can be indirectly recruited to the genome by tethering mechanisms through other DNA-bound transcription factors, expanding their regulatory potential beyond direct DNA binding [9].
Novel Signaling Pathways in Disease Pathogenesis
Recent research has uncovered several non-traditional hormonal signaling pathways with significant implications for disease development:
Hormone-Imm System Crosstalk: Sex steroid hormones have been studied for their role in treating certain depressive disorders in adults, suggesting novel neuromodulatory functions beyond their classical reproductive effects [2].
Hormonal Regulation of Metabolism: The melanocortin-3 and -4 receptors (MC3R and MC4R) directly participate in energy metabolism homeostasis. Research has shown that MC4R plays a more significant role in growth and lipid regulation than MC3R, offering potential targets for endocrine regulation of metabolic traits [13].
Ecdysone Signaling in Crustaceans: Studies in the Chinese mitten crab revealed that RxR was more stably expressed and at higher levels than EcR throughout the molting cycle, while EcR expression increased sharply during the pre-molt stage. The heterodimer complex of EcR and RXR strongly activated transcription of the ecdysone pathway's key gene E75, providing insights into evolutionary conservation of hormonal signaling mechanisms [13].
Pharmaceutical Interventions and Therapeutic Applications
Current Therapeutic Landscape
Drugs targeting specific nuclear receptors constitute 15-20% of all pharmacologic drugs, highlighting their tremendous therapeutic importance [9]. Current pharmaceutical interventions include:
Selective Estrogen Receptor Modulators (SERMs): Tamoxifen and raloxifene target the estrogen receptor (ER) and are used to treat osteoporosis and breast cancer [9].
Androgen Receptor Antagonists: Enzalutamide is used to treat prostate cancer by targeting the androgen receptor (AR) [9].
PPARγ Agonists: Thiazolidinediones are used to treat type 2 diabetes by targeting peroxisome proliferator-activated receptor-gamma (PPARγ) [9].
However, many currently available drugs often lack specificity and exhibit significant side effects, including severe heart failure, driving the development of compounds with stronger binding affinities and better specificity [9].
Emerging Therapeutic Approaches
Novel therapeutic strategies are focusing on more precise targeting of hormonal pathways:
Puberty Blockers: Research on puberty modulation, particularly in gender dysphoria, has investigated drugs like leuprolide acetate (LA) and histrelin implants (GnRH agonists). Mouse experiments using prepubertal administration of leuprolide acetate found similar long-term outcomes in ovarian function and embryologic development compared with controls, suggesting no permanent reproductive impairment with puberty blockers [2].
Congenital Adrenal Hyperplasia (CAH) Treatments: Novel CAH treatments have focused on alternative hypothalamic-pituitary-adrenal axis targets and the timing of drug delivery. New areas for research include the investigation of corticotropin-releasing factor (CRF) antagonists and abiraterone acetate, a CYP17A1 inhibitor, to treat androgen excess in CAH [2].
Hormone Replacement Formulations: Continuing research into growth hormone replacement focuses on the timing and hormone formulation (short vs long-acting GH) to limit the burden frequent injections can place on families while maintaining therapeutic efficacy [2].
Table 3: Novel Pharmaceutical Approaches Targeting Hormone Pathways
| Therapeutic Area | Drug/Treatment | Mechanism of Action | Development Stage |
|---|---|---|---|
| Prostate Cancer | Enzalutamide | Androgen receptor antagonist | Clinical use |
| Breast Cancer | Tamoxifen | Selective estrogen receptor modulator | Clinical use |
| Type 2 Diabetes | Thiazolidinediones | PPARγ agonist | Clinical use |
| Congenital Adrenal Hyperplasia | Abiraterone acetate | CYP17A1 inhibitor | Research phase |
| Precocious Puberty | Histrelin implants | GnRH agonist | Clinical use |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for Investigating Novel Hormone Actions
| Reagent/Material | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Quantitative Hormone Monitors | MIRA, Oova platforms | Hormone tracking across menstrual cycles, perimenopause | Quantitative measurement of E3G, LH, FSH, PdG in urine |
| CRISPR/Cas9 Systems | Gene knockout kits | Functional studies of hormone receptors | Targeted gene disruption in model organisms |
| Immunoassay Reagents | Co-immunoprecipitation antibodies, Luciferase assay kits | Protein-protein interaction studies | Detection of receptor dimerization and transcriptional activation |
| RNA Sequencing Kits | Transcriptomic profiling kits | Pathway analysis in hormone-treated cells | Genome-wide expression analysis of hormone-regulated genes |
| Hormone Response Element Reporters | Luciferase constructs with HRE promoters | Analysis of receptor transcriptional activity | Measurement of receptor-mediated transcription activation |
| Cell Line Models | Hormone-responsive cancer cells, Receptor-overexpressing lines | In vitro screening of hormone analogs | High-throughput drug screening and mechanism studies |
The expanding understanding of novel hormone actions in disease development and physiological processes reveals an increasingly complex landscape of endocrine regulation. From nuclear receptor mechanisms to hormonal variability in development and disease, these insights are driving innovative therapeutic approaches and research methodologies. The intricate interplay between hormonal signaling and other regulatory systems, including the microbiome, immune function, and metabolic pathways, underscores the multifaceted nature of endocrine physiology and pathology.
Future research directions will likely focus on several key areas: the development of more specific nuclear receptor modulators with reduced side effects, the elucidation of non-genomic hormone actions and their therapeutic potential, the exploration of hormonal cross-talk in complex diseases, and the application of personalized medicine approaches based on individual variability in hormone metabolism and receptor sensitivity. As research continues to uncover new dimensions of hormonal actions, these insights will undoubtedly lead to more effective and targeted interventions for a wide range of hormone-related diseases.
Feedback Mechanisms and the Regulation of Hormone Production
Hormonal feedback mechanisms are fundamental biological processes that maintain endocrine system homeostasis, ensuring precise regulation of physiological functions. These intricate loops operate through a series of detection and response systems where hormone levels themselves dictate the continuation or cessation of their own production. The central nervous system, particularly the hypothalamic-pituitary axis, serves as the primary integration center for these regulatory signals, processing inputs from throughout the body to maintain optimal hormone concentrations [14].
Recent research has significantly advanced our understanding of these mechanisms, revealing unprecedented complexity in how hormones regulate their own secretion. The neuroendocrine control of growth hormone (GH) secretion, for instance, involves multiple coordinated negative feedback loops that operate at both pituitary and hypothalamic levels, demonstrating redundant control mechanisms that ensure system reliability [14]. This sophisticated regulatory architecture enables the endocrine system to respond appropriately to diverse physiological states, from neonatal development to pregnancy and metabolic challenges like hypoglycemia and prolonged food deprivation [14].
Core Mechanisms of Hormonal Feedback Regulation
Negative Feedback Loops in Hormone Regulation
Negative feedback represents the predominant mechanism for maintaining hormonal equilibrium. This process involves a self-limiting cycle where the output of a hormonal pathway inhibits its own continued production. The hypothalamic-pituitary-target organ axis exemplifies this principle across multiple endocrine systems, creating precisely controlled feedback loops that prevent both deficiency and excess of hormone secretion.
In the growth hormone regulatory system, multiple negative feedback mechanisms detect changes in circulating levels of either GH or insulin-like growth factor 1 (IGF-1) [14]. These regulatory loops occur at both the pituitary and hypothalamic levels, indicating the presence of redundant control mechanisms that provide fail-safe protection for this critical physiological system. The complexity of this arrangement ensures that growth hormone secretion maintains its characteristic pulsatile pattern, which is essential for its proper biological effects [14].
Table 1: Key Hormonal Feedback Loops and Their Functions
| Hormone Axis | Feedback Mechanism | Primary Regulatory Function | Clinical Significance |
|---|---|---|---|
| Growth Hormone (GH) | GH/IGF-1 negative feedback at pituitary and hypothalamic levels [14] | Regulates body growth, metabolism | Imbalances affect growth, metabolic health |
| Hypothalamic-Pituitary-Thyroid (HPT) | Thyroid hormones inhibit TRH and TSH secretion | Controls metabolic rate, thermogenesis | Hypothyroidism, hyperthyroidism |
| Hypothalamic-Pituitary-Gonadal (HPG) | Sex steroids inhibit GnRH, FSH, and LH secretion | Regulates reproduction, development | Fertility issues, pubertal disorders |
| Cortisol Regulation | Cortisol inhibits CRH and ACTH secretion | Manages stress response, metabolism | Cushing's syndrome, Addison's disease |
Novel Insights into Growth Hormone Regulation
Groundbreaking research has elucidated the complex brain circuits that control growth hormone release during sleep, offering fresh insights into health and fitness [15]. A recent study published in Cell has identified specific neuronal populations in the hypothalamus that orchestrate growth hormone release during the sleep-wake cycle—growth hormone releasing hormone (GHRH) neurons and two distinct types of somatostatin neurons [15].
This research has revealed a novel feedback mechanism in the brain that keeps growth hormone levels finely balanced. The discovered circuit shows that released growth hormone regulates activity in the locus coeruleus, a brainstem region governing arousal, attention, and cognition [15]. This creates a homeostatic yin-yang effect: during sleep, growth hormone gradually accumulates to stimulate the locus coeruleus and promote wakefulness, but when the locus coeruleus becomes overexcited, it paradoxically promotes sleepiness [15]. This exquisite balance between sleep and growth hormone forms a tightly regulated system where insufficient sleep reduces growth hormone release, while excessive growth hormone can push the brain toward wakefulness [15].
Experimental Models and Research Methodologies
Animal Models in Hormone Research
The Cre-lox system has emerged as a powerful technology for investigating hormonal feedback mechanisms in a controlled manner. This methodology enables researchers to disrupt specific genes in a time- and tissue-specific manner, allowing precise interrogation of endocrine pathways [16]. The system utilizes the bacteriophage Cre recombinase enzyme, which recognizes 34 bp LoxP sites placed flanking the target gene ("floxed" gene) and induces recombination between these sites, effectively disrupting gene function [16].
In studying growth hormone receptor (GHR) function, researchers have developed standardized protocols for global Ghr disruption in adult mice using a tamoxifen (TAM)-inducible Cre-lox system [16]. This approach has revealed crucial insights about the timing of GH action, demonstrating that reducing GH signaling in adulthood produces different physiological outcomes compared to lifelong GH deficiency. Studies using this system have shown that doses of 0.25 and 0.32 mg of TAM/g of body weight are sufficient to significantly reduce Ghr and Igf1 gene expression across multiple tissues, including liver, fat, kidney, skeletal and cardiac muscle [16].
Table 2: Research Reagent Solutions for Hormone Feedback Studies
| Research Tool | Composition/Type | Primary Function in Experiments | Example Application |
|---|---|---|---|
| Tamoxifen-inducible Cre-lox system | Cre recombinase under ROSA26 promoter + floxed target genes [16] | Tissue-specific, timed gene disruption | Adult-onset GHR knockout studies [16] |
| LEAP2 Peptide | Liver-expressed antimicrobial peptide 2 [17] | Native liver-derived hormone infusion | Studying effects on glucose metabolism, food intake [17] |
| Liquid Mixed Meal | Nutridrink (1010 kJ/100 mL: 29.7g carb, 9.6g protein, 9.3g fat) [17] | Standardized metabolic challenge | Assessing postprandial glucose metabolism [17] |
| Indirect Calorimetry System | Vyntus CPX Canopy (Vyaire Medical) [17] | Measuring energy expenditure, substrate utilization | Metabolic phenotyping in hormone studies |
| YSI 2900 Biochemistry Analyzer | Enzymatic metabolite measurement system [17] | Real-time glucose, metabolite monitoring | Frequent blood sampling during hormone tests |
Human Clinical Protocol for Hormone Intervention Studies
Rigorous human clinical protocols have been developed to investigate the effects of exogenously administered hormones on physiological processes. One such protocol detailed a randomized, double-blind, placebo-controlled, crossover trial to evaluate the effects of continuous intravenous infusion of liver-expressed antimicrobial peptide 2 (LEAP2) on postprandial glucose metabolism, appetite sensations, and ad libitum food intake in humans [17].
The protocol specifies meticulous preparation of the exogenous hormone administration, with LEAP2 dissolved in saline containing 0.5% human albumin, sterile filtrated, and tested for sterility and endotoxins before use [17]. The infusion rate targets a 2–3-fold higher steady state plasma concentration than endogenous levels, achieved through administration at 25 pmol/kg/min (115 ng/kg/min) [17]. Participant selection follows strict inclusion criteria (e.g., Caucasian men aged 18–60 years with BMI 20–30 kg/m² for lean cohorts) and exclusion criteria (anemia, hepatobiliary disorders, tobacco use) to control for confounding variables [17].
The experimental design includes standardized preparations preceding each test day, with participants instructed to avoid strenuous exercise, excessive eating, and alcohol while maintaining a food diary for 48 hours prior [17]. The use of a liquid mixed meal challenge and ad libitum meal test with precise blood sampling procedures enables researchers to quantify hormonal effects on metabolic parameters with high temporal resolution [17].
Diagram 1: Growth Hormone Feedback Regulation
Recent Research Advances and Clinical Implications
Sleep-Hormone Interconnections
Recent research has illuminated the critical relationship between sleep architecture and hormonal regulation. University of California, Berkeley researchers have mapped the specific neural circuits that connect sleep stages with growth hormone release, demonstrating why lack of sleep—particularly the early, deep phase called non-REM sleep—lowers growth hormone levels [15].
Using state-of-the-art circuit tracing in mice, the team discovered that the peptide hormones controlling GH release operate differently during REM and non-REM sleep [15]. Somatostatin and GHRH surge during REM sleep to boost growth hormone, but during non-REM sleep, somatostatin decreases while GHRH increases moderately to elevate growth hormone levels [15]. This precise temporal regulation during sleep cycles highlights the sophisticated integration of neurological and endocrine systems, with implications for understanding how sleep disturbances contribute to metabolic disorders, cognitive decline, and accelerated aging.
Therapeutic Applications and Hormone Therapy
Research into hormonal feedback mechanisms has yielded significant clinical applications, particularly in the realm of hormone replacement therapy (HT). Recent years have witnessed a paradigm shift in the understanding of HT safety and efficacy, culminating in the FDA's decision to remove the "black box" warning from menopausal hormone therapy labels [18]. This regulatory change reflects evolving evidence supporting the "timing hypothesis", which posits that risks associated with HT depend on when it is initiated relative to menopause onset [19].
Studies including the Kronos Early Estrogen Replacement Study and the Danish Osteoporosis Prevention Study have demonstrated that when initiated early in menopause, HT effectively reduces vasomotor symptoms, improves sleep, preserves bone health, and may even provide cardiovascular benefits without the previously associated risks [19]. This has profound implications for clinical practice, suggesting that properly timed hormone therapy can significantly improve quality of life for menopausal women while maintaining a favorable risk-benefit profile.
Diagram 2: Hormone Intervention Study Design
Future Directions and Research Implications
The evolving understanding of hormonal feedback mechanisms continues to open new therapeutic avenues for a range of conditions. Research into the neural circuits governing growth hormone release during sleep offers promising targets for treating sleep disorders tied to metabolic conditions like diabetes, as well as neurodegenerative diseases including Parkinson's and Alzheimer's [15]. The discovery that growth hormone not only builds muscle and bone but may also have cognitive benefits through its action on the locus coeruleus suggests potential applications in cognitive health and neurological disorders [15].
Advances in molecular techniques like the Cre-lox system enable increasingly precise investigations into the timing and tissue-specificity of hormonal actions [16]. These approaches are helping resolve longstanding questions about whether reduced GH action in adulthood might confer health benefits, challenging traditional views of GH supplementation for aging populations [16]. As these technologies continue to evolve, they will undoubtedly yield more sophisticated models for understanding the complex feedback regulation that maintains endocrine homeostasis throughout the lifespan.
The integration of advanced neurobiological techniques with endocrine research represents a particularly promising direction, potentially leading to novel hormonal therapies to improve sleep quality or restore normal growth hormone balance [15]. As one researcher noted, "This circuit could be a novel handle to try to dial back the excitability of the locus coeruleus, which hasn't been talked about before" [15], highlighting how basic research into feedback mechanisms can identify unexpected therapeutic targets for clinical development.
Cross-Regulation and Interaction Networks Between Different Hormones
The regulation of development, growth, and homeostasis in complex organisms is orchestrated by intricate hormonal networks. Rather than operating in isolation, hormones function through complex interaction networks and exhibit extensive cross-regulatory relationships that integrate environmental cues with intrinsic developmental programs. In plants, this hormonal crosstalk mediates the plasticity of ontogeny, conveying environmental inputs to shape developmental outcomes [20]. Similarly, in humans, hormones regulate tissue and organ function via binding to specific receptors, and their dysregulation is implicated in a wide spectrum of diseases [21]. Understanding these networks—comprising the hormones themselves, their receptors, and the downstream signaling components—is fundamental to advancing both basic biological research and applied therapeutic development. This whitepaper synthesizes recent insights into the architecture and function of these cross-regulatory networks, providing a technical guide for researchers and drug development professionals.
Core Concepts of Hormonal Crosstalk
Hormonal crosstalk can be defined as the interdependent and often synergistic or antagonistic interactions between different hormone pathways that collectively determine a specific physiological outcome. These interactions occur at multiple levels:
- Transcriptional Cross-Regulation: One hormone pathway can directly or indirectly influence the transcription of components of another pathway. In plants, for instance, few molecular mediators of direct crosstalk have been isolated, but complex cross-regulatory relations are evident at the transcriptional level [20].
- Signal Integration: Hormone pathways can target common transcriptome modules or separate but complementary modules to fine-tune processes like cell elongation [20].
- Spatiotemporal Specificity: The outcomes of hormonal interactions are highly dependent on the tissue, cell type, and developmental stage. Recent multi-omics analyses have begun to map these organ-specific hormone distributions and their associated molecular regulatory networks [22].
The evolution of these pathways, with auxin, gibberellin, and brassinosteroid signalling arising in sequence during land plant evolution, correlates with increased morphological complexity and developmental flexibility [20]. In humans, the construction of gender-specific, cross-tissue hormone-receptor interaction networks provides valuable insights into hormone-mediated inter-organ communication [21].
Experimental Methodologies for Network Analysis
Dissecting hormonal interaction networks requires a multi-faceted experimental approach. Below are detailed methodologies for key techniques used in recent pioneering studies.
Multi-Omics Integration for Organ-Specific Hormone Mapping
A comprehensive multi-omics analysis was employed to systematically elucidate organ-specific hormone distribution and molecular regulatory networks in the plant Cinnamomum burmanni [22].
Workflow:
- Sample Collection: Plant tissues (leaves, stems, roots) were harvested and immediately frozen.
- Metabolomic Profiling: A comprehensive hormone metabolomic analysis was conducted, identifying and quantifying 70 significantly differential hormones, including auxins, cytokinins, and gibberellins.
- Transcriptomic Sequencing: RNA was extracted and sequenced for full-length transcriptomic and transcriptomic analysis.
- Data Integration via WGCNA: Weighted gene co-expression network analysis (WGCNA) was used to correlate hormone abundance data with transcriptomic data, pinpointing 50 hormone signaling-related differentially expressed genes (DEGs).
- Transcription Factor Identification: Putative transcription factors (TFs) forming core regulatory modules (e.g., ARF, bHLH, GRAS) were identified through phylogenetic and functional analysis.
This methodology successfully established the first multi-omics-driven hormonal interaction network framework for C. burmanni [22].
Mutant Analysis and Transcriptomic Profiling in Hormone Response
To investigate the role of the transcription factor ATHB1 in hormone signaling networks in Arabidopsis thaliana, a combination of genetic mutant analysis and transcriptomic profiling was used [23].
Workflow:
- Plant Material Generation:
- Mutant Lines: The athb1-3 allele was retrieved from a gene trap collection, resulting in a two- to five-fold reduction in ATHB1 expression.
- Over-Expressing (OE) Lines: The ATHB1 coding sequence was cloned under the control of the CaMV 35S promoter and transformed into plants, resulting in approximately 30-fold over-expression.
- Reporter Lines: An ATHB1::GUS reporter line was generated to monitor expression patterns.
- Hormone and Stress Treatments: Wild-type and genetically modified plants were treated with methyl jasmonate (MeJA), ethylene, or subjected to wounding and flooding stresses.
- Phenotypic Analysis: Root growth and other developmental phenotypes were assessed following MeJA application to determine hormone sensitivity.
- Microarray Analysis: A comparative microarray analysis was performed on wild-type and athb1 mutant seedlings under both normal conditions and following MeJA exposure to identify differentially expressed genes.
This approach revealed that ATHB1 is induced by ethylene, wounding, and flooding, but repressed by MeJA, and influences plant sensitivity to MeJA by modulating the expression of genes involved in jasmonate and salicylic acid signaling under normal growth conditions [23].
Quantitative Hormone Monitoring and Variability Assessment
In human clinical research, understanding the inherent variability of hormone levels is crucial for accurate assessment. A study quantified this variability using detailed hormonal sampling [10].
Workflow:
- Participant Cohort: Data from 266 individuals, including healthy volunteers and those with reproductive disorders, were analyzed from placebo-treated arms of previous studies.
- Detailed Hormonal Sampling: Participants underwent frequent blood sampling to measure reproductive hormones (LH, FSH, Testosterone, Estradiol) over several hours.
- Statistical Analysis: The variability of each hormone was quantified using the coefficient of variation (CV) and entropy. The correlation between morning and late afternoon levels was also assessed.
This methodology established the reliability of single hormone measurements and quantified the pulsatile, diurnal, and nutrient-induced variability of key reproductive hormones [10].
Table 1: Key Reagents and Research Tools for Hormone Network Analysis
| Research Tool / Reagent | Function in Research | Example Application |
|---|---|---|
| Mutant & Over-Expressing Lines | To determine the function of a specific gene by comparing phenotypes and transcriptomes of loss-of-function and gain-of-function lines to wild-type. | Investigating ATHB1's role in jasmonate and ethylene signaling [23]. |
| Hormone Metabolomic Profiling | To comprehensively identify and quantify a wide array of hormones and their related compounds in biological samples. | Revealing organ-specific accumulation of IAA, GA, and CTK in C. burmanni [22]. |
| Reporter Gene Constructs (e.g., GUS) | To visualize the spatial and temporal patterns of gene expression in response to treatments or during development. | Monitoring ATHB1 promoter activity in response to stress and hormones [23]. |
| Weighted Gene Co-expression Network Analysis (WGCNA) | A bioinformatic method used to identify clusters (modules) of highly correlated genes and link them to external sample traits. | Pinpointing hormone signaling-related DEGs correlated with hormone levels in different organs [22]. |
| Remote Hormone Monitoring Platform | A non-invasive system for frequently and quantitatively tracking hormone levels from at-home users over multiple cycles. | Studying menstrual cycle phase length variability and hormone trends across age groups [24]. |
Key Signaling Pathways and Network Components
Core Plant Hormone Signaling Pathways
Plant hormone pathways are built around central regulatory modules that often involve targeted protein degradation.
Table 2: Core Components of Major Plant Hormone Signaling Pathways
| Hormone | Receptor | Central Signaling Components | Key Regulatory Action |
|---|---|---|---|
| Auxin | TIR1/AFB F-box proteins (Nuclear) | Aux/IAA repressors, ARF transcription factors | Auxin promotes TIR1-mediated degradation of Aux/IAA proteins, releasing ARFs to activate gene expression [22]. |
| Gibberellin (GA) | GID1 (Nuclear/Cytoplasmic) | DELLA transcription repressors (GRAS family) | Bioactive GA binds GID1, forming a complex that binds DELLA proteins and targets them for degradation, releasing growth repression [22]. |
| Cytokinin (CTK) | CHK receptors (ER/PM membrane) | Histidine-containing phosphotransfer (HPt) proteins, ARR-B transcription factors | A multi-step phosphorylay relays the signal from the receptor to type-B ARRs, which activate transcription of response genes [22]. |
Documented Crosstalk Interactions
Research has uncovered numerous specific points of crosstalk between hormone pathways:
- ATHB1 as an Integrative Node: In Arabidopsis, the ATHB1 transcription factor is induced by ethylene and repressed by methyl jasmonate (MeJA). ATHB1 levels, in turn, influence plant sensitivity to MeJA's growth-inhibitory effects and modulate the expression of genes involved in jasmonate and salicylic acid signaling under normal growth conditions, positioning it as a key integrator of different hormone signaling pathways [23].
- Transcriptional Reprogramming in Cinnamomum: Multi-omics analysis suggested that transcription factors like ARF (auxin), DELLA (gibberellin), and ARR-B (cytokinin) may form a core regulatory module that mediates hormone-dependent growth, development, and terpenoid biosynthesis [22].
- Synergistic Regulation of Growth: Auxin, brassinosteroid, and gibberellin can synergistically regulate common growth processes, particularly cell elongation, suggesting they may target common transcriptome modules or separate but complementary ones [20].
Quantitative Data and Variability in Hormone Assessment
Robust hormone network analysis requires an understanding of inherent hormonal variability. Key quantitative findings from human reproductive endocrinology are summarized below.
Table 3: Variability of Human Reproductive Hormones Based on Detailed Sampling
| Hormone | Coefficient of Variation (CV) | Diurnal Decrease\n(Morning to Daily Mean) | Notes on Variability |
|---|---|---|---|
| Luteinizing Hormone (LH) | 28% | 18.4% | Most variable hormone due to pulsatile secretion [10]. |
| Testosterone | 12% | 9.2% | Falls by 14.9% between 9 am and 5 pm in healthy men; strongly reduced (34.3%) after a mixed meal [10]. |
| Estradiol | 13% | 2.1% | - |
| Follicle-Stimulating Hormone (FSH) | 8% | 9.7% | Least variable reproductive hormone [10]. |
Implications for Research and Drug Development
The insights gleaned from analyzing hormonal interaction networks have profound implications:
- Precision in Hormone Assessment: The documented variability in hormone levels underscores the limitation of single measurements and informs more reliable clinical assessment protocols. For instance, while testosterone levels drop during the day, late afternoon levels can predict morning levels, offering clinical utility [10].
- Novel Therapeutic Targets: The identification of key integrators of hormonal crosstalk, such as the ATHB1 transcription factor in plants or specific HRs in humans, reveals new potential targets for therapeutic intervention. In humans, a systematic analysis of HRs highlights their extensive involvement in cancers and nervous system diseases [21].
- Informed Breeding and Biotechnology: Understanding the core transcriptional modules (e.g., ARF, DELLA, ARR-B) that coordinate hormone signals allows for targeted genetic manipulation in crops to improve traits like stress tolerance and secondary metabolite production [22].
- Advanced Diagnostic Tools: The development of remote, quantitative hormone monitoring platforms enables the move away from outdated textbook averages for cycle tracking, allowing for personalized health assessments and fertility planning [24].
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions for Hormone Network Studies
| Category | Specific Item | Function / Application |
|---|---|---|
| Genetic Tools | T-DNA Insertion Mutants (e.g., athb1-3) | For loss-of-function studies and phenotype analysis [23]. |
| Over-Expression Constructs (e.g., 35S::ATHB1) | For gain-of-function studies to determine the effect of hyper-activation of a gene [23]. | |
| Molecular Biology | Reporter Constructs (e.g., ATHB1::GUS) | To visualize gene expression patterns in response to hormonal or environmental stimuli [23]. |
| Analytical Platforms | Metabolomic Profiling Kits | For comprehensive identification and quantification of hormone metabolites [22]. |
| Transcriptomic Sequencing Services | For genome-wide expression analysis (RNA-seq) to identify differentially expressed genes [23] [22]. | |
| Bioinformatics | WGCNA Software Packages | To identify co-expressed gene modules and correlate them with hormonal or phenotypic traits [22]. |
| Clinical Research | Quantitative At-Home Hormone Tests | For frequent, longitudinal non-invasive monitoring of hormone levels in human subjects [24]. |
Newly Discovered Hormones and Their Regulatory Mechanisms
The field of endocrinology is being reshaped by the discovery of novel hormonal mechanisms and the redefinition of functions for known hormones. This whitepaper synthesizes recent breakthroughs that are expanding our understanding of hormonal regulation, with particular emphasis on neural circuitry control, brain-synthesized hormones, and their implications for therapeutic development. Research now reveals that hormones function within complex, interconnected regulatory networks rather than operating through linear pathways. These findings are particularly transformative for understanding developmental processes, metabolic regulation, and neural-endocrine crosstalk, offering new targets for addressing conditions ranging from obesity to neurodegenerative diseases. The integration of advanced methodologies—from single-cell genomics to precise neural circuit mapping—is enabling unprecedented resolution of these regulatory systems.
Novel Neuroendocrine Regulatory Circuits
Brain Circuitry Controlling Growth Hormone Release During Sleep
The neural circuits governing pulsatile growth hormone (GH) release during sleep represent a significant advance in understanding the brain's role in somatic regulation. UC Berkeley researchers have delineated a precise feedback mechanism embedded within the hypothalamus and brainstem [15].
Key Discovery: The release of growth hormone-releasing hormone (GHRH) during non-REM sleep triggers GH secretion, which then stimulates neurons in the locus coeruleus—a brainstem region regulating arousal and cognition [15]. This creates a homeostatic balance where sleep drives GH release, and GH accumulation subsequently promotes wakefulness. Disruption of this circuit explains why sleep deprivation impairs growth, metabolic health, and cognitive function.
The experimental approach employed state-of-the-art circuit tracing and optogenetics in mice. Researchers inserted electrodes to record neuronal activity and used light to selectively stimulate hypothalamic GHRH neurons while monitoring downstream effects [15]. This revealed that somatostatin and GHRH surge during REM sleep to boost GH, while during non-REM sleep, somatostatin decreases and GHRH increases moderately to elevate GH levels [15].
Table: Growth Hormone Regulatory Neurons and Their Functions
| Neuron Type | Location | Function in GH Regulation | Activity During Sleep Phases |
|---|---|---|---|
| GHRH Neurons | Hypothalamus | Stimulate GH release | Moderate increase during non-REM sleep |
| Somatostatin Neurons (Type 1) | Hypothalamus | Inhibit GH release | Decreases during non-REM sleep |
| Somatostatin Neurons (Type 2) | Hypothalamus | Inhibit GH release | Surges during REM sleep |
| Locus Coeruleus Neurons | Brainstem | Regulate arousal; stimulated by GH | Increased activity with GH accumulation |
Neuroestrogens as Appetite Regulators
The discovery that estrogen synthesized directly in the brain functions as a potent appetite regulator represents a paradigm shift in neuroendocrinology. Previously considered primarily a reproductive hormone, estrogen produced via the aromatase enzyme in neurons—termed neuroestrogen—now emerges as a crucial metabolic regulator [25].
Mechanistic Insight: Neuroestrogen enhances expression of the melanocortin-4 receptor (MC4R) in the hypothalamus, a critical receptor for satiety signaling. Additionally, it amplifies leptin sensitivity, strengthening the body's natural appetite-suppressing pathways [25].
The experimental validation involved multiple mouse models: ovariectomized mice (lacking ovarian estrogen), aromatase-knockout mice (ArKO, lacking estrogen synthesis), and brain-specific aromatase reactivated mice (BrTG-ArKO). When aromatase was selectively restored only in the brains of ArKO mice, they exhibited significantly reduced food intake and increased hypothalamic MC4R expression compared to controls [25]. Complementary cell culture experiments confirmed neuroestrogen directly increases MC4R levels in hypothalamic neurons, independent of peripheral estrogen sources [25].
Advanced Research Methodologies
Experimental Protocols for Hormone Circuit Mapping
Circuit Mapping in Growth Hormone Regulation: The UC Berkeley team employed a sophisticated multi-technique approach to decipher GH regulatory circuits [15]:
- Electrophysiological Recording: Implantation of electrodes in specific hypothalamic regions to monitor GHRH neuron activity patterns across sleep-wake cycles in mice.
- Optogenetic Stimulation: Using light-sensitive proteins to selectively activate GHRH neurons with precise temporal control while measuring downstream GH release.
- Circuit Tracing: State-of-the-art neural tracing techniques to map connections between GHRH neurons, somatostatin neurons, and the locus coeruleus.
- Hormonal Measurement: Continuous blood sampling during sleep phases to correlate neural activity with pulsatile GH secretion patterns.
Neuroestrogen Appetite Regulation Protocol: The Fujita Health University study implemented a comprehensive strategy [25]:
Genetic Models:
- Ovariectomized mice (OVX) to eliminate ovarian estrogen
- Global aromatase knockout mice (ArKO) to disable all estrogen synthesis
- Brain-specific aromatase reactivated mice (BrTG-ArKO) to isolate neuroestrogen effects
Behavioral Measurements: Precise monitoring of food intake and body weight changes across experimental groups.
Molecular Analysis:
- Quantitative PCR and immunohistochemistry to measure MC4R expression in hypothalamic tissues
- Leptin sensitivity tests through exogenous leptin administration and food intake monitoring
- Cell culture validation using hypothalamic neurons treated with neuroestrogen
Quantitative Hormone Monitoring Technologies
Recent advances in hormone monitoring technologies enable unprecedented precision in tracking hormonal fluctuations. These platforms represent a significant evolution from traditional immunoassays to integrated digital health systems [26].
Table: Quantitative Hormone Monitoring Platforms
| Platform/Device | Hormones Measured | Biological Sample | Research/Clinical Applications |
|---|---|---|---|
| Mira Analyzer | E3G, LH, PDG | Urine | Menstrual cycle phase analysis, postpartum fertility return |
| Inito Monitor | E3G, LH, PDG | Urine | Fertility window identification, cycle abnormalities |
| Proov Tests | FSH, E3G, LH, PDG | Urine | Ovulation confirmation, luteal phase assessment |
| Oova Monitor | LH, PDG | Urine | Cycle tracking, hormone pattern identification |
| ClearBlue Fertility Monitor | Estrogen, LH | Urine | Fertility awareness, natural family planning |
These technologies have revealed critical insights, including the discovery that triggering ovulation before the first postpartum period requires higher LH thresholds than in regularly cycling women, suggesting decreased ovarian responsiveness to LH stimulation during this period [26].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Research Reagents for Hormone Mechanism Studies
| Reagent/Tool | Function/Application | Example Use in Cited Research |
|---|---|---|
| Optogenetic Constructs | Light-activated neuronal stimulation | Selective activation of GHRH neurons during sleep phases [15] |
| Aromatase Knockout (ArKO) Models | Elimination of estrogen synthesis | Determining neuroestrogen-specific effects [25] |
| Cell-Type-Specific Promoters | Targeted gene expression in specific neuron populations | Brain-specific restoration of aromatase in BrTG-ArKO mice [25] |
| Electrode Arrays | In vivo neuronal activity recording | Monitoring GHRH neuron firing patterns across sleep-wake cycles [15] |
| Quantitative Hormone Monitors | Precise measurement of hormone fluctuations | Tracking E3G, LH, and PDG across menstrual cycles [26] |
| Single-Cell RNA Sequencing | Cell-cell interaction mapping | Identifying hormone-regulated networks in human breast [27] |
Signaling Pathways and Regulatory Circuits
The intricate balance illustrated above demonstrates how sleep architecture and hormonal release maintain homeostasis. This circuit represents a significant advance in understanding how neuroendocrine systems integrate multiple signals to regulate fundamental physiological processes.
Implications for Therapeutic Development
These discoveries open transformative avenues for pharmaceutical innovation. The growth hormone sleep circuit provides novel targets for treating metabolic conditions linked to sleep disorders, including diabetes and obesity [15]. Specifically, modulating GHRH neuron activity or locus coeruleus excitability could restore normal GH pulsatility in sleep-disordered patients.
The neuroestrogen-MC4R pathway offers exceptional promise for obesity therapeutics. By enhancing MC4R expression and leptin sensitivity specifically in the brain, researchers could develop more precise appetite-suppressing treatments without systemic hormonal effects [25]. This approach could particularly benefit women navigating menopausal or postpartum metabolic changes when neuroestrogen signaling may be compromised.
Advanced hormone monitoring platforms are revolutionizing personalized medicine approaches to endocrine health. These technologies enable precise tracking of individual hormone patterns, facilitating early detection of abnormalities and customized intervention strategies for conditions like polycystic ovarian syndrome and fertility challenges [26]. The integration of these quantitative tools with electronic health records represents the future of endocrine care.
The landscape of hormonal research has fundamentally shifted from viewing hormones as isolated signaling molecules to understanding them as components of complex, brain-integrated regulatory networks. The discoveries of sleep-regulated GH circuits and appetite-controlling neuroestrogens exemplify this paradigm shift, revealing unexpected connections between neural circuits, hormonal release, and physiological outcomes. These findings not only advance basic science but also create unprecedented opportunities for therapeutic innovation across metabolic, reproductive, and neurological disorders. As research continues to unravel the intricate feedback systems governing hormonal regulation, we anticipate a new generation of precisely targeted interventions that restore endocrine balance by working with the body's innate regulatory logic.
Advanced Techniques and Translational Applications in Endocrinology
Single-Cell RNA Sequencing for Mapping Hormone Receptor Expression
Single-cell RNA sequencing (scRNA-seq) has revolutionized molecular biology by enabling transcriptomic profiling at the single-cell level, providing unprecedented insights into cellular heterogeneity, lineage differentiation, and cell-type-specific gene expression patterns [28]. This transformative technology has become particularly valuable for mapping hormone receptor expression in complex tissues, allowing researchers to identify rare cell types and characterize subtle variations in receptor expression that bulk RNA sequencing averages across cell populations [28]. The ability to analyze gene expression at single-cell resolution has proven essential for medical research, especially in understanding hormone-responsive systems including breast cancer and thyroid function, where receptor expression patterns dictate cellular identity, function, and therapeutic response [29] [28].
The application of scRNA-seq to hormone receptor research addresses a critical gap left by conventional bulk sequencing approaches, which obscure cellular heterogeneity and mask unique phenotypes by averaging gene expression across entire cell populations [28]. For hormone receptor studies, this resolution is particularly crucial because receptor expression is often heterogeneous within tissues, with important functional consequences for development, physiological regulation, and disease pathogenesis. This technical guide examines current methodologies, applications, and analytical frameworks for employing scRNA-seq specifically for mapping hormone receptor expression patterns within the broader context of hormonal regulation during development and functional maintenance.
Technical Foundations and Methodologies
Core scRNA-seq Workflow
The standard scRNA-seq workflow consists of multiple critical steps, each requiring optimization for successful hormone receptor expression profiling. The process begins with species and tissue assessment, where key factors such as cell size, viability, tissue dissociation feasibility, and the presence of rigid cell walls must be carefully considered during sample preparation and cell isolation [28]. For hormone receptor studies involving human tissues or model organisms, standard protocols for generating single-cell suspensions are typically applicable, though tissues with complex cellular compositions may require specialized dissociation methods.
Following tissue assessment, cell isolation and capture is performed using techniques such as fluorescence-activated cell sorting (FACS) or magnetic-activated cell sorting (MACS), selected based on specific cell types and research objectives [28]. The choice between droplet-based platforms (e.g., 10x Genomics Chromium system) and plate-based methods (e.g., SMART-seq2) depends on required throughput and resolution needs, with each offering distinct advantages for hormone receptor research [28] [30]. For instance, Smart-seq2 provides full-length transcript coverage, enabling more comprehensive analysis of receptor isoforms, while 10x Genomics offers higher throughput for capturing cellular heterogeneity in complex tissues [31] [30].
Library preparation and sequencing strategies must be selected according to sample characteristics [28]. For samples yielding viable single cells, droplet-based platforms provide scalability and efficiency, while for fixed cells, small samples, or rare cell populations, alternative approaches such as SPLiT-seq and SMART-seq2 enable high-resolution transcriptomic profiling even when standard droplet-based methods are not feasible [28]. The selection of appropriate library preparation methods is particularly important for hormone receptor studies aiming to detect lower-abundance receptor transcripts alongside more highly expressed genes.
Computational Analysis Framework
The computational analysis of scRNA-seq data for hormone receptor mapping involves multiple processing steps:
- Mapping and quantification strategies depend on reference genome availability. For well-annotated species with available genomic resources, reference-based pipelines such as Cell Ranger are employed, while for species lacking high-quality reference genomes, pseudo-references can be constructed from full-length transcriptome sequencing [28].
- Data preprocessing includes quality control to remove low-quality cells and genes, normalization using methods such as the NormalizeData function, identification of highly variable genes, and batch effect correction using tools such as the Harmony R package [29] [28].
- Cell type identification is performed through clustering algorithms followed by annotation using canonical marker genes, with hormone receptor expression patterns serving as key identifying features for specific cell populations [29].
Advanced analytical approaches particularly relevant to hormone receptor research include differential gene coordination network analysis (dGCNA), which identifies networks of differentially coordinated genes that have been either strengthened (hyper-coordinated) or weakened (de-coordinated) in disease states [32]. This approach has revealed cell type-specific networks of dysregulated genes with remarkable ontological specificity, allowing for comprehensive functional classification of genes involved in disease processes [32]. Additionally, trajectory inference and RNA velocity analyses track cell progression and differentiation, providing dynamic perspectives on gene expression changes over time, which is particularly valuable for understanding hormone-mediated developmental processes [28].
Table 1: Key scRNA-seq Technologies for Hormone Receptor Research
| Technology | Throughput | Transcript Coverage | Best Applications in Hormone Receptor Research |
|---|---|---|---|
| 10x Genomics Chromium | High | 3'-end counting | Large-scale cellular heterogeneity studies, receptor subpopulation identification |
| SMART-seq2 | Low | Full-length | Isoform-level receptor analysis, alternative splicing studies |
| Smart-seq | Low to moderate | Full-length | Deep transcriptomic profiling of rare cell populations |
| SPLiT-seq | Moderate | 3'-end counting | Fixed cell applications, complex tissue analyses |
Experimental Design for Hormone Receptor Studies
Sample Preparation Considerations
Successful scRNA-seq experiments for hormone receptor mapping require careful sample preparation strategies tailored to the specific biological system under investigation. For clinical samples such as breast cancer biopsies, researchers must consider sample acquisition methods, transportation conditions, and dissociation protocols that preserve RNA quality while maintaining cell viability [33] [34]. The selection of appropriate enzymatic digestion cocktails and mechanical dissociation parameters must be optimized for each tissue type to maximize yield while minimizing stress-induced gene expression changes.
For hormone receptor studies involving rare cell populations such as circulating tumor cells (CTCs), specialized enrichment techniques may be necessary before scRNA-seq analysis [30]. Approaches include size-based MetaCell technology for label-free CTC enrichment from patient blood, or immunomagnetic methods using epithelial cell adhesion molecule (EpCAM) for positive selection [30]. These pre-enrichment strategies are particularly important for capturing sufficient cells for downstream analysis when investigating hormone receptor expression in rare cellular subsets.
Single-cell suspension quality must be rigorously assessed before library preparation, with critical parameters including cell viability (typically >80%), concentration, and absence of significant debris or aggregates [29]. For hormone receptor studies specifically, researchers should verify that dissociation procedures do not preferentially select against receptor-positive cells, which could introduce bias in subsequent analyses.
Controls and Replication
Appropriate experimental controls and replication strategies are essential for generating robust scRNA-seq data for hormone receptor mapping:
- Technical replicates help account for library preparation and sequencing variability, with recommendations including processing aliquots from the same cell suspension across multiple lanes or sequencing runs.
- Biological replicates are crucial for accounting for donor-to-donor variability, with recent studies typically including 5-10 donors per condition for human tissue analyses [32] [33].
- Positive and negative control cells with known hormone receptor expression patterns should be included when possible to validate experimental and analytical workflows.
The sample size requirements for scRNA-seq experiments depend on the research question, with studies aiming to identify rare hormone receptor-expressing subpopulations typically requiring larger cell numbers (often 10,000-50,000 cells per sample) compared to studies focused on dominant cell types [33] [34].
Analytical Approaches for Hormone Receptor Expression Mapping
Identification of Hormone Receptor-Expressing Cells
The first step in analyzing scRNA-seq data for hormone receptor research involves identifying cells expressing specific hormone receptors. This process typically begins with quality control metrics including thresholds for the number of detected features per cell (200-5,000), number of transcripts per cell (1,000-20,000), and mitochondrial gene expression proportion (<20%) [29]. Following quality control, cell clustering is performed using algorithms such as those implemented in the Seurat package, with subsequent cell type annotation based on canonical marker genes, including hormone receptors themselves [29].
For hormone receptor studies, it is particularly important to recognize that receptor expression may exist on a continuum rather than as a binary present/absent classification. Dimensionality reduction techniques such as UMAP or t-SNE can reveal gradients of hormone receptor expression that may correspond to functional states or transitional populations [33] [35]. Additionally, differential expression analysis between clusters can identify hormone receptors as key markers defining specific cell subpopulations, as demonstrated in breast cancer studies where estrogen receptor (ER) expression patterns define malignant epithelial cell populations [33].
Advanced Analytical Techniques
Several advanced analytical approaches provide particular value for hormone receptor mapping:
- Differential Gene Coordination Network Analysis (dGCNA): This network-based approach identifies gene modules with altered co-expression patterns in different states, revealing cell type-specific networks of dysregulated genes [32]. Applied to pancreatic islet cells, dGCNA revealed T2D-induced cell type-specific networks with remarkable ontological specificity, identifying coordinated changes in hormone response pathways [32].
- Trajectory Inference and RNA Velocity: These methods model cellular dynamics and transitions, allowing researchers to understand how hormone receptor expression changes during differentiation processes or in response to stimuli [28] [35]. In studies of human early embryonic development, such approaches have revealed dynamic changes in gene expression, including hormone response pathways, across developmental stages [31] [36].
- Copy Number Variation (CNV) Analysis: Tools such as InferCNV can distinguish malignant from normal cells based on chromosomal alterations, which is particularly valuable in cancer studies investigating hormone receptor expression in tumor cells [33] [34].
Table 2: Key Analytical Tools for Hormone Receptor scRNA-seq Studies
| Tool Category | Representative Software | Application in Hormone Receptor Research |
|---|---|---|
| Quality Control | Seurat | Filtering low-quality cells, normalization, feature selection |
| Clustering | SCANVI, CellHint | Cell type identification using known markers including receptors |
| Trajectory Analysis | Monocle, PAGA | Modeling hormone-mediated differentiation pathways |
| Network Analysis | dGCNA, WGCNA | Identifying coordinated hormone response programs |
| Differential Expression | limma, SCDE | Identifying receptor expression changes between conditions |
Research Applications and Case Studies
Hormone Receptor Mapping in Breast Cancer
scRNA-seq has dramatically advanced our understanding of hormone receptor expression in breast cancer, particularly for estrogen receptor-positive (ER+) disease. Studies analyzing primary and metastatic ER+ breast cancer samples at single-cell resolution have identified distinct gene expression profiles of tumor cells while revealing specific subtypes of stromal and immune cells that collectively contribute to an immunosuppressive microenvironment [33]. These investigations have demonstrated that malignant cells exhibit the most remarkable diversity of differentially expressed genes between primary and metastatic sample groups, indicating pronounced transcriptional dynamics within these cellular populations [33].
The application of scRNA-seq to circulating tumor cells (CTCs) has provided particularly valuable insights into hormone receptor dynamics during cancer progression. Molecular characterization of CTCs from breast cancer patients has identified distinct integrin expression profiles and revealed three major CTC clusters—estrogen receptor-positive (ER+), human epidermal growth factor receptor 2-positive, and triple-negative—each exhibiting distinct expression profiles including key oncogenes [30]. These findings highlight how scRNA-seq can uncover heterogeneity in hormone receptor expression that might be masked in bulk analyses of primary tumors.
In the context of therapy resistance, scRNA-seq has identified molecular biomarkers predicting response to cyclin-dependent kinase 4/6 inhibitors (CDK4/6is) in patients with HR+/HER2- metastatic breast cancer [34]. This research revealed that late-progressing tumors display enhanced Myc, epithelial-mesenchymal transition (EMT), TNF-α, and inflammatory pathways compared to early-progressing tumors, providing insights into resistance mechanisms and potential therapeutic targets [34].
Thyroid Hormone Receptor Studies
scRNA-seq applications have extended to thyroid cancer research, where investigators have identified shared gene signatures between thyroid and breast cancers [29]. Integrative analyses of transcriptomic and single-cell sequencing data from both malignancies have revealed significant similarities in their transcriptional networks, with weighted gene co-expression network analysis (WGCNA) identifying consensus modules strongly associated with both cancers [29]. These shared molecular features may explain clinical observations of bidirectional cancer risk between these hormone-responsive tissues.
Research suggests that thyroid and estrogen signaling pathways may serve as pathogenic factors for both cancers, with both estrogen receptors (ERα) and thyroid-stimulating hormone receptors (TSHR) belonging to the G protein-coupled receptor (GPCR) family, activating similar signaling cascades (e.g., via cAMP/PKA, MAPK) to mediate biological effects [29]. This shared hormonal dependency implies that both tissue types may exhibit molecular similarities in their sensitivity to changes in the hormonal microenvironment, which can be effectively characterized through scRNA-seq approaches [29].
Developmental and Systems Biology Applications
Beyond cancer biology, scRNA-seq has provided fundamental insights into hormone receptor expression patterns during development. Studies of human early embryonic development have systematically explored gene expression dynamics integrating gene expression level with alternative splicing, isoform switching, and expression regulatory network analysis [31]. These investigations have found that genes involved in significant changes in these three aspects gradually decrease along embryonic development from E3 to E7 stage, providing insights into developmental regulation of hormone responsiveness [31].
In plant systems, scRNA-seq has revealed developmental trajectories and environmental regulation of callus formation in Arabidopsis, identifying transcription factor networks and gene regulatory programs involved in hormonal responses [35]. This research has highlighted the involvement of environmental factors—with low oxygen and salinity promoting callus formation, while light inhibited it—demonstrating how scRNA-seq can elucidate interactions between hormonal and environmental signaling pathways [35].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for scRNA-seq Hormone Receptor Studies
| Reagent Category | Specific Examples | Function in Hormone Receptor Research |
|---|---|---|
| Tissue Dissociation Kits | Miltenyi Biotec Tumor Dissociation Kits | Generation of single-cell suspensions from hormone-responsive tissues |
| Cell Separation Reagents | EpCAM microbeads, FACS antibodies | Enrichment of specific hormone receptor-positive cell populations |
| scRNA-seq Library Prep Kits | 10x Genomics Single Cell 3' Reagent Kits | Barcoding and preparation of single-cell libraries for sequencing |
| Single-Cell Multiome Kits | 10x Genomics Single Cell Multiome ATAC + Gene Expression | Simultaneous profiling of gene expression (including receptors) and chromatin accessibility |
| Hormone Response Assays | Luciferase-based reporter constructs, ERα signaling assays | Validation of hormone receptor activity in specific cell types |
| Reference Transcriptomes | GENCODE, Ensembl | Mapping reads to hormone receptor genes and isoforms |
Signaling Pathway Visualization
Diagram 1: Hormone Receptor Signaling Pathways. This diagram illustrates key signaling pathways for thyroid-stimulating hormone receptor (TSHR) and estrogen receptor (ERα), representing major classes of hormone receptors that can be studied using scRNA-seq approaches.
Experimental Workflow Visualization
Diagram 2: scRNA-seq Experimental Workflow. This diagram outlines the comprehensive workflow for single-cell RNA sequencing studies focused on mapping hormone receptor expression, from sample collection through data analysis and validation.
The application of scRNA-seq to hormone receptor research continues to evolve with emerging technological and analytical innovations. Multi-omics approaches that combine scRNA-seq with epigenetic profiling techniques such as single-cell ATAC-seq are providing unprecedented insights into the regulatory landscape controlling hormone receptor expression [28]. Spatial transcriptomics technologies are adding geographical context to hormone receptor expression patterns, revealing how cellular positioning within tissues influences receptor expression and function [30]. Machine learning integration is enhancing the analysis of scRNA-seq data, improving cell identification, clustering, and the detection of subtle expression patterns that might characterize hormone-responsive cellular states [30].
For researchers investigating hormone receptor expression, several key considerations will shape future studies. First, the development of standardized protocols specifically optimized for hormone-responsive tissues will improve reproducibility and data comparability across studies [28] [30]. Second, increased attention to temporal dynamics through time-course experiments will elucidate how hormone receptor expression changes during development, in response to physiological cues, and throughout disease progression [31] [35]. Finally, the integration of scRNA-seq data with clinical outcomes will strengthen the translational relevance of findings, particularly in the context of hormone-responsive cancers and endocrine disorders [34].
In conclusion, scRNA-seq has emerged as a powerful methodology for mapping hormone receptor expression with unprecedented resolution. By enabling the identification of cellular heterogeneity, revealing novel cell subpopulations, and characterizing dynamic expression changes in response to developmental, physiological, and pathological stimuli, this technology is transforming our understanding of hormone action across biological systems. As technical capabilities continue to advance and analytical methods become increasingly sophisticated, scRNA-seq will undoubtedly yield further fundamental insights into hormone receptor biology with significant implications for both basic science and therapeutic development.
CRISPR/Cas9 and Gene Editing in Functional Hormone Studies
Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and CRISPR-associated protein 9 (Cas9) constitute a revolutionary genome-editing technology derived from an adaptive immune system in bacteria and archaea [37] [38]. This system functions as an RNA-guided DNA endonuclease that recognizes target sites through RNA-DNA complementarity and produces sequence-specific double-stranded breaks (DSBs) in DNA [38]. For researchers investigating hormone function, CRISPR/Cas9 provides unprecedented precision for dissecting the genetic underpinnings of hormone synthesis, receptor signaling, and feedback mechanisms. The technology's core components include the Cas9 endonuclease protein and a guide RNA (gRNA) sequence that directs Cas9 to a specific genomic locus adjacent to a Protospacer Adjacent Motif (PAM) sequence, typically 5'-NGG-3' for the most commonly used Streptococcus pyogenes Cas9 (SpCas9) [39] [38].
In the specific context of hormone studies, CRISPR/Cas9 enables researchers to move beyond correlation to establish causation by directly modifying genes encoding hormones, their receptors, and downstream signaling components. This technical guide explores the current methodologies, applications, and experimental frameworks for implementing CRISPR/Cas9 in functional hormone research, with particular emphasis on its utility for investigating complex endocrine pathways during development and regulatory processes.
Core CRISPR/Cas9 Mechanisms and System Components
Molecular Mechanism of Action
The CRISPR/Cas9 system creates double-stranded breaks in DNA at precisely targeted locations through a two-component complex [38]. The Cas9 protein contains two nuclease domains: RuvC and HNH, which cleave opposite DNA strands to generate blunt-ended breaks [39] [38]. This cleavage is guided by a single-guide RNA (sgRNA), a synthetic fusion of CRISPR RNA (crRNA) containing the target-specific 20-nucleotide sequence, and trans-activating crRNA (tracrRNA) that serves as a scaffold for Cas9 binding [40] [38]. The system requires the presence of a PAM sequence immediately downstream of the target site for recognition and cleavage [38].
Following DNA cleavage, the cell activates endogenous repair mechanisms. The non-homologous end joining (NHEJ) pathway predominates and often results in small insertions or deletions (indels) that can disrupt gene function by causing frameshift mutations [40] [38]. Alternatively, when a donor DNA template is provided, the homology-directed repair (HDR) pathway can facilitate precise gene modifications, including specific point mutations or insertions [40]. For hormone researchers, this molecular versatility enables everything from complete gene knockouts of hormone receptors to precise introduction of disease-associated mutations for functional characterization.
Figure 1: CRISPR/Cas9 Mechanism and DNA Repair Pathways. The CRISPR/Cas9 ribonucleoprotein complex binds target DNA adjacent to PAM sequences, creating double-strand breaks repaired via NHEJ (often causing knockouts) or HDR (enabling precise edits).
CRISPR/Cas9 Toolbox for Hormone Research
The fundamental CRISPR/Cas9 system has been extensively engineered to create a diverse toolbox of gene-editing approaches, each with specific applications for hormone research [40].
CRISPR Knockout: The most straightforward application uses wild-type Cas9 to create double-strand breaks, relying on error-prone NHEJ repair to generate gene knockouts. This approach is ideal for permanently disrupting genes encoding hormones, their receptors, or signaling components to assess functional consequences [40] [38]. For example, knocking out the growth hormone receptor (GHR) gene enables researchers to study complete growth hormone resistance syndromes.
Base Editing: Catalytically impaired Cas9 fused to deaminase enzymes enables direct conversion of one DNA base to another without creating double-strand breaks [40]. Base editors are particularly valuable for introducing specific single-nucleotide polymorphisms (SNPs) known to affect hormone function or metabolism, such as polymorphisms in thyroid hormone pathway genes.
Prime Editing: A more recent innovation combines Cas9 nickase with reverse transcriptase to enable all 12 possible base-to-base conversions, as well as small insertions and deletions, without double-strand breaks [40]. This system offers particular promise for modeling endocrine disorders caused by specific point mutations with reduced risk of off-target effects.
CRISPR Interference/Activation (CRISPRi/a): Using catalytically dead Cas9 (dCas9) fused to transcriptional repressors (KRAB) or activators (VP64) enables precise regulation of gene expression without altering DNA sequence [40]. This approach allows researchers to mimic the graded hormone insufficiency or excess states commonly encountered in clinical endocrinology.
Table 1: CRISPR/Cas9 Systems for Hormone Research Applications
| System Type | Cas Enzyme | Key Components | Primary Application in Hormone Research | Editing Outcome |
|---|---|---|---|---|
| CRISPR Knockout | Wild-type Cas9 | sgRNA only | Complete loss-of-function studies of hormone receptors | Indels via NHEJ |
| HDR Editing | Wild-type Cas9 | sgRNA + donor template | Introducing specific disease-associated mutations | Precise edits via HDR |
| Base Editing | Cas9 nickase- deaminase fusion | sgRNA only | Modeling SNPs in hormone metabolic pathways | Point mutations without DSBs |
| Prime Editing | Cas9 nickase-RT fusion | pegRNA + optional sgRNA | Correcting or introducing multiple mutation types | Versatile edits without DSBs |
| CRISPRi | dCas9-KRAB fusion | sgRNA only | Reversible knockdown of hormone gene expression | Transcriptional repression |
| CRISPRa | dCas9-VP64 fusion | sgRNA only | Overexpression of hormone genes without integration | Transcriptional activation |
Experimental Design and Workflow
gRNA Design and Validation
Successful CRISPR experiments in hormone research begin with careful gRNA design. The target region within a gene of interest should be selected based on the specific experimental goal [40]. For knockout studies, targeting constitutive 5' exons or exons encoding critical protein domains maximizes the likelihood of generating null alleles [40]. For example, when targeting nuclear hormone receptors, the DNA-binding domain represents an optimal region since even small indels typically disrupt function.
gRNA design should prioritize both on-target efficiency and off-target specificity. Numerous computational tools are available to design gRNAs with minimal similarity to other genomic regions, reducing off-target effects [39] [40]. For hormone research, where pleiotropic effects are common, validating gRNA specificity is particularly important. Whenever possible, using validated gRNAs from scientific literature or plasmid repositories can save considerable time and resources [40].
Experimental Protocol: gRNA Design and Cloning
- Identify target genomic region based on experimental goal (e.g., 5' exons for knockouts, specific codons for point mutations)
- Use gRNA design tools (e.g., CRISPOR, ChopChop) to identify potential gRNAs with high on-target and low off-target scores
- Design oligonucleotides with appropriate overhangs for your chosen cloning system
- Anneal and phosphorylate oligonucleotides
- Perform restriction-ligation cloning into your gRNA expression vector
- Transform into competent bacteria and select positive clones
- Verify constructs by Sanger sequencing using vector-specific primers
- For critical experiments, test gRNA efficiency using the T7E1 assay or next-generation sequencing in a model cell line before proceeding to primary cells
Delivery Systems for Hormone Research
Selecting an appropriate delivery method is crucial for successful CRISPR experiments in hormone studies. The optimal approach depends on the target cell type, whether the application requires transient or stable modification, and the specific CRISPR system being used [40].
Plasmid Transfection: The most straightforward approach involves delivering plasmids encoding both Cas9 and gRNA via chemical transfection or electroporation [40]. This method works well for easily transfectable cell lines (e.g., HEK293) commonly used in hormone receptor studies. The main advantages include versatility and no strict size limitations, but efficiency can be low in primary endocrine cells.
Viral Delivery: Lentiviral and adeno-associated viral (AAV) vectors provide efficient delivery, particularly for difficult-to-transfect primary endocrine cells [40]. However, viral vectors have packaging size constraints, with AAV particularly limited to about 4.7kb, requiring the use of compact Cas9 orthologs like Staphylococcus aureus Cas9 (SaCas9) [39]. Lentiviral vectors can accommodate larger payloads but integrate into the genome, raising concerns about long-term Cas9 expression and potential immune responses.
Ribonucleoprotein (RNP) Delivery: Direct delivery of preassembled Cas9-gRNA complexes as ribonucleoproteins offers the fastest action and shortest exposure, reducing off-target effects [37]. This approach is ideal for primary endocrine cells and clinical applications, as it minimizes immune recognition and prevents persistent Cas9 expression. Electroporation is the most common delivery method for RNPs in hormone research.
Table 2: Delivery Methods for CRISPR/Cas9 in Hormone Research
| Delivery Method | Key Features | Ideal Applications in Hormone Research | Limitations |
|---|---|---|---|
| Plasmid Transfection | Easy to implement, versatile, no size constraints | High-throughput screening in immortalized cells, receptor studies | Low efficiency in primary cells, prolonged Cas9 expression increases off-target risk |
| Lentiviral Vectors | High efficiency, stable integration, broad tropism | Creating stable knockout cell lines, hard-to-transfect endocrine cells | Random integration, persistent Cas9 expression, immune responses |
| AAV Vectors | High efficiency, specific serotypes for different tissues, transient expression | In vivo hormone studies, targeting specific endocrine organs | Limited packaging capacity, potential pre-existing immunity |
| Ribonucleoprotein (RNP) | Rapid editing, reduced off-target effects, no vector DNA | Primary endocrine cells (pituitary, pancreatic islets), clinical applications | Requires specialized delivery (electroporation), optimization needed for each cell type |
| Lipid Nanoparticles (LNP) | Efficient in vivo delivery, clinical relevance, targets liver | Liver-targeted hormone therapies (e.g., growth hormone, thyroid hormone) | Primarily targets liver, optimization needed for other endocrine organs |
Validation and Analysis
Comprehensive validation of CRISPR edits is essential in hormone research, where partial function or hypomorphic alleles can produce misleading results. Validation should occur at multiple levels:
Genotypic Validation: Confirm intended edits at the DNA level using Sanger sequencing or next-generation sequencing. For knockout experiments, tracking indels by decomposition (TIDE) analysis can quantify editing efficiency and characterize the spectrum of induced mutations [40]. In hormone receptor studies, it's particularly important to verify biallelic editing, as heterozygous mutations may produce incomplete phenotypes due to dosage sensitivity.
Protein-Level Validation: Assess editing consequences at the protein level using Western blotting, immunofluorescence, or flow cytometry. For hormone receptors and signaling molecules, confirm loss of protein expression or detect truncated forms. Functional assays specific to the hormone pathway should follow, such as ligand binding assays for receptors or cAMP measurements for G-protein coupled receptors.
Phenotypic Validation: Implement appropriate functional assays to confirm the physiological consequences of gene editing. These might include hormone secretion assays, calcium imaging in endocrine cells, or transcriptional reporter assays for hormone-responsive genes.
Case Study: CRISPR/Cas9 Editing of Growth Hormone Receptor
Experimental Implementation
A recent groundbreaking study exemplifies the power of CRISPR/Cas9 for functional hormone research, focusing on the Growth Hormone Receptor (GHR) gene [41]. Researchers used CRISPR/Cas9 to create exon 3 deletions in HEK293 cells, modeling the naturally occurring d3GHR isoform associated with human longevity [41]. This experiment provides an excellent template for hormone researchers designing similar studies.
The experimental workflow involved designing gRNAs flanking exon 3 of the GHR gene, transfecting HEK293 cells with Cas9 and gRNA expression plasmids, and selecting clonal populations. Researchers achieved >85% editing efficiency through careful optimization of gRNA design and delivery conditions [41]. The successful generation of both homozygous (d3/d3) and heterozygous (d3/fl) isoforms enabled comprehensive comparison of hormone signaling across different genotypic states.
Figure 2: GHR Gene Editing Workflow and Functional Outcomes. CRISPR/Cas9-mediated deletion of exon 3 in the Growth Hormone Receptor gene using flanking gRNAs produces the d3GHR isoform with altered downstream signaling and improved stress resilience.
Signaling Pathway Analysis
Following successful gene editing, researchers comprehensively characterized the consequences for growth hormone signaling [41]. Homozygous d3GHR cells showed significantly reduced baseline expression of Insulin-like Growth Factor 1 (IGF-1) and components of the JAK/STAT signaling pathway compared to wild-type cells [41]. These findings demonstrate how CRISPR editing can directly probe the relationship between receptor structure and hormone signaling output.
Functional assessment under stress conditions revealed that heterozygous d3GHR cells exhibited 87% survival after 2 minutes of UV radiation compared to 67% for wild-type cells [41]. Under fasting conditions, d3GHR cells maintained 15% greater viability than wild-type controls [41]. These phenotypic differences highlight the functional consequences of receptor editing and illustrate how hormone signaling modifications can impact cellular resilience.
Advanced Applications in Hormone Research
In Vivo Hormone Studies
CRISPR/Cas9 applications have expanded to in vivo models, enabled by advanced delivery systems such as lipid nanoparticles (LNPs) that show particular tropism for the liver [42]. This delivery approach is highly relevant to hormone research, as the liver produces multiple endocrine factors including IGF-1, angiotensinogen, and hepcidin. Recent clinical advances demonstrate that LNPs can deliver CRISPR components systemically via IV injection, achieving efficient editing in hepatocytes [42].
The potential for redosing represents another significant advancement for hormone research. Unlike viral vector systems that typically permit only single administration due to immune responses, LNP delivery enables multiple doses [42]. This approach was successfully demonstrated in a personalized CRISPR treatment for an infant with CPS1 deficiency, where three LNP doses safely achieved incremental therapeutic benefits [42]. For long-term hormone studies requiring sustained editing, this redosing capability offers important flexibility.
High-Throughput Screening for Hormone Pathways
CRISPR/Cas9 enables genome-wide screening approaches to identify novel genes and pathways regulating hormone function. Pooled libraries containing thousands of gRNAs can be used to systematically knock out genes across the genome in endocrine cell populations. Subsequent selection pressures—such as hormone deprivation, ligand exposure, or stress conditions—can reveal genes essential for specific hormonal responses.
These screening approaches have identified novel regulators of insulin signaling, thyroid hormone action, and steroid hormone metabolism. The resulting datasets provide comprehensive maps of genetic networks controlling hormone responses, offering new therapeutic targets for endocrine disorders.
Research Reagent Solutions
Table 3: Essential Research Reagents for CRISPR-Based Hormone Studies
| Reagent Category | Specific Examples | Key Functions | Application Notes for Hormone Research |
|---|---|---|---|
| Cas9 Enzymes | SpCas9 (WT, nickase, dCas9), SaCas9, High-fidelity variants | DNA recognition and cleavage | High-fidelity variants reduce off-target effects in sensitive hormone signaling studies |
| gRNA Vectors | U6-promoter driven gRNA constructs, All-in-one Cas9-gRNA plasmids | Target sequence specification | Validated gRNAs for common hormone receptors save optimization time |
| Delivery Reagents | Lipofectamine CRISPRMAX, Electroporation systems, Lentiviral packaging plasmids | Introduction of editing components into cells | RNPs recommended for primary endocrine cells (pituitary, beta cells) |
| Selection Markers | Puromycin, GFP, Antibiotic resistance genes | Enrichment for successfully edited cells | Fluorescent markers enable sorting of edited cells for hormone secretion assays |
| Edit Validation Tools | T7E1 assay kits, Surveyor assay, NGS validation services | Confirmation of successful genome editing | NGS provides quantitative assessment of editing efficiency in heterogeneous endocrine tissues |
| Cell Culture Models | HEK293, Endocrine cell lines, Primary endocrine cells, iPSC-derived hormone cells | Experimental systems for editing | iPSC-derived hormone cells enable human-specific studies of rare endocrine disorders |
| Hormone Assays | ELISA kits, RIA, Transcriptional reporters, Calcium imaging | Functional assessment of editing outcomes | Multiple assay types recommended to comprehensively assess hormone pathway function |
Technical Considerations and Limitations
Addressing Off-Target Effects
Off-target activity remains a significant concern in CRISPR research, particularly in hormone studies where subtle changes in gene expression can produce profound physiological effects [39]. Cas9 can tolerate up to five mismatches between the gRNA and target DNA, potentially leading to editing at unintended genomic locations [39]. Several strategies can mitigate this risk:
High-Fidelity Cas9 Variants: Engineered Cas9 proteins with reduced off-target activity while maintaining high on-target efficiency are now available [39]. These include eSpCas9(1.1), SpCas9-HF1, and HypaCas9, which incorporate mutations that strengthen the proofreading mechanism during target recognition.
Dual Nickase Systems: Using paired Cas9 nickases with offset gRNAs requires two adjacent binding events for double-strand break formation, dramatically increasing specificity [40]. This approach is particularly valuable when editing genes with paralogs or those belonging to hormone receptor families with high sequence similarity.
Computational gRNA Design: Careful gRNA selection using tools that incorporate genomic context, chromatin accessibility, and epigenetic marks can identify guides with minimal off-target potential [40]. For hormone researchers, this is especially important when targeting genes in hormone-responsive genomic regions that may have altered chromatin states.
Delivery Challenges in Endocrine Tissues
Efficient delivery remains a primary challenge for CRISPR applications in endocrine research. Different endocrine organs present unique delivery barriers [37]. The blood-brain barrier protects hypothalamic and pituitary tissues, the extracellular matrix presents challenges in the thyroid and pancreas, and polarized epithelial structures complicate access to adrenal and reproductive tissues.
Novel delivery approaches show promise for overcoming these challenges. Cell-penetrating peptides can facilitate RNP delivery to difficult-to-transfect primary endocrine cells. Tissue-specific LNPs are being developed to target particular endocrine organs. Ultrasound-mediated microbubble destruction can temporarily disrupt barriers for localized delivery. Hormone researchers should carefully consider the optimal delivery strategy for their specific experimental system.
The CRISPR/Cas9 landscape continues to evolve rapidly, with several emerging technologies particularly relevant to hormone research. Prime editing offers more precise editing capabilities with reduced off-target effects, enabling introduction of specific hormone-related SNPs without double-strand breaks [40]. CRISPR-based epigenetic editing allows transient manipulation of hormone gene expression without permanent DNA changes, mimicking the dynamic regulation characteristic of endocrine systems [40].
Advanced delivery systems, particularly LNPs optimized for specific endocrine tissues, will expand in vivo applications for hormone studies [42] [37]. The demonstrated feasibility of redosing with LNP-based delivery opens possibilities for chronic hormone conditions requiring sustained editing [42]. Additionally, the development of CRISPR-based diagnostics compatible with hormone detection may enable future theranostic approaches in endocrinology.
In conclusion, CRISPR/Cas9 technology provides hormone researchers with an unprecedentedly precise and versatile toolkit for functional studies. By enabling targeted manipulation of genes encoding hormones, their receptors, and signaling components, this technology facilitates mechanistic studies that bridge molecular changes to physiological outcomes. As the technology continues to advance, with improvements in specificity, delivery, and editing capabilities, its impact on our understanding of hormone function during development and regulation will continue to grow, accelerating both basic research and therapeutic development in endocrinology.
Systems-Level and Computational Approaches in Neuroendocrinology
Neuroendocrinology is entering a transformative era marked by the integration of systems-level analysis and computational frameworks. This paradigm shift moves beyond traditional studies of isolated mechanisms to investigate how hormonal signaling orchestrates brain-wide neural activity and behavior [43] [5]. The primary goal of these approaches is to close the significant gap between our understanding of molecular processes—such as gene expression and cellular changes—and the emergent properties of neural populations and networks that govern behavior and cognition [5]. This is particularly crucial for understanding hormonal actions during development, where precise temporal and spatial regulation determines long-term functional outcomes [2] [44]. Systems-level and computational methods provide the tools to quantitatively describe how hormones, including sex steroids and gonadotropic hormones, regulate diverse processes from social behavior and emotional persistence to metabolic homeostasis across the lifespan [43] [2] [45].
Core Principles and Technological Foundations
Key Computational Concepts in Neuroendocrinology
Modern computational neuroendocrinology investigates how hormones implement specific algorithmic functions within neural circuits. A central concept is behavioral and neural persistence, where higher levels of hormones like estrogens and androgens promote stable, persistent behavioral states and reduce behavioral variability [5]. This persistence is theorized to be implemented neurally through mechanisms such as line attractors—a type of neural population activity that can maintain a stable state representing an ongoing internal condition [5]. Another key principle is representational drift, where the relationship between neural activity and external stimuli or behaviors changes over time despite stable behavioral outputs; this process appears to be modulated by hormonal states [5]. Hormones also regulate functional connectivity between brain regions, altering communication efficiency through changes in synaptic strength and network architecture [43] [5].
Essential Methodological Approaches
Table 1: Core Methodologies in Systems Neuroendocrinology
| Method Category | Specific Technologies | Primary Applications | Key Insights Generated |
|---|---|---|---|
| Large-Scale Neural Recording | Miniaturized microscopes, multi-fiber photometry, high-density electrophysiology [5] | Tracking population dynamics across hormone-sensitive brain regions in freely behaving animals | Hormones alter neural ensemble coordination during social behavior and decision-making |
| Cell-Type Specific Manipulation | Optogenetics, chemogenetics (DREADDs), CRISPR-mediated gene editing [5] | Establishing causal relationships between specific hormone-sensitive cell types and behavior | Identified VMHvllCckar cells as dynamically controlling female sexual behaviors over reproductive cycle [5] |
| Circuit Mapping | Monosynaptic tracing, transsynaptic viral vectors [5] | Defining connectivity patterns between hormone-sensitive nuclei | Revealed interconnected hypothalamic nodes for cyclical control of female sexual behavior [5] |
| Computational Modeling | Population dynamics analysis, network models, attractor models [5] | Formalizing how hormonal signals transform neural computations | Line attractor models explain how neuropeptide signaling maintains persistent internal states [5] |
Advanced recording technologies now enable researchers to monitor neural activity simultaneously from hundreds to thousands of neurons across multiple brain regions in freely behaving subjects [5]. This spatial and temporal resolution is crucial for capturing the distributed nature of hormone action on brain networks. When combined with cell-type-specific manipulations, these approaches establish causal links between molecular changes, neural population dynamics, and behavioral outcomes. Computational models then formalize these relationships into testable frameworks that can predict how hormonal manipulations will alter system-level functioning.
Experimental Protocols for Systems-Level Neuroendocrinology
Protocol: Recording Hormone-Mediated Neural Dynamics During Behavior
Objective: To characterize how fluctuating hormone levels alter brain-wide neural dynamics and population coding during motivated behaviors.
Materials:
- Laboratory animals (e.g., mice) with hormone-sensitivity (intact cycling females or gonadectomized with hormone replacement)
- Miniaturized microscopes (e.g., head-mounted microendoscopes) or multi-fiber photometry systems
- Viral vectors for expression of genetically encoded calcium indicators (e.g., GCaMP)
- Surgical equipment for stereotaxic surgery and device implantation
- Behavioral apparatus for social interaction, persistent behavior testing, or decision-making tasks
- Computational resources for analyzing high-dimensional neural data
Procedure:
- Animal Preparation: Perform stereotaxic surgery to deliver viral vectors expressing calcium indicators into hormone-sensitive brain regions (e.g., ventromedial hypothalamus, prefrontal cortex, medial amygdala). Allow 3-4 weeks for expression.
- Device Implantation: Implant a gradient-index (GRIN) lens for miniscope recording or optical fibers for photometry above target regions. Secure the device to the skull using dental cement.
- Hormonal State Manipulation: For studies in females, track estrous cycle stages daily via cytology. Alternatively, use ovariectomized animals with controlled hormone replacement (estradiol benzoate, progesterone) to create specific hormonal milieus.
- Neural Recording During Behavior: Acquire neural activity data while animals engage in standardized behavioral assays (e.g., social interaction test, persistent foraging, or decision-making tasks). Synchronize behavioral video with neural recording timestamps.
- Data Processing: Extract calcium transients from raw video data using computational pipelines (e.g., CNMF-E, CALM). Decompose population activity into latent dimensions using dimensionality reduction techniques (PCA, UMAP).
- Population Analysis: Identify neural ensembles that show hormone-dependent coordination. Analyze how population dynamics transition between states during behavior using methods like hidden Markov models.
Expected Outcomes: This protocol typically reveals that high-estrogen states promote more stable neural population dynamics and reduce representational drift, corresponding to increased behavioral persistence [5]. Hormone depletion often results in more variable neural trajectories and less predictable behavioral sequences.
Protocol: Mapping Hormone-Sensitive Functional Connectivity
Objective: To quantify how hormones alter functional connectivity between distributed brain networks.
Materials:
- Animals with hormone manipulations (as above)
- High-density silicon probes or multi-site recording systems
- Tissue processing equipment for immunohistochemical verification
- Computational tools for network analysis (GraphPad, custom MATLAB/Python scripts)
Procedure:
- Simultaneous Multi-region Recording: Implant recording electrodes or optical fibers in 3-5 interconnected, hormone-sensitive brain regions based on anatomical tracing studies.
- Behavioral Paradigm: Record neural activity during quiet rest periods and during specific behaviors across different hormonal states.
- Signal Processing: Calculate cross-correlation or coherence between neural signals from different regions. Compute joint peristimulus time histograms for event-related analysis.
- Network Construction: Create functional connectivity graphs where nodes represent recording sites and edges represent significant correlations in neural activity.
- Graph Theory Analysis: Compute network metrics including modularity, clustering coefficient, and hub strength for different hormonal conditions.
- Statistical Comparison: Use nonparametric tests to determine how hormonal state alters global and local network properties.
Expected Outcomes: Studies using this approach have demonstrated that estrogen increases long-range functional connectivity between prefrontal cortex and subcortical structures, facilitating coordinated social and cognitive processing [5]. These changes in functional architecture underlie hormone-dependent shifts in behavioral state.
Visualization of Systems Neuroendocrinology Frameworks
Hormone-Mediated Neural Persistence Circuit
Multi-Scale Experimental Approach
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Systems Neuroendocrinology
| Reagent/Category | Specific Examples | Function/Application | Experimental Considerations |
|---|---|---|---|
| Genetically Encoded Indicators | GCaMP (calcium), GRAB (neurotransmitters), iGABSnFR (GABA) [5] | Monitoring neural activity and transmission in specific cell populations | Select promoters (e.g., CaMKIIa, GAD) for cell-type specificity; consider kinetics for temporal resolution |
| Chemogenetic Tools | DREADDs (hM3Dq, hM4Di), PSEMs [5] | Remote control of neural activity in hormone-sensitive circuits | Validate receptor expression and functionality; titrate ligand dose for precise temporal control |
| Optogenetic Actuators | Channelrhodopsin (ChR2), Halorhodopsin (NpHR), Archaerhodopsin (Arch) [5] | Precise millisecond-scale control of defined neural populations | Match opsin properties (kinetics, wavelength) to experimental needs; verify expression patterns |
| Hormone Manipulation Tools | Leuprolide acetate (puberty blocker), Histrelin implants, hormone pellets [2] | Controlled manipulation of hormonal states for causal testing | Consider timing, dose, and formulation; verify hormone levels via blood sampling when possible |
| Viral Tracing Vectors | AAVretro, AAV1, Herpes virus, Rabies virus [5] | Mapping connectivity of hormone-sensitive circuits | Select appropriate serotype for retrograde or anterograde tracing; control for tropism and toxicity |
The selection of appropriate research tools is critical for designing rigorous experiments in systems neuroendocrinology. Combining multiple approaches—such as cell-type-specific calcium imaging during hormonal state manipulation—provides the most powerful insights into mechanism. Recent advances in neurotechnology now enable simultaneous monitoring and manipulation of neural activity across distributed networks in freely behaving subjects, finally making it possible to connect hormonal signaling with brain-wide neural dynamics and behavior [5].
Future Directions and Clinical Translation
The integration of systems-level and computational approaches in neuroendocrinology promises to revolutionize our understanding of hormone-brain interactions. Future research must focus on disentangling causal hormone effects from correlative associations, mapping the diversity of hormone receptor expression to neural functioning, and understanding how multiple hormones with different temporal profiles operate synergistically to alter neural computation and behavior [5]. These advances have direct clinical relevance for improving hormonal therapies for contraception, menopause, gender-affirming care, and mood disorders by creating tailored formulations based on a mechanistic understanding of how exogenous hormones impact brain function and emotional states [2] [5]. Furthermore, this research framework provides essential insights into developmental processes, revealing how hormonal signaling during critical periods establishes neural circuit architectures that influence behavior and vulnerability to disease throughout the lifespan [2] [44].
Hormone-Based Therapeutics for Metabolic and Inflammatory Disorders
The intricate interplay between metabolic and inflammatory processes forms the cornerstone of numerous chronic diseases. Hormone-based therapeutics have emerged as a compelling class of pharmaceuticals, offering high target specificity, well-defined physiological activities, and favorable safety profiles [46]. Advances in understanding the biological pathways regulated by hormones have paved the way for developing new medicines that exploit endogenous mechanisms for therapeutic benefit [46]. Approximately 100 hormone-based therapeutic agents have gained approval worldwide, highlighting their established importance in clinical practice [46]. This whitepaper examines recent insights into hormone research during development and functional regulation, with particular focus on their application in metabolic dysfunction-associated steatohepatitis (MASH), obesity, and related inflammatory conditions, providing researchers and drug development professionals with a comprehensive technical overview of this rapidly evolving field.
Established and Emerging Hormone-Based Therapeutics
The therapeutic landscape of hormone-based agents spans both established hormones and novel constructs engineered for enhanced efficacy. Traditional hormones like insulin, calcitonin, and adrenocorticotropic hormone have long been used clinically, initially isolated from natural sources but now predominantly produced as synthetic or recombinant agents to overcome stability and bioavailability challenges [46]. Recent research has expanded this arsenal significantly, particularly for metabolic disorders.
Table 1: Approved Hormone Therapy Medications for Metabolic and Neoplastic Conditions
| Drug Name | Generic Name | Therapeutic Class | Primary Indications |
|---|---|---|---|
| Arimidex | anastrozole | Aromatase inhibitor | Hormone-responsive cancers [47] |
| Aromasin | exemestane | Aromatase inhibitor | Hormone-responsive cancers [47] |
| Zytiga | abiraterone | Androgen biosynthesis inhibitor | Prostate cancer [47] |
| Lupron | leuprolide | GnRH agonist | Hormone-responsive cancers [47] |
| Orgovyx | relugolix | GnRH receptor antagonist | Prostate cancer [47] |
| Semaglutide | semaglutide | GLP-1 receptor agonist | Type 2 diabetes, obesity [48] |
| Tirzepatide | tirzepatide | GLP-1/GIP dual agonist | Type 2 diabetes, obesity [49] |
| Resmetirom | resmetirom | Thyroid hormone receptor-β agonist | MASH [48] |
The field has evolved substantially with the introduction of nutrient-stimulated hormone-based therapies (NuSHs), particularly incretin mimetics that exploit gut-derived hormone effects [48]. This family includes glucagon-like peptide-1 receptor agonists (GLP-1RAs), dual GLP-1/GIP agonists (e.g., tirzepatide), dual GLP-1/glucagon agonists (e.g., survodutide), and triple GLP-1/GIP/glucagon agonists (e.g., retatrutide) [48]. These agents represent a paradigm shift in managing metabolic diseases through pleiotropic mechanisms addressing both metabolic and inflammatory components.
Clinical Efficacy Data for Metabolic Disorders
Substantial clinical evidence supports the efficacy of hormone-based therapeutics in metabolic and inflammatory disorders, with MASH representing a key area of investigation. The table below summarizes quantitative outcomes from recent clinical trials.
Table 2: Clinical Efficacy of Selected Hormone-Based Therapies in Metabolic Disorders
| Therapeutic Agent | Trial Phase | Patient Population | Key Efficacy Outcomes | Statistical Significance |
|---|---|---|---|---|
| Semaglutide (0.4 mg daily) | Phase II [48] | MASH patients (n=320) | 59% achieved MASH resolution without worsening fibrosis vs. 17% with placebo | P < 0.001 |
| Semaglutide (2.4 mg weekly) | Phase III [48] | MASH with fibrosis F2-F3 (n=800) | 62.9% achieved MASH resolution without worsening fibrosis vs. 34.3% with placebo | P < 0.001 (Δ28.7%) |
| Semaglutide (2.4 mg weekly) | Phase III [48] | MASH with fibrosis F2-F3 (n=800) | 36.8% achieved fibrosis improvement without worsening steatohepatitis vs. 22.4% with placebo | P < 0.001 (Δ14.4%) |
| Tirzepatide (5, 10, 15 mg) | Phase II [48] | MASLD with T2DM | 44%, 56%, 62% MASH resolution without fibrosis worsening vs. 10% with placebo | P < 0.001 for all doses |
| Tirzepatide + MHT | Real-world [49] | Postmenopausal women (n=120) | 17% total body weight loss vs. 14% with tirzepatide alone | Superior effectiveness |
| Resmetirom | Phase III [48] | Non-cirrhotic MASH with moderate-to-advanced fibrosis | 25.9-29.9% MASH resolution without fibrosis worsening vs. 9.7% with placebo | P < 0.001 |
Recent combination approaches demonstrate enhanced therapeutic potential. A real-world study of 120 postmenopausal women over a median duration of 18 months revealed that concurrent use of tirzepatide and menopause hormone therapy (MHT) resulted in superior total body weight loss (17%) compared to tirzepatide alone (14%) [49]. Additionally, 45% of MHT users achieved at least 20% total body weight loss, compared to only 18% of non-users [49]. This suggests a broader efficacy trend for pairing these medication classes and highlights the importance of considering hormonal status in therapeutic interventions for metabolic diseases.
Experimental Protocols and Methodologies
Preclinical Assessment of Hormone Therapeutics in MASH Models
Animal Model Selection and Induction: Utilize C57BL/6 mice (8-10 weeks old) maintained on amylin liver NASH (AMLN) diet or Western diet supplemented with high fructose/glucose in drinking water for 16-36 weeks to establish MASH phenotype [48]. Monitor weekly for body weight, food intake, and general health status.
Treatment Administration: Administer test compounds (e.g., GLP-1RAs, dual/triple incretin RAs) via subcutaneous injection at predetermined doses based on prior pharmacokinetic studies. Include vehicle control and positive control groups (e.g., obeticholic acid). Treatment duration typically spans 8-12 weeks.
Endpoint Analysis: Conduct terminal procedures after 4-6 hour fasting. Collect blood via cardiac puncture for serum biochemistry (ALT, AST, glucose, insulin, lipids). Perfuse liver with cold PBS, then excise and weigh. Divide liver lobes for (1) formalin fixation and paraffin embedding for H&E, Sirius Red, and immunohistochemistry; (2) snap-freezing for RNA/protein analysis; (3) fresh-frozen for lipid quantification.
Histopathological Assessment: Apply NAFLD Activity Score (NAS) system by blinded pathologist evaluating steatosis (0-3), lobular inflammation (0-3), and hepatocyte ballooning (0-2). Define MASH resolution as NAS ≤3 with no ballooning. Assess fibrosis using Sirius Red staining with semi-quantitative scoring (0-4) or morphometric analysis.
Clinical Trial Design for MASH Therapeutics
Patient Recruitment: Enroll adults with biopsy-confirmed MASH and fibrosis stages F1-F3, excluding cirrhosis and other liver diseases. Stratify by diabetes status, fibrosis stage, and NAS.
Intervention Protocol: Implement randomized, double-blind, placebo-controlled design with 1:1 or 2:1 randomization. For semaglutide trials, administer once-weekly subcutaneous injections (2.4 mg) for 72 weeks [48]. For resmetirom, utilize oral daily dosing.
Primary Endpoints: Assess MASH resolution without worsening fibrosis OR fibrosis improvement without worsening steatohepatitis, evaluated through paired liver biopsies (baseline and week 72) [48].
Secondary Endpoints: Include changes in NAS components, liver enzyme normalization, non-invasive biomarkers (ELF, FIB-4, liver stiffness by VCTE), glycemic parameters, lipid profiles, and body weight.
Statistical Considerations: Power studies to detect minimum 15-20 percentage point difference in primary endpoints with 80-90% power at α=0.05. Employ modified intention-to-treat analysis.
Signaling Pathways and Mechanisms of Action
Figure 1: Mechanism of Action of Nutrient-Stimulated Hormone-Based Therapeutics
The signaling pathways through which hormone-based therapeutics exert their effects involve complex endocrine networks. Nutrient-stimulated hormone-based therapies (NuSHs) primarily activate GLP-1, GIP, and glucagon receptors, triggering both metabolic and anti-inflammatory effects [48]. The metabolic effects include weight loss through reduced appetite and delayed gastric emptying, improved insulin sensitivity via enhanced glucose-dependent insulin secretion, and reduced liver fat content through increased fatty acid oxidation and reduced lipogenesis [48]. Simultaneously, anti-inflammatory effects manifest as reduced pro-inflammatory cytokines, decreased macrophage retention in adipose tissue, and diminished oxidative stress [48]. These parallel pathways converge to produce therapeutic outcomes including MASH resolution, fibrosis improvement, and reduced risk of hepatocellular carcinoma (HCC).
Beyond incretin-based therapies, other hormonal pathways show therapeutic potential. Dehydroepiandrosterone demonstrates cardioprotective effects through activation of estrogen receptors via the C-Jun N-terminal Kinase pathway, preventing endoplasmic reticulum stress-mediated apoptosis in vascular cells [46]. Oxytocin alleviates testicular dysfunction in rat models by reducing oxidative damage and inflammation in testicular tissue while restoring sperm parameters [46]. Uroguanylin, produced in both the gut and brain, increases brown adipose tissue activity and improves glucose homeostasis in mice, suggesting potential for central administration in type 2 diabetes management [46]. Netrin-1 acts as a pro-inflammatory molecule that retains macrophages in adipose tissue, contributing to obesity-related metabolic dysfunction, while adiponectin exerts opposing beneficial effects [46].
Research Reagent Solutions
Table 3: Essential Research Reagents for Hormone Therapeutic Development
| Reagent Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Cell Lines | Human umbilical vein endothelial cells (HUVECs), human vascular smooth muscle cells, hepatocyte cell lines (HepG2, Huh7) | In vitro mechanistic studies | Model human vascular and hepatic responses to hormone therapies [46] |
| Animal Models | C57BL/6 mice on AMLN or Western diet, lipopolysaccharide-induced inflammation models, db/db mice | Preclinical efficacy assessment | Recapitulate human metabolic-inflammatory disease pathology for therapeutic testing [46] [48] |
| Hormone Assays | GLP-1 ELISA, insulin ELISA, adiponectin ELISA, growth hormone RIA | Biomarker quantification | Precisely measure endogenous and therapeutic hormone levels in biological samples [15] |
| Inflammation Markers | TNF-α, IL-6, IL-1β ELISA kits, multiplex cytokine panels | inflammatory pathway analysis | Quantify inflammatory mediator changes in response to hormone therapies [46] |
| Histopathology Reagents | H&E, Sirius Red, antibodies for macrophages (F4/80), collagen (Col1a1), oxidative stress markers (8-OHdG) | Tissue analysis | Visualize and quantify tissue architecture, fibrosis, inflammation, and cellular stress [48] |
| Molecular Biology Kits | RNA extraction kits, RT-PCR reagents, Western blot materials, chromatin immunoprecipitation kits | Mechanistic studies | Analyze gene expression, protein levels, and epigenetic modifications in response to treatments [48] |
The research toolkit for investigating hormone-based therapeutics requires specialized reagents that reflect the complex pathophysiology of metabolic and inflammatory disorders. Primary cells including human umbilical vein endothelial cells and vascular smooth muscle cells enable investigation of vascular effects, as demonstrated in studies of dehydroepiandrosterone's cardioprotective mechanisms [46]. Established hepatocyte cell lines (HepG2, Huh7) provide platforms for screening hepatic responses. Animal models, particularly C57BL/6 mice fed specialized diets (AMLN, Western diet), effectively recapitulate human MASH pathology for preclinical testing [48]. Lipopolysaccharide-induced inflammation models enable study of acute inflammatory responses, as utilized in oxytocin testicular protection studies [46]. Analytical tools include comprehensive hormone assays for quantifying therapeutic and endogenous hormone levels, with inflammation markers essential for evaluating treatment effects on cytokine networks. Histopathology reagents remain indispensable for assessing tissue-level changes, while molecular biology kits enable mechanistic investigation of signaling pathways.
Hormone-based therapeutics represent a rapidly advancing frontier in managing metabolic and inflammatory disorders, with nutrient-stimulated hormones offering particularly promising avenues. The efficacy of GLP-1 receptor agonists, dual and triple incretin receptor agonists, and their combinations with other endocrine therapies demonstrates the power of targeting endogenous hormonal pathways for therapeutic benefit. Future research directions should focus on elucidating the precise immunometabolic mechanisms underlying these therapeutic effects, optimizing combination approaches, and validating long-term outcomes including hepatocellular carcinoma prevention. As our understanding of hormonal regulation during development and in disease states deepens, so too will opportunities to develop increasingly targeted and effective interventions for these complex disorders.
Gene Therapy and Bispecific Antibodies as Novel Hormonal Treatments
The field of endocrinology is undergoing a transformative shift with the integration of sophisticated biotechnological platforms. Gene therapy and bispecific antibodies, while historically prominent in oncology, are emerging as powerful modalities for addressing complex hormonal disorders. This evolution aligns with the broader thesis of recent research into hormonal regulation during development, which emphasizes the intricate network of signaling pathways and feedback mechanisms that govern growth, metabolism, and reproduction [50] [13]. The traditional view of hormone replacement therapy (HRT) is being supplanted by a new paradigm focused on precision medicine, aiming to restore physiological regulation with unprecedented specificity and durability [51].
The therapeutic rationale for these novel approaches stems from the limitations of conventional hormonal treatments, which often require chronic administration, face challenges with bioavailability, and may produce suboptimal pharmacokinetic profiles. Gene therapy offers the potential for sustained, endogenous production of therapeutic hormones, while bispecific antibodies provide a means to simultaneously engage multiple components of hormonal signaling pathways, thereby achieving synergistic effects that are unattainable with monoclonal antibodies or small molecules [52] [53]. This review provides an in-depth technical analysis of these platforms, detailing their mechanisms, experimental support, and practical application in preclinical and clinical development for hormonal disorders.
Bispecific Antibodies for Hormonal Signaling Modulation
Fundamental Concepts and Engineering Strategies
Bispecific antibodies (BsAbs) are synthetic macromolecules engineered to recognize two distinct epitopes, either on the same antigen or on different antigens. This dual-targeting capability enables novel mechanisms of action that extend beyond the simple additive effects of co-administered monoclonal antibodies [52]. From a structural perspective, BsAbs are broadly classified into two categories:
- IgG-like formats (with Fc region): These constructs retain the crystallizable fragment (Fc) domain, which confers longer serum half-life through FcRn-mediated recycling, increased stability, and the potential to engage Fc-mediated effector functions such as antibody-dependent cellular cytotoxicity (ADCC) and phagocytosis (ADCP) [52].
- Non-IgG-like formats (without Fc region): This category includes smaller constructs like bispecific T-cell engagers (BiTEs) and tandem scFv. Their compact size typically results in enhanced tissue penetration and reduced immunogenicity, though often at the cost of a shorter plasma half-life [52].
The engineering of BsAbs requires sophisticated protein design strategies to ensure proper heavy and light chain pairing. Key technologies include the "knobs-into-holes" approach for facilitating heterodimerization, cross-over dual-variable domain immunoglobulins, and various fragment-based platforms that avoid chain mispairing issues [52].
Functional Mechanisms in Hormonal Pathways
BsAbs exert their therapeutic effects in hormonal disorders through several sophisticated mechanisms:
- Ligand sequestration and receptor antagonism: A single BsAb can simultaneously bind and neutralize two different soluble ligands (e.g., cytokines) or block two distinct receptor signaling pathways. This approach is particularly valuable in complex inflammatory endocrine disorders where multiple pathogenic factors are involved [54].
- Targeted receptor activation: BsAbs can be designed to function as receptor agonists by crosslinking two identical or different receptors, thereby initiating downstream signaling cascades with greater specificity than natural ligands [52].
- Precision redirection of immune cells: Although more common in oncology, this approach has applications in autoimmune endocrine diseases, where BsAbs can redirect regulatory T cells to pathogenic immune cell populations, thereby restoring immune tolerance [52] [53].
Table 1: Clinically Advanced Bispecific Antibodies for Non-Oncology Hormonal/Inflammatory Indications
| Candidate Name | Targets | Indication(s) | Development Phase | Key Mechanism |
|---|---|---|---|---|
| Sonelokimab [54] | IL-17A, IL-17F | Hidradenitis Suppurativa, Psoriatic Arthritis | Phase III | Neutralizes multiple IL-17 homodimers and heterodimers |
| Lutikizumab [54] | IL-1α, IL-1β | Hidradenitis Suppurativa, Atopic Dermatitis, Ulcerative Colitis | Phase III | Dual inhibition of IL-1 isoforms |
| PRV-3279 [54] | CD32B, CD79B | Systemic Lupus Erythematosus (SLE) | Phase IIa | B-cell modulation without depletion |
| MEDI-7352 [54] | NGF, TNFR2 | Painful Diabetic Neuropathy, Osteoarthritis | Phase II | Dual targeting of pain and inflammatory pathways |
| AZD1163 [54] | PAD2, PAD4 | Rheumatoid Arthritis | Phase I | Simultaneous inhibition of peptidylarginine deiminases |
Experimental Protocols for Bispecific Antibody Characterization
In Vitro Affinity and Binding Kinetics Assessment
Surface Plasmon Resonance (SPR) Protocol:
- Sensor chip preparation: Immobilize recombinant target antigens (e.g., hormone receptors or cytokines) on CMS sensor chips using standard amine coupling chemistry to achieve approximately 5,000-10,000 response units.
- Kinetic measurements: Perform binding kinetics using a Biacore T200 or comparable instrument. Dilute bispecific antibody samples in HBS-EP+ buffer (10 mM HEPES, 150 mM NaCl, 3 mM EDTA, 0.05% v/v Surfactant P20, pH 7.4) and inject over immobilized antigens at concentrations ranging from 0.78 nM to 100 nM with a flow rate of 30 μL/min.
- Data analysis: Calculate association rate (ka), dissociation rate (kd), and equilibrium dissociation constant (KD) using a 1:1 binding model with double referencing. Confirm simultaneous binding to both targets through sandwich assays [52].
Functional Characterization in Cell-Based Assays
Ligand Blockade Bioassay Protocol:
- Cell line preparation: Utilize hormone-responsive reporter cell lines (e.g., HEK293 cells stably transfected with pathway-specific response elements linked to luciferase or SEAP).
- Neutralization assay: Pre-incubate BsAbs (serial dilutions from 10 μg/mL to 0.01 μg/mL) with target ligands for 1 hour at 37°C before adding to cells. Include reference standards and appropriate controls.
- Response measurement: After 24-48 hours incubation, quantify reporter gene expression. Calculate IC50 values using four-parameter logistic regression [54].
Gene Therapy Strategies for Hormonal Regulation
Vector Platforms and Delivery Considerations
Gene therapy represents a paradigm shift in hormonal disorder treatment by enabling the body to produce its own therapeutic proteins, potentially offering permanent correction or long-term management with a single intervention. The primary vector systems include:
- Adeno-associated virus (AAV) vectors: The leading platform for endocrine gene therapy due to their excellent safety profile, long-term transgene expression, and serotype diversity that enables tissue-specific targeting. AAV-mediated gene transfer is being investigated for growth hormone deficiencies, diabetes insipidus, and various metabolic disorders [55].
- Lentiviral vectors: These integrate into the host genome, providing stable transgene expression in dividing cells. Their application is particularly relevant for ex vivo modification of endocrine progenitor cells.
- Non-viral approaches: Nanoparticle-based DNA delivery systems are emerging as alternatives to viral vectors, offering potentially lower immunogenicity and greater payload capacity, though with currently lower transduction efficiency.
Tissue-specific targeting is paramount for hormonal gene therapy. The liver serves as an ideal ectopic endocrine organ due to its high vascularization and protein secretion capacity. For hormones requiring regulated secretion (e.g., insulin), strategies employing glucose-responsive promoters or engineered receptors that respond to small molecule inducers are under development.
Promising Clinical Applications and Candidates
Several gene therapy approaches for hormonal disorders have advanced to clinical development:
- Growth hormone deficiency: AAV vectors encoding human growth hormone (hGH) under the control of tissue-specific promoters are being evaluated to eliminate the need for daily injections in pediatric patients [51].
- Hemophilia A: While not traditionally classified as a hormonal disorder, the success of gene therapy for hemophilia A using AAV vectors represents a proof-of-concept for protein replacement in the endocrine space. Roche's next-generation AAV gene therapy candidate SPK-8011QQ has demonstrated significantly enhanced haemostatic potency in preclinical models compared with earlier versions [55].
- Diabetes mellitus: Multiple approaches are in development, including AAV-mediated expression of glucokinase activators for glycogen storage diseases, and engineered gene circuits for glucose-responsive insulin production [51].
Table 2: Gene Therapy Candidates for Hormone-Related Disorders
| Candidate/Platform | Target Indication | Vector Type | Key Features | Development Status |
|---|---|---|---|---|
| SPK-8011QQ [55] | Hemophilia A | AAV | Enhanced FVIII expression; improved hemostatic potency | Preclinical (Phase IIb planned for 2026) |
| AAV-hGH [51] | Growth Hormone Deficiency | AAV | Liver-directed expression; potential one-time treatment | Preclinical |
| Lenti-GCG [51] | Alpha-1 Antitrypsin Deficiency | Lentiviral | Ex vivo transduction of hepatocytes | Phase I/II |
Experimental Protocols for Hormonal Gene Therapy Development
Vector Potency and Efficacy Assessment
In Vivo Efficacy Study Protocol:
- Animal models: Utilize hormone-deficient rodent models (e.g., hypophysectomized rats for GH deficiency, Brattleboro rats for diabetes insipidus).
- Dosing and administration: Administer AAV vectors via appropriate route (intravenous, intramuscular, or direct intraglandular injection) with dose escalation (e.g., 1×1011 to 1×1013 vg/kg). Include empty vector and naive controls.
- Monitoring and endpoints: Measure circulating hormone levels weekly via ELISA. Assess physiological and behavioral parameters (growth curves, water consumption). Conduct terminal studies at 3-6 months to evaluate transgene expression by qPCR and immunohistochemistry [51].
Biodistribution and Safety Evaluation
Comprehensive Toxicology Study Protocol:
- Study design: Utilize relevant animal species (mice, non-human primates) with sample sizes sufficient for statistical power (n=8-10 per group).
- Biodistribution analysis: Extract genomic DNA from tissues (liver, spleen, gonads, brain, etc.) and quantify vector genomes per μg DNA using qPCR with primers against the transgene.
- Immune monitoring: Measure neutralizing antibodies against the vector capsid and transgene product. Assess T-cell responses via ELISpot for IFN-γ secretion [55].
Integrated Signaling Pathways in Hormonal Regulation
The following diagram illustrates the molecular interplay between bispecific antibodies and gene therapy in modulating key hormonal signaling pathways:
Diagram Title: Integrated Hormonal Modulation Mechanisms
This integrated pathway illustrates how gene therapy introduces a sustainable source of therapeutic hormones, while bispecific antibodies provide precise regulation of receptor-ligand interactions, together achieving synergistic restoration of hormonal homeostasis.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Developing Novel Hormonal Therapies
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Expression Vectors | AAV serotypes (1-9), Lentiviral packaging systems, Tissue-specific promoters | Gene therapy construct development | Select serotype based on tropism for target endocrine tissue |
| Cell-based Assay Systems | Hormone-responsive reporter cells (Luc/SEAP), Primary endocrine cells, Organoid cultures | Functional characterization of BsAbs and transgene products | Validate responsiveness to native ligands; use relevant induction parameters |
| Analytical Tools | Surface Plasmon Resonance (SPR), HPLC-SEC, LC-MS for hormone quantification, ELISA kits | Characterization of binding kinetics and hormone levels | Establish reference standards for accurate quantification |
| Animal Models | Hormone-deficient models (hypophysectomized, Brattleboro), Humanized receptor models, Disease-specific transgenic mice | In vivo efficacy and safety evaluation | Monitor developmental stages as hormone effects are age-dependent [50] |
| Cytokine/Chemokine Panels | Multiplex immunoassays (Luminex), Electrochemiluminescence platforms (Meso Scale Discovery) | Immune monitoring and cytokine storm assessment | Critical for evaluating CRS with T-cell engaging BsAbs |
| Gene Editing Tools | CRISPR-Cas9 systems, Base editors, Prime editors | Creating disease models and potential therapeutic applications | Enables precise modeling of monogenic endocrine disorders |
The convergence of gene therapy and bispecific antibody platforms represents a watershed moment in molecular endocrinology. These technologies offer unprecedented opportunities to address the complex regulatory networks that govern hormonal homeostasis during development and throughout the lifespan [50] [56]. The continued refinement of delivery vectors, protein engineering strategies, and targeting approaches promises to yield increasingly sophisticated therapeutics capable of restoring endocrine function with minimal intervention.
Future directions in this field will likely focus on achieving even greater specificity through conditional gene expression systems, engineering bispecifics with integrated sensing capabilities, and developing combination approaches that leverage the strengths of both modalities. Furthermore, the application of artificial intelligence and machine learning in protein design and vector optimization will accelerate the development timeline for these complex therapeutics [57]. As our understanding of hormonal regulation during development continues to evolve [13] [56], these advanced technological platforms will enable researchers to translate fundamental biological insights into transformative treatments for patients with hormonal disorders.
Addressing Research and Clinical Challenges in Hormone Biology
Overcoming Sex-Based Disparities in Drug Metabolism and Efficacy
The historical focus on male physiology as the default in biomedical research has led to significant sex-based disparities in drug safety and efficacy. For decades, women of reproductive age were systematically excluded from clinical trials under the pretext of safeguarding them and their offspring, a practice that marginalized women's health and left critical knowledge gaps in pharmacology [58]. This review synthesizes recent insights from endocrinology and developmental biology to elucidate the hormonal mechanisms underlying these disparities and provides a technical framework for integrating sex as a biological variable in drug development. The consequences of this neglect are profound: a significant number of prescription drugs withdrawn from the market were removed due to greater adverse effects in women than in men [58]. Understanding the hormonal regulation of metabolic pathways and physiological functions is essential for developing safer, more effective therapeutics for all populations.
Historical Context and Consequences of Exclusion
The systematic exclusion of women from clinical trials has created substantial gaps in pharmacological knowledge and clinical practice. This approach, often trivialized as "bikini medicine," narrowly focused on anatomical differences while ignoring more meaningful health distinctions [58]. Although international guidelines eventually mandated women's inclusion in clinical trials, implementation faced significant challenges—many researchers failed to adhere to these guidelines or neglected to analyze results by sex, undermining policy effectiveness [58].
The real-world consequences of this exclusion are starkly evident in drug safety profiles:
- Drug Withdrawals: An analysis revealed that eight of the ten drugs removed from the market between 1997 and 2000 posed greater risks to women than men [58].
- Adverse Drug Reactions: Women experience nearly twice as many adverse drug reactions (ADRs) across all drug classes and are disproportionately hospitalized due to these reactions [58].
- Delayed Dosing Adjustments: The FDA reduced the recommended dosage of zolpidem for women by half in 2013—21 years after its initial approval—after data revealed higher risks of excessive sedation and impaired driving due to slower metabolic clearance in women [58].
Table 1: Examples of Drugs with Sex-Based Differences in Pharmacokinetics and Adverse Events
| Drug | Sex-Based Difference | Clinical Consequence | Regulatory Action |
|---|---|---|---|
| Zolpidem | 35% lower clearance rates in women; higher morning blood levels [58] | Increased risk of excessive sedation and impaired driving [58] | FDA reduced recommended dose for women by half in 2013 [58] |
| Ambien | Higher blood levels in women due to slower metabolic clearance [58] | Greater risks of adverse effects [58] | Dose adjustment for women after post-market surveillance [58] |
| Multiple withdrawn drugs | Greater adverse effects in women across multiple drug classes [58] | Increased hospitalizations and safety risks [58] | Market withdrawal [58] |
Biological Basis of Sex Differences in Drug Metabolism
Key Physiological Factors Creating Sex-Based Disparities
Biological differences between males and females significantly impact how drugs are processed in the body (pharmacokinetics) and how they produce effects (pharmacodynamics). These differences extend beyond reproductive hormones to fundamental physiological processes:
- Body Composition: Women generally have lower body weight and higher body fat percentage (affecting drug distribution and storage) [58]
- Gastrointestinal Physiology: Slower gastric emptying in women can alter drug absorption rates [58]
- Renal Function: Reduced renal clearance in women leads to slower elimination of drugs cleared by the kidneys [58]
- Hormonal Fluctuations: Menstrual cycle, pregnancy, and menopause create dynamic changes in drug metabolism [58]
A comprehensive study of 86 drugs found that 76 had higher pharmacokinetic values in women, predicting sex-specific adverse drug reactions in 88% of cases [58]. This suggests standard dosing practices often result in women being overmedicated, particularly for drugs with narrow therapeutic indices where the difference between therapeutic and toxic doses is small [58].
Molecular Mechanisms: Hepatic Enzyme Sexual Dimorphism
Sex differences in pharmacokinetics primarily reflect underlying differences in the expression of hepatic enzymes active in drug metabolism, including cytochromes P450 (P450s), sulfotransferases, glutathione transferases, and UDP-glucuronosyltransferases [59]. Research in rodent models has identified more than 1,000 genes with sex-dependent expression patterns that impart substantial sexual dimorphism to liver metabolic function and pathophysiology [59].
The primary regulator of this sexual dimorphism is the temporal pattern of plasma growth hormone (GH) release by the pituitary gland, which shows significant sex differences:
- Male Pattern: Highly pulsatile (intermittent) GH release in male animals [59]
- Female Pattern: More frequent (nearly continuous) GH release in female animals [59]
These differential GH patterns activate distinct cellular signaling pathways that regulate hepatic gene expression. The GH-activated transcription factor STAT5b, along with hepatic nuclear factor HNF4α, serve as essential mediators of the sex-dependent effects of GH on liver function [59].
Diagram 1: Hormonal regulation of hepatic enzyme expression
Hormonal Influences on Neurological Function and Drug Response
Beyond metabolic pathways, sex hormones significantly influence neurological function and cognitive processes through complex interactions with neurotransmitter systems. Recent research has illuminated how estrogen regulates dopamine activity in the brain's reward center, creating natural fluctuations in learning capabilities across the female reproductive cycle [60].
Experiments with laboratory rats demonstrated that:
- Estrogen boosts dopamine activity, strengthening "reward" signals that guide learning [60]
- Learning capabilities were enhanced when estrogen levels were increased [60]
- When estrogen activity was suppressed, learning capabilities diminished [60]
These findings have profound implications for neuropsychiatric disorders, which show significant symptom fluctuations across hormonal states [60]. The connection between hormonal regulation and neurotransmitter systems represents a critical dimension of sex-specific drug responses, particularly for psychotropic medications.
Experimental Models and Methodologies
In Vitro Cervical Mucus Model for Contraceptive Research
The development of non-hormonal contraceptives requires sophisticated models that account for female reproductive biology. Oregon Health & Science University researchers have created a novel lab model using cervical cells from rhesus macaques (which have a cervix similar to humans) to study how changes in cervical mucus during the menstrual cycle regulate fertility [61].
Experimental Protocol:
- Cell Culture: Cervical columnar epithelial cells are cultured in laboratory conditions [61]
- Hormonal Treatment: Cells are treated with estrogen or progesterone to simulate different menstrual cycle phases [61]
- RNA Sequencing: Genetic activity in cultured endocervical cells is analyzed to identify genes and pathways regulating mucus production [61]
- Target Identification: Researchers identified approximately 150-250 different genes that were substantially different under varying hormonal conditions, representing potential drug targets [61]
This model has revealed how hormones influence the synthesis of mucins (large proteins that give mucus its gel-like consistency), hydration of mucus, and stabilization of mucus structure [61]. During ovulation, high estrogen levels make mucus thinner and less viscous, creating a "slip-and-slide for sperm to enter," while progesterone thickens mucus after ovulation to prevent sperm entry [61].
Diagram 2: In vitro cervical mucus model workflow
Neuroendocrine Circuit Mapping for Hormone-Sleep Interactions
Advanced circuit tracing techniques have elucidated the complex relationship between sleep architecture and hormone regulation. UC Berkeley researchers have mapped the neuroendocrine circuits that control growth hormone release during sleep, providing insights relevant to sex-based differences in drug metabolism [15].
Methodology:
- Electrode Implantation: Researchers inserted electrodes into specific brain regions of mice, including the hypothalamus and locus coeruleus [15]
- Neural Stimulation: Hypothalamic neurons were stimulated with light (optogenetics) while measuring changes in activity [15]
- Circuit Tracing: State-of-the-art techniques mapped connections between GHRH neurons, somatostatin neurons, and the locus coeruleus [15]
- Hormone Measurement: Growth hormone levels were correlated with neural activity across sleep-wake cycles [15]
This research revealed that growth hormone not only builds muscle and bone but also regulates brain arousal through feedback mechanisms involving the locus coeruleus [15]. This intricate balance between sleep and hormone regulation has implications for understanding sex differences in metabolic disorders and optimizing dosing schedules for sex-specific therapeutics.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Investigating Sex-Based Differences in Drug Metabolism
| Reagent/Model | Function/Application | Research Context |
|---|---|---|
| Primary Cervical Epithelial Cells [61] | Study mucosal barriers and drug delivery; model hormonal regulation of fertility [61] | Non-hormonal contraceptive development [61] |
| Rhesus Macaque Model [61] | Preclinical research on reproductive physiology and hormone dynamics [61] | Cervical mucus studies and reproductive health [61] |
| GHRNA Sequencing Platforms [61] | Transcriptomic analysis of hormone-responsive genes [61] | Identification of drug targets in cervical cells [61] |
| Optogenetic Tools [15] | Precise neural circuit manipulation to study sleep-hormone relationships [15] | Mapping neuroendocrine pathways controlling growth hormone release [15] |
| Electrode Arrays for in vivo Recording [15] | Direct neural activity measurement during sleep-wake cycles [15] | Correlating hormone fluctuations with brain states [15] |
| STAT5b and HNF4α Assays [59] | Analysis of key transcription factors in hepatic sexual dimorphism [59] | Mechanistic studies of sex-dependent drug metabolism [59] |
Data Analysis and Visualization in Sex-Based Pharmacology
Effective analysis and visualization of sex-specific data are essential for identifying meaningful differences in drug responses. Quantitative comparisons between groups should include both graphical representations and numerical summaries to fully characterize sex-based variations [62].
Recommended Analytical Approaches:
- Back-to-Back Stemplots: Effective for comparing two groups with small datasets; preserves original data values [62]
- 2-D Dot Charts: Ideal for small to moderate amounts of data; allows comparison across multiple groups [62]
- Boxplots: Optimal for most comparisons; displays five-number summary (minimum, Q1, median, Q3, maximum) and identifies outliers [62]
Numerical Summary Requirements:
- Summarize data separately for each sex group [62]
- Compute differences between means and/or medians [62]
- Report standard deviations and sample sizes for each group [62]
Table 3: Comparative Analysis of Gorilla Chest-Beating Rates by Age - Example of Sex-Neutral Comparative Data Structure
| Age Group | Mean Rate (beats/10h) | Standard Deviation | Sample Size (n) | Median | IQR |
|---|---|---|---|---|---|
| Younger (<20 years) | 2.22 | 1.270 | 14 | 1.70 | ~1.50 |
| Older (≥20 years) | 0.91 | 1.131 | 11 | 0.60 | ~1.00 |
| Difference | 1.31 | - | - | 1.10 | - |
This tabular format, adapted from comparative physiological studies [62], provides a template for presenting sex-stratified pharmacological data with appropriate measures of central tendency and variability.
Overcoming sex-based disparities in drug metabolism and efficacy requires a fundamental shift in research paradigms that integrates hormonal context throughout the drug development pipeline. The historical neglect of sex differences has created dangerous knowledge gaps that continue to impact women's health outcomes. By adopting the experimental frameworks and methodological approaches outlined in this review, researchers can advance toward truly personalized medicine that accounts for the dynamic interplay between hormones, metabolic pathways, and drug responses.
Future progress depends on:
- Implementing vigilant, sex-stratified analysis in all clinical trials [58]
- Developing more sophisticated in vitro models that replicate sex-specific physiological conditions [61]
- Elucidating the molecular mechanisms by which sex hormones regulate drug-metabolizing enzymes [59]
- Recognizing the complex interactions between endocrine systems, neurological function, and pharmacological responses [60] [15]
As the field of sex-based biology matures, embracing these comprehensive approaches will be essential for developing safer, more effective therapeutics that address the unique physiological needs of all patients.
Navigating the Complexities of Hormone Pulses and Receptor Desensitization
Hormonal communication is a fundamental biological process governed by dynamic, pulsatile release patterns and sophisticated receptor-level adaptations. The hypothalamic-pituitary-gonadal (HPG) axis serves as a paradigmatic model for understanding these complex interactions, where gonadotropin-releasing hormone (GnRH) pulses dictate the secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the anterior pituitary [63]. These pulsatile signals are not merely rhythmic occurrences but represent a precise biological language that regulates development, reproduction, and metabolic functions. Receptor desensitization emerges as a critical regulatory mechanism wherein sustained exposure to hormone agonists leads to diminished cellular responses, providing an essential feedback mechanism that prevents overstimulation of hormonal pathways [63]. Recent research has revealed that synthetic GnRH analogs, such as Triptorelin, exhibit increased stability and prolonged receptor interaction compared to endogenous GnRH, making them valuable tools for probing the temporal dynamics of hormone signaling and feedback inhibition [63]. Understanding these mechanisms provides crucial insights for therapeutic interventions in endocrine disorders, cancer treatments, and developmental biology.
The complexity of hormonal signaling is further amplified by natural variability in pulse patterns across individuals and physiological states. Quantitative studies have demonstrated significant variability in reproductive hormone levels due to pulsatile secretion, diurnal rhythms, and metabolic influences [10]. Luteinizing hormone displays the highest variability (coefficient of variation: 28%), followed by sex-steroid hormones (testosterone: 12%; estradiol: 13%), while follicle-stimulating hormone is the least variable (CV: 8%) [10]. This inherent biological variability, combined with receptor-level plasticity, creates a sophisticated regulatory system that responds dynamically to developmental stages, environmental cues, and pathological conditions. The following sections explore the quantitative dimensions of hormone pulses, experimental approaches for investigating receptor dynamics, and the molecular mechanisms underlying desensitization processes.
Quantitative Analysis of Hormone Pulse Variability
Temporal Patterns and Biological Variability
Hormonal pulsatility exhibits distinct temporal patterns that are often overlooked in clinical assessments relying on single measurements. Detailed hormonal sampling reveals that initial morning values of reproductive hormones are typically higher than daily mean values, with luteinizing hormone showing an 18.4% decrease from morning measure to daily mean, follicle-stimulating hormone decreasing by 9.7%, testosterone by 9.2%, and estradiol by 2.1% [10]. These diurnal patterns interact with pulsatile secretion to create a complex hormonal landscape that requires sophisticated analytical approaches for accurate interpretation. In healthy men, testosterone levels fall between 9:00 AM and 5:00 PM by 14.9% (95% CI 4.2, 25.5%), though morning levels correlate with late afternoon levels in the same individual (r² = 0.53), enabling prediction of daily profiles from single measurements [10].
Table 1: Variability Patterns of Key Reproductive Hormones
| Hormone | Coefficient of Variation (CV) | Diurnal Decrease (Morning to Daily Mean) | Key Regulatory Influences |
|---|---|---|---|
| Luteinizing Hormone (LH) | 28% | 18.4% | GnRH pulse frequency, steroid hormone feedback, kisspeptin signaling |
| Follicle-Stimulating Hormone (FSH) | 8% | 9.7% | GnRH pulse frequency, inhibin, activin, follistatin |
| Testosterone | 12% | 9.2% | LH pulsatility, nutrient intake (34.3% decrease after mixed meal) |
| Estradiol | 13% | 2.1% | FSH activity, aromatase expression, ovarian follicle development |
Nutrient intake significantly modulates hormonal pulsatility, particularly for sex steroids. Testosterone levels demonstrate differential suppression based on feeding patterns, with a marked 34.3% decrease after a mixed meal compared to a 9.5% decrease during ad libitum feeding, a 6.0% decrease after an oral glucose load, and a 7.4% decrease after an intravenous glucose load [10]. These findings highlight the importance of standardizing sampling conditions when assessing hormonal status and designing experimental protocols that account for metabolic influences on endocrine axes.
Age-Dependent Changes in Hormonal Rhythms
Hormonal pulse patterns undergo significant modifications throughout the lifespan, reflecting developmental transitions and adaptive physiological changes. Research utilizing remote hormone monitoring platforms has revealed that follicular phase length declines with age while luteal phase length increases, demonstrating age-specific dynamics in cycle phase lengths [24]. These developmental shifts in hormonal pulsatility have profound implications for reproductive function, metabolic regulation, and age-related pathological processes. The ability to pinpoint cycle phase and cycle day with 95% confidence using age, first cycle day, and current hormone levels represents a significant advancement in personalized endocrine assessment [24].
Table 2: Age-Related Changes in Menstrual Cycle Characteristics
| Age Group | Follicular Phase Trend | Luteal Phase Trend | Clinical Implications |
|---|---|---|---|
| Younger Women (<30) | Longer duration | Shorter duration | Extended window for follicular development |
| Mid-Reproductive (30-34) | Intermediate duration | Intermediate duration | Balanced phase lengths |
| Older Women (>35) | Shorter duration | Longer duration | Compressed follicular recruitment, extended progesterone exposure |
The quantification of hormonal variability and its age-dependent modifications provides a foundation for understanding receptor-level adaptations. As hormonal pulse patterns evolve across the lifespan, receptor systems must dynamically adjust their sensitivity and response characteristics to maintain physiological homeostasis. This interplay between secretory dynamics and receptor plasticity forms the basis for the complex regulation of endocrine axes.
Experimental Models for Investigating Receptor Desensitization
GnRH Agonist Models and Protocol Design
Triptorelin, a synthetic decapeptide analog of GnRH, serves as a premier experimental tool for investigating receptor desensitization mechanisms. This potent GnRH receptor agonist demonstrates structural modifications that enhance receptor affinity and confer resistance to enzymatic degradation, making it ideal for long-term experimental protocols studying receptor desensitization [63]. The experimental utility of Triptorelin stems from its biphasic mechanism of action: an initial surge in gonadotropin secretion followed by receptor downregulation and suppression of LH and FSH release upon sustained exposure [63]. This dual-phase response provides a robust model system for dissecting the temporal dynamics of hormone signaling and feedback inhibition.
Protocol 1: Assessing GnRH Receptor Desensitization Using Triptorelin
- Cell Culture Preparation: Utilize pituitary-derived cell lines (e.g., LβT2 murine gonadotrope cells or primary pituitary cultures) maintained in appropriate media supplemented with 10% fetal bovine serum under standard culture conditions (37°C, 5% CO₂).
- Receptor Stimulation Phase: Treat cells with Triptorelin at concentrations ranging from 1-100 nM for initial characterization. For desensitization studies, use a concentration of 10 nM for varying durations (0-24 hours) to establish temporal patterns of receptor response.
- Calcium Flux Measurement: Monitor intracellular calcium mobilization using fluorometric imaging plate reader (FLIPR) systems with calcium-sensitive dyes (e.g., Fluo-4 AM) following acute Triptorelin challenge after pre-treatment periods.
- cAMP Quantification: Assess cAMP accumulation using ELISA or BRET-based biosensors at multiple timepoints following Triptorelin exposure to characterize G-protein coupling efficiency.
- Receptor Trafficking Analysis: Employ confocal microscopy with GFP-tagged GnRH receptors or immunofluorescence staining with specific antibodies to visualize receptor internalization and recycling dynamics.
- Transcriptional Downstream Effects: Quantify mRNA expression of gonadotropin subunits (LHB, FSHB) and immediate early genes (EGR1, C-FOS) using quantitative RT-PCR following various Triptorelin exposure protocols.
GHRH Receptor Splice Variant Analysis
The growth hormone-releasing hormone (GHRH) receptor system presents another compelling model for investigating receptor-level complexity in hormonal signaling. Alternative splicing generates multiple GHRH receptor variants (SV1-SV4), with splice variant 1 (SV1) demonstrating the greatest similarity to the full-length pituitary GHRH receptor and retaining functionality by eliciting cAMP signaling and mitogenic activity upon GHRH stimulation [64]. These splice variants display distinct tissue distribution patterns, with SV1 expression documented in diverse human cancers including endometrial carcinoma, prostate carcinoma, glioblastoma, and colorectal cancer [64].
Protocol 2: Characterization of GHRH Receptor Splice Variants
- Tissue Sample Preparation: Obtain human tumor specimens or appropriate cell lines (e.g., prostate cancer lines for SV1 studies) with institutional ethical approval. Prepare membrane fractions for binding assays or whole cell extracts for signaling studies.
- Radioligand Binding Assays: Utilize [¹²⁵I]-labeled GHRH analogs to assess receptor binding characteristics in membrane preparations. Perform competitive displacement experiments with unlabeled GHRH agonists and antagonists to determine binding affinities (Kd values).
- cAMP Signaling Profiling: Measure cAMP accumulation in response to GHRH(1-29)NH₂ (the biologically active fragment) and specific GHRH antagonists using ELISA-based detection systems.
- Gene Expression Quantification: Employ quantitative RT-PCR with splice variant-specific primers to determine the relative expression of GHRH receptor isoforms across different tissues and pathological conditions.
- Proliferation Assays: Assess mitogenic responses using [³H]-thymidine incorporation or MTT assays in cells expressing specific GHRH receptor variants following stimulation with GHRH analogs.
- Localization Studies: Conduct immunofluorescence microscopy with variant-specific antibodies to determine subcellular distribution of GHRH receptor splice variants under basal and stimulated conditions.
The investigation of receptor splice variants reveals remarkable plasticity in hormonal signaling systems, with SV1 expression patterns correlating with clinical outcomes in specific cancer types. Well-differentiated colorectal carcinomas and nonmetastatic tumors show stronger SV1 expression compared to poorly differentiated tumors and those with liver metastasis, suggesting a potential role in tumor differentiation [64]. These findings highlight the importance of receptor-level diversity in modulating hormonal responses across different physiological and pathological contexts.
Molecular Mechanisms of Receptor Desensitization
Signaling Pathways and Downstream Effects
The molecular architecture of receptor desensitization involves sophisticated mechanisms that operate at multiple levels of the signaling cascade. For GnRH receptors, prolonged engagement with agonists like Triptorelin induces conformational changes that alter G-protein coupling and second messenger activation [63]. This process involves differential activation of key signaling pathways, including MAPK, PKC, and calcium-calmodulin cascades, depending on receptor density and cellular context [63]. The desensitization process represents a dynamic adaptation that fine-tunes hormonal responses and prevents excessive stimulation that could lead to pathological outcomes.
The following diagram illustrates the core signaling pathways and desensitization mechanisms of GnRH receptors:
Diagram 1: GnRH Receptor Signaling and Desensitization Pathways. The pathway illustrates agonist-induced activation (yellow/blue) leading to downstream signaling (green) and subsequent desensitization mechanisms (red).
GHRH receptor signaling demonstrates parallel complexity, with receptor activation triggering cAMP-dependent pathways through Gs protein coupling that ultimately regulate growth hormone synthesis and release [64]. The presence of functionally distinct receptor splice variants adds additional layers of regulation, with SV1 maintaining the ability to activate cAMP signaling and mitogenic pathways despite structural differences from the full-length pituitary receptor [64]. This structural and functional diversity enables tissue-specific modulation of hormonal responses and creates multiple potential points for regulatory intervention.
Epigenetic and Developmental Considerations
Receptor desensitization mechanisms are not static but evolve throughout development and are influenced by epigenetic modifications. Research suggests that transient hormonal alterations during critical developmental windows can induce long-term changes in gene expression, chromatin structure, and cellular differentiation [63]. These developmental programming effects may permanently alter the set point for receptor sensitivity and desensitization kinetics, creating a biological memory of early hormonal exposures that shapes physiological responses throughout the lifespan.
The interaction between hormonal signaling and developmental transitions represents a fundamental biological phenomenon observed across diverse organisms. These transitions involve coordinated changes at multiple biological scales, from biochemical pathways to whole-organism physiology, and are typically regulated by molecular signaling pathways and genetic networks that respond to both internal and external cues [65]. Understanding how receptor desensitization mechanisms are integrated into these developmental programs provides crucial insights into the plasticity of endocrine systems and their ability to adapt to changing physiological demands.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Hormone Pulse and Desensitization Studies
| Reagent/Material | Function/Application | Example Specifications |
|---|---|---|
| Triptorelin | Synthetic GnRH agonist for inducing and studying receptor desensitization; exhibits increased receptor affinity and enzymatic stability [63] | Water-soluble lyophilized powder, ≥95% purity, working concentrations: 1-100 nM for in vitro studies |
| GHRH(1-29)NH₂ | Biologically active fragment of GHRH for receptor activation studies; contains full biological activity in N-terminal sequence [64] | Lyophilized powder, ≥98% purity, reconstituted in sterile PBS with 0.1% BSA |
| Phospho-Specific Antibodies | Detection of activated signaling intermediates in MAPK, PKC, and calcium-calmodulin pathways [63] | Validated for Western blot, immunofluorescence; specific for phosphorylated epitopes |
| cAMP BRET Biosensors | Real-time monitoring of cAMP dynamics in live cells; essential for assessing G-protein coupling efficiency [64] | Genetically encoded biosensors (e.g., EPAC-based), compatible with standard plate readers |
| Calcium-Sensitive Dyes | Monitoring intracellular calcium flux following receptor activation; indicator of initial signaling response [63] | Fluo-4 AM, Fura-2 AM; suitable for fluorometric imaging plate reader (FLIPR) systems |
| Splice Variant-Specific Primers | Quantitative assessment of receptor isoform expression; critical for evaluating GHRH-R SV1 and other variants [64] | Designed to span unique splice junctions, validated with positive control samples |
Advanced research in hormonal pulsatility and receptor desensitization increasingly relies on sophisticated monitoring platforms that enable precise quantification of hormone dynamics. Remote hormone testing systems that quantitatively track luteinizing hormone and pregnanediol-3-glucuronide through urine tests analyzed by AI-powered algorithms represent cutting-edge tools for capturing hormonal variability in natural physiological settings [24]. These systems incorporate nanotechnology that adjusts for pH, normalizes hydration levels, and filters out non-specific binding, providing researchers with unprecedented access to hormonal pulse patterns outside controlled laboratory environments [24].
The integration of these research tools with classical pharmacological approaches creates a powerful framework for dissecting the complexities of hormone pulses and receptor desensitization. As these methodologies continue to evolve, they promise to reveal new dimensions of endocrine regulation with significant implications for therapeutic development across a spectrum of physiological and pathological conditions.
Optimizing Models for Hormonal Disorders and Inter-Organ Communication
The study of endocrinology is undergoing a transformative shift from examining hormonal pathways in isolation to understanding them as components of a complex, system-wide network. Inter-organ communication (IOC) has emerged as a critical framework for deciphering how hormones mediate crosstalk between tissues to maintain metabolic homeostasis and how these processes deteriorate during aging and disease [66]. Concurrently, advances in machine learning (ML) and mathematical modeling are providing unprecedented capabilities to analyze the nonlinear dynamics and feedback mechanisms inherent in endocrine systems [67] [68]. This whitepaper provides a technical guide to cutting-edge methodologies for modeling hormonal disorders and IOC, focusing on applications for researchers and drug development professionals. It synthesizes recent insights from systems endocrinology, detailing core principles, quantitative benchmarks, experimental protocols, and computational tools essential for developing robust, clinically actionable models.
Core Principles of Inter-Organ Communication in Endocrinology
The endocrine system functions as a distributed network, with communication occurring through multiple parallel channels. Understanding these mechanisms is foundational to building accurate physiological models.
Hormonal Signaling from Non-Traditional Endocrine Organs: Organs traditionally not classified as endocrine tissues, including adipose tissue, skeletal muscle, and bone, secrete hormones with profound systemic effects [66]. Adipose tissue releases adipokines like leptin and eNAMPT, the latter being encapsulated into extracellular vesicles (EVs) and transported to remote tissues such as the hypothalamus and pancreas to enhance NAD+ biosynthesis and counteract aging [66]. Skeletal muscle secretes myokines (e.g., IL-6, irisin, FGF21) during contraction that regulate glucose disposal, stimulate white adipose tissue browning, and exert neuroprotective effects [66]. Bone-derived factors like osteocalcin modulate insulin secretion and sensitivity, illustrating a sophisticated endocrine loop between bone and metabolic tissues [66].
Circulating Metabolites and Lipokines: Circulating metabolites serve as real-time indicators of metabolic status and active signaling molecules. For instance, supplementation of alpha-ketoglutarate (α-KG), a TCA cycle intermediate, extends lifespan and reduces systemic inflammation in aged mice [66]. Similarly, mono-unsaturated fatty acids (MUFAs) function as lipokines, with dietary intake sufficient to extend lifespan in model organisms [66].
Neuronal Regulation by the Hypothalamus: The hypothalamus acts as a high-order control center, integrating peripheral signals to regulate aging and longevity. Specific neuronal subpopulations, such as those in the dorsomedial hypothalamus (DMH), can delay aging by stimulating the secretion of factors like eNAMPT from adipose tissue [66].
Machine Learning Applications in Endocrine Disorder Modeling
ML is revolutionizing the diagnosis, classification, and treatment of endocrine disorders by extracting subtle patterns from large, multimodal datasets. The table below summarizes key quantitative performance data from recent ML applications in endocrinology.
Table 1: Performance Metrics of Machine Learning Models in Endocrinology
| Target Disorder | ML Application | Key Performance Metrics | Algorithm/Model Name |
|---|---|---|---|
| Thyroid Nodule Malignancy [67] | Differentiating malignant from benign nodules | Reduced unnecessary fine needle aspirations by 27% | ThyNet (Deep Learning) |
| Thyroid Nodule Classification [67] | Nodule detection & classification | Outperformed radiologists in sensitivity, specificity, and accuracy | Multi-scale Convolutional Neural Network |
| Papillary Thyroid Carcinoma [67] | Predicting BRAFV600E mutations from US elastography | Significant differences in echogenicity, diameter ratios, and elasticity | Unspecified ML Model |
| Medullary Thyroid Carcinoma [67] | Ki67 proliferation index counting | Correlated with disease-specific survival; reliability comparable to eyeballing | Unspecified ML Algorithm |
| Central Precocious Puberty [69] | Predicting treatment outcome (Final Height - Target Height) | Weighted Mean Difference (WMD) = 1.01 cm (CI: 0.28 to 1.73) | Meta-analysis of clinical data |
ML workflows in endocrinology follow a structured pipeline: problem definition, data collection and preprocessing, model selection, and evaluation [67]. The choice of ML technique is guided by the specific clinical question and data structure.
- Supervised Learning is extensively used for classification tasks, such as detecting acromegaly from facial photographs or thyroid nodule malignancy from ultrasonography images [67].
- Unsupervised Learning helps identify novel disease subgroups, such as distinct clusters of diabetes patients, which can inform personalized treatment strategies [67].
- Reinforcement Learning is being explored for optimizing dynamic treatment regimens, such as insulin dosing, by learning through continuous interaction with patient-specific data [67].
A significant challenge in clinical implementation is the "black-box" nature of many complex models. Ensuring model transparency, addressing data imbalance, and achieving seamless integration into clinical workflow are active areas of research essential for building trust and facilitating adoption [67].
Mathematical Modeling of Endocrine-Neural Interactions
The bidirectional communication between the endocrine and nervous systems presents a complex modeling challenge due to differing timescales and strong nonlinearities. A novel framework for this integrates the Hormone Interaction Dynamics Network (HIDN) with the Adaptive Hormonal Regulation Strategy (AHRS) [68].
- Hormone Interaction Dynamics Network (HIDN): This component is a graph-based neural architecture with recurrent dynamics designed to encapsulate the spatio-temporal interdependencies among endocrine glands, hormones, and EEG signal fluctuations. It models the influence of hormones like cortisol and melatonin on neural oscillations and vice versa [68].
- Adaptive Hormonal Regulation Strategy (AHRS): This component dynamically optimizes therapeutic interventions using real-time feedback and patient-specific parameters. It ensures the model adapts to individual variability and external perturbations, bridging the gap between computational prediction and clinical application [68].
Table 2: Experimental Protocol for Hybrid Endocrine-EEG Modeling
| Protocol Step | Technical Description | Purpose |
|---|---|---|
| Data Acquisition | Simultaneous collection of high-density EEG and serial hormone level measurements (e.g., cortisol, melatonin) via immunoassays. | To capture synchronized temporal data on neural activity and hormonal fluctuations. |
| Signal Preprocessing | Application of time-frequency analysis (e.g., Wavelet Transforms) and Independent Component Analysis (ICA) to EEG data. | To extract clean neural oscillatory features (alpha, theta power) and remove artifacts. |
| Model Training & Validation | Implementation of HIDN using a graph neural network framework; training on a task like emotion recognition. | To validate the model's ability to predict hormonal dynamics from EEG features and vice versa. |
| Intervention Simulation | Employing AHRS to simulate personalized therapeutic interventions based on the model's output. | To test and optimize potential treatment strategies in silico before clinical application. |
Figure 1: IOC Signaling Pathways. The diagram illustrates the complex bidirectional communication between the central nervous system, classic endocrine glands, and peripheral tissues via hormones, metabolites, and extracellular vesicles.
Emerging Technologies and Market Landscape
Technological advancements are enabling unprecedented access to continuous hormonal data, which in turn fuels the development of more sophisticated models.
Table 3: Continuous Hormone Monitoring Market & Technologies
| Attribute | Value/Ranking | Notes and Key Players |
|---|---|---|
| Market Value (2025) | USD 325.7 Million | Projected to reach USD 716.2 Million by 2035 (CAGR 8.2%) [8]. |
| Leading Sample Type (2025) | Urine (81% Share) | Non-invasive collection ideal for at-home testing; key players: Abbott, Roche [8]. |
| Leading Application (2025) | Fertility (65% Share) | High demand for ovulation tracking; key players: Mira, Fertility Friend [8]. |
| Leading Sales Channel (2025) | Direct-to-Customer (62.7%) | Driven by consumer demand for convenience and privacy; key players: Everlywell, Modern Fertility [8]. |
| Representative Technologies | Wearable Patches (Level Zero Health), Smartphone Analyzers (Eli Health's Hormometer) | New devices use DNA-based sensors and saliva-based testing for cortisol, progesterone, etc. [8]. |
The integration of AI-powered solutions with these monitoring devices is a key growth driver, enabling real-time analysis and personalized feedback. However, the market faces challenges related to regulatory hurdles for medical device approval and significant data privacy concerns regarding sensitive health information [8].
The Scientist's Toolkit: Research Reagent Solutions
Implementing the experimental protocols for IOC and hormonal disorder research requires a specific set of reagents and tools. The following table details essential materials and their functions.
Table 4: Essential Research Reagents and Materials
| Reagent/Material | Function in Experimental Protocol |
|---|---|
| High-Density EEG System | Acquisition of neural oscillatory data with high temporal resolution for correlation with hormonal pulses [68]. |
| Hormone-Specific Immunoassay Kits | Quantitative measurement of hormone levels (e.g., cortisol, melatonin, IGF-1) from serum, saliva, or urine samples [69] [68]. |
| Extracellular Vesicle (EV) Isolation Kit | Purification of EVs from plasma or cell culture media to study their role in mediating inter-organ signaling [66]. |
| Graph Neural Network (GNN) Framework | Computational backbone for building Hormone Interaction Dynamics Networks (HIDN) to model complex endocrine interactions [68]. |
| DNA-based Biosensors | Key component in advanced continuous monitoring wearables for real-time, non-invasive tracking of specific hormones [8]. |
Figure 2: ML Development Workflow. The standard machine learning workflow in endocrine research, from problem definition to clinical implementation.
The optimization of models for hormonal disorders and inter-organ communication represents a frontier in systems endocrinology. The convergence of high-resolution continuous monitoring technologies, sophisticated mathematical frameworks like HIDN and AHRS, and powerful machine learning algorithms is creating unprecedented opportunities for breakthroughs in both basic research and therapeutic development. Future progress hinges on interdisciplinary collaboration among endocrinologists, computational biologists, and clinical practitioners to overcome challenges related to model interpretability, data privacy, and clinical integration. By adopting the tools and methodologies outlined in this guide, researchers can accelerate the development of personalized, predictive, and effective interventions for a wide spectrum of endocrine-related diseases.
Strategies for Improving Stability and Bioavailability of Hormone Therapies
Hormone therapies constitute a critical class of pharmaceuticals for treating developmental disorders, metabolic conditions, and age-related hormonal deficiencies. The therapeutic efficacy of these biological agents is fundamentally governed by their structural stability and bioavailability, which present significant challenges due to the inherent physicochemical properties of protein- and peptide-based hormones. Recent advances in our understanding of hormonal regulation during development have highlighted the precision with which endocrine signaling occurs naturally, providing valuable insights for designing more effective therapeutic strategies [2]. This technical guide synthesizes contemporary approaches to overcoming stability and bioavailability limitations in hormone therapeutics, with particular emphasis on their application in developmental endocrinology research.
The intricate role of hormones in development—from fetal growth through puberty and adulthood—requires sophisticated delivery systems that can mimic physiological patterns of hormone release [2] [70]. Hormones such as growth hormone (GH), insulin-like growth factors (IGFs), thyroid hormone, and sex steroids each present unique formulation challenges that must be addressed through multidisciplinary approaches spanning pharmaceutical technology, molecular biology, and materials science. This whitepaper examines the current landscape of stabilization technologies and bioavailability enhancement strategies, providing researchers with experimental protocols and analytical frameworks for advancing hormone-based therapeutics.
Stability Challenges and Stabilization Strategies
Fundamental Stability Challenges
Protein-based hormone therapeutics face numerous stability challenges throughout their lifecycle from manufacturing to administration. These instabilities can be broadly categorized as physical instability (unfolding, aggregation, adsorption) and chemical instability (oxidation, deamidation, hydrolysis) [71]. The structural integrity of these molecules is marginal at best, with most hormones maintaining native conformation only within limited ranges of temperature, pH, and ionic strength [71].
Temperature-induced denaturation represents a particularly significant challenge, as both elevated and sub-zero temperatures can trigger unfolding and aggregation processes. Research has demonstrated that even the robust ribonuclease A enzyme precipitates at -22°C, while serum albumin suffers damage at freezing temperatures [71]. For hormone therapies, this necessitates strict cold chain requirements that complicate distribution and increase costs. The relationship between temperature and protein stability follows a characteristic curve where the maximum free energy of folding (ΔGunfolding) occurs within a narrow temperature range, beyond which instability rapidly increases [71].
Surface-induced denaturation presents another major challenge, with interactions at air-liquid and solid-liquid interfaces promoting structural changes. The hydrophobic domains of hormones, typically buried within the native structure, become exposed during these interactions and drive aggregation through hydrophobic interactions [71]. This is particularly problematic for monoclonal antibodies and antibody-drug conjugates, where complementarity-determining regions must maintain precise conformation for biological activity [71].
Advanced Stabilization Methodologies
Stabilizing Excipients and Formulation Approaches
The strategic use of stabilizing excipients represents the frontline approach for enhancing hormone stability. Tris(hydroxymethyl)aminomethane (Tris) has emerged as a particularly effective stabilizer for human growth hormone (hGH) in aqueous solutions [72]. Experimental studies demonstrate that Tris at optimal concentrations (0.05-0.09 M) significantly enhances hGH stability through molecular interactions with specific amino acid residues including tyrosine (Tyr), proline (Pro), glutamic acid (Glu), aspartic acid (Asp), leucine (Leu), and phenylalanine (Phe) [72].
The mechanism of Tris stabilization involves the formation of hydrogen bonds between its hydroxyl groups and polar residues in the hGH structure, effectively protecting against chemical degradation and physical aggregation [72]. Molecular docking studies confirm that Tris binds specifically within hGH binding pockets, with the binding distance between donors and acceptors and hydrogen bond interactions contributing to the stabilization effect [72]. This approach reduces the need for lyophilization and enables the development of stable liquid formulations for sustained-release delivery systems.
Other effective stabilizers include sugars, polyols, amino acids, and surfactants, which act through various mechanisms including preferential exclusion, surface tension modulation, and free radical scavenging [71]. The selection of appropriate stabilizers must be guided by comprehensive compatibility studies and molecular analysis of interaction mechanisms.
Table 1: Stabilizing Excipients for Hormone Therapeutics
| Excipient Class | Representative Agents | Mechanism of Action | Application Examples |
|---|---|---|---|
| Biological Buffers | Tris, Histidine | pH maintenance, direct protein interaction | hGH stabilization in solution [72] |
| Sugars and Polyols | Sucrose, Trehalose, Sorbitol | Preferential exclusion, water replacement | Lyophilized formulations |
| Surfactants | Polysorbate 80, Poloxamer | Interface protection, reduction of aggregation | Injectable formulations [71] |
| Amino Acids | Glycine, Arginine, Proline | Ionic interaction, surface coating | Liquid and solid formulations |
| Antioxidants | Methionine, Ascorbic Acid | Free radical scavenging, oxidation prevention | Oxidatively sensitive hormones |
Protein Engineering and Modification Strategies
Genetic engineering and site-directed mutagenesis offer powerful approaches to enhancing intrinsic hormone stability. By identifying and modifying unstable regions in the protein structure, researchers can develop analogs with improved resistance to temperature, pH, and proteolytic degradation [71]. For instance, strategic mutations in growth hormone have been shown to increase thermal stability while maintaining biological activity.
Fusion technologies represent another innovative approach, with hormones conjugated to inert carrier proteins such as human serum albumin or Fc fragments to extend circulatory half-life [71]. These fusion strategies leverage the natural recycling mechanisms of the carrier proteins to reduce clearance rates and maintain therapeutic levels. For antibody-based hormone therapeutics, Fc engineering has proven particularly valuable for optimizing pharmacokinetic profiles.
Pegylation—the covalent attachment of polyethylene glycol chains—remains a widely used method for enhancing stability and extending half-life through increased hydrodynamic radius and reduced renal clearance. Recent advances in site-specific pegylation have addressed concerns about biological activity preservation while maintaining stability benefits.
Bioavailability Enhancement Strategies
Barriers to Hormone Bioavailability
The bioavailability of hormone therapies is limited by multiple physiological barriers that must be overcome for effective systemic delivery. For oral administration, these barriers include acidic gastric environment, enzymatic degradation in the gastrointestinal tract, the epithelial membrane of the intestinal mucosa, and presystemic metabolism in the gut wall and liver [73]. The lipid bilayer structure of biological membranes preferentially allows transcellular permeation of lipophilic molecules, while restricting larger, hydrophilic compounds like most protein and peptide hormones [73].
Efflux transporters, particularly P-glycoprotein (P-gp), actively pump drug molecules from enterocytes back into the intestinal lumen, significantly reducing absorption efficiency [74]. This 170 kDa ATP-dependent transmembrane protein belongs to the ABC transporter superfamily and exhibits broad substrate specificity [73]. Simultaneously, cytochrome P450 enzymes (especially CYP3A4) in the intestinal epithelium and liver mediate extensive presystemic metabolism of many hormone therapeutics [73].
For non-oral routes, additional barriers include the mucociliary clearance in nasal administration, salivary washout in buccal delivery, and alveolar macrophage clearance in pulmonary routes [73]. Each delivery pathway presents unique challenges that require tailored bioavailability enhancement strategies.
Bioavailability Enhancement Approaches
Permeation Enhancement Technologies
Permeation enhancers improve hormone absorption by modifying membrane fluidity, opening tight junctions, or inhibiting efflux transporters. Natural bioenhancers of herbal origin have gained significant attention for their multifunctional actions and favorable safety profiles [74] [73].
Piperine, the active compound from black pepper (Piper nigrum) and long pepper (Piper longum), represents one of the most extensively studied bioenhancers. It increases bioavailability of co-administered drugs by 30%-200% through multiple mechanisms including [74]:
- Inhibition of drug-metabolizing enzymes (UDP-glucuronyltransferase, CYP450)
- Modulation of gastrointestinal membrane dynamics
- Stimulation of gut amino acid transporters
- Inhibition of P-glycoprotein efflux pumps
Other effective natural bioenhancers include quercetin, genistein, naringin, and glycyrrhizin, each with distinct mechanisms targeting different absorption barriers [74]. The selection of appropriate enhancers must consider the specific physicochemical properties of the hormone and the targeted delivery route.
Table 2: Bioavailability Enhancers for Hormone Therapies
| Bioenhancer | Natural Source | Mechanism of Action | Impact on Bioavailability |
|---|---|---|---|
| Piperine | Black pepper, Long pepper | Enzyme inhibition, P-gp inhibition, membrane modification | 30%-200% increase for various drugs [74] |
| Quercetin | Various fruits, vegetables | Tight junction modulation, enzyme inhibition | Enhanced absorption of poorly permeable drugs |
| Chitosan | Crustacean shells | Mucoadhesion, tight junction opening | 2-5 fold increase for peptide drugs [73] |
| Aloe vera | Aloe plant | Intercellular membrane modulation | Enhanced didanosine absorption [73] |
| Bile Salts | Animal bile | Micelle formation, membrane fluidization | Variable enhancement dependent on formulation |
Advanced Delivery Systems
Innovative drug delivery technologies have revolutionized hormone therapy by providing controlled release profiles and enhanced absorption. Advanced delivery methods in hormone therapy include transdermal patches with enhanced adhesion, microneedle patches for painless penetration, subcutaneous pellets for sustained release, and intranasal sprays for rapid absorption [75].
Transdermal delivery systems have evolved significantly, with modern patches incorporating penetration enhancers and controlled-release membranes to maintain stable hormone levels. These systems bypass first-pass metabolism and provide steady-state delivery that mimics physiological patterns [75]. For hormone therapies requiring pulsatile release, microneedle technologies offer precise control over delivery kinetics.
Subcutaneous pellets represent another innovative approach for long-term hormone delivery. These small, sterile implants are inserted under the skin and provide continuous hormone release over several months, significantly improving patient compliance for chronic conditions [75]. The development of biodegradable pellet materials has eliminated the need for surgical removal after depletion.
Nanoparticulate systems including liposomes, polymeric nanoparticles, and solid lipid nanoparticles have shown remarkable potential for enhancing hormone bioavailability. These systems protect therapeutic molecules from degradation, facilitate transport across biological barriers, and can be functionalized with targeting ligands for tissue-specific delivery [74]. The modular design of nanocarriers allows simultaneous incorporation of multiple active agents and bioavailability enhancers.
Experimental Protocols and Methodologies
Hormone Stability Assessment Protocol
Comprehensive stability evaluation requires a multifaceted approach employing orthogonal analytical techniques. The following protocol outlines key methodologies for assessing hormone stability under pharmaceutically relevant conditions:
Sample Preparation:
- Prepare hormone solutions (1 mg/mL) in appropriate buffers (e.g., phosphate buffer 0.05 M, pH 7.4)
- Include stabilizers at varying concentrations (e.g., Tris 0.01-0.09 M)
- Divide samples for incubation under different stress conditions (5±2°C, 37±1°C)
Analytical Methods:
- High-Performance Liquid Chromatography (HPLC)
- Use C4 column (4 mm×25 cm, 5 μm, 300 Å) at 45°C
- Mobile phase: 71% Tris buffer (0.05 M, pH=7.5) and 29% n-propyl alcohol
- Flow rate: 0.5 mL/minute
- Monitor degradation peaks and retention time shifts [72]
Enzyme-Linked Immunosorbent Assay (ELISA)
- Use specific antibody pairs for target hormone
- Measure absorbance at 450 nm
- Quantify immunoreactive hormone concentration [72]
Dynamic Light Scattering (DLS)
- Measure hydrodynamic size distribution
- Monitor aggregation formation over time
- Use turbidity tests as complementary assessment [72]
UV Spectrophotometry
- Scan spectrum from 200-350 nm
- Detect structural changes through spectral shifts
- Reference standard solutions for comparison [72]
Computational Analysis:
- Perform molecular docking studies to predict stabilizer-hormone interactions
- Use AutoDock 4.2 with Lamarckian genetic algorithm
- Analyze binding conformations and interaction energies [72]
Bioavailability Enhancement Evaluation
In Vitro Permeation Studies:
- Use Franz diffusion cells with appropriate membrane (e.g., Caco-2 monolayers, porcine intestinal mucosa)
- Prepare hormone formulations with and without bioenhancers
- Sample receptor compartment at predetermined time points
- Analyze samples using HPLC or LC-MS/MS
- Calculate apparent permeability coefficients (Papp) [73]
Efflux Transporter Inhibition Assay:
- Culture Caco-2 cells until fully differentiated (21 days)
- Measure bidirectional transport (apical-to-basal and basal-to-apical)
- Calculate efflux ratio with and without inhibitors
- Specific P-gp substrates (e.g., digoxin) can be used as positive controls [73]
Enzyme Inhibition Studies:
- Prepare human liver microsomes or recombinant CYP enzymes
- Incubate with hormone substrate and NADPH regeneration system
- Include bioenhancer at test concentrations
- Quantify metabolite formation using LC-MS/MS
- Calculate IC50 values for enzyme inhibition [74]
In Vivo Pharmacokinetic Studies:
- Administer hormone formulations to appropriate animal models
- Collect serial blood samples over time course
- Process plasma samples and analyze hormone concentrations
- Calculate pharmacokinetic parameters (Cmax, Tmax, AUC, t½)
- Compare relative bioavailability between formulations [74]
Visualization of Experimental Workflows
Hormone Stability Assessment Workflow
Bioavailability Enhancement Mechanisms
The Scientist's Toolkit: Essential Research Reagents
Table 3: Research Reagent Solutions for Hormone Stabilization and Bioavailability Studies
| Reagent/Category | Function/Application | Specific Examples | Key Characteristics |
|---|---|---|---|
| Stabilizing Buffers | Maintain pH, direct protein interaction | Tris, Phosphate, Histidine buffers | Biocompatibility, hydrogen bonding capacity [72] |
| Chromatographic Media | Separation and analysis of hormones | C4 columns for HPLC, Size exclusion columns | High resolution, recovery of native conformation |
| Detection Systems | Quantification of hormones | ELISA kits, UV-Vis spectrophotometers | Sensitivity, specificity for target hormone [72] |
| Cell Culture Models | Permeability assessment | Caco-2 cells, MDCK cells | Expression of relevant transporters and enzymes |
| Molecular Modeling Software | Prediction of stabilizer interactions | AutoDock, PyMOL | Accurate docking simulations, visualization [72] |
| Natural Bioenhancers | Bioavailability enhancement | Piperine, Quercetin, Chitosan | Multi-mechanistic action, natural origin [74] [73] |
| Permeation Assay Systems | In vitro absorption studies | Franz diffusion cells, Transwell systems | Physiological relevance, reproducibility |
The field of hormone therapy stabilization and bioavailability enhancement continues to evolve rapidly, driven by advances in pharmaceutical technology and growing understanding of endocrine system function throughout development. The integration of computational modeling with empirical formulation science represents a particularly promising direction, enabling rational design of stable hormone formulations rather than reliance on trial-and-error approaches [72].
Future developments will likely focus on personalized hormone therapies tailored to individual metabolic profiles and genetic polymorphisms in drug-processing enzymes [75]. The emergence of precision pharmacology in endocrinology acknowledges the substantial inter-individual variability in treatment response, necessitating biomarker-guided approaches to therapy optimization [76]. Additionally, novel delivery systems incorporating responsive release mechanisms that adapt to physiological signals will better mimic natural hormone patterns, potentially improving therapeutic outcomes while reducing side effects.
The continuing elucidation of hormonal regulation during development provides invaluable insights for designing more sophisticated therapeutic strategies [2] [70]. As our understanding of endocrine axes matures, so too will our ability to create hormone therapies that restore physiological function with unprecedented precision. Through the strategic integration of stabilization technologies, bioavailability enhancement approaches, and developmental endocrinology principles, researchers can overcome the formidable challenges inherent in hormone-based therapeutics, ultimately improving outcomes for patients across the lifespan.
Addressing Technical Challenges in Recording Neural-Hormonal Interactions
The intricate interplay between the nervous and endocrine systems represents a fundamental frontier in physiological research, governing processes from memory formation to metabolic control. The core technical challenge in this field lies in capturing data from these two systems simultaneously, despite their vastly different operating timescales and spatial domains. Hormonal signaling occurs on a scale of seconds to days and can be distributed throughout the entire organism, whereas neural communication happens in milliseconds within highly localized circuits. This guide synthesizes recent methodological advances that are bridging this divide, providing a framework for researchers to design robust experiments that can accurately record and interpret neural-hormonal interactions within the context of modern developmental and functional regulation research.
Core Technical Challenges and Innovative Solutions
Overcoming the obstacles in recording neural-hormonal data requires a multi-faceted approach. The table below summarizes the primary challenges and the contemporary solutions being deployed in cutting-edge research.
Table 1: Key Technical Challenges and Corresponding Modern Solutions
| Technical Challenge | Impact on Data Quality | Emerging Technical Solutions |
|---|---|---|
| Temporal Resolution Disparity | Fast neural signals are missed or misaligned with slow hormonal fluctuations. | Two-photon laser scanning microscopy of live animals across multiple cycles [77]. |
| Spatial Resolution and Localization | Inability to pinpoint exact sites of hormone-neural interaction. | Spatial transcriptomics to map hormone receptor expression and local signaling [78]. |
| System Complexity & Interdependence | Difficulty isolating cause-effect relationships within feedback loops. | Computational modeling and simulation (e.g., with STEPS, MCell) to test hypotheses in silico [79]. |
| Data Integration and Analysis | Inability to correlate multi-modal, multi-scale datasets (e.g., imaging, omics, behavior). | Advanced quantitative analysis (e.g., regression, time-series, cluster analysis) to find patterns in complex data [80] [81] [82]. |
Detailed Experimental Protocols for Key Research Areas
Protocol: In Vivo Imaging of Hormone-Driven Neural Plasticity
This protocol, adapted from recent work on the estrous cycle, details the methodology for visualizing structural and functional neural changes in response to hormonal fluctuations in live animals [77].
A. Animal Model and Cycle Staging
- Use adult female mice (e.g., C57BL/6J).
- Stage the estrous cycle daily via vaginal cytology for at least two full 4-day cycles before imaging. Key stages are proestrus (high estradiol) and estrus (low estradiol).
B. Surgical Procedure: Cranial Window Implantation
- Anesthetize the mouse and secure it in a stereotaxic frame.
- Perform a craniotomy (e.g., 3-mm diameter) over the target brain region (e.g., hippocampus).
- Implant a custom-made glass cranial window, sealing it with dental acrylic to create a stable optical portal for chronic imaging.
C. In Vivo Two-Photon Microscopy
- Use a two-photon laser scanning microscope fitted with a tunable infrared laser.
- Inject a fluorescent dye (e.g., a cell-permeant Ca²⁺ indicator or a structural label like a GFP-variant) to visualize neurons.
- Image the same dendritic segments and neuronal cell bodies repeatedly over multiple estrous cycles. For spine dynamics, capture high-resolution z-stacks. For functional imaging, record calcium transients during defined behaviors or in response to stimuli.
D. Data Analysis
- Structural Analysis: Quantify dendritic spine density (spines/µm) from maximum intensity projections. Compare density across cycle stages using ANOVA.
- Functional Analysis: Analyze calcium transient kinetics (frequency, amplitude) and backpropagation signals in dendrites. Correlate with the animal's hormonal state.
- Place Cell Analysis: In a virtual reality environment, record from hippocampal place cells. Measure the reliability and specificity of place field maps across different hormonal stages.
Diagram 1: In vivo plasticity study workflow.
Protocol: Spatial Mapping of Hormone Receptor Expression
This protocol leverages spatial transcriptomics to map the expression of hormone receptors and their downstream targets within the complex architecture of neural tissue [78].
A. Tissue Preparation
- Perfuse-fix the brain with RNase-free fixative (e.g., 4% PFA).
- Dissect the region of interest (e.g., hippocampus, hypothalamus) and embed it in OCT compound.
- Cryosection the tissue at a defined thickness (e.g., 10-20 µm) and mount on specialized slides compatible with spatial transcriptomics.
B. Spatial Transcriptomics Library Preparation
- Permeabilize the tissue to release mRNA.
- Hybridize the mRNA to barcoded oligonucleotides on the slide surface. Each barcode corresponds to a specific spatial location (spot diameter ~50-100 µm).
- Perform reverse transcription to create cDNA libraries with spatial barcodes.
- Harvest the cDNA and prepare libraries for next-generation sequencing.
C. Sequencing and Bioinformatic Analysis
- Sequence the libraries on a high-throughput platform (e.g., Illumina).
- Map the sequenced reads to a reference genome and assign them to spatial locations using the barcodes.
- Use computational pipelines to identify clusters of spots with similar gene expression profiles and overlay this with hormone receptor gene expression (e.g., estrogen receptor alpha, progesterone receptor).
Diagram 2: Spatial transcriptomics protocol.
Quantitative Data Analysis Methods
The complex, multi-modal datasets generated in this field demand robust quantitative analysis methods. The table below outlines essential techniques.
Table 2: Essential Quantitative Data Analysis Methods for Neural-Hormonal Research [80] [81] [82]
| Analysis Method | Primary Function | Application Example in Neural-Hormonal Research |
|---|---|---|
| Time Series Analysis | Model temporal patterns and relationships over time. | Analyzing cyclical changes in dendritic spine density or place cell reliability across a 4-day estrous cycle [77]. |
| Regression Analysis | Model and predict the relationship between dependent and independent variables. | Predicting changes in neuronal firing rate (dependent) based on serum estradiol levels and dendritic spine count (independent variables). |
| Cluster Analysis | Identify natural groupings or subtypes within a dataset without pre-defined categories. | Discovering novel subtypes of hormone-sensitive neurons from single-cell RNA sequencing data [78]. |
| Cohort Analysis | Track the behavior of specific groups (cohorts) over time. | Comparing the longitudinal trajectory of neural plasticity in a cohort of animals with high vs. low cortisol response. |
| Factor Analysis | Reduce data dimensionality to identify latent, unobserved variables. | Identifying latent physiological states (e.g., "stress susceptibility") from correlated measures of hormone levels, neural activity, and behavior. |
The Scientist's Toolkit: Research Reagent Solutions
Successful experimentation relies on a suite of reliable reagents and tools. The following table details key items for studying neural-hormonal interactions.
Table 3: Essential Research Reagents and Tools for Neural-Hormonal Research
| Item | Function / Description | Example Application |
|---|---|---|
| Two-Photon Microscope | High-resolution, deep-tissue imaging of neural structure and function in live animals. | Chronic imaging of dendritic spine dynamics in the hippocampus of behaving mice across hormone cycles [77]. |
| Spatial Transcriptomics Kit (e.g., 10x Genomics Visium) | Enables genome-wide mRNA sequencing with spatial context from tissue sections. | Mapping the co-expression of estrogen receptors with synaptic markers in specific hippocampal sublayers [78]. |
| Hormone Assay Kits (ELISA, RIA, MS) | Precisely quantify hormone concentrations (e.g., estradiol, cortisol) from serum or tissue extracts. | Correlating serum estradiol levels with observed neural changes during the estrous cycle [77]. |
| Neurolucida Software | 3D reconstruction and morphological analysis of neurons from microscopic images. | Quantifying changes in dendritic arborization and spine density following hormonal manipulation. |
| NEST / NEURON Simulator | Simulates electrical activity and plasticity in networks of neurons. | Building in silico models to test how hormonal modulation of ion channels affects network-level output [79]. |
| c-Fos Antibodies | Immunohistochemical marker for recently activated neurons. | Identifying neural populations activated by a specific hormonal pulse or stressful stimulus. |
Visualization of a Key Signaling Pathway
The following diagram illustrates a simplified estrogen-dependent signaling pathway that modulates synaptic plasticity, a core interaction in neural-hormonal research.
Diagram 3: Estrogen signaling in synaptic plasticity.
Validating Mechanisms and Cross-Species Comparative Endocrinology
Validating Novel Hormone Functions in Disease Models
The validation of novel hormone functions represents a critical pillar in understanding the intricate physiology of development, aging, and disease pathogenesis. Hormones, as primary signaling molecules, regulate a vast array of biological processes, and dysregulation of their pathways is implicated in numerous conditions from cancer to metabolic disorders. Contemporary research has moved beyond merely characterizing hormone levels to elucidating their complex mechanisms of action, leveraging advanced computational models, sophisticated assay technologies, and multi-optic integration. This guide provides a comprehensive technical framework for validating novel hormone functions within disease models, contextualized by recent insights into hormonal regulation across the lifespan. It addresses the entire workflow from computational prediction and in vitro functional analysis to clinical correlation, providing researchers and drug development professionals with validated methodologies to accelerate discovery and therapeutic translation.
Computational Prediction and Biomarker Discovery
The initial discovery phase for novel hormone functions increasingly relies on machine learning (ML) and bioinformatic analysis of large-scale clinical and molecular datasets. This approach allows for the identification of complex, non-linear patterns that may elude conventional statistical methods.
Machine Learning for Hormone-Related Outcomes
A recent large-scale study demonstrated the application of ML to predict early natural menopause, an endocrine transition point with significant health implications. The study developed a questionnaire-based model using data from 18,015 postmenopausal women across China [83].
Key Methodology:
- Algorithms Evaluated: Ten machine learning algorithms were trained and compared.
- Feature Selection: The Boruta algorithm was employed for dimensionality reduction, identifying 70 predictive factors from initial variables encompassing anthropometrics, sociodemographics, lifestyle factors, medical histories, and reproductive characteristics [83].
- Optimal Model: The XGBoost model performed optimally, achieving an Area Under the Curve (AUC) of 0.745 in the test set. It also showed a precision of 0.84, recall of 0.78, and an F1-score of 0.81 [83].
- Model Simplification: A simplified model using the top 20 predictive factors was developed, retaining an AUC of 0.731. Critical predictors identified via SHapley Additive exPlanations (SHAP) analysis included age, income, geographic region, height, number of siblings, and breastfeeding duration [83].
- Validation: External validation using an independent dataset (CHARLS) yielded an AUC of 0.68, demonstrating moderate generalizability and highlighting the impact of population differences and missing predictors [83].
This study exemplifies how ML can transform accessible questionnaire data into a tool for predicting hormone-mediated life events, offering a non-invasive alternative to clinical biomarker tests.
Genomic Signature Development
Beyond predictive modeling, genomic signatures derived from hormone-related genes offer powerful tools for disease prognosis and classification. A seminal study on endometrial cancer (EC), a hormone-driven malignancy, developed a novel estrogen/progesterone-related gene signature [84].
Key Methodology:
- Data Source: RNA-seq and clinical data for 397 EC patients were obtained from The Cancer Genome Atlas (TCGA) [84].
- Gene Set Identification: Estrogen and progesterone-related gene sets were sourced from the Molecular Signatures Database (MSigDB) [84].
- Differential Analysis: The
limmaR package was used to identify estrogen/progesterone-related differentially expressed genes (DEGs) between tumor and normal tissues [84]. - Signature Construction: Univariate and multivariate Cox regression analyses identified five genes (CDC25B, GNG3, ITIH3, PRXL2A, SDHB) significantly associated with overall survival (OS). A risk score formula was established:
Risk Score = Σ (Coefficient(mRNAi) × Expression(mRNAi))[84]. - Validation: The signature was validated as an independent prognostic factor. The low-risk group had significantly longer OS. A nomogram incorporating the risk score and clinical stage was built to predict survival probability at 2, 5, and 8 years [84].
Table 1: Performance Metrics of Featured Computational Models
| Model Feature | Early Menopause Prediction (XGBoost) [83] | EC Prognostic Gene Signature [84] |
|---|---|---|
| Primary Purpose | Prediction | Prognostication |
| Key Input Variables | 20 questionnaire-based factors (e.g., age, income) | 5 estrogen/progesterone-related genes |
| Sample Size | 18,015 | 397 |
| Optimal Model/AUC | 0.745 | N/A* |
| Key Performance Metrics | Precision: 0.84, Recall: 0.78, F1: 0.81 | Hazard Ratio (High vs. Low Risk): Significant |
| Validation Approach | External (AUC: 0.68) | Internal (KM Plot) |
| Key Technologies/Tools | XGBoost, Boruta, SHAP | Limma, Cox Regression, CIBERSORT |
*The study used Kaplan-Meier survival analysis and risk distribution curves instead of AUC for performance demonstration [84].
The following workflow outlines the standard pipeline for the computational discovery of hormone-related biomarkers and models:
Experimental Validation and Assay Techniques
Computational predictions require rigorous experimental validation to establish causal relationships and mechanistic insights. This phase relies on robust assay systems and careful functional analysis.
Hormone Measurement and Assay Validation
Accurate quantification of hormone levels is foundational. While various methods exist, Enzyme Immunoassays (EIAs) are widely used due to their sensitivity, cost-effectiveness, and rapidity [85]. A standardized protocol for validating EIA kits for steroid hormone analysis in fish plasma highlights critical considerations applicable to mammalian and clinical research [85].
Key Methodology: EIA Validation Protocol The protocol mandates validation for three parameters before measuring novel samples or species:
- Parallelism: Ensures the sample dilution curve is parallel to the standard curve, confirming equivalent antibody binding affinity. This step determines the optimal sample dilution to avoid analyte saturation [85].
- Accuracy: Assessed by spiking samples with known quantities of the standard hormone and calculating the percentage recovery. Recoveries of 80-120% are typically considered acceptable, confirming the assay accurately measures the hormone in the specific sample matrix [85].
- Precision: Evaluated by measuring both intra-assay (within-plate) and inter-assay (between-plate) coefficient of variation (CV). A CV of less than 10-15% indicates high reproducibility and assay reliability [85].
This validation is crucial because commercial EIA kits are often designed for mammalian hormones, and cross-reactivity or matrix effects in non-mammalian samples or novel disease contexts can lead to systematic errors [85].
2In VitroandIn VivoFunctional Analysis
Following biochemical measurement, functional validation is essential. The endometrial cancer study provides a template for this process [84].
Key Methodology: Functional Validation of Signature Genes
- In Vitro Models: Human EC cell lines (Ishikawa, AN3CA) were cultured and transfected with silencing RNA (siRNA) or lentiviral vectors to knock down the expression of signature genes (PRXL2A, GNG3) [84].
- Functional Assays:
- Proliferation: Cell proliferation was significantly inhibited following knockdown of PRXL2A and GNG3.
- Clonogenicity: Colony formation ability was assessed, which was also markedly reduced after gene knockdown [84].
- In Vivo Validation: The inhibition of PRXL2A expression in a xenograft mouse model significantly suppressed tumor growth, providing compelling evidence of its functional role in EC pathogenesis [84].
Table 2: Essential Research Reagent Solutions for Experimental Validation
| Reagent / Material | Specific Example | Function in Validation | Technical Note |
|---|---|---|---|
| Validated EIA Kits | 17β-estradiol (E2), Testosterone (T) Kits [85] | Quantifies steroid hormone concentrations in plasma, tissue homogenates, or cell culture supernatant. | Must be validated for parallelism, accuracy, and precision in the specific sample matrix. |
| Cell Line Models | Ishikawa, AN3CA Endometrial Cancer Cells [84] | In vitro models for testing gene function via knockdown/overexpression and assessing phenotypes. | Authenticate cell lines regularly to avoid cross-contamination. |
| Gene Silencing Tools | siRNA, Lentiviral shRNA [84] | Knocks down expression of target genes to investigate loss-of-function effects. | Include scrambled siRNA controls to account for off-target effects. |
| Antibodies | Anti-FLAG (DYKDDDDK), Anti-ITIH3 [84] | Detects protein expression via Western Blotting; used for confirming knockdown/overexpression. | Optimize antibody dilution for specific signal-to-noise ratio. |
| qRT-PCR Reagents | SYBR Premix Ex Taq, Specific Primers [84] | Measures mRNA expression levels of target genes. Normalize to a reference gene (e.g., GAPDH). | Design primers to span exon-exon junctions to avoid genomic DNA amplification. |
| In Vivo Model | Mouse Xenograft [84] | Provides an in vivo system to validate the impact of gene modulation on disease phenotypes like tumor growth. | Follow institutional animal ethics guidelines. |
Advanced Hormone Monitoring Technologies
Emerging technologies enable more granular hormone tracking. A study utilizing a remote fertility testing system (Oova) quantitatively tracked luteinizing hormone (LH) and pregnanediol-3-glucuronide (PdG) in urine through an AI-powered smartphone app [24]. This platform identified significant variations in follicular and luteal phase lengths across age groups, demonstrating that population-level hormone data can pinpoint cycle phase and day with 95% confidence when age and current hormone levels are known [24]. Such technologies highlight the move towards high-resolution, personalized hormone profiling.
The experimental validation workflow integrates these components into a cohesive strategy:
Clinical Translation and Therapeutic Implications
The ultimate goal of validating novel hormone functions is to inform clinical decision-making and develop new therapeutic strategies. Menopausal Hormone Therapy (MHT) guidelines illustrate the translation of hormonal research into clinical practice, emphasizing a patient-centered approach [86]. A thorough evaluation, including comprehensive medical history, physical examination, and relevant diagnostics (e.g., mammography, bone density assessment), is required prior to initiating MHT to assess indications and contraindications [86].
Furthermore, the five-gene signature for endometrial cancer was incorporated into a nomogram, a clinical tool that combines the molecular signature with traditional staging to provide a personalized prediction of patient survival probability [84]. This exemplifies how validated genomic findings can be operationalized to enhance risk assessment and potentially guide treatment intensity.
The integration of computational prediction, experimental validation, and clinical application creates a powerful feedback loop for advancing the field of endocrine research. This multi-optic integration strategy is summarized as follows:
Endocrine systems orchestrate development, growth, and reproduction across the animal kingdom through complex signaling pathways. Cross-species analysis reveals both deeply conserved mechanisms and lineage-specific adaptations in hormonal regulation. This whitepaper synthesizes recent advances in our understanding of endocrine axes from crustaceans to mammals, framed within the context of ongoing research into hormonal regulation during development. For researchers and drug development professionals, these insights highlight both model systems for basic research and potential targets for therapeutic intervention.
Mounting evidence reveals that endocrine axis cross-talk represents a fundamental principle of physiological regulation conserved across vertebrate and invertebrate lineages [87]. In aquatic vertebrates, thyroid hormones have been shown to influence reproductive processes, while in mammals, circadian rhythms exhibit extensive bidirectional communication with endocrine function [88] [87]. Simultaneously, environmental endocrine disrupting chemicals (EDCs) have been demonstrated to perturb these finely-tuned systems across diverse species, highlighting both shared vulnerability and the utility of comparative approaches for identifying mechanisms of action [88] [89].
Comparative Anatomy of Endocrine Systems
Crustacean Neuroendocrine Organs
The crustacean neuroendocrine system centers on several key structures that integrate neural and hormonal signaling:
- XO-SG Complex: The X-organ-sinus gland complex, located in the eyestalk, serves as the primary neuroendocrine center, producing, storing, and releasing multiple neurohormones including crustacean hyperglycemic hormone (CHH), molt-inhibiting hormone (MIH), and gonad-inhibiting hormone (GIH) [90].
- Y-Organ: This gland produces ecdysteroids that regulate the molting process, analogous to the role of the thyroid gland in vertebrates [90].
- Androgenic Gland (AG): Unique to male crustaceans, this gland regulates sexual differentiation through insulin-like androgenic gland factor (IAG), which determines male primary and secondary sexual characteristics [91].
Mammalian Endocrine Axes
Mammalian endocrine regulation operates through several major axes:
- Hypothalamic-Pituitary-Gonadal (HPG) Axis: Regulates reproduction, sexual development, and behavior through gonadotropin-releasing hormone (GnRH), follicle-stimulating hormone (FSH), luteinizing hormone (LH), and sex steroids [2].
- Hypothalamic-Pituitary-Thyroid (HPT) Axis: Controls metabolism, growth, and development through thyroid-stimulating hormone (TSH), thyroxine (T4), and triiodothyronine (T3) [2].
- Circadian System: The suprachiasmatic nucleus (SCN) of the hypothalamus serves as the central pacemaker, coordinating 24-hour rhythms in physiology and behavior that exhibit extensive bidirectional communication with endocrine function [88].
Table 1: Comparative Endocrine Organs and Their Primary Functions Across Species
| Species Group | Endocrine Organ | Primary Hormones | Core Functions |
|---|---|---|---|
| Crustaceans | XO-SG Complex | CHH, MIH, GIH | Glucose metabolism, molt inhibition, reproduction |
| Crustaceans | Y-Organ | Ecdysteroids | Molting and growth regulation |
| Crustaceans | Androgenic Gland | Insulin-like androgenic gland factor (IAG) | Male sexual differentiation |
| Mammals | Gonads | Estradiol, progesterone, testosterone | Reproduction, sexual development |
| Mammals | Thyroid | Thyroxine (T4), Triiodothyronine (T3) | Metabolism, growth, development |
| Mammals | Suprachiasmatic Nucleus | Circadian clock genes | Physiological and behavioral rhythms |
Molecular Mechanisms and Signaling Pathways
Insulin-like Signaling in Sexual Differentiation
The discovery that insulin-like hormones regulate sexual differentiation across divergent species represents a remarkable example of molecular conservation. In crustaceans, insulin-like androgenic gland factor (IAG) serves as the primary masculinizing hormone [91]. The IAG signaling pathway begins with IAG expression in the androgenic gland, followed by receptor binding on target tissues, activation of intracellular cascades, and ultimately regulation of genes controlling male sexual development.
In the giant freshwater prawn Macrobrachium rosenbergii, Mr-IAG expression begins as early as 20 days after metamorphosis, preceding the appearance of external male sexual characteristics [91]. Mr-IAG silencing experiments demonstrate its necessity for spermatogenesis and development of male secondary sexual characteristics, establishing its role as a master regulator of crustacean masculinization [91].
Figure 1: IAG Signaling Pathway in Crustacean Sexual Differentiation
Circadian-Endocrine Integration
The circadian clock exhibits extensive integration with endocrine function across species, creating bidirectional regulatory networks. In mammals, circadian rhythmicity is present at all levels of endocrine control, from hormone synthesis and release to target tissue sensitivity [88]. This integration is mediated by nuclear receptor signaling, with various hormones directly modulating clock gene expression and circadian physiology.
Molecular analysis reveals that numerous hormones, including glucocorticoids and reproductive hormones, alter clock gene expression via nuclear receptor binding and subsequent genomic action, modulating physiological processes such as nutrient metabolism, stress response, and reproductive physiology [88]. This circadian-endocrine integration is conserved but manifests with species-specific characteristics—while mammals rely primarily on the SCN as a central pacemaker, in teleost fish, peripheral tissues are directly entrainable by light [88].
Table 2: Circadian Gene Ablation Effects on Endocrine Physiology in Mouse Models
| Category | Clock Gene | Tissue Specificity | Physiological Phenotype |
|---|---|---|---|
| Reproductive Physiology | Clock | Systemic | Estrous cycle alterations, impaired fertility |
| Reproductive Physiology | Bmal1 | Gonad-specific | Impaired gonadal steroidogenesis |
| Metabolic Dysregulation | Bmal1 | Pancreas-specific | Altered glucose homeostasis, pancreatic dysfunction |
| Metabolic Dysregulation | Clock | Liver-specific | Altered lipid profiles, disrupted feeding rhythms |
| HPA Axis | Per1, Per2 | Adrenal-specific | Altered rhythmicity of steroid production, impaired stress response |
Endocrine Axis Cross-Talk
Thyroid-reproductive axis cross-talk represents a well-documented example of endocrine interaction conserved across vertebrate species. Research in rainbow trout (Oncorhynchus mykiss) alevins demonstrates that waterborne exposure to T3 (triiodothyronine) modulates estrogen-responsive gene expression, providing evidence for molecular-level interactions between these endocrine systems during early development [87].
The molecular mechanisms underlying this cross-talk include:
- Receptor Crosstalk: Thyroid hormone receptors (TRs) can bind to and activate estrogen-responsive elements (EREs), influencing transcription of genes traditionally considered estrogen-regulated [87].
- Shared Response Elements: Genes such as the steroidogenic enzyme cytochrome P45019A2 in zebrafish contain consensus sequences for both EREs and thyroid hormone-responsive elements, enabling integrated regulation [87].
- Permissive Actions: Thyroid hormones produce changes in target tissues that enhance responsiveness to other hormones, as demonstrated by T3 stimulation of vitellogenin (an estrogen-responsive gene) production in goldfish [87].
Experimental Approaches and Methodologies
IAG Expression Analysis in Crustaceans
Temporal expression profiling of Mr-IAG in Macrobrachium rosenbergii provides a methodology for investigating endocrine regulation of sexual development:
- Animal Staging: Collect specimens across developmental stages (from 20 days after metamorphosis to adulthood) and different male morphotypes (small, orange-clawed, blue-clawed) [91].
- Tissue Processing: Dissect androgenic glands and prepare extracts for protein and RNA analysis [91].
- Antibody Production: Generate recombinant pro-Mr-IAG peptide and use it to produce specific antibodies for immunohistochemistry and Western blotting [91].
- Mass Spectrometry Verification: Confirm the identity of Mr-IAG protein in AG extracts using mass spectrometry [91].
- Expression Quantification: Measure Mr-IAG transcript levels using quantitative PCR across developmental stages and morphotypes [91].
This methodology revealed that Mr-IAG expression precedes external sexual character development and varies significantly between reproductive morphotypes, with higher expression in sexually active morphotypes [91].
Endocrine Axes Cross-Talk Assay
The experimental approach for investigating thyroid-estrogen interactions in rainbow trout alevins:
- Hormone Exposure: Conduct 20-23 day waterborne exposures with T3 (0.5-50 μg/L) and E2 (0.02-0.5 μg/L) individually and in combination [87].
- Morphometric Analysis: Measure length, weight, and deformity rates as whole-organism endpoints [87].
- Gene Expression Analysis: Quantify transcript levels of vitellogenin (vtg), estrogen receptors (ERα, ERβ1, ERβ2), and thyroid hormone receptors (TRα, TRβ) in liver tissue using qPCR [87].
- Statistical Analysis: Employ ANOVA with post-hoc tests to identify significant treatment effects [87].
This experimental design demonstrated that T3 significantly altered estrogen-responsive gene expression, providing direct evidence of endocrine axis cross-talk during early development [87].
Figure 2: Experimental Workflow for Assessing Endocrine Axis Cross-Talk
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Endocrine Axis Investigation
| Reagent/Category | Specific Examples | Research Application | Function |
|---|---|---|---|
| Hormone Agonists/Antagonists | 17β-estradiol, T3, IAG inhibitors | Functional studies of endocrine pathways | Modulate specific hormonal signaling for gain/loss-of-function studies |
| Molecular Biology Tools | qPCR primers for vtg, ERs, TRs, IAG | Gene expression analysis | Quantify transcript levels of endocrine-responsive genes |
| Antibody Reagents | Anti-Mr-IAG, anti-vitellogenin | Protein localization and quantification | Detect and localize endocrine factors in tissues and extracts |
| Hormone Measurement | ELISA, RIA kits | Hormone level quantification | Measure circulating or tissue hormone concentrations |
| Gene Silencing Tools | dsRNA for Mr-IAG | Functional validation | Knock down specific endocrine factors to assess function |
Implications for Environmental and Therapeutic Applications
Endocrine Disrupting Chemicals (EDCs)
The cross-species conservation of endocrine axes has significant implications for understanding the impacts of EDCs. Studies demonstrate that EDCs can dysregulate core clock genes and circadian rhythm networks in parallel with endocrine and metabolic alterations across species [88]. Of particular concern is evidence for transgenerational effects of EDCs in multiple vertebrate species, with epigenetic mechanisms identified as the prevalent means by which EDCs mediate these effects [89].
Research reveals that EDCs disrupt reproductive, neuroendocrine, cardiovascular, and metabolic health across species, with exposure during embryonic and fetal development producing severe impacts on growth and physiology that are frequently sexually dimorphic [88]. The parallel between endocrine and circadian disruption following EDC exposure highlights the interconnected nature of these systems and suggests potential mechanisms for EDC actions.
Therapeutic Implications
Understanding cross-species endocrine principles informs therapeutic development, particularly in hormone replacement therapies (HRT). Recent research on menopausal hormone therapy reveals that timing of initiation relative to menopause onset significantly influences neurological outcomes, with early initiation showing potential neuroprotective effects on Alzheimer disease-related biomarkers [92]. However, emerging evidence also suggests that hormone therapy may influence autoimmune disease risk in postmenopausal women, highlighting the need for careful consideration of individual risk factors [93].
The timing hypothesis—that benefits of HRT depend on initiation shortly after menopause—parallels findings in other endocrine contexts, including the importance of critical developmental windows for hormonal actions [94] [93]. These cross-cutting principles emphasize the importance of temporal factors in endocrine therapies across mammalian systems.
Future Research Directions
Several promising avenues for future research emerge from cross-species endocrine analysis:
- Mechanisms of Transgenerational Effects: Further investigation is needed to understand how EDCs produce multi- and transgenerational effects across different species, particularly the specific epigenetic mechanisms involved [89].
- Circadian-Endocrine Interactions: Additional research is warranted to understand the nature of interaction between circadian and endocrine systems in mediating physiological effects of EDC exposure at environmental levels [88].
- Human-Relevant Dosing: Addressing the limitation that current animal models often use doses and administration routes of EDCs that may not reflect human exposure scenarios [89].
- Non-Rodent Mammalian Models: Expanding research on transgenerational effects of EDCs in non-rodent mammals to better understand potential human implications [89].
This cross-species analysis of endocrine axes reveals both profound conservation of fundamental principles and lineage-specific innovations. For researchers and drug development professionals, these insights highlight model systems for basic research, potential targets for therapeutic intervention, and important considerations for environmental risk assessment. As our understanding of endocrine cross-talk and circadian-endocrine integration deepens, new opportunities will emerge for targeting these regulatory networks in clinical applications.
Comparative Efficacy of Hormone-Based vs. Conventional Therapies
Hormone-based therapies represent a paradigm shift in the management of numerous conditions, from oncology to endocrinology, moving beyond conventional approaches to target the underlying molecular and signaling pathways driving disease pathogenesis. Framed within the context of recent insights into the functional regulation of hormones during development, this whitepaper provides a comparative analysis of therapeutic efficacy. For researchers and drug development professionals, understanding the precise mechanisms of hormone-based interventions—including monoclonal antibodies, selective receptor modulators, and targeted kinase inhibitors—is crucial for advancing personalized medicine. This document synthesizes current data, delineates direct comparative efficacy through structured tables, details experimental protocols for key studies, and visualizes critical signaling pathways and workflows to serve as a foundational resource for ongoing research and development.
The therapeutic landscape is undergoing a significant transformation, driven by an enhanced understanding of hormonal signaling in development and disease. Hormone-based therapies are increasingly defined by their precision, targeting specific receptors, downstream signaling cascades, and immune-mediated responses against hormone-driven pathologies. This targeted approach often contrasts with conventional therapies, such as broad-spectrum chemotherapy or non-specific anti-inflammatory drugs, which can be limited by off-target effects and significant toxicity.
Recent research has unveiled the profound complexity of hormone signaling networks, including the dynamic crosstalk between pathways such as estrogen receptor (ER) and HER2 in breast cancer, or the role of VEGF and Wnt in the proliferation of benign gynecological conditions like adenomyosis [95] [96] [97]. This molecular stratification is critical for optimizing therapeutic outcomes. For instance, in breast cancer, molecular subtyping using tools like the PAM50 assay can predict response to therapy and is an independent prognostic factor for long-term survival [95] [97]. Similarly, the emergence of neurokinin receptor antagonists for menopausal vasomotor symptoms exemplifies a non-hormonal, yet still targeted, approach that modulates the specific neural pathways responsible for symptoms [86]. This whitepaper delves into the comparative efficacy of these sophisticated mechanisms against conventional standards of care, providing a technical guide for the scientific community.
Comparative Efficacy Analysis by Disease Area
The efficacy of hormone-based versus conventional therapies varies significantly across different disease states. The tables below provide a structured, quantitative comparison of treatment outcomes, including pathological complete response (pCR) rates, symptom reduction, and progression-free survival, based on recent clinical trials and cohort studies.
Table 1: Efficacy in Breast Cancer by Molecular Subtype
| Molecular Subtype / Therapeutic Regimen | Hormone-Based / Targeted Therapy pCR Rate | Conventional Chemotherapy pCR Rate | Key Clinical Trials / References |
|---|---|---|---|
| HR+/HER2+ (MUKDEN I - HER2-Enriched) | 55.6% (ADC + TKI) [97] | 32.6% (Chemo + Tar) [97] | MUKDEN Trials [97] |
| HR+/HER2+ (MUKDEN II - ER-Activated) | 47.8% (ET + CDK4/6i + Tar) [97] | 32.6% (Chemo + Tar) [97] | MUKDEN Trials [97] |
| HR+/HER2- (Low Risk, Premenopausal) | 5-yr tamoxifen monotherapy [95] | N/A (Standard of Care) | SOFT, TEXT Trials [95] |
| HR+/HER2- (High Risk, Premenopausal) | Ovarian suppression + AI/SERM [95] | N/A (Standard of Care) | SOFT, TEXT Trials [95] |
Note: pCR (pathological complete response); ADC (Antibody-Drug Conjugate); TKI (Tyrosine Kinase Inhibitor); ET (Endocrine Therapy); Tar (Targeted Therapy); AI (Aromatase Inhibitor); SERM (Selective Estrogen Receptor Modulator).
Table 2: Efficacy in Menopause and Benign Gynecologic Disease
| Condition / Symptom | Hormone-Based Therapy Efficacy | Conventional / Non-Hormonal Therapy Efficacy | Key Clinical Trials / References |
|---|---|---|---|
| Menopausal Vasomotor Symptoms | ~75% reduction (standard-dose MHT) [86] | ~65% reduction (low-dose MHT); Moderate relief (SSRI/SNRI) [86] | 2025 MHT Guidelines [86] |
| Adenomyosis (Pain & Bleeding) | Hormonal suppression (GnRH agonists, progestins) [96] | NSAIDs for symptomatic relief [96] | Frontiers in Cell Biology [96] |
| Genitourinary Syndrome of Menopause | Highly effective (low-dose vaginal estrogen) [86] [98] | Moderate relief (vaginal moisturizers) [98] | 2025 MHT Guidelines [86] |
Note: MHT (Menopausal Hormone Therapy); SSRI (Selective Serotonin Reuptake Inhibitor); SNRI (Serotonin–Norepinephrine Reuptake Inhibitor); NSAIDs (Non-Steroidal Anti-Inflammatory Drugs).
Molecular Mechanisms and Signaling Pathways
The efficacy of hormone-based therapies is rooted in their ability to precisely disrupt disease-specific signaling pathways. The following diagrams, generated using Graphviz DOT language, illustrate key mechanisms and the points of intervention for modern targeted therapies.
Diagram 1: HR+/HER2+ Breast Cancer Signaling and Targeted Blockade
Diagram 2: Key Pathways in Adenomyosis Pathogenesis
Experimental Protocols and Methodologies
To ensure reproducibility and validate the efficacy data presented, this section outlines detailed experimental protocols from landmark studies cited in this whitepaper.
Protocol: Molecular Subtyping of HR+/HER2+ Breast Cancer (MUKDEN Trials)
Objective: To classify HR+/HER2+ breast cancer into molecular subtypes using non-negative matrix factorization (NMF) clustering and validate the subtypes' predictive value for neoadjuvant therapy response [97].
Materials:
- Fresh-frozen or FFPE (Formalin-Fixed Paraffin-Embedded) tumor tissue from pretreatment biopsies.
- RNA extraction kit (e.g., Qiagen RNeasy).
- Microarray or RNA-seq platform for transcriptomic profiling.
- IHC staining equipment and antibodies for ER, PR, HER2, Ki-67, and CD8.
Methodology:
- Cohort Selection: Enroll patients with confirmed HR+/HER2+ breast cancer scheduled for neoadjuvant therapy. Obtain informed consent.
- Tissue Processing and RNA Extraction: Section tissue samples and extract total RNA. Assess RNA quality and integrity (e.g., RIN >7.0).
- Gene Expression Profiling: Hybridize RNA to microarray chips or prepare libraries for RNA sequencing.
- Unsupervised Clustering: Perform NMF clustering on the transcriptomic data from the training set to identify stable molecular subtypes.
- Bioinformatic Validation:
- Validate the identified subtypes in an independent internal cohort and public datasets (e.g., TCGA-BRCA) using submap analysis.
- Perform functional enrichment analysis (KEGG, GSEA) to define subtype-specific biological pathways.
- IHC-Based Classifier Development: Develop a minimal IHC antibody panel (e.g., ER, HER2, Ki-67, CD8) to approximate the mRNA-based subtypes and validate concordance.
- Correlation with Clinical Outcomes: Statistically compare pCR rates across different molecular subtypes and treatment regimens (e.g., ADC+TKI vs. Chemo+Tar vs. ET+CDK4/6i+Tar) using chi-square tests.
Protocol: Evaluating Targeted Therapy in Adenomyosis Models
Objective: To investigate the efficacy of signaling pathway inhibitors (e.g., targeting VEGF, PI3K, Wnt) in preclinical models of adenomyosis [96].
Materials:
- Mouse model of adenomyosis (e.g., induced by tamoxifen or pituitary grafting).
- Small molecule inhibitors (e.g., VEGF inhibitor, PI3K inhibitor, Wnt inhibitor).
- Control vehicles (e.g., DMSO/saline).
- Histology equipment for H&E and immunohistochemical staining.
- Antibodies for Ki-67, CD31, β-catenin, p-AKT.
Methodology:
- Model Induction and Grouping: Induce adenomyosis in experimental mice. Randomize mice into treatment and control groups (n ≥ 8 per group).
- Treatment Administration: Administer therapeutic agents via oral gavage or intraperitoneal injection at predetermined doses. Control groups receive vehicle only. Continue treatment for 4-8 weeks.
- Pain Behavior Monitoring: Assess hyperalgesia using a von Frey filament test or hot plate test at baseline and weekly during treatment.
- Tissue Harvesting and Processing: Euthanize mice, collect uterine horns, and weigh them. Fix tissues for histology and snap-freeze for molecular analysis.
- Histopathological and Molecular Analysis:
- Section tissues and stain with H&E to measure lesion size and extent.
- Perform IHC staining for proliferation marker (Ki-67), angiogenesis marker (CD31), and pathway activation markers (nuclear β-catenin, p-AKT).
- Quantify staining using image analysis software.
- Statistical Analysis: Compare lesion weights, pain thresholds, and quantification of IHC markers between treatment and control groups using Student's t-test or ANOVA.
The Scientist's Toolkit: Research Reagent Solutions
The following table catalogs essential reagents and tools, as derived from the cited experimental protocols, for conducting research in hormone-based therapeutics.
Table 3: Essential Reagents for Hormone Therapy Research
| Reagent / Tool | Function / Application | Specific Example / Catalog Context |
|---|---|---|
| PAM50 Assay | Molecular subtyping of breast cancer; generates a Risk of Recurrence (ROR) score. | Proprietary gene expression signature; used for classifying luminal A, luminal B, HER2-enriched, and basal-like subtypes [95] [97]. |
| Anti-HER2 Antibody-Drug Conjugates (ADCs) | Targeted delivery of cytotoxic agents to HER2-positive cells; induces cell death. | Trastuzumab emtansine (T-DM1) or trastuzumab deruxtecan (T-DXd); used in HR+/HER2+ breast cancer trials [97]. |
| CDK4/6 Inhibitors | Reverses hormone therapy resistance by inhibiting cell cycle progression from G1 to S phase. | Dalpiciclib, Palbociclib, Abemaciclib; used in combination with endocrine therapy in MUKDEN trials [97]. |
| Neurokinin-3 Receptor Antagonists | Non-hormonal treatment for vasomotor symptoms; blocks NK3R in the hypothalamus. | Fezolinetant, Elinzanetant; used in clinical trials for menopausal hot flashes [86]. |
| VEGF/VEGFR Inhibitors | Inhibits angiogenesis; potential application in adenomyosis and oncology. | Small molecule TKIs or monoclonal antibodies; studied in preclinical adenomyosis models [96]. |
| PI3K/Akt/mTOR Inhibitors | Targets a key survival and proliferation pathway; overcomes resistance in hormone-driven cancers and benign diseases. | Everolimus (mTOR inhibitor); Alpelisib (PI3K inhibitor); used in breast cancer and researched in adenomyosis [96] [97]. |
| IHC Antibody Panels | Approximates molecular subtypes in clinical samples when genomic profiling is unavailable. | Antibodies against ER, PR, HER2, Ki-67, and CD8; used to develop surrogate classifiers for HR+/HER2+ subtypes [97]. |
The comparative analysis presented in this whitepaper unequivocally demonstrates the superior efficacy and precision of modern hormone-based and targeted therapies over conventional approaches in well-defined patient subgroups. The success of these strategies is intrinsically linked to a deep understanding of hormonal signaling and the molecular taxonomy of disease, as illustrated by the MUKDEN classification in breast cancer and the pathway-centric view of adenomyosis.
The future of hormone-based therapy lies in further personalization and the development of novel agents to overcome resistance. Promising directions include the use of proteolysis-targeting chimeras (PROTACs) for enhanced receptor degradation, bipolar androgen therapy, and combination regimens with PARP inhibitors guided by genomic profiling [99]. Furthermore, the integration of multi-omics data and functional drug testing using patient-derived organoids will be crucial for identifying the most effective, individualized therapeutic combinations. As our insights into the functional regulation of hormones during development and disease continue to expand, so too will our ability to design ever-more effective and targeted therapeutic interventions, solidifying the central role of precision medicine in the future of healthcare.
Gender-Specific Hormone-Receptor Interaction Networks
Gender-specific hormone-receptor interaction networks represent fundamental regulatory systems that orchestrate sexual dimorphism in development, physiological function, and disease susceptibility. This whitepaper synthesizes recent advances in our understanding of how estrogen, androgen, and progesterone receptors establish and maintain sex-specific signaling networks across neural, immune, and endocrine systems. Through integrated genomic, epigenomic, and single-cell analyses, researchers have begun decoding the complex circuitry through which hormone receptors direct organizational and activational effects across the lifespan. Within the context of broader thesis research on hormonal mechanisms in development and functional regulation, this review highlights emerging experimental frameworks and computational tools that are transforming our capacity to map and manipulate these networks with precision. The insights presented herein provide a technical foundation for developing targeted therapeutic strategies that account for sex-specific biological differences.
Sex hormones exert their effects through complex receptor-mediated networks that operate across developmental timescales and physiological states. The organizational effects of hormones occur primarily during critical developmental windows, where they permanently shape tissue architecture and cellular composition, while activational effects represent transient, often reversible modulation of physiological processes in mature organisms [100] [101]. These paradigms are implemented through sophisticated gene regulatory networks directed by nuclear hormone receptors including estrogen receptors (ERα, ERβ), androgen receptor (AR), and progesterone receptor (PR).
Recent single-cell transcriptomic and epigenomic profiling has revealed that these receptors coordinate sexually dimorphic gene expression programs through mechanisms that extend beyond simple hormone-receptor-DNA ternary complexes [101] [102]. The emerging picture is one of complex interaction networks featuring cell-type-specific receptor expression, chromatin landscape remodeling, and extensive crosstalk between hormonal signaling pathways and other regulatory systems. These networks establish and maintain sex differences in neural circuitry, immune function, and metabolic regulation throughout life.
Table 1: Core Hormone Receptors in Gender-Specific Networks
| Receptor | Primary Ligands | Expression Patterns | Major Functions |
|---|---|---|---|
| ERα | 17β-estradiol | Hypothalamus, BNSTp, hippocampus, immune cells | Neural differentiation, inflammatory regulation, metabolic control |
| ERβ | 17β-estradiol | SCN, SON, PVN, immune cells | Modulates ERα activity, neuroprotection, immune modulation |
| AR | Testosterone, DHT | Mammillary nuclei, preoptic area, myeloid cells | Masculinization of neural circuits, immunosuppression |
| PR | Progesterone | Reproductive tissues, hypothalamus, immune cells | Reproductive behavior, neuroendocrine regulation, immunomodulation |
Molecular Mechanisms of Hormone-Receptor Signaling
Genomic Signaling Pathways
The canonical pathway for hormone receptor function involves direct DNA binding and transcriptional regulation. Upon ligand binding, receptors undergo conformational changes, dimerize, and translocate to the nucleus where they recognize specific hormone response elements in regulatory regions of target genes [101] [102]. Advanced genomic mapping in neural circuits has identified 1,930 E2-induced ERα-bound loci in limbic brain regions, with most being brain-specific compared to peripheral tissues [101]. These binding events occur primarily at distal enhancer elements and are enriched for genes involved in synaptic plasticity, neuron wiring, and neurodevelopmental processes.
The molecular architecture of these interactions exhibits sophisticated regulatory logic. For instance, in the bed nucleus of the stria terminalis (BNSTp), estrogen receptor activation opens 7,293 chromatin regions while closing only 123 regions, indicating a predominantly permissive effect on chromatin accessibility [101]. Remarkably, 89% of these estrogen-responsive regions contain estrogen response elements, demonstrating that direct receptor binding rather than indirect signaling pathways drives most chromatin remodeling [102].
Non-Genomic and Rapid Signaling Mechanisms
Beyond genomic actions, sex hormones exert effects through membrane-initiated steroid signaling (MISS) that involves activation of kinase cascades and second messenger systems [103]. These non-genomic mechanisms enable rapid cellular responses that complement the slower transcriptional regulation. For example, estrogen can activate membrane receptors like ER-X to mediate rapid calcium flux modifications, while androgens can trigger phosphorylation cascades independently of DNA binding [103] [104].
These non-genomic pathways engage in extensive crosstalk with other signaling systems. Estrogen signaling modulates the master inflammatory transcription factor NF-κB through multiple mechanisms including direct protein-protein interactions, inhibition of DNA binding, and induction of the NF-κB inhibitor IκB [103]. This enables hormonal regulation of inflammatory processes without direct genomic binding. Similarly, androgen receptor can cross-talk with glucocorticoid receptor signaling, with ChIP-seq studies revealing shared binding sites that enable integrated regulation of target genes [103].
Diagram 1: Integrated Genomic and Non-Genomic Hormone Signaling Pathways. This diagram illustrates the parallel mechanisms through which sex hormones mediate cellular effects, highlighting the convergence of rapid membrane-initiated signaling with slower genomic regulation.
Epigenetic Regulation and Chromatin Dynamics
Epigenetic mechanisms play crucial roles in establishing and maintaining sex-specific gene expression patterns. X-chromosome inactivation patterns in females, sex-biased DNA methylation, and histone modifications all contribute to sexual dimorphism [100]. Transcriptomic analyses of human astrocytes reveal sex-specific differences in genes encoding chromatin remodeling factors, suggesting that epigenetic regulation represents a fundamental layer of hormone-receptor network control [100].
During aging, these epigenetic landscapes undergo sex-specific modifications. Compared to middle-aged females, younger female astrocytes show higher levels of the activating histone mark H3-trimethyl lysine-4 (H3K4me3), indicating age-dependent epigenetic changes that may underlie differential disease susceptibility [100]. Additionally, genes on the female X-chromosome can escape inactivation or undergo age-dependent expression shifts, creating another dimension of sexual dimorphism in gene regulation [100].
Neural System Implementation
Developmental Programming of Neural Circuits
The brain exhibits remarkable sexual dimorphism in structure and function, orchestrated primarily through hormone-receptor interactions during critical developmental windows. In males, the perinatal testosterone surge—after aromatization to estradiol—activates ERα signaling that promotes neuronal survival in specific regions and establishes male-typical neural circuitry [100] [101]. This organizational programming creates enduring structural differences, such as the male BNSTp being 1.5-2 times larger than in females [101] [102].
Single-cell RNA sequencing has identified specific male-biased neuron types marked by molecular signatures including Nfix and Esr2 expression [102]. These neuronal populations display a transcriptomic identity matching Lamp5+ neurogliaform interneurons and are selectively activated during male-typical social behaviors [101]. The establishment of these sex-specific neural populations illustrates how hormone-receptor networks direct cellular differentiation during development.
Table 2: Sex Differences in Astrocyte Biology Across Lifespan
| Developmental Stage | Male Characteristics | Female Characteristics | Functional Consequences |
|---|---|---|---|
| Early Development | Faster maturation (P7-P14), vimentin+ markers | Delayed maturation, different gene expression peaks | Earlier network assembly in males, different susceptibility to developmental disruption |
| Adulthood | More astrocytes in amygdala, hypothalamus | More astrocytes in hippocampus | Region-specific differences in synaptic regulation and stress response |
| Aging | Preserved glutamate uptake, mitochondrial functions | Increased GFAP+ reactivity, pro-inflammatory phenotype | Higher neuroinflammation in aged females, differential neurodegenerative risk |
| Response to Injury | Maintained functional capabilities after ischemia | Enhanced cytokine secretion, immune cell recruitment | Worse stroke outcomes in postmenopausal females |
Adult Plasticity and Aging Trajectories
In adulthood, hormone-receptor networks continue to shape neural function through activational effects that modulate circuit activity and plasticity. Astrocytes exhibit striking sexual dimorphism in aging patterns, with female astrocytes showing widespread upregulation of reactivity markers like GFAP and adopting pro-inflammatory phenotypes [100]. This shift contributes to the elevated neuroinflammation and increased dementia risk observed in postmenopausal women [100].
Genetic risk factors interact with sex-specific aging trajectories. The APOE4 allele associated with Alzheimer's disease exacerbates astrocytic inflammation particularly in females, with APOE4-expressing astrocytes showing 1.5-2.5 times higher expression of pro-inflammatory cytokines like IL-6, IL-1β, and TNFα compared to males [100]. This highlights how hormone-receptor networks interface with genetic background to determine individual susceptibility profiles.
Immune System Regulation
Innate Immune Dimorphism
The immune system displays profound sexual dimorphism, with females generally mounting stronger innate and adaptive immune responses than males [104]. This differential responsiveness is mediated through sex-specific hormone-receptor networks operating across immune cell types. Neutrophils, for instance, exhibit delayed apoptosis in females, a phenomenon further enhanced by estradiol and progesterone treatment [104]. Androgens promote neutrophilic differentiation and granulopoiesis while suppressing pro-inflammatory cytokine production, creating fundamentally different inflammatory milieus between sexes.
Myeloid cell development is directly influenced by androgen receptor signaling, with men showing greater bone marrow monocyte differentiation and increased blood monocyte concentrations [104]. Transcriptomic analyses reveal that AR activation in monocytes differentially regulates cytokine production in males versus females, with male monocytes showing increased IL-1β and IL-12 production following testosterone treatment [104]. These cell-intrinsic differences illustrate how hormone-receptor networks establish sex-specific immune baselines.
Adaptive Immunity and Autoimmune Susceptibility
In the adaptive immune system, sex hormones differentially regulate T-cell and B-cell responses, contributing to the higher prevalence of autoimmune disorders in females. Estrogens generally enhance humoral immunity, increasing B-cell maturation and antibody production, while androgens and progestogens exert immunosuppressive effects [104]. The balance between Th1 and Th2 responses also shows sexual dimorphism, with females typically exhibiting stronger Th1 responses [104].
The expression patterns of hormone receptors in immune cells create a complex regulatory network. For instance, group 2 innate lymphoid cells express ERα when isolated from the uterus but selectively express AR transcripts in bone marrow and tissue-resident populations [103]. This tissue-specific receptor expression enables localized hormonal control of immune responses, adding another layer of complexity to gender-specific immune regulation.
Diagram 2: Sex-Specific Immune Regulation by Hormone Networks. This diagram outlines the key differences in immune cell function and cytokine profiles between males and females, highlighting pathways that contribute to differential disease susceptibility.
Experimental Approaches and Methodologies
Genomic Mapping Techniques
Comprehensive mapping of hormone-receptor interaction networks requires sophisticated genomic approaches. Low-input CUT&RUN profiling enables genome-wide mapping of transcription factor binding sites in small numbers of cells, overcoming limitations of traditional ChIP-seq when working with rare cell populations [101]. This method has identified 1,930 E2-induced ERα-bound loci across three interconnected limbic brain regions, revealing the brain-specific nature of many estrogen receptor binding events [101].
Assay for Transposase-Accessible Chromatin with sequencing (ATAC-seq) maps chromatin accessibility dynamics in response to hormonal stimulation. When applied to BNSTp Esr1+ cells, this approach detected 7,293 chromatin regions that increase accessibility following estradiol treatment, with nearly all ERα-binding sites overlapping these open chromatin regions [101]. This demonstrates the tight coupling between receptor binding and chromatin remodeling.
Single-Cell Resolution Approaches
Single-cell RNA sequencing (scRNA-seq) has revolutionized our understanding of cellular heterogeneity in hormone-responsive tissues. When applied to the BNST, this approach identified seven distinct Esr1+ neuron types, with two subpopulations (marked by Nfix and Esr2) showing male-biased abundance [102]. This cellular-resolution mapping reveals how hormone-receptor networks operate in specific cell types to establish sexual dimorphism.
Translating Ribosome Affinity Purification (TRAP) enables cell-type-specific translatome profiling by isolating ribosome-bound mRNAs from genetically defined cell populations. When combined with estrogen treatment in Esr1Cre/+;Rpl22HA/+ mice, this method identified 358 genes regulated by oestradiol in BNSTp Esr1+ cells, including genes involved in neuron wiring and synaptic plasticity [101]. This provides insights into the functional consequences of receptor activation in specific cellular contexts.
Table 3: Experimental Protocols for Mapping Hormone-Receptor Networks
| Method | Key Applications | Technical Considerations | Representative Findings |
|---|---|---|---|
| CUT&RUN | Genome-wide TF binding mapping | Low-input, high signal-to-noise ratio | 1,930 E2-induced ERα loci in limbic brain |
| scRNA-seq | Cellular heterogeneity analysis | Requires cell dissociation, clustering | Identification of male-biased Nfix+ neurons |
| ATAC-seq | Chromatin accessibility profiling | Identifies regulatory elements | 7,293 E2-open chromatin regions in BNSTp |
| TRAP-seq | Cell-type-specific translatomes | Genetic access to cell types required | 358 E2-regulated genes in BNSTp Esr1+ cells |
| Hormone Manipulation | Starvation/replacement paradigms | Controls endogenous hormone levels | Replicates neonatal programming windows |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Hormone-Receptor Network Studies
| Reagent/Cell System | Key Applications | Technical Function | Experimental Considerations |
|---|---|---|---|
| Esr1Cre/+;Rpl22HA/+ mice | Cell-type-specific translatome analysis | TRAP sequencing of ERα+ cells | Enables purification of ribosome-bound mRNAs from specific cells |
| MCF-7 breast cancer cells | ERα signaling validation | Reference cell line for ERα studies | Well-characterized ERα responses, useful for method validation |
| CUT&RUN kit | Low-input TF binding profiling | Genome-wide mapping with high sensitivity | Superior to ChIP-seq for small cell numbers, minimal background |
| ATAC-seq kit | Chromatin accessibility mapping | Identifies open/closed chromatin regions | Requires careful nuclei isolation, Tn5 transposition optimization |
| 17β-estradiol (E2) | Estrogen receptor activation | Canonical ER ligand for stimulation | Dose and timing critical for physiological vs. pharmacological effects |
| Anastrozole (Arimidex) | Estrogen synthesis inhibition | Aromatase inhibitor for hormone manipulation | Nearly complete estrogen blockade in post-menopausal models |
Gender-specific hormone-receptor interaction networks represent fundamental organizing principles in biology that shape development, physiological function, and disease susceptibility across the lifespan. The integration of genomic, epigenomic, and single-cell approaches has revealed unprecedented detail about how these networks establish and maintain sexual dimorphism at molecular, cellular, and circuit levels. These insights are catalyzing a paradigm shift in biomedical research toward sex-informed models of biology and disease.
Future research directions include developing more sophisticated experimental models that capture the dynamics of hormone-receptor networks across developmental trajectories, integrating multi-omic datasets to build predictive network models, and translating these fundamental insights into targeted therapeutic strategies that account for sex-specific biological differences. As these efforts progress, they will undoubtedly reveal new dimensions of complexity in gender-specific hormone-receptor networks while providing innovative approaches for addressing sex-biased diseases and optimizing treatments based on biological sex.
Validation of Hormone-Mediated Inter-Organ Communication Pathways
The validation of hormone-mediated inter-organ communication (IOC) is a cornerstone of modern endocrinology and physiology, critical for understanding systemic metabolic homeostasis, aging, and development. This whitepaper provides a comprehensive technical guide to the methodologies and experimental frameworks for validating these complex pathways. It details cutting-edge approaches for identifying novel hormonal factors, tracing their tissue of origin and site of action, and confirming their functional roles in vivo. Designed for researchers, scientists, and drug development professionals, this document synthesizes recent advances in the field, with a specific focus on insights relevant to hormonal roles in development and functional regulation. The protocols and analytical frameworks presented herein are essential for deciphering the intricate dialogue between organs and for developing targeted therapeutic interventions.
Inter-organ communication represents a critical physiological machinery for maintaining robust metabolic networks and a healthy lifespan [66]. The traditional view of endocrine organs has been expanded to include tissues such as adipose tissue, skeletal muscle, and bone, which secrete hormonal factors, now classified as adipokines, myokines, and osteokines, respectively [66]. These factors include proteins, metabolites, and extracellular vesicle (EV)-encapsulated molecules that orchestrate systemic homeostasis. Over time, the delicate balance of IOC is disrupted, leading to physiological deterioration and age-related pathologies [66]. Consequently, the rigorous validation of these pathways is paramount for understanding fundamental biology and for identifying novel therapeutic targets for a range of metabolic and age-related diseases. This guide outlines the core principles and methodologies for the definitive validation of these pathways, providing a roadmap for researchers in this dynamic field.
Analytical Frameworks for Pathway Validation
Validating a hormone-mediated IOC pathway requires a multi-faceted approach that moves beyond correlation to establish causation. The following frameworks are essential for confirming the source, target, and function of a putative signaling molecule.
Table 1: Key Analytical Frameworks for Validating IOC Pathways
| Framework Category | Core Objective | Key Techniques & Technologies | Primary Readout |
|---|---|---|---|
| Factor Identification & Characterization | To discover and biochemically characterize novel circulating factors. | Proteomics, Metabolomics, EV Purification, RNA-seq | Identification of specific hormones, metabolites, or miRNAs [66]. |
| Spatial Validation (Source & Target) | To definitively identify the tissue of origin and the target organ(s). | Cell-type-Specific Knockout/Knockdown, Tissue-Specific Promoter-Driven Expression, Parabiosis | Ablation of factor in source tissue abolishes systemic effect; factor detected in target tissue [66]. |
| Functional Validation (Gain/Loss of Function) | To establish the necessity and sufficiency of the factor for the observed phenotype. | Recombinant Protein Administration, Neutralizing Antibodies, Genetic Loss-of-Function Models | Phenotypic rescue or mimicry (gain-of-function); phenotype blockade (loss-of-function) [66]. |
| Signaling Mechanism Elucidation | To delineate the molecular signaling cascade in the target cell. | Receptor Binding Assays, Phosphoproteomics, Pharmacological Inhibitors, Second Messenger Assays | Identification of receptor, downstream kinases/transcription factors, and target gene expression. |
| Physiological & Phenotypic Assessment | To quantify the organism-level metabolic or functional consequences. | Metabolic Cages (energy expenditure), Glucose/Insulin Tolerance Tests, Lifespan Analysis, Body Composition Analysis | Improved glucose homeostasis, extended healthspan, altered energy expenditure [66]. |
Experimental Workflow for Pathway Validation
The following diagram outlines a generalized, iterative workflow for the discovery and validation of a novel hormone-mediated IOC pathway, integrating the frameworks described above.
Detailed Experimental Protocols
This section provides detailed methodologies for key experiments cited in contemporary IOC research.
Protocol: Validation of an Exercise-Induced Myokine
Objective: To identify and validate a novel myokine released during exercise that mediates remote communication to adipose tissue.
Background: Skeletal muscle functions as an endocrine organ during contraction, secreting myokines like FGF21 and irisin, which stimulate WAT browning and thermogenesis [66].
Materials:
- Animal Model: C57BL/6J mice (8-12 weeks old) with treadmill apparatus.
- Reagents: Recombinant myokine protein, neutralizing antibody (Anti-Myokine), TRIzol reagent, RNA extraction kit, qPCR reagents, primers for Ucp1, Pgc1α, Dio2.
- Equipment: Microcentrifuge, thermocycler, real-time PCR system, cryostat.
Procedure:
- Exercise Intervention: Subject mice to a single bout of treadmill running (60 min at 15 m/min) or maintain as sedentary controls.
- Plasma Collection & Analysis: Collect plasma pre- and post-exercise via submandibular bleeding. Perform quantitative proteomic analysis (e.g., LC-MS/MS) or a specific ELISA if available to identify/confirm elevated circulating myokine.
- Tissue-Specific Knockdown: Employ siRNA or AAV-mediated knockdown of the myokine gene specifically in the skeletal muscle of a separate cohort. Repeat exercise protocol and plasma collection to confirm muscle as the source.
- Functional Gain-of-Function: Administer recombinant myokine (e.g., 5 μg/dose, i.p.) to sedentary mice daily for 7 days.
- Functional Loss-of-Function: Pre-treat exercising mice with a neutralizing antibody against the myokine (e.g., 10 μg/g body weight, i.p.) prior to the exercise bout.
- Endpoint Analysis: 24 hours after the final intervention, sacrifice animals and collect inguinal white adipose tissue (iWAT).
- Molecular Phenotyping:
- RNA Extraction & qPCR: Isolate total RNA from iWAT, synthesize cDNA, and perform qPCR for browning markers (Ucp1, Pgc1α, Dio2). Use GAPDH as a housekeeping control.
- Data Analysis: Normalize data using the 2^–ΔΔCt method. Compare gene expression levels between control, exercise, recombinant protein, and antibody-treated groups using one-way ANOVA with post-hoc testing. A significant increase in browning markers in exercised and recombinant-treated groups, which is blocked by the neutralizing antibody, validates the functional role of the myokine.
Protocol: Tracing Extracellular Vesicle (EV)-Mediated Communication
Objective: To track the fate and function of EVs secreted from a specific tissue (e.g., adipose tissue) to a target organ (e.g., hypothalamus) and assess their role in aging.
Background: Adipose tissue secretes eNAMPT in EVs, which remotely enhances NAD+ biosynthesis in the hypothalamus and counteracts aging [66].
Materials:
- Cell Line: Primary adipocytes from a donor mouse strain.
- EV Labeling: Lipophilic dye (e.g., DiR or PKH67).
- Animal Model: Young (3-month) and aged (20-month) recipient mice.
- Reagents: EV isolation kit (e.g., polymer-based precipitation or size-exclusion chromatography), NAD+/NADH quantification kit.
Procedure:
- EV Isolation and Labeling:
- Culture primary adipocytes from donor mice. Collect conditioned media and isolate EVs using a standardized kit.
- Resuspend the EV pellet in PBS and label with a lipophilic dye (e.g., PKH67) according to the manufacturer's protocol. Remove excess dye via ultracentrifugation.
- In Vivo Injection and Tracking:
- Intravenously inject PKH67-labeled EVs (100 μg protein in 100 μL PBS) into recipient mice.
- After 6-24 hours, perfuse animals, harvest the brain, and prepare cryosections.
- Imaging and Quantification:
- Image hypothalamic sections using a confocal microscope. Co-stain with neuronal markers (e.g., NeuN) to confirm cellular uptake.
- Quantify fluorescence intensity in the hypothalamus as a measure of EV delivery.
- Functional Assessment:
- Treat aged mice with EVs isolated from young mice (i.p., twice weekly for 1 month).
- Measure hypothalamic NAD+ levels using a bioluminescent assay kit.
- Conduct behavioral tests (e.g., rotarod, open field) to assess functional improvements.
- Data Interpretation: Successful delivery of labeled EVs to hypothalamic neurons, coupled with an increase in NAD+ levels and improved behavioral outcomes in EV-treated aged mice, validates the functional EV-mediated IOC pathway.
Current Research Applications and Findings
The validation frameworks outlined above have been successfully applied to elucidate novel IOC pathways with significant implications for development and metabolism. Recent studies have leveraged these methods to uncover sophisticated endocrine circuits.
Table 2: Validated Hormone-Mediated Inter-Organ Communication Pathways
| Hormonal Factor | Source Organ | Target Organ | Validated Function | Key Experimental Evidence |
|---|---|---|---|---|
| eNAMPT (in EVs) | White Adipose Tissue | Hypothalamus | Delays aging, extends lifespan [66]. | Neuronal activation in DMH stimulates WAT secretion; plasma EVs enhance hypothalamic NAD+; supplementation extends lifespan [66]. |
| FGF21 | Skeletal Muscle (Exercise) | White Adipose Tissue | Stimulates WAT browning, promotes thermogenesis [66]. | Elevated in muscle and plasma post-exercise; recombinant FGF21 induces Ucp1 in WAT. |
| Osteocalcin | Bone | Pancreas, Adipose Tissue | Increases insulin secretion and sensitivity, lowers blood glucose [66]. | Osteoblast-specific knockout models show insulin resistance; administration improves glucose tolerance. |
| Gut Microbiota-Derived Metabolites (e.g., SCFAs) | Intestine | Brain (CNS) | Modulates neurodevelopment, immune function, and behavior [105]. | GF mice show behavioral deficits; metabolite supplementation (e.g., butyrate) rescues phenotypes; receptor (GPCR) knockouts block effects. |
| Platelet Factor 4 (PF4) | Platelets | Hippocampus | Attenuates age-related neuroinflammation, improves cognitive function [66]. | Systemic administration in aged mice reduces neuroinflammation and improves performance in memory tasks. |
The Hypothalamus as a High-Order Control Center
A paradigm-shifting application of IOC validation has identified the hypothalamus as a master regulator of aging via communication with peripheral organs. Specific neuronal subpopulations in the dorsomedial hypothalamus (DMH) can be activated to stimulate the secretion of eNAMPT from white adipose tissue [66]. This remote signaling, mediated via EVs, enhances NAD+ biosynthesis in the hypothalamus, creating a feed-forward loop that significantly delays aging and extends lifespan in mice [66]. This pathway was validated using advanced techniques including chemogenetics (to activate specific neurons), tissue-specific manipulation of eNAMPT, and detailed tracking of EV fate and function, showcasing the power of integrated validation frameworks.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for IOC Pathway Validation
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Recombinant Proteins | Gain-of-function studies; to test sufficiency of a hormonal factor. | Administering recombinant osteocalcin to assess improvements in glucose tolerance [66]. |
| Neutralizing Antibodies | Loss-of-function studies; to block the activity of an endogenous hormone. | Injecting anti-myokine antibody to block exercise-induced adipose tissue browning [66]. |
| Adeno-Associated Viruses (AAVs) with Tissue-Specific Promoters | For cell-type-specific gene overexpression or knockdown in vivo. | Using AAV driven by an adiponectin promoter to knock down a gene exclusively in adipose tissue. |
| Cre-loxP Mouse Models | Generation of tissue-specific or inducible knockout animals. | Crossing a mouse with loxP sites flanking the eNAMPT gene with an adipocyte-specific Cre driver to create a fat-specific KO [66]. |
| Extracellular Vesicle Isolation Kits | Purification of EVs from cell culture media or biological fluids for functional studies. | Isolating EVs from young mouse plasma to test their rejuvenating effects in aged mice [66]. |
| Lipophilic Tracers (e.g., PKH67, DiR) | Fluorescent or bioluminescent labeling of EVs or membranes for in vivo tracking. | Labeling adipose-derived EVs with PKH67 to trace their uptake in the hypothalamus [66]. |
| Metabolite Assay Kits (e.g., NAD+/NADH) | Quantitative measurement of key metabolites in tissues. | Quantifying hypothalamic NAD+ levels after treatment with young plasma EVs [66]. |
| GC/MS and LC-MS/MS Systems | Untargeted and targeted identification/quantification of metabolites and proteins. | Profiling plasma to discover new aging- or exercise-associated biomarkers [66]. |
Conclusion
The synthesis of recent research underscores hormones as central regulators of development, metabolism, and behavior, with their spatial and temporal expression tightly controlled by complex feedback loops. The integration of foundational knowledge with advanced methodologies like single-cell genomics and computational modeling is decoding the intricacies of hormonal networks. Addressing historical challenges, such as sex-based differences in pharmacology, is critical for developing safer, more effective therapies. The promising translation of basic research into clinical applications, including novel hormone-based drugs for metabolic, inflammatory, and neurodegenerative diseases, highlights a pivotal shift towards personalized medicine. Future research must prioritize understanding the causal effects of hormones on neural computation, mapping hormone-receptor interactions across the lifespan, and leveraging these insights to create next-generation, targeted endocrine therapies that improve patient outcomes across diverse populations.
References
- 1. 9.2: Signaling Pathways, Hormones and Endocrine System [https://med.libretexts.org/Bookshelves/Veterinary_Medicine/Book%3A_Introductory_Animal_Physiology_(Hinic-Frlog)/9%3A_Maintaining_Internal_Balance/9.2%3A_Signaling_Pathways_Hormones_and_Endocrine_System]
- 2. Recent insights into the role of hormones during ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1340432/full]
- 3. The central signaling pathways related to metabolism ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06656-3]
- 4. Novel perspectives on growth hormone regulation of ... [https://pubmed.ncbi.nlm.nih.gov/40270715/]
- 5. Hormonal regulation of behavioral and emotional persistence [https://www.sciencedirect.com/science/article/abs/pii/S1074742725000450]
- 6. Jack of all trades: Crosstalk between FERONIA signaling ... [https://pubmed.ncbi.nlm.nih.gov/39972666/]
- 7. Association between wearable sensor signals and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12410205/]
- 8. Continuous Hormone Monitoring Market Growth 2025-2035 [https://www.futuremarketinsights.com/reports/continuous-hormone-monitoring-market]
- 9. Nuclear receptors in health and disease: signaling ... [https://www.nature.com/articles/s41392-025-02270-3]
- 10. Quantifying the variability in the assessment of ... [https://www.sciencedirect.com/science/article/pii/S0015028223019994]
- 11. Case Reports from Women Using a Quantitative Hormone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10608103/]
- 12. Using Hormone Data and Age to Pinpoint Cycle Day within ... [https://www.mdpi.com/1648-9144/59/7/1348]
- 13. Editorial: Recent insights into the role of hormones during ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1454714/full]
- 14. Negative Feedback Loops and Hormonal Factors that ... [https://pubmed.ncbi.nlm.nih.gov/40908533/]
- 15. Sleep strengthens muscle and bone by boosting growth ... [https://news.berkeley.edu/2025/09/08/sleep-strengthens-muscle-and-bone-by-boosting-growth-hormone-levels-uc-berkeley-researchers-discover-how/]
- 16. Standardizing protocols dealing with growth hormone ... [https://www.sciencedirect.com/science/article/abs/pii/S1096637418300674]
- 17. Protocol for assessing the effects of exogenous hormone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9900611/]
- 18. FDA lifts HRT warning: A new era for hormone health [https://www.bodyrejuvenationmd.com/womens-health/fda-lifts-hrt-warning/]
- 19. Views of Menopause and Hormone Therapy Associations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12415175/]
- 20. Hormone Signalling Crosstalk in Plant Growth Regulation [https://www.sciencedirect.com/science/article/pii/S0960982211002855]
- 21. A systematic analysis of human hormone receptors [https://link.springer.com/article/10.1007/s11427-024-2950-4]
- 22. Multi-omics analysis of organ-specific hormone distribution ... [https://www.frontiersin.org/journals/plant-science/articles/10.3389/fpls.2025.1662457/full]
- 23. ATHB1 Interacts with Hormone-Related Gene Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468107/]
- 24. Using Hormone Data and Age to Pinpoint Cycle Day within ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10384168/]
- 25. Neuroestrogen: The brain's secret weapon against hunger [https://www.sciencedaily.com/releases/2025/05/250501122254.htm]
- 26. Quantitative Hormone Monitoring of the Menstrual Cycle [https://www.mdpi.com/journal/medicina/special_issues/quantitative_hormone_monitoring]
- 27. Mapping hormone-regulated cell-cell interaction networks ... [https://www.sciencedirect.com/science/article/pii/S2405471222002757]
- 28. Applications and techniques of single-cell RNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284766/]
- 29. Single-cell RNA-seq combined with bulk ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1609189/full]
- 30. Single-cell RNA-sequencing of circulating tumour cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12500777/]
- 31. Single‐Cell Analysis of Alternative Splicing and Gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12239682/]
- 32. Single-cell mRNA-regulation analysis reveals cell type ... [https://www.nature.com/articles/s41467-025-65060-z]
- 33. Single-cell RNA sequencing reveals different cellular ... [https://www.nature.com/articles/s41523-025-00808-w]
- 34. Single-cell RNA sequencing identifies molecular biomarkers ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02226-9]
- 35. Single-cell RNA sequencing reveals developmental ... [https://link.springer.com/article/10.1007/s44154-025-00255-4]
- 36. Single Cell RNA Sequencing and Its Impact on ... [https://pubmed.ncbi.nlm.nih.gov/40869062/]
- 37. CRISPR/Cas9 therapeutics: progress and prospects - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9841506/]
- 38. Multi-faceted CRISPR/Cas technological innovation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10201107/]
- 39. CRISPR/Cas9 Landscape: Current State and Future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10671331/]
- 40. Plan Your CRISPR Experiment [https://www.addgene.org/guides/crispr/plan-your-experiment/]
- 41. CRISPR-Cas9 mediated d3GHR knockout in HEK293 cells [https://www.sciencedirect.com/science/article/pii/S0531556524002328]
- 42. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 43. Hormonal regulation of behavioral and emotional persistence [https://pubmed.ncbi.nlm.nih.gov/40436262/]
- 44. Editorial: Recent insights into the role of hormones during ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11297355/]
- 45. About - Research Training in Neuroendocrinology [https://med.virginia.edu/neuroendocrinology/overview/]
- 46. Editorial: Therapeutic effects of endogenous hormones in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12500605/]
- 47. Hormone Therapy Drug Chart [https://www.cancerhealth.com/drugs/classes/hormone-therapy]
- 48. Nutrient-stimulated Hormone-based Therapies [https://www.xiahepublishing.com/m/2310-8819/JCTH-2025-00303]
- 49. Combination of obesity medication tirzepatide and ... [https://www.endocrine.org/news-and-advocacy/news-room/endo-annual-meeting/endo-2025-press-releases/castaneda-press-release]
- 50. Recent insights into the role of hormones during ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10841574/]
- 51. Hormone Replacement Therapy Market and Growth ... [https://www.delveinsight.com/blog/hormone-replacement-therapy]
- 52. Bispecific antibodies: unleashing a new era in oncology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12320366/]
- 53. The $40 Billion Race: Bispecific Antibodies Are Redefining ... [https://www.forbes.com/sites/williamhaseltine/2025/09/18/the-40-billion-race-bispecific-antibodies-are-redefining-cancer-therapy/]
- 54. 6 Promising Bispecific Antibodies Beyond Oncology [https://www.delveinsight.com/blog/6-promising-bispecific-antibodies-beyond-oncology]
- 55. Roche to present new data from its broad and innovative ... [https://www.roche.com/media/releases/med-cor-2025-11-03b]
- 56. Hormones, developmental plasticity, and adaptive evolution [https://www.sciencedirect.com/science/article/abs/pii/S0303720719303806]
- 57. Hormone Therapy Market Analysis and Revenue Trends ... [https://www.towardshealthcare.com/insights/hormone-therapy-market-sizing]
- 58. Investigating Insomnia: Closing the Gender Gap in Clinical... [https://acrpnet.org/2025/10/21/investigating-insomnia-closing-the-gender-gap-in-clinical-pharmacology]
- 59. differences in the expression of hepatic Sex ... drug metabolizing [https://pubmed.ncbi.nlm.nih.gov/19483103/]
- 60. Study Sheds New Light on How Hormones Influence ... [https://www.nyu.edu/about/news-publications/news/2025/november/study-sheds-new-light-on-how-hormones-influence-decision-making-.html]
- 61. Researchers create lab model that could lead to new, non- ... [https://news.ohsu.edu/2025/01/13/researchers-create-lab-model-that-could-lead-to-new-non-hormonal-birth-control-methods]
- 62. 14 Comparing quantitative data between individuals [https://bookdown.org/pkaldunn/SRM-Textbook/BetweenQuantData.html]
- 63. Triptorelin: The Crossroads of Endocrine and ... [https://cherwell.org/2025/08/15/triptorelin-the-crossroads-of-endocrine-and-neurobiological-research/]
- 64. Growth hormone-releasing hormone receptor (GHRH-R) and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12137518/]
- 65. Developmental transitions involve common biological ... [https://www.sciencedirect.com/science/article/pii/S2405844025013763]
- 66. Inter-organ communication is critical machinery to regulate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12170921/]
- 67. Machine learning in endocrinology: current applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572088/]
- 68. Mathematical modeling of the interaction between ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1543185/full]
- 69. Efficacy of combined gonadotropin-releasing hormone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537404/]
- 70. Recent insights into the role of hormones during ... [https://pubmed.ncbi.nlm.nih.gov/38318293/]
- 71. Instability Challenges and Stabilization Strategies of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9699111/]
- 72. Enhancement of The Stability of Human Growth Hormone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7211290/]
- 73. Drug Bioavailability Enhancing Agents of Natural Origin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6359194/]
- 74. Bioavailability enhancers of herbal origin: An overview - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3634921/]
- 75. Hormone Therapy in 2025: What You Need to Know About the ... [https://vallabellewellness.com/hormone-therapy-in-2025-what-you-need-to-know-about-the-latest-trends/]
- 76. Precision pharmacology in menopause: advances ... [https://www.frontiersin.org/journals/reproductive-health/articles/10.3389/frph.2025.1694240/full]
- 77. Hormone cycles shape the structure and function of key ... [https://news.ucsb.edu/2025/021876/hormone-cycles-shape-structure-and-function-key-memory-regions-brain]
- 78. 2025 Research Symposium Agenda - NETRF [https://netrf.org/for-researchers/2025-research-symposium/2025-research-symposium-agenda/]
- 79. Simulation software [https://www.cnsorg.org/software]
- 80. A Practical Guide to Quantitative Data Analysis Methods ... [https://www.looppanel.com/blog/quantitative-data-analysis-methods]
- 81. Quantitative Data Analysis. A Complete Guide [2025] [https://www.6sigma.us/six-sigma-in-focus/quantitative-data-analysis/]
- 82. Data Analysis Methods: 7 Essential Techniques for 2025 [https://atlan.com/data-analysis-methods/]
- 83. Development and validation of questionnaire-based ... [https://www.nature.com/articles/s44294-025-00098-4]
- 84. Comprehensive Analysis and Experimental Validation of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9225250/]
- 85. Development of a validation protocol of enzyme ... [https://www.sciencedirect.com/science/article/abs/pii/S0022098117301296]
- 86. The 2025 Menopausal Hormone Therapy Guidelines [https://pmc.ncbi.nlm.nih.gov/articles/PMC12438153/]
- 87. Reproductive and thyroid endocrine axis cross-talk in ... [https://www.sciencedirect.com/science/article/abs/pii/S0016648021001489]
- 88. Cross-species physiological interactions of endocrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7993548/]
- 89. A cross-species comparative approach to assessing multi [https://www.sciencedirect.com/science/article/pii/S001393512101358X]
- 90. A brief and updated introduction to the neuroendocrine ... [https://www.sciencedirect.com/science/article/abs/pii/S0303720724001217]
- 91. Expression of an Androgenic Gland-Specific Insulin-Like ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3262648/]
- 92. Recapping TMS 2025: Evolving Insights and Future ... [https://www.pharmacytimes.com/view/recapping-tms-2025-evolving-insights-and-future-directions-in-menopause-care]
- 93. New insights on hormone therapy and autoimmune ... [https://www.contemporaryobgyn.net/view/new-insights-on-hormone-therapy-and-autoimmune-disease-risk-with-xuezhi-daniel-jiang-md-phd]
- 94. Reconsidering Hormone Replacement Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565178/]
- 95. Current Endocrine Therapy in Hormone-Receptor-Positive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299218/]
- 96. Signaling pathways and advances in targeted therapy for ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1685525/full]
- 97. Molecular classification of hormone receptor-positive ... [https://www.nature.com/articles/s41392-025-02181-3]
- 98. Review of hormonal replacement therapy options for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463494/]
- 99. Emerging therapies to overcome antiandrogen resistance ... [https://www.sciencedirect.com/science/article/pii/S266700542500047X]
- 100. Sex-Specific Properties of Astrocytes: From Development to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12350529/]
- 101. Gene regulation by gonadal hormone receptors underlies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9159952/]
- 102. Gene regulation by gonadal hormone receptors underlies ... [https://www.nature.com/articles/s41586-022-04686-1]
- 103. Sex Hormone Receptor - an overview [https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/sex-hormone-receptor]
- 104. Gender-Specific Impact of Sex Hormones on the Immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10094624/]
- 105. decoding the gut–immune–brain axis in health and disease [https://www.nature.com/articles/s41423-025-01333-3]