Personalizing HRT: A Precision Medicine Framework for Metabolic and Cardiovascular Risk Stratification
This article synthesizes the latest evidence and emerging trends in tailoring Hormone Replacement Therapy (HRT) to individual metabolic and cardiovascular risk profiles.
Personalizing HRT: A Precision Medicine Framework for Metabolic and Cardiovascular Risk Stratification
Abstract
This article synthesizes the latest evidence and emerging trends in tailoring Hormone Replacement Therapy (HRT) to individual metabolic and cardiovascular risk profiles. Aimed at researchers, scientists, and drug development professionals, it explores the foundational science linking menopause to accelerated cardiovascular disease, including its impact on lipids, blood pressure, and insulin resistance. The content delves into methodological frameworks for risk assessment, leveraging genetic insights and advanced imaging. It further addresses troubleshooting through formulation optimization, timing of initiation, and management of side effects. Finally, it validates these approaches through comparative analysis of therapeutic regimens, recent clinical data, and evolving regulatory landscapes, providing a comprehensive roadmap for the development of next-generation, personalized hormone therapies.
The Menopausal Metabolic Shift: Unraveling the Link Between Estrogen Decline and Cardiovascular Pathogenesis
FAQs: Mechanisms and Research Models
1. What are the primary mechanistic pathways linking estrogen loss to accelerated atherosclerosis in experimental models? Research indicates that the loss of estrogen leads to endothelial dysfunction, adverse lipid profile changes, and increased arterial inflammation, which collectively accelerate atherosclerosis [1] [2] [3]. The primary pathways involved are:
- Endothelial Dysfunction: Estrogen deficiency reduces the synthesis and release of nitric oxide (NO), a potent vasodilator, and increases the release of vasoconstrictors like endothelin-1 [1] [4] [3].
- Lipid Metabolism Dysregulation: Menopause is associated with a 10-20% increase in low-density lipoprotein cholesterol (LDL-C) and a rise in lipoprotein(a) [Lp(a)] by approximately 25%. Estrogen's role in upregulating apolipoprotein B100 (apoB100) receptors is lost, impairing LDL clearance [5] [4] [2].
- Vascular Remodeling and Inflammation: Oestrogen modulates matrix metalloproteinases (MMPs). Its deficiency disrupts normal vascular remodeling and promotes a pro-inflammatory state, evidenced by increases in pro-inflammatory cytokines [6] [4].
2. Our cell studies show conflicting results for estrogen's atheroprotective effects. What key experimental factors could explain this? Discrepancies often arise from critical variables related to the timing and formulation of estrogen exposure.
- Timing of Intervention (The "Timing Hypothesis"): Beneficial effects on the vasculature are most consistently observed when estrogen is administered soon after menopause or ovariectomy in model systems. Delayed administration may coincide with established subclinical atherosclerosis, limiting efficacy or causing harm [4] [7] [8].
- Estrogen Formulation and Dose: 17-beta-estradiol (E2) is the primary physiological form and often shows favorable metabolic effects. Conjugated equine estrogens (CEE), used in some major trials, can have different metabolic impacts, particularly on liver-derived clotting factors and triglycerides when administered orally [4] [3] [9]. Furthermore, inappropriately high doses can trigger excessive vascular remodeling and inflammatory responses [4].
- Model System: The choice of model (e.g., human endothelial cells, rodent ovariectomy models, or non-human primates) can influence outcomes due to differences in receptor expression and metabolic pathways [3].
3. Which circulating protein biomarkers show the most significant association with early menopause and future CVD risk in human cohorts? Recent large-scale proteomic studies have identified specific biomarkers. The table below summarizes key findings from an analysis of 71 protein biomarkers in 1,565 postmenopausal women from the Framingham Heart Study [6].
Table 1: Protein Biomarkers Associated with Early Menopause and Cardiovascular Outcomes
| Biomarker | Association with Early Menopause | Representative Biological Pathway | Link to Incident CVD |
|---|---|---|---|
| Adrenomedullin | Higher levels | Neurohormonal Regulation | Associated with all-cause death; effect modified by early menopause status [6]. |
| Resistin | Higher levels | Inflammation / Adipokine Signaling | Predicts incident cardiovascular outcomes [6]. |
| Insulin Growth Factor-1 (IGF-1) | Lower levels | Metabolic / Growth Factor | Lower levels associated with lower risk of cardiovascular events [6]. |
| CNTN1 (Contactin-1) | Lower levels | Neuronal Adhesion | Lower levels associated with lower risk of cardiovascular events [6]. |
4. What is the recommended protocol for assessing subclinical atherosclerosis in a menopausal research cohort? The gold standard non-invasive method is the Coronary Artery Calcium (CAC) scan, a non-invasive CT scan [10]. A standard protocol is:
- Equipment: Non-contrast cardiac computed tomography (CT) scanner.
- Procedure: Acquire sequential images (e.g., 3 mm slices) through the coronary arteries. The Agatston score is calculated based on the area and density of calcium deposits.
- Data Interpretation: A CAC score of 0 indicates very low risk. Scores of 1-99, 100-399, and ≥400 indicate mild, moderate, and severe plaque burden, respectively [10].
- Application in Research: A 2024 study demonstrated that post-menopausal women show a significantly faster rate of CAC progression (e.g., double the median increase in scores per year compared to men with similar baseline profiles), making it a robust endpoint for interventional studies [10].
5. How does the route of HRT administration (oral vs. transdermal) impact thrombosis risk in preclinical and clinical data? The route of administration critically impacts the "first-pass" hepatic metabolism and thus the risk of thrombotic events.
- Oral Estrogen: Passes through the liver, significantly increasing the synthesis of coagulation factors (e.g., thrombin, fibrinogen) and leading to a higher risk of venous thromboembolism (VTE) [4] [3].
- Transdermal Estrogen: Delivers estrogen directly into the systemic circulation, bypassing first-pass liver metabolism. This route has a neutral effect on the coagulation system and is not associated with an increased risk of VTE, making it preferable for women at elevated baseline thrombotic risk [4] [3] [9].
Table 2: Metabolic and Vascular Effects of Different HRT Formulations
| Parameter | Oral Estrogen | Transdermal Estrogen | Notes |
|---|---|---|---|
| LDL Cholesterol | ↓↓ (9-18 mg/dL) | ↓ | Significant reduction with oral route [5] [4]. |
| Triglycerides | ↑ | ↓ or | Oral route can worsen hypertriglyceridemia [5] [4] [3]. |
| Coagulation | ↑ Risk of VTE | No increased risk | Key differentiator for safety [4] [3]. |
| Insulin Sensitivity | ↑↑ (Pronounced effect) | ↑ | Oral estrogen has a stronger impact on glucose metabolism [4] [7]. |
Experimental Protocols
Protocol: Assessing Atherosclerotic Progression Using Coronary Artery Calcium (CAC) Scoring
Application: To quantitatively measure the progression of subclinical coronary atherosclerosis in a longitudinal cohort study of menopausal women [10]. Materials:
- Non-contrast electrocardiogram (ECG)-gated cardiac CT scanner.
- Phantoms for calibration (if quantitative comparison across sites is needed).
- Dedicated workstations with CAC scoring software (e.g., for calculating the Agatston score). Method:
- Participant Preparation: No specific patient preparation (fasting, contrast) is required.
- Image Acquisition: Position the participant supine. Perform a scout scan to localize the heart. Acquire non-contrast CT images from the carina to the diaphragm during a single breath-hold. Use ECG-gating to minimize motion artifact.
- Image Analysis:
- Identify and trace regions of interest (ROI) with a radiodensity >130 Hounsfield Units (HU) and an area ≥1 mm² within the coronary arteries (left main, left anterior descending, circumflex, and right coronary).
- The software calculates the Agatston score by multiplying the area of each calcified plaque by a density factor (1 for 130-199 HU, 2 for 200-299 HU, 3 for 300-399 HU, and 4 for ≥400 HU).
- The scores for all lesions in all coronary arteries are summed to yield the total CAC score.
- Quality Control: Ensure inter- and intra-observer variability is assessed and minimized. Troubleshooting:
- Problem: High motion artifact degrading image quality.
- Solution: Ensure proper breath-hold coaching and use of ECG-gating. Consider beta-blockers for participants with high heart rates if clinically permissible.
- Problem: Inconsistent scoring between different analysts or software versions.
- Solution: Implement a standardized training and certification process for analysts. Use the same software version for all analyses in a given study.
Protocol: Proteomic Biomarker Profiling for Cardiovascular Risk Stratification
Application: To identify and validate circulating protein biomarkers associated with early menopause and incident CVD, elucidating underlying pathophysiological pathways [6]. Materials:
- Ethylenediaminetetraacetic acid (EDTA) or citrate plasma samples (fasting preferred).
- Multiplex immunoassay platform (e.g., Luminex xMAP).
- Commercially available or custom-designed panels targeting CVD-related proteins (e.g., biomarkers of inflammation, adiposity, neurohormonal function).
- Laboratory automation equipment for high-throughput processing.
- Statistical analysis software (e.g., R, SAS). Method:
- Sample Collection and Preparation: Collect peripheral blood via venipuncture. Centrifuge to isolate plasma within 30-60 minutes of collection. Aliquot and store samples at -80°C. Avoid repeated freeze-thaw cycles.
- Biomarker Measurement: Perform multiplexed assays according to manufacturer protocols. Briefly:
- Incubate plasma samples with antibody-coated magnetic beads.
- Wash to remove unbound protein.
- Add a biotinylated detection antibody followed by a streptavidin-phycoerythrin reporter.
- Measure fluorescence on the analyzer. Include standards and controls in each run.
- Data Pre-processing: Use a 5-parameter logistic (5-PL) curve to convert fluorescence intensities to protein concentrations. Exclude biomarkers with a high proportion (>25%) of values below the detection limit.
- Statistical Analysis:
- Normalize biomarker concentrations using rank-based inverse normal transformation.
- Use multivariable linear regression to test associations between early menopause (exposure) and biomarker levels (outcome), adjusting for covariates (age, BMI, smoking, etc.).
- Account for multiple hypothesis testing using methods like Benjamini-Hochberg False Discovery Rate (FDR) correction. Troubleshooting:
- Problem: High inter-assay coefficient of variation (CV).
- Solution: Use freshly prepared standards, calibrate equipment regularly, and pool a large-volume quality control sample to run across all plates.
- Problem: Plate effects or batch-to-batch variation.
- Solution: Randomize samples across plates. Include technical replicates and use statistical methods (e.g., ComBat) to adjust for batch effects during analysis.
Data Presentation
Table 3: Quantifiable Cardiovascular Risk Factor Changes During Menopause and with HRT
| Risk Factor | Change with Menopause (vs. Pre-menopause) | Effect of Oral HRT | Effect of Transdermal HRT |
|---|---|---|---|
| Systolic BP | ↑ 4–7 mm Hg [5] | ↓ 1–6 mm Hg [5] | Neutral or ↓ DBP by up to 5 mm Hg [5] |
| LDL-C | ↑ 10–20 mg/dL (14–19%) [5] | ↓ 9–18 mg/dL [5] [4] | ↓ [4] |
| HDL-C | Initially ↑, then ↓ [5] | ↑ [5] [4] | ↑ [4] |
| Triglycerides | ↑ [2] | ↑ [5] [4] | ↓ or [5] [4] |
| Fasting Glucose / HbA1c | HbA1c ↑ ~5% [5] | HbA1c ↓ up to 0.6% [5] [7] | Improves insulin sensitivity [7] |
| Lp(a) | ↑ ~25% [5] | ↓ 20–30% [5] | Not well defined |
| CAC Progression | Accelerated (2x male rate in statin users) [10] | May ↓ progression [5] | May ↑ progression [5] |
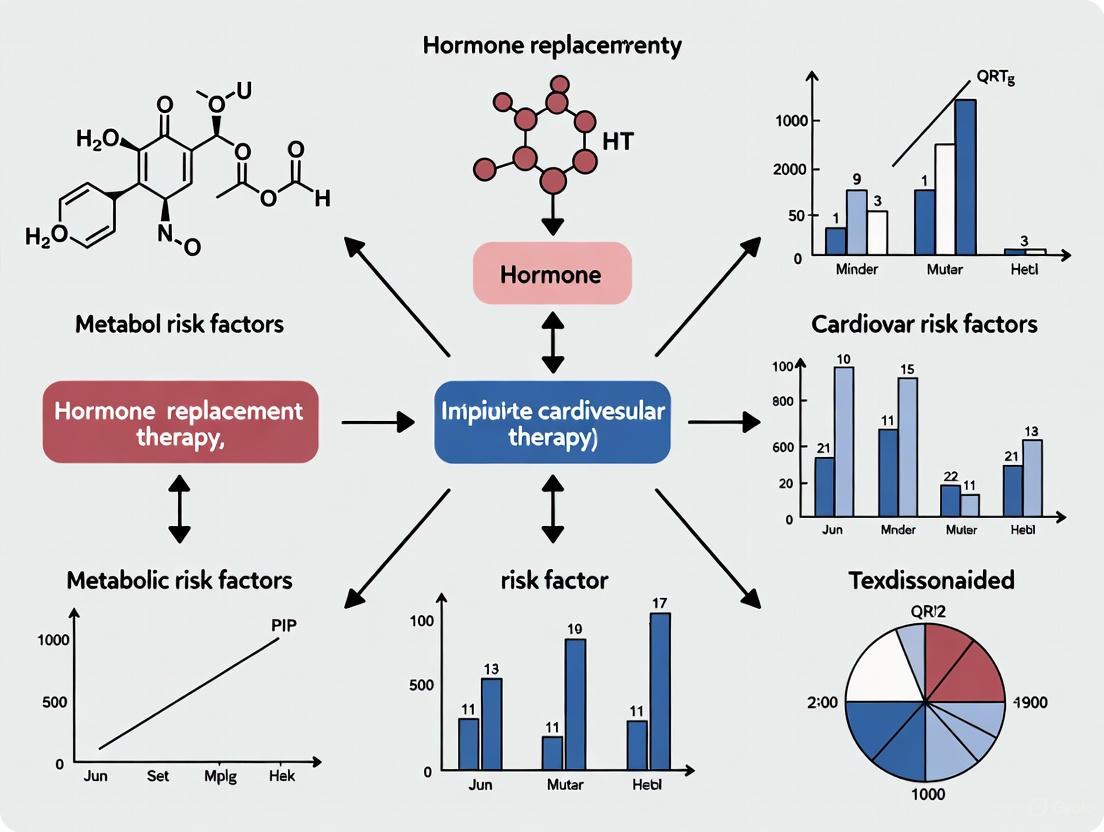
Signaling Pathways and Workflows
Mechanistic Pathways of Menopause-Accelerated Atherosclerosis
Workflow for Biomarker and CAC Progression Study
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for Investigating Menopause and ASCVD
| Research Tool | Function / Application | Example Use Case |
|---|---|---|
| Luminex xMAP Multiplex Assays | Simultaneously quantify multiple protein biomarkers (e.g., adrenomedullin, resistin) from a single small-volume plasma sample [6]. | Discovery and validation of novel protein biomarkers associated with early menopause in cohort studies [6]. |
| Coronary Artery Calcium (CAC) Scoring Software | Quantifies calcified plaque burden in coronary arteries from non-contrast CT scans using the Agatston score [10]. | Primary endpoint for assessing subclinical atherosclerosis progression in interventional or observational studies [10]. |
| 17-Beta-Estradiol (E2) | The primary physiological estrogen used in in vitro and in vivo models to study molecular mechanisms of estrogen action [3]. | Investigating the direct effects of estrogen on endothelial cell nitric oxide synthase (eNOS) expression and function [4] [3]. |
| Transdermal Estradiol Patches | Preclinical and clinical formulation that delivers estrogen without first-pass liver metabolism [4] [3]. | Comparing the metabolic and thrombotic safety of different HRT routes in animal models or clinical trials [4] [3]. |
| Ovariectomized (OVX) Rodent Models | Surgical model of menopause by removing ovaries, inducing rapid estrogen deficiency [8]. | Studying the causal effects of estrogen loss on weight gain, lipid metabolism, and vascular function in a controlled setting [8]. |
Technical FAQs: Hormonal Mechanisms and Metabolic Pathways
FAQ 1: How does menopause and Menopause Hormone Therapy (MHT) quantitatively impact key atherosclerotic cardiovascular disease (ASCVD) risk factors?
Menopause induces a constellation of adverse changes in cardiovascular risk factors, while the effects of MHT are complex and depend on formulation, route of administration, and timing of initiation. The table below summarizes the quantitative effects based on current literature [5].
Table 1: Quantitative Effects of Menopause and MHT on Key Risk Factors
| Risk Factor | Effect of Menopause | Effect of Menopause Hormone Therapy (MHT) |
|---|---|---|
| Blood Pressure (BP) | Systolic BP ↑ 4–7 mm Hg; Diastolic BP ↑ 3–5 mm Hg [5]. | Oral estrogen ↓ SBP by 1–6 mm Hg; Transdermal estrogen ↓ DBP by up to 5 mm Hg; Combined therapy (estrogen + progesterone) may ↑ SBP [5]. |
| Lipid Profile: LDL-C | ↑ LDL by 10–20 mg/dL (or 14–19%) [5]. | Oral MHT ↓ LDL by 9–18 mg/dL [5]. Estrogen-based therapy reduced LDL by ~11% in the WHI trials [11]. |
| Lipid Profile: HDL-C | Initially ↑ during peri-menopause, then declines [5]. | Oral MHT ↑ HDL [5]. WHI trials showed HDL increased by 13% (estrogen-only) and 7% (estrogen-plus-progesterone) [11]. |
| Lipid Profile: Lp(a) | ↑ by ~25% during menopause [5]. | Oral MHT ↓ Lp(a) by 20–30% [5]. WHI trials showed a 15-20% reduction [11]. |
| Insulin Resistance | ↑ Insulin resistance (OR 1.40–1.59); ↑ HbA1c by ~5% [5]. | MHT can ↑ insulin sensitivity; ↓ HbA1c by up to 0.6%; ↓ fasting glucose by ~20 mg/dL [5]. |
| Adiposity | ↑ Visceral and pericardial fat deposition [5]. | Modest ↓ in visceral fat and BMI (~1 kg/m²); preserves lean tissue mass [5]. |
FAQ 2: What is the proposed biological mechanism behind MHT's impact on lipoprotein(a) and why is it significant for drug development?
Lipoprotein(a), or Lp(a), is a genetic, independent risk factor for ASCVD and aortic stenosis. Unlike other lipoproteins, its concentration is largely genetically determined and, until recently, has been resistant to pharmacological modification [11]. The finding that oral estrogen-based MHT can significantly reduce Lp(a) by 15-20% provides a crucial proof-of-concept that Lp(a) levels can be modulated therapeutically [11]. This is significant for drug development as it validates biological pathways that can be targeted by novel, more specific therapeutics. The mechanism is thought to involve the downregulation of Lp(a) synthesis in the liver, likely via estrogen receptor-mediated effects on gene expression. However, it is critical to note that this reduction in Lp(a) with MHT has not been demonstrated to translate directly into a reduction in cardiovascular events, highlighting the need for further research into the causal nature of Lp(a) and the development of targeted therapies [5] [11].
FAQ 3: How does the route of administration (oral vs. transdermal) alter the risk-benefit profile of MHT, particularly concerning thrombosis and mental health?
The route of administration fundamentally alters the metabolism of MHT, leading to different risk profiles. Oral estrogen undergoes first-pass metabolism in the liver, which can have beneficial effects on lipid profiles (lowering LDL, raising HDL) but also increases the production of coagulation factors and triglycerides, elevating the risk of venous thromboembolism and stroke [5] [11]. In contrast, transdermal estrogen bypasses the liver, entering the bloodstream directly. This results in more neutral effects on triglycerides and coagulation factors, offering a safer thrombotic profile [11]. Emerging evidence also suggests that the route of administration may impact mental health; one recent study found that transdermal hormone therapy was associated with a lower incidence of anxiety and depression compared to oral formulations [12].
Experimental Protocols & Methodologies
Protocol 1: Long-Term Biomarker Analysis for MHT Clinical Trials
This protocol is adapted from the Women's Health Initiative (WHI) and subsequent analyses to evaluate the long-term effect of hormone therapy on cardiovascular biomarkers [11].
- Objective: To assess the long-term (e.g., 6-year) effects of specific MHT formulations on a comprehensive panel of cardiovascular biomarkers, including lipids, lipoprotein(a), insulin resistance, and coagulation factors.
- Materials:
- Study Population: Postmenopausal women (e.g., ages 50-79), randomized into intervention and control groups.
- Interventions: Active drugs (e.g., conjugated equine estrogen 0.625 mg/day for women with hysterectomy; conjugated equine estrogen plus medroxyprogesterone acetate 2.5 mg/day for women with uterus) versus matched placebo [11].
- Sample Collection Tubes: Serum separator tubes for lipids and Lp(a); EDTA tubes for HbA1c; sodium citrate tubes for coagulation factors.
- Key Assay Kits: Direct LDL-C assay, Lp(a) immunoturbidimetric assay, HbA1c HPLC kit, automated glucose assay, fibrinogen activity assay.
- Methodology:
- Baseline Assessment: Collect fasting blood samples and clinical data prior to randomization.
- Randomization & Blinding: Randomize participants to active treatment or placebo groups using a computer-generated system. Maintain double-blinding.
- Longitudinal Sampling: Collect follow-up fasting blood samples at predefined intervals (e.g., Year 1, Year 3, Year 6).
- Laboratory Analysis:
- Centrifuge blood samples to isolate plasma/serum.
- Analyze samples in a centralized, certified laboratory.
- Measure LDL-C, HDL-C, total cholesterol, triglycerides, Lp(a), glucose, and HbA1c using standardized, validated methods.
- Analyze coagulation factors (e.g., fibrinogen, Factor VII).
- Statistical Analysis: Use mixed-effects models to compare the longitudinal change in each biomarker from baseline between the treatment and placebo groups, adjusting for relevant covariates.
Protocol 2: Assessing Vascular Health via Coronary Artery Calcium (CAC) Scoring
This protocol is used to evaluate the impact of menopause and MHT on subclinical atherosclerosis [5].
- Objective: To quantify the burden of subclinical coronary atherosclerosis using Coronary Artery Calcium (CAC) scoring in menopausal women, with or without MHT.
- Materials:
- Participants: Cohort of women at various stages of the menopause transition.
- Imaging Equipment: Multi-detector computed tomography (CT) scanner.
- Software: Dedicated CAC scoring software (e.g., Agatston score algorithm).
- Methodology:
- Participant Preparation: No specific preparation is required, though participants should avoid caffeine and smoking prior to the scan.
- CT Scan Acquisition: Perform a non-contrast, electrocardiographically-gated CT scan of the heart. Scan parameters typically include 3 mm slice thickness.
- Image Analysis:
- Identify and quantify calcified plaques in the coronary arteries (left main, left anterior descending, circumflex, right coronary).
- The software automatically highlights regions with a density > 130 Hounsfield Units.
- Calculate the total Agatston score, which is the product of the area of calcification and a density factor.
- Data Interpretation: A CAC score of 0 indicates no plaque; 1-99 mild plaque; 100-399 moderate plaque; and ≥400 extensive plaque. Studies show menopause is associated with increased CAC scores (OR 2.37) [5].
Signaling Pathways and Experimental Workflows
Diagram 1: Menopause-Induced ASCVD Risk Pathway.
Diagram 2: MHT Administration Route Impact.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Hormonal Impact Research
| Research Reagent / Material | Function / Application | Example Use-Case |
|---|---|---|
| Conjugated Equine Estrogens (CEE) | A complex mixture of estrogens derived from pregnant mares' urine; a classic oral MHT formulation. | Used as the active intervention in the WHI trials to study the effects of oral estrogen on long-term cardiovascular biomarkers [5] [11]. |
| Medroxyprogesterone Acetate (MPA) | A synthetic progestin; added to estrogen therapy in women with a uterus to prevent endometrial hyperplasia. | Used in combination with CEE in the WHI to assess the impact of combined MHT on breast cancer and CVD risk [5]. |
| Micronized Progesterone | A bioidentical progesterone; considered to have a more favorable side-effect and risk profile compared to synthetic progestins. | Studied in contemporary MHT regimens for its neutral or beneficial effects on blood pressure and cardiovascular risk compared to MPA [5]. |
| Transdermal Estradiol Patches/Gels | Delivers 17β-estradiol directly through the skin, bypassing first-pass liver metabolism. | Used in clinical studies to compare the thrombotic and metabolic safety profile (e.g., triglycerides, coagulation factors) against oral formulations [5] [11] [12]. |
| Lipoprotein(a) [Lp(a)] Immunoassay | A specific assay to quantify plasma Lp(a) concentration, a genetic risk factor for ASCVD. | Critical for evaluating the significant Lp(a)-lowering effect of oral estrogen therapy in clinical trials [5] [11]. |
| Coronary Artery Calcium (CAC) Scoring Software | Quantifies calcified plaque burden in coronary arteries from non-contrast CT scans (Agatston score). | Used in observational and interventional studies to measure the effect of menopause and MHT on subclinical atherosclerosis [5]. |
Frequently Asked Questions (FAQs)
Q1: What is the established quantitative link between early natural menopause and metabolic syndrome? A large-scale study analyzing electronic health records of over 234,000 women who experienced natural menopause found that the prevalence of metabolic syndrome was 13.5% in the early menopause group, compared to 10.8% in the late menopause group. This translates to a 27% higher relative risk of developing metabolic syndrome for women with early natural menopause, even after adjusting for confounders like BMI, race, and medication use [13] [14].
Q2: How does early menopause modify the risk of cardiovascular disease in the presence of metabolic syndrome? Subgroup analyses from cohort studies reveal a powerful synergistic effect. In one study, postmenopausal women with metabolic syndrome had a two-fold higher risk of CVD (HR 2.01). However, this association was most pronounced in women with early menopause (defined as before age 45), who faced a significantly higher risk (HR 3.86) compared to their peers without early menopause [15].
Q3: What are the key biological pathways and biomarkers implicated in the increased CVD risk for women with early menopause? Proteomic analyses have identified that early menopause is associated with alterations in specific CVD-related protein biomarkers. A study of 71 biomarkers in 1,565 postmenopausal women found seven were significantly associated with early menopause [6]. Key pathways involved include:
- Inflammation and Adipokine Signaling: Biomarkers like resistin (higher in early menopause) link adipose tissue dysfunction to inflammation [6].
- Neurohormonal Regulation: Adrenomedullin (higher in early menopause) is a vasoactive peptide, and its elevated levels were associated with all-cause death specifically in women with early menopause [6].
- Growth Factor Signaling: Insulin-like growth factor-1 (IGF-1) was lower in women with early menopause, suggesting a disruption in metabolic and repair pathways [6].
Q4: How has the FDA's recent decision on Hormone Therapy (HT) labels impacted its consideration for risk mitigation? In late 2024, the FDA initiated the removal of the "black box" warning—the strictest safety warning—from systemic hormone therapy labels. This decision, based on a re-assessment of data including evidence from younger cohorts starting therapy soon after menopause onset, aims to reduce unwarranted fear and underutilization. The updated labels will facilitate more nuanced, evidence-based discussions about the individualized benefits and risks of HT [16] [17].
Q5: What is the "timing hypothesis" and how does it influence HT recommendations for cardiometabolic health? The "timing hypothesis" posits that the cardiovascular effects of HT depend critically on when it is initiated relative to menopause onset. Age-stratified analyses of the Women's Health Initiative data show that absolute risks of adverse events are much lower in women who start HT under age 60 or within 10 years of menopause onset. Initiating HT in this window may have more favorable effects on cardiometabolic biomarkers, such as lowering LDL cholesterol and insulin resistance, compared to later initiation in women with established atherosclerosis [18].
Key Experimental Protocols & Data Summaries
Protocol: Large-Scale Cohort Study for MetS and CVD Risk Assessment
Objective: To investigate the association between metabolic syndrome (MetS) and incident cardiovascular disease (CVD) in postmenopausal women, and to assess effect modification by age at menopause [15].
Methodology Overview:
- Cohort: The Kailuan cohort study. The analysis included 5,210 postmenopausal women after age-matching.
- Design: Prospective cohort study with a median follow-up of 15.53 years.
- Exposure: Metabolic syndrome, defined by standard criteria (e.g., ATP III).
- Outcomes: Incident CVD events (cerebrovascular disease and myocardial infarction), adjudicated by review of medical records.
- Statistical Analysis: Multivariable Cox proportional hazards models were used to calculate hazard ratios (HRs) and 95% confidence intervals (CIs), adjusted for confounders. Stratified analyses were performed by age at menopause (early <45 years vs. later ≥45 years).
Summary of Key Findings: Table: Association Between Metabolic Syndrome and Cardiovascular Disease in Postmenopausal Women [15]
| Outcome | Adjusted Hazard Ratio (HR) | 95% Confidence Interval |
|---|---|---|
| Composite CVD | 2.01 | 1.64 - 2.46 |
| Cerebrovascular Disease | 1.83 | 1.47 - 2.27 |
| Myocardial Infarction | 3.28 | 1.97 - 5.46 |
| CVD in Early Menopause Subgroup | 3.86 | 1.29 - 11.53 |
Protocol: Proteomic Biomarker Discovery for CVD Risk Stratification
Objective: To identify circulating protein biomarkers associated with early menopause and to test whether early menopause modifies the association of these biomarkers with incident cardiovascular outcomes [6].
Methodology Overview:
- Cohort: 1,565 postmenopausal women from the Framingham Heart Study (FHS) Offspring and Third Generation cohorts, free of prevalent CVD.
- Biomarker Measurement: 71 circulating CVD protein biomarkers were measured using a multiplexed Luminex xMAP platform. Biomarkers were selected based on prior associations with atherosclerosis.
- Statistical Analysis:
- Association Testing: Linear regression was used to examine the cross-sectional association between early menopause (age <45) and rank-normalized biomarker levels.
- Multiple Testing Correction: A Benjamini-Hochberg adjusted p-value <0.1 was set as significant.
- Effect Modification: Cox models with interaction terms were used to test if early menopause modified biomarker-outcome associations for HF, major CVD, and all-cause death.
Summary of Key Findings: Table: Select Protein Biomarkers Associated with Early Menopause and Incident CVD [6]
| Biomarker | Direction in Early Menopause | Proposed Biological Pathway | Interaction with Incident Outcomes |
|---|---|---|---|
| Adrenomedullin | Higher | Neurohormonal Regulation, Vascular Tone | Modified association with all-cause death |
| Resistin | Higher | Inflammation, Adipokine Signaling | - |
| Insulin-like Growth Factor-1 (IGF-1) | Lower | Growth Factor Signaling, Metabolism | - |
| CNTN1 (Contactin-1) | Lower | Neuronal Adhesion | - |
Protocol: Assessing Long-Term Effects of Hormone Therapy on Cardiovascular Biomarkers
Objective: To evaluate the long-term effect of commonly prescribed estrogen-based hormone therapies on a panel of cardiovascular biomarkers [19].
Methodology Overview:
- Trial Data: Analysis of data from the Women's Health Initiative (WHI), a long-term randomized controlled trial.
- Interventions: Conjugated equine estrogens (CEE) alone (for women with hysterectomy) or CEE plus medroxyprogesterone acetate (MPA) (for women with uterus).
- Comparison: Placebo.
- Outcomes: Percent change in key cardiovascular biomarkers, including lipids, lipoprotein(a), and measures of insulin resistance.
Summary of Key Findings: Table: Percent Change in Cardiovascular Biomarkers with Hormone Therapy vs. Placebo in the WHI [19]
| Cardiovascular Biomarker | CEE Alone | CEE + MPA |
|---|---|---|
| HDL-C ("Good" Cholesterol) | +13% | +7% |
| LDL-C ("Bad" Cholesterol) | -11% | -11% |
| Lipoprotein(a) | -15% | -20% |
| Insulin Resistance (HOMA-IR) | -14% | -8% |
| Triglycerides | Increase (data not specified) | Increase (data not specified) |
Signaling Pathways and Experimental Workflows
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Investigating Menopause-Associated Cardiometabolic Risk
| Research Reagent / Material | Function & Application in the Field |
|---|---|
| Multiplexed Protein Biomarker Panels (e.g., Luminex xMAP) | Simultaneously quantifies dozens of circulating proteins (e.g., adrenomedullin, resistin) from a single small-volume plasma/serum sample to discover and validate biomarker signatures [6]. |
| Electronic Health Record (EHR) Data Repositories | Provides large-scale, longitudinal real-world data for phenotyping (e.g., age at menopause), identifying outcomes (e.g., MetS, CVD), and conducting retrospective cohort studies [13] [14]. |
| Validated Hormone Therapy Formulations (Oral CEE/MPA, Transdermal Estradiol) | Critical for interventional studies examining the effects of different HT types, doses, and routes of administration on cardiometabolic biomarkers and clinical outcomes [19] [18]. |
| Standardized Metabolic Syndrome Criteria (e.g., NCEP ATP III) | Provides a consistent, clinical definition for patient stratification and endpoint adjudication in observational and interventional studies [15]. |
| Bioinformatics Pipelines for Multiple Testing Correction (e.g., Benjamini-Hochberg) | Essential for robust statistical analysis in high-dimensional data (e.g., proteomics) to control the false discovery rate and identify truly significant associations [6]. |
FAQs: Estrogen and Genetic Pathways in Cardiovascular Research
Q1: What is the evidence that estrogen directly modulates genes associated with coronary artery disease (CAD) risk? A 2025 systematic review of CAD genome-wide association studies (GWAS) found that 26 out of 61 identified genes (43%) have evidence of modulation by estrogen. These genes were primarily discovered in studies that adjusted for sex, with nearly half also appearing in sex-stratified analyses. The affected genes are functionally categorized into lipid synthesis and metabolism (12 genes), vascular integrity (11 genes), and thrombosis (3 genes). This indicates a substantial genetic interface between estrogen signaling and CAD pathways [20].
Q2: Why is studying sex-stratified genetic associations critical for understanding CAD? Studies that do not segregate data by sex assume that genetic contributions to CAD are identical between men and women, which can introduce bias and reduce trait specificity. If true sex differences exist, sex-stratified analyses actually increase statistical power to detect them, rather than reducing it. Despite this, of 60 eligible CAD GWASs reviewed, only 3 reported significant SNPs from sex-stratified analyses that were mapped to genes, highlighting a significant gap in current research methodologies [20].
Q3: How does the "critical window of hormone therapy" influence experimental outcomes in cardiovascular protection models? The "critical window" hypothesis posits that the timing of estrogen intervention is crucial. Positive outcomes are most likely when treatment is initiated in the pre-menopause phase or immediately post-menopause. Many of estrogen's cardioprotective effects are mediated by the vasculature. Therefore, in vitro and in vivo experiments designed to model post-menopausal hormone therapy must carefully control the timing of estrogen intervention relative to the loss of ovarian function to yield clinically relevant results [21].
Q4: What are the key differences between genomic and non-genomic estrogen signaling in cardiovascular cells? Estrogen signaling occurs via two primary mechanisms:
- Genomic Signaling (Slow): Estrogen binds to nuclear estrogen receptors (ERα and ERβ), which then act as transcription factors to regulate gene expression over hours to days. This includes effects on mitochondrial biogenesis and lipid metabolism genes [20] [22].
- Non-genomic Signaling (Rapid): Estrogen activates membrane-associated receptors (including GPER), triggering rapid signal transduction cascades (within seconds to minutes) that regulate vascular tone, for instance, by stimulating nitric oxide (NO) release [21] [22]. The specific receptors and downstream effects are summarized in the pathway diagram in Section 3.
Q5: My data on Hormone Replacement Therapy (HRT) and inflammatory markers like CRP are conflicting. How should I interpret this? Your observations reflect a known complexity. Oral estrogen therapy is consistently associated with elevations in the inflammatory marker C-reactive protein (CRP). However, transdermal estradiol overall has no significant effect on CRP. This suggests that the route of administration is a critical variable. Furthermore, while certain HRT formulations can change biomarker levels (like lowering Lp(a)), there is currently no direct evidence that these specific changes result in modified cardiovascular risk. Your experimental design should therefore prioritize functional cardiovascular endpoints alongside biomarker levels [23].
Experimental Protocols for Key Investigations
Protocol 1: Identifying Estrogen-Modulated CAD Genes from GWAS Data
This protocol outlines a bioinformatic workflow for scoping reviews to determine if CAD-associated genes are estrogen-modulated [20].
Workflow Overview: The diagram below outlines the key steps for a systematic review to identify and analyze estrogen-modulated CAD genes from GWAS data.
Detailed Methodology:
Literature Search Strategy:
- Databases: Conduct parallel searches in MEDLINE (via Ovid) and EMBASE (via Ovid).
- Search Terms: Combine synonyms for:
- Phenotype: "Coronary Artery Disease" OR "Coronary Heart Disease"
- Study Type: "Genome Wide Association Study" OR "GWAS"
- Filters: No initial language or date restrictions. Include manual searching of citations and the GWAS catalog.
Study Selection & Data Extraction:
- Inclusion Criteria: Original GWAS or GWAS meta-analysis where CAD is defined as luminal stenosis >50%, MI, CABG, and/or PCI.
- Data Extraction: Use a standardized form to capture:
- Study design and population demographics (including sex representation).
- All genome-wide significant SNPs and their mapped genes.
- Whether sex-stratified analyses were performed and their significant gene hits.
Analysis of Estrogen Modulation:
- Curate a final list of unique genes from all included studies.
- Perform a systematic literature search for each gene to find evidence of direct or indirect regulation by estrogen (e.g., via ER binding sites, changes in expression levels in response to estrogen).
- Categorize genes by their primary role in cardiovascular pathophysiology (e.g., lipid metabolism, vascular integrity).
Protocol 2: Assessing HRT Formulation Impact on CVD Biomarkers via Meta-Analysis
This protocol is based on a 2025 meta-analysis standard for evaluating the effects of specific HRT formulations on cardiovascular disease risk factors [24].
Workflow Overview: The diagram below shows the systematic process for conducting a meta-analysis on HRT and cardiovascular biomarkers.
Detailed Methodology:
Search Strategy:
- Databases: Search PubMed/Medline, Web of Science, SCOPUS, and Embase from inception to current date.
- Keywords: Use a combination of MeSH and non-MeSH terms. Example: ("Medroxyprogesterone Acetate" OR "hormone replacement therapy" OR estradiol) AND transdermal AND ("randomized controlled trial" OR RCT).
- Supplementary: Scan reference lists of relevant articles.
Eligibility Criteria (PICOS):
- Population (P): Postmenopausal women.
- Intervention (I): Transdermal estrogens combined with oral medroxyprogesterone acetate (MPA).
- Comparison (C): Placebo or control group.
- Outcomes (O): Lipid parameters (LDL-C, TC, TG, HDL-C), ApoB, Lp(a).
- Study Design (S): Randomized Controlled Trials (RCTs) only.
Data Synthesis and Analysis:
- Data Extraction: Independently extract data by two investigators: study design, participant characteristics, intervention dosage, trial duration, and mean/SD of post-intervention outcomes.
- Risk of Bias: Use the Cochrane ROB2 tool.
- Statistical Analysis: Calculate weighted mean differences (WMDs) and 95% confidence intervals (CIs) using a random-effects model. Assess heterogeneity with I² statistic. Perform sensitivity analysis and assess publication bias with funnel plots and Egger's test.
Estrogen Signaling Pathways in Cardiovascular Protection
The following diagram integrates the genomic and non-genomic pathways through which estrogen modulates cardiovascular function, highlighting key targets and functional outcomes relevant to CAD [21] [22] [25].
Quantitative Data on Menopause, MHT, and Cardiovascular Risk Factors
Table 1: Impact of Menopause and Menopause Hormone Therapy (MHT) on Key Cardiovascular Risk Factors [5]
This table summarizes the changes in major risk factors due to menopause and the modifying effects of different MHT formulations, providing critical data for experimental variable selection and hypothesis generation.
| Risk Factor | Effect of Menopause | Effect of Oral MHT | Effect of Transdermal MHT |
|---|---|---|---|
| Blood Pressure | Systolic ↑ 4–7 mm Hg; Diastolic ↑ 3–5 mm Hg [5] | SBP ↓ 1–6 mm Hg; Combined therapy may ↑ SBP [5] | Diastolic ↓ up to 5 mm Hg; Neutral/beneficial effects [5] |
| Lipids: LDL-C | Increases by 10–20 mg/dL (14–19%) [5] | Reduces by 9–18 mg/dL [5] [11] | Significantly reduces (WMD: -12.17 mg/dL) [24] |
| Lipids: Lp(a) | Increases by ~25% [5] | Reduces by 15–20% [11] [23] | No statistically significant change [24] |
| Lipids: HDL-C | Initially increases, then declines [5] | Increases by 7–13% [11] | No statistically significant change [24] |
| Insulin Resistance | Odds Ratio increases (1.40–1.59) [5] | Reduces HbA1c (up to 0.6%), improves insulin sensitivity [5] | (Data often combined with oral; transdermal considered metabolically neutral/positive) |
| Inflammation (CRP) | (Attributed to hormonal changes) [23] | Consistently elevates CRP [23] | No significant effect [23] |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Investigating Estrogen-Mediated Cardiovascular Pathways
This table lists key reagents, their functions, and research considerations for studying estrogen's role in cardiovascular genetics and pathophysiology.
| Reagent / Tool | Primary Function in Research | Key Considerations & Alternatives |
|---|---|---|
| 17β-Estradiol (E2) | The primary endogenous estrogen used in in vitro and in vivo models to study physiologic estrogen signaling [22]. | Consider dose, duration, and timing of administration to model pre- vs. post-menopausal states ("critical window") [21]. |
| Estrogen Receptor Modulators | • ERα/ERβ Agonists/Antagonists (e.g., PPT, DPN): To dissect receptor-specific effects.• GPER-Selective Agonists (e.g., G-1): To isolate rapid, non-genomic signaling [21]. | Verify receptor selectivity and potency for your specific cell type or model system. |
| Human-Identical HRT Formulations | • Micronized Progesterone: Often used in combination with estrogen for preclinical studies modeling contemporary HRT with a better safety profile [5]. | Contrast with synthetic progestins (e.g., MPA) to investigate differential effects on thrombosis and inflammation. |
| siRNA/shRNA for CAD Genes | To knock down expression of estrogen-modulated CAD candidate genes (e.g., those involved in lipid metabolism or vascular integrity) identified from GWAS [20]. | Use in relevant cell lines (e.g., endothelial cells, hepatocytes, vascular smooth muscle cells) to validate gene function. |
| Antibodies for Cardiovascular Markers | • eNOS / p-eNOS: Assess endothelial function and non-genomic signaling.• PGC-1α: Monitor mitochondrial biogenesis (genomic signaling).• ICAM-1/VCAM-1: Evaluate vascular inflammation [21] [22]. | Ensure validation in your specific model species and tissue. |
FAQs: Regulatory and Research Implications
Q1: What specific "black box" warnings has the FDA recently removed from Hormone Replacement Therapy (HRT) labels?
The U.S. Food and Drug Administration (FDA) is initiating the removal of most "black box" warnings from menopausal hormone therapy (MHT) products. The specific warnings being removed are those related to the risks of cardiovascular disease, breast cancer, and probable dementia [26] [27] [28]. It is important to note that the FDA is not seeking to remove the boxed warning for endometrial cancer for systemic estrogen-alone products [26] [29]. The agency is also removing the recommendation to use the lowest effective dose for the shortest duration, a guideline that had been part of the safety warnings for decades [28].
Q2: What was the primary scientific rationale behind the FDA's decision to remove these warnings?
The decision was based on a comprehensive reassessment of scientific evidence, which revealed that the initial warnings, largely based on the Women's Health Initiative (WHI) study from the early 2000s, were misleading for the typical MHT patient [26] [30]. Key rationales include:
- Age Discrepancy: The average age of women in the WHI study was 63, over a decade past the average age of menopause onset (51 years). The health risks observed in this older cohort do not accurately reflect the risk-benefit profile for younger, healthier women (typically ages 45-55) initiating MHT for symptom relief [26] [28].
- Outdated Formulations: The WHI study used a specific hormone formulation (conjugated equine estrogen with medroxyprogesterone acetate) that is no longer in common use. Contemporary formulations, such as transdermal estradiol and micronized progesterone, have been shown to carry a lower risk profile [5] [31] [32].
- Updated Evidence: A reanalysis of data and newer studies focusing on younger women who start therapy within 10 years of menopause onset shows a more favorable benefit-risk ratio, including potential reductions in all-cause mortality and fracture risk [27] [28].
Q3: How does the timing of HRT initiation influence cardiovascular risk, and what is the new FDA recommendation?
Extensive research now supports the concept of a "critical window of opportunity" for initiating HRT. When started in younger women (under age 60 or within 10 years of menopause onset), HRT has been associated with a reduction in all-cause mortality and a 50% reduction in heart attack risk [26] [27] [5]. The FDA's updated labeled recommendation reflects this, advising consideration of starting systemic hormone therapy for moderate to severe vasomotor symptoms in women < 60 years old or < 10 years since menopause onset [27] [28]. Initiating therapy beyond this window or in older women does not demonstrate the same cardiovascular benefits and may carry increased risks [5] [33].
Q4: What are the critical experimental variables when designing studies to evaluate the safety of different HRT formulations?
When designing preclinical and clinical studies for HRT safety, researchers must account for several critical variables to avoid the confounding factors that plagued earlier research. The following table outlines key parameters that should be standardized and reported.
Table: Key Experimental Variables for HRT Formulation Safety Studies
| Variable Category | Specific Parameters to Control | Research Rationale |
|---|---|---|
| Hormone Formulation | Type of estrogen (e.g., estradiol vs. CEE); Type of progestogen (e.g., MPA vs. micronized progesterone) [5] [32]. | Synthetic vs. bio-identical formulations have different metabolic and thrombotic risk profiles [5] [31]. |
| Delivery Route | Oral vs. transdermal (patch, gel) vs. local (cream, ring) [5] [30]. | Route impacts first-pass liver metabolism, significantly affecting lipid profiles, clotting factor production, and inflammatory markers [5] [30]. |
| Subject Demographics | Age and time since menopause onset (categorized as <10 years vs. >10 years) [27] [5] [28]. | Age and menopausal status are primary determinants of vascular response to hormone therapy [5]. |
| Baseline CV Risk | Blood pressure, lipid profiles, presence of subclinical atherosclerosis (e.g., CAC score) [5]. | Baseline cardiovascular health modifies the individual's risk-benefit calculation from HRT [5]. |
| Study Duration | Short-term (symptom relief) vs. long-term (chronic disease prevention) follow-up [30] [32]. | Risks like breast cancer show a slow, incremental increase primarily with prolonged use (>4-5 years) [30]. |
Q5: Which signaling pathways are implicated in the differential cardiovascular effects of oral versus transdermal estrogen?
The cardiovascular effects of estrogen are mediated primarily through Estrogen Receptors (ERα and ERβ) but are significantly modulated by the route of administration. Oral estrogen undergoes first-pass metabolism in the liver, leading to disproportionate effects on hepatic protein synthesis. In contrast, transdermal delivery provides a more physiological hormonal level that avoids this first-pass effect. The diagram below illustrates the key divergent pathways.
Q6: What methodologies are recommended for assessing the impact of HRT on subclinical atherosclerosis in research settings?
To evaluate the effect of HRT on atherosclerosis progression, a multi-modal approach using imaging and biomarker analysis is recommended. The workflow below provides a detailed protocol.
Protocol: Assessing HRT Impact on Subclinical Atherosclerosis
Objective: To quantify the change in subclinical atherosclerotic burden in response to different HRT formulations over a 12-24 month period.
Step 1: Baseline Subject Characterization
- Recruitment: Enroll women aged 45-55 within 6-36 months of menopause onset.
- Clinical Data: Collect full medical history, medication use, and menopausal status.
- Biomarker Panel: Measure fasting lipids (LDL-C, HDL-C, Triglycerides), Lipoprotein(a) [Lp(a)], HbA1c, fasting insulin, and high-sensitivity CRP [5].
Step 2: Baseline Vascular Imaging
- Coronary Artery Calcium (CAC) Scoring: Non-contrast CT scan to quantify calcified plaque. A CAC score of >0 indicates presence of subclinical atherosclerosis [5].
- Carotid Intima-Media Thickness (CIMT): High-resolution B-mode ultrasound to measure the thickness of the inner two layers of the carotid artery. Increased CIMT is a validated marker of atherosclerosis and predictor of future events [5].
Step 3: Randomization and Intervention
- Randomize subjects into study groups (e.g., oral estrogen vs. transdermal estrogen vs. placebo, all combined with micronized progesterone if uterus present).
- Standardize the progestogen component to isolate the effect of the estrogen formulation and delivery route.
Step 4: Follow-up and Endpoint Analysis
- Duration: 12-24 months.
- Repeat Biomarkers: Collect the same biomarker panel at 6-month intervals.
- Repeat Imaging: Perform follow-up CIMT at 12 and 24 months. CAC scoring may be repeated at 24 months due to its slower progression.
- Primary Endpoint: Mean change in CIMT from baseline to study conclusion.
- Secondary Endpoints: Changes in CAC score, lipid levels, Lp(a), and inflammatory markers.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for HRT Formulation and Cardiovascular Risk Research
| Research Reagent / Material | Function and Application |
|---|---|
| 17β-Estradiol (Bio-identical) | The primary experimental estrogen used to study physiological ER signaling; available for creating oral, transdermal, and subcutaneous formulations [5] [32]. |
| Medroxyprogesterone Acetate (MPA) vs. Micronized Progesterone | Critical for comparative safety studies. MPA is a synthetic progestin linked to higher breast cancer and CVD risk in WHI, while micronized progesterone is bio-identical and associated with a lower risk profile [5] [31]. |
| Transdermal Delivery Patches (Matrix/Reservoir) | Enables the study of route-dependent effects by delivering hormones directly through the skin, bypassing first-pass liver metabolism and its associated impacts on clotting factors and lipids [5] [30]. |
| ERα and ERβ-Specific Agonists/Antagonists | Pharmacological tools to dissect the distinct roles of estrogen receptor subtypes in cardiovascular tissues, helping to elucidate mechanisms and identify potential therapeutic targets [5]. |
| Human Hepatocyte Cell Lines (e.g., HepG2) | In vitro models for screening the impact of different hormone formulations on hepatic protein synthesis, including the production of SHBG, clotting factors, and CRP [5]. |
| Lipoprotein(a) [Lp(a)] Assay | A key biomarker assay. Menopause causes a ~25% increase in Lp(a), a strong independent risk factor for ASCVD. Oral estrogen can lower Lp(a) levels by 20-30%, providing a mechanistic endpoint [5]. |
Experimental Pathway for HRT Personalization
The ultimate goal of modern HRT research is to move beyond a one-size-fits-all approach. The following diagram outlines a logical framework for developing a personalized HRT strategy based on an individual's metabolic and cardiovascular risk profile.
A Precision Framework for HRT: Integrating Risk Assessment, Biomarkers, and Personalized Protocols
The historical "one-size-fits-all" approach to Menopause Hormone Therapy (MHT) has evolved into a paradigm of personalized medicine, driven by evidence that the cardiovascular (CV) effects of MHT are highly dependent on patient-specific factors. Research consistently demonstrates that the benefit-risk profile of MHT is not uniform but is significantly influenced by a woman's age, time since menopause, and baseline cardiovascular risk [5] [34]. The seminal Women's Health Initiative (WHI) study, which reported increased risks of coronary heart disease and stroke, primarily enrolled older, postmenopausal women (mean age 63) [35]. Subsequent analyses revealed that these risks are not necessarily applicable to younger women (aged 50-59) initiating therapy closer to the onset of menopause [5]. This understanding forms the core rationale for developing and implementing sophisticated stratification algorithms in clinical trials and therapeutic decision-making. Proper stratification is no longer a mere research enhancement; it is a critical component for accurate safety assessment, efficacy evaluation, and the ultimate individualization of care for persons experiencing menopause.
Core Stratification Parameters and Their Quantitative Foundations
An effective stratification algorithm is built upon three foundational, interdependent pillars. The quantitative changes in CV risk factors associated with both menopause and MHT provide the essential data for constructing these models.
Table 1: Quantitative Effects of Menopause and MHT on Key Cardiovascular Risk Factors
| Risk Factor | Effect of Menopause | Effect of MHT (Varies by Formulation) |
|---|---|---|
| Blood Pressure (BP) | Systolic BP ↑ 4–7 mm Hg; Diastolic BP ↑ 3–5 mm Hg [5] | Oral estrogen: ↓ SBP by 1–6 mm Hg; Transdermal estrogen: ↓ DBP by up to 5 mm Hg [5] |
| Lipid Profile | Total cholesterol ↑ 10–14%; LDL ↑ 10–20 mg/dL; ApoB ↑ 8–15% [5] | Oral estrogen: ↓ LDL (9–18 mg/dL), ↑ HDL; Transdermal: more favorable for triglycerides [5] |
| Insulin Resistance | Odds Ratio for insulin resistance: 1.40–1.59; HbA1c ↑ by ~5% [5] | ↑ Insulin sensitivity; ↓ HbA1c by up to 0.6%; ↓ fasting glucose by ~20 mg/dL [5] |
| Body Composition | ↑ Visceral and pericardial fat deposition [5] | Modest ↓ in visceral fat and BMI (~1 kg/m²); preserves lean tissue mass [5] |
| Lipoprotein(a) [Lp(a)] | ↑ by ~25% during menopause; significantly ↑ ASCVD risk at levels >50 mg/dL [5] | Oral estrogen ↓ Lp(a) by 20–30% [5] |
The Critical Window: Age and Time Since Menopause
The "timing hypothesis" is central to modern MHT stratification. Initiating therapy in women younger than 60 or within 10 years of menopause onset is associated with a more favorable CV risk profile, potentially allowing stabilization of vulnerable atherosclerotic plaque before advanced disease is present [5] [34]. Conversely, initiating MHT in women over 60 or more than 10 years post-menopause may pose higher risks, as this population is more likely to have established subclinical atherosclerosis, which can be destabilized by hormonal therapy [35].
Comprehensive Baseline Cardiovascular Risk Assessment
A thorough baseline assessment extends beyond age. A structured evaluation should include [5] [34]:
- Traditional CV Risk Factors: A full lipid panel (LDL, HDL, triglycerides), blood pressure measurement, fasting glucose/HbA1c, and smoking status.
- Risk-Enhancing Factors: This includes female-specific conditions like pre-eclampsia and premature menopause, as well as elevated Lipoprotein(a) [Lp(a)] levels. Universal screening for Lp(a) is recommended, as levels rise during menopause and significantly increase atherosclerotic cardiovascular disease (ASCVD) risk [5].
- Assessment for Subclinical Atherosclerosis: For women with uncertain risk or risk-enhancing factors, imaging such as Coronary Artery Calcium (CAC) scoring can directly quantify plaque burden. A CAC score of zero denotes low risk, whereas a high score may contraindicate MHT or necessitate aggressive risk factor modification prior to consideration [5].
MHT Formulation and Route of Administration
The choice of hormone formulation is a modifiable risk factor within the algorithm. Contemporary research indicates that low-dose transdermal estradiol and micronized progesterone have a more favorable metabolic and cardiovascular risk profile compared to older oral synthetic formulations like conjugated equine estrogen (CEE) and medroxyprogesterone acetate (MPA) [5] [34]. Transdermal estrogen avoids the first-pass liver metabolism, resulting in less activation of the renin-angiotensin system and a lower risk of venous thromboembolism and stroke compared to oral formulations [5] [36].
Experimental Protocol: Implementing a Stratification Workflow
This protocol provides a step-by-step methodology for integrating a stratification algorithm into an MHT clinical trial or a structured clinical practice.
Step 1: Participant Enrollment and Initial Categorization
- Recruit eligible participants based on the study's inclusion/exclusion criteria (e.g., menopausal status, symptom severity).
- At baseline, document precise age and calculate "time since menopause" (TSM), defined as the time elapsed since the final menstrual period (FMP). Categorize participants as either "Early" (< 10 years from FMP and age < 60) or "Late" (≥ 10 years from FMP or age ≥ 60) [5].
Step 2: Comprehensive Baseline Cardiovascular Risk Profiling
- Collect data on all traditional CV risk factors (see Table 1).
- Phlebotomy: Measure lipid panel (LDL-C, HDL-C, Triglycerides), HbA1c, and Lp(a).
- Conduct physical measurements: Blood pressure, BMI, waist circumference.
- Obtain a detailed personal and family medical history, focusing on female-specific risk enhancers (e.g., history of pre-eclampsia, gestational diabetes, premature ovarian insufficiency).
Step 3: Advanced Risk Stratification via CAC Scoring (If Indicated)
- For participants in the "Late" category or those in the "Early" category with risk-enhancing factors, perform a non-contrast Cardiac CT for CAC scoring [5].
- Stratify participants into risk sub-groups based on Agatston score:
- CAC = 0: Low risk.
- CAC 1-100: Moderate risk.
- CAC >100: High risk.
Step 4: Stratum-Specific MHT Assignment
- Assign MHT formulation and dose based on the stratified group:
- "Early" + Low CV Risk: Consider standard-dose transdermal estradiol + micronized progesterone.
- "Early" + Moderate/High CV Risk or "Late" + CAC=0: Consider low-dose transdermal estradiol + micronized progesterone.
- "Late" + CAC >100: Generally avoid systemic MHT; consider non-hormonal alternatives or low-dose vaginal estrogen for local symptoms [5] [35].
Step 5: Ongoing Monitoring and Endpoint Adjudication
- Monitor CV risk factors at regular intervals (e.g., 3, 6, 12 months).
- Adjudicate primary CV endpoints (e.g., myocardial infarction, stroke, venous thromboembolism) by a blinded clinical endpoints committee.
- Analyze outcomes within and across pre-specified strata to assess the algorithm's predictive power.
The following workflow diagram visualizes this stratified approach to MHT decision-making.
Frequently Asked Questions (FAQs) and Troubleshooting Guide
FAQ 1: What is the single most important stratification variable to prevent CV adverse events in MHT trials? While all three core parameters are crucial, time since menopause is arguably the most critical. The accelerated increase in CVD risk after menopause is driven by hormonal, metabolic, and vascular changes. Initiating MHT in the "early" phase (within 10 years of menopause) appears to be key to avoiding the harm demonstrated in earlier trials that enrolled older, postmenopausal women with likely established atherosclerosis [5] [34].
FAQ 2: How do we handle stratification for participants with premature ovarian insufficiency (POI)? Women with POI (menopause before age 40) represent a special population. They have a prolonged state of estrogen deficiency, leading to significantly higher long-term risks of CVD, osteoporosis, and cognitive decline [37]. The stratification algorithm does not apply to them in the same way. For these individuals, MHT is generally recommended until the average age of natural menopause (~51 years) to mitigate these long-term risks, regardless of "time since menopause" [37].
FAQ 3: We are seeing an imbalance in CV events between study arms despite randomization. What could be the cause and how can we correct for it? This is a classic problem that stratification aims to prevent. Cause: Standard randomization can, by chance, lead to an imbalance in key prognostic factors (e.g., more high-risk participants in the active treatment arm). Solution: Implement stratified randomization techniques. This involves dividing your population into strata (e.g., "Early/Low Risk," "Early/High Risk," "Late/Low Risk," etc.) and then randomizing within each stratum to ensure perfect balance across treatment arms for these critical categories [38]. For ongoing trials, stratify your analysis by these baseline risk groups to understand if the effect of MHT differs by subgroup.
FAQ 4: Our trial uses a novel MHT formulation. Can we assume it has a safer CV profile based on its biochemical effects? No. While contemporary formulations like transdermal estradiol and micronized progesterone have more favorable metabolic effects (e.g., neutral blood pressure, less pro-thrombotic), definitive evidence for improved long-term CV outcomes is still limited [5] [34]. You must still apply the same rigorous stratification and monitoring protocols. The algorithm optimizes safety within a given risk-benefit context but does not eliminate the need for vigilant safety surveillance.
FAQ 5: How should "baseline CV risk" be operationalized in a statistical analysis plan? It is best to pre-specify a composite variable. One robust method is to use the pooled cohort equations (PCEs) to calculate a 10-year ASCVD risk score for each participant at baseline. Participants can then be categorized as Low (<5%), Borderline (5-<7.5%), or Intermediate/High (≥7.5%) risk. This provides a standardized, continuous, or categorical variable for use in covariate adjustment or subgroup analysis [5].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for MHT Stratification Studies
| Item | Function/Application in Research |
|---|---|
| Micronized Progesterone | A body-identical progesterone used in contemporary MHT regimens to protect the endometrium without negating the beneficial metabolic effects of estrogen; considered to have a superior risk profile compared to synthetic progestins like MPA [5] [36]. |
| Transdermal 17β-Estradiol Patches/Gels | Deliver estradiol identical to human ovarian estradiol, bypassing first-pass liver metabolism. This results in a more favorable impact on blood pressure, triglycerides, and clotting factors compared to oral estrogens, making it the preferred formulation for CV risk stratification studies [5] [37]. |
| Lipoprotein(a) [Lp(a)] Assay | A critical diagnostic for baseline risk assessment. Lp(a) is an independent, genetic risk factor for ASCVD that rises during menopause. Its measurement is recommended for personalized risk assessment, as levels >50 mg/dL significantly enhance CV risk [5]. |
| Coronary Artery Calcium (CAC) Scan | A non-contrast CT imaging technique that quantifies calcified plaque in the coronary arteries. The Agatston score provides a direct measure of subclinical atherosclerosis burden and is a powerful tool for reclassifying CV risk, especially in older women considering MHT [5] [34]. |
| Validated Menopause-Specific Quality of Life (MENQOL) Questionnaire | A patient-reported outcome (PRO) instrument essential for quantifying the burden of vasomotor symptoms, which is the primary indication for MHT. It ensures that the therapeutic benefit is measured alongside potential risks [37]. |
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary clinical value of Coronary Artery Calcium (CAC) scoring in subclinical disease detection?
CAC scoring is a specialized CT scan that detects calcium deposits in the heart's arteries, which is a direct marker of atherosclerotic plaque buildup [39]. Its primary value lies in early risk stratification for individuals who are asymptomatic but have intermediate or uncertain risk for coronary artery disease [39]. A CAC score of zero indicates a very low future heart attack risk, while higher scores (e.g., 100-300 for moderate plaque, >300 for extensive plaque) signify progressively greater risk [39]. This allows for more personalized treatment plans, including decisions on medication use and intensity of lifestyle interventions, before clinical symptoms manifest.
FAQ 2: How does Carotid Intima-Media Thickness (CIMT) function as a biomarker, and what do its measurements signify?
CIMT is a sonographic measurement of the thickness of the inner two layers of the carotid artery wall—the intima and media [40]. It serves as a validated biomarker for subclinical atherosclerosis. An increase in CIMT represents structural changes and early plaque development in the arterial wall. Quantitative studies have established that a reduction in CIMT of 0.01 mm is associated with a 9% reduction in the risk of Major Adverse Cardiovascular Events (MACE) [41]. It is particularly useful for assessing overall vascular health and the impact of therapeutic interventions.
FAQ 3: Can these tools be used to evaluate cardiovascular risk in the context of Hormone Replacement Therapy (HRT) research?
Yes, these tools are critical for personalizing HRT based on cardiovascular risk. Research highlights significant sex-specific differences in cardiovascular risk markers [42]. For instance, in individuals without coronary artery disease (CAD), parameters like the Ankle-Brachial Index (ABI) and CIMT show a stronger inverse correlation with cardiovascular risk scores in women compared to men [42]. This evidence underscores the necessity of using sex-specific risk models. Therefore, CAC and CIMT can provide objective, quantitative data to stratify risk in women being considered for HRT, especially given that initiating HRT after age 60 or more than 10 years after menopause may increase the risk of cardiovascular events [43].
FAQ 4: What are the key methodological challenges in measuring aortic calcium, and why is it not routinely recommended for screening?
Measuring aortic calcium (e.g., in the thoracic or abdominal aorta) presents several methodological challenges that limit its current clinical utility for routine screening [40]. These include the inability of standard CT to differentiate between intimal (atherosclerotic) and medial (related to aging and other conditions) calcification, the large and heterogeneous anatomical area of the aorta leading to inconsistent measurement segments across studies, and a lack of standardized reporting methods [40]. While aortic calcification is common and associated with cardiovascular events, the evidence base is not as robust or consistent as for CAC, and thus it is not currently recommended for screening.
FAQ 5: How do modern concepts of "High-Risk Plaque" extend beyond traditional calcium scoring?
Modern cardiology has moved beyond the simplistic concept of "vulnerable plaque" prone to rupture. The current understanding, as outlined in a 2025 JACC position statement, defines "High-Risk Plaque" through a multi-factorial lens [44]. While calcium scoring measures one aspect—calcified plaque burden—the high-risk plaque concept also includes features like a thin fibrous cap, a large lipid-rich necrotic core, intraplaque inflammation, hemorrhage, and positive remodeling, many of which are not heavily calcified [44]. Advanced imaging techniques like OCT and IVUS are required to visualize these features, which, along with the overall plaque burden and the myocardial area at risk, determine the likelihood of a clinical event [44].
Troubleshooting Guides
Issue 1: Inconsistent or Unreliable CIMT Measurements
| Potential Cause | Solution |
|---|---|
| Incorrect Probe Placement | Ensure the probe is placed on the far wall of the common carotid artery, 1-2 cm proximal to the bifurcation. Use anatomical landmarks consistently. |
| High Observer Variability | Adhere to the Mannheim Consensus criteria for plaque definition. Standardize protocols across all sonographers in the study, and perform regular inter- and intra-observer variability assessments. |
| Poor Image Resolution | Use a high-frequency linear array transducer (e.g., >7 MHz). Adjust gain and depth settings to optimize image clarity of the intima-media double-line. |
Issue 2: Discrepancies Between CAC Score and Other Risk Assessments
| Potential Cause | Solution |
|---|---|
| Mismatched Risk Profiles | A high CAC score in a clinically low-risk patient underscores the value of CAC for reclassifying risk. Integrate the score with traditional risk factors (e.g., using the MESA calculator) for a comprehensive view [39]. |
| Non-Calcified Plaque | CAC scoring only detects calcified plaque. In patients with a low CAC score but high clinical suspicion, consider alternative imaging like CCTA to identify non-calcified or high-risk plaque features [44]. |
| Technical Artifacts | Verify the scan quality. Motion artifacts can affect scores. Ensure the CT scanner is properly calibrated for CAC acquisition and that the Agatston scoring method is applied correctly. |
Issue 3: Interpreting CAC Scores in Special Populations (e.g., Women, Younger Adults)
| Potential Cause | Solution |
|---|---|
| Underestimation of Risk in Women | Be aware that traditional risk scores may underestimate risk in women. CAC provides a direct measure of atherosclerotic burden. A non-zero score in a woman warrants attention, as some data suggests aortic calcium may be a particularly strong predictor in females [42] [40]. |
| Uncertainty in Younger Adults | A CAC score of zero in a young adult (<40) is common and confirms low near-term risk. However, a positive score, even if low, is a powerful marker of elevated long-term risk and should trigger aggressive preventive management. |
Data Presentation: Quantitative Scoring and Risk Stratification
Table 1: Coronary Artery Calcium (CAC) Agatston Score Interpretation [39]
| Agatston Score | Risk Category | Plaque Burden Interpretation | Clinical Implication |
|---|---|---|---|
| 0 | Very Low | No identifiable plaque | Low risk of future cardiac event; consider maintaining current prevention strategies. |
| 1 - 99 | Mild | Minimal to moderate plaque | Higher risk than zero; likely warrants risk factor modification (e.g., statins). |
| 100 - 299 | Moderate | Moderate plaque deposit | Relatively high risk of heart attack in next 3-5 years; strongly consider intensive medical therapy. |
| >= 300 | High | Extensive plaque burden | Highest risk category; indicates widespread atherosclerotic disease and need for aggressive treatment. |
Table 2: Association Between Vascular Parameters and MACE Risk Reduction [41]
| Biomarker | Measured Change | Associated MACE Risk Reduction | Notes / Context |
|---|---|---|---|
| Percent Atheroma Volume (PAV) | 1% absolute decrease | 25% | Measured via IVUS or CCTA; a key efficacy endpoint in drug trials (e.g., YN001). |
| Carotid IMT | 0.01 mm decrease | 9% | Measured via ultrasound; a surrogate endpoint for cardiovascular risk. |
| Total Atheroma Volume (TAV) | Significant decrease | Reduced Risk | Absolute volume change is also a critical indicator of therapeutic efficacy. |
Experimental Protocols
Protocol 1: Standardized Methodology for Coronary Artery Calcium (CAC) Scoring
Principle: To non-invasively quantify the burden of coronary artery calcification using non-contrast cardiac CT, expressed as an Agatston score.
Materials: CT scanner with cardiac gating capability, ECG monitor, workstations with validated CAC scoring software.
Procedure:
- Patient Preparation: Instruct the patient to avoid smoking and caffeine for several hours before the scan to stabilize heart rate [39].
- Patient Positioning: Position the patient supine on the scanner table. Apply adhesive electrode patches on the chest (and sometimes arms/legs) for ECG monitoring [39].
- Scan Acquisition: Perform a non-contrast, prospectively ECG-triggered CT scan of the heart during a single breath-hold. The scan typically covers from the carina to the diaphragm. The tube voltage is usually 120 kVp.
- Image Reconstruction: Reconstruct images with a standard kernel and a slice thickness of 3 mm.
- Calcium Scoring: On a dedicated workstation, a trained technologist or physician identifies and traces regions of interest with a density ≥130 Hounsfield Units within the coronary arteries. The software calculates the total Agatston score, which is the product of the calcified plaque area and a density factor [39].
- Quality Control: Ensure the scan is free from significant motion artifacts and that all coronary arteries (Left Main, Left Anterior Descending, Left Circumflex, Right Coronary) have been adequately assessed.
Protocol 2: Standardized Methodology for Carotid Intima-Media Thickness (CIMT) Measurement
Principle: To obtain high-resolution ultrasound measurements of the intima-media complex of the far wall of the common carotid artery as a surrogate marker of subclinical atherosclerosis.
Materials: High-resolution ultrasound system with a linear array transducer (≥7 MHz), patient examination table, coupling gel.
Procedure:
- Patient Preparation: The patient rests in a supine position with the neck slightly extended for 5-10 minutes before the examination.
- Artery Interrogation: Using the ultrasound transducer, locate the common carotid artery. Identify the key anatomical landmarks: the flow divider of the carotid bulb and the straight segment of the common carotid artery 1-2 cm proximal to the bulb.
- Image Optimization: Adjust depth, gain, and focus to achieve a clear, longitudinal view of the far wall of the common carotid artery. The characteristic "double-line" pattern of the intima-media boundaries must be visible.
- Image Acquisition: Acquire cine loops or still images of the far wall from multiple angles (e.g., anterior, lateral, and posterior). Perform measurements on both the left and right arteries.
- Offline Analysis: Use automated edge-detection software to measure the distance between the lumen-intima and media-adventitia interfaces. The result is typically expressed as the mean of the maximum CIMT across all measured segments.
- Plaque Assessment: During the scan, note the presence of any focal plaque, defined as a focal structure encroaching into the arterial lumen by at least 0.5 mm or 50% of the surrounding CIMT value, or with a thickness of >1.5 mm [40].
Visualization: Experimental Workflows and Pathophysiological Concepts
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Vascular Biomarker Research
| Item / Category | Function in Research | Example Application |
|---|---|---|
| CT Scanner with Cardiac Gating | Acquires motion-free images of the heart for precise quantification of coronary calcium. | Essential for performing CAC scoring according to standardized protocols. |
| Agatston Scoring Software | Automates the identification and calculation of calcified plaque area and density. | The standard software for deriving the CAC Agatston score from CT DICOM images. |
| High-Frequency Linear Ultrasound | Provides high-resolution images of superficial arteries for precise wall thickness measurement. | Required for acquiring high-quality images for CIMT and carotid plaque assessment. |
| Automated CIMT Edge-Detection Software | Reduces observer variability by automatically detecting the intima-media boundaries. | Used for objective and reproducible analysis of CIMT from ultrasound cine loops. |
| Intravascular Ultrasound (IVUS) | An invasive catheter-based technique providing high-resolution, cross-sectional images of coronary arteries from inside the vessel. | Used in clinical trials to precisely measure changes in total atheroma volume (TAV) and percent atheroma volume (PAV) [44] [41]. |
| Optical Coherence Tomography (OCT) | An invasive catheter-based technique offering ultra-high resolution (micrometer-level) for detailed plaque characterization. | Used to identify high-risk plaque features like thin fibrous caps, macrophages, and cholesterol crystals [44]. |
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1.1: What is the primary genetic rationale for incorporating estrogen-responsive variants into a polygenic risk score (PRS) for cardiovascular and metabolic risk assessment? Estrogen signaling directly influences cardiovascular and metabolic health through complex pathways. The biological rationale is that individuals carry numerous genetic variants that modulate how their bodies respond to estrogen. A PRS that aggregates these variants can provide a stable, lifelong measure of an individual's inherent sensitivity to estrogen, which is crucial for understanding their baseline risk and potential response to hormone-related therapies. This is superior to single-time hormone level measurements, which are highly dynamic. Key pathways involved include estrogen receptor signaling in vascular endothelium, lipid metabolism regulation, and insulin sensitivity modulation [45] [5].
FAQ 1.2: Our PRS for estrogen-responsive genes shows a significant association in initial cohorts but fails to validate in an external dataset. What are the primary factors we should investigate? This is typically due to three main factors:
- Ancestral Heterogeneity: PRS derived from genome-wide association studies (GWAS) in one ancestral population (e.g., European) often show reduced performance in other populations due to differences in linkage disequilibrium and allele frequencies [46]. Solution: Ensure your validation cohort is ancestrally matched to your discovery cohort, or use cross-ancestry PRS methods.
- Phenotype Heterogeneity: The definition of "estrogen response" or the clinical endpoint (e.g., "cardiovascular risk") may differ between cohorts. Solution: Harmonize phenotype definitions strictly across cohorts. For composite outcomes, ensure sub-phenotypes are balanced.
- Technical Batch Effects: Differences in genotyping arrays, imputation quality, or sample processing can introduce noise. Solution: Apply stringent quality control metrics uniformly and re-genotype a subset of samples if necessary.
FAQ 1.3: When integrating a PRS with clinical risk factors like menopausal status, should we assume a multiplicative or additive model? Current evidence, particularly from large-scale breast cancer PRS studies, generally supports a multiplicative model [47]. This means the relative risk imparted by the PRS is consistent across different strata of clinical risk factors. For example, the odds ratio per standard deviation of the PRS is similar for pre- and post-menopausal women. You can test this in your data using likelihood ratio tests comparing models with and without an interaction term between the PRS and the clinical factor [47].
FAQ 1.4: How do we account for the differential effects of various hormone therapy (HT) formulations in our genetic risk model? This requires careful modeling. Different HT formulations (e.g., oral vs. transdermal estrogen, synthetic vs. micronized progesterone) have distinct metabolic and cardiovascular risk profiles [5]. Your analysis should:
- Stratify by Formulation: Treat different HT types as separate exposures in your model.
- Incorporate Dosage: Where possible, model dose as a continuous or ordinal variable.
- Include Interaction Terms: Test for statistical interaction between the PRS and the specific HT formulation. For instance, a high genetic risk might be more strongly associated with adverse outcomes with oral synthetic therapy compared to transdermal estrogen [5].
FAQ 1.5: What is the recommended method for validating a newly developed estrogen-responsive PRS before clinical application? A robust validation pipeline involves:
- External Validation: Test the PRS in one or more independent cohorts that were not used in the PRS development. This assesses generalizability [48] [46].
- Prognostic Validation: Demonstrate that the PRS predicts future incidents of the disease or trait of interest (e.g., coronary artery disease, breast cancer) in a prospective study design [49].
- Clinical Utility Validation: Show that the PRS, when added to existing clinical risk models (e.g., PREVENT for CVD), improves risk classification metrics like the Net Reclassification Improvement (NRI) [49]. Evidence shows that adding PRS to the PREVENT tool improved NRI by 6%, correctly reclassifying millions of individuals in the US [49].
Data Synthesis: Quantitative Findings
Table 1: Association of Early Menopause with Cardiometabolic Syndrome (CMS) Components and Cardiovascular Disease (CVD) Risk. Data synthesized from meta-analyses and large cohort studies. [50]
| Risk Factor / Outcome | Comparison Group | Effect Size (95% CI) | P-value |
|---|---|---|---|
| Hypertension Risk | Early Menopause (<45) vs. Later Menopause | OR 1.10 (1.01 - 1.19) | p = 0.03 |
| Type 2 Diabetes Risk | Early Menopause vs. Menopause at 45-55 | OR 1.15 (1.04 - 1.26) | p = 0.003 |
| Waist Circumference | Premature Menopause vs. Controls | MD 1.78 cm (0.74 - 2.83) | p = 0.0008 |
| Total Cholesterol | Premature Menopause vs. Controls | MD 17.60 mg/dL (10.83 - 24.38) | p < 0.00001 |
| Coronary Heart Disease | Premature Menopause vs. Later Menopause | RR 1.52 (1.22 - 1.91) | Not Reported |
| Myocardial Infarction | Premature Menopause (Korean Cohort) vs. ≥50 yrs | HR 1.40 (1.31 - 1.50) | Not Reported |
| Ischemic Stroke | Premature Menopause (Korean Cohort) vs. ≥50 yrs | HR 1.24 (1.17 - 1.31) | Not Reported |
Table 2: Differential Effects of Menopause Hormone Therapy (MHT) Formulations on Cardiovascular Risk Factors. [5]
| Risk Factor | Effect of Oral Estrogen (CEE) | Effect of Transdermal Estrogen | Key Considerations |
|---|---|---|---|
| Blood Pressure | ↓ SBP by 1-6 mm Hg | ↓ DBP by up to 5 mm Hg; more neutral effect | Combined therapy (with progesterone) may increase SBP. |
| Lipid Profile | ↓ LDL (9-18 mg/dL); ↑ HDL; ↑ Triglycerides | More favorable triglyceride profile (less elevation) | Oral estrogen's effect on lipids does not translate to overall CVD risk reduction. |
| Insulin Resistance | ↑ Insulin sensitivity; ↓ HbA1c (up to 0.6%) | Similar benefits | Effects are dose and formulation dependent, most pronounced with early initiation. |
| Thrombotic Risk | ↑ Risk of Venous Thromboembolism (VTE) | Lower risk than oral formulations | Risk is dose-dependent. |
| Myocardial Infarction | CEE+MPA formulation ↑ risk (HR 1.29) | Safer profile than oral | Age and time since menopause initiation critical for risk. |
Experimental Protocols & Methodologies
Protocol 3.1: Development of a Polygenic Risk Score for an Estrogen-Responsive Trait
This protocol outlines the key steps for constructing a PRS, based on methods used in recent studies linking genetic risk for hormone levels to hippocampal volume and breast cancer aggressiveness [45] [48].
1. GWAS Summary Statistics:
- Objective: Obtain effect sizes (beta coefficients, odds ratios) and p-values for genetic variants from a large-scale GWAS. The foundational GWAS for reproductive hormones by Ruth et al. (2016) involved 2,913 individuals [45].
- Procedure: Use pre-existing, publicly available summary statistics from consortia like BCAC or UK Biobank. Ensure the GWAS phenotype is relevant (e.g., circulating estradiol levels, breast cancer risk).
2. Target Genotype Data:
- Objective: Acquire genotype data for your study cohort where the PRS will be applied and validated.
- Procedure: Genotype study participants using high-density arrays (e.g., OncoArray, iCOGS). Perform stringent quality control (QC): call rate >98%, Hardy-Weinberg equilibrium p > 1x10⁻⁶, minor allele frequency checks. Impute to a reference panel (e.g., 1000 Genomes) to increase genomic coverage [47] [48].
3. PRS Construction:
- Objective: Calculate an individual-level score that sums the trait-associated alleles, weighted by their effect sizes from the GWAS.
- Procedure:
- Clumping and Thresholding: Prune SNPs in linkage disequilibrium (LD) (e.g., r² < 0.1 within a 250kb window). Construct scores at multiple p-value thresholds (e.g., PT < 0.001, 0.05, 0.1, 0.5, 1).
- Advanced Methods: Apply methods like PRS-CS or LDpred which use Bayesian shrinkage to model LD and effect sizes more continuously, often improving performance [46].
- Formula: ( PRSi = \sum{j=1}^{M} \betaj * G{ij} ) where ( \betaj ) is the effect size of SNP j from the GWAS, and ( G{ij} ) is the allele count (0,1,2) for SNP j in individual i.
4. Validation:
- Objective: Determine the predictive performance of the PRS.
- Procedure:
- Internal Validation: Use 5-fold cross-validation within your cohort to select the optimal p-value threshold or tuning parameter, preventing overfitting [48].
- External Validation: Test the best-fit PRS in a completely independent cohort.
- Association Analysis: Use linear regression (for continuous traits) or logistic regression (for case-control status) to test the association between the standardized PRS and your outcome, adjusting for age, genetic ancestry (principal components), and other relevant covariates [45].
Protocol 3.2: Testing PRS-Clinical Risk Factor Interactions in Hormone Therapy Context
This protocol details how to assess whether the effect of a PRS is modified by clinical factors like HT use, based on methodologies from BCAC and cardiovascular risk studies [47] [49].
1. Study Population:
- Clearly define your exposure (HT use), including formulation, dose, and duration. Stratify users by type (e.g., estrogen-only vs. combined, oral vs. transdermal).
2. Statistical Model:
- Fit a regression model that includes an interaction term between the PRS and the HT variable.
- Model Example (Logistic Regression):
Logit(Outcome) = β₀ + β₁(PRS) + β₂(HT) + β₃(PRS * HT) + Covariates - Here, ( β₃ ) is the interaction coefficient. A significant ( β₃ ) indicates that the effect of the PRS on the outcome differs by HT status.
3. Stratified Analysis:
- If an interaction is detected, conduct analyses separately within HT user and non-user groups to report stratum-specific effects.
4. Goodness-of-Fit Test:
- Perform a likelihood ratio test comparing the full model (with interaction term) to a reduced model (without interaction term) to formally assess the improvement in model fit. Use a stringent significance threshold (e.g., Bonferroni-corrected) to account for multiple testing [47].
Signaling Pathways & Experimental Workflows
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Resources for PRS Development and Validation.
| Item / Resource | Function / Application | Key Considerations |
|---|---|---|
| GWAS Summary Statistics | Source of SNP effect sizes and p-values for PRS weight calculation. | Ensure ancestry match with target cohort. Use large, well-powered studies (e.g., from BCAC, GIANT, CKDGen). |
| Genotyping Arrays | High-throughput platform for genotyping target cohort samples. | Select arrays with good genome-wide coverage (e.g., Global Screening Array, OncoArray). Imputation is typically required. |
| Imputation Reference Panels | To infer ungenotyped variants, increasing SNP density for PRS. | TOPMed or 1000 Genomes Project panels offer high imputation accuracy. |
| PRS Calculation Software | Implements algorithms to construct the score from genotypes and weights. | PLINK: Basic clumping/thresholding. PRS-CS/LDpred2: Advanced, continuous shrinkage methods for improved accuracy. |
| Statistical Software (R/Python) | For data QC, association testing, and interaction analysis. | Essential packages: bigsnpr (R for LDpred2), PLINK2, statsmodels (Python). |
| Validated Clinical Endpoints | Precisely defined phenotypes for association testing (e.g., MI, stroke, T2D). | Harmonization of endpoint definitions across discovery and validation cohorts is critical to avoid misclassification. |
Leveraging AI and Machine Learning for Predictive Risk Modeling and Dosage Optimization in HRT
Core Concepts in AI for HRT Research
This section outlines the fundamental principles for applying artificial intelligence (AI) and machine learning (ML) to individualize Hormone Replacement Therapy (HRT) based on metabolic and cardiovascular risk factors.
The Clinical Rationale for Personalization
The menopausal transition triggers significant metabolic and cardiovascular changes, including alterations in lipid profiles, increased insulin resistance, and a shift towards visceral adiposity, which collectively elevate the risk of chronic diseases [51] [5] [52]. Traditional, population-wide HRT dosing strategies often fail to account for this inter-individual variability in risk factors and treatment response. AI and ML models can integrate multi-modal data—from electronic health records (EHRs), genomic sequencing, medical imaging, and wearable sensors—to move HRT from a one-size-fits-all approach to a personalized, predictive strategy [51]. This is encapsulated by the "timing hypothesis," where initiating therapy within ten years of menopause onset and before age 60 is critical for optimizing the benefit-risk profile, particularly for cardiovascular outcomes [5] [52].
AI and ML Model Archetypes
Different ML models are suited to specific tasks in HRT research:
- Supervised Learning: Used for prediction and classification tasks, such as forecasting an individual's 5-year cardiovascular risk or classifying them into high, intermediate, or low-risk categories for breast cancer based on mammogram data [53] [54].
- Deep Learning (DL) & Convolutional Neural Networks (CNNs): Primarily applied to analyze complex image data. For instance, deep convolutional neural networks can extract subtle, sub-visual patterns from mammograms to predict breast cancer risk more accurately than traditional measures like breast density [53] [54].
- Natural Language Processing (NLP): Can mine unstructured clinical notes in EHRs to identify underreported symptoms like hot flashes or mood disorders, providing a more complete picture for risk assessment [51].
Experimental Protocols & Methodologies
This section provides detailed methodologies for key experiments in AI-driven HRT research.
Developing an Image-Only AI Model for Breast Cancer Risk Stratification
This protocol details the process for creating and validating an AI model that predicts 5-year breast cancer risk from screening mammograms, a key consideration for HRT safety [53] [54].
- Objective: To train and validate a deep learning model for 5-year breast cancer risk stratification using only mammographic images, outperforming traditional risk markers like breast density.
- Materials:
- Datasets: A large, multi-site, international dataset of bilateral 2D screening mammograms. The model in the cited study was trained on 421,499 mammograms from 27 facilities across Europe, South America, and the U.S. [53] [54].
- Labels: Five-year cancer outcomes, typically extracted from tumor registries and medical records.
- Computing Infrastructure: High-performance computing clusters with modern GPUs (e.g., NVIDIA V100 or A100) to handle deep learning on high-resolution images.
- Methodology:
- Data Curation & Partitioning: Mammograms are partitioned into three independent sets: Training (~70%), Validation (~15%), and Test (~15%). The test set must be temporally and geographically distinct to ensure generalizability.
- Preprocessing: Standardize image resolution and apply intensity normalization across all mammograms. Data augmentation techniques (e.g., random rotations, flipping) may be applied to the training set to improve model robustness.
- Model Architecture & Training:
- A Deep Convolutional Neural Network (e.g., a ResNet or DenseNet architecture) is used as the core.
- The model is trained using a binary cross-entropy loss function, with the objective to output a probability of cancer development within 5 years.
- The training process involves feeding the mammograms (from women who did and did not develop cancer) to allow the model to learn discriminative tissue patterns.
- Model Calibration: The model's output probabilities are calibrated on the independent validation set to ensure they reflect true cancer incidence rates (e.g., using Platt scaling or isotonic regression).
- Validation & Analysis: The calibrated model is applied to the held-out test set. Risk categories are defined using established thresholds (e.g., National Comprehensive Cancer Network: average <1.7%, intermediate 1.7-3.0%, high >3.0%). Performance is evaluated using statistical models that account for follow-up time, and cancer incidence rates are compared across AI risk categories and breast density categories.
Building a Predictive Model for Cardiovascular Risk Post-Menopause
This protocol describes the workflow for creating a multimodal ML model to stratify cardiovascular risk in menopausal women, a crucial element for HRT decision-making [5].
- Objective: To develop an ML model that integrates clinical, laboratory, and imaging data to predict the 10-year risk of a major adverse cardiovascular event (MACE) in perimenopausal and postmenopausal women.
- Data Sources & Feature Engineering:
- Electronic Health Records (EHRs): Structured data (age, BMI, blood pressure) and unstructured data (clinical notes mined with NLP for symptoms).
- Laboratory Values: Features include LDL-C, HDL-C, Lipoprotein(a) [Lp(a)], HbA1c, and fasting glucose [5].
- Imaging Data: Features derived from Coronary Artery Calcium (CAC) scoring and carotid intima-media thickness (CIMT) [5].
- Feature Selection: Use techniques like Recursive Feature Elimination (RFE) or tree-based importance rankings to select the most predictive features for the model.
- Methodology:
- Cohort Definition: Define a retrospective cohort of menopausal women with at least 10 years of follow-up data. The primary outcome is the first occurrence of MACE (myocardial infarction, stroke, coronary revascularization).
- Data Preprocessing: Handle missing data using multiple imputation. Normalize or standardize continuous variables.
- Model Selection & Training: Train and compare multiple ML models, including:
- Cox Proportional-Hazards Model (baseline).
- Random Survival Forests (for handling non-linear relationships).
- Gradient Boosting Machines (e.g., XGBoost).
- Validation: Validate model performance using bootstrapping or time-split validation. Assess discrimination using the C-index and calibration by comparing predicted vs. observed risk.
In Silico Simulation for HRT Dosage Optimization
This protocol uses AI to model the effects of different HRT regimens on metabolic parameters.
- Objective: To simulate the impact of various transdermal estradiol doses, with and without micronized progesterone, on key metabolic outcomes (e.g., LDL-C, HbA1c, systolic BP) in women with varying baseline risk profiles.
- Methodology:
- Virtual Cohort Generation: Create a in silico cohort based on real-world demographic and clinical data, mirroring the distribution of age, time-since-menopause, BMI, and baseline metabolic parameters found in populations like the Multi-Ethnic Study of Atherosclerosis (MESA) [51].
- Model Architecture: Develop a Bayesian network or a reinforcement learning model. The model learns the probabilistic relationships between patient covariates, HRT regimen (type, dose, route), and changes in metabolic outcomes from existing clinical trial and observational data.
- Simulation & Optimization: The model runs simulations across the virtual cohort for different HRT strategies. It can identify the "optimal" regimen that maximizes improvements in metabolic parameters while minimizing negative effects for specific patient subgroups (e.g., women with T2DM [7]).
Data Management & Preprocessing
Robust data management is the foundation of reliable AI models.
FAIR Data Principles
Implement the FAIR (Findable, Accessible, Interoperable, Reusable) principles. This involves using standardized ontologies for clinical terms (e.g., SNOMED CT) and ensuring rich metadata is captured for all datasets, including imaging and biomarker data [55]. As emphasized in industry practices, "If AI is to mean anything, we need to capture more than results. Every condition and state must be recorded, so models have quality data to learn from" [55].
Troubleshooting Data Quality
| Problem | Symptom | Solution |
|---|---|---|
| Missing Lab Data | Model training fails or produces biased predictions. | Implement multiple imputation techniques after assessing the pattern of missingness (e.g., Missing Completely at Random). Avoid simple mean imputation. |
| Unstructured Clinical Notes | Inability to incorporate crucial symptom data (e.g., hot flash severity). | Apply Natural Language Processing (NLP) pipelines with named entity recognition (NER) to extract specific symptoms and their context from clinical notes [51]. |
| Dataset Shift | Model performs well on training/validation data but poorly on new data from a different hospital. | Employ domain adaptation techniques during model training. Continuously monitor model performance on incoming data and retrain with new data as needed. |
| Inconsistent Imaging Data | Poor generalization of image-based AI models. | Enforce strict standardization in image acquisition protocols. Use advanced preprocessing techniques for intensity normalization and spatial alignment. |
Computational Methods & Technical Specifications
This section details the technical implementation of AI models.
Workflow for Predictive Risk Modeling
The diagram below illustrates the end-to-end workflow for developing a predictive risk model in HRT research.
Key Computational Tools & Reagents
Table: Essential Research Reagent Solutions for AI-driven HRT Studies
| Item / Reagent | Function / Explanation | Example Use Case |
|---|---|---|
| Structured EHR Data | Provides baseline clinical variables (age, BMI, BP, lab values) for model feature engineering. | Core dataset for training cardiovascular risk prediction models [51] [5]. |
| Medical Imaging Repositories | Source data for deep learning models (e.g., mammograms, CAC scans). | Training image-only AI models for breast cancer risk stratification [53] [54]. |
| Wearable Sensor Data | Enables real-time, continuous monitoring of physiological parameters (e.g., sleep, heart rate). | Capturing objective data on vasomotor symptoms like night sweats [51]. |
| Genomic & Biomarker Data | Provides information on genetic predispositions and specific protein/metabolite levels. | Incorporating Lp(a) levels or genetic variants into refined risk models [5]. |
| Python (with Scikit-learn, PyTorch/TensorFlow) | The primary programming environment for building, training, and evaluating ML/DL models. | Implementing a random survival forest for time-to-event cardiovascular data. |
| NLP Libraries (e.g., spaCy, ClinicalBERT) | Tools for processing and extracting information from unstructured clinical text. | Identifying mentions of "hot flashes" or "mood swings" in physician notes [51]. |
| SHAP (SHapley Additive exPlanations) | A game theory-based method for interpreting the output of any ML model. | Explaining which features (e.g., high Lp(a), CAC score) most influenced a high-risk prediction [5]. |
Frequently Asked Questions (FAQs)
Q1: How do we address and mitigate algorithmic bias in HRT risk models, especially against underrepresented racial or ethnic groups? A1: Bias mitigation requires a multi-pronged approach. First, intentionally curate diverse, multi-ethnic training and validation datasets that adequately represent the target population. Second, employ algorithmic fairness toolkits to audit models for disparate performance across subgroups. Techniques like adversarial de-biasing or re-weighting training data can help reduce these biases. Continuous monitoring of real-world performance after deployment is essential to identify and correct emergent biases [51].
Q2: Our deep learning model for mammography risk shows high accuracy on the test set but fails in prospective validation. What are the potential causes? A2: This is a classic sign of dataset shift. The model may have learned to recognize artifacts specific to your training data (e.g., scanner manufacturer, hospital-specific imaging protocols) rather than generalizable biological features. Solutions include:
- Domain Adaptation: Using techniques during training to make the model invariant to the data source.
- Extended Data Augmentation: Incorporating a much wider variety of image transformations.
- Prospective Fine-Tuning: Retraining the final layers of the model on a small amount of data from the new deployment site [53] [54].
Q3: What are the key regulatory and data privacy considerations when developing AI models for HRT using real-world patient data? A3: Compliance with regulations like HIPAA (in the U.S.) and GDPR (in Europe) is non-negotiable. This typically involves:
- De-identification: Strict removal of all 18 HIPAA-defined identifiers from the dataset.
- Data Anonymization / Pseudonymization: Using tokens instead of direct identifiers.
- Secure Data Environments: Conducting all analysis within a secure, access-controlled trusted research environment (TRE). Federated learning, where the model is sent to the data instead of moving the data, is an increasingly popular strategy to maintain privacy [51] [55].
Q4: How can we validate that our AI model for HRT dosage optimization leads to clinically meaningful improvements, not just statistical significance? A4: Move beyond standard metrics. Design a prospective, randomized controlled trial (RCT) where patients are stratified by the AI model's recommendation. The primary endpoint should be a clinically relevant outcome, such as:
- Reduction in moderate-to-severe vasomotor symptoms.
- Improvement in a composite score of metabolic syndrome components.
- Increase in medication adherence rates. Comparing these hard endpoints between "AI-guided dosing" and "standard of care" groups provides the highest level of evidence for clinical utility [7].
Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
FAQ 1: What are the key pharmacokinetic advantages of transdermal estrogen over oral formulations? Transdermal estrogen offers several key advantages by bypassing first-pass liver metabolism. This results in more stable serum hormone levels and avoids the high concentrations of estrogen metabolites produced in the liver. Crucially, it reduces the production of liver-synthesized clotting factors and inflammatory markers, leading to a lower risk of venous thromboembolism (VTE) compared to oral formulations [5] [56]. It also has more favorable effects on blood pressure, with transdermal estrogen decreasing diastolic blood pressure by up to 5 mm Hg, while combined oral therapy can increase systolic blood pressure [5].
FAQ 2: How does the progestogen component in HRT influence metabolic risk profiles? The choice of progestogen significantly impacts metabolic and cardiovascular risk. Synthetic progestins, such as medroxyprogesterone acetate (MPA), have been associated with adverse cardiovascular effects and a higher risk of breast cancer [56]. In contrast, bioidentical micronized progesterone has a more favorable risk profile, with minimal impact on blood pressure and lipid metabolism, and is preferred for its neutral metabolic effects, especially in women with higher cardiovascular risk [5] [56].
FAQ 3: What evidence supports the use of bioidentical hormones, and how do they differ from compounded preparations? Bioidentical hormones approved by the FDA, such as micronized 17β-estradiol and micronized progesterone, have the same molecular structure as endogenous human hormones and are manufactured under strict regulatory standards [37] [56]. They are effective for managing vasomotor and genitourinary symptoms and preserving bone density [56]. Compounded bioidentical hormone therapies are not FDA-approved, lack standardized dosing, and have variable potency and purity. Major professional organizations recommend FDA-approved formulations over custom-compounded products due to a lack of high-quality safety and efficacy data for the latter [57].
FAQ 4: What is the "timing hypothesis," and how does it influence MHT initiation? The "timing hypothesis" suggests that the cardiovascular effects of Menopause Hormone Therapy (MHT) depend on when therapy is initiated relative to the onset of menopause. Initiating MHT in younger women (typically under 60 or within 10 years of menopause) may potentially have neutral or cardioprotective effects on the vasculature [5]. In contrast, starting MHT later in older, postmenopausal women with existing subclinical atherosclerosis is associated with an increased risk of coronary heart disease and stroke, as demonstrated in early trials like the Women's Health Initiative [5].
Troubleshooting Guide: Addressing Common Research and Clinical Challenges
Challenge 1: Interpreting Varied Cardiovascular Outcomes in MHT Trials
- Problem: Inconsistent findings on cardiovascular risk between observational studies and randomized controlled trials.
- Solution: Carefully account for the formulation, route, and timing of therapy. Older trials used specific synthetic oral formulations (CEE with MPA) in older participants, whereas contemporary studies using transdermal estradiol and micronized progesterone in younger women show more neutral or favorable cardiovascular risk profiles [5]. Always stratify results by participant age, time since menopause, and baseline cardiovascular health.
Challenge 2: Ensuring Endometrial Safety in Research Protocols
- Problem: Unopposed estrogen therapy in women with an intact uterus increases the risk of endometrial hyperplasia and cancer.
- Solution: In any study design or clinical protocol involving women with a uterus, estrogen must be combined with an adequate dose and duration of a progestogen [37]. Bioidentical micronized progesterone (typically 100-200 mg/day orally) is the preferred agent for endometrial protection due to its more favorable metabolic profile compared to synthetic progestins [56].
Challenge 3: Standardizing Bioidentical Hormone Preparations in Research
- Problem: Compounded bioidentical hormones have variable potency and lack standardized dosing.
- Solution: For research purposes, prioritize the use of FDA-approved bioidentical hormones (e.g., micronized estradiol and progesterone) to ensure consistency, reliability, and reproducibility of results [57]. Independent testing has confirmed significant variability in the hormone content of compounded preparations, which can confound research outcomes [57].
Table 1: Metabolic and Cardiovascular Risk Profiles of Different MHT Formulations
| Risk Factor / Metric | Oral Estrogen (CEE) | Transdermal Estradiol (≤ 50 mcg) | Bioidentical Micronized Progesterone | Synthetic Progestin (MPA) |
|---|---|---|---|---|
| VTE Risk | Increased [56] | Neutral / Lower Risk [56] | Not Established | Increased (with oral estrogen) [56] |
| Blood Pressure | ↓ SBP by 1-6 mm Hg; Combined therapy may ↑ SBP [5] | Neutral / ↓ DBP by up to 5 mm Hg [5] | Neutral [5] | May ↑ SBP in combined therapy [5] |
| Lipid Profile | ↓ LDL (9-18 mg/dL); ↑ HDL; ↑ Triglycerides [5] | More favorable TG profile (less elevation) [5] | Neutral | May attenuate HDL rise |
| Insulin Resistance | Improves insulin sensitivity; ↓ HbA1c up to 0.6% [5] | Improves insulin sensitivity; ↓ fasting glucose ~20 mg/dL [5] | Neutral | Less favorable |
| Breast Cancer Risk | CEE alone ↓ risk; CEE+MPA ↑ incidence [37] | Likely lower risk than oral [56] | Lower risk vs. synthetic [56] | ↑ Risk vs. bioidentical [56] |
| Lipoprotein(a) | ↓ Lp(a) by 20-30% [5] | Effect less pronounced than oral [5] | Not Established | Not Established |
Table 2: Pharmacokinetic and Dosing Parameters for Common HRT Formulations
| Formulation | Typical Starting Dose | Key Pharmacokinetic Features | Primary Indications | Key Considerations |
|---|---|---|---|---|
| Oral Estradiol | 0.5 to 1 mg/day [56] | First-pass liver metabolism; fluctuating levels; high estrone:estradiol ratio [56] | Moderate-severe vasomotor symptoms [37] | Avoid in women with high VTE risk, liver disease, or hypertriglyceridemia [56] |
| Transdermal Estradiol | 0.025 to 0.05 mg/day [56] | Bypasses first-pass metabolism; steady-state delivery; physiological estradiol:estrone ratio [56] | Moderate-severe vasomotor symptoms; high CV risk patients [5] [56] | Preferred for patients with hypertension, obesity, metabolic syndrome, or high VTE risk [5] |
| Conjugated Equine Estrogens (CEE) | 0.3 to 0.45 mg/day | Multiple estrogen compounds; some non-human; extensive liver metabolism [56] | Moderate-severe vasomotor symptoms [37] | Associated with a complex mix of risks/benefits; not recommended first-line [56] |
| Micronized Progesterone (Oral) | 100 to 200 mg/day [56] | Metabolized to neurosteroids; has sedative effect [37] | Endometrial protection; sleep aid [37] | Take at bedtime; preferred progestogen for its metabolic neutrality [37] [56] |
Experimental Protocols
Protocol 1: Assessing Thrombotic Risk of Different HRT Formulations In Vivo
Objective: To compare the effect of oral versus transdermal estrogen formulations on markers of coagulation and inflammation in an ovariectomized rodent model.
Methodology:
- Animal Model: Use mature, ovariectomized female rodents (e.g., rats). Randomize into groups: Control (vehicle), Oral Estradiol, Transdermal Estradiol (patch), and Oral CEE.
- Dosing & Administration: Dose formulations to achieve physiological estradiol levels. Treat for a period of 12 weeks.
- Blood Collection & Analysis: Collect blood samples at baseline, 4, 8, and 12 weeks. Analyze plasma for:
- Primary Endpoints: Thrombin generation potential, Levels of Factor V, Factor VIII, and fibrinogen.
- Secondary Endpoints: High-sensitivity C-reactive protein (hs-CRP), Liver-synthesized proteins (e.g., SHBG).
- Statistical Analysis: Use ANOVA with post-hoc tests to compare changes over time and between groups.
Protocol 2: Evaluating the Impact of Progestogens on Metabolic Parameters
Objective: To investigate the differential effects of bioidentical progesterone versus synthetic progestins on insulin sensitivity and lipid metabolism in a postmenopausal model.
Methodology:
- Study Design: A randomized, controlled trial in postmenopausal women or an ovariectomized non-human primate model.
- Intervention Groups: All participants receive a standardized dose of transdermal estradiol. They are then randomized to receive one of the following progestogens:
- Group 1: Micronized progesterone (200 mg/day, cyclic)
- Group 2: Medroxyprogesterone acetate (MPA) (5 mg/day, cyclic)
- Group 3: Estradiol-only (no progestogen, for reference)
- Assessments: Conduct the following at baseline and after 6 months of therapy:
- Hyperinsulinemic-euglycemic clamp to measure insulin sensitivity.
- Fasting lipid profile (LDL-C, HDL-C, Triglycerides).
- Body composition analysis (DEXA scan) to measure visceral adiposity.
- Outcome Analysis: Compare the mean change in insulin sensitivity and lipid parameters between the three groups using appropriate statistical models, adjusting for baseline values.
Signaling Pathways and Workflows
HRT Metabolic Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for HRT Formulation and Metabolic Research
| Research Reagent / Material | Function & Application in HRT Research |
|---|---|
| Micronized 17β-Estradiol | The primary bioidentical estrogen used in FDA-approved formulations; serves as the gold standard for comparing pharmacokinetics and efficacy in experimental models [37] [56]. |
| Micronized Progesterone | Bioidentical progesterone used for endometrial protection in research protocols; critical for studying the metabolic neutrality of progestogens compared to synthetic alternatives [56] [57]. |
| Transdermal Delivery Systems (Patches/Gels) | Enables the study of non-oral administration routes; used to investigate first-pass metabolism bypass and its associated benefits on coagulation and inflammatory markers [5] [56]. |
| Conjugated Equine Estrogens (CEE) | A mixture of estrogens used as a comparator in research to understand the effects of non-human and complex estrogen blends on various tissue systems and global health outcomes [37] [5]. |
| Medroxyprogesterone Acetate (MPA) | A synthetic progestin commonly used as a negative control in experiments designed to highlight the differential metabolic and cardiovascular risks between progestogen types [5] [56]. |
| Sex Hormone-Binding Globulin (SHBG) Assay | A key biomarker for hepatic estrogenic activity; significantly increased by oral estrogen but minimally affected by transdermal administration [5]. |
| Hyperinsulinemic-Euglycemic Clamp | The gold-standard methodology for precisely assessing insulin sensitivity and resistance in vivo following treatment with different HRT formulations [5]. |
| Lipoprotein(a) [Lp(a)] Assay | A critical independent risk factor for atherosclerotic cardiovascular disease (ASCVD); levels increase during menopause and are reduced by oral estrogen, providing a key metric for CVD risk assessment [5]. |
Optimizing Therapeutic Outcomes: Navigating Formulation, Timing, and Comorbidities in HRT
FAQ: Core Concept and Biological Basis
What is the Critical Window Hypothesis in the context of Menopausal Hormone Therapy (MHT)? The Critical Window Hypothesis, also known as the timing hypothesis, posits that the effects of MHT on long-term health outcomes—including cardiovascular and neurological systems—are dependent on the timing of initiation relative to menopause. The hypothesis suggests that initiating therapy early, during the perimenopausal transition or within 10 years of menopause onset (generally before age 60), is associated with benefits or reduced risks. In contrast, initiation later in postmenopause (e.g., after age 65) is associated with increased risks of adverse events such as coronary heart disease, stroke, and dementia [5] [58] [59].
What is the proposed biological mechanism for this critical window? The mechanism is linked to the health of the vascular and neuronal systems at the time of estrogen reintroduction. Initiating therapy early is thought to help maintain vascular endothelial function and slow the progression of subclinical atherosclerosis. In the brain, estrogen receptors are upregulated during the perimenopausal transition as a compensatory mechanism for declining natural estrogen. If MHT is initiated while these receptors are still abundant, estrogen can bind and exert its neuroprotective effects. However, if initiation is delayed until years after menopause, a point is reached where estrogen receptors decline significantly, and the brain may no longer respond beneficially to exogenous hormones. Furthermore, introducing estrogen after the establishment of significant vascular pathology or atherosclerotic plaque may destabilize these lesions [5] [59] [60].
FAQ: Cardiovascular Health and MHT Timing
How does the initiation timing of MHT influence cardiovascular risk? Large-scale clinical and observational data show a clear divergence in cardiovascular risk based on the timing of MHT initiation:
- Perimenopausal/Early Postmenopausal Initiation: Initiation within 10 years of menopause or before age 60 is associated with a neutral or potentially reduced risk of coronary heart disease. One analysis suggested cardiovascular disease risk may be reduced by as much as 50% [26] [5] [61].
- Late Postmenopausal Initiation: Initiation in women who are more than 10 years past menopause onset, particularly over age 65, is associated with an increased risk of coronary heart disease and stroke [5] [59].
What are the specific effects of MHT on cardiovascular biomarkers? MHT has varied effects on biomarkers, which can be summarized as follows:
Table 1: Effects of Menopause and Systemic MHT on Key Cardiovascular Biomarkers
| Biomarker | Effect of Menopause | Effect of Systemic MHT |
|---|---|---|
| LDL Cholesterol | Increases by 10-20 mg/dL (14-19%) [5] | Decreases by 9-18% [5] [11] |
| HDL Cholesterol | Initially increases, then declines [5] | Increases by 7-13% [11] |
| Lipoprotein(a) [Lp(a)] | Increases by ~25% [5] | Decreases by 15-20% (oral estrogen) [5] [11] |
| Insulin Resistance | Increases (OR 1.40-1.59) [5] | Improves insulin sensitivity; reduces HbA1c by up to 0.6% [5] |
| Systolic Blood Pressure | Increases by 4-7 mmHg [5] | Variable: Oral may slightly decrease; Combined therapy may increase; Transdermal has neutral/beneficial effect [5] |
FAQ: Cognitive Health, Dementia, and MHT Timing
Is there evidence that MHT timing affects the risk of Alzheimer's disease and cognitive decline? Yes, emerging evidence strongly suggests timing is a critical modifier for cognitive outcomes. Observational studies and meta-analyses indicate that initiation of estrogen therapy in midlife, within 5-10 years of the final menstrual period, is associated with a significantly lower risk of dementia (up to 32-35% reduction). Conversely, when combination hormone therapy is initiated after age 65, the same analyses show an increased risk of Alzheimer's disease (up to 38% increase) [59] [58]. The Women's Health Initiative Memory Study (WHIMS), which enrolled older women (average age 65+), found that conjugated equine estrogen (CEE) plus medroxyprogesterone acetate (MPA) doubled the risk of all-cause dementia [58].
What are the neuroprotective mechanisms of estrogen? Estrogen exerts multiple protective effects on the brain through widespread estrogen receptors (ERα and ERβ) in regions critical for memory and cognition, such as the hippocampus and prefrontal cortex. Key mechanisms include:
- Enhancing Synaptic Plasticity: Promoting long-term potentiation (LTP) and increasing dendritic spine density to support learning and memory [60].
- Modulating Neurotransmitters: Upregulating cholinergic, serotonergic, and dopaminergic systems, which are crucial for cognition, mood, and attention [60].
- Supporting Cerebrovascular Health: Improving cerebral blood flow and maintaining the integrity of the blood-brain barrier [60].
- Reducing Oxidative Stress and Inflammation: Providing resilience against cellular damage implicated in neurodegenerative diseases [60].
FAQ: Formulation, Regimen, and Risk Assessment
How do different MHT formulations (oral vs. transdermal) impact risk profiles? The route of administration significantly influences the risk-benefit profile, particularly for cardiovascular outcomes:
- Transdermal Estradiol: Bypasses first-pass liver metabolism. This is associated with a lower risk of venous thromboembolism (VTE), a neutral effect on triglycerides and coagulation factors, and a more favorable impact on blood pressure. It is often preferred for women with elevated VTE risk, hypertension, migraines with aura, or hypertriglyceridemia [5] [61].
- Oral Estrogens: Undergo first-pass metabolism in the liver. While effective at improving lipid profiles (lowering LDL, raising HDL) and significantly lowering Lp(a), they increase the risk of VTE, triglycerides, and coagulation factors [5] [11] [61].
- Progestogen Component: The type of progestogen matters. Micronized progesterone is generally associated with a more favorable risk profile (particularly for breast cancer and cardiovascular effects) compared to synthetic medroxyprogesterone acetate (MPA) [5] [61].
What should a pre-therapy cardiovascular risk assessment for MHT initiation include? A comprehensive, person-centered risk assessment is recommended before initiating MHT. This should include [5] [34]:
- Evaluation of Traditional CV Risk Factors: Blood pressure, lipid profile, diabetes status, smoking, and family history.
- Assessment of Female-Specific Risk Enhancers: History of preeclampsia, gestational diabetes, premature menopause, or polycystic ovary syndrome.
- Consideration of Subclinical Atherosclerosis: For women with uncertain risk, imaging such as Coronary Artery Calcium (CAC) scoring can refine risk stratification.
- Universal Screening for Lipoprotein(a): Due to its strong genetic association with ASCVD risk and responsiveness to oral MHT.
The Scientist's Toolkit: Key Reagents and Experimental Models
Table 2: Essential Reagents and Models for Research on the Critical Window Hypothesis
| Reagent / Model | Function in Research |
|---|---|
| Conjugated Equine Estrogens (CEE) | A historically common oral estrogen formulation used in seminal trials (e.g., WHI). Serves as a comparator to study formulation-specific effects [5] [58] [11]. |
| 17β-Estradiol (Oral & Transdermal) | The primary human estrogen. Used to study the effects of bio-identical estrogen and compare pharmacokinetics of different administration routes [5] [61]. |
| Medroxyprogesterone Acetate (MPA) | A synthetic progestin. Used to investigate the impact of progestogens on estrogen's effects, particularly in models of breast cancer and cardiovascular risk [5] [58]. |
| Micronized Progesterone | A bio-identical progesterone. Studied as a potentially safer alternative to synthetic progestins for endometrial protection in EPT regimens [5] [61]. |
| Ovariectomized (OVX) Rodent Models | Provides a controlled model of surgical menopause. Essential for isolating the effects of estrogen loss and replacement timing on neurobiological, vascular, and metabolic outcomes [60]. |
| APOE-transgenic Mouse Models | Used to study the interaction between the chief genetic risk factor for Alzheimer's and estrogen therapy timing, allowing for the investigation of personalized risk [60]. |
Experimental Protocols for Investigating the Critical Window
Protocol 1: Evaluating the Timing Hypothesis in a Rodent Model of Neuroprotection
- Objective: To determine the differential effects of early versus late initiation of 17β-estradiol on Alzheimer's disease pathology and cognitive behavior.
- Animal Model: Female APOE-transgenic mice (e.g., APOE4 knock-in).
- Intervention Groups: (1) Sham control; (2) OVX at midlife (simulating menopause); (3) OVX + 17β-estradiol implant initiated immediately post-OVX (Early); (4) OVX + 17β-estradiol implant initiated 5 months post-OVX (Late).
- Outcome Measures:
- Cognitive Testing: Morris Water Maze for spatial memory, conducted after hormone treatment.
- Pathological Analysis: Post-mortem brain immunohistochemistry for amyloid-beta plaque load and phosphorylated tau in the hippocampus and cortex.
- Synaptic Markers: Western blot analysis of PSD-95 and synaptophysin levels.
- Key Methodology: Ensure consistent estradiol serum levels across treatment groups via slow-release pellets. The "late" group should represent a period equivalent to ~10+ human postmenopausal years.
Protocol 2: Assessing Vascular and Metabolic Outcomes in a Clinical Trial Framework
- Study Design: Randomized, placebo-controlled trial in recently menopausal women (<3 years since last period) vs. late postmenopausal women (>10 years since last period).
- Intervention: Low-dose transdermal 17β-estradiol (e.g., 0.025 mg/day) with cyclic micronized progesterone (200 mg/12 days) for women with a uterus vs. matched placebo.
- Primary Endpoint: Change in flow-mediated dilation (FMD) of the brachial artery, a measure of endothelial function, at 6 months.
- Secondary Endpoints:
- Change in coronary artery calcium (CAC) score via CT at baseline and 2 years.
- Changes in lipid profile, Lp(a), and HOMA-IR (a measure of insulin resistance).
- Ambulatory 24-hour blood pressure monitoring.
- Key Methodology: Stratify randomization by time-since-menopause and baseline metabolic syndrome status. Use central laboratory processing and blinded core labs for imaging analysis.
Visualization of Research Concepts and Workflows
Diagram 1: The Critical Window Hypothesis: Conceptual Framework
Diagram 2: Experimental Protocol for Neuroprotection
Frequently Asked Questions (FAQs) on HRT and Cardiovascular Safety
FAQ 1: What is the primary cardiovascular safety advantage of transdermal estradiol over oral estrogen? The primary advantage is the significant reduction in the risk of venous thromboembolism (VTE). Unlike oral estrogens, transdermal estradiol does not increase the risk of VTE, likely because it bypasses the liver and thus avoids the first-pass metabolism that adversely affects the coagulation cascade, including thrombin generation and resistance to activated protein C [62] [63]. Furthermore, large-scale studies indicate that transdermal estradiol shows no clear increase in myocardial infarction or composite cardiovascular disease, unlike some oral formulations [63].
FAQ 2: How does micronized progesterone differ from synthetic progestins in its effect on cardiovascular risk? Micronized progesterone has a more favorable safety profile regarding thrombotic risk and metabolic effects. Evidence suggests that micronized progesterone, unlike some synthetic progestins like medroxyprogesterone acetate (MPA), does not increase the risk of venous thromboembolism [62]. It also has a neutral or beneficial effect on blood pressure and, when combined with transdermal estrogen, further reduces the incidence of new-onset diabetes [62] [5]. It is considered to have a neutral effect on the vasculature [62].
FAQ 3: How does the "Timing Hypothesis" influence the expected cardiovascular outcomes of HRT? The "Timing Hypothesis" posits that the cardioprotective effects of HRT are dependent on when therapy is initiated relative to menopause. Initiating HRT in women younger than 60 years old and/or within 10 years of menopause is associated with a significant reduction in all-cause mortality and coronary heart disease [64]. In contrast, initiating HRT in older women or those more than 10 years post-menopause shows no such benefit and may even increase risks, likely because estrogen has beneficial effects on healthy endothelium but can have adverse effects on established atherosclerotic plaques [64] [65].
FAQ 4: For a patient with a high baseline risk of venous thromboembolism, what would be the recommended HRT formulation? For such patients, the recommended regimen would be transdermal estradiol combined with micronized progesterone [62] [66]. This combination is recommended specifically because it avoids the increased risk of VTE associated with oral estrogens and synthetic progestins [62] [5] [66].
FAQ 5: What are the key metabolic differences between oral and transdermal estrogen formulations? The key metabolic differences are summarized in the table below [5] [66]:
Table: Metabolic and Cardiovascular Risk Profile of HRT Formulations
| Risk Factor | Oral Estrogen | Transdermal Estradiol | Micronized Progesterone / Dydrogesterone |
|---|---|---|---|
| Venous Thromboembolism (VTE) | Significantly increases risk [63] | No clear increase in risk [62] [63] | Does not increase risk (vs. increased risk with some synthetics) [62] [66] |
| Ischemic Heart Disease | Small increase in risk with estrogen+progestin [63] | Borderline reduction in risk; greater safety [63] | Neutral vascular effect [62] |
| Lipid Profile | Reduces LDL; increases HDL and triglycerides [5] | More favorable effect on triglycerides (less elevation) [5] | Not associated with adverse lipid changes |
| Blood Pressure | Minor reduction in SBP, but combined therapy may increase SBP [5] | Neutral or beneficial (can decrease DBP) [5] | Neutral or beneficial effect [62] |
| Insulin Resistance | Improves insulin sensitivity, reduces HbA1c [5] | Improves insulin sensitivity, reduces HbA1c [5] | Reduces incidence of new-onset diabetes [62] |
Troubleshooting Common Research Challenges
Challenge 1: Interpreting Conflicting Results from WHI vs. More Recent Studies
- Problem: Early clinical trials like the Women's Health Initiative (WHI), which used oral conjugated equine estrogen (CEE) and medroxyprogesterone acetate (MPA), demonstrated increased cardiovascular risks. These findings conflict with observational data and contemporary trials showing cardiovascular benefit or safety.
- Solution: The discrepancy is largely explained by the Timing Hypothesis and differences in formulation.
- Cohort Timing: The WHI predominantly enrolled older women (mean age >63 years) who were many years post-menopause. Cardioprotection is observed primarily when HRT is initiated in younger women (<60 years) within 10 years of menopause [64].
- Formulation: The WHI used specific synthetic formulations (CEE and MPA). Contemporary research indicates that transdermal estradiol and micronized progesterone have safer risk profiles, particularly for thrombosis [62] [65].
- Protocol Adjustment: When designing studies or interpreting data, always stratify results by age and time-since-menopause of the cohort, and specify the exact hormonal formulations used. The results of the WHI should not be applied to contemporary, bioidentical formulations [65].
Challenge 2: Modeling the "Timing Hypothesis" in Preclinical Atherosclerosis Studies
- Problem: Designing an animal experiment to recapitulate the differential effects of estrogen on early versus established atherosclerosis.
- Solution: Implement an intervention protocol that varies the timing of estrogen administration relative to the stage of atherosclerosis development.
- Experimental Workflow: The following diagram outlines a classic preclinical study design to test the Timing Hypothesis, based on work in ApoE-deficient mice [64]:
- Detailed Methodology:
- Animal Model: Utilize apolipoprotein E deficient (ApoE-/-) mice on a high-fat diet to induce atherosclerosis.
- Grouping:
- Early Intervention Group: Initiate transdermal estradiol (e.g., via subcutaneous pellet or patch) at the beginning of the high-fat diet, coinciding with the start of atherogenesis.
- Late Intervention Group: Initiate the same dose of transdermal estradiol after a predetermined period (e.g., 8-10 weeks) when established atherosclerotic lesions are present.
- Control Group: Receive a placebo pellet for the duration of the study.
- Endpoint Analysis: Quantify atherosclerotic lesion area in the aortic sinus or en face aorta at the end of the study. The expected result is that estrogen prevents the formation of new lesions in the early intervention group but has no significant effect on pre-existing lesions in the late intervention group, supporting the healthy endothelium hypothesis [64].
Challenge 3: Selecting Biomarkers for Assessing Vascular Health in HRT Clinical Trials
- Problem: Choosing appropriate intermediate endpoints to evaluate the vascular effects of different HRT formulations short of large-scale clinical event trials.
- Solution: A multi-modal approach using imaging and serum biomarkers provides a comprehensive assessment.
- Primary Imaging Endpoint: Carotid Artery Intima-Media Thickness (CIMT). This is a validated, non-invasive ultrasound method to quantify subclinical atherosclerosis. Studies like EPAT have shown that estradiol reduces the progression of CIMT in healthy postmenopausal women [64].
- Secondary Imaging Endpoint: Coronary Artery Calcium (CAC) Scoring. This CT-based technique quantifies calcified plaque in the coronary arteries, a strong predictor of future CV events. The effect of HRT on CAC may vary by formulation [5].
- Key Serum Biomarkers:
- Lipoprotein(a) (Lp(a)): A genetically determined, independent risk factor for ASCVD. Levels rise during menopause. Oral estrogen significantly reduces Lp(a) levels, though this does not necessarily translate to reduced event rates [5].
- Metabolic Markers: Fasting glucose, insulin, and HbA1c to assess insulin resistance, which is often improved by MHT [5].
The Scientist's Toolkit: Key Research Reagents & Materials
Table: Essential Reagents for Investigating HRT and Cardiovascular Pathophysiology
| Item | Function / Application in Research |
|---|---|
| 17β-Estradiol (Transdermal Patch/Gel) | The gold-standard bioidentical estrogen for investigating the effects of non-oral administration. Used in both in vivo models (rodents, non-human primates) and in vitro systems to study vascular and metabolic effects without first-pass liver metabolism [62] [65]. |
| Micronized Progesterone | Bioidentical progesterone preparation. A critical reagent for comparative studies against synthetic progestins (e.g., MPA) to demonstrate differential effects on thrombosis, inflammation, and vascular function [62] [66]. |
| Human Umbilical Vein Endothelial Cells (HUVECs) | A standard in vitro model for studying the direct effects of hormones on endothelial cell health, including proliferation, nitric oxide production, inflammation, and apoptosis [64]. |
| Apolipoprotein E Deficient (ApoE-/-) Mice | A widely used murine model for studying atherosclerosis. Essential for testing the "Timing Hypothesis" and evaluating the atheroprotective effects of different HRT formulations in a controlled manner [64]. |
| Carotid Ultrasound System (High-Frequency) | For non-invasive, serial measurement of carotid artery intima-media thickness (CIMT) in clinical and large-animal studies. This is a primary endpoint in atherosclerosis imaging trials like EPAT [64]. |
FAQs: Navigating HRT in Complex Clinical Scenarios
FAQ 1: What are the primary HRT-associated risks for a patient with a personal history of breast cancer? For patients with a history of breast cancer, particularly hormone receptor-positive (HR-positive) disease, systemic HRT is generally not recommended. A 2021 analysis of four studies found that systemic HRT was associated with an 80% higher risk of breast cancer recurrence in this population. [67] The primary concern is that exogenous hormones may stimulate the growth of residual cancer cells. [68] However, for vaginal symptoms, low-dose vaginal estrogen is generally considered safe, as studies show it does not increase the risk of dying from breast cancer, and most of the hormones stay in the vaginal tissue. [67]
FAQ 2: How does the type of HRT formulation influence thrombotic risk? The risk of venous thromboembolism (VTE) is strongly influenced by the route of estrogen administration.
- Oral Estrogens: Increase the risk of VTE. This is linked to the "hepatic first-pass effect," where high estrogen concentration in the liver alters the synthesis of coagulation and anticoagulation factors, creating a prothrombotic state. [69] [7]
- Transdermal Estrogens: Appear to have a lower or neutral impact on thrombotic risk. Because they are absorbed directly into the systemic circulation, they bypass the liver and do not cause the same pronounced changes in hemostatic markers. [69] [7] Transdermal estrogen is often the preferred option for women with elevated cardiovascular or thrombotic risk. [5] [7]
FAQ 3: What is the "Timing Hypothesis" and how does it guide HRT initiation? The "Timing Hypothesis" posits that the cardiovascular effects of HRT are dependent on when therapy is initiated relative to age and menopause. [64] Initiation in women younger than 60 years old or within 10 years of menopause onset is associated with a reduction in all-cause mortality and coronary heart disease. [64] [70] Conversely, starting HRT in women older than 60 or more than 10 years post-menopause may increase the risk of coronary heart disease and stroke, likely due to the presence of established atherosclerosis on which estrogen can have adverse effects. [5] [64]
FAQ 4: What strategies can be used to minimize risks while managing menopausal symptoms in high-risk patients?
- For Breast Cancer History: Focus on non-hormonal therapies first (e.g., cognitive behavioral therapy, SSRIs/SNRIs for hot flashes). If hormonal therapy is necessary, low-dose vaginal estrogen is a safe option for genitourinary symptoms. For systemic symptoms, the decision must be highly personalized, acknowledging that some patients may accept a potential increase in recurrence risk for a significant improvement in quality of life. [67]
- For Thrombotic Risk: Use transdermal estrogen formulations instead of oral ones. Select the lowest effective dose for the shortest duration needed to manage symptoms. [5] [7] A thorough pre-therapy cardiovascular and thrombotic risk assessment is essential. [70]
FAQ 5: How do progestogens influence the risk profile of combination HRT? Progestogens are added to estrogen therapy in women with a uterus to prevent estrogen-induced endometrial hyperplasia and cancer. [67] [68] However, the type of progestogen matters. Some studies suggest that micronized progesterone has a more favorable risk profile for breast cancer and cardiovascular disease compared to synthetic progestins like medroxyprogesterone acetate (MPA). [5] The combination of conjugated equine estrogen (CEE) with MPA was associated with an increased risk of breast cancer and myocardial infarction in older studies. [5] [64]
Table 1: Impact of Menopause and HRT on Key Cardiovascular and Cancer Risks
| Risk Factor | Effect of Menopause | Effect of Oral HRT | Effect of Transdermal HRT |
|---|---|---|---|
| Breast Cancer Risk | Not applicable | • Combination HRT: Increases risk with use >5 years. [67]• Estrogen-only: Not linked to higher risk in women without a uterus. [67] | Believed to have lower risk than oral, but more data needed. |
| Venous Thromboembolism (VTE) Risk | Not applicable | Increased risk, especially in older women. [69] [7] | Lower or neutral risk compared to oral. [69] [7] |
| Stroke Risk | Increased ischemic stroke risk (HR 1.1–2.0). [5] | Increased risk (~40%). [5] | Lower risk with doses <50 mcg; risk unaffected by initiation timing. [5] |
| Lipid Profile | ↑ LDL (10–20 mg/dL), ↑ Total Cholesterol (10–14%). [5] | ↓ LDL (9–18 mg/dL), ↑ HDL. [5] | More favorable for triglycerides (less elevation than oral). [5] |
| Lipoprotein(a) [Lp(a)] | Increases by ~25%. [5] | Decreases Lp(a) by 20–30%. [5] | Lesser effect than oral estrogen. [5] |
Table 2: HRT Guidance Based on Patient Risk Profile
| Patient Risk Profile | Recommended HRT Strategy | Key Considerations & Rationale |
|---|---|---|
| History of Breast Cancer | • Avoid systemic HRT, especially for HR-positive cancer. [67]• Low-dose vaginal estrogen is generally safe for GSM. [67] | Systemic HRT increases recurrence risk. Vaginal estrogen has minimal systemic absorption. Decision-making should be personalized with oncology. [67] [68] |
| Elevated Thrombotic Risk | • Transdermal estrogen is preferred. [69] [7]• Use lowest effective dose and shortest duration. [67] | Transdermal route bypasses hepatic first-pass, minimizing prothrombotic changes in hemostatic factors. [69] |
| Type 2 Diabetes | • Consider for symptom relief; early initiation (<10 years of menopause) is key. [7]• Transdermal estrogen preferred due to cardiovascular risk. [7] | HRT can improve glycemic control (↓ HbA1c by ~0.6%) and insulin sensitivity. [7] |
| General Population (Aged <60 / Within 10 Yrs of Menopause) | • Early initiation of appropriate HRT formulation. | Associated with reduction in all-cause mortality and CVD. [64] Adheres to the "Timing Hypothesis." [64] |
Experimental Protocols
Protocol 1: Assessing the Impact of Estrogen on Hemostatic Markers In Vitro
Objective: To evaluate the procoagulant potential of different estrogen formulations and doses by measuring their effect on key hemostatic parameters in a hepatocyte cell culture model.
Methodology:
- Cell Culture: Use a human hepatocyte cell line (e.g., HepG2). Culture cells in standard conditions.
- Treatment Groups: Treat cells with various estrogens:
- Ethinyl Estradiol (EE) (e.g., 0.01 µM, 0.1 µM)
- 17β-Estradiol (E2) (e.g., 0.1 µM, 1 µM)
- Conjugated Equine Estrogens (CEE) (e.g., 0.1 µg/mL, 1 µg/mL)
- Vehicle control Incubate for 24-72 hours. [69]
- Sample Collection: Collect cell culture supernatant and lysates.
- Outcome Measures (Assays):
- ELISA: Quantify procogulant factors (Fibrinogen, Factor VII, Factor VIII) and anticoagulant factors (Protein S, Antithrombin) in the supernatant. [69]
- qPCR: Analyze mRNA expression of genes encoding these factors (e.g., F2, F7, F8, PROS1, SERPINC1) to confirm genomic action via Estrogen Response Elements (EREs). [69]
- Functional Assays: Perform thrombin generation assays on supernatant to assess global coagulant potential.
Protocol 2: Evaluating the "Timing Hypothesis" in an Animal Model of Atherosclerosis
Objective: To determine whether the stage of atherosclerosis development influences the cardiovascular effects of hormone therapy.
Methodology:
- Animal Model: Use ovariectomized ApoE-/- mice to simulate postmenopausal estrogen deficiency and accelerate atherosclerosis.
- Study Groups:
- Treatment Duration: Continue treatment for 8-12 weeks.
- Outcome Measures:
- Histological Analysis: At endpoint, quantify atherosclerotic lesion size in the aortic sinus (Oil Red O staining).
- Immunohistochemistry: Analyze plaque composition for stability markers (e.g., collagen content, macrophage infiltration).
- Vascular Function: Assess endothelial-dependent vasodilation in isolated aortic rings.
Signaling Pathways and Workflows
Diagram 1: Molecular Pathway of Estrogen-Induced Thrombotic Risk. This diagram illustrates the genomic mechanism by which oral estrogen increases thrombotic risk, primarily through the hepatic first-pass effect, leading to altered synthesis of hemostatic proteins. Transdermal administration bypasses this pathway, resulting in a lower risk profile. [69]
Diagram 2: Clinical Decision Workflow for HRT in High-Risk Patients. This workflow provides a structured approach to personalizing HRT, integrating critical decision points based on patient history (breast cancer, thrombosis) and clinical characteristics (uterus status) to optimize safety. [5] [67] [70]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating HRT Mechanisms and Risks
| Research Reagent / Material | Function / Application in HRT Research |
|---|---|
| Human Hepatocyte Cell Line (e.g., HepG2) | In vitro model to study the "hepatic first-pass effect" of oral estrogens on the synthesis of hemostatic proteins (coagulation factors, Protein S). [69] |
| Ovariectomized ApoE-/- Mouse Model | In vivo model to study the "Timing Hypothesis" and the impact of HRT on the progression and stability of atherosclerosis in a controlled, postmenopausal-state setting. [64] |
| 17β-Estradiol (E2) & Ethinyl Estradiol (EE) | Key estrogen compounds for experimental use. E2 is used in modern HRT and research, while EE is used in contraceptives; comparing them helps elucidate differential risk profiles. [69] |
| Specific ELISA Kits | Quantify protein levels of key hemostatic markers (e.g., Fibrinogen, Factor VIII, Protein S, D-Dimer) in plasma or cell culture supernatant to assess thrombotic risk. [69] |
| Antibodies for Plaque Characterization | Antibodies against markers like α-SMA (smooth muscle cells, plaque stability), MAC-3 (macrophages, inflammation), and Collagen I/III used in immunohistochemistry to analyze atherosclerotic plaque composition in animal models. [64] |
Troubleshooting Guides and FAQs: Core Intervention Strategies
FAQ 1: What are the foundational components of an effective lifestyle modification program for Metabolic Syndrome (MetS)?
Effective lifestyle modification is the cornerstone of MetS management and is based on behavior therapy combined with specific dietary and exercise recommendations [71]. The intervention aims to provide patients with skills to permanently change eating and activity habits, rather than addressing the root causes of these behaviors [71].
Core Components:
- Structured Dietary Changes: Implementation of a low-calorie, low-fat diet or Mediterranean-style diet pattern. The Diabetes Prevention Program (DPP) demonstrated that a low-calorie, low-fat diet can reduce the incidence of MetS by 41% [71].
- Progressive Physical Activity: A combination of aerobic exercise and resistance training. Adding aerobic exercise to a nutritional weight-loss approach resulted in significantly more cases of MetS resolving (95%) compared to diet alone (75%) [71].
- Behavioral and Cognitive Strategies: Techniques include self-monitoring, stimulus control, problem-solving, and cognitive restructuring to build a mindset favoring long-term change [71].
- Delivery Format: Can be delivered face-to-face, in groups, or in a combined format [71].
Troubleshooting Common Challenges:
- Challenge: Patient adherence to nutritional prescriptions and physical activity declines over time.
- Solution: Integrate long-term maintenance strategies, such as periodic booster sessions, continuous support, and combining lifestyle modification with other approaches like pharmacotherapy or meal replacements [71].
FAQ 2: How does Menopausal Hormone Therapy (MHT) interact with the components of Metabolic Syndrome?
MHT's effects on MetS are formulation-dependent and influenced by the timing of initiation. Modern MHT formulations, particularly those containing estradiol, can have a favorable impact on several metabolic parameters [5] [72] [73].
- Mechanistic Insights and Troubleshooting:
- Glucose Metabolism: A common finding is that MHT improves insulin resistance and reduces the risk of developing type 2 diabetes [5] [73]. It is postulated that estrogen helps protect pancreatic β-cells and maintain insulin secretion [73].
- Troubleshooting Conflicting Data: If studies report no effect on glucose homeostasis, scrutinize the participant characteristics (e.g., presence of obesity, which can confound results) and the methods used to assess insulin sensitivity (e.g., hyperinsulinemic-euglycemic clamp vs. IVGTT) [72].
- Lipid Profile: MHT generally leads to a significant reduction in LDL-C and total cholesterol, and an increase in HDL-C [5] [73]. A notable exception is that oral estrogen often increases triglyceride levels, whereas transdermal estrogen has a more neutral or favorable effect [5] [66].
- Troubleshooting Adverse Lipid Responses: If a patient on MHT exhibits a problematic increase in triglycerides, consider switching from an oral to a transdermal estrogen formulation [66].
- Body Composition: MHT is associated with a modest reduction in total and visceral adiposity and can help attenuate the menopause-related shift toward central fat distribution [5] [73].
- Troubleshooting Inconsistent Results: Discrepancies in weight and body fat outcomes across studies (e.g., some Cochrane reviews find no effect) may be related to the specific type, dose, and duration of MHT used [73].
- Glucose Metabolism: A common finding is that MHT improves insulin resistance and reduces the risk of developing type 2 diabetes [5] [73]. It is postulated that estrogen helps protect pancreatic β-cells and maintain insulin secretion [73].
FAQ 3: What is the "timing hypothesis" for MHT and cardiovascular risk, and how does it influence trial design?
The "timning hypothesis" proposes that the cardiovascular benefits of MHT are maximized, and risks minimized, when therapy is initiated close to the time of menopause (typically defined as <60 years old or within 10 years of menopause) [5] [66]. Early clinical trials like the Women's Health Initiative (WHI), which primarily enrolled older women (mean age 63), found increased risks of coronary heart disease and stroke with oral conjugated equine estrogen plus medroxyprogesterone acetate [5]. Subsequent analyses and trials focusing on younger, healthier women closer to menopause have shown more favorable outcomes for atherosclerosis and metabolic health [5] [66].
- Troubleshooting Trial Interpretation:
- Challenge: A trial reports negative cardiovascular outcomes for MHT.
- Solution: Critically evaluate the baseline characteristics of the cohort, specifically the mean age and time since menopause. Results from studies in older women with established atherosclerosis cannot be extrapolated to younger, healthier women initiating MHT early in menopause [5].
Quantitative Data Synthesis
Table 1: Synergistic Effects of Lifestyle and Pharmacological Interventions on Metabolic Syndrome Components
| Intervention | Waist Circumference | LDL-C & Total Cholesterol | Triglycerides | HDL-C | Fasting Glucose / Insulin Resistance | Blood Pressure |
|---|---|---|---|---|---|---|
| Lifestyle Modification (LSM) [71] | Significant reduction with 7-10% weight loss target. | Improves with weight loss. | ≥150 mg/dL is a diagnostic criterion; improves with LSM. | <40/50 mg/dL (M/F) is a diagnostic criterion; improves with LSM. | Primary driver of improvement. DPP showed 41% reduction in diabetes incidence. | Improves with weight loss and DASH diet. |
| Menopausal Hormone Therapy (MHT) [5] [72] [73] | Modest reduction in visceral adiposity; prevents central fat shift. | Reduction of 9-18 mg/dL (LDL-C). | Formulation-dependent. Oral estrogen may increase; transdermal is neutral. | Increase. | Improvement. Reduces HbA1c (up to 0.6%) and fasting glucose. | Variable. Oral may slightly increase SBP; transdermal may reduce DBP. |
| Synergistic Effect | LSM provides major reduction; MHT may help maintain favorable fat distribution. | Additive or synergistic improvement in atherogenic lipid profile. | LSM counters potential TG increase from oral MHT. | Additive or synergistic increase in protective HDL. | Potentially additive improvements in insulin sensitivity. | LSM is primary; MHT's effect is secondary and formulation-specific. |
Table 2: Impact of MHT Formulation on Metabolic and Cardiovascular Risk Parameters
| Parameter | Oral Estrogen (e.g., CEE) | Transdermal Estrogen (e.g., Estradiol) | Progestogen Component (e.g., MPA vs. Micronized Progesterone) |
|---|---|---|---|
| Lipid Profile | LDL-C ↓, HDL-C ↑, Triglycerides ↑↑ | LDL-C ↓, HDL-C ↑, Triglycerides →/↓ (more favorable) | MPA may attenuate estrogen's beneficial lipid effects. Micronized progesterone/dydrogesterone is more neutral. |
| Insulin Sensitivity | Improvement | Improvement | Micronized progesterone is preferred for a better metabolic profile. |
| Blood Pressure | Minor SBP reduction, but combined therapy may increase SBP. | Neutral or beneficial (can reduce DBP by up to 5 mmHg). | - |
| Thrombotic Risk | Increased risk of Venous Thromboembolism (VTE). | Lower risk of VTE. | - |
| General Cardiovascular Risk | Associated with increased CHD and stroke risk in older women. | Safer profile, particularly for coronary heart disease. | - |
Experimental Protocols & Methodologies
Protocol 1: Assessing the Efficacy of a Combined Lifestyle and MHT Intervention in an Animal Model of Postmenopausal MetS
1. Objective: To evaluate the synergistic effects of diet, exercise, and hormone therapy on glucose tolerance and visceral adiposity in an ovariectomized (OVX) rodent model.
2. Materials:
- Animals: Adult female rodents (e.g., Sprague-Dawley rats or C57BL/6 mice).
- Surgical Procedure: Equipment for OVX or sham surgery.
- Interventions:
- Diet: High-fat diet (HFD) to induce MetS vs. control chow.
- Exercise: Voluntary running wheels or forced treadmill running system.
- Pharmacological: 17β-Estradiol pellets or vehicle, Progesterone/Micronized Progesterone.
- Assessment Tools: Metabolic cages, Dual-energy X-ray absorptiometry (DEXA) for body composition, Glucose and Insulin tolerance test kits, CLAMS (Comprehensive Lab Animal Monitoring System).
3. Methodology:
- Phase 1: Model Induction (4-6 weeks)
- Randomize animals into two groups: Sham-operated (control) and OVX.
- House all OVX animals on a HFD to accelerate the development of MetS components (insulin resistance, dyslipidemia, weight gain).
- Phase 2: Intervention (8-12 weeks)
- Randomize OVX+HFD animals into the following groups (n=10-12/group):
- Group 1: OVX + HFD (Vehicle)
- Group 2: OVX + HFD + MHT (e.g., Estradiol + Progesterone)
- Group 3: OVX + HFD + Exercise (Voluntary wheel running)
- Group 4: OVX + HFD + MHT + Exercise (Combined Intervention)
- Administer MHT via subcutaneous pellet or oral gavage. Record daily running wheel revolutions.
- Randomize OVX+HFD animals into the following groups (n=10-12/group):
- Phase 3: Endpoint Analysis
- Perform an Intraperitoneal Glucose Tolerance Test (IPGTT) and Insulin Tolerance Test (ITT) after an overnight fast.
- Euthanize animals and collect tissues: weigh visceral fat pads (mesenteric, perirenal), liver; collect blood for lipid profiling (total cholesterol, TG, HDL-C).
- Analyze body composition via DEXA scanning prior to tissue collection.
4. Data Analysis: Compare results using two-way ANOVA (factors: MHT, Exercise) followed by post-hoc tests to identify synergistic interactions between the pharmacological and lifestyle interventions.
Protocol 2: Clinical Research Protocol for a Personalized MHT Study in Women with MetS
1. Objective: To determine the effect of different MHT formulations on the resolution of MetS in early postmenopausal women, with and without concurrent structured lifestyle intervention.
2. Study Design: Randomized, double-blind, placebo-controlled, 2x2 factorial trial.
3. Participant Population:
- Inclusion: Women within 3-10 years of natural menopause, meeting the International Diabetes Federation (IDF) criteria for MetS.
- Exclusion: History of breast cancer, venous thromboembolism, CVD, or contraindications to MHT.
4. Intervention Groups (12-month duration):
- Arm A: Placebo MHT + Standard Care Lifestyle Advice
- Arm B: Active MHT (e.g., transdermal estradiol + micronized progesterone) + Standard Care Lifestyle Advice
- Arm C: Placebo MHT + Intensive Lifestyle Modification Program (based on DPP)
- Arm D: Active MHT + Intensive Lifestyle Modification Program
5. Primary and Secondary Endpoints:
- Primary: Change in the number of MetS criteria met from baseline to 12 months.
- Secondary: Resolution of MetS; changes in HOMA-IR, lipid profile, visceral adiposity (measured by DEXA or CT), high-sensitivity CRP.
6. Statistical Analysis: Intention-to-treat analysis. Use logistic regression to assess the odds of MetS resolution, testing for an interaction between MHT and lifestyle intervention.
Signaling Pathways and Metabolic Regulation
Diagram 1: Estrogen Receptor Signaling in Metabolic Tissues
This diagram outlines the core pathways through which estrogen signaling impacts key metabolic processes in the liver, adipose tissue, and pancreas, influencing MetS components.
Diagram 2: Integrated Management of Metabolic Syndrome
This workflow visualizes the decision-making process for individualizing MetS management in postmenopausal women, integrating lifestyle and pharmacological strategies.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Models for Investigating MetS and HRT
| Item / Category | Function / Purpose in Research | Examples & Notes |
|---|---|---|
| In Vivo Models | To study pathophysiology and intervention efficacy in a controlled system. | Ovariectomized Rodent: Standard model for surgical menopause. SHHR model: Combines hypertension and obesity. Zucker Diabetic Fatty (ZDF) Rat: Model for T2D and obesity. |
| Hormone Formulations | To test the metabolic effects of specific estrogen and progestogen types. | 17β-Estradiol (E2): Gold-standard bioactive estrogen. Conjugated Equine Estrogens (CEE): Used in key trials (e.g., WHI). Medroxyprogesterone Acetate (MPA) vs. Micronized Progesterone: To compare progestogen effects. |
| Metabolic Phenotyping | To accurately quantify components of MetS in model systems. | CLAMS (Comprehensive Lab Animal Monitoring System): Measures energy expenditure, RER, locomotor activity. DEXA: For precise body composition (lean/fat mass). EchoMRI: For rapid body composition analysis. |
| Assays for Glucose Metabolism | To assess insulin sensitivity and glucose homeostasis. | Hyperinsulinemic-Euglycemic Clamp: Gold-standard for in vivo insulin sensitivity. Glucose & Insulin Tolerance Tests (GTT/ITT): Standard in vivo functional tests. ELISA/Kits: For measuring insulin, adipokines (leptin, adiponectin). |
| Lipid Profiling Assays | To quantify changes in the atherogenic lipid profile. | Enzymatic Colorimetric Assays: For measuring plasma TG, Total-C, HDL-C, LDL-C. Fast Protein Liquid Chromatography (FPLC): For detailed lipoprotein separation. |
| Histology & Imaging | To examine tissue morphology and lipid accumulation. | H&E Staining: General tissue histology. Oil Red O Staining: For neutral lipids (in liver/fat). Immunofluorescence: For detecting specific proteins (e.g., ERα, insulin receptors). |
Troubleshooting Guide: Common Barriers to HRT Continuity
This guide assists researchers and clinicians in diagnosing and addressing common failure points in Hormone Replacement Therapy (HRT) treatment continuity, within the context of individualizing therapy based on metabolic and cardiovascular risk factors.
FAQ 1: What are the primary cost-related barriers to long-term HRT adherence, and how can they be quantified for intervention studies?
- Answer: The financial burden of HRT can be significant and is a major determinant of treatment discontinuation. The table below summarizes key cost-related barriers and potential metrics for research.
| Barrier & Mechanism | Impact on Continuity | Quantifiable Metrics for Research |
|---|---|---|
| High Direct Drug Cost [74]: List prices for branded or compounded formulations create patient financial toxicity. | Leads to prescription abandonment, self-directed dose reduction, or abrupt cessation. | • Prescription Abandonment Rate• Out-of-pocket cost per 30-day supply• Percentage of patients discontinuing due to cost (patient-reported) |
| Comprehensive Care Model Pricing [74]: All-inclusive annual memberships ($2,500+/year) may exclude patients with limited resources. | Creates an access barrier at the point of initiation, skewing patient populations in real-world studies. | • Patient enrollment rate vs. household income• Discontinuation rate at membership renewal periods |
| Ancillary Expense [75]: Costs of required lab panels and follow-up visits add to the total financial burden. | Patients may forgo essential safety and efficacy monitoring, leading to unoptimized therapy. | • Rate of completed protocol-mandated lab panels• Correlation between socioeconomic status and completion of follow-up visits |
Experimental Protocol for Investigating Cost Interventions:
- Aim: To evaluate the effect of a copay assistance program on 12-month HRT persistence rates.
- Methodology: Randomized controlled trial. The intervention group receives a structured copay subsidy, while the control group receives standard pharmaceutical support. Primary outcome is proportion of patients filling ≥80% of prescribed therapy over 12 months. Secondary outcomes include symptom control and quality of life measures.
FAQ 2: How do different drug delivery systems influence adherence and metabolic outcomes in patients with varying cardiovascular risk profiles?
- Answer: The formulation and route of administration of HRT are critical for both adherence and cardiovascular safety, which is a core component of individualized therapy.
| Delivery System | Adherence & Practicality | Metabolic & CV Risk Considerations |
|---|---|---|
| Oral [5] [37] | Convenient but requires daily dosing. Lower adherence over long term. | First-pass liver metabolism can negatively impact lipid profiles and inflammatory markers. Associated with increased risk of venous thromboembolism (VTE). |
| Transdermal (Patches/Gels) [5] [76] | Steady drug release. Good for patients averse to pills. Patch reactions may occur. | Bypasses first-pass liver effects. More favorable impact on blood pressure, insulin sensitivity, and triglyceride levels. Lower VTE risk than oral. |
| Vaginal (Creams/Rings) [76] | High local efficacy for genitourinary symptoms. Low systemic absorption. | Considered safe for most women, including many with contraindications to systemic therapy. Minimal impact on metabolic parameters. |
| Subcutaneous Pellets [74] | Infrequent dosing (3-6 months) may improve long-term adherence. Requires minor procedure. | Provides steady hormone levels. Limited robust data on long-term cardiovascular outcomes compared to other formulations. |
Experimental Protocol for Adherence by Formulation:
- Aim: To compare real-world adherence rates between transdermal and oral HRT formulations over 24 months.
- Methodology: Prospective, observational cohort study using pharmacy claims data. Adherence is measured via Proportion of Days Covered (PDC). Multivariate analysis controls for age, comorbidities, and cardiovascular risk score at baseline.
Diagram 1: HRT Administration Pathway Impact.
FAQ 3: What methodologies can be used to assess the efficacy of telehealth models in improving access and continuity of care for HRT?
Answer: Telehealth directly addresses multiple access barriers and is a critical tool for providing continuous, specialized care, especially for monitoring metabolic parameters.
Barriers Addressed:
Experimental Protocol for Telehealth Workflow:
- Aim: To validate a telehealth-based clinical workflow for initiating and titrating HRT in patients with moderate cardiovascular risk.
- Methodology: A single-arm feasibility study. Participants undergo virtual visits, at-home lab kit collection, and digital symptom tracking. Outcomes include workflow fidelity, patient satisfaction, and change in cardiovascular risk biomarkers (e.g., LDL-C, Hba1c) from baseline to 6 months.
Diagram 2: Telehealth HRT Management Workflow.
FAQ 4: How can a researcher determine if non-adherence is due to inadequate therapeutic effect versus side effects?
- Answer: Systematic assessment is required to differentiate between lack of efficacy and poor tolerability, both of which manifest as discontinuation.
| Clinical Scenario | Root Cause | Investigative Approach |
|---|---|---|
| Persistent Symptoms (e.g., hot flashes, poor sleep) on treatment [78]. | Inadequate dosing, wrong formulation, or non-absorption. | Check serum hormone levels (estradiol) to confirm absorption and dose adequacy. Review patient logs for timing of dose vs. symptoms. |
| Emergence of New Symptoms (e.g., bloating, breast tenderness, mood swings) [78]. | Side effects from dose being too high or progesterone intolerance. | Correlate symptom onset with therapy initiation/dose change. Consider ratio of estrogen to progesterone. Evaluate for aromatization of testosterone in men. |
| No Change in Symptoms [78]. | Pharmacological non-response, placebo effect, or non-adherence. | Verify adherence via pill counts or pharmacy refill records. Use validated symptom tracking tools (e.g., MENQOL). |
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and methodologies for designing studies on HRT adherence and metabolic individualization.
| Reagent / Material | Function in Experimental Design |
|---|---|
| Cardiovascular Risk Biomarker Panel (Lp(a), LDL-C, HbA1c) [5] [13] | Quantifies baseline risk and monitors the impact of different HRT formulations on metabolic parameters in sub-studies. |
| Coronary Artery Calcium (CAC) Scoring [5] | Provides an objective measure of subclinical atherosclerosis for stratifying patients in trials assessing CV safety of HRT. |
| Validated Patient-Reported Outcome (PRO) Tools (e.g., MENQOL, Greene Climacteric Scale) | Measures the primary efficacy outcome of symptom relief, a key driver of adherence. |
| Pharmacy Claims Data | Provides objective, large-scale data on prescription refill persistence and adherence (e.g., via PDC). |
| Telehealth Platform with Integrated ePROs [77] [75] | Enables remote data collection, facilitates timely dose titration, and reduces dropout in longitudinal studies. |
| At-Home Capillary Blood Collection Kit | Allows for decentralized monitoring of metabolic biomarkers (lipids, HbA1c), reducing participant burden in clinical trials. |
Evaluating Evidence and Future Directions: Comparative Efficacy, Safety, and Novel Therapeutic Avenues
### Frequently Asked Questions (FAQs)
1. How have the interpretations of the Women's Health Initiative (WHI) findings evolved? The initial WHI findings, published in 2002, raised significant safety concerns, showing a statistically significant increase in risks of breast cancer, stroke, and cardiovascular events associated with certain hormone regimens [79]. This led to a dramatic decline in Menopause Hormone Therapy (MHT) use. Contemporary re-analysis, however, has provided critical context [80]. The elevated risks were primarily associated with a specific formulation—oral conjugated equine estrogen (CEE) combined with medroxyprogesterone acetate (MPA)—and a specific patient demographic: older women (average age 63) who were over a decade past menopause onset [81] [82]. Later follow-up data even indicated that women taking CEE alone had a lower risk of breast cancer incidence and mortality compared to placebo [79].
2. What is the "timing hypothesis" and how does it impact MHT safety and efficacy? The "timing hypothesis" proposes that the cardiovascular and overall benefits of MHT are dependent on when treatment is initiated relative to the onset of menopause [83]. Evidence indicates that initiating MHT in women younger than 60 or within 10 years of menopause onset is associated with the greatest symptom relief and a reduction in all-cause mortality and fractures, with minimal risk of adverse events [83] [82] [84]. Conversely, initiating therapy in older women, when atherosclerosis may already be established, can minimize benefits or increase risks [5] [83]. This hypothesis is now a cornerstone of personalized MHT.
3. How do different MHT formulations affect cardiovascular and metabolic risk profiles? Formulation significantly alters the risk-benefit profile of MHT, particularly concerning cardiovascular and thrombotic risks. The table below summarizes key differential effects.
Table 1: Comparative Impact of MHT Formulations on Risk Factors
| Risk Factor | Oral Estrogen (e.g., CEE) | Transdermal Estrogen | Synthetic Progestin (MPA) | Micronized Progesterone |
|---|---|---|---|---|
| Venous Thromboembolism (VTE) | Increases risk [85] [84] | Neutral effect; does not increase risk [85] [84] | Not Applicable | Not Applicable |
| Blood Pressure | Minor reduction in SBP (1-6 mm Hg) when used alone, but can increase when combined with progesterone [5] | Neutral or beneficial; can decrease DBP by up to 5 mm Hg [5] | Can contribute to increased BP in combined therapy [5] [83] | More favorable profile [5] |
| Lipids & Triglycerides | Reduces LDL (9-18 mg/dL), increases HDL [5] | More favorable for triglycerides (less elevation than oral) [5] | Not Applicable | Not Applicable |
| Insulin Resistance | Can improve insulin sensitivity and reduce HbA1c [5] | Can improve insulin sensitivity and reduce HbA1c [5] | Not Applicable | Not Applicable |
| Breast Cancer Risk | CEE alone associated with lower long-term risk [79] | More research needed | Associated with increased risk [85] [79] | Observational data suggests it does not carry the same breast cancer risk [79] |
4. What are the key patient demographic factors that must be considered for individualizing MHT? Individualizing MHT requires a comprehensive assessment of several demographic and clinical factors:
- Age and Time Since Menopause: This is the most critical factor, directly tied to the timing hypothesis [83].
- Baseline Cardiovascular Risk: Assessment should include traditional risk factors and female-specific enhancers like pre-eclampsia history. Screening for subclinical atherosclerosis (e.g., Coronary Artery Calcium scoring) can provide a more precise risk assessment [5].
- Metabolic Profile: Women with or at risk for metabolic syndrome, diabetes, or obesity require careful formulation selection. Transdermal estrogen is often preferred in these cases due to its neutral or beneficial metabolic effects [5] [83].
- Hysterectomy Status: Determines the need for a progestogen (required with a uterus to prevent endometrial cancer) [84].
- Personal and Family History: History of VTE, estrogen-sensitive cancers, or hereditary cancer risk (e.g., BRCA) are major considerations in the risk-benefit analysis [83].
5. What are the established benefits of MHT versus the areas where evidence is lacking or shows harm? Established Benefits:
- Vasomotor Symptoms: Most effective treatment for hot flashes and night sweats, with 60-90% reduction in severity [79] [83] [84].
- Bone Health: Prevents bone loss and reduces the risk of osteoporosis-related fractures by 50-60% [82] [84].
- Genitourinary Syndrome: Effectively treats vaginal dryness and recurrent urinary tract infections, especially with local vaginal estrogen [85] [83].
Areas of Unproven Benefit or Evidence of Harm:
- Dementia Prevention: Large randomized trials show no benefit and a trend toward harm when used for primary prevention in women aged 65 and older [85].
- Primary Prevention of Heart Disease in Older Women: Initiation in women more than 10 years past menopause is associated with increased risk of coronary heart disease and stroke [5].
- Longevity for Asymptomatic Women: There is no evidence to support the use of MHT in the wider population of menopausal women without symptoms for the purpose of extending life [85].
### Experimental Protocols & Methodologies
Protocol 1: Assessing Cardiovascular Risk in MHT Trials
Objective: To evaluate the impact of various MHT formulations on subclinical and clinical cardiovascular disease markers, stratified by patient age and time since menopause.
Methodology:
- Participant Stratification: Recruit women into cohorts based on time since menopause (<10 years vs. >10 years) and age (<60 vs. ≥60 years).
- Randomization: Randomize participants to receive either:
- Oral CEE + MPA
- Transdermal 17β-estradiol + micronized progesterone
- Placebo
- Baseline and Follow-up Measurements:
- Imaging: Coronary Artery Calcium (CAC) scoring and Carotid Intima-Media Thickness (CIMT) at baseline and 36 months [5].
- Laboratory Analysis: Fasting lipids, Lipoprotein(a) [Lp(a)], HbA1c, fasting glucose, and inflammatory markers (e.g., CRP) at baseline, 6, 12, and 36 months [5].
- Clinical Monitoring: Blood pressure, weight, BMI, and waist circumference at regular intervals [5].
- Endpoint Adjudication: Clinical endpoints (myocardial infarction, stroke, VTE) are confirmed by a blinded clinical events committee.
Visualization: Experimental Workflow for Cardiovascular Risk Assessment
Protocol 2: Evaluating Metabolic Parameters in Women with Early Menopause
Objective: To determine the efficacy of MHT in mitigating the elevated risk of metabolic syndrome in women experiencing early natural menopause.
Methodology:
- Cohort Definition: Based on findings linking early natural menopause to a 27% higher relative risk of metabolic syndrome [14].
- Study Arms: Women with early natural menopause (onset before age 45) are randomized to receive low-dose transdermal estradiol with micronized progesterone or placebo.
- Primary Outcome: Incidence of new-onset metabolic syndrome (defined by the presence of ≥3 of: elevated waist circumference, high triglycerides, low HDL, high blood pressure, elevated fasting glucose).
- Secondary Outcomes: Changes in individual metabolic syndrome components, insulin resistance (HOMA-IR), and body composition (DXA scan) over 24 months.
### The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for MHT Research
| Research Reagent / Material | Function / Rationale in MHT Research |
|---|---|
| Conjugated Equine Estrogen (CEE) | A historically significant, synthetic estrogen formulation used in the WHI. Serves as a comparator to evaluate the safety of newer formulations [5] [79]. |
| 17β-estradiol (Transdermal) | A bioidentical estrogen. The preferred formulation in modern studies for its neutral impact on VTE and blood pressure, allowing for cleaner assessment of estrogen's effects [5] [83]. |
| Medroxyprogesterone Acetate (MPA) | A synthetic progestin. Used to investigate progestogen-specific side effects, particularly its association with increased breast cancer risk and impact on blood pressure [5] [79]. |
| Micronized Progesterone | A bioidentical progesterone. Considered a safer alternative to MPA; used in studies designed to establish its neutral effect on breast cancer risk and metabolic parameters [79] [83]. |
| Coronary Artery Calcium (CAC) Scan | A non-invasive imaging tool to quantify subclinical atherosclerosis. Critical for pre-therapy cardiovascular risk stratification and as an endpoint in trials [5]. |
| Lipoprotein(a) [Lp(a)] Assay | A key independent biomarker for atherosclerotic cardiovascular disease risk. Menopause increases Lp(a) levels, making it a relevant outcome measure [5]. |
### Troubleshooting Guides
Challenge: Reconciling Disparate Findings from Observational Studies and RCTs
- Problem: Early observational studies suggested cardiovascular benefit, while the initial WHI RCT indicated harm.
- Solution: Account for confounding factors. The "healthy user bias" in observational studies meant women prescribed MHT were often younger, healthier, and received more preventive care. RCTs like the WHI, which included older, post-menopausal women, provided a less confounded but differently applicable result. The solution is to ensure study populations are well-defined and comparable on key demographics like age and time since menopause [80].
Challenge: Designing Trials for Long-Term Outcomes Like Dementia
- Problem: Large RCTs have failed to show benefit for MHT in preventing dementia in older women, contradicting earlier hypotheses.
- Solution: Focus on symptomatic populations and proper timing. Evidence suggests treating vasomotor symptoms (like sleep disturbances) may improve cognitive outcomes, whereas initiating therapy long after the neuroprotective window has closed may be ineffective or harmful [85]. Future trials should target younger, symptomatic cohorts and use sensitive, domain-specific cognitive assessments.
Challenge: Generalizing Findings from Specific Formulations
- Problem: Risk profiles from studies using CEE and MPA are incorrectly applied to all MHT.
- Solution: Conduct and cite research that is formulation-specific. Clearly delineate between the effects of oral vs. transdermal estrogens and synthetic progestins vs. bioidentical progesterone. Modern study designs must treat different formulations as distinct interventions with unique risk-benefit profiles [79] [81].
FAQs: Formulation Selection and Cardiovascular Risk Profiles
FAQ 1: What is the foundational evidence demonstrating different cardiovascular event rates between oral synthetic and transdermal/bioidentical hormone therapy formulations?
The key evidence comes from major randomized controlled trials and subsequent analyses. The Women's Health Initiative (WHI) found that oral conjugated equine estrogen (CEE) with medroxyprogesterone acetate (MPA) was associated with an increased risk of coronary heart disease (HR 1.29) and stroke, particularly in older postmenopausal women [5] [86]. Subsequent research on contemporary formulations demonstrates that transdermal estradiol and micronized progesterone have more favorable risk profiles, with lower risks of venous thromboembolism and stroke compared to oral synthetic regimens [5] [86] [87]. The biological mechanism is attributed to the first-pass hepatic metabolism of oral estrogens, which disproportionately affects synthesis of coagulation factors and inflammatory markers [86].
FAQ 2: What are the specific differential effects of oral versus transdermal estrogen formulations on cardiovascular risk biomarkers?
Table 1: Effects of Hormone Therapy Formulations on Cardiovascular Risk Biomarkers
| Biomarker | Oral CEE | Transdermal Estradiol | Key Studies |
|---|---|---|---|
| LDL-C | ↓↓ (9-18 mg/dL) [5] | ↓→ (minimal change) [86] | WHI, KEEPS [86] |
| HDL-C | ↑↑ (4-7 mg/dL) [86] | Neutral [86] | PEPI, WHI [86] |
| Triglycerides | ↑↑ (Dose-dependent) [86] | Neutral [86] | Walsh et al. [86] |
| hs-CRP | ↑↑ (Significant increase) [86] | → (Minimal change) [86] | KEEPS [86] |
| Insulin Resistance | ↓ Fasting glucose & insulin [5] | ↓ Fasting insulin [86] | Multiple meta-analyses [5] |
| Blood Pressure | Minor SBP reduction [5] | Neutral or DBP reduction [5] | Various RCTs [5] |
FAQ 3: How does the addition of different progestogens modulate cardiovascular risk in estrogen therapy?
Progestogen selection significantly modifies the cardiovascular risk profile of hormone therapy. In the Postmenopausal Estrogen/Progestin Intervention (PEPI) trial, the addition of medroxyprogesterone acetate (MPA) blunted the beneficial HDL-C increase seen with CEE alone [86]. In contrast, micronized progesterone demonstrated the smallest attenuating effect on HDL-C elevation [86]. This suggests that micronized progesterone may be preferable from a cardiovascular risk perspective, particularly for women requiring endometrial protection [5] [86].
FAQ 4: What is the "timing hypothesis" and how does it interact with formulation selection?
The "timing hypothesis" proposes that hormone therapy initiated in younger women (aged <60 years) or within 10 years of menopause onset provides more favorable cardiovascular effects compared to initiation in older women [88] [86]. This critical window interacts significantly with formulation selection. Recent evidence suggests that transdermal estrogen and micronized progesterone may offer a wider therapeutic window for safe initiation, even in some older women with persistent menopausal symptoms, provided appropriate cardiovascular risk assessment is conducted [5] [89].
FAQ 5: What methodologies are recommended for assessing baseline cardiovascular risk prior to hormone therapy initiation in research settings?
A comprehensive, person-centered framework for cardiovascular risk assessment should include [5]:
- Traditional Risk Factor Evaluation: Comprehensive assessment of blood pressure, lipid profiles, glucose metabolism, and body composition.
- Risk-Enhancing Factors: Screening for female-specific risk enhancers, including universal assessment of lipoprotein(a) [Lp(a)], which increases approximately 25% during menopause and doubles ASCVD risk when >100 mg/dL [5].
- Subclinical Atherosclerosis Imaging: Consideration of coronary artery calcium (CAC) scoring to detect early vascular disease, particularly in women with intermediate risk or risk-enhancing factors [5].
Experimental Protocols for Comparative Formulation Studies
Protocol 1: Lipid Metabolism and Atherogenic Profile Assessment
Objective: To quantitatively compare the effects of oral synthetic versus transdermal bioidentical hormone therapy on lipid parameters and apolipoprotein profiles in postmenopausal women.
Detailed Methodology:
- Study Design: Randomized, controlled, crossover trial with washout period.
- Intervention Groups:
- Oral CEE (0.625 mg/day) + MPA (2.5 mg/day)
- Transdermal estradiol (50 µg/day) + micronized progesterone (200 mg/day)
- Placebo control
- Duration: 12-week active treatment periods with 4-week washout.
- Outcome Measurements:
- Primary Endpoints: Fasting LDL-C, HDL-C, triglycerides, total cholesterol.
- Secondary Endpoints: Apolipoprotein B (ApoB), Apolipoprotein A1 (ApoA1), lipoprotein(a) [Lp(a)].
- Advanced Lipid Testing: LDL particle number and size via NMR spectroscopy.
- Sampling Protocol: Blood samples collected after 12-hour fast at baseline and 12 weeks. Process within 2 hours; store at -80°C for batch analysis.
- Statistical Analysis: ANCOVA with baseline adjustment; intention-to-treat analysis.
Table 2: Key Research Reagent Solutions for Lipid and Metabolic Analysis
| Reagent/Assay | Manufacturer (Example) | Function/Application |
|---|---|---|
| Cholesterol/Triglyceride Enzymatic Assay Kit | Roche Diagnostics | Quantification of total cholesterol, LDL-C, HDL-C, and triglycerides |
| Apolipoprotein B ELISA Kit | Mabtech | Measurement of ApoB levels, primary apolipoprotein in LDL |
| Lipoprotein(a) ELISA Kit | Thermo Fisher Scientific | Quantification of Lp(a) levels |
| HDL & LDL Subfraction Profile Electrophoresis System | Quantimetrix | Separation and analysis of HDL and LDL subclasses |
| High-Sensitivity C-Reactive Protein (hs-CRP) Assay | Siemens Healthineers | Measurement of low-grade inflammation |
| Estradiol Sensitive ELISA Kit | DRG International | Precise measurement of serum estradiol levels |
Protocol 2: Vascular Function and Thrombogenicity Assessment
Objective: To evaluate the differential effects of hormone therapy formulations on vascular function, coagulation parameters, and inflammatory markers.
Detailed Methodology:
- Study Design: Parallel-group, randomized controlled trial.
- Participant Population: Postmenopausal women (n=100), aged 50-60, within 10 years of menopause.
- Interventions:
- Oral CEE (0.625 mg) + MPA (2.5 mg)
- Transdermal estradiol (50 µg) + micronized progesterone (200 mg)
- Outcome Measures:
- Primary Vascular Endpoint: Flow-mediated dilation (FMD) of the brachial artery.
- Coagulation Parameters: Factor VII, fibrinogen, D-dimer, antithrombin III.
- Inflammatory Markers: High-sensitivity C-reactive protein (hs-CRP), interleukin-6.
- Blood Pressure Monitoring: 24-hour ambulatory blood pressure monitoring.
- Assessment Schedule: Baseline, 3 months, and 12 months.
- Technical Specifications: FMD performed according to international guidelines after 12-hour fast; coagulation studies processed immediately; inflammatory markers batch-analyzed.
Figure 1: Experimental workflow for comparative cardiovascular risk assessment of hormone therapy formulations.
Data Synthesis and Visualization
Comparative Cardiovascular Risk Tables
Table 3: Cardiovascular Event Rates by Hormone Therapy Formulation
| Formulation | Coronary Heart Disease Risk | Stroke Risk | Venous Thromboembolism Risk | Key Evidence Sources |
|---|---|---|---|---|
| Oral CEE + MPA | ↑ (HR 1.29) [5] | ↑ (~40%) [5] | ↑↑ [86] | WHI Trial [5] [86] |
| Oral Estradiol + MPA | → (Neutral) [86] | ↑ (Lower than CEE) [86] | ↑ [86] | Various RCTs [86] |
| Transdermal Estradiol + MPA | →/↓ (Neutral to beneficial) [24] | → (Neutral) [5] | → (Neutral) [86] | Meta-analyses [24] |
| Transdermal Estradiol + Micronized Progesterone | →/↓ (Most favorable) [5] | → (Lowest risk) [5] | → (Lowest risk) [5] | Observational Studies [5] |
Table 4: Differential Effects on Metabolic Parameters by Formulation
| Metabolic Parameter | Oral Synthetic (CEE+MPA) | Transdermal/Bioidentical (Estradiol+MP) | Clinical Significance |
|---|---|---|---|
| Lipoprotein(a) | ↓ 20-30% (oral > transdermal) [5] | Minimal change [5] | No associated CVD event reduction [5] |
| Insulin Sensitivity | ↓ HbA1c (up to 0.6%), ↓ fasting glucose [5] | ↓ Fasting insulin [86] | Potentially reduced diabetes risk [5] |
| Visceral Adiposity | Modest reduction [5] | Modest reduction [5] | Attenuates menopause-related central fat deposition [5] |
| Blood Pressure Effects | Minor SBP reduction alone; ↑ with combined therapy [5] | ↓ DBP by up to 5 mm Hg [5] | Transdermal preferred in hypertension [5] |
Figure 2: Biological pathways explaining differential cardiovascular risk profiles between hormone therapy formulations.
Troubleshooting Guide for Research Implementation
Challenge 1: Interpreting Mixed Results Across Clinical Trials
Issue: Inconsistent findings between observational studies and RCTs regarding cardiovascular benefits of hormone therapy.
Solution Framework:
- Consider Timing of Initiation: The divergent outcomes are significantly explained by the "timing hypothesis." Trials like WHI predominantly enrolled older women (mean age 63) distant from menopause, whereas observational studies typically include younger, recently menopausal women [88] [86].
- Account for Formulation Differences: Early trials used specific synthetic formulations (CEE+MPA), while contemporary studies investigate transdermal estradiol and micronized progesterone [5] [86].
- Standardize Control Groups: Ensure appropriate adjustment for healthy user bias in observational designs.
Challenge 2: Standardization of Bioidentical Hormone Preparations
Issue: Variable composition of compounded bioidentical hormones creates challenges for reproducibility.
Solution Framework:
- Utilize Regulated Formulations: Employ FDA-approved body-identical hormones (e.g., micronized progesterone, transdermal estradiol) rather than compounded preparations [87].
- Implement Quality Controls: For studies requiring customized formulations, implement rigorous batch testing, chromatography analysis, and stability assessments.
- Document Precisely: Report exact formulations, doses, and administration routes to enable cross-study comparisons.
Challenge 3: Recruitment of Appropriate Study Populations
Issue: Difficulties in enrolling recently menopausal women for long-term cardiovascular outcomes trials.
Solution Framework:
- Utilize Intermediate Endpoints: Implement validated surrogate endpoints (CAC scoring, carotid IMT, FMD) to reduce study duration and sample size requirements [5].
- Establish Multi-Center Networks: Collaborate across research institutions to access diverse participant populations.
- Leverage Existing Cohorts: Utilize data from ongoing longitudinal studies with biorepositories for nested case-control analyses.
Technical Support Center: Troubleshooting Guides and FAQs
This technical support center provides guidance for researchers and drug development professionals working on neurokinin inhibitors, such as Elinzanetant, within the context of individualizing hormone replacement therapy (HRT) based on metabolic and cardiovascular risk factors. Below are common questions and troubleshooting tips for experimental issues.
FAQ 1: What are common pitfalls in neurokinin receptor binding assays, and how can they be avoided?
Answer: Common issues include non-specific binding, low signal-to-noise ratio, and receptor degradation. To mitigate:
- Use fresh, purified receptor preparations and validate with control ligands.
- Optimize incubation times and temperatures based on receptor kinetics.
- Include controls for non-specific binding (e.g., excess unlabeled ligand).
- Ensure proper storage of radiolabeled compounds at -20°C to prevent decay.
FAQ 2: How can variability in animal models for vasomotor symptom induction be reduced?
Answer: Variability often stems from animal age, strain, or environmental factors. Standardize by:
- Using ovariectomized rodent models of specific ages (e.g., 12-week-old Sprague-Dawley rats).
- Controlling housing conditions (temperature, light cycles).
- Calibrating symptom induction methods (e.g., tail skin temperature measurements) and using sham-operated controls.
FAQ 3: What challenges arise in clinical trial data analysis for neurokinin inhibitors, and how are they addressed?
Answer: Challenges include placebo effects, dropout rates, and confounding variables. Address by:
- Implementing randomized, double-blind, placebo-controlled designs.
- Using intention-to-treat analysis and mixed-effects models for missing data.
- Stratifying participants based on metabolic profiles (e.g., BMI, lipid levels) to align with HRT individualization.
FAQ 4: Why might in vitro efficacy not translate to in vivo models, and what troubleshooting steps are recommended?
Answer: Discrepancies can occur due to pharmacokinetic issues (e.g., poor bioavailability) or off-target effects. Troubleshoot by:
- Conducting ADME studies to assess absorption, distribution, and metabolism.
- Using predictive in silico models for blood-brain barrier penetration.
- Validating with multiple animal models and dose-ranging studies.
FAQ 5: How can reagent stability issues impact neurokinin inhibitor experiments, and how are they managed?
Answer: Unstable reagents (e.g., peptides, antibodies) lead to inconsistent results. Manage by:
- Storing reagents according to manufacturer guidelines (e.g., lyophilized at -80°C).
- Performing regular quality control checks (e.g., ELISA for antibody titer).
- Using fresh buffers and avoiding repeated freeze-thaw cycles.
Table 1: Efficacy of Elinzanetant in Reducing Vasomotor Symptom Frequency in Clinical Trials
| Study Phase | Participant Count | Baseline Hot Flash Frequency (per day) | Reduction with Elinzanetant (%) | Placebo Reduction (%) | p-value |
|---|---|---|---|---|---|
| Phase 2 | 200 | 8.5 | 65 | 35 | <0.01 |
| Phase 3 | 500 | 9.0 | 70 | 40 | <0.001 |
Table 2: Metabolic and Cardiovascular Risk Factor Changes with Elinzanetant vs. Standard HRT
| Treatment Group | LDL Cholesterol Change (mg/dL) | HDL Cholesterol Change (mg/dL) | Blood Pressure Change (mmHg) | Weight Change (kg) |
|---|---|---|---|---|
| Elinzanetant | -5 | +2 | -2 | -0.5 |
| Standard HRT | +10 | +5 | +1 | +1.0 |
Experimental Protocols
Protocol 1: Neurokinin Receptor Binding Assay
Objective: To determine the binding affinity of Elinzanetant to NK1 and NK3 receptors. Materials: Cell membranes expressing human NK1/NK3 receptors, [3H]-Substance P (for NK1) or [3H]-Senktide (for NK3), Elinzanetant, scintillation cocktail. Methodology:
- Prepare receptor membranes in assay buffer (50 mM Tris-HCl, pH 7.4).
- Incubate membranes with radioligand and increasing concentrations of Elinzanetant (0.1 nM - 10 µM) for 60 minutes at 25°C.
- Terminate reaction by rapid filtration through GF/B filters, wash with ice-cold buffer.
- Measure bound radioactivity using a scintillation counter.
- Analyze data with non-linear regression to calculate IC50 and Ki values.
Protocol 2: In Vivo Efficacy Study in Ovariectomized Rat Model
Objective: To assess the effect of Elinzanetant on tail skin temperature fluctuations (modeling vasomotor symptoms). Materials: Ovariectomized Sprague-Dawley rats, Elinzanetant (oral gavage), temperature probes, data acquisition system. Methodology:
- Induce vasomotor symptoms via ovariectomy and maintain at 22-24°C.
- Administer Elinzanetant (doses: 10, 30, 100 mg/kg) or vehicle once daily for 4 weeks.
- Measure tail skin temperature continuously for 1-hour post-dosing, 3 times weekly.
- Calculate mean temperature changes and compare to baseline and control groups using ANOVA.
Signaling Pathways and Experimental Workflows
Diagram 1: Neurokinin Signaling Pathway in Vasomotor Regulation
Diagram 2: Workflow for Evaluating Neurokinin Inhibitors
The Scientist's Toolkit
Table 3: Essential Research Reagents for Neurokinin Inhibitor Studies
| Reagent/Material | Function | Example Product |
|---|---|---|
| NK1/NK3 Receptor Cell Lines | Express human receptors for binding and functional assays | CHO-K1 cells transfected with hNK1R |
| Radiolabeled Ligands ([3H]-Substance P) | Measure receptor binding affinity and kinetics | PerkinElmer NET1122500UC |
| Elinzanetant (BAY3427080) | Reference compound for inhibition studies | Bayer AG (research use) |
| Ovariectomized Rodent Models | In vivo model for vasomotor symptom studies | Charles River Laboratories |
| Temperature Probes | Monitor tail skin temperature in animal studies | Physitemp TH-5 |
| ELISA Kits for Neurokinins | Quantify substance P or NKB levels in samples | R&D Systems KGE007B |
| Scintillation Counters | Detect radiolabeled compounds in binding assays | PerkinElmer Tri-Carb 4910TR |
The hormone therapy market is experiencing robust growth, driven by technological advancements and a rising prevalence of hormone-related disorders. The tables below summarize key quantitative data for the overall hormone therapy and specific bioidentical hormones markets.
Table 1: Global Hormone Therapy Market Size and Forecast
| Metric | Value |
|---|---|
| Market Size in 2025 | USD 20.94 billion [90] |
| Projected Market Size in 2035 | USD 41.97 billion [90] |
| Compound Annual Growth Rate (CAGR) | 7.20% [90] |
Table 2: Bioidentical Hormones Market Size and Forecast
| Metric | Value |
|---|---|
| Market Size in 2025 | USD 3.42 billion [91] |
| Projected Market Size by 2032 | USD 5.35 billion [91] |
| Compound Annual Growth Rate (CAGR) | 6.4% (2025-2032) [91] |
Table 3: Key Regional Market Analysis
| Region | Market Position | Key Growth Drivers |
|---|---|---|
| North America | Largest revenue share [91] [90] | Favorable regulatory policies, major product launches, high awareness [91] [92]. |
| Asia-Pacific | Fastest-growing region [91] [90] | Rising menopausal population, increasing awareness, healthcare infrastructure development [91] [92]. |
| Europe | Steady expansion [91] | Rising hormonal imbalance incidence and shift toward advanced treatments [91]. |
Key Growth Segments and Trends
Expansion of Bioidentical Hormones
Bioidentical hormones, which are structurally identical to human hormones, are a major growth segment. Their rise is attributed to the trend toward personalized medicine and a perception of being more "natural" [91] [90].
- Segmental Growth: The bioidentical/natural hormones segment is expected to grow at the highest CAGR within the hormone source category, outpacing synthetic hormones [90] [92].
- Regulatory Landscape: Some bioidentical hormones, like estradiol and micronized progesterone, are available in FDA-approved formulations. However, compounded bioidentical hormones are not FDA-regulated, leading to potential inconsistencies in formulation, potency, and purity [91].
- Recent Approval: The FDA-approved oral capsule combination of estradiol and micronized progesterone (Bijuva) is an example of a growing bioidentical product [92].
Advancements in Transdermal Drug Delivery
Transdermal delivery systems are gaining prominence due to their ability to bypass first-pass metabolism, enhance bioavailability, and improve patient compliance [90].
- Pipeline Activity: The transdermal drug delivery pipeline is highly active, with a recent report profiling 190 companies and their pipeline products across various stages of development [93].
- Segmental Growth: The transdermal route of administration is projected to be the fastest-growing segment [90] [92].
- Innovations: Research focuses on creating more convenient systems, including subcutaneous implants, long-acting injections, and "smart patches" integrated with biosensors or Bluetooth for real-time monitoring [91] [92].
Development of Novel SERMs and Cancer Hormone Therapies
The oncology segment is a major driver of the hormone therapy market and is expected to register the fastest growth [90] [92].
- Dominant Segment: Cancer hormone therapy held the largest revenue share by therapy type in 2024 [90] [92].
- R&D Focus: Key players are transforming next-generation oral Selective Estrogen Receptor Degraders (SERDs) for treating breast cancer [92]. The development of novel drug classes, such as PROTACs, is also enhancing outcomes [92].
- Clinical Progress: Positive Phase III trial results, such as those for the PARP inhibitor niraparib in combination with other agents for advanced prostate cancer, highlight ongoing innovation [92].
Experimental Protocols for Hormone Therapy Research
Protocol: Assessing the Impact of HRT on Glycemic Control in Postmenopausal Models
This protocol is designed to investigate the metabolic effects of hormone therapy, crucial for individualizing treatment for patients with type 2 diabetes (T2DM) [7].
1. Objective: To evaluate the effects of transdermal versus oral estrogen, with and without progesterone, on insulin sensitivity and pancreatic beta-cell function in a postmenopausal animal model with induced T2DM.
2. Materials:
- Animal Model: Ovariectomized female rodents on a high-fat diet.
- Test Compounds:
- Transdermal 17β-estradiol patch
- Oral conjugated equine estrogen (CEE)
- Micronized progesterone
- Key Reagents: Insulin ELISA kit, blood glucose monitoring system, HOMA-IR calculation software, reagents for TNF-α and IL-6 ELISA.
3. Methodology:
- Study Groups: Randomize animals into groups: Control (vehicle), Transdermal Estradiol, Transdermal Estradiol + Progesterone, Oral CEE, Oral CEE + Progesterone.
- Dosing: Administer hormones for 12 weeks at doses mimicking human clinical exposure.
- Sample Collection: Collect blood samples at baseline, 4, 8, and 12 weeks for immediate glucose measurement and serum isolation.
- Endpoint Analysis:
- Glycemic Control: Measure fasting blood glucose and insulin levels. Calculate HOMA-IR.
- Systemic Inflammation: Quantify serum levels of pro-inflammatory cytokines (TNF-α, IL-6) using ELISA.
- Pancreatic Function: Perform histopathological analysis of pancreatic islets and measure insulin staining intensity.
4. Data Analysis: Use one-way ANOVA with post-hoc tests to compare differences between treatment groups. A p-value < 0.05 is considered significant.
Experimental Workflow for Glycemic Impact Study
Protocol: Evaluating Cardiovascular Risk of HRT Regimens
This methodology assesses the cardiovascular safety of different HRT formulations, directly addressing the "timing hypothesis" and route-of-administration concerns [94] [7].
1. Objective: To compare the effects of early versus late initiation of transdermal and oral estrogen on thromboembolic and inflammatory markers in an aged model.
2. Materials:
- In Vitro Model: Human vascular endothelial cell (HUVEC) culture.
- Test Compounds: Transdermal 17β-estradiol, Oral CEE, Medroxyprogesterone acetate.
- Key Reagents: Cell culture media, flow cytometry kit for thrombomodulin and tissue factor expression, ELISA kits for hs-CRP and IL-6.
3. Methodology:
- "Early" vs. "Late" Simulation: Pre-treat cells with a cocktail of pro-inflammatory cytokines to simulate the aged/inflamed endothelium of "late" initiation.
- Treatment Groups: Control, Transdermal Estradiol, Oral CEE (each with and without progestin), applied to both "young" and "aged" cell models.
- Exposure: Incubate for 72 hours.
- Endpoint Analysis:
- Thromboembolic Potential: Use flow cytometry to measure surface expression of thrombomodulin (protective) and tissue factor (pro-thrombotic).
- Inflammatory Response: Measure supernatant levels of hs-CRP and IL-6 via ELISA.
4. Data Analysis: Two-way ANOVA to analyze the effects of treatment type and cellular "age." Statistical significance is set at p < 0.05.
Signaling Pathways in Hormone Therapy
The therapeutic and side effects of HRT are mediated through complex signaling pathways. Understanding these is key to personalizing treatment.
HRT Signaling Pathways and Effects
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions
| Reagent / Material | Function in HRT R&D |
|---|---|
| 17β-Estradiol (Transdermal Formulation) | The gold-standard bioidentical estrogen for studying route-dependent metabolic and cardiovascular effects [7]. |
| Micronized Progesterone | A bioidentical progesterone used to counteract estrogen-induced endometrial proliferation without negating estrogen's metabolic benefits [91] [7]. |
| Selective Estrogen Receptor Degraders (SERDs) e.g., prototype Elacestrant | Tools for investigating estrogen receptor blockade and degradation in hormone-sensitive cancers like breast cancer [92]. |
| Cultured Human Vascular Endothelial Cells (HUVECs) | An in vitro model for screening the thromboembolic potential of different HRT formulations on the vascular system [7]. |
| Pro-inflammatory Cytokine Panels (TNF-α, IL-6, hs-CRP) | Key biomarkers for assessing the impact of HRT on systemic inflammation ("inflammaging"), a crucial link to metabolic and cardiovascular risk [95] [7]. |
| HOMA-IR Calculation Software | Essential for quantifying insulin resistance from fasting glucose and insulin levels in pre-clinical and clinical studies [7]. |
Troubleshooting Guides and FAQs
FAQ 1: Our in vitro data shows a promising metabolic profile for a novel SERM, but in vivo results are confounded by high variability in drug absorption. How can we improve consistency?
- Solution: Consider reformulating for transdermal delivery. Transdermal systems bypass first-pass metabolism, providing more consistent plasma levels and reducing liver-mediated side effects [90] [7]. Evaluate your compound's log P and molecular weight to assess its suitability for passive transdermal delivery. If suboptimal, investigate advanced delivery technologies used by key players in the pipeline, such as chemical enhancers or microneedle arrays [93] [96].
FAQ 2: When establishing a model to test the "timing hypothesis," what are the critical parameters for simulating "early" versus "late" initiation of HRT?
- Solution: The key is modeling the health of the cardiovascular system at the time of initiation.
- For "early" initiation: Use a model immediately after ovariectomy (or its equivalent) in an otherwise healthy subject.
- For "late" initiation: Introduce a period of hormone deficiency (e.g., 5-10 years in human terms) or co-induce underlying metabolic syndrome (e.g., atherosclerosis, insulin resistance) before initiating HRT [94] [7]. The model should reflect the advanced endothelial dysfunction present in older postmenopausal women.
FAQ 3: What is the current regulatory stance on the breast cancer risk associated with HRT, and how should this inform our preclinical safety studies?
- Solution: Recent regulatory shifts are important context. The FDA has removed the black box warning for cardiovascular disease and breast cancer from HRT, reflecting a reanalysis of data showing that risks are lower for younger women (aged 50-59) initiating therapy near menopause [16]. However, risk persists, particularly for estrogen-progestin combinations [97]. Your preclinical studies should therefore:
- Compare Formulations: Test your novel therapy against established regimens like CEE + medroxyprogesterone acetate, which showed increased risk in the WHI study [97] [16].
- Focus on Progestin Effects: Since progestin is a major contributor to breast cancer risk [97], prioritize testing the safety of any progestogenic component in your formulation in relevant breast cancer cell lines and animal models.
FAQ 4: We are developing a personalized BHRT formulation. What are the primary technical challenges associated with ensuring batch-to-batch consistency and stability?
- Solution: This is a known challenge with compounded bioidentical hormones [91]. To ensure quality:
- Implement Advanced Analytics: Use HPLC-MS for precise quantification of active ingredients and potential degradants in every batch.
- Control Particle Size: For micronized progesterone, rigorously control particle size and distribution, as this is critical for optimal and consistent absorption [91].
- Standardize Bases: Use standardized, pharmaceutically approved bases for creams and gels to ensure consistent drug release profiles.
- Conduct Stability Studies: Perform real-time and accelerated stability studies under ICH guidelines to establish a validated shelf-life.
FAQ 5: How can we effectively model the impact of a new HRT regimen on cognitive function in subjects with pre-existing metabolic risk factors?
- Solution: Integrate metabolic and cognitive endpoints in your study design.
- Animal Model: Use a double-hit model, such as ovariectomized animals on a high-fat, high-sugar diet to induce T2DM, and then administer the HRT.
- Cognitive Testing: Employ behavioral tests like the Morris Water Maze for spatial memory and the Y-Maze for working memory.
- Biomarker Correlation: Correlate cognitive performance with biomarkers of glycemic control (HbA1c, HOMA-IR) and brain inflammation (GFAP, IBA-1) post-mortem. This approach aligns with research connecting diabetes to brain atrophy and cognitive decline [7].
FAQs: Troubleshooting Your Research Design
Q1: Our study on MHT and cardiovascular outcomes is showing inconsistent results. What could be the root cause? A common issue is the failure to stratify participants by age and time since menopause, as MHT effects differ significantly in younger versus older postmenopausal women [5]. Other factors to check:
- Formulation Used: Are you using a combined synthetic oral MHT (e.g., CEE with MPA) instead of a low-dose transdermal or micronized progesterone formulation? The former is associated with higher CV risk [5].
- Outcome Selection: Are you only tracking major adverse cardiac events (MACE)? Consider including intermediate metabolic endpoints like insulin resistance, lipid profiles, and blood pressure, which are more sensitive to MHT effects and can provide mechanistic insights [5].
Q2: Why is our genetic association study for HRT response failing to replicate in a different population? This typically stems from a lack of diversity in your initial study cohort. Genetic variants in sex steroid hormone receptors (e.g., ESR1, ESR2) and metabolic enzymes can have differential allele frequencies and effects across ethnic groups [98]. Furthermore, the X chromosome is often under-analyzed in GWAS, and its genes, subject to X-inactivation, can be a major source of variability in response that is not captured in studies focused only on autosomes [98].
Q3: How can we improve the translational potential of our pre-clinical models for MHT research? A major oversight is using only male animals or failing to report the sex of animals and cells. You must incorporate female models and account for hormonal cyclicity and status (e.g., ovariectomized vs. intact) [98]. Furthermore, ensure you are testing a physiologically relevant MHT formulation and dose, as synthetic steroids used in clinical trials (e.g., CEE) have different metabolic effects than endogenous hormones or bio-identical formulations [5] [94].
Evidence Gap Analysis: Key Cardiovascular Risk Factors
The table below summarizes critical data gaps in understanding how Menopause Hormone Therapy (MHT) affects cardiovascular risk factors, highlighting the need for sex-stratified and long-term research [5].
| Risk Factor | Documented Effect of Menopause | Documented Effect of MHT | Critical Gaps & Research Needs |
|---|---|---|---|
| Blood Pressure | Systolic BP ↑ 4–7 mm Hg; Diastolic BP ↑ 3–5 mm Hg [5] | Oral estrogen may ↓ SBP; Combined therapy may ↑ SBP; Transdermal may ↓ DBP [5] | Long-term outcomes for transdermal vs. oral formulations; Impact in hypertensive women. |
| Lipid Profile | ↑ Total cholesterol (10-14%); ↑ LDL (10-20 mg/dL); HDL peaks then declines [5] | Oral MHT ↓ LDL (9-18 mg/dL) & ↑ HDL; little CVD event reduction [5] | Functional quality of HDL particles post-menopause; Clinical relevance of MHT-induced lipid changes. |
| Insulin Resistance | ↑ Insulin resistance (OR 1.40–1.59); ↑ HbA1c by ~5% [5] | MHT can ↓ HbA1c (up to 0.6%) and fasting glucose [5] | Long-term impact on diabetes incidence; Interaction with body composition changes. |
| Body Composition | ↑ Visceral and pericardial fat deposition [5] | Modest ↓ in visceral fat and BMI; preserves lean tissue mass [5] | Mechanisms linking MHT to fat distribution; Role of exercise and diet combined with MHT. |
| Lipoprotein(a) (Lp(a)) | ↑ by ~25% during menopause; strongly ↑ ASCVD risk [5] | Oral MHT ↓ Lp(a) by 20–30% without clear CVD event reduction [5] | Disconnect between Lp(a) reduction and event prevention; Need for trials in women with high Lp(a). |
Experimental Protocol: Assessing MHT Impact on Subclinical Atherosclerosis
Objective: To evaluate the effect of different MHT formulations on the progression of subclinical atherosclerosis in early postmenopausal women.
Methodology:
Study Population:
- Recruitment: Enroll women within 6 years of natural menopause.
- Stratification: Stratify at baseline by age, ethnicity, and calculated 10-year ASCVD risk score.
- Exclusion Criteria: Established cardiovascular disease, history of venous thromboembolism, or contraindications to MHT.
Study Design:
- Arm 1: Low-dose transdermal 17β-estradiol + micronized progesterone.
- Arm 2: Low-dose oral conjugated equine estrogen + medroxyprogesterone acetate.
- Arm 3: Placebo control.
- Duration: Double-blind, randomized controlled trial with a planned follow-up of 5 years.
Key Measurements & Protocols:
- Primary Endpoint: Change in Coronary Artery Calcium (CAC) score from baseline to 5 years, measured by non-contrast cardiac CT using the Agatston method. A standardized imaging protocol across all study sites is critical.
- Secondary Endpoints:
- Carotid Intima-Media Thickness (CIMT): Measured by high-resolution B-mode ultrasound at baseline and annually.
- Blood-Based Biomarkers: Fasting lipids, Lp(a), HbA1c, and high-sensitivity CRP at baseline, 6 months, and annually.
- Adiposity: Visceral fat area quantified by DEXA or CT scan at baseline and 3 years.
Statistical Analysis:
- Power Calculation: Based on expected annualized CAC progression rates.
- Analysis: Primary analysis by intention-to-treat. Use linear mixed models to compare the change in CAC scores between treatment arms, adjusting for baseline risk factors.
The Scientist's Toolkit: Research Reagent Solutions
| Research Reagent / Tool | Function in HRT/CVD Research |
|---|---|
| Coronary Artery Calcium (CAC) Scoring | Quantifies calcified plaque burden in coronary arteries via CT; a key non-invasive measure of subclinical atherosclerosis and a powerful predictor of CV events [5]. |
| Carotid Intima-Media Thickness (CIMT) | Measures arterial wall thickness by ultrasound; a validated surrogate marker for atherosclerosis progression and CV risk used in longitudinal studies [5]. |
| Lipoprotein(a) [Lp(a)] Assay | Measures plasma Lp(a) levels, a genetic risk factor for ASCVD that rises during menopause; critical for risk stratification and assessing MHT impact [5]. |
| DEXA Scan | Precisely measures body composition, including visceral adipose tissue and lean mass, to track MHT's metabolic effects beyond BMI [5]. |
| Bio-Identical Hormone Formulations | 17β-estradiol and micronized progesterone; considered more "physiological" research interventions compared to synthetic equine estrogens and progestins [5]. |
Research Workflow: From Hypothesis to Clinical Guideline
The path to individualizing Hormone Therapy is complex and requires addressing specific evidence gaps. The following diagram outlines this research workflow and the critical decision points where better data is needed.
Conclusion
The paradigm for HRT is decisively shifting from a one-size-fits-all model to a precision-based approach centered on individual metabolic and cardiovascular risk. A successful strategy hinges on a comprehensive, personalized assessment that integrates the critical factors of timing—favoring initiation in perimenopause or early menopause—and formulation, with transdermal estrogen and micronized progesterone demonstrating a superior cardiovascular safety profile. Future progress in women's cardiovascular health depends on a concerted research effort to elucidate the genetic underpinnings of hormone-responsive cardiovascular disease, the development of novel, tissue-selective hormone analogs, and the design of inclusive, long-term clinical trials that prioritize sex-specific endpoints. For researchers and drug developers, this presents a pivotal opportunity to create next-generation therapeutics and decision-support tools that fully individualize care, ultimately reducing the significant burden of cardiovascular disease in postmenopausal women.
References
- 1. , Postmenopausal estimators for coronary... hormone replacement risk [https://pubmed.ncbi.nlm.nih.gov/10399059/]
- 2. Cardiovascular Disease Risk in Women with Menopause [https://pmc.ncbi.nlm.nih.gov/articles/PMC12156203/]
- 3. Menopause and women's cardiovascular health: is it really an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10074318/]
- 4. Establishing the risk related to hormone ... - The Pharmaceutical Journal [https://pharmaceutical-journal.com/article/research/establishing-the-risk-related-to-hormone-replacement-therapy-and-cardiovascular-disease-in-women]
- 5. Cardiovascular Risk Associated with Menopause and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511246/]
- 6. Protein Biomarkers of Early Menopause and Incident ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10492938/]
- 7. Optimizing hormone for replacement ... therapy postmenopausal [https://www.explorationpub.com/Journals/eemd/Article/101430]
- 8. The menopausal transition period and cardiovascular risk [https://www.nature.com/articles/s41569-023-00926-7?error=cookies_not_supported&code=907de49b-eba1-4a35-82a3-ff8f74171728]
- 9. Menopause and women's cardiovascular health: is it really ... [https://www.archivesofmedicalscience.com/Menopause-and-women-s-cardiovascular-health-is-it-really-an-obvious-relationship,157308,0,2.html]
- 10. Heart Health Declines Rapidly After Menopause [https://www.acc.org/About-ACC/Press-Releases/2024/04/01/21/39/heart-health-declines-rapidly-after-menopause]
- 11. Can hormone therapy improve heart health in menopausal ... [https://pennstatehealthnews.org/2025/04/can-hormone-therapy-improve-heart-health-in-menopausal-women/]
- 12. Oral or Transdermal Hormone Therapy? The Mental Health ... [https://menopause.org/press-releases/oral-or-transdermal-hormone-therapy-the-mental-health-risks-are-not-the-same]
- 13. Early Natural Menopause Linked with Higher Risk of ... [https://menopause.org/press-releases/early-natural-menopause-linked-with-higher-risk-of-metabolic-syndrome]
- 14. Early Natural Menopause Linked to 27% Higher Risk [https://www.healthline.com/health-news/early-menopause-metabolic-syndrome-risk]
- 15. Association between metabolic syndrome and risk of ... [https://pubmed.ncbi.nlm.nih.gov/41190382/]
- 16. FDA to Remove Black Box Warnings on HRT Labels [https://www.healthline.com/health-news/hormone-replacement-therapy-fda-removes-black-box-warnings]
- 17. Forum Health Applauds FDA Decision to Remove "Black ... [https://www.wcia.com/business/press-releases/cision/20251124CG30566/forum-health-applauds-fda-decision-to-remove-black-box-warnings-from-menopause-hormone-therapy]
- 18. Menopausal Hormone Therapy and Heart Risk - Consult QD [https://consultqd.clevelandclinic.org/menopausal-hormone-therapy-and-heart-risk-updated-guidance-is-at-hand]
- 19. Is Hormone Therapy Good for Heart Health? [https://menopause.org/press-releases/is-hormone-therapy-good-for-heart-health]
- 20. Frontiers | Exploring associations between estrogen and gene candidates identified by coronary artery disease genome-wide association studies [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1502985/full]
- 21. Signalling mechanisms in the cardiovascular protective effects of estrogen: With a focus on rapid/membrane signalling - PubMed [https://pubmed.ncbi.nlm.nih.gov/34746830/]
- 22. Cardio-Metabolic Health and HRT in Menopause [https://pmc.ncbi.nlm.nih.gov/articles/PMC10494270/]
- 23. New markers for cardiovascular disease risk in women: impact of endogenous estrogen status and exogenous postmenopausal hormone therapy - PubMed [https://pubmed.ncbi.nlm.nih.gov/12788842/]
- 24. The effects of transdermal estrogens combined with ... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-025-01664-1]
- 25. Gender-specific regulation of cardiovascular function: estrogen as key player - PubMed [https://pubmed.ncbi.nlm.nih.gov/15280095/]
- 26. HHS Advances Women's Health, Removes Misleading ... [https://www.fda.gov/news-events/press-announcements/hhs-advances-womens-health-removes-misleading-fda-warnings-hormone-replacement-therapy]
- 27. FACT SHEET: FDA Initiates Removal of “Black Box ... [https://www.hhs.gov/press-room/fact-sheet-fda-initiates-removal-of-black-box-warnings-from-menopausal-hormone-replacement-therapy-products.html]
- 28. FDA Requests Labeling Changes Related to HRT [https://www.fda.gov/drugs/drug-safety-and-availability/fda-requests-labeling-changes-related-safety-information-clarify-benefitrisk-considerations]
- 29. FDA Removes Black-Box Warnings on Hormone ... [https://www.sgo.org/news/fda-removes-black-box-warnings-on-hormone-replacement-therapy/]
- 30. What to know about menopause hormone therapy after ... [https://www.pbs.org/newshour/health/what-to-know-about-menopause-hormone-therapy-after-fda-removed-black-box-warnings]
- 31. FDA to Remove Black Box Warnings From HRT, Debate ... [https://www.ajmc.com/view/fda-to-remove-black-box-warnings-from-hrt-debate-ensues]
- 32. FDA Strips Breast Cancer Warning from Menopause ... [https://www.scientificamerican.com/article/fda-strips-breast-cancer-warning-from-menopause-hormone-therapy/]
- 33. Estrogen and Heart Health After Menopause: What New ... [https://activated.health/estrogen-and-heart-health-after-menopause-what-new-research-shows/]
- 34. A Review and Contemporary Approach to Risk Assessment [https://pubmed.ncbi.nlm.nih.gov/41066010/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=0lTTYlkC1gejWa1v9zP--eaczAMrEaCCOGpeJGIpPqf&fc=None&ff=20251022233356&v=2.18.0.post22+67771e2]
- 35. Hormone Therapy in Postmenopausal Persons: Primary ... [https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/menopausal-hormone-therapy-preventive-medication]
- 36. AACE Releases Guidelines for Menopausal Hormone ... [https://www.aafp.org/pubs/afp/issues/2012/1101/p864.html]
- 37. Hormone Replacement Therapy - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK493191/]
- 38. Stratified Sampling [https://docs.statsig.com/experiments/advanced-setup/stratified-sampling]
- 39. 冠状动脉钙化扫描- 妙佑医疗国际 [https://www.mayoclinic.org/zh-hans/tests-procedures/heart-scan/about/pac-20384686]
- 40. 采用动脉钙化标志物早期识别亚临床动脉粥样硬化 [https://www.haoyishu.org/web/article/9529]
- 41. 茵诺医药YN001 Ib/IIa期临床数据在ESC 2025全球首发 [https://www.innovmedicine.com/news/details_25_192.html]
- 42. 性别特异性亚临床器官损伤差异与心血管风险分层 [https://www.ebiotrade.com/newsf/2025-10/20251014222633081.htm]
- 43. 罗阿奇博士:60岁以上女性激素替代疗法的建议探讨- 心脑血管 [https://www.familydoctor.cn/news/aqi-boshi-yishang-nvxingjisu-tidailiaofa-jianyi-tantao-258929.html]
- 44. 超越“易损斑块”:2025年JACC高危冠状动脉斑块立场综述 [http://www.360doc.com/content/25/0625/15/67580395_1156192567.shtml]
- 45. Polygenic risk for circulating reproductive hormone levels ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6597945/]
- 46. Breaking binary in cardiovascular disease risk prediction [https://www.nature.com/articles/s44325-024-00041-7]
- 47. Combined Associations of a Polygenic Risk Score and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7936056/]
- 48. Development and testing of a polygenic risk score for ... [https://www.nature.com/articles/s41698-023-00382-z]
- 49. AHA 2025: New study from Genomics shows polygenic risk ... [https://www.genomics.com/newsroom/aha-2025-new-study-from-genomics-shows-polygenic-risk-scores-improve-the-accuracy-of-cardiovascular-disease-risk-prediction]
- 50. Early Menopause and Heart Disease: A Crosstalk With ... [https://e-cmsj.org/DOIx.php?id=10.51789%2Fcmsj.2024.4.e8]
- 51. Artificial Intelligence in Postmenopausal Health: From Risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12608235/]
- 52. Menopause, Heart Disease, and Benefits of Hormone ... [https://www.massgeneralbrigham.org/en/about/newsroom/articles/menopause-heart-disease-hormone-therapy]
- 53. AI model outperforms breast density assessment in ... [https://www.news-medical.net/news/20251126/AI-model-outperforms-breast-density-assessment-in-breast-cancer-risk-stratification.aspx]
- 54. AI outperforms breast density for breast cancer risk [https://www.femtechworld.co.uk/news/cancer/ai-outperforms-breast-density-for-breast-cancer-risk/]
- 55. Inside ELRIG's Drug Discovery 2025 [https://www.drugtargetreview.com/article/190237/inside-elrigs-drug-discovery-2025/]
- 56. Bioidentical Hormone Replacement Therapy (HRT) [https://globalrph.com/2024/12/bioidentical-hormone-replacement-therapy-hrt/]
- 57. Compounded Bioidentical Menopausal Hormone Therapy [https://www.acog.org/clinical/clinical-guidance/clinical-consensus/articles/2023/11/compounded-bioidentical-menopausal-hormone-therapy]
- 58. The Critical Window Hypothesis of Hormone Therapy and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3780981/]
- 59. Doctors looking into estrogen therapy to prevent dementia ... [https://www.nbcnews.com/health/womens-health/estrogen-dementia-prevention-hormone-replacement-women-perimenopause-rcna245664]
- 60. Estrogen, menopause, and Alzheimer's disease [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1634302/full]
- 61. Menopausal Hormone Therapy—Risks, Benefits and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12652300/]
- 62. The Value of Transdermal Estradiol and Micronized ... [https://pubmed.ncbi.nlm.nih.gov/22432811/]
- 63. Transdermal Beats Oral Estrogen for CVD Safety of ... [https://mdedge.com/obgyn/article/271877/menopause/transdermal-beats-oral-estrogen-cvd-safety-hormone-therapy]
- 64. Menopausal Hormone Replacement Therapy and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9178928/]
- 65. Estrogen and cardiovascular disease [https://www.sciencedirect.com/science/article/abs/pii/S003306202400015X]
- 66. Cardiovascular health and the menopause, metabolic health [https://www.sciencedirect.com/science/article/abs/pii/S1521690X23000556]
- 67. Hormone Replacement Therapy (HRT) and Breast Cancer ... [https://www.breastcancer.org/risk/risk-factors/using-hormone-replacement-therapy]
- 68. HRT and Breast Cancer Risk Explained | BCRF [https://www.bcrf.org/about-breast-cancer/hrt-breast-cancer-risk/]
- 69. Chapter 3. Impact of estrogens on hemostasis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488444/]
- 70. The 2025 Menopausal Hormone Therapy Guidelines [https://pmc.ncbi.nlm.nih.gov/articles/PMC12438153/]
- 71. Lifestyle modification in the management of the metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3047997/]
- 72. Effect of menopausal hormone therapy on components of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5933555/]
- 73. Effect of Postmenopausal Hormone Therapy on Metabolic ... [https://www.mdpi.com/2077-0383/13/14/4043]
- 74. Join Our All-Inclusive HRT Membership Program [https://vitallivinghealthcare.com/hrt/membership-program/]
- 75. The Benefits of Using Telehealth For Your HRT Program [https://openloophealth.com/blog/the-benefits-of-using-telehealth-for-your-hrt-program]
- 76. How to Talk to Your Doctor If They Don't Want to Prescribe ... [https://www.joinmidi.com/post/hrt-cheat-sheet]
- 77. Gender-Affirming Care Without Walls: Utilization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9829154/]
- 78. Signs HRT Is Not Working [https://www.healthline.com/health/is-my-hrt-working]
- 79. Time to Rethink Hormone Replacement Therapy Warnings [https://udshealth.com/blog/rethink-hormone-replacement-therapy-warnings/]
- 80. Is HRT in menopause healthy? US label change triggers ... [https://www.nature.com/articles/d41586-025-03687-0]
- 81. Beyond the Black Box: Reassessing HRT for Modern Women [https://www.epicbrokers.com/insights/beyond-the-black-box-reassessing-hrt-for-modern-women/]
- 82. HHS Advances Women's Health, Removes Misleading ... [https://www.hhs.gov/press-room/hhs-advances-womens-health-removes-misleading-fda-warnings-hormone-replacement-therapy.html]
- 83. Hormone Therapy for Menopause: Timing, Safety, and Best ... [https://www.ajmc.com/view/hormone-therapy-for-menopause-timing-safety-and-best-candidates]
- 84. Review of hormonal replacement therapy options for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463494/]
- 85. Doctors respond to 'data-free' decision over menopause ... [https://www.theguardian.com/us-news/2025/nov/24/menopause-hormone-therapy]
- 86. Menopausal Hormone Therapy and Cardiovascular Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC8063246/]
- 87. Fact or Fiction? The Role of Regulated Body-Identical ... [https://www.sciencedirect.com/science/article/pii/S1751485122000460]
- 88. individualizing risk assessment for hormone therapy ... [https://pubmed.ncbi.nlm.nih.gov/25321420/]
- 89. Ongoing Individualized Hormone Therapy Appears to ... [https://menopause.org/press-releases/ongoing-individualized-hormone-therapy-appears-to-have-no-age-limit]
- 90. Hormone Therapy Market Analysis and Revenue Trends ... [https://www.towardshealthcare.com/insights/hormone-therapy-market-sizing]
- 91. Bioidentical Hormones Market Size, Trends & Forecast ... [https://www.consegicbusinessintelligence.com/press-release/bioidentical-hormones-market-trends-forecast-2025-2032]
- 92. Hormone Therapy Market to Reach USD 41.97 Billion by ... [https://www.globenewswire.com/news-release/2025/11/18/3189926/0/en/Hormone-Therapy-Market-to-Reach-USD-41-97-Billion-by-2035-Growing-at-7-20-CAGR.html]
- 93. Transdermal Drug Delivery Pipeline Report Featuring 190 [https://www.globenewswire.com/news-release/2024/12/20/3000659/28124/en/Transdermal-Drug-Delivery-Pipeline-Report-Featuring-190-Companies-Product-Overview-Stages-of-Development-Segments-Regulatory-Path.html]
- 94. Risk factors for cardiovascular disease and hormone therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1860737/]
- 95. Rejuvenation Roundup July 2025 [https://www.lifespan.io/news/rejuvenation-roundup-july-2025/]
- 96. A Comprehensive Analysis of the Transdermal Drug ... [https://finance.yahoo.com/news/comprehensive-analysis-transdermal-drug-delivery-220300635.html]
- 97. Individualizing HT considering metabolic risk factors and ... [https://pubmed.ncbi.nlm.nih.gov/25720618/]
- 98. Improving clinical outcomes through attention to sex and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8435014/]