Optimizing Hormone Replacement Therapy in Postmenopausal Women with Type 2 Diabetes: A Comprehensive Review of Efficacy, Safety, and Novel Therapeutic Synergies
This article provides a comprehensive analysis for researchers and drug development professionals on optimizing Hormone Replacement Therapy (HRT) for postmenopausal women with type 2 diabetes (T2DM).
Optimizing Hormone Replacement Therapy in Postmenopausal Women with Type 2 Diabetes: A Comprehensive Review of Efficacy, Safety, and Novel Therapeutic Synergies
Abstract
This article provides a comprehensive analysis for researchers and drug development professionals on optimizing Hormone Replacement Therapy (HRT) for postmenopausal women with type 2 diabetes (T2DM). It synthesizes recent evidence on the metabolic benefits of HRT, including improved glycemic control and insulin sensitivity, while critically evaluating cardiovascular and oncological risks. The review emphasizes the critical importance of therapy personalization, highlighting the superior safety profile of transdermal estrogen formulations over oral ones in this population. It further explores the 'timing hypothesis' for early intervention and examines emerging data on synergistic effects between HRT and contemporary diabetes medications like GLP-1 receptor agonists and SGLT2 inhibitors. The article concludes by identifying key gaps in the current evidence base and proposing future directions for clinical research and drug development to enhance treatment outcomes for this growing patient demographic.
The Metabolic Interplay: Menopause, Diabetes, and the Rationale for HRT
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary mechanistic links between declining estrogen and the onset of insulin resistance? The decline in estrogen, particularly 17β-estradiol (E2), disrupts glucose homeostasis through multiple interconnected pathways. Estrogen acts primarily through Estrogen Receptor alpha (ERα) to enhance insulin sensitivity in key metabolic tissues. In skeletal muscle, ERα activation promotes glucose uptake and insulin signaling. In the liver, it suppresses gluconeogenesis. In adipose tissue, it regulates lipid storage and inhibits pro-inflammatory adipokine release. The loss of estrogenic signaling leads to increased systemic inflammation, ectopic lipid accumulation in liver and muscle, and impaired insulin receptor signaling [1] [2] [3]. Furthermore, estrogen deficiency is associated with reduced pancreatic β-cell function and survival, compromising insulin secretion [4] [3].
FAQ 2: How does menopause-associated fat redistribution specifically contribute to cardiometabolic risk? Menopause triggers a shift from a gynoid (pear-shaped, peripheral) to an android (apple-shaped, central) fat distribution. This is clinically significant because [5] [2]:
- Visceral Adiposity: Central fat is metabolically active, releasing pro-inflammatory cytokines (e.g., TNF-α, IL-6) and free fatty acids into the portal circulation. This promotes hepatic insulin resistance and dyslipidemia.
- Dysfunctional Adipose Tissue: The adipocytes in visceral depots are more susceptible to hypertrophy and hypoxia, leading to fibrosis, macrophage infiltration, and a diabetogenic adipokine profile (e.g., reduced adiponectin) [1].
- Ectopic Fat Deposition: When subcutaneous adipose tissue's storage capacity is exceeded, lipids accumulate in the liver, skeletal muscle, and heart, further driving insulin resistance and cardiovascular dysfunction [3].
FAQ 3: What is the "Timing Hypothesis" for Hormone Replacement Therapy (HRT) and its cardiometabolic benefits? The "Timing Hypothesis" posits that the cardiovascular and metabolic benefits of HRT are maximized, and risks minimized, when therapy is initiated early in the menopausal transition (typically within 10 years of menopause onset and before the age of 60) [4] [3]. In younger, recently postmenopausal women, HRT can improve insulin sensitivity, beta-cell function, and lipid profiles, and may delay the onset of type 2 diabetes (T2DM). In contrast, initiating HRT in older women with established atherosclerosis may exacerbate underlying vascular inflammation and increase the risk of thromboembolic events [6] [4] [7].
FAQ 4: How do different HRT formulations (oral vs. transdermal) impact cardiovascular risk profiles? The route of estrogen administration significantly influences its metabolic and thrombotic effects.
- Transdermal Estrogen: This route is generally preferred for women with T2DM or elevated cardiovascular risk. It avoids first-pass liver metabolism, leading to more stable physiological hormone levels. This results in a more favorable impact on liver-synthesized proteins, with a lower risk of inducing hypertension, thromboembolism, and stroke compared to oral formulations [4] [7].
- Oral Estrogen: The first-pass hepatic effect can be advantageous for improving the lipid profile (e.g., lowering LDL-C) but simultaneously increases the production of pro-coagulant factors and C-reactive protein (CRP), potentially elevating thrombotic risk [4] [3].
Table 1: Comparison of HRT Formulation Impacts on Cardiometabolic Risk Factors
| Risk Factor | Transdermal Estrogen | Oral Estrogen |
|---|---|---|
| Insulin Sensitivity | Improves, neutral effect [4] | Improves [3] |
| Thromboembolic Risk | Lower risk [4] [7] | Higher risk [4] |
| Stroke Risk | Neutral or lower risk [7] | Can be increased [4] |
| Lipid Profile | Modest improvement [4] | Greater LDL-C reduction, but can increase triglycerides [3] |
| Hypertension | Neutral effect [4] | Can increase risk [4] |
FAQ 5: What is the role of progestogens in HRT regimens for women with type 2 diabetes? The addition of progestogen is necessary for women with an intact uterus to prevent estrogen-induced endometrial hyperplasia. However, the choice of progestogen is critical as it can modulate the metabolic benefits of estrogen. Some progestogens (e.g., medroxyprogesterone acetate) can attenuate estrogen's positive effects on insulin sensitivity and lipid metabolism. Therefore, regimens for women with T2DM should prioritize progestogens with a more neutral metabolic profile, such as micronized progesterone [3].
Troubleshooting Common Experimental Challenges
Challenge 1: Inconsistent Metabolic Phenotypes in Ovariectomized Rodent Models
- Problem: High variability in weight gain, insulin resistance, and fat distribution after ovariectomy (OVX).
- Solution:
- Standardize Diet and Age: Use animals of a consistent age (e.g., 12-16 weeks) and control dietary intake precisely. A high-fat diet post-OVX can amplify and standardize the metabolic phenotype [8].
- Confirm OVX Efficacy: Measure uterine weight at endpoint as a bioassay for successful estrogen depletion. A significant reduction in uterine weight confirms procedure efficacy.
- Control for Timing: Initiate experiments or HRT interventions immediately after OVX to model the "window of opportunity" and avoid the confounding effects of long-established metabolic dysfunction [3].
Challenge 2: Accurately Assessing Tissue-Specific Insulin Resistance In Vivo
- Problem: Whole-body measures like HOMA-IR lack tissue-specific resolution.
- Solution:
- Hyperinsulinemic-Euglycemic Clamp: This is the gold standard. Combine it with radioactive tracers (e.g., 2-deoxyglucose) to precisely quantify glucose disposal rates in specific tissues like skeletal muscle and adipose tissue [3].
- Functional Tissue Analysis: Ex vivo analysis of insulin-stimulated Akt phosphorylation in muscle, liver, and adipose tissue biopsies provides a direct readout of insulin signaling pathway integrity.
Challenge 3: Modeling the Complex Hormonal Milieu of Perimenopause
- Problem: Most models use sharp, surgical OVX, which does not replicate the gradual, fluctuating hormonal decline of natural menopause.
- Solution:
- The VCD Model: Use 4-vinylcyclohexene diepoxide (VCD) in rodents to induce gradual ovarian follicle depletion, mimicking the hormonal fluctuations and transition period of human perimenopause.
- Longitudinal Sampling: In clinical or large-animal studies, conduct frequent longitudinal hormone level monitoring (estradiol, FSH) to correlate individual hormonal trajectories with metabolic outcomes [2].
Challenge 4: Disentangling the Effects of Aging vs. Estrogen Deficiency
- Problem: It is difficult to determine if observed metabolic deficits are due to aging itself or the loss of ovarian function.
- Solution:
- Use of Young OVX vs. Aged Animals: Compare young OVX rodents with aged, naturally postmenopausal rodents.
- HRT Reversal: If a metabolic parameter (e.g., insulin resistance) is reversed by short-term HRT in an OVX model, it is more likely a direct consequence of estrogen deficiency rather than irreversible aging [3].
- Statistical Control: In human studies, use multivariate regression models to control for age, thereby isolating the independent effect of menopausal status or hormone levels [9].
Synthesis of Key Quantitative Data
Table 2: Impact of Menopausal Status and HRT on Key Cardiometabolic Parameters
| Parameter | Premenopausal State | Postmenopausal State (Untreated) | Postmenopausal State (with HRT) |
|---|---|---|---|
| Estradiol (E2) Level | 100-250 pg/mL [2] | ~10 pg/mL [2] | Variable (therapy-dependent) |
| HOMA-IR | Reference | Increased by ~13% [4] | Can be reduced by up to 36% in women with T2DM [4] |
| T2DM Incidence | Reference | Increased [6] [10] | Up to 30% reduction in at-risk women [4] [3] |
| LDL-C | Reference | Increases during late perimenopause/early postmenopause [2] | Decreased (oral estrogen > transdermal) [4] [3] |
| Visceral Fat Mass | Reference | Significantly increased [5] [3] | Reduced or prevented [1] [3] |
Core Experimental Protocols
Protocol 1: Assessing the Metabolic Phenotype in a Murine OVX Model
- Animals: 12-week-old C57BL/6 female mice.
- OVX Surgery: Anesthetize mice. Make a dorsal midline incision, locate and excise the ovaries. Suture muscle and skin. Sham-operated controls undergo identical procedure without ovary removal.
- HRT Intervention: Randomize OVX mice into groups receiving either vehicle, transdermal 17β-estradiol (e.g., 0.1 µg/day patch), or oral conjugated estrogens via gavage. Begin treatment immediately post-surgery.
- Metabolic Monitoring: Monitor body weight and food intake weekly. At 8 weeks post-OVX, perform:
- Glucose Tolerance Test (GTT): Fast mice for 6 hours, inject glucose (2g/kg i.p.), measure blood glucose at 0, 15, 30, 60, and 120 minutes.
- Insulin Tolerance Test (ITT): Fast mice for 4 hours, inject insulin (0.75 U/kg i.p.), measure blood glucose as in GTT.
- Terminal Analysis: Euthanize mice. Collect blood for hormone/lipid panels. Weigh and snap-freeze metabolic tissues (liver, quadriceps, gonadal/ subcutaneous fat) for molecular analysis. Weigh uteri.
Protocol 2: Evaluating Tissue-Specific Insulin Signaling via Western Blot
- Tissue Lysate Preparation: Homogenize ~50 mg of frozen liver, muscle, or adipose tissue in RIPA buffer containing protease and phosphatase inhibitors. Centrifuge and quantify protein concentration.
- Western Blotting: Resolve 30 µg of protein by SDS-PAGE and transfer to a PVDF membrane.
- Immunoblotting: Block membrane and probe with primary antibodies overnight at 4°C.
- Targets: Phospho-Akt (Ser473), Total Akt, Phospho-IRβ (Tyr1150/1151), Total IRβ.
- Detection and Analysis: Incubate with HRP-conjugated secondary antibodies, develop with ECL reagent, and visualize. Quantify band density. Express p-Akt/Akt and p-IR/IR ratios to assess insulin pathway activation.
Protocol 3: Measuring Endogenous Sex Hormones in Postmenopausal Human Serum via LC-MS/MS
- Sample Collection: Draw fasting venous blood. Centrifuge to isolate serum. Store at -80°C.
- Sample Preparation: Thaw samples. Perform liquid-liquid extraction to isolate hormones.
- LC-MS/MS Analysis:
- Chromatography: Use a C18 reverse-phase column with a gradient of methanol/water with ammonium acetate.
- Mass Spectrometry: Operate in positive electrospray ionization (ESI+) mode. Use Multiple Reaction Monitoring (MRM) for high specificity. Key analytes: Estradiol, Estrone, Testosterone, Dihydrotestosterone (DHT), Androstenedione [9].
- Quantification: Quantify hormone levels using stable isotope-labeled internal standards and a calibration curve. This method is superior to RIA for low hormone levels in postmenopausal women [9].
Signaling Pathways and Experimental Workflows
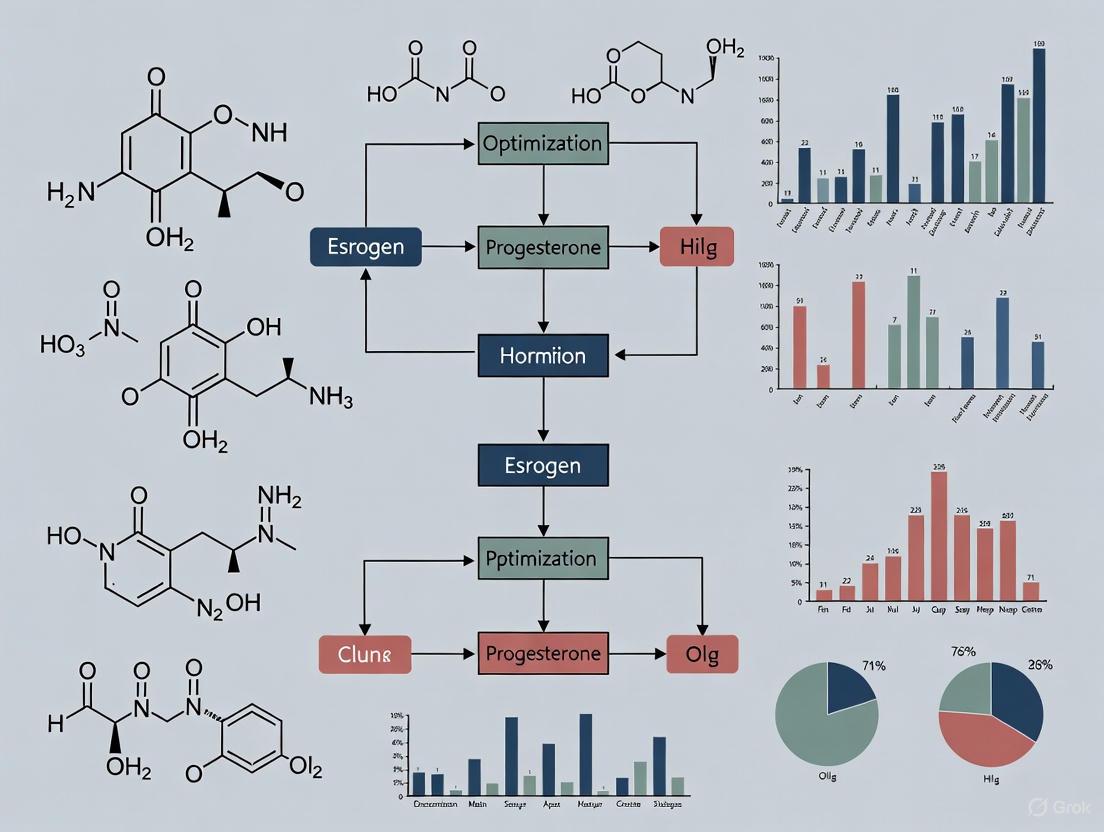
Diagram 1: Estrogen Signaling & Menopausal Disruption in Metabolism (Width: 760px)
Diagram 2: Experimental Workflow for HRT & Metabolism Research (Width: 760px)
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating Estrogen-Metabolism Crosstalk
| Reagent / Material | Function / Application | Specific Example / Note |
|---|---|---|
| Ovariectomized (OVX) Rodent Models | Preclinical model for surgical menopause; allows for controlled HRT studies. | C57BL/6 mice are common; uterine weight is a critical endpoint for confirming estrogen deficiency [3]. |
| 4-Vinylcyclohexene Diepoxide (VCD) | Chemical to induce gradual ovarian follicle atrophy, modeling human perimenopause. | Provides a more translational model of natural menopause compared to acute OVX. |
| 17β-Estradiol (E2) | The primary endogenous estrogen for in vitro and in vivo replacement studies. | Available in various formulations: pellets for sustained release, injections, or dissolved in drinking water/diet [1]. |
| Selective Estrogen Receptor Modulators (SERMs) & Knockout Models | To dissect the specific roles of ERα vs. ERβ in metabolic tissues. | ERα global knockout (αERKO) and tissue-specific (e.g., AdipoERα) mice are vital tools [1] [3]. |
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Gold-standard for precise quantification of low levels of sex steroids in postmenopausal serum/plasma. | Superior to RIA for sensitivity and specificity in measuring estradiol, estrone, androgens [9]. |
| Phospho-Specific Antibodies | For detecting activation states of insulin signaling pathways in tissue lysates. | Antibodies against p-Akt (Ser473), p-IRβ (Tyr1150/1151) are essential for Western blot analysis. |
| Hyperinsulinemic-Euglycemic Clamp Setup | The definitive in vivo method for quantifying whole-body insulin sensitivity. | Requires programmable infusion pumps, glucose analyzers, and radioactive/stable isotope tracers for tissue-specific disposal rates [3]. |
The age at which a woman experiences natural menopause is a significant determinant of long-term cardiometabolic health. A growing body of evidence establishes early menopause as a potent clinical marker for an increased risk of Type 2 Diabetes Mellitus (T2DM) and Metabolic Syndrome (MetS). MetS represents a cluster of conditions—including central obesity, dyslipidemia, hypertension, and insulin resistance—that collectively elevate the risk for cardiovascular disease and T2DM [11] [12]. Understanding this relationship is crucial for developing targeted prevention strategies, particularly in the context of optimizing Hormone Replacement Therapy (HRT) regimens for women with or at risk for T2DM. This technical resource synthesizes the key epidemiological data, explores underlying mechanisms, and provides practical research guidance for investigators in this field.
Key Epidemiological Findings:
- Metabolic Syndrome Risk: A large-scale study of over 234,000 women found that those experiencing early natural menopause had a 27% increased relative risk of developing MetS compared to those with later menopause [13].
- Type 2 Diabetes Risk: A 2024 meta-analysis of 19 studies concluded that early menopause is associated with a 24% higher odds of developing T2DM (Pooled OR = 1.24, 95% CI: 1.09–1.40). The same analysis found a significantly higher hazard of T2DM among women with early menopause (Pooled HR = 1.31, 95% CI: 1.05–1.64) [14].
- Disease Severity Link: The relationship with T2DM is not merely temporal; research indicates that women with longer-standing T2DM (>10 years duration) and those with microvascular complications (retinopathy, nephropathy) experience menopause approximately two years earlier than their non-diabetic counterparts [15].
Table 1: Quantified Risk of T2DM and Metabolic Syndrome Associated with Early Menopause
| Condition | Risk Measure | Magnitude of Increase | Source Type |
|---|---|---|---|
| Metabolic Syndrome | Relative Risk | 27% | Large-Scale Cohort [13] |
| Type 2 Diabetes (Odds) | Pooled Odds Ratio (OR) | 24% | Meta-Analysis (19 studies) [14] |
| Type 2 Diabetes (Hazard) | Pooled Hazard Ratio (HR) | 31% | Meta-Analysis [14] |
| Early Menopause Prevalence | Prevalence Ratio | 2.3-fold higher in T2DM vs non-T2DM | Cross-Sectional Study [15] |
Key Pathophysiological Pathways
The link between early menopause and metabolic dysfunction is driven by the decline in estrogen and its multifaceted role in metabolism.
Estrogen Deficiency and Central Metabolism
The decline in estrogen during menopause has a direct impact on body composition and energy balance. Estrogen deficiency is associated with:
- Increased Visceral Adiposity: A redistribution of fat to the abdominal area, independent of age and total body fat [12].
- Reduced Energy Expenditure: A decrease in basal metabolic rate and fat oxidation [3].
- Insulin Resistance: Estrogen enhances insulin sensitivity by modulating insulin receptor expression and insulin signaling. Its deficiency contributes to systemic insulin resistance [3] [4].
The following diagram illustrates the core pathway through which estrogen deficiency leads to T2DM and MetS.
The Bidirectional Relationship
The relationship between menopause and T2DM is complex and often bidirectional. While early menopause increases the risk of T2DM, pre-existing T2DM can also accelerate reproductive aging. One proposed mechanism is that the microvascular complications of diabetes (retinopathy, nephropathy) may damage the highly vascularized ovarian tissue, potentially leading to earlier follicular depletion and menopause [15]. This creates a feedback loop that exacerbates both conditions.
Experimental Protocols & Research Methodologies
For researchers investigating this association, several well-established methodologies are central to the field.
Core Epidemiological Study Designs
- Cross-Sectional Analysis: Used to determine the prevalence of T2DM/MetS in pre- vs. post-menopausal women or to compare the mean age at menopause in women with and without T2DM at a single point in time [15] [16].
- Key Protocol: Recruit defined cohorts (e.g., premenopausal, perimenopausal, postmenopausal). Confirm menopausal status via 12 months of amenorrhea (excluding other causes). T2DM status is confirmed via HbA1c ≥6.5%, physician diagnosis, or glucose tolerance tests. Data analysis employs multivariable regression to adjust for confounders like age, BMI, and smoking [15] [16].
- Prospective Cohort Studies: Ideal for establishing temporal sequence and calculating hazard ratios (HR). These studies follow premenopausal women over time to observe the onset of menopause and subsequent development of T2DM [14].
- Meta-Analysis: The gold standard for synthesizing evidence. A rigorous protocol (e.g., PRISMA) is followed, including a systematic search of multiple databases, quality assessment of studies (e.g., Newcastle-Ottawa Scale), and pooled analysis of effect sizes (Odds Ratios, Hazard Ratios) using appropriate statistical models [14].
Assessing Metabolic Parameters in Clinical Research
To move beyond epidemiological association and explore mechanisms, precise measures of glucose homeostasis and body composition are essential.
- Glucose Homeostasis:
- Hyperinsulinemic-Euglycemic Clamp: The gold-standard method for directly measuring insulin sensitivity in peripheral tissues [3] [12].
- Intravenous Glucose Tolerance Test (IVGTT) with Modeling: Used to assess insulin sensitivity and beta-cell function [12].
- Homeostatic Model Assessment of Insulin Resistance (HOMA-IR): A simpler, widely used index calculated from fasting glucose and insulin levels. A meta-analysis showed HRT can reduce HOMA-IR by 13% [4] [17].
- Body Composition Analysis:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Assays for Investigating Menopause and Metabolic Disease
| Item / Assay | Specific Function / Example | Research Application |
|---|---|---|
| ELISA Kits | Quantifying serum 17β-Estradiol, Testosterone, SHBG | Measure endogenous sex hormone levels for correlation with metabolic markers. |
| Metabolic Panel Assays | Enzymatic colorimetric tests for LDL-C, TG, HbA1c (HPLC method) | Determine lipid profiles and glycemic control as defined by ADA criteria [16]. |
| Body Composition Tools | DEXA Scan; CT Scan for VAT measurement | Objectively track changes in visceral fat and lean mass in study cohorts [12]. |
| HRT Formulations | Transdermal 17β-Estradiol; Oral Conjugated Estrogens; Medroxyprogesterone Acetate | Investigate the metabolic effects of different MHT types, routes, and progestogen additions [3] [4]. |
Hormone Therapy: Mechanisms & Research Considerations
Menopausal Hormone Therapy (MHT) is a critical intervention to study in the context of mitigating diabetes risk post-menopause.
Mechanisms of Action on Glucose Metabolism
MHT, particularly estrogen, improves glycemic control through several mechanisms, as shown in the diagram below.
Evidence from a meta-analysis of 17 randomized controlled trials confirms that MHT (both estrogen-alone and estrogen-plus-progestogen) significantly reduces insulin resistance in healthy postmenopausal women [17]. Furthermore, a recent retrospective cohort study demonstrated that MHT use in perimenopausal individuals with prediabetes led to a sustained decrease in diabetes risk over 20 years (HR = 0.69, 95% CI: 0.58–0.83) [18].
Formulation and Timing in Research Design
When designing studies on MHT, the formulation and timing are critical variables.
- Route of Administration: Transdermal estrogen is often preferred in studies involving women with cardiovascular risk factors due to its lower risk of venous thromboembolism compared to oral estrogen [4].
- Timing Hypothesis: The beneficial metabolic effects of MHT are most pronounced when initiated early, within 10 years of menopause or before the age of 60 [4]. Research protocols must carefully account for this window of intervention.
Frequently Asked Questions (FAQs) for Researchers
Q1: How is "early menopause" consistently defined in epidemiological studies? Early menopause is typically defined as the permanent cessation of menstruation between the ages of 40 and 45 years. Menopause before age 40 is classified as premature ovarian insufficiency [15] [14]. Consistent use of these definitions is vital for cohort homogeneity and cross-study comparisons.
Q2: What are the key confounding factors that must be adjusted for in statistical analyses? Robust studies adjust for a range of potential confounders, including:
- Demographics: Age, race, and socioeconomic status.
- Lifestyle Factors: Smoking status, physical activity level, and alcohol use.
- Anthropometrics: Body Mass Index (BMI) and waist circumference.
- Medical History: Parity, use of oral contraceptives, and family history of T2DM [15] [16] [14].
Q3: Does MHT's protective effect against diabetes hold in high-risk populations, such as those with obesity? Stratified analyses suggest that the benefit may vary. One study found that MHT significantly reduced diabetes risk in individuals with a BMI < 30 kg/m², but the effect was not significant in those with a BMI ≥ 30 kg/m² [18]. This highlights the need for subgroup analysis in clinical trials.
Q4: What is the relationship between surgical menopause and metabolic risk? Surgical menopause (bilateral oophorectomy) is strongly linked to a higher incidence of MetS and a 57% increased risk of diabetes compared to natural menopause, likely due to the abrupt and severe withdrawal of estrogen [11] [3]. This cohort should be analyzed separately in research studies.
Frequently Asked Questions (FAQs): Estrogen & Metabolic Research
FAQ 1: What is the primary clinical evidence linking estrogen to improved glycemic control? Large, randomized controlled trials and a recent meta-analysis of 17 trials conclusively show that Menopausal Hormone Therapy (MHT) reduces insulin resistance and delays the onset of type 2 diabetes in women [3] [17]. The protective effect is more pronounced with estrogen-alone therapy compared to estrogen-plus-progestogen regimens [17].
FAQ 2: Which estrogen receptor is primarily responsible for its metabolic benefits? Estrogen receptor alpha (ERα) is the primary mediator of estrogen's beneficial effects on glucose homeostasis [19] [20]. Studies show that the loss of ERα, but not estrogen receptor beta (ERβ), results in insulin resistance and obesity, while ERα-specific agonists can reverse diet-induced insulin resistance [20].
FAQ 3: How does the route of estrogen administration (oral vs. transdermal) impact its metabolic effects? The meta-analysis indicates that both oral and transdermal hormone therapy significantly reduce insulin resistance in healthy postmenopausal women [17]. The molecular mechanisms affected can vary with the route of administration, which may explain historical discrepancies in study outcomes [3].
FAQ 4: What is the role of the newly identified gene IER3 in estrogen-related diabetes mechanisms? A 2025 bioinformatics study identified IER3 as a significantly downregulated estrogen-related gene in diabetes patients, with a diagnostic AUC of 0.723 [21]. Its expression correlates strongly with immune cell infiltration, suggesting a novel role in the immunoregulatory mechanisms of diabetes, presenting a potential new biomarker and therapeutic target [21].
Experimental Troubleshooting Guides
Issue 1: Inconsistent Results in Assessing Estrogen's Effect on Insulin Sensitivity
| Potential Cause | Recommended Solution |
|---|---|
| Use of different assessment methods (e.g., HOMA-IR vs. hyperinsulinemic-euglycemic clamp) [3]. | Standardize the lab's internal method. For publication, include a secondary method to allow for cross-study comparisons. |
| Variations in MHT formulations (estrogen type, progestogen addition, administration route) [3]. | Precisely report the formulation, dosage, and route of administration. In animal studies, use controlled-release pellets for consistent hormone levels [19]. |
| Sex disparities in animal models, particularly in knockout models [19]. | Include both male and female animals in the study design and analyze data by sex. For in vivo work, use liver-specific Foxo1 knockout (L-F1KO) models to isolate hepatic mechanisms [19]. |
Issue 2: Investigating the Cell-to-Organism Pathway of Estrogen Action
| Potential Cause | Recommended Solution |
|---|---|
| Difficulty isolating tissue-specific effects (e.g., central nervous system vs. peripheral tissues) [20]. | Use tissue-specific or cell-specific knockout mouse models (e.g., endothelial cell-specific ERα knockout) [22]. Compare subcutaneous vs. intracerebroventricular E2 delivery [20]. |
| Complexity of the signaling cascade, involving genomic and non-genomic pathways [20]. | Employ specific inhibitors of key pathway nodes (e.g., PI3K, Akt) in primary hepatocyte cultures [19]. Use mutant ERα models that can only signal through non-classical pathways [20]. |
Table 1: Clinical and Pre-clinical Quantitative Findings on Estrogen and Glucose Metabolism
| Finding / Metric | Quantitative Result | Context / Model | Source |
|---|---|---|---|
| Reduction in Diabetes Incidence | 35%-62% reduction | Postmenopausal women on MHT / HRT [20]. | Large-scale clinical trials [20] |
| Effect on Fasting Glucose (Mice) | ~16-22% reduction | OVX and male mice with E2 implant vs. placebo [19]. | Pre-clinical study [19] |
| Diagnostic Potential of IER3 | AUC: 0.723 | Downregulation of estrogen-related gene IER3 in human DM patients [21]. | Bioinformatics study (2025) [21] |
| Risk Increase from Early Menopause | 32% greater risk | Menopause before age 40 vs. age 50-54 [3]. | EPIC-InterAct study [3] |
Detailed Experimental Protocols
Protocol 1: Assessing the Role of Hepatic Foxo1 in Estrogen-Mediated Suppression of Gluconeogenesis
This protocol is adapted from the research that established the critical dependency of E2's glycemic effects on hepatic Foxo1 [19].
1. Animal Model Preparation:
- Ovariectomy (OVX): Perform bilateral ovariectomy on female control (Foxo1L/L) and liver-specific Foxo1 knockout (L-F1KO) mice to induce an estrogen-deficient state.
- Hormone Replacement: At the time of OVX, subcutaneously implant a 60-day sustained-release pellet containing either placebo or 0.05 mg 17β-estradiol (E2).
- Grouping: Include male control and L-F1KO mice with and without E2 implants to investigate sex-specific effects.
2. Metabolic Phenotyping (after 8 weeks of treatment):
- Fasting Blood Glucose: Measure after a 16-hour fast.
- Glucose Tolerance Test (GTT): Administer glucose (e.g., 2 g/kg body weight) intraperitoneally to 16-hour fasted mice. Measure blood glucose at 0, 15, 30, 60, and 120 minutes.
- Pyruvate Tolerance Test (PTT): Administer sodium pyruvate (e.g., 2 g/kg) to 16-hour fasted mice to assess gluconeogenic flux. Measure blood glucose as in GTT.
- Insulin Tolerance Test (ITT): Administer human regular insulin (e.g., 0.75 U/kg) to 5-hour fasted mice. Measure blood glucose at 0, 15, 30, 60, and 120 minutes.
- Serum Collection: Collect blood via cardiac puncture after fasting for hormone analysis (insulin, glucagon, E2).
3. In Vitro Validation in Primary Hepatocytes:
- Hepatocyte Isolation: Isolate primary hepatocytes from control and L-F1KO mice using collagenase perfusion.
- Glucose Production Assay: Culture hepatocytes and treat with 100 nmol/L E2. Measure glucose output in HGP buffer containing gluconeogenic substrates (lactate and pyruvate).
- Signaling Pathway Inhibition: Pre-treat cells with specific inhibitors (e.g., for PI3K or Akt) 30 minutes prior to E2 exposure to delineate the pathway.
4. Molecular Analysis:
- Gene Expression: Analyze mRNA levels of gluconeogenic genes (G6pc, Pck1) in liver tissue or hepatocytes using qRT-PCR.
- Protein Analysis: Perform Western blotting on liver lysates to assess phosphorylation of Akt (Ser473) and Foxo1 (Ser253), and total protein levels.
Diagram Title: Estrogen Suppresses Hepatic Gluconeogenesis via ERα-PI3K-Akt-Foxo1 Signaling
Protocol 2: Evaluating Endothelial Cell-Mediated Insulin Delivery to Muscle
This protocol is based on the 2023 discovery of estrogen's role in facilitating insulin transport across the endothelium [22].
1. Genetic Model Generation:
- Generate endothelial cell-specific estrogen receptor knockout mice (EC-ERα-KO) using Cre-lox technology.
2. In Vivo Metabolic Characterization:
- Subject EC-ERα-KO and control mice on both standard and high-fat diets to metabolic tests (GTT, ITT) as described in Protocol 1.
- Compare responses between male and female (both intact and OVX) mice to dissect sex-specific and estrogen-dependent effects.
3. In Vitro Insulin Transport Assay:
- Cell Culture: Grow primary endothelial cells or an immortalized endothelial cell line on Transwell permeable supports.
- Estrogen Treatment: Stimulate cells with physiological concentrations of E2 (e.g., 1-10 nM).
- Insulin Transport Measurement: Add insulin to the apical chamber and measure the rate of its appearance in the basolateral chamber using ELISA.
- Genetic Silencing: Use siRNA to knock down candidate genes (e.g., SNX5) to confirm their functional role in the insulin transport process.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Investigating Estrogen's Metabolic Actions
| Reagent / Model | Function / Application in Research | Key Consideration |
|---|---|---|
| Liver-specific Foxo1 KO (L-F1KO) Mouse [19] | Determines the liver-autonomous requirement of Foxo1 in E2-mediated suppression of gluconeogenesis. | Sex-specific responses to E2 are observed; E2 fails to lower glucose in male L-F1KO mice [19]. |
| Endothelial-specific ERα KO Mouse [22] | Isolates the role of vascular estrogen signaling in whole-body glucose disposal and insulin delivery. | Knockout in both sexes demonstrates that endothelial ERα is critical for E2's anti-diabetic action [22]. |
| ERα-specific Agonist (e.g., PPT) [20] | Used to dissect the metabolic functions of ERα separate from ERβ. | In vivo administration increases insulin-stimulated glucose uptake in skeletal muscle [20]. |
| SNX5 siRNA [22] | Validates the role of the sorting nexin 5 protein in estrogen-stimulated insulin transcytosis. | Silencing SNX5 in endothelial cells ablates the insulin transport effect of E2, confirming its key role [22]. |
| Hyperinsulinemic-Euglycemic Clamp | The gold-standard method for assessing whole-body insulin sensitivity in vivo. | Can be combined with tissue-specific tracers to quantify glucose uptake into specific organs like muscle [3]. |
Troubleshooting Common Research Challenges
Challenge 1: Inconsistent Glycemic Outcomes in Preclinical Models
- Problem: Variable results in glucose tolerance tests following HRT intervention.
- Investigation & Solution:
- Verify Ovariectomy: Confirm complete ovariectomy in animal models; incomplete estrogen depletion causes variable results.
- Control for Fat Distribution: Monitor and report central abdominal fat mass using DXA; HRT-induced changes in fat distribution significantly influence glycemic outcomes [23] [3].
- Standardize Progestogen: Different progestogens blunt estrogen's metabolic benefits to varying degrees. Use consistent, well-defined progestogens like micronized progesterone or dydrogesterone for comparability [24].
Challenge 2: Confounding Effects of Aging versus Estrogen Deficiency
- Problem: Difficulty isolating the effects of estrogen deficiency from chronological aging in metabolic studies.
- Investigation & Solution:
- Utilize Surgical Models: Ovariectomized young animal models allow study of estrogen deficiency independent of advanced aging.
- Apply "Timing Hypothesis": In clinical research, stratify cohorts based on time since menopause (<10 years vs. >10 years). Metabolic benefits are more pronounced with early intervention [3] [24] [25].
Challenge 3: Discrepancies in Insulin Sensitivity Measurements
- Problem: Different methods (e.g., HOMA-IR vs. hyperinsulinemic-euglycemic clamp) yield conflicting results on HRT-induced insulin sensitivity improvement.
- Investigation & Solution:
- Select Appropriate Assays: Understand that HOMA-IR primarily reflects hepatic insulin resistance, while the clamp technique measures peripheral (muscle) insulin sensitivity. Estrogen affects both pathways [3].
- Report Methodology Consistently: Clearly specify the insulin sensitivity assessment method used to enable valid cross-study comparisons [3].
Frequently Asked Questions (FAQs) for Experimental Design
Q1: What are the key mechanistic pathways by which HRT impacts lipid metabolism and body composition?
- A: Estrogen, primarily via Estrogen Receptor α (ERα), mediates its effects through multiple pathways:
- Central Nervous System: In the ventromedial hypothalamus, E2-ERα signaling regulates sympathetic nervous system output to adipose tissue, reducing visceral fat accumulation and promoting energy expenditure [3].
- Direct Tissue Effects: In muscle and liver, estrogen enhances insulin receptor expression and signaling, improving insulin sensitivity [24].
- Lipid Metabolism: Estrogen increases fat oxidation and reduces fat storage, counteracting the menopausal shift towards visceral adiposity [3] [24].
Q2: How does the route of estrogen administration influence metabolic and inflammatory outcomes?
- A: The administration route critically impacts the risk profile and some metabolic effects.
- Oral Estrogen: Undergoes first-pass metabolism in the liver, leading to a more pronounced improvement in lipid profiles (e.g., significant reduction in total cholesterol) but also increased production of clotting factors and inflammatory markers like C-reactive protein (CRP) [24].
- Transdermal Estrogen: Avoids first-pass liver metabolism, providing a more favorable safety profile with non-significant risks of venous thromboembolism (VTE) and neutral effects on inflammatory markers. It is preferred for subjects with higher cardiovascular risk [24] [26].
Q3: Which progestogen has the most favorable profile for combination therapy in metabolic research?
- A: The choice of progestogen is critical as it can modulate estrogen's benefits.
- Micronized Progesterone and Dydrogesterone are associated with a non-significant increase in breast cancer risk and have minimal negative impact on insulin resistance and lipid metabolism [24] [26].
- Medroxyprogesterone Acetate (MPA) is reported to blunt some of estrogen's beneficial metabolic effects and may be associated with a higher risk profile [23] [26].
Q4: What is the optimal timing for HRT initiation to study metabolic benefits?
- A: The "window of opportunity" hypothesis is crucial. The most consistent metabolic benefits—including improved glycemic control, lipid metabolism, and reduced diabetes incidence—are observed when HRT is initiated in perimenopausal or early postmenopausal women (within 10 years of menopause onset or before age 60) [24] [25] [18]. Initiating therapy late (after age 60 or >10 years post-menopause) in animals or humans with established atherosclerosis may yield neutral or negative outcomes.
Quantitative Data Synthesis
Table 1: Metabolic Effects of 6-Month HRT in Postmenopausal Women with Type 2 Diabetes [23]
| Metabolic Parameter | Change with HRT (Mean ± SD) | Change with Observation (Mean ± SD) | P-value |
|---|---|---|---|
| Central Abdominal Fat | -175 ± 51 g | -24 ± 56 g | 0.05 |
| Waist-to-Hip Ratio | -0.03 ± 0.01 | 0.01 ± 0.009 | 0.007 |
| HbA1c | -0.34 ± 0.24% | 0.6 ± 0.4% | 0.04 |
| Total Cholesterol | -0.6 ± 0.1 mmol/L | 0.2 ± 0.2 mmol/L | 0.001 |
| Resting Energy Expenditure | 33 ± 23 kJ/day | -38 ± 23 kJ/day | 0.04 |
Table 2: Long-Term Diabetes Risk Reduction with MHT in Individuals with Prediabetes [18]
| Cohort Characteristic | Hazard Ratio (HR) for Diabetes Development | 95% Confidence Interval |
|---|---|---|
| Overall (Aged 46-60) | 0.693 | 0.577, 0.832 |
| By BMI (kg/m²): | ||
| BMI ≤ 24.9 | Significant Risk Reduction | Reported |
| BMI 25 - 29.9 | Significant Risk Reduction | Reported |
| BMI ≥ 30 | No Significant Risk Reduction | Reported |
Detailed Experimental Protocols
Protocol 1: Assessing Body Composition and Fat Distribution via DXA
- Objective: To quantitatively evaluate the impact of HRT on total body fat, lean mass, and central abdominal fat distribution.
- Methodology:
- Subject Preparation: Participants should be fasted and in a voided state to minimize gut and bladder content interference.
- Positioning: Position the subject supine on the DXA scanner table with arms at sides, slightly separated from the body. Use foam supports under the knees and feet for comfort and stability.
- Scanning & Analysis: Perform a total body scan. Use the regional analysis feature to define a region of interest (ROI) for central abdominal fat. A standard ROI is the area between the top of the iliac crest and the bottom of the rib cage. The software automatically calculates fat mass, lean mass, and bone mineral density for the whole body and the defined ROI [23].
- Key Parameters: Central abdominal fat mass (g), total fat mass (kg), lean body mass (kg), waist-to-hip ratio (WHR).
Protocol 2: Evaluating Insulin Sensitivity via Hyperinsulinemic-Euglycemic Clamp
- Objective: To measure peripheral insulin sensitivity accurately.
- Methodology:
- Baseline Period: After an overnight fast, administer a primed, continuous infusion of insulin (e.g., 40 mU/m²/min) to achieve steady-state hyperinsulinemia.
- Glucose Infusion: Simultaneously, initiate a variable-rate infusion of 20% glucose to maintain blood glucose at a predetermined euglycemic level (e.g., 5.0 mmol/L or 90 mg/dL). Blood glucose is measured every 5-10 minutes.
- Steady-State Measurement: The clamp period typically lasts for 120 minutes. The mean glucose infusion rate (GIR) during the final 30 minutes, when steady-state is achieved, represents the whole-body insulin-mediated glucose disposal rate (M-value), expressed in mg/kg/min [3].
- Key Parameters: M-value, steady-state insulin level.
Signaling Pathways and Experimental Workflows
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Assays for Investigating HRT's Metabolic Impact
| Item/Category | Specific Examples | Function in Research |
|---|---|---|
| Estrogen Formulations | Conjugated Equine Estrogen (CEE), Micronized 17β-Estradiol | Replenishes estrogen levels; used to compare metabolic effects of different estrogen types [23] [27]. |
| Progestogens | Medroxyprogesterone Acetate (MPA), Micronized Progesterone, Dydrogesterone | Protects endometrium in models with intact uterus; critical for studying how different progestogens modulate estrogen's metabolic benefits [23] [24]. |
| Body Composition Analysis | Dual-Energy X-ray Absorptiometry (DXA) | Precisely quantifies total fat mass, lean mass, and regional fat distribution (e.g., central abdominal fat) [23] [3]. |
| Glycemic Control Assays | HbA1c, Fasting Glucose, Oral/Intravenous Glucose Tolerance Test (OGTT/IVGTT) | Standard measures for assessing long-term and acute glycemic control [23] [3]. |
| Insulin Sensitivity Assays | Hyperinsulinemic-Euglycemic Clamp, HOMA-IR | Gold-standard and surrogate measures for assessing peripheral and hepatic insulin sensitivity [3]. |
| Lipid Profile Assays | Total Cholesterol, LDL-C, HDL-C, Triglycerides, ApoB | Evaluates the impact of HRT on lipid metabolism and cardiovascular risk factors [23] [24]. |
| Inflammatory Biomarkers | High-sensitivity CRP (hs-CRP), TNF-α, IL-6 | Measures systemic inflammation, which is linked to insulin resistance and cardiovascular disease [4]. |
Designing Personalized HRT Regimens: From Patient Stratification to Regimen Selection
This technical support center provides specialized guidance for researchers and drug development professionals working within the complex field of Hormone Replacement Therapy (HRT) optimization for postmenopausal women with Type 2 Diabetes Mellitus (T2DM). The interplay between cardiovascular (CV), thrombotic, and oncological risks presents significant challenges in designing robust clinical experiments and interpreting their outcomes. The protocols, troubleshooting guides, and FAQs contained herein are designed to address specific methodological issues and enhance the quality and reproducibility of your research. The content is framed within the context of a broader thesis on optimizing HRT regimens, focusing on the critical need for integrated patient risk profiling before and during therapeutic intervention. This resource synthesizes current evidence and established methodologies to support your experimental workflows, from initial patient stratification to the assessment of metabolic and cognitive outcomes.
Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
FAQ 1: What are the key cardiovascular risk factors to document during patient screening for an HRT study in postmenopausal women with T2DM?
- Answer: A comprehensive baseline cardiovascular (CV) assessment is critical. You should document factors outlined in contemporary cardio-oncology guidelines, as they provide a structured framework for risk stratification that is adaptable to HRT research [28]. These include:
- Previous Cardiovascular Disease (CVD): Heart failure, cardiomyopathy, myocardial infarction, stable angina, severe valvular heart disease, and arterial vascular disease [28].
- Cardiac Imaging Parameters: Left ventricular ejection fraction (LVEF), with particular attention to an LVEF <50% or even a "borderline" LVEF of 50–54% [28].
- Cardiac Biomarkers: Elevated baseline levels of cardiac troponin (cTn) and B-type natriuretic peptides (NPs) [28].
- Age and CV Risk Factors: Age ≥65 years, hypertension, chronic kidney disease, diabetes mellitus, and hyperlipidaemia [28].
- Lifestyle Risk Factors: Current smoking and obesity (BMI >30 kg/m²) [28].
FAQ 2: According to recent evidence, what is the recommended timing for HRT initiation in postmenopausal women with T2DM to maximize benefit and minimize risk?
- Answer: Current evidence supports the "timing hypothesis." HRT should be initiated early, ideally within 10 years of menopause onset, to achieve cognitive and metabolic benefits [4]. Starting therapy beyond this window or in older postmenopausal women may increase the risk of thromboembolic events and negative cardiovascular effects [4] [3].
FAQ 3: Which route of estrogen administration is preferred for study participants with T2DM who are at moderate to high cardiovascular risk?
- Answer: Transdermal estrogen is generally preferred over oral estrogen for women with T2DM and elevated CV risk. Evidence indicates that transdermal estrogen has a lower associated risk of venous thromboembolism (VTE) and a more neutral or potentially beneficial effect on cardiovascular health [4].
FAQ 4: We are observing inconsistent effects of HRT on insulin sensitivity in our preclinical models. What could explain these discrepancies?
- Answer: Discrepancies in insulin sensitivity outcomes can arise from several methodological factors [3]:
- Formulation Differences: The type of estrogen and the addition of specific progestogens (e.g., drospirenone) can significantly influence metabolic outcomes [3] [29].
- Route of Administration: Oral and transdermal estrogen may have different metabolic effects.
- Assessment Method: The choice of insulin sensitivity measurement (e.g., HOMA-IR vs. hyperinsulinemic-euglycemic clamp) can yield different results. The clamp technique is considered the gold standard but is more complex [3].
FAQ 5: How should we assess and stratify the risk of Venous Thromboembolism (VTE) in our study cohort?
- Answer: While no single dominant score exists for HRT-specific VTE risk, you should adopt a systematic approach. Integrate known risk factors from the literature, which include a personal or family history of VTE, obesity, and the use of oral (as opposed to transdermal) estrogen formulations [4]. For reference, consult established risk assessment models from related fields, such as the Khorana score or other cancer-associated thrombosis (CAT) scores, to ensure a comprehensive assessment [30].
Troubleshooting Common Experimental Challenges
Problem: High Drop-out Rates or Adverse Event Reporting in Clinical Trial Phases.
- Potential Cause: Inadequate pre-screening and risk stratification, leading to the enrollment of participants for whom the HRT regimen is inappropriate.
- Solution:
- Implement the HFA-ICOS risk stratification tool as a structured pre-screening checklist to identify patients at "High" or "Very High" risk for CV toxicity prior to enrollment [28]. This tool effectively categorizes pre-existing conditions.
- Establish a multidisciplinary review team (endocrinologist, cardiologist, gynecologist) to evaluate patient-specific risks before final inclusion [4].
- Clearly define and document exclusion criteria, such as uncontrolled hypertension, significant liver disease, or a history of recent surgery [29].
Problem: Inconsistent Glycemic Control Data in Study Participants.
- Potential Cause: Reliance on a single metric or an inappropriate method for the study population.
- Solution:
- Implement a multi-parameter glycemic assessment protocol. This should include HbA1c, fasting plasma glucose (FPG), and fasting insulinemia to calculate HOMA-IR [29].
- For more detailed physiological insight, consider employing the hyperinsulinemic-euglycemic clamp technique in a subset of participants, acknowledging its complexity [3].
- Strictly standardize the timing of blood sample collection in relation to HRT administration and meals.
Problem: Confounding Effects of Concomitant Medications on Primary Endpoints.
- Potential Cause: Failure to account for the metabolic effects of common diabetes medications, such as GLP-1 receptor agonists and SGLT2 inhibitors.
- Solution:
- Document all concomitant medications at baseline and throughout the study.
- Use stratified randomization during trial design to ensure balanced distribution of participants using these drugs across study arms.
- Statistically adjust for the use of these medications as covariates in the final analysis model. Future research should specifically investigate the interplay between HRT and modern diabetes therapies [4].
Experimental Protocols and Data Presentation
Protocol: Comprehensive Baseline Cardiovascular Risk Stratification
Objective: To systematically identify patients at high risk for cardiovascular toxicity prior to enrollment in an HRT intervention study.
Methodology:
- Medical History & Physical Exam: Conduct a comprehensive review of systems focusing on CV history, thrombotic events, and cancer. Perform a physical exam including BMI and waist circumference [28].
- Diagnostic Tests:
- 12-lead Electrocardiogram (ECG): Assess for arrhythmias and measure QTc interval [28].
- Transthoracic Echocardiogram (TTE): Quantify Left Ventricular Ejection Fraction (LVEF) and assess for structural heart disease [28].
- Blood Biomarkers: Measure fasting lipid profile, renal function (eGFR), cardiac troponin (cTn), and B-type Natriuretic Peptides (NPs) [28].
- Risk Categorization: Utilize the adapted HFA-ICOS risk table (see Table 1) to assign a baseline risk category (Low, Moderate, High, Very High).
Table 1: Adapted HFA-ICOS Baseline CV Risk Stratification for HRT Research [28]
| Risk Factor Category | Specific Risk Factor | Risk Level for HRT Studies |
|---|---|---|
| Previous CVD | Heart Failure / Cardiomyopathy | Very High |
| Myocardial Infarction / Stable Angina | High | |
| Severe Valvular Heart Disease | High | |
| Cardiac Imaging | LVEF <50% | High |
| LVEF 50–54% | Moderate | |
| Cardiac Biomarkers | Elevated Baseline NPs or cTn | Moderate |
| Age & CVRF | Age ≥80 years | High |
| Age 65–79 years | Moderate | |
| Hypertension / Diabetes / Chronic Kidney Disease | Moderate | |
| Lifestyle Factors | Obesity (BMI >30 kg/m²) / Current Smoker | Moderate |
Protocol: Assessing the Impact of HRT on Insulin Resistance (HOMA-IR)
Objective: To evaluate the effect of a specific HRT regimen on insulin sensitivity in postmenopausal women with T2DM over a 12-month period.
Methodology (Based on a Prospective Clinical Study) [29]:
- Study Population: Postmenopausal women with T2DM, confirmed by FSH >30 mIU/ml and estradiol <20 pg/mL.
- Intervention: Randomize participants to HRT group (e.g., 1mg 17β-estradiol + 2mg drospirenone orally daily) or non-HRT control group.
- Sample Collection & Analysis:
- Collect blood samples after a 12-hour fast at baseline and 12 months.
- Analyze samples for Fasting Plasma Glucose (FPG) and Fasting Insulinemia.
- Calculation:
- Calculate the Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) using the formula: HOMA-IR = (Fasting Glucose [mmol/L] × Fasting Insulin [µU/mL]) / 22.5
- Statistical Analysis: Compare within-group changes (baseline vs. 12 months) using a paired t-test and between-group differences using an independent samples t-test. A p-value <0.05 is considered statistically significant.
Table 2: Expected Metabolic Outcomes from a 12-Month HRT Intervention [29]
| Metabolic Parameter | HRT Group (Baseline) | HRT Group (12 Months) | Control Group (Baseline) | Control Group (12 Months) |
|---|---|---|---|---|
| Fasting Plasma Glucose (mmol/L) | 7.8 ± 0.9 | 6.9 ± 0.6 * | 7.8 ± 1.1 | 8.0 ± 0.9 |
| HbA1c (%) | 7.6 ± 0.5 | 7.1 ± 0.4 * | 7.9 ± 0.5 | 7.9 ± 0.6 |
| Fasting Insulin (µU/mL) | 12.2 ± 3.4 | 10.1 ± 2.8 * | 12.3 ± 3.2 | 12.5 ± 3.5 |
| HOMA-IR | 4.23 ± 1.7 | 3.11 ± 1.2 * | 4.31 ± 1.8 | 4.45 ± 1.9 |
*Statistically significant change from baseline (p < 0.001).
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for HRT Mechanistic and Clinical Research
| Item Name | Function / Application | Example / Specification |
|---|---|---|
| 17β-Estradiol | The primary estrogen used in HRT formulations for research; allows study of estrogen's direct metabolic effects [29]. | Pharmaceutical grade; specify oral or transdermal delivery system. |
| Drospirenone | A progestogen often combined with estradiol; has anti-mineralocorticoid activity which may be beneficial in metabolic syndrome [29]. | Pharmaceutical grade; used in combination therapy. |
| ELISA Kits (Insulin, cTn, NPs) | For quantitative measurement of key biomarkers in serum/plasma to assess insulin resistance and cardiovascular strain [29] [28]. | High-sensitivity, validated kits for clinical research. |
| HOMA2 Calculator | Software tool for calculating HOMA2 indices (%B, %S, IR) from fasting glucose and insulin, providing a more refined estimate than the classic HOMA-IR [29]. | Available from the University of Oxford. |
| Hyperinsulinemic-Euglycemic Clamp Setup | The gold-standard method for directly measuring whole-body insulin sensitivity in a subset of participants for deep phenotyping [3]. | Requires controlled infusion pumps and frequent glucose monitoring. |
| Structured Clinical Interview Protocol | Standardized tool for consistent and comprehensive assessment of menopausal symptoms, medication history, and adverse events across the study cohort. | Based on Menopause Rating Scale (MRS) or similar. |
Visualizations: Pathways and Workflows
Integrated Risk Assessment Workflow
HRT & Insulin Sensitivity Signaling Pathway
Technical Support Center: Troubleshooting HRT Regimens for Research in Type 2 Diabetes
Frequently Asked Questions (FAQs)
FAQ 1: Why is the transdermal route of estrogen administration recommended over oral for HRT regimens in women with type 2 diabetes?
The key difference lies in the metabolic pathway and associated thromboembolic risk. Oral estrogen undergoes first-pass metabolism in the liver, which can impair the balance between clotting and anti-clotting proteins and increase the production of triglycerides [31]. Transdermal estrogen bypasses this first-pass effect, entering the circulation directly through the skin, and is associated with a significantly lower risk of venous thromboembolism (VTE) [32] [33]. For women with type 2 diabetes, who already have an elevated baseline cardiovascular risk, this safety profile is crucial. A 2025 real-world study found that oral estrogen doubled the risk of pulmonary embolism and increased heart disease risk by 21% compared to transdermal formulations in this population [31].
FAQ 2: What is the evidence supporting micronized progesterone as the optimal progestogen in HRT, especially for women with type 2 diabetes?
Micronized progesterone, a body-identical hormone, is preferred over synthetic progestogens due to its superior safety profile, particularly regarding breast cancer risk and metabolic impact [33]. Evidence suggests that for the first 5 years of use, estrogen combined with micronized progesterone is not associated with an increased risk of breast cancer [33]. Furthermore, its metabolic profile is more neutral. This is critical for women with type 2 diabetes, as some synthetic progestogens can worsen insulin resistance. Micronized progesterone is not associated with the diabetogenic effect that has been observed with other progestogen formulations, such as 17-alpha-hydroxyprogesterone caproate [34] [35].
FAQ 3: How does the timing of HRT initiation relative to menopause affect metabolic outcomes in research populations?
The "timing hypothesis" or "window of opportunity" suggests that initiating HRT early in menopause (within 10 years of onset or before age 60) provides the most benefit for metabolic parameters and cardiovascular risk reduction [4] [36] [3]. Early initiation is linked to improved insulin sensitivity, preserved pancreatic beta-cell function, and a lower incidence of type 2 diabetes [4] [3]. Starting HRT beyond this window, particularly in older women with established vascular disease, may be associated with increased risks [4].
FAQ 4: What are the critical methodological considerations when designing studies to compare HRT formulation effects on glucose homeostasis?
Discrepancies in study outcomes often stem from the methods used to assess glucose metabolism [3]. Researchers should note that clinical indices like HOMA-IR may show different results compared to steady-state methods like the hyperinsulinemic-euglycemic clamp (the gold standard for measuring insulin sensitivity) [3]. Consistency in assessment tools is vital for valid comparisons. Furthermore, study design must account for key confounders in women with type 2 diabetes, including age, time since menopause, BMI, HbA1c levels, and history of hypertension, to isolate the effect of the HRT formulation [31].
Troubleshooting Guides
Problem: Inconsistent Findings on HRT's Impact on Lipid Profiles
- Potential Cause: The route of estrogen administration significantly influences lipid metabolism. Oral estrogens consistently increase triglycerides, which can be a concern in diabetic dyslipidemia, while transdermal estrogens have a more neutral effect [37].
- Solution: When designing protocols or interpreting data, explicitly stratify outcomes by administration route. The table below summarizes typical lipid profile changes to guide expected outcomes.
Table 1: Comparative Effects of HRT Formulations on Metabolic Parameters
| Parameter | Oral Estrogen | Transdermal Estrogen | Notes |
|---|---|---|---|
| VTE Risk | Significantly Increased [32] [31] | Neutral/Safer Profile [32] [33] [31] | Strongest differentiating factor. |
| Triglycerides | Increases (e.g., +20.7% with CEE) [37] | Neutral effect [37] | Critical for patients with hypertriglyceridemia. |
| HDL Cholesterol | Increases (e.g., +9.0% with CEE) [37] | Neutral effect [37] | The clinical benefit of this increase is debated. |
| Glycemic Control | Improves insulin sensitivity [4] [3] | Improves insulin sensitivity [4] [3] | Both routes show benefit vs. no HRT. |
| Breast Cancer Risk (with Progestogen) | Small increased risk with synthetic progestogens [33] | No increased risk for first 5 years with micronized progesterone [33] | Progestogen type is a key variable. |
Problem: Patient Selection Bias in Observational Studies
- Potential Cause: Women prescribed transdermal HRT are often those with higher baseline cardiovascular risk (e.g., obesity, diabetes), creating a "channeling bias" where higher-risk patients are directed to the supposedly safer therapy [31].
- Solution: In data analysis, employ rigorous statistical methods like propensity score matching to control for confounders such as age, BMI, HbA1c, and hypertension history [31]. This allows for a more valid comparison between treatment groups.
Problem: Concerns About Progestogen's Impact on Glucose Tolerance
- Potential Cause: The use of certain synthetic progestogens, which have been linked to an increased risk of gestational diabetes and may worsen insulin resistance [34].
- Solution: Standardize the use of body-identical micronized progesterone in research protocols where possible. Evidence suggests vaginal micronized progesterone is not associated with a higher risk of gestational diabetes, supporting its metabolically neutral profile [35].
Experimental Protocols & Methodologies
Protocol 1: Assessing the Impact of HRT Route on Glucose Metabolism in a Rodent Model of Type 2 Diabetes
This protocol is designed to isolate the effect of estrogen administration route on glucose homeostasis, independent of progestogen.
- Animal Model: Use ovariectomized female mice or rats fed a high-fat diet to model postmenopausal type 2 diabetes.
- Study Groups:
- Group 1: Control (vehicle)
- Group 2: Oral 17β-estradiol (administered via drinking water or gavage)
- Group 3: Transdermal 17β-estradiol (administered via slow-release subcutaneous pellet)
- Ensure doses are physiologically comparable.
- Duration: 8-12 weeks of treatment.
- Endpoint Measurements:
- Insulin Sensitivity: Perform an insulin tolerance test (ITT).
- Glucose Tolerance: Perform an intraperitoneal or oral glucose tolerance test (GTT).
- Tissue Analysis: Collect tissues for:
- Liver: Analyze gene expression of gluconeogenic enzymes (PEPCK, G6Pase).
- Skeletal Muscle and Adipose Tissue: Assess insulin signaling pathway activation (e.g., via Western blot for p-AKT/AKT) in response to insulin stimulation.
- Body Composition: Monitor changes in visceral adiposity using MRI or by weighing fat pads at sacrifice.
The diagram below illustrates the key metabolic pathways and tissue-specific effects of estrogen that this protocol aims to investigate.
Protocol 2: Clinical Research Methodology for Comparing HRT Formulations
This outlines a robust clinical study design based on recent high-quality research [31].
- Study Design: Retrospective cohort or prospective observational study using electronic health records.
- Population: Identify postmenopausal women with type 2 diabetes initiating HRT. Key inclusion criteria: age 45-60, confirmed T2D diagnosis.
- Exposure Groups:
- Cohort A: Transdermal estrogen (patch/gel) + micronized progesterone.
- Cohort B: Oral estrogen + micronized progesterone.
- Control Cohort: Age-matched women with T2D not using HRT.
- Matching: Use propensity score matching (1:1) to control for age, ethnicity, BMI, HbA1c, hypertension, and diabetes duration.
- Follow-up: Minimum 5 years.
- Primary Outcomes: Incidence of:
- Venous thromboembolism (VTE: DVT, PE)
- Ischemic heart disease
- Ischemic stroke
- Secondary Outcomes: Incidence of breast, endometrial, and ovarian cancers; changes in HbA1c and lipid panels.
- Statistical Analysis: Use Cox proportional hazards models to calculate hazard ratios (HR) and 95% confidence intervals (CI) for outcomes between matched groups.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for HRT Formulation Research
| Item / Reagent | Function / Rationale | Example & Notes |
|---|---|---|
| 17β-Estradiol (for research) | The primary biologically active estrogen for in vitro and in vivo studies. | Use in cell culture (dissolved in ethanol/DMSO) or animal models (oral gavage, subcutaneous pellets, transdermal patches). |
| Micronized Progesterone | The body-identical progestogen for endometrial protection with a favorable metabolic and breast safety profile. | Available for clinical research. Contrast with synthetic progestogens (e.g., medroxyprogesterone acetate) to highlight differential effects. |
| Transdermal Delivery Systems | To administer estradiol while bypassing first-pass liver metabolism. | Research-grade patches or gels for animal or human studies. Allows direct comparison with oral administration. |
| Hyperinsulinemic-Euglycemic Clamp | The gold-standard method for precisely quantifying whole-body insulin sensitivity. | Critical for high-fidelity metabolic studies beyond simpler tests like HOMA-IR [3]. |
| Propensity Score Matching Software (e.g., R, Stata) | Statistical method to reduce confounding bias in observational studies, creating comparable treatment and control groups. | Essential for analyzing real-world data to approximate the balance of a randomized controlled trial [31]. |
FAQs: Addressing Key Research Questions
1. What is the mechanistic basis for the "Timing Hypothesis" in menopausal hormone therapy (MHT)? The "Timing Hypothesis" proposes that the cardiovascular and metabolic benefits of MHT are dependent on initiation timing relative to menopause. Initiating therapy in women younger than 60 or within 10 years of menopause allows MHT to exert protective effects on the vascular endothelium before advanced atherosclerosis sets in. Starting therapy beyond this window, when vascular aging is more advanced, may negate benefits and increase risks of adverse events [38] [39].
2. How does MHT influence insulin resistance and glycemic control in postmenopausal women with type 2 diabetes (T2DM)? A 2024 meta-analysis of 17 randomized controlled trials concluded that MHT significantly reduces insulin resistance in healthy postmenopausal women [17]. For women with T2DM, the improvements are even more pronounced, with studies showing a 36% reduction in fasting blood glucose and HOMA-IR (Homeostatic Model Assessment of Insulin Resistance). Estrogen enhances insulin sensitivity by modulating insulin receptor expression, improving pancreatic beta-cell function, and reducing systemic inflammation [4].
3. What are the recommended MHT formulations and routes of administration for women with T2DM and cardiovascular risk factors? Transdermal estrogen (patches, gels) is the preferred route for women with T2DM or elevated cardiovascular risk. Unlike oral estrogen, transdermal administration has a neutral effect on blood pressure and does not increase the risk of venous thromboembolism (VTE) or stroke, making it a safer option [38] [4] [40]. For women with a uterus, progestogen must be added to prevent endometrial cancer; micronized progesterone or dydrogesterone are preferred progestogens due to their lower impact on breast cancer risk [39].
4. What are the critical experimental considerations when modeling the Timing Hypothesis in preclinical studies? Key considerations include the choice of animal model and the timing of intervention. Non-human primates that experience a natural menopause are genetically closest to humans, but rodents are more practical. Ovariectomy in rodents models surgical menopause, creating rapid, severe estrogen deficiency, which differs from the gradual decline in natural menopause. Studies should be designed to compare early intervention (immediately after ovariectomy) versus late intervention to mirror the human clinical window [3] [41].
Troubleshooting Guides for Experimental Design
Challenge: Translating Animal Model Data to Human Clinical Outcomes
- Problem: Data from ovariectomized rodent models does not fully replicate the human condition of natural menopause, which involves gradual hormonal changes and aging.
- Solution: Consider using aged rodent models or non-human primates that experience natural menopause for more translatable results. When using ovariectomized models, explicitly state this limitation and correlate findings with sub-studies of women with surgical versus natural menopause [3].
- Methodology: Implement a dual-model approach:
- Ovariectomy Model: For studying rapid estrogen depletion and the effects of immediate MHT initiation.
- Aged Model: For studying the interaction between hormonal decline and chronological aging, and the effects of late MHT initiation.
Challenge: Discrepancies in Assessing MHT's Effect on Glucose Homeostasis
- Problem: Different methods for assessing insulin sensitivity (e.g., HOMA-IR vs. hyperinsulinemic-euglycemic clamp) can yield conflicting results on the metabolic benefits of MHT [3].
- Solution: Utilize multiple complementary methods within the same study to provide a comprehensive picture.
- Standardized Protocol:
- Primary Measure: Hyperinsulinemic-euglycemic clamp (the gold standard for measuring whole-body insulin sensitivity).
- Secondary Measures: HOMA-IR (for basal insulin resistance) and Intravenous Glucose Tolerance Test (IVGTT) with minimal model analysis (to assess beta-cell function and insulin sensitivity).
- Additional Biomarkers: Measure glycated hemoglobin (HbA1c), fasting glucose, and inflammatory cytokines (e.g., TNF-α, IL-6) [4] [3].
Quantitative Data Synthesis
Table 1: Metabolic and Clinical Outcomes of MHT Based on Timing and Formulation
| Outcome Measure | Effect of Early MHT Initiation ( | Effect of Late MHT Initiation | Influence of Formulation |
|---|---|---|---|
| Insulin Resistance | ~30% reduction in T2DM incidence; 13% reduction in HOMA-IR in non-diabetic women [4] [17] | Limited to no benefit; potential for harm in older women with established vascular disease [38] [42] | Estrogen-alone therapy shows more prominent reduction than combined therapy [17] |
| Cardiovascular Risk | Cardiovascular protection; significant reduction in stroke risk observed in some cohorts [38] [4] [42] | Small increase in stroke risk (~4.9%); no cardiovascular benefit [38] [42] | Transdermal estrogen has neutral/beneficial effect; oral estrogen may increase VTE and stroke risk [38] [40] |
| Breast Cancer Risk | Lower odds of breast cancer when started in perimenopause [42] [39] | Risk increases with longer duration of use and older age [40] | Progestogen component is decisive; progesterone/dydrogesterone have lower risk than synthetic progestins [39] |
| Bone Mineral Density | Prevents post-menopausal bone loss and reduces fracture risk [40] [41] | Effective at preventing bone loss, but risk-benefit profile less favorable [38] | All systemic MHT formulations are effective [41] |
Table 2: Key Reagent Solutions for Investigating MHT in Metabolic Research
| Research Reagent | Function in Experimental Models | Application Notes |
|---|---|---|
| 17β-Estradiol (E2) | The primary physiological estrogen; used to investigate mechanisms of estrogen receptor activation on glucose homeostasis and energy expenditure [3]. | Administered via subcutaneous pellet, oral gavage, or in drinking water to ovariectomized rodents. Dosing must be calibrated to achieve physiological, not supraphysiological, levels. |
| Conjugated Equine Estrogens (CEE) | A complex mixture of estrogens derived from pregnant mares' urine; used to model the formulation tested in the WHI trial [3] [39]. | Useful for translational studies comparing the effects of specific estradiol formulations versus the complex mixture used in major clinical trials. |
| Medroxyprogesterone Acetate (MPA) | A synthetic progestogen; used to study the impact of progestogens on estrogen's beneficial effects, particularly on breast cancer risk [39]. | Often used in combination with CEE in rodent models to replicate the WHI combined therapy arm. Associated with more negative metabolic and breast tissue effects. |
| Progesterone / Dydrogesterone | Natural progesterone or its isomer; considered a "body-identical" progestogen with a safer risk profile, particularly for breast tissue [39]. | The preferred progestogen for combination therapy in experimental models aiming to mimic modern, optimized clinical practice. |
| Transdermal Estradiol Patches/Gels | Enables non-oral delivery of estradiol, bypassing first-pass liver metabolism [38] [4]. | Used in clinical-style experiments in animal models or human studies to investigate the route-of-administration-dependent effects on clotting factors, lipids, and inflammatory markers. |
Experimental Protocols
Protocol 1: Assessing the Timing Hypothesis in an Ovariectomized Rodent Model of T2DM
Objective: To evaluate the metabolic effects of initiating MHT early versus late after estrogen depletion in a diabetic context.
Materials:
- Animal Model: Adult female Zucker Diabetic Fatty (ZDF) rats or similar T2DM model.
- Reagents: 17β-Estradiol pellets (for slow-release), progesterone or MPA for injection, vehicle control.
- Equipment: Equipment for hyperinsulinemic-euglycemic clamp, metabolic cages, dual-energy X-ray absorptiometry (DEXA) scanner.
Methodology:
- Baseline Phase: At 12 weeks of age, perform baseline measurements of body weight, fasting glucose, and body composition via DEXA.
- Ovariectomy (OVX): Perform OVX or sham surgery on all animals.
- Intervention Groups:
- Group 1 (Early MHT): Initiate MHT (e.g., E2 pellet + progesterone injections) immediately post-OVX.
- Group 2 (Late MHT): Initiate identical MHT regimen 8 weeks post-OVX, after metabolic dysfunction is established.
- Group 3 (OVX Control): Receive vehicle treatment post-OVX.
- Group 4 (Sham Control): Undergo sham surgery and receive vehicle.
- Outcome Measures: At the end of the study period (e.g., 20 weeks of age), conduct:
- Hyperinsulinemic-euglycemic clamp to measure insulin sensitivity.
- IVGTT to assess beta-cell function.
- Body composition analysis (DEXA) to quantify fat and lean mass distribution.
- Tissue collection for molecular analysis (e.g., insulin signaling pathway proteins in muscle and liver, hypothalamic neuropeptides).
Protocol 2: Evaluating the Impact of MHT Formulations on Metabolic and Bone Parameters
Objective: To compare the effects of oral versus transdermal estrogen, combined with different progestogens, on glycemic control and bone quality.
Materials:
- Animal Model: Ovariectomized non-human primates or aged mice.
- Reagents: Oral estradiol, transdermal estradiol patches, Medroxyprogesterone Acetate (MPA), micronized progesterone.
- Analytical Equipment: Raman microspectrometer, liquid chromatography-mass spectrometry (LC-MS) for hormone level verification.
Methodology:
- Group Allocation: Ovariectomized animals are randomized into several groups:
- Oral Estradiol + MPA
- Oral Estradiol + Progesterone
- Transdermal Estradiol + MPA
- Transdermal Estradiol + Progesterone
- Vehicle Control
- Treatment Duration: Administer treatments for a period relevant to the model (e.g., 2 years in primates, 3 months in mice).
- Metabolic Phenotyping: Periodically measure body weight, food intake, glucose tolerance, and fasting insulin.
- Bone Quality Analysis: Post-sacrifice, collect iliac crest or femoral bone biopsies.
- Analyze using Raman microspectroscopy to determine bone compositional properties at the ultrastructural level, including mineral/matrix ratio, mineral maturity, and collagen cross-links at precisely defined tissue ages [41].
- Data Integration: Correlate metabolic outcomes (e.g., HOMA-IR) with bone quality parameters to understand systemic versus tissue-specific effects of different MHT regimens.
Visualization of Mechanisms and Workflows
Estrogen Signaling in Glucose Metabolism
Experimental Workflow for Timing Hypothesis
FAQs: HRT Dosing in Type 2 Diabetes Research
FAQ 1: What are the key considerations for selecting an HRT formulation in women with T2DM? The primary considerations are the route of administration and the type of progestogen. For women with T2DM, who have an elevated baseline cardiovascular risk, a transdermal estrogen patch is strongly preferred over oral estrogen. Evidence shows that compared to transdermal delivery, oral estrogen doubles the risk of pulmonary embolism and is associated with a 21% increased risk of heart disease in this population [31] [43]. For the progestogen component, selections with neutral effects on glucose metabolism, such as natural progesterone, dydrogesterone, or transdermal norethisterone, are recommended to avoid exacerbating insulin resistance [44].
FAQ 2: What defines "low-dose" and "short-duration" therapy in clinical protocols? "Low-dose" therapy utilizes the minimum effective dose to manage vasomotor symptoms. In practice, low-dose transdermal estrogen patches (e.g., delivering 0.014 to 0.025 mg/day) achieve this goal while minimizing risks [45]. "Short-duration" typically means treatment for less than five years, which aligns with safety data showing a favorable risk-benefit profile within this window for women with T2DM [31] [4]. Treatment should be re-assessed annually to determine if ongoing therapy is warranted.
FAQ 3: What metabolic parameters should be monitored during HRT trials in T2DM subjects? A core set of parameters should be tracked to assess efficacy and safety. Glycemic control should be evaluated via HbA1c, fasting blood glucose, and HOMA-IR calculations [4] [44]. Lipid profiles (LDL-C, HDL-C, and triglycerides) and markers of coagulation and inflammation should also be monitored [46]. Regular assessment of body composition (e.g., waist circumference, visceral fat) is valuable, as menopause and T2DM both predispose to adverse changes in fat distribution [3].
FAQ 4: How does the "timing hypothesis" influence study design for HRT in T2DM? The "timing hypothesis" posits that the cardiovascular benefits of HRT are greatest when initiated in younger women (aged <60 years or within 10 years of menopause onset) versus later [4] [44]. This has critical implications for study design. Clinical trials should stratify participants based on time since menopause rather than chronological age alone. Protocols must clearly define and document the menopausal age of participants to ensure valid analysis of cardiovascular and metabolic outcomes [3] [45].
FAQ 5: What are common pitfalls in designing monitoring protocols for HRT trials? A common pitfall is infrequent re-assessment. Hormone therapy is not "set-it-and-forget-it"; it requires regular monitoring and potential adjustment for a significant minority (20-30%) of patients [47]. Another pitfall is failing to account for the interaction between HRT and glucose-lowering medications. Newer agents like GLP-1 receptor agonists and SGLT2 inhibitors can independently improve glycemic control and cardiovascular risk, which may confound the assessment of HRT's effects [4] [46].
Experimental Protocols & Methodologies
Protocol for Assessing the Impact of HRT on Glycemic Control
Objective: To evaluate the effects of different HRT formulations on insulin sensitivity and beta-cell function in postmenopausal women with T2DM over a 12-month period.
Methodology Details:
- Study Population: Postmenopausal women (amenorrhea for ≥12 months) aged 45-60, with a diagnosis of T2DM, within 10 years of menopause onset. Key exclusion criteria include history of venous thromboembolism, breast cancer, or active liver disease [45] [44].
- Intervention Groups: Randomized, double-blind design with three arms:
- Transdermal 17β-estradiol (low-dose) + micronized progesterone.
- Oral estradiol (low-dose) + dydrogesterone.
- Placebo patch and oral placebo.
- Assessment Schedule: Baseline, 3 months, 6 months, and 12 months.
- Primary Endpoints:
- Secondary Endpoints: Changes in lipid profile, inflammatory markers (e.g., hs-CRP, IL-6), body composition via DXA scan, and quality of life questionnaires [4] [46].
Protocol for Cardiovascular Safety and Re-assessment
Objective: To monitor the cardiovascular safety of low-dose, short-duration HRT in postmenopausal women with T2DM.
Methodology Details:
- Study Population: As in Protocol 2.1.
- Monitoring Schedule: Baseline, 6 months, and then annually for 5 years.
- Key Safety Endpoints:
- Incidence of Venous Thromboembolism (VTE): Deep vein thrombosis (DVT) and pulmonary embolism (PE), confirmed by imaging [31] [43].
- Incidence of Arterial Thrombotic Events: Ischemic heart disease (hospitalization for unstable angina, myocardial infarction) and ischemic stroke, adjudicated by a clinical events committee [31] [48].
- Re-assessment Trigger Points: Therapy should be re-evaluated, and consideration given to discontinuation if:
Data Presentation: Quantitative Findings
Table 1: Cardiovascular Risk Profile of Oral vs. Transdermal HRT in Women with T2DM
| Cardiovascular Event | Oral HRT Risk vs. Transdermal | Transdermal HRT Risk vs. No HRT | Key References |
|---|---|---|---|
| Pulmonary Embolism | 2.0x increased risk (100% higher) | No significant difference | [31] [43] |
| Ischemic Heart Disease | 1.21x increased risk (21% higher) | 0.75x risk (25% lower) | [31] [43] |
| Deep Vein Thrombosis (DVT) | No significant difference | No significant difference | [31] |
| Ischemic Stroke | No significant difference | No significant difference / Potential protective effect (HR: 0.76) | [31] [48] |
Table 2: Metabolic Effects of HRT in Postmenopausal Women with T2DM
| Metabolic Parameter | Effect of HRT (vs. Placebo/No HRT) | Magnitude of Change | Key References |
|---|---|---|---|
| HbA1c | Reduction | -0.56 percentage points | [4] [46] |
| Fasting Glucose | Reduction | -20.7 mg/dL | [46] |
| HOMA-IR (Insulin Resistance) | Reduction | -36% | [44] |
| Incident T2DM (in women without diabetes) | Reduction | -30% | [44] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for HRT and T2DM Research
| Research Reagent / Material | Function / Application in HRT-T2DM Studies |
|---|---|
| 17β-estradiol (Transdermal Patches) | The preferred form of estrogen for interventional studies in T2DM due to its safer cardiovascular risk profile [31] [44]. |
| Micronized Progesterone / Dydrogesterone | Progestogens with a neutral metabolic profile, used to protect the endometrium without negating estrogen's beneficial effects on insulin sensitivity [4] [44]. |
| Oral Estradiol Valerate/Conjugated Estrogens | Comparator oral estrogen formulations used to contrast metabolic and cardiovascular outcomes against transdermal routes [31] [3]. |
| HOMA-IR Calculation Software | Algorithmic tool using fasting glucose and insulin levels to provide a simple, widely accepted index of insulin resistance in large cohort studies [3] [44]. |
| ELISA Kits for Inflammatory Markers (hs-CRP, IL-6, TNF-α) | To quantify low-grade systemic inflammation, a key pathophysiological link between T2DM, menopause, and cardiovascular disease [4]. |
Visualization: Pathways and Workflows
HRT Decision and Monitoring Workflow
Estrogen Signaling and T2DM Risk
Technical Support Center: Troubleshooting Guides and FAQs
This technical support center provides troubleshooting guidance for common interdisciplinary challenges faced by researchers and clinical trial professionals working on Hormone Therapy (HRT) regimens for women with type 2 diabetes.
Frequently Asked Questions (FAQs)
Q1: What is the evidence base for considering Menopausal Hormone Therapy (MHT) in women with type 2 diabetes? A: Large, randomized controlled trials suggest that MHT using estrogens delays the onset of type 2 diabetes in women [3]. The proposed mechanisms include improved β-cell insulin secretion, enhanced insulin sensitivity, and improved glucose effectiveness [3]. Furthermore, MHT mitigates menopausal-related metabolic changes, such as increased visceral adiposity and decreased energy expenditure, which are risk factors for diabetes progression [3].
Q2: How can our research team effectively coordinate between endocrinology, cardiology, and gynecology specialists? A: The primary challenge is often finding time for collaboration [49]. Effective strategies include:
- Leveraging Shared Technology: Using a unified electronic health record (EHR) system for real-time communication, chart review, and sharing clinical notes among specialists [49].
- Direct Communication: Bypassing administrative hurdles by sharing direct contact information (e.g., cell phones for scheduling calls) for quick consultations [49].
- Patient-Centric Coordination: Proactively sending patient histories, lab results, and clinical notes to all involved specialists before patient visits to ensure a cohesive care plan [49].
- Structured Models: Implementing formal models where specialists, such as endocrinologists, work directly with primary care providers in case management and team guidance [50].
Q3: What are the key cardiovascular considerations when designing HRT trials for postmenopausal women with diabetes? A: There is a recognized focus on cardiovascular risk reduction in patients with type 2 diabetes [49]. Key considerations include:
- Cardioprotective Medications: Investigating the role of newer diabetes medications, such as GLP-1 receptor agonists and SGLT-2 inhibitors, which have demonstrated benefits in preventing cardiac events [49].
- Collaborative Responsibility: Establishing clear protocols among endocrinologists, cardiologists, and primary care physicians for managing and prescribing medications with cardiovascular benefits [49].
- Guideline Adherence: Following joint professional guidelines, such as those from the American Diabetes Association and the American College of Cardiology, to standardize care and define roles [49] [51].
Q4: What methodologies are recommended for assessing glucose homeostasis in MHT clinical trials? A: Discrepancies in study outcomes often arise from the physiological differences in assessment methods [3]. A combination of the following is recommended:
- Continuous Glucose Monitoring (CGM): For real-world insights into glycemic control, capturing metrics like time in range and glycemic variability [52] [51].
- Hyperinsulinemic-euglycemic clamp: Considered the gold standard for directly measuring insulin sensitivity [3].
- Intravenous Glucose Tolerance Test (IVGTT): For assessing insulin secretion and sensitivity [3].
- HbA1c and Fasting Glucose: Standard biochemical markers for long-term and point-in-time glycemic control [50].
Troubleshooting Common Interdisciplinary Research Challenges
| Challenge | Root Cause | Proposed Solution & Workaround | Key Performance Indicator |
|---|---|---|---|
| Discordant Care Plans | Lack of communication and inconsistent messaging between specialties [49]. | Implement regular interdisciplinary case conferences (virtual or in-person). Utilize shared EHR for note-passing and real-time chats [49]. | Standardization of treatment protocols across sites; >90% patient records with notes from relevant specialties. |
| Patient Recruitment & Retention | Competitive trial landscape; specific comorbidity and menopausal status requirements [53]. | Leverage advanced data modeling and proprietary patient databases. Use patient concierge services and centralized lifestyle support to improve retention [53]. | Enrollment rate; screen failure rate; patient drop-out rate. |
| Inconsistent Endpoint Measurement | Use of different methodologies and assays across clinical sites [3] [52]. | Implement a central laboratory for harmonized data and consistent assay performance. Provide detailed manuals for complex procedures like clamp studies [52]. | Coefficient of variation for key biomarkers (e.g., HbA1c, insulin) across sites. |
| Managing Complex Comorbidities | Uncertainty over which specialist manages overlapping conditions (e.g., cardiovascular risk) [49]. | Define and document clear responsibility matrices in the study protocol. Foster collaboration to avoid therapeutic inertia [49]. | Proportion of eligible patients prescribed cardioprotective diabetes medications. |
Detailed Experimental Protocols for Key Assessments
Protocol 1: Assessing Insulin Sensitivity via Hyperinsulinemic-Euglycemic Clamp
- Objective: To quantitatively measure insulin-mediated glucose disposal.
- Materials: Intravenous catheters, insulin infusion solution, 20% dextrose solution, frequent sampling glucose analyzer.
- Methodology:
- After an overnight fast, baseline blood samples are drawn for glucose and insulin.
- A primed-continuous intravenous insulin infusion is started at a constant rate (e.g., 40 mU/m²/min) to achieve hyperinsulinemia.
- A variable-rate 20% dextrose infusion is simultaneously started and adjusted every 5-10 minutes based on bedside glucose measurements to maintain euglycemia (~5.0 mmol/L).
- The clamp period typically lasts 120 minutes. The glucose infusion rate (GIR) during the final 30 minutes is calculated.
- Data Analysis: The GIR required to maintain euglycemia is a direct measure of whole-body insulin sensitivity. The mean GIR (mg/kg/min) over the steady-state period is the primary outcome.
Protocol 2: Implementing a Specialist-Involved Collaborative Care Model
- Objective: To integrate specialist expertise into the primary research/clinical care framework to improve patient outcomes [50].
- Materials: Shared EHR or communication platform, standardized referral and feedback forms, defined meeting schedules.
- Methodology:
- Role Definition: Clearly outline the responsibilities of the endocrinologist, cardiologist, and gynecologist within the trial (e.g., protocol for managing cardiovascular risk, adverse events).
- Structured Communication: Establish weekly or bi-weekly virtual "huddles" for the core research team to discuss patient progress and management challenges [49].
- Co-management: Specialists actively participate in creating and supervising management plans. This may involve e-consults, shared appointments, or case discussions [50].
- Feedback Loop: Specialists provide structured feedback to the primary research team, and outcomes are tracked against standards of care [50] [51].
- Data Analysis: Compare outcomes like HbA1c reduction, medication adherence, and patient satisfaction scores between intervention and control groups. A meta-analysis of such models showed a mean HbA1c reduction of -0.57% (95% CI: -0.86 to -0.27) [50].
Visualization of Workflows and Pathways
Diagram 1: Multidisciplinary Patient Care Workflow
Diagram 2: Estrogen Signaling in Glucose Homeostasis
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function in Research | Application Note |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Provides real-time, ambulatory measurement of interstitial glucose levels; captures glycemic variability (TIR, GV) [52]. | Ideal for long-term, real-world efficacy studies of HRT regimens. Aligns with latest ADA guidance for T2D monitoring [51]. |
| ELISA/Kits for Metabolic Biomarkers | Quantifies specific proteins and hormones (e.g., Insulin, C-peptide, Adipokines) from serum/plasma samples. | Essential for assessing beta-cell function and insulin resistance. Use validated, high-sensitivity kits from a central lab [52]. |
| Dual-Energy X-Ray Absorptiometry (DXA) | Precisely measures body composition (lean mass, fat mass, visceral fat) and bone mineral density [3]. | Critical for tracking MHT-induced changes in body composition and fat distribution independent of weight [3]. |
| Hyperinsulinemic-Euglycemic Clamp Setup | The gold-standard research method for directly quantifying insulin sensitivity in vivo [3]. | Complex and resource-intensive. Required for mechanistic studies to definitively prove MHT's metabolic effects [3]. |
| Stable, Formulated HRT Compounds | The investigational products, including oral and transdermal estrogens, and various progestogens. | The route of administration (oral vs. transdermal) and progestogen type are key variables that can influence metabolic outcomes [3]. |
| Electronic Health Record (EHR) System | Facilitates secure data collection, sharing of patient histories, and communication among research specialists [49]. | A shared platform is foundational for successful interdisciplinary collaboration and data integrity. |
Mitigating Risks and Overcoming Clinical Challenges in Complex Patients
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary thromboembolic safety consideration when choosing an HRT administration route for a woman with type 2 diabetes?
The most significant and well-established safety difference is the risk of venous thromboembolism (VTE). Oral estrogen is associated with a higher risk of VTE, while the transdermal route (patches, gels) demonstrates a significantly lower risk and is considered safer for women with T2DM, particularly those with moderate to high cardiovascular risk [32] [54] [55]. The increased risk with oral administration is attributed to the first-pass liver metabolism, which increases the production of pro-coagulant factors [54].
FAQ 2: How does the route of estrogen administration influence cardiovascular disease (CVD) risk in this population?
Evidence indicates that the HRT administration route differentially impacts cardiovascular risk markers and outcomes:
- Oral Estrogen: Associated with an increased risk of ischemic heart disease (IHD) and cerebral infarction (ischemic stroke) in women with T2DM [55].
- Transdermal Estrogen: Shows a more favorable profile. In women with T2DM, its use was associated with a reduced risk of IHD compared to non-users and no increased risk of cerebral infarction compared to non-users [55]. Its neutral effect on cardiovascular risk makes it the preferred choice for women with T2DM and established CVD risk factors [56] [4].
FAQ 3: Does HRT formulation affect glycemic control in postmenopausal women with T2DM?
Yes. Menopausal Hormone Therapy (MHT), in general, has been shown to improve glycemic control. It reduces insulin resistance and can lower glycated hemoglobin (HbA1c) by approximately 0.56% in women with T2DM [56] [4]. While both routes can be beneficial, oral 17β-estradiol is noted for having more pronounced beneficial effects on glucose metabolism [56]. However, the choice must balance these metabolic benefits against the individual patient's thromboembolic and cardiovascular risk profile.
FAQ 4: What is the "timing hypothesis" and how does it influence HRT initiation in women with T2DM?
The "timing hypothesis" proposes that initiating HRT early in the menopausal transition (within 10 years of menopause or before age 60) provides the greatest cardiovascular benefit and the lowest risk of adverse events [4]. This is critical for women with T2DM, as initiating HRT late (e.g., >10 years post-menopause) in women with established atherosclerosis is associated with an increased thromboembolic risk and no additional cardiovascular benefit [56]. Early initiation leverages a window of opportunity when the vasculature is more responsive to estrogen's protective effects.
Troubleshooting Guides & Experimental Protocols
Guide 1: Investigating Route-Specific Thrombosis Risk
Objective: To compare the pro-thrombotic potential of oral versus transdermal estrogens using in vitro and in vivo models.
Background: Oral estrogen undergoes first-pass hepatic metabolism, leading to a heightened synthesis of clotting factors and a significantly increased risk of VTE compared to the transdermal route [54]. This protocol outlines a methodology to quantify this risk.
Experimental Workflow:
Methodology:
- In Vitro Model:
- Cell Culture: Utilize a human hepatocyte cell line (e.g., HepG2) maintained in standard culture conditions.
- Treatment Groups:
- Control (Vehicle)
- Oral Estrogen (e.g., Conjugated Equine Estrogens - CEE)
- Transdermal Estrogen (e.g., 17β-estradiol)
- Concentrations should reflect clinically relevant serum levels post-administration.
- Analysis: After 24-72 hours of exposure, collect cell culture supernatant and lysates.
- Measure the production of key coagulation factors (Factor V, VIII, prothrombin) via ELISA.
- Assess global hemostatic capacity using thrombin generation assays (Calibrated Automated Thrombogram).
- In Vivo Model:
- Animal Model: Use ovariectomized female mice or rats to simulate the postmenopausal state.
- Treatment: Administer estrogens via oral gavage vs. transdermal patches designed for rodents over 4-8 weeks.
- Thrombosis Induction: Employ an established model, such as the FeCl₃-induced carotid artery injury model.
- Primary Outcome Measures:
- Time to vessel occlusion (measured by Doppler flow probe).
- Thrombus size and composition (histological analysis).
Troubleshooting Table:
| Symptom | Possible Cause | Corrective Action |
|---|---|---|
| No significant difference in clotting factors between groups. | Dosage may be too low or exposure time too short. | Conduct a dose-response study. Measure serum estrogen levels to confirm bioavailability. |
| High variability in in vivo thrombosis data. | Inconsistent injury induction or animal model strain. | Standardize the FeCl₃ concentration and application time. Use an inbred animal strain. |
| Transdermal patch poor adhesion in rodents. | Animal activity damaging the patch. | Use secure bandaging and consider a jacket-and-tether system for prolonged studies. |
Guide 2: Evaluating Impact on Atherosclerosis and Metabolic Parameters
Objective: To assess the differential effects of oral and transdermal HRT on the progression of atherosclerosis and glycemic control in a diabetic, postmenopausal animal model.
Background: The choice of HRT route significantly impacts cardiovascular and metabolic outcomes. Transdermal estrogen is preferred for women with T2DM at moderate to high cardiovascular risk due to its safer profile [56] [4] [55]. This protocol tests these clinical observations in a controlled preclinical setting.
Experimental Workflow:
Methodology:
- Animal Model Development:
- Induce surgical menopause via ovariectomy in female ApoE⁻/⁻ or LDLR⁻/⁻ mice.
- Feed a high-fat diet (e.g., 45% kcal from fat) and/or use a low-dose streptozotocin protocol to induce a T2DM-like state.
- Confirm diabetes (fasting blood glucose >200 mg/dL) and allow atherosclerosis to develop for 4-8 weeks.
Treatment Groups:
- Control (Vehicle)
- Oral HRT (e.g., CEE with or without Medroxyprogesterone Acetate - MPA)
- Transdermal HRT (e.g., 17β-estradiol patch with or without progesterone/progestin like Norethisterone Acetate - NETA or Micronized Progesterone - P4)
Outcome Measures (at 10-12 weeks of treatment):
- Metabolic: Intraperitoneal Glucose Tolerance Test (IPGTT), Insulin Tolerance Test (ITT), fasting insulin, HbA1c.
- Cardiovascular: Plasma lipid profile (LDL, HDL, Triglycerides). Quantification of atherosclerotic lesion size in the aortic root and en face aorta (Oil Red O staining).
- Molecular: Analyze insulin signaling pathway activation (p-AKT/AKT ratio) in muscle and liver tissue via western blot.
Troubleshooting Table:
| Symptom | Possible Cause | Corrective Action |
|---|---|---|
| Failure to induce diabetes. | Streptozotocin dose is suboptimal or animal strain is resistant. | Titrate streptozotocin dose. Confirm β-cell damage by measuring insulin/C-peptide. |
| No difference in atherosclerosis. | Treatment duration may be too short, or baseline lesions too advanced. | Initiate HRT treatment earlier in the disease process and extend the study duration. |
| Adverse event (e.g., high mortality) in oral HRT group. | Potentially related to pro-thrombotic effects or metabolic stress. | Reduce the dosage of oral estrogen and monitor health status more frequently. |
Table 1: Comparative Thrombotic and Cardiovascular Risk of HRT Routes in Women with T2DM
| Outcome Measure | Oral HRT | Transdermal HRT | Notes & Comparative Analysis |
|---|---|---|---|
| Venous Thromboembolism (VTE) Risk | Significantly increased [32] [54] | Lower risk; similar to non-users in T2DM [55] | Strongest clinical difference; clear evidence supports transdermal route for VTE safety [32]. |
| Ischemic Heart Disease (IHD) Risk | Increased (HR 1.34, CI 1.08-1.66) [55] | Reduced vs. non-users (HR 0.78, CI 0.61-0.99) [55] | In T2DM, oral use increases risk, while transdermal may be protective. |
| Cerebral Infarction (Stroke) Risk | Increased (HR 1.59, CI 1.07-2.39) [55] | No increased risk vs. non-users with T2DM [55] | Transdermal route shows a safer profile for stroke risk. |
| Impact on Glycemic Control | Improves glycemic control; oral 17β-estradiol has pronounced benefits [56] | Improves glycemic control [56] | Both routes are beneficial, though some data favor oral for metabolic effects. Risk-benefit assessment is key. |
| Recommended Patient Profile | Women with low CVD risk, soon after menopause [56] | Women with moderate/high CVD risk, obesity, T2DM [56] [55] | CVD risk stratification is imperative before initiation [56]. |
Table 2: Key Progestogens and Their Metabolic Effects for Use in T2DM
| Progestogen | Administration Route | Effect on Glucose Metabolism | Clinical Recommendation |
|---|---|---|---|
| Micronized Progesterone | Oral | More neutral effect [56] | Preferred option for women with intact uterus and T2DM [56]. |
| Dydrogesterone | Oral | More neutral effect [56] | Preferred option for women with intact uterus and T2DM [56]. |
| Norethisterone Acetate (NETA) | Transdermal | More neutral effect [56] | Indicated for use with transdermal estrogen in women with T2DM [56]. |
| Medroxyprogesterone Acetate (MPA) | Oral | Less favorable metabolic profile | Not recommended as first-line in T2DM based on current evidence [56]. |
The Scientist's Toolkit: Essential Research Reagents & Models
Table 3: Key Reagents and Models for HRT Route Investigation
| Item | Function/Explanation | Example Products/Models |
|---|---|---|
| 17β-estradiol | The primary human estrogen; gold standard for experimental studies of physiological estrogen action. | Sigma-Aldrich E8875; used in both oral and transdermal formulation studies. |
| Conjugated Equine Estrogens (CEE) | A complex mixture of estrogens derived from horse urine; used in major clinical trials (e.g., WHI). | Premarin; used to model classic oral HRT and its specific effects. |
| ApoE⁻/⁻ or LDLR⁻/⁻ Mice | Genetically modified mice that develop hypercholesterolemia and atherosclerosis on a high-fat diet. | Jackson Laboratory Stock #002052 (ApoE), #002207 (LDLR). Essential for CVD outcome studies. |
| Ovariectomized Rat/Mouse | Standard preclinical model for surgical menopause, allowing controlled hormone replacement. | Charles River Laboratories; provides a consistent baseline for interventional studies. |
| Calibrated Automated Thrombogram (CAT) | Instrumental assay to measure thrombin generation in plasma, a key global marker of thrombotic potential. | Thrombinoscope; crucial for quantifying the pro-coagulant state induced by different HRT routes. |
| HbA1c & HOMA-IR Assays | HbA1c reflects long-term glycemic control; HOMA-IR estimates insulin resistance from fasting glucose/insulin. | ELISA kits (e.g., Crystal Chem); standard methods for assessing metabolic impact of HRT. |
FAQs: HRT and Comorbidities
FAQ 1: What is the updated FDA guidance on HRT boxed warnings, and how does it impact risk-benefit discussions for patients with comorbidities?
In November 2025, the U.S. Food and Drug Administration (FDA) announced the removal of the boxed warnings (also known as "black box" warnings) related to cardiovascular disease, breast cancer, and probable dementia from most menopausal hormone therapy (MHT) products [57] [58] [59]. This decision was based on a comprehensive reassessment of scientific evidence, which found that the original warnings—prompted by the Women's Health Initiative (WHI) study—were overstated and primarily applied to an older population (average age 63) using formulations no longer common [57] [60]. The FDA concluded that these broad warnings had led to significant underutilization of HRT among symptomatic women who would likely benefit [57].
For researchers and clinicians, this regulatory change shifts the risk-benefit paradigm:
- Risk Contextualization: The removed warnings were not supported for the typical younger menopause cohort (ages 45-55). Warnings for endometrial cancer for systemic estrogen-alone products remain [57].
- Individualized Assessment: The update emphasizes nuanced, personalized risk evaluation rather than blanket contraindications. This is particularly crucial for women with preexisting cardiovascular disease (CVD) or high breast cancer risk [57] [61].
- Research Implications: Future clinical protocols and observational studies should reflect this updated regulatory stance, no longer weighting these particular risks as prominently in study designs or informed consent documents.
FAQ 2: How does the route of HRT administration (oral vs. transdermal) modulate cardiovascular risk, particularly in women with preexisting CVD or elevated cardiometabolic risk?
The route of estrogen administration is a critical determinant of cardiovascular risk, especially in susceptible populations. Evidence from a large 2024 Swedish register-based emulated target trial (n=919,614) provides key comparative data [62].
Table: Cardiovascular Risk Profiles of Different HRT Regimens
| HRT Regimen | Venous Thromboembolism (VTE) Risk | Ischemic Heart Disease Risk | Cerebral Infarction & Myocardial Infarction Risk |
|---|---|---|---|
| Oral Combined (E+P) | Increased (HR 1.61-2.00) [62] | Increased (HR 1.21) [62] | Not significantly increased in primary analysis [62] |
| Oral Estrogen-Only | Increased (HR 1.57) [62] | Data not specified in results | Data not specified in results |
| Transdermal Estrogen | No increased risk [62] | No increased risk [62] | No increased risk [62] |
| Tibolone | No increased risk [62] | Increased (HR 1.46) [62] | Increased (HR ~1.94-1.97) [62] |
Mechanism Explanation: Oral estrogen undergoes first-pass liver metabolism, which increases the production of coagulation factors and can induce a pro-thrombotic state. Transdermal administration bypasses this first-pass effect, resulting in a more favorable cardiovascular risk profile [4] [62]. For women with type 2 diabetes, who already have an elevated baseline risk of CVD, transdermal estrogen is generally the preferred option due to its neutral effects on thrombotic risk [4].
FAQ 3: What is the differential risk profile of estrogen-only (E-HT) versus estrogen-plus-progestin (EP-HT) therapy on breast cancer incidence, and how should this guide therapy for high-risk patients?
Robust data confirms that breast cancer risk profiles differ significantly between HRT types. A large-scale NIH analysis from July 2025, which included data from over 459,000 women under 55, found opposing associations [63]:
- Estrogen-only Therapy (E-HT): Associated with a 14% reduction in breast cancer incidence compared to non-users. This protective effect was more pronounced with earlier initiation and longer duration of use [63].
- Estrogen-plus-Progestin Therapy (EP-HT): Associated with a 10% increase in breast cancer incidence. The risk was higher (18%) among women using EP-HT for more than two years [63].
Clinical and Research Translation:
- Patient Selection: For high-risk women with a uterus, the decision to use EP-HT requires careful counseling, weighing the quality-of-life benefits against the elevated breast cancer risk. For high-risk women without a uterus, E-HT may be a viable option that does not increase—and may even reduce—breast cancer risk [61] [63].
- Risk Magnitude: The absolute risk increase with EP-HT is modest. The cumulative risk of breast cancer before age 55 was estimated at 4.5% for EP-HT users versus 4.1% for never-users [63].
- Formulation & Duration: Research should focus on optimizing progestin type and regimen to minimize mitogenic stimulation while providing adequate endometrial protection.
Troubleshooting Guides
Guide 1: Troubleshooting HRT-Associated Cardiovascular Risk in Clinical Trial Design
Problem: An investigational HRT regimen shows promising efficacy for vasomotor symptoms but is associated with increased incidence of venous thromboembolism (VTE) in early-phase trials.
Investigation & Solution Protocol:
- Step 1: Differentiate by Administration Route. Determine if the regimen is oral. If yes, consider reformulating to a transdermal patch or gel, as the Swedish trial data clearly shows transdermal estrogen does not carry the same VTE risk as oral formulations [62].
- Step 2: Apply the "Timing Hypothesis." Re-evaluate the patient population. Are participants predominantly younger (<60 years) and within 10 years of menopause onset? The cardiometabolic risks of HRT are significantly lower in this group. Restrict trial eligibility to this cohort to better demonstrate a positive benefit-risk profile [57] [4].
- Step 3: Analyze Progestogen Component. For combination therapy, review the type of progestogen. Some synthetic progestins (e.g., medroxyprogesterone acetate) may have a less favorable risk profile than natural progesterone or newer progestins. Consider switching this component [4] [62].
- Step 4: Implement Enhanced Monitoring. For trials that must include higher-risk participants, institute a rigorous VTE monitoring protocol, including education on symptom recognition and potentially baseline D-dimer testing.
Guide 2: Troubleshooting Breast Cancer Risk Concerns in Patients with a High-Risk Profile
Problem: A patient with a strong family history of breast cancer (but no personal history) and an intact uterus experiences severe vasomotor symptoms. Standard EP-HT is effective but raises concerns about increasing her baseline breast cancer risk.
Investigation & Solution Protocol:
- Step 1: Quantify Baseline Risk. Perform a formal breast cancer risk assessment (e.g., using Gail model) and consider genetic counseling/testing for BRCA1/2 mutations to precisely quantify baseline risk [61].
- Step 2: Consider Vaginal Estrogen. If symptoms are primarily genitourinary (e.g., vaginal dryness), switch to or add low-dose vaginal estrogen. This provides localized symptom relief with minimal systemic absorption and no established increase in breast cancer risk [61].
- Step 3: Evaluate Estrogen-Only Option with LNG-IUD. For a patient with an intact uterus, unopposed estrogen is contraindicated due to endometrial cancer risk. A potential strategy is to use transdermal estrogen (for its favorable metabolic and breast risk profile) combined with a levonorgestrel-releasing intrauterine device (LNG-IUD) for endometrial protection. This may offer a better risk profile than oral EP-HT [61] [64].
- Step 4: Optimize Dose and Duration. Use the lowest effective dose of EP-HT for the shortest acceptable duration (e.g., less than 3-5 years), as risk increases with duration of use [61] [63].
Experimental Pathway for Risk Assessment
The following pathway outlines a systematic approach for evaluating HRT suitability in patients with comorbidities, integrating the latest evidence.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for HRT and Comorbidity Research
| Research Reagent / Material | Function in Experimental Design |
|---|---|
| Transdermal 17β-Estradiol Patches | Provides continuous transdermal estrogen delivery; critical for studies focusing on cardiovascular safety as it avoids first-pass liver metabolism and associated VTE risk [4] [62]. |
| Micronized Progesterone | A body-identical progesterone used in combination HRT; considered to have a potentially safer risk profile (particularly for breast and cardiovascular outcomes) compared to some synthetic progestins [4] [64]. |
| Levonorgestrel-Releasing IUD (LNG-IUD) | Provides localized endometrial protection in women with a uterus receiving systemic estrogen; allows investigation of estrogen-only systemic benefits while mitigating endometrial cancer risk, potentially avoiding the systemic breast cancer risk associated with oral progestins [61] [64]. |
| Validated Menopause-Specific QoL Instruments | Tools like the Greene Climacteric Scale or MENQOL questionnaire are essential for quantifying patient-centered outcomes, especially when weighing treatment benefits against potential risks in vulnerable populations [64]. |
| Biobanked Serum Samples | Crucial for correlating clinical outcomes with biomarkers of inflammation (e.g., IL-6, TNF-α), glycemic control (HbA1c, HOMA-IR), and coagulation factors in longitudinal studies [4] [62]. |
FAQs: Hormone Therapy and Cognitive Function in Women with T2DM
Q1: What is the relationship between menopausal hormone therapy (MHT) and cognitive decline risk in older women with type 2 diabetes (T2DM)?
Evidence from the Women's Health Initiative Memory Study (WHIMS) indicates that the effect of MHT on cognitive impairment risk differs significantly for women with T2DM. Through a maximum of 18 years of follow-up, older women (aged 65-80) with T2DM who were assigned to MHT had a substantially increased risk of probable dementia (HR 2.12, 95% CI 1.47–3.06) and cognitive impairment (HR 2.20, 95% CI 1.70–2.87) compared to women without these conditions. This suggests that in older women with T2DM, MHT may exacerbate the increased risk for cognitive impairment conveyed by diabetes itself [65].
Q2: Does the timing of MHT initiation relative to menopause affect cognitive outcomes?
Yes, the timing of initiation appears to be critical, supporting the "critical window" hypothesis. Meta-analyses of randomized controlled trials indicate that when MHT is initiated in midlife or close to menopause onset, estrogen therapy is associated with improved verbal memory (SMD=0.394, 95% CI 0.014, 0.774). In contrast, initiation in late life (age ≥60) has no cognitive benefits and may be associated with decline, particularly with estrogen-progestogen therapy [66]. This timing effect may be partially mediated by MHT's protective effects against diabetes risk, which in turn benefits late-life memory [67].
Q3: How does MHT formulation influence cognitive effects?
Formulation significantly influences cognitive outcomes. Estrogen-only therapy for surgical menopause has been associated with improved global cognition (SMD=1.575, 95% CI 0.228, 2.921), whereas estrogen-progestogen therapy for spontaneous menopause has been associated with a decline in Mini Mental State Exam (MMSE) scores compared to placebo (SMD=-1.853, 95% CI -2.974, -0.733) [66]. The adverse cognitive effects of combined MHT in women with T2DM appear to be more pronounced with unopposed conjugated equine estrogens [65].
Experimental Protocols for Investigating MHT-Cognition Interactions in T2DM Models
Protocol 1: Assessing Cognitive Outcomes in Preclinical T2DM Models
This protocol outlines methodology for evaluating MHT effects on cognitive endpoints in diabetic models, adapted from longitudinal clinical studies [65] [67].
- Subject Characteristics: Utilize animal models of T2DM (e.g., db/db mice, HFD-fed rodents). Include both hysterectomized and intact uterus models to compare estrogen-only vs. combined therapy.
- Treatment Groups:
- Group 1: T2DM model + Estrogen (17β-estradiol recommended)
- Group 2: T2DM model + Estrogen-Progestogen (e.g., MPA)
- Group 3: T2DM model + Vehicle (Placebo control)
- Group 4: Non-diabetic control + Vehicle
- Critical Timing Intervention: Administer treatment at early-stage (representing "midlife") versus late-stage ("late-life") diabetes to test the critical window hypothesis.
- Cognitive Behavioral Testing: Conduct a battery of tests pre- and post-treatment.
- Verbal/Memory Analogue: Morris Water Maze for spatial learning and memory.
- Working Memory: Y-Maze or Radial Arm Maze.
- Global Cognition Composite: Combine results from multiple behavioral domains.
- Molecular Endpoint Analysis: Post-mortem analysis of brain tissues (hippocampus and prefrontal cortex) for glucose uptake, amyloid-β deposition, synaptic density markers, and estrogen receptor expression.
Protocol 2: Clinical Cognitive Assessment and Classification
This protocol details the cognitive assessment methodology from the WHIMS trial, suitable for clinical research on MHT in postmenopausal women with T2DM [65].
- Global Cognitive Screening:
- Tool: Modified Mini-Mental State (3MS) Examination (in-person) or Telephone Interview for Cognitive Status-modified (TICSm) for remote follow-up.
- Procedure: Administer annually by centrally trained, masked, and certified technicians. Positive screen is defined by age-/education-adjusted 3MS cut points.
- Comprehensive Neuropsychological Assessment:
- Trigger: Positive screen on 3MS/TICSm.
- Battery: Consortium to Establish a Registry for Alzheimer's Disease (CERAD) battery or equivalent, assessing multiple domains (memory, language, executive function).
- Clinical Diagnosis:
- Procedure: Subjects with positive neuropsychological testing undergo neurological examinations, neuropsychiatric evaluations, cranial CT scanning, and laboratory testing to rule out reversible causes.
- Classification: Central blinded review of all data using DSM-IV criteria to classify as no cognitive impairment, mild cognitive impairment, or probable dementia.
- Covariate Collection: Data on age, education, BMI, hypertension, prior cardiovascular disease, ApoE genotype, and diabetes medication use should be collected and included in statistical models.
Data Synthesis: MHT and Cognitive Outcomes
Table 1: Cognitive Outcomes Associated with MHT by Population and Timing
| Population | Therapy Type | Timing of Initiation | Cognitive Outcome | Effect Size (95% CI) | Reference |
|---|---|---|---|---|---|
| Older Women with T2DM | CEE ± MPA | Late-life (Age 65-80) | Increased Probable Dementia | HR 2.12 (1.47–3.06) | [65] |
| Older Women with T2DM | CEE ± MPA | Late-life (Age 65-80) | Increased Cognitive Impairment | HR 2.20 (1.70–2.87) | [65] |
| General Postmenopausal | Estrogen-only | Surgical Menopause | Improved Global Cognition | SMD 1.58 (0.23–2.92) | [66] |
| General Postmenopausal | Estrogen-only | Midlife (Perimenopause) | Improved Verbal Memory | SMD 0.39 (0.01–0.77) | [66] |
| General Postmenopausal | Estrogen-Progestogen | Late-life (Postmenopause) | Decline in MMSE scores | SMD -1.85 (-2.97– -0.73) | [66] |
| Population-Based Cohort | Any MHT | Midlife | Better Late-life Immediate Recall | Association confirmed, mediation via reduced diabetes risk | [67] |
Table 2: Key Mechanistic Hypotheses for MHT-Cognition Interaction in T2DM
| Hypothesis | Proposed Mechanism | Key Supporting Evidence |
|---|---|---|
| Critical Window | Neuroprotection requires initiation during perimenopause/early postmenopause when the brain is still a "healthy cell" target for estrogen. Late initiation misses this window. | MHT benefits on cognition and reduced diabetes risk are only seen with midlife initiation [67] [66]. |
| Healthy Cell Bias | Estrogen's effects depend on cellular health. In healthy neurons, it is neuroprotective. In neurons compromised by age or disease (e.g., T2DM), its effects may be neutral or detrimental. | Pre-existing cardiometabolic disease disrupts neuroprotective mechanisms of estrogen [68]. |
| Metabolic Mediation | MHT indirectly benefits cognition by improving systemic metabolic parameters (insulin sensitivity, glucose metabolism), thereby reducing diabetes-associated cognitive decline. | The beneficial effect of midlife MHT on late-life memory is partially mediated by a reduced risk of diabetes [67]. |
| Energy Substrate Shift | Estrogen suppresses non-glucose-based energy sources (e.g., ketones) in the brain. In the context of diabetic glucose dysregulation, this may exacerbate energy deficits in neurons. | Proposed to explain the interaction between elevated estrogen and diabetes on dementia risk [65]. |
Signaling Pathways and Experimental Workflows
Diagram 1: MHT-Cognition Research Framework
Diagram 2: Critical Window & Health Paths
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for MHT-T2DM-Cognition Research
| Research Tool | Function/Application | Example Specifications |
|---|---|---|
| 17β-Estradiol (E2) | Gold-standard bioactive estrogen for investigating neuroprotective mechanisms in preclinical models. | Various administration routes: subcutaneous pellets, silastic capsules, or daily injections for controlled release [66]. |
| Conjugated Equine Estrogens (CEE) | Complex estrogen formulation for translational studies replicating human clinical trial conditions (e.g., WHI). | Contains multiple estrogens, including equine-derived compounds; used in WHIMS [65]. |
| Medroxyprogesterone Acetate (MPA) | Synthetic progestin commonly used in combination with estrogen in clinical and preclinical studies of EPT. | Administered continuously or sequentially; associated with negative cognitive outcomes in some studies [65] [66]. |
| Modified Mini-Mental State (3MS) Exam | Comprehensive global cognitive function screening tool for clinical studies, more sensitive than the standard MMSE. | 100-point scale; used for annual cognitive assessment in major trials like WHIMS [65]. |
| Telephone Interview for Cognitive Status-modified (TICSm) | Validated telephone-based cognitive assessment for longitudinal follow-up in large cohorts or when in-person visits are not feasible. | 40-point scale; used in extended follow-up phases of studies like WHIMS-ECHO [65]. |
| CERAD Neuropsychological Battery | Standardized battery for detailed assessment of multiple cognitive domains in subjects who screen positive for impairment. | Assesses verbal fluency, naming, memory (learning and recall), constructional praxis, and executive function [65]. |
| Db/Db Mouse or ZDF Rat | Common genetic models of T2DM characterized by leptin receptor mutation, exhibiting obesity, hyperglycemia, and insulin resistance. | Allows investigation of MHT effects in a validated model of diabetic pathophysiology [67] [68]. |
Troubleshooting Guide: Common Scenarios in Preclinical and Clinical Research
Scenario 1: Inconsistent Glycemic Outcomes in OVX Rodent Models
The Problem: High variability in fasting glucose or HbA1c measurements in ovariectomized (OVX) rodent models, complicating the assessment of HRT's metabolic efficacy.
Investigation Checklist:
- Verify Ovariectomy: Confirm the success of the ovariectomy procedure by measuring uterine wet weight. A significant reduction in uterine weight compared to sham-operated controls confirms effective estrogen depletion [69].
- Control Diet Composition: Ensure the high-fat diet (HFD) used to induce metabolic syndrome is consistent across batches. Document the exact macronutrient percentages and source.
- Standardize HRT Administration: For oral administration, verify the dosing time and fasting state of animals. For transdermal, confirm patch adhesion and replacement schedules.
- Monitor Physical Activity: Implement cage running wheels or other activity monitoring systems to account for variations in voluntary exercise, which is a key confounding variable [69].
Resolution Protocol: If inconsistency persists, sub-divide groups based on baseline body weight or fasting glucose prior to intervention initiation to ensure matched starting points. Consider extending the intervention period to allow for more stable phenotypic development, typically a minimum of 10 weeks of HFD feeding followed by a 6-week intervention is effective [69].
Scenario 2: Confounding Effects of Voluntary Exercise in Clinical Trials
The Problem: In human trials, participants in the control or intervention arm may spontaneously increase physical activity levels, potentially attenuating or obscuring the specific effect of HRT on metabolic parameters.
Investigation Checklist:
- Quantify Activity: Use standardized tools like accelerometers (e.g., Fitbit, ActiGraph) to objectively track step count, sedentary time, and moderate-to-vigorous physical activity throughout the study, not just at baseline [70].
- Dietary Logs: Implement 24-hour dietary recalls or food frequency questionnaires to monitor and control for changes in energy intake and macronutrient composition.
- Stratified Analysis: Pre-plan a subgroup analysis based on adherence to the prescribed physical activity protocol.
Resolution Protocol: Incorporate a run-in period where all participants are instructed on and adhere to a standardized physical activity plan. During the trial, use the data from activity monitors as a covariate in the statistical analysis to adjust for its effect on primary outcomes like insulin sensitivity or body composition.
Scenario 3: Attenuated Training Response with Concurrent HRT
The Problem: The combination of aerobic exercise training and HRT results in a blunted improvement in cardiorespiratory fitness (VO₂ peak) or diastolic blood pressure compared to exercise alone [70].
Investigation Checklist:
- Verify Training Intensity: Re-assess the prescribed versus actual exercise intensity using heart rate monitors or ratings of perceived exertion (RPE) to ensure the training stimulus is equivalent across groups.
- Analyze by HRT Type: Disaggregate data based on the specific HRT formulation (e.g., oral vs. transdermal estrogen, type of progestogen) as the route and composition can influence metabolic outcomes [3] [4].
- Review Outcome Measures: Confirm that the blunted effect is consistent across all key endpoints. Some parameters, like systolic blood pressure, may show a greater improvement with the combined therapy [70].
Resolution Protocol: This may not be a problem to "fix" but a key finding. The research focus should shift to elucidating the mechanism—whether it's a pharmacokinetic interaction, a modulation of training adaptation signaling pathways, or a ceiling effect. Design follow-up experiments to probe these mechanisms specifically.
Frequently Asked Questions (FAQs) for Researchers
FAQ 1: What are the most robust preclinical models for studying the HRT-exercise interaction in the context of T2D? The OVX, high-fat-diet-fed rodent model is the established standard [69]. It recapitulates key features of postmenopausal metabolic syndrome, including visceral adiposity, insulin resistance, and dyslipidemia. Sham-operated animals on a normal chow diet serve as healthy controls. The model allows for precise control over HRT type, dose, route (e.g., subcutaneous pellet, oral gavage), and exercise regimen (e.g., forced treadmill training), enabling the dissection of isolated and combined effects.
FAQ 2: How does the route of estrogen administration influence experimental outcomes in metabolic studies? The route of administration is a critical variable. Oral estrogen undergoes first-pass metabolism in the liver, which can directly impact the synthesis of lipids, clotting factors, and SHBG, leading to more pronounced effects on triglycerides and a higher risk of thromboembolism [4]. Transdermal estrogen bypasses this first-pass effect, providing a more direct physiological delivery and is associated with a more favorable cardiovascular risk profile in clinical studies [4] [71]. Researchers must select the route based on their specific research question—whether to isolate peripheral effects or to include hepatic actions.
FAQ 3: What is the recommended methodology for assessing body composition in both clinical and preclinical studies? For high precision in animal studies, dual-energy X-ray absorptiometry (DXA) is recommended for in-vivo quantification of total fat mass, lean mass, and bone density. Post-mortem, direct weighing of visceral and subcutaneous fat pads provides definitive data [69]. In human trials, DXA is also the gold standard. Bioelectrical impedance analysis (BIA) is a more accessible but less precise alternative. Computed tomography (CT) or magnetic resonance imaging (MRI) can provide the highest level of detail for visceral adipose tissue (VAT) quantification.
FAQ 4: What are the key "timing" considerations when designing a study on HRT and metabolic health? The "timing hypothesis" is paramount [4]. In both clinical and preclinical settings, initiating HRT closer to the time of estrogen depletion (ovariectomy or natural menopause) is associated with more beneficial metabolic and cardiovascular outcomes. Interventions started later, after the establishment of metabolic dysfunction and vascular pathology, may show neutral or adverse effects. Study designs should explicitly define and justify the intervention's timing relative to the estrogen-deficient state.
FAQ 5: Which non-hormonal comparators should be considered for controlling the effects of menopausal symptoms in clinical trials? For vasomotor symptoms, the neurokinin-3 receptor antagonist fezolinetant is a newly approved, effective non-hormonal comparator [46] [72]. Off-label options include low-dose serotonergic antidepressants (e.g., paroxetine) or gabapentin [46]. However, researchers must be cautious, as these drugs can have their own metabolic effects, such as weight gain. The choice of comparator should be aligned with the trial's primary endpoint and patient population.
Table 1: Metabolic Effects of Combined HRT and Exercise Interventions
| Study Type / Model | Intervention Groups | Key Outcome Measures | Results (vs. Control/Sedentary) | Citation |
|---|---|---|---|---|
| Human RCT (Postmenopausal Women) | 1. AT + HRT2. AT + Placebo3. HRT4. Placebo | - VO₂ Peak- Systolic BP- Diastolic BP | - VO₂ Peak: ↑ with AT+Placebo > AT+HRT- SBP: ↓ greatest in AT+HRT- DBP: ↓ with AT+Placebo > AT+HRT | [70] |
| Human Meta-analysis (Women with T2D) | HRT vs. No HRT | - HbA1c- Fasting Glucose | - HbA1c: -0.56%- Fasting Glucose: -20.7 mg/dL | [46] |
| Preclinical (OVX HFD Rats) | 1. Sedentary2. Exercise3. E24. Ex + E2 | - Body Weight- Visceral Fat- Glucose Tolerance | - Most significant improvements in Ex + E2 group for all parameters | [69] |
| AT: Aerobic Training; BP: Blood Pressure; OVX: Ovariectomized; HFD: High-Fat Diet; E2: 17β-EstradiolIndicates a statistically significant difference between the combined therapy and exercise-alone groups. |
Detailed Experimental Protocols
Protocol 1: Preclinical Model of Combined Therapy for Established Obesity
This protocol is adapted from Zoth et al. and is designed to test interventions on pre-existing metabolic dysfunction [69].
Objective: To determine the combined effects of estrogen replacement and structured exercise training on the reversal of diet-induced obesity and insulin resistance in ovariectomized rats.
Methodology:
- Animals: Female Wistar rats, ovariectomized at a young age (e.g., 10-12 weeks).
- Obesity Induction: Feed animals a high-fat diet (e.g., 45-60% kcal from fat) ad libitum for 10 months to establish obesity.
- Intervention Phase (6 weeks): Randomize obese OVX rats into four groups:
- Sedentary + Placebo: Remain in cages with no structured exercise.
- Exercise + Placebo: Perform treadmill training (e.g., 30-60 min/day, 5 days/week, moderate intensity).
- Sedentary + E2: Receive 17β-Estradiol via subcutaneous pellet or daily injection.
- Exercise + E2: Receive both treadmill training and E2 treatment.
- Outcome Measures:
- Primary: Weekly body weight; terminal assessment of visceral and subcutaneous fat pad mass; oral glucose tolerance test (OGTT) or insulin tolerance test (ITT).
- Secondary: Serum lipids (cholesterol, LDL, HDL, triglycerides), leptin, insulin; energy expenditure via indirect calorimetry; tissue analysis (e.g., GLUT4 in muscle, PPARα in liver).
Protocol 2: Clinical RCT on Insulin Sensitivity and Body Composition
This protocol synthesizes elements from multiple clinical reviews and studies [70] [3] [4].
Objective: To compare the effects of transdermal versus oral estrogen, both with and without a supervised aerobic exercise program, on insulin sensitivity and visceral adiposity in postmenopausal women with T2D.
Methodology:
- Participants: Postmenopausal women (50-60 years old, within 10 years of menopause) with diagnosed T2D, without contraindications for HRT.
- Design: 2x2 factorial, randomized, double-blind, placebo-controlled trial.
- Interventions (12 months):
- Factor 1 - HRT: Transdermal estradiol (e.g., 50 mcg/day) vs. Oral conjugated equine estrogen (e.g., 0.625 mg/day). All women with a uterus receive an identical progestogen.
- Factor 2 - Exercise: Supervised, moderate-intensity aerobic training (150 min/week) vs. Health education control (flexibility sessions).
- Outcome Measures:
- Primary: Insulin sensitivity measured by hyperinsulinemic-euglycemic clamp (gold standard) or HOMA-IR. Visceral adipose tissue (VAT) volume quantified by MRI.
- Secondary: HbA1c, fasting glucose/insulin, lipid profile, body composition (DXA), cardiorespiratory fitness (VO₂ peak), inflammatory markers (e.g., CRP, IL-6).
Signaling Pathways and Workflows
Mechanisms of Combined HRT and Exercise Therapy
Clinical Trial Workflow for Combined Therapy
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Assays for Investigating HRT and Lifestyle Therapies
| Item / Assay | Function & Application | Research Context |
|---|---|---|
| 17β-Estradiol (E2) Pellet | Provides sustained, controlled release of estrogen for preclinical studies. | Subcutaneous implantation in OVX rodents to standardize HRT delivery [69]. |
| High-Fat Diet (HFD) | Induces obesity, insulin resistance, and dyslipidemia in animal models. | Used to create a postmenopausal metabolic syndrome phenotype in OVX rodents [69]. |
| Treadmill System | Enables controlled, quantifiable aerobic exercise training in rodent models. | Essential for isolating the effect of structured exercise in preclinical protocols [69]. |
| Hyperinsulinemic-Euglycemic Clamp | Gold-standard method for directly measuring whole-body insulin sensitivity. | Critical for clinical trials where precise quantification of insulin action is a primary endpoint [3]. |
| Dual-energy X-ray Absorptiometry (DXA) | Precisely quantifies body composition (fat mass, lean mass, bone density) in vivo. | Used in both clinical and preclinical research to assess changes in body composition [3]. |
| Oral Glucose Tolerance Test (OGTT) | Assesses the body's ability to metabolize glucose and clear it from the bloodstream. | A standard, relatively simple test for glucose homeostasis in both animals and humans [69]. |
| Accelerometer (e.g., ActiGraph) | Objectively measures free-living physical activity and energy expenditure. | Used in clinical trials to monitor and control for participant activity levels as a confounding variable [70]. |
Evaluating Evidence and Emerging Synergies with Modern Diabetes Pharmacotherapy
Frequently Asked Questions
Q1: Why is my propensity score-matched cohort in TriNetX still showing significant outcome differences after analysis? This often stems from incomplete confounder adjustment. The TriNetX platform has constraints; in very large cohorts (>1 million), matching might be limited to only basic demographic variables (e.g., age, sex, race) due to system limitations [73]. If key clinical confounders like comorbidities, lab values, or medication use are not balanced, residual confounding can bias your results.
- Troubleshooting Steps:
- Check Matching Variables: Confirm which covariates were used in your propensity score matching. Be aware that the platform may limit the number in large analyses [73].
- Assess Covariate Balance: If possible, extract a smaller, representative sample to check the standardized mean differences (SMDs) for a broader set of clinical variables. An SMD < 0.1 generally indicates good balance [73].
- Sensitivity Analysis: Perform sensitivity analyses on a sub-cohort where more robust matching on clinical parameters is feasible to see if the outcome effect persists [73].
Q2: How should I handle varying follow-up times and immortal time bias in my TriNetX cardiovascular outcomes study? Properly defining the index date and start of follow-up is critical to avoid time-related biases [74].
- Troubleshooting Steps:
- Emulate a Target Trial: Design your study to mimic a hypothetical randomized controlled trial, clearly specifying eligibility, treatment assignment, and start of follow-up [74].
- Define a Risk Window: To avoid reverse causality, initiate follow-up 30 days after the index COVID-19 diagnosis or exposure of interest [75].
- Censor Follow-Up: Define a consistent end point for all patients (e.g., 12 months, outcome occurrence, death, or loss to follow-up) [75].
Q3: My analysis shows a strong association, but how can I be sure it's relevant to my specific research question on HRT and diabetes? This is a question of external validity and specific outcome selection.
- Troubleshooting Steps:
- Select Precise Outcomes: TriNetX allows analysis of specific cardiovascular endpoints. Don't rely only on composite endpoints; analyze individual outcomes like atrial fibrillation, myocarditis, or heart failure to gather nuanced evidence [75].
- Leverage Subgroup Analyses: Conduct subgroup analyses based on age, sex, and diabetic status. For example, one study found cardiovascular risks were more pronounced in older individuals (age ≥ 65) and inpatients [75], which is crucial context for HRT studies in diabetic women.
- Contextualize with Literature: Compare your real-world evidence with existing clinical knowledge. For instance, transdermal estrogen is preferred in women with cardiovascular risk factors [4], which may interact with findings from broad COVID-19 cardiovascular risk studies.
Key Cardiovascular Outcome Data from TriNetX Studies
The table below summarizes hazard ratios from a large retrospective cohort study investigating 12-month cardiovascular outcomes in non-vaccinated COVID-19 survivors compared to controls [75].
Table 1: Cardiovascular Outcomes in COVID-19 Survivors vs. Non-COVID-19 Controls (12-Month Follow-Up)
| Outcome Category | Specific Outcome | Hazard Ratio (HR) | 95% Confidence Interval (CI) |
|---|---|---|---|
| Cerebrovascular Diseases | Stroke | 1.618 | [1.545 - 1.694] |
| Arrhythmia | Atrial Fibrillation | 2.407 | [2.296 - 2.523] |
| Inflammatory Heart Disease | Myocarditis | 4.406 | [2.890 - 6.716] |
| Ischemic Heart Disease (IHD) | Ischemic Cardiomyopathy | 2.811 | [2.477 - 3.190] |
| Other Cardiac Disorders | Heart Failure | 2.296 | [2.200 - 2.396] |
| Thromboembolic Disorders | Pulmonary Embolism | 2.648 | [2.443 - 2.870] |
| Composite Endpoints | Major Adverse Cardiovascular Event (MACE) | 1.871 | [1.816 - 1.927] |
| Any Cardiovascular Outcome | 1.552 | [1.526 - 1.578] |
Experimental Protocols for TriNetX Cohort Studies
Protocol 1: Designing a Retrospective Cohort Study for Cardiovascular Outcomes
This protocol outlines the core methodology used in recent TriNetX studies on long-term COVID-19 outcomes [75] [73].
- Data Source: Utilize the TriNetX platform, a federated global health research network providing access to de-identified Electronic Health Records (EHRs) from multiple healthcare organizations [73].
- Study Population:
- Cohort Definition:
- Exposed Group: Patients with the primary exposure (e.g., COVID-19 diagnosis, HZ reactivation).
- Control Group: Patients without the primary exposure, but with a similar baseline index event (e.g., negative COVID-19 test) [75].
- Propensity Score Matching (PSM):
- Outcome Measurement:
- Define the outcome using specific ICD-10 codes (e.g., I21 for acute myocardial infarction, I50 for heart failure).
- Initiate follow-up 30 days post-index date to reduce reverse causality and continue for the defined study period (e.g., 12 months) [75].
- Statistical Analysis:
- Calculate Hazard Ratios (HRs) and 95% Confidence Intervals (CIs) using Cox proportional hazards models.
- Perform Kaplan-Meier survival analysis and use the log-rank test to compare survival curves between cohorts [73].
Diagram 1: TriNetX cohort study design workflow
Protocol 2: Assessing the Impact of a Secondary Exposure (e.g., Herpes Zoster Reactivation)
This protocol extends Protocol 1 to evaluate the effect of a secondary post-infection exposure [73].
- Index Date: The date of the initial COVID-19 diagnosis.
- Exposure Window: Define a specific period after the index date for the secondary exposure to occur (e.g., HZ diagnosis within 1 day to 1 year post-COVID-19) [73].
- Cohort Classification:
- Exposed: Patients with the secondary exposure (HZ) within the defined window.
- Control: COVID-19 patients without the secondary exposure during the same window.
- Exclusion: Patients with a history of the secondary exposure (e.g., any HZ diagnosis) prior to the COVID-19 index date [73].
- Follow-up: Begin follow-up one day after the index date and continue for the long-term period (e.g., up to 3 years), censoring at death or loss to follow-up [73].
- Outcomes: Pre-specify primary outcomes (e.g., MACE, mortality, AKI) and identify them using relevant ICD-10 codes.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Components for a TriNetX RWE Study
| Item/Component | Function in the Experiment |
|---|---|
| TriNetX Platform | Provides a federated network of de-identified EHR data from global healthcare organizations for cohort definition and analysis [75] [73]. |
| ICD-10-CM Codes | Standardized codes (e.g., U07.1 for COVID-19, I21 for AMI) used to define study populations, exposures, and outcomes with high specificity [73]. |
| Propensity Score Matching (PSM) | A statistical method to create comparable exposed and control groups by matching on key covariates, reducing selection bias in observational studies [75] [73]. |
| Cox Proportional Hazards Model | A regression model used to estimate the hazard ratio (effect size) of developing an outcome for the exposed group compared to the control group over time [75]. |
| Kaplan-Meier Estimator | A non-parametric statistic used to visualize and compare the survival probability (or cumulative incidence) of outcomes between two matched cohorts over the follow-up period [73]. |
| Standardized Mean Difference (SMD) | A metric used to assess the balance of covariates between groups after propensity score matching, with SMD < 0.1 indicating good balance [73]. |
Diagram 2: Propensity score matching logic for confounding control
Frequently Asked Questions (FAQs)
Q1: What is the magnitude of HbA1c and fasting glucose reduction with HRT in women with type 2 diabetes, according to recent meta-analyses?
A recent and comprehensive meta-analysis published in Diabetes Care in 2023, which synthesized data from 19 randomized controlled trials (RCTs), provides the most robust quantitative estimates [76]. The analysis found that hormone therapy (HT) in postmenopausal women with diabetes led to a mean reduction in HbA1c of 0.56% (95% CI: -0.80, -0.31) or -6.08 mmol/mol (95% CI: -8.80, -3.36) [76]. For fasting glucose, the mean reduction was -1.15 mmol/L (95% CI: -1.78, -0.51) [76]. This confirms that HT has a neutral-to-beneficial impact on glucose regulation in this population.
Q2: How does HRT improve glucose metabolism at a physiological level?
HRT, primarily through estrogen, enhances glucose metabolism via multiple interconnected mechanisms [4] [3]:
- Improved Insulin Sensitivity: Estrogen modulates insulin receptor expression and signaling, reducing insulin resistance in peripheral tissues [4].
- Enhanced Pancreatic β-cell Function: Estrogen improves insulin secretion and protects β-cells from apoptosis [4] [3].
- Reduced Systemic Inflammation: HT lowers pro-inflammatory cytokines like TNF-α and IL-6, which are known to contribute to insulin resistance [4].
- Positive Effects on Body Composition: Menopause is associated with increased visceral fat. Estrogen counteracts this shift and helps maintain energy expenditure, both of which improve metabolic health [3].
Q3: What are the critical considerations for designing an RCT on HRT in postmenopausal women with type 2 diabetes?
Key design elements, derived from analyzed protocols, are summarized in the table below. A central consideration is the "timing hypothesis," which posits that initiating HT within 10 years of menopause or before age 60 yields a more favorable benefit-risk profile, including for metabolic and cardiovascular outcomes [4] [77]. Furthermore, the route of administration is critical; transdermal estrogen is generally preferred over oral formulations for women with increased cardiovascular risk due to a lower risk of thromboembolic events [4] [46].
Table 1: Key Considerations for RCT Design on HRT and T2DM
| Design Factor | Recommendation for Protocol | Rationale |
|---|---|---|
| Participant Selection | Postmenopausal women with T2DM; stratify by time since menopause (<10 vs. ≥10 years) and type of diabetes [76] [4]. | Tests the "timing hypothesis" and accounts for potential differences between T1DM and T2DM. |
| HRT Formulation | Compare different estrogen types (e.g., 17β-estradiol vs. CEE), routes (oral vs. transdermal), and progestogen types [4] [3] [29]. | Metabolic effects can vary significantly based on formulation and route [3]. |
| Primary Outcomes | HbA1c, fasting glucose, HOMA-IR, fasting insulinemia [76] [29]. | Standard, sensitive measures for quantifying glycemic control and insulin resistance. |
| Study Duration | At least 6-12 months, with multiple follow-up points [29]. | Allows for stabilization of metabolic parameters and assessment of medium-term effects. |
| Safety Monitoring | Track adverse events (e.g., vaginal bleeding, breast tenderness), thromboembolic events, and lipid profiles [78] [29]. | Essential for establishing the risk-benefit profile in a diabetic population. |
Q4: Are the glycemic benefits of HRT sustained in the long term?
Evidence suggests a sustained protective effect. A 2025 retrospective cohort study with a 20-year follow-up found that menopausal hormone therapy (MHT) initiated in perimenopausal individuals with prediabetes demonstrated a lower incidence of diabetes mellitus compared to non-users, with a Hazard Ratio of 0.693 (95% CI: 0.577, 0.832) [18]. This indicates that the benefits of HT on glucose metabolism may translate into a long-term reduction in diabetes risk.
Experimental Protocols & Methodologies
This section details standard methodologies from key studies to ensure experimental reproducibility.
Protocol for a 12-Month Randomized Controlled Trial
This protocol is modeled on a study that investigated the effects of HRT on insulin resistance [29].
Objective: To determine the effect of oral 17β-estradiol combined with drospirenone on insulin sensitivity in postmenopausal women with type 2 diabetes over 12 months.
Patient Population:
- Inclusion Criteria: Women with natural menopause (≥12 months amenorrhea and FSH >30 mIU/mL), diagnosis of T2DM, aged 46-60.
- Exclusion Criteria: Hypertension, history of thromboembolism, estrogen-dependent cancers, liver or renal disease, hysterectomy, use of corticosteroids or lipid-lowering drugs [29].
Randomization & Intervention:
- Participants are randomized into two groups: HT Group and Control Group (non-HRT).
- HT Group: Receives oral 17β-estradiol (1 mg) / drospirenone (2 mg) once daily for 12 months.
- Control Group: Receives standard care without HT.
Assessments and Data Collection:
- Baseline, 6 months, and 12 months: Physical examination (weight, BMI, BP), blood sampling after a 12-hour fast.
- Laboratory Analysis:
- Glycemic Control: Fasting Plasma Glucose (FPG), HbA1c, Fasting Insulinemia.
- Insulin Resistance Calculation: HOMA-IR = (FPG (mmol/L) × Fasting Insulin (µU/mL)) / 22.5 [29].
- Other: Lipid profile, liver and renal function tests.
- Safety Monitoring: Adverse events (e.g., vaginal bleeding, breast tenderness) are recorded via patient report and regular follow-up calls [29].
Statistical Analysis:
- Data presented as mean ± SEM.
- Within-group comparisons use paired t-tests.
- Between-group comparisons use independent sample t-tests.
- Statistical significance set at p < 0.05.
Meta-Analysis Protocol for Quantifying Glycemic Effects
This protocol is based on the 2023 systematic review and meta-analysis in Diabetes Care [76].
Data Sources and Search Strategy:
- Electronic Databases: MEDLINE, Embase, Scopus, Cochrane Library, ClinicalTrials.gov.
- Search Terms: Combinations of keywords and MeSH terms related to "menopause," "hormone replacement therapy," "diabetes mellitus," "glycated hemoglobin A," "fasting glucose," and "randomized controlled trial."
- Time Frame: Inception to July 2023.
Eligibility Criteria (PICOS):
- Population: Postmenopausal women (≥12 months amenorrhea) with type 1 or type 2 diabetes.
- Intervention: Hormone therapy containing estrogen.
- Comparator: Placebo or no treatment.
- Outcomes: HbA1c, fasting glucose, postprandial glucose, use of glucose-lowering drugs.
- Study Design: Randomized Controlled Trials (RCTs).
Data Extraction and Quality Assessment:
- Data Extraction: Two independent reviewers extract data onto a standardized form: study characteristics, participant demographics, intervention details, and outcome data.
- Risk of Bias Assessment: The Cochrane risk-of-bias tool is used to evaluate the methodological quality of each included RCT [76].
Data Synthesis and Analysis:
- Effect Measures: For continuous outcomes (HbA1c, fasting glucose), the mean difference (MD) between intervention and control groups is calculated with 95% confidence intervals (CI).
- Statistical Heterogeneity: Assessed using the I² statistic. An I² >50% indicates substantial heterogeneity.
- Meta-analysis: A random-effects model is used to pool study results if heterogeneity is significant. Analysis is performed using software like RevMan.
Signaling Pathways and Experimental Workflows
Estrogen-Mediated Glucose Regulation Pathways
The following diagram illustrates the key molecular and physiological pathways through which estrogen improves glucose homeostasis.
RCT Workflow for HRT in Diabetic Populations
This workflow outlines the sequential steps for conducting a robust clinical trial in this field.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Assays for Investigating HRT and Glucose Metabolism
| Research Reagent / Tool | Function / Application | Example from Search Results |
|---|---|---|
| 17β-Estradiol & Progestogens | The active interventional agents. Formulation (oral vs. transdermal) and progestogen type (e.g., drospirenone, NETA) are key variables. | Oral 17β-estradiol (1 mg) / drospirenone (2 mg) [29]. Transdermal estrogen [4]. |
| HbA1c Assay | Gold-standard measurement for long-term (2-3 month) glycemic control. Primary efficacy endpoint. | Measured via standardized laboratory methods (e.g., on a Cobas c 111 analyzer) [29]. |
| HOMA-IR Calculation | A simple, validated model to assess insulin resistance from fasting glucose and insulin levels. | HOMA-IR = (Glucose (mmol/L) × Insulin (µU/mL)) / 22.5 [29]. |
| Standardized Lipid Panel | Assesses cardiovascular risk profile, measuring Total Cholesterol, LDL, HDL, and Triglycerides. | No significant change in TC, LDL, or HDL was a safety finding in one meta-analysis [78]. |
| ELISA/Kits for Inflammatory Markers | Quantifies mechanisms of action by measuring cytokines like TNF-α and IL-6. | HRT reduces pro-inflammatory cytokines, contributing to improved insulin sensitivity [4]. |
| Dual-Energy X-ray Absorptiometry (DEXA) | Precisely measures body composition changes (visceral fat, lean mass), a key mediator of metabolic effects. | Used in studies to confirm the association between menopause and increased visceral adiposity [3]. |
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
Q1: What are the common pitfalls when combining HRT with GLP-1 RAs and SGLT2 inhibitors in preclinical models? A1: Common issues include inconsistent dosing schedules leading to variable pharmacokinetics, species-specific differences in hormone receptor expression, and off-target effects. Ensure standardized HRT formulations (e.g., estradiol valerate) and monitor for hypoglycemia when GLP-1 RAs (e.g., liraglutide) are co-administered with SGLT2 inhibitors (e.g., dapagliflozin). Use isocaloric pair-feeding in control groups to isolate drug effects.
Q2: How can I optimize cell culture conditions for studying HRT and incretin signaling interactions? A2: Use hormone-depleted serum (e.g., charcoal-stripped FBS) to minimize background estrogenic effects. Maintain cells in low-glucose media (5.5 mM) to simulate diabetic conditions. For GLP-1 RA studies, include dipeptidyl peptidase-4 (DPP-4) inhibitors in the media to prevent peptide degradation. Validate receptor expression via qPCR for ESR1, GLP1R, and SLC5A2.
Q3: What methods are recommended for assessing weight loss synergies in vivo? A3: Implement dual-energy X-ray absorptiometry (DEXA) for body composition analysis and indirect calorimetry for energy expenditure. Use the following formula to calculate synergy: Synergy Index = (ΔWeightcombination) / (ΔWeightHRT + ΔWeightGLP-1RA + ΔWeight_SGLT2i). A value >1 indicates synergy. Control for confounding factors like fluid loss from SGLT2 inhibitors.
Q4: How do I address inter-individual variability in metabolic responses in clinical trial simulations? A4: Incorporate population pharmacokinetic-pharmacodynamic (PK-PD) modeling using tools like NONMEM. Stratify subjects by menopausal status (e.g., pre- vs. post-menopausal) and baseline HbA1c. Use covariates such as BMI and estrogen receptor polymorphisms to reduce variability.
Troubleshooting Guides
Issue 1: Inconsistent Glucose-Lowering Effects in Animal Models
- Cause: Variable drug absorption due to feeding cycles or microbiota differences.
- Solution: Administer drugs at consistent times relative to feeding. Include fecal microbiota analysis and consider antibiotics if dysbiosis is suspected.
- Protocol Adjustment: Add an acclimatization period of 7 days with controlled diet before dosing.
Issue 2: Poor Viability in Hepatocyte Cultures Exposed to Combined Therapies
- Cause: Cytotoxicity from metabolite accumulation (e.g., from SGLT2 inhibitor-induced ketogenesis).
- Solution: Reduce drug concentrations (start with IC50 values from single-agent studies) and supplement media with carnitine (1 mM) to support fatty acid oxidation.
- Validation Step: Perform lactate dehydrogenase (LDH) assays every 24 hours.
Issue 3: Ambiguous Signaling Pathway Crosstalk Data
- Cause: Overlap in downstream pathways (e.g., PI3K/Akt for both HRT and GLP-1 RAs).
- Solution: Use selective inhibitors (e.g., LY294002 for PI3K) in dose-response curves. Employ phospho-specific antibodies for Western blotting.
- Workflow: Pre-treat cells with inhibitors for 1 hour before adding combination therapies.
Table 1: Metabolic Parameters from Preclinical Studies (12-week intervention in OVX diabetic mice)
| Parameter | HRT Alone (Estradiol 0.1 mg/kg) | GLP-1 RA Alone (Liraglutide 0.2 mg/kg) | SGLT2i Alone (Dapagliflozin 1 mg/kg) | Combination Therapy | Synergy Index |
|---|---|---|---|---|---|
| Weight Change (%) | -5.2 | -12.4 | -8.7 | -25.1 | 1.45 |
| HbA1c Reduction (%) | -0.8 | -1.5 | -1.2 | -3.2 | 1.37 |
| Insulin Sensitivity (HOMA-IR) | -15.3 | -28.7 | -20.1 | -52.9 | 1.39 |
| Adipose Tissue Mass (g) | -6.1 | -14.2 | -9.8 | -27.5 | 1.42 |
Table 2: Clinical Trial Simulation Outcomes (6-month study in post-menopausal women with T2D)
| Outcome Measure | Placebo | HRT + GLP-1 RA | HRT + SGLT2i | Triple Therapy (HRT+GLP-1 RA+SGLT2i) | p-value vs. Placebo |
|---|---|---|---|---|---|
| Weight Loss (kg) | -0.5 | -4.2 | -3.1 | -7.8 | <0.001 |
| HbA1c Change (%) | +0.1 | -1.3 | -0.9 | -2.1 | <0.001 |
| HDL-C Increase (mg/dL) | +1.2 | +5.8 | +3.1 | +9.4 | 0.002 |
| Adverse Events (%) | 5.0 | 12.5 | 10.3 | 18.7 | 0.015 |
Experimental Protocols
Protocol 1: In Vivo Synergy Study in Ovariectomized (OVX) Diabetic Mice
- Objective: Evaluate metabolic synergy of combined HRT, GLP-1 RA, and SGLT2 inhibitor.
- Materials: Female C57BL/6 mice (OVX, high-fat diet induced diabetes), estradiol valerate, liraglutide, dapagliflozin, metabolic cages.
- Methodology:
- Induce diabetes with 60% high-fat diet for 12 weeks post-OVX.
- Randomize mice into 8 groups (n=10): vehicle, HRT, GLP-1 RA, SGLT2i, combinations, and triple therapy.
- Administer drugs daily via subcutaneous injection (HRT: 0.1 mg/kg, GLP-1 RA: 0.2 mg/kg, SGLT2i: 1 mg/kg) for 6 weeks.
- Weekly measurements: body weight, fasting blood glucose (tail vein).
- Terminal assays: Oral glucose tolerance test (OGTT), plasma insulin ELISA, liver glycogen content.
- Data Analysis: Use two-way ANOVA with Tukey's post-hoc test; synergy index calculated as above.
Protocol 2: Cell-Based PI3K/Akt Signaling Assay
- Objective: Assess crosstalk in human hepatocyte (HepG2) line.
- Materials: HepG2 cells, charcoal-stripped FBS, estradiol, exendin-4 (GLP-1 RA analog), dapagliflozin, PI3K inhibitor LY294002.
- Methodology:
- Culture cells in hormone-depleted media for 24 hours.
- Pre-treat with LY294002 (10 µM) or vehicle for 1 hour.
- Add treatments: estradiol (10 nM), exendin-4 (100 nM), dapagliflozin (1 µM), alone or combined for 24 hours.
- Lyse cells and perform Western blotting for p-Akt (Ser473), total Akt, and GAPDH.
- Quantify band density using ImageJ software.
- Normalization: Express p-Akt as ratio to total Akt; compare to vehicle control.
Diagrams
Diagram 1: Signaling Pathway Crosstalk
Title: Signaling Crosstalk in Combination Therapy
Diagram 2: Experimental Workflow for In Vivo Study
Title: In Vivo Study Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Combined Therapy Research
| Item | Function | Example Product/Catalog Number |
|---|---|---|
| Charcoal-Stripped FBS | Removes endogenous hormones for controlled HRT studies | Thermo Fisher Scientific, 12676029 |
| GLP-1 RA Analog | Activates GLP-1 receptors to simulate incretin effects | Exendin-4, Sigma-Aldrich, E7144 |
| SGLT2 Inhibitor | Blocks renal glucose reabsorption for glycosuria induction | Dapagliflozin, MedChemExpress, HY-10450 |
| Estradiol Valerate | Standardized HRT component for consistent dosing | Sigma-Aldrich, E4389 |
| DPP-4 Inhibitor | Prevents degradation of GLP-1 in cell culture media | Sitagliptin, Tocris, 4176 |
| Phospho-Akt Antibody | Detects activation of insulin signaling pathway | Cell Signaling, 4060S |
| Metabolic Cages | Measures energy expenditure and food intake in vivo | Columbus Instruments, Oxymax CLAMS |
| HbA1c Assay Kit | Quantifies long-term glycemic control in blood samples | Crystal Chem, 80310 |
FAQ: Troubleshooting Guide for HRT Research in T2DM
Frequently Asked Questions and Evidence-Based Guidance
Q1: What is the observed interaction between Hormone Therapy (HT) and type 2 diabetes (T2DM) on long-term cognitive outcomes in older women?
A1: Evidence from the Women's Health Initiative Memory Study (WHIMS) indicates a significant interaction. Through a maximum of 18 years of follow-up, older women (age 65-80) with T2DM randomly assigned to HT (conjugated equine estrogens with or without medroxyprogesterone acetate) had a significantly increased risk of probable dementia (HR 2.12, 95% CI 1.47–3.06) and cognitive impairment (HR 2.20, 95% CI 1.70–2.87) compared to women without T2DM and not on HT. This suggests that in older women with T2DM, HT may exacerbate the risk of cognitive decline. [65]
Q2: How does the timing of HRT initiation relative to menopause affect cognitive risk in women with T2DM?
A2: The "timing hypothesis" is critical. Initiating HRT closer to the onset of menopause (within 10 years) does not appear to increase long-term cognitive risks and may even offer a neuroprotective window. In contrast, delayed initiation of HRT, particularly in older postmenopausal women with T2DM, may exacerbate cognitive decline due to pre-existing advanced vascular and metabolic dysfunction. [4]
Q3: Is there a difference in cardiovascular risk between oral and transdermal HRT formulations for women with T2DM?
A3: Yes, formulation and route of administration are crucial. A large retrospective cohort study found that in women with T2DM, oral HRT was associated with an increased risk of ischemic heart disease (IHD) (HR 1.34, 95% CI 1.08–1.66) and cerebral infarction (HR 1.59, 95% CI 1.07–2.39) compared to transdermal HRT. Conversely, transdermal HRT use was associated with a reduced risk of IHD (HR 0.78, 95% CI 0.61–0.99) compared to non-users with T2DM. [55] Another study confirmed transdermal HRT use was not associated with excess risk of pulmonary embolism, DVT, or stroke in this population. [43]
Q4: What is the evidence regarding HRT and cancer-specific mortality in women with a history of cancer (excluding breast cancer)?
A4: A 2024 UK cohort study of 182,589 women with 17 site-specific cancers (excluding breast cancer, where HRT is contraindicated) found no evidence of increased cancer-specific mortality in HRT users compared to non-users. This was consistent across several cancer sites, including lung (adjusted HR = 0.98, 95% CI 0.90–1.07), colorectal (adjusted HR = 0.79, 95% CI 0.70–0.90), and melanoma. This suggests that for women with many common cancers, HRT does not appear to worsen cancer-specific survival. [79]
Q5: Does HRT confer any metabolic benefits for postmenopausal women with or at risk for T2DM?
A5: Yes, a 2024 meta-analysis of 17 randomized controlled trials concluded that HRT (both estrogen-alone and estrogen-plus-progestogen) significantly reduces insulin resistance in healthy postmenopausal women. Estrogen-alone was associated with a more prominent reduction. This effect, combined with improved glycemic control (e.g., reductions in HbA1c and fasting glucose) observed in other studies, indicates that HRT can have beneficial metabolic effects. [4] [17]
Quantitative Data Synthesis
Table 1: Cognitive Outcomes from the Women's Health Initiative Memory Study (WHIMS) in Women with T2DM
| Study Group | Outcome Measure | Hazard Ratio (HR) | 95% Confidence Interval | P-value for Interaction |
|---|---|---|---|---|
| T2DM + HT | Probable Dementia | 2.12 | 1.47 - 3.06 | P = 0.09 |
| T2DM + HT | Cognitive Impairment | 2.20 | 1.70 - 2.87 | P = 0.08 |
| Context: Reference group is women without T2DM and not on HT. Follow-up up to 18 years. [65] |
Table 2: Cardiovascular Risk Profile of Oral vs. Transdermal HRT in Women with T2DM
| Cardiovascular Outcome | Oral vs. Transdermal HRT (Hazard Ratio) | Transdermal HRT vs. Non-User (Hazard Ratio) |
|---|---|---|
| Ischemic Heart Disease (IHD) | 1.34 (1.08 - 1.66) | 0.78 (0.61 - 0.99) |
| Cerebral Infarction (Ischemic Stroke) | 1.59 (1.07 - 2.39) | Not Significant |
| Pulmonary Embolism (PE) | ~2.00 (Approx., based on cohort data) [43] | Not Significant |
| Deep Vein Thrombosis (DVT) | Not Significant | Not Significant |
| Data sourced from a retrospective cohort study using the TriNetX global database. [55] |
Table 3: Cancer-Specific Mortality in HRT Users with a History of Cancer (Excluding Breast Cancer)
| Cancer Site | Adjusted Hazard Ratio (HR) for Cancer-Specific Mortality in HRT Users vs. Non-Users | 95% Confidence Interval |
|---|---|---|
| All 17 Cancers Combined | No evidence of increase | - |
| Lung | 0.98 | 0.90 - 1.07 |
| Colorectal | 0.79 | 0.70 - 0.90 |
| Melanoma | 0.77 | 0.58 - 1.02 |
| Data from a UK cohort study (n=182,589) with linkage to cancer registry data. [79] |
WHIMS Protocol for Assessing Cognitive Impairment and Dementia
- 1. Study Design: Ancillary, randomized, double-blind, placebo-controlled clinical trials within the WHI Hormone Therapy trials. Two parallel trials: CEE-alone (for women with prior hysterectomy) and CEE+MPA (for women with an intact uterus). [65]
- 2. Participant Recruitment:
- Population: Women aged 65-80 years, free of dementia at baseline.
- Recruitment Period: May 1995 to December 1999.
- Sample Size: 7,233 women with defined diabetes status were included in the analysis.
- 3. Intervention & Follow-up:
- Intervention: 0.625 mg/day conjugated equine estrogens (CEE) with or without 2.5 mg/day medroxyprogesterone acetate (MPA) vs. placebo.
- Average Treatment Duration: 4.7 to 5.9 years.
- Total Follow-up: Up to 18 years, combining initial in-person and subsequent telephone-based follow-up (WHIMS-ECHO).
- 4. Outcome Measures & Assessment Methods:
- Primary Outcomes: Incident probable dementia and any cognitive impairment (combined mild cognitive impairment or dementia).
- Screening Tool: Global cognitive function assessed annually using the 100-point Modified Mini-Mental State (3MS) exam (in-person) and later the Telephone Interview for Cognitive Status-modified (TICSm).
- Diagnostic Workup: Participants screening positive underwent extensive neuropsychological testing (CERAD battery), neurological examinations, neuropsychiatric evaluations, and cranial CT scans to rule out reversible causes and confirm diagnosis based on DSM-IV criteria.
- 5. Data Analysis:
- Statistical Model: Proportional hazards regression to assess interaction between diabetes status and treatment assignment on cognitive outcomes.
- Covariates: Models were adjusted for age and baseline cognitive scores.
Signaling Pathways and Conceptual Diagrams
Diagram 1: Proposed Pathway for HT Exacerbation of Cognitive Risk in T2DM
Diagram 2: HRT Decision Pathway for Women with T2DM
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Resources for HRT in T2DM Research
| Item / Resource | Function / Application in Research |
|---|---|
| TriNetX Analytics Platform | A global federated health research network providing de-identified electronic health records for large-scale, real-world retrospective cohort studies on drug safety and outcomes. [55] |
| WHI & WHIMS Datasets | Curated, publicly available datasets from the Women's Health Initiative cohorts, enabling longitudinal analysis of HT effects on cognitive, cardiovascular, and cancer outcomes in older women, including those with T2DM. [65] |
| Modified Mini-Mental State (3MS) Exam | A 100-point extended version of the MMSE; a validated and sensitive tool for global cognitive assessment and screening for dementia in large-scale clinical trials. [65] |
| Telephone Interview for Cognitive Status-modified (TICSm) | A validated telephone-based cognitive assessment tool enabling cost-effective longitudinal follow-up of cognitive function in large, geographically dispersed cohorts after initial in-person studies. [65] |
| Conjugated Equine Estrogens (CEE) | A specific, well-studied formulation of estrogens used in major trials like WHI. Essential for replicating previous study protocols or conducting comparative effectiveness research against other estrogen formulations. [65] |
| Medroxyprogesterone Acetate (MPA) | A specific synthetic progestin. Critical for studying the differential effects of combined estrogen-progestin therapy versus estrogen-alone therapy, particularly in women with an intact uterus. [65] |
| Transdermal Estradiol Patches | A standardized method for delivering non-oral estrogen in clinical trials, crucial for investigating the route-of-administration hypothesis regarding cardiovascular and thrombotic risk. [55] [4] |
What is the clinical rationale for developing non-hormonal alternatives like NK3R antagonists for vasomotor symptoms?
Hormone Replacement Therapy (HRT) is the most effective treatment for menopausal vasomotor symptoms (VMS), such as hot flashes and night sweats [25]. However, its use is contraindicated for some women, including those with a history of breast cancer, venous thromboembolism, or active liver disease [80]. Furthermore, for a key patient population in this thesis—postmenopausal women with Type 2 Diabetes (T2DM)—the decision to use HRT requires careful risk-benefit analysis. While HRT can improve glycemic control and reduce the risk of developing T2DM, it carries specific risks, such as an increased risk of stroke and thromboembolic events, particularly with oral formulations [4] [3] [25]. This clinical dilemma creates a pressing need for effective, non-hormonal therapeutics for the management of VMS, especially for women with T2DM for whom HRT is not suitable.
Quantitative Efficacy Benchmarking
How does the efficacy of Neurokinin-3 Receptor Antagonists (NK3Ras) compare to established non-hormonal treatments?
Benchmarking the efficacy of new agents against standard care is fundamental. The table below summarizes key efficacy outcomes from placebo-controlled randomized trials for NK3R antagonists and the commonly prescribed SNRI, venlafaxine/desvenlafaxine.
Table 1: Efficacy Benchmarking: NK3R Antagonists vs. SNRIs for Vasomotor Symptoms
| Agent Class | Reduction in HF Frequency (from baseline) | Time to Significant Effect | Key Efficacy Findings |
|---|---|---|---|
| NK3R Antagonists (e.g., Fezolinetant, MLE4901) | 62% to 93% [80] [81] | By Day 3 (72% reduction) [81] | Rapid, significant reduction in HF frequency, severity, and bother; improvements in sleep interference and quality of life [81] [82]. |
| SNRIs (e.g., Venlafaxine, Desvenlafaxine) | 48% to 67% (at weeks 8-12) [80] | Not specified (data reported at weeks 8-12) [80] | Modest reduction in HF frequency; efficacy data considered most convincing among older non-hormonal options [80]. |
Table 2: Safety and Tolerability Profile Comparison
| Agent Class | Common Adverse Effects | Serious Safety Considerations | Clinical Advantages |
|---|---|---|---|
| NK3R Antagonists | Nausea, diarrhea, headache, cough [82] [83] | Transient elevation of liver transaminases (may be compound-specific, not a class effect) [80] [82] [83] | No estrogen exposure; does not interact with tamoxifen; superior efficacy and tolerability vs. SNRIs in Phase 2 trials [80]. |
| SNRIs (e.g., Venlafaxine) | Nausea (frequently reported), dizziness, dry mouth [80] | Drug interactions (e.g., paroxetine is a potent CYP2D6 inhibitor, contra-indicated with tamoxifen) [80] | A well-established non-hormonal option; venlafaxine is preferred in breast cancer survivors on tamoxifen [80]. |
Experimental Protocols & Methodologies
What is a standard experimental protocol for a clinical trial assessing NK3R antagonist efficacy in postmenopausal women?
The following workflow and methodology are adapted from a published phase 2, randomized, double-blind, placebo-controlled, crossover trial [81].
Detailed Methodology:
- Study Population: Recruit women aged 40-62 years who are postmenopausal (≥12 months since last menstrual period) and experience ≥7 hot flashes per 24 hours, some of which are self-reported as "bothersome" or "severe" [81].
- Study Design: A single-center, randomized, double-blind, placebo-controlled, crossover trial.
- Baseline Period: A 2-week "run-in" period establishes a steady-state baseline for symptom recording and familiarizes participants with data collection tools [81].
- Randomization & Intervention: Eligible participants are randomized to one of two sequences:
- Sequence 1: 4 weeks of oral NK3R antagonist (e.g., MLE4901, twice daily) followed by a 2-week washout period, then 4 weeks of matched placebo (twice daily).
- Sequence 2: 4 weeks of placebo followed by a 2-week washout, then 4 weeks of active treatment [81].
- Outcome Measures:
- Primary Outcome: Total number of hot flashes during the fourth week of each treatment period.
- Secondary Outcomes:
- HF severity and bother (recorded twice daily).
- Hot Flash Related Daily Interference Scale (HFRDIS).
- Menopause-Specific Quality of Life (MENQOL) questionnaire.
- Objective VMS measurement via skin conductance monitor (e.g., Bahr monitor) [81].
- Statistical Analysis: Analysis is performed on both intention-to-treat and per-protocol datasets using generalized linear mixed models, accounting for period, sequence, and treatment effects [81].
The Scientist's Toolkit: Research Reagent Solutions
What are the key reagents and tools for investigating the NK3R signaling pathway?
Table 3: Essential Research Reagents for NK3R Pathway Investigation
| Reagent / Tool | Function / Application in Research | Example Use Case |
|---|---|---|
| Selective NK3R Agonists (e.g., Senktide) | Potently and selectively activates NK3R to study receptor function and downstream signaling. Used to establish in vitro and in vivo models of NK3R activation [83] [84]. | Eliciting hot flash-like responses in animal models to test efficacy of novel antagonists [84]. |
| Selective NK3R Antagonists (e.g., Osanetant (SR142801), Talnetant (SB223412) | Validated tool compounds for blocking NK3R activity. Critical for mechanistic studies to confirm on-target effects and for benchmarking new drug candidates [83]. | Preclinical validation of NK3R's role in the hypothalamic-pituitary-gonadal axis and thermoregulation. |
| Endogenous Peptide Agonists (e.g., Neurokinin B (NKB), Substance P (SP)) | Natural ligands for tachykinin receptors. NKB is the primary endogenous agonist for NK3R. Used to study physiological receptor activation and signaling [84]. | Structural biology studies (e.g., cryo-EM) to elucidate receptor-ligand binding modes and activation mechanisms [84]. |
| Cryo-EM Structural Analysis | Technique for determining high-resolution structures of protein complexes. Reveals molecular details of NK3R bound to agonists and the Gq protein [84]. | Rational drug design by identifying key interaction residues between NK3R and different peptide agonists/antagonists [84]. |
| Engineered Gq Protein Chimera | A modified Gαq protein used to stabilize the active-state GPCR-G protein complex for structural studies [84]. | Facilitating the formation of a stable NK3R–Gq complex for high-resolution cryo-EM structure determination [84]. |
Signaling Pathway Visualization
What is the mechanistic pathway by which NK3R antagonists alleviate vasomotor symptoms?
The therapeutic action of NK3R antagonists is based on a targeted intervention in the hypothalamic thermoregulatory pathway. The following diagram illustrates the pathophysiology of VMS and the site of drug action.
Frequently Asked Questions (FAQs)
Q1: Are elevations in liver transaminases a class effect of all NK3R antagonists? Early phase 2 studies with MLE4901 reported transient elevations in liver transaminases, leading to its discontinuation [82]. However, subsequent research with structurally dissimilar NK3R antagonists, such as fezolinetant and elinzanetant, has not demonstrated the same hepatotoxicity in later-phase trials [82]. This suggests the liver enzyme elevation may be an idiosyncratic effect related to the specific chemical structure of MLE4901 rather than a universal class effect [82] [83].
Q2: How does the efficacy of NK3R antagonists like fezolinetant compare to HRT? While NK3R antagonists represent a breakthrough in non-hormonal therapy, current clinical guidelines still recognize HRT as the most effective treatment for vasomotor symptoms [25]. The primary advantage of NK3R antagonists is their ability to provide significant relief without systemic estrogen exposure, making them a vital option for women with contraindications to HRT. Direct head-to-head trials comparing NK3R antagonists to HRT are needed to quantify any efficacy gap.
Q3: What is the significance of developing a dual NK1/NK3 receptor antagonist like elinzanetant? Dual antagonism may offer additional therapeutic benefits. While NK3R antagonism primarily targets VMS, Neurokinin-1 (NK1) receptor antagonists have established anxiolytic and antidepressant properties and are also used to treat nausea and vomiting [82]. By targeting both receptors, a drug like elinzanetant could potentially address a broader range of menopausal symptoms, including mood disturbances and sleep issues, beyond just hot flashes.
Q4: From a research perspective, what is the "message-address model" for tachykinin receptor selectivity? This is a key pharmacological concept for understanding ligand-receptor interactions in this family. The model divides endogenous neurokinin peptides (like NKB and SP) into two distinct parts:
- The "message" is the conserved C-terminal region (-Phe-X-Gly-Leu-Met-NH2), which is responsible for receptor activation.
- The "address" is the divergent N-terminal region, which confers receptor subtype selectivity (e.g., preference for NK3R over NK1R) [84]. This model is crucial for rational drug design, guiding the development of selective agonists and antagonists.
Conclusion
Optimizing HRT for postmenopausal women with T2DM requires a nuanced, highly personalized approach grounded in a robust risk-benefit analysis. The evidence strongly supports transdermal estrogen as the preferred route due to its favorable cardiovascular and thrombotic safety profile compared to oral formulations. Initiating therapy early in the menopausal transition is critical for maximizing metabolic and potential cognitive benefits while minimizing risks. Future research must prioritize prospective, long-term studies focusing on diverse populations, the interaction of HRT with novel diabetes drugs like GLP-1s and SGLT2 inhibitors, and the development of refined clinical algorithms that integrate comprehensive cardiovascular risk assessment tools. For drug developers, these findings highlight a significant opportunity to create next-generation, tissue-selective HRT formulations and combination therapies specifically designed for the unique metabolic milieu of the diabetic postmenopausal woman.
References
- 1. Importance of estrogen receptors in adipose tissue function [https://pmc.ncbi.nlm.nih.gov/articles/PMC3773840/]
- 2. Estrogen and Metabolism: Navigating Hormonal Transitions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12431702/]
- 3. Menopausal Hormone Therapy and Type 2 Diabetes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5460681/]
- 4. Optimizing hormone replacement therapy for ... [https://www.explorationpub.com/Journals/eemd/Article/101430]
- 5. Metabolic syndrome, insulin resistance and menopause [https://gremjournal.com/journal/02-03-2023/metabolic-syndrome-insulin-resistance-and-menopause-the-changes-in-body-structure-and-the-therapeutic-approach/]
- 6. Environmental and social determinants of cardiovascular risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540180/]
- 7. Impact of sex and menopausal hormonal therapy on ... [https://pubmed.ncbi.nlm.nih.gov/40659706/]
- 8. Epigenetic programming of estrogen receptor in adipocytes ... [https://insight.jci.org/articles/view/173423]
- 9. Cardiometabolic Risk Factors and Endogenous Sex ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9037133/]
- 10. Diabetes and Cardiovascular Risk in Menopausal Women [https://www.healthcare-bulletin.co.uk/article/diabetes-and-cardiovascular-risk-in-menopausal-women-an-emerging-concern-3760/]
- 11. During Metabolic Syndrome Menopause [https://pubmed.ncbi.nlm.nih.gov/30179134/]
- 12. Effect of menopausal hormone therapy on components of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5933555/]
- 13. Early Natural Menopause Linked with Higher Risk of ... [https://menopause.org/press-releases/early-natural-menopause-linked-with-higher-risk-of-metabolic-syndrome]
- 14. The association between age of menopause and type 2 ... [https://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-024-00858-0]
- 15. Cross-Sectional analysis of the association between type 2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12487247/]
- 16. characteristics and risk factors of Epidemiological in Chinese... T 2 DM [https://lipidworld.biomedcentral.com/articles/10.1186/s12944-019-1091-7]
- 17. New Meta-Analysis Shows That Hormone Therapy Can ... [https://menopause.org/press-releases/new-meta-analysis-shows-that-hormone-therapy-can-significantly-reduce-insulin-resistance]
- 18. Menopausal hormone therapy decreases the likelihood of ... [https://www.sciencedirect.com/science/article/pii/S1262363624000387]
- 19. Estrogen Improves Insulin Sensitivity and Suppresses ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6341301/]
- 20. Estrogen: An Emerging Regulator of Insulin Action and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4391691/]
- 21. The biological and immunological significance of the estrogen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436140/]
- 22. Study reveals how estrogen exerts its anti-diabetic effects [https://www.utsouthwestern.edu/newsroom/articles/year-2023/oct-estrogen-anti-diabetic-effects.html]
- 23. Effects of postmenopausal hormone replacement therapy ... [https://pubmed.ncbi.nlm.nih.gov/10480500/]
- 24. Type-2 diabetes and hormone replacement therapy (HRT) [https://mydiabetesmyway.scot.nhs.uk/resources/external/type-2-diabetes-and-hormone-replacement-therapy-hrt/]
- 25. Menopause Topics: Hormone Therapy [https://menopause.org/patient-education/menopause-topics/hormone-therapy]
- 26. Primary care HRT guidance [https://www.chelwest.nhs.uk/professionals/gp-hrt-advice-guidance]
- 27. Hormone Replacement Therapy - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK493191/]
- 28. Strategies for risk stratification and cardiovascular toxicity ... [https://www.escardio.org/Councils/Council-for-Cardiology-Practice-(CCP)/Cardiopractice/strategies-for-risk-stratification-and-cardiovascular-toxicity-prevention-in-pat]
- 29. Effects of Hormone Replacement Therapy on Insulin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4884259/]
- 30. Risk assessment models of cancer-associated thrombosis [https://www.sciencedirect.com/science/article/pii/S2666572721000444]
- 31. Study warns women with type 2 diabetes against using oral ... [https://www.news-medical.net/news/20250915/Study-warns-women-with-type-2-diabetes-against-using-oral-estrogen-therapy.aspx]
- 32. Effects of transdermal versus oral hormone replacement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10147786/]
- 33. The dangers of compounded bioidentical hormone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6808563/]
- 34. Is the use of vaginal progesterone a factor in pregnant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12452144/]
- 35. Vaginal progesterone for the prevention of preterm birth ... [https://www.sciencedirect.com/science/article/abs/pii/S0301211518309692]
- 36. Reconsidering Hormone Replacement Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565178/]
- 37. Effects of transdermal and oral estrogen replacement on ... [https://pubmed.ncbi.nlm.nih.gov/12419087/]
- 38. Hormone Therapy for Menopause: Timing, Safety, and Best ... [https://www.ajmc.com/view/hormone-therapy-for-menopause-timing-safety-and-best-candidates]
- 39. Optimizing menopausal hormone therapy: for treatment ... [https://www.sciencedirect.com/science/article/pii/S2414644722000252]
- 40. Benefits and risks of hormone replacement therapy (HRT) [https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/benefits-and-risks-of-hormone-replacement-therapy-hrt/]
- 41. Effect of hormone replacement therapy on bone formation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8022851/]
- 42. Menopause Society Meeting 2025 [https://honehealth.com/edge/menopause-society-meeting-2025-2/?srsltid=AfmBOoq6AdO3gaz4G5ywecy3b3_3zhwU0HD1xGse1DtdvCV3_LNXXAra]
- 43. Oral HRT linked to higher heart disease risk in women ... [https://www.medicalnewstoday.com/articles/oral-hrt-linked-to-higher-heart-disease-risk-in-women-with-diabetes]
- 44. Type 2 Diabetes Mellitus and Menopausal Hormone Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC6848654/]
- 45. The 2020 Menopausal Hormone Therapy Guidelines - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7475284/]
- 46. How menopausal hormone therapy may impact diabetes [https://www.healio.com/news/endocrinology/20250909/consider-impact-on-glucose-risks-when-prescribing-menopausal-ht-for-women-with-diabetes]
- 47. Optimizing Hormone Replacement: Why Regular ... [https://www.theblendinstitute.com/blog/optimizing-hormone-replacement-why-regular-monitoring-is-key]
- 48. Impact of sex and menopausal hormonal therapy on ... [https://www.nature.com/articles/s41598-025-01768-8]
- 49. Collaboration Connection: Finding the Time for Teamwork [https://endocrinenews.endocrine.org/collaboration-connection/]
- 50. The involvement of specialists in primary healthcare teams ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11837382/]
- 51. The American Diabetes Association Releases Standards of ... [https://diabetes.org/newsroom/press-releases/american-diabetes-association-releases-standards-care-diabetes-2025]
- 52. Diabetes CRO [https://www.medpace.com/therapeutics/therapeutic-depth/endocrine-metabolic/diabetes/]
- 53. Metabolic (Diabetes) and Endocrine Research [https://www.ppd.com/therapeutic-expertise/metabolic-endocrine/]
- 54. Hormonal therapies and venous thrombosis - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9399360/]
- 55. Effects of hormone replacement therapy (HRT) in midlife ... [https://www.sciencedirect.com/science/article/pii/S1470211825001083]
- 56. Menopausal Hormone Therapy in Women with Type 2 Diabetes Mellitus: An Updated Review | Diabetes Therapy [https://link.springer.com/article/10.1007/s13300-024-01546-1]
- 57. FDA Requests Labeling Changes Related to HRT [https://www.fda.gov/drugs/drug-safety-and-availability/fda-requests-labeling-changes-related-safety-information-clarify-benefitrisk-considerations]
- 58. HHS Advances Women's Health, Removes Misleading ... [https://www.fda.gov/news-events/press-announcements/hhs-advances-womens-health-removes-misleading-fda-warnings-hormone-replacement-therapy]
- 59. HHS Advances Women's Health, Removes Misleading ... [https://www.hhs.gov/press-room/hhs-advances-womens-health-removes-misleading-fda-warnings-hormone-replacement-therapy.html]
- 60. Watch: FDA's Marty Makary on hormone replacement ... [https://www.npr.org/sections/shots-health-news/2025/11/10/nx-s1-5604283/fda-menopause-hormone-therapy]
- 61. Hormone Replacement Therapy (HRT) and Breast Cancer ... [https://www.breastcancer.org/risk/risk-factors/using-hormone-replacement-therapy]
- 62. Contemporary menopausal hormone therapy and risk of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11600536/]
- 63. Breast cancer risk in younger women may be influenced by ... [https://www.niehs.nih.gov/news/factor/2025/7/feature/2-feature-hormone-therapy-breast-cancer-risk]
- 64. Information resources for advice on HRT – SPS [https://www.sps.nhs.uk/articles/information-resources-for-advice-on-hrt/]
- 65. Impact of Type 2 Diabetes and Postmenopausal Hormone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4657616/]
- 66. Systematic review and meta-analysis of the effects ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1350318/full]
- 67. Associations Between Midlife Menopausal Hormone Therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10551825/]
- 68. Cardiometabolic health, menopausal estrogen therapy and ... [https://www.sciencedirect.com/science/article/pii/S009130222300016X]
- 69. Metabolic effects of estrogen substitution in combination ... [https://www.sciencedirect.com/science/article/abs/pii/S096007601200026X]
- 70. Combined effect of physical exercise and hormone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10241482/]
- 71. Navigating diabetes through the menopause transition [https://www.mymenopausecentre.com/gp-resources/navigating-diabetes-through-the-menopause-transition-what-you-need-to-know-about-perimenopause-postmenopause-and-hrt/]
- 72. The 2025 Menopausal Hormone Therapy Guidelines [https://pmc.ncbi.nlm.nih.gov/articles/PMC12438153/]
- 73. Cardiorenal outcomes after herpes zoster reactivation in COVID-19... [https://www.nature.com/articles/s41598-025-16398-3?error=cookies_not_supported&code=eaa8ad6b-7518-4097-b8b8-7b7eeb66b2e4]
- 74. Methods for real-world studies of comparative effects [https://www.nice.org.uk/corporate/ecd9/chapter/methods-for-real-world-studies-of-comparative-effects]
- 75. Long-term cardiovascular in COVID-19 survivors among... outcomes [https://pubmed.ncbi.nlm.nih.gov/35971425/]
- 76. Effect of Postmenopausal Hormone Therapy on Glucose ... [https://pubmed.ncbi.nlm.nih.gov/37729504/]
- 77. A systematic review and meta-regression analysis to ... [https://www.sciencedirect.com/science/article/pii/S2352906718301957]
- 78. Effectiveness and safety of hormone replacement therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11826161/]
- 79. Hormone replacement therapy and cancer mortality in ... [https://www.nature.com/articles/s41416-024-02767-8]
- 80. Neurokinin 3 Receptor Antagonists Compared With Serotonin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8478773/]
- 81. Neurokinin 3 receptor antagonism rapidly improves vasomotor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6092106/]
- 82. Neurokinin-3 Receptor Antagonists: A Novel Approach to ... [https://womensmentalhealth.org/posts/neurokinin-3-receptor-antagonists-for-menopausal-vasomotor-symptoms/]
- 83. Neurokinin 3 Receptor Antagonist - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/neurokinin-3-receptor-antagonist]
- 84. Structural insights into neurokinin 3 receptor activation by ... [https://www.nature.com/articles/s41421-023-00564-w]