MK-677 and Capromorelin in Clinical Trials: A Comprehensive Review of Mechanisms, Efficacy, and Future Directions for GHS Therapeutics
This article provides a detailed analysis of the clinical development of two prominent growth hormone secretagogues (GHS), MK-677 (ibutamoren) and capromorelin.
MK-677 and Capromorelin in Clinical Trials: A Comprehensive Review of Mechanisms, Efficacy, and Future Directions for GHS Therapeutics
Abstract
This article provides a detailed analysis of the clinical development of two prominent growth hormone secretagogues (GHS), MK-677 (ibutamoren) and capromorelin. Targeting researchers, scientists, and drug development professionals, it synthesizes evidence from key clinical trials investigating these orally active ghrelin receptor agonists for conditions including sarcopenia, frailty, and functional decline in aging populations. The review covers foundational mechanisms of action through the GHS-R1a receptor, methodological approaches in trial design, analysis of functional outcomes like lean body mass and physical performance, and troubleshooting of challenges such as desensitization and metabolic side effects. It concludes with a comparative evaluation of their clinical profiles and a forward-looking perspective on the potential of GHS in modern therapeutics.
Unlocking the Science: The Discovery, Mechanism, and Preclinical Foundations of GHS
The Reverse Pharmacology Journey: From Synthetic GHRP-6 to the Discovery of Ghrelin and GHS-R1a
Reverse pharmacology is a powerful approach that begins with the observation of a compound's biological effects and works backward to elucidate its endogenous targets and pathways. The discovery of the ghrelin system stands as a landmark example of this methodology's success. This journey commenced with the development of synthetic growth hormone-releasing peptides (GHRPs), which were engineered to stimulate GH secretion [1]. The first in this class, GHRP-6 (His-DTrp-Ala-Trp-DPhe-Lys-NH2), was identified by endocrinologist Cyril Bowers in the early 1980s after he observed that certain enkephalin analogs could stimulate GH release from pituitary cultures [1]. This synthetic peptide, and others like GHRP-2 and hexarelin that followed, demonstrated potent GH-releasing and appetite-stimulating activities in mammals, strongly suggesting the existence of an undiscovered endogenous system [2] [1].
The critical breakthrough came in 1996 when Howard et al. discovered an orphan G-protein-coupled receptor (GPCR) in humans and pigs that was activated by these synthetic GHSs [2]. They named this receptor the Growth Hormone Secretagogue Receptor Type 1a (GHS-R1a). This discovery set the stage for the final step in the reverse pharmacology process: the identification of the receptor's natural ligand. In 1999, Kojima and colleagues isolated a 28-amino-acid peptide from rat stomach extracts that bound to and activated GHS-R1a [2]. They named this hormone "ghrelin" and found it possessed a unique post-translational modification—an n-octanoyl group esterified to the serine-3 residue—essential for its biological activity [3] [2]. This reverse pharmacology journey, from synthetic GHRP-6 to the discovery of ghrelin and its receptor, unlocked an entirely new endocrine system with profound implications for physiology and therapeutic development.
GHS-R1a: Receptor Structure and Signaling Mechanisms
Molecular Architecture of GHS-R1a
GHS-R1a is a classical class A G-protein-coupled receptor comprising 366 amino acids in humans [3] [4]. The gene encoding GHS-R1a (GHSR) is located on chromosome 3q26.31 and consists of two exons separated by one intron [2]. Exon 1 encodes the first 265 amino acids, including transmembrane domains (TMD) 1-5, while exon 2 encodes the remaining 101 amino acids, encompassing TMD 6 and 7 [2]. An alternative splice variant of this gene, known as GHS-R1b, consists of 289 amino acids and is formed from the first exon and part of the intron [2]. Unlike GHS-R1a, GHS-R1b does not bind ghrelin or synthetic GHSs and lacks the ability to mobilize intracellular Ca2+, though it may modulate GHS-R1a signaling [3] [5].
Recent structural biology advances have illuminated the unique topology of the GHS-R1a binding pocket. Crystallography and cryo-electron microscopy studies reveal that the binding pocket is characterized by a wide gap between TM6 and TM7 and is bifurcated into two cavities by a salt bridge between Glu124 and Arg283 [3]. The larger cavity I and smaller cavity II accommodate different portions of ghrelin and synthetic ligands. The octanoyl moiety of acylated ghrelin is nestled within cavity II, which is crucial for receptor activation, while the peptide backbone primarily occupies cavity I [3]. Non-peptide agonists like ibutamoren (MK-0677) occupy both cavities, mimicking the first four residues of ghrelin, including the octanoyl moiety [3].
Signaling Pathways and Constitutive Activity
GHS-R1a exhibits one of the highest constitutive signaling activities among GPCRs, evoking signals at approximately 50% of the maximal ghrelin response even in the absence of ligand [3]. This receptor primarily couples to Gαq/11 proteins, activating phospholipase C (PLC) to generate inositol trisphosphate (IP3) and diacylglycerol (DAG), leading to mobilization of intracellular Ca2+ stores [3]. GHS-R1a also signals through other G protein isoforms, including Gαi/o and Gα13, as well as β-arrestin scaffold proteins, enabling a complex array of downstream effects [3].
Table 1: Key GHS-R1a-Mediated Signaling Pathways and Functional Outcomes
| Signaling Pathway | Key Effectors | Primary Physiological Outcomes | Therapeutic Implications |
|---|---|---|---|
| Gαq/11 | PLC, IP3, DAG, Ca2+ | GH secretion, appetite stimulation | Growth disorders, cachexia |
| Gαi/o | cAMP modulation | Metabolic regulation, insulin secretion | Diabetes, metabolic syndrome |
| β-arrestin | ERK signaling, receptor internalization | Potential neuroprotective effects | Epilepsy, neurodegenerative diseases |
| Constitutive Activity | Basal signaling tone | Energy homeostasis regulation | Potential target for inverse agonists |
The complexity of GHS-R1a signaling is further enhanced by its ability to form homodimers and heterodimers with other GPCRs, including GHS-R1b, serotonin 5-HT2c, dopamine D1 and D2, somatostatin SST5, and melanocortin MC3 receptors [3]. This receptor promiscuity allows ghrelin to integrate with multiple neurotransmitter and hormone systems, explaining its diverse physiological roles [3] [1]. Additionally, the melanocortin receptor accessory protein 2 (MRAP2) has been identified as an important modulator that potentiates Gαq/11-dependent signaling while inhibiting β-arrestin recruitment and suppressing the receptor's constitutive activity [3].
Diagram 1: GHS-R1a Signaling Complexity. The receptor exhibits high constitutive activity and signals through multiple G-protein and β-arrestin pathways, resulting in diverse physiological outcomes. Receptor heterodimerization with other GPCRs further expands its functional versatility.
Key Experimental Models and Research Tools
In Vitro Assays for GHS-R1a Function
The study of GHS-R1a function relies on several well-established in vitro methodologies that enable researchers to quantify receptor activation, signaling pathway engagement, and ligand-receptor interactions.
Calcium Mobilization Assay: This is a primary functional assay for GHS-R1a activity due to the receptor's strong coupling to Gαq/11 and subsequent intracellular Ca2+ release. Cells stably expressing GHS-R1a (typically HEK293 or CHO cells) are loaded with a fluorescent calcium indicator such as Fluo-4 or Fura-2. Ligand-induced fluorescence changes are measured using a fluorometer or fluorescence plate reader, providing real-time kinetic data on receptor activation. Ghrelin typically produces half-maximal effective concentration (EC50) values ranging from 6.1×10-8 to 3.2×10-8 M in calcium release assays [4].
Inositol Phosphate (IP) Accumulation Assay: This method directly measures the production of IP1, IP2, and IP3, which are downstream products of PLC activation. The assay often utilizes cells pre-labeled with [3H]-myo-inositol. After ligand stimulation, inositol phosphates are extracted and separated by anion-exchange chromatography, and radioactivity is quantified by scintillation counting. Ghrelin demonstrates higher potency in this assay (EC50 = 3.4×10-10 M for IP3 accumulation) compared to calcium mobilization [4].
Radioligand Binding Assays: These competitive binding experiments determine the affinity (Ki or Kd) of ligands for GHS-R1a. Membrane preparations from GHS-R1a-expressing cells or tissues are incubated with a radiolabeled ligand such as [125I][His9]-ghrelin (Kd = 4×10-10 M) in the presence of increasing concentrations of unlabeled test compounds [4]. Specific binding is calculated by subtracting nonspecific binding (determined in the presence of an excess of unlabeled ghrelin) from total binding.
β-Arrestin Recruitment Assays: These assays measure GHS-R1a activation through β-arrestin pathway engagement, often utilizing enzyme fragment complementation (e.g., PathHunter) or bioluminescence resonance energy transfer (BRET) technologies. Such assays have revealed that ghrelin induces β-arrestin recruitment with an EC50 of 7.1×10-9 M [4].
Table 2: Key Pharmacological Tools for GHS-R1a Research
| Compound | Type | Key Pharmacological Parameters | Research Applications |
|---|---|---|---|
| Ghrelin (human) | Endogenous agonist | pKd = 8.6–9.4 (Kd = 2.3×10-9 – 3.6×10-10 M) [4] | Reference standard for receptor activation |
| GHRP-6 | Synthetic peptide agonist | pEC50 = 8.3–9.1 (Calcium release, IP3 accumulation) [4] | Prototypical GHS; cardioprotection studies [1] |
| Ibutamoren (MK-677) | Non-peptide agonist | pKi = 9.3 (Ki = 4.6×10-10 M) [4] | Long-term GH stimulation studies |
| [D-Lys3]-GHRP-6 | Competitive antagonist | Antagonizes ghrelin-induced Ca2+ mobilization [6] | Mechanism studies; islet transplantation research [6] |
| PF-05190457 | Inverse agonist | High affinity and selective [7] | Studies of constitutive receptor activity |
| Capromorelin | Oral agonist | hGHS-R1a EC50 = 0.49 nM for derivative 4b [8] | Veterinary and potential human therapeutics [9] [8] |
In Vivo Models and Translational Approaches
Animal models have been instrumental in characterizing the physiological roles of the ghrelin system. Rodent studies consistently demonstrate that administration of ghrelin or GHS-R1a agonists stimulates food intake, body weight gain, and GH secretion [3] [5]. Large animal models, particularly felines, have provided critical translational insights, leading to the approval of the GHS-R1a agonist capromorelin for veterinary use. In a randomized, placebo-controlled field study of client-owned cats with chronic kidney disease and unintended weight loss, capromorelin (2 mg/kg orally once daily for 55 days) produced a mean body weight increase of +5.18%, compared to a -1.65% change in the placebo group—a treatment effect of +6.81% [9].
Diagram 2: Key Experimental Assays for GHS-R1a Research. Multiple in vitro methodologies enable comprehensive characterization of receptor function, signaling pathway engagement, and ligand-receptor interactions.
Research Reagent Solutions: A Scientist's Toolkit
A well-equipped laboratory investigating the ghrelin system requires specific pharmacological tools, assay kits, and biological reagents. The following table details essential research solutions for studying GHS-R1a function and modulation.
Table 3: Essential Research Reagents for GHS-R1a Investigations
| Reagent/Category | Specific Examples | Function/Application | Key Features |
|---|---|---|---|
| Reference Agonists | Ghrelin (human/rat), GHRP-6, Ibutamoren (MK-0677) [7] [4] | Receptor activation standards; positive controls for functional assays | Ghrelin: endogenous ligand (pEC50 = 7.2–9.5) [4] |
| Antagonists & Inverse Agonists | [D-Lys3]-GHRP-6, PF-05190457, PF-04628935 [6] [7] | Mechanism studies; blocking endogenous ghrelin effects; constitutive activity research | [D-Lys3]-GHRP-6: competitive antagonist for islet studies [6] |
| Cell-Based Assay Systems | GHS-R1a-expressing cell lines (HEK293, CHO); β-arrestin recruitment kits | Functional screening of novel compounds; pathway bias assessment | Stable cell lines ensure consistent receptor expression levels |
| Radioligands | [125I][His9]-ghrelin, [125I][Tyr4]-ghrelin, [35S]ibutamoren [4] | Binding affinity studies; receptor localization and quantification | High specific activity required for sensitive detection |
| Antibodies | Anti-GHS-R1a, anti-ghrelin, anti-phospho-ERK | Western blot, immunohistochemistry, ELISA applications | Validation for specific applications is critical |
| Animal Models | Ghrelin knockout mice, GHS-R1a deficient mice, diet-induced obesity models | In vivo validation of compound efficacy and physiological effects | Transgenic models help elucidate specific pathway functions |
Therapeutic Applications and Clinical Translation
Agonist Applications: Cachexia, Anorexia, and Growth Disorders
GHS-R1a agonists have shown significant promise in conditions characterized by weight loss, muscle wasting, and inadequate growth. Capromorelin exemplifies this therapeutic approach, having received regulatory approval for managing weight loss in cats with chronic kidney disease. In the pivotal field study, capromorelin treatment produced a statistically significant increase in body weight (+5.18% from baseline) compared to placebo (-1.65%), with a treatment effect of +6.81% (P<0.0001) over 55 days [9]. The drug was well-tolerated, with hypersalivation being the primary adverse effect observed exclusively in the active treatment group [9].
In human medicine, the non-peptide agonist ibutamoren (MK-0677) has been extensively studied for its ability to restore the pulsatile secretion of GH in elderly subjects and in catabolic conditions [3]. Similarly, research continues to develop even more potent oral agonists, with recent capromorelin derivatives demonstrating remarkable potency (EC50 = 0.49 nM for compound 4b) and oral bioavailability (43.6% in dogs) [8]. In a preclinical study, 10-day oral administration of this derivative increased both body weight and length in 4-week-old rats, supporting its potential application for growth hormone deficiency [8].
Antagonist Applications: Metabolic and Endocrine Disorders
Conversely, GHS-R1a antagonists may offer therapeutic benefits in conditions where reduced ghrelin signaling could be advantageous. Research in pancreatic islets has revealed that the GHS-R1a antagonist [D-Lys3]-GHRP-6 (DLS) promotes insulin production and improves glucose-stimulated insulin secretion [6]. Treatment with DLS (4.0 µg/mL) significantly increased insulin content in mouse islets (269.01 ± 12.19 ng/islet vs. 222.01 ± 4.62 ng/islet in controls) and enhanced the stimulation index by approximately two-fold (3.04 ± 0.51 vs. 1.59 ± 0.19 in controls) [6]. These effects appear mediated through suppression of somatostatin production from δ cells, highlighting the potential of GHS-R1a antagonists to improve β-cell function and islet transplantation outcomes [6].
Beyond Metabolism: Cardioprotection and Cytoprotection
Notably, the therapeutic potential of GHS-R1a ligands extends beyond metabolic and endocrine applications. GHRP-6 and hexarelin have demonstrated significant cardioprotective and cytoprotective properties in preclinical models, reducing cellular death following ischemic insults [1]. These peptides activate survival pathways such as PI-3K/AKT1, enhance antioxidant defenses, reduce inflammation, and decrease reactive oxygen species spillover in cardiac, neuronal, gastrointestinal, and hepatic cells [1]. The cardioprotective effects appear to be mediated through both GHS-R1a and CD36 receptors, with hexarelin showing specific binding in human myocardium, ventricles, atria, and coronary arteries [1]. These multifaceted protective actions position GHS-R1a ligands as promising candidates for conditions involving parenchymal organ damage, though clinical translation remains underway.
The reverse pharmacology journey from synthetic GHRP-6 to the discovery of ghrelin and its receptor GHS-R1a has unveiled a remarkably complex physiological system with extensive therapeutic implications. The high constitutive activity of GHS-R1a, its promiscuous signaling through multiple G proteins and β-arrestin, and its ability to form heterodimers with other GPCRs create both challenges and opportunities for drug development. Future research directions will likely focus on developing biased ligands that selectively engage therapeutic pathways while avoiding those linked to adverse effects [3]. For instance, ligands favoring β-arrestin recruitment might offer antiepileptic benefits, while those selectively activating Gi/o and G13 pathways could optimize gastric emptying without undesirable endocrine effects [3].
The continued structural elucidation of GHS-R1a bound to various ligands provides a rational foundation for drug design, enabling researchers to exploit the unique bifurcated binding pocket of this receptor [3]. As our understanding of ghrelin signaling deepens, and as compounds with improved pharmacokinetic and pharmacodynamic profiles emerge, the clinical translation of GHS-R1a-targeted therapies will undoubtedly expand, potentially addressing conditions ranging from cachexia and growth disorders to diabetes, cardiovascular disease, and neurodegenerative conditions. The ghrelin system continues to validate the power of reverse pharmacology as an approach for discovering new endocrine pathways and developing novel therapeutic strategies.
Ghrelin is a 28-amino acid peptide hormone primarily produced in the oxyntic glands of the gastric fundus, renowned as the "hunger hormone" for its critical role in regulating appetite and energy homeostasis [10] [11]. This unique hormone undergoes a essential post-translational modification (octanoylation at Serine-3) that is absolutely required for its biological activity, mediated by the ghrelin O-acyltransferase (GOAT) enzyme [10]. Ghrelin exerts its effects through binding to the growth hormone secretagogue receptor 1a (GHS-R1a), a G-protein coupled receptor (GPCR) predominantly expressed in the hypothalamus and pituitary gland, as well as in various peripheral tissues including heart, lung, liver, and kidney [10] [11].
MK-677 (Ibutamoren) and Capromorelin represent a class of synthetic, orally active small molecules known as ghrelin receptor agonists or growth hormone secretagogues (GHS) [10] [12]. These compounds were strategically designed to mimic the effects of endogenous ghrelin while overcoming its pharmaceutical limitations, particularly its short serum half-life, making them therapeutically viable [10]. Originally investigated for their ability to stimulate growth hormone (GH) secretion, the discovery of ghrelin and its receptor subsequently revealed their broader therapeutic potential for treating conditions characterized by appetite loss, weight loss, muscle wasting, and growth hormone deficiency [10].
Molecular Mechanisms of Action
Ghrelin Receptor Binding and Activation
Both MK-677 and Capromorelin function as potent, selective, orally-active agonists of the ghrelin receptor (GHS-R1a) [12] [10]. Structural biology studies using cryo-electron microscopy have illuminated the molecular details of how these agonists activate the receptor. The GHS-R1a receptor contains a deep binding pocket divided into two cavities (Cavity I and Cavity II) by a critical salt bridge between residues E124³·³³ and R283⁶·⁵⁵ [11].
MK-677 binds deeply within this pocket, engaging with key receptor residues to stabilize an active conformation [11]. The binding mode shares significant overlap with that of endogenous ghrelin, particularly in the interaction with the salt bridge that divides the binding cavity. Molecular mutagenesis studies confirm that residues E124³·³³, R283⁶·⁵⁵, and Q120³·²⁹ are essential for receptor activation by both ghrelin and MK-677 [11].
Capromorelin exhibits a similar binding profile, functioning as a selective ghrelin receptor agonist that activates GHS-R1a with high affinity [10] [13]. As small molecule agonists, both compounds demonstrate optimized oral bioavailability and longer half-lives compared to the endogenous peptide ghrelin, making them superior candidates for therapeutic development [10].
Intracellular Signaling Pathways
Activation of GHS-R1a by MK-677, Capromorelin, or endogenous ghrelin initiates multiple intracellular signaling cascades through G-protein dependent mechanisms:
- Gαq/11 Pathway: Receptor activation stimulates phospholipase C (PLC), leading to inositol trisphosphate (IP3) production and diacylglycerol (DAG) formation. This results in intracellular calcium mobilization and protein kinase C (PKC) activation [11] [14].
- Gαi/o Pathway: Ghrelin receptor activation also couples to Gi proteins, modulating adenylate cyclase activity and cAMP levels in certain cell types [11] [14].
- Gs Coupling: In some neuronal populations, GHS-R1a demonstrates Gs/olf coupling, potentially contributing to the regulation of dopamine reward signaling [14].
Table 1: Key Signaling Pathways Activated by Ghrelin Receptor Agonists
| Signaling Pathway | G-Protein Coupling | Key Effectors | Biological Outcomes |
|---|---|---|---|
| Gαq/11 Pathway | Gq/11 | PLCβ, IP₃, DAG, Ca²⁺, PKC | Appetite stimulation, GH secretion [11] |
| Gαi/o Pathway | Gi/o | Adenylate cyclase, cAMP | Modulation of glucose-induced insulin release [11] |
| Gs Pathway | Gs | Adenylate cyclase, cAMP, PKA | Dopamine signaling modulation (in specific neurons) [14] |
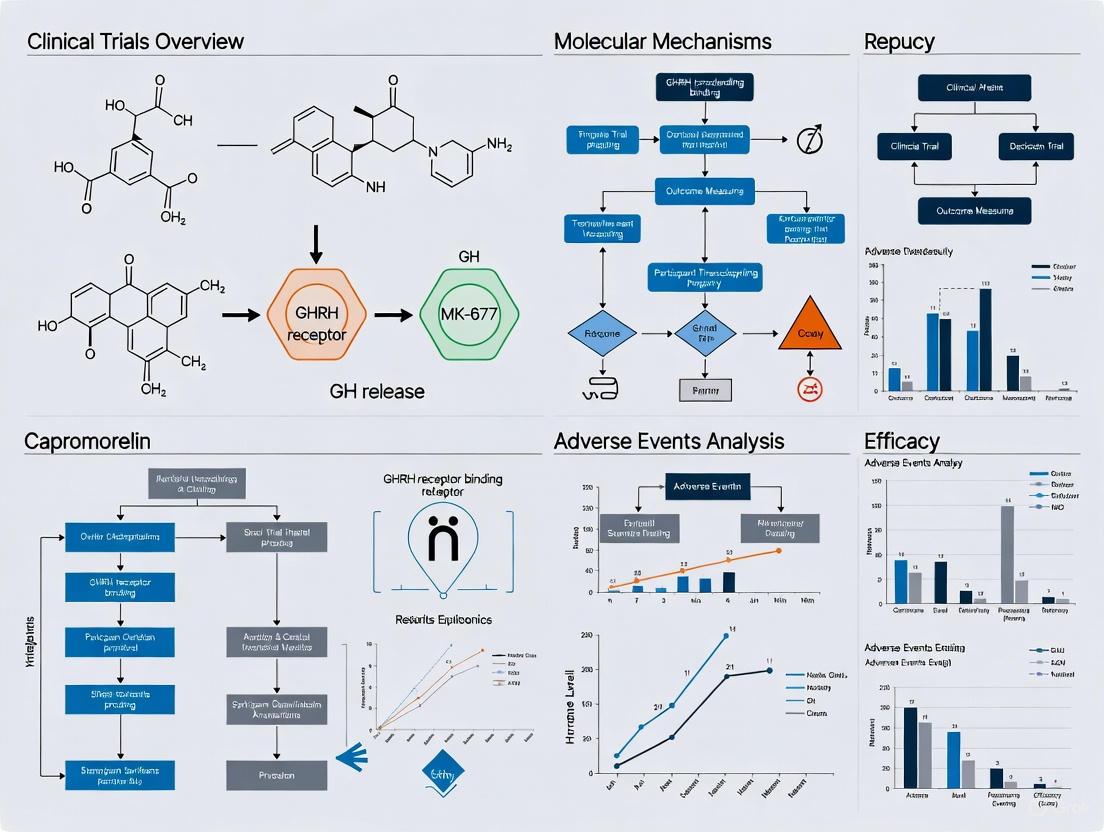
The following diagram illustrates the core signaling pathway activated by MK-677 and Capromorelin:
Diagram 1: Core Gq Signaling Pathway of GHSR Agonists
Growth Hormone and IGF-1 Axis Stimulation
A primary action of both MK-677 and Capromorelin is the stimulation of the GH-IGF-1 axis through a multi-tiered mechanism:
- Hypothalamic Action: Agonist binding to GHS-R1a in the hypothalamus stimulates growth hormone-releasing hormone (GHRH) production while reducing somatostatin secretion, creating a permissive environment for GH release [15].
- Pituitary Action: Direct activation of GHS-R1a in the anterior pituitary potentiates GHRH signaling and promotes GH synthesis and secretion [15] [13].
- Hepatic Action: Increased GH levels stimulate insulin-like growth factor 1 (IGF-1) production in the liver, creating sustained anabolic effects throughout the body [13].
This multi-level regulation results in significant increases in both GH and IGF-1 levels. In clinical studies, MK-677 treatment produced a 1.76-fold increase in the geometric mean IGF-1 levels in hemodialysis patients compared to baseline [16]. Similarly, Capromorelin administration in dogs sustainably increased IGF-1 levels by approximately 60-70% compared to placebo [13].
Pharmacological Profiles and Clinical Applications
Comparative Pharmacological Properties
Table 2: Pharmacological Comparison of MK-677 and Capromorelin
| Parameter | MK-677 (Ibutamoren) | Capromorelin |
|---|---|---|
| Administration Route | Oral | Oral |
| Receptor Selectivity | Selective GHS-R1a agonist [12] | Selective GHS-R1a agonist [10] |
| Elimination Half-life | 4-6 hours (in beagles); IGF-1 elevation sustained ~24h [12] | ~1.19 hours (Tmax ~0.83h) in dogs [10] |
| Key Metabolic Pathway | Hepatic metabolism [12] | Hepatic metabolism [10] |
| FDA Approval Status | Investigational (Orphan Drug Designation) [12] | Approved for veterinary use (dogs & cats) [9] [13] |
| Primary Indications (Under Investigation) | Growth hormone deficiency, frailty, cachexia [12] [16] | Appetite stimulation, weight management in chronic disease [9] [13] |
Clinical Applications and Efficacy
MK-677 has demonstrated significant clinical effects across multiple patient populations. In a randomized crossover study of hemodialysis patients with protein-energy wasting, MK-677 treatment resulted in a 65% greater increase in IGF-1 levels compared to placebo (ratio of geometric means: 1.65, 95% CI 1.33-2.04; P < 0.001) [16]. Elderly subjects treated with MK-677 showed increased fat-free mass, and studies in hip fracture patients demonstrated improvements in stair climbing power and gait speed [14]. The drug has also been shown to significantly increase rapid eye movement sleep by 20-50% and slow-wave sleep by approximately 50% in different age groups [12].
Capromorelin has shown remarkable efficacy in veterinary medicine. In a randomized, masked, placebo-controlled study of cats with chronic kidney disease and unintended weight loss, capromorelin treatment for 55 days resulted in a +5.18% mean change in body weight compared to -1.65% in the placebo group, representing a treatment effect of +6.81% (P < 0.0001) [9]. Similarly, in client-owned inappetent dogs, capromorelin significantly improved appetite (68.6% vs 44.6% with placebo, P = 0.008) and increased mean body weight (1.8% vs 0.1% with placebo, P < 0.001) after just 4 days of treatment [13].
Experimental Protocols and Research Methodologies
Protocol: IGF-1 Response Assessment in Clinical Trials
Objective: To quantitatively evaluate the effect of ghrelin receptor agonists on serum IGF-1 levels in human subjects.
Methodology Overview: This protocol follows a randomized, blinded, placebo-controlled crossover design as implemented in the MK-677 hemodialysis study [16].
Detailed Procedures:
Subject Selection:
- Enroll patients with documented condition (e.g., ESRD with PEW, sarcopenia)
- Key inclusion: Stable medical regimen, ≥5% unintentional weight loss
- Key exclusion: Cancer, diabetes mellitus, congestive heart failure
Study Design:
- Implement randomized crossover design with washout period
- Treatment arms: Active drug (e.g., MK-677 10-25mg/day) vs. placebo
- Duration: 3-month treatment periods separated by 1-month washout [16]
Blood Collection & Processing:
- Collect serum samples at baseline and regular intervals (e.g., days 15, 27, 55)
- Process samples within 2 hours of collection
- Store at -80°C until batch analysis
IGF-1 Quantification:
- Utilize validated immunoassay (ELISA or RIA)
- Perform duplicate measurements
- Report as geometric means with 95% confidence intervals
Statistical Analysis:
- Employ mixed-effects models adjusting for pre-intervention IGF-1
- Calculate ratio of geometric means (active vs. placebo)
- Statistical significance: P < 0.05
The experimental workflow for clinical evaluation is systematically outlined below:
Diagram 2: Clinical Trial Crossover Design Workflow
Protocol: Body Weight Efficacy Assessment in Veterinary Studies
Objective: To evaluate the effect of capromorelin on body weight maintenance and gain in client-owned cats with chronic disease.
Methodology Overview: Adapted from the multicenter field study of capromorelin in cats with chronic kidney disease [9].
Detailed Procedures:
Animal Enrollment:
- Enroll client-owned cats with documented CKD and ≥5% unintentional weight loss
- Stable comorbidity treatments allowed
- Exclude cats with diabetes mellitus, cancer, or congestive heart failure
Randomization & Masking:
- Randomize 2:1 (active:placebo) using computer-generated tables
- Maintain investigator blinding through treatment coding
- Block randomization by site with block length of three
Dosing Regimen:
- Capromorelin oral solution: 2 mg/kg (0.1 ml/kg) once daily
- Placebo: Identical vehicle control at same volume
- Duration: 55 days with weight-based dosing calculated at day 0
Efficacy Assessments:
- Body weight measurement to nearest 0.1 kg at days 0, 15, 27, 55
- Body condition scoring (9-point scale)
- Muscle condition scoring
- Food intake documentation
Safety Monitoring:
- Clinical pathology (hematology, serum chemistry, urinalysis)
- Adverse event documentation
- Physical examinations at scheduled visits
Statistical Analysis:
- Mixed models with treatment as fixed effect
- Site and site*treatment as random effects
- Treatment effect calculated as LSM percent change
Protocol: Analytical Detection in Human Hair
Objective: To detect and quantify MK-677 incorporation in human hair for doping control purposes.
Methodology Overview: Adapted from forensic toxicology methods for ibutamoren detection [15].
Detailed Procedures:
Sample Preparation:
- Collect hair strands (preferably posterior vertex, ~25 mg)
- Cut into 1-2 cm segments
- Decontaminate with dichloromethane (2x5 mL)
- Dry under nitrogen stream
Extraction:
- Incubate in 1 mL methanol at 40°C for 18 hours
- Add internal standard (deuterated MK-677)
- Evaporate to dryness under nitrogen
- Reconstitute in 50 μL mobile phase
LC-MS/MS Analysis:
- Column: C18 reversed-phase (100 × 2.1 mm, 1.8 μm)
- Mobile phase: A: ammonium formate buffer; B: acetonitrile
- Gradient elution: 5-95% B over 15 minutes
- Flow rate: 0.3 mL/min
- Injection volume: 10 μL
MS Detection:
- ESI positive ionization mode
- MRM transitions: m/z 529.2→510.2 (quantifier); 529.2→301.1 (qualifier)
- Calibration range: 0.5-250 pg/mg
- LOD: 0.1 pg/mg; LLOQ: 0.5 pg/mg [15]
Validation Parameters:
- Linearity: R² > 0.99
- Precision: CV < 15% at LLOQ
- Accuracy: 85-115% of nominal values
- Selectivity: No interference at retention time
Research Reagent Solutions
Table 3: Essential Research Materials for Ghrelin Receptor Agonist Studies
| Reagent/Material | Specifications | Research Application | Example Sources |
|---|---|---|---|
| GHS-R1a Expression System | HEK-293T cells expressing human GHS-R1a | Binding assays, signaling studies [14] | Commercial cDNA, stable cell lines |
| Ghrelin Receptor Agonists | MK-677 (≥98% purity), Capromorelin (≥98% purity) | In vitro and in vivo pharmacology | Pharmaceutical standards, chemical suppliers |
| LC-MS/MS System | HPLC with tandem mass spectrometer, C18 column | Bioanalytical quantification [15] | Agilent, Thermo Fisher, Sciex |
| IGF-1 Immunoassay | ELISA or RIA kits, validated for species | Serum IGF-1 quantification [16] | Commercial diagnostic kits |
| cAMP & IP3 Assays | HTRF, ELISA, or radioimmunoassay kits | G-protein coupling characterization [14] | Cisbio, PerkinElmer, Revvity |
| Animal Disease Models | Rodent cachexia models, feline CKD model | In vivo efficacy assessment [9] | Commercial research models |
MK-677 and Capromorelin represent a significant advancement in ghrelin receptor agonist therapeutics, demonstrating how targeted activation of the ghrelin receptor can produce clinically meaningful outcomes in conditions characterized by wasting, appetite loss, and growth hormone axis dysfunction. Their oral bioavailability and sustained pharmacokinetic profiles distinguish them from both endogenous ghrelin and injectable growth hormone formulations.
The comprehensive data from both clinical and veterinary studies provide robust evidence for their efficacy in increasing IGF-1 levels, promoting weight gain, and improving body composition. Continued research into the precise molecular mechanisms of GHS-R1a activation, optimization of dosing regimens, and exploration of potential applications in related metabolic disorders will further advance this promising class of therapeutics. The experimental protocols outlined provide rigorous methodological frameworks for future investigations in both basic science and clinical applications.
The Growth Hormone Secretagogue Receptor 1a (GHS-R1a) is a G protein-coupled receptor (GPCR) that serves as the primary target for ghrelin, often referred to as the "hunger hormone" [17]. This receptor plays a pivotal role in a wide array of physiological processes, most notably in the regulation of energy homeostasis, body weight, and growth hormone release [18] [17]. First identified as the target of synthetic growth hormone secretagogues (GHS), GHS-R1a was subsequently cloned from human pituitary and hypothalamus, establishing its fundamental role in neuroendocrine pathways [18]. The receptor is characterized by its high basal constitutive activity, meaning it signals significantly even in the absence of its natural ligand, ghrelin [19] [20]. This intrinsic activity provides a tonic signal that is essential for normal physiological function, particularly within the growth hormone axis [17].
GHS-R1a is expressed in various tissues throughout the body, with high concentrations found in the pituitary gland and specific brain regions such as the hypothalamus, ventral tegmental area (VTA), hippocampus, and substantia nigra [19] [17]. Outside the central nervous system, GHS-R1a is also present in peripheral organs including the liver, skeletal muscle, and the heart [17] [21]. The broad distribution of this receptor underscores its involvement in diverse biological functions beyond growth hormone secretion, including the modulation of food intake, glucose and lipid metabolism, gastrointestinal motility, immune function, and cell protection in neuronal and cardiovascular systems [18]. The complexity of GHS-R1a-mediated signaling, coupled with its ability to form heterodimers with other GPCRs, makes it a compelling target for therapeutic interventions in metabolic, neurodegenerative, and age-related diseases [19] [22].
Molecular Structure of GHS-R1a
Genetic Organization and Isoforms
The GHSR gene is located on chromosome 3q26.2 in humans and encodes two distinct transcripts through alternative splicing: GHSR1a and GHSR1b [18] [17]. The GHSR1a isoform is encoded by a 1.1 kb noncontiguous open reading frame divided by a noncoding intron of approximately 2 kb. This transcript produces a functional protein consisting of 366 amino acids with a molecular mass of approximately 41 kDa, featuring the characteristic seven transmembrane domains (TM I-VII) typical of GPCRs [18]. The GHSR1b variant, in contrast, contains 298 amino acids corresponding to the first five transmembrane domains encoded by exon 1, plus a unique 24-amino acid tail encoded by an alternatively spliced intronic sequence [18]. Importantly, GHSR1b does not bind or respond to ghrelin or synthetic GHSs, but it functions as an endogenous modulator by decreasing cell surface expression of GHSR1a and acting as a repressor of its constitutive activity when co-expressed [18] [17].
Structural Domains and Key Residues
As a member of the GPCR family, GHS-R1a contains seven transmembrane α-helix hydrophobic domains connected by three intra- and extracellular loops, beginning with an extracellular N-terminal domain and ending with an intracellular C-terminal domain [18]. The transmembrane domains form a round calyx-like structure with Pro residues positioned centrally within the TM helices [18]. Among the seven TM domains, TM III occupies a central position, while TM V is the most peripheral [18]. Several key amino acid residues are critical for GHS-R1a function, including three conserved residues (Glu140-Arg141-Tyr142) located at the intracellular end of TM III that are essential for the isomerization between active and inactive conformations [18]. Additionally, two conserved cysteine residues (Cys116 and Cys198) on extracellular loops 1 and 2 form a disulfide bond that is crucial for receptor function, as disruption of this bond completely abolishes the activity of all agonists [18].
The ligand binding pocket of GHS-R1a is deep within the cavity created by the TM domains, with the main binding pocket composed of six amino acids located in TM III, TM VI, and TM VII [18]. Specific residues have been identified as critical for ligand binding and receptor activation, including Glu124 in TM III, which is essential for electrostatic interaction with ligands, and Arg283 in TM VI, which interacts with Glu124 and is necessary for both constitutive and agonist-induced signaling [18]. Furthermore, the Glu187 residue in the second extracellular loop is critical for ghrelin binding and GHS-R1a activation [18]. These evolutionarily conserved structural elements highlight the importance of specific molecular interactions in GHS-R1a function and signaling.
Table 1: Key Structural Domains and Residues of GHS-R1a
| Structural Element | Location | Functional Significance |
|---|---|---|
| Transmembrane Domains | TM I-VII | Forms the core receptor structure; TM III central for activation |
| Disulfide Bond | Between Cys116 (ECL1) and Cys198 (ECL2) | Essential for receptor stability and function |
| Conserved Triad | Intracellular end of TM III (Glu140-Arg141-Tyr142) | Critical for isomerization between active/inactive states |
| Ligand Interaction Site | TM III (Glu124), TM VI (Arg283) | Key for ligand binding and receptor activation |
| Ghrelin Binding Site | TM III, VI, and VII | Comprises six amino acids forming the main binding pocket |
| Extracellular Loop 2 | Contains Glu187 | Critical for ghrelin binding and receptor activation |
G-Protein Coupling and Primary Signaling Cascades
Heterotrimeric G-Protein Engagement
Upon binding with ghrelin, GHS-R1a undergoes a conformational change in its transmembrane α-helices, which alters the configuration of the intracellular loops and facilitates interaction with heterotrimeric G-proteins [18]. This interaction triggers the exchange of GDP for GTP on the G protein α subunit, leading to the dissociation of Gα from Gβγ subunits and the initiation of downstream signaling cascades [18]. GHS-R1a exhibits a remarkable ability to couple to multiple G protein families, demonstrating significant promiscuity in G protein coupling that contributes to the diversity of its physiological effects [22]. The receptor preferentially couples to Gαq/11 proteins, but substantial evidence confirms it also engages Gαi/o and Gα12/13 families under various conditions [22]. This multi-G protein coupling capacity allows GHS-R1a to activate several parallel signaling pathways, enabling the receptor to regulate distinct physiological processes in a cell- and context-specific manner.
The constitutive activity of GHS-R1a represents a fundamental aspect of its signaling behavior, with the receptor exhibiting approximately 50% of its maximal signaling capacity even in the absence of agonist stimulation [19] [20]. This intrinsic activity results from the inherent structural properties of the receptor rather than environmental influences [19]. The physiological relevance of this constitutive signaling is demonstrated by naturally occurring mutations that suppress it without affecting ghrelin-mediated activation; these mutations are associated with both obesity and short stature, suggesting that inverse agonism rather than simple antagonism may be required to fully suppress GHS-R1a function in therapeutic contexts [20] [17].
Calcium Mobilization Pathways
The most well-characterized signaling pathway activated by GHS-R1a is the mobilization of intracellular calcium ([Ca2+]i), which serves as a hallmark response to receptor activation [18]. Two primary mechanisms mediate GHS-R1a-induced calcium signaling, with the phospholipase C (PLC)/inositol trisphosphate (IP3) pathway representing the dominant route [18]. Upon Gαq/11 activation, GHS-R1a stimulates PLC activity, leading to the hydrolysis of phosphatidylinositol 4,5-bisphosphate (PIP2) and the generation of IP3 and diacylglycerol (DAG). IP3 then binds to receptors on the endoplasmic reticulum, triggering the release of calcium from intracellular stores [18] [14]. This pathway is particularly important for growth hormone release from pituitary somatotrophs, where calcium serves as a key trigger for hormone secretion [18].
A second, more debated mechanism involves the protein kinase A (PKA)/cAMP pathway [18]. While GHS-R1a primarily couples to Gαq/11, evidence suggests that under certain conditions or in specific cell types, the receptor may influence cAMP levels, potentially through Gαi/o coupling or cross-talk with other signaling systems [14]. Additionally, studies have revealed that GHS-R1a activation can increase resting intracellular calcium levels in skeletal muscle through a mechanism that is not blocked by nifedipine or removal of external Ca2+, suggesting the involvement of intracellular store release rather than voltage-gated calcium channel influx [21]. This pathway in skeletal muscle appears to be mediated through PKC activation and contributes to modifications of the electrical and contractile properties of muscle fibers [21].
Figure 1: G-Protein Coupling and Primary Signaling Cascades of GHS-R1a. The receptor primarily activates Gαq/11, leading to calcium mobilization via the PLC-IP3 pathway, with secondary coupling to Gαi/o and Gαs modulating cAMP levels.
Downstream Intracellular Signaling Networks
Kinase Activation Pathways
Beyond initial second messenger generation, GHS-R1a activation engages multiple downstream kinase pathways that mediate many of its physiological effects. One significant pathway involves the mitogen-activated protein kinase (MAPK) cascade, which plays a crucial role in regulating cell proliferation, differentiation, and survival [17] [22]. GHS-R1a-mediated MAPK activation has been implicated in the receptor's neuroprotective and cardioprotective effects, potentially through the regulation of anti-apoptotic signals [18]. Additionally, GHS-R1a stimulates the protein kinase B (PKB/AKT) pathway, which serves as a central node in metabolic regulation, cell survival, and growth processes [17]. AKT activation by GHS-R1a contributes to the receptor's effects on glucose metabolism and may underlie its ability to promote neuronal and cardiovascular cell protection [18].
Another critical kinase pathway modulated by GHS-R1a is the AMP-activated protein kinase (AMPK) system, a key energy sensor that regulates cellular metabolism [18] [17]. AMPK activation in response to GHS-R1a signaling influences food intake and energy expenditure, particularly in hypothalamic neurons where it integrates information about nutrient status [18]. The mammalian target of rapamycin (mTOR) pathway, which coordinates cell growth with energy availability, is also regulated by GHS-R1a signaling, though the precise mechanisms and functional consequences remain an active area of investigation [18]. The interplay between these kinase pathways allows GHS-R1a to coordinate complex physiological responses that integrate metabolic status with growth and survival signals.
Functional Consequences of Signaling Activation
The diverse signaling pathways activated by GHS-R1a translate into a broad spectrum of physiological effects with important clinical implications. In the central nervous system, GHS-R1a signaling influences neurotransmitter release, synaptic plasticity, and neuronal excitability [17] [21]. These effects underlie the receptor's roles in regulating feeding behavior, reward processing, learning and memory, and neuroprotection [19] [17]. Specifically, GHS-R1a activation in the hippocampus enhances long-term potentiation (LTP) and increases dendritic spine density, cellular correlates of learning and memory [17]. In the ventral tegmental area, GHS-R1a signaling modulates dopamine neuron activity, linking metabolic state with motivated behaviors [17].
In peripheral tissues, GHS-R1a signaling produces equally diverse effects. In skeletal muscle, GHS-R1a activation reduces resting chloride and potassium conductances through a PKC-dependent mechanism, modulating the electrical and contractile properties of muscle fibers [21]. In the cardiovascular system, GHS-R1a signaling exerts protective effects against ischemia and reperfusion damage, independent of growth hormone stimulation [21]. In the pancreas, GHS-R1a influences insulin secretion and glucose homeostasis, while in gastrointestinal tissue, it regulates motility and secretion [18]. The receptor also plays roles in immune function, attenuating proinflammatory cascades and modulating immune responses [18]. This remarkable functional diversity stems from the complex intracellular signaling networks engaged by GHS-R1a in a cell- and tissue-specific manner.
Table 2: Key Downstream Signaling Pathways Activated by GHS-R1a
| Signaling Pathway | Key Mediators | Physiological Consequences |
|---|---|---|
| Calcium Mobilization | PLC, IP3, DAG, PKC | GH secretion, muscle contraction, neuronal excitation |
| MAPK Signaling | ERK1/2, JNK, p38 | Cell proliferation, differentiation, survival |
| Metabolic Regulation | AMPK, AKT | Food intake, glucose homeostasis, energy expenditure |
| cAMP Modulation | PKA, CREB | Gene transcription, synaptic plasticity |
| mTOR Pathway | mTORC1, S6K | Cell growth, protein synthesis, autophagy regulation |
Biased Signaling and Allosteric Modulation
Concepts in Functional Selectivity
GHS-R1a exhibits the phenomenon of biased signaling (also known as functional selectivity), wherein different ligands stabilize distinct receptor conformations that preferentially activate specific downstream signaling pathways over others [22]. This property has profound implications for drug discovery, as it raises the possibility of developing therapeutics that selectively target beneficial pathways while avoiding those responsible for undesirable side effects [22]. For GHS-R1a, biased ligands could potentially separate the growth hormone-releasing effects from the orexigenic actions, or isolate the neuroprotective properties from metabolic effects [22]. The structural basis for biased signaling in GHS-R1a involves specific regions of the receptor, particularly the extracellular loops (ECLs), which serve as critical determinants of both ligand-dependent and -independent bias [22].
Several naturally occurring mutations in GHS-R1a provide compelling evidence for the physiological relevance of biased signaling. For instance, the Ala204Glu mutation in the second extracellular loop markedly reduces ghrelin-induced β-arrestin signaling efficacy without significantly affecting ghrelin binding or G protein signaling [22]. Mice expressing the homologous ECL2 mutation display reduced ghrelin-stimulated food intake and growth hormone secretion, along with age-dependent reductions in body weight and length [22]. Similarly, the Phe279Leu mutation also abolishes GHS-R1a constitutive activity and is associated with abnormal body weight in humans [22]. These observations highlight the potential for developing biased ligands that target specific signaling outcomes for therapeutic purposes.
Receptor Oligomerization and Allosteric Modulation
GHS-R1a has the capacity to form both homodimers (with itself) and heterodimers with other GPCRs, significantly expanding its signaling versatility and functional repertoire [19] [17] [22]. Known heterodimerization partners include the dopamine D1 and D2 receptors, serotonin 2C receptor (5-HT2cR), melanocortin-3 receptor (MC3R), somatostatin receptor-5 (SST5), orexin 1 receptor (OX1R), and the GHSR1b splice variant [19] [17]. These dimeric complexes exhibit altered signaling properties, trafficking patterns, and ligand binding characteristics compared to the monomeric receptors [22]. For example, heterodimerization with dopamine receptors potentially links ghrelin signaling to dopaminergic pathways, which may be relevant for reward processing and feeding behavior [17].
In addition to dimerization, GHS-R1a function is modulated by interactions with accessory proteins such as melanocortin receptor accessory protein 2 (MRAP2) [22]. MRAP2 interacts with GHS-R1a in hypothalamic and pancreatic cells, where it blunts constitutive activity and biases ghrelin-stimulated signaling toward Gq over β-arrestin pathways [22]. This interaction appears to be required for ghrelin's orexigenic and insulinostatic effects, highlighting the importance of accessory proteins in shaping GHS-R1a signaling outcomes [22]. The discovery of these complex modulatory mechanisms reveals multiple layers of regulation that fine-tune GHS-R1a signaling in different physiological contexts, offering additional targets for therapeutic intervention.
Experimental Protocols for GHS-R1a Signaling Studies
Calcium Mobilization Assay
The calcium mobilization assay represents a fundamental method for investigating GHS-R1a activation and function, particularly given that increased intracellular calcium concentration ([Ca2+]i) serves as a hallmark response to receptor activation [18] [23]. This protocol utilizes fluorescent calcium indicators such as Fura-2 to measure real-time changes in intracellular calcium levels following receptor stimulation.
Protocol Steps:
- Cell Preparation: Culture cells expressing GHS-R1a (e.g., HEK293 cells transiently or stably transfected with GHSR1a cDNA) on appropriate imaging plates to achieve 70-90% confluency at time of assay [18].
- Dye Loading: Incubate cells with Fura-2 AM (4-5 μM) in assay buffer for 45-60 minutes at 37°C protected from light [21].
- Dye Removal and Equilibration: Replace dye-containing solution with fresh assay buffer and incubate for an additional 30 minutes to allow complete ester hydrolysis of the acetoxymethyl (AM) ester form to the active free acid form.
- Calcium Measurement: Place the plate in a fluorescence plate reader or imaging system with temperature control maintained at 37°C. Monitor fluorescence emission at 510 nm while alternating excitation between 340 nm and 380 nm.
- Ligand Application: After establishing a stable baseline, add ghrelin or test compounds at various concentrations and continue recording for several minutes to capture the calcium response.
- Data Analysis: Calculate the 340/380 nm fluorescence ratio and plot against time. Determine peak responses and EC50 values using appropriate nonlinear regression analysis.
Key Applications:
- Characterization of agonist potency and efficacy at GHS-R1a
- Assessment of antagonist/inverse agonist activity through inhibition of ghrelin responses
- Investigation of GHS-R1a constitutive activity by measuring basal calcium levels
- Study of allosteric modulators in combination with orthosteric ligands
GTPγS Binding Assay
The guanosine 5'-O-[γ-thio]triphosphate (GTPγS) binding assay provides a direct measure of G protein activation following receptor stimulation, making it particularly valuable for studying the initial steps in GHS-R1a signaling and its coupling preferences to different G protein families [20].
Protocol Steps:
- Membrane Preparation: Prepare membranes from cells expressing GHS-R1a (e.g., HEK293 cells transfected with ghrelin receptor cDNA and/or specific G protein subunits) using differential centrifugation [20].
- Reaction Mixture: Combine membranes (10-20 μg protein) in assay buffer containing 20 mM HEPES, 100 mM NaCl, 10 mM MgCl2, and 0.1% bovine serum albumin (BSA) [20].
- GDP Addition: Include 10 μM GDP in the reaction mixture to suppress basal G protein activity and enhance signal-to-noise ratio [20].
- Ligand Pre-incubation: Add varying concentrations of ghrelin, test compounds, or vehicle control and incubate for 5-10 minutes at room temperature.
- Initiate Reaction: Add [35S]GTPγS (0.1-0.6 nM final concentration) and continue incubation for 60-120 minutes at 30°C with gentle agitation [20].
- Termination and Detection: Terminate reactions by rapid filtration through GF/C filters using a cell harvester, followed by multiple washes with ice-cold buffer. Measure bound radioactivity by liquid scintillation counting [20].
- Data Analysis: Calculate specific binding by subtracting nonspecific binding (determined in the presence of excess unlabeled GTPγS). Fit concentration-response curves using nonlinear regression to determine EC50 and Emax values.
Key Applications:
- Determination of G protein coupling efficiency and preferences
- Assessment of ligand efficacy and potency in receptor activation
- Investigation of constitutive GHS-R1a activity through basal GTPγS binding
- Study of allosteric modulators in combination with orthosteric ligands
Dynamic Mass Redistribution Assay
The dynamic mass redistribution (DMR) assay provides a label-free, holistic approach to monitoring integrated cellular responses following GHS-R1a activation, capturing the complex downstream signaling events beyond initial G protein activation [23].
Protocol Steps:
- Cell Preparation: Seed cells expressing GHS-R1a onto specialized biosensor-compatible microplates and culture until形成 confluent monolayer (typically 24-48 hours).
- Equilibration: Pre-equilibrate the cell plate and all reagents in the assay instrument to minimize thermal perturbations during measurement.
- Baseline Recording: Measure baseline DMR signal for approximately 10 minutes to establish stability before compound addition.
- Ligand Application: Add ghrelin or test compounds using integrated fluidics while continuously monitoring the DMR response.
- Signal Monitoring: Continue recording for at least 60-90 minutes to capture the full temporal profile of the cellular response.
- Data Analysis: Extract key parameters from the DMR response curves including amplitude, kinetic profiles, and integrated response areas. Apply multivariate analysis to classify response patterns.
Key Applications:
- Comprehensive profiling of functional responses to GHS-R1a ligands
- Identification of biased signaling profiles through distinct kinetic signatures
- Investigation of allosteric modulator effects on receptor signaling
- Assessment of pathway-selective activation in different cellular contexts
Figure 2: Experimental Workflow for Key GHS-R1a Signaling Assays. Three primary methodologies for investigating GHS-R1a function: Calcium mobilization for downstream signaling, GTPγS binding for G protein activation, and dynamic mass redistribution for integrated cellular responses.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for GHS-R1a Signaling Studies
| Reagent Category | Specific Examples | Research Applications |
|---|---|---|
| GHS-R1a Agonists | Ghrelin, Capromorelin, MK-677 (Ibutamoren), GHRP-6, Hexarelin, L-692,585 [9] [20] [24] | Receptor activation studies, pathway characterization, in vivo efficacy testing |
| GHS-R1a Antagonists/Inverse Agonists | [D-Lys-3]-GHRP-6, [D-Arg1, D-Phe5, D-Trp7,9, Leu11]-Substance P, Cortistatin-8, LEAP-2, GSK1614343, PF-05190457 [20] [22] [21] | Blockade of ghrelin responses, assessment of constitutive activity, control experiments |
| Cell Lines | HEK293 transfected with GHSR1a, CHO cells expressing GHSR1a, Pituitary-derived cell lines, Neuronal cultures [18] [20] | In vitro signaling studies, high-throughput screening, mechanistic investigations |
| Antibodies | Anti-GHSR1a antibodies, Phospho-specific antibodies (pERK, pAKT, pAMPK), Secondary detection antibodies [18] [22] | Receptor localization, expression analysis, pathway activation assessment |
| Signal Transduction Assay Kits | Calcium flux assays (Fura-2, Fluo-4), cAMP detection kits, IP3 accumulation assays, ERK/MAPK phosphorylation kits [18] [23] [21] | Quantification of specific signaling pathway activation |
| Animal Models | GHSR knockout mice, Tissue-specific GHSR conditional knockouts, Aged rat models [19] [22] [21] | In vivo validation, physiological relevance assessment, therapeutic potential evaluation |
Clinical Applications and Therapeutic Context
Growth Hormone Secretagogues in Clinical Trials
The understanding of GHS-R1a signaling pathways has direct relevance to the clinical development of growth hormone secretagogues such as MK-677 (Ibutamoren) and capromorelin for various therapeutic applications. Capromorelin, a selective ghrelin receptor agonist, has demonstrated efficacy in promoting weight gain in cat models with chronic kidney disease, with a treatment effect of +6.81% body weight compared to placebo over 55 days [9]. In aged rats, chronic treatment with capromorelin and similar compounds has shown potential for increasing lean body mass and improving functional performance measures such as stair climb and tandem walk [14]. These effects are mediated through the GHS-R1a receptor, which upon activation stimulates growth hormone secretion and subsequently increases insulin-like growth factor 1 (IGF-1) release from the liver, promoting anabolic metabolism [9].
Recent research has revealed a more nuanced role for GHS-R1a agonists beyond simple appetite stimulation. These compounds appear to function as nutrient sensors that not only stimulate food-seeking behaviors but also directly promote weight gain with increases in both adipose and lean body mass [9]. Importantly, ghrelin and its mimetics may target muscle cells directly, resulting in improved muscle strength and survival independent of growth hormone release [9]. This direct action on muscle tissue has significant implications for treating conditions such as sarcopenia and cachexia, where preservation of lean body mass is clinically important. Clinical trials in elderly human subjects have demonstrated that capromorelin treatment for 12 months increased body weight, lean body mass, and improved functional performance measures including tandem walk and stair climbing ability [14].
Signaling Pathways in Therapeutic Effects
The diverse therapeutic effects of GHS-R1a agonists can be mapped onto specific intracellular signaling pathways, offering opportunities for improved therapeutic targeting through biased ligand development. The growth hormone-releasing effects primarily involve Gαq/11-mediated calcium mobilization in pituitary somatotrophs, leading to growth hormone secretion and subsequent increases in IGF-1 levels [18] [9]. The orexigenic effects (appetite stimulation) involve multiple pathways, including AMPK activation in hypothalamic neurons and modulation of neuropeptide Y (NPY) and agouti-related peptide (AgRP) expression [18] [17]. The metabolic effects on glucose and lipid homeostasis involve complex interactions between central nervous system signaling and peripheral actions in tissues such as liver, muscle, and pancreas, with both G protein-dependent and β-arrestin-mediated pathways contributing to these effects [18] [22].
The direct effects on muscle function appear to involve PKC-mediated pathways that modulate ion channel activity, particularly resting chloride and potassium conductances [21]. In skeletal muscle, GHS-R1a activation reduces chloride conductance through inhibition of ClC-1 channels and decreases potassium conductance, resulting in altered electrical properties and contractile function [21]. These peripheral actions may account for some of the functional improvements observed with GHS-R1a agonist treatment in age-related muscle wasting conditions. Additionally, the neuroprotective and cardioprotective effects of GHS-R1a activation likely involve MAPK and AKT signaling pathways that promote cell survival and inhibit apoptotic processes [18]. The emerging understanding of these pathway-specific effects provides a roadmap for developing next-generation GHS-R1a-targeted therapeutics with improved efficacy and safety profiles.
The signaling pathways activated by GHS-R1a represent a complex network of intracellular events that translate receptor activation into diverse physiological effects. From the initial G protein coupling events through to the engagement of downstream kinase cascades, the receptor demonstrates remarkable signaling versatility that underlies its pleiotropic functions. The concepts of constitutive activity, biased signaling, and receptor oligomerization add layers of complexity to GHS-R1a pharmacology, while simultaneously offering opportunities for more precise therapeutic interventions. The experimental approaches outlined provide robust methodologies for investigating these signaling mechanisms, essential for advancing both basic understanding and clinical applications of GHS-R1a-targeted compounds. As research continues to elucidate the intricate relationships between specific signaling pathways and physiological outcomes, the potential for developing increasingly selective GHS-R1a modulators for conditions ranging from growth disorders to metabolic diseases and age-related musculoskeletal decline continues to expand.
Growth Hormone Secretagogues (GHS) represent a class of compounds that stimulate growth hormone (GH) release through a distinct mechanism from endogenous growth hormone-releasing hormone (GHRH). The discovery of the GHS receptor (GHSR) and its endogenous ligand, ghrelin, opened new avenues for therapeutic intervention in conditions of GH deficiency, age-related frailty, and muscle wasting disorders [25] [26]. Preclinical research utilizing animal models has been instrumental in elucidating the complex mechanisms of GHS action, their effects on somatic growth, and their potential clinical applications. This application note synthesizes key insights from animal studies on two prominent GHS compounds—MK-677 (ibutamoren) and capromorelin—providing researchers with structured data, experimental protocols, and mechanistic frameworks to guide future investigational strategies.
The therapeutic promise of GHS lies in their ability to rejuvenate the pulsatile secretion of GH, thereby restoring the GH/insulin-like growth factor-1 (IGF-1) axis to a more youthful pattern without the need for direct GH injection [25]. Unlike recombinant GH therapy, which bypasses natural regulatory mechanisms, GHS promote an endogenous, pulsatile GH release that remains subject to normal feedback inhibition, potentially reducing the risk of hyperstimulation [25]. Animal models ranging from rodents to canines have provided critical evidence for both the efficacy and limitations of these compounds, highlighting the complex neuroendocrine adaptations that occur with prolonged GHS administration.
Quantitative Outcomes in Animal Models
Table 1: Comparative Effects of GHS Administration in Preclinical Models
| Model System | Compound & Dose | Duration | Key GH/IGF-1 Outcomes | Somatic/Growth Measures | Molecular Adaptations |
|---|---|---|---|---|---|
| Sprague-Dawley Rats [27] | MK-677 (4 mg/kg/day, oral) | 6 weeks | Initial 1.8-fold ↑ in peak GH; No sustained IGF-1 increase | No significant change in body length, weight, or tibial growth plate width | ↑ Hypothalamic somatostatin (SST) mRNA & protein; ↓ Pituitary SSTR2 |
| mdx Mice (DMD model) [28] | EP80317 / JMV2894 (320 µg/kg/d, s.c.) | 8 weeks | No detectable GHSR1a transcript; No circulating IGF-1 increase | ↑ Forelimb force; ↓ Diaphragm & gastrocnemius echodensity (fibrosis) | ↓ TGF-β1, Col1a1, IL-6, CD68; ↑ Sirt-1, PGC-1α, MEF2c |
| mdx Mice (DMD model) [28] | JMV2894 (320 µg/kg/d, s.c.) | 8 weeks | Receptor-independent actions | Improved ex vivo diaphragm isometric force & calcium indices | Direct anti-fibrotic action; Potential binding to ADAMTS-5 & MMP-9 |
| Healthy Older Dogs [29] | GHRH plasmid (pVAX1 vector, electroporation) | 180 days | Bidirectional IGF-1 modulation (↑ if low baseline) | ↑ Limb thickness (muscle mass surrogate); ↑ Activity & exercise tolerance | ↑ Naïve CD4+ & CD8+ T cells; Potential immunosenescence delay |
Detailed Experimental Protocols
Protocol: Evaluating Acute and Chronic GH Response to MK-677 in Rats
This established protocol assesses the GH stimulatory effect and growth-promoting potential of orally administered GHS in a rodent model [27].
- Animal Model: Female Sprague-Dawley rats (approximately 4 weeks old). House under standard conditions (21±2°C, 60±10% humidity, 12-h light/dark cycle) with free access to chow and water.
- Formulation: Prepare MK-677 at 1 mg/mL in distilled water. Administer via stomach tube. Use distilled water (4 mL/kg) as vehicle control.
- Acute GH Secretion: After an 8-hour fast, administer MK-677 (2 or 4 mg/kg). Collect blood samples from the tail vein at 0, 30, 60, 90, and 120 minutes post-administration. Centrifuge samples to harvest plasma, and store at -70°C until GH analysis by ELISA.
- Chronic Growth Study: Administer MK-677 (4 mg/kg/day) via stomach tube between 08:00 and 10:00 for 6 weeks. Measure body weight and body length (nose-to-anus) daily. Collect blood samples every 2 weeks for IGF-I measurement. Following the treatment period, euthanize animals and collect tissues for analysis.
- Tissue Analysis: Isolate pituitary gland and hypothalamus. Assess mRNA expression of GH, GHRH, GHSR, SST, and somatostatin receptors (SSTRs) using RT-PCR. Analyze protein expression via Western immunoblotting with specific antibodies (GHSR, SST, SSTR-2, SSTR-5).
- Histological Examination: For tibia growth plate analysis, fix right tibia in 4% paraformaldehyde for 24 hours. Decalcify in EDTA-G solution for 10-14 days at 4°C. Embed in paraffin, section at 5 µm, and stain with hematoxylin and eosin to measure growth plate width.
Protocol: Assessing Functional and Anti-fibrotic Effects of GHS in mdx Mice
This protocol evaluates the therapeutic potential of GHS in Duchenne muscular dystrophy (DMD) model, focusing on functional improvement and pathology modulation [28].
- Animal Model: Male mdx mice (C57BL/10ScSnDmdmdx/J) and wild-type controls (C57BL/10ScSn/J). Begin treatment at 4 weeks of age.
- Test Compounds: EP80317 and JMV2894 (GHS compounds). Synthesize compounds in-house and verify purity. Dissolve in appropriate vehicle for subcutaneous injection.
- Dosing Regimen: Administer compounds at 320 µg/kg/day subcutaneously for 8 weeks. Include vehicle-treated mdx and wild-type control groups.
- In vivo Functional Assessment:
- Forelimb Grip Strength: Measure weekly using a grip strength meter. Calculate recovery score as: (GHS-treated mdx - vehicle mdx) / (wild-type - vehicle mdx) × 100.
- Muscle Echodensity: Use high-resolution ultrasound to assess fibrosis in diaphragm and gastrocnemius muscle at baseline and endpoint.
- Ex vivo Muscle Function: Following treatment, euthanize animals and excise diaphragm muscle. Measure isometric force production and calcium-related indices in an ex vivo muscle bath system.
- Molecular and Histological Analysis:
- Gene Expression: Isolate RNA from muscle tissues. Analyze expression of fibrotic (TGF-β1, Col1a1), inflammatory (IL-6, CD68), and metabolic (Sirt-1, PGC-1α, MEF2c) markers using RT-qPCR.
- Fibrosis Quantification: Stain muscle cross-sections with Masson's Trichrome or Picrosirius Red to visualize collagen deposition. Quantify fibrotic area using image analysis software.
- Receptor Expression Analysis: Examine GHSR1a transcript levels in skeletal muscle tissues using sensitive detection methods (RT-PCR, RNase protection assay).
Signaling Pathways and Mechanisms of Action
The mechanistic diagram illustrates the dual pathway through which GHS modulate GH secretion: (1) direct stimulation of GHRH neurons and (2) inhibition of somatostatin (SST)-producing neurons in the hypothalamus [25] [30]. This combined action results in amplified pulsatile GH release from pituitary somatotrophs. Chronic administration studies in rats reveal adaptive neuroendocrine changes, including marked upregulation of hypothalamic SST expression and decreased pituitary SSTR2 receptor expression, potentially explaining the observed desensitization to GHS over time [27]. Importantly, certain GHS compounds demonstrate receptor-independent actions, particularly in dystrophic muscle, where they exert direct anti-fibrotic effects and improve calcium handling without detectable GHSR1a transcript or increased circulating IGF-1 [28].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for GHS Investigations
| Reagent / Material | Function & Application | Example Usage in Preclinical Studies |
|---|---|---|
| MK-677 (Ibutamoren) | Orally active, non-peptide GHSR agonist; induces pulsatile GH release | Chronic growth studies in rats; GH secretion kinetics [25] [27] |
| Capromorelin | Orally active GHS with shorter half-life; increases IGF-1 and lean body mass | Studies in older adults; functional decline models [25] |
| EP80317 & JMV2894 | Synthetic GHS compounds with anti-fibrotic properties; potential receptor-independent actions | DMD mdx mouse model; muscle function and fibrosis studies [28] |
| GHSR1a Antibodies | Detection and quantification of GHS receptor expression in tissues | Western immunoblotting in hypothalamic and pituitary tissues [27] |
| GH & IGF-1 ELISA Kits | Quantitative measurement of hormone levels in serum/plasma | Monitoring acute GH response and chronic IGF-1 elevation [27] |
| Somatostatin (SST) & SSTR Antibodies | Analysis of inhibitory pathway components in neuroendocrine tissues | Investigating feedback mechanisms and desensitization [27] |
| DMD mdx Mouse Model | Dystrophin-deficient model for neuromuscular pathology | Evaluating GHS effects on muscle function, fibrosis, and inflammation [28] |
Discussion and Research Implications
The preclinical evidence synthesized in this application note reveals both the promise and complexity of GHS therapeutics. While MK-677 demonstrates robust initial GH stimulation, its inability to promote longitudinal growth in rats despite elevated GH pulses highlights the critical importance of counter-regulatory mechanisms, particularly somatostatin upregulation [27]. This desensitization phenomenon represents a significant challenge for clinical translation that requires further mechanistic investigation.
The contrasting findings in mdx mouse models suggest alternative pathways for GHS action beyond traditional GH/IGF-1 axis stimulation. The significant functional improvements and anti-fibrotic effects observed with EP80317 and JMV2894 administration, independent of GHSR1a signaling or IGF-1 elevation, indicate these compounds may have direct effects on muscle pathophysiology [28]. This receptor-independent activity, potentially through interaction with metalloproteases like ADAMTS-5 and MMP-9, opens new avenues for therapeutic development in muscular dystrophies and other fibrotic disorders.
From a research perspective, these findings highlight several critical considerations for future preclinical studies: (1) the necessity of including chronic administration protocols to identify adaptive neuroendocrine responses; (2) the importance of evaluating both GH/IGF-1 dependent and independent mechanisms of action; and (3) the value of utilizing multiple animal models that address specific research questions, from somatic growth to neuromuscular pathology. The bidirectional modulation of IGF-1 observed in canine studies with GHRH therapy further suggests that baseline endocrine status significantly influences treatment response, an important factor for clinical trial design [29].
As research advances, the development of next-generation GHS compounds that minimize desensitization while maximizing beneficial anabolic and anti-fibrotic effects represents a promising frontier. The integration of these preclinical insights will be essential for optimizing therapeutic strategies that target the GH/IGF-1 axis across a spectrum of clinical conditions.
Clinical Trial Designs and Efficacy Endpoints: Analyzing Human Studies of MK-677 and Capromorelin
Application Note: Clinical Trial Designs for Growth Hormone Secretagogues
Growth Hormone Secretagogues (GHSs) represent a class of therapeutic agents that stimulate the endogenous release of growth hormone (GH) by targeting the ghrelin receptor (GHS-R1a) in the pituitary and hypothalamus [31] [32]. Unlike exogenous GH administration, GHSs promote a more physiological, pulsatile release of GH that is subject to the body's natural feedback mechanisms, potentially offering a superior safety profile [32] [26]. This application note provides a consolidated reference of pivotal trial designs for key GHS compounds, detailing population demographics, dosing regimens, and study durations to inform clinical development strategies for researchers and drug development professionals. The data herein are framed within the broader objective of establishing GHSs as viable treatments for conditions of muscle wasting, cachexia, and GH deficiency.
Comparative Analysis of GHS Clinical Trials
Table 1: Overview of Pivotal GHS Clinical Trial Designs
| GHS Compound | Target Indication | Study Duration | Population Demographics & Key Criteria | Dosing Regimen |
|---|---|---|---|---|
| LUM-201 [31] | Pediatric Growth Hormone Deficiency (GHD) | 12-month primary endpoint; up to 3-year extension | N=150; Prepubertal, treatment-naïve children with GHD. PEM-positive: IGF-1 >30 ng/mL and peak GH ≥5 ng/mL after LUM-201 test dose. | 1.6 mg/kg/day, oral |
| Ibutamoren (MK-0677) [32] | Sarcopenia/Frailty in Elderly | 12 months | Older adults (age 60-81 years) with mild functional limitation. | Once daily, oral |
| Capromorelin [32] | Sarcopenia/Frailty in Elderly | Not specified (study terminated early for efficacy) | Older adults with mild functional limitation. | Once daily, oral |
| Anamorelin (RC-1291) [33] | Cancer Anorexia-Cachexia Syndrome (CACS) | 12 weeks | Patients with cancer cachexia. | 25 mg, 50 mg, or 75 mg, once daily, oral |
| Ghrelin (synthetic) [34] | Cachexia (CHF, COPD) | 3 weeks | Patients with congestive heart failure (CHF) or chronic obstructive pulmonary disease (COPD). | Intravenous injections |
Table 2: Efficacy and Safety Outcomes from GHS Clinical Trials
| GHS Compound | Primary Efficacy Endpoints | Key Efficacy Outcomes | Reported Safety Findings |
|---|---|---|---|
| LUM-201 [31] | Growth velocity over 12 months | Increased IGF-1; increased height SDS | Safety monitoring includes lab tests, ECGs, and adverse events |
| Ibutamoren (MK-0677) [32] | Body composition, functional measures | Increased lean body mass; increased GH and IGF-1 to youthful levels; reversal of nitrogen wasting | Mild increases in blood glucose and insulin resistance; musculoskeletal pain; fluid retention |
| Capromorelin [32] | Body composition, functional measures | Increased body weight, lean body mass, walking speed, and stair climbing power | Small increases in fasting glucose and glycosylated hemoglobin |
| Anamorelin (RC-1291) [33] | Body weight, appetite | Increased body weight (1.25-1.16 kg vs placebo); dose-dependent increase in GH and IGF-1; improved appetite | Mild increases in insulin resistance |
| Ghrelin (synthetic) [34] | Body weight, cytokine levels | Increased food intake (27-28%); improved lean body mass; decreased proinflammatory cytokines | Well-tolerated; mild and transient side effects (abdominal discomfort, flushing, somnolence) |
Experimental Protocols for Key GHS Assessments
Protocol 1: Predictive Enrichment Marker (PEM) Stratification for Patient Selection
Objective: To identify GHD patients who are likely responders to LUM-201 therapy by assessing the functional integrity of their GH secretion pathway [31].
Methodology:
- Screening: Obtain informed consent from treatment-naïve, prepubertal children with a confirmed diagnosis of GHD.
- Baseline Blood Sample: Collect a baseline blood sample to measure fasting IGF-1 concentration. A level >30.0 ng/mL is required for provisional eligibility.
- LUM-201 Challenge Test: Administer a single oral dose of LUM-201 at 1.6 mg/kg.
- Post-Dose Blood Sampling: Collect serial blood samples at predetermined intervals (e.g., 30, 60, 90 minutes) post-administration to measure peak serum GH concentration.
- PEM Classification: A patient is classified as "PEM-positive" if their peak GH concentration is ≥5.0 ng/mL following the challenge dose. Only PEM-positive subjects are eligible for randomization in the pivotal trial.
Materials:
- LUM-201
- Phlebotomy kit
- IGF-1 and GH immunoassay kits
- Centrifuge and -80°C freezer for sample processing and storage
Protocol 2: Assessment of Body Composition and Physical Function in Sarcopenia Trials
Objective: To evaluate the efficacy of GHSs (e.g., Ibutamoren, Capromorelin) on muscle mass and physical performance in elderly subjects [32].
Methodology:
- Randomization: Randomize eligible older adults (e.g., 60-85 years) with mild functional limitations to receive either the GHS or a matched placebo once daily.
- Baseline and Periodic Assessments:
- Body Composition: Measure lean body mass (LBM) and fat mass at baseline, 6 months, and 12 months using Dual-Energy X-ray Absorptiometry (DEXA).
- Muscle Strength: Assess handgrip strength using a hand dynamometer and lower body strength via one-repetition maximum (1-RM) leg press at the same intervals.
- Physical Function: Evaluate functional capacity using timed tests such as gait speed (4-meter walk), chair rise test, and stair climbing power at baseline and follow-up visits.
- Biochemical Analysis: Draw fasting blood samples at each visit to quantify GH, IGF-1, and IGFBP-3 levels. Monitor safety markers, including fasting glucose and HbA1c.
Materials:
- DEXA scanner
- Hand dynamometer
- Leg press machine
- Stopwatch, chair, marked walkway
- Phlebotomy kit and immunoassay analyzers
Signaling Pathways of Ghrelin and Growth Hormone Secretagogues
Diagram 1: GHS Mechanisms of Action. GHSs act through GHS-R1a-dependent and independent pathways to stimulate GH release, increase appetite, promote anabolism, and exert anti-inflammatory effects [33] [26] [34].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for GHS Investigations
| Reagent/Material | Function/Application | Example in Context |
|---|---|---|
| GHS Compounds | Act as agonists for the GHS-R1a to stimulate endogenous GH release. | LUM-201, Ibutamoren (MK-0677), Capromorelin, Anamorelin [31] [32]. |
| Immunoassay Kits | Quantify hormone and biomarker levels in serum/plasma. | IGF-1, GH, and IGFBP-3 kits for monitoring pharmacodynamic response and efficacy [31] [32]. |
| Cell Lines Engineered to Over-Express GHS-R1a | Used for in vitro screening of GHS activity and receptor binding studies. | Critical for the initial identification of ghrelin and for characterizing receptor-ligand interactions [26]. |
| DEXA Scanner | Precisely measures body composition (lean mass, fat mass) in clinical trials. | Used to assess primary efficacy outcomes in sarcopenia and cachexia trials [32]. |
| Animal Models of Cachexia/Sarcopenia | Preclinical models for evaluating the therapeutic potential of GHSs. | Tumor-bearing mice for cachexia; aged mice or rodent models of muscle wasting for sarcopenia [33] [34]. |
| RT-PCR/Western Blot Reagents | Analyze gene and protein expression of markers like MuRF1 and atrogin-1 in muscle. | Used to investigate the molecular mechanisms behind GHS-mediated protection against muscle proteolysis [34]. |
Growth Hormone Secretagogues (GHS), such as MK-677 (ibutamoren) and capromorelin, represent a class of orally active compounds that stimulate the endogenous release of growth hormone (GH) and insulin-like growth factor-1 (IGF-1) by acting as ghrelin receptor agonists [14] [26]. These agents have been investigated extensively in clinical trials for their potential to counteract age-related and disease-associated declines in muscle mass and function. This document provides a structured analysis of primary efficacy endpoints—specifically changes in lean body mass, appendicular fat, and body weight—from key clinical studies, serving as a reference for researchers and drug development professionals working in metabolic disorders and sarcopenia.
Quantitative Efficacy Data from Clinical Trials
Clinical trials have consistently demonstrated that GHS administration significantly impacts body composition parameters. The data below summarize key findings from human studies.
Table 1: Efficacy of MK-677 (Ibutamoren) in Healthy Older Adults Over 12 Months [25] [35]
| Body Composition Parameter | Placebo Group Change (kg) | MK-677 Group Change (kg) | P-value |
|---|---|---|---|
| Fat-Free Mass (FFM) | -0.5 (95% CI, -1.1 to 0.2) | +1.1 (95% CI, 0.7 to 1.5) | <0.001 |
| Total Appendicular FFM | -0.3 (95% CI, -0.6 to 0.1) | +0.5 (95% CI, 0.3 to 0.8) | <0.001 |
| Body Weight | +0.8 (95% CI, -0.3 to 1.8) | +2.7 (95% CI, 2.0 to 3.5) | 0.003 |
| Increase in Total Appendicular Fat | +0.24 | +1.1 | 0.001 |
In a two-year, double-blind, placebo-controlled trial, 65 healthy older adults received either 25 mg of MK-677 or placebo daily. The GH and IGF-I levels in the MK-677 group were significantly increased to profiles typical of healthy young adults. The data show that MK-677 not only prevented the age-related decline in FFM but actively increased it, while also leading to a significant increase in body weight and a specific increase in appendicular fat [35].
Table 2: Efficacy of Capromorelin in Older Adults with Functional Limitations Over 12 Months [14] [25]
| Parameter | Capromorelin Effect | Clinical Outcome |
|---|---|---|
| Lean Body Mass | Increased | Sustained gains observed |
| Body Weight | Increased | Consistent with LBM and fat mass gains |
| Physical Function | Improved | Increased stair climb power and tandem walking speed |
A study of 395 older adults (65-84 years) receiving various dosing regimens of capromorelin demonstrated sustained gains in body weight and lean body mass over one year. Importantly, this study also reported improvements in functional performance measures, a key differentiator from some other GHS trials [14] [25].
Table 3: Efficacy of Capromorelin in Cats with Chronic Kidney Disease (55-Day Study) [9]
| Parameter | Capromorelin Group (Mean Change) | Placebo Group (Mean Change) | Treatment Effect (Capromorelin - Placebo) | P-value |
|---|---|---|---|---|
| Body Weight | +5.18% (95% CI, 3.45–6.91) | -1.65% (95% CI, –3.82 to 0.55) | +6.81% (95% CI, 4.21–9.42) | <0.0001 |
| Absolute Body Weight | - | - | +0.25 kg (95% CI, 0.15–0.35) | - |
A randomized, placebo-controlled field study in client-owned cats with chronic kidney disease and unintended weight loss showed that capromorelin was highly effective in promoting weight gain over a 55-day treatment period, reversing the weight loss observed in the placebo group [9].
Experimental Protocols for Key Clinical Endpoints
Protocol: Body Composition Assessment via Dual-Energy X-ray Absorptiometry (DXA)
Objective: To quantitatively measure changes in fat-free mass, total fat mass, and regional (appendicular) body composition in response to GHS treatment.
Methodology:
- Instrumentation: Use a Hologic QDR-2000 densitometer or equivalent. Calibrate the device daily according to manufacturer specifications.
- Subject Preparation: Subjects should fast for a minimum of 4 hours prior to scanning and wear light, metal-free clothing.
- Positioning: Position the subject supine on the scanning table with limbs slightly abducted from the body, as per the manufacturer's positioning guidelines.
- Scanning and Analysis: Perform a total body scan. Analyze the scan using the manufacturer's software to determine:
- Total Fat-Free Mass (FFM)
- Total Fat Mass
- Appendicular Lean Soft Tissue: Sum of lean mass in both arms and legs, used as an estimate of total skeletal muscle mass.
- Appendicular Fat Mass: Sum of fat mass in both arms and legs.
- Data Normalization: Calculate the relative skeletal muscle index as TASM (kg)/height (m²) to normalize for stature [35].
- Frequency: Conduct scans at baseline, 6 months, and 12 months during long-term trials.
Protocol: Body Weight and Functional Correlation
Objective: To monitor changes in total body weight and correlate with functional performance measures.
Methodology:
- Body Weight Measurement: Use a calibrated digital scale. Measure weight to the nearest 0.1 kg with the subject in light clothing without shoes.
- Functional Tests:
- Stair Climb Power: Time the subject as they ascend a standard flight of stairs (e.g., 10 steps) as quickly as possible. Calculate power output [14].
- Tandem Walk: Assess dynamic balance by having the subject walk in a straight line, placing the heel of one foot directly in front of the toes of the other. Measure speed and/or errors [14].
- 6-Minute Walk: Measure the total distance walked in 6 minutes along a pre-measured, flat corridor [14].
- Schedule: Perform weight and functional measurements at baseline and each scheduled visit (e.g., Days 15, 27, and 55 in an 8-week study) [9].
Signaling Pathways and Experimental Workflows
GHS Signaling Pathway
The following diagram illustrates the mechanism of action of MK-677 and capromorelin via the ghrelin receptor.
Clinical Trial Workflow for Body Composition Endpoints
The following diagram outlines a standardized workflow for a clinical trial assessing the primary efficacy endpoints of GHS.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Materials for GHS Research
| Item | Function/Application in Research | Example/Note |
|---|---|---|
| MK-677 (Ibutamoren) | Orally active GHS; research standard for long-term GH pulsatility restoration. | Typically administered at 25 mg/day in clinical studies [25] [35]. |
| Capromorelin | Orally active GHS; used in studies focusing on functional improvement and weight gain. | Dosed at 2 mg/kg in feline studies; various regimens (e.g., 10 mg/day) in human trials [14] [9]. |
| Recombinant Human GH | Positive control for GH receptor pathway activation; comparator for GHS efficacy. | Used in parallel studies to contrast exogenous vs. endogenous GH elevation [36]. |
| ELISA Kits (GH, IGF-1) | Quantification of serum GH and IGF-1 levels to confirm target engagement. | Essential for monitoring hormonal response in pre-clinical and clinical settings [27]. |
| GHSR1a Antibodies | Detection and localization of GHS receptor expression in tissue samples. | Used in Western immunoblotting and immunohistochemistry [27]. |
Within clinical trials for function-promoting therapies, such as growth hormone secretagogues (GHS) like MK-0677 (ibutamoren) and capromorelin, the selection of robust, responsive, and clinically meaningful functional outcome measures is paramount [25] [32] [37]. Demonstrating efficacy requires moving beyond simple physiological biomarkers to performance-based measures that directly reflect a patient's physical capacity and functional independence. This document provides detailed application notes and standardized protocols for two key functional measures—Stair Climb Power and Tandem Walking Tests—framed within the context of GHS clinical trials. These measures are highly relevant for assessing the impact of anabolic interventions on lower-limb muscle power and dynamic balance, both critical domains for mobility and quality of life in aging and functionally limited populations [25] [37] [38].
Stair Climb Power Test (SCPT)
Rationale and Clinical Relevance
The SCPT is a functionally relevant measure of lower-limb muscle power, a neuromuscular attribute that declines earlier and more rapidly than strength with age and is strongly linked to mobility limitations [39] [37] [40]. Stair climbing is among the most frequently reported difficult tasks for older adults with mobility limitation, making it a patient-important outcome [37]. In trials of function-promoting anabolic therapies (FPTs), including GHS, the SCPT has shown greater responsiveness to intervention compared to other measures like gait speed, potentially due to a higher ceiling effect [37]. Its relevance in GHS trials is underscored by its use in evaluating physical performance improvements following treatment with capromorelin [25].
Table 1: Summary of Stair Climb Power Test Configurations and Performance Data
| Stair Model | Population | Reliability (ICC) | Criterion Validity (r vs. Leg Press) | Key Findings & Context |
|---|---|---|---|---|
| 4-Step SCPT [39] | Community-dwelling older adults (≥65 yrs, at risk for mobility decline) | 0.951 (Excellent) | 0.85 - 0.96 | MDC90 = 44.0 Watts. Explains ~31% of variance in SPPB. Feasible for settings with space constraints. |
| 10-/12-Step SCPT [37] | Older men with mobility limitation (low testosterone) | 0.91 - 0.97 (Excellent) | Associated with leg press strength & power | Sensitive to change with testosterone therapy. Loaded condition (20% body mass) may increase responsiveness. |
| Multi-Step (3,6,12) [40] | Community-dwelling older adults (≥65 yrs) | 0.66 - 0.95 (Good-Excellent) | N/A (Sensor-based power) | Power production reliable across stair models. A 3-step staircase is a feasible alternative, but tracking requires identical stair models. |
Table 2: SCPT Response in GHS and Related Anabolic Trials
| Intervention | Trial Population | SCPT Findings | Reference |
|---|---|---|---|
| Capromorelin (GHS) [25] | Older adults (65-84 yrs) at risk of functional decline | Increased stair climb power and tandem walking speed after 1 year of treatment. | [25] |
| Testosterone (FPT) [37] | Older, mobility-limited men | Changes in testosterone levels were associated with changes in unloaded and loaded SCPT, but not with gait speed. | [37] |
Detailed Experimental Protocol
The following protocol synthesizes the best practices from the cited literature for a 12-step SCPT, with modifications for shorter flights noted [37].
Equipment and Setup
- Staircase: A well-lit, 12-step interior staircase with handrails. Each step's rise height should be measured to the nearest millimeter and summed for the total vertical rise.
- Safety Equipment: Orange cones to mark the endpoint.
- Timing System: An electronic timing system with switch mats is recommended for high precision. Alternatively, a stopwatch can be used.
- Weight Scales: To measure participant body mass.
- Loading Bags (for Loaded SCPT): Two canvas tote bags and weight plates to equal 20% of the participant's body mass, divided evenly.
Subject Preparation
- Participants should wear comfortable clothing and athletic shoes with non-slip soles.
- Body mass (in kg) is measured with shoes and clothing.
- Resting heart rate and blood pressure are measured after a 5-minute seated rest.
- Participants are screened for contraindications (e.g., unstable cardiovascular disease, severe balance problems, acute musculoskeletal pain).
Test Procedure
- Demonstration: The examiner provides a scripted demonstration, climbing the stairs one step at a time, as fast as safely possible without running, skipping steps, or using the handrail (unless necessary for balance).
- Positioning: The participant stands one stride length behind the first timing mat or a designated start line.
- Instructions: On the command "Go," the participant ascends the stairs as quickly and safely as possible.
- Timing: Timing begins when the participant steps on the first switch mat (or crosses the start line) and stops when both feet are on the 12th step.
- Assistance: An examiner follows behind the participant to provide physical assistance if needed, without pacing them.
- Rest: After the ascent, the participant descends with assistance, is seated, and rests for 1.5-2 minutes before the next trial.
- Trials: A minimum of two trials are performed. The best (highest power) or average of the trials is used for analysis.
Stopping Criteria
The test is immediately stopped for any report of chest discomfort, significant shortness of breath, feeling faint or lightheaded, or if the participant does not reach the top within 2 minutes.
Data Calculation
Power (Watts) is calculated using the following equation, where the loaded condition includes the added mass:
Power (W) = [Body Mass (kg) + Load Carried (kg)] × 9.81 m/s² × Total Rise (m) / Time (s)
Workflow and Logical Relationships
Diagram 1: SCPT Experimental Workflow
Tandem Walking and Stance Tests
Rationale and Clinical Relevance
Tandem tests challenge dynamic and static balance by reducing the base of support, requiring integration of sensory and motor systems [41]. Impaired balance is a primary risk factor for falls, a critical endpoint in trials involving older populations. The 10-second tandem stance test is a quick, equipment-free tool that has demonstrated utility in predicting gait impairment and the need for a walking aid [41]. Furthermore, tandem walking speed was identified as a functional outcome that improved with capromorelin treatment in older adults at risk of functional decline [25]. For populations with greater impairment, such as those with type 2 diabetes, the more challenging Circular Tandem Walk Test (CTWT) has been validated for fall risk assessment [42].
Table 3: Tandem Test Performance Data and Clinical Cut-offs
| Test | Population | Key Associations & Predictive Values | Clinical Cut-off |
|---|---|---|---|
| 10-Sec Tandem Stance [41] | Community-dwelling older adults (mean ~76 yrs) | Inability to hold position: OR=5.19 for requiring a prescribed walking aid. Correlated with gait speed, stride length, and falls history. | Inability to maintain the position for 10 seconds indicates significant balance impairment. |
| Circular Tandem Walk Test (CTWT) [42] | Older adults with Type 2 Diabetes | Optimal cutoff for fallers vs. non-fallers: 15.2 seconds. Sensitivity=80.0%, Specificity=86.1%, AUC=0.915. Strongly correlated with fear of falling (FES-I). | ≥15.2 seconds indicates high fall risk in older adults with T2DM. |
Detailed Experimental Protocol
- Equipment: A stopwatch. A railing or wall for initial support is recommended for safety.
- Positioning: The participant stands holding onto a railing while placing one foot directly in front of the other, heel-to-toe. The foot placed in front (preferred or non-preferred) should be recorded.
- Instruction and Timing: The researcher demonstrates the position. The participant is instructed to release the railing, and timing starts. The test continues for up to 10 seconds or until the participant moves their feet out of position, touches the ground with the other foot, or requires external support.
- Trials: The test is performed twice with one foot in front, then twice with the other foot in front. No practice is allowed.
- Equipment: A circular pattern 5 cm wide, with a radius of 35 cm (measured to the inner line), creating a circumference of 220 cm. A stopwatch.
- Positioning: The participant stands at the starting point on the circle, in a heel-to-toe position.
- Instruction and Timing: On the "Start" command, the participant walks heel-to-toe along the circular pattern as fast as possible but safely. Timing begins on the command and stops when the participant's foot fully touches the ground on the 10th step.
- Safety: The researcher should be positioned nearby to prevent a fall.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Equipment for Functional Outcome Assessment
| Item | Function/Application | Protocol Context |
|---|---|---|
| Electronic Timing System (e.g., switch mats) | Provides high-precision timing for ascent/descent tasks, reducing human reaction time error. | Critical for standardized SCPT in multi-site drug trials [37]. |
| Portable Staircase (3-4 steps) | Enables measurement of lower-limb power in clinical settings without access to a full flight of stairs. | 4-step SCPT is reliable and valid; 3-step model is a feasible alternative [39] [40]. |
| Body-Fixed Sensor System | Captures kinematic data (e.g., power production per step) throughout a flight of stairs, beyond mean power. | Used in research to analyze different performance phases (acceleration, peak power, fatigue) [40]. |
| Keiser Leg Press Machine (or equivalent) | Provides gold-standard measurement of isotonic leg strength and power for criterion validity testing. | Used to validate the SCPT and other functional measures [39] [37]. |
| Short Physical Performance Battery (SPPB) | A composite measure of lower-extremity function (balance, gait, chair stand) used for participant characterization. | Used to define mobility-limited populations in trials; SCPT explains a significant portion of its variance [25] [39] [37]. |
Integration in GHS Clinical Trials
Logical Framework for Measure Selection
Diagram 2: Role of Functional Measures in GHS Trial Efficacy Assessment
Application Notes for Trial Design
- Population Definition: The SCPT is highly relevant for mobility-limited older adults (e.g., SPPB score 4-9) who frequently report difficulty climbing stairs [37]. Tandem tests are particularly useful for populations at high risk of falls, such as those with diabetic peripheral neuropathy [42].
- Responsiveness: SCPT, especially the loaded version (LSCP), may be more sensitive to detect changes from anabolic interventions like GHS compared to gait speed [25] [37].
- Standardization is Critical: To ensure data consistency across trial sites, protocols for instructions, number of steps, step height, timing method, and handling of handrail use must be rigorously standardized [37] [40].
Within the context of clinical research on growth hormone secretagogues (GHS), such as MK-0677 (ibutamoren) and capromorelin, the precise analysis of key biomarkers is paramount for evaluating drug efficacy and understanding physiological impact. This document details the application notes and protocols for assessing two critical endpoints: the sustained elevation of Insulin-like Growth Factor-1 (IGF-1) and the characterization of 24-hour Growth Hormone (GH) pulsatility profiles. The GH/IGF-1 axis is a central regulator of metabolism and body composition, and its targeted activation represents a promising therapeutic strategy for conditions like sarcopenia and frailty [25] [43]. The protocols herein are framed within the broader thesis of GHS clinical trials, providing standardized methodologies for researchers and drug development professionals to generate reliable, comparable data on the pharmacodynamic effects of these novel compounds.
Background and Significance
The GH/IGF-1 Axis in Physiology and Therapeutics
The GH/IGF-1 axis is a complex endocrine system essential for growth, metabolism, and tissue homeostasis. Pituitary-derived GH stimulates hepatic production of IGF-1, which mediates many of GH's anabolic effects [44] [45]. Unlike GH, which is secreted in a pulsatile manner with a short half-life, IGF-1 is released more stably, has a longer half-life, and exhibits minimal diurnal variation, making it a superior biomarker for integrated GH secretion over a 24-hour period [46] [45]. In circulation, over 98% of IGF-1 is bound to a family of IGF binding proteins (IGFBPs), with IGFBP-3 being the most abundant, forming a ternary complex that prolongs IGF-1's half-life and modulates its bioactivity [44].
A universal feature of human aging is a progressive decline in the production of GH and IGF-1, which contributes to adverse body composition changes such as decreased muscle mass and increased adiposity [25] [43]. GHS, including the orally active agents MK-0677 and capromorelin, offer a therapeutic approach to rejuvenate this axis. These small molecules act as ghrelin receptor agonists, amplifying the pulsatile release of endogenous GH and subsequently increasing circulating IGF-1 levels [25] [14]. This restoration of a youthful hormonal pulsatility profile is a key differentiator from exogenous GH administration, as it leverages the body's inherent regulatory feedback mechanisms to prevent hyperstimulation [25] [47].
Key Biomarkers in GHS Trials
In clinical trials for GHS, two primary biomarkers are routinely monitored:
- IGF-1 Levels: Serum IGF-1 serves as the primary biomarker for assessing the chronic, integrated biological activity of a GHS. Sustained elevation of IGF-1 confirms target engagement and systemic biological effect [25] [46].
- 24-hour GH Pulsatility: Detailed profiling of GH secretion over a 24-hour period is critical for demonstrating that the GHS produces an amplification of the endogenous pulsatile pattern characteristic of a healthy, young axis, rather than a constant, non-physiological elevation [25].
The following diagram illustrates the core physiological pathway targeted by GHS and the key biomarkers measured in clinical trials.
Clinical trials of MK-0677 and capromorelin have consistently demonstrated their ability to significantly elevate key biomarkers. The following tables summarize quantitative outcomes related to IGF-1 levels and body composition changes.
Table 1: Biomarker Changes in Older Adults Following 12 Months of GHS Therapy
| Parameter | Placebo Group Change (kg) | MK-0677 (25 mg/day) Group Change (kg) | Capromorelin (10 mg/Night) Group Change | Citation |
|---|---|---|---|---|
| Fat-Free Mass (FFM) | -0.5 (CI, -1.1 to 0.2) | +1.1 (CI, 0.7 to 1.5)* | Increased (absolute LBM) | [25] |
| Total Appendicular FFM | -0.3 (CI, -0.6 to 0.1) | +0.5 (CI, 0.3 to 0.8)* | Not Specified | [25] |
| Body Weight | +0.8 (CI, -0.3 to 1.8) | +2.7 (CI, 2.0 to 3.5)* | Increased | [25] |
| Serum IGF-1 | Not Specified | 1.8-fold increase (CI, 1.56- to 2.0-fold) | Increased | [25] |
Table 2: Functional Outcomes in Older Adults at Risk of Functional Decline (Capromorelin, 1 Year)
| Functional Measure | Outcome with Capromorelin | Citation |
|---|---|---|
| Stair Climb Power | Increased | [25] [14] |
| Tandem Walking Speed | Increased | [25] [14] |
| Other Functional Measures | Non-significant effects | [25] |
Experimental Protocols
Protocol 1: Assessment of 24-hour GH Pulsatility Profiles
4.1.1 Objective: To characterize the pulsatile secretion pattern of GH over a 24-hour period in subjects before and after administration of a GHS (e.g., MK-0677 or capromorelin).
4.1.2 Materials and Reagents:
- Intravenous cannula for serial blood sampling
- EDTA or heparinized blood collection tubes
- Refrigerated centrifuge
- -80°C freezer for serum/plasma storage
- Validated GH immunoassay kit (e.g., ELISA or ECLIA)
4.1.3 Procedure:
- Subject Preparation: Admit subjects to a clinical research unit. Standardize meals and physical activity for 24 hours prior to and during the sampling period.
- Baseline Sampling: Insert an intravenous cannula and begin serial blood sampling. A typical protocol involves drawing blood every 10-20 minutes over 24 hours to adequately capture GH pulses [25].
- Drug Administration: Following baseline assessment, initiate daily oral dosing with the GHS (e.g., MK-0677 at 25 mg/day or capromorelin at 10 mg/night).
- Post-Treatment Sampling: After a predetermined treatment period (e.g., 2 weeks or 1 month), repeat the 24-hour serial blood sampling protocol under identical conditions.
- Sample Processing: Centrifuge blood samples promptly after collection, aliquot serum or plasma, and store at -80°C until analysis.
- GH Analysis: Quantify GH concentrations in all samples using a validated, sensitive immunoassay. Perform all assays in duplicate.
- Data Analysis: Analyze the resulting GH concentration-time series using deconvolution analysis or the Cluster algorithm to identify the number, amplitude, and duration of GH pulses. Calculate the total area under the curve (AUC) for 24-hour GH secretion.
Protocol 2: Measurement of Sustained IGF-1 Elevation
4.2.1 Objective: To monitor the long-term effects of a GHS on circulating levels of IGF-1 and its binding protein, IGFBP-3.
4.2.2 Materials and Reagents:
- Serum-separating tubes
- Validated IGF-1 immunoassay kit
- Validated IGFBP-3 immunoassay kit
- Equipment for sample processing and storage (as in Protocol 1)
- Acid-ethanol solution (if required for pre-assay extraction to dissociate IGFs from binding proteins)
4.2.3 Procedure:
- Baseline Blood Draw: Collect a single fasting blood sample from subjects prior to initiation of GHS treatment.
- Initiate Dosing: Administer the GHS orally once daily.
- Serial Monitoring: Collect subsequent fasting blood samples at regular intervals (e.g., weekly for the first month, then monthly). Consistent timing of sample collection relative to dosing is critical.
- Sample Processing: Allow blood to clot in serum-separating tubes, centrifuge, and store serum aliquots at -80°C.
- IGF-1 and IGFBP-3 Analysis: Measure serum IGF-1 and IGFBP-3 concentrations using validated immunoassays. Note that most IGF-1 assays require a pre-treatment step to remove interfering IGFBPs; follow manufacturer instructions meticulously [44] [46].
- Data Analysis: Express IGF-1 values as absolute concentrations and as a percentage of the age-specific upper limit of normal. The molar ratio of IGF-1 to IGFBP-3 can be calculated as an estimate of free, bioavailable IGF-1 [44] [46].
The following workflow diagram maps the logical sequence of these key experimental protocols.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for GHS Clinical Biomarker Analysis
| Research Reagent / Material | Function and Application in GHS Trials |
|---|---|
| MK-0677 (Ibutamoren) | An orally active, non-peptidyl GHS used as the reference investigational product. Binds the ghrelin receptor to potently stimulate pulsatile GH release. Typical clinical dose: 25 mg once daily [25] [48]. |
| Capromorelin | An orally active ghrelin receptor agonist used as a comparator GHS. Has a shorter half-life than MK-0677, sometimes requiring twice-daily dosing to sustain IGF-1 elevation [25] [14]. |
| Sensitive GH Immunoassay | For the quantitative measurement of GH in serum from frequent sampling. Critical for accurate pulse analysis. Methods include ELISA (Enzyme-Linked Immunosorbent Assay) and ECLIA (Electrochemiluminescence Immunoassay) [49]. |
| IGF-1 Immunoassay | For the quantitative measurement of total IGF-1 in serum. Requires a pre-analytical step to dissociate IGF-1 from its binding proteins. ECLIA platforms are commonly used [46]. |
| IGFBP-3 Immunoassay | For the quantitative measurement of IGFBP-3, the primary carrier of IGF-1 in circulation. Used to calculate the IGF-1/IGFBP-3 molar ratio [44] [46]. |
| Acid-Ethanol Solution | Used in the pre-treatment of serum samples for IGF-1 analysis to precipitate IGFBPs, ensuring accurate measurement of total IGF-1 concentration [44]. |
Addressing Clinical Challenges: Desensitization, Safety, and Side Effect Management
Growth Hormone Secretagogues (GHS), including the orally active molecules MK-677 (ibutamoren) and capromorelin, represent a promising therapeutic class for restoring pulsatile GH secretion in conditions of age-related decline and muscle wasting [25]. Their mechanism of action involves targeting the ghrelin receptor (GHS-R1a), a G-protein coupled receptor that potently stimulates GH release [50]. A significant barrier to their long-term efficacy, however, is the rapid onset of desensitization. This phenomenon, observed both in vitro and in vivo, limits the sustained therapeutic potential of these compounds [51] [50]. This Application Note synthesizes key preclinical and clinical findings to elucidate the role of hypothalamic somatostatin upregulation in GHS desensitization and provides detailed protocols for investigating and overcoming this adaptive response in drug development research.
KEY EVIDENCE: QUANTITATIVE DATA ON DESENSITIZATION
The following tables summarize critical quantitative findings from prolonged GHS dosing studies, highlighting the disconnect between acute GH stimulation and sustained growth promotion.
Table 1: Preclinical Study of Prolonged MK-677 Administration in Rats
| Parameter | Baseline/Finding | Source |
|---|---|---|
| Dosing Regimen | 4 mg/kg, orally, for 6 weeks | [51] |
| Acute GH Response | 1.8-fold increase in peak GH concentration | [51] |
| Somatic Growth (6 weeks) | No increase in body weight, body length, or tibia length | [51] |
| IGF-I Levels (6 weeks) | No significant change in serum IGF-I | [51] |
| GH Response at 6 weeks | Abolished | [51] |
| Hypothalamic SST mRNA | Markedly increased | [51] |
| Pituitary SSTR-2 mRNA | Decreased | [51] |
Table 2: Clinical Trial Outcomes of GHS in Older Adults
| Parameter | MK-0677 (Ibutamoren) | Capromorelin |
|---|---|---|
| Study Duration | Up to 2 years | 1 year (study terminated early) |
| GH & IGF-I | Increased pulsatile GH secretion; Elevated IGF-1 | Increased IGF-1 (required higher/sustained dosing) |
| Body Composition | Increased Fat-Free Mass (FFM) by +1.1 kg and body weight by +2.7 kg at 12 months [25] | Increased Lean Body Mass and body weight [25] |
| Functional Outcomes | No significant improvement in muscle strength or function in healthy older adults [25] | Improved stair climb power and tandem walking speed in older adults at risk of functional decline [25] [14] |
| Key Limitation | Functional benefits not demonstrated in healthy elderly | Early termination due to prespecified efficacy criteria not being met (increased weight without significant %LBM change) [25] |
MECHANISMS: SOMATOSTATIN-MEDIATED INHIBITION & RECEPTOR DESENSITIZATION
The observed desensitization is a multi-faceted process involving rapid receptor signaling fatigue and a slower, adaptive hypothalamic feedback mechanism.
- Hypothalamic Somatostatin Upregulation: Prolonged stimulation of the GHS-R1a by MK-677 has been shown to trigger a counter-regulatory response in the hypothalamus, characterized by a marked increase in somatostatin (SST) mRNA and protein expression [51]. SST, also known as Growth Hormone-Inhibiting Hormone, is the primary negative regulator of GH secretion. It is produced in the hypothalamus and acts directly on pituitary somatotrophs to inhibit GH release [52]. This increased inhibitory tone is a primary mechanism blunting the GH response over time.
- GHS Receptor (GHS-R1a) Desensitization: At the cellular level, the GHS-R1a is susceptible to rapid desensitization. In vitro studies using cells transfected with the human GHS-R1a demonstrate that repeated stimulation with a GHS like hexarelin leads to a marked attenuation of the intracellular calcium response within minutes [50] [53]. This rapid desensitization is a hallmark of many G-protein coupled receptors and would contribute to the diminished efficacy observed with continuous dosing.
- Altered Receptor Expression: The compensatory response also involves changes in receptor expression. In the rat model, prolonged MK-677 administration led to decreased mRNA expression for the somatostatin receptor subtype 2 (SSTR2) in the pituitary [51]. Since SSTR2 is a critical mediator of SST's inhibitory actions on GH release, its downregulation may represent a failed attempt by the somatotroph to escape the heightened SST tone.
The following diagram illustrates the signaling pathways and logical relationships involved in GHS desensitization.
EXPERIMENTAL PROTOCOLS
Here, we provide detailed methodologies for key experiments cited in this research.
Protocol: Assessing Chronic GHS Effects on Somatic Growth and Hypothalamic-Pituitary Axis in Rats
This protocol is adapted from the pivotal study demonstrating MK-677-induced somatostatin upregulation [51].
- Objective: To evaluate the long-term growth-promoting effects of a GHS and investigate molecular adaptations in the hypothalamic-pituitary axis.
- Materials:
- Animals: Young, growing rats (e.g., Sprague-Dawley).
- Test Compound: MK-677 (ibutamoren) in vehicle (e.g., 0.5% methylcellulose).
- Equipment: Scale, calipers, microdissection tools, real-time PCR system, western blot apparatus, ELISA kits for GH and IGF-I.
- Methodology:
- Dosing & Monitoring: Randomize rats into control and treatment groups. Administer GHS (e.g., 4 mg/kg) or vehicle orally once daily for 6+ weeks. Monitor body weight and length (nose-to-anus) weekly.
- Terminal Analysis: At the end of the treatment period, euthanize animals and collect tissues.
- Somatic Measures: Record final body weight, body length, and tibia length. Measure epiphyseal plate width histologically.
- Blood Collection: Collect serum for IGF-I and GH assay via ELISA.
- Tissue Collection: Rapidly remove and freeze hypothalamus and pituitary glands for molecular analysis.
- Molecular Analysis:
- Gene Expression: Extract total RNA from hypothalamic and pituitary tissues. Perform RT-qPCR to quantify mRNA levels of GH, GHRH, GHSR, somatostatin (SST), and somatostatin receptors (e.g., SSTR2). Normalize to housekeeping genes (e.g., GAPDH, β-actin).
- Protein Expression: Analyze protein levels of key targets like hypothalamic SST and pituitary SSTR2 via western blot.
The experimental workflow for this protocol is outlined below.
Protocol: In Vitro GHS Receptor Desensitization Assay
This protocol is based on studies demonstrating rapid calcium signal desensitization in GHS-R1a transfected cells [50] [53].
- Objective: To characterize the rapid desensitization kinetics of the GHS-R1a in a controlled cell system.
- Materials:
- Cell Line: Chinese Hamster Ovary (CHO) cells.
- Plasmids: cDNA encoding human GHS-R1a.
- Reagents: Lipofectamine transfection reagent, hexarelin (or other GHS), fura-2 AM calcium-sensitive dye, standard cell culture materials.
- Equipment: Fluorescence microscope with ratiometric capability, perfusion system for rapid buffer exchange.
- Methodology:
- Cell Culture & Transfection: Culture CHO cells under standard conditions. Transiently transfect with GHS-R1a cDNA; include mock-transfected controls.
- Calcium Imaging: 24-48 hours post-transfection, load cells with fura-2 AM dye. Use a perfusion system to maintain cells in a physiological buffer.
- Stimulation & Desensitization: Measure baseline intracellular calcium. Stimulate cells with a maximal dose of hexarelin (e.g., 100 nM) for a short period (e.g., 60 sec), then wash. After a short interval (2-5 min), re-stimulate with the same dose of hexarelin and measure the calcium response.
- Data Analysis: Quantify the peak calcium response for both the first and second stimulations. Calculate the percent desensitization as:
[1 - (2nd Peak / 1st Peak)] * 100.
THE SCIENTIST'S TOOLKIT: RESEARCH REAGENT SOLUTIONS
Table 3: Essential Materials for GHS Desensitization Research
| Item | Function/Description | Example(s) |
|---|---|---|
| Orally Active GHS | Small molecule agonists of the GHS-R1a used for in vivo prolonged dosing studies. | MK-677 (Ibutamoren), Capromorelin [51] [25] |
| Peptide GHS Analogue | Potent peptide agonist used for in vitro receptor studies and acute stimulation. | Hexarelin [50] [53] |
| GHS-R1a cDNA | Plasmid for transient or stable transfection to create recombinant cell systems for receptor pharmacology. | Human GHS-R1a cDNA [50] |
| Calcium-Sensitive Dye | Fluorescent indicator for measuring intracellular calcium flux, a key downstream signal of GHS-R1a activation. | Fura-2 AM [50] [53] |
| Somatostatin ELISA/Kits | For quantifying somatostatin protein levels in hypothalamic tissue extracts or plasma. | N/A (Commercial kits available) |
| qPCR Primers/Probes | For quantifying mRNA expression of target genes (SST, SSTR2, GHRH, GH, GHSR) in hypothalamic and pituitary tissues. | Custom-designed primers [51] |
| Selective Receptor Ligands | Tool compounds for probing specific somatostatin receptor subtypes involved in feedback. | sst1/sst2 receptor agonists/antagonists [54] |
The upregulation of hypothalamic somatostatin presents a fundamental challenge to the sustained efficacy of continuous GHS therapy. Future drug development must focus on strategies that circumvent or modulate this adaptive inhibitory response. Promising avenues include the development of intermittent dosing regimens ("drug holidays") to allow the hypothalamic-pituitary axis to reset, combination therapies with somatostatin receptor antagonists, and novel GHS-R1a agonists with unique signaling properties (e.g., biased agonism) that are less prone to triggering somatostatin feedback. The protocols and insights provided here form a foundation for such advanced investigative work.
Within clinical research on growth hormone secretagogues (GHSs) such as MK-677 (Ibutamoren) and capromorelin, the management of metabolic side effects is a paramount safety consideration. GHSs stimulate the pulsatile release of endogenous growth hormone (GH), consequently increasing insulin-like growth factor 1 (IGF-1) levels [32]. This mechanism, while therapeutically beneficial for conditions like muscle wasting or weight loss, is frequently accompanied by dose-related insulin resistance and hyperglycemia [55] [32]. These Application Notes and Protocols provide detailed methodologies for monitoring and managing these metabolic derangements in clinical trial populations, ensuring patient safety and data integrity.
Pathophysiology and Quantitative Risk Profile
Understanding the metabolic impact of GHSs is critical for protocol design. The table below summarizes key metabolic effects and their reported frequencies from clinical investigations.
Table 1: Documented Metabolic Side Effects of GH Secretagogues in Clinical Research
| Side Effect | Reported Frequency / Magnitude | Relevant Secretagogue | Notes |
|---|---|---|---|
| Reduced Insulin Sensitivity | Common [32] | MK-677 (Ibutamoren) [32] | A primary metabolic concern in clinical trials. |
| Increased Fasting Blood Glucose | Reported [56] | MK-677 (Ibutamoren) [56] | Contributes to overall hyperglycemia risk. |
| Increased HbA1c | Reported [56] | MK-677 (Ibutamoren) [56] | Indicates longer-term glycemic control issues. |
| Increased Appetite | Common, transient effect [32] | MK-677 (Ibutamoren), GHRP-2 [32] | Can indirectly affect metabolic parameters via weight gain. |
| Weight Gain | Documented [55] | MK-677 (Ibutamoren) [55] | Associated with fluid retention and increased appetite. |
| Water Retention / Swelling | Common side effect [55] | MK-677 (Ibutamoren) [55] | A frequent, though not directly metabolic, adverse event. |
The underlying pathophysiology involves the antagonism of insulin action by GH and IGF-1, pushing the endocrine pancreas to compensate for reduced insulin sensitivity. In susceptible individuals, this can lead to persistent hyperglycemia [32]. One clinical trial on MK-677 was halted prematurely due to diabetes-like impacts, including elevated blood glucose and HbA1c [56]. The following diagram illustrates this metabolic signaling pathway.
Essential Materials: The Researcher's Toolkit
Table 2: Key Research Reagent Solutions for Metabolic Phenotyping
| Research Reagent / Material | Function / Application |
|---|---|
| MK-677 (Ibutamoren) | Orally bioavailable GHS; investigational drug for frailty, weight loss [55] [32]. |
| Capromorelin | Orally available GHS; used in veterinary research for weight gain in chronic disease [9]. |
| Human Growth Hormone (hGH) ELISA | Quantifies endogenous GH pulsatility in response to GHS administration [32]. |
| IGF-1 Immunoassay | Measures downstream effector of GH; levels are sustained and correlate with GH activity [32]. |
| HbA1c Point-of-Care Analyzer | Provides critical measure of long-term (2-3 month) glycemic control; essential for screening and monitoring [57] [58]. |
| Continuous Glucose Monitor (CGM) | Tracks interstitial glucose concentrations in real-time, identifying post-dose hyperglycemia [58]. |
| Insulin Sensitivity Assay (HOMA-IR) | Calculates insulin resistance from fasting glucose and insulin levels [56]. |
Core Monitoring Protocol for Insulin Resistance & Hyperglycemia
This protocol outlines a comprehensive strategy for detecting and characterizing metabolic side effects in GHS clinical trials.
4.1 Objective: To systematically monitor for the emergence and progression of insulin resistance and hyperglycemia in study participants receiving GH secretagogues.
4.2 Pre-Study Screening (Within 30 Days of Baseline):
- Medical History: Document history of diabetes, prediabetes, polycystic ovary syndrome (PCOS), or gestational diabetes.
- Physical Exam: Include Body Mass Index (BMI) and waist circumference.
- Fasting Blood Samples:
4.3 In-Study Monitoring Schedule: Table 3: In-Study Metabolic Monitoring Schedule
| Timepoint | Glucose | HbA1c | Insulin/IGF-1 | Other |
|---|---|---|---|---|
| Baseline | Fasting & 2-hr post-prandial | X | X (Insulin, IGF-1) | Weight, BMI |
| Bi-weekly (Weeks 2, 4) | Fasting | Weight, AE check | ||
| Monthly (Weeks 4, 8, 12) | Fasting & 2-hr post-prandial | X | X (IGF-1) | Weight, BMI, AE check |
| Study End | Fasting & 2-hr post-prandial | X | X (Insulin, IGF-1) | Weight, BMI, Final AE log |
| Continuous (High-Risk) | Real-time CGM with POC-BG confirmation [58] | As needed |
4.4 Hyperglycemia Intervention Thresholds & Actions: Adhere to institutional and Endocrine Society guidelines. For non-critically ill patients, a glycemic goal of 100-180 mg/dL (5.6-10.0 mmol/L) is recommended if achieved without hypoglycemia [57] [58].
- Single BG >180 mg/dL (10.0 mmol/L): Confirm with a second test. Review diet and activity.
- Persistent BG >180 mg/dL (10.0 mmol/L): Consider initiating scheduled insulin therapy per protocol [58].
- Fasting BG >250 mg/dL (13.9 mmol/L) or symptomatic hyperglycemia: Requires immediate medical evaluation and likely intervention with insulin.
The workflow for managing a patient with hyperglycemia is standardized as follows.
Experimental Protocol: Hyperinsulinemic-Euglycemic Clamp
For definitive assessment of insulin sensitivity in a subset of participants, the hyperinsulinemic-euglycemic clamp is the gold standard.
5.1 Objective: To quantitatively measure whole-body insulin sensitivity in response to GHS administration.
5.2 Materials:
- Intravenous catheters (one for infusion, one for blood sampling)
- Insulin infusion solution
- 20% Dextrose solution
- Blood glucose analyzer (at bedside)
- Pump for controlled infusions
5.3 Methodology:
- Basal Period: After an overnight fast, measure fasting glucose and insulin levels.
- Insulin Infusion: Begin a primed, continuous intravenous infusion of insulin (e.g., 40 mU/m²/min) to create a steady-state hyperinsulinemic plateau.
- Glucose Infusion: Simultaneously, initiate a variable-rate infusion of 20% dextrose.
- Euglycemic Clamp: Measure plasma glucose every 5-10 minutes. Adjust the dextrose infusion rate to "clamp" blood glucose at a target euglycemic level (e.g., 90-95 mg/dL or 5.0-5.3 mmol/L).
- Steady-State Measurement: The procedure typically lasts 2 hours. The steady-state is reached when the glucose infusion rate (GIR) stabilizes (usually in the final 30 minutes). The mean GIR over this period (mg/kg/min) is the primary outcome measure, representing the M-value for whole-body insulin sensitivity. A lower M-value indicates greater insulin resistance.
Within the clinical development of Growth Hormone Secretagogues (GHSs) such as MK-677 (Ibutamoren) and capromorelin, the primary efficacy endpoints of increased lean body mass and physical function are well-documented. However, a comprehensive understanding of the adverse event profile, particularly for events that are transient or manageable, is crucial for risk-benefit assessment and trial safety monitoring. This application note details the specific profiles of two transient endocrine events—increases in cortisol and prolactin—and the musculoskele-tal adverse event of pain, synthesizing quantitative data from clinical trials and providing standardized protocols for their monitoring in a research setting.
Quantitative Adverse Event Profile
Data from key clinical trials reveal a distinct pattern in the incidence and nature of these adverse events. The following tables summarize the quantitative findings for MK-677 (Ibutamoren) and capromorelin.
Table 1: Adverse Event Profile of MK-677 (Ibutamoren) in Clinical Trials
| Adverse Event | Incidence / Magnitude | Study Duration | Population | Notes |
|---|---|---|---|---|
| Transient Cortisol Increase | Reported as transient [32] | Up to 2 years [25] | Healthy older adults (60-81 years) [25] | Well-tolerated; not considered clinically significant [32]. |
| Transient Prolactin Increase | Reported as transient [32] | Up to 2 years [25] | Healthy older adults [25] | Well-tolerated [32]. |
| Musculoskeletal Pain | Reported side effect [32] | Not specified | Older adults post-hip fracture [14] | Observed alongside fluid retention [32]. |
| Fluid Retention | Very Common [59] | Not specified | Not specified | Leads to side effects like edema and carpal tunnel symptoms [59]. |
| Insulin Resistance | Increased fasting glucose; decreased insulin sensitivity [60] | 1 year [25] | Healthy older adults [25] | A consistent finding across studies; requires monitoring [25]. |
Table 2: Adverse Event Profile of Capromorelin in Clinical Trials
| Adverse Event | Incidence / Magnitude | Study Duration | Population | Notes |
|---|---|---|---|---|
| Transient Cortisol Increase | Sustained elevation required repeated dosing to prevent [25] | 1 year [14] [25] | Older adults (65-84) with mild functional limitation [25] | Dosing regimen was adjusted to manage this effect [25]. |
| Musculoskeletal Pain | Not explicitly reported | 1 year [14] | Older adults with functional limitation [14] | Study reported improvements in physical function (stair climb, walk speed) [14]. |
| Body Composition | Increased lean body mass and body weight [25] | 1 year [25] | Older adults with functional limitation [25] | Absolute LBM increased, but % LBM did not due to concomitant weight gain [25]. |
| Insulin Resistance | Very mild increase [25] | 1 year [25] | Older adults with functional limitation [25] | Not thought to be clinically significant [25]. |
Experimental Monitoring Protocols
To ensure consistent data collection for these specific adverse events in clinical trials, the following standardized monitoring protocols are recommended.
Protocol for Monitoring Transient Endocrine Effects
This protocol outlines the procedure for assessing the transient increases in cortisol and prolactin.
- 1. Objective: To characterize the pharmacokinetic and pharmacodynamic profile of cortisol and prolactin release following GHS administration.
- 2. Materials:
- GHS investigational product (e.g., MK-677, capromorelin) and placebo.
- Sterile blood collection equipment (venflons, serum tubes).
- Refrigerated centrifuge.
- -80°C freezer for sample storage.
- Validated immunoassay kits for serum cortisol and prolactin.
- 3. Subject Preparation: Subjects fast overnight for at least 10 hours and remain fasted until the 4-hour post-dose blood draw. Water is allowed.
- 4. Dosing & Sampling: Baseline (T=0) blood samples for cortisol and prolactin are collected immediately before the morning dose of the GHS. Subsequent samples are collected at 30, 60, 90, 120, and 240 minutes post-dose. For full 24-hour profiling, samples are taken every 20-30 minutes via an indwelling catheter.
- 5. Data Analysis: Plot concentration-time curves for cortisol and prolactin. Calculate the maximum concentration (C~max~) and time to C~max~ (T~max~). Compare the area under the curve (AUC) for the dosing interval against baseline and placebo data.
Protocol for Monitoring Musculoskeletal Pain and Discomfort
This protocol provides a structured method for capturing subjective and objective measures of musculoskeletal pain.
- 1. Objective: To systematically assess the incidence, severity, and functional impact of musculoskeletal pain in subjects receiving GHS.
- 2. Tools:
- Visual Analog Scale (VAS) or Numerical Rating Scale (NRS): For subjective pain intensity (0-10).
- Standardized Case Report Form (CRF): To document the location, duration, and character of pain.
- Physical Function Questionnaires: e.g., Health Assessment Questionnaire (HAQ).
- Goniometer: For measuring joint range of motion.
- Manual muscle testing or dynamometer for strength assessment.
- 3. Assessment Schedule: Conduct assessments at baseline, weeks 2, 4, 8, 12, and 24, and at the end of the study.
- 4. Procedure:
- Inquire about any new or worsened pain in muscles or joints.
- For any affirmative response, have the subject rate pain severity on the VAS/NRS.
- Document the exact location of pain on a body diagram in the CRF.
- Palpate the affected area for tenderness and assess range of motion.
- Inquire about impact on sleep and daily activities.
- 5. Data Analysis: Report the incidence rate of musculoskeletal pain. Analyze changes in VAS/NRS scores from baseline. Correlate pain reports with functional performance measures (e.g., stair climb, walk speed).
Signaling Pathways and Mechanistic Insights
GHSs exert their effects by binding to and activating the Growth Hormone Secretagogue Receptor (GHS-R1a), a G-protein coupled receptor. The following diagram illustrates the key signaling pathways that lead to both the release of Growth Hormone (GH) and the observed adverse events.
The activation of the GHS-R1a initiates a cascade primarily through the Gq/11 protein pathway, leading to the activation of phospholipase C (PLC) [14]. PLC hydrolyzes PIP₂ to generate IP₃ and DAG. IP₃ triggers the release of calcium from intracellular stores, while DAG activates Protein Kinase C (PKC). This signaling cascade potently stimulates the release of GH from pituitary somatotrophs [32]. However, the GHS-R is also expressed in other cell types, including corticotrophs and lactotrophs of the pituitary. The activation of PKC in these cells is understood to be the mechanism behind the transient increases in cortisol and prolactin observed in clinical trials [32]. This represents a class effect of GHSs, though its manifestation (transience and magnitude) may vary with the specific compound and dosing regimen.
The Scientist's Toolkit: Key Research Reagents
For researchers investigating the mechanisms and effects of GHSs, the following table lists essential reagents and their applications.
Table 3: Essential Research Reagents for GHS Investigations
| Reagent / Material | Function / Application in Research | Example Use Case |
|---|---|---|
| Ibutamoren (MK-677) | Orally active GHS; used to stimulate endogenous GH pulsatility. | In vivo studies to assess body composition changes, functional improvement, and endocrine profiles in aging or frailty models [25]. |
| Capromorelin | Orally active GHS; used as a comparative agent to other secretagogues. | Preclinical and clinical studies on sarcopenia and functional decline; investigating dosing regimens to manage cortisol release [14] [25]. |
| GHRP-6 | A synthetic hexapeptide GHS; foundational tool for mechanistic studies. | In vitro assays (e.g., rat pituitary cell cultures) to study GH release mechanisms and receptor activation [61] [32]. |
| Ghrelin | The natural endogenous ligand for the GHS-R1a. | Used as a control or comparator in studies to evaluate the potency and efficacy of synthetic GHSs [61]. |
| Rat Pituitary Cell Assay | Primary cell-based system for screening GHS activity. | Functional assay to test and validate the potency of new GHS compounds or analogs before in vivo studies [32]. |
| Validated Immunoassays | Quantitative measurement of hormones (GH, IGF-1, Cortisol, Prolactin). | Essential for pharmacokinetic/pharmacodynamic profiling and safety monitoring in both preclinical and clinical studies [25] [32]. |
| GHSR1a Antagonists | Small molecules that block the GHS receptor. | Tool compounds for confirming receptor-mediated effects and in mechanistic studies to dissect signaling pathways [14]. |
Optimizing Therapeutic Windows: Balancing Efficacy with Safety through Dosing and Formulation
Growth Hormone Secretagogues (GHS), such as MK-677 (ibutamoren) and capromorelin, represent a promising class of investigational drugs capable of restoring pulsatile growth hormone (GH) and insulin-like growth factor-1 (IGF-1) secretion. Their therapeutic potential spans conditions from sarcopenia and frailty in older adults to metabolic and muscular diseases [25] [28]. The primary challenge in their clinical development lies in optimizing the therapeutic window—the balance between achieving clinical efficacy, such as increased lean body mass and physical function, and managing side effects, including transient insulin resistance and weight gain [25]. These Application Notes and Protocols provide a structured framework for evaluating this balance through dosing and formulation strategies, framed within ongoing clinical trials research.
Quantitative Efficacy and Safety Profiles of Key GHS
Clinical trials have generated quantitative data essential for comparing the efficacy and safety of leading GHS. The table below summarizes key parameters from studies on MK-677 and capromorelin, providing a baseline for therapeutic window optimization.
Table 1: Comparative Clinical Outcomes of MK-677 and Capromorelin in Older Adults
| Parameter | MK-677 (25 mg/day) | Capromorelin (10 mg/Night) |
|---|---|---|
| Study Duration | 12 months [25] | 12 months [25] |
| Change in Lean Body Mass (LBM) | +1.1 kg (CI, 0.7 to 1.5) [25] | Increased (absolute LBM) [25] |
| Change in Body Weight | +2.7 kg (CI, 2.0 to 3.5) [25] | Increased [25] |
| Change in IGF-1 Levels | Sustained elevation [25] | Sustained elevation (required higher/repeated dosing) [25] |
| Functional Measures | Not significant in healthy elderly [25] | Increased stair climb power, tandem walking speed [25] |
| Common Adverse Events | Increased appetite, water retention [25] [62] | Similar to MK-677 [25] |
| Metabolic Effects | Mild, transient insulin resistance [25] [62] | Mild, transient insulin resistance [25] |
Experimental Protocol: Preclinical Assessment of GHS in a Murine Model
This protocol outlines a multidisciplinary in vivo and ex vivo approach for evaluating the efficacy and mechanisms of GHS, based on established preclinical models [28].
3.1. Objective To assess the functional, histological, and molecular effects of GHS administration on muscle function, fibrosis, and inflammation in the mdx mouse model of Duchenne Muscular Dystrophy (DMD).
3.2. Materials and Reagents
- Test Compounds: EP80317 or JMV2894 (GHS compounds) [28].
- Vehicle: Appropriate solvent for subcutaneous administration.
- Animals: 4-week-old male mdx mice and wild-type (C57BL/10) controls.
- Key Equipment: Grip strength meter, high-resolution ultrasound imaging system, ex vivo muscle force transducer system, equipment for RT-PCR and histological analysis.
3.3. Dosing and Treatment Regimen
- Group Allocation: Randomize mdx mice into Vehicle, GHS-1 (EP80317, 320 µg/kg/d), and GHS-2 (JMV2894, 320 µg/kg/d) groups [28].
- Administration: Administer compounds or vehicle subcutaneously, once daily for 8 weeks [28].
3.4. In Vivo Functional Assessments
- Forelimb Grip Strength: Measure weekly using a grip strength meter. Calculate a recovery score towards wild-type performance [28].
- Muscle Echogenicity: Perform ultrasound imaging of the diaphragm and gastrocnemius muscles at baseline and study endpoint. Reduced echodensity indicates decreased fibrosis [28].
3.5. Ex Vivo and Endpoint Analysis
- Muscle Isometric Force: Excise the diaphragm muscle post-sacrifice and measure isometric force ex vivo [28].
- Histological Analysis: Process muscle tissues for staining to quantify fibrosis (e.g., Masson's Trichrome) [28].
- Gene Expression Profiling: Isulate RNA from muscle tissue and perform RT-PCR to analyze expression levels of fibrosis- (TGF-β1, Col1a1), inflammation- (IL-6, CD68), and metabolism-related (Sirt-1, PGC-1α, MEF2c) genes [28].
Signaling Pathways and Mechanisms of Action
GHS exert their effects through a complex interplay of receptor-mediated and potential receptor-independent pathways. The diagram below illustrates the primary signaling cascade and investigated mechanisms based on preclinical research.
The Scientist's Toolkit: Essential Research Reagents
The following table details key materials required for conducting GHS research, from in vivo studies to analytical verification.
Table 2: Key Research Reagent Solutions for GHS Investigation
| Item | Function/Description | Example Application |
|---|---|---|
| MK-677 (Ibutamoren) | Orally active, non-peptide GHSR agonist with ~24-hour half-life [25] [63]. | Clinical & preclinical research on GH pulsatility, body composition, and sleep architecture [25]. |
| Capromorelin | Orally active GHSR agonist with a shorter half-life than MK-677 [25]. | Clinical trials investigating functional improvement in older adults at risk of decline [25]. |
| EP80317 / JMV2894 | Synthetic GHS compounds with a wide action profile, including potential anti-fibrotic effects [28]. | Preclinical mechanistic studies in disease models like DMD (mdx mice) [28]. |
| Research-Grade Formulations | Liquid suspensions or solutions with verified concentration and purity, accompanied by Certificates of Analysis (COA) [63]. | Ensures dosing accuracy and reproducibility in longitudinal animal studies [63]. |
| IGF-1 ELISA Kit | Quantifies serum or plasma IGF-1 levels, a primary biomarker for GHS biological activity [25]. | Monitoring target engagement and efficacy in both clinical and preclinical settings. |
| Primers for Fibrosis/Inflammation Markers | Gene-specific primers (e.g., for TGF-β1, Col1a1, IL-6) for RT-PCR analysis [28]. | Molecular analysis of GHS effects on tissue remodeling and inflammation [28]. |
Optimizing the therapeutic window for GHS is a multi-faceted endeavor requiring careful consideration of dosing frequency, compound selection, and patient population. The data and protocols provided herein establish a foundation for designing rigorous research strategies that prioritize both efficacy and safety. Future work should focus on refining formulations to improve selectivity and mitigate metabolic side effects, further expanding the clinical potential of this unique drug class.
Comparative Efficacy and Therapeutic Positioning: GHS vs. Recombinant GH and Androgen Therapy
Growth Hormone Secretagogues (GHS) represent a class of therapeutic agents that stimulate the endogenous release of growth hormone (GH) through targeted interaction with the ghrelin receptor, also known as the growth hormone secretagogue receptor (GHSR1a) [25] [26]. This application note provides a structured comparison of two prominent GHS—MK-677 (ibutamoren) and capromorelin—focusing on their clinical efficacy, safety profiles, and appropriate experimental protocols. Both compounds are orally active, non-peptide agonists of the GHSR1a, yet they possess distinct pharmacokinetic and pharmacodynamic properties that influence their therapeutic application [25] [32]. The objective of this document is to furnish researchers and drug development professionals with a consolidated, data-driven resource to inform preclinical and clinical study design for these compounds, framed within the broader context of GHS research.
Quantitative Clinical Outcomes Comparison
Direct head-to-head clinical trials comparing MK-677 and capromorelin are not extensively documented in the available literature. However, independent studies in similar populations allow for an indirect comparison of their efficacy and safety. The table below summarizes key clinical outcomes from pivotal trials for each compound.
Table 1: Indirect Comparison of Clinical Outcomes from MK-677 and Capromorelin Trials in Older Adults
| Clinical Parameter | MK-677 (Ibutamoren) | Capromorelin |
|---|---|---|
| Study Duration | 12 months [25] | 12 months [25] |
| Dosing Regimen | 25 mg, once daily [25] | 10 mg each night or 10 mg twice a day [25] |
| Change in Lean Body Mass (LBM) | +1.1 kg (CI, 0.7 to 1.5) [25] | Increased (absolute LBM), but % LBM not significant [25] |
| Change in Body Weight | +2.7 kg (CI, 2.0 to 3.5) [25] | Increased [25] |
| IGF-1 Elevation | Sustained increase [25] [32] | Sustained increase (required higher/repeated dosing) [25] |
| Functional Outcomes | Not significant in healthy elderly [25] | Increased stair climb power and tandem walking speed [25] |
| Common Adverse Events | Increased appetite, elevated fasting glucose & HbA1c [25] [64] | Fatigue, insulin resistance, insomnia [14] |
| Key Patient Population | Healthy older adults [25] | Older adults at risk of functional decline [25] |
In addition to human data, recent veterinary research underscores the efficacy of capromorelin in a different model of catabolic states. A 55-day study in client-owned cats with chronic kidney disease and unintended weight loss demonstrated that capromorelin led to a mean body weight increase of +5.18%, compared to a -1.65% change in the placebo group, resulting in a treatment effect of +6.81% [9]. This highlights its potential for managing cachexia.
Detailed Experimental Protocols
To ensure the reproducibility of research findings, this section outlines standardized protocols for evaluating the efficacy of GHS in clinical and preclinical settings, based on methodologies reported in the literature.
Protocol for Clinical Evaluation in Age-Related Decline
This protocol is adapted from trials investigating the impact of GHS on body composition and function in older adults [25].
- Objective: To assess the efficacy and safety of a GHS in improving lean body mass and physical function in elderly subjects.
- Study Design: Randomized, double-blind, placebo-controlled, parallel-group or modified-crossover trial.
- Subjects:
- Intervention:
- Active Treatment: MK-677 at 25 mg orally once daily, or Capromorelin at 10 mg orally each night or twice daily [25].
- Control: Matching placebo.
- Duration: 6 months to 2 years [25].
- Key Efficacy Endpoints:
- Primary: Change from baseline in total lean body mass (measured by DEXA).
- Secondary: Change in body weight, appendicular lean mass, fat mass, serum IGF-1 levels, and functional measures (e.g., stair climb power, tandem walk speed) [25].
- Safety Monitoring: Frequent assessment of fasting glucose, HbA1c, insulin, cortisol, prolactin, and adverse events [25] [64].
Protocol for Preclinical Evaluation in a Rodent Model
This protocol is based on studies investigating the growth-promoting effects of GHS in rats [27].
- Objective: To determine the effects of a GHS on somatic growth and endocrine parameters in vivo.
- Animals: Young (e.g., 4-week-old) female Sprague-Dawley rats.
- Dosing Formulation: GHS (e.g., MK-677) prepared at 1 mg/mL in distilled water [27].
- Experimental Groups: Vehicle control (distilled water) vs. GHS-treated group (e.g., 4 mg/kg).
- Administration: Oral administration via stomach tube once daily for 6 weeks [27].
- Data Collection:
- Body Measurements: Record body weight and body length (nose-to-anus) daily or weekly.
- Blood Sampling: Collect serum at baseline and every 2 weeks for IGF-1 analysis by ELISA. Perform GH stimulation tests at the start and end of the study.
- Tissue Analysis: Upon sacrifice, collect tibia for histomorphometric analysis of epiphyseal plate width. Harvest pituitary and hypothalamus for mRNA and protein expression analysis of GH, GHRH, GHSR, and somatostatin [27].
Signaling Pathways and Mechanisms of Action
Both MK-677 and capromorelin are agonists of the GHSR1a, a G-protein coupled receptor primarily located in the pituitary and hypothalamus [25] [26]. The activation of this receptor initiates a signaling cascade that results in the pulsatile release of endogenous GH. The following diagram illustrates the core signaling pathway and physiological effects.
Diagram 1: GHS Signaling Pathway and Effects. MK-677 and capromorelin act as agonists at the GHSR1a, mimicking the action of endogenous ghrelin to stimulate pulsatile GH release, which in turn drives systemic effects both directly and via IGF-1. Note the negative feedback loop.
A critical distinction between GHS and recombinant GH therapy is that GHS promote a pulsatile release of GH that remains subject to the body's natural negative feedback mechanisms, primarily through IGF-1, which may help prevent persistent supratherapeutic GH levels [32]. Furthermore, GHSR1a activation has been shown to influence appetite centers in the hypothalamus, explaining the orexigenic (appetite-stimulating) effect commonly observed with these agents [26] [64].
The Scientist's Toolkit: Essential Research Reagents
Successful investigation of GHS requires a specific set of reagents and assays. The following table details key materials for studying the pharmacology and efficacy of compounds like MK-677 and capromorelin.
Table 2: Key Research Reagent Solutions for GHS Investigations
| Reagent / Material | Function and Application in GHS Research |
|---|---|
| GHSR1a Expression Systems | Cell lines (e.g., HEK-293) engineered to overexpress the human GHSR1a are used for initial compound screening, binding affinity studies (e.g., using [35S]MK-0677), and signal transduction assays [26]. |
| MK-677 (Ibutamoren) | A potent, orally active, and long-acting benzolactam GHS used as a reference standard in vitro and in vivo. Its high oral bioavailability and ~4.7-hour half-life make it suitable for once-daily dosing in animal studies and clinical trials [25] [32]. |
| Capromorelin | An orally active spiropiperidine GHS used as a reference standard. Compared to MK-677, it may have a shorter half-life, necessitating twice-daily dosing in some species to sustain IGF-1 elevation [25] [14]. |
| GH & IGF-1 ELISA Kits | Essential for quantifying hormone levels in serum and tissue culture media. IGF-1 levels are often used as a surrogate marker for integrated GH secretion due to its longer half-life [25] [27]. |
| Rat Pituitary Cell Cultures | Primary cultures are a foundational functional assay for testing the GH-releasing potency of GHS and for studying synergism with GHRH [25] [32]. |
MK-677 and capromorelin are both effective GHS that amplify the pulsatile secretion of GH, leading to increased IGF-1 levels and anabolic outcomes such as increased lean body mass. The indirect comparison suggests that while both agents produce similar effects on body composition, differences in their pharmacokinetics and study populations may influence functional outcomes and tolerability. MK-677's once-daily dosing is a potential advantage, but its impact on glucose metabolism warrants careful monitoring. Capromorelin has demonstrated efficacy in improving physical function and, in veterinary medicine, has proven effective for weight gain. The choice between these agents in a research or development context should be guided by the specific therapeutic goals, desired dosing regimen, and the risk-benefit profile of the target population. Future direct comparative trials are needed to definitively establish their relative efficacy and safety.
The therapeutic elevation of growth hormone (GH) levels has traditionally been achieved through administration of recombinant human GH (rhGH). While effective, this approach bypasses the body's intricate regulatory systems, leading to non-physiological hormone profiles and potential disruption of endogenous feedback mechanisms. In contrast, growth hormone secretagogues (GHSs) such as MK-677 (ibutamoren) and capromorelin represent a paradigm shift by stimulating the body's own pulsatile GH release mechanisms through targeted activation of the ghrelin receptor (GHS-R1a) [65]. This pharmacological strategy preserves the natural rhythmicity of GH secretion and maintains intact negative feedback loops, potentially offering superior safety and efficacy profiles compared to direct hormone replacement [66] [67]. This Application Note details the experimental evidence, molecular mechanisms, and research methodologies supporting these advantages within clinical trials research frameworks.
Quantitative Comparative Analysis: GHS vs. Recombinant GH
Table 1: Comparative Analysis of GH Secretagogues versus Recombinant GH
| Parameter | Recombinant GH | MK-677 (Ibutamoren) | Capromorelin |
|---|---|---|---|
| Mechanism of Action | Direct hormone replacement; bypasses endogenous regulation [65] | Oral GHS-R1a agonist; stimulates endogenous GH secretion [49] [65] | Oral GHS-R1a agonist; stimulates endogenous GH secretion [68] |
| Secretory Profile | Non-physiological, constant elevation [65] | Preserved pulsatile secretion [65] [69] | Preserved pulsatile secretion (inferred from mechanism) |
| Feedback Loops | Overrides IGF-1 negative feedback, potentially causing suppression [66] | Preserves hypothalamic-pituitary (GH/IGF-1) negative feedback [66] [65] | Preserves hypothalamic-pituitary (GH/IGF-1) negative feedback [68] |
| Administration Route | Subcutaneous/Intramuscular injection | Oral [49] [65] | Oral [68] |
| Key Experimental Findings | N/A | Increased peak GH by 1.8-fold acutely; prolonged admin increased hypothalamic somatostatin [49] | 3 mg/kg/day for 7d increased body weight and IGF-1 in rhesus macaques [68] |
| Primary Research Applications | Severe GH deficiency, replacement therapy | Age-related decline, muscle wasting, functional restoration [65] [67] | Inappetence, weight loss, cachexia [68] |
Table 2: Experimental Outcomes from Preclinical and Clinical GHS Studies
| Study Compound | Model System | Dosing Regimen | Efficacy Outcomes | Safety & Feedback Observations |
|---|---|---|---|---|
| MK-677 [49] | Female Sprague-Dawley Rats (~4 weeks old) | 4 mg/kg orally for 6 weeks | Acute: 1.8-fold ↑ peak GH.Chronic: No significant increase in body growth, body length, or serum IGF-1. | GH response abolished after 6 weeks; ↑ hypothalamic somatostatin mRNA & protein; ↓ SSTR-2 in pituitary. |
| Capromorelin [68] | Rhesus Macaques (Healthy Adults) | 3 mg/kg orally daily for 7 days | Significant Increase vs. Controls: Body weight (10.5 vs. 10.1 kg) and IGF-1 levels (758 vs. 639 ng/mL). | No appreciable changes in hematologic/biochemical values; well-tolerated. |
| LUM-201 [69] | Pediatric GHD Patients (n=22) | 1.6 and 3.2 mg/kg/day for 6 months | Altered GH pulsatility pattern; changes correlated with height velocity. | Demonstrates the ability to modulate the endogenous GH secretory pattern. |
Detailed Experimental Protocols
Protocol for Assessing Chronic MK-677 Effects in a Rodent Model
This protocol is adapted from the study investigating the effects of prolonged MK-677 administration in rats [49].
I. Research Objective To investigate the sustained effects of oral MK-677 on somatic growth, GH secretion, and the expression of key genes and proteins in the GH regulatory axis.
II. Materials and Reagents
- Test Compound: MK-677, prepared as a 1 mg/mL solution in distilled water.
- Animals: Female Sprague-Dawley rats, approximately 4 weeks of age.
- Key Reagents:
- ELISA kits for rat GH and IGF-1.
- TRIzol reagent for RNA isolation.
- Specific antibodies for GHSR, somatostatin, and SSTR-2 for Western immunoblotting.
- Equipment for RT-PCR.
III. Methodology
- Acute GH Response Test:
- Fast rats for 8 hours with water ad libitum.
- Administer MK-677 (2 or 4 mg/kg) or vehicle (distilled water) via gastric tube.
- Collect blood samples from the tail vein at 0, 30, 60, 90, and 120 minutes post-administration.
- Centrifuge samples to obtain plasma and store at -70°C for GH analysis by ELISA.
Chronic Dosing and Growth Study:
- Administer MK-677 (4 mg/kg) or vehicle orally daily for 6 weeks.
- Measure body weight and body length (nose-to-anus) daily.
- Collect blood samples every 2 weeks for IGF-1 analysis.
- At the endpoint (6 weeks), sacrifice animals and collect tissues:
- Pituitary and Hypothalamus: Snap-freeze for mRNA and protein analysis.
- Tibia: Fix in 4% paraformaldehyde for decalcification, paraffin embedding, and sectioning for growth plate width measurement (H&E staining).
Molecular Analysis:
- Gene Expression: Perform RT-PCR on pituitary and hypothalamic tissues for GH, GHRH, GHSR, SST, and SSTR mRNA expression.
- Protein Expression: Conduct Western immunoblotting for GHSR, SST, and SSTR-2 protein levels.
IV. Data Analysis
- Compare AUC for GH profiles, longitudinal growth data, and IGF-1 levels between treated and control groups.
- Analyze correlations between molecular expression data (mRNA and protein) and physiological outcomes.
Protocol for Evaluating Capromorelin Efficacy in Non-Human Primates
This protocol is adapted from the study testing capromorelin in rhesus macaques [68].
I. Research Objective To evaluate the safety and efficacy of a short-term course of capromorelin on body weight and IGF-1 levels in healthy adult rhesus macaques.
II. Materials and Reagents
- Test Compound: Capromorelin oral solution (FDA-approved for dogs).
- Animals: Healthy adult rhesus macaques.
- Key Reagents:
- ELISA kit for IGF-1.
- Equipment for standard hematology and clinical biochemistry analysis.
III. Methodology
- Study Design:
- Assign subjects to treatment (n=3 males, 3 females) or control (n=2 males, 2 females) groups.
- Administer capromorelin at 3 mg/kg or a equivalent volume of placebo orally once daily for 7 days.
- Monitoring and Sampling:
- Observe and record clinical signs daily.
- Weigh animals before, during, and at the end of the treatment period.
- Collect blood samples before, during, and after treatment for:
- IGF-1 level measurement.
- Standard hematology and biochemistry panels to assess safety.
IV. Data Analysis
- Use ANOVA or mixed-model analysis to compare baseline-adjusted mean body weights and IGF-1 levels between treated and control groups.
- Review hematology and biochemistry data for any significant shifts outside normal ranges.
Signaling Pathways and Neuroendocrine Mechanisms
The following diagram illustrates the complex hypothalamic-pituitary-liver axis regulated by GH secretagogues, highlighting the preservation of endogenous feedback loops.
Diagram 1: Neuroendocrine Regulation of GH Secretion by GHS. GHSs act as agonists at the GHS-R1a receptor, stimulating GHRH and inhibiting somatostatin (SST) release from the hypothalamus [66] [67]. This leads to pulsatile GH release from the pituitary, subsequent IGF-1 production by the liver, and intact negative feedback to regulate the system. Chronic MK-677 administration can increase hypothalamic SST expression, a potential desensitization mechanism [49].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for GHS Research
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| MK-677 (Ibutamoren) | Potent, orally active, non-peptidyl GHSR agonist with long half-life (~24h) [49] [65]. | Investigating sustained GH elevation and its effects on body composition in chronic disease or aging models [49]. |
| Capromorelin Oral Solution | Orally active GHSR agonist; FDA-approved for use in dogs [68]. | Studying appetite stimulation and weight gain in NHP models or translational veterinary research [68]. |
| GH & IGF-1 ELISA Kits | Quantify hormone levels in serum/plasma to assess compound efficacy and feedback loop activity [49] [68]. | Measuring acute GH response profiles and chronic IGF-1 changes in pre-clinical and clinical studies. |
| GHSR, SST, SSTR Antibodies | Detect protein expression and localization in hypothalamic and pituitary tissues via Western blot or IHC [49]. | Elucidating molecular adaptation mechanisms in the GH axis following prolonged GHS exposure [49]. |
| RT-PCR Assays | Measure mRNA expression of key genes (GH, GHRH, GHSR, SST, SSTRs) in neuroendocrine tissues [49]. | Profiling transcriptional changes in the GH regulatory pathway in response to treatment. |
The data consolidated in this Application Note robustly demonstrate that growth hormone secretagogues offer a physiologically nuanced alternative to recombinant GH therapy. The critical advantage lies in their capacity to preserve the endogenous pulsatile secretion of GH and maintain functional negative feedback loops via IGF-1 and hypothalamic somatostatin [66] [65] [67]. This results in a more natural hormonal profile, potentially mitigating long-term risks associated with non-pulsatile, high-dose rhGH therapy.
However, research challenges remain, notably the potential for desensitization with prolonged use, as observed with MK-677, possibly mediated by upregulated somatostatin signaling [49]. Future clinical trials research should prioritize the optimization of dosing regimens that maximize anabolic benefits while avoiding counter-regulatory responses. Furthermore, the differential effects of GHSs on various populations—from pediatric GH deficiency to age-related sarcopenia—warrant continued investigation using the detailed protocols and analytical frameworks outlined herein.
Male hypogonadism is a clinical syndrome characterized by low serum testosterone levels and symptoms such as decreased libido, reduced bone mass, increased fat mass, and other metabolic disturbances [36]. While testosterone therapy (TTh) remains the gold standard treatment, its benefits on body composition are not always consistent across different patient populations [36]. Emerging evidence suggests that Growth Hormone Secretagogues (GHS) may offer a novel adjunctive approach to managing hypogonadal symptoms, particularly for addressing fat gain and muscular atrophy that may persist despite adequate TTh [36].
GHS represent a class of synthetic peptide or non-peptide agents that stimulate endogenous growth hormone (GH) release through direct growth hormone-releasing hormone (GHRH) mimicry or via interactions with ghrelin/growth hormone secretagogue receptors (GHS-R) [36]. Unlike recombinant GH therapy, which is tightly regulated and carries potential safety concerns, GHS promote pulsatile GH secretion that is subject to the body's natural negative feedback mechanisms, potentially offering a safer physiological profile [32]. This application note examines the current evidence and proposes experimental protocols for evaluating GHS as adjunctive therapy to testosterone in hypogonadal management.
Growth Hormone Secretagogues: Mechanisms and Key Compounds
Physiological Mechanisms of Action
GHS exert their effects primarily through two distinct mechanisms targeting the GH axis:
- GHRH Mimicry: Compounds such as sermorelin act as GHRH analogs, binding to GHRH receptors in the pituitary and stimulating GH release through the cAMP/protein kinase A pathway [70] [36].
- Ghrelin Receptor Agonism: Compounds including capromorelin, ibutamoren (MK-677), and various growth hormone-releasing peptides (GHRP-2, GHRP-6, ipamorelin) mimic ghrelin by binding to GHS-R, a G protein-coupled receptor that activates phospholipase C and intracellular calcium mobilization [9] [14] [32].
These mechanisms work synergistically when combined [32]. The resulting GH release stimulates hepatic insulin-like growth factor-1 (IGF-1) production, which mediates many anabolic effects while providing negative feedback to prevent uncontrolled GH secretion [9] [32].
Key GHS Compounds and Characteristics
Table 1: Key Growth Hormone Secretagogue Compounds and Characteristics
| Compound | Class | Primary Mechanism | Oral Availability | Half-Life | Key Clinical Findings |
|---|---|---|---|---|---|
| Capromorelin | Ghrelin Agonist | GHS-R Agonism | High (Oral Solution) | Designed for daily dosing [9] | +5.18% body weight in cats with CKD; improved lean body mass & physical function in elderly humans [9] [14] |
| Ibutamoren (MK-677) | Ghrelin Agonist | GHS-R Agonism | >60% [32] | ~4-6 hours [32] | Increased IGF-1 levels, increased fat-free mass, improved sleep architecture [32] |
| Sermorelin | GHRH Analog | GHRH Receptor Agonism | Low (requires injection) [70] | Short (requires multiple daily doses) [70] | Increased GH pulsatility, elevated IGF-1 in elderly to youthful levels [36] |
| GHRP-2 | Synthetic Peptide | GHS-R Agonism | 0.3-1.0% [32] | ~30 minutes [32] | Increased growth velocity in children, appetite stimulation [32] |
| GHRP-6 | Synthetic Peptide | GHS-R Agonism | 0.3% [32] | ~20 minutes [32] | Appetite stimulation, restored GH secretion in obesity [32] |
| Ipamorelin | Synthetic Peptide | GHS-R Agonism | Low (requires injection) | Short (requires multiple doses) | Selective GH release without affecting cortisol or prolactin [71] |
| CJC-1295 | GHRH Analog | GHRH Receptor Agonism | Low (requires injection) | Long (modified for sustained release) | Increased baseline GH secretion and pulsatility [71] |
Figure 1: GHS Signaling Pathways and Mechanisms of Action. GHS compounds work through two primary mechanisms: GHRH mimicry or ghrelin receptor agonism, both ultimately stimulating pituitary GH secretion and downstream anabolic effects.
Efficacy Endpoints in Clinical Trials
Table 2: Summary of Quantitative Efficacy Data from GHS Clinical Studies
| Study Compound & Population | Study Design | Key Efficacy Endpoints | Results | Safety Findings |
|---|---|---|---|---|
| Capromorelin in cats with CKD [9] | Randomized, masked, placebo-controlled, multicenter field study (n=176 cats) | Body weight change over 55 days | +5.18% body weight (capromorelin) vs. -1.65% (placebo); Treatment effect: +6.81% (P<0.0001) | Hypersalivation significant in capromorelin group; Other AEs not significantly different between groups |
| GHRP/SERM in hypogonadal men [72] | Retrospective review (n=14 men on TTh) | IGF-1 level changes | Baseline: 159.5 ng/mL; Post-treatment: 239.0 ng/mL (p<0.0001) | Well tolerated; No significant changes in LH, FSH, or estradiol |
| Ibutamoren in healthy elderly [32] | Multiple clinical trials | Body composition changes | Increased fat-free mass; Decreased LDL cholesterol; Improved functional recovery post-hip fracture | Increased appetite, musculoskeletal pain, fluid retention, decreased insulin sensitivity |
| Testosterone + GHRP-2/GHRH in older men [73] | Randomized, double-blind, crossover design (n=7) | GH and IGF-1 secretion | Testosterone increased fasting GH (P<0.01) and IGF-1 (P=0.003); Did not alter responses to secretagogues | Testosterone supplementation did not potentiate secretagogue efficacy |
Safety and Tolerability Profile
The safety profile of GHS is generally favorable, with most adverse effects being mild and transient [32]. Common side effects include increased appetite, mild fluid retention, and transient elevations in cortisol and prolactin (particularly with GHRP-6 and ibutamoren) [32]. A significant consideration is the potential for decreased insulin sensitivity and increased fasting blood glucose levels, which has been observed with ibutamoren and capromorelin [14] [32]. Notably, a clinical trial of capromorelin in older adults was stopped prematurely due to increased body weight and fasting glucose, despite improvements in lean mass and functional performance [14]. Hypersalivation has been specifically reported with capromorelin in feline studies [9].
Experimental Protocols for GHS Evaluation
In Vitro Receptor Binding and Activation Assays
Objective: To evaluate the binding affinity and functional activity of GHS compounds at GHS-R and GHRH receptors.
Materials:
- HEK-293 or CHO-K1 cells stably expressing human GHS-R or GHRH receptor
- Test compounds (capromorelin, ibutamoren, sermorelin, GHRP-2, GHRP-6)
- Radiolabeled ghrelin (for GHS-R) or GHRH (for GHRH receptor)
- cAMP assay kit (for GHRH receptor signaling)
- IP3 assay kit or calcium flux dyes (for GHS-R signaling)
- Cell culture reagents and equipment
Methodology:
- Cell Culture: Maintain recombinant cell lines in appropriate media with selection antibiotics.
- Receptor Binding:
- Plate cells at 50,000 cells/well in 96-well plates.
- Incubate with test compounds and fixed concentration of radiolabeled ligand for 1 hour at 4°C.
- Determine IC50 values by measuring displacement of radiolabeled ligand.
- Functional Assays:
- GHS-R Activity: Measure intracellular calcium flux using fluorescent dyes or IP3 accumulation after compound exposure.
- GHRH Receptor Activity: Quantify cAMP production using ELISA or FRET-based assays.
- Data Analysis: Calculate EC50 and Emax values for functional responses. Compare potency and efficacy across compound classes.
In Vivo Efficacy Study in Hypogonadal Animal Model
Objective: To assess the effects of GHS alone and in combination with testosterone on body composition and metabolic parameters in hypogonadal animals.
Materials:
- Orchidectomized male rodent model (rats or mice)
- Test compounds: Testosterone propionate, selected GHS (e.g., capromorelin, ibutamoren)
- DEXA or MRI for body composition analysis
- Metabolic cages for energy expenditure assessment
- ELISA kits for GH, IGF-1, testosterone, and metabolic biomarkers
Methodology:
- Induction of Hypogonadism: Perform orchidectomy or sham surgery under anesthesia.
- Treatment Groups (n=10-12/group):
- Sham control
- Hypogonadal + vehicle
- Hypogonadal + testosterone (physiological replacement dose)
- Hypogonadal + GHS
- Hypogonadal + testosterone + GHS
- Dosing Protocol: Administer compounds daily for 8-12 weeks. Testosterone via slow-release implant; GHS via oral gavage (ibutamoren, capromorelin) or subcutaneous injection (sermorelin, GHRPs).
- Endpoint Assessments:
- Weekly: Body weight, food intake
- Bi-weekly: Body composition (DEXA)
- Terminal (week 8-12): Serum hormones, tissue weights, muscle histology, gene expression of anabolic/catabolic markers
Figure 2: Experimental Workflow for In Vivo Efficacy Studies. HGX = Hypogonadal.
Clinical Trial Protocol for Adjunctive Therapy in Hypogonadal Men
Objective: To evaluate the safety and efficacy of GHS as adjunctive therapy to testosterone in men with hypogonadism and suboptimal response to TTh.
Study Design: Randomized, double-blind, placebo-controlled, parallel-group study.
Population: Hypogonadal men (total testosterone <300 ng/dL) on stable TTh for ≥3 months with persistent symptoms (increased fat mass, decreased lean mass, reduced vitality).
Interventions:
- Active group: Stable TTh + GHS (e.g., capromorelin 10-30mg daily or ibutamoren 10-25mg daily)
- Control group: Stable TTh + matching placebo
Primary Endpoints:
- Change in lean body mass (DEXA) from baseline to 6 months
- Change in visceral adipose tissue (MRI) from baseline to 6 months
Secondary Endpoints:
- Change in IGF-1 levels
- Change in fasting glucose and HOMA-IR
- Changes in strength (grip strength, leg press)
- Patient-reported outcomes (quality of life, energy levels)
Safety Monitoring: Comprehensive metabolic panel, hemoglobin A1c, cortisol, prolactin, adverse event monitoring throughout study.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Research Reagents for GHS Investigations
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| GHS Compounds | Capromorelin, Ibutamoren, GHRP-2, GHRP-6, Ipamorelin, Sermorelin | In vitro screening and in vivo efficacy studies | Source purity critical; use pharmaceutical-grade from compounding pharmacies for clinical studies [71] |
| Cell-Based Assay Systems | HEK-293/GHS-R, CHO-K1/GHRH-R stable cell lines | Receptor binding and functional characterization | Validate receptor expression and coupling; monitor passage number effects |
| Animal Models | Orchidectomized rodents, aged rodent models | Efficacy studies in controlled hypogonadal state | Confirm hormone depletion; consider genetic background influences |
| Analytical Tools | IGF-1 ELISA, GH ELISA, LC-MS/MS for hormone quantification | Biomarker quantification in serum and tissues | Establish assay sensitivity and dynamic range for expected concentrations |
| Body Composition Instruments | DEXA, MRI, EchoMRI | Longitudinal body composition analysis | Calibrate instruments regularly; use consistent positioning |
| Molecular Biology Reagents | qPCR assays for anabolic/catabolic genes | Mechanism of action studies | Normalize to appropriate housekeeping genes |
Growth Hormone Secretagogues represent a promising therapeutic class for addressing the body composition limitations that may persist with testosterone therapy alone in hypogonadal men. Current evidence, while limited, suggests that GHS can effectively increase IGF-1 levels, promote lean mass accretion, and reduce adiposity through mechanisms that preserve physiological pulsatile GH secretion [72] [36] [32].
Future research should prioritize well-controlled clinical trials combining GHS with testosterone in clearly defined hypogonadal populations, particularly those with demonstrated suboptimal response to TTh alone. Important considerations include patient stratification strategies, long-term safety monitoring (especially regarding glucose metabolism), and optimization of dosing regimens to maximize benefit-risk profiles. The development of novel GHS compounds with improved tissue selectivity and metabolic profiles may further enhance the therapeutic potential of this approach in hypogonadal management.
Growth hormone secretagogues (GHSs) represent a class of therapeutic agents that stimulate the ghrelin receptor, also known as the growth hormone secretagogue receptor (GHS-R), to enhance pulsatile growth hormone (GH) release and insulin-like growth factor-1 (IGF-1) production [26]. The GHS-R is a G-protein coupled receptor expressed in the hypothalamus and pituitary gland that functions as a subtle enhancer of the GH-insulin-like growth factor-1 (IGF-1) axis and energy homeostasis [26]. This application note provides a comprehensive analysis of the regulatory status, discontinued indications, and future clinical potential of two prominent GHSs: capromorelin and ibutamoren (MK-677), with structured data presentation and experimental protocols for research applications.
Mechanisms of Action and Signaling Pathways
GHSs function as agonists of the GHS-R, mimicking the effects of the endogenous hormone ghrelin [9]. The binding of GHSs to GHS-R initiates a complex signaling cascade that ultimately regulates growth and metabolism.
Table 1: Key Components of the GHS Signaling Pathway
| Component | Type | Primary Function | Localization |
|---|---|---|---|
| Ghrelin | Endogenous Hormone | Natural GHS-R agonist; stimulates appetite & GH secretion | Stomach (primarily) |
| GHS-R (Growth Hormone Secretagogue Receptor) | G-protein coupled receptor | Mediates effects of ghrelin & synthetic GHSs | Hypothalamus, Pituitary |
| Growth Hormone (GH) | Pituitary Hormone | Anabolic effects; stimulates IGF-1 production | Pituitary Gland |
| Insulin-like Growth Factor-1 (IGF-1) | Liver-derived Hormone | Mediates many growth-promoting effects of GH | Liver (circulating) |
The mechanistic understanding of GHS action reveals that these compounds bind to GHS-R in both the hypothalamus, to stimulate appetite and food-seeking behaviors, and the pituitary gland, to stimulate secretion of GH [9]. The subsequent increase in GH stimulates IGF-1 release from the liver, creating a powerful anabolic axis that influences body composition, muscle mass, and energy metabolism [9] [26].
Figure 1: Core Signaling Pathway of Growth Hormone Secretagogues (GHSs)
Comparative Analysis of Capromorelin and Ibutamoren
Development Status and Key Indications
Table 2: Clinical Development Status of Select Growth Hormone Secretagogues
| Compound | Current Approved Status | Key Studied Indications | Discontinued/Failed Indications | Regulatory Status |
|---|---|---|---|---|
| Capromorelin | Approved for veterinary use (cats) | Chronic weight loss in cats with CKD [9] | Human aging/frailty (development unclear) | WADA Prohibited (S2.2.4) [74] |
| Ibutamoren (MK-677) | Not approved for human use | Hip fracture recovery, Alzheimer's disease, aging/frailty [64] | Hip fracture recovery (trials halted) [64] | WADA Prohibited (S2.2.4) [74] |
Efficacy Data from Clinical Studies
Table 3: Quantitative Efficacy Outcomes from Clinical Trials
| Trial Parameter | Capromorelin (Cats with CKD) | Ibutamoren (Human Studies) |
|---|---|---|
| Study Duration | 55 days [9] | 2 weeks - 24 months [64] |
| Body Weight Change | +5.18% (95% CI 3.45-6.91) [9] | Increased LBM in elderly [64] |
| Placebo Comparison | -1.65% (95% CI -3.82-0.55) [9] | Varied across studies [64] |
| Treatment Effect | +6.81% (P<0.0001) [9] | Not consistently quantified |
| Lean Body Mass | Not specifically measured | Sustained gains demonstrated [64] |
Discontinued Indications and Safety Concerns
Analysis of Clinical Trial Failures and Haltings
The development pathway for GHSs has been marked by both promising therapeutic effects and significant safety concerns that have limited clinical translation. Ibutamoren specifically demonstrated concerning safety signals in certain patient populations that led to trial discontinuations:
Congestive Heart Failure Risk: A randomized, double-blinded, placebo-controlled trial investigating ibutamoren for recovery after hip fracture in elderly patients was stopped early due to safety concerns. The study identified that 6.5% of patients in the ibutamoren group (4/61) developed congestive heart failure compared to 1.7% (1/60) in the placebo group [64].
Glucose Metabolism Impairment: Multiple studies with ibutamoren demonstrated significant disturbances in glucose homeostasis. Chapman et al. observed that ibutamoren 25 mg/d increased glucose concentrations by 25.3% and 26.9% above baseline at 2 and 4 weeks, respectively, in healthy elderly patients [64]. Additionally, a large trial in Alzheimer's patients found more participants with increased blood glucose levels in the ibutamoren group (15.4%) versus placebo (4.6%) [64].
Thrombosis Events: Bach et al. reported more thromboses in the ibutamoren group compared to placebo in a study of hip fracture recovery, though these events were not believed to be drug-related by the investigators [64].
Comparative Safety Profiles
Figure 2: Adverse Event Profiles of Growth Hormone Secretagogues
Experimental Protocols
Protocol for Evaluating GHS Efficacy in Weight Loss Models
This protocol outlines methodology for assessing the efficacy of GHS compounds in animal models of disease-related weight loss, based on the successful capromorelin field study in cats with chronic kidney disease [9].
Objective: To evaluate the effectiveness of GHS administration in reversing unintended weight loss and promoting weight gain in subjects with chronic disease.
Materials and Reagents:
- Test compound (GHS such as capromorelin or ibutamoren)
- Vehicle control (identical formulation without active compound)
- Animal model with documented chronic disease and ≥5% unintentional weight loss
- Precision weighing scale (accurate to 0.1 kg)
- Clinical pathology equipment for hematology, serum chemistry, and urinalysis
Methods:
- Subject Enrollment: Select subjects with confirmed chronic disease (e.g., CKD per IRIS guidelines) and documented unintended weight loss of at least 5% over a defined period. Exclude subjects with congestive heart failure, active cancer, or diabetes mellitus [9].
- Randomization and Masking: Randomize subjects 2:1 to treatment or control groups using computer-generated randomization tables with block length of three. Maintain masking of investigators, examining veterinarians, and study staff throughout the trial [9].
- Dosing Protocol: Administer GHS compound at 2 mg/kg (0.1 ml/kg) orally once daily for 55 days. Control group receives vehicle control at same volume. Calculate dose based on day 0 body weight without adjustment during study [9].
- Endpoint Assessments:
- Primary Efficacy Endpoint: Body weight measurements in kilograms recorded to at least one-tenth kg at days 0, 15, 27, and 55.
- Safety Assessments: Clinical pathology tests (hematology, serum chemistry), physical examinations, and adverse event monitoring throughout study.
- Additional Parameters: Body condition scoring, muscle condition scoring, and food intake documentation.
- Statistical Analysis: Use mixed models with treatment as fixed effect and site as random effect. Report two-tailed P values and 95% confidence intervals for change in body weight with alpha = 0.05.
Protocol for Assessing Metabolic Impacts of GHS Treatment
This protocol addresses the critical safety assessment of GHS effects on glucose metabolism, based on observed hyperglycemia in ibutamoren clinical trials [64].
Objective: To evaluate the impact of GHS treatment on glucose homeostasis and insulin sensitivity.
Materials and Reagents:
- Test compound (GHS)
- Vehicle control
- Glucose assay kit
- Insulin ELISA kit
- HbA1c measurement system
- Equipment for oral glucose tolerance tests (OGTT)
Methods:
- Study Design: Randomized, controlled design with baseline and periodic metabolic assessments.
- Glucose Monitoring:
- Measure fasting blood glucose at baseline and weekly intervals.
- Perform oral glucose tolerance tests at baseline and after 4 weeks of treatment.
- Monitor hemoglobin A1c (HbA1c) levels at baseline and study conclusion.
- Insensitivity Assessment: Evaluate insulin sensitivity through:
- Fasting insulin levels
- Homeostatic model assessment of insulin resistance (HOMA-IR)
- Insulin response during OGTT
- Statistical Analysis: Compare metabolic parameters between treatment and control groups using appropriate statistical tests (t-tests, ANOVA with repeated measures).
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for GHS Investigations
| Reagent/Category | Specific Examples | Research Application | Function in GHS Studies |
|---|---|---|---|
| Synthetic GHS Compounds | Capromorelin, Ibutamoren (MK-677), Ipamorelin, Tabimorelin [74] | In vitro and in vivo efficacy studies | GHS-R agonists to stimulate GH release and appetite |
| GHS-R Expression Systems | Engineered cell lines overexpressing GHS-R [26] | Receptor binding and signaling studies | Target for identifying endogenous agonists and compound screening |
| Ghrelin Detection Assays | Ghrelin ELISA, Ghrelin mRNA measurement (RT-PCR) [26] | Mechanistic and physiological studies | Quantify endogenous ligand levels and regulation |
| GH/IGF-1 Axis Biomarkers | GH ELISA, IGF-1 immunoassays, IGFBP-3 measurements | Efficacy and safety pharmacodynamics | Monitor downstream effects of GHS receptor activation |
| Glucose Homeostasis Tools | Glucose assays, Insulin ELISAs, HbA1c tests, OGTT protocols [64] | Safety and metabolic impact assessments | Evaluate hyperglycemia risk and insulin sensitivity changes |
| Body Composition Methods | DEXA scans, BCS, MCS, precision weight scales [9] | Efficacy endpoint measurements | Quantify changes in lean body mass, adipose tissue, and muscle mass |
Regulatory Status and Prohibited Use
The World Anti-Doping Agency (WADA) explicitly prohibits GHSs in athletic competition. Both capromorelin and ibutamoren are classified under "S2.2 Peptide Hormones and Their Releasing Factors" specifically in the category of "Growth Hormone Releasing Factors" that includes "growth hormone secretagogues (GHS) and their mimetics" [74]. The prohibition applies at all times for both in- and out-of-competition testing [74].
Future Clinical Potential and Research Directions
Despite safety challenges that have limited clinical development, several potential therapeutic applications warrant further investigation:
Condition-Specific Cachexia: The demonstrated efficacy of capromorelin in cats with CKD-associated weight loss suggests potential for targeted use in specific cachexia populations where risk-benefit ratio may be favorable [9].
Ghrelin Replacement Strategy: Research suggests GHSs might function as "ghrelin replacement therapy" particularly in elderly populations where ghrelin production declines with age. Studies show ghrelin mRNA increases during development but declines to 5% of peak levels by 19 months in mice [26].
Pulsatile GH Restoration: Unlike direct GH administration, GHSs amplify the natural pulsatile secretion of GH, potentially offering a more physiological approach to GH augmentation that might reduce adverse effects [26].
Future research directions should focus on identifying patient populations with the most favorable risk-benefit profile, developing GHS compounds with improved safety profiles, particularly regarding glucose metabolism, and exploring targeted delivery systems to minimize systemic exposure.
Conclusion
The clinical investigation of MK-677 and capromorelin validates the GHS class as a potent strategy for restoring GH pulsatility and improving body composition in aging and frail populations. While both compounds demonstrate significant increases in lean body mass and IGF-1 levels, their differential effects on functional outcomes and distinct side effect profiles underscore the need for precision in therapeutic application. Future research must prioritize overcoming metabolic side effects and desensitization, potentially through novel compound design or combination therapies. The promising results in specific functional domains, coupled with the oral bioavailability of these agents, solidify their position as a compelling area for continued biomedical research, particularly for conditions like sarcopenia, cachexia, and metabolic syndrome where current therapeutic options remain limited.
References
- 1. Synthetic Growth Hormone-Releasing Peptides (GHRPs) [https://pmc.ncbi.nlm.nih.gov/articles/PMC5392015/]
- 2. Frontiers | Ghrelin Receptors in Non-Mammalian Vertebrates [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2013.00081/full]
- 3. Advances in the Development of Nonpeptide Small Molecules ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8883476/]
- 4. Ghrelin receptor [https://www.guidetopharmacology.org/GRAC/ObjectDisplayForward?objectId=246]
- 5. Physiological, pathological and potential therapeutic roles ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644607000827]
- 6. Therapeutic effects of acylated ghrelin-specific receptor ... [https://www.nature.com/articles/s41598-021-00740-6]
- 7. Ghrelin Receptors [https://www.tocris.com/pharmacology/ghrelin-receptors]
- 8. Article Design, Biological Characterization, and Discovery ... [https://www.sciencedirect.com/org/science/article/abs/pii/S1520480425003163]
- 9. Capromorelin promotes weight gain in cats with unintended ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12603007/]
- 10. Capromorelin: a ghrelin receptor agonist and novel therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5813110/]
- 11. Structural basis of human ghrelin receptor signaling by ... [https://www.nature.com/articles/s41467-021-26735-5]
- 12. Ibutamoren [https://en.wikipedia.org/wiki/Ibutamoren]
- 13. The Use of Capromorelin for Inappetence [https://todaysveterinarypractice.com/pharmacology/the-use-of-capromorelin-for-the-clinical-problem-of-inappetence/]
- 14. Capromorelin - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/capromorelin]
- 15. II. Case example with ibutamoren (MK-677), a growth ... [https://www.sciencedirect.com/science/article/abs/pii/S0009898125004577]
- 16. Oral ghrelin receptor agonist MK-0677 increases serum ... [https://pubmed.ncbi.nlm.nih.gov/28340044/]
- 17. Growth hormone secretagogue receptor [https://en.wikipedia.org/wiki/Growth_hormone_secretagogue_receptor]
- 18. The Growth Hormone Secretagogue Receptor: Its Intracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3975427/]
- 19. A new understanding of GHSR1a [https://www.sciencedirect.com/science/article/abs/pii/S1568163720303226]
- 20. Growth Hormone Secretagogues and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2769045/]
- 21. Growth hormone secretagogues modulate the electrical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1573883/]
- 22. Ghrelin Receptor Signaling in Health and Disease: A Biased ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9852078/]
- 23. In vitro pharmacological characterization of growth ... [https://www.sciencedirect.com/science/article/pii/S0014299924005697]
- 24. Design, Biological Characterization, and Discovery of ... [https://pubmed.ncbi.nlm.nih.gov/40091212/]
- 25. Growth Hormone Secretagogues as Potential Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10272984/]
- 26. Growth hormone secretagogues: prospects and potential ... [https://www.sciencedirect.com/science/article/abs/pii/S1521690X04000247]
- 27. Effect of the Orally Active Growth Hormone Secretagogue ... [https://eymj.org/DOIx.php?id=10.3349/ymj.2018.59.10.1174]
- 28. Growth hormone secretagogues modulate inflammation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10130389/]
- 29. Wellness-enhancing effects of the canine growth hormone ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1609405/full]
- 30. Article Neuroendocrine circuit for sleep-dependent growth ... [https://www.sciencedirect.com/science/article/pii/S0092867425006269]
- 31. Phase 3 pivotal trial design of daily oral LUM-201’ [https://www.endocrine-abstracts.org/ea/0110/ea0110p648]
- 32. The Safety and Efficacy of Growth Hormone Secretagogues [https://pmc.ncbi.nlm.nih.gov/articles/PMC5632578/]
- 33. CLINICAL DEVELOPMENT OF GHRELIN AXIS DERIVED ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4121852/]
- 34. Ghrelin for cachexia | Journal of Cachexia, Sarcopenia and ... [https://link.springer.com/article/10.1007/s13539-010-0011-5]
- 35. Effects of an Oral Ghrelin Mimetic on Body Composition and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2757071/]
- 36. Beyond the androgen receptor: the role of growth hormone ... [https://tau.amegroups.org/article/view/33160/28655]
- 37. The Stair Climb Power Test as an Efficacy Outcome in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7984416/]
- 38. Is Stair Climb Power a Clinically Relevant Measure of Leg ... [https://www.sciencedirect.com/science/article/abs/pii/S0003999307001013]
- 39. Reliability, Validity, and Minimal Detectable Change of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6257032/]
- 40. Older adults' lower-limb muscle power production throughout ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0296074]
- 41. Ten-Second Tandem Stance Test: A Potential Tool to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8904864/]
- 42. Optimal cutoff score of the circular tandem walk test for ... [https://www.nature.com/articles/s41598-024-78934-x]
- 43. Pharmacological targeting of age-related changes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7100900/]
- 44. Insulin-Like Growth Factor-1 (IGF-1) and Its Monitoring in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7913862/]
- 45. Growth hormone/insulin-like growth factor I axis in health ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1456195/full]
- 46. Normative data for insulin-like growth factor-1 and ... [https://www.nature.com/articles/s41598-025-25235-6]
- 47. Repeat administration of the GH secretagogue MK-0677 ... [https://pubmed.ncbi.nlm.nih.gov/9071975/]
- 48. MK-0677 (ibutamoren mesylate) for the treatment of ... [https://www.sciencedirect.com/science/article/abs/pii/S0167494310002530]
- 49. Effect of the Orally Active Growth Hormone Secretagogue MK ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6240568/]
- 50. Rapid desensitisation of the GH secretagogue (ghrelin) ... [https://pubmed.ncbi.nlm.nih.gov/14669829/]
- 51. Effect of the Orally Active Growth Hormone Secretagogue ... [https://pubmed.ncbi.nlm.nih.gov/30450851/]
- 52. Physiology, Somatostatin - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK538327/]
- 53. Rapid desensitisation of the GH secretagogue (ghrelin) ... [https://link.springer.com/article/10.1007/BF03347357]
- 54. Somatostatin triggers rhythmic electrical firing in ... [https://www.nature.com/articles/srep24394]
- 55. Beyond the Hype: Potential Health Risks of MK-677 [https://www.getsmartaboutdrugs.gov/news-statistics/2025/07/08/beyond-hype-potential-health-risks-mk-677]
- 56. What you need to know about MK-677 (Ibutamoren) [https://healthymale.org.au/health-article/what-you-need-to-know-about-mk-677-ibutamoren/]
- 57. Management of Diabetes and Hyperglycemia in ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK279093/]
- 58. Inpatient Hyperglycemia Guideline Resources [https://www.endocrine.org/clinical-practice-guidelines/inpatient-hyperglycemia-guideline-resources]
- 59. MK-677 Side Effects: What You Should Know [https://elive-health.com/mk-677-side-effects/]
- 60. Ibutamoren (MK 677) Not OK - Don't Be Fooled By Marketing! [https://www.sportintegrity.gov.au/news/integrity-blog/2022-05/ibutamoren-mk-677-not-ok-dont-be-fooled-marketing]
- 61. Effects of growth hormone secretagogues on the release ... [https://www.sciencedirect.com/science/article/abs/pii/S1090023305001206]
- 62. - MK Side Effects | What Researchers Must Know 677 [https://www.peptides.org/mk-677-side-effects/]
- 63. Umbrella Labs Launches Research-Only Retatrutide, MK ... [https://finance.yahoo.com/news/umbrella-labs-launches-research-only-045700524.html]
- 64. Ibutamoren - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/medicine-and-dentistry/ibutamoren]
- 65. MK-677 (Ibutamoren): Unlocking Growth, Recovery, and ... [https://swolverine.com/blogs/blog/ibutamoren-mk-677-benefits-uses-side-effects?srsltid=AfmBOoqHrRMXum4s0JQDYa3_2roaAv5YQ_7y-HH8QHAc7NHHVnajWlNP]
- 66. Negative Feedback Loops and Hormonal Factors that ... [https://pubmed.ncbi.nlm.nih.gov/40908533/]
- 67. Growth Hormone in Aging - Endotext - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK279163/]
- 68. Evaluating the Safety and Efficacy of Capromorelin in Rhesus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11193426/]
- 69. SAT-186 Higher Order Time Series Interactions Within The ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12545624/]
- 70. Sermorelin: What It Is, FDA Status, Benefits, and Safety ... [https://healthon.com/blogs/journal/sermorelin-general?srsltid=AfmBOop2HoIBoBy5Y6kdB4-EaI8voQJc4bTOxYX-CUCIcWQuZnIG0YY0]
- 71. CJC-1295 + Ipamorelin | Benefits, Safety & Buying Advice ... [https://www.innerbody.com/cjc-1295-and-ipamorelin]
- 72. Growth Hormone Secretagogue Treatment in Hypogonadal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5675260/]
- 73. Testosterone supplementation in healthy older men drives GH ... [https://pubmed.ncbi.nlm.nih.gov/16189179/]
- 74. The Prohibited List | World Anti Doping ... [https://www.wada-ama.org/en/prohibited-list]