Hormonal Dynamics Across Menstrual Cycle Patterns: From Foundational Biology to Clinical and Therapeutic Applications
This article provides a comprehensive analysis of the hormonal trends underlying diverse menstrual cycle patterns, synthesizing foundational endocrinology with contemporary large-scale data analytics.
Hormonal Dynamics Across Menstrual Cycle Patterns: From Foundational Biology to Clinical and Therapeutic Applications
Abstract
This article provides a comprehensive analysis of the hormonal trends underlying diverse menstrual cycle patterns, synthesizing foundational endocrinology with contemporary large-scale data analytics. Tailored for researchers and drug development professionals, it explores the physiological basis of cycle variability, innovative methodologies for cycle phase detection, the impact of demographic factors like age and BMI on cycle characteristics, and the implications for validating therapeutic interventions. The synthesis aims to bridge the gap between basic science, real-world evidence, and the development of personalized hormone therapies and diagnostic tools.
The Endocrine Architecture of the Menstrual Cycle: Defining Normal and Variable Patterns
The Hypothalamic-Pituitary-Ovarian (HPO) Axis and Phase Regulation
The Hypothalamic-Pituitary-Ovarian (HPO) axis represents the primary regulatory system controlling the female reproductive cycle, orchestrating a complex series of hormonal events that occur in a precise, cyclical pattern. This sophisticated neuroendocrine axis integrates signals from the hypothalamus, pituitary gland, and ovaries to regulate menstrual cycle physiology through intricate feedback mechanisms. Understanding the phase regulation of the HPO axis is fundamental to reproductive endocrinology, providing critical insights for developing therapeutic interventions for ovulatory disorders, which account for approximately 25% of infertility diagnoses [1]. This guide objectively compares hormonal trends and experimental data across different menstrual cycle patterns, providing researchers and drug development professionals with methodological frameworks for investigating this essential physiological system.
HPO Axis Regulatory Mechanics and Phase Characteristics
Core Components and Signaling
The HPO axis functions as a synchronized communication network between the hypothalamus, anterior pituitary gland, and ovaries, regulating reproductive hormones through bidirectional signaling [1]. The hypothalamic unit contains specialized Gonadotropin-Releasing Hormone (GnRH) neurons that originate in the embryonic olfactory placode and migrate to the arcuate nucleus during fetal development [2]. These neurons release GnRH in pulsatile patterns approximately every hour when devoid of feedback influences, with this pulsatile release being absolutely essential for normal gonadotropin secretion [2]. The anterior pituitary gonadotropes respond to these GnRH pulses by synthesizing and releasing the gonadotropins Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH), which then act on ovarian receptors to stimulate folliculogenesis and steroid hormone production [2].
Menstrual Cycle Phase Regulation
The menstrual cycle is systematically divided into two primary phases—the follicular and luteal phases—separated by ovulation and ending with either fertilization or menstruation [3]. The follicular phase begins with menses and involves follicular recruitment, selection, and maturation under rising FSH influence, culminating in rising estradiol levels [2] [4]. The luteal phase begins after ovulation when the ruptured follicle transforms into the corpus luteum, secreting progesterone and estradiol in a characteristic bell-shaped pattern that lasts 13-15 days unless pregnancy occurs [2] [5].
The following table summarizes the key hormonal characteristics and regulatory mechanisms across menstrual cycle phases:
Table 1: Hormonal Regulation and Characteristics Across Menstrual Cycle Phases
| Cycle Phase | Duration | Dominant Hormones | Key Regulatory Mechanisms | Primary Ovarian Events |
|---|---|---|---|---|
| Follicular Phase | ~14 days (variable) | Low-to-rising estradiol, moderate FSH | Negative feedback of low estrogen on FSH/LH; switch to positive feedback near end | Follicular recruitment, selection, and maturation of dominant follicle |
| Ovulation | ~24 hours | Peak LH surge, high estradiol | Sustained high estradiol triggers positive feedback and GnRH surge | Rupture of mature follicle and oocyte release |
| Luteal Phase | 13-15 days (fixed) | High progesterone, moderate estradiol | Negative feedback of progesterone and estrogen on FSH/LH | Corpus luteum formation and secretory activity; regression if no pregnancy |
Feedback Control Systems
The HPO axis employs sophisticated feedback mechanisms that switch between negative and positive regulation to control cycle progression. During most of the cycle, moderate estrogen levels exert negative feedback on GnRH and gonadotropin secretion [4]. However, in a critical regulatory shift, high estrogen levels in the late follicular phase (in the absence of progesterone) initiate positive feedback on the HPG axis, resulting in the preovulatory GnRH and LH surges necessary for ovulation [4] [5]. The mechanisms enabling this switch are not fully understood but involve increased GnRH receptor expression and enhanced gonadotrope sensitivity [5]. Following ovulation, progesterone dominates and, in the presence of estrogen, re-establishes negative feedback throughout the luteal phase [4].
Experimental Methodologies for HPO Axis Investigation
Hormonal Assessment Protocols
Longitudinal hormonal monitoring across the menstrual cycle requires precise methodological approaches. The GnRH stimulation test represents a conventional diagnostic protocol that involves an initial baseline blood draw, intravenous administration of GnRH, followed by multiple blood samples collected over two hours, with a final sample taken 24 hours post-administration [1]. This test assesses FSH, LH, and sex hormone dynamics to evaluate GnRH function and pituitary responsiveness. For comprehensive hormonal mapping, the DUTCH Cycle Mapping Plus protocol utilizes dry urine samples collected throughout the menstrual cycle to assess sex hormone variability and cortisol patterns, providing a non-invasive method for evaluating HPO axis function [1].
Cycle Phase Determination Methods
Accurate menstrual cycle phase determination is essential for valid HPO axis research. The following table compares common methodological approaches for cycle phase assessment:
Table 2: Methodological Approaches for Menstrual Cycle Phase Determination
| Method Type | Specific Techniques | Key Measured Parameters | Accuracy Considerations | Practical Applications |
|---|---|---|---|---|
| Counting Methods | Forward counting from menstruation; backward counting from next menses | Cycle day assignment based on start date of bleeding | Limited accuracy; assumes standardized cycle length | Initial screening; large epidemiological studies |
| Ovulation Detection | Urinary LH surge detection; basal body temperature (BBT) tracking | LH peak identification; BBT biphasic pattern confirmation | High accuracy for ovulation timing; BBT confirms ovulation after occurrence | Fertility monitoring; phase-specific interventions |
| Hormonal Verification | Serum progesterone (>3 ng/mL indicates ovulation); estradiol levels | Direct measurement of steroid hormones from blood samples | Highest accuracy; resource-intensive | Clinical trials; precise endocrine profiling |
The most rigorous research protocols implement LH peak detection or serum progesterone measurement to definitively confirm ovulation and phase assignment, as counting methods alone frequently misclassify cycle phases [6]. For determining ovulatory cycles via BBT, researchers typically define a biphasic pattern as a difference greater than 0.3°C between the mean luteal phase temperature (10 days preceding next menstruation) and follicular phase temperature (first 10 days from cycle start) [7].
Advanced Assessment Techniques
Functional medicine laboratories often incorporate Anti-Müllerian Hormone (AMH) testing to assess ovarian reserve and follicular status, with particularly high levels indicating conditions like Polycystic Ovarian Syndrome (PCOS) [1]. Complete thyroid panels including thyroid antibodies help evaluate thyroid involvement in HPO axis dysfunction, as both primary hypothyroidism and autoimmune thyroiditis can disrupt ovulatory function [1]. For structural assessment, magnetic resonance imaging (MRI) can identify intracranial tumors, pituitary abnormalities, or other anatomical variants that may disrupt HPO axis signaling at the hypothalamic or pituitary level [1].
Quantitative Hormonal Trends and Dysregulation Patterns
Normative Hormonal Fluctuations
In normally cycling women, characteristic hormonal patterns emerge across phases. FSH demonstrates a small but significant rise at the end of the preceding menstrual cycle, initiating recruitment of secondary early antral follicles [2]. Estradiol levels rise progressively during follicular development, reaching peak concentrations (approximately 200-400 pg/mL) just before ovulation when the dominant follicle achieves maturation [2]. The LH surge rises dramatically (near-tripling baseline levels) to trigger ovulation, while progesterone remains low during the follicular phase but rises sharply after ovulation to peak levels approximately 7 days post-ovulation [2] [5].
Body Mass Index (BMI) Influence on Cycle Characteristics
Recent large-scale research utilizing smartphone application data from 8,745 participants with 191,426 menstrual cycles has quantified the nonlinear relationship between BMI and menstrual cycle regularity [7]. The findings demonstrate that individuals with a BMI of 20 kg/m² showed optimal cycle characteristics, with both lower and higher BMI values associated with progressively greater cycle irregularities:
Table 3: BMI Impact on Menstrual Cycle Parameters (Adapted from Itoi et al., 2025)
| BMI Category | Cycle Length Change vs. BMI 20 | Infrequent Menstrual Bleeding Risk (OR) | Absent Menstrual Bleeding Risk (OR) | Biphasic Cycle Proportion |
|---|---|---|---|---|
| Underweight (≤16 kg/m²) | +1.03 days | Significantly higher | 1.78 | Decreased |
| Normal (18.5-22.9 kg/m²) | Reference | Reference | Reference | Optimal |
| Overweight (23-24.9 kg/m²) | Minimal change | 1.56 | Not significant | Slightly decreased |
| Obese (25-35 kg/m²) | +1.06 days | 2.63 | 1.94 | Significantly decreased |
This research established an inverted J-shaped relationship between BMI and the proportion of biphasic cycles, confirming that both low and high BMI increase the risk of anovulatory cycles and potential ovulatory infertility [7]. The data specifically indicated that AMB risk became significantly higher at BMI values ≤19 kg/m² or ≥26 kg/m² compared to the optimal BMI of 20 kg/m² [7].
HPO Axis Dysfunction Classification
The World Health Organization categorizes ovulatory disorders resulting from HPO axis dysfunction into three distinct groups [1]. Group 1 (Hypothalamic Pituitary Failure) involves disrupted communication between the hypothalamus and pituitary leading to absent GnRH release, with conditions including idiopathic hypogonadotropic hypogonadism, Kallmann Syndrome, and intracranial tumors [1]. Group 2 (Eugonadal Ovulatory Dysfunction) represents a broad spectrum where HPO compromise occurs despite normal gonadal function, encompassing PCOS, obesity, hyperprolactinemia, and primary hypothyroidism [1]. Group 3 (Primary Ovarian Insufficiency) occurs when primary dysfunction originates in the ovaries themselves due to genetic factors (Turner Syndrome), autoimmune conditions, environmental toxins, or cancer treatments [1].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for HPO Axis Investigation
| Reagent/Material | Specific Application | Research Function | Example Methodologies |
|---|---|---|---|
| GnRH Analogues | GnRH stimulation tests; pulsatility studies | Assess pituitary responsiveness; investigate pulse generator function | Diagnostic testing for hypothalamic amenorrhea |
| LH/FSH Immunoassays | Serum and urine hormone measurement | Quantify gonadotropin levels across cycle phases | LH surge detection; follicular phase FSH assessment |
| Steroid Hormone ELISA Kits | Estradiol, progesterone measurement | Monitor ovarian steroidogenesis output | Luteal phase adequacy assessment; follicular development |
| AMH Detection Kits | Ovarian reserve testing | Evaluate follicular pool and recruitment | PCOS diagnosis; fertility assessment |
| RNA In Situ Hybridization Probes | Kisspeptin and GnRH neuron studies | Investigate neuronal regulation of HPO axis | Neuroendocrine mechanism research |
| BBT Tracking Devices | Ovulation confirmation | Detect post-ovulatory temperature rise | Fertility monitoring; cycle phase verification |
| MRI Contrast Agents | Hypothalamic-pituitary imaging | Visualize structural abnormalities | Tumor identification; anatomical assessment |
Integrated Data Interpretation and Research Implications
The investigation of HPO axis phase regulation reveals complex interactions between neurological, endocrine, and metabolic systems. Research consistently demonstrates that optimal BMI maintenance (approximately 20 kg/m²) supports regular ovulatory function, while deviations in either direction disrupt cycle regularity and ovulation rates [7]. The two-cell theory of estrogen production provides a fundamental framework for understanding ovarian steroidogenesis, where theca cells (under LH stimulation) produce androgens that granulosa cells (under FSH influence) convert to estrogens through aromatase activity [5]. This cooperative process ensures appropriate estrogen levels for both negative and positive feedback effects on the central components of the HPO axis.
Emerging research has also elucidated interactions between the HPO axis and the Hypothalamic-Pituitary-Adrenal (HPA) axis, with a recent meta-analysis of 121 longitudinal studies demonstrating higher cortisol concentrations in the follicular phase compared to the luteal phase (dSMC = 0.12, p = .004) [8] [6]. This cross-system interaction may explain how psychological and physical stressors can disrupt menstrual cyclicity through HPA-mediated effects on GnRH pulsatility. Additionally, the discovery of kisspeptin signaling has advanced understanding of how metabolic and environmental inputs regulate the GnRH pulse generator, with kisspeptin neurons acting as intermediaries in transmitting sex steroid feedback to GnRH neurons [2].
For researchers investigating HPO axis function, incorporating multiple assessment methodologies strengthens experimental validity. Combining temporal hormone mapping with functional status biomarkers and structural imaging when indicated provides a comprehensive approach to characterizing HPO axis phase regulation across normal and pathological states. These integrated approaches facilitate the development of targeted interventions for ovulatory disorders and reproductive conditions affecting this essential regulatory system.
HPO Axis Regulatory Signaling and Feedback Pathways
Methodological Approaches for HPO Axis Investigation
The menstrual cycle is a quintessential physiological rhythm governed by precise fluctuations in key reproductive hormones. For researchers and drug development professionals, quantifying the production rates of estrogen and progesterone across the follicular, ovulatory, and luteal phases provides critical insights into female reproductive health and endocrine pathophysiology [9] [10]. These hormonal dynamics not only regulate ovulation and endometrial preparation but exert systemic influences on metabolism, cardiovascular function, and neural connectivity [10] [11] [12].
Advanced metabolomic studies reveal that of 397 metabolites tested, 208 show significant changes throughout the menstrual cycle, with rhythmic patterns observed in neurotransmitter precursors, glutathione metabolism, and urea cycle components [10]. This biochemical rhythmicity underscores the far-reaching impact of estrogen and progesterone fluctuations beyond reproductive tissues. Furthermore, emerging digital health technologies now enable correlation of hormonal status with real-time physiological biomarkers, offering new paradigms for monitoring endocrine function [11].
This comparison guide synthesizes current experimental data on hormonal production rates, detailing the methodologies enabling precise quantification and presenting standardized reference values for research applications. We focus specifically on the comparative dynamics of estrogen and progesterone across distinct menstrual phases, providing a foundation for diagnostic development and therapeutic innovation.
Hormonal Dynamics Across Menstrual Phases
Phase-Specific Hormonal Patterns
The menstrual cycle comprises three principal phases characterized by distinct endocrine milieus. The follicular phase begins with menstruation, marked by low estrogen and progesterone levels, followed by gradual estrogen elevation driven by developing ovarian follicles [9] [13]. The ovulatory phase features a surge in luteinizing hormone (LH) and follicle-stimulating hormone (FSH), triggering ovulation approximately 16-32 hours post-LH peak [9] [14]. The luteal phase follows ovulation, characterized by progesterone dominance from the corpus luteum, with elevated estrogen levels during most of this phase [9].
Table 1: Hormonal Concentration Ranges Across Menstrual Cycle Phases
| Hormone | Follicular Phase | Ovulatory Phase | Luteal Phase | Measurement Method |
|---|---|---|---|---|
| Estradiol | 20-400 pg/mL [13] | 150-750 pg/mL [13] | 30-450 pg/mL [13] | LC-MS, Immunoassay |
| Progesterone | <1 ng/mL | 5-20 ng/mL [13] | Serum immunoassay | |
| LH | 0.61-16.3 IU/mL (midcycle peak) [13] | Immunoassay | ||
| FSH | 5-20 mIU/mL [13] | Immunoassay |
Recent research utilizing wearable technology has quantified the physiological impact of these hormonal fluctuations. A groundbreaking study analyzing over 45,000 cycles demonstrated that resting heart rate increases by an average of 2.73 BPM from the follicular to luteal phase, while heart rate variability decreases by 4.65 ms, reflecting the measurable cardiovascular influence of hormonal changes [11].
Comprehensive Hormonal Fluctuations
The endocrine orchestration of the menstrual cycle involves complex feedback systems between the hypothalamus, pituitary, and ovaries. The hypothalamic-pituitary-ovarian axis regulates this process through both negative and positive feedback mechanisms [9] [15]. Gonadotropin-releasing hormone (GnRH) from the hypothalamus stimulates pituitary release of FSH and LH, which in turn modulate ovarian production of estrogen and progesterone [15].
Table 2: Hormonal Reference Values for Cycle Phase Classification in Research Settings
| Cycle Phase | Estradiol (pg/mL) | Progesterone (ng/mL) | LH (IU/mL) | FSH (IU/mL) |
|---|---|---|---|---|
| Early Follicular | 20-400 [13] | <1 | Low | 5-20 [13] |
| Late Follicular | Rising | <1 | Rising | Variable |
| Ovulatory | 150-750 [13] | Initial rise | 0.61-16.3 [13] | Surge |
| Luteal | 30-450 [13] | 5-20 [13] | Low | Low |
Metabolomic analyses further reveal that these hormonal shifts associate with significant systemic changes. During the luteal phase, 39 amino acids and derivatives and 18 lipid species demonstrate decreased concentrations, potentially indicating an anabolic state during the progesterone peak with recovery during menstruation and follicular phase [10]. These findings highlight the extensive metabolic impact of menstrual cycle hormonal fluctuations.
Experimental Quantification Methodologies
Analytical Techniques for Hormone Assessment
Accurate quantification of estrogen and progesterone across menstrual phases relies on sophisticated analytical platforms, each with distinct advantages and limitations. The following experimental protocols represent current best practices for hormonal assessment in research settings.
Liquid Chromatography-Mass Spectrometry (LC-MS) and Gas Chromatography-Mass Spectrometry (GC-MS)
- Application: Comprehensive metabolomic profiling of steroid hormones and their metabolites [10]
- Protocol: Plasma and urine samples are collected at specific cycle phases (menstrual, follicular, periovular, luteal, premenstrual). Samples undergo protein precipitation, liquid-liquid extraction, and derivatization before analysis. Chromatographic separation precedes mass spectrometric detection with selective ion monitoring [10]
- Sensitivity: Capable of detecting hormone concentrations in picogram per milliliter range
- Advantages: High specificity, ability to measure multiple analytes simultaneously, distinction between structurally similar hormones
Immunoassays
- Application: Clinical measurement of estradiol, progesterone, LH, and FSH [13]
- Protocol: Serum samples collected during specific cycle phases (e.g., days 2-3 for FSH/estradiol; days 19-22 for progesterone). Competitive binding assays using antibody-antigen reactions with enzymatic, chemiluminescent, or fluorescent detection [13]
- Platforms: Includes tests from Access Medical Laboratories, ZRT Laboratories, and Boston Heart Diagnostics
- Considerations: Antibody specificity challenges with structurally similar steroids; more cost-effective than MS
High-Performance Liquid Chromatography with Fluorescence Detection (HPLC-FLD)
- Application: Quantification of B vitamins and cofactors that interact with hormonal pathways [10]
- Protocol: Serum or plasma samples undergo deproteinization, followed by chromatographic separation with fluorescence detection for specific analytes like riboflavin
- Utility: Assessment of micronutrient status relevant to hormone metabolism
DUTCH Complete Testing (Dried Urine Test for Comprehensive Hormones)
- Application: Comprehensive hormone metabolite profiling [13]
- Protocol: Urine collection during luteal phase with analysis of estrogen, progesterone, androgen metabolites, cortisol patterns, and organic acids via LC-MS/MS
- Advantage: Non-invasive collection with insights into hormone metabolism pathways and clearance
Flow Cytometric Receptor Quantification
- Application: Measurement of estrogen and progesterone receptors at cellular level [16]
- Protocol: Cell lines or clinical samples stained with fluorescent-labeled monoclonal antibodies against ERα and PgR. Quantification using Molecules of Equivalent Soluble Fluorochrome (MESF) units via flow cytometry [16]
- Advantage: Not affected by endogenous steroid competition, single-cell resolution
Phase Classification in Research Protocols
Standardized phase classification is essential for reproducible hormonal research. The following criteria, adapted from large-scale metabolomic studies, enable precise phase determination [10]:
- Menstrual Phase (Days 1-5): Characterized by low estradiol and progesterone, with menstrual bleeding
- Follicular Phase (Days 1-13): Rising estradiol levels, with FSH initially elevated then decreasing as dominant follicle emerges
- Periovulatory Phase: Detected via urinary LH surge testing or serum LH elevation, occurring 16-32 hours before ovulation
- Luteal Phase (Days 15-28): Elevated progesterone with moderate estrogen levels, further subdivided into early, mid, and late luteal
- Premenstrual Phase: Declining progesterone and estrogen preceding menstruation
For increased precision, some research protocols implement the "5-phase cycle classification" incorporating serum hormones, urinary LH, and self-reported cycle timing [10]. Dense sampling protocols with collections every 1-2 days throughout the cycle (as in DUTCH Cycle Mapping) provide the highest temporal resolution for capturing hormonal dynamics [13].
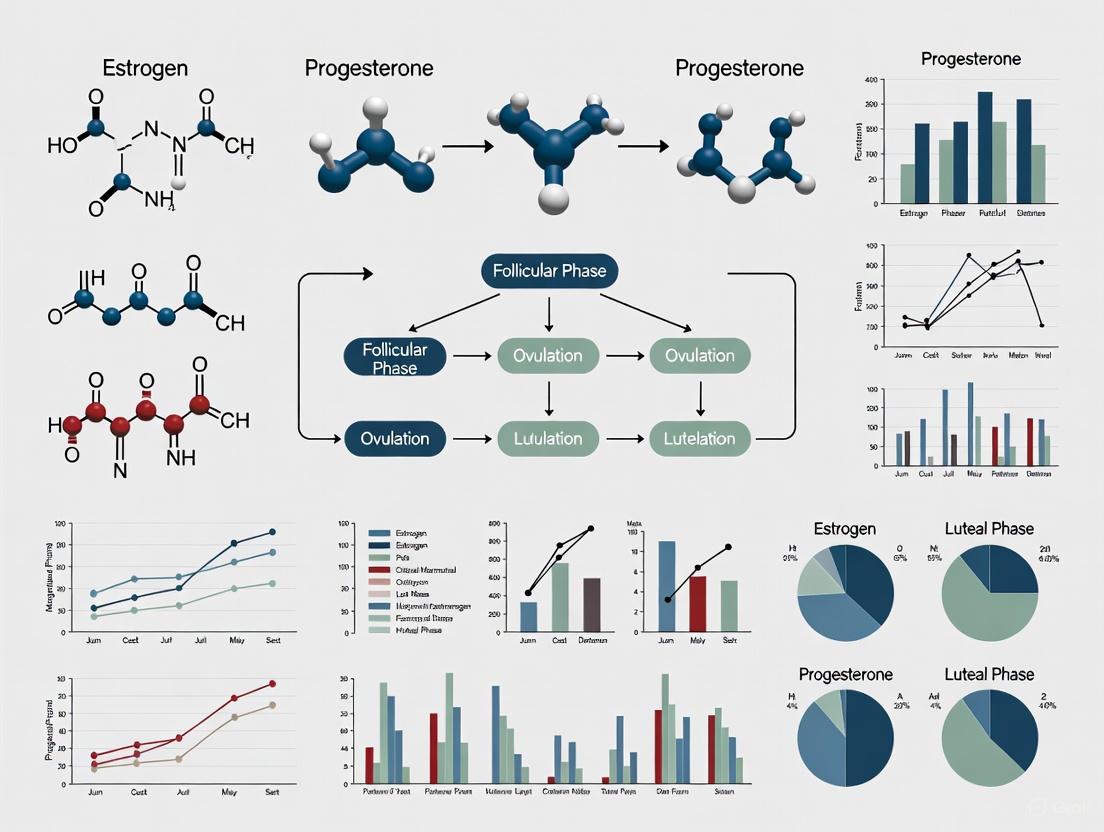
Signaling Pathways and Hormonal Regulation
The endocrine orchestration of the menstrual cycle involves complex interactions between hypothalamic, pituitary, and ovarian hormones. The following diagram illustrates the key regulatory pathways and feedback mechanisms.
This hypothalamic-pituitary-ovarian axis demonstrates the complex regulatory network governing menstrual cycle hormonal production. Note the dual positive and negative feedback mechanisms of estradiol, which transition according to concentration and duration of exposure [9] [15]. The positive feedback loop at high mid-cycle estradiol levels triggers the LH surge essential for ovulation, while progesterone maintains consistent negative feedback throughout the luteal phase [9].
Research Reagent Solutions
Table 3: Essential Research Reagents for Hormonal Quantification
| Reagent/Category | Specific Examples | Research Application | Key Characteristics |
|---|---|---|---|
| Chromatography Standards | Deuterated estradiol (estradiol-d4), Progesterone-d9 | LC-MS/MS quantification | Isotope-labeled internal standards for precise quantification |
| Immunoassay Kits | Access FSH, Estradiol, LH, Progesterone assays (Roche); ZRT Salivary Hormone Kits | Clinical hormone measurement | Antibody-based detection with enzymatic or chemiluminescent signal |
| Monoclonal Antibodies | ERα (clone ID5), PgR (clone PR-2C5) | Flow cytometric receptor quantification [16] | Specific epitope recognition, fluorescent conjugation capability |
| Sample Preparation | Solid-phase extraction cartridges (C18), Protein precipitation reagents (methanol, acetonitrile) | Sample clean-up prior to analysis | Efficient hormone extraction, matrix interference removal |
| Quality Controls | Bio-Rad Liquichek Unassayed Chemistry Controls; UTAK steroid controls | Method validation | Known concentration materials for assay precision and accuracy |
| Cell Culture Models | MCF-7 breast cancer cells, T47D cells | Receptor binding studies [16] | Endogenous hormone receptor expression, responsive to hormonal manipulation |
| Calibration Materials | MESF (Molecules of Equivalent Soluble Fluorochrome) beads [16] | Flow cytometry standardization | Quantitative fluorescence reference for cellular receptor count |
Comparative Data Synthesis
The quantitative profiles of estrogen and progesterone across menstrual phases demonstrate predictable yet variable patterns essential for understanding female endocrine physiology. Estradiol shows the greatest dynamic range, increasing approximately 20-fold from early follicular to ovulatory phases, while progesterone exhibits the most dramatic phase-dependent shift, rising from negligible follicular levels to dominant luteal concentrations [9] [13].
These hormonal fluctuations correlate with measurable physiological changes beyond the reproductive system. Recent research utilizing wearable technology has established that cardiovascular metrics follow consistent patterns throughout the menstrual cycle, with resting heart rate lowest during menstruation and peaking in the luteal phase, while heart rate variability shows the opposite pattern [11]. The magnitude of these cardiovascular changes, quantified as "Cardiovascular Amplitude," may provide a novel digital biomarker for hormonal status and cycle regularity [11].
Metabolomic studies further reveal that the luteal phase is associated with decreased levels of 39 amino acids and derivatives and 18 lipid species, potentially indicating an anabolic state during the progesterone peak [10]. This systematic metabolic rhythmicity underscores the far-reaching impact of menstrual cycle hormones and offers potential diagnostic applications for hormone-related disorders.
For researchers investigating hormonal contraceptives, comparative studies reveal that combined oral contraceptives (OCs) create a hypogonadal state characterized by suppressed endogenous hormone production, with synthetic hormones potentially mimicking hyperprogestogenic brain states despite overall endocrine suppression [12]. This paradoxical effect highlights the complexity of endocrine disruption and replacement strategies.
Standardized hormonal quantification across menstrual phases provides essential reference data for developing targeted interventions for ovulatory disorders, luteal phase defects, and hormone-sensitive conditions. The experimental methodologies detailed herein enable precise characterization of these endocrine patterns for both research and clinical applications.
Menstrual cycle variability is a critical factor in women's health, influencing everything from fertility to metabolic health. While total cycle length is the most commonly tracked metric, a growing body of evidence demonstrates that this variability stems predominantly from differences in the follicular phase duration. This phase, encompassing the time from menstruation onset to ovulation, exhibits substantially greater fluctuation than the subsequent luteal phase. Understanding this dynamic is essential for researchers studying reproductive endocrinology, drug development professionals designing hormone-based therapies, and clinicians interpreting cycle data in both research and clinical settings. This analysis examines the quantitative evidence supporting follicular phase variability and the experimental methodologies enabling these insights, providing a foundation for comparative studies of hormone trends across different menstrual cycle patterns.
Quantitative Evidence of Phase Variability
Multiple large-scale studies provide compelling quantitative evidence that follicular phase length is the principal contributor to menstrual cycle variability, while the luteal phase remains relatively stable.
Table 1: Comparative Phase Length Variability Across Key Studies
| Study & Population | Cycle Length (Days) | Follicular Phase Length (Days) | Luteal Phase Length (Days) | Key Findings on Variability |
|---|---|---|---|---|
| Bull et al. (2019) [17]: 124,648 women, 612,613 cycles | 29.3 (mean) | 16.9 (95% CI: 10-30) | 12.4 (95% CI: 7-17) | Follicular phase contributed most to cycle length variation; luteal phase more stable |
| Fehring et al. (2006) [18]: 141 women, 1,060 cycles | 28.9 (SD = 3.4) | Not specified | Not specified | 42.5% of women showed intracycle variability >7 days; follicular phase contributed most to this variability |
| Prior et al. (2024) [19]: 53 women, 676 ovulatory cycles | Variance: 10.3 days | Variance: 11.2 days | Variance: 4.3 days | Within-woman follicular phase variances significantly greater than luteal phase variances (P < 0.001) |
The data consistently demonstrate that the standard deviation and variance of follicular phase length substantially exceed those of the luteal phase across diverse populations. The luteal phase typically maintains a more consistent duration of approximately 12-14 days in normally ovulatory cycles, while follicular phase length can vary considerably between women and even within the same woman across consecutive cycles [20] [17].
Experimental Protocols for Phase Determination
Research characterizing menstrual cycle variability relies on precise methodologies for determining ovulation, which demarcates the follicular and luteal phases. The following experimental approaches represent gold standards in the field.
Hormonal Assay Protocol (North Carolina Early Pregnancy Study)
The North Carolina Early Pregnancy Study employed rigorous hormonal monitoring to precisely identify ovulation timing [21]:
- Daily Urine Collection: Participants collected first-morning urine specimens throughout their menstrual cycles, providing a consistent biological matrix for hormone measurement.
- Hormone Metabolite Analysis: Specimens were assayed for estrone-3-glucuronide (E1-3G), a metabolite of estrogen, and pregnanediol-3-glucuronide (Pd-3G), a metabolite of progesterone, using immunoassay techniques.
- Ovulation Estimation: The day of ovulation was estimated using a validated algorithm based on the ratio of Pd-3G to E1-3G, which identifies the initial rise in progesterone metabolites following ovulation.
- Cycle Phase Calculation: Follicular phase length was calculated as the number of days from the first day of menses up to (but not including) the estimated day of ovulation.
This protocol allowed researchers to precisely quantify follicular phase length and examine factors influencing its variability, including marijuana use, oral contraceptive history, and reproductive history [21].
Basal Body Temperature (BBT) Methodology
The prospective 1-year study by Prior et al. utilized basal body temperature tracking to determine ovulatory timing [19]:
- Daily Temperature Measurement: Participants recorded first morning oral temperature immediately upon waking, before any physical activity.
- Quantitative BBT Analysis (QBT): Researchers applied a validated least-squares quantitative basal temperature algorithm to identify the biphasic pattern characteristic of ovulation.
- Phase Determination: The day of ovulation was identified as the day before the sustained BBT rise, with follicular phase length calculated from menses onset to this point.
- Quality Control: Cycles with temperature data for fewer than 50% of days were excluded from analysis to ensure reliability.
This methodology enabled the collection of extensive longitudinal data (694 cycles) with confirmation of ovulation, providing robust evidence of greater within-woman variability in follicular versus luteal phase length [19].
Integrated Hormonal and Metabolic Profiling
Advanced metabolic studies combine hormonal phase determination with comprehensive biochemical profiling [22]:
- Multi-Phase Classification: Serum hormones (estradiol, progesterone, FSH, LH), urinary luteinizing hormone tests, and self-reported menstrual timing were integrated to establish a 5-phase cycle classification system.
- High-Throughput Metabolomics: Plasma and urine samples were analyzed using LC-MS and GC-MS platforms to quantify 397 metabolites and micronutrients across cycle phases.
- Statistical Analysis: Phase-to-phase comparisons were conducted with false discovery rate (FDR) correction to identify rhythmic metabolites, with 71 reaching FDR <0.20 threshold.
This approach revealed significant metabolic rhythmicity throughout the menstrual cycle, with 39 amino acids and derivatives and 18 lipid species decreasing during the luteal phase, providing biochemical correlates to phase-specific physiological states [22].
Endocrine Regulation of Follicular Phase Variability
The greater variability observed in the follicular phase stems from the complex endocrine regulation governing follicular development and ovulation. The hypothalamic-pituitary-ovarian (HPO) axis coordinates this process through precisely timed hormonal interactions.
Figure 1: Hormonal Regulation of the Follicular Phase. The hypothalamic-pituitary-ovarian axis coordinates follicular development through pulsatile GnRH secretion, FSH stimulation, and estradiol-mediated positive feedback that triggers the LH surge and ovulation.
The follicular phase begins with the removal of negative feedback inhibition following the decline of progesterone, estrogen, and inhibin A from the previous cycle's corpus luteum [23]. This allows FSH levels to rise during the late luteal phase, recruiting a cohort of ovarian follicles. Typically, 11-20 eggs begin developing, but only one reaches full maturity as the dominant follicle [24]. The extended duration and complexity of this selection process, influenced by numerous factors, accounts for the greater variability observed in follicular versus luteal phase length.
Table 2: Factors Associated with Follicular Phase Length Variability
| Factor | Association with Follicular Phase Length | Supporting Evidence |
|---|---|---|
| Age | Decreases by 0.19 days per year from age 25-45 [17] | Analysis of 612,613 cycles showing progressive shortening |
| Oral Contraceptive Use | Recent use (within 90 days) associated with 2.3-day lengthening [21] | Prospective cohort study with hormonal confirmation |
| Marijuana Use | Occasional use associated with 3.5-day lengthening [21] | Dose-response relationship observed |
| Body Mass Index (BMI) | Higher BMI (>35) associated with 0.4-day greater cycle variation [17] | Analysis of 124,648 app users |
| Miscarriage History | Associated with 2.2-day shortening [21] | Adjusted for age and OC use |
The transition from negative to positive feedback of estradiol at the anterior pituitary represents a critical threshold in follicular phase completion. This shift, which requires estradiol levels >200 pg/mL for approximately 50 hours, triggers the LH surge that initiates ovulation [20]. The time required to reach this threshold varies between cycles and individuals, contributing significantly to follicular phase variability.
Essential Research Reagent Solutions
The following research tools and reagents are essential for conducting rigorous menstrual cycle phase analysis and hormone trend comparison studies.
Table 3: Essential Research Reagents for Menstrual Cycle Studies
| Research Solution | Application | Function in Experimental Protocols |
|---|---|---|
| Urinary Estrone-3-Glucuronide (E1-3G) & Pregnanediol-3-Glucuronide (Pd-3G) Assays | Ovulation timing | Biomarkers for estimating day of ovulation via metabolite ratios [21] |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits for FSH, LH, Estradiol, Progesterone | Hormonal phase classification | Quantify serum hormone levels for precise cycle phase determination [22] |
| Liquid Chromatography-Mass Spectrometry (LC-MS) Platforms | Metabolic profiling | Identify and quantify rhythmic metabolites across menstrual phases [22] |
| Basal Body Temperature (BBT) Tracking Devices | Ovulation detection | Detect post-ovulatory temperature rise for phase length calculation [19] |
| Urinary Luteinizing Hormone (LH) Test Strips | Ovulation prediction | Identify LH surge preceding ovulation for fertile window identification [17] |
These research tools enable the precise hormone measurements and physiological monitoring necessary for comparing hormone trends across different menstrual cycle patterns. The combination of hormonal assays with metabolic profiling platforms represents particularly powerful methodology for comprehensive cycle phase analysis.
The collective evidence from large-scale observational studies, detailed hormonal monitoring, and metabolic profiling consistently identifies the follicular phase as the primary source of menstrual cycle variability. This understanding has profound implications for research design in women's health, drug development, and clinical practice. Studies investigating cycle-related phenomena must account for this inherent variability rather than assuming standardized phase lengths across populations. Future research should continue to elucidate the complex factors influencing follicular phase duration, including genetic predispositions, environmental influences, and physiological states. Such investigations will further refine our understanding of menstrual cycle dynamics and enhance our ability to interpret hormone trends across diverse cycle patterns.
Menstrual cycle characteristics are increasingly recognized as critical vital signs for overall health, with growing evidence linking long or irregular cycles to conditions such as infertility, cardiometabolic disease, and premature mortality [25] [26] [27]. For researchers and drug development professionals, understanding the baseline variations in cycle patterns across different demographic groups is essential for designing clinical trials, interpreting real-world evidence, and developing targeted therapies. Historically, clinical guidelines for menstrual cycle parameters have been primarily based on studies of White populations, leaving significant gaps in our understanding of how these patterns manifest across diverse racial and ethnic groups [25] [26]. This guide synthesizes recent large-scale research to objectively compare how age, body mass index (BMI), race, and ethnicity influence menstrual cycle length and variability, providing a foundational reference for scientific and clinical applications.
Key Findings at a Glance
The following tables summarize the core quantitative relationships between demographic factors and menstrual cycle characteristics, based on aggregated data from large cohort studies including the Apple Women's Health Study (AWHS) which analyzed 165,668 cycles from 12,608 participants [25] [26] [27].
Table 1: Mean Cycle Length Differences by Demographic Factors (Reference: White, Age 35-39, Healthy BMI)
| Demographic Factor | Category | Mean Difference in Cycle Length (Days) | 95% Confidence Interval |
|---|---|---|---|
| Age Group | <20 | +1.6 | +1.3 to +1.9 |
| 20-24 | +1.4 | +1.2 to +1.7 | |
| 25-29 | +1.1 | +0.9 to +1.3 | |
| 30-34 | +0.6 | +0.4 to +0.7 | |
| 40-44 | -0.5 | -0.3 to -0.7 | |
| 45-49 | -0.3 | -0.1 to -0.6 | |
| ≥50 | +2.0 | +1.6 to +2.4 | |
| Race/Ethnicity | Asian | +1.6 | +1.2 to +2.0 |
| Hispanic | +0.7 | +0.4 to +1.0 | |
| Black | -0.2 | -0.1 to +0.6 | |
| BMI Category | Overweight | +0.3 | +0.1 to +0.5 |
| Class 1 Obese | +0.5 | +0.3 to +0.8 | |
| Class 2 Obese | +0.8 | +0.5 to +1.0 | |
| Class 3 Obese | +1.5 | +1.2 to +1.8 |
Table 2: Cycle Variability and Irregularity Patterns by Demographic Factors
| Demographic Factor | Category | Cycle Variability Change vs. Reference | Odds Ratio for Long Cycles | Odds Ratio for Short Cycles |
|---|---|---|---|---|
| Age Group (Ref: 35-39) | <20 | +46% | 1.85 | 0.90 |
| 45-49 | +45% | 1.72 | 2.44 | |
| ≥50 | +200% | 6.47 | 3.25 | |
| Race/Ethnicity (Ref: White) | Asian | Increased | 1.43 | - |
| Hispanic | Increased | 1.26 | - | |
| BMI Category (Ref: Healthy) | Class 3 Obese | Increased | ~1.30* | - |
Note: Specific odds ratio estimates for BMI and short cycles were not fully reported in the available sources, though the association with long cycles is well-established [27].
Detailed Experimental Protocols and Methodologies
The Apple Women's Health Study (AWHS) Protocol
The Apple Women's Health Study represents one of the most comprehensive large-scale digital cohorts for menstrual health research, with methodology designed for robust epidemiological analysis [25] [26] [27].
- Study Population and Eligibility: The analysis included 12,608 participants contributing 165,668 menstrual cycles. Participants were excluded if they reported a history of polycystic ovary syndrome, uterine fibroids, hysterectomy, or current hormone use to isolate natural menstrual patterns [25].
- Data Collection: Menstrual cycle data was collected through mobile tracking applications, with cycle length defined as the number of days from the first day of menstrual flow to the day before the next period begins. Survey data on demographic characteristics, including self-reported race, ethnicity, and BMI, were collected through the Common Demographics survey in the Apple Research App [25] [27].
- Statistical Analysis: Researchers employed linear mixed effects models to estimate differences in cycle length associated with age, race/ethnicity, and BMI, adjusted for potential confounders. Cycle variability was quantified using within-individual standard deviations of cycle length. The analysis specifically used the 35-39 age group as the reference for age-related comparisons because this group demonstrated the lowest cycle variability [26] [27].
Hormone Monitoring Protocol for Cycle Phase Characterization
A separate study utilizing at-home hormone monitoring technology provides insights into the endocrine mechanisms underlying demographic variations in cycle characteristics [28] [29].
- Hormone Tracking System: The study employed the Oova platform, a remote fertility testing system that quantitatively tracks luteinizing hormone (LH) and pregnanediol-3-glucuronide (PdG) through urine test cartridges. The system uses advanced nanotechnology that adjusts for pH, normalizes hydration levels, and filters out non-specific binding [28].
- Data Acquisition and Analysis: Participants collected daily urine samples either through midstream or dip format. Test results were captured and interpreted by an AI-powered smartphone app that utilizes computer vision algorithms to adjust for lighting, shadows, and movement. The platform establishes each user's unique hormone baseline levels, with daily fluctuations compared to this personalized baseline rather than population averages [28].
- Cycle Phase Definitions: The follicular phase was defined as the period from the first day after bleeding cessation to the date of the peak LH level. The luteal phase was defined as the days from the first day after ovulation to the day before the next menstrual cycle. Ovulation was confirmed by detecting a rise in progesterone within 72 hours after the highest LH levels were detected [28].
Research Methodology for Demographic Menstrual Cycle Studies
Essential Research Reagent Solutions
Table 3: Key Research Materials and Technologies for Menstrual Cycle Studies
| Research Tool | Primary Function | Key Features | Representative Use in Cited Studies |
|---|---|---|---|
| Digital Menstrual Tracking Platforms | Large-scale cycle data collection | Mobile app interface, longitudinal design, real-time data capture | Apple Women's Health Study (165,668 cycles) [25] [27] |
| At-home Hormone Monitoring Systems | Quantitative LH and PdG tracking | Urine test cartridges, AI-powered analysis, personalized baselines | Oova platform for cycle phase characterization [28] |
| Demographic Survey Instruments | Collection of participant characteristics | Standardized questionnaires, self-reported race/ethnicity and BMI | Common Demographics survey in AWHS [25] |
| Statistical Modeling Approaches | Analysis of cycle variability | Linear mixed effects models, quantile regression | Analysis of age, BMI, and ethnic variations [26] [27] |
Biological Mechanisms and Pathways
The observed demographic variations in menstrual cycle characteristics are mediated through multiple endocrine pathways that respond to factors such as age, metabolic status, and potentially genetic or environmental influences associated with racial and ethnic backgrounds.
- Age-Related Hormonal Changes: With advancing age, particularly after 35-39 years, follicular phase length declines while luteal phase length may increase slightly, reflecting diminishing ovarian reserve and alterations in hypothalamic-pituitary-ovarian axis function [28] [30]. The significant increase in cycle variability after age 45 (200% higher in those over 50 compared to ages 35-39) corresponds to the peri-menopausal transition characterized by erratic hormonal fluctuations and anovulatory cycles [25] [30].
- BMI and Hormonal Disruption: Obesity influences menstrual cycles through multiple mechanisms. Adipose tissue produces additional estrogen through aromatization of androgens, potentially disrupting the normal feedback mechanisms of the hypothalamic-pituitary-ovarian axis. This estrogen excess can suppress follicular development and ovulation, leading to longer and more variable cycles [25]. The dose-response relationship between BMI category and cycle length (from +0.3 days for overweight to +1.5 days for Class 3 obesity) supports this mechanistic pathway [26] [27].
- Racial and Ethnic Variations: The longer cycles observed in Asian and Hispanic participants compared to White women may reflect differences in hormonal levels or ovarian reserve across ethnic groups. Some studies have reported higher anti-Mullerian hormone levels among Hispanic and Asian women compared to White women of the same age, suggesting potential differences in follicular dynamics [31] [27]. Additionally, variations in exposure to social, cultural, and environmental stressors across different ethnic groups may contribute to these differences through effects on neuroendocrine function [25].
Biological Pathways Linking Demographics to Cycle Changes
Implications for Research and Drug Development
For researchers and pharmaceutical professionals, these findings have significant implications for clinical trial design and therapeutic development.
- Clinical Trial Design: Demographic stratification in trials evaluating reproductive therapies should account for the natural variations in cycle patterns across age, BMI, and ethnic groups. The established baselines enable more accurate participant selection and endpoint assessment [26] [27].
- Personalized Medicine Approaches: The documented differences in cycle characteristics support the development of demographic-specific parameters for evaluating menstrual health, moving beyond the historical one-size-fits-all approach based primarily on White populations [25] [32].
- Drug Efficacy Assessment: Understanding natural cycle variations enhances the ability to distinguish true treatment effects from demographic-driven baseline differences in studies of fertility treatments, hormonal therapies, and interventions for menstrual disorders [28] [27].
The comprehensive analysis of demographic influences on menstrual cycle parameters reveals complex interactions between age, BMI, race, and ethnicity that must be considered in both research and clinical contexts. The patterns established through large-scale digital cohort studies provide an evidence base for refining clinical guidelines and developing more personalized approaches to menstrual health. For the research and drug development community, these findings underscore the importance of demographic considerations in trial design, endpoint selection, and interpretation of results when evaluating therapies targeting reproductive health and endocrine function. Future research should focus on elucidating the specific genetic, environmental, and socioeconomic factors that drive the observed racial and ethnic differences in menstrual cycle characteristics.
Innovative Methodologies for Tracking Hormonal Shifts and Cycle Phases
The study of women's health, particularly hormonal and menstrual physiology, has been historically constrained by reliance on infrequent clinical visits and subjective self-reporting. Digital biomarkers – defined as physiological, behavioral, and environmental data collected via digital devices like smartphones and wearables – are revolutionizing this field by enabling continuous, objective, and real-world data collection [33] [34]. These biomarkers provide unprecedented insights into the dynamic patterns of menstrual cycles, moving beyond the oversimplified "textbook" 28-day model. The global market for digital biomarkers is expanding rapidly, projected to grow from $5 billion in 2025 to $18.8 billion by 2030, reflecting their increasing adoption in medical research and clinical practice [34]. This guide provides a comparative analysis of the digital biomarkers and methodologies currently transforming research on hormone trends and menstrual cycle patterns.
Comparative Analysis of Digital Biomarkers for Cycle Tracking
Different digital biomarkers offer distinct advantages and limitations for capturing the physiological changes associated with menstrual cycle phases. The table below compares the primary biomarkers used in large-scale app-based studies.
Table 1: Comparison of Digital Biomarkers for Menstrual Cycle Research
| Digital Biomarker | Physiological Correlation | Data Collection Method | Key Research Findings | Considerations for Researchers |
|---|---|---|---|---|
| Basal Body Temperature (BBT) | Rise in progesterone post-ovulation increases resting body temperature [35]. | Ear thermometers, intravaginal sensors, or wearable patches [36]. | Detects biphasic pattern confirming ovulation; mean luteal phase length is 12.4 days [37]. | Requires measurement at rest upon waking; cycle phase is determined retrospectively [35]. |
| Resting Heart Rate (RHR) | Influenced by estrogen and progesterone; tends to be lowest during menstruation and peaks in the luteal phase [38]. | Consumer wearables (e.g., WHOOP, Fitbit, Huawei Band) during sleep or rest. | Average increase of 2.73 BPM from follicular to luteal phase [38]. | Provides real-time, forward-looking insights; sensitive to confounders like illness, stress, and alcohol. |
| Heart Rate Variability (HRV) | Reflects autonomic nervous system balance, modulated by hormonal shifts [38]. | Consumer wearables (e.g., WHOOP, Fitbit, Huawei Band) during sleep or rest. | Average decrease of 4.65 ms from follicular to luteal phase [38]. | A higher value indicates better recovery; sensitive to the same confounders as RHR. |
| Physical Activity & Sleep | Hormonal changes can influence energy levels, sleep quality, and activity patterns. | Wearable accelerometers and gyroscopes. | Used in models for postpartum depression recognition; associated with stress and lifestyle factors [39] [37]. | Provides behavioral context; best used in combination with physiological biomarkers. |
Experimental Protocols for Validating Digital Biomarkers
To ensure the validity and reliability of digital biomarker data, researchers employ rigorous experimental protocols. The following section details key methodologies from recent landmark studies.
Protocol for Fertile Window and Menses Prediction
A prospective observational cohort study conducted in Shanghai aimed to develop machine-learning algorithms for predicting the fertile window and menstruation using BBT and heart rate.
- Study Population and Design: The study recruited 89 regular menstruators and 25 irregular menstruators, following them for at least four menstrual cycles. Participants were healthy women aged 18-45, excluded if they had major diseases, were breastfeeding, or were taking hormone-interfering medications [35].
- Data Collection:
- Basal Body Temperature (BBT): Measured daily upon waking using an ear thermometer (Braun IRT6520) after lying horizontally for 5 minutes [35].
- Heart Rate (HR): Recorded continuously during sleep using the Huawei Band 5, worn every night. Data was synced with a smartphone each morning [35].
- Ovulation Confirmation (Gold Standard): Determined via transvaginal/abdominal ultrasound and serum hormone level measurements (LH, E2, FSH, progesterone). Monitoring began between cycle days 8-12 and continued until follicle rupture was confirmed [35].
- Data Analysis: The cycles were divided into menstrual, follicular, fertile (5 days before to day of ovulation), and luteal phases. Linear mixed models assessed parameter changes, and probability function estimation models with machine learning were developed for prediction [35].
- Key Outcome: The algorithm combining BBT and HR predicted the fertile window in regular menstruators with an accuracy of 87.46% (AUC=0.8993) and menses with 89.60% accuracy [35].
Protocol for Large-Scale Menstrual Cycle Characterization
A study published in npj Digital Medicine analyzed over 600,000 cycles from the Natural Cycles app to establish real-world cycle characteristics and their associations with age and BMI.
- Data Source: Anonymized data from 124,648 users, including 17.4 million BBT measurements and user-inputted information on menstruation, age, and BMI [37].
- Cycle Selection: From 1.4 million recorded cycles, 612,613 ovulatory cycles with valid temperature data entered on at least 50% of days were included. Ovulation was estimated by the app's algorithm based on the BBT rise [37].
- Validation: The algorithm's Estimated Day of Ovulation (EDO) was validated by comparing the distributions of follicular and luteal phase lengths to established clinical data sets from Baird et al. and Lenton et al. [37].
- Key Findings:
- The mean cycle length was 29.3 days, with a mean follicular phase of 16.9 days and a mean luteal phase of 12.4 days.
- Only 16% of women exhibited the classic 28-day cycle, and only 12% had a consistent 28-day cycle with ovulation on day 14 [40] [37].
- Cycle and follicular phase length decreased with age (~0.18 and ~0.19 days per year from age 25-45), while luteal phase length remained stable [37].
Protocol for Postpartum Depression (PPD) Recognition
A cross-sectional study using the All of Us Research Program data set explored the use of consumer wearables for recognizing postpartum depression.
- Data Source and Cohort: Analysis utilized the Registered Tier v6 data set. The cohort included women with valid Fitbit data who gave birth, comprising fewer than 20 with PPD and 39 without PPD [39].
- Digital Biomarkers: Features extracted from Fitbit data included:
- Heart Rate Metrics: Daily average, SD, minimum, maximum, and quartile values.
- Physical Activity: Total daily steps.
- Energy Expenditure: Calories burned, including basal metabolic rate (BMR) [39].
- Machine Learning Modeling: Intraindividual models were built using algorithms like Random Forest, Generalized Linear Models, SVM, and k-NN to classify four periods: prepregnancy, pregnancy, postpartum without depression, and postpartum with depression (PPD) [39].
- Key Findings:
- Random Forest models performed best (mAUC=0.85; κ=0.80) at discerning the PPD period.
- The most predictive biomarker for PPD was calories burned during the basal metabolic rate.
- Individualized models surpassed the performance of traditional cohort-based models [39].
Visualization of Research Workflows
The following diagram illustrates the generalized workflow for employing digital biomarkers in menstrual cycle and women's health research, as demonstrated by the cited protocols.
Figure 1: A generalized workflow for digital biomarker research in women's health, illustrating the sequence from participant recruitment to data-driven insights.
The Scientist's Toolkit: Essential Research Reagent Solutions
For researchers designing studies in this domain, the following table details key digital and analytical "reagents" and their functions.
Table 2: Essential Reagent Solutions for Digital Biomarker Research
| Tool Category | Specific Examples | Research Function | Key Characteristics |
|---|---|---|---|
| Consumer Wearables | Huawei Band 5, Fitbit devices, WHOOP | Continuous, passive collection of physiological data (HR, HRV, activity, sleep) in real-world settings. | Facilitates large-scale, longitudinal data acquisition; consumer-grade acceptability [35] [39] [38]. |
| Specialized Sensors | Braun IRT6520 ear thermometer, OvuSense intravaginal logger | High-fidelity measurement of specific biomarkers like BBT for precise ovulation detection. | Provides clinical-grade accuracy for validating consumer device data or for primary endpoint measurement [36] [35]. |
| Data Integration & Analytics Platforms | Natural Cycles app algorithm, custom ML pipelines (R, Python) | Processes raw sensor data, integrates multi-modal inputs, and applies statistical and ML models for analysis and prediction. | Enables handling of large, complex datasets; crucial for feature engineering and model development [35] [37]. |
| Validation Tools (Gold Standards) | Transvaginal ultrasound, serum hormone assays (LH, E2, FSH, progesterone) | Provides ground-truth data for confirming ovulation and menstrual cycle phases to validate digital biomarker algorithms. | Essential for establishing the clinical validity and regulatory credibility of digital biomarker endpoints [35]. |
Discussion and Research Implications
The integration of digital biomarkers from app-based studies is providing a more nuanced and accurate picture of menstrual cycle patterns and their relationship to women's health. Key insights confirm significant individual variability, debunking uniform models like the 28-day cycle [40] [37]. The emergence of novel metrics, such as Cardiovascular Amplitude from WHOOP, which quantifies RHR and HRV fluctuations across the cycle, offers new avenues for assessing cycle regularity and hormonal health beyond mere length tracking [38].
These methodologies also hold profound implications for drug development and clinical trials. Digital biomarkers can streamline data collection, providing continuous, objective endpoints that are more sensitive than episodic clinic visits [33] [34]. This is particularly relevant for conditions like postpartum depression, where individualized models using wearable data show promise for early recognition, potentially enabling timely intervention [39].
However, challenges remain, including data standardization, device validation, and navigating regulatory landscapes for these novel endpoints [33] [34]. Furthermore, researchers must account for confounding factors such as age, baseline fitness, and hormonal contraceptive use, which can modulate digital biomarker signals [38]. Despite these hurdles, the objective, high-resolution data afforded by digital biomarkers is undeniably advancing women's health research from a paradigm of averages to one of personalized, dynamic understanding.
For decades, the clinical and research communities have relied on a limited toolkit for menstrual cycle and ovulation tracking, with Basal Body Temperature (BBT) charting being one of the most common methods. Despite its widespread use, BBT is characterized by significant limitations, including low sensitivity (approximately 22%) in detecting ovulation and a high susceptibility to disruption by environmental factors, sleep irregularities, and measurement inconsistencies [41]. The imperative for more reliable and sophisticated methodologies has catalyzed the exploration of novel, non-invasive technologies. This guide objectively compares the performance of emerging methods—vocal acoustic analysis, continuous wrist temperature sensing, wearable cardiovascular monitoring, and integrated wearable biosensors—against traditional BBT and each other. It is framed within broader research on comparing hormone trends across different menstrual cycle patterns, providing researchers and drug development professionals with a data-driven overview of the next generation of cycle tracking technologies.
Performance Comparison of Emerging Tracking Methods
The table below summarizes the key performance metrics and characteristics of emerging non-invasive tracking methods compared to the traditional BBT approach.
Table 1: Performance Comparison of Non-Invasive Menstrual Cycle and Ovulation Tracking Methods
| Tracking Method | Reported Ovulation Detection Accuracy/Performance | Key Measured Parameters | Data Collection Protocol | Advantages for Hormone Trend Research |
|---|---|---|---|---|
| Vocal Acoustic Analysis | • 81% of participants showed vocal shift within fertile window (Fundamental Frequency SD & 5th percentile) [42] | • Fundamental frequency (mean, SD, 5th/95th percentile) [42] | • Daily voice recordings of fixed phrase upon waking [42] | • Captures subtle, hormone-driven tissue hydration changes [42] • Highly scalable via smartphones [42] |
| Continuous Wrist Skin Temperature | • Sensitivity: 0.62 (vs. 0.23 for BBT) [43] • True-positive rate: 54.9% (vs. 20.2% for BBT) [43] | • Wrist skin temperature (99th percentile during sleep) [43] | • Worn during sleep, requires ≥4 hours of uninterrupted data [43] | • Captures circadian rhythm temperature variations missed by point measurements [43] • Higher sensitivity for detecting ovulatory shifts [43] |
| Wearable Cardiovascular Monitoring | • RHR peaks at cycle day 26, RMSSD nadir at day 27 (population-level, n=11,590) [44] • Fluctuation pattern is attenuated with hormonal birth control [44] | • Resting Heart Rate (RHR) • Heart Rate Variability (RMSSD) [44] | • Continuous wrist-worn PPG sensor [44] • Longitudinal tracking across cycles [44] | • Provides large-scale, objective physiological data on cycle variability [44] • Links cardiovascular dynamics to hormonal fluctuations [44] |
| Smart Menstrual Health Patch | • 92.3% accuracy in ovulation prediction vs. LH tests [45] | • Basal Body Temperature • Hormone fluctuations (estrogen, progesterone via interstitial fluid) [45] | • Continuous wear across multiple cycles [45] | • Multi-parameter data fusion (temperature + direct hormone markers) [45] • Potential for identifying cycle disorders (PCOS, endometriosis) [45] |
| Traditional BBT (Oral) | • Sensitivity: ~0.23 [43] • Approx. 22% accuracy in detecting ovulation [41] | • Single-point oral temperature upon waking [41] | • Measured immediately upon waking, before any activity [41] | • Established, low-cost method [41] • Clear biphasic pattern in ovulatory cycles [41] |
Detailed Experimental Protocols and Methodologies
Vocal Acoustic Analysis for Fertility Tracking
A 2025 JMIR Formative Research study provides a robust protocol for longitudinal vocal analysis [42].
Objective: To explore how fundamental frequency (F0) features vary between menstrual phases using daily voice recordings and to apply changepoint detection to pinpoint the day of vocal shifts [42].
Participant Cohort:
- 16 naturally cycling, English-speaking, cis-gender female participants.
- All reported consistent menstrual cycles (1-4 days variation) and were not using hormonal birth control [42].
Data Collection Workflow:
- Daily Protocol: Upon waking each morning, participants performed three tasks:
- Voice Recording: Recorded themselves saying "Hello, how are you?" in a quiet environment using a custom mobile app.
- Hormone Test: Self-administered a consumer-grade luteinizing hormone (LH) urine test (Easy@Home Ovulation Tests) and took a picture of the result.
- BBT Measurement: Measured and recorded their basal body temperature.
- Timing: Data collection began the day after menstruation ended and continued for one full menstrual cycle.
- Data Management: All data was submitted via the mobile app to a secure cloud database [42].
Analytical Workflow:
- Feature Extraction: Fundamental frequency features (mean, standard deviation, 5th percentile, and 95th percentile) were extracted from each voice recording.
- Phase Comparison: F0 features were compared between the follicular and luteal phases, identified via the LH surge.
- Changepoint Detection: Applied to each feature's longitudinal data to identify the specific day when vocal behavior statistically shifted [42].
Key Quantitative Findings:
- Fundamental Frequency SD: 9.0% lower in the luteal phase compared to the follicular phase.
- 5th Percentile of F0: 8.8% higher in the luteal phase.
- For the significant features (F0 SD and 5th percentile), 81% of participants exhibited changepoints within their fertile window [42].
Figure 1: Vocal Acoustic Analysis Experimental Workflow
Continuous Wrist Temperature Sensing
A 2021 prospective comparative study established a protocol for comparing wrist skin temperature to BBT [43].
Objective: To determine the diagnostic accuracy of continuously measured wrist skin temperature during sleep versus oral BBT for detecting ovulation, using LH tests as a reference standard [43].
Participant Cohort:
- 57 healthy women contributing 193 cycles (170 ovulatory, 23 anovulatory).
- Aged 18-45, not on hormonal therapy, and without conditions affecting menstrual cycles [43].
Data Collection Workflow:
- Wrist Temperature: Participants wore an Ava Fertility Tracker bracelet (v2.0) on the dorsal side of the wrist during sleep each night. The first 90 and last 30 minutes of data were excluded, and the 99th percentile of the remaining data was used as the daily temperature value [43].
- BBT: Measured orally each morning immediately upon waking using a Lady-Comp digital thermometer [43].
- LH Test: ClearBlue Digital Ovulation Tests were performed daily starting from a cycle day calculated based on the participant's average cycle length until a surge was detected or menstruation began [43].
Analytical Workflow:
- Ovulation was defined as the day following the LH surge.
- Diagnostic accuracy (sensitivity, specificity) of temperature shifts detected by each method was calculated against the LH reference.
- Correlation and agreement between the two temperature curves were analyzed across menstrual phases [43].
Large-Scale Cardiovascular Fluctuation Analysis
A 2024 npj Digital Medicine study introduced a novel metric for quantifying menstrual cycle-related cardiovascular changes [44].
Objective: To derive a "cardiovascular amplitude" metric quantifying fluctuations in resting heart rate (RHR) and heart rate variability (RMSSD) across the menstrual cycle and investigate its association with age, BMI, and birth control use [44].
Participant Cohort:
- 11,590 participants (9,968 naturally cycling, 1,661 using birth control pills).
- Over 45,811 unique menstrual cycles and 1.24 million days of data from a global population [44].
Data Collection Workflow:
- Participants used wrist-worn devices with photoplethysmography (PPG) capabilities to continuously monitor RHR and RMSSD.
- Menstrual cycle data (start and end of bleeding) was self-reported via connected apps [44].
Analytical Workflow:
- Population Modeling: Generalized Additive Mixed Models (GAMMs) established the population-level relationship between cycle day and RHR/RMSSD offsets from the cycle mean.
- Cardiovascular Amplitude (RHRamp/RMSSDamp): Defined for RHR as the mean of the final 7 days of the cycle minus the mean of days 2-8. For RMSSD, it was the mean of days 2-8 minus the mean of the final 7 days.
- Cohort Analysis: GLMs assessed the association of amplitude with age, BMI, and birth control status [44].
Key Findings:
- RHR: Nadir near cycle day 5, peak near day 26.
- RMSSD: Peak near cycle day 5, nadir near day 27.
- Amplitude Attenuation: Cardiovascular amplitude was significantly reduced in older participants and those using hormonal birth control, reflecting dampened hormonal fluctuations [44].
The Researcher's Toolkit: Essential Reagents & Solutions
Table 2: Key Research Reagent Solutions for Vocal Acoustic and Menstrual Cycle Research
| Item / Solution | Function / Application | Example Products / Protocols |
|---|---|---|
| Consumer LH Urine Tests | Reference standard for pinpointing ovulation and the LH surge in experimental protocols. | Easy@Home Ovulation Tests [42], ClearBlue Digital Ovulation Test [43] |
| Fundamental Frequency (F0) Analysis Software | Extracts quantifiable pitch-related acoustic features (mean, SD, percentiles) from voice recordings for statistical analysis. | Custom analysis scripts (e.g., Python, Praat) for F0 feature extraction [42] |
| Wrist-Worn Wearable Sensors | Enables continuous, passive monitoring of physiological parameters (temperature, RHR, HRV) during sleep or daily life. | Ava Fertility Tracker bracelet [43], Commercial PPG-based activity trackers [44] |
| Digital Basal Body Thermometers | Provides a digital, precise point measurement for oral BBT as a baseline comparison for novel methods. | Lady-Comp computerized fertility tracker [43] |
| Custom Mobile Data Collection Apps | Standardizes and centralizes longitudinal data collection (voice, test results, BBT) in a real-world setting. | Klick Applied Science custom app [42] |
| Changepoint Detection Algorithms | Identifies the precise statistical moment (day) when a longitudinal data stream (e.g., vocal features) shifts behavior. | Applied to F0 feature time series to identify fertile window transition [42] |
Logical Pathway from Hormonal Shift to Detectable Signal
The physiological pathways linking hormonal fluctuations to measurable non-invasive signals are complex. The following diagram illustrates the logical pathway from hormonal shifts to the detectable signals captured by the methods discussed in this guide.
Figure 2: Hormonal Shift to Detectable Signal Pathway
The emerging landscape of non-invasive menstrual cycle tracking extends far beyond the limitations of traditional BBT. Vocal acoustic analysis offers a highly scalable, smartphone-based method that captures subtle, hormone-induced tissue changes. Continuous wrist temperature and wearable cardiovascular monitoring provide more sensitive, objective, and longitudinal physiological data streams, enabling a more nuanced view of the menstrual cycle's impact on core physiology. The experimental data confirms that these methods generally offer superior sensitivity and richer datasets for researching hormone trends across diverse cycle patterns compared to BBT.
A critical challenge for the field, particularly for vocal biomarkers, is the current lack of standardized master protocols for data collection and analysis, which can hinder reproducibility and cross-study comparison [46]. Future research should focus on establishing these standards and further validating these technologies in larger, more diverse populations. For researchers and drug development professionals, these technologies open new avenues for investigating cycle-related disorders, the impact of pharmaceuticals on menstrual health, and the fundamental interplay between hormones and broader physiology.
The luteinizing hormone (LH) surge is a definitive endocrine event in the human menstrual cycle, characterized by an abrupt, substantial rise in luteinizing hormone secretion from the anterior pituitary gland. This hormonal surge serves as the primary trigger for ovulation, typically occurring approximately 35–44 hours after surge onset and 10–12 hours after the LH peak [47]. The precise detection of this surge is therefore critical for multiple applications in reproductive medicine, including fertility planning, timed intercourse, and artificial reproductive techniques [48] [47]. From a research perspective, accurate LH surge identification enables scientists to establish temporal relationships between ovulation and other physiological parameters, facilitating investigations into how hormone fluctuations affect metabolic processes, physical performance, and health outcomes across different menstrual cycle patterns [49].
The LH surge results from a complex neuroendocrine signaling cascade originating in the hypothalamus. Under the influence of rising estradiol levels produced by the dominant follicle, the anterior pituitary gland releases a massive bolus of LH into the bloodstream [50]. This LH surge induces the resumption of meiosis in the oocyte and triggers the rupture of the follicular wall, leading to ovulation [47]. The urinary detection of LH metabolites provides a non-invasive alternative to serum measurements while maintaining high diagnostic accuracy, with studies demonstrating that a positive urinary LH test predicts ovulation within 48 hours with high reliability [47].
Gold Standard Methodologies for LH Surge Detection
Laboratory-Based Reference Methods
The clinical gold standard for detecting ovulation is transvaginal ultrasonography, which visualizes follicular development, rupture, and corpus luteum formation [47]. However, for specifically identifying the LH surge, serial serum LH measurements via immunoassay represent the biochemical gold standard. These laboratory-based methods provide quantitative LH values with high sensitivity and specificity but require repeated venipuncture, making them impractical for routine clinical use or long-term research studies [47] [51].
For research applications, especially those requiring precise cycle phase identification, urinary LH detection combined with urinary pregnanediol-3-glucuronide (PdG) measurement provides a practical yet accurate alternative. PdG, a metabolite of progesterone, rises following ovulation and provides retrospective confirmation that ovulation has occurred [48] [47]. This combined approach enables researchers to precisely identify the fertile window and confirm ovulation in study populations without the need for frequent blood draws [28].
Methodological Considerations for Urinary LH Detection
A comprehensive comparison of published methodologies for determining the onset of the LH surge in urine has identified three major methodological categories distinguished by how baseline LH levels are established [48]:
- Method #1 (Fixed Days): Uses fixed cycle days for baseline assessment without prior cycle information.
- Method #2 (Peak-Based): Determines baseline days based on the identified peak LH day.
- Method #3 (Retrospective Estimation): Uses a provisional estimate of the LH surge day to identify the appropriate baseline period.
Research comparing these methods on 254 ovulatory cycles from 227 women found that the most reliable approach for calculating baseline LH utilized 2 days before the estimated surge day plus the previous 4-5 days [48]. This method requires retrospective estimation of the LH surge day to identify the most appropriate part of the cycle for baseline calculation. The surge itself is typically defined as the first sustained rise in LH levels to at least 2.5-fold the standard deviation above the mean baseline level [48]. These methodological differences significantly impact LH surge day determination, highlighting the importance of consistent methodology when comparing across studies.
Table 1: Comparison of Major Methodologies for Determining Urinary LH Surge Onset
| Method Category | Baseline Determination | Pros | Cons | Research Applicability |
|---|---|---|---|---|
| Fixed Days (Method #1) | Predetermined cycle days | Simple, requires no prior cycle information | Less accurate with cycle length variability | Limited for precise phase mapping |
| Peak-Based (Method #2) | Based on identified peak LH day | More personalized to individual cycle | Requires complete cycle data | Moderate for retrospective analysis |
| Retrospective Estimation (Method #3) | Provisional surge estimate to identify baseline | Most accurate baseline identification | Complex, requires complete data | High for precise research cycle classification |
Point-of-Care Applications and Technologies
Lateral Flow Immunoassay Technology
LH rapid test kits represent the most widely adopted point-of-care application for LH surge detection. These devices utilize immunochromatographic assay technology consisting of a sample pad, conjugate pad containing gold-labeled antibodies, nitrocellulose membrane with immobilized antibodies, and an absorbent pad [52]. When a urine sample is applied, LH molecules bind to the gold-labeled antibodies, and the complex migrates via capillary action to the detection zone where it binds to immobilized antibodies, producing a visible test line [52]. Most commercially available tests have a sensitivity threshold of 20-25 mIU/mL, effectively detecting the natural LH surge concentration in urine which typically ranges from 20 to 100 mIU/mL [47] [53].
The primary clinical utility of these point-of-care tests includes: predicting ovulation for natural conception or fertility treatments, monitoring ovarian stimulation during fertility therapies, and serving as a diagnostic tool for conditions like polycystic ovary syndrome (PCOS) characterized by aberrant LH levels [52]. In research settings, these tests provide a practical method for participants to self-detect the LH surge in field-based studies where laboratory access is limited.
Digital Health Platforms and Emerging Technologies
Recent technological innovations have integrated traditional lateral flow technology with digital readers and smartphone applications that quantitatively track LH and PdG levels. These systems use advanced nanotechnology that adjusts for urine pH, normalizes hydration levels, and filters out non-specific binding [28]. The integration of computer vision algorithms accommodates variables like lighting and movement, while machine learning establishes personalized hormone baselines rather than relying on population norms [28]. This approach has demonstrated that calculated cycle lengths tend to be shorter than self-reported lengths, highlighting the inaccuracy of relying on recalled cycle characteristics in research settings [28].
A particularly promising emerging technology involves the development of aptamer-based sensors for continuous LH monitoring. Aptamers are short, single-stranded synthetic DNA or RNA oligonucleotides that bind to specific targets like LH and undergo conformational changes that can be transformed into electrochemical, fluorescent, or colorimetric readouts [51]. Unlike antibodies, aptamers can be engineered for enhanced stability and binding affinity, offering potential for portable, continuous monitoring devices that could revolutionize LH pulsatility assessment in research and clinical practice [51].
Table 2: Comparison of LH Detection Technologies and Their Research Applications
| Technology Type | Detection Principle | Sensitivity | Key Advantages | Research Applications |
|---|---|---|---|---|
| Laboratory Immunoassays | Antibody-antigen binding (ELISA) | High (<0.1 mIU/ml) | Quantitative, high precision | Gold standard validation, assay development |
| Lateral Flow Rapid Tests | Immunochromatographic | Moderate (20-25 mIU/ml) | Rapid, convenient, low cost | Field studies, large population screening |
| Digital Health Platforms | Immunoassay + computer vision | Variable with platform | Quantitative, personalized baselines | Longitudinal studies, cycle variability research |
| Aptamer-Based Sensors | Oligonucleotide binding | Under development | Potential for continuous monitoring | Pulsatility studies, real-time dynamics |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for LH Surge Detection Studies
| Item | Function/Application | Technical Considerations |
|---|---|---|
| Urinary LH Immunoassay Kits | Quantitative measurement of LH in urine | Select assays detecting intact LH; consider inter-assay CV <5% [48] |
| Urinary PdG Immunoassay Kits | Confirmation of ovulation via progesterone metabolite | Post-ovulatory rise confirms luteal phase; intra-assay CV <10% [48] [47] |
| LH Rapid Test Strips | Preliminary surge screening or participant self-testing | Sensitivity threshold ~25 mIU/mL; visual or digital reading [53] |
| Aptamer-Based Sensors | Emerging technology for continuous LH monitoring | Electrochemical, mass-sensitive, or optical readouts [51] |
| Sample Preservation Solutions | Maintain analyte stability in urine samples | Sodium azide commonly used; standardized freeze-thaw cycles [48] |
| Automated Immunoassay Platform | High-throughput sample processing (e.g., AutoDELFIA) | Batch analysis of complete cycles on single plates reduces variability [48] |
Experimental Protocols for LH Surge Detection
Protocol for Urinary LH Surge Detection in Research Populations
For studies investigating menstrual cycle characteristics across different population patterns, the following protocol adapted from peer-reviewed methodologies provides robust LH surge identification [48]:
Participant Selection Criteria: Include premenopausal women with regular menstrual cycles (21-42 days), no fertility medications, no diagnosed PCOS, and at least two natural cycles prior to study entry.
Sample Collection: Participants collect first morning void urine samples daily throughout complete menstrual cycles (from menses to subsequent menses). Samples should be collected in containers with preservative (e.g., sodium azide), refrigerated upon collection, and stored at -80°C before analysis.
Hormonal Analysis: Conduct batch analyses with complete cycles analyzed on single assay plates to minimize inter-assay variability. Use quantitative immunoassays for LH and PdG with appropriate quality controls:
- LH assay should detect intact LH with sensitivity of ≤0.1 mIU/mL and inter-assay coefficient of variation (CV) <5%
- PdG assay should have sensitivity of ≤0.021 μg/mL and inter-assay CV <10%
Cycle Inclusion Criteria: Include only cycles demonstrating unambiguous ovulatory characteristics—detectable LH surges followed by peaks, with consistent rise in PdG levels confirming ovulation.
LH Surge Determination Algorithm:
- Calculate baseline LH using 2 days before the estimated surge day plus the previous 4-5 days
- Define surge threshold as the first sustained rise in LH exceeding 2.5 times the standard deviation above the mean baseline level
- Confirm ovulation with sustained rise in PdG levels (>5 μg/mL for three consecutive days) [47]
Protocol for Validating Point-of-Care Tests in Clinical Research
When evaluating commercial LH detection kits for research applications, this validation protocol ensures reliable data [53]:
Test Administration: Participants perform urine tests with first morning void 12 hours after suspected surge or trigger administration in controlled studies.
Result Documentation: Photograph test results within the manufacturer's specified timeframe (typically 40 seconds to 10 minutes) using standardized lighting conditions.
Verification Method: Compare point-of-care test results with quantitative laboratory measurements from samples collected concurrently.
Statistical Analysis: Calculate false positive and false negative rates, sensitivity, specificity, and accuracy relative to gold standard measures.
Threshold Determination: Establish population-specific or assay-specific LH thresholds for surge identification when possible, rather than relying solely on manufacturer recommendations.
Comparative Data Analysis and Research Implications
The methodological approaches to LH surge detection have significant implications for research comparing hormone trends across different menstrual cycle patterns. A study of 4,123 cycles found that calculated cycle lengths tend to be shorter than self-reported cycle lengths, highlighting the inaccuracy of recall-based cycle characteristics in research settings [28]. Furthermore, significant differences in cycle phase lengths occur across age groups, with follicular phase length declining with age while luteal phase length increases [28].
The substantial methodological variation in LH surge detection approaches can significantly impact research findings. Studies have identified that different detection methods can yield different determinations of LH surge day, complicating cross-study comparisons [48]. This variability underscores the need for methodological standardization in menstrual cycle research, particularly when investigating patterns across diverse populations or cycle characteristics.
Research comparing LH detection technologies reveals important performance characteristics. Traditional laboratory immunoassays provide the highest sensitivity and precision but lack practicality for field-based studies. Lateral flow tests offer convenience but may have slightly lower sensitivity compared to laboratory assays [52]. Digital platforms strike a balance by providing quantitative data with home-based convenience, while emerging aptamer-based technologies promise continuous monitoring capabilities that could transform our understanding of LH pulsatility in naturalistic settings [51].
Graph 1: Neuroendocrine Pathway of LH Surge and Detection Methodologies. This diagram illustrates the hormonal cascade leading to the LH surge, from hypothalamic GnRH secretion to ovarian feedback, and the corresponding detection methodologies used in research and clinical practice.
Graph 2: Experimental Workflow for LH Surge Detection Research. This workflow outlines the key steps in conducting LH surge detection studies, from participant recruitment through data analysis, highlighting the three major methodological approaches for baseline calculation.
The accurate prediction of ovulation and the fertile window is a cornerstone of reproductive health, with implications ranging from natural conception to the timing of assisted reproductive technologies. The classical textbook model of a 28-day cycle with ovulation on day 14 is an inadequate oversimplification for a significant portion of the population. Large-scale data reveals that only 12.4% of women actually exhibit a 28-day cycle, despite 25.3% perceiving this to be their cycle length [54] [55]. Furthermore, over half of all women (52%) experience cycle length variations of five days or more [54]. This substantial intra- and inter-individual variability underscores the critical limitation of calendar-based methods and establishes the imperative for more sophisticated, data-driven prediction models that can adapt to diverse populations and cycle patterns.
The clinical necessity for precision is paramount. In the context of Natural Cycle Frozen Embryo Transfers (NC-FET), for example, the synchronization between embryo development and the endometrial window of implantation is critical. Discrepancies of more than ±1.5 days can significantly reduce implantation rates [56]. This review provides a comparative analysis of emerging statistical and machine learning models for ovulation prediction, evaluating their performance, underlying methodologies, and applicability across different population cohorts, thereby contributing to a broader understanding of hormone trends across varied menstrual cycle patterns.
Comparative Performance of Ovulation Prediction Modalities
The following table summarizes the performance metrics of various ovulation prediction methods as reported in recent studies, providing a quantitative basis for comparison.
Table 1: Comparative Performance of Ovulation Prediction Methods and Models
| Prediction Method / Model | Reported Accuracy | Sensitivity & Specificity | Key Predictive Features | Study Population & Validation Method |
|---|---|---|---|---|
| Machine Learning (Clinical Hormonal Model) [56] | 93.85% (vs. REI determination)92.89% (vs. documented ovulation) | N/R | Progesterone (P4) level, Luteinizing Hormone (LH), Estrogen (E2), follicle diameter, endometrial thickness | 500+ cycles; Validated against clinician determination and combined LH surge/follicular rupture. |
| Wearable Sensor (Ava Bracelet) [57] | 90% (for fertile window) | N/R | Wrist Skin Temperature (WST), Heart Rate, Respiratory Rate, Heart Rate Variability (HRV), Skin Perfusion | 237 women; Validated with urinary LH tests. |
| BBT + HR (Huawei Band 5) - Regular Cycles [58] | 87.46% (fertile window) | Sensitivity: 69.30%Specificity: 92.00%AUC: 0.8993 | Basal Body Temperature (BBT), Heart Rate (HR) | 89 regular menstruators (305 cycles); Gold standard: ultrasound & serum hormones. |
| BBT + HR (Huawei Band 5) - Irregular Cycles [58] | 72.51% (fertile window) | Sensitivity: 21.00%Specificity: 82.90%AUC: 0.5808 | Basal Body Temperature (BBT), Heart Rate (HR) | 25 irregular menstruators (77 cycles); Gold standard: ultrasound & serum hormones. |
| Preovulatory Progesterone ML Model [59] | 85.28% (Random Forest)78.83% (Classification Trees) | P4 ≥ 0.65 ng/ml for ovulation in 24h:Accuracy >92% | Preovulatory Progesterone (P4), LH, E2, Follicle Diameter | 771 patients (NC-FET); Validated via ultrasound-confirmed ovulation. |
| Ultrahuman Cycle Algo 2.0 [60] | N/R (Precision improvement claimed) | N/R | Temperature, HRV, Resting Heart Rate deflection patterns | Trained on >500,000 cycles; Benchmarked against LH tests and a medical-grade device. |
| Connected Ovulation Test (Urinary Hormones) [54] [55] | N/R | LH surge detected in 97.9% of cycles | Urinary Estrone-3-Glucuronide (E3G), Luteinizing Hormone (LH) | 32,595 women (75,981 cycles); Ovulation day determined from test results. |
Note: N/R indicates metrics that were Not Reported in the cited search results.
Detailed Experimental Protocols and Methodologies
Clinical Hormone-Based Machine Learning Models
The development of high-accuracy machine learning models for clinical settings, such as the one achieving 93.85% accuracy, involves a rigorous data collection and model training pipeline [56].
Workflow: Clinical ML Model Development
1. Data Collection & Ovulation Determination:
- Patient Cohort: Recruitment of women with regular menstrual cycles undergoing NC-FET, ensuring a population with confirmed ovulation events [56] [59].
- Ultrasound Monitoring: Transvaginal ultrasounds begin on cycle day 8-10. Scanning continues every 2-3 days until a dominant follicle reaches ~14mm, after which it is performed daily until follicular rupture is observed. The day of rupture is defined as the ovulation day [59].
- Hormonal Assays: When the leading follicle exceeds 14mm, daily morning blood draws are conducted to measure serum levels of LH, Estradiol (E2), and Progesterone (P4) using electrochemiluminescence immunoassay (ECLIA) or similar methods [56] [59].
2. Feature Engineering & Model Training:
- Feature Extraction: The model incorporates a multitude of features, including absolute hormone levels (P4, LH, E2), their ratios (e.g., E2/P4), and relative changes between consecutive measurements. Follicle diameter and endometrial thickness are also included [56].
- Model Development: Datasets are split into training (e.g., 80%) and validation (e.g., 20%) sets. Algorithms such as Random Forest and Classification Trees are trained to classify the proximity to ovulation (e.g., within 24, 48, or 72 hours) [59]. The model's feature importance analysis, as shown in one study, ranked progesterone level on the second test day as the top predictor, followed by LH, estrogen, and follicle size [56].
Wearable Sensor-Based Algorithm Development
Wearable devices offer a passive, at-home method for predicting the fertile window by tracking physiological parameters.
Workflow: Wearable Sensor Data Processing
1. Study Protocol:
- Cohort: Prospective longitudinal studies enroll hundreds of women trying to conceive, who are required to have regular cycles [57].
- Data Collection: Participants wear a wearable device (e.g., a bracelet) nightly during sleep. The device continuously measures Wrist Skin Temperature (WST), Resting Heart Rate, Heart Rate Variability (HRV), and Respiratory Rate [60] [57].
- Ground Truth: Participants use urinary LH test kits to identify the LH surge and log their menstruation dates in a companion app. This data is used to label the fertile window and confirm ovulation for the algorithm [57].
2. Algorithm Mechanism:
- Machine Learning Integration: A ranking-based machine learning model evaluates each day in the cycle for biological plausibility based on deflection patterns in temperature, HRV, and resting heart rate [60].
- Adaptive Learning: Advanced algorithms put extra weight on recent cycle history and intra-cycle data, making them more resilient to fluctuations caused by stress and disrupted sleep, which are known to alter temperature and HRV patterns [60].
The Scientist's Toolkit: Key Reagents and Materials
Table 2: Essential Research Reagents and Materials for Ovulation Prediction Studies
| Item | Function & Application in Research |
|---|---|
| Electrochemiluminescence Immunoassay (ECLIA) | Used for precise quantification of serum hormone levels (LH, E2, P4). Provides high sensitivity and repeatability, crucial for establishing reliable hormonal feature sets for machine learning models [59]. |
| Transvaginal Ultrasound Probe | The gold-standard tool for tracking follicular growth and determining the exact day of follicular rupture (ovulation). It provides essential ground truth data for model training and validation [58] [59]. |
| Urinary Luteinizing Hormone (LH) Test Kits | Provide a practical and reliable method for detecting the LH surge in ambulatory settings. Used as a reference method to validate the timing of ovulation predicted by wearable sensors and apps [54] [57]. |
| Wearable Sensor (Research Grade) | Devices (e.g., wristbands, rings) equipped with photoplethysmography (PPG) and temperature sensors to passively collect physiological data (HR, HRV, WST) from participants in free-living conditions [58] [61] [57]. |
| Electronic Diary / Smartphone App | Enables participants to log menstruation, intercourse, and other cycle-related symptoms. This self-reported data is vital for correlating physiological signals with cycle phases and outcomes [57] [55]. |
Discussion: Insights and Clinical Implications
Key Biomarkers and Technological Convergence
The comparative analysis reveals a hierarchy in predictive features. In clinical settings, preovulatory progesterone (P4) has emerged as a top indicator, potentially superior to LH for predicting imminent ovulation within 24 hours when levels reach a threshold of ≥ 0.65 ng/ml [59]. For consumer-grade wearables, nocturnal wrist skin temperature and resting heart rate are the most robust signals, reflecting the thermogenic effect of post-ovulation progesterone release and general cardiovascular changes across the cycle [61] [57].
A significant trend is the technological convergence of these approaches. Clinical models are becoming more sophisticated by integrating multiple data types (hormones, ultrasound), while consumer devices are leveraging large datasets (>500,000 cycles in one case) to improve their algorithmic precision [60]. The ultimate goal is a multi-modal approach that combines the reliability of hormonal biomarkers with the convenience of continuous, passive physiological monitoring.
Performance in Diverse Populations
A critical finding from the literature is the varying performance of prediction models across different populations. Algorithms combining BBT and HR demonstrated high accuracy (87.46%) for predicting the fertile window in women with regular cycles but showed a marked decrease in performance (72.51% accuracy, 21% sensitivity) for women with irregular cycles [58]. This highlights a significant challenge and an area for future development, as irregular menstruators represent a population for whom improved prediction tools could offer substantial clinical benefit. The ability of newer algorithms to adapt to recent cycle history and stress-induced patterns is a promising step toward personalization for these users [60].
Impact on Clinical Outcomes
The translation of accurate ovulation prediction to tangible clinical outcomes is most evident in reproductive medicine. The study on NC-FET found that when the embryo transfer date was aligned with the ovulation day determined by a machine learning model, clinical pregnancy rates were significantly higher (34.6% vs. 25.9%) compared to cycles where the physician's determination mismatched with the model [56]. This provides compelling evidence that AI-driven ovulation prediction can directly enhance the success rates of fertility treatments by optimizing embryo-endometrium synchronization.
Addressing Irregularities and Optimizing Hormone Therapy Strategies
Polycystic ovary syndrome (PCOS) is the most common endocrine disorder among reproductive-aged women worldwide, with a prevalence ranging from 5% to 26% depending on the diagnostic criteria applied and the population studied [62]. This complex condition serves as a critical nexus connecting irregular menstrual cycles, elevated gynecological cancer risk, and significant cardiometabolic dysfunction. The pathophysiological patterns underlying these connections involve intricate interactions between endocrine axes, metabolic signaling pathways, and chronic inflammatory processes [63]. Understanding these mechanistic relationships is essential for researchers and drug development professionals seeking to identify novel therapeutic targets and develop targeted interventions for this heterogeneous syndrome.
The diagnostic framework for PCOS typically relies on the Rotterdam criteria, which require at least two of the following three features: chronic anovulation, clinical or biochemical hyperandrogenism, and polycystic ovarian morphology [62]. However, emerging research suggests that irregular menstrual cycles alone—even without a formal PCOS diagnosis—may serve as an important biomarker for underlying metabolic dysfunction and future health risks [64] [65]. This article examines the pathophysiological pathways connecting irregular cycles to PCOS, endometrial cancer risk, and cardiometabolic sequelae, providing a comprehensive analysis of current research findings and methodological approaches for investigating these relationships.
Pathophysiological Mechanisms Linking Irregular Cycles to Systemic Health Risks
Endocrine Dysregulation and H-P-O Axis Dysfunction
The hypothalamic-pituitary-ovarian (H-P-O) axis plays a crucial role in maintaining reproductive cyclicity, and its dysregulation represents a fundamental abnormality in PCOS [63]. In affected individuals, increased pituitary sensitivity to gonadotropin-releasing hormone (GnRH) leads to excessive luteinizing hormone (LH) secretion relative to follicle-stimulating hormone (FSH). Studies indicate that approximately 75% of women with PCOS exhibit elevated LH levels, with 94% demonstrating a significantly increased LH/FSH ratio [63].
This hormonal imbalance stimulates ovarian theca cells to produce excess androgens, creating a self-perpetuating cycle of hyperandrogenism and anovulation. Elevated androgen levels further disrupt follicular maturation while inhibiting dominant follicle selection, leading to the characteristic accumulation of immature ovarian follicles [63]. The resulting oligo-ovulation or anovulation manifests clinically as irregular menstrual cycles, which serve as both a diagnostic criterion for PCOS and a marker of underlying endocrine dysfunction.
Table 1: Key Endocrine Alterations in PCOS Pathophysiology
| Endocrine Parameter | Alteration in PCOS | Functional Consequences |
|---|---|---|
| LH/FSH Ratio | Increased (≥2-3:1) | Enhanced ovarian androgen production, impaired follicular development |
| Androgen Levels | Elevated (clinical or biochemical hyperandrogenism) | Hirsutism, acne, ovulatory dysfunction |
| Anti-Müllerian Hormone (AMH) | 2-3 fold increase | Follicular arrest, inhibition of aromatase activity |
| Insulin Signaling | Significant resistance with compensatory hyperinsulinemia | Amplified ovarian steroidogenesis, reduced SHBG |
Metabolic Dysfunction and Insulin Resistance
Insulin resistance represents an independent pathogenic driver in PCOS, affecting approximately 70% of women with the condition regardless of adiposity [62] [63]. The resulting hyperinsulinemia exacerbates hyperandrogenism through multiple mechanisms: insulin synergizes with LH to enhance ovarian androgen production, reduces hepatic sex hormone-binding globulin (SHBG) synthesis, and may independently stimulate adrenal androgen secretion [62].
The bidirectional relationship between hyperinsulinemia and hyperandrogenism creates a vicious cycle that sustains both metabolic and reproductive abnormalities. Insulin resistance in PCOS involves impaired post-receptor signaling pathways, particularly in the phosphatidylinositol-3-kinase (PI3K) pathway, while mitogen-activated protein (MAP) kinase signaling remains largely intact [62]. This specific signaling defect has important implications for both metabolic homeostasis and endometrial proliferation, potentially contributing to increased cancer risk.
Recent research has also highlighted the role of adipokines and inflammatory mediators in PCOS pathophysiology. Leptin levels are typically elevated while adiponectin is reduced, creating a metabolic environment characterized by inflammation, oxidative stress, and impaired glucose homeostasis [66]. These alterations contribute to the chronic low-grade inflammatory state observed in PCOS, which further promotes insulin resistance and creates a permissive environment for cellular transformation.
Immune Dysregulation and Chronic Inflammation
PCOS is characterized by a state of chronic low-grade inflammation marked by elevated levels of C-reactive protein (CRP) and proinflammatory cytokines including IL-6, IL-18, and IFN-γ [66] [63]. This inflammatory milieu contributes to both metabolic dysfunction and reproductive abnormalities while potentially facilitating carcinogenesis through several mechanisms.
Immune cell populations are significantly altered in PCOS. Studies have identified a shift from anti-inflammatory M2 macrophages to pro-inflammatory M1 macrophages, sustaining chronic inflammation within the ovarian microenvironment [66]. Additionally, dendritic cell proportions and natural killer (NK) cell function are often impaired, compromising antitumor immunity. T lymphocyte populations also demonstrate imbalance, with a shift toward Th1 dominance that may impair oocyte quality and ovulation while contributing to endometrial instability [66].
B lymphocytes have recently emerged as important players in PCOS pathophysiology. Beyond their role in antibody production, B cells contribute to antigen presentation and T cell activation, potentially exacerbating insulin resistance. In PCOS mouse models, CD19 antibody infusion significantly reduced peripheral B lymphocyte counts, decreased cystic follicle numbers, and increased corpus luteum formation, suggesting potential therapeutic targets [66].
Diagram 1: Pathophysiological Pathways in PCOS. This diagram illustrates the interconnected endocrine, metabolic, and inflammatory pathways that drive PCOS manifestations and associated health risks.
Quantifying Health Risks: Evidence from Recent Studies
Cardiometabolic Disease Risk Profile
Recent large-scale studies have quantified the substantial cardiometabolic risks associated with PCOS and irregular menstrual cycles. A comprehensive meta-analysis of 23 cohort studies demonstrated that women with PCOS had significantly increased risks of hypertension (risk ratio [RR]: 1.75, 95% CI 1.42-2.15), type 2 diabetes (RR: 3.00, 95% CI 2.56-3.51), and non-fatal cerebrovascular events (RR: 1.41, 95% CI 1.02-1.94) compared to women without PCOS [67]. Lipid abnormalities were also evident, with elevated total cholesterol (mean difference [MD]: 7.14 mg/dl) and reduced HDL-C (MD: -2.45 mg/dl) [67].
The 2024 Apple Women's Health Study (AWHS) analysis of 60,789 participants provided further evidence linking menstrual cycle patterns to cardiometabolic risk, even in the absence of formal PCOS diagnosis [64] [65]. This research found that irregular cycles alone were associated with obesity (prevalence odds ratio [POR]: 1.38), prediabetes (POR: 1.78), type 2 diabetes (POR: 1.38), and metabolic syndrome (POR: 1.73) [64]. Notably, prolonged time to menstrual regularity (more than five years from menarche) was independently associated with several cardiometabolic conditions, suggesting that early cycle patterns may serve as biomarkers for future metabolic dysfunction.
Table 2: Cardiometabolic Risk Profile in PCOS and Irregular Cycles
| Cardiometabolic Condition | PCOS Association (POR/RR) | Irregular Cycles Association (POR) | Population Reference |
|---|---|---|---|
| Type 2 Diabetes | RR: 3.00 [67] | POR: 1.38 [64] | Meta-analysis (n=23 studies); AWHS (n=60,789) |
| Hypertension | RR: 1.75 [67] | POR: 1.20 [64] | Meta-analysis (n=23 studies); AWHS (n=60,789) |
| Obesity | POR: 2.94 [64] | POR: 1.38 [64] | AWHS (n=60,789) |
| Coronary Artery Disease | POR: 2.92 [64] | Not significant | AWHS (n=60,789) |
| Stroke | RR: 1.41 [67] | POR: 1.80 (heart attack) [64] | Meta-analysis (n=23 studies); AWHS (n=60,789) |
| Dyslipidemia | MD TC: +7.14 mg/dl [67] | POR: 1.29 [64] | Meta-analysis (n=23 studies); AWHS (n=60,789) |
Endometrial Cancer Risk Mechanisms
The association between PCOS and endometrial cancer risk is mediated through multiple interconnected pathways. Chronic anovulation results in unopposed estrogen stimulation of the endometrium, lacking the protective effect of progesterone that normally follows ovulation [62] [63]. This hormonal imbalance leads to endometrial hyperplasia, which may progress to carcinoma if left untreated. Additional contributing factors include insulin resistance, chronic inflammation, and immune dysregulation, all of which create a permissive environment for cellular transformation and tumor progression [66].
Molecular studies have identified several mechanisms through which PCOS-related endocrine and metabolic abnormalities may promote endometrial carcinogenesis. Hyperinsulinemia activates key signaling pathways such as PI3K/AKT, enhancing tumor cell growth and survival [66]. Androgen excess may directly stimulate endometrial proliferation through both direct receptor-mediated effects and indirect mechanisms involving insulin-like growth factor (IGF) signaling. The chronic inflammatory state in PCOS further contributes to carcinogenesis through oxidative stress, DNA damage, and impaired immune surveillance [66].
Recent research has also highlighted the potential role of neurotransmitter metabolism and immune checkpoint activation in PCOS-related cancer risk. Studies suggest that women with PCOS may exhibit T cell dysfunction, increased M2 macrophages, and activation of the PD-1/PD-L1 immune checkpoint pathway, creating an immunosuppressive microenvironment that facilitates tumor immune escape [66]. These findings have important implications for both risk stratification and therapeutic development.
Research Methodologies and Experimental Approaches
Digital Cohort Studies and Menstrual Cycle Tracking
The recent Apple Women's Health Study (AWHS) exemplifies the innovative methodologies being employed to investigate menstrual cycle patterns and their health implications [68] [64]. This prospective digital application-based cohort has enrolled over 50,000 participants across the United States, collecting self-reported data on sociodemographic characteristics, medical history, reproductive history, hormonal symptoms, and lifestyle factors.
The study defined PCOS cases as self-reported physician diagnosis, while "possible PCOS" was identified among participants without formal diagnosis but displaying both androgen excess and a history of irregular cycles—meeting two of the three Rotterdam criteria based on available data [68]. This approach allowed researchers to capture both clinically diagnosed cases and undiagnosed individuals, providing a more comprehensive understanding of the PCOS spectrum and its health implications.
Wearable technology has further enhanced menstrual cycle research by enabling continuous physiological monitoring. A recent study analyzing data from WHOOP members introduced "Cardiovascular Amplitude" as a novel metric quantifying fluctuations in resting heart rate (RHR) and heart rate variability (HRV) across the menstrual cycle [38]. This research found that RHR increased by an average of 2.73 BPM from the follicular to luteal phase, while HRV decreased by 4.65 ms, with 93% of participants demonstrating predictable patterns [38]. Such objective biometric measures complement self-reported cycle data and may help identify anovulatory cycles or other abnormalities.
Molecular and Immunological Techniques
Advanced molecular techniques have provided crucial insights into the pathophysiological mechanisms underlying PCOS and its associated health risks. Genome-wide association studies (GWAS) have identified multiple PCOS-associated genetic loci involved in insulin signaling, ovarian steroidogenesis, and steroid hormone biosynthesis [62]. The DENND1A gene has been particularly implicated as a potential risk marker [62].
Immunological research has employed flow cytometry and cytokine profiling to characterize the chronic low-grade inflammation and immune dysregulation in PCOS. Studies have identified significant alterations in immune cell populations, including increased proinflammatory M1 macrophages, reduced natural killer (NK) cells, and T lymphocyte imbalances [66]. Mendelian randomization approaches have further identified specific immune phenotypes associated with PCOS risk, particularly memory B cells [66].
Animal models of PCOS have been instrumental in elucidating pathogenic mechanisms and testing potential interventions. These models typically involve induction of hyperandrogenism (using compounds like dihydrotestosterone) or metabolic disruption, resulting in ovarian morphology and endocrine profiles resembling human PCOS [66] [63]. Recent studies in PCOS mouse models have demonstrated that CD19 antibody infusion reduces cystic follicle numbers and improves ovarian function, highlighting the potential of immunomodulatory approaches [66].
Diagram 2: Experimental Approaches in PCOS Research. This diagram outlines the complementary human studies and animal models used to investigate PCOS pathophysiology and associated health risks.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for PCOS Investigations
| Research Tool Category | Specific Examples | Research Applications |
|---|---|---|
| Hormonal Assays | ELISA kits for Testosterone, Androstenedione, SHBG, AMH | Quantification of hyperandrogenism and endocrine parameters |
| Metabolic Profiling Reagents | Glucose tolerance test materials, Insulin ELISA, Lipid panels | Assessment of insulin resistance and dyslipidemia |
| Molecular Biology Tools | GWAS arrays, RNA sequencing kits, PCR primers for DENND1A | Genetic association studies and gene expression analysis |
| Immunological Reagents | Flow cytometry antibodies (CD19, CD3, CD56), cytokine panels | Immune cell phenotyping and inflammatory mediator measurement |
| Animal Model Compounds | Dihydrotestosterone (DHT), Letrozole, Dehydroepiandrosterone | Induction of PCOS phenotypes in rodent models |
| Cell Culture Systems | Human theca cells, granulosa cell lines, ovarian cortical tissue | In vitro studies of steroidogenesis and folliculogenesis |
| Biometric Monitoring | WHOOP straps, Apple Watch, other research-grade wearables | Physiological tracking across menstrual cycles |
The pathophysiological patterns linking irregular menstrual cycles to PCOS, endometrial cancer risk, and cardiometabolic dysfunction involve complex interactions across endocrine, metabolic, and immune systems. The evidence reviewed demonstrates that irregular cycles—whether occurring within the context of formal PCOS diagnosis or as an isolated finding—represent an important clinical biomarker warranting increased attention from researchers and clinicians alike.
Recent large-scale studies have quantified the substantial health risks associated with these patterns, with women with PCOS facing significantly elevated risks of type 2 diabetes (RR: 3.00), hypertension (RR: 1.75), and cerebrovascular events (RR: 1.41) [67]. Even in the absence of PCOS diagnosis, irregular cycles are associated with meaningful increases in cardiometabolic risk [64] [65]. The mechanisms connecting menstrual cycle abnormalities to endometrial cancer risk involve unopposed estrogen exposure, insulin-mediated signaling pathways, and chronic inflammation with associated immune dysregulation [66] [63].
For drug development professionals and researchers, these findings highlight several promising therapeutic targets. The intricate relationship between hyperinsulinemia and hyperandrogenism suggests that insulin sensitizers may address both metabolic and reproductive features of PCOS. The emerging role of immune dysregulation and specific inflammatory pathways reveals potential opportunities for immunomodulatory interventions. Additionally, the development of targeted therapies for endometrial cancer prevention in high-risk women with chronic anovulation represents an important avenue for future research.
Future investigations should continue to leverage digital health technologies and wearable devices to obtain objective, continuous physiological data across menstrual cycles. Combining these rich phenotypic data with advanced molecular profiling will further elucidate the heterogeneous mechanisms underlying PCOS and its associated health risks, ultimately enabling more personalized approaches to risk stratification and therapeutic intervention.
The evaluation of Hormone Therapy (HT) presents a central challenge in medical research: how to reconcile often contradictory evidence from Randomized Controlled Trials (RCTs) and observational studies. This divergence has profound implications for clinical practice, drug development, and our understanding of hormone trends across different physiological contexts. For decades, observational studies suggested significant cardiovascular benefits from menopausal HT, while subsequent large RCTs revealed increased risks for certain conditions [69] [70]. This guide objectively compares these methodological approaches, examines the quantitative data they generate, and provides the experimental protocols necessary for critical appraisal within hormone trend research.
Methodological Frameworks: Understanding the Fundamental Differences
The discrepancy in HT findings stems primarily from fundamental differences in study design, population characteristics, and data collection methods. Understanding these methodological distinctions is crucial for interpreting the conflicting evidence base.
Core Design Principles and Implementation
Table 1: Fundamental Methodological Differences Between RCTs and Observational Studies of HT
| Feature | Randomized Controlled Trials (RCTs) | Observational Studies |
|---|---|---|
| Allocation to Treatment | Random assignment to HT or control group [71] | Participants/physicians self-select treatments based on individual factors [70] |
| Control for Confounding | Balances known and unknown confounders through randomization [71] | Relies on statistical adjustment; residual confounding likely [70] |
| Blinding | Typically double-blinded (participant and investigator) [71] | Generally not blinded; patients and clinicians know treatment status [72] |
| Population Characteristics | Often older women with more baseline risk factors enrolled for safety [69] | Often includes healthier, younger women initiating HT near menopause [69] |
| Outcome Ascertainment | Systematic, protocol-driven assessment for all events [69] | Potential for detection bias; beliefs may influence diagnosis [72] |
| Hypothesis Testing | Explanatory: Efficacy under ideal conditions [71] | Pragmatic: Effectiveness in real-world settings [71] |
The "Timing Hypothesis" as a Potential Explanatory Model
A leading theory to reconcile the divergent findings is the "Timing Hypothesis," which posits that the cardiovascular effects of HT depend on when treatment is initiated relative to menopause [69]. This hypothesis suggests that initiating HT in younger women (aged <60 or within 10 years of menopause) may be neutral or beneficial, while initiating it later in older women may be harmful. This critical modifying factor was not adequately controlled in early observational studies and was systematically missed in initial RCTs that enrolled predominantly older populations [69] [70].
Quantitative Data Comparison: Cardiovascular and Cancer Outcomes
Systematic reviews and meta-analyses provide the most robust quantitative comparisons between study designs. The table below summarizes key findings from a 2020 meta-analysis of 26 RCTs and 47 observational studies on HT and cardiovascular disease [69].
Table 2: Comparative Risk Estimates for HT from RCTs vs. Observational Studies (Summary Estimates with 95% CI)
| Health Outcome | RCT Summary Estimate (95% CI) | Observational Study Summary Estimate (95% CI) | Notes on Discrepancy |
|---|---|---|---|
| Venous Thromboembolism (VTE) | 1.70 (1.33 - 2.16) [69] | 1.32 (1.13 - 1.54) [69] | Consistent direction; magnitude differs. Risk higher with oral administration. |
| Stroke | 1.14 (1.04 - 1.25) [69] | Not significantly increased [69] | Detection bias in observational studies possible; older RCT population at higher baseline risk. |
| Myocardial Infarction (MI) | Not significantly decreased [69] | 0.79 (0.75 - 0.84) [69] | The landmark discrepancy. Likely due to confounding by socioeconomic status/health behavior in observational studies. |
| Breast Cancer Risk (EPT) | Increased risk (WHI RCT) [73] | Varied findings [73] | Observational studies show more mixed results, potentially influenced by confounding factors. |
Detailed Experimental Protocols in Hormone Therapy Research
Protocol 1: The Women's Health Initiative (WHI) RCT Design
The WHI represents one of the most influential RCTs examining HT, with a design that has been extensively analyzed for its strengths and limitations [70].
- Objective: To assess the major benefits and risks of postmenopausal hormone therapy (E-alone and E+P) on cardiovascular disease, cancer, and fractures.
- Study Population: 27,347 postmenopausal women aged 50-79 recruited at 40 US clinical centers from 1993-1998 [70].
- Inclusion/Exclusion: Women were eligible for the E+P trial if they had a uterus; for the E-alone trial if they had prior hysterectomy. Key exclusions included medical conditions predicting less than 3 years survival, prior cancer, and others [70].
- Randomization & Blinding: Participants were randomly assigned to active hormone therapy or matching placebo using a randomized, double-blind, placebo-controlled design [70].
- Interventions:
- E+P Arm: Conjugated Equine Estrogens (CEE) 0.625 mg/day plus medroxyprogesterone acetate (MPA) 2.5 mg/day.
- E-Alone Arm: CEE 0.625 mg/day.
- Follow-up & Outcome Ascertainment: Semiannual follow-up with self-report, with outcomes adjudicated by physicians based on medical records, autopsy reports, and death certificates [70].
- Statistical Analysis: Primary analysis was intention-to-treat. The trial was designed for 8.5 years of follow-up but stopped early due to identified risks [70].
Protocol 2: Prospective Cohort Observational Study Design
Observational studies like the Nurses' Health Study employed different methodologies that influenced their findings [72].
- Objective: To investigate the association between self-reported menopausal hormone use and incidence of coronary heart disease.
- Study Population: Large cohorts of postmenopausal nurses followed over time with biennial questionnaires.
- Data Collection: HT exposure was self-reported or obtained from gynecologists' prescriptions [74]. Outcome data often came from participant reports supplemented by medical record review [72].
- Confounder Adjustment: Statistical adjustment for known confounders such as age, smoking, BMI, hypertension, and socioeconomic status. However, residual confounding remains a limitation [70].
- Key Methodological Limitation: Unlike RCTs, observational studies typically did not systematically attempt to detect silent myocardial infarctions. Furthermore, ascertainment bias was possible if women taking HT (believed to be cardioprotective) or their physicians were less likely to attribute symptoms to heart disease [72].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Hormone Therapy Investigations
| Reagent/Material | Function in HT Research | Examples & Specifications |
|---|---|---|
| Conjugated Equine Estrogens (CEE) | Estrogen component of HT; derived from pregnant mares' urine. | Premarin; used in WHI trials at 0.625 mg/day [73]. |
| Synthetic Progestins | Counteracts estrogen's endometrial cancer risk in women with a uterus. | Medroxyprogesterone Acetate (MPA/Provera) at 2.5 mg/day in WHI E+P arm [73]. |
| Micronized Progesterone | Bio-identical progesterone alternative to synthetic progestins. | Not used in major RCTs; often employed in "bio-identical" HT [73]. |
| Placebo Formulations | Inert control substance for blinding in RCTs. | Matched in appearance and packaging to active intervention [70]. |
| Validated Assay Kits | Quantify hormone levels (estradiol, FSH, testosterone) for baseline stratification. | Used to confirm menopausal status and monitor adherence [73]. |
| Standardized Case Report Forms | Systematic data collection on outcomes, adherence, and adverse events. | Critical for ensuring consistent data across multiple trial sites [70]. |
Analysis and Path Forward
Reconciling RCT and observational data requires acknowledging that each method answers different but complementary questions. RCTs excel at establishing causal efficacy under controlled conditions, while observational studies reflect real-world effectiveness. The discrepancies in HT research have highlighted critical biological and methodological insights, foremost being the Timing Hypothesis and the importance of population characteristics.
Future research on hormone trends across menstrual cycles and menopausal transitions should prioritize:
- RCTs with Greater Heterogeneity: Including participants stratified by age and time since menopause.
- Advanced Statistical Methods: Utilizing propensity score matching and other techniques to minimize confounding in observational data.
- Standardized Outcome Ascertainment: Ensuring consistent, blinded endpoint assessment across study designs.
- Integration of Genetic and Genomic Data: Understanding how individual variability affects treatment response.
No single study design can fully characterize the complex effects of hormone therapy. A cumulative program of research that combines rigorous RCTs with well-designed observational studies, grounded in biological understanding, remains essential for advancing women's health and drug development.
The landscape of Hormone Therapy (HT) is undergoing a significant transformation, moving away from traditional, standardized formulations toward highly personalized treatment strategies. This shift is largely driven by the integration of bioidentical hormones and sophisticated delivery systems, aligned with a deeper understanding of individual hormonal patterns across the menstrual lifespan. Bioidentical hormones are defined as compounds that are structurally identical to the hormones naturally produced in the human body, such as 17β-estradiol, progesterone, and testosterone [75] [76]. This stands in contrast to synthetic hormones (e.g., conjugated equine estrogens or medroxyprogesterone acetate), which are designed to mimic the effects of natural hormones but have different molecular structures [75].
The clinical rationale for this trend is rooted in the desire for treatments that align more closely with individual physiological processes. The molecular structure of a hormone dictates its interaction with specific receptors in the body, which in turn influences its biological effects, metabolism, and potential side effects [75] [76]. The push for personalization is further supported by large-scale data on menstrual cycle patterns, which reveal that cycle characteristics and associated symptoms are not static but change dynamically with age [77]. Understanding these individual patterns is thus crucial for developing HT that is not only effective in alleviating symptoms like vasomotor disturbances but also in sync with the patient's unique hormonal milieu.
Comparative Analysis: Bioidentical versus Synthetic Hormones
The fundamental difference between bioidentical and synthetic hormones lies in their biochemical origin and structure, which translates into distinct pharmacological and clinical profiles.
Molecular Structure and Source
- Bioidentical Hormones: These are typically derived from plant sterols (e.g., soy or wild yams) and are then chemically modified in a laboratory to achieve a molecular structure that is identical to that of endogenous human hormones [76]. Common examples include micronized 17β-estradiol and micronized progesterone.
- Synthetic Hormones: These are artificially created compounds. While they mimic the function of natural hormones, their structure is different. Examples include conjugated equine estrogens (CEE) derived from horse urine and progestins like medroxyprogesterone acetate (MPA) [75] [78].
Safety and Efficacy Profiles
Evidence from clinical studies and reviews highlights divergent safety and efficacy outcomes between these two classes.
Table 1: Comparative Safety and Efficacy Profiles of Bioidentical vs. Synthetic Hormones
| Aspect | Bioidentical Hormones | Synthetic Hormones |
|---|---|---|
| Breast Cancer Risk | Studies suggest a potentially reduced risk compared to synthetics [79]. | Certain formulations (e.g., CEE+MPA) are associated with an increased risk [78]. |
| Venous Thromboembolism (VTE) | Transdermal bioidentical estradiol appears to carry a lower risk of blood clots [79] [80]. | Oral estrogen therapy is associated with a higher risk of VTE [80]. |
| Cardiovascular & Lipid Profile | Bioidentical progesterone does not negatively impact blood lipids or vasculature; may be neutral or beneficial [79]. | Many synthetic progestins can attenuate the beneficial lipid effects of estrogen and may increase cardiovascular risk [79] [78]. |
| Endometrial Protection | Micronized progesterone is effective in protecting the endometrium when combined with estrogen [79]. | Synthetic progestins are also used for endometrial protection [75]. |
| Metabolic Pathway | Transdermal delivery avoids first-pass liver metabolism, minimizing impact on liver-synthesized proteins [81] [78]. | Oral administration undergoes significant first-pass liver metabolism, increasing production of proteins like angiotensinogen (linked to blood pressure) and clotting factors [78]. |
| Symptom Relief | Effective in alleviating menopausal symptoms like vasomotor symptoms and vaginal dryness [75] [79]. | Effective in alleviating menopausal symptoms [75]. |
A comprehensive 2006 review concluded that bioidentical hormones, particularly progesterone, demonstrate a superior safety profile in areas such as breast cancer incidence and cardiovascular risk compared to their synthetic counterparts [79]. However, it is critical to note that a key report from the National Academies of Sciences, Engineering, and Medicine (2020) emphasized the limited body of rigorous evidence on the safety and effectiveness of compounded bioidentical hormone therapy (cBHT), citing a lack of large-scale randomized controlled trials [82].
Advanced Delivery Systems in Hormone Therapy
The route of administration is a pivotal factor in personalizing HT, as it influences hormone pharmacokinetics, side effects, and patient compliance.
Table 2: Comparison of Hormone Therapy Delivery Systems
| Delivery System | Examples | Key Advantages | Key Disadvantages/Limitations |
|---|---|---|---|
| Oral | Tablets (e.g., CEE, micronized estradiol) | Convenient, familiar, widespread availability [78]. | First-pass liver metabolism, higher risk of VTE and hypertension, fluctuating hormone levels [81] [78]. |
| Transdermal | Patches, gels, creams, emulsions [75] [78] | Avoids first-pass liver effect, steady hormone levels, lower risk of VTE, customizable dosing with creams [81] [80] [78]. | Skin irritation (patches), potential for imprecise dosing with user-applied creams [78]. |
| Intravaginal | Creams, rings, tablets [80] | Localized effect for urogenital symptoms, low systemic absorption with some forms [80]. | Primarily for local symptoms; systemic absorption varies by product. |
| Intranasal | Sprays [78] | Rapid absorption, avoids first-pass metabolism [78]. | Frequent dosing may be required, potential for nasal irritation. |
| Sublingual | Tablets [78] | Rapid absorption, avoids first-pass metabolism [78]. | Can cause fluctuating hormone levels, requires multiple daily doses. |
Experimental Protocol for Transdermal Delivery
A 2011 pilot study provides a clear methodological framework for investigating a biorhythmic transdermal delivery system [81].
- Objective: To evaluate the efficacy of a combined 17β-estradiol and progesterone transdermal emulsion in relieving climacteric symptoms and to assess its ability to mimic the natural ovarian secretory pattern.
- Study Design: An open, non-randomized, between-patient trial conducted over 6 months.
- Participants: 29 healthy, non-hysterectomized menopausal women (aged 44-56) with a Kupperman index >25.
- Intervention: A lipophilic base cream containing micronized 17β-estradiol and progesterone was applied daily in a 28-day cyclic regimen:
- Week 1: 0.05 mg/mL 17β-estradiol + 25 mg/mL progesterone
- Week 2: 0.30 mg/mL 17β-estradiol + 50 mg/mL progesterone
- Week 3: 0.20 mg/mL 17β-estradiol + 100 mg/mL progesterone
- Week 4: 0.10 mg/mL 17β-estradiol + 100 mg/mL progesterone
- Key Outcome Measures:
- Primary Efficacy: Change in Kupperman index from baseline to 3 and 6 months.
- Pharmacokinetics: Saliva and serum levels of 17β-estradiol and progesterone quantified at baseline, 3, and 6 months. Diurnal rhythm was assessed via saliva samples collected at 0, 6, 12, and 24 hours on day 6 of week 2.
- Hormone Assay: Saliva hormones were analyzed using High-Performance Liquid Chromatography (HPLC).
- Results: The study reported a 93% improvement in climacteric symptoms. Saliva 17β-estradiol levels increased significantly from 0.6 ± 0.3 pg/mL (baseline) to 14.1 ± 3.3 pg/mL (6 months). The time to maximum concentration (Tmax) was 6 hours, and baseline levels were reached within 24 hours, indicating a diurnal rhythm [81].
Diagram: Experimental workflow for transdermal hormone therapy study.
The Research Context: Menstrual Cycle Patterns and Personalization
The drive toward personalized HT is firmly grounded in endocrinological research that maps the natural history of the menstrual cycle. A 2024 analysis of real-world data from over 19 million users of a period-tracking application provided unprecedented insight into how cycle patterns evolve with age [77].
- Cycle Length and Variability: The data shows that with advancing age, menstrual cycles tend to become shorter and more variable until the menopausal transition (around ages 40-44), after which both cycles and periods become longer and significantly more variable. The proportion of individuals with irregular cycles was highest in the 51-55 age group (44.7%) [77].
- Symptom Spectrum: The log of menstrual cycle-related symptoms also varies dramatically with age. For instance, cramps and acne are logged less frequently in older participants, while headaches, backaches, stress, and insomnia are more common. Symptoms like breast tenderness and fatigue peak between ages 20-40 [77].
These findings underscore that a "one-size-fits-all" HT approach is physiologically incongruent. They provide a strong rationale for formulations and delivery systems that can be tailored to mimic an individual's natural hormonal patterns or to address age-specific symptom profiles.
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagents for Hormone Therapy Investigations
| Reagent / Material | Function in Research | Example from Literature |
|---|---|---|
| Micronized 17β-Estradiol | The primary bioidentical estrogen used in formulations to study its pharmacokinetics and pharmacodynamics [81] [78]. | Used in a transdermal emulsion to relieve climacteric symptoms and restore physiological levels [81]. |
| Micronized Progesterone | The primary bioidentical progesterone used for endometrial protection and to study its synergistic effects with estrogen [79] [81]. | Combined with estradiol in a transdermal cream to create a cyclical regimen [81]. |
| High-Performance Liquid Chromatography (HPLC) | An analytical technique for the precise quantification of hormone concentrations in biological fluids like saliva and serum [81]. | Used to measure saliva concentrations of 17β-estradiol and progesterone for pharmacokinetic analysis [81]. |
| Transdermal Delivery Vehicle (Lipophilic Base) | A cream or gel formulation that facilitates the absorption of hormones through the skin, enabling non-oral delivery routes [81]. | A lipophilic emulsion-type base was used as the carrier for 17β-estradiol and progesterone [81]. |
| Kupperman Index | A validated quantitative assessment tool used to measure the severity of menopausal symptoms in clinical trials [81]. | Served as the primary efficacy endpoint to quantify symptom relief after 3 and 6 months of treatment [81]. |
| Saliva Sampling Kits | Non-invasive method to collect samples for measuring the free, biologically active fraction of steroid hormones [81]. | Used to track diurnal hormone rhythms and calculate pharmacokinetic parameters like Tmax [81]. |
Diagram: Hormone signaling pathways for receptor activation.
The convergence of bioidentical hormone formulations and advanced, customizable delivery systems represents a paradigm shift in hormone therapy. This trend is powerfully supported by a growing body of research into the dynamic nature of menstrual cycle patterns throughout the reproductive lifespan. The evidence indicates that bioidentical hormones, particularly when delivered via transdermal routes, offer a pharmacokinetic and safety profile that aligns more closely with human physiology than many traditional synthetic alternatives.
For researchers and drug development professionals, the future lies in leveraging real-world data on cycle variability and symptomatology to inform the design of truly personalized HT. The experimental protocols and tools detailed herein provide a framework for such innovation. Future work should focus on robust, long-term clinical trials that further validate the efficacy and safety of these personalized approaches, ultimately leading to more precise and effective treatments tailored to an individual's unique hormonal signature.
Within the broader research on hormone trends across menstrual cycle patterns, a critical challenge in endocrinology and drug development is the effective tailoring of therapeutic strategies to specific patient demographics. Individual characteristics such as age, body mass index (BMI), and menopausal status significantly influence hormonal physiology, disease risk, and, consequently, treatment response [77] [83]. This guide objectively compares the performance of various therapeutic approaches and their modulation by demographic factors, synthesizing current experimental data to inform researchers and scientists. The following sections provide a detailed comparison of demographic-based hormonal changes, analyze the efficacy of targeted therapies, and summarize the experimental protocols and reagent tools essential for advancing this field.
Demographic Variations in Hormonal Physiology and Metabolism
Understanding baseline physiological variations across demographic groups is fundamental to tailoring therapies. Real-world data from large cohorts reveals significant differences in cycle characteristics and metabolic profiles.
2.1 Age-Related Changes in Menstrual Cycle Patterns An analysis of data from over 19 million users of the Flo period-tracking application chronicled clear age-associated patterns in menstrual cycle characteristics [77]. Cycle length and variability, as well as the frequency of logged symptoms, demonstrate dynamic changes across the reproductive lifespan.
Table 1: Age-Associated Changes in Menstrual Cycle Characteristics [77]
| Age Group | Trend in Cycle Length | Trend in Cycle Variability | Most Frequently Logged Symptoms |
|---|---|---|---|
| 18-25 | --- | --- | Mood swings, Cramps, Acne |
| 26-40 | Shortens | Increases | Breast tenderness, Fatigue |
| 41-45 | Shortest | Most Variable | Headache, Backache, Stress, Insomnia |
| 46-50 | Begins to lengthen | Highly Variable | Headache, Backache, Stress, Insomnia |
| 51-55 | Lengthens | Highly Variable | Mood swings, Headache, Backache |
The proportion of individuals with irregular cycles is lowest in the 36-40 age group (28.3%) and highest in the 51-55 group (44.7%), highlighting the perimenopausal transition [77]. With higher age, cycles tend to get shorter and more variable until the age of 40-44, after which they become longer and more variable as women approach menopause.
2.2 Metabolic Shifts Associated with Menopause The transition to menopause induces multiple metabolic changes independent of chronological aging. Cross-sectional and longitudinal evidence from quantitative NMR metabolomics studies shows that post-menopausal females exhibit unfavorable alterations in their metabolic profiles compared to pre-menopausal females, including [84] [83]:
- Worsened Glycemic Control: Higher fasting glucose and HbA1c, increased postprandial glucose responses, and unfavorable continuous glucose monitor (CGM) measures such as greater glycemic variability and reduced time in healthy glycaemic range [84].
- Atherogenic Lipoprotein Profile: Increased concentrations of very small VLDL, IDL, LDL, remnant cholesterol, and reduced LDL particle size [83].
- Increased Inflammation: Suggested by elevated levels of the inflammatory biomarker GlycA (glycoprotein acetyls) [84] [83].
These changes are not solely due to aging; an age-matched analysis confirmed that higher glycaemic postprandial responses are specifically linked to menopausal status [84].
2.3 Body Mass Index (BMI) and Breast Cancer Risk The relationship between BMI and breast cancer risk differs significantly by subtype and menopausal status. A population-based case-control study in women aged 20-44 found that a large increase in BMI from age 18 to reference date (≥10 kg/m²) was associated with a 2.0-fold increased risk of triple-negative breast cancer (TNBC) [85]. In contrast, for estrogen receptor-positive (ER+) disease, the same BMI increase was associated with a reduced risk, but only among nulliparous women (OR=0.3), indicating complex interactions between BMI, reproductive history, and cancer subtype [85].
Comparative Analysis of Therapeutic Approaches
Demographic factors are crucial not only for understanding disease risk but also for optimizing therapeutic interventions. Data from clinical trials provide evidence for tailoring specific drug classes.
3.1 Selective Estrogen Receptor Modulators (SERMs) Across Demographics SERMs, such as tamoxifen and raloxifene, exhibit modulated efficacy based on patient characteristics. A randomized phase II presurgical trial in premenopausal women with ER+ breast cancer tested a weekly low-dose tamoxifen (10 mg/week) versus raloxifene (60 mg/day) versus placebo [86]. The primary endpoint, modulation of the proliferation marker Ki-67, was not significantly affected by either treatment in the overall study population. However, a critical finding emerged within the tamoxifen arm: women with an extensive CYP2D6 metabolism phenotype showed a significant reduction in Ki-67 and a marked increase in Sex Horm-Binding Globulin (SHBG), highlighting the importance of pharmacogenetics in drug response [86].
Both tamoxifen and raloxifene significantly modulated circulating biomarkers in premenopausal women, including reducing the IGF-I/IGFBP-3 ratio, cholesterol, and fibrinogen, while increasing estradiol [86]. Furthermore, case reports indicate that raloxifene, like tamoxifen, can stimulate postmenopausal uterine mucosa in some patients, a finding that necessitates consideration of menopausal status when evaluating the risk-benefit profile of these drugs [87].
3.2 Menopausal Hormone Therapy (MHT) and Metabolic Health The use of MHT has been a subject of extensive research following large trials like the Women's Health Initiative (WHI). An analysis of the PREDICT 1 cohort found that MHT use was associated with favorable outcomes for visceral fat, fasting glucose and insulin, and postprandial triglyceride measures [84]. This suggests a potential metabolic benefit that must be weighed against other risks when considering MHT for symptomatic menopausal women.
The dissemination of clinical trial results has a direct and rapid impact on clinical practice. An analysis of a pharmacy benefits management database showed that HRT prescriptions declined significantly immediately after the publication of the WHI results, with the biggest decline observed in women aged 55-64 [88]. This demonstrates how new evidence can swiftly alter the therapeutic landscape for specific demographic groups.
Experimental Protocols and Methodologies
To ensure the reproducibility and critical evaluation of the data presented, this section outlines the key methodological frameworks from the cited studies.
4.1 Protocol for a Presurgical SERM Trial The study comparing low-dose tamoxifen and raloxifene in premenopausal women provides a model for preoperative clinical trial design [86].
- Study Design: Three-arm, randomized, double-blind clinical trial (tamoxifen 10 mg/week vs. raloxifene 60 mg/day vs. placebo in a 2:2:1 ratio).
- Duration: 6 weeks of treatment before scheduled surgery.
- Participants: Premenopausal women with confirmed ER-positive early breast cancer.
- Primary Endpoint: Tissue change in the proliferation marker Ki-67.
- Secondary Endpoints: Modulation of estrogen and progesterone receptors, and a panel of circulating biomarkers (IGF system, hormones, cardiocirculatory, and bone metabolism biomarkers).
- Biological Specimens: Fasting blood samples and core biopsies of the primary tumor were collected at baseline and at surgery.
- Compliance Monitoring: Pill count, patient calendar, and drug plasma concentration measurements.
4.2 Methodology for Characterizing Menopausal Metabolic Changes The longitudinal study of menopausal metabolism in the ALSPAC cohort employed a rigorous approach to isolate the effects of reproductive aging from chronological aging [83].
- Cohort: 3,312 midlife women (median age 48) at baseline, with a subgroup of 1,492 followed up ~2.5 years later.
- Exposure Assessment: Women were categorized according to the STRAW criteria for reproductive aging (Pre-menopause, Menopausal Transition, Post-menopause) based on detailed questionnaires. Women with surgical menopause or using hormone therapy were excluded.
- Metabolic Profiling: A high-throughput NMR metabolomics platform was used to quantify 74 metabolic measures from fasting plasma samples, covering lipoprotein subclasses, fatty acids, amino acids, and glycemic traits.
- Statistical Analysis: Cross-sectional associations were tested at baseline. In longitudinal analyses, the change in metabolic biomarkers for each change in reproductive-status category was compared to the reference group (women who remained pre-menopausal at both time points), thereby helping to distinguish age-related changes from those due to change in reproductive status.
Diagram Title: Menopause & Biological Aging Study Workflow
Signaling Pathways and Key Reagents
5.1 Estrogen Signaling and SERM Action Selective Estrogen Receptor Modulators (SERMs) function by differentially binding to estrogen receptors (ERs) in various tissues, acting as agonists in some and antagonists in others. This tissue-specific activity is central to their therapeutic application and side effect profile.
Diagram Title: SERM Tissue-Specific Signaling Mechanism
5.2 The Scientist's Toolkit: Key Research Reagents and Materials The following table details essential reagents and materials used in the featured studies, which are critical for reproducing and extending research in this field.
Table 2: Essential Research Reagents and Materials
| Reagent / Material | Function / Application | Example Usage in Context |
|---|---|---|
| EDTA Blood Collection Tubes | Plasma separation for metabolomic and biomarker analysis. | Used in large cohorts (ALSPAC, PREDICT) for high-throughput NMR metabolomics [84] [83]. |
| NMR Metabolomics Platform | Quantitative analysis of lipoproteins, fatty acids, amino acids, glycoproteins, etc. | Profiling 74+ metabolic measures to characterize menopausal metabolic shifts [83]. |
| Anti-Ki-67 Antibody (IHC) | Immunohistochemical staining for cell proliferation marker. | Primary endpoint in presurgical SERM trials to measure antiproliferative effect [86]. |
| CYP2D6 Genotyping Assay | Pharmacogenetic analysis of drug metabolism phenotype. | Identifying "extensive metabolizer" status correlating with tamoxifen efficacy [86]. |
| Continuous Glucose Monitor (CGM) | Measures interstitial glucose for glycemic variability assessment. | Evaluating postprandial metabolism and time-in-range in menopausal studies [84]. |
| Electrochemiluminescent Immunoassays | High-sensitivity quantification of hormones (estradiol, testosterone) and bone markers (CTX). | Measuring circulating biomarker changes in response to SERM treatment [86]. |
| STRAW Criteria Questionnaire | Standardized classification of reproductive aging stages. | Defining exposure (menopausal status) in epidemiological studies [83]. |
The integration of demographic factors—specifically age, BMI, and menopausal status—is indispensable for developing precise and effective therapeutic strategies in endocrinology and oncology. Evidence demonstrates that physiological benchmarks, from menstrual cycle patterns to systemic metabolism, vary significantly across these demographic groups. Consequently, the efficacy of interventions like SERMs and MHT is inherently modulated by these same factors. Future research and drug development must therefore prioritize demographic-stratified analyses and trial designs. Leveraging advanced methodologies, such as high-throughput metabolomics, pharmacogenetics, and wearable-derived digital biomarkers, will be key to deepening our understanding of these complex interactions and optimizing therapeutic approaches for diverse patient populations.
Validating Biomarkers and Comparing Therapeutic Outcomes Across Populations
The accurate detection of ovulation is a cornerstone of reproductive health research, drug development, and clinical fertility assessments. Traditional methods, including urinary luteinizing hormone (LH) tests and transvaginal ultrasound, have established the gold standard for identifying the fertile window. The emergence of digital health technologies, particularly smartphone-connected hormone monitors, promises to make this precise tracking more accessible while generating rich, quantitative datasets for research. This review objectively compares the performance of a novel digital endpoint—the Inito Fertility Monitor (IFM)—against established methods of ovulation detection, focusing on validation data, experimental protocols, and relevance for research on diverse menstrual cycle patterns.
Comparative Performance of Ovulation Detection Methods
The table below summarizes the key characteristics and performance metrics of different ovulation detection methods, highlighting the position of digital endpoints relative to traditional techniques.
| Method | Primary Measured Analytic(s) | Detection Capability | Key Performance Metrics | Primary Use Context |
|---|---|---|---|---|
| Digital Endpoint (Inito Fertility Monitor) [89] [90] | Urinary E3G, LH, PdG, FSH | Predicts fertile window (via E3G/LH) & confirms ovulation (via PdG) | High correlation with ELISA (E3G, PdG, LH); 100% specificity for novel ovulation confirmation criterion [90] | Home-use, clinical research, longitudinal cohort studies |
| Traditional Urinary LH Test (OPK) [91] [92] | Urinary Luteinizing Hormone (LH) | Predicts ovulation (typically 24-36 hours prior) | ~99% accuracy for detecting LH surge; less reliable for irregular cycles/PCOS [91] | Home-use, patient self-monitoring |
| Transvaginal Ultrasound [91] | Follicle development (physical size) | Visualizes follicle growth and confirms follicle rupture | Clinical gold standard for visualizing ovulation; does not directly measure hormone levels [91] | Clinical and research settings |
| Laboratory Hormone Assay (ELISA) [90] [93] | Urinary or serum E3G, PdG, LH, etc. | Quantifies hormone levels for prediction and confirmation | Laboratory reference method for quantitative hormone analysis [90] | Research and specialized clinical diagnostics |
| Basal Body Temperature (BBT) [91] [92] | Body temperature shift | Confirms ovulation after it has occurred (via progesterone rise) | Identifies biphasic pattern; cannot predict ovulation in advance [92] | Home-use, retrospective confirmation |
Experimental Validation of a Digital Endpoint: The Inito Fertility Monitor
A 2023 study provides a direct validation of the Inito Fertility Monitor (IFM) as a digital endpoint against laboratory-based methods [90].
Experimental Protocol and Methodology
- Objective: To evaluate the accuracy of the IFM in measuring urinary E3G, PdG, and LH, and to identify hormone trends in natural menstrual cycles [90].
- Study Population: The validation study recruited 152 women total, divided into two groups. Group I (n=100) provided daily first-morning urine samples for laboratory analysis. Group II (n=52) used the IFM device for testing at home. Participants were aged 21-45 with no diagnosed infertility conditions and regular cycle lengths [90].
- Laboratory Comparison: Urine samples were analyzed in parallel using the IFM and standard laboratory ELISA kits (Arbor EIA kits for E3G/PdG; DRG ELISA kit for LH). All ELISA samples were measured in triplicate [90].
- Data Analysis: The accuracy of IFM was assessed by calculating the recovery percentage of spiked hormone standards and establishing the correlation and coefficient of variation (CV) between IFM results and ELISA measurements [90].
Quantitative Performance Data
The following table summarizes the key analytical results from the validation study, demonstrating the technical performance of the digital monitor [90].
| Performance Metric | E3G | PdG | LH |
|---|---|---|---|
| Average Coefficient of Variation (CV) | 4.95% | 5.05% | 5.57% |
| Recovery Percentage | Accurate | Accurate | Accurate |
| Correlation with ELISA | High | High | High |
The study also proposed a novel, digital criterion for confirming ovulation based on urinary PdG levels. This criterion distinguished ovulatory from anovulatory cycles with 100% specificity and had an area under the receiver operating characteristic (ROC) curve of 0.98 [90]. Furthermore, a previously unobserved hormone trend was identified in 94.5% of the ovulatory cycles studied, demonstrating the capability of dense, digital data collection to reveal new physiological patterns [90].
The Researcher's Toolkit: Essential Reagents and Materials
For researchers designing studies to validate digital fertility endpoints or track hormone trends, the following core materials and methods are essential.
| Item | Function in Protocol | Example |
|---|---|---|
| Smartphone-Based Hormone Monitor | Quantitative, home-based measurement of multiple urinary hormone metabolites over a cycle. | Inito Fertility Monitor (measures E3G, PdG, LH, FSH) [89] [90]. |
| Reference Laboratory Immunoassays | Gold-standard method for validating the quantitative accuracy of a home-use device. | Laboratory ELISA Kits (e.g., Arbor EIA for E3G/PdG; DRG ELISA for LH) [90]. |
| Transvaginal Ultrasound | Clinical gold standard for visually confirming follicular growth and rupture (ovulation). | Used in clinical settings to track follicle size and collapse [91]. |
| Urine Collection Kit | Standardized collection of first-morning urine samples for centralized lab analysis or device calibration. | Provided to study participants for daily at-home collection [90]. |
| Cycle Mapping Service | Comprehensive hormonal profiling from multiple urine samples across a full menstrual cycle. | ZRT Laboratory Menstrual Cycle Mapping (assesses estrogen, progesterone, LH patterns) [93]. |
Workflow and Hormone Relationships in Ovulation Detection
The following diagram illustrates the logical workflow for validating a digital endpoint against reference methods and the corresponding hormonal events in the menstrual cycle.
Figure 1: Experimental validation workflow for comparing digital hormone measurements against laboratory and clinical standards.
The core physiological relationship between the hormones measured by advanced digital tests is shown in the diagram below.
Figure 2: Key hormone sequence in the menstrual cycle. Multihormone digital tests track this cascade to predict and confirm ovulation.
The global hormone therapy (HT) market represents a dynamic and rapidly evolving field, driven by a complex interplay of demographic trends, clinical research advancements, and technological innovations. As of 2025, this market is estimated to be valued between $22.20 billion and $30.53 billion, with projections indicating growth to approximately $38.18 billion to $45.06 billion by 2032-2033, reflecting a compound annual growth rate (CAGR) of 5.72% to 6.21% [94] [95]. This sustained expansion occurs within a nuanced clinical context where therapeutic effectiveness must be continually balanced against established risks, particularly for postmenopausal women. A foundational understanding of this landscape requires integrating commercial market data with evidence from rigorous clinical trials and systematic reviews that have shaped therapeutic protocols and prescribing patterns. The growing aging population worldwide serves as a primary growth driver, with the number of postmenopausal women expected to exceed 1.2 billion by 2030, substantially increasing the potential patient population seeking treatment for menopausal symptoms and related hormonal disorders [96].
The clinical application of hormone therapies extends beyond menopause management to include treatment for conditions such as hypothyroidism, male hypogonadism, growth hormone deficiency, and various cancers. However, menopause management continues to dominate the application segment, accounting for approximately 23.2% of the global market share in 2025 [95]. This predominance reflects both the high prevalence of menopausal symptoms and the ongoing clinical need to optimize risk-benefit profiles for different patient populations. The following analysis systematically compares market trends with clinical trial data to provide researchers, scientists, and drug development professionals with an evidence-based framework for evaluating hormone therapy effectiveness across multiple dimensions.
Market Trends and Growth Dynamics
Current Market Size and Projections
The hormone therapy market demonstrates consistent global growth patterns, with varying estimates reflecting different methodological approaches and market definitions across analysis firms. The market is expected to reach between $40 billion and $55 billion by 2035, according to synthesized projections [96]. This growth trajectory is underpinned by several key factors, including increased awareness about menopause management, growing cases of hormonal imbalances, and continuous demand for effective treatments to alleviate symptoms associated with aging and hormonal disorders [94].
Table 1: Global Hormone Therapy Market Size Projections
| Source | 2024/2025 Base Value | Projection Year | Projected Value | CAGR |
|---|---|---|---|---|
| ResearchAndMarkets.com | $22.20 billion (2024) | 2033 | $38.18 billion | 6.21% |
| Coherent Market Insights | $30.53 billion (2025) | 2032 | $45.06 billion | 5.72% |
| Marketlook Consulting | $27.28 billion (2025) | 2029 | $37.9 billion | 8.6% |
| Consolidated Range | $22-31 billion | 2030-2035 | $38-55 billion | 5.8-8.6% |
Key Market Drivers and Segmentation Analysis
The hormone therapy market's growth is propelled by demographic shifts, particularly the upward trend of the aging global population. Between 2021 and 2031, the percentage of women aged 50 and above increased from 22% to 26% of the female population, significantly expanding the addressable market for menopause-related hormone therapies [94]. Concurrently, increased awareness about menopause and hormonal health, driven by media campaigns, healthcare professionals, and advocacy groups, has encouraged more women to seek medical treatment for symptoms like hot flashes, night sweats, and mood swings [94].
The market exhibits distinct segmentation patterns across therapy types, formulations, and applications:
- By Therapy Type: Estrogen therapy dominates with 30.1% market share in 2025, followed by combination therapies, testosterone therapy, and thyroid hormone replacement [95].
- By Product Formulation: Tablets and capsules lead with 32.2% market share due to their convenience, cost-effectiveness, and established manufacturing processes, followed by patches, gels/creams, and injections [95].
- By Application: Menopause management holds the largest share (23.2%), followed by osteoporosis, hypothyroidism, growth hormone deficiency, and cancer applications [95].
- By Region: North America dominates with 39.3% market share in 2025, while the Asia-Pacific region exhibits the fastest growth (23.5% market share) driven by improving healthcare infrastructure and rising awareness [95].
Technological advancements in hormone replacement therapy have led to the development of safer and more efficient products, including bioidentical hormone therapies and improved delivery systems like patches, gels, and creams that offer more personalized and less invasive treatment options [94]. These innovations have improved patient satisfaction by reducing side effects and enhancing convenience, further driving market adoption.
Clinical Evidence: Efficacy and Risk Profiles
Cardiovascular Outcomes: Clinical Trials vs. Observational Data
The relationship between hormone therapy and cardiovascular disease represents one of the most extensively studied yet contentious areas in women's health. A systematic review and meta-analysis of seven randomized clinical trials published in 2006 provided crucial insights into this association. The analysis found that hormone therapy had no significant effect on all-cause mortality (relative risk 1.02, 95% CI 0.93-1.13), non-fatal acute myocardial infarction (RR 1.00, 95% CI 0.88-1.14), or coronary heart disease mortality (RR 0.99, 95% CI 0.82-1.21). However, it significantly increased the risk of all stroke (RR 1.29, 95% CI 1.13-1.48) [97].
The discrepancy between earlier observational studies and randomized controlled trials has been addressed through methodological frameworks designed to align these different data sources. Hernán et al. (2008) developed an analytic framework that, when applied to the Women's Health Initiative data, demonstrated that properly aligned observational studies could produce estimates comparable to RCT findings [98]. This approach allows researchers to: (1) estimate treatment effects from observational data that are comparable to their RCT counterparts; (2) include early events that occur soon after treatment initiation; (3) estimate various treatment effects of clinical relevance while adjusting for time-varying confounders; (4) assess the generalizability of RCT findings; and (5) combine both data types to study associations that cannot be addressed by a single study [98].
Metabolic Changes Across the Menstrual Cycle
Understanding baseline metabolic rhythmicity in the menstrual cycle provides essential context for evaluating hormone therapy interventions. A comprehensive study of 34 healthy premenopausal women analyzed metabolic patterns across five menstrual cycle phases (menstrual, follicular, periovular, luteal, and pre-menstrual) revealed significant rhythmicity in 208 of 397 metabolites and micronutrients tested, with 71 reaching the false discovery rate threshold of 0.20 [49].
Table 2: Significant Metabolic Changes Across Menstrual Cycle Phases
| Metabolite Category | Specific Changes | Phase with Maximum Effect |
|---|---|---|
| Amino Acids & Biogenic Amines | 39 amino acids and derivatives decreased | Luteal phase (37 compounds significant in L-M contrast) |
| Phospholipids | 18 lipid species significantly reduced | Luteal phase (17 species met FDR threshold for L-F contrast) |
| Vitamins & Cofactors | Vitamin D (25-OH vitamin D) significantly decreased | Menstrual phase showed highest levels |
| Organic Acids | Inositol, pyroglutamic acid, methylmalonic acid met FDR threshold | Luteal phase compared to menstrual and periovulatory |
| Acylcarnitines | Trend toward increase in periovulatory phase | Periovulatory phase (most changes in O-M contrast) |
These findings demonstrate that the luteal phase is characterized by decreased levels of many metabolites, possibly indicative of an anabolic state during the progesterone peak with recovery during menstruation and the follicular phase. The reduced metabolite levels observed may represent a time of vulnerability to hormone-related health issues such as PMS and PMDD [49]. For researchers evaluating hormone therapies, these natural rhythmic patterns must be considered when designing studies and interpreting results, particularly for therapies that may alter or mimic these natural cycles.
Methodological Frameworks for Hormone Therapy Research
Analytical Approaches for Aligning Observational and Trial Data
The methodological framework proposed by Hernán et al. provides a structured approach for comparing and integrating observational and randomized trial data, specifically applied to postmenopausal hormone therapy and coronary heart disease [98]. This framework employs sophisticated statistical methods, including inverse probability weighting and marginal structural models, to account for time-varying confounders and selection biases that frequently complicate the interpretation of observational data. The approach enables researchers to emulate target trials using observational data, creating comparable estimates that bridge the efficacy-effectiveness gap between highly controlled trials and real-world clinical practice.
The application of this framework to hormone therapy research allows for the investigation of critical questions that cannot be adequately addressed by randomized trials alone, including long-term effects, timing of initiation relative to menopause onset ("timing hypothesis"), and effects in underrepresented patient populations. By formally aligning inclusion criteria, treatment strategies, outcome definitions, and follow-up procedures between observational and randomized data sources, researchers can generate more robust evidence regarding the comparative effectiveness of different hormone therapy approaches [98].
Longitudinal Study Designs for Hormone Monitoring
Several landmark studies have established methodological standards for assessing hormonal patterns across the menopausal transition and in response to therapies. These include:
The Study of Women's Health Across the Nation (SWAN) and Daily Hormone Study (DHS): This study implemented a prospective, multicenter design with annual serum sampling targeted to the early follicular phase (days 2-5 after menses) for menstruating women. The DHS subset collected daily first-morning-void urine throughout one complete menstrual cycle, allowing for detailed characterization of hormonal fluctuations [30].
The Penn Ovarian Aging Study (POAS): This longitudinal cohort study collected blood samples in the early follicular phase (days 2-6) during 28 study visits over 14 years, with a unique design featuring back-to-back monthly samples and 9-month spacing of paired visits in the first five years [30].
The Seattle Midlife Women's Health Study: This community-based study collected first morning voided urine on the 6th day of the cycle at monthly intervals, then quarterly, and finally annually over a 10-year period, assessing estrone glucuronide, FSH, testosterone, cortisol, and catecholamines [30].
These studies highlight the importance of standardized timing for biological sampling, accounting for phase of menstrual cycle, and utilizing appropriate statistical methods for analyzing longitudinal hormone data. Each study also combined biological measures with comprehensive symptom assessments, menstrual calendars, and quality of life measures, providing multidimensional insights into the hormone-symptom relationship.
Research Reagent Solutions for Hormone Therapy Studies
Table 3: Essential Research Reagents and Materials for Hormone Therapy Investigations
| Reagent/Material | Application in Research | Specific Examples/Notes |
|---|---|---|
| LC-MS/MS and GC-MS Systems | Metabolomic and lipidomic profiling | Used to analyze 397+ metabolites in plasma and urine; detects amino acids, lipids, organic acids [49] |
| HPLC-FLD Systems | Vitamin and micronutrient quantification | Measures B vitamins and other micronutrients in plasma [49] |
| Immunoassay Kits | Hormone level measurement | Detects estradiol, progesterone, LH, FSH in serum/urine; used in SWAN, POAS, Rotterdam studies [30] |
| Automated Clinical Chemistry Analyzers | Standard clinical parameters | Measures CRP, HDL, triglycerides, cholesterol, glucose in serum [49] |
| Standardized Urine Collection Systems | Daily hormone monitoring | First-morning-void collection for estrone glucuronide, FSH tracking in SWAN DHS [30] |
| DNA/RNA Extraction Kits | Genetic and molecular studies | Banked samples for genomics in Rotterdam Study; potential for personalized therapy research [30] |
These research tools enable comprehensive characterization of hormonal patterns, metabolic responses, and genetic factors influencing treatment efficacy and safety. The integration of multiple analytical platforms is essential for capturing the complexity of endocrine systems and their interactions with therapeutic interventions.
Visualization of Research Methodology and Market Dynamics
Hormone Therapy Research Workflow
Hormone Therapy Market Dynamics
The comparative analysis of hormone therapy market trends and clinical trial data reveals a field characterized by steady commercial growth alongside increasingly nuanced clinical understanding. The market expansion, driven predominantly by demographic shifts and product innovation, occurs in parallel with evolving clinical perspectives on appropriate patient selection, timing of initiation, and therapy duration. The integration of observational data with randomized trial evidence through sophisticated methodological frameworks has been particularly valuable in addressing questions about long-term effects and real-world effectiveness.
For researchers and drug development professionals, several key considerations emerge. First, the natural metabolic rhythmicity of the menstrual cycle provides important baseline data for evaluating therapeutic interventions and their metabolic impacts. Second, the alignment of observational and trial data enables more comprehensive assessment of therapeutic effectiveness across diverse patient populations. Third, market trends toward personalized approaches and novel delivery systems reflect ongoing efforts to optimize the risk-benefit profile of hormone therapies.
Future directions in hormone therapy research will likely focus on further personalization of treatment approaches, leveraging genetic, metabolic, and clinical characteristics to match patients with optimal therapies and formulations. Additionally, continued evaluation of long-term outcomes, particularly in special populations and with newer formulations, will be essential for refining clinical practice and guiding further therapeutic innovation.
Menstrual cycle characteristics and their underlying hormonal drivers are increasingly recognized as vital signs of female health, with implications for fertility, cardiometabolic disease risk, and overall well-being. Historically, the clinical understanding of menstrual physiology has been largely based on studies conducted in homogeneous, predominantly White populations. This narrow evidence base fails to account for potential biological and physiological variations across racially and ethnically diverse groups. Such oversights can lead to misdiagnosis, inappropriate treatment protocols, and inadequate inclusion criteria for clinical research. This comparative guide synthesizes current evidence on hormonal and cycle characteristic variations across racial and ethnic groups, providing researchers and drug development professionals with objective data and methodological frameworks to advance precision medicine in women's health.
Quantitative Comparison of Menstrual Cycle Characteristics
Variations in Cycle Length and Regularity
Comprehensive data from large-scale studies reveal significant variations in menstrual cycle characteristics across demographic groups. The Apple Women's Health Study (AWHS), analyzing 165,668 cycles from 12,608 participants, provides robust evidence of these differences [25] [27].
Table 1: Menstrual Cycle Length Variations by Age, Race/Ethnicity, and BMI
| Characteristic | Subgroup | Mean Cycle Length (Days) | Difference vs. Reference (Days) | Cycle Variability | Odds Ratio for Long Cycles (>40 days) |
|---|---|---|---|---|---|
| Age Group | <20 years | 30.3 | +1.6 vs. 35-39 [25] | 5.3 days [25] | 1.85 [27] |
| 35-39 years | 28.7 (reference) | Reference | 3.8 days [25] | Reference | |
| 40-44 years | 28.2 | -0.5 vs. 35-39 [27] | 4-11 days [25] | 1.72 [27] | |
| 45-49 years | 28.4 | -0.3 vs. 35-39 [27] | Increased by 46% vs. 35-39 [27] | 1.72 [27] | |
| ≥50 years | 30.8 | +2.0 vs. 35-39 [27] | Increased by 200% vs. 35-39 [27] | 6.47 [27] | |
| Race/Ethnicity | White | 29.1 | Reference | 4.8 days [25] | Reference |
| Black | 28.9 | -0.2 vs. White [25] | 4.7 days [25] | Not significant [27] | |
| Asian | 30.7 | +1.6 vs. White [25] | 5.04 days [25] | 1.43 [27] | |
| Hispanic | 29.8 | +0.7 vs. White [25] | 5.09 days [25] | 1.26 [27] | |
| BMI Category | Healthy (18.5-24.9) | 28.9 | Reference | 4.6 days [25] | Reference |
| Overweight (25-29.9) | 29.2 | +0.3 vs. Healthy [27] | - | 1.13 [27] | |
| Class 1 Obesity (30-34.9) | 29.4 | +0.5 vs. Healthy [27] | 5.1 days [25] | 1.30 [27] | |
| Class 2 Obesity (35-39.9) | 29.6 | +0.8 vs. Healthy [27] | 4.8 days [25] | 1.30 [27] | |
| Class 3 Obesity (≥40) | 30.4 | +1.5 vs. Healthy [27] | 5.4 days [25] | 1.30 [27] |
Hormonal Variations Across Racial and Ethnic Groups
Significant differences in key reproductive hormones across racial and ethnic groups highlight the need for population-specific understanding of ovarian function and reserve.
Table 2: Hormonal Characteristics by Race/Ethnicity
| Hormone | Population | Findings | Study |
|---|---|---|---|
| Anti-Müllerian Hormone (AMH) | Caucasian | Higher levels until age 35 compared to other ethnic groups [99] | Bleil et al. |
| Black | 25.2% lower than Caucasian women, independent of age, BMI, smoking, and HIV status [99] | Seifer et al. | |
| Hispanic | 24.6% lower than Caucasian women, though not statistically significant [99] | Seifer et al. | |
| Chinese | Significantly greater AMH levels prior to age 25 than Caucasian women [99] | Bleil et al. | |
| Estrogen Metabolites | Chinese-American | Lower adjusted total-cycle estrone conjugates (E1c) excretion [100] | SWAN DHS |
| Japanese-American | Lower adjusted total-cycle estrone conjugates (E1c) excretion [100] | SWAN DHS |
Figure 1: Hormonal Regulation of the Menstrual Cycle. This pathway illustrates the hypothalamic-pituitary-ovarian axis showing feedback mechanisms that vary across cycle phases and potentially across populations.
Experimental Protocols and Methodologies
Key Study Designs for Hormonal Assessment
Understanding the methodological approaches used in major studies provides context for interpreting comparative data on hormonal and cycle characteristics.
Table 3: Key Longitudinal Studies of Menstrual Cycle Characteristics
| Study | Design | Population | Data Collection | Key Contributions |
|---|---|---|---|---|
| Apple Women's Health Study (AWHS) [25] [27] | Digital cohort using menstrual tracking apps | 12,608 US participants; diverse racial/ethnic representation | Self-tracked menstrual cycle data; demographic and lifestyle surveys | Large-scale quantification of cycle length variations by age, race/ethnicity, and BMI |
| Study of Women's Health Across the Nation (SWAN) [30] [100] | Prospective, multicenter longitudinal study | 3,302 women aged 42-52 at baseline; multiple racial/ethnic groups | Annual serum samples (early follicular phase); Daily Hormone Study (DHS) subset with first-morning urine | Documented ethnic differences in reproductive hormones in midlife women |
| SWAN Daily Hormone Study (DHS) [30] [100] | Intensive longitudinal substudy | 848 SWAN participants | Daily first-morning voided urine for one complete menstrual cycle (up to 50 days) | Characterized daily hormone patterns across menstrual cycles |
| Penn Ovarian Aging Study (POAS) [30] | Longitudinal cohort | 436 Black and White women aged 35-47 at enrollment | Early follicular phase blood samples (days 2-6) collected every 9 months for first 5 years, then annually | Examined racial differences in reproductive hormones with back-to-back monthly samples |
Hormonal Assessment Protocols
Standardized protocols for hormonal assessment are critical for valid cross-population comparisons. The following methodologies represent best practices from major studies:
Early Follicular Phase Serum Sampling Protocol (SWAN, POAS, Melbourne Studies) [30]:
- Timing: Days 2-5 of menstrual cycle (first day of menstruation = day 1)
- Procedures: Fasting blood samples, processed and frozen at -80°C
- Hormones analyzed: FSH, estradiol, LH, inhibins A and B, SHBG, testosterone, DHEAS
- Standardization: Consistent timing across all participants within follicular phase
Daily Urinary Hormone Assessment Protocol (SWAN DHS) [30] [100]:
- Collection: First-morning voided urine daily for one complete menstrual cycle
- Maximum collection: 50 days if no next cycle onset
- Hormone metabolites: Estrone conjugates (E1c), pregnanediol glucuronide (PdG), FSH, LH
- Additional data: Concurrent daily symptom diaries
- Analytical method: Chemiluminescent assays
Digital Menstrual Tracking Protocol (Apple Women's Health Study) [25] [27]:
- Data collection: Mobile app tracking of menstrual flow days
- Cycle calculation: Number of days from first day of period to day before next period
- Validation: Comparison of self-tracked data with typical cycle length recall
- Inclusion criteria: Minimum of three consecutive cycles for variability assessment
Figure 2: Experimental Workflow for Cross-Population Menstrual Cycle Research. This diagram outlines key methodological considerations for studies examining hormonal and cycle characteristics across diverse populations.
The Scientist's Toolkit: Research Reagent Solutions
Essential Materials for Hormonal and Menstrual Cycle Research
Table 4: Key Research Reagents and Materials for Menstrual Cycle Studies
| Reagent/Assay | Application | Key Features | Representative Use in Literature |
|---|---|---|---|
| Chemiluminescent Immunoassays | Quantitative measurement of reproductive hormones in serum and urine | High sensitivity for low hormone levels; minimal cross-reactivity | SWAN DHS urinary FSH, LH, E1C, Pdg [30] [100] |
| Enzyme-Linked Immunosorbent Assay (ELISA) | AMH measurement in serum | Standardized for ovarian reserve assessment; commercial kits available | Ethnic variation studies in AMH [99] |
| Mobile Menstrual Tracking Applications | Digital collection of cycle characteristic data | Real-time data entry; large sample size capability; longitudinal design | Apple Women's Health Study [25] [27] |
| Ancestry Informative Markers (AIMs) | Genetic characterization of ethnicity | Single-nucleotide polymorphisms for ancestral attribution | Olcha et al. study of AMH and genetic ancestry [99] |
| Liquid Chromatography-Mass Spectrometry (LC-MS/MS) | Gold standard for steroid hormone quantification | High specificity and accuracy for hormonal profiling | Reference method for hormone assay validation [30] |
Discussion and Research Implications
The collective evidence demonstrates significant variations in menstrual cycle characteristics and hormonal profiles across racial and ethnic groups. These differences persist after adjustment for age, BMI, and lifestyle factors, suggesting biological, environmental, or genetic influences that warrant further investigation.
The observed patterns have important implications for clinical practice and research methodology. First, the established norms for menstrual cycle parameters (28-day cycle with minimal variability) may not adequately represent the physiological ranges for Asian and Hispanic women, who demonstrate consistently longer and more variable cycles. Second, the assessment of ovarian reserve using AMH requires population-specific reference ranges, as levels are significantly lower in Black and Hispanic women compared to White women. Third, the interaction between obesity and menstrual function appears to vary by ethnicity, with more pronounced effects observed in Hispanic women and potentially different mechanisms in Asian women.
For drug development professionals, these findings highlight the necessity of including diverse populations in clinical trials for hormonal therapies, contraceptives, and fertility treatments. The variations in baseline hormone levels and cycle characteristics could significantly impact drug pharmacokinetics, pharmacodynamics, and overall treatment response.
Future research should prioritize elucidating the underlying mechanisms of these differences, including genetic polymorphisms in hormone metabolism pathways, environmental exposures, and socio-cultural factors that may influence menstrual function. Additionally, the development of population-specific reference ranges for key reproductive biomarkers would enhance clinical diagnostic capabilities and research validity.
The integration of digital health technologies, as demonstrated by the Apple Women's Health Study, provides unprecedented opportunities for large-scale menstrual cycle research across diverse populations. These methodologies complement traditional biochemical approaches and offer robust platforms for advancing our understanding of menstrual health disparities.
Within the broader research on hormone trends across different menstrual cycle patterns, the longitudinal validation of hormone therapy's (HT) impact on long-term health outcomes represents a critical area of investigation. For researchers and drug development professionals, understanding the robust methodological frameworks for assessing sustained benefits and risks is paramount. This guide objectively compares the long-term outcomes of various hormone therapy approaches, with a specific focus on bone density and cardiovascular risk, by synthesizing data from multiple longitudinal studies and clinical trials. The analysis presented herein provides a comprehensive overview of experimental designs, quantitative outcomes, and methodological considerations essential for evaluating HT's enduring impact on women's health.
Comparative Analysis of Long-Term Hormone Therapy Outcomes
Table 1: Key Longitudinal Studies on Hormone Therapy Health Outcomes
| Study/Reference | Therapy Type | Study Duration | Population | Primary Bone Density Findings | Primary Cardiovascular Findings | Other Health Outcomes |
|---|---|---|---|---|---|---|
| 20-Year HT Study (2023) [101] | Transdermal Estradiol (0.025-0.050 mg/d) | 20 years | 56 hysterectomized postmenopausal women | Increase in T-score vertebral densitometry (P=0.014) [101] | Trend in LDL reduction & HDL increase; Decreased VLDL (P=0.05) [101] | Mean Kupperman index decreased from 26.7 to 12.0 (P<0.001) [101] |
| Study of Women's Health Across the Nation (SWAN) [102] [30] | Natural Menopausal Transition | Up to 10 years | 511 premenopausal or early perimenopausal women | N/A | Whole cycle hormones stable until 3 years before FMP; then gonadotropins increased [102] | Percentage of ELA cycles remained high until 5 years before FMP (87.9%) [102] |
| Prostate Cancer ADT Study (2007) [103] | LHRH Agonists (Androgen Deprivation Therapy) | Variable | Men with prostate cancer | Bone loss; Increased fracture risk [103] | Increased HDL, LDL, and triglycerides; Decreased insulin sensitivity [103] | Weight gain; Decreased libido; Erectile dysfunction; Fatigue [103] |
Table 2: Quantitative Metabolic and Bone Mineral Density Changes in Hormone Therapy
| Parameter | Baseline Mean | Follow-up Mean | Change | P-value | Study |
|---|---|---|---|---|---|
| Kupperman Index | 26.7 | 12.0 | -14.7 | <0.001 | 20-Year HT Study [101] |
| VLDL Cholesterol | Not specified | Not specified | Significant decrease | 0.05 | 20-Year HT Study [101] |
| T-score Vertebral Densitometry | Not specified | Not specified | Significant increase | 0.014 | 20-Year HT Study [101] |
| LDL Cholesterol (with ADT) | Not specified | Not specified | Significant increase | <0.05 | Prostate Cancer ADT Study [103] |
| Insulin Sensitivity (with ADT) | Not specified | Not specified | Marked decrease | <0.05 | Prostate Cancer ADT Study [103] |
Experimental Protocols and Methodological Frameworks
Longitudinal Study Designs for Hormone Therapy Assessment
20-Year Prospective Observational Longitudinal Study Protocol [101]
This study exemplifies a robust framework for evaluating long-term HT impacts:
- Population: 56 hysterectomized postmenopausal women with mean age of 67.1 years after 20 years of follow-up
- Intervention: Transdermal estradiol with initial dose of 0.050 mg/day, reduced to 0.025 mg/day at age 60 years
- Data Collection Timepoints: Baseline (t0), 5 years (t1), 10 years (t2), 15 years (t3), and 20 years (t4)
- Parameters Measured:
- Menopause symptoms: Kupperman index (11 symptoms including hot flashes, sleep difficulty, irritability, depression, joint pain)
- Cardiovascular: Blood pressure, lipid profiles (total cholesterol, LDL, HDL, VLDL, triglycerides)
- Bone health: T-score vertebral densitometry, incidence of fractures
- Safety: Breast cancer incidence via mammography and/or sonography
- Statistical Analysis: Bivariate analyses, multivariate generalized estimating equations (GEE) for longitudinal data using R package geepack
The Study of Women's Health Across the Nation (SWAN) Daily Hormone Study Protocol [102] [30]
SWAN implemented a comprehensive approach to characterizing natural hormonal changes:
- Population: 511 premenopausal or early perimenopausal women within 10 years before menopause
- Design: Multicenter prospective study across 7 US sites
- Biospecimen Collection: Daily urine samples for one entire menstrual cycle or up to 50 days annually
- Primary Outcomes: Evidence of luteal activity (ELA), menstrual cycle/segment length, integrated urinary LH, FSH, estrone conjugates, and pregnanediol glucuronide (Pdg)
- Hormone Assay Methods: Urinary metabolites measured to reflect circulating hormone levels
- Data Analysis: Hormone patterns organized around the final menstrual period (FMP)
Recent technological advances have enabled new approaches to longitudinal hormone tracking:
- Platform: Oova at-home fertility testing system
- Methodology: Quantitative tracking of LH and PdG through urine test cartridges
- Technology: AI-powered smartphone app with computer vision algorithms to adjust for pH, normalize hydration levels, and filter out non-specific binding
- Cycle Phase Determination:
- Follicular phase: First day after bleeding cessation to date of peak LH level
- Luteal phase: First day after ovulation to day before next menstrual cycle
- Ovulation confirmation: Rise in progesterone within 72 hours after highest LH levels detected
- Validation: Following Clinical and Laboratory Standards Institute (CLSI) document EP05-A2 protocol
Signaling Pathways and Hormonal Interactions
Menstrual Cycle Hormonal Regulation Pathway
Longitudinal Hormone Study Design Workflow
Research Reagent Solutions for Hormone Therapy Studies
Table 3: Essential Research Reagents and Materials for Hormone Therapy Investigations
| Reagent/Material | Application in Hormone Research | Specific Examples from Studies |
|---|---|---|
| Immunoassay Kits | Quantitative measurement of hormone levels in serum, urine, and other biofluids | LH, FSH, estrone conjugates, pregnanediol glucuronide (PdG) assays used in SWAN DHS [102] [30] |
| LC-MS/MS Platforms | High-resolution metabolomic profiling for comprehensive hormone and metabolite quantification | Used for analysis of 397 metabolites and micronutrients in menstrual cycle metabolomics study [49] |
| Hormone Formulations | Investigational products for therapeutic intervention studies | Transdermal estradiol (0.025-0.050 mg/d) used in 20-year HT study [101] |
| Bone Densitometry Systems | Quantitative assessment of bone mineral density changes | DXA scans for T-score vertebral densitometry measurements [101] |
| Digital Pathology Platforms | AI-based analysis of tissue samples for biomarker development | Multimodal AI-derived predictive biomarker for prostate cancer therapy response [104] |
| Remote Hormone Monitoring Systems | At-home quantitative hormone tracking for longitudinal data collection | Oova platform for LH and PdG tracking in urine [28] |
Discussion and Research Implications
The longitudinal validation of hormone therapy outcomes requires sophisticated methodological approaches that can capture complex physiological relationships over extended timeframes. The studies analyzed demonstrate that well-designed longitudinal investigations can provide critical insights into the sustained impacts of HT on bone health, cardiovascular risk factors, and overall quality of life.
For researchers developing new hormone therapies, these methodological frameworks offer templates for constructing robust clinical trial designs. The 20-year study protocol [101] demonstrates the importance of long-term follow-up, appropriate dose adjustments across age groups, and multidimensional outcome assessment. Similarly, the SWAN Daily Hormone Study [102] [30] illustrates the value of high-frequency biospecimen collection for capturing cyclic hormone patterns and their evolution during reproductive aging.
Emerging technologies, particularly remote hormone monitoring platforms [28] and AI-driven analytical approaches [104], present new opportunities for enhancing the precision and scalability of longitudinal hormone therapy research. These tools enable more frequent data collection in real-world settings while reducing participant burden—addressing key limitations of traditional clinical study designs.
Future research directions should focus on integrating multi-omics approaches with longitudinal clinical phenotyping to identify biomarkers predictive of treatment response and long-term outcomes. Additionally, comparative effectiveness research across different hormone formulations, dosages, and administration routes will provide valuable evidence for personalizing hormone therapy based on individual patient characteristics and risk profiles.
Conclusion
The integration of foundational endocrinology with large-scale, real-world data is revolutionizing our understanding of menstrual cycle patterns and their associated hormone trends. Key takeaways confirm that cycle variability is predominantly governed by the follicular phase and is significantly influenced by demographic factors such as age and BMI. For researchers and drug developers, this underscores the limitations of a one-size-fits-all model and highlights the critical need for personalized medicine approaches. Future directions must focus on the continued validation of digital biomarkers as reliable clinical endpoints, the design of inclusive trials that account for demographic diversity, and the development of next-generation hormone therapies with optimized safety and efficacy profiles based on individual hormonal phenotypes. This synthesis provides a robust framework for advancing both biomedical research and clinical applications in women's health.
References
- 1. Hypothalamic-Pituitary-Ovarian ( HPO ) Axis Dysfunction: Lab Testing... [https://www.rupahealth.com/post/hypothalamic-pituitary-ovarian-hpo-axis-dysfunction-lab-testing-diagnosis-and-treatment]
- 2. The Hypothalamic-Hypophyseal-Ovarian Axis and the Menstrual Cycle ... [https://www.glowm.com/section-view/heading/The%20Hypothalamic-Hypophyseal-Ovarian%20Axis%20and%20the%20Menstrual%20Cycle/item/282]
- 3. The Hypothalamic – Pituitary – Ovarian and Oral... | SpringerLink Axis [https://link.springer.com/chapter/10.1007/978-3-319-44558-8_1]
- 4. Menstrual Cycle - HPG Axis - Stages - TeachMePhysiology [https://teachmephysiology.com/reproductive-system/development-maturation/menstrual-cycle/]
- 5. The Ovarian Cycle [https://books.byui.edu/bio_461_principles_o/the_ovarian_cycle]
- 6. HPA axis activity across the menstrual cycle - a systematic review and meta-analysis of longitudinal studies - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0091302222000218]
- 7. Your BMI could be affecting your menstrual — cycle ... researchers [https://www.news-medical.net/news/20250302/Your-BMI-could-be-affecting-your-menstrual-cyclee28094researchers-explain-how.aspx]
- 8. HPA axis activity across the menstrual - a systematic review... cycle [https://pubmed.ncbi.nlm.nih.gov/35597328/]
- 9. Hormonal Control of Menstrual Cycle: Phases & Key Hormones [https://www.vedantu.com/biology/hormonal-control-of-menstrual-cycle]
- 10. rhythmicity: metabolic Menstrual in healthy women cycle patterns [https://www.nature.com/articles/s41598-018-32647-0?error=cookies_not_supported&code=c2b0f47f-f3fa-446a-b0d9-e25758e4a985]
- 11. Empowering Your Health: New WHOOP Research Reveals Key... [https://www.whoop.com/tw/en/thelocker/new-whoop-research-on-the-menstrual-cycle/]
- 12. Hormone-based models for comparing menstrual cycle and hormonal contraceptive effects on human resting-state functional connectivity - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9649880/]
- 13. Functional Medicine Labs and Supplements to Support Each Phase of... [https://www.rupahealth.com/post/functional-medicine-labs-and-supplements-to-support-each-phase-of-the-menstrual-cycle]
- 14. Current ovulation and luteal tracking methods and technologies... phase [https://pmc.ncbi.nlm.nih.gov/articles/PMC11837971/]
- 15. Physiology, Endocrine Hormones - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK538498/]
- 16. Quantitative fluorescence cytometric measurement of estrogen and progesterone receptors: correlation with the hormone binding assay - PubMed [https://pubmed.ncbi.nlm.nih.gov/12889594/]
- 17. Real-world menstrual characteristics of more than 600,000... cycle [https://www.nature.com/articles/s41746-019-0152-7?error=cookies_not_supported&code=e3833bca-e4e5-4efc-85df-384944c5f240]
- 18. Variability in the phases of the menstrual cycle - PubMed [https://pubmed.ncbi.nlm.nih.gov/16700687/]
- 19. Prospective 1-year assessment of within-woman variability of follicular and luteal phase lengths in healthy women prescreened to have normal menstrual cycle and luteal phase lengths - PubMed [https://pubmed.ncbi.nlm.nih.gov/39320898/]
- 20. The Normal Menstrual Cycle and the Control of Ovulation - Endotext - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK279054/]
- 21. Life-Style and Reproductive Factors Associated with Follicular ... Phase [https://pmc.ncbi.nlm.nih.gov/articles/PMC2834565/]
- 22. rhythmicity: metabolic Menstrual in healthy women... cycle patterns [https://pmc.ncbi.nlm.nih.gov/articles/PMC6167362/]
- 23. Proliferative and Follicular Phases of the Menstrual Cycle - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK542229/]
- 24. Follicular Phase Of Menstrual Cycle: Hormone Levels & Length [https://my.clevelandclinic.org/health/body/23953-follicular-phase]
- 25. today: how Menstrual vary by cycles , weight... menstrual cycles age [https://hsph.harvard.edu/research/apple-womens-health-study/study-updates/menstrual-cycles-today-how-menstrual-cycles-vary-by-age-weight-race-and-ethnicity/]
- 26. Menstrual cycle length variation by demographic characteristics from the Apple Women’s Health Study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10226714/]
- 27. variation by demographic characteristics from... Menstrual cycle length [https://www.nature.com/articles/s41746-023-00848-1?error=cookies_not_supported&code=6cd9e3e3-4f08-4f68-bffa-ce8473b49930]
- 28. Using Hormone Data and Age to Pinpoint Cycle Day within the Menstrual Cycle - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10384168/]
- 29. Using Hormone Data and Age to Pinpoint Cycle Day within the Menstrual Cycle - PubMed [https://pubmed.ncbi.nlm.nih.gov/37512159/]
- 30. Menstrual cycle hormone changes associated with reproductive aging and how they may relate to symptoms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6226272/]
- 31. The interplay between variations of menstrual and cycle ... length age [https://www.news-medical.net/news/20230531/The-interplay-between-variations-of-menstrual-cycle-length-and-age-ethnicity-and-body-weight.aspx]
- 32. Variation in menstrual cycle length by age, race/ethnicity, and body mass index in a large digital cohort of women in the US | medRxiv [https://www.medrxiv.org/content/10.1101/2022.09.30.22280382v1]
- 33. in the Digital : 5 Uses You'll Actually See ( Biomarker ) Real World 2025 [https://www.linkedin.com/pulse/digital-biomarker-real-world-5-uses-youll-actually-see-2025-xfwte]
- 34. Global Markets Report Digital | Rising Adoption of... Biomarkers 2025 [https://finance.yahoo.com/news/digital-biomarkers-global-markets-report-094800528.html]
- 35. Tracking of menstrual cycles and prediction of the fertile window via measurements of basal body temperature and heart rate as well as machine-learning algorithms | Reproductive Biology and Endocrinology | Full Text [https://rbej.biomedcentral.com/articles/10.1186/s12958-022-00993-4]
- 36. Advances in biomonitoring technologies for women’s health | Nature Communications [https://www.nature.com/articles/s41467-025-63501-3]
- 37. Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles | npj Digital Medicine [https://www.nature.com/articles/s41746-019-0152-7]
- 38. Empowering Your Health: New WHOOP Research Reveals Key... [https://www.whoop.com/hk/en/thelocker/new-whoop-research-on-the-menstrual-cycle/]
- 39. JMIR mHealth and uHealth - Harnessing Consumer Wearable Digital Biomarkers for Individualized Recognition of Postpartum Depression Using the All of Us Research Program Data Set: Cross-Sectional Study [https://mhealth.jmir.org/2024/1/e54622/]
- 40. debunk common belief that women get... | ScienceDaily Researchers [https://www.sciencedaily.com/releases/2025/03/250303141152.htm]
- 41. Physiology, Ovulation And Basal Body Temperature - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK546686/]
- 42. JMIR Formative Research - Longitudinal Changes in Pitch-Related... [https://formative.jmir.org/2025/1/e65448/]
- 43. The Accuracy of Wrist Skin Temperature in Detecting Ovulation Compared to Basal Body Temperature: Prospective Comparative Diagnostic Accuracy Study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8238491/]
- 44. A Novel method for quantifying fluctuations in wearable derived daily cardiovascular parameters across the menstrual cycle | npj Digital Medicine [https://www.nature.com/articles/s41746-024-01394-0]
- 45. Smart menstrual health monitoring patch: a non-invasive ai-driven solution for cycle tracing | ECEESPE2025 | Joint Congress of the European Society for Paediatric Endocrinology (ESPE) and the European Society of Endocrinology (ESE) 2025: Connecting Endocrinology Across the Life Course | Endocrine Abstracts [https://www.endocrine-abstracts.org/ea/0110/ea0110rc16.5]
- 46. Frontiers | Master protocols in vocal development to reduce... biomarker [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1619183/full]
- 47. Detection of ovulation, a review of currently available methods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5689497/]
- 48. Comparison between the different methods developed for determining... [https://link.springer.com/article/10.1007/s00404-015-3732-z]
- 49. Menstrual cycle rhythmicity: metabolic patterns in healthy women | Scientific Reports [https://www.nature.com/articles/s41598-018-32647-0]
- 50. Physiology, Menstrual Cycle - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK500020/]
- 51. Using Aptamers as a Novel Method for Determining GnRH/ LH ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7582658/]
- 52. Luteinizing Hormone Rapid Test Kits: Applications, Benefits, and Clinical Utility [https://www.jalmedical.com/luteinizing-hormone-rapid-test-kits-applications-benefits-clinical-utility/]
- 53. Frontiers | Self-Detection of the LH Surge in Urine After GnRH Agonist Trigger in IVF—How to Minimize Failure to Retrieve Oocytes [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2020.00221/full]
- 54. Real-life insights on menstrual cycles and ovulation using big data - PubMed [https://pubmed.ncbi.nlm.nih.gov/32328534/]
- 55. Real-life insights on menstrual cycles and ovulation using big data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7164578/]
- 56. Improved clinical pregnancy rates in natural frozen-thawed embryo... [https://www.nature.com/articles/s41598-024-80356-8?error=cookies_not_supported&code=b64635a7-4a12-40f7-8a6d-e9d66cab9a76]
- 57. Journal of Medical Internet Research - Wearable Sensors Reveal... [https://www.jmir.org/2019/4/e13404]
- 58. Tracking of menstrual and prediction of the cycles via... fertile window [https://pmc.ncbi.nlm.nih.gov/articles/PMC9375297/]
- 59. Preovulatory progesterone levels are the top indicator for ovulation ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-024-01495-0]
- 60. Introducing: Cycle and Ovulation algo 2.0 - Ultrahuman [https://blog.ultrahuman.com/blog/cycle-and-ovulation-algo-2-0/]
- 61. What Is the Fertile ? - The Pulse Blog Window [https://ouraring.com/blog/what-is-fertile-window/]
- 62. Polycystic Ovarian Syndrome - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK459251/]
- 63. Physiopathology of polycystic ovary syndrome in endocrinology, metabolism and inflammation | Journal of Ovarian Research | Full Text [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01621-6]
- 64. and PCOS tied to irregular cycles cardiometabolic risks [https://www.contemporaryobgyn.net/view/pcos-and-irregular-cycles-tied-to-cardiometabolic-risks]
- 65. periods linked with increased Irregular for risk ... cardiometabolic [https://hsph.harvard.edu/news/irregular-periods-linked-with-increased-risk-for-cardiometabolic-conditions/]
- 66. Frontiers | The relationship between polycystic ovary syndrome and gynecological cancers: neurotransmitter metabolism changes and immune regulation [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1578470/full]
- 67. Long-term cardiometabolic disease risk in women with PCOS ... [https://pubmed.ncbi.nlm.nih.gov/32995872/]
- 68. Frontiers | Utilizing a digital cohort to understand the health burden and lifestyle characteristics across the life course in individuals with polycystic ovary syndrome and possible PCOS [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1585628/full]
- 69. A systematic review and meta-analysis of effects of menopausal... [https://www.nature.com/articles/s41598-020-77534-9?error=cookies_not_supported]
- 70. Comparing hormone therapy effects in two RCTs and two large observational studies that used similar methods for comprehensive data collection and outcome assessment - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3717474/]
- 71. Randomized controlled trial - Wikipedia [https://en.wikipedia.org/wiki/Randomized_controlled_trial]
- 72. The discrepancy between observational and studies ... randomized [https://pubmed.ncbi.nlm.nih.gov/14644895/]
- 73. Menopausal Hormone and Cancer Therapy Risk [https://www.cancer.org/cancer/risk-prevention/medical-treatments/menopausal-hormone-replacement-therapy-and-cancer-risk.html]
- 74. Good agreement between physician and self-reported hormone therapy data in a case-control study - PubMed [https://pubmed.ncbi.nlm.nih.gov/17998083/]
- 75. . Bioidentical Therapy | Winona vs Synthetic Hormone [https://bywinona.com/journal/bioidentical-hormones-vs-synthetic-hormones]
- 76. : What’s the Difference in HRT? Bioidentical vs Synthetic Hormones [https://www.tryeden.com/post/bioidentical-vs-synthetic-hormones]
- 77. Chronicling menstrual across the reproductive lifespan... cycle patterns [https://www.nature.com/articles/s41598-024-60373-3?error=cookies_not_supported&code=1833e042-ed62-4605-9820-f00f65cfc119]
- 78. Drug delivery systems for hormone therapy - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S0168365906000630]
- 79. A comprehensive review of the safety and efficacy of bioidentical hormones for the management of menopause and related health risks - PubMed [https://pubmed.ncbi.nlm.nih.gov/17217322/]
- 80. in menopausal Advances hormonal therapy delivery systems [https://link.springer.com/article/10.2165/00137696-200503010-00002]
- 81. Efficacy of biorhythmic transdermal combined hormone treatment in relieving climacteric symptoms: a pilot study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3068872/]
- 82. The Safety and Effectiveness of Compounded Bioidentical Hormone Therapy - The Clinical Utility of Compounded Bioidentical Hormone Therapy - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK562865/]
- 83. Metabolic characterization of menopause: cross-sectional and longitudinal evidence | BMC Medicine | Full Text [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-018-1008-8]
- 84. is associated with postprandial metabolism, metabolic... Menopause [https://pmc.ncbi.nlm.nih.gov/articles/PMC9669773/]
- 85. Height, BMI , BMI and the risk of change positive... estrogen receptor [https://pmc.ncbi.nlm.nih.gov/articles/PMC4013221/]
- 86. A randomized phase II presurgical trial of weekly low-dose tamoxifen ... [https://breast-cancer-research.biomedcentral.com/articles/10.1186/bcr3439]
- 87. Similarity of uterine mucosa changes in patients treated by raloxifen... [https://pubmed.ncbi.nlm.nih.gov/12168910/]
- 88. The Impact of Clinical Trials on the Use of Hormone Replacement Therapy: A Population-Based Study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1490267/]
- 89. 5 Best Ovulation Tests of 2025 , Based on Our Testing [https://www.thebump.com/a/best-ovulation-predictor-kits]
- 90. of urinary reproductive Validation measurements using... hormone [https://pmc.ncbi.nlm.nih.gov/articles/PMC10247788/]
- 91. Taking an Ovulation Test When Pregnant: Will the LH Surge Stay High? [https://shop.miracare.com/en-gb/blogs/resources/ovulation-test-when-pregnant]
- 92. Best Ovulation Tests Of 2025 – Forbes Health [https://www.forbes.com/health/womens-health/best-ovulation-tests/]
- 93. Mapping by ZRT Laboratory Menstrual Cycle [https://www.rupahealth.com/lab-tests/zrt-laboratory-menstrual-cycle-mapping]
- 94. Replacement Hormone Growth Therapy Report... Market Trends [https://www.businesswire.com/news/home/20250410095331/en/Hormone-Replacement-Therapy-Market-Growth-Trends-Report-2025-2033-Increased-Incidence-of-Menopause-and-Aging-Demography-Advances-in-HRT-Products-and-Treatment-Options---ResearchAndMarkets.com]
- 95. Size & Opportunities, Hormone -2032 Therapy Market 2025 [https://www.coherentmarketinsights.com/industry-reports/hormone-therapy-market]
- 96. Global Hormone Replacement Therapy Report ( Market –2035)... 2025 [https://www.linkedin.com/pulse/global-hormone-replacement-therapy-market-report-zlgrc]
- 97. and cardiovascular disease: a systematic review... Hormone therapy [https://pubmed.ncbi.nlm.nih.gov/16398764/]
- 98. An Analytic Framework for Aligning Observational and Randomized... [https://link.springer.com/article/10.1007/s12561-012-9073-6]
- 99. /Race and Age-Specific Ethnicity of Serum AMH in... Variations [https://pmc.ncbi.nlm.nih.gov/articles/PMC7900163/]
- 100. Body size and ethnicity are associated with menstrual ... cycle [https://pubmed.ncbi.nlm.nih.gov/15181033/]
- 101. Benefits for cardiovascular system, bone , and quality of life... density [https://pmc.ncbi.nlm.nih.gov/articles/PMC11465755/]
- 102. Menstrual Cycle Hormone Changes in Women Traversing Menopause: Study of Women's Health Across the Nation - PubMed [https://pubmed.ncbi.nlm.nih.gov/28368525/]
- 103. Possible complications of hormone - Harvard therapy Health [https://www.health.harvard.edu/blog/possible-complications-of-hormone-therapy-2009031019]
- 104. Development and Validation of an Artificial Intelligence Digital... [https://pubmed.ncbi.nlm.nih.gov/40239134/]