Estradiol and Cognitive Performance: Molecular Mechanisms, Clinical Evidence, and Therapeutic Implications
This article synthesizes current research on the multifaceted mechanisms by which estradiol modulates cognitive performance.
Estradiol and Cognitive Performance: Molecular Mechanisms, Clinical Evidence, and Therapeutic Implications
Abstract
This article synthesizes current research on the multifaceted mechanisms by which estradiol modulates cognitive performance. It explores the foundational neurobiology, including genomic and non-genomic signaling pathways, receptor distribution, and key brain regions such as the hippocampus and prefrontal cortex. The review critically assesses methodological approaches in both clinical and preclinical settings, highlighting the impact of formulation, timing, and administration route on cognitive outcomes. It addresses challenges in therapeutic application, including the critical period hypothesis and individual risk factors, and provides a comparative analysis of estradiol-based therapies against other hormonal and non-hormonal targets. Aimed at researchers and drug development professionals, this analysis aims to bridge foundational science with clinical translation for the development of targeted cognitive therapeutics.
The Neurobiological Basis: How Estradiol Modulates Brain Function and Cognition
Estradiol, the most potent estrogen, exerts profound influence on brain function through two distinct classes of signaling mechanisms: genomic and non-genomic pathways. The genomic pathway represents the classical mechanism involving nuclear estrogen receptors (ERα and ERβ) acting as ligand-dependent transcription factors to regulate gene expression over hours to days [1] [2]. In contrast, the non-genomic pathway encompasses rapid signaling events (within seconds to minutes) initiated at the plasma membrane or in the cytoplasm, independently of direct transcriptional regulation [3] [4]. These pathways collectively mediate estradiol's effects on neuronal survival, synaptic plasticity, cognitive function, and neuroprotection, with significant implications for understanding hormonal influences on brain health and disease pathogenesis.
Table 1: Core Characteristics of Genomic vs. Non-Genomic Estradiol Signaling
| Feature | Genomic Signaling | Non-Genomic Signaling |
|---|---|---|
| Temporal Profile | Slow (hours to days) | Rapid (seconds to minutes) |
| Primary Receptors | Nuclear ERα, ERβ | Membrane-associated ERα, ERβ, GPER1 |
| Signaling Initiation | Intranuclear receptor binding | Membrane/cytoplasmic activation |
| Key Mechanisms | Gene transcription via ERE/AP-1/Sp1 | Kinase activation (MAPK, PI3K/Akt), Ca²⁺ flux |
| Biological Outcomes | Protein synthesis, long-term plasticity | Rapid neuromodulation, synaptic efficacy |
| Experimental Inhibition | Transcription inhibitors (actinomycin D) | Kinase inhibitors, receptor antagonists |
Genomic Signaling Mechanisms
Classical Transcriptional Regulation
The genomic pathway begins with estradiol passively diffusing across the plasma membrane and nuclear envelope due to its lipophilic nature [1]. Inside the nucleus, estradiol binds to classical estrogen receptors ERα or ERβ, prompting receptor dimerization and binding to specific DNA sequences known as estrogen response elements (EREs) located in promoter regions of target genes [1] [2]. The ligated receptor complex recruits co-regulator proteins that modify chromatin structure and facilitate the assembly of the transcriptional machinery, ultimately leading to regulated expression of target genes [1].
This mechanism results in the synthesis of new proteins that underlie long-term functional and structural changes in neurons. Key neuroprotective genes induced through genomic signaling include neurotrophic factors (nerve growth factor, brain-derived neurotrophic factor, neurotrophins 3 and 4, insulin-like growth factor 1), anti-apoptotic proteins (Bcl-2, Bcl-x), and proteins that maintain cellular architecture such as neurofilament and microtubulin-associated proteins [1].
Non-ERE-Dependent Genomic Regulation
Beyond the classical ERE-mediated transcription, estrogen receptors can regulate gene expression through protein-protein interactions with other DNA-binding transcription factors. ERs can dock to AP-1 transcription factors and influence gene transcription in the absence of an ERE [5]. Similarly, interaction with Sp1 transcription factors enables regulation of genes like CCND1 (coding for cyclin D1) through Sp1-binding sites in their promoter regions [5]. This mechanism significantly expands the repertoire of genes amenable to estrogenic regulation beyond those containing canonical ERE sequences.
Non-Genomic Signaling Mechanisms
Membrane-Initiated Estradiol Signaling
Non-genomic signaling is characterized by rapid cellular responses that occur too quickly to involve transcription and translation. These effects are mediated through estrogen receptors localized at or near the plasma membrane, including membrane-associated forms of ERα, ERβ, and the G protein-coupled estrogen receptor 1 (GPER1) [3] [4].
A key mechanism enabling membrane localization of classical ERs involves post-translational palmitoylation. This reversible lipid modification, catalyzed by palmitoyl acyltransferase enzymes DHHC7 and DHHC21, increases receptor lipophilicity and facilitates association with lipid membranes [3]. Mutation of the ER palmitoylation site eliminates membrane function while preserving nuclear activity, demonstrating the functional segregation of these signaling pathways [3].
Receptor Complexes and Signaling Cascades
Membrane estrogen receptors functionally couple with various signaling systems. In neurons, ERα and ERβ have been shown to functionally couple to group I and II metabotropic glutamate receptors (mGluRs), initiating mGluR signaling upon estradiol stimulation independent of glutamate [3]. This interaction is facilitated by caveolin proteins (Cav1-3) which organize signaling molecules into functional microdomains, with Cav1 and Cav3 generating distinct signaling complexes that isolate estrogen activation of group I from group II mGluR signaling [3].
Table 2: Major Non-Genomic Estradiol Signaling Pathways in the Brain
| Signaling Pathway | Initial Events | Key Effectors | Functional Outcomes |
|---|---|---|---|
| Src/Ras/ERK Cascade | Src activation, Ras phosphorylation | ERK1/2, CREB | Neuritogenesis, synaptic plasticity |
| PI3K/Akt Pathway | PI3K recruitment, PIP3 formation | Akt, eNOS, GSK-3β | Cell survival, metabolic regulation |
| Ca²⁺ Signaling | Mobilization of intracellular Ca²⁺ | CaMKII, PKC | Neurotransmitter release, excitability |
| cAMP Pathway | Adenylate cyclase activation | PKA, CREB | Gene expression, synaptic plasticity |
| mGluR Coupling | ER-mGluR functional interaction | IP₃, DAG | Neural excitability, behavior |
Upon estradiol binding, these membrane-associated receptor complexes activate multiple intracellular signaling cascades:
MAPK/ERK Pathway: Estradiol activates c-Src, leading to phosphorylation of Shc and subsequent Ras activation, which initiates the MAPK cascade resulting in ERK phosphorylation and activation of transcription factors like CREB [6]. This pathway plays a central role in the neuritogenic actions of estradiol [6].
PI3K/Akt Pathway: Estradiol stimulates PI3K activity, leading to Akt phosphorylation which promotes neuronal survival through inhibition of pro-apoptotic factors and activation of endothelial nitric oxide synthase (eNOS) [1] [4].
Calcium Signaling: Estradiol rapidly modulates intracellular calcium concentrations, affecting neuronal excitability and synaptic function through activation of calcium-dependent enzymes [4].
The dynamics of membrane ER signaling are tightly regulated. Estradiol initially promotes ERα trafficking to the membrane, then induces receptor internalization via phosphorylation by G protein-coupled receptor kinase 2 (GRK2) and recruitment of β-arrestin-1, which links ERα to the AP-2 adaptor complex for clathrin-mediated endocytosis [3]. This internalization both curtails signaling and facilitates endosomal signaling, extending cellular responsiveness [3].
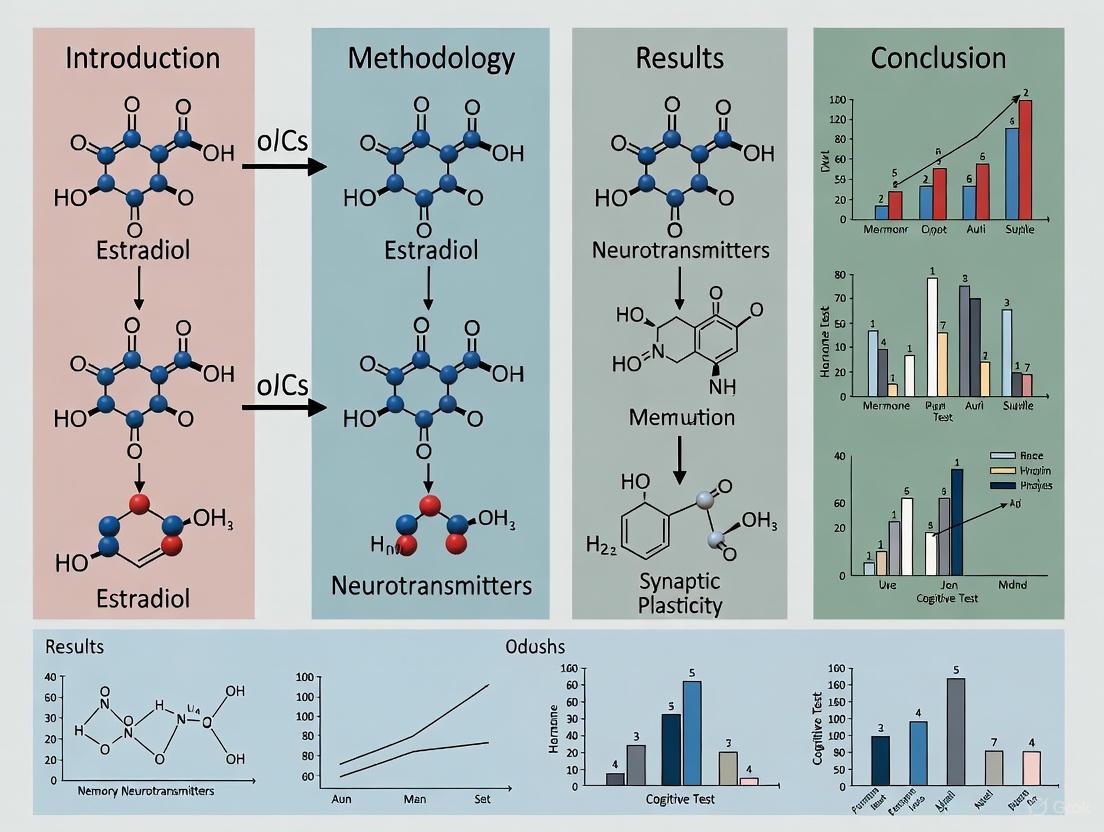
Diagram 1: Genomic and non-genomic estradiol signaling mechanisms in neurons.
Signaling Cross-Talk and Integration
Transcriptional Cross-Talk
The genomic and non-genomic pathways do not operate in isolation but engage in extensive cross-talk. Non-genomic signaling can indirectly influence gene expression through kinase-mediated phosphorylation of transcription factors and co-regulators. For instance, activation of the Src/Ras/Erk cascade by estradiol leads to phosphorylation of nuclear ER and other transcription factors, modulating their transcriptional activity [5]. This mechanism enables integration of rapid membrane-initiated signals with longer-term genomic responses.
Evidence for this cross-talk comes from studies showing that inhibition of the Src/Ras/Erk pathway with PD 98059 partially suppresses transcription of ER target genes (TFF1, ER, PR, BRCA1) induced by estradiol and certain xenoestrogens [5]. Similarly, estradiol activation of PI3K/Akt signaling modulates the activity of various transcription factors involved in cell survival and metabolism [1].
Interaction with Neurotrophic Signaling
Estradiol signaling extensively interacts with neurotrophic factor pathways, particularly brain-derived neurotrophic factor (BDNF) and insulin-like growth factor-I (IGF-I) signaling [6]. Estradiol increases BDNF expression through genomic mechanisms while simultaneously activating BDNF signaling pathways through non-genomic mechanisms. Similarly, estradiol and IGF-I show synergistic activation of both MAPK and PI3K cascades, enhancing neuritogenesis beyond what either signal achieves independently [6].
Estradiol also modulates Notch signaling, which inhibits neurite outgrowth. In hippocampal neurons, estradiol inhibits Notch signaling through GPR30, thereby promoting dendritic complexity [6]. These interactions demonstrate how estradiol coordinates multiple signaling systems to regulate neuronal development and plasticity.
Experimental Approaches and Methodologies
Investigating Genomic Signaling
Chromatin Immunoprecipitation (ChIP) Assays:
- Purpose: Identify direct binding of estrogen receptors to genomic DNA at EREs or other regulatory elements.
- Methodology: Crosslink proteins to DNA with formaldehyde, immunoprecipitate ER-DNA complexes using specific antibodies, reverse crosslinks, and quantify target sequences by PCR or sequencing [1].
- Key Applications: Mapping ER binding sites genome-wide, characterizing receptor interactions with non-ERE promoter elements (AP-1, Sp1 sites).
Gene Expression Profiling:
- Purpose: Comprehensive analysis of transcriptional programs regulated by estradiol.
- Methodology: RNA sequencing or microarray analysis of cells or tissue samples treated with estradiol versus vehicle control, with or without transcription inhibitors.
- Key Applications: Identification of estrogen-target genes, distinction between primary and secondary transcriptional responses [5].
Analyzing Non-Genomic Signaling
Kinase Activity Assays:
- Purpose: Measure rapid activation of signaling cascades following estradiol treatment.
- Methodology: Western blot analysis using phospho-specific antibodies for activated kinases (p-ERK, p-Akt, p-Src) at short time points (2-30 minutes) after estradiol exposure [3] [5].
- Pharmacological Inhibition: Use of specific inhibitors (PD 98059 for MEK, LY294002 for PI3K, ICI 182,780 for ER) to establish pathway specificity and ER dependence.
Calcium Imaging:
- Purpose: Visualize rapid estradiol-induced changes in intracellular calcium concentrations.
- Methodology: Load cells with fluorescent calcium indicators (Fura-2, Fluo-4), treat with estradiol, and monitor fluorescence changes in real-time using confocal microscopy [4].
- Key Applications: Demonstrate rapid signaling independent of transcription, characterize spatial and temporal dynamics of calcium signaling.
Membrane Receptor Localization:
- Purpose: Establish plasma membrane localization of estrogen receptors.
- Methodology: Cell fractionation followed by Western blotting, immunofluorescence with membrane markers, biotinylation of surface proteins [3].
- Palmitoylation Inhibition: Use of 2-bromopalmitate or DHHC enzyme knockdown to disrupt membrane localization and test functional consequences [3].
Table 3: Experimental Models for Studying Estradiol Signaling in the Brain
| Model System | Key Applications | Methodological Considerations |
|---|---|---|
| Primary Neuronal Cultures | Neurite outgrowth, synapse formation, rapid signaling | Maintain relevant neuronal phenotypes, hormone deprivation |
| Immortalized Cell Lines (e.g., HT-22, MCF-7) | Signaling pathway mapping, receptor trafficking | May lack complete neuronal characteristics |
| Brain Explants/Organotypic Cultures | Circuit-level responses, cellular interactions | Preserve native architecture and some connectivity |
| Rodent OVX Model | Cognitive testing, neuroprotection, therapy evaluation | Surgical vs. natural menopause considerations |
| Transgenic Models (ER knockouts, reporter lines) | Receptor-specific functions, pathway necessity | Compensation during development, cell-type specificity |
Behavioral and Cognitive Assessments
Morris Water Maze:
- Purpose: Assess spatial learning and memory in rodent models of estrogen deficiency and replacement.
- OVX Model Methodology: Female rats undergo ovariectomy to remove endogenous estrogen source, followed by estradiol or vehicle treatment, then tested for acquisition and retention of platform location [7].
- Outcome Measures: Escape latency, path length, time in target quadrant during probe trial [7].
Domain-Specific Cognitive Testing:
- Purpose: Evaluate specific cognitive domains affected by estradiol in human populations.
- Methodology: Comprehensive test batteries assessing episodic memory, prospective memory, executive functions, processing speed, and visuospatial processing [8] [9].
- Clinical Applications: Correlate hormonal status, menopausal stage, and hormone therapy with cognitive performance across domains [8].
Diagram 2: Experimental approaches for investigating estradiol signaling mechanisms.
Functional Outcomes and Clinical Implications
Neuroprotection and Cognitive Function
Estradiol signaling through both genomic and non-genomic mechanisms exerts significant neuroprotective effects. Genomic signaling promotes neuronal survival through induction of anti-apoptotic proteins (Bcl-2, Bcl-x) and down-regulation of pro-apoptotic factors (BAX) [1]. Non-genomic signaling provides rapid protection against excitotoxicity and oxidative stress through kinase-mediated pathways [1] [4].
Clinical and epidemiological studies demonstrate that earlier age at menopause is significantly associated with lower scores across multiple cognitive domains, including episodic memory, prospective memory, and executive functions [8]. Conversely, estradiol-based menopausal hormone therapy shows domain-specific benefits, with transdermal estradiol associated with higher episodic memory scores and oral estradiol with higher prospective memory scores [8]. The critical window hypothesis posits that timing of estrogen therapy initiation relative to menopause is crucial for cognitive benefits, with early intervention near menopause onset showing the most favorable outcomes [9].
Therapeutic Implications and Drug Development
Understanding the distinct mechanisms of genomic versus non-genomic signaling has important implications for therapeutic development. The ideal profile for neuroprotective agents might involve maximizing beneficial non-genomic signaling while minimizing potentially harmful genomic effects, particularly in reproductive tissues [1].
Selective Estrogen Receptor Modulators (SERMs) and estrogen derivatives that preferentially activate neuroprotective signaling pathways with reduced feminizing or proliferative effects represent promising approaches [1]. Additionally, administration route significantly influences therapeutic efficacy, with transdermal estradiol bypassing hepatic metabolism and achieving more favorable E2:E1 ratios compared to oral formulations [8].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Investigating Estradiol Signaling
| Reagent/Category | Specific Examples | Research Applications | Mechanistic Insight |
|---|---|---|---|
| ER Agonists | 17β-estradiol (E2), PPT (ERα-specific), DPN (ERβ-specific) | Receptor-specific activation, pathway mapping | Distinguish ERα vs. ERβ mediated effects |
| ER Antagonists | ICI 182,780 (Faslodex), Tamoxifen, MPP (ERα-specific) | Receptor necessity, pathway blockade | Differentiate ER-dependent vs independent effects |
| Signaling Inhibitors | PD 98059 (MEK inhibitor), LY294002 (PI3K inhibitor), PP2 (Src inhibitor) | Pathway dissection, cross-talk analysis | Establish specific pathway contributions |
| Gene Expression Tools | siRNA/shRNA (ER knockdown), CRISPR/Cas9 (ER knockout) | Functional receptor studies | Determine necessity of specific receptors |
| Detection Reagents | Phospho-specific antibodies, ER subtype antibodies, calcium indicators | Pathway activation, localization studies | Visualize and quantify signaling events |
| Experimental Models | OVX rodents, ER knockout mice, neuronal cell cultures | In vivo and in vitro functional studies | Translate mechanistic insights to functional outcomes |
The mechanisms of estradiol action in the brain encompass both genomic and non-genomic signaling pathways that operate in a highly integrated manner to regulate neuronal function, plasticity, and survival. The genomic pathway mediates longer-term adaptive responses through regulation of gene expression, while non-genomic signaling enables rapid modulation of neuronal excitability and function. Extensive cross-talk between these pathways, combined with interactions with neurotrophic signaling systems, creates a complex regulatory network through which estradiol influences cognitive performance and neuroprotection.
Understanding the distinct yet interconnected nature of these signaling mechanisms provides critical insights for developing targeted therapeutic approaches for cognitive decline associated with estrogen deficiency during menopause and in neurodegenerative diseases. Future research focusing on tissue-specific and pathway-selective estrogenic compounds holds promise for maximizing cognitive benefits while minimizing potential risks associated with broader estrogen receptor activation.
The intricate modulation of cognitive performance by estradiol is fundamentally rooted in the precise neuroanatomical distribution and signaling dynamics of its receptors, estrogen receptor alpha (ERα) and estrogen receptor beta (ERβ). These receptors are not uniformly distributed throughout the brain; instead, they exhibit region-specific expression patterns within hippocampal and prefrontal circuits that are critical for learning, memory, and executive function [10]. The differential localization of ER subtypes creates distinct signaling microenvironments that influence synaptic plasticity, neurogenesis, and neurotransmitter systems essential for cognitive processing [11] [12]. Understanding this precise receptor mapping provides a crucial foundation for deciphering estrogen's complex effects on cognitive performance and for developing targeted therapeutic interventions for cognitive disorders. This review synthesizes current evidence on ERα and ERβ distribution within cognitive circuits, examining their distinct roles, signaling mechanisms, and implications for maintaining brain health across the lifespan.
Regional Distribution Patterns of ERα and ERβ
Hippocampal Complex Distribution
The hippocampus, a structure vital for memory formation and spatial navigation, demonstrates a complex and dynamic expression of both estrogen receptors throughout development and adulthood. During human hippocampal development, both ERα and ERβ are expressed from mid-gestation (around 15-17 gestational weeks) through adulthood, with prominent expression in pyramidal cells of Ammon's horn and the dentate gyrus [11]. A seminal study on human postmortem tissue revealed that ERα expression is detectable in the cortical plate as early as 9 gestational weeks, with intensity decreasing during prenatal development but increasing again from birth to adulthood [11]. In contrast, ERβ appears later around 15 gestational weeks but persists widely throughout the adult cortex [11].
In the adult brain, ERβ demonstrates higher protein expression levels in the cerebral cortex and hippocampus compared to ERα, as confirmed by Western blot analyses [11]. This relative abundance suggests potentially different functional roles for these receptor subtypes in cognitive processing. Ultrastructural studies in rat models have further revealed that hippocampal estrogen receptors are strategically localized at both nuclear and extranuclear sites, including dendritic spines and presynaptic terminals, enabling them to rapidly influence synaptic transmission and plasticity [12].
Table 1: Developmental Expression Patterns of ERα and ERβ in Human Hippocampus and Cortex
| Developmental Period | ERα Expression | ERβ Expression | Primary Locations |
|---|---|---|---|
| Early Prenatal (9 GW) | High | Not detected | Proliferating zones, cortical plate |
| Mid-Prenatal (15-17 GW) | Decreasing | Emerging | Cortical plate, proliferating zones |
| Late Prenatal | Low | Increasing | Widespread cortical layers |
| Adulthood | Increased | High, widespread | Cortical layers II-VI, hippocampal pyramidal cells |
GW = Gestational Weeks
Prefrontal Cortex Distribution
The prefrontal cortex (PFC), which governs executive functions including working memory, decision-making, and cognitive flexibility, exhibits a distinct ER expression profile. Immunohistochemical analyses demonstrate that ERβ is widely distributed throughout cortical layers II-VI in the adult human brain, while ERα shows more restricted expression [11]. This extensive ERβ distribution in the PFC positions it to significantly influence higher-order cognitive processes.
Notably, ER density in the frontal cortex appears dynamically regulated by hormonal status, with evidence suggesting increased ER density in the frontal cortex after menopause, possibly representing a compensatory mechanism following estrogen decline [8]. This adaptive response highlights the plasticity of ER expression in response to hormonal changes and may contribute to the varied cognitive responses to hormone therapy observed at different menopausal stages.
Subcellular Localization and Implications
The subcellular compartmentalization of estrogen receptors critically determines their functional roles in neuronal signaling. Ultrastructural evidence has revealed that a significant population of ERα in hippocampal neurons is located at extranuclear sites, including dendritic spines, axon terminals, and mitochondrial membranes [12]. This strategic positioning enables estradiol to rapidly modulate synaptic transmission and intracellular signaling cascades without requiring genomic activation.
The presence of ERα at presynaptic terminals suggests presynaptic regulatory mechanisms, while postsynaptic localization positions estrogen receptors to directly influence postsynaptic density signaling and dendritic spine morphology [12]. These findings collectively support an expanded model of estrogen signaling that integrates both rapid membrane-initiated events and longer-term genomic regulation to fine-tune neuronal function in cognitive circuits.
Diagram 1: Dual Signaling Mechanisms of Estrogen Receptors in Cognitive Circuits. Estradiol activates both genomic (nuclear) and rapid (extranuclear) signaling pathways through ERα and ERβ to enhance synaptic plasticity and cognitive function.
Functional Implications for Cognitive Performance
Receptor-Specific Roles in Cognitive Domains
The distinct distribution patterns of ERα and ERβ enable these receptor subtypes to differentially regulate specific cognitive domains through their unique influences on hippocampal and prefrontal circuitry. Research indicates that ERβ activation appears particularly important for certain types of memory processing, as demonstrated by studies showing that ERβ agonism enhances extinction memory recall for heroin-conditioned cues in a sex-specific manner, with females showing greater sensitivity to ERβ modulation in the basolateral amygdala [13].
The preferential localization of ERβ in cortical layers II-VI positions it to integrate information across multiple cortical processing streams, potentially influencing cognitive flexibility and executive control [11]. In contrast, ERα's prominent expression in hippocampal pyramidal cells and its role in regulating spine density suggest a more specialized function in spatial memory and consolidation processes. This functional dissociation is further supported by observations that earlier age at menopause, which results in premature estrogen decline, is significantly associated with lower scores across multiple cognitive domains, including episodic memory, prospective memory, and executive functions [8].
Hormonal Therapy and Cognitive Outcomes
The timing, route of administration, and receptor specificity of estrogen-based interventions significantly influence their cognitive outcomes, reflecting the complex interplay between ER distribution and hormonal status. Clinical evidence indicates that transdermal estradiol preparations are associated with higher episodic memory scores, while oral estradiol is linked to better prospective memory performance [8]. This differential effect likely reflects variations in receptor activation patterns influenced by first-pass metabolism and the distinct E2:E1 ratios achieved through different administration routes.
The "critical window" hypothesis proposes that optimal cognitive benefits from estrogen therapy occur when initiated near menopause onset, before age-related brain changes become established [9]. This temporal sensitivity may reflect the dynamic nature of ER expression and the capacity for synaptic reorganization in response to estrogen fluctuations. Supporting this concept, studies show that hormone therapy started within approximately two years of oophorectomy is associated with better episodic memory, working memory, and visuospatial processing in later life [9].
Table 2: Cognitive Domain Sensitivity to Estrogen Receptor Modulation
| Cognitive Domain | Primary Neural Substrate | ER Subtype Involvement | Therapeutic Response |
|---|---|---|---|
| Episodic Memory | Hippocampus, Medial Temporal Lobe | ERα (hippocampal), ERβ (cortical) | Transdermal E2 beneficial |
| Executive Function | Prefrontal Cortex | ERβ (predominant in PFC) | Limited MHT response |
| Prospective Memory | Frontal & Medial Temporal Lobes | ERβ, possibly ERα | Oral E2 beneficial |
| Working Memory | Prefrontal Cortex, Hippocampus | Both ERα and ERβ | Hormone therapy post-oophorectomy beneficial |
Experimental Models and Methodological Approaches
Protocol: ER Distribution Mapping in Human Brain Development
Understanding the methodological approaches for mapping estrogen receptors provides critical context for interpreting distribution data and designing future studies.
Tissue Preparation and Sectioning:
- Obtain human brain specimens from gestational weeks 9 through adulthood, with postmortem intervals under 12 hours
- Fix tissue in 4% paraformaldehyde in 0.1 M phosphate buffer (pH 7.4) for 24-48 hours
- Cryoprotect in 30% sucrose solution until sinking
- Section coronally at 40μm thickness using a freezing microtome
- Collect serial sections systematically throughout hippocampal and prefrontal regions
Immunohistochemistry Protocol:
- Perform antigen retrieval with citrate buffer (pH 6.0) at 80°C for 30 minutes
- Block endogenous peroxidases with 3% H₂O₂ in methanol for 15 minutes
- Incubate with blocking solution (10% normal goat serum, 0.3% Triton X-100) for 2 hours
- Apply primary antibodies: Mouse anti-ERα (1:1000) and Rabbit anti-ERβ (1:2000) in blocking solution for 48 hours at 4°C
- Incubate with biotinylated secondary antibodies (1:500) for 2 hours at room temperature
- Process with ABC elite kit for 90 minutes followed by DAB peroxidase substrate
- Counterstain with thionin, dehydrate, clear, and coverslip
Quantification and Analysis:
- Use stereological counting methods with systematic random sampling
- Employ optical fractionator for unbiased cell counting
- Determine staining intensity via densitometry with image analysis software
- Conduct double immunofluorescence with confocal microscopy for subcellular localization [11]
Protocol: Ovariectomy and Estradiol Replacement in Rodent Models
The ovariectomized (OVX) rat model represents a cornerstone experimental approach for investigating estrogen deficiency and replacement effects on cognitive function and neural mechanisms.
Surgical Procedure:
- Anesthetize female albino rats (150-180g) with ketamine/xylazine (80/10 mg/kg, i.p.)
- Make bilateral dorsal incisions parallel to the spinal column
- Isolate and excise ovaries following vessel cauterization
- For sham operations: expose ovaries without removal
- Administer postoperative analgesia for 72 hours
Estradiol Replacement Protocol:
- For OVX+E2 group: administer 17β-estradiol subcutaneously (1-5 μg/day) dissolved in sesame oil
- For control groups: administer vehicle alone
- Treatment duration typically 4-8 weeks postsurgery
Cognitive and Molecular Assessments:
- Spatial learning and memory testing using Morris Water Maze (4 trials/day for 5 days)
- Neurotransmitter analysis via HPLC in hippocampal and prefrontal tissue
- Serum estradiol, nerve growth factor (NGF), and amyloid precursor protein measurements by ELISA
- Gene expression analysis of Cx43, LRP1, and RAGE using RT-PCR
- Synaptic density evaluation via Postsynaptic Density Protein 95 (PSD-95) immunohistochemistry [7]
Diagram 2: Experimental Workflow for Ovariectomy and Estradiol Replacement Studies. This rodent model examines the effects of estrogen deficiency and replacement on cognitive function and underlying neural mechanisms.
Molecular Signaling Pathways in Cognitive Circuits
Genomic and Non-Genomic Signaling Mechanisms
Estrogen receptors regulate cognitive function through diverse molecular pathways that can be broadly categorized into genomic and non-genomic signaling mechanisms. Genomic signaling involves ER dimerization, binding to estrogen response elements (EREs) in target gene promoters, and recruitment of coregulator complexes to modulate transcription of genes involved in synaptic plasticity, neuroprotection, and metabolism [10]. This classical mechanism underlies many of estrogen's longer-term effects on neuronal structure and function.
In parallel, non-genomic signaling occurs rapidly through membrane-associated ERs that activate intracellular kinase cascades, including MAPK/ERK, PI3K/Akt, and PKC pathways [10]. These rapid signaling events can modulate ion channel activity, neurotransmitter release, and dendritic spine dynamics within minutes, providing a mechanism for estradiol to immediately influence neuronal excitability and synaptic transmission. The integration of these complementary signaling modes allows for precise spatiotemporal control of estrogen actions in hippocampal and prefrontal circuits supporting cognitive function.
Receptor-Specific Signaling and Cross-Talk
ERα and ERβ exhibit both overlapping and distinct signaling properties that contribute to their specialized functions in cognitive circuits. While both receptors can activate common pathways, they also display preferential signaling biases; for instance, ERβ shows particularly strong interactions with metabotropic glutamate receptor signaling and enhances BDNF/CREB pathways implicated in synaptic plasticity and memory consolidation [14]. Additionally, ER signaling exhibits extensive cross-talk with other receptor systems, including dopamine, serotonin, and glutamate receptors, enabling estradiol to fine-tune diverse neurotransmitter systems essential for cognitive performance [10].
The relative balance between ERα and ERβ signaling appears crucial for optimal cognitive function, with evidence suggesting that disruption of this balance contributes to neuropsychiatric symptoms in conditions like polycystic ovary syndrome (PCOS), where reduced ERβ activity relative to ERα dominance has been proposed as a mechanism underlying cognitive and affective disturbances [14]. This receptor interplay represents a promising target for developing selective estrogen receptor modulators with improved therapeutic profiles for cognitive disorders.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Estrogen Receptor Research in Cognitive Circuits
| Reagent/Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| ER Agonists | 17β-estradiol (endogenous), DPN (ERβ-selective) | Receptor-specific activation, cognitive behavioral studies | DPN: 1.0 mg/kg SC for systemic administration; 10 pg IC for BLA infusions |
| ER Antagonists | ICI 182,780 (general ER), PHTPP (ERβ-selective) | Receptor mechanism studies, pathway blockade | Specificity varies; validate with multiple antagonists |
| Antibodies | Mouse anti-ERα, Rabbit anti-ERβ | IHC, Western blot, cellular localization | Challenge with antibody specificity; use multiple validation methods |
| Animal Models | Ovariectomized rats, ER knockout mice | Hormone depletion studies, receptor-specific functions | Consider compensatory mechanisms in knockout models |
| Behavioral Assays | Morris Water Maze, cue-induced reinstatement | Spatial memory, extinction memory recall | Test multiple cognitive domains for comprehensive assessment |
The precise distribution of ERα and ERβ within hippocampal and prefrontal circuits creates a sophisticated regulatory network through which estradiol modulates cognitive performance. The distinct spatial-temporal expression patterns of these receptor subtypes during development and their dynamic regulation throughout the lifespan enable complex cognitive processing while also creating vulnerabilities to hormonal fluctuations. Future research should prioritize the development of more selective pharmacological tools to target specific ER populations in defined brain regions, ultimately enabling more precise therapeutic interventions for cognitive disorders associated with estrogen signaling deficits. The integration of human neuroimaging with molecular approaches in animal models will be essential for translating these fundamental discoveries into clinical applications that preserve and enhance cognitive function across the lifespan, particularly in populations experiencing hormonal transitions.
Estradiol (17β-estradiol), the most bioactive endogenous estrogen, exerts profound influences on the structure and function of the hippocampus, a brain region critical for learning, memory, and stress regulation [15] [16]. This whitepaper synthesizes current research on the mechanisms by which estradiol modulates hippocampal plasticity, focusing on synaptic formation, dendritic spine dynamics, and neuroprotective pathways. Understanding these hormonal mechanisms is paramount for developing targeted therapies for cognitive aging and neurodegenerative disorders, which display significant sex differences in prevalence and progression [15] [7]. The evidence underscores that estradiol operates through genomic, non-genomic, and neurosteroid pathways to maintain cognitive function, with implications for drug development in conditions involving hippocampal dysfunction [16].
Molecular Mechanisms of Estradiol Action
Estradiol signals through multiple receptor systems to orchestrate its effects on hippocampal plasticity. The classic genomic actions involve estrogen receptor alpha (ERα) and estrogen receptor beta (ERβ), which are ligand-dependent transcription factors found in the nucleus and at extranuclear sites within hippocampal neurons [15] [16]. Upon binding, these receptors dimerize and translocate to the nucleus, where they bind to estrogen response elements (EREs) on DNA, initiating gene transcription and protein synthesis that underlie long-lasting structural changes [16]. Additionally, the G protein-coupled estrogen receptor 1 (GPER1) mediates rapid, non-genomic signaling cascades [15].
Table: Estrogen Receptors in the Hippocampus
| Receptor Type | Primary Location | Signaling Mechanism | Key Functions in Hippocampus |
|---|---|---|---|
| ERα | Nucleus, Dendrites [15] | Genomic (slow, sustained) [16] | Modulates spine density; influences neurogenesis [15] |
| ERβ | Nucleus, Dendrites [15] | Genomic (slow, sustained) [16] | Contributes to neuroprotection and synaptic plasticity [15] |
| GPER1 | Plasma Membrane [15] | Non-genomic (rapid) [16] | Activates intracellular signaling pathways (e.g., MAPK) [16] |
A more recent paradigm highlights estradiol's role as a neurosteroid, synthesized de novo from cholesterol within hippocampal neurons themselves [16]. This local synthesis allows for rapid modulation of synaptic function and memory consolidation independent of peripheral hormone levels [16]. The signaling pathways activated by estradiol receptor binding, particularly the MAPK and PI3K pathways, are crucial for downstream effects on neuronal growth, survival, and structural plasticity [17].
Figure 1: Estradiol Signaling Pathways in Hippocampal Plasticity. Estradiol (E2) acts via classical genomic signaling through nuclear ERα and ERβ to regulate gene transcription, and via rapid non-genomic signaling through membrane-associated GPER1 to activate kinase pathways. E2 can also be synthesized locally in the hippocampus, acting as a neurosteroid to modulate synaptic function and memory [15] [16].
Structural Plasticity: Dendritic Spines and Synaptic Formation
Dendritic spines are the primary sites of excitatory synaptic input in the hippocampus, and their density and morphology are robustly modulated by estradiol. Fluctuations in circulating estradiol across the estrous cycle in rodents cause dynamic changes in apical CA1 dendritic spine density, with the highest densities (approximately 30% higher) coinciding with phases of high estradiol [15]. Ovariectomy (OVX), which removes the primary source of estrogens, decreases spine density, a effect that can be reversed by exogenous estradiol administration [15] [18].
Table 1: Quantitative Effects of Estradiol on Dendritic Spine Density
| Experimental Model | Intervention | Hippocampal Region | Effect on Spine Density | Citation |
|---|---|---|---|---|
| Ovariectomized (OVX) Rats | Estradiol Benzoate | CA1 | Increased density, peaking at 2-3 days post-treatment [15] | [15] |
| Dissociated Hippocampal Cultures | 17β-estradiol | Pyramidal Neurons | ~2-fold increase in density [18] | [18] |
| Female Rats Across Estrous Cycle | Natural fluctuation | CA1 | ~30% higher density at proestrus (high E2) vs. low E2 phases [15] | [15] |
The mechanism involves estradiol-mediated decrease in inhibitory tone from GABAergic interneurons, leading to a shift toward enhanced excitation in pyramidal neurons [18]. This excitation drives the activation of cyclic AMP response element binding protein (CREB) phosphorylation, a critical step for the formation of novel dendritic spines [18]. Subsequent to spine formation, estradiol increases the density of glutamatergic receptors and enhances synaptic network activity [18]. The shape of spines is also functionally significant, with estradiol promoting the formation of mature "mushroom" spines, which are stable and support memory, and thin "learning" spines, which are more plastic [15].
Functional Correlates: Cognitive Performance and Neuroprotection
The structural changes induced by estradiol have direct functional consequences for hippocampal-dependent cognition and neuronal resilience.
Cognitive Performance Across the Lifespan
Estradiol modulates various cognitive domains, particularly memory. In animal models, estradiol enhances performance on spatial learning and memory tasks, such as the Morris water maze [7]. In humans, the "critical window" or "timing" hypothesis proposes that estradiol replacement is most beneficial for cognition when initiated close to the time of menopause. Recent large-scale observational studies provide supporting evidence:
- Menopause Age: Earlier age at menopause is associated with lower performance in episodic memory, prospective memory, and executive functions [8] [19].
- Hormone Therapy (HT) Route: The administration route of estradiol-based HT affects different cognitive domains. Transdermal estradiol is associated with higher episodic memory scores, while oral estradiol is linked to better prospective memory [8] [19]. This is potentially because oral estradiol undergoes first-pass hepatic metabolism, converting it to less potent estrone [8].
- Surgical Menopause: Oophorectomy prior to natural menopause is linked to cognitive risk, which can be mitigated by HT initiated around the time of surgery [9].
Table 2: Association of Estradiol-Based Hormone Therapy with Cognitive Domains in Postmenopausal Women
| Cognitive Domain | Key Brain Region | Association with Transdermal E2 | Association with Oral E2 | Evidence Class |
|---|---|---|---|---|
| Episodic Memory | Medial-temporal lobes [8] | Significantly higher scores [8] [19] | Not significant | Class III [8] |
| Prospective Memory | Frontal & Medial-temporal lobes [8] | Not significant | Significantly higher scores [8] [19] | Class III [8] |
| Executive Functions | Frontal lobes [8] | Not significant | Not significant | Class III [8] |
Furthermore, estradiol modulates reward-based learning by influencing dopaminergic signaling in the nucleus accumbens, a region interconnected with the hippocampus. Elevated endogenous estradiol predicts enhanced reward prediction errors and reinforcement learning, linked to reduced expression of dopamine reuptake transporters [20].
Neuroprotective Mechanisms
Estradiol confers neuroprotection through multiple interconnected pathways, countering processes that lead to cognitive decline and neurodegeneration.
- Synaptic Health: Estradiol upregulates key synaptic proteins like Postsynaptic Density Protein 95 (PSD-95), which is crucial for synaptic stability and function. Its deficiency, as in OVX models, leads to reduced PSD-95 and impaired cognition [7].
- Amyloid-β (Aβ) Clearance: Estradiol modulates proteins involved in Aβ trafficking across the blood-brain barrier (BBB). It upregulates Lipoprotein receptor-related protein 1 (LRP1), which facilitates Aβ clearance from the brain, and downregulates the receptor for advanced glycation end products (RAGE), which mediates Aβ influx into the brain [7].
- Neuroinflammation and Neurotrophic Support: Estradiol deficiency increases pro-inflammatory signaling, which is ameliorated by replacement. It also maintains levels of neurotrophic factors like Nerve Growth Factor (NGF), supporting neuronal survival [7].
- Cellular Communication: Estradiol increases the expression of the gap junction protein connexin-43 (Cx43), thereby enhancing intercellular communication and potentially supporting metabolic coupling and neuronal health [7].
Figure 2: Neuroprotective Mechanisms of Estradiol and Consequences of its Deficiency. Estradiol deficiency leads to a cascade of detrimental events in the hippocampus, including synaptic instability, impaired amyloid-β clearance, neuroinflammation, reduced neurotrophic support, and disrupted cellular communication, collectively increasing the risk for cognitive decline and neurodegeneration [7].
Experimental Models and Methodologies
Research on estradiol and hippocampal plasticity relies on well-established in vivo and in vitro models.
Key Experimental Protocols
Protocol 1: Ovariectomized (OVX) Rat Model of Menopause [7]
- Purpose: To investigate the effects of estradiol deficiency and replacement on cognitive function and molecular markers.
- Procedure:
- Surgery: Female rats undergo bilateral ovariectomy or a sham operation under anesthesia.
- Recovery & Grouping: Animals are allowed to recover and are then divided into groups (e.g., OVX, OVX + 17β-estradiol treatment, sham control).
- Treatment: 17β-estradiol is administered via subcutaneous injection or other routes for a specified period.
- Cognitive Testing: Spatial learning and memory are assessed using the Morris Water Maze. Rats are trained to find a hidden platform, and metrics like escape latency and time spent in the target quadrant are measured.
- Tissue Collection: Hippocampal tissue and serum are collected for molecular analysis.
- Downstream Analysis:
- ELISA: To quantify serum estrogen, NGF, Aβ, and PSD-95 levels.
- RT-PCR: To measure gene expression of Cx43, LRP1, and RAGE.
- HPLC: To analyze neurotransmitter levels (e.g., acetylcholine, monoamines).
Protocol 2: Primary Hippocampal Neuronal Culture & Dendritic Spine Analysis [18]
- Purpose: To directly visualize and quantify the rapid effects of estradiol on dendritic spine formation and morphology.
- Procedure:
- Cell Culture: Hippocampal pyramidal neurons are dissociated from rat embryos and cultured on poly-D-lysine-coated coverslips.
- Treatment: Cultures are treated with 17β-estradiol (e.g., 10 nM) for 24-48 hours. Controls receive vehicle.
- Pharmacological Blockade: To probe mechanisms, cultures can be co-treated with antagonists (e.g., NMDA receptor blockers, ER antagonists) or inhibitors of signaling pathways (e.g., MAPK inhibitors).
- Immunocytochemistry: Neurons are fixed and stained for spine visualization (e.g., using DiI or GFP-actin) and synaptic markers (e.g., synapsin I, PSD-95).
- Downstream Analysis:
- Confocal Microscopy: High-resolution imaging of dendritic segments.
- Image Analysis: Using software to quantify spine density, spine type classification (thin, stubby, mushroom), and synaptic puncta density.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating Estradiol's Role in Hippocampal Plasticity
| Reagent / Material | Function / Application | Example Use in Research |
|---|---|---|
| 17β-estradiol | The most potent endogenous estrogen; used for replacement studies. | Administered to OVX rodents or added to neuronal cultures to restore estrogenic signaling [7]. |
| OVX Rodent Model | A model for surgical menopause, inducing a state of estradiol deficiency. | Used to study the consequences of estrogen loss and efficacy of replacement therapies [15] [7]. |
| Morris Water Maze | A behavioral apparatus to assess spatial learning and memory. | Tests cognitive function in rodents after OVX and estradiol replacement [7]. |
| ER-specific Agonists/Antagonists | Compounds that selectively activate or block ERα or ERβ. | Used to dissect the specific receptor mediating estradiol's effects in vitro and in vivo [15]. |
| Primary Hippocampal Neuronal Cultures | In vitro system for mechanistic studies. | Allows direct observation of estradiol's effects on spine density and synaptogenesis [18]. |
| Antibodies for PSD-95, Synapsin I | Markers for postsynaptic and presynaptic structures, respectively. | Used in immunohistochemistry or Western blot to quantify synaptic changes [18] [7]. |
| ELISA Kits for NGF, Aβ, PSD-95 | Quantify protein levels in tissue homogenates or serum. | Measures biochemical correlates of neuroprotection and synaptic integrity [7]. |
Estradiol is a pivotal regulator of hippocampal plasticity, exerting its effects through a sophisticated interplay of genomic, non-genomic, and neurosteroid mechanisms. It directly promotes structural changes by increasing dendritic spine density and synaptogenesis, while concurrently enabling functional enhancements in learning, memory, and reinforcement learning. Furthermore, its broad neuroprotective actions safeguard against processes linked to neurodegenerative diseases. Future research and drug development must account for critical variables such as the "critical window" for intervention, the route of administration, and individual risk factors like APOE ε4 status to translate these mechanistic insights into effective, personalized therapies for cognitive decline [8] [19] [9].
Estradiol, the most potent endogenous estrogen, exerts profound neuromodulatory effects critical for cognitive function by interacting with the cholinergic and serotonergic systems. This review synthesizes evidence from preclinical and clinical studies demonstrating that estradiol regulates key neurobiological substrates for learning, memory, and affective processing. Through genomic and non-genomic mechanisms, estradiol enhances cholinergic function in the basal forebrain and modulates serotonergic signaling via regulation of synthesis, transport, and receptor expression. The clinical implications of these interactions are explored, including the differential cognitive effects of hormone therapy formulations and the potential for targeted interventions in cognitive aging and neuropsychiatric conditions. Understanding these complex neurotransmitter interactions provides a foundation for developing precision medicine approaches to maintain brain health in aging women.
Estradiol's role in the brain extends far beyond reproductive functions to encompass complex modulation of neurotransmitter systems integral to cognitive processes. The cholinergic system, particularly vulnerable in age-related cognitive decline and Alzheimer's disease, and the serotonergic system, implicated in mood and affective components of cognition, represent two critical targets of estradiol action. This review examines the mechanistic basis for estradiol's interactions with these systems and their collective impact on cognitive performance within the context of hormonal influences on brain health across the lifespan. Understanding these interactions provides crucial insights for developing hormone-based strategies to support cognitive function during reproductive transitions and in later life.
Estradiol-Mediated Modulation of the Cholinergic System
Neurobiological Foundations
The basal forebrain cholinergic system serves as a primary regulator of attention, learning, and memory formation—cognitive domains that display significant sensitivity to estradiol status. Extensive research demonstrates that basal forebrain cholinergic neurons depend on estradiol support for adequate functioning [21] [22]. Estradiol modulates cholinergic neurotransmission through multiple mechanisms, including regulation of:
- High-affinity choline uptake
- Choline acetyltransferase (ChAT) activity and mRNA expression
- Nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF) expression
- Acetylcholine release and receptor dynamics
Table 1: Estradiol Effects on Cholinergic Markers in Preclinical Models
| Cholinergic Marker | Effect of Estradiol | Brain Region | Functional consequence |
|---|---|---|---|
| Choline acetyltransferase (ChAT) | Increases activity & mRNA expression | Basal forebrain, hippocampus | Enhanced acetylcholine synthesis |
| High-affinity choline uptake | Upregulates | Cortex, hippocampus | Increased acetylcholine production |
| Nerve growth factor (NGF) | Increases expression | Basal forebrain | Enhanced cholinergic neuron survival |
| Acetylcholine release | Potentiates | Hippocampus, cortex | Improved synaptic transmission |
Molecular Mechanisms
Estradiol exerts both genomic and non-genomic effects on cholinergic function. Genomic actions involve classical estrogen receptor (ERα and ERβ) binding to estrogen response elements (EREs) in cholinergic gene promoters, modulating transcriptional activity over hours to days. Non-genomic mechanisms include rapid activation of kinase signaling pathways (MAPK, PI3K) within minutes, influencing cholinergic neurotransmission and synaptic plasticity. These mechanisms collectively enhance cholinergic function, particularly in brain regions critical for cognition such as the basal forebrain, hippocampus, and prefrontal cortex [21] [22].
The trophic effects of estradiol on cholinergic neurons are particularly relevant to cognitive aging. Loss of p75 neurotrophin receptors (p75NTR) on basal forebrain cholinergic neurons—receptors modulated by estrogen—is associated with early cognitive dysfunction even without evidence of cellular loss [21]. This suggests estradiol plays a permissive role in maintaining cholinergic signaling integrity during aging.
Functional Consequences for Cognition
Estradiol-cholinergic interactions manifest behaviorally in multiple cognitive domains:
- Attentional processes: Partitioning of attentional resources and performance on effort-demanding tasks
- Working memory: Maintenance and manipulation of information over short intervals
- Episodic memory: Formation and retrieval of contextual memories
- Executive function: Inhibition of irrelevant information and cognitive flexibility
Cholinergic antagonism studies in humans demonstrate that estradiol enhances cholinergic-mediated cognitive performance, with estradiol administration attenuating scopolamine-induced deficits in verbal learning, memory, and attention in postmenopausal women [22]. Functional neuroimaging reveals that these behavioral improvements correlate with normalized brain activation patterns in prefrontal and parietal regions during working memory tasks, providing neural correlates for estradiol-cholinergic interactions.
Diagram 1: Estradiol signaling pathways in cholinergic neurons. Estradiol acts through genomic and non-genomic mechanisms to enhance cholinergic function.
Estradiol Regulation of Serotonergic Signaling
Genomic Regulation of Serotonergic Genes
Estradiol exerts sophisticated control over the serotonergic system through coordinated regulation of genes encoding synthetic enzymes, receptors, and transporters. The molecular mechanisms involve both classical estrogen receptor binding to estrogen response elements (EREs) and transcriptional cross-talk through protein-protein interactions with other transcription factors [23].
Table 2: Estradiol Regulation of Serotonergic Gene Expression
| Gene Target | Regulation by Estradiol | Mechanism | Functional Outcome |
|---|---|---|---|
| Tryptophan hydroxylase-2 (TPH2) | Increased expression | ER binding to ERE in promoter | Enhanced serotonin synthesis |
| Serotonin transporter (SERT) | Increased expression | ER binding to ERE in promoter | Increased serotonin reuptake |
| Serotonin-1A receptor (5-HT1A) | Decreased expression | ER tethering to Sp1, C/EBPβ | Altered autoreceptor function |
| Monoamine oxidase A (MAO-A) | Decreased expression | ER tethering to AP-1, Sp1 | Reduced serotonin degradation |
| Monoamine oxidase B (MAO-B) | Decreased expression | ER binding to ERE in promoter | Reduced serotonin degradation |
The net effect of these coordinated genomic actions is enhanced serotonergic neurotransmission, which may underlie estradiol's mood-stabilizing and antidepressant effects observed in clinical populations [23]. This is particularly relevant during periods of hormonal fluctuation such as the menopausal transition, when declining estradiol levels may contribute to increased vulnerability to depressive symptoms.
Receptor-Specific Mechanisms
Estradiol signals through two nuclear estrogen receptors (ERα and ERβ) and the membrane-associated G protein-coupled estrogen receptor (GPER1), with receptor distribution and relative abundance influencing serotonergic modulation. ERβ appears particularly important for serotonergic regulation, with high expression in raphe nuclei and limbic regions involved in mood regulation. Additionally, estradiol-induced activation of intracellular signaling pathways (Src/MAPK, PI3K/AKT) modulates serotonin receptor sensitivity and downstream signaling efficacy, providing mechanisms for rapid serotonergic modulation independent of genomic effects [23] [24].
Implications for Affective Cognition
The serotonergic system plays a well-established role in mood regulation, with estradiol's serotonergic effects manifesting in several cognitive-affective domains:
- Emotional memory processing
- Affective bias in decision-making
- Stress responsiveness
- Reward processing
The higher prevalence of depression in women, particularly during periods of hormonal transition (puberty, postpartum, perimenopause), underscores the clinical relevance of estradiol-serotonergic interactions [23]. These periods represent "windows of vulnerability" where serotonergic stability is compromised by fluctuating hormone environments.
Diagram 2: Estradiol regulation of serotonergic gene expression. Estradiol modulates multiple components of serotonin signaling through genomic and non-genomic mechanisms.
Integrative Cognitive Outcomes and Clinical Evidence
Synergistic Effects on Cognitive Domains
The convergent modulation of cholinergic and serotonergic systems by estradiol produces integrated effects on cognitive function that extend beyond the contributions of either system alone. The cholinergic system primarily supports effortful cognitive processes—sustained attention, working memory maintenance, and explicit memory encoding—while the serotonergic system influences affective bias, emotional memory, and cognitive flexibility. Estradiol's simultaneous enhancement of cholinergic function and modulation of serotonergic signaling creates an optimal neurochemical environment for complex cognitive operations requiring integration of cognitive and affective information [21] [23] [24].
Clinical Studies and Hormone Therapy Considerations
Recent clinical evidence demonstrates that the cognitive effects of estradiol-based hormone therapy are domain-specific and formulation-dependent. A large cross-sectional study of 7,251 postmenopausal women from the Canadian Longitudinal Study on Aging found that earlier age at menopause was associated with lower performance across all cognitive domains, highlighting the importance of hormonal timing [25] [26]. Crucially, the study revealed differential cognitive effects based on administration route:
- Transdermal estradiol was associated with better episodic memory (remembering past experiences) compared to no hormone therapy
- Oral estradiol was associated with better prospective memory (remembering to perform future tasks) compared to no hormone therapy
- Neither administration route significantly affected executive functions
These findings underscore that estradiol formulation matters for cognitive outcomes and suggest that first-pass hepatic metabolism of oral estradiol may influence its neurocognitive effects through alterations in bioactive metabolites or protein binding [25] [26].
Individual Difference Factors
The cognitive response to estradiol is modulated by several individual difference factors:
- APOE genotype: APOE ε4 carriers show enhanced sensitivity to both the beneficial effects of estradiol and the cognitive risks associated with early menopause
- Reproductive history: Parity influences cognitive outcomes, with the association between earlier menopause and executive function particularly pronounced in women with four or more children
- Timing of intervention: The "critical period" hypothesis suggests earlier initiation of hormone therapy following menopause produces more favorable cognitive outcomes
These moderating variables highlight the need for personalized approaches when considering estradiol-based interventions for cognitive support.
Experimental Approaches and Research Methods
Cholinergic-Estradiol Interaction Protocols
Investigation of estradiol-cholinergic interactions in humans has employed sophisticated pharmacological challenge designs:
Diagram 3: Experimental design for estradiol-cholinergic interaction studies. This pharmacological fMRI approach examines how estradiol modulates brain response to cholinergic challenge.
Protocol Details:
- Participants: Carefully screened postmenopausal women, typically within early postmenopausal window (3-6 years since final menstrual period)
- Estradiol administration: Transdermal estradiol (100μg/day) or oral estradiol (1-2mg/day) for 2-3 months to achieve stable physiological levels
- Cholinergic challenge: Acute administration of scopolamine (muscarinic antagonist) or mecamylamine (nicotinic antagonist) at standardized doses
- Assessment: Cognitive testing focusing on attention, working memory, and episodic memory domains; functional MRI during working memory tasks (n-back, delayed match-to-sample)
- Controls: Placebo-controlled, crossover designs where participants receive both active drug and placebo in counterbalanced order
This approach allows researchers to determine how estradiol pretreatment modulates behavioral and neural responses to cholinergic disruption, providing a window into estradiol-cholinergic interactions [21] [22].
Serotonergic-Estradiol Research Methods
Investigation of estradiol's serotonergic effects employs complementary approaches:
- Molecular studies: Reporter assays, chromatin immunoprecipitation, and promoter analysis to map ER binding sites on serotonergic genes
- Neurochemical measures: Microdialysis in raphe nuclei and terminal regions to measure serotonin release and turnover
- Receptor imaging: PET imaging with 5-HT1A and 5-HT2A ligands to quantify receptor availability
- Genetic approaches: ERα and ERβ knockout models to dissect receptor-specific contributions
These methods have elucidated how estradiol coordinates serotonergic gene expression through both classical ERE-mediated mechanisms and protein-protein interactions with transcription factors including Sp1, AP-1, C/EBPβ, and NF-κB at promoter regions lacking canonical ERE sequences [23].
Research Reagent Solutions
Table 3: Essential Research Tools for Investigating Estradiol-Neurotransmitter Interactions
| Research Tool | Specific Application | Function/Mechanism |
|---|---|---|
| Selective Estrogen Receptor Modulators | ||
| Tamoxifen | Probing ER involvement | Mixed ER agonist/antagonist; crosses BBB |
| Raloxifene | CNS ER modulation | SERM with tissue-specific actions |
| Estrogen Receptor Agonists | ||
| PPT (Propylpyrazoletriol) | ERα-specific actions | Selective ERα agonist |
| DPN (Diarylpropionitrile) | ERβ-specific actions | Selective ERβ agonist |
| G-1 | GPER1-specific signaling | Selective GPER1 agonist |
| Cholinergic Tools | ||
| Scopolamine | Muscarinic receptor blockade | Non-selective muscarinic antagonist |
| Mecamylamine | Nicotinic receptor blockade | Non-competitive nicotinic antagonist |
| Oxotremorine | Muscarinic receptor activation | Muscarinic receptor agonist |
| Serotonergic Agents | ||
| WAY-100635 | 5-HT1A receptor blockade | Selective 5-HT1A antagonist |
| Citalopram | Serotonin reuptake inhibition | SSRI; increases synaptic 5-HT |
| Fenfluramine | Serotonin release | Promotes 5-HT release and blocks reuptake |
| Molecular Biology Reagents | ||
| ERα/ERβ siRNA | Receptor-specific knockdown | Selective receptor silencing |
| ERE-luciferase reporters | ER transcriptional activity | Measures ER-mediated gene expression |
| ChIP assays | ER-DNA interactions | Maps ER binding to target genes |
These research tools enable dissection of estradiol's mechanisms in modulating cholinergic and serotonergic function, from receptor-specific contributions to downstream transcriptional regulation.
Estradiol orchestrates complex interactions with cholinergic and serotonergic systems through complementary genomic and non-genomic mechanisms. The convergence of these neurotransmitter effects supports key cognitive domains vulnerable in aging and neuropsychiatric conditions. Future research should prioritize:
- Development of receptor-specific estradiol analogs that maximize cognitive benefits while minimizing peripheral risks
- Elucidation of critical period windows for hormone interventions to optimize cognitive outcomes
- Examination of how individual difference factors (genetics, reproductive history, health status) modulate treatment response
- Integration of multi-modal imaging with pharmacological challenges to map circuit-level effects of estradiol-neurotransmitter interactions
The evolving understanding of estradiol's neuromodulatory actions continues to inform targeted therapeutic approaches for maintaining cognitive health across the lifespan, particularly during reproductive transitions when women are at increased risk for cognitive decline and mood disturbances. By leveraging the intricate interactions between estradiol and neurotransmitter systems, researchers can develop more effective, personalized strategies for cognitive support in aging populations.
This whitepaper synthesizes functional neuroimaging evidence elucidating the profound impact of 17β-estradiol (E2) on the neural circuitry underlying memory formation. A growing body of research indicates that E2 enhances memory consolidation through coordinated actions in the hippocampus and medial prefrontal cortex (mPFC), brain regions critical for episodic and spatial memory. This review details the experimental protocols and functional imaging methodologies that have uncovered E2-mediated changes in brain activation, functional connectivity, and synaptic plasticity. Framed within the broader thesis of hormonal mechanisms in cognitive performance, this evidence provides a neurobiological foundation for understanding sex differences in cognitive aging and the elevated risk of neurodegenerative disorders in postmenopausal women, offering critical insights for targeted therapeutic development.
The steroid hormone 17β-estradiol (E2) is a potent regulator of non-reproductive brain functions, with profound implications for learning and memory. The hippocampus and prefrontal cortex, brain structures densely populated with estrogen receptors, are exquisitely sensitive to E2 fluctuations [27] [28]. Research conducted over the past decade has begun to unravel the molecular and systems-level mechanisms through which E2 modulates cognitive performance, moving beyond a sole focus on the hippocampus to encompass network-level interactions [27] [29].
A pivotal thesis in this field posits that E2 enhances memory consolidation by orchestrating synchronized activity across a network of brain regions, rather than acting on isolated structures. This coordination is particularly evident between the dorsal hippocampus (DH) and the medial prefrontal cortex (mPFC), which show E2-induced increases in functional connectivity and dendritic spine density concurrent with improved memory performance [27] [29]. The timing of E2 administration is critical, with effects following a "healthy cell bias" where benefits are most pronounced when treatment coincides with preserved neural architecture [30] [28].
Understanding these mechanisms is clinically urgent. Women are at substantially greater risk for Alzheimer's disease (AD) than men, even after accounting for longer lifespans [27]. The decline in circulating E2 levels during menopause is thought to contribute to this vulnerability, rendering neurons more susceptible to age-related decline [27] [31]. This whitepaper consolidates functional neuroimaging evidence from rodent and human studies to delineate E2-induced changes in hippocampal and prefrontal activation, providing a technical foundation for researchers and drug development professionals aiming to translate these findings into novel cognitive therapeutics.
Estradiol and Memory Consolidation: Core Mechanisms
Molecular Signaling Pathways
E2 enhances memory through rapid, non-genomic signaling and slower, genomic pathways. In the dorsal hippocampus, post-training E2 infusion rapidly activates cell-signaling cascades such as the ERK/MAPK pathway, leading to increased dendritic spine density on CA1 pyramidal neurons within hours [27] [28]. This spinogenesis is temporally aligned with the window for memory consolidation, suggesting a direct structural correlate of E2-mediated memory enhancement.
The canonical estrogen receptors, ERα and ERβ, as well as the membrane-associated G protein-coupled estrogen receptor (GPER), are localized throughout the hippocampus and prefrontal cortex [27]. These receptors can act as nuclear transcription factors and interact with neurotransmitter receptors at the membrane to stimulate intracellular signaling [27]. Hippocampal E2 synthesis occurs de novo independently of ovarian sources, providing localized hormone regulation that influences synaptic plasticity in both sexes [27].
Table 1: Key Molecular Players in E2-Mediated Memory Consolidation
| Molecule/Pathway | Function in E2 Signaling | Effect on Memory |
|---|---|---|
| ERα & ERβ | Classical nuclear receptors; also mediate rapid membrane signaling | Genomic and non-genomic regulation of memory formation [27] |
| GPER | G protein-coupled membrane estrogen receptor | Activates rapid cell-signaling cascades (e.g., ERK) [27] |
| ERK/MAPK Pathway | Key intracellular signaling cascade | Critical for E2-induced spinogenesis and memory consolidation [27] [28] |
| Dendritic Spines | Postsynaptic sites of excitatory connections | Increased density in hippocampal CA1 and mPFC correlates with memory enhancement [29] [28] |
Functional Circuitry: Hippocampus-Prefrontal Cortex Interactions
A paradigm shift in the field recognizes that E2-mediated memory consolidation requires the concurrent activity of multiple brain regions. Chemogenetic inhibition of the mPFC during E2 infusion into the DH completely blocks the enhancing effects of E2 on both object recognition and spatial memory, demonstrating that mPFC activity is obligatory for DH-dependent memory consolidation [29]. This finding indicates a functional circuit where E2 action in one node (the DH) requires the functional integrity of another (the mPFC).
Resting-state functional MRI (fMRI) studies in humans corroborate these circuit-level findings. In postmenopausal women, higher E2 levels are associated with enhanced functional connectivity between the parahippocampal gyrus and the precuneus, a key hub of the default mode network (DMN) [31]. The DMN is implicated in memory and cognitive function, and its modulation by E2 may underlie the hormone's effects on cognitive performance [30].
Diagram Title: E2 Modulates Memory via a Hippocampal-Prefrontal Circuit
Experimental Protocols & Key Findings
Rodent Models: Behavioral Tasks and Intracranial Infusions
Protocol: Object Recognition (OR) and Object Placement (OP) Tasks
- Purpose: To assess nonspatial (OR) and spatial (OP) memory consolidation in rodents. These one-trial tasks capitalize on rodents' innate preference for novelty [29].
- Subjects: Young adult ovariectomized (OVX) female mice or rats to control for endogenous hormone fluctuations.
- Procedure:
- Training: The subject is placed in an arena with two identical objects for a set exploration time (e.g., 30 seconds total).
- Infusion: Immediately post-training, the subject receives a bilateral microinfusion of E2 or vehicle directly into the dorsal hippocampus (DH) or medial prefrontal cortex (mPFC).
- Testing:
- OR: Conducted 48 hours post-training. One familiar object is replaced with a novel object. More time spent with the novel object indicates successful memory consolidation.
- OP: Conducted 24 hours post-training. One object is moved to a novel location. More time spent with the moved object indicates intact spatial memory.
- Key Findings: Post-training infusion of E2 into either the DH or mPFC significantly enhances performance on both OR and OP tasks compared to vehicle controls, confirming E2's role in memory consolidation within these structures [29].
Protocol: Chemogenetic Inhibition During E2 Infusion
- Purpose: To test the necessity of concurrent mPFC activity for E2-mediated memory enhancement in the DH.
- Subjects: OVX female mice.
- Procedure:
- Surgery: Bilateral cannulation of the DH for E2 infusion and viral vector injection into the mPFC to express inhibitory DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) in excitatory neurons.
- Behavioral Testing: After recovery, mice undergo OR/OP training.
- Post-Training: Simultaneous infusion of E2 (or vehicle) into the DH and systemic injection of the DREADD ligand CNO (or vehicle) to inhibit mPFC neurons.
- Key Findings: Chemogenetic inhibition of the mPFC completely blocks the memory-enhancing effect of DH E2 infusion. This demonstrates that mPFC activity is required for E2-mediated, DH-dependent memory consolidation [29].
Table 2: Summary of Key Rodent Model Findings
| Experimental Manipulation | Behavioral Outcome (vs. Control) | Neural Correlate |
|---|---|---|
| DH E2 Infusion | Enhanced OR and OP memory [29] | ↑ Spine density in DH CA1 and mPFC [29] |
| mPFC E2 Infusion | Enhanced OR and OP memory [29] | ↑ Spine density in mPFC (apical dendrites) [29] |
| mPFC Inhibition + DH E2 | Blocks memory enhancement [29] | Disrupts functional hippocampal-prefrontal circuit |
Human Studies: Functional Neuroimaging and Hormonal Manipulation
Protocol: Resting-State fMRI in Postmenopausal Women
- Purpose: To examine the relationship between serum E2 levels and functional connectivity in estrogen-sensitive brain regions.
- Subjects: Cognitively healthy postmenopausal women not undergoing hormone therapy.
- Procedure:
- Blood Sampling: Venous blood is drawn on the same day as the MRI scan to assess serum E2 levels via radioimmunoassay.
- MRI Acquisition: High-resolution structural and resting-state BOLD fMRI scans are obtained. Participants are instructed to rest quietly with their eyes open.
- Data Analysis: Functional connectivity is analyzed using ROI-to-ROI approaches in software like CONN or SPM. Key regions of interest (ROIs) include the hippocampus, parahippocampal gyrus, dorsolateral prefrontal cortex (DLPFC), and precuneus.
- Key Findings: Higher E2 levels are associated with enhanced functional connectivity between the parahippocampal gyrus and the precuneus. This suggests E2 modulates connectivity within memory-related networks, even in the resting state [31].
Protocol: Pharmacological fMRI and Cognitive Testing
- Purpose: To investigate the effects of estrogen therapy or estrogen suppression on brain activation during cognitive tasks.
- Subjects: Premenopausal, perimenopausal, or postmenopausal women.
- Procedure:
- Hormonal Manipulation: Administration of conjugated equine estrogens, 17β-estradiol, or an aromatase inhibitor (e.g., letrozole) to suppress endogenous E2 synthesis.
- Cognitive Testing During fMRI: Participants perform cognitive tasks (e.g., verbal memory, mental rotation) in the scanner.
- Data Analysis: Brain activation patterns and performance accuracy are compared across treatment groups or correlated with hormone levels.
- Key Findings:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for Investigating E2 Effects
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| 17β-Estradiol (E2) | The primary experimental estrogen for in vivo and in vitro studies. | Microinfusion into brain regions (DH, mPFC) to study localized effects on memory [29] [28]. |
| Ovariectomized (OVX) Rodent Model | Standardized model for studying E2 in a low-estrogen background. | Base model for all E2 replacement studies; allows control over hormone exposure [29] [28]. |
| DREADD Technology (AAV-CaMKIIα-hM4Di) | Chemogenetic tool for targeted neuronal inhibition. | Testing necessity of mPFC activity in E2-mediated memory consolidation [29]. |
| Clozapine-N-Oxide (CNO) | Inert ligand that activates DREADD receptors. | Administered systemically to inhibit mPFC neurons expressing hM4Di during behavioral testing [29]. |
| Golgi-Cox Staining Kit | Histological method for visualizing neuronal morphology. | Quantifying changes in dendritic spine density in DH and mPFC following E2 administration [29]. |
| Radioimmunoassay (RIA) Kits | Sensitive quantification of hormone levels from serum or tissue. | Measuring circulating E2 levels in human subjects or rodent models [31]. |
| Aromatase Inhibitor (Letrozole) | Suppresses endogenous E2 synthesis by inhibiting the aromatase enzyme. | Modeling E2 deficiency in rodents and studying resulting cognitive and functional connectivity changes [30]. |
Discussion and Future Directions
The convergent evidence from rodent and human studies solidifies the thesis that estradiol is a critical modulator of a hippocampal-prefrontal circuit essential for memory consolidation. The efficacy of E2 is highly dependent on experimental parameters, including the timing of administration, the specific brain region targeted, and the hormonal status of the subject. The discovery that de novo E2 synthesis occurs in the hippocampus opens new avenues for drug discovery, suggesting that targeting local E2 production or signaling may offer therapeutic benefits without the systemic risks associated with hormone replacement therapy [27].
Future research must prioritize several key areas:
- Mechanistic Resolution: Delineate the distinct contributions of ERα, ERβ, and GPER to functional connectivity and memory using receptor-specific agonists and antagonists.
- Translational Bridging: Develop more sophisticated fMRI tasks in rodents that are analogous to human memory paradigms to enable direct cross-species comparisons of E2's effects on brain activation.
- Therapeutic Optimization: Systematically explore the "critical window" hypothesis to define the optimal timing and formulation for hormone-based interventions to preserve cognitive health in aging women.
The tools and experimental protocols detailed herein provide a roadmap for researchers to further dissect the hormonal mechanisms of estradiol on cognitive performance, ultimately informing the development of novel, evidence-based therapeutics for cognitive decline.
From Bench to Bedside: Research Models and Clinical Assessment of Estradiol's Cognitive Effects
The evaluation of learning and memory in rodent models is a cornerstone of behavioral neuroscience, particularly in the study of cognitive disorders and the development of novel therapeutic strategies. Within this research domain, the influence of hormonal mechanisms on cognition has garnered significant attention, with estradiol emerging as a critical neuroprotective agent. A comprehensive understanding of the behavioral tools available to assess specific memory domains is essential for designing rigorous experiments that can elucidate estradiol's effects. This technical guide provides an in-depth overview of key behavioral paradigms for assessing spatial, episodic, and social memory in rodents, with particular emphasis on their application within research investigating the cognitive impacts of estradiol. The protocols, data interpretation guidelines, and methodological considerations outlined herein are designed to assist researchers in selecting and implementing appropriate models for their specific investigative needs.
Behavioral Paradigms for Spatial Memory
Spatial memory, the ability to encode and recall information about one's environment and spatial orientation, is primarily dependent on the integrity of the hippocampus and associated medial temporal lobe structures. This cognitive domain is highly sensitive to hormonal fluctuations, including those involving estradiol [7].
Morris Water Maze (MWM)
The Morris Water Maze is a quintessential test for assessing spatial learning and reference memory in rodents. It capitalizes on the rodent's innate ability to use distal spatial cues to navigate to a hidden escape platform.
Experimental Protocol:
- Apparatus: A large circular pool (typically 1.5-2.0 m in diameter) filled with opaque water maintained at ~22-25°C. A hidden platform is submerged ~1-1.5 cm below the water surface in a fixed location.
- Habituation: Animals are gently introduced to the water and allowed to swim freely for 60 seconds without the platform present to reduce initial anxiety.
- Acquisition Training: Conducted over 4-6 days, with 2-4 trials per day. Each trial starts with the rodent placed in the water facing the pool wall at one of four variable start points. The trial ends when the animal finds the platform or after a pre-set time (e.g., 60-90 seconds). Animals remaining on the platform are allowed to remain for 15-20 seconds to consolidate spatial cues.
- Probe Trial: After the final training session, the platform is removed, and the animal is allowed to swim for 60-90 seconds. This trial assesses spatial memory retention by measuring the animal's preference for the target quadrant where the platform was previously located.
- Data Analysis: Key parameters during acquisition include escape latency (time to find the platform) and path efficiency. During the probe trial, time spent in target quadrant, number of platform location crossings, and average proximity to the former platform location are analyzed.
Considerations for Estradiol Research: Estradiol has been shown to enhance performance in the MWM. Ovariectomized (OVX) rats, a model of estrogen deficiency, exhibit significant impairments in spatial learning and memory, which are ameliorated by 17β-estradiol replacement therapy [7]. The MWM is thus a sensitive tool for probing the hippocampal-dependent cognitive effects of estradiol manipulation.
Y-Maze and Modified Y-Maze
Y-Maze tasks assess spatial working memory based on the rodent's innate tendency to explore a novel arm.
Experimental Protocol (Modified Y-Maze [32]):
- Apparatus: The modified version often uses a radial arm maze setup with three open arms arranged in a Y-shape, promoting reliance on distal cues.
- Training Phase: A single 10-minute session where one arm (the "novel" arm) is blocked. The rodent can freely explore the two accessible arms.
- Inter-Trial Interval (ITI): A delay is imposed (e.g., 10 minutes to 24 hours).
- Test Phase: The previously blocked arm is opened. The rodent is returned to the maze and allowed to explore all three arms for 5-10 minutes.
- Data Analysis: The primary measure is the percentage of time spent in the novel arm versus the familiar arms. A score significantly above chance (33.3%) indicates intact spatial recognition memory.
Table 1: Key Spatial Memory Paradigms and Their Features
| Paradigm | Memory Type Assessed | Primary Neural Substrate | Key Outcome Measures | Sensitivity to Estradiol |
|---|---|---|---|---|
| Morris Water Maze | Spatial Reference Memory & Learning | Hippocampus | Escape latency, Time in target quadrant, Platform crossings | High - E2 replacement improves performance in OVX models [7] |
| Y-Maze (Spontaneous Alternation) | Spatial Working Memory | Hippocampus, Prefrontal Cortex | % Alternation, Number of arm entries | Moderate - Spontaneous alternation is sensitive to E2 levels |
| Radial Arm Maze | Spatial Working & Reference Memory | Hippocampus | Working memory errors, Reference memory errors | High - E2 modulates performance, especially under high cognitive demand |
| Novel Object Location (NOL) | Spatial Recognition Memory | Hippocampus | Discrimination Index (Time with moved vs. unmoved object) | High - A simple, rapid test sensitive to E2 administration |
Behavioral Paradigms for Episodic-like Memory
Episodic memory involves the conscious recollection of autobiographical events embedded in their specific spatial and temporal contexts. Modeling this complex memory system in rodents is challenging but has been achieved using tasks that require the integration of "what," "where," and "when" information [33] [34].
Integrated "What-Where-When" Paradigms
These tasks are designed to capture the integrated nature of episodic memory by requiring rodents to remember an object (what), its location (where), and the temporal context of its encounter (when).
Experimental Protocol (e.g., K-EM Paradigm [33]):
- Apparatus: An open field arena containing multiple distinct objects.
- Sample Phase 1: The rodent is exposed to two identical objects (A1 and A2) placed in specific locations within the arena.
- Sample Phase 2: After a delay (e.g., 50-60 min), the rodent is re-exposed to the arena. One of the familiar objects (A1) remains in its original location, while the other is replaced with a novel object (B) in a new location.
- Test Phase: After a final delay, the rodent is tested for its exploration of the objects. Intact episodic-like memory is demonstrated by a preference for the object that is both novel and out of its original temporal context.
- Data Analysis: Exploration time is manually or automatically scored. A temporal memory score (exploration of the temporally novel object) and a spatial memory score (exploration of the displaced object) are calculated. The critical measure is the successful integration of these components.
Considerations for Estradiol Research: The integration of diverse memory components is a key feature of episodic memory that is sensitive to hormonal status. Tasks like the K-EM paradigm have been used to demonstrate that estradiol contributes to the binding of "what," "where," and "when" information into a coherent memory trace [33]. Estradiol's effects on synaptic plasticity in the hippocampus and prefrontal cortex are believed to underpin these functions.
Novel Object Recognition (NOR) and Temporal Order Memory
While NOR primarily tests recognition memory, its variants can probe aspects of episodic memory, particularly temporal order.
Experimental Protocol (Temporal Order Memory):
- Sample Phase 1: The rodent is exposed to two identical copies of object A.
- Sample Phase 2: After a long delay (e.g., 4-24 hours), the rodent is exposed to two identical copies of a novel object B.
- Test Phase: After a short delay (e.g., 1 hour), the rodent is presented with one copy of the "old" object A and one copy of the "less old" object B.
- Data Analysis: Intact temporal order memory is indicated by a preference for exploring the "less old" object (B), demonstrating memory for the relative timing of the experiences.
Behavioral Paradigms for Social Memory
While rodents do not possess verbal memory, social memory paradigms assess the ability to recognize and remember conspecifics, which is a fundamental form of non-verbal declarative memory highly relevant to social cognition deficits in neuropsychiatric disorders.
Three-Chamber Social Test
This test assesses social motivation and social recognition memory [35].
Experimental Protocol:
- Apparatus: A rectangular, three-chambered box with openings between chambers.
- Habituation: The test rodent is placed in the middle chamber and allowed to explore all three empty chambers.
- Sociability Phase: An unfamiliar conspecific (Stranger 1) is enclosed in a small wire cage in one side chamber. An identical empty cage is placed in the opposite chamber. The test rodent is allowed to explore for 10-15 minutes.
- Social Novelty Phase: A second unfamiliar conspecific (Stranger 2) is placed in the previously empty cage. The now-familiar Stranger 1 remains in its location. The test rodent is again allowed to explore.
- Data Analysis: Time spent sniffing or in close proximity to each wire cage is measured. A socially motivated animal will spend more time with Stranger 1 than the empty cage (sociability) and more time with the novel Stranger 2 than the familiar Stranger 1 (social recognition memory).
Habituation-Dishabituation Paradigm
This simple test is highly effective for measuring social recognition memory based on olfactory cues [35].
Experimental Protocol:
- Apparatus: The test rodent's home cage or a neutral arena.
- Habituation Trials: An ovariectomized or juvenile conspecific (the "stimulus" animal) is introduced to the test rodent's cage for 1-2 minutes and then removed. This is repeated 3-4 times with a short inter-trial interval (e.g., 10 min).
- Dishabituation Trial: After the final habituation trial, a novel stimulus animal is introduced.
- Data Analysis: The duration of social investigation (sniffing, following, grooming) by the test rodent is recorded. Intact social memory is indicated by a progressive decrease in investigation across habituation trials (habituation) and a significant increase in investigation when the novel animal is introduced (dishabituation).
Table 2: Key Non-Spatial Memory Paradigms and Their Features
| Paradigm | Memory Type Assessed | Primary Neural Substrate | Key Outcome Measures | Sensitivity to Estradiol |
|---|---|---|---|---|
| Three-Chamber Test | Social Motivation & Recognition | Prefrontal Cortex, Amygdala, Hippocampus | Time spent with novel vs. familiar conspecific | Moderate - E2 influences social motivation and recognition [35] |
| Habituation-Dishabituation | Social Recognition Memory | Olfactory Bulb, Hippocampus, Medial Prefrontal Cortex | Investigation time across trials; Dis-habituation score | High - Rapid test sensitive to hormonal status [35] |
| Novel Object Recognition (NOR) | Object Recognition Memory | Perirhinal Cortex, Hippocampus | Discrimination Index (Time with novel vs. familiar object) | High - A robust and simple test strongly modulated by E2 [33] |
| K-EM / What-Where-When | Episodic-like Memory | Hippocampus, Prefrontal Cortex | Integrated memory score, Temporal memory score | High - Designed to test integrated memory, a key target of E2 action [33] |
Estradiol Signaling and Cognitive Performance: A Mechanistic Workflow
Research into the hormonal mechanisms of estradiol on cognitive performance typically follows a logical workflow, from model creation to molecular analysis. The following diagram synthesizes the key stages and experimental considerations involved in this process.
Essential Research Reagent Solutions
The following table details key reagents and materials essential for conducting the behavioral and mechanistic research described in this guide, with a focus on estradiol manipulation studies.
Table 3: Essential Research Reagents and Materials
| Reagent/Material | Function/Application | Example Use in Protocol | Key Considerations |
|---|---|---|---|
| 17β-Estradiol (E2) | The primary biologically active estrogen for hormone replacement therapy in preclinical models. | Administered via subcutaneous injection, oral gavage, or transdermal patch to OVX rodents. | Dose, timing, and route of administration are critical. Transdermal may offer advantages for hippocampal-dependent memory [8]. |
| Ovariectomized (OVX) Rodents | The gold-standard experimental model for studying estrogen deficiency and the effects of replacement therapy. | Used as the base model in all phases of research to simulate post-menopausal conditions. | Ensure sufficient post-surgical recovery (e.g., 1-2 weeks) before initiating experiments. |
| Estrogen Receptor Agonists/Antagonists | Pharmacological tools to dissect the specific roles of ERα vs. ERβ receptor subtypes in cognitive function. | Injected intracerebroventricularly or systemically prior to behavioral testing to probe receptor mechanisms. | Selectivity and dose must be empirically validated for the cognitive endpoint being measured. |
| Morris Water Maze Pool & Tracking Software | Core apparatus for assessing spatial learning and memory. Automated tracking is essential for objective data collection. | The pool is filled with opaque water (with non-toxic white tempera paint) and a hidden platform. | Maintain consistent water temperature and lighting. Ensure numerous distal visual cues are present. |
| Three-Chamber Apparatus | Standardized equipment for assessing social motivation and social recognition memory. | Typically a clear Plexiglas rectangular box divided into three interconnected chambers. | Stimulus animals must be age-, sex-, and strain-matched and habituated to the wire containment cups. |
| Open Field Arena with Objects | Versatile apparatus for Novel Object Recognition, Object Location, and integrated episodic-like memory tasks. | A simple square or circular arena made of opaque plastic or wood, with various disposable objects. | Objects must be thoroughly cleaned between trials and animals to remove odor cues. Object preference should be pre-validated. |
| ELISA Kits (e.g., for NGF, PSD-95, Aβ) | To quantify changes in key neurobiological markers post-behavioral testing. | Brain tissue (e.g., hippocampus, prefrontal cortex) is homogenized and analyzed post-mortem. | Tissue should be fresh-frozen or preserved in RNAlater immediately after sacrifice to preserve integrity. |
The behavioral paradigms detailed in this guide provide a robust toolkit for investigating the nuanced effects of estradiol and other hormonal manipulations on distinct cognitive domains in rodents. The selection of an appropriate paradigm must be guided by the specific research question, whether it pertains to hippocampal-dependent spatial memory, complex integrated episodic-like memory, or social recognition. The consistent finding that estradiol replacement can ameliorate cognitive deficits in OVX models underscores the hormone's critical role in maintaining cognitive health. By employing these standardized, validated protocols within a rigorous mechanistic workflow, researchers can continue to advance our understanding of the hormonal mechanisms of cognitive performance and contribute to the development of novel therapeutic strategies for cognitive decline associated with hormonal changes.
The design of cognitive test batteries for clinical trials requires a nuanced understanding of the specific memory domains affected by hormonal fluctuations, particularly estradiol. Estradiol, the most potent estrogen, exerts profound effects on brain structure and function through binding to estrogen receptors densely located in the hippocampus, frontal cortex, and other regions crucial for memory formation and retrieval [8]. The menopausal transition, characterized by declining estradiol levels, presents a critical window for investigating hormonal influences on cognition and for designing trials that can accurately detect intervention effects [19]. This whitepaper provides an in-depth technical guide for selecting and implementing cognitive test batteries that are sensitive to the effects of estradiol on three key memory domains: episodic, prospective, and working memory, with the aim of standardizing approaches in clinical research and drug development.
Core Cognitive Domains and Assessment Methodologies
Domain Definitions and Neuroanatomical Substrates
Episodic Memory: This domain involves the conscious recollection of everyday events, including contextual details about times, locations, associated emotions, and other situational knowledge [19]. It is primarily governed by the integrity of the medial-temporal lobes, particularly the hippocampus, a region rich in estrogen receptors [8] [19].
Prospective Memory: This is the memory for remembering to perform a planned action or intention at a future time, such as taking medication at a specified time or remembering to call a friend [19]. Its processes require the involvement of both the frontal and medial-temporal lobes [8].
Executive Functions/Working Memory: Executive functions are essential mental skills that enable planning, organizing, and completing tasks to achieve goals. Working memory, a key subcomponent, allows for the temporary storage and manipulation of information. These functions are primarily governed by the frontal lobes [19].
Validated Cognitive Test Batteries
Researchers can select from several well-validated test batteries to assess these domains. The choice of battery and specific tests should be aligned with the primary research question, the population under study, and the specific cognitive domain of interest.
Table 1: Cognitive Test Batteries and Their Applications
| Test Battery | Specific Test | Cognitive Domain Measured | Key Task Description | Sensitivity to Hormonal Effects |
|---|---|---|---|---|
| Cambridge Neuropsychological Test Automated Battery (CANTAB) | Pattern Recognition Memory (PRM) | Episodic Memory (Visual Recognition) | Recognizing previously seen patterns from novel ones. | Differentiates amnestic Mild Cognitive Impairment (aMCI) from controls [36]. |
| Delayed Matching to Sample (DMS) | Episodic Memory (Visual Recall) | Identifying a previously seen sample image after a delay. | Combined with other tests, achieves 80% predictive accuracy for aMCI [36]. | |
| Paired Associates Learning (PAL) | Episodic Memory (Visuospatial Learning) | Remembering the locations of pattern pairs. | Total errors significantly predict aMCI status [36]. | |
| NIH Toolbox Cognition Battery (CB) | Picture Sequence Memory Test (TPSMT) | Episodic Memory | Reproducing the order of an arbitrarily ordered sequence of pictures. | Sensitive to age-related changes; useful in developmental and aging studies [37]. |
| Custom Domain-Specific Tests | — | Prospective Memory | Remembering to perform a future action (e.g., pressing a button at a specific time). | Oral estradiol associated with higher scores compared to no hormone therapy [8]. |
The CANTAB battery has demonstrated significant utility in detecting subtle deficits in visual episodic memory. A study found that a model combining the total percent correct for PRM and DMS with the total errors from PAL (six shapes adjusted) achieved a sensitivity of 72% and a specificity of 83% in discriminating patients with amnestic Mild Cognitive Impairment from healthy controls, with an overall predictive accuracy of 80% [36]. This high level of discrimination is essential for trials aiming to detect preventative or therapeutic effects in at-risk populations.
Hormonal Mechanisms and Research Evidence
Impact of Menopause Timing and Estradiol-Based Therapy
Recent large-scale observational studies have clarified the associations between menopause, hormone therapy, and cognitive performance. A cross-sectional analysis of 7,251 postmenopausal women from the Canadian Longitudinal Study on Aging revealed that an earlier age at menopause was significantly associated with lower scores across all three cognitive domains: episodic memory (β = 0.050, p < 0.001), prospective memory (β = 0.047, p < 0.001), and executive functions (β = 0.061, p < 0.001) [8]. This underscores the importance of considering lifetime exposure to ovarian hormones in trial design.
Crucially, the route of administration of estradiol-based menopausal hormone therapy (MHT) appears to have domain-specific effects [8] [19]:
- Transdermal Estradiol: Associated with higher episodic memory scores compared to no MHT (Cohen's d = 0.303) [8].
- Oral Estradiol: Associated with higher prospective memory scores compared to no MHT (Cohen's d = 0.283) [8].
- Executive Functions: Neither administration route showed a significant effect, suggesting this domain may be less sensitive to MHT interventions [8].
The differential effects are hypothesized to stem from the distinct metabolic pathways of oral versus transdermal estradiol. Oral estradiol undergoes first-pass hepatic metabolism, converting it to estrone (E1), which has a lower affinity for estrogen receptors. Transdermal estradiol bypasses this process, resulting in a more favorable E2:E1 ratio and potentially greater efficacy for hippocampal function, which is critical for episodic memory [8].
Diagram 1: MHT administration routes and cognitive domain effects.
Underlying Neuropathology: Tau and Synaptic Integrity
Beyond behavioral performance, hormonal factors are linked to Alzheimer's disease (AD) pathology. A study published in Science Advances found that among women over age 70, HRT use was associated with faster accumulation of tau protein in key brain regions of the temporal lobe compared to non-users [19]. This association was not observed in women under 70, supporting the "critical window" hypothesis for hormone therapy. Furthermore, earlier menopause has been linked to greater synaptic loss and AD pathology, suggesting that the premature loss of ovarian hormones makes the brain more vulnerable to degenerative processes [19]. These findings highlight the importance of considering both the timing of intervention and pathological biomarkers in trial design.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents and Methodological Components
| Item/Reagent | Function/Application in Research | Technical Notes |
|---|---|---|
| CANTAB | Computerized battery for sensitive assessment of visual memory and executive function. | Automated administration reduces tester bias. Useful for detecting aMCI [36]. |
| NIH Toolbox Picture Sequence Memory Test (TPSMT) | Measures episodic memory via sequence recall of pictured items. | Adjusts sequence length (6-15 pictures) for ability; high test-retest reliability [37]. |
| APOE ε4 Genotyping Assay | Identifies genetic risk factor for late-onset sporadic Alzheimer's disease. | Important for stratifying participants, as APOE ε4 status can moderate menopause effects [8]. |
| Estradiol (E2) Immunoassay Kits | Precisely quantify serum E2 levels in participants. | Essential for correlating hormone levels with cognitive outcomes. |
| Transdermal E2 Patches/Gels | Form of MHT that bypasses hepatic first-pass metabolism. | In studies, associated with benefits for episodic memory [8] [19]. |
| Oral Estradiol Tablets | Form of MHT that undergoes first-pass liver metabolism. | In studies, associated with benefits for prospective memory [8]. |
| PET Imaging Ligands for Tau (e.g., AV-1451) | Quantify in vivo tau neurofibrillary tangle burden in the brain. | Used to investigate biological mechanisms linking HRT to Alzheimer's pathology [19]. |
Experimental Protocol for a Clinical Trial Investigating Estradiol Effects
This section outlines a detailed protocol for a clinical trial designed to investigate the effects of estradiol-based MHT on memory domains.
Participant Recruitment and Stratification
- Inclusion Criteria: Recruit postmenopausal women aged 45-65, with menopause defined as at least 12 months of spontaneous amenorrhea. Participants should be within 5 years of menopause onset to target the potential "critical window" for intervention [19].
- Exclusion Criteria: Major exclusion criteria include a history of hormone-dependent cancer, venous thromboembolism, severe liver disease, current use of cognitive-enhancing medications, or existing diagnosis of mild cognitive impairment or dementia.
- Stratification: Stratify participants based on key moderating variables: APOE ε4 carrier status (ε4+ vs. ε4-) and number of children (0, 1-3, 4+), as these factors have been shown to interact with the cognitive effects of menopause and MHT [8].
Intervention and Blinding
- Study Arms: A randomized, double-blind, placebo-controlled design with three parallel arms:
- Transdermal Estradiol Group: Apply a transdermal patch delivering a standard dose (e.g., 0.05 mg/day).
- Oral Estradiol Group: Take a daily oral tablet of estradiol (e.g., 1 mg/day). A progestogen must be added for women with a uterus for endometrial protection.
- Placebo Group: Use identical-appearing transdermal patches and oral tablets containing no active ingredient.
- Treatment Duration: The intervention period should be a minimum of 12 months to allow for detectable changes in cognitive performance and potential underlying biomarkers.
Outcome Assessment Schedule
Assessments should be conducted at baseline (pre-intervention), and at 6 and 12 months post-randomization.
Table 3: Outcome Assessment Schedule and Measures
| Assessment Domain | Baseline (Month 0) | Follow-up 1 (Month 6) | Follow-up 2 (Month 12) |
|---|---|---|---|
| Primary Cognitive Outcomes | |||
| Episodic Memory | CANTAB-PAL, PRM, DMS [36] | CANTAB-PAL, PRM, DMS | CANTAB-PAL, PRM, DMS |
| Prospective Memory | Custom/validated task [8] | Custom/validated task | Custom/validated task |
| Executive Function | CANTAB relevant tests | CANTAB relevant tests | CANTAB relevant tests |
| Secondary Outcomes | |||
| Hormone Levels | Serum E2, E1 | Serum E2, E1 | Serum E2, E1 |
| AD Biomarkers (subsample) | Tau-PET, Amyloid-PET [19] | — | Tau-PET, Amyloid-PET |
| Safety & Covariates | Medical history, APOE genotyping [8] | Adverse events | Adverse events |
Diagram 2: Clinical trial workflow for estradiol and memory study.
Statistical Analysis Plan
- Primary Analysis: Use an intention-to-treat (ITT) approach. Analyze continuous cognitive outcome scores using linear mixed-effects models to account for repeated measures within participants over time. The models will include fixed effects for treatment group, time, and the group-by-time interaction, adjusting for baseline cognitive score, age, and education.
- Moderator Analysis: Test for interactions between treatment group and pre-specified moderators (APOE ε4 status, number of children) by including relevant interaction terms in the mixed models.
- Mediation Analysis: In exploratory analyses, use structural equation modeling to test whether the effect of MHT on cognitive change is mediated by changes in tau-PET signal accumulation, as suggested by prior research [19].
Estradiol, the most potent endogenous estrogen, exerts profound effects on a wide array of physiological systems, including the central nervous system. Research into the hormonal mechanisms of estradiol on cognitive performance has revealed that its efficacy is significantly influenced by its formulation and route of administration [16]. The pharmacokinetic (PK) profile of estradiol—governed by how it is delivered to the systemic circulation—directly impacts its availability to the brain and its subsequent biological actions [38]. Understanding the distinct PK characteristics of oral and transdermal estradiol is therefore not merely a technical consideration but a fundamental aspect of designing and interpreting research on cognitive function. This guide provides a detailed technical comparison of these two primary administration routes, framing the discussion within the context of cognitive neuroscience research.
Quantitative Pharmacokinetic Profile
The route of administration fundamentally alters the absorption, metabolism, and systemic availability of estradiol. The table below summarizes the critical PK parameters for oral and transdermal estradiol, which are essential for designing dosing regimens in clinical research.
Table 1: Comparative Pharmacokinetics of Oral vs. Transdermal Estradiol
| Parameter | Oral Estradiol | Transdermal Estradiol |
|---|---|---|
| Bioavailability | Low (~5%; range 0.1-12%) [38] | High (bypasses first-pass metabolism) [38] |
| First-Pass Metabolism | Extensive in liver and intestines [38] | Negligible [38] |
| Primary Metabolites | Estrone (E1), Estrone Sulfate (E1-S), and their glucuronides [38] | Parent estradiol (E2) [39] |
| Estradiol:Estrone (E2:E1) Ratio | Low (~0.15-0.25) [38] | Near-physiological (~1.0) [38] |
| Elimination Half-Life | 13-20 hours [38] | ~37 hours (gel) [38] |
| Key Impact on Liver | High hepatic exposure; impacts synthesis of SHBG, clotting factors [39] [38] | Minimal hepatic exposure [39] |
Clinical and Research Implications of PK Differences
The data in Table 1 have direct implications for research on cognitive function:
- Metabolic Profile and Neurological Activity: The metabolic products of estradiol are not merely inactive waste products. Some catechol estrogens are biologically active and can influence neuronal function and carcinogenic processes [40] [41]. The oral route generates a much broader and more complex profile of circulating metabolites, notably a high concentration of estrone, which is a less potent estrogen than estradiol. In contrast, the transdermal route delivers estradiol directly, resulting in a more physiological E2:E1 ratio [38]. This cleaner metabolic profile can simplify the interpretation of cognitive outcomes in research settings.
- Hepatic Effects and Brain Health: The first-pass liver metabolism associated with oral administration has systemic consequences. It stimulates the hepatic synthesis of sex hormone-binding globulin (SHBG) and various clotting factors [39]. Elevated SHBG can bind to circulating estradiol, potentially reducing the fraction of free, biologically active hormone available to cross the blood-brain barrier. Furthermore, the increased risk of venous thromboembolism (VTE) associated with oral therapy is a critical safety consideration in long-term interventional studies [39]. Transdermal administration, by avoiding this first-pass effect, presents a lower risk of VTE and has a minimal impact on SHBG, which may be preferable for studies involving older participants or those with cardiovascular risk factors [39] [42].
Mechanistic Pathways to Cognitive Function
Estradiol's enhancement of cognitive function, particularly verbal memory and processing speed, is supported by evidence from animal and human studies [16] [43] [44]. The pharmacokinetic profile of the administered estradiol influences the activation of these neurobiological pathways.
Estradiol Signaling Pathway in the Brain
The following diagram illustrates the key cellular mechanisms through which estradiol modulates cognitive function, showing pathways that are influenced by sustained and stable estradiol levels.
Diagram 1: Estradiol signaling pathways for cognitive function.
Linking Pharmacokinetics to Neurobiological Outcomes
Stable serum levels of estradiol, as achieved with transdermal delivery, are theorized to provide optimal support for the pathways in Diagram 1. Functional neuroimaging studies in humans provide direct evidence for these mechanisms. For instance, estrogen therapy has been shown to enhance hippocampal and prefrontal cortex function during the retrieval stage of episodic memory tasks, which is a key process for cognitive performance [44]. These brain regions are rich in estrogen receptors and are critical for memory formation and recall [16] [44]. A randomized controlled trial using fMRI found that transdermal estradiol enhanced activation in the prefrontal cortex (Brodmann area 11) during a verbal memory task, an area involved in higher-order executive functions [44]. Furthermore, a cross-sectional analysis of older women showed that higher endogenous serum estradiol levels were significantly correlated with better performance on the Digit Symbol Substitution Test (DSST), which assesses processing speed, sustained attention, and working memory [43]. This suggests that maintaining adequate estradiol levels is relevant for specific cognitive domains in aging women.
Experimental Protocols for Pharmacokinetic and Cognitive Assessment
To rigorously investigate the effects of estradiol formulation on cognitive outcomes, researchers must employ standardized protocols for PK analysis and cognitive testing.
Protocol for a Comparative Pharmacokinetic Study
Objective: To characterize and compare the serum pharmacokinetic profiles of oral micronized estradiol versus transdermal estradiol gel in a postmenopausal cohort.
Methodology:
- Participants: Recruit healthy postmenopausal women (e.g., aged 50-65). Exclude participants on hormone therapy, with contraindications to estrogen, or with significant cognitive impairment.
- Dosing: After a washout period, participants are randomized to receive either oral micronized estradiol (e.g., 1-2 mg/day) or transdermal estradiol gel (e.g., 0.75-1.5 mg/day). Doses should be equated based on prior clinical data to achieve similar steady-state estradiol levels where possible.
- Blood Sampling: Collect venous blood samples at baseline and at predetermined time points post-administration. For a single-dose PK profile, samples should be taken frequently over 24-36 hours. For steady-state assessment, trough levels are measured over multiple days or weeks.
- Bioanalytical Analysis:
- Sample Processing: Use liquid-liquid or solid-phase extraction to isolate steroids from serum.
- Mass Spectrometry: Quantify serum levels of estradiol (E2) and estrone (E1) using LC-MS/MS (liquid chromatography tandem mass spectrometry). This is the gold standard for specificity and sensitivity, capable of detecting the low pg/mL concentrations found in postmenopausal women [43]. The protocol from the NHANES study uses isotope-dilution LC-MS/MS, which provides high accuracy [43].
- Data Analysis: Calculate standard PK parameters for E2, including C~max~, T~max~, area under the curve (AUC~0-24h~), and elimination half-life. Critically, also calculate the E2:E1 ratio for each route.
Protocol for Assessing Cognitive Outcomes
Objective: To evaluate the impact of estradiol route of administration on cognitive domains, particularly verbal memory and executive function.
Methodology:
- Cognitive Assessment Battery: Administer a standardized set of tests pre-intervention and at regular intervals during treatment. Key tests include:
- CERAD Word List Learning Test: Assesses immediate and delayed verbal episodic memory, a domain sensitive to estrogen effects [43] [44].
- Digit Symbol Substitution Test (DSST): Measures processing speed, sustained attention, and working memory, which has been positively correlated with serum estradiol levels [43].
- Animal Fluency Test (AFS): Evaluates semantic memory and executive function components of verbal fluency [43].
- Functional Neuroimaging (fMRI): To obtain a direct biomarker of brain function, conduct fMRI scans during cognitive tasks. A standard protocol is to scan participants during the encoding and retrieval phases of an episodic memory task [44]. The blood-oxygen-level-dependent (BOLD) signal in the hippocampus and prefrontal cortex serves as the primary outcome, providing a neurophysiological correlate of the cognitive effects of estradiol administration route.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents, assays, and materials required for conducting research on estradiol pharmacokinetics and its cognitive effects.
Table 2: Key Research Reagents and Materials
| Item/Category | Function/Application | Examples & Technical Notes |
|---|---|---|
| Estradiol Formulations | Investigational interventions for clinical trials. | Micronized Estradiol Tablets (e.g., Estrace); Transdermal Gel (e.g., EstroGel); Transdermal Patches (e.g., Estradot) [39] [38] [42]. |
| LC-MS/MS System | Gold-standard quantification of serum steroid hormones. | Quantifies estradiol, estrone, and metabolites with high specificity and sensitivity down to pg/mL levels. Critical for accurate PK profiling [43] [41]. |
| Validated Immunoassays | Higher-throughput, but less specific, measurement of estradiol. | ELISA or RIA kits. Can be used for large-scale screening but are prone to cross-reactivity with metabolites; less reliable for postmenopausal levels [45]. |
| Cognitive Test Batteries | Standardized assessment of cognitive domains sensitive to estradiol. | CERAD, DSST, and Animal Fluency tests are well-validated and have been used in large studies like NHANES to link estradiol to cognition [43]. |
| fMRI Platform | Non-invasive measurement of task-induced brain activation. | Used to visualize and quantify estradiol's effects on hippocampal and prefrontal cortex function during memory tasks [44]. |
The choice between oral and transdermal estradiol is more than a matter of convenience; it is a fundamental methodological decision that shapes the pharmacokinetic and metabolic landscape of a research study. The oral route, with its high first-pass metabolism, creates a distinct hormonal milieu characterized by high estrone levels and significant hepatic impact, which may introduce confounding variables in cognitive research. The transdermal route, by delivering estradiol directly into the systemic circulation, provides a more physiological E2:E1 ratio and a cleaner safety profile. For research focused on elucidating the hormonal mechanisms of estradiol on cognitive performance, the transdermal route offers a distinct advantage by minimizing complex metabolic interference and providing stable hormone levels that are conducive to supporting the genomic and membrane-initiated signaling pathways critical for synaptic plasticity, memory, and executive function. Future studies should continue to leverage precise PK monitoring and advanced neuroimaging to further unravel the connection between hormone delivery, brain activation, and cognitive outcomes.
Estradiol (E2), the most potent form of estrogen, plays a critical role in brain function and has been implicated in the pathogenesis of cognitive decline and Alzheimer's disease [43] [16] [46]. The sharp decline in estradiol levels during menopause has been identified as a potential contributor to the increased risk of cognitive impairment and neurodegenerative diseases observed in older women [47] [46]. Assessing serum estradiol levels as a biomarker for cognitive health presents a valuable opportunity for researchers investigating the hormonal mechanisms underlying cognitive performance. This technical guide provides an in-depth framework for measuring serum estradiol and correlating these measurements with cognitive outcomes, specifically designed for researchers, scientists, and drug development professionals working in this field.
Estradiol and Cognitive Function: Mechanistic Background
Estradiol exerts its effects on cognitive function through multiple complementary mechanisms, acting as both a potent hormone and a neurosteroid [16]. The hormone interacts with estrogen receptors (ERα, ERβ, and GPER1) distributed throughout brain regions critical for learning and memory, including the hippocampus, prefrontal cortex, and basal forebrain [16] [46]. These interactions trigger both genomic signaling pathways that alter protein synthesis and non-genomic mechanisms that rapidly modulate neuronal function through membrane receptors and intracellular signaling pathways [16] [46].
Estradiol demonstrates significant neuroprotective properties, enhancing synaptic plasticity, promoting dendritic spine formation, and maintaining metabolic homeostasis in neurons [46]. These mechanisms collectively contribute to the hormone's ability to modulate cognitive processes, particularly those involving memory consolidation, processing speed, and executive function [16]. The decline in estradiol levels during menopausal transition has been associated with detectable changes in brain morphology and connectivity, providing a physiological basis for investigating its role in cognitive aging [46].
Table: Estradiol Mechanisms Relevant to Cognitive Function
| Mechanism Type | Specific Action | Brain Regions Involved | Cognitive Domains Affected |
|---|---|---|---|
| Genomic Signaling | Alters gene transcription via nuclear estrogen receptors | Hippocampus, Prefrontal Cortex | Long-term memory, Executive function |
| Non-genomic Signaling | Activates intracellular kinase pathways via membrane receptors | Hippocampus, Basal Forebrain | Working memory, Processing speed |
| Neurotrophic Effects | Promotes dendritic spine formation, Synaptic plasticity | Cerebral Cortex, Hippocampus | Learning, Memory consolidation |
| Metabolic Regulation | Maintains neuronal energy homeostasis, Reduces oxidative stress | Whole brain | Sustained attention, Processing speed |
Methodological Considerations for Serum Estradiol Measurement
Analytical Techniques
The accurate measurement of serum estradiol, particularly at the low concentrations typical in postmenopausal women, presents significant technical challenges [48]. Two primary analytical approaches are currently employed:
Immunoassays (IA) utilize antibody-based detection and are widely available but show substantial variability, especially at concentrations below 20-30 pg/mL [48]. This limitation is particularly problematic for cognitive aging research focused on postmenopausal populations, where estradiol concentrations typically range from 2.5-30 pg/mL [48]. The reported bias for immunoassays can range from -2.4% to 235%, with many assays unable to reliably measure levels below 10 pg/mL [48].
Mass Spectrometry (MS) methods, particularly liquid chromatography tandem mass spectrometry (LC-MS/MS) and isotope dilution gas chromatography/mass spectrometry (ID-GC/MS), offer superior sensitivity and specificity for low-level estradiol measurement [43] [48]. These techniques demonstrate lower coefficients of variation (often <15%) and better accuracy in the concentration ranges most relevant to cognitive aging research [49] [48]. The CDC Hormone Standardization Program (HoSt) has established reference measurement procedures using MS technology to improve standardization across laboratories [48].
Preanalytical Factors
Standardization of preanalytical procedures is essential for generating reliable, comparable data:
- Sample Collection: Blood should be collected in appropriate serum tubes following a standardized protocol [48]
- Timing: For premenopausal women, cycle phase documentation is critical due to significant fluctuations (e.g., pre-follicular phase vs. late follicular phase) [43]
- Processing: Rapid processing and freezing at -80°C preserves sample integrity [48]
- Quality Control: Incorporation of blinded duplicate samples and quality control pools in each batch is recommended [45]
Table: Comparison of Estradiol Measurement Techniques
| Parameter | Immunoassays (IA) | Mass Spectrometry (MS) |
|---|---|---|
| Sensitivity | Variable; many assays cannot reliably measure <10 pg/mL | Superior; can measure concentrations as low as 1-2 pg/mL with appropriate methods |
| Precision at Low Concentrations | Poor to moderate (CV often >15%) | Good to excellent (CV often <15%) |
| Specificity | Subject to cross-reactivity with related compounds | High specificity due to physical separation and mass detection |
| Throughput | High | Moderate to high |
| Cost | Lower | Higher |
| Standardization | Poor between different platforms | Better, especially when aligned with reference methods |
| Recommended Use | Initial screening in clinical settings | Research requiring accurate low-level quantification |
Cognitive Performance Assessment
The selection of cognitive assessment tools should be guided by the specific domains most sensitive to estradiol fluctuations. The National Health and Nutrition Examination Survey (NHANES) cognitive battery provides a validated approach, incorporating three distinct tests that capture different cognitive domains [43]:
Consortium to Establish a Registry for Alzheimer's Disease Word Learning Subtest (CERAD) assesses immediate and delayed verbal learning and memory [43]. Participants learn a list of words across multiple trials, with delayed recall tested after approximately 8-10 minutes. This test primarily engages hippocampal-dependent memory processes [43].
Animal Fluency Test (AFS) evaluates verbal fluency and executive function by asking participants to name as many animals as possible within one minute [43]. Performance depends on semantic memory retrieval, cognitive flexibility, and processing speed, engaging frontal and temporal networks [43].
Digit Symbol Substitution Test (DSST) measures processing speed, sustained attention, and working memory [43]. Participants match symbols to numbers according to a key within two minutes. This test has demonstrated particular sensitivity to estradiol levels in older women, with higher levels associated with better performance [43].
Additional assessments commonly used in estradiol research include the Rey Auditory Verbal Learning Test, various spatial memory tasks, and tests of verbal memory that may fluctuate across the menstrual cycle in premenopausal women [16].
Correlation Methodologies and Statistical Approaches
Experimental Designs
Multiple study designs can be employed to investigate estradiol-cognition relationships:
Cross-sectional Analyses examine the relationship between estradiol levels and cognitive performance at a single time point [43]. This approach identified that older women with estradiol levels >7.49 pg/mL demonstrated significantly better performance on the DSST test compared to those with lower levels (<3.68 pg/mL) [43].
Longitudinal Studies track changes in both estradiol and cognitive performance over time, offering insights into temporal relationships [50]. The Early Versus Late Intervention Trial with Estradiol (ELITE) exemplifies this approach, measuring cognitive and biomarker changes over 2.5-5 years in relation to estradiol intervention [50].
Intervention Studies investigate how experimentally manipulated estradiol levels affect cognition [51]. These trials have yielded mixed results, with some showing cognitive improvements and others finding no association between achieved estradiol levels and cognitive change [51].
Statistical Analysis
Appropriate statistical approaches are critical for valid interpretation:
- Data Transformation: Natural log transformation is often applied to both estradiol levels and cognitive test scores to normalize distributions [45]
- Multiple Linear Regression: Models should adjust for key covariates including age, education, race/ethnicity, body mass index, and health conditions like hypertension and diabetes [43]
- Stratified Analyses: Examining effects within specific subgroups (e.g., by APOE ε4 carrier status, time since menopause, or obesity status) can reveal important modifiers [50] [47]
- Handling of Assay Variability: Incorporation of reliability parameters (coefficients of variation, intraclass correlation coefficients) from validation studies improves accuracy of effect estimates [45] [48]
Diagram: Experimental Workflow for Estradiol-Cognition Correlation Studies. This workflow outlines the key steps in conducting studies investigating the relationship between serum estradiol levels and cognitive performance, highlighting essential quality control measures.
Research Reagent Solutions and Essential Materials
Table: Key Research Reagents and Materials for Estradiol-Cognition Studies
| Item Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Estradiol Assays | CDC ID-LC-MS/MS Reference Method, Commercial Immunoassays, In-house LC-MS/MS | Quantification of serum estradiol concentrations | Select method based on required sensitivity; MS methods preferred for low-level detection in postmenopausal populations |
| Cognitive Assessments | CERAD Word List, Animal Fluency Test, Digit Symbol Substitution Test | Measurement of specific cognitive domains | Computerized versus paper-and-pencil administration; standardized administration protocols critical |
| Sample Collection | Serum separator tubes, EDTA plasma tubes, Needles, Tourniquets | Biological specimen collection | Tube type, processing time, and storage conditions affect analyte stability |
| Laboratory Equipment | LC-MS/MS systems, Luminex platforms, Freezers (-80°C) | Sample processing, analysis, and storage | Equipment calibration and maintenance schedules impact measurement reliability |
| Quality Control Materials | Blinded duplicate samples, Quality control pools, Certified reference materials | Monitoring assay performance and variability | Should cover concentration ranges relevant to study population |
Interpreting Results and Addressing Methodological Challenges
Accounting for Biological and Analytical Variability
The interpretation of estradiol-cognition correlations must consider significant sources of variability:
Biological Variability: Estradiol levels fluctuate throughout the menstrual cycle in premenopausal women, with higher levels during the late follicular and mid-luteal phases potentially enhancing verbal fluency and memory abilities [43]. In postmenopausal women, estradiol production shifts to peripheral tissues, resulting in consistently low but still biologically relevant concentrations [47].
Analytical Variability: Substantial between-laboratory differences in estradiol measurements have been documented, with absolute levels differing markedly between labs for most assays [49] [48]. This variability is particularly pronounced at low concentrations characteristic of postmenopausal women, where some assays demonstrate overestimation biases [49].
Critical Period Hypothesis
The timing of estradiol exposure relative to menopause appears to critically influence its cognitive effects—a concept known as the "critical period" or "window of opportunity" hypothesis [50] [46]. Evidence suggests that estradiol-containing menopausal hormone therapy initiated early in postmenopause may influence Alzheimer's disease-related biomarkers, particularly amyloid-β measures, while similar interventions in late postmenopause show no significant effects [50]. This temporal sensitivity must be considered when designing studies and interpreting correlations between estradiol levels and cognitive outcomes.
The assessment of serum estradiol as a biomarker for cognitive performance requires meticulous methodological rigor across all phases of research—from sample collection and analytical measurement to cognitive assessment and statistical analysis. While substantial evidence supports the role of estradiol in maintaining cognitive function, particularly in the domains of processing speed, working memory, and verbal fluency, significant methodological challenges remain. The standardization of estradiol measurements, careful selection of cognitive assessments sensitive to hormonal effects, and appropriate consideration of timing factors in study design will advance our understanding of the hormonal mechanisms underlying cognitive performance and inform the development of targeted interventions for cognitive decline.
The quest to understand the hormonal mechanisms of estradiol on cognitive performance necessitates sophisticated tools capable of quantifying subtle changes in brain function and pathology. Neuroimaging endpoints provide an objective, in-vivo means to measure these biological effects, serving as critical biomarkers in both basic research and clinical drug development. This technical guide details the application of functional Magnetic Resonance Imaging (fMRI), Positron Emission Tomography (PET), and Single-Photon Emission Computed Tomography (SPECT) for quantifying brain activation and pathology within the specific context of estradiol research. We frame this discussion around the established need for reliable, sensitive biomarkers to investigate the impact of estradiol on cognitive function, a relationship supported by evidence that higher estradiol levels in older women are associated with better performance on tests of processing speed, sustained attention, and working memory [43].
Core Neuroimaging Modalities: Technical Principles and Applications
The selection of an appropriate neuroimaging modality is dictated by the specific research question, whether it pertains to brain network dynamics, molecular targets, or neuropathological burden. The following table summarizes the primary applications of each modality in the context of estradiol and cognitive research.
Table 1: Core Neuroimaging Modalities for Estradiol and Cognitive Research
| Modality | Primary Measured Signal | Key Applications in Estradiol Research | Spatial Resolution | Temporal Resolution |
|---|---|---|---|---|
| fMRI | Blood-Oxygen-Level-Dependent (BOLD) signal, reflecting hemodynamic changes | Mapping task-induced brain activation (e.g., during memory encoding/recall); assessing functional connectivity between brain networks [52]. | 1-3 mm | Seconds |
| PET | Concentration of a radiolabeled tracer targeting specific molecular pathways | Quantifying neuroreceptor density (e.g., serotonin, dopamine); measuring cerebral glucose metabolism (FDG-PET); imaging amyloid/tau pathology [53] [54]. | 4-5 mm | Minutes to Hours |
| SPECT | Gamma rays from a radiolabeled tracer, similar to PET | Dopamine transporter (DAT) imaging with DaTscan; cerebral blood flow perfusion [54]. | 7-10 mm | Minutes to Hours |
Functional Magnetic Resonance Imaging (fMRI)
fMRI is an indispensable tool for non-invasively mapping brain activity with high spatial resolution. Its utility in estradiol research lies in its ability to detect modulations in neural circuitry during cognitive task performance or at rest. The BOLD signal, while an indirect measure of neural activity, provides a robust correlate of regional brain engagement. For instance, quantitative meta-analyses of fMRI studies on cognitive control tasks, such as the antisaccade task, consistently reveal activation in a fronto-striatal-parietal network and the cerebellum [52]. Estradiol's influence can be investigated by examining how it modulates activation within these well-characterized networks during cognitive performance.
Positron Emission Tomography (PET)
PET imaging offers unparalleled capability for quantifying specific molecular and functional processes in the brain. Its role in estradiol research is multifaceted. FDG-PET, which measures the cerebral metabolic rate of glucose, is a sensitive marker for neurodegeneration, aiding in the differential diagnosis of dementias [53]. In the context of estradiol's neuroprotective effects, FDG-PET could be used to assess whether hormone therapy helps maintain neuronal metabolic integrity. Furthermore, Amyloid and Tau PET tracers allow for the in-vivo detection and quantification of Alzheimer's disease pathology [53]. This is particularly relevant given the link between post-menopausal estrogen decline and increased risk for Alzheimer's disease [16] [43]. Quantitative analysis of PET data is crucial, as it improves diagnostic accuracy and reporting confidence; for example, combining visual and quantitative analysis of FDG-PET increases sensitivity from 78% to 96% and specificity from 50% to 84% for detecting neurodegenerative patterns [54] [55].
Single-Photon Emission Computed Tomography (SPECT)
While similar to PET in its use of radiopharmaceuticals, SPECT is more widely available and often used for specific indications. DaTscan is a critical SPECT tool for imaging the integrity of the dopaminergic system, helping to differentiate Parkinsonian syndromes from essential tremor [54]. Given estradiol's known interactions with dopaminergic systems, DaTscan could be a valuable endpoint in studies investigating estradiol's role in motor and non-motor functions. Perfusion SPECT measures regional cerebral blood flow, which can show patterns characteristic of different dementias, though with generally lower resolution and diagnostic accuracy than FDG-PET [53] [54].
Methodological Workflow for Neuroimaging Experiments
A rigorous, standardized protocol is essential for generating reliable and reproducible neuroimaging data. The following diagram and workflow outline the key stages of a neuroimaging study, from design to data analysis.
Experimental Protocol: Linking Estradiol to Cognitive Performance via fMRI
Objective: To determine the effect of serum estradiol levels on prefrontal cortex activation during a working memory task.
Participant Characterization:
- Recruit postmenopausal women (e.g., aged ≥60 years) stratified by serum estradiol levels [43].
- Key Covariates: Measure and control for age, race/ethnicity, education level, hypertension, diabetes, and sleep disorders [43].
- Cognitive Assessment: Administer standardized cognitive tests such as the Digit Symbol Substitution Test (DSST) to assess processing speed and working memory prior to scanning [43].
Hormonal Assay:
- Collect venous blood after an overnight fast.
- Quantify serum estradiol levels using a high-sensitivity method such as isotope dilution liquid chromatography tandem mass spectrometry (ID-LC-MS/MS) [43].
fMRI Acquisition Parameters (Sample 3T Protocol):
- Sequence: T2*-weighted echo-planar imaging (EPI) for BOLD contrast.
- Voxel Size: 3.0 x 3.0 x 3.0 mm³ (or finer).
- Repetition Time (TR): 2000 ms.
- Task Design: Blocked or event-related design using an N-back working memory paradigm.
- Structural Scan: High-resolution T1-weighted MPRAGE for anatomical co-registration.
Data Analysis Workflow:
- Preprocessing: Realignment, slice-time correction, co-registration to structural scan, normalization to standard stereotactic space (e.g., MNI), and smoothing.
- First-Level Analysis: Model the BOLD response to the working memory task versus control condition for each participant, generating individual activation maps.
- Second-Level Analysis: Enter individual contrast images into a multiple regression model at the group level, with serum estradiol level as a continuous predictor, while including key covariates (e.g., age). Threshold the statistical map at p < 0.05, family-wise error (FWE) corrected.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Neuroimaging Studies
| Item / Reagent | Function / Role in Research | Example Use Case |
|---|---|---|
| ID-LC-MS/MS Assay | Gold-standard method for precise quantification of serum estradiol levels. | Stratifying research participants by hormonal status or using as a continuous variable in regression models with neuroimaging endpoints [43]. |
| FDG (Fludeoxyglucose) | PET radiopharmaceutical for measuring regional cerebral metabolic rate of glucose, a marker of neuronal function. | Identifying patterns of hypometabolism characteristic of Alzheimer's disease or frontotemporal dementia to investigate estradiol's neuroprotective effects [53]. |
| Amyloid PET Tracers | Radioligands (e.g., florbetapir, flutemetamol) that bind to beta-amyloid plaques in the brain. | Quantifying amyloid pathology in vivo to test if estradiol influences Alzheimer's disease pathology load [53]. |
| DaTscan (Ioflupane I-123) | SPECT radiopharmaceutical that binds to dopamine transporters in the striatum. | Assessing the integrity of the nigrostriatal pathway, which can be influenced by estradiol-dopamine interactions [54]. |
| Cognitive Test Batteries | Standardized pen-and-paper or computerized tests to quantify cognitive domains. | Providing behavioral correlates to neuroimaging data. The DSST, CERAD, and Animal Fluency tests are commonly used [43]. |
| Quantitative Analysis Software | Software tools (commercial or in-house) for processing and quantifying neuroimaging data. | Essential for generating objective metrics like SUVr for PET, or activation clusters for fMRI, improving diagnostic accuracy and statistical power [54]. |
Quantitative Data and Diagnostic Performance
The transition from qualitative assessment to quantitative imaging is a cornerstone of modern neuroimaging research, providing objective and reproducible endpoints.
Table 3: Diagnostic Performance of Visual vs. Quantitative Neuroimaging Analysis
| Scan Type | Analysis Method | Performance Metrics | Implication for Research |
|---|---|---|---|
| FDG PET [55] [56] | Visual Reporting Only | Sensitivity: 78-96%, Specificity: 50-59% | High false-positive rate limits clinical and research utility. |
| Visual + Quantitative | Sensitivity: 96-98%, Specificity: 73-84% | Marked improvement in accurately classifying disease states, enhancing statistical power in trials. | |
| Amyloid PET [52] [43] | Visual Reporting Only | Sensitivity: 80-85%, Specificity: 38-91% | Inconsistent and often poor specificity reported in some studies. |
| Visual + Quantitative | Sensitivity: 85-92%, Specificity: 91% | Consistently high accuracy, crucial for patient stratification in prevention trials. | |
| DaTscan [57] [16] | Visual Reporting Only | Inter-observer Agreement: 0.8; Accuracy: 79% | Significant variability between raters. |
| Visual + Quantitative | Inter-observer Agreement: 0.95; Accuracy: 86% | Greatly improved reproducibility and diagnostic confidence. |
Integrating Neuroimaging Endpoints into a Thesis on Estradiol
To effectively frame neuroimaging endpoints within a thesis on the hormonal mechanisms of estradiol, consider the following integrative model:
This model posits that estradiol exerts its effects on cognition through multiple neural mechanisms, which can be quantified using specific neuroimaging endpoints. For example:
- Estradiol's rapid membrane actions and influence on synaptic plasticity could be measured via fMRI during a cognitive challenge, testing for enhanced activation or connectivity in prefrontal-hippocampal circuits [16].
- Its neuroprotective effects against Alzheimer's pathology could be assessed by investigating the correlation between serum estradiol levels and Amyloid PET burden in a cohort of older women [53] [43].
- The decline in estradiol levels after menopause is associated with measurable cognitive changes, such as reduced processing speed and working memory (as measured by the DSST), providing a direct behavioral link that neuroimaging can help explain mechanistically [43].
In conclusion, fMRI, PET, and SPECT provide a powerful suite of tools for quantifying the biological impact of estradiol on the brain. By employing rigorous experimental protocols and quantitative analysis methods, researchers can move beyond correlations to establish causal mechanisms, thereby strengthening the evidence base for the role of estradiol in cognitive health and disease.
Navigating Complexities: Timing, Formulation, and Individual Factors in Therapy
The Critical Window Hypothesis posits that the neuroprotective and cognitive effects of menopausal hormone therapy (MHT) are critically dependent on the timing of initiation relative to menopause onset [58] [59]. This concept, also known as the "critical period" or "timing" hypothesis, suggests that a finite window of opportunity exists—typically within 10 years of menopause or before age 60—during which estrogen-containing therapies can confer cognitive benefits and potentially reduce Alzheimer's disease risk [59]. Initiation beyond this window appears neutral or potentially detrimental to cognitive health [58] [60].
This hypothesis provides a compelling framework for reconciling contradictory findings between early observational studies (which suggested protective effects) and the Women's Health Initiative Memory Study (WHIMS), which found increased dementia risk with MHT initiation in women aged 65 and older [58] [60]. The biological rationale centers on the concept of "healthy cell bias"—that estrogen benefits neurons that remain healthy but may adversely affect those already compromised by age-related pathology [59] [60]. This whitepaper examines the mechanistic foundations, clinical evidence, and methodological approaches for investigating this critical period for estrogen's effects on cognitive performance.
Biological Mechanisms Underlying the Critical Window
Estradiol Signaling Pathways in the Brain
Estradiol exerts its effects on cognition through multiple complementary mechanisms that vary in their temporal dynamics. The hormone operates through both genomic and non-genomic pathways to influence neuronal function, with the prefrontal cortex and hippocampus—regions critical for memory and executive function—serving as primary targets [16] [59].
Genomic signaling involves classical nuclear estrogen receptors (ERα and ERβ) that function as ligand-dependent transcription factors. Upon estrogen binding, these receptors dimerize and bind to estrogen response elements (EREs) in target genes, initiating cascades that alter protein synthesis and produce long-lasting changes in neural function [16]. These mechanisms likely underlie estrogen's roles in sexual differentiation during development and functional changes across the menstrual cycle, pregnancy, and menopause.
Non-genomic signaling occurs rapidly (seconds to minutes) through membrane-associated estrogen receptors that activate intracellular signaling pathways, including MAPK/ERK and PI3K/Akt [16] [61]. This rapid signaling enhances synaptic plasticity and consolidates memory formation through mechanisms independent of gene transcription. More recently, intra-neuronal estradiol synthesis has been identified, suggesting estradiol may also function as a neurosteroid to promote memory through local production within the hippocampus and prefrontal cortex [16] [61].
Neuroprotective Effects of Estrogen
Estradiol promotes multiple neuroprotective mechanisms that collectively support cognitive function. These include enhancing synaptic plasticity through increased dendritic spine density and synapse formation in hippocampal and cortical regions [16] [59]. The hormone also supports neurogenesis in the dentate gyrus of the hippocampus and provides metabolic support by maintaining mitochondrial function and promoting cerebral glucose utilization [16]. Additionally, estradiol reduces Alzheimer's pathology by decreasing β-amyloid production and accumulation and modulates cerebrovascular function by enhancing cerebral blood flow and reducing vascular inflammation [62] [59].
The critical window emerges because these beneficial mechanisms operate most effectively on neurons that remain structurally and metabolically healthy. With advancing age and prolonged estrogen deprivation, neurons accumulate pathological changes that may render them unresponsive or vulnerable to estrogen's effects [59] [60]. This explains the time-dependent nature of MHT efficacy—early intervention preserves neuronal health, while later intervention may adversely affect already compromised neural systems.
Clinical Evidence and Research Findings
Key Observational Studies and Randomized Trials
The clinical evidence base for the Critical Window Hypothesis derives from numerous observational studies and randomized controlled trials conducted across different timing scenarios. The table below summarizes the design and findings of pivotal studies in this domain.
Table 1: Key Clinical Studies on Critical Window Hypothesis and Cognitive Outcomes
| Study Name | Design | Participants | Timing of Initiation | Key Cognitive Findings | Reference |
|---|---|---|---|---|---|
| WHIMS (Women's Health Initiative Memory Study) | RCT | Women aged ≥65 years | Late initiation (≥65 years) | Increased risk of all-cause dementia; no cognitive benefit | [58] [60] |
| Cache County Study | Observational | Women aged ≥73 years | Varied timing | Former users showed reduced AD risk; current users only benefited with ≥10 years use | [58] |
| KEEPS (Kronos Early Estrogen Prevention Study) | RCT | Women within 3 years of menopause | Early initiation (within 3 years of menopause) | No harm to cognition; modest mood benefits | [59] |
| ELITE (Early vs Late Intervention Trial with Estradiol) | RCT | Early (within 6 years) vs Late (≥10 years) postmenopause | Early vs Late postmenopause | Early initiation associated with beneficial Aβ biomarker changes | [62] |
| NHANES Analysis | Cross-sectional | Women ≥60 years | Natural variation in estradiol | Higher estradiol levels associated with better processing speed and working memory | [43] |
Recent biomarker studies provide mechanistic insights into these clinical observations. Data from the ELITE trial demonstrate that oral 17β-estradiol initiated early in postmenopause significantly accelerated the decline in amyloid-β40 compared with placebo, with more pronounced effects in early postmenopausal women and ApoE4 carriers [62]. Neuroimaging studies further support the biological plausibility of the critical window, showing enhanced hippocampal and prefrontal structure in early MHT initiators but increased tau and amyloid pathology in late initiators [59].
Impact of Formulation and Menopause Type
The cognitive effects of MHT vary significantly by formulation and type of menopause. Estrogen-only regimens appear most protective when initiated early, while continuous conjugated equine estrogen/medroxyprogesterone acetate (CEE/MPA) has shown increased dementia risk regardless of timing [58] [59]. The type of menopause also influences this relationship, with surgical menopause representing a particularly compelling scenario for early intervention. The abrupt estrogen withdrawal following oophorectomy creates a pronounced neuroendocrine challenge, and initiating MHT near the time of surgery appears to mitigate associated cognitive risks, especially in younger women [59] [60].
Table 2: Formulation and Menopause Type Effects on Critical Window
| Factor | Early Initiation Effect | Late Initiation Effect | Clinical Implications |
|---|---|---|---|
| Estrogen-Only Therapy | Potential cognitive benefit and reduced AD risk | Neutral or slightly increased risk | Most favorable profile for cognitive protection |
| CEE/MPA Combination | Increased risk of cognitive decline | Increased dementia risk | Unfavorable profile regardless of timing |
| Surgical Menopause | Strong evidence for cognitive protection | Limited benefit | Clear indication for early intervention |
| Natural Menopause | Modest cognitive benefits possible | Neutral or adverse effects | Individualize based on symptom burden |
Methodological Approaches for Critical Window Research
Experimental Protocols and Assessment Methods
Investigating the Critical Window Hypothesis requires sophisticated methodological approaches spanning molecular analyses, neuroimaging, and cognitive assessment. The following experimental workflow represents a comprehensive approach for evaluating timing effects in both clinical and preclinical settings.
Hormone Assessment Methodologies
Accurate assessment of hormonal status is fundamental to critical window research. The following protocols detail standardized approaches for measuring key hormonal biomarkers.
Serum Estradiol Measurement via ID-LC-MS/MS
- Sample Collection: Venipuncture performed morning after overnight fast
- Processing: Serum separation, storage at -80°C until analysis
- Analysis Method: Isotope dilution liquid chromatography tandem mass spectrometry (ID-LC-MS/MS) [63] [43]
- Quality Control: Use of standards provided by CDC for routine analysis
- Data Interpretation: Values typically categorized into tertiles for analysis (e.g., T1: <3.68 pg/mL, T2: 3.68-7.49 pg/mL, T3: >7.49 pg/mL) [43]
Comprehensive Menopausal Biomarker Panel
- FSH Measurement: Immunoassay of serum samples with elevated levels indicating menopausal status
- AMH Assessment: Measured as marker of ovarian reserve, with low/non-detectable levels indicating perimenopausal or postmenopausal status [63]
- Additional Steroid Hormones: Estrone, progesterone, testosterone, DHEA via mass spectrometry
- Hypothalamic-Pituitary Markers: Gene expression analysis of CYP19A1 (aromatase), ESR1/ESR2, GPER1, and GNRHR in postmortem tissue [63]
Cognitive Assessment Protocols
Standardized cognitive assessment is critical for evaluating MHT effects across domains vulnerable to aging and menopause-related changes.
CERAD Word List Learning Test
- Domain Assessed: Verbal learning and memory
- Administration: Three learning trials of 10 unrelated words, delayed recall after 8-10 minutes
- Scoring: Total immediate recall (0-30), delayed recall (0-10), recognition discrimination
- Procedure: Words presented visually or audibly at 2-second intervals, immediate recall after each trial, interference task before delayed recall [43]
Digit Symbol Substitution Test (DSST)
- Domain Assessed: Processing speed, sustained attention, working memory
- Administration: 2-minute timed test matching symbols to numbers using key
- Scoring: Number of correct matches (0-133)
- Procedure: Participants shown key with numbers 1-9 paired with symbols, must fill in corresponding symbols for 133 random numbers [43]
Animal Fluency Test (AFT)
- Domain Assessed: Semantic memory, executive function, language production
- Administration: 1-minute generation of animal names
- Scoring: Total correct animals named, excluding repetitions or errors
- Procedure: Instructions to name as many different animals as possible within time limit [43]
Research Tools and Reagent Solutions
Table 3: Essential Research Reagents for Critical Window Investigations
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Hormone Assays | ID-LC-MS/MS for estradiol; Immunoassays for FSH, LH, AMH | Quantifying circulating hormone levels | CDC-standardized methods preferred for estradiol; establish lab-specific reference ranges |
| Molecular Biology Reagents | qPCR kits for ESR1, ESR2, CYP19A1; RNA extraction kits | Gene expression analysis in target tissues | Use postmortem hypothalamic/pituitary tissue when possible [63] |
| Cognitive Assessment Tools | CERAD, DSST, Animal Fluency tests | Standardized cognitive phenotyping | Administer in fixed order with standardized instructions [43] |
| Neuroimaging Biomarkers | fMRI, amyloid-PET, tau-PET, structural MRI | Assessing brain structure, function, and pathology | Focus on hippocampal-prefrontal networks; analyze network instability [64] [59] |
| Alzheimer Biomarker Assays | Aβ40, Aβ42, p-tau181, GFAP, NfL measurements | Quantifying Alzheimer-related pathology | Plasma-based assays now available for large-scale screening [62] |
| Cell Culture Models | Primary neuronal cultures, hormone treatment protocols | Mechanistic studies of estrogen signaling | Include timing variables relative to differentiation state |
| Animal Models | Ovariectomized rodents, non-human primates | Controlled intervention timing studies | Surgical menopause models particularly relevant [16] |
The Critical Window Hypothesis represents a paradigm shift in understanding how timing fundamentally shapes MHT's effects on cognitive outcomes. Converging evidence from molecular studies, neuroimaging, biomarker analyses, and cognitive testing indicates that early initiation of estrogen-containing therapies—particularly within 10 years of menopause or before age 60—may confer neuroprotective benefits, while later initiation shows reduced efficacy or potential harm.
The biological mechanisms underlying this temporal pattern involve the changing responsiveness of neural systems to estrogen's genomic and non-genomic signaling, influenced by the accumulating pathologies of brain aging. Methodological advances in hormone assessment, cognitive testing, and biomarker measurement now enable more precise investigation of these timing effects.
For researchers and drug development professionals, these findings highlight the importance of considering menopausal timing as a critical variable in clinical trial design and therapeutic development. Future research should focus on refining optimal timing windows for specific formulations, identifying genetic and biological factors that modify timing effects, and developing targeted interventions that capitalize on estrogen's neuroprotective mechanisms during the critical window of maximum benefit.
The cognitive consequences of menopausal hormone therapy (MHT) are domain-specific and critically dependent on administration route. This whitepaper synthesizes recent clinical evidence and underlying neurobiological mechanisms to explain why transdermal estradiol preferentially enhances episodic memory, while oral administration shows greater benefit for prospective memory. We present a unified model grounded in first-pass hepatic metabolism, blood-brain barrier dynamics, and region-specific estrogen receptor distribution. Supported by quantitative data from large-scale clinical studies and detailed experimental protocols, this analysis provides a framework for precision medicine approaches in cognitive aging and informs targeted drug development for postmenopausal women.
Estradiol (E2), the most potent endogenous estrogen, exerts profound effects on brain regions critical for learning and memory. Cognitive domains are not uniformly sensitive to hormonal modulation; rather, their differential reliance on distinct neural substrates and receptor populations creates a landscape of selective vulnerability and enhancement [16]. Episodic memory—the ability to recall personal experiences and context-rich events—depends heavily on the integrity of the medial temporal lobe, particularly the hippocampus [65]. In contrast, prospective memory—remembering to perform intended actions in the future—relies on a fronto-parietal network that supports planning, monitoring, and cue detection [66]. The route of estradiol administration emerges as a critical determinant of cognitive outcomes by fundamentally altering hormone bioavailability and distribution to these specialized brain networks.
Clinical Evidence: Route-Dependent Cognitive Effects
Large-Scale Cohort Findings
Analysis of the Canadian Longitudinal Study on Aging (CLSA) baseline data provides compelling evidence for route-specific cognitive enhancement. The cohort included 7,251 postmenopausal women (mean age 60.5 ± 10.2 years) with comprehensive cognitive assessment and MHT history [8] [67].
Table 1: Association between E2-based MHT Administration Route and Cognitive Domain Performance
| Cognitive Domain | Administration Route | Effect Size (Cohen's d) | Statistical Significance | Comparison Group |
|---|---|---|---|---|
| Episodic Memory | Transdermal E2 | 0.303 | p = 0.007 | Never MHT users |
| Prospective Memory | Oral E2 | 0.283 | p = 0.015 | Never MHT users |
| Executive Functions | Neither route | Not significant | p = 0.345 | Never MHT users |
The dissociation is clear: transdermal estradiol significantly enhanced episodic memory, while oral administration benefited prospective memory. Neither route produced significant effects on executive functions, demonstrating domain selectivity rather than global cognitive enhancement [8].
Impact of Menopause Timing and Individual Factors
Beyond administration route, menopause timing significantly influences cognitive outcomes. Earlier age at menopause was associated with lower performance across all domains (episodic memory β = 0.050, p < 0.001; prospective memory β = 0.047, p < 0.001; executive functions β = 0.061, p < 0.001) [8]. This effect was particularly pronounced for executive functions in women with grand parity (4+ children β = 0.215, p < 0.001) and APOE ε4 carriers (β = 0.070, p < 0.001), highlighting the importance of individual risk profiles [8].
Metabolic Mechanisms: First-Pass Hepatic Metabolism
The route-dependent cognitive effects stem from fundamental differences in estradiol metabolism and bioavailability.
Oral Administration Pathway
Oral estradiol undergoes extensive first-pass hepatic metabolism after absorption from the gastrointestinal tract [8]. The liver converts a significant portion of estradiol (E2) to estrone (E1) and estrone sulfate via the cytochrome P450 system, resulting in an unnatural E2:E1 ratio that favors the less potent estrone [8]. This hepatic processing also stimulates the synthesis of sex hormone-binding globulin (SHBG), further reducing bioavailable estradiol through increased protein binding [8]. The resulting hormonal profile that reaches cerebral circulation is characterized by lower E2 bioavailability and altered estrogenic potency.
Transdermal Administration Pathway
Transdermal delivery bypasses hepatic first-pass metabolism entirely. Estradiol absorbed through the skin enters the systemic circulation directly, maintaining physiological E2:E1 ratios and avoiding induction of SHBG production [8]. This route preserves estradiol potency and results in higher bioavailable E2 concentrations in cerebral circulation.
Table 2: Pharmacokinetic Differences Between Administration Routes
| Parameter | Oral Estradiol | Transdermal Estradiol |
|---|---|---|
| First-Pass Metabolism | Extensive | Negligible |
| E2:E1 Ratio | Low (E1 > E2) | Physiological (E2 > E1) |
| SHBG Induction | Significant | Minimal |
| Bioavailable E2 | Reduced | Higher |
| Hepatic Impact | Significant | Negligible |
Neural Substrates and Receptor Distribution
The domain-specific cognitive effects reflect differential estrogen receptor distribution and region-specific neuroplasticity mechanisms.
Episodic Memory: Hippocampal Vulnerability and Protection
The hippocampus, rich in both estrogen receptor alpha (ERα) and beta (ERβ), is particularly responsive to estradiol modulation [16]. Estradiol enhances hippocampal neuroplasticity through multiple mechanisms: increased spine density, potentiation of glutamatergic transmission, and promotion of long-term potentiation [16]. Transdermal estradiol, with its superior delivery of bioactive E2 to the hippocampus, provides greater support for these plasticity mechanisms. Animal models demonstrate that subcutaneous E2 administration (similar to transdermal in humans) specifically regulates hippocampal structure and function, while conjugated equine estrogens (CEEs, primarily estrone) may actually reduce hippocampal neuroplasticity at certain doses [8] [16].
Prospective Memory: Fronto-Parietal Network Engagement
Prospective memory relies on the frontal lobes for intention maintenance and the parietal cortex for cue detection [66] [68]. The frontal cortex shows increased ER density after menopause, potentially enhancing its sensitivity to hormonal modulation [8]. Oral estradiol, despite its altered metabolic profile, may provide sufficient receptor activation to support the fronto-parietal networks underlying prospective memory. The cognitive operations involved—cue detection, intention retrieval, and task coordination—align with the functions of these estrogen-sensitive regions.
Diagram 1: Metabolic and Cognitive Pathways of Oral vs. Transdermal Estradiol
Experimental Protocols and Methodologies
Large-Scale Cohort Study Design
The Canadian Longitudinal Study on Aging (CLSA) methodology provides a robust framework for investigating hormone-cognition relationships [8] [67]:
Participant Recruitment:
- 7,251 postmenopausal women from a population-based observational cohort
- Age range: 45-85 years at baseline
- Exclusion criteria: significant cognitive impairment preventing independent interview completion
Cognitive Domain Assessment:
- Episodic Memory: Measured using the Consortium to Establish a Registry for Alzheimer's Disease (CERAD) word list learning test, assessing immediate recall, delayed recall, and recognition [43]
- Prospective Memory: Assessed through both time-based (remembering at specific times) and event-based (remembering in response to cues) paradigms [66]
- Executive Functions: Evaluated using the Mental Alternation Test, assessing cognitive flexibility and working memory
Hormone Therapy Classification:
- Current E2-based MHT users categorized by administration route: oral vs. transdermal
- Never-users of any MHT form as comparison group
- Adjustment for covariates: age, education, vascular risk factors, body mass index
Statistical Analysis:
- Linear regression models testing association between cognitive performance and menopause variables
- Effect modification analysis for APOE ε4 status and parity
- Class III evidence classification for clinical implications
Serum Estradiol Measurement Protocol
Cross-sectional studies examining endogenous estradiol-cognition relationships employ precise hormone assessment methods [43]:
Blood Collection and Processing:
- Morning venipuncture after overnight fast
- Serum separation via centrifugation at appropriate g-force
- Storage at -80°C until analysis
Estradiol Quantification:
- Method: Isotope dilution liquid chromatography tandem mass spectrometry (ID-LC-MS/MS)
- Laboratory: CDC Division of Laboratory Sciences (standardized protocol)
- Sensitivity: Detection limits sufficient for low postmenopausal levels
- Quality control: Internal standards and replicate samples
Cognitive Assessment Battery:
- CERAD: Verbal learning subtest with immediate and delayed recall
- Animal Fluency Test (AFS): Semantic category fluency measuring executive function and language
- Digit Symbol Substitution Test (DSST): Processing speed, sustained attention, and working memory
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Hormone-Cognition Studies
| Reagent/Material | Specific Application | Function/Rationale |
|---|---|---|
| ID-LC-MS/MS System | Serum estradiol quantification | Gold standard for sensitive and specific hormone measurement in low postmenopausal ranges [43] |
| L1CAM Antibody | Neural-derived exosome isolation | Immunoabsorption purification of neuron-specific extracellular vesicles for biomarker studies [69] |
| CERAD Word List | Episodic memory assessment | Standardized verbal learning test with established normative data for older adults [43] |
| Prospective Memory Task | Event- and time-based PM assessment | Computerized or paper-pencil tasks embedding intentions in ongoing activities [66] |
| APOE Genotyping Kit | Genetic risk stratification | Identification of ε4 allele carriers as effect modifiers in hormone-cognition relationships [8] |
| SHBG ELISA Kit | Bioavailable hormone estimation | Measurement of sex hormone-binding globulin to calculate free estradiol index [70] |
Implications for Research and Drug Development
The route-dependent dissociation of cognitive effects has profound implications for therapeutic development. First, the critical period hypothesis suggests that timing of initiation relative to menopause onset significantly influences outcomes [16]. Second, individual characteristics including APOE genotype, reproductive history, and cognitive status modulate treatment response [8]. Third, formulation specificity must be considered, as conjugated equine estrogens (CEEs) have demonstrated fewer cognitive benefits than estradiol-based preparations [8].
Future research should prioritize:
- Mechanistic studies linking administration route to region-specific brain changes using neuroimaging
- Personalized approaches incorporating genetic, hormonal, and cognitive profiling
- Formulation optimization to maximize target engagement in specific neural networks
- Combination therapies leveraging route-specific advantages for multi-domain cognitive protection
The administration route of estradiol-based menopausal hormone therapy fundamentally determines its cognitive domain specificity through distinct metabolic pathways and neural targeting. Transdermal estradiol, preserving bioactive E2, preferentially enhances hippocampal-dependent episodic memory, while oral administration, despite hepatic conversion, sufficiently engages fronto-parietal networks to benefit prospective memory. This dissociation underscores the necessity of route consideration in both clinical management and pharmaceutical development. A precision medicine approach that accounts for administration route, menopause timing, genetic profile, and individual cognitive vulnerabilities will optimize therapeutic outcomes for postmenopausal women.
Within the broader investigation into the hormonal mechanisms of estradiol on cognitive performance, a critical frontier lies in understanding why individuals respond differently to hormonal influences. It is well-established that estradiol modulates cognitive function through diverse mechanisms, including genomic actions and rapid membrane-initiated signaling, enhancing processes like memory consolidation [16]. However, clinical and observational studies reveal significant heterogeneity in cognitive outcomes. This variability underscores the importance of moderating factors—variables that systematically alter the strength or direction of the relationship between estradiol exposure and cognitive performance [71]. This review synthesizes evidence on three key moderators—APOE ε4 genotype, reproductive history (particularly parity), and overall health status. We examine how these factors interact with estradiol's mechanisms to shape cognitive trajectories, with the aim of informing more precise, personalized approaches to cognitive health in women.
Estradiol's Mechanisms of Cognitive Action: A Primer
Estradiol, the primary form of estrogen, exerts multifaceted effects on the brain through several distinct but interconnected mechanisms. A comprehensive understanding of these mechanisms provides the necessary context for appreciating how moderating factors influence cognitive outcomes.
Genomic and Non-Genomic Signaling Pathways
The classical model of estradiol action involves genomic signaling. Estradiol binds to intracellular estrogen receptors (ERα and ERβ), which then function as ligand-dependent transcription factors, dimerize, and bind to estrogen response elements (EREs) on DNA to initiate gene transcription and protein synthesis [16]. This process underlies long-lasting organizational and developmental effects on neural circuits.
Complementing this slow-onset pathway, estradiol also initiates rapid, non-genomic signaling through membrane-associated estrogen receptors (mERs). These receptors, located in cell bodies, spines, and presynaptic terminals, activate intracellular signaling cascades, such as the MAPK and PI3K/Akt pathways, within seconds to minutes [16]. This rapid modulation is crucial for synaptic plasticity and the acute enhancement of memory consolidation. Furthermore, emerging evidence suggests estradiol can be synthesized locally within the brain, acting as a neurosteroid to influence cognition independently of peripheral gonadal sources [16].
The following diagram illustrates the core pathways through which estradiol signals in the brain to influence cognitive function:
Neuroimaging Evidence of Estradiol's Effects
Functional neuroimaging studies in humans provide compelling evidence for estradiol's impact on brain regions critical for cognition. Several studies show that estrogen therapy enhances activation in the hippocampus and parahippocampal gyrus during the retrieval stage of episodic memory tasks [44]. For instance, one O-15 water PET study found that women on hormone therapy (HT) showed increased cerebral blood flow in the inferior frontal cortex and parahippocampal gyrus during verbal and figural memory recognition compared to non-users [44]. A subsequent longitudinal study from the same cohort further demonstrated that HT users exhibited increased blood flow over time to the right hippocampus and right entorhinal cortex during verbal recognition, correlating with better memory performance [44]. Estradiol also modulates prefrontal cortex function, particularly during tasks involving executive function and working memory manipulation [44]. These neural effects translate to behavioral improvements, especially in verbal episodic memory, a cognitive domain sensitive to hormonal changes and predictive of Alzheimer's disease risk [44].
Key Moderating Factors in Estradiol-Cognition Research
APOE ε4 Genotype
The APOE ε4 allele is the strongest common genetic risk factor for sporadic Alzheimer's disease. Its interaction with estradiol and lifestyle factors creates a complex moderating landscape.
- Moderating Role: APOE ε4 genotype moderates the relationship between physical activity and cognitive decline. While ε4 carriers show steeper cognitive decline, higher levels of physical activity, particularly walking, significantly slow this decline, with effects varying by race and sex [72].
- Interaction with Hormone Therapy: The APOE ε4 genotype may also moderate the response to hormone therapy (HT). Some studies suggest that the cognitive benefits of HT, particularly in verbal memory, are more pronounced in non-carriers of the APOE ε4 allele [73]. However, other large-scale studies, such as those in the UK Biobank, have found that while APOE ε4 was independently associated with reduced processing speed and executive function, it did not significantly influence the associations between various female-specific reproductive factors and cognition [73]. This indicates that the moderating effect of APOE ε4 might be specific to certain interventions like HT rather than a universal modifier of all hormonal associations.
Table 1: APOE ε4 as a Moderator of Physical Activity and Hormone Therapy Effects on Cognition
| Moderated Relationship | Nature of Moderation | Key Findings | Study Population |
|---|---|---|---|
| Physical Activity → Cognitive Decline | Strength & Specificity of Effect | Walking slowed decline in DSST (executive function/speed) in ε4 carriers: Black women (β=.39), White women (β=.60), White men (β=.45). Walking also slowed decline in global cognition (3MS), with greater effects in Black patients [72]. | Older Black & White adults (Health ABC Study) [72] |
| Hormone Therapy → Cognitive Performance | Presence & Direction of Effect | HT use reduced risk of low cognitive performance almost by half compared to never-users, but only in APOE ε4 non-carriers [73]. | Middle-aged & older women (Nurses' Health Study) [73] |
| Female-Specific Factors (e.g., reproductive span) → Cognition | Lack of Significant Moderation | APOE ε4 was associated with worse processing speed/executive function but did not modify the associations between reproductive history, hormone use, and cognition [73]. | 221,124 women from UK Biobank [73] |
Parity (Reproductive History)
A woman's history of childbirths, or parity, is a significant life experience with long-term implications for hormonal exposure and cognitive aging.
- Moderating Role: Parity moderates the relationship between physical activity and cognitive health in later life. The positive association between self-reported walking and cognitive performance is strongest among women at risk for cognitive decline, specifically nulliparous women (those who have never given birth) and grand multiparous women (those with a high number of births) [72].
- Association with Cognition: Beyond its moderating role, parity itself is associated with cognitive outcomes. A longer reproductive span, older age at menopause, and older age at first and last birth are generally associated with better cognitive performance later in life [73]. The relationship between the number of live births and cognition appears non-linear, with some studies suggesting that having two children is associated with the best outcomes compared to having no, one, or three or more children [73].
Table 2: Parity as a Moderator and Independent Factor in Cognitive Aging
| Aspect of Parity | Role | Key Findings | Study/Source |
|---|---|---|---|
| Parity Group | Moderator of Physical Activity → Cognition | The positive relationship between physical activity and cognitive performance (3MS, DSST) was only significant in nulliparous and grand multiparous women [72]. | Barha et al., 2023 (Health ABC Study) [72] |
| Number of Live Births | Independent Factor / Non-linear association | Compared to two children, having no, one, or three or more children is linked to poorer performance in verbal memory and executive function [73]. | Read & Grundy, 2017 [73] |
| Reproductive Span | Independent Factor | A longer reproductive span (menarche to menopause) is positively associated with cognitive performance later in life [73]. | UK Biobank Study [73] |
| Hormonal Contraceptive Use | Independent Factor | A history of hormonal contraceptive use shows one of the strongest positive associations with late-life cognition (max Cohen's d = 0.1) [73]. | UK Biobank Study [73] |
Health Status and Lifestyle Factors
General health and modifiable lifestyle factors constitute a third category of moderators, influencing the cognitive reserve and the brain's resilience to age-related decline.
- Moderating Role: Overall health status, often quantified through composite lifestyle scores, can moderate the impact of genetic risk on brain health. A cross-sectional study using UK Biobank MRI data found that both the presence of an APOE ε4 allele and non-favourable lifestyles were independently associated with worse brain health markers, including smaller grey matter and hippocampal volumes [74]. However, the interaction between lifestyle and APOE ε4 status on these brain metrics was generally non-significant, suggesting an additive rather than a synergistic (multiplicative) model [74]. This means a healthy lifestyle benefits brain health regardless of genetic risk.
- Specific Health Conditions: Comorbidities like hypertension, diabetes, and sleep disorders are often included as covariates in studies of estradiol and cognition, as they are known to influence cognitive function independently [43]. Their role as potential moderators of estradiol's effects warrants further investigation.
The following diagram synthesizes how these three key moderating factors interact with estradiol's pathways to influence cognitive outcomes:
Experimental Protocols for Investigating Moderation
Assessing Moderation via Multiple Regression
Testing for moderating effects is typically accomplished through moderated multiple regression (MMR) [75] [71]. The following protocol outlines the key steps for a robust moderation analysis involving continuous and categorical variables.
Protocol Steps:
- Variable Preparation: For continuous independent variables (X) and moderators (M), it is often recommended to center the variables (subtract the sample mean from each score) to reduce multicollinearity and aid interpretation. Categorical moderators (e.g., APOE ε4 carrier vs. non-carrier) should be appropriately coded (e.g., dummy coding) [71].
- Create Interaction Term: Generate a new variable that is the product of the centered independent variable and the centered moderator variable (
X_c * M_c) [75] [71]. - Hierarchical Regression Analysis:
- Interpret the Interaction: A statistically significant coefficient (
b₃) for the interaction term indicates a moderation effect. The sign and magnitude ofb₃indicate how the moderator changes the relationship [71]. - Probe Significant Interactions: If the interaction is significant, conduct simple slopes analysis to determine the relationship between X and Y at specific levels of the moderator (e.g., at the mean, and ±1 standard deviation from the mean for continuous moderators) [71]. Plotting these interactions is crucial for interpretation.
Cognitive and Biomarker Assessment Protocols
Cognitive Domain Assessment: Research in this field typically focuses on specific cognitive domains sensitive to hormonal and genetic influences:
- Executive Function/Processing Speed: Often measured by the Digit Symbol Substitution Test (DSST) [72] [43].
- Global Cognition: Often measured by the Modified Mini-Mental State Examination (3MS) [72].
- Verbal Episodic Memory: Assessed using tests like the CERAD Word Learning Test (immediate and delayed recall) [43] [44].
- Verbal Fluency: Assessed using tests like the Animal Fluency Test (AFS) [43].
Biomarker Measurement:
- Serum Estradiol: Measured using high-sensitivity methods like isotope dilution liquid chromatography tandem mass spectrometry (ID-LC-MS/MS) to accurately capture low postmenopausal levels [43].
- APOE Genotyping: Conducted via standard genetic analysis from blood or saliva samples.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Research on Estradiol, Cognition, and Moderating Factors
| Item Name | Function/Application | Technical Notes |
|---|---|---|
| ID-LC-MS/MS | Quantification of low serum estradiol levels in postmenopausal women. | Gold standard for sensitivity and specificity. Essential for accurately measuring low hormone levels in older cohorts [43]. |
| APOE Genotyping Kit | Determination of APOE ε2, ε3, ε4 allele status from DNA. | Critical for stratifying participants by genetic risk. Standard PCR-based methods are widely used. |
| Cognitive Test Batteries | Assessment of domain-specific cognitive function (e.g., memory, executive function). | Standardized tests like DSST, 3MS, and CERAD are validated for large-scale epidemiological studies [72] [43]. |
| Structural & Functional MRI | Measurement of brain volume (e.g., hippocampus) and functional activation during cognitive tasks. | fMRI probes neural targets of estradiol (hippocampus, PFC). Structural MRI quantifies atrophy related to APOE ε4 and lifestyle [74] [44]. |
| Centered Variables & Interaction Term | Statistical control of multicollinearity in moderated multiple regression. | Created by subtracting the mean from raw scores (X, M) before forming the product term (X*M) for regression analysis [75] [71]. |
The journey to fully elucidate the hormonal mechanisms of estradiol on cognitive performance must account for the critical influence of moderating factors. Evidence indicates that APOE ε4 genotype moderates the effectiveness of both lifestyle interventions and possibly hormone therapy, while parity defines subgroups of women who derive differential cognitive benefit from physical activity. General health and lifestyle further contribute additively to brain health outcomes, sometimes independently of genetic risk. The implication for researchers and drug development professionals is clear: a one-size-fits-all approach is untenable. Future research must prioritize large, diverse cohorts and integrate multimodal data—genetic, hormonal, lifestyle, and neuroimaging—to disentangle these complex interactions. Embracing this nuanced, personalized science is paramount for developing effective strategies to mitigate cognitive aging and reduce the risk of dementia in women.
In the investigation of hormonal mechanisms, particularly the effects of estradiol on cognitive performance, the ability to draw valid causal inferences is paramount. Confounding variables represent a fundamental threat to the internal validity of observational and experimental research, often creating spurious associations or masking true effects. A confounder is a variable that is associated with both the exposure (e.g., estradiol therapy) and the outcome (e.g., cognitive performance), but is not part of the causal pathway between them [76] [77]. In the specific context of estradiol research, failing to adequately address confounding can lead to erroneous conclusions about therapeutic efficacy, safety profiles, and underlying biological mechanisms, ultimately hampering drug development efforts.
The challenging nature of this field is exemplified by a recent 2025 Class III evidence study which found that while both earlier age at menopause and the type of estradiol-based hormone therapy (HT) were associated with cognitive performance, causality could not be established due to the cross-sectional, observational nature of the evidence [25]. This highlights the critical need for rigorous methodological approaches to confounding control throughout the research process—from initial study design to final statistical analysis—to advance our understanding of estradiol's effects on cognitive health.
Theoretical Framework: Categories and Characteristics of Confounders
Defining Confounding in Hormone and Cognitive Research
Confounding occurs when the observed association between an exposure and outcome is distorted by the mixing of effects with an extraneous factor [76]. A true confounding variable must satisfy three specific conditions: (1) it must be independently associated with the outcome, (2) it must be associated with the exposure, and (3) it must not be an intermediate between exposure and outcome [76] [77]. In estradiol-cognition research, this manifests when a variable influences both a woman's likelihood of receiving hormone therapy and her cognitive performance through pathways separate from the hormone treatment itself.
A special case particularly relevant to therapeutic research is confounding by indication, where the clinical indication for prescribing a treatment is itself associated with the outcome [76]. For example, if women with more severe menopausal symptoms (who may have different baseline cognitive profiles) are preferentially prescribed transdermal rather than oral estradiol, any observed cognitive differences between administration routes could be confounded by this initial clinical presentation.
Major Confounder Categories in Estradiol-Cognition Research
Table 1: Categories of Confounding Variables in Estradiol and Cognitive Research
| Category | Key Variables | Research Impact | Examples from Literature |
|---|---|---|---|
| Socioeconomic Factors | Education, income, occupation, healthcare access | Influences cognitive reserve, health behaviors, and treatment access | Education adjusted for in CLSA study of menopause age and cognition [25] |
| Lifestyle Factors | Smoking, physical activity, diet, alcohol use, cognitive engagement | Directly affects neuroplasticity, cardiovascular health, and estrogen metabolism | Vascular risk factors adjusted for in estradiol-cognition association research [25] |
| Comorbidities & Health Status | Vascular conditions, diabetes, depression, inflammatory disorders | Impacts brain health through multiple physiological pathways | Comorbidity distinctions crucial for understanding disease interactions [78] [79] |
| Reproductive & Genetic Factors | APOE ε4 status, reproductive history, age at menopause, oophorectomy | Modifies susceptibility to cognitive decline and response to interventions | APOE ε4 carrier status showed greater effect size for executive function in early menopause [25] |
The complex interrelationships between these confounding variables create particular challenges for research design. As illustrated in the recent IGNITE study, a woman's lifetime estrogen exposure is shaped by multiple factors including reproductive surgeries, hormone therapy use, and genetic profile, all of which may interact to influence cognitive outcomes [9].
Measurement and Assessment of Potential Confounders
Methodological Framework for Confounder Identification
The process of confounder identification requires both theoretical grounding and empirical assessment. Domain knowledge is essential for anticipating potential confounders based on established biological mechanisms and previous research findings [80]. In estradiol research, this includes understanding the endocrine system, neurobiology of aging, and social determinants of health. Researchers should create a comprehensive list of potential confounders during the study design phase through systematic literature review and consultation with content experts.
Statistical methods can supplement theoretical approaches for confounder identification. The change-in-estimate criterion suggests that a variable should be considered a confounder if adjusting for it changes the exposure-outcome association by approximately 10% or more [76]. This empirical approach helps prioritize variables for adjustment in statistical models, though it should be guided by theoretical understanding to avoid inappropriate adjustment for mediators or colliders.
Comorbidity Conceptualization and Measurement
Comorbidity presents particular challenges for confounding control in estradiol-cognition research, especially in older populations. The science of comorbidity remains plagued by conceptual and measurement issues, with heterogeneous definitions and inadequate nosological systems complicating research efforts [79]. Comorbidity can be conceptualized as a "distinct additional clinical entity" occurring alongside an index disease (e.g., menopause), while multimorbidity refers to the co-occurrence of multiple conditions without privileging an index condition [78] [79].
Van Weel and Schellevis proposed a useful categorization of comorbidity relationships that includes: (1) causal (diseases with common pathophysiology), (2) complicating (disease-specific complicating morbidity), (3) concurrent (coexisting conditions without causal relation), and (4) intercurrent (interacting acute illness) [79]. Understanding these patterns is essential for appropriate measurement and control of comorbidity in estradiol research.
Comorbidity Relationship Types
Study Design Strategies for Confounding Control
Primary Prevention of Confounding through Design
The most effective approach to confounding control occurs during study design, before data collection begins. Randomization represents the gold standard, as random assignment of participants to exposure groups (e.g., estradiol formulation) theoretically ensures that both known and unknown confounders are equally distributed between groups [80] [77]. However, randomization is not always feasible in hormone research due to ethical and practical constraints, particularly when studying long-term cognitive outcomes.
When randomization is not possible, restriction provides a straightforward method for controlling confounding by limiting study participation to individuals with specific characteristics [80]. For example, a study might restrict participants to a narrow age range of postmenopausal women or to those with specific APOE genotypes. While this improves internal validity, it may limit generalizability of findings.
Matching offers another pre-data collection approach, where researchers ensure that compared groups are similar on key potential confounders [80]. In case-control studies of estradiol and cognition, researchers might match each woman receiving hormone therapy with one not receiving therapy based on age, education, and menopausal age. While effective, matching can be logistically challenging and does not address confounding by unmeasured variables.
Addressing Confounding by Indication
Confounding by indication presents particular challenges in therapeutic research on estradiol and cognition, as treatment decisions are based on clinical presentations that may themselves relate to outcomes [76]. The only way to definitively address this form of confounding is through study designs that ensure the same range of condition severity exists in compared treatment groups, and that treatment choice is not based on that severity [76]. This often necessitates randomized designs or careful prospective observational studies that measure and account for all clinical factors influencing treatment decisions.
Statistical Approaches for Confounding Adjustment
Stratification and Multivariable Methods
After data collection, statistical methods can adjust for confounding during analysis. Stratification involves examining the exposure-outcome relationship within homogeneous strata of the confounding variable [76] [80]. For example, researchers might analyze the association between estradiol therapy and cognitive performance separately within different educational attainment groups. The Mantel-Haenszel method provides a weighted average of the stratum-specific estimates, generating an overall effect estimate adjusted for the confounding variable [80].
Multivariable regression methods offer a more flexible approach that can simultaneously adjust for multiple confounders [76] [80]. These models estimate the independent association between exposure and outcome while holding constant the other variables in the model. The choice of specific model (linear regression for continuous outcomes, logistic regression for binary outcomes, Cox regression for time-to-event outcomes) depends on the nature of the cognitive outcome being studied.
Table 2: Statistical Methods for Confounding Control
| Method | Procedure | Advantages | Limitations | Implementation Example |
|---|---|---|---|---|
| Stratification | Divide data into subgroups based on confounder values | Intuitive, transparent | Limited to few confounders, small sample strata | Analyze estradiol-cognition association within separate APOE ε4 carrier/non-carrier groups [25] |
| Multivariable Regression | Mathematical modeling including exposure and confounders | Handles multiple confounders, provides effect estimates | Model dependence, assumptions (linearity, additivity) | Linear regression adjusting for age, education, vascular risk [25] |
| Propensity Score Methods | Create composite score for probability of exposure based on confounders | Mimics randomization, handles multiple confounders | Only adjusts for measured confounders | Matching women with similar probabilities of receiving transdermal vs. oral estradiol |
| Instrumental Variable Analysis | Uses variable associated with exposure but not outcome | Addresses unmeasured confounding | Requires valid instrument, complex interpretation | Using physician prescribing preference as instrument for hormone therapy type |
Addressing Residual Confounding
Residual confounding refers to confounding that remains after statistical adjustment, often due to imperfect measurement of confounders [81]. This represents a particular threat in estradiol-cognition research, where variables like socioeconomic status or cognitive engagement may be crudely measured. The impact of residual confounding is increased by large sample sizes and high reliability in exposure and outcome measurements, while being attenuated by high reliability in confounder measurement [81].
The dangers of residual confounding are exemplified by research on socioeconomic background, cognitive ability, and educational attainment, where apparent evidence of discrimination was better explained by residual confounding [81]. In hormone research, this might manifest as spurious associations between therapy type and cognitive outcomes due to imperfect measurement of health-seeking behaviors or subtle clinical differences influencing treatment decisions.
Applied Experimental Protocols for Estradiol-Cognition Research
Protocol: CLSA Study on Menopause Age and Estradiol Therapy
A recent investigation from the Canadian Longitudinal Study of Aging (CLSA) provides an exemplary protocol for addressing confounding in estradiol-cognition research [25] [26]. This cross-sectional observational study examined associations between menopause age, estradiol-based hormone therapy, and cognitive performance in 7,251 cognitively normal postmenopausal women.
Cognitive Domain Assessment: The study employed a multi-domain cognitive assessment covering:
- Episodic memory: Word recall tests assessing ability to remember past events
- Prospective memory: Tasks measuring ability to remember future intentions
- Executive functions: Tests evaluating planning, problem-solving, and cognitive control
Confounder Adjustment: Linear regression models adjusted for:
- Age (continuous)
- Education level (categorical)
- Vascular risk factors (composite)
Hormone Therapy Characterization: Detailed assessment of estradiol-based HT including:
- Administration route (transdermal vs. oral)
- Formulation type (patches, gels, vaginal rings, creams, tablets)
- Comparison to never-users
This protocol revealed important differential associations: transdermal estradiol was associated with better episodic memory (β=0.413, 95% CI 0.294-0.533), while oral estradiol was associated with better prospective memory (β=0.208, 95% CI 0.037-0.378), highlighting the importance of considering formulation-specific effects [25].
Protocol: IGNITE Study on Lifetime Estrogen Exposure
The Investigating Gains in Neurocognition in an Intervention Trial of Exercise (IGNITE) study provides another methodological template, examining lifetime estrogen exposure and domain-specific cognitive performance in 461 postmenopausal women [9].
Comprehensive Cognitive Battery:
- Montreal Cognitive Assessment (MoCA) for global cognition
- Factor-analytically derived composites for:
- Episodic memory
- Processing speed
- Working memory
- Executive function/attentional control
- Visuospatial processing
Estrogen Exposure Assessment:
- Surgical history (oophorectomy)
- Hormone therapy use (type, timing, duration)
- Birth control history
- APOE genotyping
Statistical Adjustment:
- Multivariable regression models
- Examination of effect modification by APOE status
- Consideration of timing variables (critical window hypothesis)
This comprehensive approach revealed that hormone therapy use after oophorectomy was associated with better episodic memory (β=0.106, p=0.02), working memory (β=0.120, p=0.005), and visuospatial processing (β=0.095, p=0.03), while birth control use was associated with better performance on MoCA (β=0.093, p=0.04), working memory (β=0.102, p=0.02), and executive function (β=0.103, p=0.02) [9].
Confounding Control Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Tools for Confounding Control in Estradiol Research
| Tool Category | Specific Instruments/Measures | Research Application | Considerations |
|---|---|---|---|
| Cognitive Assessment | CLSA Cognitive Battery, MoCA, Factor-analytic composites | Domain-specific cognitive measurement | Test reliability, cultural appropriateness, practice effects |
| Hormone Assessment | HT type, administration route, duration, timing | Characterization of exposure | Recall bias, prescription vs. actual use, formulation differences |
| Genetic Analysis | APOE ε4 genotyping, other relevant polymorphisms | Assessment of effect modification | Sample collection, ethical considerations, statistical power |
| Comorbidity Measures | Charlson Index, CIRS, disease counts | Quantification of health status | Predictive validity, administrative vs. clinical data |
| Socioeconomic Metrics | Education, income, occupation, neighborhood indices | Measurement of social determinants | Comprehensive assessment, life-course approaches |
| Statistical Software | R, SAS, Stata, Python | Implementation of advanced methods | Appropriate modeling, assumption checking, transparency |
Addressing confounding variables in research on estradiol and cognitive performance requires meticulous attention to study design, comprehensive measurement of potential confounders, and appropriate statistical analysis. The increasing sophistication of research in this field—exemplified by studies that examine domain-specific cognitive outcomes, different hormone formulations, and effect modification by genetic factors—demands equally sophisticated approaches to confounding control.
Future methodological advances should focus on improved measurement of key constructs, particularly subtle socioeconomic and lifestyle factors that may create residual confounding. Additionally, greater application of causal inference methods, including instrumental variable analysis and marginal structural models, may help address unmeasured confounding in observational studies of estradiol and cognitive health. As our understanding of the complex interplay between hormonal mechanisms, brain aging, and cognitive function evolves, so too must our methodological rigor in addressing the confounding variables that can obscure true relationships and impede therapeutic development.
Estradiol-based Menopausal Hormone Therapy (MHT) presents a complex risk-benefit profile that varies significantly by administration route, formulation, and patient characteristics. Recent research indicates that transdermal estradiol is associated with enhanced episodic memory, while oral estradiol demonstrates benefits for prospective memory. Conversely, earlier age at menopause onset correlates with reduced cognitive performance across multiple domains. Health risks include route-dependent effects on hepatic metabolism, cardiovascular biomarkers, and thrombosis potential. This analysis synthesizes current evidence to guide researchers and clinicians in optimizing estradiol-based interventions for cognitive health while mitigating associated risks, with particular emphasis on the mechanistic pathways underlying these differential effects.
Estradiol, the most potent endogenous estrogen, exerts profound effects on brain structure and function through widespread estrogen receptor distribution. The neuroprotective properties of estradiol have been demonstrated in animal models and human observational studies, yet therapeutic applications have yielded conflicting results due to methodological variations and critical differences in formulation and administration route. The hormonal mechanisms underpinning estradiol's effects on cognition involve both genomic and non-genomic signaling pathways that modulate synaptic plasticity, neurogenesis, and neurotransmitter systems in key brain regions including the hippocampus, prefrontal cortex, and basal forebrain [82] [8].
The timing hypothesis of hormone therapy suggests that the cognitive benefits of estradiol are most pronounced when initiated during the critical window of perimenopause or early postmenopause, aligning with the concept of neuroprotection rather than neuronal restoration after significant neurodegenerative changes have occurred. Understanding the complex interplay between estradiol pharmacokinetics, receptor dynamics, and cognitive domain specificity is essential for designing targeted therapeutic strategies that maximize benefit while minimizing potential harms [8].
Cognitive Benefits of Estradiol Therapy: Domain-Specific Effects
Differential Cognitive Outcomes by Administration Route
Recent large-scale observational studies have revealed that the cognitive effects of estradiol-based MHT are not uniform but demonstrate significant domain-specificity based on administration route.
Table 1: Cognitive Domain Performance by Estradiol Administration Route
| Administration Route | Cognitive Domain | Effect Size | Statistical Significance | Study Population |
|---|---|---|---|---|
| Transdermal E2 | Episodic Memory | Cohen's d = 0.303 | p = 0.007 | 7,251 postmenopausal women [8] |
| Oral E2 | Prospective Memory | Cohen's d = 0.283 | p = 0.015 | 7,251 postmenopausal women [8] |
| Neither route | Executive Function | Not significant | p = 0.345 | 7,251 postmenopausal women [8] |
The Canadian Longitudinal Study on Aging (CLSA), comprising 7,251 postmenopausal women with mean age 60.5 years at baseline, demonstrated that transdermal estradiol was associated with significantly better episodic memory performance compared to no hormone therapy, while oral estradiol was associated with significantly better prospective memory performance [82] [8]. Neither administration route showed significant effects on executive function, indicating domain-specific mechanisms rather than global cognitive enhancement.
The observed differential effects may be explained by variations in estrogen receptor density across brain regions and the distinct pharmacokinetic profiles of administration routes. Episodic memory, primarily mediated by the hippocampus, may be more responsive to the stable estradiol concentrations achieved with transdermal administration, while prospective memory, involving frontal and medial-temporal regions, may benefit from the metabolic byproducts or pulsatile delivery of oral estradiol [8].
Impact of Menopause Timing on Cognitive Outcomes
The relationship between menopause age and cognitive performance reveals critical considerations for therapeutic timing:
Table 2: Association Between Menopause Age and Cognitive Performance
| Cognitive Domain | Effect of Earlier Menopause | Effect Size (β) | Statistical Significance |
|---|---|---|---|
| Episodic Memory | Reduced performance | β = 0.050 | p < 0.001 |
| Prospective Memory | Reduced performance | β = 0.047 | p < 0.001 |
| Executive Function | Reduced performance | β = 0.061 | p < 0.001 |
Earlier age at menopause onset (mean age 50.5 ± 4.2 years in the CLSA cohort) was significantly associated with reduced performance across all cognitive domains tested [8]. This association was particularly pronounced for executive function in APOE ε4 carriers (β = 0.070, p < 0.001) and women with four or more children (β = 0.215, p < 0.001), suggesting potential gene-hormone interactions and parity-related modifications of cognitive aging trajectories [8].
These findings support the critical window hypothesis, wherein earlier estrogen deprivation may accelerate age-related cognitive decline, and earlier intervention may yield greater neuroprotective benefits. The modified effect in APOE ε4 carriers highlights the importance of genetic stratification in future clinical trials and therapeutic decision-making.
Pharmacokinetic Mechanisms Underlying Route-Dependent Effects
The administration route of estradiol significantly influences its pharmacokinetic profile, which in turn affects both cognitive efficacy and risk profiles.
Diagram 1: Metabolic Pathways of Oral vs. Transdermal Estradiol
Oral Administration Pharmacokinetics
Oral estradiol undergoes significant first-pass hepatic metabolism, resulting in low bioavailability (approximately 5% with range of 0.1-12%) [38]. This metabolic process converts estradiol to estrone and various conjugates, creating an estrone-to-estradiol ratio that differs markedly from physiological conditions. The resulting hepatic exposure to high estrogen concentrations stimulates synthesis of proteins including sex hormone-binding globulin (SHBG), thyroid-binding globulin, and various coagulation factors, which may contribute to the thrombotic and cardiovascular risks associated with oral estrogen therapy [38].
The typical pharmacokinetic profile of oral estradiol includes rapid absorption with peak concentrations within 4-6 hours, followed by a decline with an elimination half-life of approximately 13-20 hours. The fluctuating levels and metabolite profile may preferentially engage certain cognitive networks, potentially explaining the domain-specific benefits observed in prospective memory [8] [38].
Transdermal Administration Pharmacokinetics
Transdermal estradiol delivery bypasses first-pass hepatic metabolism, resulting in more stable serum levels and a physiological estradiol-to-estrone ratio that closely mimics premenopausal patterns [8] [38]. This route provides sustained delivery with half-lives ranging from 37 hours for gels to several days for patches, maintaining consistent receptor engagement without the peaks and troughs characteristic of oral administration.
The stable hormone levels achieved with transdermal delivery may be particularly beneficial for hippocampal-dependent memory processes that require consistent estrogen receptor signaling for synaptic plasticity. This pharmacokinetic advantage may underlie the specific episodic memory benefits observed with transdermal estradiol in recent studies [82] [8].
Health Risks and Safety Considerations
Route-Dependent Risk Profiles
The administration route of estradiol significantly influences its safety profile, particularly regarding cardiovascular, thrombotic, and metabolic parameters:
Table 3: Health Risks Associated with Estradiol Therapy by Administration Route
| Risk Category | Oral Estradiol | Transdermal Estradiol | Mechanistic Basis |
|---|---|---|---|
| Thrombotic Risk | Increased | Neutral | First-pass hepatic effects on coagulation factors [38] |
| Cardiovascular Biomarkers | Adverse effects | Neutral/Favorable | Hepatic synthesis of inflammatory markers [8] |
| Liver Metabolism | Significant impact | Minimal impact | Bypass of first-pass metabolism [38] |
| Hypertension | Potential increase | Neutral | Renin-angiotensin system effects [83] |
| Weight/BMI | Potential increase | Neutral/Favorable | Metabolic effects [83] |
Clinical evidence indicates that transdermal estradiol does not increase cardiovascular or liver disease biomarkers seen with oral estradiol, making it a potentially safer option for women with elevated baseline risk for these conditions [8]. The Kronos Early Estrogen Prevention Study (KEEPS) found that conjugated equine estrogens (CEEs), but not transdermal estradiol, increased white matter hyperintensities and ventricular volumes compared with placebo, further supporting the safety advantage of non-oral delivery [8].
Additional Risk Modifiers
Beyond administration route, several patient-specific factors influence the risk-benefit calculus for estradiol therapy:
Timing of Initiation: The critical window hypothesis suggests that initiation during perimenopause or early postmenopause (typically before age 60) provides maximal neuroprotective benefit with reduced cardiovascular risks [8].
APOE Genotype: APOE ε4 carriers may experience differential cognitive effects and potentially modified risk profiles, though current evidence remains preliminary [8].
Formulation Considerations: Bioidentical estradiol demonstrates distinct pharmacological properties compared to synthetic estrogens or animal-derived conjugated estrogens, with potential implications for both efficacy and safety [38].
Experimental Protocols and Methodological Considerations
CLSA Cognitive Assessment Protocol
The Canadian Longitudinal Study on Aging employed comprehensive cognitive assessment methodologies that can inform future research design:
Participant Characteristics:
- 7,251 cognitively healthy postmenopausal women
- Mean age at baseline: 60.5 ± 10.2 years
- Mean age at menopause: 50.5 ± 4.2 years
- MHT users: 4% transdermal, 2% oral, 94% never users [82] [8]
Cognitive Domain Assessments:
- Episodic Memory: Measured using standardized recall tests assessing ability to remember past events and information
- Prospective Memory: Evaluated through tasks requiring remembering to perform future actions (appointments, medication)
- Executive Function: Assessed using tests of cognitive flexibility, planning, and complex attention [8]
Statistical Controls: Analyses controlled for age, years of education, vascular risk factors, and significant group differences. Additional moderation analyses examined APOE ε4 status and parity as potential effect modifiers [8].
Neuroimaging Protocols for Estradiol Effects
Advanced neuroimaging methodologies provide insights into the neural mechanisms underlying estradiol's cognitive effects:
fMRI Assessment Parameters (based on related trial):
- Tasks employed: Verbal fluency and mental rotation paradigms
- Imaging technique: Blood oxygen level-dependent (BOLD) signaling
- Timing: Baseline and 26-week follow-up
- Analysis: Regional brain activation patterns comparing treatment and placebo groups [83]
In one randomized controlled trial, functional magnetic resonance imaging performed on participants using tasks of verbal fluency and mental rotation showed that the mental rotation task was associated with increased blood oxygen level-dependent signalling in the placebo group in both occipital lobes and in the left superior parietal lobe after 26 weeks (P < 0.05), with no changes over time seen in the treatment group, suggesting potential neural efficiency effects [83].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents for Estradiol and Cognitive Function Studies
| Reagent/Material | Function/Application | Example Specifications |
|---|---|---|
| Estradiol Formulations | Experimental intervention | Micronized oral tablets (0.1-2mg); Transdermal patches (14-100μg/d) [38] |
| Cognitive Assessment Platforms | Outcome measurement | Computerized cognitive batteries; Standardized memory tests [8] [83] |
| Genotyping Arrays | Effect modification analysis | APOE ε4 allele detection; Genome-wide association studies [84] [8] |
| Immunoassay Kits | Hormone level quantification | Estradiol, estrone, SHBG measurements; Lower detection limit 175 pmol/L [84] |
| fMRI Paradigms | Neural mechanism elucidation | Verbal fluency, mental rotation tasks; BOLD signal acquisition [83] |
| Genetic Databases | GWAS and Mendelian randomization | UK Biobank (n=361,975); CLSA data [84] [8] |
The risk-balance profile of estradiol therapy reveals complex interactions between administration routes, cognitive domains, and individual patient characteristics. The current evidence supports a precision medicine approach that considers menopause timing, genetic background, and specific cognitive concerns when formulating therapeutic strategies.
Future research should prioritize several key areas:
- Elucidation of molecular mechanisms underlying domain-specific cognitive effects
- Long-term randomized trials comparing administration routes with standardized cognitive outcomes
- Integration of multimodal biomarkers including neuroimaging, genetic profiling, and hormone level monitoring
- Development of personalized risk prediction models incorporating clinical, genetic, and lifestyle factors
The evolving understanding of estradiol's effects on cognitive health continues to refine therapeutic approaches, moving toward increasingly tailored interventions that maximize cognitive benefits while minimizing potential risks.
Evidence Synthesis and Future Directions: Estradiol Versus Emerging Therapeutic Targets
The impact of menopausal hormone therapy (MHT) on cognitive function remains a critically important yet contentious area of women's health research. This technical review synthesizes current evidence on the differential effects of estradiol (E2)-based formulations versus conjugated equine estrogens (CEEs) on cognitive outcomes. Accumulating evidence indicates that E2-based MHT, particularly via transdermal administration, demonstrates superior efficacy for specific cognitive domains including episodic and prospective memory, while CEE formulations show more limited benefits. The underlying mechanisms involve complex interactions between estrogen receptor dynamics, metabolic pathways, and the timing of intervention relative to menopausal transition. This analysis provides researchers and drug development professionals with a comprehensive framework for understanding hormonal mechanisms and developing targeted therapeutic strategies for cognitive preservation in postmenopausal women.
Estrogens, particularly 17β-estradiol (E2), exert wide-ranging effects on the central nervous system through both genomic and non-genomic mechanisms. These hormones play a fundamental role in modulating higher-order cognitive function, cerebral metabolism, and neurobiological aging [85]. The menopausal transition marks a critical period of neuroendocrine change characterized by declining ovarian function and a substantial reduction in circulating E2 levels, creating a vulnerable window for cognitive decline [86].
The "critical window hypothesis" posits that the timing of estrogen intervention is paramount for cognitive protection, with early initiation around menopause onset providing maximal benefit compared to later initiation [9]. This framework is essential for understanding the divergent outcomes observed in clinical trials of different MHT formulations. Beyond timing, the specific estrogenic composition of MHT—whether native human estradiol or mixed equine estrogens—appears to significantly influence cognitive outcomes through distinct pharmacokinetic and receptor-binding profiles.
Mechanistic Foundations: Estrogen Receptor Dynamics and Signaling Pathways
Estrogen Receptor Distribution and Function
Estrogen signals through multiple receptor subtypes distributed throughout brain regions critical for cognition:
ERα and ERβ: Classical nuclear receptors that function as ligand-dependent transcription factors, regulating gene expression in regions including the hippocampus, prefrontal cortex, and basal forebrain [86]. These receptors are located in both nuclear and extranuclear sites, with extranuclear pools mediating rapid nongenomic signaling [86].
GPER1 (G protein-coupled estrogen receptor 1): Membrane-associated receptor that activates intracellular signaling cascades [86].
Table 1: Estrogen Receptor Distribution in Cognitive Brain Regions
| Brain Region | Primary Cognitive Role | Receptor Subtypes Present | Aging-Related Changes |
|---|---|---|---|
| Prefrontal Cortex | Executive function, working memory | ERα, ERβ, GPER1 | Increased ER density post-menopause [85] |
| Hippocampus | Episodic memory, spatial navigation | ERα, ERβ, GPER1 | Synaptic ERα decreases with age [86] |
| Posterior Cingulate Cortex | Memory integration, self-referential thought | ERα, ERβ | Significant postmenopausal increase in ER density [85] |
Recent in vivo neuroimaging studies using 18F-FES PET have revealed that brain estrogen receptor density increases progressively over the menopausal transition independently of plasma E2 levels, with postmenopausal women showing significantly higher ER density in the pituitary, posterior cingulate cortex, and caudate compared to premenopausal women [85]. This upregulated receptor availability may represent a compensatory neuroadaptive response to estrogen deficiency and has important implications for MHT dosing strategies.
Molecular Signaling Pathways
Estradiol enhances cognitive function through multiple complementary mechanisms:
Figure 1: Estradiol signaling pathways in cognitive enhancement. E2 activates both membrane-associated and nuclear estrogen receptors, initiating rapid signaling cascades and genomic effects that collectively enhance synaptic plasticity, provide neuroprotection, and ultimately improve cognitive function through multiple convergent mechanisms [16] [86] [87].
Recent research has illuminated that estrogen naturally boosts learning capabilities by enhancing dopamine activity in the brain's reward center, strengthening reward signals that guide learning throughout the brain [87]. This mechanism is particularly relevant for reward-based learning and decision-making processes.
Comparative Clinical Efficacy: Estradiol vs. CEE Formulations
Domain-Specific Cognitive Outcomes
Recent large-scale observational studies provide compelling evidence for domain-specific cognitive benefits of estradiol-based MHT:
Table 2: Cognitive Domain Responses to Different MHT Formulations
| Cognitive Domain | E2-Based MHT Effects | CEE-Based MHT Effects | Key Evidence |
|---|---|---|---|
| Episodic Memory | Transdermal E2 associated with significantly higher scores (β=0.050, p<0.001) [8] | Limited to no benefit; may increase white matter hyperintensities [8] | CLSA cohort (n=7,251): transdermal E2 showed Cohen d=0.303 vs. no MHT [8] |
| Prospective Memory | Oral E2 associated with improved performance (Cohen d=0.283) [8] [25] | No significant improvements demonstrated | CLSA: oral E2 significantly improved scores vs. never users (p=0.015) [8] |
| Executive Functions | No significant effect (p=0.345) [8] | No significant effect | KEEPS trial: CEEs showed no significant effect on executive function [8] |
| Global Cognition | Hormone therapy after oophorectomy associated with better episodic memory, working memory, and visuospatial processing [9] | Mixed results; timing-dependent effects | IGNITE study: HT after oophorectomy associated with multiple domain improvements [9] |
The Canadian Longitudinal Study on Aging (CLSA) baseline data analysis of 7,251 postmenopausal women revealed that earlier age at menopause was significantly associated with lower scores across all cognitive domains tested (episodic memory β=0.050, p<0.001; prospective memory β=0.047, p<0.001; executive functions β=0.061, p<0.001) [8] [25]. This association underscores the importance of timely intervention, particularly for women experiencing early menopause.
Administration Route Considerations
The route of E2 administration significantly influences its cognitive effects:
Transdermal E2: Bypasses first-pass hepatic metabolism, providing more stable blood levels and similar E2:E1 ratios as premenopausal women [8]. Associated with stronger episodic memory performance, potentially due to more favorable effects on hippocampal plasticity [8] [88].
Oral E2: Undergoes significant hepatic first-pass metabolism, converting estradiol to estrone (E1) and reducing bioavailability [8]. Nonetheless, associated with better prospective memory, possibly through hepatic synthesis of neuroactive metabolites [8].
Notably, neither administration route significantly affected executive functions (p=0.345) [8], suggesting this cognitive domain may be less responsive to estrogen modulation or require different therapeutic approaches.
Critical Experimental Protocols and Methodologies
Human Cognitive Assessment Protocols
The CLSA study employed comprehensive cognitive assessment across three primary domains [8]:
Episodic Memory Protocol:
- Assessment: Immediate and delayed recall of validated word lists
- Scoring: Number of correctly recalled items after specified delay intervals
- Neural substrate: Medial temporal lobe (hippocampus) integrity
Prospective Memory Protocol:
- Assessment: Remembering to perform future tasks or intentions
- Scoring: Accuracy in executing previously instructed actions at appropriate times
- Neural substrate: Frontal and medial-temporal lobes
Executive Function Protocol:
- Assessment: Task-switching, inhibition, and cognitive flexibility tests
- Scoring: Response accuracy and latency measures
- Neural substrate: Prefrontal cortex
Neuroimaging and Biomarker Protocols
Advanced neuroimaging techniques have provided critical insights into estrogen receptor dynamics:
18F-FES PET Imaging Protocol [85]:
- Tracer: 16α-18F-fluoro-17β-estradiol (18F-FES), selective binding affinity for ERs, especially ERα
- Image Acquisition: Dynamic PET scanning following intravenous tracer administration
- Analysis: Graphic Logan plots to derive distribution volume ratios (DVR) relative to cerebellar gray matter
- Applications: Quantification of ER density in pituitary, hypothalamus, hippocampus, and cortical regions in relation to menopausal status and cognitive performance
This protocol has demonstrated that postmenopausal women exhibit significantly higher ER density in cognitively relevant brain regions compared to premenopausal women, correctly classifying 100% of women as being postmenopausal or premenopausal based on pituitary, caudate, PCC and middle frontal DVR [85].
Research Reagent Solutions and Methodological Toolkit
Table 3: Essential Research Reagents and Materials for Estrogen-Cognition Studies
| Reagent/Material | Primary Application | Technical Function | Example Use |
|---|---|---|---|
| 18F-FES PET Tracer | In vivo ER quantification | Selective binding to ERα for PET imaging | Measuring brain ER density in menopausal stages [85] |
| ERα/ERβ Selective Agonists | Receptor mechanism studies | Dissecting specific receptor subtype contributions | Determining relative roles of ER subtypes in cognitive tasks |
| Aromatase Inhibitors | Neurosteroid research | Blocking brain-derived estradiol synthesis | Investigating local vs. peripheral estrogen effects [89] |
| Conditional Knockout Models | Genetic approaches | Cell-type specific receptor deletion | Forebrain neuron-specific ER knockout mice [89] |
| CLSA Cognitive Battery | Human cognitive assessment | Domain-specific cognitive profiling | Episodic, prospective memory and executive function testing [8] |
| Custom MHT Formulations | Administration route studies | Testing bioavailability and efficacy | Transdermal vs. oral E2 comparisons [8] |
Discussion and Future Directions
The evidence reviewed demonstrates clear differential effects between estradiol-based MHT and conjugated equine estrogens on cognitive outcomes. E2-based formulations, particularly transdermal administration, show consistent benefits for hippocampal-dependent episodic memory, while oral E2 appears more beneficial for prospective memory. In contrast, CEE formulations demonstrate limited cognitive benefits and may potentially adversely affect cerebrovascular health [8].
Several critical factors emerge as determinants of cognitive response to MHT:
Timing and Critical Window Hypothesis
The timing of MHT initiation relative to menopause onset appears crucial for cognitive benefits. The "critical window hypothesis" suggests that optimal timing for estrogen therapy is around the time of menopause when estrogen levels are changing, but before other age-related brain changes occur [9]. This is supported by findings that estrogen initiated near menopause onset was associated with improved verbal memory, while later initiation had no effects [9].
Individual Risk Factors
Specific patient characteristics modulate MHT effects on cognition:
APOE ε4 Status: Earlier age at menopause was associated with greater executive function decline in APOE ε4 carriers (β=0.070, 95% CI 0.016-0.123, p<0.001) compared to non-carriers [8], suggesting genetic vulnerability to estrogen deprivation.
Reproductive History: The association between earlier menopause age and executive function decline was pronounced in women with 4 or more children (β=0.215, 95% CI 0.133-0.296, p<0.001) [8], indicating potential interaction between parity and estrogen exposure.
Surgical Menopause: Hormone therapy use started within 2 years of oophorectomy was associated with better episodic memory (β=0.106, p=0.02), working memory (β=0.120, p=0.005), and visuospatial processing (β=0.095, p=0.03) in later life [9].
Future Research Priorities
Several key areas require further investigation:
Mechanistic Studies: Further elucidation of how different estrogen formulations and administration routes influence specific neural circuits and molecular pathways underlying cognitive processes.
Personalized Approaches: Development of biomarkers, including neuroimaging and genetic profiles, to identify women most likely to benefit from specific MHT regimens.
Novel Therapeutic Strategies: Exploration of selective estrogen receptor modulators (SERMs), tissue-specific estrogens, and combination therapies that maximize cognitive benefits while minimizing risks.
Substantial evidence supports the superior efficacy of estradiol-based MHT over conjugated equine estrogens for specific cognitive domains, particularly when administered during the critical window near menopause onset. The mechanisms underlying these differential effects involve complex interactions between administration route, metabolic pathways, estrogen receptor dynamics, and individual risk factors. Future research should focus on optimizing formulation, timing, and personalization of MHT to maximize cognitive benefits while minimizing potential risks, ultimately contributing to preserved cognitive health in postmenopausal women.
For decades, the focus on the hormonal basis of cognitive decline and Alzheimer's disease (AD) pathology in postmenopausal women has centered predominantly on the decline of estradiol. However, recent research reveals a more nuanced picture, identifying Follicle-Stimulating Hormone (FSH) as a potent, independent driver of Alzheimer's disease-like pathogenesis. This whitepaper synthesizes emerging evidence that elevated FSH levels, characteristic of the menopausal transition, directly promote cerebral amyloid-β (Aβ) deposition, Tau pathology, and cognitive impairment via specific neuronal signaling pathways. We detail the molecular mechanisms, present consolidated quantitative data, and outline essential experimental protocols and reagents, providing researchers and drug development professionals with a comprehensive overview of FSH as a promising therapeutic target for AD.
The longstanding hypothesis linking cognitive decline in aging women to the loss of estradiol has yielded inconsistent clinical outcomes, with estrogen replacement therapy showing variable effects on cognition [16] [44]. This discrepancy has prompted the investigation of alternative hormonal mediators. During the menopausal transition, estradiol levels decline, but this change is preceded and accompanied by a sharp and sustained rise in FSH [90] [91]. A growing body of evidence now positions this elevated FSH as a key pathogenic hormone in its own right.
Critical findings demonstrate that FSH acts directly on neurons in the hippocampus and cortex, accelerating the core pathologies of Alzheimer's Disease: amyloid-β plaques and neurofibrillary tangles [92]. This FSH-driven pathway operates independently of estradiol, offering a compelling explanation for the increased vulnerability to AD in postmenopausal women and opening a new frontier for therapeutic intervention.
Quantitative Evidence: Correlating FSH with Cognitive Decline and AD Pathology
Epidemiological and interventional studies provide robust quantitative evidence linking FSH to cognitive impairment and Alzheimer's pathology. The table below summarizes key findings from recent clinical and preclinical research.
Table 1: Summary of Key Quantitative Findings on FSH and Cognitive Decline
| Study Model | Key Finding | Quantitative Result | Citation |
|---|---|---|---|
| Postmenopausal Women (n=884) | Association between serum FSH and cerebral Aβ deposition | Higher FSH levels correlated with greater Aβ burden on amyloid PET; FSH levels were highest in AD dementia, followed by MCI, and lowest in cognitively normal participants. | [93] |
| Postmenopausal Women (n=731) | Association between serum estradiol and cognitive test scores | Higher estradiol (>7.49 pg/mL) associated with higher DSST scores (β=0.61, p<0.05), indicating better processing speed and working memory. No significant relationship was found for FSH in this specific study. | [43] |
| Ovariectomized 3xTg-AD Mice | Effect of FSH-blocking antibody (FSH-Ab) on Aβ and Tau | FSH-Ab treatment substantially reduced Aβ40, Aβ42, and phosphorylated Tau levels in the hippocampus and brain extracts. | [92] |
| Ovariectomized 3xTg-AD Mice | Effect of FSH-Ab on cognitive performance | FSH-Ab treatment reversed spatial memory deficits in the Morris Water Maze, reducing latency to find the platform and increasing time spent in the target quadrant. | [92] |
| ApoE4-TR Mice | Additive effect of FSH and ApoE4 on neuronal death | FSH exposure significantly increased neurotoxicity (LDH assay); this effect was further augmented by ApoE4 but not ApoE3. | [91] |
Mechanistic Insights: The FSH-FSHR Signaling Pathway in the Brain
FSH exerts its effects by binding to the Follicle-Stimulating Hormone Receptor (FSHR), a G protein-coupled receptor historically associated with gonadal tissues. It is now established that FSHRs are also expressed in extragonadal tissues, including neurons in the human and mouse cortex and hippocampus [90] [92].
The following diagram illustrates the characterized neuronal signaling pathway by which FSH drives Alzheimer's disease-like pathology.
The diagram outlines the core C/EBPβ/δ-secretase pathway. Upon FSH binding, neuronal FSHR activates associated Gαi proteins [94]. This triggers the upregulation of the transcription factor C/EBPβ, which in turn transactivates the gene encoding AEP (asparagine endopeptidase), also known as δ-secretase [91] [92]. Activated AEP cleaves both amyloid precursor protein (APP) and Tau proteins at specific residues (APP N585 and Tau N368), leading to the formation of Aβ peptides and the generation of Tau fragments that are prone to hyperphosphorylation and aggregation into neurofibrillary tangles [90] [91]. Furthermore, this pathway promotes the release of pro-inflammatory cytokines, contributing to a chronic neuroinflammatory state that exacerbates pathology and culminates in cognitive decline [90].
Essential Experimental Models and Protocols
To investigate the role of FSH in cognitive decline, several key experimental approaches have been developed. The following workflow describes a standard protocol for evaluating FSH's effect in vivo.
Detailed Protocol for Evaluating FSH in AD Mouse Models
1. Animal Model Selection:
- Common Models: Female 3xTg-AD (harboring APP, PSEN1, and MAPT mutations) or APP/PS1 mice are frequently used. To model menopause, these mice undergo ovariectomy (OVX) at ~3-4 months of age, which drastically reduces estradiol and increases endogenous FSH [92].
- Genetic Models: FSHR knockout (FSHR-/-) or haploinsufficient (FSHR+/-) mice crossed with AD models are used to establish a causal role for FSH signaling [94].
2. Intervention:
- FSH Administration: Recombinant human FSH is administered via intraperitoneal (i.p.) injection to intact mice (e.g., 5 IU) to directly test its pathogenic effects [92].
- FSH Blockade: A specific anti-FSHβ antibody (FSH-Ab, e.g., 200 μg per mouse every 2 days, i.p.) is administered to OVX mice for 8-16 weeks to assess therapeutic potential [92]. A humanized version, MS-Hu6, is also available [94].
3. Behavioral Phenotyping (Cognitive Assessment):
- Morris Water Maze (MWM): The gold-standard test for hippocampal-dependent spatial learning and memory. Key metrics include latency to find a hidden platform, path length, and time spent in the target quadrant during a probe trial [91] [92].
- Novel Object Recognition (NOR): Tests non-spatial episodic memory by measuring the animal's preference for a novel object over a familiar one [92].
4. Tissue Collection & Analysis:
- After behavioral tests, animals are perfused, and brains are collected.
- Biochemical Analysis: Brain hemispheres are homogenized for protein extraction. ELISA is used to quantify Aβ40 and Aβ42 levels. Western blotting assesses levels of C/EBPβ, active AEP, APP N-terminal fragments, Tau N368 fragments, and phosphorylated Tau [91] [92].
- Histopathology: Brain sections are immunostained for Aβ plaques (e.g., 6E10 antibody) and neurofibrillary tangles (e.g., AT8 antibody). Quantification is performed via image analysis [92].
5. Molecular Analysis:
- Gene Expression: RT-PCR or qPCR to measure FSHR, C/EBPβ, and AEP mRNA levels in cortical and hippocampal tissues [90] [92].
- Cell Culture Validation: Primary rat cortical neurons or human neuroblastoma cells (SH-SY5Y) are treated with FSH (e.g., 30 ng/mL) in the presence or absence of ApoE3/ApoE4 to validate direct neuronal effects and the involved pathway in a controlled setting [91].
The Scientist's Toolkit: Key Research Reagents
The table below catalogs essential reagents and models used in this field, as cited in the literature.
Table 2: Key Research Reagents and Models for Investigating FSH in Cognitive Decline
| Reagent / Model | Specific Example / Catalog | Function and Application in Research |
|---|---|---|
| Anti-FSH Antibody | FSH-Ab (mouse-specific); MS-Hu6 (humanized) | Blocks FSH action in vivo to investigate its pathological role and assess therapeutic potential. MS-Hu6 shows good blood-brain barrier permeability [94] [92]. |
| AD Mouse Models | 3xTg-AD, APP/PS1, ApoE4-TR | Models that develop Aβ and/or Tau pathology. ApoE4-TR mice are particularly useful for studying gene-hormone interactions [91] [92]. |
| Recombinant FSH | Recombinant human FSH | Used to administer exogenous FSH to mice or treat neuronal cultures to directly induce and study the C/EBPβ/AEP signaling pathway [91]. |
| FSHR Antibodies | Anti-FSHR (e.g., Thermo PA5-50963) | Detect FSHR protein expression in brain tissue and neuronal cultures via Western Blot and Immunofluorescence [90]. |
| Neuronal Cell Lines | SH-SY5Y (human neuroblastoma); Primary cortical/hippocampal neurons | In vitro models to study direct FSH signaling in neurons, including cytokine release, APP/Tau processing, and neurotoxicity [90] [91]. |
The evidence compellingly positions FSH as a critical, independent risk factor for cognitive decline and Alzheimer's pathology in postmenopausal women, operating through a defined neuronal signaling axis. This understanding moves the field beyond the estradiol-centric view and clarifies why estrogen-based therapies have yielded mixed results.
Future research must focus on several key areas:
- Translational Clinical Trials: Investigating the efficacy and safety of FSH-blocking therapies, such as the humanized antibody MS-Hu6, in humans is the logical next step. Special consideration should be given to women carrying the ApoE4 allele, who may be at highest risk [91] [94].
- Mechanistic Elucidation: Further exploration of how FSH signaling intersects with other AD risk factors, including its role in neuroinflammation and its potential effects on the cerebral vasculature, is warranted [90] [95].
- Therapeutic Windows: Determining the optimal timing for intervention—whether during the perimenopausal FSH surge or later in postmenopause—will be crucial for clinical success [94].
In conclusion, targeting the FSH-FSHR signaling pathway represents a highly promising and novel strategy for mitigating the disproportionate burden of Alzheimer's disease in women.
Alzheimer's disease (AD) displays a pronounced sex disparity, affecting nearly two-thirds of all diagnosed individuals. The neuropathological hallmarks of AD—amyloid-β (Aβ) plaques and hyperphosphorylated tau neurofibrillary tangles—often exhibit earlier deposition and faster progression in women compared to age-matched men. A compelling hypothesis implicates the sharp decline in estradiol during the menopausal transition as a key driver of this increased neuropathological vulnerability. This whitepaper synthesizes current evidence on how estradiol-containing Menopausal Hormone Therapy (MHT) influences Aβ and tau pathology in postmenopausal women, framing these findings within the broader thesis of estradiol's role in cognitive performance and brain health. Understanding these relationships is critical for developing targeted, sex-specific therapeutic and preventive strategies for AD.
Estradiol's Neuroprotective Mechanisms and Signaling Pathways
Estradiol (17β-estradiol, E2) exerts multifaceted neuroprotective effects via complex signaling mechanisms. Its actions are primarily mediated through estrogen receptors ERα and ERβ, which are widely distributed in brain regions critical for cognition, including the hippocampus, prefrontal cortex, and entorhinal cortex [96] [97]. These receptors function as ligand-activated transcription factors, regulating gene expression by binding to estrogen response elements (EREs) on DNA.
Key Molecular Pathways
- Synaptic Plasticity and Neurotransmission: Estradiol enhances synaptic connectivity through long-term potentiation (LTP), increased dendritic spine density, and heightened expression of synaptic proteins. It also modulates key neurotransmitter systems, including upregulating choline acetyltransferase for acetylcholine synthesis, and influencing serotonergic and dopaminergic signaling [96].
- Amyloid-β Pathology: Estradiol reduces amyloid-beta accumulation in the brain by influencing the amyloid precursor protein (APP) processing pathway. It promotes the non-amyloidogenic pathway, thereby reducing the production of pathogenic Aβ peptides [7].
- Tau Phosphorylation: The two primary estrogen receptors, ERα and ERβ, appear to have opposing effects on tau phosphorylation. ERα increases tau hyperphosphorylation by elevating miR-218 levels, which decreases PTPa levels. Conversely, ERβ inhibits tau phosphorylation by limiting miR-218 and restoring the balance of kinase and phosphatase activity [97].
- Mitochondrial Function and Neuroinflammation: Estradiol supports mitochondrial function and reduces neuroinflammation. It also enhances cerebral blood flow and glucose metabolism, helping to counteract the development of microvascular lesions associated with dementia [7].
The diagram below illustrates the core signaling pathways through which estradiol influences AD-related pathology.
Impact of Estradiol Therapy on AD Biomarkers: Empirical Evidence
Clinical and neuroimaging studies provide direct, albeit complex, evidence of how estradiol-based MHT influences the trajectory of AD biomarkers. The effects are highly dependent on timing of initiation, formulation, and route of administration.
Longitudinal Biomarker Studies
Table 1: Key Findings from Longitudinal Studies on MHT and AD Biomarkers
| Study / Population | MHT Formulation | Amyloid-β (Aβ) Findings | Tau Pathology Findings | Cognitive Correlation |
|---|---|---|---|---|
| ELITE Trial (Early Postmenopause) [50] | Oral 17β-estradiol (1 mg/day) | Significantly accelerated decline in Aβ40 vs. placebo (p=0.049). Numerically greater declines in Aβ42 & increases in Aβ42/Aβ40 ratio (non-significant). | No significant effects on p-tau181. | Not assessed in this analysis. |
| ELITE Trial (ApoEε4 Carriers, Early Postmenopause) [50] | Oral 17β-estradiol (1 mg/day) | More pronounced decline in Aβ40 and Aβ42 vs. placebo (non-significant). | No significant effects on p-tau181. | Not assessed in this analysis. |
| Tau-PET Study (Older Women, >70 yrs) [98] | Not Specified | Marginally faster rates of global Aβ accumulation in older HT users vs. non-users (p=0.051). | Faster regional tau accumulation in entorhinal cortex, inferior temporal & fusiform gyri. | Indirect effect of HT on cognitive decline mediated by regional tau accumulation. |
| Tau-PET Study (Younger Women, <70 yrs) [98] | Not Specified | Minimal effect of HT on Aβ accumulation. | Negligible associations with tau accumulation. | No significant association with cognitive decline. |
The Critical Window Hypothesis
The critical window hypothesis (or timing hypothesis) is a central concept for interpreting the divergent outcomes of MHT studies [96]. This hypothesis posits that the neuroprotective benefits of estradiol are most likely to be realized when therapy is initiated during a specific "window of opportunity" close to the time of menopause (typically within 5-10 years), before significant age-related neuropathology and vascular damage become established.
- Supporting Evidence: Data from the ELITE trial and others suggest that MHT initiated in early postmenopause may favorably influence certain Aβ biomarkers, whereas initiation in late postmenopause (≥10 years after menopause) shows no such benefit and may even be detrimental [50].
- Mechanistic Basis: The perimenopausal and early postmenopausal brain, while experiencing estrogen loss, may retain sufficient plasticity and healthy neurovascular systems to respond positively to estrogen repletion. In contrast, initiating therapy later may be ineffective or harmful due to the presence of advanced, irreversible pathology like significant Aβ plaques or neurofibrillary tangles, or compromised cerebrovascular integrity [96].
Methodologies for Investigating Estradiol-AD Pathology Links
Research in this field employs a range of sophisticated techniques, from neuroimaging in human cohorts to detailed molecular biology in animal models.
Human Neuroimaging and Cohort Studies
Positron Emission Tomography (PET) is a cornerstone technology for in vivo quantification of Aβ and tau burden in the human brain.
- Aβ-PET Imaging: Utilizes radiotracers like Pittsburgh Compound B (PiB) to measure fibrillar Aβ plaque deposition in regions such as the frontal, lateral, temporal, and retrosplenial cortices. Scans are typically conducted over multiple years to track accumulation rates [98].
- Tau-PET Imaging: Employs radiotracers like Flortaucipir to assess the accumulation of hyperphosphorylated tau tangles, often focusing on Braak stage-related regions like the entorhinal cortex and inferior temporal gyrus [98].
- Plasma Biomarker Analysis: Increasingly used to measure concentrations of biomarkers like Aβ40, Aβ42, GFAP, NfL, and p-tau181 using highly sensitive technologies such as Single Molecule Array (SIMOA) [50]. This allows for larger-scale, longitudinal monitoring of pathological changes.
Table 2: Experimental Models and Their Applications in Estradiol-AD Research
| Model System | Key Characteristics | Primary Applications | Example Findings |
|---|---|---|---|
| Ovariectomized (OVX) Rodents [7] | Surgical removal of ovaries to mimic estrogen loss of menopause. | Study molecular mechanisms of estrogen deficiency and replacement. | E2 loss impaired spatial learning/memory; reduced synaptic proteins; increased neuroinflammation. E2 replacement reversed deficits. |
| Transgenic AD Mouse Models [96] | Genetically engineered to express human AD-related mutations (e.g., in APP, PSEN1). | Investigate interaction between estrogen signaling and specific AD pathologies. | Chemically induced perimenopause increased hippocampal Aβ accumulation and glial activation. |
| Human Cell Cultures (e.g., HEK293/tau) [97] | Cells transfected to express human tau protein. | Elucidate specific molecular pathways (e.g., tau phosphorylation). | ERα overexpression increased tau hyperphosphorylation via miR-218/PTPA pathway, while ERβ decreased it. |
| Human Longitudinal Cohorts (e.g., CLSA, ELITE) [8] [50] | Large-scale observational studies or clinical trials in postmenopausal women. | Examine real-world associations and effects of MHT on cognition and biomarkers. | Earlier menopause age linked to lower cognitive scores. Transdermal E2 associated with better episodic memory. |
Molecular Biology Techniques
- Receptor Analysis: Techniques like RNA interference (RNAi) and specific receptor antagonists (e.g., MPP/PHTPP for nuclear ERs, G15 for GPER1) are used to dissect the specific roles of different estrogen receptors [97].
- Pathway Analysis: Western blotting, RT-PCR, and ELISA are standard for quantifying protein and gene expression changes in pathways involved in synaptic plasticity (e.g., PSD-95), neuroinflammation, and Aβ processing (e.g., RAGE, LRP1) [7].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating Estradiol Mechanisms in AD Models
| Reagent / Tool | Function / Target | Research Application |
|---|---|---|
| 17β-estradiol [7] | Primary endogenous estrogen; agonist for ERα, ERβ, and mERs. | Gold standard for estrogen replacement in in vivo (OVX models) and in vitro studies. |
| Receptor Antagonists (MPP, PHTPP, G15) [97] | Selective antagonists for ERα, ERβ, and GPER1, respectively. | To pharmacologically dissect the contribution of specific receptor subtypes to observed effects. |
| Aβ and Tau Radioligands (PiB, Flortaucipir) [98] | High-affinity binders to Aβ plaques and tau tangles. | Enable quantification and tracking of AD neuropathology in vivo using PET neuroimaging. |
| SIMOA Assay Kits [50] | Ultra-sensitive digital ELISA technology. | Measure low-abundance plasma biomarkers of neurodegeneration (Aβ, p-tau181, NfL, GFAP). |
| shRNA Plasmids (targeting ERα/ERβ) [97] | Knock down expression of specific estrogen receptors. | Genetically validate the role of ER subtypes in cellular models of tau phosphorylation and neuroprotection. |
The link between estradiol therapy and Aβ/tau burden in postmenopausal women is complex and modulated by critical factors such as the timing of intervention, the specific estrogen formulation, and individual genetic background. The prevailing evidence supports the critical window hypothesis, suggesting that early initiation of estradiol-based MHT may help maintain healthy AD biomarker profiles, while late initiation could exacerbate tau pathology and accelerate cognitive decline. Future research must focus on personalized treatment frameworks that integrate age, timing, APOE genotype, vascular health, and specific MHT formulations to optimize the neuroprotective potential of estradiol for preventing Alzheimer's disease in women.
The investigation into estradiol-based Menopausal Hormone Therapy (MHT) and its impact on cognitive performance represents a critical, yet complex, frontier in neuroendocrinology. Accumulating evidence suggests that the decline in estradiol during menopause contributes to cognitive changes, positioning estradiol not merely as a reproductive hormone but as a key neuromodulator. This whitepaper analyzes the current clinical data through the lens of Class III evidence, as defined by the American Academy of Neurology, which encompasses findings from observational studies, cross-sectional analyses, and retrospective cohorts. This level of evidence is crucial for generating hypotheses and identifying associations, though it cannot establish causality. Recent large-scale studies, including analyses from the Canadian Longitudinal Study on Aging (CLSA), provide robust Class III data that illuminate how factors such as age at menopause initiation, MHT formulation, and route of administration are associated with differential cognitive outcomes across distinct cognitive domains [25]. This analysis frames these clinical findings within the broader thesis of estradiol's fundamental hormonal mechanisms, exploring its genomic, non-genomic, and neurosteroid actions in the brain.
Neurobiological Mechanisms of Estradiol in the Brain
To critically evaluate the clinical evidence, one must first understand the multifaceted mechanisms through which estradiol modulates brain function. Estradiol's actions extend beyond classic genomic signaling to include rapid membrane-initiated effects and local synthesis within the brain.
Genomic and Non-Genomic Signaling Pathways
Estradiol exerts its effects via two primary mechanisms. The classical genomic pathway involves estradiol binding to intracellular estrogen receptors (ERα and ERβ), which then dimerize and bind to estrogen response elements (EREs) on DNA, acting as ligand-dependent transcription factors to alter protein synthesis and elicit long-lasting changes in neural function [16]. These receptors are densely located in brain areas critical for memory, including the hippocampus, medial prefrontal cortex, and basal forebrain [16].
Complementing this, estradiol also activates non-genomic pathways by binding to membrane-associated estrogen receptors, including those localized in cell bodies, spines, and presynaptic terminals. This binding initiates rapid intracellular signaling cascades (within seconds to minutes) via kinases such as MAPK and PI3K/Akt, which can modulate synaptic plasticity, neuroprotection, and immediate cognitive processes [16] [44]. These rapid mechanisms are implicated in the consolidation of memory.
The diagram below illustrates the integration of these pathways in a neuronal context:
Functional Impact on Neural Circuits
Neuroimaging studies provide compelling evidence for these mechanisms in humans. Functional MRI and PET studies show that estrogen therapy modulates brain activity during memory tasks. Specifically, it enhances hippocampal and parahippocampal function during the retrieval stage of episodic memory and increases activation in the prefrontal cortex, an area critical for executive functions and working memory [44]. These neurophysiological effects are believed to underpin the cognitive enhancements observed in some clinical studies, particularly when estradiol interacts with cholinergic and serotonergic neurotransmitter systems [44].
Analysis of Current Class III Evidence
The most robust Class III evidence comes from large-scale, cross-sectional observational studies that have examined the association between menopausal factors, MHT use, and cognitive performance.
Key Studies and Methodologies
The following table summarizes the design and primary cognitive findings of two pivotal studies providing Class III evidence.
Table 1: Key Class III Studies on Estradiol and Cognitive Performance
| Study | Design & Participants | Cognitive Domains Assessed | Primary Findings |
|---|---|---|---|
| CLSA Study (Puri et al., 2025) [25] | - Design: Cross-sectional observational- Participants: 7,251 postmenopausal women (mean age: 60.5)- Data Source: Canadian Longitudinal Study on Aging (CLSA) | - Episodic Memory- Prospective Memory- Executive Functions | - Earlier menopause age was associated with lower scores across all domains.- Transdermal estradiol was associated with higher episodic memory.- Oral estradiol was associated with higher prospective memory. |
| NHANES Analysis (Xu et al., 2024) [43] | - Design: Cross-sectional analysis- Participants: 731 women aged ≥60- Data Source: U.S. National Health and Nutrition Examination Survey (NHANES) 2013-2014 | - Processing Speed / Attention (DSST)- Verbal Learning (CERAD)- Verbal Fluency (AFT) | - Higher serum estradiol levels were associated with higher DSST scores, indicating better processing speed and working memory.- No significant associations were found with CERAD or AFT scores. |
Impact of Menopause Timing and MHT Administration Route
A critical finding from the Class III evidence is the significant association between the timing of menopause and cognitive performance. The CLSA study reported that every one-year decrease in age at menopause was associated with a statistically significant decrease in scores for episodic memory (β = 0.050, p < 0.001), prospective memory (β = 0.047, p < 0.001), and executive functions (β = 0.061, p < 0.001) [25]. This suggests that a shorter lifetime exposure to endogenous estradiol may have long-term implications for cognitive health.
Furthermore, the route of estradiol administration appears to have a domain-specific effect on cognition, a nuance that is crucial for precision medicine. The CLSA data indicates that the cognitive benefits of MHT are not uniform but are influenced by the method of delivery [25]:
- Transdermal Estradiol: Associated with higher episodic memory scores (Cohen's d = 0.303) compared to no MHT.
- Oral Estradiol: Associated with higher prospective memory scores (Cohen's d = 0.283) compared to no MHT.
- Executive Functions: Neither administration route showed a significant association (p = 0.345).
This differential impact is visualized in the following workflow, which maps the critical factors identified in the evidence to their specific cognitive outcomes:
Emerging Evidence from Biomarker Studies
Beyond cognitive scores, Class III evidence is evolving to include the impact of MHT on Alzheimer's disease (AD) biomarkers. A secondary analysis of the Early versus Late Intervention Trial with Estradiol (ELITE) presented in 2025 investigated the effect of oral estradiol on plasma AD biomarkers in early (<6 years postmenopause) versus late (≥10 years postmenopause) women [50]. The findings provide partial support for the critical window hypothesis, which posits that initiating therapy early in menopause confers greater neuroprotective benefits. The analysis found that among early postmenopausal women, MHT was associated with numerically greater declines in Aβ42 and increases in the Aβ42/Aβ40 ratio, suggesting a potentially favorable shift in amyloid pathology, though these changes did not reach statistical significance. Notably, MHT significantly accelerated the decline of Aβ40 in the overall cohort (p=0.049) and had no effect on biomarkers in late postmenopausal women [50].
Experimental Protocols & Research Reagents
For researchers seeking to replicate or build upon this field of inquiry, understanding the detailed methodologies and key reagents is essential.
Detailed Methodology from Key Studies
CLSA Cognitive Assessment Protocol [25]: The CLSA employed a battery of standardized cognitive tests administered to a large national cohort. The specific domains and tests were:
- Episodic Memory: Assessed using tests like the Rey Auditory Verbal Learning Test, which involves the immediate and delayed recall of word lists.
- Prospective Memory: Assessed via tasks that require participants to remember to perform a future action (e.g., pressing a button in response to a specific cue after a delay).
- Executive Functions: Evaluated using instruments like the Mental Alternation Task or the Controlled Oral Word Association Test, which measure cognitive flexibility, inhibition, and verbal fluency.
- Statistical Analysis: Linear regression models were used to test associations between cognitive performance (dependent variable) and menopause age/MHT use (independent variables), with adjustments for age, education, and vascular risk factors.
NHANES Serum Estradiol Measurement Protocol [43]: This study provides a model for correlating systemic hormone levels with cognitive performance.
- Blood Sample Collection: Venous blood was drawn from participants after an overnight fast.
- Estradiol Quantification: Serum estradiol levels were measured using isotope dilution liquid chromatography tandem mass spectrometry (ID-LC-MS/MS), a gold-standard method for hormone assay accuracy and sensitivity, developed by the Centers for Disease Control and Prevention (CDC).
- Cognitive Tests:
- Digit Symbol Substitution Test (DSST): Assesses processing speed, sustained attention, and working memory.
- CERAD Word Learning Test: Assesses immediate and delayed verbal memory.
- Animal Fluency Test (AFT): Assesses semantic memory and executive function.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Tools for Research on Estradiol and Cognition
| Item / Reagent | Function / Application in Research | Example from Search Results |
|---|---|---|
| 17-β Estradiol | The primary bioactive estrogen used in MHT formulations for both in vivo and in vitro studies. | Used in the CLSA (MHT type) and ELITE trial (1 mg oral dose) [25] [50]. |
| ID-LC-MS/MS | Gold-standard method for precise and accurate quantification of serum steroid hormone levels. | Used in the NHANES analysis to measure participant serum estradiol [43]. |
| Cognitive Test Batteries | Standardized tools to assess specific cognitive domains (memory, executive function, fluency). | CLSA: Episodic/Prospective memory tests. NHANES: CERAD, DSST, Animal Fluency [25] [43]. |
| ApoE Genotyping Kits | To determine ApoE ε4 carrier status, a major genetic risk factor for Alzheimer's disease, for stratified analysis. | CLSA study examined effect modification by ApoE ε4 status [25]. |
| SIMOA Technology Kits | Highly sensitive immunoassay technology for quantifying neurodegenerative biomarkers in plasma (e.g., Aβ40, Aβ42, GFAP, NfL). | Used in the ELITE trial analysis to measure Alzheimer's disease blood biomarkers [50]. |
| fMRI / PET Protocols | Neuroimaging techniques to visualize and quantify estradiol's effect on brain activity and function during cognitive tasks. | Used to show estradiol enhances hippocampal and prefrontal activation [44]. |
The body of Class III evidence convincingly demonstrates an association between estradiol-based MHT and cognitive performance, with critical modifiers being the age at menopause, route of administration, and cognitive domain assessed. The consistent signal that transdermal and oral estradiol have domain-specific benefits, coupled with biomarker data suggesting a potential impact on Alzheimer's disease pathology, provides a strong scientific rationale for further investigation.
However, the inherent limitations of Class III evidence must be acknowledged. Cross-sectional and observational studies cannot prove causation, and confounding factors may influence the results. The field now requires prospective, randomized controlled trials (RCTs) designed with these nuances in mind—specifically testing different administration routes in women initiating therapy early in menopause and using sensitive, domain-specific cognitive tests and AD biomarkers as primary outcomes. Furthermore, integrating the neurobiological mechanisms of estradiol action with these clinical findings will be essential for developing the next generation of targeted therapeutics for cognitive aging in women. The existing Class III evidence provides a robust and necessary map for guiding these future endeavors.
Estradiol, the most potent estrogen, exerts profound influence on brain function through complex signaling mechanisms. Traditionally viewed as a circulating hormone, our understanding has expanded to include its role as a neurosteroid synthesized directly within the brain (neuroestradiol, nE2) [99]. Estradiol signaling occurs through both genomic pathways (hours to days) via nuclear estrogen receptors and rapid, non-genomic pathways (seconds to minutes) initiated at membrane receptors [100] [101]. These mechanisms collectively regulate neuronal connectivity, synaptic plasticity, and cognitive function [102]. The emerging recognition that estradiol functions as a neuromodulator in cortical and hippocampal circuits reveals new therapeutic opportunities for cognitive disorders, particularly those affecting women during hormonal transitions [99] [102].
This review explores the molecular machinery of intraneuronal estradiol synthesis and membrane receptor signaling, with emphasis on therapeutic targeting for cognitive enhancement. We synthesize current understanding of how estradiol-sensitive signaling pathways coordinate neuronal function and how their dysregulation may contribute to cognitive decline. Within the broader thesis of hormonal mechanisms influencing cognitive performance, we examine evidence that targeting neuroestradiol systems represents a promising frontier for intervention in age-related cognitive decline and neurodegenerative diseases [9].
Molecular Mechanisms of Intraneuronal Estradiol Synthesis
The Neuroestradiol Synthesis Pathway
The brain maintains the capacity for local estradiol synthesis through the expression of steroidogenic enzymes. Aromatase (CYP19A1), the rate-limiting enzyme that converts androgens to estrogens, is centrally involved in this process [99]. However, the complete steroidogenic pathway from cholesterol to estradiol requires coordinated action of multiple enzymes:
Table: Key Enzymes in Neuroestradiol Synthesis
| Enzyme | Gene | Function in Neuroestradiol Synthesis | Cellular Localization |
|---|---|---|---|
| StAR | STARD1 | Cholesterol translocation into mitochondria | Mitochondrial membrane |
| P450scc | CYP11A1 | Conversion of cholesterol to pregnenolone | Inner mitochondrial membrane |
| 3β-HSD | HSD3B | Conversion of pregnenolone to progesterone | Endoplasmic reticulum |
| CYP17A1 | CYP17 | Hydroxylase/lyase activity for androgen synthesis | Endoplasmic reticulum |
| Aromatase | CYP19A1 | Conversion of androgens to estrogens | Synaptic terminals, endoplasmic reticulum |
The presence of these enzymes in neurons provides a direct pathway for de novo biosynthesis of estradiol from cholesterol [102]. Critically, aromatase has been identified at pre-synaptic terminals in multiple brain regions including hippocampus, hypothalamus, and cerebral cortex [102]. This synaptic localization places the estradiol synthesis machinery at ideal locations for rapid, localized modulation of synaptic function.
Regulation of Neuroestradiol Production
Neuroestradiol synthesis is dynamically regulated by neuronal activity. In the zebra finch cortex, aromatase activity is controlled by depolarization-sensitive calcium-dependent events, providing a mechanism for activity-dependent estradiol production [102]. This rapid biosynthesis (within minutes) enables estradiol to function as a neuromodulator that fine-tunes synaptic strength in response to experience [102].
Evidence from multiple species indicates that brain-synthesized estradiol significantly influences neuronal physiology independent of peripheral sources. Even following gonadectomy, significant estradiol concentrations persist in specific brain regions, with studies demonstrating that approximately 60-70% of hippocampal estradiol remains after ovariectomy in rodents [99]. This local synthesis enables region-specific regulation of estradiol signaling that may be targeted for therapeutic benefit.
Membrane-Initiated Estradiol Signaling Mechanisms
Estrogen Receptor Variants and Membrane Localization
Estradiol initiates rapid signaling through receptors localized at the plasma membrane. While classical nuclear estrogen receptors (ERα and ERβ) can translocate to the membrane, additional receptors including the G-protein coupled estrogen receptor (GPER1) contribute to membrane-initiated signaling [100] [103].
Table: Membrane Estrogen Receptors and Their Signaling Properties
| Receptor | Membrane Localization Mechanism | Primary Signaling Pathways | Neuronal Functions |
|---|---|---|---|
| mERα | Palmitoylation by DHHC7/DHHC21, caveolin interaction | mGluR1/5 coupling, ERK/MAPK activation, PI3K/Akt | Dendritic spine formation, synaptic plasticity, lordosis behavior |
| mERβ | Palmitoylation by DHHC7/DHHC21 | mGluR2/3 coupling, cAMP modulation | Neuroprotection, inhibitory neurotransmission |
| GPER1 | Intrinsic membrane protein (GPCR) | EGFR transactivation, ERK/MAPK, PI3K/Akt | Neuroprotection, cognitive function, metabolic regulation |
The trafficking of classical ERs to the membrane requires post-translational modifications, particularly S-palmitoylation at conserved cysteine residues [3]. This lipid modification increases receptor hydrophobicity, facilitating association with membrane microdomains. Two specific palmitoyl acyltransferases, DHHC7 and DHHC21, mediate ER palmitoylation and surface trafficking in neurons [3]. Mutation of the palmitoylation site eliminates membrane signaling without affecting nuclear functions, demonstrating the specificity of this targeting mechanism [3].
Caveolin Proteins and Signaling Microdomains
Caveolin proteins (Cav1-3) organize estrogen receptors and their effector systems into functional signaling microdomains [3]. These membrane proteins create spatial compartments that determine signaling specificity by isolating different estrogen-responsive pathways within the same neuron. Specifically, Cav1 and Cav3 generate distinct complexes that separate estrogen activation of group I from group II metabotropic glutamate receptor (mGluR) signaling [3].
The interaction between membrane ERs and mGluRs provides a mechanism for estradiol to influence multiple signaling pathways without requiring glutamate binding [3]. This arrangement allows estradiol to activate mGluR signaling directly, affecting downstream effectors including ERK1/2 and CREB that regulate synaptic plasticity and cognitive function.
Receptor Dynamics and Trafficking
Membrane estrogen receptors exhibit dynamic regulation by estradiol itself. Estradiol initially promotes ERα trafficking to the membrane, then induces internalization through a mechanism involving GRK2 phosphorylation and β-arrestin-1 (Arrb1) recruitment [3]. This internalization both terminates signaling and potentially facilitates endosomal signaling, with Arrb1 serving as a scaffold for downstream signaling molecules like Ras/Raf/MEK [3].
The discovery of an ERα splice variant missing exon 4 (ERαΔ4) that predominates in neuronal membranes suggests additional complexity in membrane estrogen signaling [3]. This variant appears particularly important for membrane-initiated signaling in neuronal and glial cells.
Diagram 1: Membrane Estrogen Receptor Signaling Pathways. Estradiol activates membrane-localized receptors (mERα, mERβ, GPER1) organized in caveolin-containing microdomains. These receptors couple to mGluRs and kinase pathways, ultimately regulating gene expression, dendritic spine remodeling, and synaptic plasticity.
Experimental Approaches for Studying Neuroestradiol Systems
Measuring Neuroestradiol Synthesis and Dynamics
Investigating intraneuronal estradiol synthesis requires specialized methodologies that can distinguish centrally-produced estradiol from peripheral sources:
Microdialysis with Mass Spectrometry: This approach allows continuous sampling of extracellular fluid in specific brain regions with high temporal resolution. When coupled with LC-MS/MS, it provides sensitive detection of estradiol fluctuations in response to physiological stimuli. The technique has revealed that estradiol concentrations in the hippocampus can change within 15-30 minutes following neuronal activation [99].
Aromatase Activity Assays: Using tritiated-androgen substrates (³H-androstenedione), aromatase activity can be measured in tissue samples by detecting tritiated water production. This method has demonstrated that aromatase activity increases following glutamatergic stimulation in cortical and hippocampal tissues [102].
Genetic Manipulation of Steroidogenic Enzymes: Conditional knockout mice with neuron-specific deletion of aromatase or other steroidogenic enzymes (e.g., StAR, 3β-HSD) enable researchers to isolate the contributions of neuroestradiol to cognitive function. Studies using these models have identified specific roles for neuroestradiol in hippocampal-dependent memory and dendritic spine formation [99].
Visualizing Membrane Receptor Signaling
Advanced imaging and molecular techniques are essential for studying rapid estradiol signaling:
Fluorescence Resonance Energy Transfer (FRET): FRET-based biosensors can visualize real-time conformational changes in estrogen receptors and downstream signaling molecules following estradiol application. This technique has revealed that membrane ER activation occurs within seconds of estradiol exposure [3].
Surface Biotinylation and Protein Cross-linking: These biochemical approaches allow researchers to distinguish membrane-localized receptors from intracellular pools. Using these methods, researchers have demonstrated that only ~2-5% of total cellular ERα is present at the plasma membrane under basal conditions, but this pool mediates rapid signaling [3].
Electrophysiological Recordings: Patch-clamp techniques in brain slices can measure rapid estradiol effects on neuronal excitability and synaptic transmission. These studies have shown that estradiol can enhance NMDA receptor currents within 5-10 minutes through membrane-initiated signaling [102].
Diagram 2: Experimental Workflow for Studying Neuroestradiol Systems. A multi-method approach is required to investigate neuroestradiol synthesis, membrane signaling, and functional outcomes, with integration across methodological domains.
Cognitive Implications and Therapeutic Applications
Estradiol and Cognitive Performance
Clinical and preclinical evidence demonstrates that estradiol significantly influences multiple cognitive domains through both genomic and membrane-initiated mechanisms:
Episodic Memory: The hippocampus, rich in estrogen receptors, is particularly sensitive to estradiol modulation. Research shows that estradiol enhances long-term potentiation (LTP), a cellular correlate of memory, through both nuclear and membrane receptors [102]. Clinical studies indicate that transdermal estradiol specifically benefits episodic memory in postmenopausal women [8].
Executive Function: Prefrontal cortex-dependent cognitive functions are modulated by estradiol via membrane receptor signaling. Earlier age at menopause is associated with lower executive function scores, with more pronounced effects in APOE ε4 carriers and women with higher parity [8].
Prospective Memory: This future-oriented memory function shows sensitivity to estrogen exposure, with oral estradiol administration associated with higher prospective memory scores in postmenopausal women [8].
Timing and Formulation Considerations
The therapeutic potential of estradiol-based interventions depends critically on timing and administration route:
Critical Window Hypothesis: The timing of estrogen therapy initiation relative to menopause significantly influences outcomes. Studies indicate that estrogen therapy started within 2 years of oophorectomy is associated with better episodic memory, working memory, and visuospatial processing in later life [9]. Conversely, initiation after age 70 may accelerate tau accumulation in temporal lobe regions [19].
Administration Route Effects: The route of estradiol administration influences its cognitive effects, likely due to differential metabolism and brain distribution. Transdermal estradiol bypasses first-pass hepatic metabolism, resulting in E2:E1 ratios similar to premenopausal women and is associated with higher episodic memory scores [8]. Oral estradiol undergoes hepatic conversion to estrone and is associated with higher prospective memory scores [8].
Table: Cognitive Domain Sensitivity to Estradiol Interventions
| Cognitive Domain | Neural Substrate | Most Effective Intervention | Effect Size (Cohen's d) |
|---|---|---|---|
| Episodic Memory | Medial temporal lobe (hippocampus) | Transdermal estradiol (early postmenopause) | 0.303 [8] |
| Prospective Memory | Frontotemporal networks | Oral estradiol | 0.283 [8] |
| Executive Function | Prefrontal cortex | Not significantly improved by current E2-based MHT | N/S [8] |
| Working Memory | Prefrontal cortex | Estrogen therapy after oophorectomy | β = 0.120 [9] |
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Research Tools for Investigating Neuroestradiol Systems
| Reagent/Category | Specific Examples | Research Application | Key Findings Enabled |
|---|---|---|---|
| Aromatase Inhibitors | Letrozole, Anastrozole, Exemestane | Block neuroestradiol synthesis | Hippocampal memory impairments reversible with estradiol replacement [99] |
| Membrane-Impermeable Estrogens | E2-BSA, E2-HRP | Selective activation of membrane receptors | Rapid spine formation and kinase activation independent of genomic signaling [3] |
| Selective ER Agonists/Antagonists | PPT (ERα-selective), DPN (ERβ-selective), G1 (GPER-selective) | Receptor-specific pathway activation | Distinct roles for ERα (reproductive behavior) vs. ERβ (neuroprotection) [3] |
| Palmitoylation Inhibitors | 2-bromopalmitate, DHHC7/21 siRNA | Disrupt membrane receptor localization | Elimination of membrane ER signaling without affecting genomic functions [3] |
| Caveolin Disruptors | Methyl-β-cyclodextrin, Caveolin siRNA | Disrupt membrane signaling microdomains | Loss of mER-mGluR coupling specificity [3] |
| Aromatase Reporter Systems | Aromatase-Luciferase, Aromatase-GFP | Visualize and quantify aromatase expression | Activity-dependent aromatase expression at synapses [102] |
Future Directions and Therapeutic Development
The expanding understanding of neuroestradiol synthesis and membrane receptor signaling reveals several promising therapeutic avenues:
Targeted Receptor Modulation
Future therapeutic development should focus on receptor-specific agonists that target beneficial pathways while minimizing side effects. The differential effects of ERα versus ERβ activation suggest that ERβ-selective agonists may provide neuroprotection and cognitive benefits without the proliferative effects associated with ERα activation [103]. Similarly, GPER1-selective ligands show promise for enhancing synaptic plasticity while potentially avoiding cardiovascular risks associated with classical ER activation [103].
Enzyme-Targeted Approaches
Modulating neuroestradiol synthesis through brain-specific aromatase inhibitors or enhancers represents another strategic approach. Rather than systemic hormone manipulation, fine-tuning local estradiol production in specific brain regions could optimize cognitive function while minimizing peripheral effects. Research indicates that allosteric modulation of aromatase activity might achieve more precise control than traditional competitive inhibitors [99].
Timing and Formulation Optimization
The consistent evidence for a critical window for beneficial effects underscores the need for precisely timed interventions. Future research should establish biomarkers that identify optimal timing for individual patients. Similarly, developing formulations with controlled regional distribution could maximize brain effects while minimizing peripheral exposure. Nanoparticle-based delivery systems that target estradiol or estradiol mimetics to specific brain regions represent an emerging frontier [19].
Targeting intraneuronal estradiol synthesis and membrane receptor signaling represents a promising therapeutic horizon for cognitive enhancement and neuroprotection. The complex interplay between neuroestradiol production, membrane receptor dynamics, and downstream signaling effects provides multiple points for intervention. Success in this arena will require careful consideration of timing, receptor specificity, and individual risk factors.
Future research should prioritize the development of brain-specific delivery systems, personalized timing protocols, and receptor-selective compounds that maximize cognitive benefits while minimizing risks. As our understanding of the intricate spatial and temporal regulation of estradiol signaling in the brain continues to evolve, so too will opportunities to harness this system for therapeutic benefit in cognitive aging and neurodegenerative diseases.
Conclusion
The evidence unequivocally demonstrates that estradiol exerts significant, domain-specific effects on cognitive performance through multiple complementary mechanisms involving genomic signaling, rapid membrane actions, and interactions with key neurotransmitter systems. The efficacy of estradiol-based interventions is critically dependent on multiple factors including formulation, administration route, timing of initiation, and individual patient characteristics. Future research must prioritize randomized controlled trials that account for these variables, particularly the therapeutic window of opportunity and the differential effects of specific estradiol formulations. Furthermore, investigation into FSH as a parallel therapeutic target and the development of compounds that leverage estradiol's neuroprotective mechanisms without its associated risks represent promising frontiers. For drug development professionals, these findings underscore the necessity of precision medicine approaches that consider hormonal status, genetic profile, and individual health history in the design of cognitive therapeutics for aging women.
References
- 1. Structure–Non-Genomic Neuroprotection Relationship of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1905848/]
- 2. Genomic and non-genomic actions of estrogen [https://pubmed.ncbi.nlm.nih.gov/25436542/]
- 3. ESTRADIOL MEMBRANE-INITIATED SIGNALING IN THE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5744592/]
- 4. The estrogen–brain interface in neuroinflammation [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1671552/full]
- 5. Distinct effect profiles of environmental estrogens [https://www.sciencedirect.com/science/article/abs/pii/S0041008X10000748]
- 6. Molecular mechanisms involved in the regulation of ... [https://www.sciencedirect.com/science/article/abs/pii/S0960076011001932]
- 7. Impacts on cognitive dysfunction in a post-menopausal ... [https://www.sciencedirect.com/science/article/abs/pii/S1098882325000772]
- 8. Association Between Menopause Age and Estradiol-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12380479/]
- 9. Lifetime estrogen exposure and domain-specific cognitive ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1524474/full]
- 10. Beyond Hot Flashes: The Role of Estrogen Receptors in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469143/]
- 11. patterns of Distribution and beta in the... estrogen receptor alpha [https://pubmed.ncbi.nlm.nih.gov/17570500/]
- 12. An Expanded View of Estrogen Localization... | SpringerLink Receptor [https://link.springer.com/chapter/10.1007/978-1-4615-0339-2_3]
- 13. Estrogen receptor beta signaling enhances extinction ... [https://www.nature.com/articles/s41398-024-03001-y]
- 14. Targeting Estrogen Receptors in PCOS [https://www.sciencedirect.com/science/article/pii/S1043661825004335]
- 15. Structural plasticity of the hippocampus in response to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6423800/]
- 16. Estradiol and cognitive function: Past, present and future - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4318702/]
- 17. Hormonal regulation of hippocampal dendritic morphology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2633690/]
- 18. Estradiol Induces Formation of Dendritic Spines in ... [https://www.sciencedirect.com/science/article/pii/S0018506X01916885]
- 19. Latest research on hormone replacement therapy and ... [https://www.parsemus.org/2025/11/latest-research-on-hormone-replacement-therapy-and-brain-health/]
- 20. Estrogen modulates reward prediction errors and ... [https://www.nature.com/articles/s41593-025-02104-z]
- 21. Estrogen-Cholinergic Interactions: Implications for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4573353/]
- 22. Estrogen–cholinergic interactions: Implications for ... [https://www.sciencedirect.com/science/article/abs/pii/S0018506X15300015?via%3Dihub]
- 23. Role of Estradiol in the Expression of Genes Involved in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6520586/]
- 24. The impact of estradiol on serotonin, glutamate, and ... [https://pubmed.ncbi.nlm.nih.gov/38586193/]
- 25. Association Between Menopause Age and Estradiol-Based ... [https://pubmed.ncbi.nlm.nih.gov/40865026/]
- 26. Hormone therapy type matters for memory performance ... [https://www.aan.com/PressRoom/home/PressRelease/5280]
- 27. Estrogenic regulation of memory consolidation: A look beyond ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5787049/]
- 28. Uncovering the Mechanisms of Estrogen Effects on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2440702/]
- 29. Concurrent Medial Prefrontal Cortex and Dorsal ... [https://www.eneuro.org/content/6/4/ENEURO.0271-19.2019]
- 30. Estrogen, Cognitive Performance, and Functional Imaging ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2022.866122/full]
- 31. Estradiol Associations with Brain Functional Connectivity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10885742/]
- 32. A novel Y-maze paradigm with enhanced sensitivity to subtle ... [https://bmcmethods.biomedcentral.com/articles/10.1186/s44330-025-00043-6]
- 33. Probing the nature of episodic memory in rodents [https://www.sciencedirect.com/science/article/abs/pii/S0149763422004195]
- 34. Neuroscientist's Behavioral Toolbox for Studying Episodic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11366770/]
- 35. From rodents to humans: Rodent behavioral paradigms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10679632/]
- 36. Do the Cambridge Neuropsychological Test Automated Battery episodic memory measures discriminate amnestic mild cognitive impairment? - PubMed [https://pubmed.ncbi.nlm.nih.gov/24150876/]
- 37. III. NIH Toolbox Cognition Battery (CB): measuring episodic memory - PubMed [https://pubmed.ncbi.nlm.nih.gov/23952201/]
- 38. Pharmacokinetics of estradiol [https://en.wikipedia.org/wiki/Pharmacokinetics_of_estradiol]
- 39. Comparative Evidence Between Transdermal and Oral ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK614934/]
- 40. Estradiol metabolism: an endocrine biomarker for modulation ... [https://pubmed.ncbi.nlm.nih.gov/9167995/]
- 41. Estradiol metabolites as biomarkers of endometrial cancer ... [https://www.sciencedirect.com/science/article/abs/pii/S0960076017303187]
- 42. Comparative Evidence Between Transdermal and Oral ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK614933/]
- 43. Association between serum estradiol levels and cognitive ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2024.1356791/full]
- 44. Mechanisms of Action of Estrogen in the Brain [https://pmc.ncbi.nlm.nih.gov/articles/PMC4999426/]
- 45. Endogenous estradiol and inflammation biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC7472689/]
- 46. The Role of Estrogen in Brain and Cognitive Aging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6694379/]
- 47. Associations of estrogen with modifiable and non‐modifiable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12631545/]
- 48. High variability in serum estradiol measurements in men ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5699465/]
- 49. Reliability and validity of serum sex hormone measurements [https://pubmed.ncbi.nlm.nih.gov/8922302/]
- 50. Estradiol-Containing MHT May Impact Alzheimer Disease ... [https://www.pharmacytimes.com/view/estradiol-containing-mht-may-impact-alzheimer-disease-related-biomarkers-in-postmenopausal-women]
- 51. Estrogen levels do not correlate with improvement in cognition [https://pubmed.ncbi.nlm.nih.gov/12580705/]
- 52. Quantitative meta-analysis of fMRI and PET studies reveals ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2013.00749/full]
- 53. The use of neuroimaging techniques in the early and ... [https://www.nature.com/articles/s41380-023-02215-8]
- 54. Brain PET and SPECT imaging and quantification: a survey of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10498883/]
- 55. Understanding WCAG 2 Contrast and Color Requirements [https://webaim.org/articles/contrast/]
- 56. Color Contrast | Digital Accessibility - Michigan State University [https://webaccess.msu.edu/tutorials/basics/color-contrast]
- 57. Quantitative PET in the 2020s: a roadmap - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9358699/]
- 58. The Critical Window Hypothesis of Hormone Therapy and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3780981/]
- 59. FAQs On The Critical Window Hypothesis for Menopausal ... [https://www.patientcareonline.com/view/faqs-on-the-critical-window-hypothesis-for-menopausal-hormone-therapy-s-neuroprotective-effects]
- 60. Postmenopausal hormone therapy and cognition [https://www.sciencedirect.com/science/article/abs/pii/S0018506X15000690]
- 61. Estradiol and cognitive function: Past, present and future [https://www.sciencedirect.com/science/article/pii/S0018506X14001846]
- 62. Recapping TMS 2025: Evolving Insights and Future ... [https://www.pharmacytimes.com/view/recapping-tms-2025-evolving-insights-and-future-directions-in-menopause-care]
- 63. Postmortem tissue biomarkers of menopausal transition [https://www.nature.com/articles/s41380-025-03177-9]
- 64. Brain aging shows nonlinear transitions, suggesting a midlife ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11912423/]
- 65. Episodic Memory: A Comparative Approach - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3678104/]
- 66. From episodic to habitual prospective memory: ERP ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2014.00489/full]
- 67. Estradiol-based Menopausal Hormone Therapy is ... [https://www.medrxiv.org/content/10.1101/2025.01.13.25320471v1]
- 68. The Differences Between Prospective And Retrospective ... [https://www.betterhelp.com/advice/memory/differences-between-prospective-memory-and-retrospective/]
- 69. Growth Hormone-Releasing Hormone Modulation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6487872/]
- 70. Endogenous Hormones and Cognitive Decline in Women [https://www.mdpi.com/2673-4184/4/2/9]
- 71. Moderating Variable In Statistics [https://www.simplypsychology.org/moderating-variable.html]
- 72. Physical Activity May Offset Cognitive Decline Risk in ... [https://www.neurologylive.com/view/physical-activity-may-offset-cognitive-decline-risk-apoe-4-carriers-study-finds]
- 73. Associations between reproductive history, hormone use ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2022.1014605/full]
- 74. Associations and interactions between APOE e4 genotype ... [https://pubmed.ncbi.nlm.nih.gov/41140810/]
- 75. Moderation (statistics) [https://en.wikipedia.org/wiki/Moderation_(statistics)]
- 76. Assessing bias: the importance of considering confounding [https://pmc.ncbi.nlm.nih.gov/articles/PMC3503514/]
- 77. Biases and Confounding [https://www.healthknowledge.org.uk/public-health-textbook/research-methods/1a-epidemiology/biases]
- 78. Defining Comorbidity: Implications for Understanding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2713155/]
- 79. The Conceptualization and Measurement of Comorbidity [https://pmc.ncbi.nlm.nih.gov/articles/PMC3800641/]
- 80. Confounding variables in statistics: How to identify and ... [https://www.statsig.com/perspectives/confounding-variables-statistics-identify-control]
- 81. Dangers of residual confounding: a cautionary tale featuring ... [https://bmcpsychology.biomedcentral.com/articles/10.1186/s40359-021-00653-z]
- 82. Hormone Therapy Type Key to Memory Benefits After Menopause [https://www.medscape.com/viewarticle/hormone-therapy-type-key-memory-benefits-after-menopause-2025a1000nat]
- 83. Continuous-combined oral estradiol /drospirenone has no detrimental... [https://research.monash.edu/en/publications/continuous-combined-oral-estradioldrospirenone-has-no-detrimental/]
- 84. Genome-wide Association Study of Estradiol Levels and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8530739/]
- 85. In vivo brain estrogen receptor density by neuroendocrine ... [https://www.nature.com/articles/s41598-024-62820-7]
- 86. Estrogen Effects on Cognitive and Synaptic Health Over the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4491541/]
- 87. Study Sheds New Light on How Hormones Influence ... [https://www.nyu.edu/about/news-publications/news/2025/november/study-sheds-new-light-on-how-hormones-influence-decision-making-.html]
- 88. Estradiol-Based Hormone Therapy Linked to Better ... [https://elcaminowomen.com/blog/menopause/estradiol-based-hormone-therapy-linked-to-better-memory-in-cognitively-normal-postmenopausal-women.html]
- 89. Brain-derived estrogen and neural function [https://www.sciencedirect.com/science/article/pii/S0149763421005078]
- 90. From hormones to neurodegeneration: how FSH drives ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12206753/]
- 91. FSH and ApoE4 contribute to Alzheimer's disease-like ... [https://www.nature.com/articles/s41467-023-42282-7]
- 92. FSH blockade improves cognition in mice with Alzheimer's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9940301/]
- 93. Follicle-Stimulating Hormone Linked to Cognitive Decline ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1697255/full]
- 94. Targeting FSHR is a highly promising strategy for ... [https://www.nature.com/articles/s41380-025-03048-3]
- 95. Research progress on FSH-FSHR signaling in the ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1506450/full]
- 96. Estrogen, menopause, and Alzheimer's disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12256231/]
- 97. Estrogen Receptors: A New Frontier in Alzheimer's Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11354998/]
- 98. Associations between hormone therapy use and tau ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11881894/]
- 99. Synthesis and impact of neuroestradiol on hippocampal ... [https://www.sciencedirect.com/science/article/pii/S2451965022000205]
- 100. Estrogen receptor signaling mechanisms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6533072/]
- 101. Estrogen receptor signaling mechanisms - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/31036290/]
- 102. Rapid Estradiol Modulation of Neuronal Connectivity and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3356153/]
- 103. Estrogen Signaling Pathway [https://www.creative-diagnostics.com/estrogen-signaling-pathway.htm]