Establishing Age-Specific Thyroid Hormone Reference Intervals in Older Adults Using Data Mining Algorithms
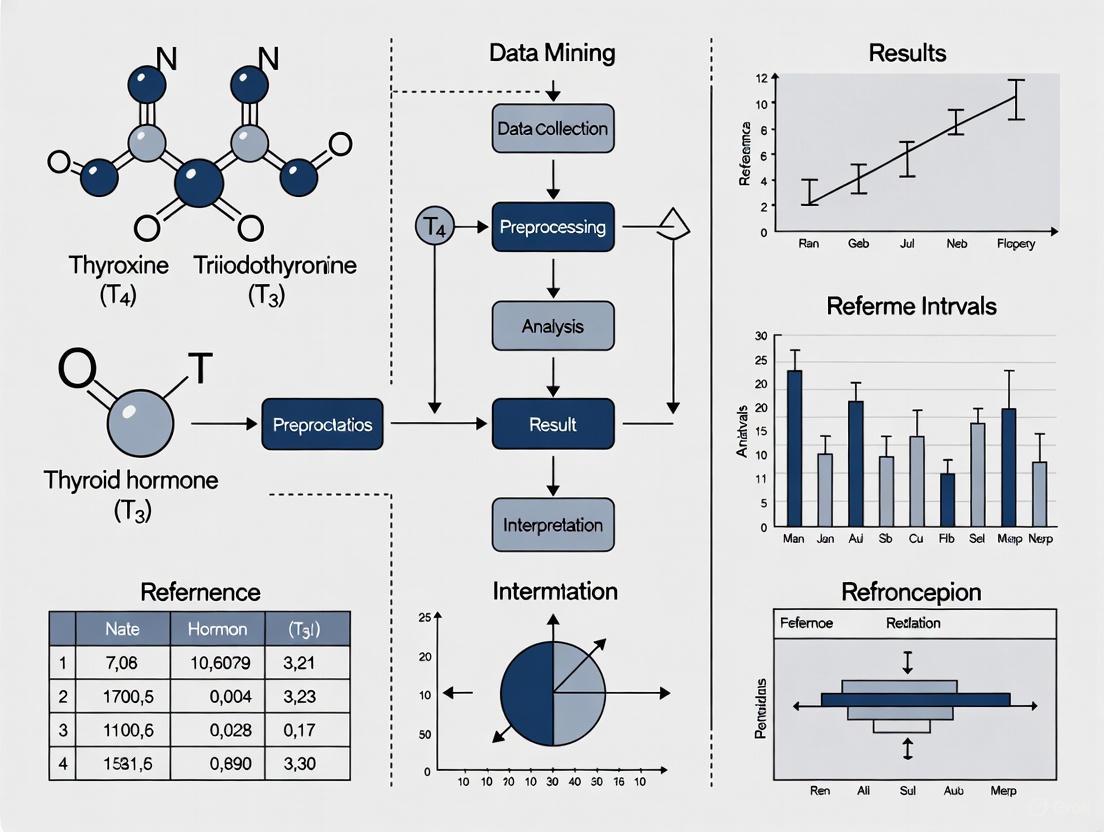
This article explores the critical application of data mining algorithms for establishing precise reference intervals (RIs) for thyroid hormones in the growing older adult population.
Establishing Age-Specific Thyroid Hormone Reference Intervals in Older Adults Using Data Mining Algorithms
Abstract
This article explores the critical application of data mining algorithms for establishing precise reference intervals (RIs) for thyroid hormones in the growing older adult population. It addresses the physiological changes in thyroid function with aging and the limitations of applying general population RIs to the elderly, which can lead to misdiagnosis of conditions like subclinical hypothyroidism. The content systematically reviews foundational concepts, compares the performance of key data mining methodologies like Hoffmann, Bhattachary, EM, kosmic, and refineR, provides solutions for common analytical challenges, and presents frameworks for clinical validation. Aimed at researchers and clinical professionals, this review synthesizes current evidence to guide the development of accurate, evidence-based, and clinically relevant RIs for geriatric thyroid care.
Why Age Matters: The Physiological and Clinical Imperative for Geriatric Thyroid Reference Intervals
The global population is undergoing a significant demographic shift, with projections indicating that nearly one-fifth of the U.S. population will be over 65 years old by 2030, rising to one-quarter by 2040 [1]. This aging trend is accompanied by an increased prevalence of thyroid disorders among older adults, creating an urgent need for age-specific diagnostic approaches. Thyroid cancer incidence among adults aged 55 and older increased dramatically by 185% from 1990 to 2021, with deaths and disability-adjusted life years (DALYs) rising by 116% and 108%, respectively [2]. The diagnosis and management of thyroid disorders in the elderly present unique challenges due to age-related physiological changes, comorbidities, polypharmacy, and the subtle, often atypical presentation of symptoms that can mimic normal aging [1].
Compounding these challenges is the fundamental issue that standard thyroid reference intervals (RIs) are primarily derived from younger populations, potentially leading to misdiagnosis in elderly patients. Research has demonstrated that thyroid-stimulating hormone (TSH) levels follow a U-shaped pattern across the lifespan, with elderly individuals often exhibiting higher TSH levels alongside decreases in free triiodothyronine (FT3) [1]. Without age-specific RIs, there is significant risk of both overdiagnosis leading to unnecessary treatment and underdiagnosis allowing progressive disease. This application note establishes the scientific basis for elderly-specific thyroid diagnostics and provides detailed protocols for developing and validating age-appropriate reference intervals.
Age-Related Changes in Thyroid Physiology
The aging process significantly impacts thyroid gland morphology and function. Thyroid volume typically shrinks after age 50, with histological changes including fibrosis, atrophy, and lymphocytic infiltration [3]. Iodine metabolism is also altered in the elderly, potentially related to low-salt diets and decreased absorption capacity due to comorbidities and medications [3].
Hormonal patterns shift characteristically with advancing age. Multiple studies have confirmed that TSH levels increase in healthy elderly individuals, while free T4 (FT4) remains relatively stable or increases slightly, and T3 (both total and free) typically decreases [3] [4]. This pattern differs markedly from younger populations and reflects complex alterations in the hypothalamic-pituitary-thyroid axis. Some researchers suggest that the age-related decline in thyroid function may represent an adaptive mechanism that could offer survival benefits in the elderly, contrasting with younger populations where low-normal thyroid status associates with increased cardiovascular risk [1].
Table 1: Age-Related Changes in Thyroid Hormone Parameters
| Parameter | Direction of Change with Aging | Clinical Implications |
|---|---|---|
| TSH | Increases | May represent normal aging rather than pathology |
| Free T4 | Remains stable or slight increase | Maintains metabolic homeostasis |
| Free T3 | Decreases | Contributes to metabolic slowing |
| Reverse T3 | Increases | Reduced clearance and conversion |
| Thyroid Volume | Decreases | Fibrosis and atrophy of gland tissue |
Establishing Age-Specific Reference Intervals: Experimental Evidence
Comparative Studies of Reference Intervals
Multiple studies have quantitatively demonstrated the necessity of age-specific reference intervals for thyroid function tests. A comprehensive prospective study of 1,200 subjects stratified by age established distinct TSH reference intervals for different age groups: 0.4-4.3 mU/L for ages 20-59 years, 0.4-5.8 mU/L for ages 60-79 years, and 0.4-6.7 mU/L for subjects 80 years or older [4]. The investigators reported that using manufacturer-defined ranges (without age segmentation) would have resulted in 6.5% of subjects aged 60-79 years and 12.5% of those over 80 years being misdiagnosed with elevated TSH [4].
Similarly, research on 22,207 Chinese subjects, including 2,254 (10.15%) aged ≥65 years, established specific RIs for the elderly population: TSH 0.55-5.14 mIU/L, FT3 3.68-5.47 pmol/L, and FT4 12.00-19.87 pmol/L [3]. The study further refined these intervals by sex, establishing TSH ranges of 0.56-5.07 mIU/L for elderly men and 0.51-5.25 mIU/L for elderly women [3]. When applying these age and sex-specific RIs instead of whole-group references, the prevalence of subclinical hypothyroidism decreased significantly from 9.83% to 6.29% (p < 0.001), demonstrating the substantial clinical impact of appropriate reference intervals [3].
Table 2: Comparison of Thyroid Reference Intervals Across Age Groups
| Study | Population | TSH Reference Interval (mIU/L) | FT4 Reference Interval | FT3 Reference Interval |
|---|---|---|---|---|
| Silva et al. (2013) [4] | 20-59 years | 0.4 - 4.3 | NR | NR |
| Silva et al. (2013) [4] | 60-79 years | 0.4 - 5.8 | NR | NR |
| Silva et al. (2013) [4] | ≥80 years | 0.4 - 6.7 | NR | NR |
| Yang et al. (2023) [3] | ≥65 years (overall) | 0.55 - 5.14 | 12.00 - 19.87 pmol/L | 3.68 - 5.47 pmol/L |
| Yang et al. (2023) [3] | ≥65 years (men) | 0.56 - 5.07 | NR | NR |
| Yang et al. (2023) [3] | ≥65 years (women) | 0.51 - 5.25 | NR | NR |
Longitudinal Patterns in Elderly Populations
Longitudinal studies provide further evidence for age-specific thyroid function trajectories. A study of 994 community-dwelling men aged ≥70 years without known thyroid disease found that over a mean follow-up period of 8.7 years, TSH concentrations increased while FT4 showed little change [5]. Among men who were euthyroid at baseline, 20.0% developed subclinical or overt hypothyroidism during follow-up, while only 0.7% developed subclinical or overt hyperthyroidism [5]. Higher baseline TSH was a strong predictor for progression to hypothyroidism (fully-adjusted odds ratio per 2.7-fold increase in TSH = 65.4, 95% CI = 31.9-134, p < 0.001) [5]. A baseline TSH concentration ≥2.34 mIU/L demonstrated 76% sensitivity and 77% specificity for predicting the development of subclinical or overt hypothyroidism in this elderly male population [5].
Comprehensive Protocol for Establishing Elderly-Specific Reference Intervals
Subject Recruitment and Selection Criteria
Objective: To establish validated reference intervals for thyroid hormones in populations aged ≥65 years through rigorous prospective recruitment and comprehensive exclusion criteria.
Materials:
- Laboratory information system with thyroid hormone records
- Siemens ADVIA Centaur XP Immunoassay System or equivalent
- Questionnaire for health status and medication use
- Thyroid ultrasonography equipment
- Aliquot tubes for serum storage at -80°C
Procedural Details:
Participant Recruitment: Recruit 2,000+ subjects aged ≥65 years from routine health checkups, stratified by sex and 5-year age categories (65-69, 70-74, 75-79, 80-84, ≥85 years) to ensure adequate representation across the elderly spectrum [3] [4].
Initial Screening: Apply exclusion criteria via structured questionnaire and interview:
- Personal or family history of thyroid disease
- Thyroid surgery or radioactive iodine treatment
- Use of medications with known interference on TSH or FT4 measurements (lithium, amiodarone, dopamine agonists, etc.)
- Iodine-containing compounds within previous 6 months
- Hospitalization due to illness or accident within previous 6 months
- Positive thyroid peroxidase antibodies (TPOAb) >60,000 IU/L or thyroglobulin antibodies (TgAb) >41,000 IU/L [3]
Physical Examination: Perform thyroid palpation to exclude subjects with goiter or thyroid nodules [4].
Laboratory Assessment: Conduct comprehensive testing including:
Thyroid Ultrasonography: Perform thyroid US on a subset of participants to exclude those with structural abnormalities; compare hormone levels between subjects with normal US and those without US to confirm exclusion necessity [4].
Statistical Analysis for Reference Intervals:
- Use the Tukey method to remove outliers [3]
- Calculate non-parametric reference intervals as the 2.5th and 97.5th percentiles of the distribution
- Establish separate reference intervals for sex and age subgroups within the elderly population
- Compare prevalence of subclinical hypothyroidism using whole-group RIs versus age-specific RIs [3]
Data Mining and Machine Learning Approaches
Objective: To leverage computational approaches for enhancing thyroid disorder diagnosis in elderly populations using large-scale laboratory data and electronic health records.
Materials:
- Thyroid disease datasets (e.g., UCI Machine Learning Repository, local laboratory data)
- Python/R programming environments with scikit-learn, TensorFlow, or PyTorch
- SMOTE-NC (Synthetic Minority Oversampling Technique-Nominal Continuous) for data balancing
- Light Gradient Boosting Machine (LGBM) classifier
- SHAP (Shapley Additive exPlanations) for model interpretability
Procedural Details:
Data Acquisition and Preprocessing:
- Acquire thyroid disease dataset with approximately 3,772 observations and 30 features [6]
- Handle missing values using imputation methods appropriate for laboratory data
- Encode categorical variables using one-hot encoding or label encoding
- Normalize continuous variables to standard scales
Addressing Class Imbalance:
- Apply SMOTE-NC to generate synthetic samples for minority classes
- Balance distribution between "sick" and "negative" categories [6]
- Validate synthetic data quality through visualization and statistical testing
Model Development and Hyperparameter Tuning:
- Implement LightGBM classifier with fine-tuned hyperparameters
- Compare against benchmark models: Random Forest, SVM, K-Nearest Neighbors, Decision Trees, Artificial Neural Networks [7] [6]
- Conduct hyperparameter optimization using grid search or Bayesian optimization
- Employ k-fold cross-validation to prevent overfitting
Model Interpretation with Explainable AI:
- Apply SHAP analysis to identify feature importance [6]
- Generate force plots for individual predictions
- Create summary plots to visualize global feature impacts
- Identify age-specific predictive factors for thyroid disorders in elderly
Validation and Performance Assessment:
- Evaluate models using accuracy, precision, recall, F1-score, and AUC-ROC
- Validate on external datasets or temporal validation splits
- Compare performance against clinical expert diagnoses
- Assess clinical utility through decision curve analysis
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Elderly Thyroid Studies
| Research Tool | Specification/Example | Application in Elderly Thyroid Research |
|---|---|---|
| Immunoassay System | Siemens ADVIA Centaur XP Immunoassay System [3] | Precise measurement of TSH, FT4, FT3, TPOAb, TgAb with quality control |
| Thyroid Hormone Panels | TSH, FT4, FT3, TT4, TT3 assays [3] | Comprehensive assessment of thyroid function status |
| Antibody Testing Kits | TPOAb, TgAb assays with established cut-offs [3] | Identification of autoimmune thyroiditis common in elderly |
| Sample Collection System | Greiner Bio-One vacuette blood collection tubes [3] | Standardized sample acquisition for reference interval studies |
| Quality Control Materials | BIO RAD lyphochek Immunoassay Plus Control [3] | Daily quality assurance for assay precision and accuracy |
| Data Mining Software | Python/R with scikit-learn, LightGBM, SHAP [6] | Development of predictive models for thyroid disorder diagnosis |
| Ultrasonography System | High-resolution thyroid ultrasound [4] | Structural assessment to exclude subjects with thyroid abnormalities |
Clinical Implications and Future Directions
The establishment of validated, age-specific reference intervals for thyroid function tests in elderly populations has profound implications for clinical practice and public health. With subclinical hypothyroidism affecting 3-16% of the elderly population and hyperthyroidism occurring in 0.5-4% [1], appropriate diagnostic criteria are essential for avoiding both overdiagnosis and underdiagnosis. The 2025 American Thyroid Association Guidelines for Differentiated Thyroid Cancer highlight the evolving landscape of thyroid management, though specific recommendations for elderly populations remain limited [8].
Future research directions should focus on:
- Developing cost-effective strategies for implementing age-specific reference intervals in clinical laboratories
- Validating machine learning algorithms for thyroid disorder prediction in diverse elderly populations
- Establishing trajectories of thyroid function change in the oldest-old (≥85 years)
- Investigating the impact of age-specific diagnostics on hard clinical outcomes
- Integrating functional medicine approaches with conventional diagnostics for comprehensive elderly thyroid care [1]
As the global population continues to age, the development and implementation of elderly-specific thyroid diagnostics will be crucial for optimizing care, reducing unnecessary treatments, and improving quality of life in this vulnerable population.
Thyroid hormone reference intervals (RIs) are fundamental for the accurate diagnosis and management of thyroid dysfunction. Current clinical practice largely relies on RIs derived from the general adult population, applying a "one-size-fits-all" approach irrespective of age [9]. However, compelling evidence from recent large-scale studies demonstrates that thyroid function undergoes significant changes throughout the lifespan [10] [9] [3]. Failing to account for these age-related shifts can lead to over-diagnosis of subclinical thyroid conditions, particularly in older adults, and potentially result in unnecessary lifelong treatment [10] [11]. This application note, situated within a broader thesis on data mining for thyroid hormone RIs in older adults, synthesizes documented quantitative changes in thyroid-stimulating hormone (TSH), free triiodothyronine (FT3), and free thyroxine (FT4) levels with age. It further provides detailed protocols for establishing age-specific RIs and visualizes the underlying physiological concepts and analytical workflows.
Documented Age-Related Changes in Thyroid Hormones
Extensive research, including large cross-sectional analyses and longitudinal studies, confirms that thyroid hormone levels are not static across adulthood. The table below summarizes the key quantitative changes in TSH, FT3, and FT4 with advancing age.
Table 1: Documented Age-Related Shifts in Thyroid Hormone Levels
| Hormone | Documented Change with Age | Key Quantitative Findings | Population & Study Details |
|---|---|---|---|
| TSH | Increases with age, particularly after 50 in women and 60 in men [10] [9] [12]. | - Upper normal limit (97.5th percentile) increases from 4.0 mIU/L at age 50 to 6.0 mIU/L at age 90 (a 50% increase) [10]. - Median TSH increases from 1.49 mIU/L to 1.81 mIU/L over 13 years in a longitudinal study (ΔTSH = +0.32 mIU/L) [12]. - RIs for elderly (≥65 yrs): 0.55-5.14 mIU/L [3]. | Analysis of >7.6 million TSH measurements; Dutch population [10]. Community-based longitudinal cohort [12]. Chinese population [3]. |
| FT4 | Remains relatively stable throughout adulthood [10] [9] [12]. | - No significant longitudinal change (16.6 pmol/L vs. 16.6 pmol/L over 13 years) [12]. - RIs for elderly (≥65 yrs): 12.00-19.87 pmol/L [3]. | Longitudinal cohort [12]. Chinese population [3]. |
| FT3 | Decreases with age [9] [1] [3]. | - RIs for elderly (≥65 yrs): 3.68-5.47 pmol/L [3]. - Strong negative linear correlation with phenotypic age, a measure of biological aging [13]. | Chinese population [3]. Analysis of NHANES data [13]. |
The following diagram illustrates the typical trajectory of these hormones across the human lifespan, based on the documented evidence.
Implications for Diagnosis and Clinical Practice
The established age-related shifts in thyroid hormones have profound implications for clinical practice and research, primarily concerning the diagnosis of subclinical hypothyroidism (SCH).
Table 2: Impact of Age-Specific Reference Intervals on Subclinical Hypothyroidism (SCH) Diagnosis
| Scenario | Diagnosis Rate Using Standard RIs | Diagnosis Rate Using Age-Specific RIs | Implication |
|---|---|---|---|
| Women aged 50-60 | 13.1% | 8.6% | ~34% relative reduction in SCH diagnosis [10]. |
| Women aged 90-100 | 22.7% | 8.1% | ~64% relative reduction in SCH diagnosis [10]. |
| Men aged 60-70 | 10.9% | 7.7% | ~29% relative reduction in SCH diagnosis [10]. |
| Men aged 90-100 | 27.4% | 9.6% | ~65% relative reduction in SCH diagnosis [10]. |
Adopting age-specific RIs can dramatically reduce the over-diagnosis of SCH in older adults, thereby preventing unnecessary levothyroxine treatment [10] [11]. Evidence suggests that treating mild SCH (TSH < 7.0 mIU/L) in older individuals does not confer benefits for cardiovascular health or cognitive function and may pose risks, including overtreatment [14] [11]. Furthermore, a J-shaped association has been observed between TSH and frailty in older adults, with levels in the upper half of the standard reference range (2.7–4.8 mIU/L) associated with a significantly higher risk of frailty [15].
Experimental Protocols for Establishing Age-Specific RIs
Protocol: RI Derivation from Large Laboratory Datasets Using Data Mining Algorithms
This protocol details the methodology for establishing age-specific RIs from large-scale laboratory data, a approach validated in recent research [16] [3].
1. Sample Collection & Pre-processing:
- Source: Extract retrospective thyroid hormone test results (TSH, FT4, FT3) from Laboratory Information Systems (LIS), alongside patient age and sex [10] [3].
- Inclusion Criteria: Ambulatory/community-dwelling individuals undergoing routine health check-ups are preferred to better represent the "healthy" state [16] [3].
- Exclusion Criteria: Apply robust data filtering to remove:
- Records with missing critical data (age, sex, key hormone values) [3].
- Known thyroid disease, pregnancy, or non-thyroidal illness [3].
- Positive thyroid peroxidase (TPOAb) or thyroglobulin (TgAb) antibodies to exclude underlying autoimmune thyroiditis [3].
- Outliers using statistical methods (e.g., Tukey's method) [3].
- Pre-analytical Standardization: Ensure standardized sample collection (e.g., morning fasting blood draws), handling, and calibration of immunoassay systems (e.g., Siemens ADVIA Centaur, Roche Cobas) to minimize technical variability [3].
2. Data Analysis & Algorithm Selection:
- Partition Data: Stratify the cleaned dataset into age and sex cohorts (e.g., 18-29, 30-39, ..., ≥65 years) [10] [3].
- Algorithm Application: Apply multiple data mining algorithms to establish RIs (2.5th - 97.5th percentiles) for each cohort. Recommended algorithms include:
- For physical examination/health check-up data: Transformed Hoffmann, Transformed Bhattacharyya, Kosmic, and refineR algorithms have shown good performance and consistency [16].
- For outpatient/patient data: The Expectation Maximization (EM) algorithm, particularly when combined with a Box-Cox transformation for skewed data, is recommended [16].
- Validation: Compare the algorithm-derived RIs with those obtained from a rigorously selected sub-cohort of "healthy" older adults to assess accuracy [16].
The workflow for this protocol is summarized in the following diagram.
Protocol: Longitudinal Assessment of Thyroid Function in Aging Cohorts
This protocol is designed to track intra-individual changes in thyroid function over time, providing critical insight into the aging process itself.
1. Cohort Setup & Baseline Assessment:
- Cohort: Enlist a large, community-based cohort of adults with a broad age range at baseline [12].
- Baseline Measurement: Collect initial serum samples for TSH, FT4, FT3, TPOAb, and TgAb. Record comprehensive participant data, including demographics, health status, and lifestyle factors [12].
2. Follow-up & Longitudinal Analysis:
- Time Interval: Conduct follow-up assessments after a substantial period (e.g., 10+ years) using the same laboratory methods to ensure comparability [12].
- Statistical Analysis:
- Perform paired analyses (e.g., paired t-tests) to assess mean changes in hormone levels within individuals over time [12].
- Use multivariate regression models to analyze the relationship between the change in TSH (ΔTSH) and baseline age, gender, and baseline TSH levels [12].
- This approach can reveal patterns such as a more pronounced TSH increase in older individuals and those with lower baseline TSH, suggesting an age-related alteration in set-point rather than occult disease [12].
Table 3: Key Research Reagent Solutions for Thyroid Aging Studies
| Category / Item | Function / Application | Examples / Notes |
|---|---|---|
| Immunoassay Systems | Automated measurement of serum TSH, FT4, FT3, TPOAb, and TgAb levels. | Siemens ADVIA Centaur XP [3], Abbott ARCHITECT [9], Roche Cobas e601 [9]. |
| Quality Control Materials | Ensuring precision and accuracy of hormone measurements through internal quality control. | BIO RAD Lyphochek Immunoassay Plus Control [3]. |
| Reference Materials | Participating in external quality assessment (EQA) schemes to ensure inter-laboratory comparability. | National Center for Clinical Laboratories (NCCL) programs [3]. |
| Data Mining Algorithms | Establishing reference intervals from large, complex laboratory datasets. | refineR, Kosmic, Transformed Hoffmann/Bhattacharyya, Expectation Maximization (EM) [16]. |
| Specialized Functional Panels | Comprehensive assessment of interconnected systems influencing thyroid health. | Adrenal Function Profile (e.g., Doctor's Data), Comprehensive Gut Health Map (e.g., GI-MAP by Diagnostic Solutions) [1]. |
Visualizing the Thyroid-Aging Physiological Framework
The complex interplay of hormonal changes and their functional consequences can be conceptualized within the following framework.
The diagnosis of subclinical hypothyroidism (SCH) hinges on biochemical markers, specifically an elevated thyroid-stimulating hormone (TSH) level with normal free thyroxine (FT4) concentrations. However, the reliance on a "one-size-fits-all" reference interval (RI) for TSH, without accounting for demographic variables like age, leads to significant overdiagnosis and potential overtreatment, particularly in older adult populations. Research confirms that TSH levels naturally increase with age, a physiological adaptation rather than a pathological state [17] [18]. Using the standard RI for all adults misclassifies a substantial number of euthyroid older adults as having SCH, triggering unnecessary clinical investigations, patient anxiety, and inappropriate initiation of levothyroxine therapy [19] [20]. This application note details the clinical impact of this discrepancy and provides protocols for establishing age-specific RIs using robust data mining approaches, framing the discussion within a broader thesis on improving thyroid hormone diagnostics for older adults.
Quantitative Data: Prevalence and Reclassification
The following tables summarize key quantitative findings from recent studies, illustrating the scale of misdiagnosis and the specific age-adjusted RIs required for accurate diagnosis.
Table 1: Impact of Age-Specific TSH Reference Intervals on SCH Prevalence
| Study Population | SCH Prevalence (Standard RI) | SCH Prevalence (Age-Specific RI) | Relative Reduction |
|---|---|---|---|
| Chinese cohort (≥65 years) [19] | 10.28% | 3.74% | 63.6% |
| NHANES-based analysis [20] | 5.9% (≥70 years) | Not specified | 48.5% reclassified as normal |
| Chinese multicenter data [20] | Not specified | Not specified | 73.5% reclassified as normal |
Table 2: Established Age-Specific TSH Reference Intervals (RIs)
| Age Group | Established TSH Reference Interval (mIU/L) | Source |
|---|---|---|
| 65-70 years | 0.65 – 5.51 | [19] |
| 71-80 years | 0.85 – 5.89 | [19] |
| >80 years | 0.78 – 6.70 | [19] |
| Pragmatic Clinical Guide (e.g., for a 70-year-old) | ≤7.0 | [18] |
Experimental Protocols for Establishing Age-Specific RIs
Protocol 1: Cohort Study for RI Establishment and Outcome Assessment
This protocol, adapted from a multicenter prospective study, is designed to prospectively observe elderly SCH patients and establish age-specific RIs [17].
1. Study Population & Ethical Approval:
- Participants: Recruit patients aged ≥60 years diagnosed with SCH (TSH <10 mIU/L and normal FT4). A key step is defining the reference population based on the National Academy of Clinical Biochemistry (NACB) guidelines: euthyroid individuals negative for thyroid autoantibodies, without personal or family history of thyroid disease, and with normal thyroid ultrasound [19].
- Ethics: Obtain approval from the institutional ethics committee (e.g., Medical Science Research Ethics Committee). Acquire informed consent from all participants [17].
2. Data and Sample Collection:
- Clinical Data: Register baseline demographics and medical history.
- Questionnaires: Administer standardized scales including the Montreal Cognitive Assessment (MoCA-B), Hamilton Depression Scale (HAMD), and fatigue scales.
- Laboratory Tests: Perform thyroid function tests (TSH, FT4, FT3), thyroid autoantibodies (TPOAb, TgAb), blood lipid analysis, and other relevant biochemistry.
- Imaging: Conduct thyroid ultrasound examinations [17].
3. Data Analysis and RI Calculation:
- Stratification: Stratify the reference population into age groups (e.g., 65-70, 71-80, >80 years).
- Statistical Determination: Calculate the 2.5th and 97.5th percentiles for TSH and FT4 within each age stratum to establish the age-specific RIs [19].
- Outcome Monitoring: For longitudinal cohorts, define endpoint events (e.g., TSH ≥10 mIU/L or decline in FT4 for 60-80-year-olds; decrease in FT4 for >80-year-olds) and monitor patients at regular intervals [17].
4. Socio-Economic Analysis: Compare medical costs associated with follow-up using general versus age-specific TSH RIs to quantify the economic impact of reclassification [17].
Protocol 2: Data Mining Algorithms for RI Derivation from Big Data
This protocol validates the use of clinical laboratory "big data" and advanced data mining algorithms to establish RIs, bypassing the need for costly and logistically challenging direct recruitment of healthy volunteers [21] [22].
1. Database Establishment:
- Source Data: Extract laboratory test results for thyroid hormones (TSH, FT4, FT3) and other biochemical parameters from the Laboratory Information System (LIS). Data can be sourced from both general physical examination populations and outpatient populations.
- Derived Databases: Create two datasets for validation:
- Derived Database*: A "standard" dataset with reference individuals selected via strict, traditional exclusion criteria (e.g., no known thyroid disease, normal ultrasound, negative antibodies).
- Derived Database#: A "patient big data" dataset, which is the physical examination population downloaded directly from the LIS without stringent pre-screening [22].
2. Data Preprocessing and Cleaning:
3. Application of Data Mining Algorithms:
4. Model Validation and Performance Assessment:
- Consistency Check: Use the comparative confidence interval (CI) method to check if the limits of the RIs derived from the patient big data (RIs#) fall within the 90% CI of the standard RIs (RIs*).
- Decision Consistency: Apply the new RIs to an external database and calculate the consistency rate of classification decisions compared to the standard RIs. Rates >98% indicate successful validation [22].
- Machine Learning Evaluation: When using ML for prediction, evaluate models using Area Under the Curve (AUC), sensitivity, specificity, and accuracy [23] [24].
The workflow for this data mining approach is illustrated below.
<75 chars: Data Mining RI Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Assays for Thyroid Hormone RI Research
| Item | Function/Application | Key Notes |
|---|---|---|
| Electrochemiluminescence Immunoassay (ECLIA) | Primary method for quantifying TSH, FT4, FT3, TRAb, TgAb, and TPOAb. | Used with commercial kits (e.g., Roche Diagnostics) for high-sensitivity measurement [23] [25]. |
| Thyroid Autoantibody Assays | Identify autoimmune thyroiditis (Hashimoto's), a key exclusion criterion for reference populations and a predictor of SCH progression. | Includes TPOAb and TgAb. TPOAb positivity is a significant risk factor for progression [17] [23]. |
| Direct Chemiluminescence Assays | Alternative platform for thyroid function test measurement. | Used in various clinical settings with specific commercial kits (e.g., Siemens Healthcare) [25]. |
| Biochemistry Profile Panels | For assessing secondary effects of SCH (e.g., dyslipidemia) and as inputs for machine learning models. | Key parameters: Total Cholesterol, LDL-C, Triglycerides, Creatinine, Uric Acid, Liver Enzymes (AST, ALT, γGTP) [23] [19] [24]. |
| Ultrasound Imaging System | To confirm the absence of structural thyroid disease in reference populations and to assess thyroid volume. | A necessary tool for applying NACB criteria to reference individuals [23] [19]. |
The evidence is clear that implementing age-specific RIs for thyroid hormones, particularly TSH, is critical for the accurate diagnosis of SCH in older adults. The use of inappropriate, non-stratified RIs results in substantial overdiagnosis, affecting up to 73.5% of those labeled with SCH in some populations [20]. This misclassification has direct consequences for clinical trial enrollment, drug development targeting true thyroid dysfunction, and the safety of older adults who may be exposed to unnecessary thyroid hormone therapy.
The methodologies outlined here, from prospective cohort studies to advanced data mining of laboratory big data, provide a robust pathway for refining RIs. For researchers and drug development professionals, adopting these approaches is essential for ensuring that clinical studies and subsequent diagnostic criteria are based on a physiologically accurate understanding of thyroid function across the human lifespan. Future efforts should focus on the widespread adoption of these protocols to generate locally relevant RIs and their integration into routine clinical laboratory reporting and international guidelines.
Application Note: The Imperative for Stratified Thyroid Hormone Reference Intervals in Older Adults
Thyroid dysfunction prevalence increases significantly with age, becoming a major public health concern in older adult populations. Current clinical practice often employs a "one-size-fits-all" approach to thyroid function test reference intervals (RIs). However, emerging evidence demonstrates that thyroid function varies substantially based on demographic factors including sex, ethnicity, and age. This application note details the critical need for stratified RIs in both research and clinical practice for older adults, highlighting how failure to account for these factors leads to significant misclassification of thyroid disease states. Implementing stratified RIs will improve diagnostic accuracy, enhance research validity, and optimize treatment decisions for the growing aging population.
Quantitative Evidence for Stratification
Analysis of large-scale population studies provides compelling evidence for implementing stratified RIs. The table below summarizes key findings from recent investigations examining how thyroid function parameters vary across demographic subgroups.
Table 1: Thyroid Hormone Variations by Demographic Factors in Adult Populations
| Demographic Factor | Impact on Thyroid Parameters | Magnitude of Effect | Study Details |
|---|---|---|---|
| Advancing Age | TSH 97.5th percentile increases with age [26] [27]. | Prevalence of subclinical hypothyroidism increased from 2.4% (ages 20-29) to 5.9% (age ≥70) using fixed RIs [26]. | Analysis of 8,308 NHANES participants [26]. |
| Total T3 (TT3) levels decline with age [26] [27]. | Not quantified in results. | ||
| Sex | Women have higher TT4 levels than men [26] [28]. | TSH, ATG, and ATPO were significantly higher in women; TT3 was higher in men (p<0.05) [28]. | Study of 3,123 individuals in Lanzhou, China [28]. |
| TSH, antithyroglobulin (ATG), and anti-thyroid peroxidase (ATPO) antibodies are higher in women [28]. | The 97.5th centile for TSH in Whites and Mexican Americans was ~1.0 mIU/L higher when anti-thyroid antibodies were not excluded [29]. | NHANES III analysis of disease-free vs. reference populations [29]. | |
| Race/Ethnicity | White participants have higher TSH levels compared to other racial groups [26] [27]. | TSH distribution and reference limits were lower in Blacks than in Whites or Mexican Americans [29]. | NHANES III analysis of Whites, Blacks, and Mexican Americans [29]. |
| Autoimmune Status | Presence of anti-thyroid antibodies elevates the upper TSH reference limit [29]. | 48.5% of persons with subclinical hypothyroidism and 31.2% with subclinical hyperthyroidism were reclassified as normal [26] [27]. | Cross-sectional analysis of 8,308 NHANES participants [26]. |
Clinical and Research Impact
The use of fixed, non-stratified RIs has profound implications for disease diagnosis and management in older adults. When age-, sex-, and race-specific RIs were applied to a large U.S. cohort, a substantial proportion of patients were reclassified, profoundly impacting perceived disease prevalence and subsequent management decisions [26] [27]. This is particularly critical in older adults, where the symptoms of thyroid dysfunction are often atypical and can be mistaken for normal aging or other common geriatric conditions [30] [31]. For instance, hyperthyroidism may present merely as atrial fibrillation or unexplained weight loss, while hypothyroidism might be misattributed to natural declines in cognitive function or physical energy [30]. Furthermore, the relationship between thyroid function and mortality risk exhibits significant sex differences in the elderly; one study found that each 1-mU/L higher TSH within the normal range was associated with a decreased mortality risk in men (HR 0.83) but not in women [32]. These findings underscore that applying inappropriate RIs can lead to both overdiagnosis and underdiagnosis, with direct consequences for patient outcomes and health resource utilization.
Protocol: Establishing Stratified Reference Intervals for Thyroid Hormones in Older Adults
Scope and Application
This protocol outlines a standardized procedure for developing age-, sex-, and ethnicity-specific reference intervals (RIs) for thyroid-stimulating hormone (TSH), free thyroxine (FT4), free triiodothyronine (FT3), total thyroxine (TT4), and total triiodothyronine (TT3) in older adult populations (≥65 years). It is designed for use by clinical researchers, laboratory scientists, and public health professionals seeking to establish population-specific RIs that improve the accuracy of thyroid disorder diagnosis in aging populations.
Pre-Analytical Phase: Participant Selection and Criteria
A critical first step involves defining a rigorously characterized reference population.
2.2.1 Inclusion Criteria:
- Community-dwelling adults aged ≥65 years, stratified into age decades (e.g., 65-74, 75-84, ≥85).
- Self-reported perception of good health [28].
- Residence in an area with well-characterized iodine status (e.g., iodine-adequate) [28].
2.2.2 Exclusion Criteria: The following conditions and factors mandate exclusion from the reference population:
- Personal history of thyroid disease, goiter, thyroid surgery, or thyroid irradiation [28] [29] [33].
- Family history of thyroid disease in first-degree relatives [28] [30].
- Abnormal thyroid ultrasonography findings [28].
- Presence of anti-thyroid peroxidase (ATPO) or anti-thyroglobulin (ATG) antibodies above the established cut-off [28] [29].
- Use of medications known to affect thyroid function (e.g., levothyroxine, antithyroid drugs, amiodarone, lithium, glucocorticoids, phenytoin, estrogens) [28] [31] [33].
- Presence of conditions associated with non-thyroidal illness (acute or chronic), pregnancy, type 2 diabetes mellitus, uncontrolled hypertension, hepatitis, or other significant chronic diseases [28] [31].
- Abnormal serum levels of TSH (e.g., >10 mIU/L or <0.1 mIU/L with normal T4) or values that are outliers based on statistical methods [29] [33].
The workflow for defining the final reference population is summarized in the diagram below.
Analytical Phase: Laboratory Procedures and Data Collection
2.3.1 Specimen Collection and Handling:
- Blood samples should be collected in the morning (e.g., 6:00-9:00 AM) after an 8-12 hour fast [28].
- Serum should be separated by centrifugation and analyzed within a specified timeframe (e.g., within 6 hours) to ensure stability of analytes [28].
2.3.2 Laboratory Analysis:
- Thyroid hormones (TSH, FT4, FT3, TT4, TT3) and anti-thyroid antibodies (ATPO, ATG) must be measured using standardized, high-quality platforms, such as chemiluminescent microparticle immunoassays (e.g., Abbott Architect, Siemens ADVIA Centaur) [28] [33].
- The specific analyzer and reagent kit lot numbers must be documented, as RIs are method-dependent [28] [33].
- Daily quality control procedures using two reference standards must be performed before sample testing to ensure analytical precision and accuracy [28].
Post-Analytical Phase: Statistical Analysis and RI Establishment
2.4.1 Data Distribution Assessment:
- Test all thyroid parameters for normality using statistical tests (e.g., Kolmogorov-Smirnov test) [28] [33].
- Log-transform non-normally distributed data (e.g., TSH) for analysis if necessary [29].
2.4.2 Establishing Reference Limits:
- Calculate the 2.5th and 97.5th percentiles as the lower and upper reference limits, respectively, to define the central 95% interval [28] [26].
- Use non-parametric methods if data is not normally distributed, even after transformation.
- Employ quantile regression analysis to model the effect of covariates like age, sex, and race on the 2.5th, 50th (median), and 97.5th percentiles of the TSH distribution [29]. This allows for the development of equations to predict subpopulation-specific limits.
2.4.3 Stratification and Reporting:
- Establish and report separate RIs for key strata: sex (male, female), age groups (e.g., 65-74, 75-84, ≥85), and major racial/ethnic groups (e.g., non-Hispanic White, non-Hispanic Black, Mexican American, Asian) [29] [26].
- Compare the established RIs with manufacturer-provided intervals to quantify potential misclassification rates [28] [33].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Thyroid Hormone Reference Interval Studies
| Item | Specification/Function | Representative Example/Note |
|---|---|---|
| Immunoassay Analyzer | Automated platform for precise measurement of thyroid hormones and antibodies. | Abbott Architect i2000 [28]; Siemens ADVIA Centaur XP [33]. |
| Reagent Kits | Assay-specific kits for quantifying TSH, FT4, FT3, TT4, TT3, ATPO, and ATG. | Lot numbers must be documented as RIs are method-dependent [28] [33]. |
| Quality Control Materials | Used to verify assay precision and accuracy before sample testing. | Two levels of qualified control sera run daily [28]. |
| Data Analysis Software | Software for statistical analysis, including normality testing and percentile calculation. | SPSS, R, or STATA with quantile regression capabilities [28] [29]. |
| Ethics Approval Documentation | Institutional Review Board (IRB) approval ensuring the study conforms to ethical standards. | Required before participant recruitment (e.g., protocol: 2022-359) [28]. |
| Informed Consent Forms | Documents obtained from all participants after explaining the study's purpose. | Mandatory for ethical research involving human subjects [28] [33]. |
The establishment of age-, sex-, and ethnicity-specific reference intervals for thyroid hormones is no longer a theoretical concept but a practical necessity for accurate diagnosis and effective management of thyroid disorders in older adults. The protocols and data summarized in this document provide a clear roadmap for researchers and clinicians to move beyond a one-size-fits-all model. Adopting this stratified approach will minimize misdiagnosis, refine clinical decision-making, and ultimately improve health outcomes for our rapidly aging global population. Future research should focus on validating these approaches in diverse ethnic groups and establishing the long-term clinical benefits of using stratified RIs in geriatric care.
From Data to Diagnostics: A Practical Guide to Data Mining Algorithms for RI Establishment
Application Notes
The Role of LIS and EHR in Establishing Reference Intervals
Laboratory Information Systems (LIS) and Electronic Health Records (EHR) provide vast repositories of real-world data that are invaluable for establishing age-specific reference intervals (RIs) for thyroid hormones. The integration of these systems enables researchers to access large-scale demographic, clinical, and laboratory data necessary for robust statistical analysis. For older adults, this is particularly crucial as thyroid function changes with aging, and traditional RIs derived from younger populations may not be clinically appropriate [34]. The use of LIS/EHR data allows for the development of RIs that better reflect the physiological changes in thyroid function observed in the elderly population.
Data Mining Algorithms for RI Establishment
Several data mining algorithms have been validated for establishing RIs from LIS and EHR data. A 2022 study comparing five different algorithms found that consistency across algorithms was greater in physical examination data compared to outpatient data [21]. The transformed Hoffmann, transformed Bhattacahrya, kosmic, and refineR algorithms demonstrated particularly good performance in calculating RIs from physical examination data. For patient data with obvious skewness, the Expectation Maximization (EM) algorithm combined with Box-Cox transformation is recommended [21].
Special Considerations for Older Adult Populations
When establishing thyroid hormone RIs for older adults using LIS/EHR data, several physiological factors must be considered. Thyrotropin (TSH) levels tend to increase with age, particularly in women, with the upper limit of the serum TSH RI increasing by approximately 0.3 mIU/L for every 10-year increase in age after 40 [34]. This age-related change necessitates specialized RIs for the elderly population, as demonstrated by a recent Australian study of healthy adults aged ≥70 years which proposed a TSH RI of 0.34–3.75 mU/L [35].
Experimental Protocols
Protocol 1: Establishing TSH Reference Intervals from LIS/EHR Data
Data Extraction and Preprocessing
- Data Source Identification: Extract thyroid function test results (TSH, FT4, FT3) from the LIS, linked with demographic data (age, sex) from EHRs for patients aged ≥65 years.
- Exclusion Criteria Application:
- Exclude patients with diagnosed thyroid disorders (hypothyroidism, hyperthyroidism, thyroid cancer)
- Exclude patients taking thyroid-related medications (levothyroxine, antithyroid drugs)
- Exclude individuals with positive thyroid antibodies (TPOAb, TgAb) if available
- Exclude patients with severe non-thyroidal illness, dementia, or life-threatening conditions [35]
- Exclude samples with hemolysis, lipemia, or icterus that may interfere with assays
- Data Cleaning: Remove statistical outliers using the Tukey method (values outside 1.5 × interquartile range).
Statistical Analysis and RI Calculation
- Data Partitioning: Stratify data by age groups (65-70, 71-75, 76-80, 81-85, >85 years) and sex.
- Normality Assessment: Test data distribution using Shapiro-Wilk test and visual inspection of Q-Q plots.
- Algorithm Application: Apply multiple data mining algorithms to establish RIs:
- refineR Algorithm: Implement using the refineR package in R with default parameters
- Kosmic Algorithm: Apply with Box-Cox transformation for normalization
- Transformed Hoffmann Method: Utilize the Hoffmann approach with appropriate data transformation
- Expectation Maximization (EM): Use for datasets with obvious skewness [21]
- RI Determination: Calculate the middle 95th percentile (2.5th to 97.5th percentile) of the normalized data for each algorithm.
- Method Comparison: Use bias ratio (BR) matrix to compare limits of RIs established using different algorithms [21].
- Validation: Validate proposed RIs by assessing disease incidence over time using Cox proportional hazard regression models [35].
Protocol 2: Validation of Established Reference Intervals
Longitudinal Validation
- Cohort Identification: Identify a validation cohort from EHR data meeting the same inclusion/exclusion criteria as the derivation cohort.
- Follow-up Period: Track thyroid-related clinical outcomes over a defined period (minimum 5 years recommended).
- Outcome Assessment: Monitor for development of overt thyroid dysfunction, cardiovascular events, and mortality.
- Statistical Analysis: Use Cox proportional hazard models to assess association between baseline TSH levels and subsequent clinical outcomes [35].
Algorithm Performance Comparison
- Reference Standard Comparison: Compare algorithm-derived RIs with those established using healthy older adults recruited through strict criteria [21].
- Bias Assessment: Calculate bias between different methods using standardized approaches.
- Clinical Correlation: Assess correlation between algorithm-derived RIs and clinical outcomes.
Data Presentation
Established TSH Reference Intervals for Older Adults
Table 1: TSH Reference Intervals for Older Adults from Recent Studies
| Population | Age Range | TSH Reference Interval (mU/L) | Data Source | Establishment Method | Study/Reference |
|---|---|---|---|---|---|
| Australian Healthy Elderly | ≥70 years | 0.34 - 3.75 | ASPREE Trial | Logarithmic transformation, middle 95th percentile | [35] |
| German Population | 60-79 years | 0.25 - 2.12 | Epidemiologic Survey | Direct sampling, median (IQR) presented | [34] |
| Australian Population | ≥60 years | 0.47 - 6.25 (females, 60-69) 0.51 - 5.33 (males, ≥70) | Epidemiologic Survey | Population sampling | [34] |
| Japanese Outpatients | ≥70 years | 0.75 - 5.37 | Outpatient Data | Immunoassay, direct sampling | [34] |
Performance Comparison of Data Mining Algorithms
Table 2: Comparison of Data Mining Algorithms for Establishing Thyroid Hormone RIs from LIS/EHR Data
| Algorithm | Data Type | Performance | Recommended Use | Key Reference |
|---|---|---|---|---|
| Transformed Hoffmann | Physical Examination Data | Good | Primary algorithm for physical examination data | [21] |
| Transformed Bhattacahrya | Physical Examination Data | Good | Secondary algorithm for verification | [21] |
| Kosmic | Physical Examination Data | Good | Primary algorithm for normal distributions | [21] |
| refineR | Physical Examination Data | Good | Alternative primary algorithm | [21] |
| Expectation Maximization (EM) | Patient Data | High consistency with healthy older adult RIs | Skewed data distributions | [21] |
Visualizations
Workflow for RI Establishment from LIS/EHR
Algorithm Selection Decision Tree
The Scientist's Toolkit
Research Reagent Solutions
Table 3: Essential Reagents and Materials for Thyroid Hormone RI Research
| Item | Function/Application | Specifications/Examples |
|---|---|---|
| Commercial Immunoassay Kits | Measurement of thyroid hormones | Chemiluminescence microparticle immunoassays (e.g., Abbott Architect) [35] |
| Thyroid Antibody Assays | Exclusion of autoimmune thyroid disease | TPOAb, TgAb immunoassays [34] |
| Statistical Software | Data analysis and RI calculation | R with refineR, Kosmic packages; Python with scipy, statsmodels [21] |
| Data Mining Algorithms | RI establishment from real-world data | Transformed Hoffmann, Bhattacahrya, Kosmic, refineR, EM [21] |
| Laboratory Information System | Source of laboratory test data | LIS with export capabilities for thyroid function tests |
| Electronic Health Record System | Source of clinical and demographic data | EHR with research data export functionality |
| Quality Control Materials | Assay performance verification | Commercial QC sera for thyroid function tests |
| Data Anonymization Tools | Patient privacy protection | De-identification software for research data extraction |
The establishment of accurate reference intervals (RIs) is a cornerstone of clinical diagnostics, providing essential benchmarks for the interpretation of laboratory test results. For thyroid hormones in older adults, this is particularly crucial given the profound physiological changes that occur with aging and the high prevalence of thyroid dysfunction in this demographic. Traditional direct methods for establishing RIs require costly and time-consuming recruitment of carefully selected healthy individuals, often making them impractical for many clinical settings [36]. Consequently, indirect data mining approaches utilizing real-world data from laboratory information systems have emerged as a viable and efficient alternative [37].
These indirect methods leverage sophisticated algorithms to separate the underlying distribution of healthy individuals from mixed datasets that include both pathological and non-pathological results. Among the most prominent algorithms employed for this purpose are the Hoffmann, Bhattacharya, and Expectation-Maximization (EM) methods. Each algorithm operates on distinct principles and demonstrates unique strengths and limitations when applied to thyroid hormone data in older populations [16] [21]. This article provides a comprehensive examination of these three algorithms, detailing their theoretical foundations, implementation protocols, and performance characteristics specifically within the context of geriatric thyroid hormone research.
Theoretical Foundations of the Algorithms
Hoffmann Algorithm
The Hoffmann algorithm is a graphical separation method based on the fundamental assumption that within a mixed population dataset, healthy individuals constitute the majority and their test results follow a Gaussian or near-Gaussian distribution. The algorithm operates by constructing a cumulative frequency distribution of the test values and leveraging the statistical properties of a normal distribution to isolate the healthy component [36] [16].
The core principle involves plotting the cumulative frequency of data points against their values. For a Gaussian distribution, this plot produces a characteristic sigmoidal curve. The Hoffmann method then identifies the linear portion of this curve after proportional frequency transformation, which corresponds to the central, healthy population. The slope and intercept of this linear segment are used to calculate the mean and standard deviation of the reference population, from which the reference intervals (typically the 2.5th and 97.5th percentiles) are derived [16]. Its relative simplicity and intuitive graphical output have made it a historically popular choice, though it may struggle with significantly skewed distributions without appropriate data transformation.
Bhattacharya Algorithm
The Bhattacharya method is another graphical separation technique designed to disentangle a Gaussian distribution of healthy individuals from a larger mixed dataset. Unlike Hoffmann, it uses a different transformational approach to achieve linearization of the healthy population's distribution [16] [37].
The algorithm begins by generating a frequency histogram of the test values. It then calculates the natural logarithms of the ratios between successive frequencies in the histogram bins. For a pure normal distribution, plotting these logarithmic differences against the bin values produces a straight line. The presence of a linear segment in the transformed plot indicates the portion of the data representing the healthy population. The parameters of this line (slope and intercept) provide estimates of the mean and standard deviation of the reference distribution. The Bhattacharya method shares the Hoffmann's limitations with strongly non-Gaussian data but has been widely adopted in laboratory medicine due to its computational efficiency and generally reliable performance with physical examination data [16].
Expectation-Maximization (EM) Algorithm
The Expectation-Maximization algorithm is a general-purpose iterative algorithm for finding maximum likelihood estimates of parameters in statistical models, especially when dealing with incomplete data or latent variables [38]. In the context of establishing RIs, the "latent variable" is the unknown health status of each individual contributing a data point.
The EM algorithm operates through two repeating steps in each iteration. The Expectation (E) step calculates the probability that each data point belongs to the healthy population (rather than a pathological population) based on the current parameter estimates. The Maximization (M) step then updates the estimates of the mean and standard deviation of the healthy population using the probabilities calculated in the E-step as weights [38] [39]. This iterative process continues until the parameter estimates converge, meaning they show minimal change between iterations. A significant advantage of the EM algorithm is its ability to model complex, skewed distributions often encountered in clinical data, particularly when combined with data transformation techniques like Box-Cox transformation [16] [21].
Table 1: Core Principles and Characteristics of the Data Mining Algorithms
| Algorithm | Theoretical Basis | Primary Mechanism | Key Assumptions |
|---|---|---|---|
| Hoffmann | Graphical Method | Cumulative frequency distribution and linearization | Healthy population is the majority and follows a Gaussian distribution |
| Bhattacharya | Graphical Method | Logarithmic transformation of frequency ratios | Underlying healthy population distribution is Gaussian or transformable to Gaussian |
| Expectation-Maximization (EM) | Statistical Iteration | E-step and M-step iteration for maximum likelihood estimation | Model specification is correct; data can be from a mixture of distributions |
Application to Thyroid Hormone Reference Intervals in Older Adults
Performance Comparison in Geriatric Populations
Research specifically validating these algorithms for thyroid hormones in older adults has yielded critical insights into their relative performance. A 2022 study established RIs for thyroid-stimulating hormone (TSH), free thyroxine (FT4), free triiodothyronine (FT3), total thyroxine (TT4), and total triiodothyronine (TT3) using the five data mining algorithms applied to both physical examination data and outpatient data from older adults [16] [21].
The findings revealed that the consistency between different algorithms was significantly higher when using physical examination data compared to general outpatient data. This is likely because physical examination populations represent a healthier cohort with a lower prevalence of pathological conditions that can distort thyroid hormone levels. For physical examination data, the transformed Hoffmann, transformed Bhattacharya, kosmic, and refineR algorithms all demonstrated good performance in calculating RIs for thyroid hormones. However, the EM algorithm exhibited a unique strength when applied to the more heterogeneous outpatient data, particularly for handling TSH, which often displays a skewed distribution. The RIs for TSH established using the EM algorithm on patient data showed high consistency with RIs established from rigorously selected healthy older adults [16] [21].
Impact of Data Distribution and Transformation
The shape of the data distribution is a critical factor in algorithm selection. Thyroid hormone data, especially TSH, is often right-skewed and not natively Gaussian [36]. The graphical methods (Hoffmann and Bhattacharya) generally perform well for data that is Gaussian or near-Gaussian. For handling skewed data, these algorithms are often used in their "transformed" versions, where a Box-Cox transformation is applied to the data prior to processing to make its distribution more symmetric [16].
The EM algorithm, especially when combined with Box-Cox transformation, is particularly adept at handling data with significant skewness. This makes it a valuable tool for analyzing TSH levels in older adults. A 2023 study confirmed that while the EM algorithm performed excellently on skewed TSH data, its performance was more limited for other, less skewed thyroid hormones like FT4 and FT3 [36]. Therefore, the choice of algorithm should be guided by the distribution characteristics of the specific analyte.
Table 2: Algorithm Performance for Thyroid Hormone RIs in Older Adults (Based on [16] [21])
| Algorithm | Recommended Data Source | Performance on TSH (Skewed) | Performance on FT4/FT3 (Near-Gaussian) |
|---|---|---|---|
| Hoffmann (Transformed) | Physical Examination | Good with transformation | Very Good |
| Bhattacharya (Transformed) | Physical Examination | Good with transformation | Very Good |
| EM (with Box-Cox) | Outpatient/Patient Data | Excellent | Limited / Variable |
| kosmic | Physical Examination | Good | Very Good |
| refineR | Physical Examination | Good | Very Good |
Experimental Protocols for Reference Interval Establishment
Data Collection and Preprocessing Protocol
Materials and Reagents:
- Source Data: Laboratory Information System (LIS) data from a physical examination center or outpatient clinics [36] [16].
- Analytical Platform: Automated immunoassay analyzer (e.g., Siemens ADVIA Centaur XP, Mindray CL-6000i) [36] [40].
- Assay Kits: Manufacturer-provided reagents and calibrators for thyroid hormones (TSH, FT4, FT3, TT4, TT3) [36] [37].
- Sample Tubes: Vacuum blood collection tubes with procoagulant (e.g., Vacuette, Greiner Bio-One) [36] [37].
- Software: Statistical computing environment (R recommended, version 4.0.5 or later) with necessary packages (
refineR,forecastfor Box-Cox) [36].
Procedure:
- Data Extraction: Export all laboratory test results for the target thyroid hormones (TSH, FT3, FT4, TT3, TT4) over a defined period (e.g., 2014-2018), along with necessary demographic variables (sex, age) [36].
- Data Cleaning:
- Remove entries with missing values for the analytes of interest, sex, or age [37].
- If multiple results exist per individual, retain the first or last result based on study design to ensure independence [37].
- Exclude individuals outside the target age range (e.g., for older adults, define as ≥60 or ≥65 years) [16].
- Stratification: Partition the data into subgroups based on sex and age groups (e.g., 60-69, 70-79, ≥80 years) to account for biological variation [16] [40].
- Outlier Removal: Apply the Tukey method to identify and remove outliers within each subgroup. This involves calculating the first (Q1) and third (Q3) quartiles and defining fences as Q1 - 1.5×IQR and Q3 + 1.5×IQR (IQR = Q3 - Q1). Data points outside these fences are considered outliers [36] [37].
- Data Transformation (If Applicable): For algorithms requiring Gaussian-like data, apply a Box-Cox transformation to each subgroup's data to reduce skewness [36] [16].
Protocol for Implementing the Hoffmann Algorithm
- Input Preprocessed Data: Use the cleaned, stratified, and potentially transformed data from the previous protocol.
- Cumulative Frequency Calculation: For each subgroup, sort the data and calculate the cumulative frequency percentage for each data point.
- Linearization and Identification:
- Plot the cumulative frequency percentage against the test values.
- Identify the central, linear portion of the resulting sigmoidal curve. This segment corresponds to the healthy population.
- Parameter Estimation:
- Perform linear regression on the identified linear segment. The slope (m) and intercept (c) of the regression line are used to estimate the mean (μ) and standard deviation (σ) of the healthy distribution.
- The mean is estimated as μ = -c/m.
- The standard deviation is estimated as σ = 1/m.
- RI Calculation: Calculate the 2.5th and 97.5th percentiles of the estimated healthy distribution as the reference limits: RI = μ ± 1.96σ [16].
Protocol for Implementing the Bhattacharya Algorithm
- Input Preprocessed Data: Use the cleaned, stratified data. Transformation is often applied beforehand.
- Histogram Generation: Create a frequency histogram of the test values for the subgroup. The choice of bin width can influence results and should be consistent.
- Ratio Calculation: For each pair of adjacent bins (i and i+1), calculate the natural logarithm of the ratio of their frequencies: ln(fᵢ₊₁ / fᵢ).
- Linearization and Identification:
- Plot the calculated logarithmic ratios against the midpoint values of the corresponding bin pairs.
- Identify the linear segment in this plot, which represents the healthy population.
- Parameter Estimation:
- Perform linear regression on the identified linear segment. The slope (m) and intercept (c) of the line are related to the distribution parameters.
- The mean is estimated as μ = -c/m.
- The standard deviation is estimated as σ = 1/√(-m).
- RI Calculation: Calculate the reference limits from the estimated parameters: RI = μ ± 1.96σ [16] [37].
Protocol for Implementing the EM Algorithm
- Input Preprocessed Data: Use the cleaned, stratified data. The EM algorithm can handle raw skewed data, but transformation may still be applied.
- Model Initialization: Provide initial guesses for the parameters of the healthy distribution (mean μₕ and standard deviation σₕ) and, in a two-component model, for the pathological distribution(s) and their mixing proportions.
- Iteration:
- E-Step: Estimate the posterior probability (responsibility) that each data point xᵢ belongs to the healthy distribution, given the current parameter estimates.
- M-Step: Update the parameters (μₕ, σₕ) of the healthy distribution by calculating a weighted mean and standard deviation, using the responsibilities from the E-step as weights.
- Convergence Check: Calculate the log-likelihood after each M-step. If the change in log-likelihood between iterations is below a pre-specified tolerance level (e.g., 10⁻⁶), the algorithm has converged. If not, return to the E-Step [38] [39].
- RI Calculation: Once converged, use the final parameters of the healthy distribution to calculate the nonparametric (2.5th and 97.5th percentiles) or parametric (μ ± 1.96σ) reference intervals.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Thyroid Hormone RI Studies
| Item Name | Function / Application | Example Specifications / Vendors |
|---|---|---|
| Automated Immunoassay Analyzer | Quantification of thyroid hormone levels (TSH, FT4, FT3, etc.) in serum samples. | Siemens ADVIA Centaur XP, Mindray CL-6000i, Roche Cobas e602 [36] [40] |
| Thyroid Hormone Assay Kits & Calibrators | Provide specific antibodies and reagents for the precise and accurate measurement of each hormone. | Manufacturer-provided kits and calibrators (e.g., Siemens, Mindray, Beckman Coulter) [36] [37] |
| Vacuum Blood Collection Tubes | Standardized collection of serum samples for testing, ensuring sample quality and minimizing pre-analytical variance. | Vacuette tubes (Greiner Bio-One) with procoagulant [36] [37] |
| Statistical Computing Software | Data preprocessing, algorithm implementation (Hoffmann, Bhattacharya, EM), statistical analysis, and visualization. | R (with packages refineR, mixtools, forecast), Python (with scikit-learn, SciPy) [36] [41] [39] |
| Quality Control Materials | Monitor the precision and accuracy of the analytical process, ensuring the reliability of the underlying data. | Commercially available internal quality control (IQC) materials at multiple concentration levels [36] |
The Hoffmann, Bhattacharya, and Expectation-Maximization algorithms provide powerful, complementary tools for establishing reference intervals for thyroid hormones in older adults using real-world data. The choice of algorithm is not one-size-fits-all but should be a strategic decision based on the source and distribution of the data. For physical examination data, which tends to be healthier and more Gaussian, the transformed Hoffmann and Bhattacharya algorithms are excellent choices due to their simplicity and effectiveness. In contrast, for more complex and skewed data derived from general patient populations, the EM algorithm, particularly when enhanced with Box-Cox transformation, demonstrates superior capability, especially for analytes like TSH. By adhering to the detailed protocols outlined for data preprocessing and algorithm implementation, researchers and clinical laboratories can reliably establish validated, population-specific RIs, thereby enhancing the accuracy of thyroid function assessment for the growing geriatric population.
The establishment of accurate reference intervals (RIs) is fundamental to the interpretation of clinical laboratory results and subsequent medical decision-making. For thyroid hormones, which exhibit complex variation across age, ethnicity, and geographic populations, this is particularly crucial [42] [9]. Traditional direct methods for establishing RIs require the costly and ethically challenging recruitment of hundreds of healthy individuals, making population-specific studies difficult [43] [44]. Indirect methods, which leverage vast amounts of existing real-world data (RWD) from laboratory information systems, present a powerful alternative [43] [22]. These algorithms statistically separate the distribution of physiological ("healthy") test results from the pathological within mixed datasets.
The kosmic and refineR algorithms represent the latest generation of these indirect methods. They are designed to overcome the limitations of earlier approaches, such as the Hoffman and Bhattacharya methods, which were limited to Gaussian distributions and required subjective visual inspection [45] [43]. Their application is especially relevant for thyroid function testing in older adults, where age-specific RIs are critical to avoid misdiagnosis, as thyroid-stimulating hormone (TSH) levels naturally increase with age [4] [9]. This application note provides a detailed comparison of these two advanced algorithms, complete with experimental data and implementation protocols for researchers.
Algorithm Comparative Analysis: kosmic vs. refineR
Theoretical Foundations and Methodologies
The core assumption of both kosmic and refineR is that the distribution of non-pathological results in a dataset can be modeled using a Box-Cox transformed normal distribution, which accommodates the skewed data commonly encountered in laboratory medicine [43]. Despite this shared foundation, their modeling approaches are fundamentally different.
The kosmic algorithm employs a forward modeling approach [43]. It operates by applying a Box-Cox transformation to the observed data and then iteratively fitting a Gaussian distribution to various truncated portions of this transformed data. The optimal model is selected by minimizing the Kolmogorov-Smirnov distance between the cumulative density of the truncated observed data and the fitted Gaussian model [45] [43]. This method is an advancement of the Reference Limit Estimator (RLE) and is designed to be more robust and automated than its predecessors.
In contrast, the refineR algorithm introduces a novel inverse modeling approach [43]. Instead of transforming the data first, it tests a parametric model (a Box-Cox transformed normal distribution) directly against a histogram of the original, untransformed data. It uses an asymmetric confidence band to identify bins in the histogram that most likely represent non-pathological samples. A multi-level grid search is then used to find the model parameters (λ, μ, σ) that maximize the likelihood of the observed data within this central region, using a cost function based on the Poisson likelihood [43] [44]. This inverse method ensures that the model is optimal in the original domain where the RIs are ultimately defined.
Performance and Validation in Thyroid Hormone Analysis
Multiple studies have validated the performance of both algorithms for establishing RIs for thyroid hormones, with a specific focus on their application in older adults and specialized populations. The following table summarizes key comparative findings from recent research.
Table 1: Performance Comparison of kosmic and refineR Algorithms for Thyroid Hormone RIs
| Study Context | Algorithm | Thyroid Hormone | Established RI | Key Comparative Finding |
|---|---|---|---|---|
| Adult Hospital Population [45] | kosmic | TSH | 0.53 - 7.00 mIU/L | Showed a higher upper reference limit (URI) for TSH compared to kit literature. |
| refineR | TSH | 0.55 - 8.19 mIU/L | Showed a higher upper reference limit (URI) for TSH compared to kit literature. | |
| Hoffman | TSH | 0.3 - 4.0 mIU/L | Provided a TSH URI comparable to kit literature (0.38-4.28 mIU/L). | |
| Older Adults [16] [21] | kosmic, refineR, Transformed Hoffman & Bhattacharya | TSH, FT3, FT4 | N/S | All four algorithms showed good performance and consistency when applied to physical examination data. |
| Expectation-Maximization (EM) | TSH | N/S | Outperformed others with patient data, showing high consistency with RIs from healthy older adults. | |
| Chinese High-Altitude Population [42] | refineR | TSH, FT3, FT4 | Established (e.g., TSH: 0.764–5.784 μIU/ml) | Successfully established specific RIs for a special population, differing from manufacturer's ranges. |
| Neonatal Pakistani Population [44] | refineR | TSH | 0.67-15.0 μIU/mL (0-5 days); 0.65-8.6 μIU/mL (6-30 days) | Results aligned with global literature, validating the algorithm's applicability for demographic-specific RIs. |
A large-scale validation study comparing five data mining algorithms for thyroid hormones in older adults concluded that the transformed Hoffmann, transformed Bhattacharya, kosmic, and refineR algorithms all showed good performance when using physical examination data [16] [21]. However, if only patient data is available, an Expectation-Maximization (EM) algorithm combined with a Box-Cox transformation is recommended for skewed data [16] [21].
Overall, a benchmark simulation study reported that refineR achieved the lowest mean percentage error (2.77%) among the methods tested. When assessing the success rate of RIs falling within an acceptable error margin, refineR (82.5%) was superior to kosmic (70.8%) and the direct method with N=120 samples (67.4%), though it was inferior to the direct method with N=400 samples (90.1%) [43].
Workflow and Implementation
The procedural workflow for both algorithms, from data preparation to RI derivation, can be visualized as follows. This provides a logical map for researchers to understand the key stages of the process.
Diagram 1: Workflow of kosmic and refineR algorithms
Detailed Experimental Protocol for RI Establishment
This protocol is adapted from multiple validation studies [45] [44] [42] and provides a step-by-step guide for establishing RIs for thyroid hormones using the refineR algorithm.
Title: Establishment of Population-Specific Reference Intervals for Thyroid Hormones in Older Adults Using the refineR Algorithm.
1. Objective: To determine the 2.5th and 97.5th percentile reference intervals for Thyroid Stimulating Hormone (TSH), Free Triiodothyronine (FT3), and Free Thyroxine (FT4) in an older adult population (e.g., ≥60 years) using real-world data and the refineR algorithm.
2. Materials and Equipment: Table 2: Research Reagent Solutions and Essential Materials
| Item | Function/Description | Example |
|---|---|---|
| Laboratory Information System (LIS) Data | Source of real-world thyroid hormone results, including patient age, sex, and test date. | Retrospective data from hospital or health network. |
| Statistical Software Environment | Platform for data cleaning, analysis, and algorithm execution. | R statistical programming language (v4.0.5 or higher). |
| refineR Package | Implements the core algorithm for reference interval estimation. | refineR package (v1.0.0) from CRAN. |
| Immunoassay Analyzer | System for precise measurement of thyroid hormone levels. | Cobas e601 (Roche), ADVIA Centaur (Siemens), etc. |
| Quality Control (QC) Materials | Ensures accuracy and precision of underlying hormone measurements. | Commercial QC sera at two levels, aligned with platform. |
3. Procedure:
Step 1: Ethical Approval and Data Extraction
- Obtain approval from the institutional ethical review board.
- Extract thyroid hormone test results (TSH, FT3, FT4) from the LIS for the desired timeframe (e.g., 1-6 years). Include fields for a unique patient identifier, test date, age, and sex.
- Apply inclusion criteria (e.g., patients aged ≥60 years). It is not necessary to exclude results based on clinical diagnosis a priori.
Step 2: Data Cleaning and Preprocessing
- Remove duplicate samples from the same individual. A common strategy is to keep only the first result for each patient.
- Remove any analytically implausible or erroneous values (e.g., negative values, values exceeding the analyzer's measuring range).
- Stratify the data into subgroups if needed (e.g., by age decades or sex). A minimum sample size of several thousand per subgroup is recommended for robust indirect estimation [45] [44].
Step 3: Execution of the refineR Algorithm
- Load the refined R package in the R environment using the command
library(refineR). - For each analyte and subgroup, use the
getRI()function with the vector of test results as the primary input. No other parameters are strictly required, as the algorithm automatically determines search regions. - The algorithm will perform the following steps internally [43] [44]:
- a. Preprocessing: Identify the parameter search regions and the principal peak of the data distribution.
- b. Model Optimization: Conduct a multi-level grid search for the optimal Box-Cox transformation parameter (λ), mean (μ), and standard deviation (σ) that best explains the non-pathological distribution. The cost function is based on a maximum likelihood approach.
- c. RI Calculation: Derive the central 95% RI (2.5th to 97.5th percentiles) from the optimal model.
Step 4: Bootstrap Confidence Intervals
- To determine the confidence intervals (CIs) for the calculated RIs, use a bootstrap approach.
- The
getRI()function may integrate this, or it can be performed by running the algorithm on 200 bootstrap samples of the original data (random resampling with replacement) [45]. - The 2.5th and 97.5th percentiles of the resulting 200 RIs define the 95% CI for each reference limit.
Step 5: Results Interpretation and Reporting
- Compare the established RIs with those from the manufacturer's kit insert or standard textbooks.
- Report the final RIs along with their 95% CIs, the sample size (N), and the key model parameters (λ, μ, σ) for transparency and reproducibility.
The kosmic and refineR algorithms represent significant advancements in the field of indirect reference interval estimation, offering robust, data-driven solutions for establishing population-specific RIs. For thyroid hormone testing in older adults, where traditional "one-size-fits-all" RIs can lead to misdiagnosis, these tools are particularly valuable [4] [9]. While both algorithms show strong performance, refineR's novel inverse modeling approach may provide a slight edge in precision, especially with datasets containing a high fraction of pathological samples [43]. The choice between them, or the use of other methods like EM for specific patient datasets, depends on the data characteristics and research goals [16]. The provided protocols and analyses equip researchers and laboratory professionals with the necessary information to harness these powerful tools, ultimately contributing to more personalized and accurate clinical diagnostics.
The accurate establishment of Thyroid-Stimulating Hormone (TSH) Reference Intervals (RIs) is critical for the precise diagnosis and management of thyroid disorders in older adults. Current laboratory practice often employs a "one-size-fits-all" approach to RIs, despite substantial evidence that thyroid function changes significantly with age [46] [10]. Thyroid-stimulating hormone (TSH) concentrations are higher at the extremes of life and show a U-shaped longitudinal trend in iodine-sufficient Caucasian populations [46]. In older adults, the normal TSH distribution curve shifts to the right, and it is increasingly recognised that higher TSH levels may represent a normal part of ageing [46]. This case study examines the application of the Expectation Maximization (EM) algorithm as a data mining approach to establish age-specific TSH RIs, addressing the crucial need for refined diagnostic parameters in our aging global population.
Background and Rationale
Age-Related Changes in Thyroid Physiology
Thyroid function demonstrates dynamic changes throughout the human lifespan. After the age of 40, the upper limit of the serum TSH RI increases by 0.3 mIU/L for every 10-year increase in age [34]. Research indicates that older individuals may have slightly elevated levels of thyrotropin and higher upper limits of reference intervals [34]. This physiological shift creates a fundamental problem for clinicians: using standard adult RIs for older patients can lead to overdiagnosis of subclinical hypothyroidism and potentially unnecessary treatment [10].
The aging process affects the hypothalamic-pituitary-thyroid axis, leading to an alteration in the TSH setpoint without a corresponding decline in free thyroxine (FT4) levels [47]. Serum TSH levels increase in older adults, presumably due to a reduction in TSH bioactivity or a decreased responsiveness of the thyroid to TSH [34]. This physiological adaptation must be distinguished from pathological thyroid failure, necessitating age-appropriate reference intervals.
Current Limitations in Reference Interval Establishment
Traditional methods for establishing RIs rely on stringent inclusion criteria to select healthy reference populations, which can be time-consuming, costly, and often impractical for age-specific stratification [4]. The International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) Committee developed comprehensive guidelines for establishing reference intervals, but many clinical laboratories struggle with implementation due to resource constraints [4]. Data mining algorithms offer a promising alternative by leveraging large existing datasets from clinical laboratories to derive RIs, potentially overcoming these limitations.
Experimental Protocol: EM Algorithm Application
Data Collection and Preprocessing
Two data sets were derived from the population undergoing a physical examination [48]. The initial phase involves simplified preprocessing to ensure data quality while maintaining sufficient sample size for robust analysis.
- Data Sources: Laboratory information systems containing thyroid function test results from both physical examination populations and outpatient settings [16].
- Sample Considerations: Large sample sizes are crucial; recent studies have analyzed over 7.6 million TSH measurements to establish age-specific RIs [10].
- Exclusion Criteria:
- Past or present history of thyroid disease
- Positive thyroid peroxidase antibodies (TPOAb) and thyroglobulin antibodies (TGAb)
- Palpable goiter or thyroid abnormalities on ultrasound
- Medications known to interfere with thyroid function tests
- Abnormal lipid profile, C-reactive protein levels, or other laboratory indicators of systemic illness [4]
Algorithm Implementation
The Expectation Maximization (EM) algorithm is particularly suited for handling the statistical challenges inherent in laboratory data, including non-Gaussian distributions and the presence of outliers.
- Handling Skewness: If patient data is used, then an EM algorithm combined with Box-Cox transformation is recommended for data with obvious skewness [16]. This transformation helps normalize the data distribution, improving the accuracy of interval estimation.
- Comparison Algorithms: The performance of the EM algorithm should be evaluated against other data mining approaches, including:
- Validation Framework: Algorithm-calculated RIs are compared with standard RIs calculated from a Reference data set in which reference individuals were selected following strict inclusion and exclusion criteria [48].
Performance Assessment
Objective assessment of the methods is implemented by the bias ratio (BR) matrix [48]. The BR matrix provides a standardized approach for comparing the limits of RIs established using different algorithms, with lower BR values indicating better agreement with reference standards.
Table 1: Performance Comparison of Data Mining Algorithms for TSH RI Establishment
| Algorithm | Data Type | Bias Ratio (BR) | Recommended Use |
|---|---|---|---|
| EM Algorithm | Patient data | 0.063 (for TSH) [48] | Data with significant skewness |
| Transformed Hoffmann | Physical examination data | Good performance [16] | Gaussian or near-Gaussian distributions |
| Transformed Bhattacharya | Physical examination data | Good performance [16] | Gaussian or near-Gaussian distributions |
| Kosmic | Physical examination data | Good performance [16] | Gaussian or near-Gaussian distributions |
| RefineR | Physical examination data | Good performance [16] | Gaussian or near-Gaussian distributions |
Results and Data Analysis
Age-Specific TSH Reference Intervals
Implementation of the EM algorithm and other data mining approaches reveals significant age-dependent variation in TSH levels. Studies calculating age-specific normal ranges for TSH have discovered that TSH levels are naturally higher in children compared to adults. In adults, TSH levels tend to increase with age, especially after 50 in women and 60 in men [10].
Table 2: Age-Specific TSH Reference Intervals Established Through Data Mining Approaches
| Age Group | TSH Reference Interval | Population Characteristics |
|---|---|---|
| 20-59 years | 0.4 - 4.3 mU/L [4] | Strictly selected healthy adults |
| 60-79 years | 0.4 - 5.8 mU/L [4] | Strictly selected healthy older adults |
| ≥80 years | 0.4 - 6.7 mU/L [4] | Strictly selected very old adults |
| Women (50 years) | Upper limit: 4.0 mIU/L [10] | Population-based data |
| Women (90 years) | Upper limit: 6.0 mIU/L [10] | Population-based data |
Impact on Clinical Diagnosis
The implementation of age-specific RIs has profound implications for diagnosing thyroid dysfunction in older adults. Research demonstrates that using age-specific normal ranges for TSH and FT4 could significantly reduce the number of people diagnosed with subclinical hypothyroidism [10]. Specific findings include:
- Among women aged 50-60, the rate of subclinical hypothyroidism would drop from 13.1% to 8.6%
- Among women aged 90-100, it would decline from 22.7% to 8.1%
- Similar decreases were seen in men, with the diagnosis falling from 10.9% to 7.7% in men aged 60-70 and from 27.4% to 9.6% in those aged 90-100 [10]
Workflow and Conceptual Framework
The process of establishing TSH RIs using data mining algorithms follows a systematic workflow that integrates data processing, algorithm application, and clinical implementation.
Figure 1: Experimental workflow for establishing TSH reference intervals using data mining algorithms
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for TSH RI Studies
| Reagent/Material | Specification | Application in Protocol |
|---|---|---|
| TSH Immunoassay Reagents | Manufacturer-specific platforms (Roche, Abbott, etc.) [34] | Primary TSH measurement; RIs should be established for each assay [34] |
| Thyroid Autoantibody Tests | TPOAb, TGAb immunoassays | Exclusion of autoimmune thyroid disease from reference population [4] |
| Box-Cox Transformation | Statistical software implementation (R, Python) | Normalization of skewed data distributions before EM algorithm application [16] |
| Bias Ratio Matrix | Custom statistical calculation | Objective performance assessment of different algorithms [48] |
| Laboratory Information System | Access to historical test data | Source of big data for mining algorithm application [16] |
Discussion and Clinical Implications
Algorithm Performance Considerations
The EM algorithm demonstrates particular utility in specific scenarios. The RIs of Thyroid Stimulating Hormone (TSH) established using Expectation maximization (EM) and patient data were highly consistent with the RIs established using data from healthy older adults [16]. However, algorithm performance varies depending on data characteristics:
- EM algorithm combined with simplified preprocessing can handle data with significant skewness, but its performance is limited in other scenarios [48].
- Transformed Hoffmann, transformed Bhattacahrya, kosmic and refineR algorithms showed good performance in calculating RIs from physical examination data [16].
- Consistency across different algorithms in physical examination data was found to be greater than that of outpatient data [16].
Implications for Clinical Practice and Research
Implementation of age-specific TSH RIs derived through data mining approaches addresses a critical need in geriatric medicine. Using age-specific reference intervals, a significant percentage of elderly will not be misdiagnosed as having subclinical hypothyroidism [4]. This has substantial implications for:
- Reducing unnecessary treatment: Avoiding levothyroxine therapy in older adults with age-appropriately elevated TSH levels
- Resource allocation: Decreasing monitoring burden for patients and healthcare systems
- Clinical trial design: Ensuring appropriate participant selection based on age-appropriate thyroid function criteria
Future research directions should focus on validating these approaches across diverse ethnic populations and developing standardized protocols for implementing data mining-derived RIs in clinical laboratory practice.
Navigating Analytical Challenges: Data Preprocessing, Skewness, and Algorithm Selection
In the data mining research of reference intervals for thyroid hormones in older adults, data quality is paramount. Outliers—data points that deviate significantly from other observations—can distort statistical analyses and lead to inaccurate reference intervals. The Tukey method, also known as the boxplot method, provides a robust, distribution-free approach for outlier detection that is particularly valuable for clinical and laboratory data [49]. This technique uses the Interquartile Range (IQR) to identify unusual values without assuming a normal distribution, which is crucial when working with biological data like thyroid function tests where population distributions may shift with age [50]. Within the specific context of establishing reliable reference intervals for thyroid hormones in older adults, appropriate outlier management ensures that derived ranges accurately reflect the true physiological state of the population, rather than technical artifacts or rare pathological cases.
Understanding the Tukey Method
Theoretical Foundation
The Tukey method, developed by John Tukey, utilizes the Interquartile Range (IQR) to identify potential outliers in a dataset [49]. The IQR represents the spread of the middle 50% of the data and is calculated as the difference between the third quartile (Q3, 75th percentile) and the first quartile (Q1, 25th percentile). This measure of dispersion is robust to extreme values, making it particularly suitable for outlier detection compared to standard deviation, which assumes normality and is sensitive to outliers [49] [51].
Tukey defined fences to identify outliers:
- Lower fence: Q1 - k × IQR
- Upper fence: Q3 + k × IQR
Any data point falling below the lower fence or above the upper fence is considered an outlier. The multiplier k determines the sensitivity of outlier detection; Tukey originally suggested k=1.5 for identifying "outliers" and k=3 for identifying "far outliers" [49]. This method is especially valuable in clinical research contexts like thyroid hormone studies, where population-based reference intervals must not be unduly influenced by extreme values that may represent measurement error rather than true physiological states.
Application to Thyroid Hormone Data
In research on reference intervals for thyroid hormones in older adults, the Tukey method offers significant advantages. Thyroid-stimulating hormone (TSH) distributions naturally shift with age, and using fixed reference intervals can misclassify healthy older adults as having subclinical hypothyroidism [18] [50]. The Tukey method accommodates this by defining outliers relative to the data's own distribution rather than against a predetermined range. This approach helps distinguish genuine outliers from the natural age-related rightward shift in TSH distribution, enabling researchers to establish more accurate, age-appropriate reference intervals that reflect true thyroid status rather than statistical artifacts.
Table 1: Advantages of Tukey's Method for Thyroid Hormone Research
| Feature | Advantage | Relevance to Thyroid Research |
|---|---|---|
| Non-parametric | Does not assume normal distribution | Handles naturally skewed TSH distributions in older adults |
| Resistant Statistics | Unaffected by extreme values | Prevents outliers from influencing their own detection thresholds |
| Visualization | Can be displayed via boxplots | Allows intuitive data quality assessment |
| Adaptable Sensitivity | Multiplier k can be adjusted | Enables tuning based on research goals and population characteristics |
| Simple Computation | Easy to calculate and implement | Accessible to researchers without advanced statistical expertise |
Experimental Protocols
Protocol 1: Tukey Outlier Detection in R
Objective: To identify outliers in thyroid hormone dataset using R programming language.
Materials: R statistical environment, dataset containing thyroid hormone measurements (e.g., TSH, FT4).
Procedure:
- Import Data: Load the thyroid hormone dataset into R.
- Calculate Quartiles:
- Compute IQR:
- Establish Fences (using k=1.5):
- Identify Outliers:
- Visualize with Boxplot:
Interpretation: Points beyond the whiskers in the resulting boxplot represent potential outliers that may require further investigation [49].
Protocol 2: Tukey Outlier Detection in Python
Objective: To implement Tukey's method for outlier detection in Python.
Materials: Python with NumPy and pandas libraries.
Procedure:
- Import Libraries:
- Define Quartile Function:
- Outlier Elimination Function:
- Apply to Data:
Interpretation: This function returns data with outliers removed, suitable for creating cleaned datasets for reference interval calculation [51].
Protocol 3: Visual Outlier Assessment
Objective: To create enhanced boxplots for visualizing outliers in thyroid hormone data.
Materials: R with ggplot2 package.
Procedure:
- Create Basic Boxplot:
- Highlight Outliers:
Interpretation: This visualization clearly distinguishes potential outliers from the main data distribution, facilitating decisions about data inclusion or exclusion [49].
Workflow Visualization
Outlier Management Workflow for Thyroid Data
Research Reagent Solutions
Table 2: Essential Materials for Thyroid Hormone Research and Outlier Analysis
| Item | Function | Example Application |
|---|---|---|
| Statistical Software (R/Python) | Data manipulation, statistical analysis, and visualization | Implementing Tukey method, generating boxplots, calculating reference intervals |
| Immunoassay Kits | Quantitative measurement of thyroid hormones (TSH, FT4, FT3) | Generating raw data for reference interval studies |
| Laboratory Information System (LIS) | Storage and retrieval of patient test results | Exporting large datasets for outlier analysis and data cleaning |
| Quality Control Materials | Monitoring assay performance and precision | Identifying outliers resulting from technical errors rather than biological variation |
| Clinical Data Repository | Access to patient demographics and clinical information | Contextualizing outliers with clinical metadata (age, sex, comorbidities) |
The Tukey method provides a robust, transparent approach for outlier detection in thyroid hormone research, particularly valuable when establishing reference intervals for older adults. Its non-parametric nature accommodates the age-related shifts in TSH distribution that complicate fixed reference intervals. By implementing the protocols outlined, researchers can systematically identify and manage outliers, leading to more accurate reference intervals that better reflect true thyroid status in older populations. This methodology supports the development of evidence-based diagnostic criteria that acknowledge the physiological changes of aging, potentially reducing overtreatment of subclinical hypothyroidism in older adults while still identifying clinically significant thyroid dysfunction.
In the data-driven field of medical research, particularly in establishing reference intervals (RIs) for biomarkers, the assumption of normally distributed data is fundamental for many statistical procedures. However, laboratory data, including thyroid hormone measurements in older adults, often exhibit substantial skewness and non-Gaussian characteristics. The Box-Cox transformation addresses this challenge through a family of power transformations that can normalize skewed data, stabilize variance, and enable more accurate parametric statistical analysis [52]. This technique is especially valuable in geriatric laboratory medicine, where accurate RI establishment is critical for clinical decision-making but complicated by age-related physiological changes and difficulty in obtaining large reference populations [53] [54].
Within the specific context of developing thyroid hormone RIs for older adults, the Box-Cox transformation provides a methodological framework for handling the non-Gaussian distributions commonly encountered in real-world laboratory data. This approach enables researchers to derive robust, statistically sound reference intervals that more accurately reflect the thyroid physiology of an aging population.
Theoretical Foundation of Box-Cox Transformation
Mathematical Formulation
The Box-Cox transformation is defined as a continuous function of the power parameter λ (lambda) that makes the transformed data approximately normal distributed. For a positive-valued variable Y, the one-parameter Box-Cox transformation is given by:
$$yi^{(\lambda)} = \begin{cases} \dfrac{yi^\lambda - 1}{\lambda (GM(y))^{\lambda-1}} & \text{if } \lambda \neq 0 \\ \, \\ GM(y) \ln y_i & \text{if } \lambda = 0 \end{cases} \[6pt]$$
where $GM(y) = \left(\prod{i=1}^n yi\right)^{\frac{1}{n}}$ is the geometric mean of the observations [52]. The inclusion of the geometric mean in the denominator serves to make the likelihood function comparable across different λ values, enabling the selection of an optimal transformation parameter.
For data containing zero or negative values, the two-parameter Box-Cox transformation incorporates a shift parameter α:
$$\tau(yi;\lambda,\alpha) = \begin{cases} \dfrac{(yi + \alpha)^\lambda - 1}{\lambda (GM(y+\alpha))^{\lambda-1}} & \text{if } \lambda \neq 0 \\ \, \\ GM(y+\alpha) \ln(y_i + \alpha) & \text{if } \lambda = 0 \end{cases}$$
which requires $y_i + \alpha > 0$ for all observations [52] [55].
Practical Interpretation of λ Values
The power parameter λ determines the specific form of the transformation, with special cases corresponding to common transformations:
Table 1: Interpretation of Box-Cox Transformation Parameters
| λ Value | Transformation | Formula | Common Application Context |
|---|---|---|---|
| λ = 1 | No transformation | Y | Approximately normal data |
| λ = 0.5 | Square root | √Y | Moderate right skewness |
| λ = 0 | Natural logarithm | ln(Y) | Positive skewness (log-normal) |
| λ = -0.5 | Reciprocal square root | 1/√Y | Moderate left skewness |
| λ = -1 | Reciprocal | 1/Y | Substantial left skewness |
In practice, the optimal λ is determined empirically from the data through maximum likelihood estimation, with values typically falling between -2 and 2 [52] [56].
Application in Reference Interval Establishment
Box-Cox Transformation in Laboratory Medicine
The establishment of reference intervals represents a fundamental application of Box-Cox transformations in clinical chemistry. RIs are defined as the central 95% range of reference values from healthy individuals, and the accurate determination of these intervals is crucial for clinical decision-making [55]. The traditional direct method for establishing RIs requires recruiting a large number of carefully selected healthy individuals, which is particularly challenging for special populations like older adults [53].
The indirect method, which utilizes real-world data from laboratory information systems, has emerged as a practical alternative. This approach leverages Box-Cox transformations to normalize the distribution of test results from apparently healthy individuals, enabling parametric estimation of RIs [53]. A 2024 study demonstrated this application by establishing RIs for serum tumor markers in an apparently healthy elderly population in Southwestern China using Box-Cox transformation combined with the Tukey method for outlier removal [53].
Performance Characteristics in Real-World Settings
Recent research has evaluated the performance of different Box-Cox formulations for RI establishment. A 2023 systematic comparison revealed important practical considerations:
Table 2: Performance Comparison of Box-Cox Formulations for Reference Interval Establishment
| Method | Gaussian Transformation Success Rate | Strengths | Limitations |
|---|---|---|---|
| One-parameter Box-Cox (1pBC) | 66.9% of 776 datasets | Simple implementation; computationally efficient | Fails with highly skewed distributions; biased RI estimation for remote distributions |
| Two-parameter Box-Cox (2pBC) with grid search | Variable performance | Handles data with zeros/negatives | Parameter estimation challenges; widely fluctuating λ |
| Optimized two-parameter Box-Cox (2pBCopt) | 82.4% of 776 datasets | Unbiased prediction of distribution shape; handles various distribution types | More complex implementation; computationally intensive |
The two-parameter Box-Cox transformation with optimized parameter fitting (2pBCopt) demonstrated superior performance for real-world laboratory data, successfully achieving Gaussian transformation (defined as |skewness| < 0.1 and |kurtosis| < 0.3) in the majority of cases [55].
Experimental Protocol: Establishing Thyroid Hormone Reference Intervals for Older Adults
Study Population Definition and Eligibility Criteria
The establishment of reliable reference intervals for thyroid hormones in older adults requires careful participant selection with specific consideration of age-related physiological changes.
Table 3: Eligibility Criteria for Thyroid Hormone Reference Interval Study in Older Adults
| Category | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Health Status | Apparently healthy; no history of thyroid disease; normal thyroid ultrasonography | Known thyroid disease; abnormal thyroid ultrasound; elevated thyroid antibodies |
| Age Range | ≥60 years (stratified by decade: 60-69, 70-79, ≥80) | <60 years |
| Medication | No medications affecting thyroid function | Lithium, amiodarone, antithyroid agents; iodine supplements |
| Laboratory Findings | Normal liver enzymes (ALT ≤50 U/L males, ≤40 U/L females); normal creatinine (≤111 μmol/L males, ≤81 μmol/L females); normal hematological parameters | Abnormal basic metabolic panel; anemia; leukocytosis/leukopenia |
| Sample Quality | Fasting venous blood collected morning (7-10 AM); proper processing | Hemolyzed, icteric, or lipemic samples; improper handling |
This protocol adapts exclusion criteria from established thyroid studies [57] with specific modifications for elderly populations [53].
Laboratory Analysis Protocol
Sample Collection: Collect fasting venous blood (2-4 mL) in serum separation tubes between 7:00 and 10:00 AM to minimize diurnal variation effects.
Processing: Allow blood to clot for 30 minutes, then centrifuge at 2200×g for 10 minutes at room temperature.
Analysis: Analyze serum samples within 2 hours of collection using electrochemiluminescence immunoassays (e.g., Roche Elecsys or Abbott Architect systems).
Quality Control: Implement internal quality control using Westgard multi-rules (13S, 22S, R4S) with cumulative coefficient of variation <5% for all assays [53] [54].
External Validation: Participate in external quality assessment programs (e.g., National Centre for Clinical Laboratories, College of American Pathologists).
Statistical Analysis Workflow
The following workflow diagram illustrates the comprehensive protocol for establishing thyroid hormone reference intervals using Box-Cox transformation:
Box-Cox Transformation Implementation
Normality Assessment: Test raw data distribution using Shapiro-Wilk test or skewness-kurtosis criteria (absolute skewness <3, absolute kurtosis <10) [53].
Parameter Estimation: Determine optimal λ using maximum likelihood method (e.g.,
MASS::boxcox()in R). Search range typically spans -3 to 3 with sufficient resolution (100+ points) [56].Data Transformation: Apply the selected transformation to the thyroid hormone values:
- For λ ≠ 0: ( Y^{(\lambda)} = \frac{Y^\lambda - 1}{\lambda \times GM(Y)^{\lambda-1}} )
- For λ = 0: ( Y^{(0)} = GM(Y) \times \ln(Y) )
Post-Transformation Verification: Confirm normalized distribution using the same normality tests. Iterate with adjusted λ if transformation is suboptimal.
Outlier Handling: Apply Tukey's method to remove outliers after transformation: lower limit = P25 - 1.5×IQR, upper limit = P75 + 1.5×IQR [53] [54].
Reference Interval Calculation and Validation
After successful normalization:
Calculate Transformed RIs: Compute the 2.5th and 97.5th percentiles parametrically on the transformed scale.
Back-Transform RIs: Apply the inverse Box-Cox transformation to return RIs to the original scale:
- For λ ≠ 0: ( Y = (\lambda \times Y^{(\lambda)} + 1)^{1/\lambda} )
- For λ = 0: ( Y = \exp(Y^{(0)} / GM(Y)) )
Stratification Decision: Use standard deviation ratio (SDR) from nested ANOVA to determine if age/sex partitioning is warranted (SDR > 0.3 indicates significant difference) [54].
Validation: Verify RIs using bootstrap resampling (1000+ iterations) or an independent validation dataset.
Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for Thyroid Hormone RI Studies
| Category | Specific Items | Function/Application | Quality Control Requirements |
|---|---|---|---|
| Sample Collection | Serum separation tubes (2-4 mL Vacuette); tourniquets; sterile needles | Standardized blood collection | Lot verification; expiration monitoring |
| Immunoassay Systems | Roche Cobas e801; Abbott Architect i2000; Siemens Advia Centaur | Thyroid hormone measurement | Platform-specific calibration; participation in EQA programs |
| Assay Kits | TSH, fT3, fT4, TPO-Ab, Tg-Ab, TRAb electrochemiluminescence assays | Quantitative hormone and antibody detection | CV <5% for precision; verification of reference materials |
| Quality Control Materials | Lyphochek Tumor Marker Plus Control; platform-specific QC materials | Daily performance monitoring | Westgard rules implementation; cumulative CV <5% |
| Data Analysis Software | R Statistical Environment with MASS package; MedCalc; Minitab | Statistical analysis and Box-Cox transformation | Version control; validation of statistical algorithms |
Advanced Methodological Considerations
Handling Challenging Data Distributions
While the standard Box-Cox transformation effectively handles many non-Gaussian distributions, researchers establishing thyroid hormone RIs in older adults may encounter specific challenges:
Highly Skewed Distributions: When the one-parameter Box-Cox transformation fails (occurring in approximately 33% of real-world datasets) [55], the optimized two-parameter approach (2pBCopt) significantly improves success rates by simultaneously optimizing both power (λ) and shift (α) parameters.
Adaptive Box-Cox Transformation: For metabolomic data with diverse distribution types, an adaptive Box-Cox (ABC) transformation has been developed that tunes the power parameter based on normality test results, outperforming conventional transformations for both positively and negatively skewed distributions [58]. This approach may be adapted for thyroid hormone datasets with complex distributional characteristics.
Multiple Comparison Considerations: When establishing RIs for multiple thyroid parameters (TSH, fT3, fT4, antibodies), implement false discovery rate control to account for multiple hypothesis testing in stratification decisions.
Age-Specific Considerations for Older Adults
Thyroid hormone reference intervals for older adults require special methodological considerations:
Stratification by Narrower Age Bands: While traditional approaches may use decade-based stratification (60-69, 70-79, 80+), finer stratification may be necessary to capture subtle age-related changes in thyroid physiology.
Comorbidity Adjustment: Carefully consider the inclusion/exclusion of individuals with age-prevalent conditions that may indirectly affect thyroid function (e.g., renal impairment, cardiac disease).
Medication Profiling: Document all medications, as polypharmacy is common in older adults and many drugs can influence thyroid function test results without causing overt thyroid dysfunction.
The Box-Cox transformation provides a powerful, flexible method for handling non-Gaussian distributions in the establishment of thyroid hormone reference intervals for older adults. When implemented within a rigorous experimental protocol that includes appropriate participant selection, standardized laboratory methods, and comprehensive statistical analysis, this approach enables researchers to derive accurate, age-specific RIs that reflect the unique thyroid physiology of an aging population. The optimized two-parameter Box-Cox transformation (2pBCopt) particularly offers superior performance for real-world laboratory datasets, successfully normalizing distributions in over 80% of cases and providing a robust foundation for clinical decision-making in geriatric thyroid management.
The establishment of accurate reference intervals (RIs) is a cornerstone of clinical diagnostics, providing essential benchmarks for interpreting patient laboratory results. Within thyroid hormone testing, this is particularly crucial given the global prevalence of thyroid disorders, with clinical hyperthyroidism and hypothyroidism affecting 0.2–1.3% and 0.2–5.3% of the population, respectively [59]. Traditional direct methods for establishing RIs are often hampered by tedious, costly, and time-consuming processes for recruiting healthy individuals, frequently leading laboratories to adopt non-validated RIs from other sources [59]. The indirect approach, which utilizes data mining algorithms on real-world data (RWD) from routine laboratory information systems, presents a powerful alternative. It is more economical and flexible, making it especially valuable for specific populations, such as older adults, where recruiting reference individuals is particularly challenging [48] [59]. The performance of these algorithms, however, is highly dependent on the characteristics of the data source and its underlying distribution. This article provides a structured framework for selecting the optimal data mining algorithm based on these critical factors, specifically within the context of research on thyroid hormones.
Key Data Mining Algorithms and Their Performance Characteristics
Data mining algorithms are designed to distinguish the distribution of healthy individuals from mixed datasets that include pathological samples. Their performance varies significantly based on their underlying principles and the data distribution they encounter.
Table 1: Characteristics and Performance of Key Data Mining Algorithms
| Algorithm | Principle | Best-Suited Data Distribution | Performance Notes |
|---|---|---|---|
| Expectation-Maximization (EM) | Iterative algorithm that estimates parameters by alternating between expectation and maximization steps [59]. | Significantly skewed data [48] [59]. | Excellent for skewed TSH data (Bias Ratio=0.063); performance poorer for other thyroid hormones [48]. |
| Hoffmann | Graphical method based on cumulative frequency distribution [59]. | Gaussian or near-Gaussian distributions [48] [59]. | Performs well for FT3, FT4, TT3, and TT4; results match standard RIs [48]. |
| Bhattacharya | Graphical method that separates Gaussian components from a mixed distribution [59]. | Gaussian or near-Gaussian distributions [48] [59]. | Similar performance to Hoffmann for FT3, FT4, TT3, and TT4 [48]. |
| refineR | Parametric method utilizing Box-Cox transformation and model selection [59]. | Skewed or non-Gaussian distributions after Box-Cox transformation [59]. | Robust performance for various hormones; effective for FT3, FT4, TT3, and TT4 [48]. |
| kosmic | Parametric approach similar to refineR, designed for efficiency with large datasets [59]. | Skewed or non-Gaussian distributions after Box-Cox transformation [59]. | Effective for establishing RIs from real-world data [59]. |
Experimental Protocols for RI Establishment
A standardized protocol is essential for generating reliable and reproducible RIs. The following workflow outlines a robust methodology for establishing RIs for thyroid hormones using the indirect approach.
The diagram below illustrates the comprehensive workflow for establishing reference intervals, from data collection to final validation.
Protocol 1: Data Sourcing and Preprocessing
Objective: To collect and prepare a dataset from the Laboratory Information System (LIS) suitable for indirect RI estimation.
- Data Extraction: Derive results for thyroid-related hormones (TSH, FT4, TT4, FT3, TT3) and necessary demographic data (sex, age) from the LIS for individuals undergoing physical examination [59].
- Simplified Preprocessing: Perform a two-step preprocessing routine without applying strict health-based exclusion criteria [59].
- Step 1: Apply a random sampling strategy to balance the sex ratio and age composition of the dataset.
- Step 2: Identify and remove outliers for each variable within subgroups using the Tukey method [59].
- Data Splitting: Establish a separate "Reference data set" for validation by recruiting presumably healthy individuals following strict inclusion and exclusion criteria (e.g., normal BMI, blood pressure, no history of serious diseases, negative thyroid antibodies) [59].
Protocol 2: Algorithm Application and Validation
Objective: To establish and validate RIs using selected data mining algorithms.
- Distribution Assessment: For the preprocessed test data, assess the distribution of each thyroid hormone (e.g., using histograms and normality tests).
- Algorithm Selection: Based on the distribution, select the appropriate algorithm(s) as guided by Table 1.
- RI Calculation: Execute the chosen algorithms to calculate the 2.5th and 97.5th percentiles as the RIs.
- Performance Validation: Objectively evaluate the algorithm-derived RIs by comparing them with the standard RIs from the Reference data set. Use a Bias Ratio (BR) matrix for quantitative assessment, where a lower BR indicates higher consistency with the standard RIs [48].
The Scientist's Toolkit: Research Reagent Solutions
The following reagents and materials are essential for the experimental workflows described in the protocols.
Table 2: Essential Research Reagents and Materials
| Item | Function / Application | Specification Example |
|---|---|---|
| Fasting Blood Samples | Source for serum/plasma to measure thyroid hormone levels [59]. | Collected in procoagulant vacuum tubes (e.g., Vacuette) [59]. |
| CHEMILUMINESCENCE Immunoassay Analyzer | Automated, high-throughput measurement of TSH, FT4, FT3, TT3, and TT4 [59]. | ADVIA Centaur XP (Siemens Healthineers) [59]. |
| Assay Calibrators and Controls | Calibration and quality control to ensure accuracy and reliability of hormone measurements [59]. | Manufacturer-provided calibrators and quality control products [59]. |
| Bioelectrical Impedance Analysis (BIA) Device | Assessment of body composition, specifically Visceral Fat Area (VFA) and Subcutaneous Fat Area (SFA), for metabolic studies [60]. | DUALSCAN HDS-2000 (Omron Healthcare) [60]. |
| Digital Immunoassay (d-IA) Platform | Ultra-sensitive, quantitative measurement of TSH using single-molecule imaging technology, requiring small sample volumes [61]. | Benchtop d-IA analyzer with functional sensitivity of ~0.00228 μIU/mL [61]. |
| TSH-Specific Antibodies | Key reagents for immunoassays; monoclonal antibodies against TSH β-subunit for capture and α-subunit for detection [61]. | Immobilized on magnetic beads (e.g., Magnosphere MS300/Tosyl) [61]. |
The strategic selection of data mining algorithms, guided by data distribution characteristics, is fundamental to establishing accurate reference intervals for thyroid hormones. The EM algorithm demonstrates superior performance for heavily skewed data like TSH, while Hoffmann, Bhattacharya, and refineR are more suitable for Gaussian or near-Gaussian distributions, as seen with FT3, FT4, TT3, and TT4. By implementing the standardized protocols and validation frameworks outlined herein—including the critical use of a Bias Ratio matrix for objective evaluation—researchers can reliably leverage real-world data to generate RIs that are both statistically sound and clinically relevant, thereby advancing personalized medicine and metabolic research in older adult populations.
Real-world clinical data are fundamental for advancing medical research, including the development of reference intervals for thyroid hormones in older adults. However, such data are often characterized by significant challenges, including scarcity of well-defined reference populations, sparsity of observations for specific demographic subgroups, and pervasive missing data. These issues can compromise the validity and generalizability of research findings if not properly addressed. Missing data, in particular, is a common problem in almost all clinical and epidemiological research studies, complicating data preprocessing and analysis, reducing statistical power, and potentially introducing bias into treatment effect estimates [62]. This application note provides detailed protocols and analytical frameworks for mitigating these data quality issues, with a specific focus on thyroid hormone research in aging populations.
Establishing Robust Reference Intervals for Thyroid Hormones in Older Adults
Establishing reliable reference intervals (RIs) for thyroid hormones in older adults requires meticulous attention to participant selection and data quality. A prospective study designed to establish RIs for Thyroid-Stimulating Hormone (TSH) and Free Thyroxine (FT4) exemplifies this rigorous approach [4].
Experimental Protocol: Prospective Reference Interval Establishment
- Objective: To determine age-specific RIs for TSH and FT4 in a reference population over 60 years old and compare them to young subjects.
- Study Population: 1200 subjects of both sexes, stratified by age groups (20-49, 50-59, 60-69, 70-79, and ≥80 years).
- Inclusion/Exclusion Criteria:
- Questionnaire: An initial questionnaire was administered to exclude individuals with personal or familial thyroid disease, use of medications known to interfere with TSH or FT4 measurements, recent hospitalization, or smoking [4].
- Physical Examination: Exclusion of subjects with goiter or other thyroid abnormalities on palpation.
- Laboratory Testing: Exclusion based on positive thyroid peroxidase antibodies (TPOAb), thyroglobulin antibodies (TGAb), abnormal lipid profile, elevated C-reactive protein (CRP), abnormal blood count, or renal dysfunction. Subjects with TSH <0.1 mU/L or >10.0 mU/L were also excluded [4].
- Laboratory Methods: Serum levels of TSH and FT4 were measured using standardized immunoassays.
- Statistical Analysis: Reference intervals were established for different age cohorts, and statistical tests (e.g., comparison of means between age groups) were applied.
The application of this rigorous protocol revealed significant age-dependent shifts in thyroid hormone levels, which are summarized in Table 1.
Table 1: Age-Specific Reference Intervals for TSH and FT4 [4]
| Age Group (Years) | TSH Reference Interval (mU/L) | FT4 Reference Interval (ng/dL) |
|---|---|---|
| 20 - 59 | 0.4 - 4.3 | Manufacturer's Range Used |
| 60 - 79 | 0.4 - 5.8 | 0.7 - 1.7 |
| ≥ 80 | 0.4 - 6.7 | 0.7 - 1.7 |
The data demonstrates that the TSH reference range increases with age, while FT4 levels decrease. Using the manufacturer's range (without age segmentation) would have led to a misdiagnosis of elevated TSH in 6.5% of subjects aged 60-79 and 12.5% of those aged 80 or older [4]. This underscores the critical importance of employing age-specific RIs to avoid overdiagnosis of subclinical hypothyroidism in the elderly.
A Systematic Framework for Handling Missing Clinical Data
The presence of missing values is a major impediment to deriving knowledge from clinical data [63]. A systematic review of imputation methods provides an evidence-based framework for selecting the most appropriate technique [62].
Protocol for Handling Missing Data
- Step 1: Characterize the Missingness. Before imputation, analyze the structure of the missing data [62].
- Mechanism: Identify the pattern of why data is missing—whether it is Missing Completely at Random (MCAR), Missing at Random (MAR), or Missing Not at Random (MNAR).
- Pattern: Determine if the missingness is univariate, multivariate, monotone, or arbitrary.
- Ratio: Calculate the percentage of missing values for each variable.
- Step 2: Select an Imputation Method. The choice of method should be guided by the characteristics identified in Step 1. The evidence map from the systematic review suggests the following alignments [62]:
- Conventional Statistical Methods (e.g., MICE, Regression): Often suitable for MCAR and MAR data with low-to-moderate missingness ratios. These were used in 45% of the reviewed studies.
- Machine/Deep Learning Methods (e.g., XGBoost, Neural Networks): Can handle complex, non-linear relationships and may be more robust for higher missingness ratios or arbitrary patterns. These were employed in 31% of studies.
- Hybrid Methods: Combine approaches for potentially improved performance, used in 24% of studies.
- Step 3: Implement and Validate. Perform the imputation, creating a single or multiple completed datasets. For multiple imputation, analyze each dataset separately and pool the results. Validate the imputation model's performance, for instance, through simulation studies [62] [64].
Comparative Analysis of Imputation Methods
Table 2: Common Imputation Methods and Their Applications in Clinical Data [63] [62]
| Method Category | Specific Technique | Description | Best Suited For |
|---|---|---|---|
| Conventional Statistical | MICE (Multiple Imputation by Chained Equations) | Iterative technique that imputes missing data by modeling each variable conditional on the others. | MAR data, mixed data types (continuous, categorical). A widely used and robust approach [63] [62]. |
| Mean/Median Imputation | Replaces missing values with the mean or median of the observed data for that variable. | MCAR data (as a simple baseline). Can severely underestimate variance and is generally not recommended [64]. | |
| Machine Learning | Tree-Based Methods (e.g., XGBoost, LightGBM) | Uses ensemble decision trees to predict missing values based on other observed variables. | Complex datasets with non-linear relationships; competitive performance in challenges [63]. |
| k-Nearest Neighbors (k-NN) | Imputes missing values based on the values from 'k' most similar subjects (neighbors) in the dataset. | MAR data, when the dataset is sufficiently large to find meaningful neighbors. | |
| Neural Networks | Advanced models that can learn complex patterns to predict missing values. | Large, complex datasets with high-dimensionality and arbitrary missing patterns [62]. |
A recent benchmark evaluation, the Data Analytics Challenge on Missing data Imputation (DACMI), confirmed that machine learning models like LightGBM and XGBoost, alongside statistical models like MICE, can achieve strong imputation performance for clinical laboratory data when coupled with carefully engineered features [63].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Thyroid Function Studies
| Item | Function/Brief Explanation |
|---|---|
| Thyroid Stimulating Hormone (TSH) Immunoassay Kit | Quantifies serum TSH levels; the primary test for screening thyroid dysfunction and defining reference intervals [4] [65]. |
| Free Thyroxine (FT4) Immunoassay Kit | Measures the biologically active, unbound fraction of thyroxine in serum; crucial for differentiating subclinical and overt thyroid disease [4] [65]. |
| Free Triiodothyronine (FT3) Immunoassay Kit | Measures the active thyroid hormone; used in comprehensive thyroid function testing, particularly in hyperthyroidism [66]. |
| Thyroid Peroxidase Antibody (TPOAb) Test | Detects autoimmune thyroiditis (Hashimoto's disease); an essential exclusion criterion for defining a healthy reference population [4]. |
| Thyroglobulin Antibody (TGAb) Test | Detects antibodies against thyroglobulin; used alongside TPOAb to rule out autoimmune thyroid disease in reference populations [4]. |
| HIV-1 Viral Load Test (e.g., Cobas Amplicor) | Critical for studies involving populations with comorbidities like HIV, as viral load and HAART exposure can significantly impact thyroid function [66]. |
| Flow Cytometry System (e.g., BD FACS Calibur) | For determining CD4+ T-cell counts; an important clinical variable in immunocompromised populations that may be correlated with endocrine dysfunction [66]. |
Visualizing Workflows and Data Relationships
Workflow for Establishing Reference Intervals
Protocol for Managing Missing Data
Logical Relationship: Data Issues to Mitigation Strategies
Benchmarking Success: Validating and Comparing Algorithm Performance for Clinical Accuracy
Reference intervals (RIs) are fundamental tools in clinical diagnostics, providing the framework for interpreting laboratory test results and informing patient management decisions. For thyroid hormones, establishing accurate RIs becomes particularly crucial in older adult populations, where age-related physiological changes can significantly alter thyroid function parameters. The definition of the "gold standard" for RI establishment has evolved considerably, pivoting on the critical distinction between RIs derived from rigorously selected healthy cohorts and those obtained through indirect data mining methods applied to larger, more heterogeneous clinical populations. This application note examines this central comparison within the broader context of data mining research for thyroid hormones in older adults, providing detailed protocols and analytical frameworks to guide researchers and drug development professionals in their methodological decisions.
Established RIs from Rigorously Selected Healthy Populations
The conventional approach for establishing RIs involves direct sampling from carefully screened healthy individuals following standardized guidelines. This method aims to define the physiological range by excluding individuals with conditions that might influence the analyte of interest.
Key Studies and Reference Intervals
Table 1: Thyroid Hormone Reference Intervals from Select Healthy Cohort Studies
| Population | Sample Size | TSH RI (mIU/L) | FT4 RI (pmol/L) | FT3 RI (pmol/L) | Notes | Citation |
|---|---|---|---|---|---|---|
| Chinese Adults | 20,303 | 0.71–4.92 | 12.2–20.1 | 3.9–6.0 | Sex-specific differences observed for all hormones except TT4 | [67] |
| Korean Population | 5,987 | 0.59–7.03 | N/R | N/R | Wider intervals in females (0.56-7.43) vs males (0.62-6.57) | [68] |
| Chinese Pediatrics | 1,279 | Age-dependent | Age-dependent | Age-dependent | Significant age and sex partitioning required | [40] |
| Austrian Children | 1,209-1,395 | Age-dependent | Age-dependent | Age-dependent | Highest levels in first month of life, declining with age | [69] |
Abbreviations: RI (Reference Interval), TSH (Thyroid-Stimulating Hormone), FT4 (Free Thyroxine), FT3 (Free Triiodothyronine), N/R (Not Reported)
The Korean National Health and Nutrition Examination Survey (KNHANES) demonstrated the importance of population-specific RIs, reporting an overall TSH reference interval of 0.59–7.03 mIU/L in a meticulously selected reference population of 5,987 individuals. Notably, this study revealed significantly wider TSH intervals in females (0.56–7.43 mIU/L) compared to males (0.62–6.57 mIU/L), highlighting the necessity of gender-specific partitioning [68].
Similarly, a comprehensive Chinese study established RIs for thyroid-associated hormones in 20,303 euthyroid adults, reporting a TSH interval of 0.71–4.92 mIU/L. This research further identified significant sex differences for all hormones except total T4, with TSH levels higher in females than males [67].
Experimental Protocol: Establishing RIs via Rigorous Healthy Cohort Selection
Protocol Title: Direct Reference Interval Establishment through Rigorously Selected Healthy Cohorts
1. Study Population Definition and Eligibility Criteria
- Inclusion Criteria: Ambulatory individuals without personal or family history of thyroid dysfunction; negative thyroid autoantibodies (TPOAb <34 IU/mL); normal thyroid ultrasound; no medications affecting thyroid function; euthyroid status confirmed by normal FT4 and TSH levels.
- Exclusion Criteria: Pregnancy; acute or chronic illness affecting thyroid function; abnormal BMI percentiles; pituitary disorders; recent surgery or hospitalization; iodine-containing supplement use.
2. Pre-analytical Procedures
- Sample collection following standardized phlebotomy procedures after 8-12 hour fast
- Morning blood draw (7:00-9:00 AM) to account for diurnal TSH variation
- Serum separation within 2 hours of collection
- Storage at -80°C until batch analysis
3. Analytical Measurements
- Hormone measurement using standardized immunoassay platforms (e.g., Siemens Advia Centaur XP, Roche Cobas, Mindray CL-6000i)
- Implementation of rigorous quality control procedures following CLSI guidelines
- Participation in external quality assurance programs (e.g., CAP surveys)
4. Statistical Analysis
- Assessment of data distribution (Gaussian vs. non-Gaussian)
- Log-transformation of non-normally distributed parameters (e.g., TSH)
- Calculation of 2.5th and 97.5th percentiles with 90% confidence intervals
- Partitioning by age, sex, and other relevant demographic factors using validated statistical criteria
5. Validation Procedures
- Transferability verification using methodology comparable to initial establishment
- Clinical validation through assessment of diagnostic performance in patient cohorts
Figure 1: Workflow for Establishing RIs from Rigorously Selected Healthy Cohorts
Data Mining Approaches for RI Establishment
The emergence of big data in healthcare has facilitated alternative approaches to RI establishment through sophisticated computational methods applied to existing clinical and laboratory datasets.
Algorithm Performance and Comparison
Table 2: Comparison of Data Mining Algorithms for Thyroid Hormone RI Establishment in Older Adults
| Algorithm | Data Source | Performance | Advantages | Limitations | Citation |
|---|---|---|---|---|---|
| Transformed Hoffmann | Physical examination data | Good consistency with RIs from healthy cohorts | Effective with relatively healthy populations | Requires data pre-processing | [16] [21] |
| Transformed Bhattacahrya | Physical examination data | Good consistency with RIs from healthy cohorts | Robust for mixed distributions | Complex implementation | [16] [21] |
| Kosmic | Physical examination data | Good consistency with RIs from healthy cohorts | Handles overlapping distributions | Computational intensity | [16] [21] |
| RefineR | Physical examination data | Good consistency with RIs from healthy cohorts | Identifies latent Gaussian components | Requires large sample sizes | [16] [21] |
| Expectation Maximization (EM) | Patient data | High consistency with RIs from healthy older adults | Effective with skewed data | May require Box-Cox transformation | [16] [21] |
A comprehensive methodological comparison evaluated five data mining algorithms for establishing thyroid hormone RIs in older adults. The study revealed that transformed Hoffmann, transformed Bhattacahrya, Kosmic, and RefineR algorithms demonstrated good performance when applied to physical examination data, showing high consistency with RIs derived from healthy older adults. For patient data, which typically exhibits more skewness, the Expectation Maximization (EM) algorithm combined with Box-Cox transformation proved most effective [16] [21].
Experimental Protocol: Indirect RI Derivation Using Data Mining Algorithms
Protocol Title: Indirect Reference Interval Establishment through Data Mining of Laboratory Databases
1. Data Extraction and Pre-processing
- Extract laboratory test results from Laboratory Information System (LIS) with associated demographic data
- Implement data cleaning procedures to remove duplicates and erroneous entries
- Anonymize data to ensure patient confidentiality
- Exclude repeated measurements from the same individual using appropriate statistical methods
2. Data Filtering and Selection
- Apply statistical outlier detection methods (e.g., Tukey's method)
- Exclude pathological values using ICD coding when available
- Stratify data by age, sex, and other relevant demographic variables
3. Algorithm Application and Selection
- Apply multiple data mining algorithms (Hoffmann, Bhattacahrya, Kosmic, RefineR, EM)
- Select optimal algorithm based on data characteristics:
- For physical examination data: Transformed Hoffmann, Bhattacahrya, Kosmic, or RefineR
- For patient data: EM algorithm with Box-Cox transformation for skewed distributions
4. Statistical Analysis and RI Calculation
- Implement appropriate transformations for non-Gaussian distributions
- Calculate 2.5th and 97.5th percentiles using selected algorithm
- Determine confidence intervals for calculated limits
5. Validation and Verification
- Compare derived RIs with those from healthy populations when available
- Assess clinical concordance through physician review
- Evaluate diagnostic performance in patient cohorts
Figure 2: Algorithm Selection Workflow for Data Mining Approaches to RI Establishment
Comparative Analysis and Clinical Implications
Methodological Comparison
The fundamental distinction between these approaches lies in their underlying philosophy: the healthy cohort model seeks to define physiological normality through rigorous exclusion, while data mining approaches aim to extract signal from noisy clinical data through sophisticated computational techniques.
A study by Li et al. demonstrated that when applied to physical examination data, certain data mining algorithms (transformed Hoffmann, transformed Bhattacahrya, Kosmic, and RefineR) could produce RIs highly consistent with those derived from healthy cohorts [16]. This suggests that for relatively healthy populations, data mining approaches can yield clinically valid results with significantly reduced resource investment.
However, the performance of these algorithms varies considerably with data source quality. The same study found greater consistency across algorithms when applied to physical examination data compared to outpatient data, highlighting the critical importance of data source characteristics in determining methodological suitability [16].
Clinical Relevance in Older Adult Populations
The establishment of age-appropriate thyroid hormone RIs carries particular significance for older adult populations. A recent systematic review and meta-analysis revealed a J-shaped association between TSH levels and frailty in older adults, with TSH levels in the upper half of the reference range (2.7-4.8 mIU/L) associated with significantly increased frailty risk (OR: 1.30 for 2.7 mIU/L to 2.06 for 4.8 mIU/L) [15] [70]. This relationship underscores the clinical importance of accurate RI definition in this population, as values conventionally considered "normal" may carry different prognostic implications for older adults.
The choice between methodological approaches also has practical implications for resource allocation. The direct method requires substantial investment in participant recruitment, screening, and sample collection, while data mining approaches leverage existing clinical data, potentially offering significant cost and time savings.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Thyroid Hormone RI Studies
| Category | Specific Items | Function/Application | Examples/Specifications |
|---|---|---|---|
| Immunoassay Systems | Automated analyzers | Quantitative measurement of thyroid hormones | Siemens Advia Centaur XP, Roche Cobas, Mindray CL-6000i |
| Assay Kits | TSH, FT4, FT3, TPOAb, TgAb | Specific analyte detection | Manufacturer-specific reagent kits with calibrated standards |
| Quality Control Materials | Internal and external QC | Assay performance verification | Commercial quality control sera at multiple concentrations |
| Sample Collection | Serum separation tubes | Standardized pre-analytical procedures | Vacuette tubes with procoagulant gel |
| Data Analysis Software | Statistical packages | Data management and RI calculation | R, SPSS, MedCalc, SAS |
| Reference Materials | Certified calibrators | Assay standardization and harmonization | Traceable to international reference standards |
Both rigorously selected healthy cohorts and advanced data mining approaches offer distinct advantages for establishing thyroid hormone reference intervals in older adults. The traditional healthy cohort method remains the gold standard for defining physiological normality but requires substantial resources. Data mining algorithms applied to well-curated datasets can produce clinically valid RIs with significantly improved efficiency, particularly for physical examination data. The optimal methodological approach depends on research objectives, available resources, and intended clinical applications. For drug development and clinical research involving older adults, understanding the provenance and limitations of applied RIs is essential for accurate result interpretation and appropriate clinical decision-making.
Within the specialized field of establishing reference intervals (RIs) for thyroid hormones in older adults, data mining algorithms are indispensable for analyzing vast clinical datasets. The selection of an optimal algorithm, however, presents a significant challenge due to the lack of standardized, objective evaluation protocols. The Bias Ratio (BR) Matrix has emerged as a novel quantitative framework that enables the rigorous, head-to-head comparison of data mining algorithms, thereby facilitating method selection based on empirical performance metrics rather than convention alone [48] [71]. This framework is particularly critical for thyroid hormone research in aging populations, where subtle changes in hormone levels, such as the natural rise in Thyroid-Stimulating Hormone (TSH) with age, must be accurately characterized to avoid overdiagnosis [10]. This document outlines the application of the BR Matrix, providing detailed protocols for its implementation in a research setting focused on geriatric thyroidology.
Theoretical Foundation of the Bias Ratio Matrix
Definition and Mathematical Formulation
The Bias Ratio (BR) is a concrete metric originally developed in finance to detect abnormalities in return distributions [72]. In the context of clinical data mining, it has been adapted to measure the alignment between algorithm-derived RIs and a reference standard.
The core mathematical formulation of the Bias Ratio for a single RI limit (upper or lower) is as follows [48] [71]: Bias Ratio (BR) = (Algorithm-derived Limit - Reference Limit) / Allowable Deviation
The Allowable Deviation is a predefined value, often derived from analytical performance specifications or clinical requirements. This calculation generates a unitless value where:
- A BR of 0 indicates perfect agreement with the reference standard.
- A BR close to 0 signifies high consistency and minimal bias.
- Positive or negative BR values indicate the direction and magnitude of the bias.
A BR Matrix is then constructed by calculating the BR for both the upper and lower limits of the RIs established by multiple algorithms, creating a standardized comparison table [48] [71].
The Workflow of Algorithm Assessment Using the BR Matrix
The following diagram illustrates the logical flow of using the BR Matrix for objective algorithm assessment, from data preparation to final algorithm selection.
Application in Thyroid Hormone Reference Interval Research
Performance of Data Mining Algorithms for Thyroid Hormones
Research has systematically evaluated five common data mining algorithms—Hoffmann, Bhattacharya, Expectation-Maximization (EM), kosmic, and refineR—for establishing RIs for thyroid hormones in both non-elderly and older adult populations [21] [48] [71]. The BR Matrix was central to these evaluations, quantifying each algorithm's performance against RIs derived from rigorously selected healthy individuals.
The table below summarizes a synthesized finding from these studies, illustrating how a BR Matrix might be populated for the upper reference limit (URL) of TSH in an older adult cohort. The BR values are illustrative examples based on reported performances.
Table 1: Exemplar Bias Ratio Matrix for TSH Upper Reference Limit in Older Adults
| Data Mining Algorithm | Calculated URL (mIU/L) | Reference URL (mIU/L) | Bias Ratio (BR) | Performance Interpretation |
|---|---|---|---|---|
| Expectation-Maximization (EM) | 4.8 | 4.8 | 0.063 [48] | Excellent Consistency |
| kosmic | 4.5 | 4.8 | -0.5 | Moderate Negative Bias |
| refineR | 4.6 | 4.8 | -0.3 | Mild Negative Bias |
| Transformed Hoffmann | 5.0 | 4.8 | 0.3 | Mild Positive Bias |
| Transformed Bhattacharya | 5.1 | 4.8 | 0.4 | Moderate Positive Bias |
Key Research Findings via the BR Matrix
Application of the BR Matrix in recent studies has yielded critical insights for the field:
- Algorithm Selection is Context-Dependent: The EM algorithm demonstrated outstanding performance for TSH (BR = 0.063), particularly when applied to patient data with significant skewness, often after Box-Cox transformation [21] [48]. In contrast, the Hoffmann, Bhattacharya, and refineR algorithms showed superior performance for free and total thyroid hormones (FT4, FT3, TT4, TT3), which often exhibit Gaussian or near-Gaussian distributions in physical examination data [48] [71].
- Impact of Data Source: Consistency between different algorithms was found to be greater when using physical examination data compared to general outpatient data, which contains a higher proportion of pathological results [21]. The BR Matrix effectively quantified this difference in robustness.
- Driving Clinical Decisions: The objective rankings from the BR Matrix support the recommendation to use age-specific RIs. For example, the upper normal limit for TSH in a 90-year-old may be 6.0 mIU/L, which is 50% higher than the limit for a 50-year-old [10]. Using these age-adjusted RIs can dramatically reduce overdiagnosis of subclinical hypothyroidism in the elderly, from 22.7% to 8.1% in women aged 90-100 [10].
Experimental Protocols
Core Protocol: Evaluating Algorithms with the BR Matrix
This protocol provides a step-by-step methodology for using the BR Matrix to assess data mining algorithms for establishing thyroid hormone RIs.
Objective: To objectively compare the performance of five data mining algorithms (Hoffmann, Bhattacharya, EM, kosmic, refineR) against a reference standard for calculating thyroid hormone RIs in an older adult population.
Materials: See Section 5.1 for the "Scientist's Toolkit" of required reagents and software.
Step-by-Step Workflow:
Data Set Establishment
- Reference Data Set: Recruit reference individuals following strict inclusion/exclusion criteria (e.g., normal BMI, blood pressure, no history of major diseases, negative thyroid antibodies, normal thyroid ultrasound) [71]. This cohort should be age-stratified to reflect the older adult population (e.g., >60 years).
- Test Data Set: Derive data from laboratory information systems for individuals undergoing physical examinations. Perform simplified preprocessing: random sampling to balance age/sex ratios and outlier removal using the Tukey method [71].
Reference Interval Establishment (Gold Standard)
- Use the Transformed Parametric (TP) method on the Reference Data Set to establish the reference upper and lower limits for each thyroid hormone (TSH, FT4, FT3, TT4, TT3). These are your reference values (
Reference_Limit).
- Use the Transformed Parametric (TP) method on the Reference Data Set to establish the reference upper and lower limits for each thyroid hormone (TSH, FT4, FT3, TT4, TT3). These are your reference values (
Candidate RI Calculation
Bias Ratio Calculation
- For each algorithm and each hormone, calculate the Bias Ratio for the upper (URL) and lower (LRL) reference limits.
BR = (Algorithm_Limit - Reference_Limit) / Allowable_Deviation- The Allowable Deviation should be defined a priori based on clinical goals or analytical performance standards. A typical approach is to use a percentage of the reference interval.
Matrix Construction and Performance Assessment
- Construct a BR Matrix (see Table 1) with algorithms as rows and hormones/limits as columns.
- Rank algorithms based on the absolute value of their BR (
|BR|) for each hormone. The algorithm with the|BR|closest to zero for a given hormone and data type is considered the best performer.
The following workflow diagram visualizes this multi-step experimental protocol.
Supplementary Protocol: Assessing Impact of Age-Specific RIs
Objective: To quantify the clinical impact of implementing algorithm-derived, age-specific RIs compared to fixed RIs across all ages.
Methodology:
- Use the optimal algorithm identified in Protocol 4.1 to establish age-stratified RIs (e.g., 50-59, 60-69, 70-79, 80+ years).
- Apply both the fixed RIs and the new age-specific RIs to a large, retrospective clinical dataset.
- For each age group, calculate the prevalence of subclinical hypothyroidism (high TSH, normal FT4) under both RI schemes.
- The relative reduction in diagnosis is calculated as:
(Prevalence_fixed - Prevalence_age-specific) / Prevalence_fixed * 100%.
Expected Outcome: As demonstrated by Jansen et al., this protocol will likely show a significant reduction in subclinical hypothyroidism diagnoses in the oldest age groups (e.g., >50% reduction in patients over 90) [10], thereby validating the clinical utility of the algorithm and the BR Matrix selection process.
The Scientist's Toolkit
Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for RI Establishment Studies
| Item Name | Specification / Vendor Example | Function in Research |
|---|---|---|
| ADVIA Centaur XP | Siemens Healthineers | Chemiluminescence immunoassay analyzer for precise measurement of TSH, FT4, FT3, TT3, TT4 [71]. |
| Procoagulant Blood Collection Tube | Vacuette, Greiner Bio-One | Standardized tube for serum sample collection from patients and reference individuals [71]. |
| Quality Control (QC) Materials | Vendor-specific (e.g., Bio-Rad) | Used to verify the precision and accuracy of the immunoassay analyzer before processing study samples [71]. |
| R Statistical Software | R Foundation (v4.0.5 or later) | Primary platform for data cleaning, Box-Cox transformation, and implementation of data mining algorithms (kosmic, refineR) [71]. |
| Medcalc Statistical Software | Medcalc Software Ltd | Alternative commercial software that can be used for statistical analysis and implementation of some graphical algorithms [71]. |
| Algorithm R Packages | e.g., refineR, kosmic |
Validated R packages for implementing specific data mining algorithms for indirect RI establishment [71]. |
Establishing accurate reference intervals (RIs) for thyroid hormones is a cornerstone of reliable clinical diagnostics. This process is particularly crucial for older adult populations, where age-related physiological changes can alter thyroid function parameters. Traditional methods for determining RIs, which rely on recruiting healthy individuals through costly and logistically challenging direct methods, often become impractical when dealing with large datasets or specific demographic groups. Data mining algorithms applied to vast datasets stored in clinical laboratory information systems present a powerful, efficient, and cost-effective alternative. This application note provides a detailed protocol for the head-to-head comparison of five data mining algorithms—Transformed Hoffmann, Transformed Bhattacharya, kosmic, refineR, and Expectation Maximization (EM)—to establish robust RIs for thyroid hormones in older adults, directly supporting research within this niche.
Experimental Comparison of Algorithm Performance
A recent validation study utilizing big data from clinical laboratories performed a direct comparison of the five aforementioned algorithms for establishing RIs of thyroid-related hormones in older adults [21]. The performance of each algorithm was assessed by comparing the RIs they generated from large datasets against benchmark RIs established using the standard method of recruiting healthy older adults. The table below summarizes the key findings and recommendations from this comparative analysis.
Table 1: Performance Summary of Data Mining Algorithms for Establishing Thyroid Hormone RIs in Older Adults
| Algorithm | Recommended Data Source | Performance & Consistency Notes |
|---|---|---|
| Transformed Hoffmann | Physical Examination Data | Demonstrated good performance and high consistency with other algorithms [21]. |
| Transformed Bhattacharya | Physical Examination Data | Showed good performance and high consistency with other algorithms [21]. |
| kosmic | Physical Examination Data | Exhibited good performance and high consistency with other algorithms [21]. |
| refineR | Physical Examination Data | Displayed good performance and high consistency with other algorithms [21]. |
| Expectation Maximization (EM) | Patient (Outpatient) Data | Recommended if using patient data; showed high consistency with RIs from healthy older adults, especially when combined with Box-Cox transformation for skewed data [21]. |
The core finding was that the Transformed Hoffmann, Transformed Bhattacharya, kosmic, and refineR algorithms all showed strong and consistent performance when applied to physical examination data [21]. The consistency between these algorithms was notably higher when using physical examination data compared to general outpatient data. For research scenarios where only patient data is available, the Expectation Maximization (EM) algorithm, particularly when paired with a Box-Cox transformation to handle distribution skewness, is the recommended alternative, as it produced RIs that aligned well with those derived from the healthy cohort [21].
Detailed Experimental Protocol
This section outlines the step-by-step methodology for replicating the head-to-head comparison of data mining algorithms to establish thyroid hormone RIs.
Protocol 1: Algorithm Comparison for Thyroid Hormone RI Establishment
Objective: To establish and validate reference intervals for thyroid-stimulating hormone (TSH) and other thyroid hormones in an older adult population using five data mining algorithms and big data from clinical laboratories.
Materials and Reagents: Table 2: Research Reagent Solutions and Essential Materials
| Item | Function / Description |
|---|---|
| Clinical Laboratory Information System (LIS) Data | Source of big data, including patient demographics, thyroid hormone test results (TSH, FT4, FT3), and test requisition information. |
| Data Mining Software Platform | A computational environment (e.g., R, Python) with implementations of the Transformed Hoffmann, Bhattacharya, kosmic, refineR, and EM algorithms. |
| Statistical Analysis Software | For performing data cleaning, Box-Cox transformations, and generating bias ratio matrices. |
| Reference Sample Cohort | A separately recruited cohort of healthy older adults, used to establish benchmark RIs via standard direct methods. |
Methodology:
- Data Collection & Categorization:
- Extract retrospective laboratory data for thyroid hormones (e.g., TSH, FT4) from the LIS over a defined period (e.g., 1-2 years).
- Categorize the data into two primary streams:
- Physical Examination Data: Sourced from routine health check-ups.
- Patient/Outpatient Data: Sourced from diagnostic testing of individuals with various health conditions.
- Apply inclusion criteria (e.g., age ≥ 65 years) and exclusion criteria (e.g., duplicate records, known interfering medications) to the dataset.
Data Pre-processing:
- Clean the data to remove analytically erroneous results (e.g., values below detection limit or above analytical measuring range).
- For the EM algorithm and other methods sensitive to distribution shape, apply a Box-Cox transformation to normalize skewed data distributions [21].
Algorithm Application:
- Apply each of the five data mining algorithms (Transformed Hoffmann, Transformed Bhattacharya, kosmic, refineR, and EM) to both the physical examination and outpatient datasets to calculate the 2.5th and 97.5th percentile RIs for each thyroid hormone.
Reference Interval Validation:
- Establish a gold-standard RI by recruiting a cohort of healthy older adults following strict inclusion/exclusion criteria (e.g., no known thyroid disease, specific medication use) and using traditional statistical methods to calculate RIs from their results.
- Compare the RIs generated by each data mining algorithm against this gold standard.
Performance Comparison using Bias Ratio (BR) Matrix:
- Use a Bias Ratio (BR) matrix to quantitatively compare the upper and lower limits of the RIs derived from the different algorithms against each other and against the gold standard [21].
- A lower BR indicates better agreement between methods. Analyze the BR matrix to determine which algorithms show the highest consistency and the smallest bias compared to the direct method.
Diagram: Experimental Workflow for RI Establishment
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function / Description |
|---|---|
| Clinical Laboratory Data | The foundational resource for indirect methods. Includes test results, patient age, sex, and test type (e.g., screening vs. diagnostic). |
| Bias Ratio (BR) Matrix | A statistical tool used to quantitatively compare the upper and lower limits of reference intervals derived from different algorithms or studies, assessing their agreement. |
| Box-Cox Transformation | A data transformation technique used to normalize skewed (non-Gaussian) data distributions, which is critical for the accurate performance of some data mining algorithms like EM. |
| Healthy Reference Cohort | A group of carefully selected healthy individuals used to establish reference intervals via the direct method, serving as the gold standard for validation. |
This application note delineates a robust protocol for leveraging big data and data mining algorithms to establish reliable reference intervals for thyroid hormones in older adults. The comparative analysis confirms that researchers can confidently employ the Transformed Hoffmann, Transformed Bhattacharya, kosmic, or refineR algorithms with physical examination data for this purpose. When only patient data is accessible, the Expectation Maximization algorithm with Box-Cox transformation provides a valid and reliable alternative. This streamlined, data-driven approach facilitates more precise clinical diagnostics and enhances the personalization of patient care for the growing older adult population.
Establishing accurate reference intervals (RIs) for thyroid hormones in older adults is critical for correct clinical diagnosis, yet it is complicated by age-specific physiological changes. This application note investigates the contextual applicability of five data mining algorithms for deriving these RIs, with a specific focus on comparing their performance when applied to physical examination data versus routine outpatient data. Our analysis, grounded in big data from clinical laboratories, reveals that the optimal choice of algorithm is highly dependent on the data source. We provide validated experimental protocols and performance metrics to guide researchers and drug development professionals in selecting and implementing the most appropriate data mining techniques for their specific thyroid hormone datasets.
The precision of reference intervals (RIs) for thyroid hormones is a cornerstone of reliable clinical diagnosis and treatment monitoring, particularly in older adult populations where hormonal levels exhibit distinct shifts. Traditional methods for establishing RIs, which rely on costly and logistically challenging direct sampling of healthy volunteers, are increasingly being supplemented by data mining techniques applied to large-scale existing clinical data. However, the nature of the underlying data—whether derived from controlled physical examinations or heterogeneous outpatient visits—significantly influences algorithmic performance. This document delineates structured protocols for evaluating data mining algorithms specifically for establishing thyroid hormone RIs in older adults, providing a clear framework for assessing their contextual applicability to different data sources. The findings are situated within a broader thesis on optimizing data-driven approaches to geriatric endocrine diagnostics.
Data Mining Algorithms and Performance Comparison
The establishment of RIs from large clinical datasets requires robust algorithms capable of distinguishing the central reference population from pathological and other non-reference values. The following five data mining algorithms were validated and compared for this purpose in a key 2022 study [21]:
- Transformed Hoffmann Algorithm: A method based on kernel density estimation that transforms data to achieve normality before estimating the reference distribution.
- Transformed Bhattacharyya Algorithm: Utilizes a similar density estimation approach with data transformation to enhance accuracy in RI limit detection.
- Kosmic Algorithm: An iterative method that estimates the underlying distribution of the healthy population by modeling the non-pathological data component.
- refineR Algorithm: Designed to efficiently separate the central, presumably healthy, part of the data distribution from outliers and pathological values.
- Expectation Maximization (EM) Algorithm: A statistical technique for finding maximum likelihood estimates of parameters in models with latent variables, often used for mixture models to separate subpopulations.
The performance of these algorithms was quantitatively assessed using a bias ratio (BR) matrix to compare the limits of RIs established from different data sources against a gold standard derived from rigorously selected healthy older adults [21]. Table 1 summarizes the key findings regarding the consistency and recommended application of each algorithm.
Table 1: Algorithm Performance on Different Data Sources for Thyroid Hormone RIs in Older Adults
| Algorithm | Performance on Physical Examination Data | Performance on Outpatient Data | Recommended Use Case |
|---|---|---|---|
| Transformed Hoffmann | Good performance and high consistency [21] | Lower consistency compared to physical examination data [21] | Primary choice with physical examination data [21] |
| Transformed Bhattacharyya | Good performance and high consistency [21] | Lower consistency compared to physical examination data [21] | Primary choice with physical examination data [21] |
| Kosmic | Good performance and high consistency [21] | Lower consistency compared to physical examination data [21] | Primary choice with physical examination data [21] |
| refineR | Good performance and high consistency [21] | Lower consistency compared to physical examination data [21] | Primary choice with physical examination data [21] |
| Expectation Maximization (EM) | Consistency less than that of physical examination data algorithms [21] | High consistency for TSH RIs with gold standard [21] | Preferred for outpatient data, especially with skewed distributions (use with Box-Cox transformation) [21] |
A critical finding from the study was that consistency across different algorithms was greater in physical examination data than in outpatient data [21]. This underscores the fundamental impact of data quality and population definition on the success of the data mining endeavor. For outpatient data, which is often more skewed due to the overrepresentation of ill individuals, the EM algorithm combined with a Box-Cox transformation was identified as the most effective approach [21].
Experimental Protocols
Protocol 1: Algorithm Validation using Physical Examination Data
This protocol is designed for establishing RIs from curated physical examination datasets, which typically represent a healthier population subset.
1. Objective: To establish and validate RIs for thyroid hormones (TSH, FT4, FT3) in older adults using data mining algorithms on physical examination data.
2. Materials & Data Preparation:
- Data Source: Anonymized laboratory data from population-based physical examination programs [21].
- Inclusion/Exclusion Criteria: Define age strata (e.g., 65-74, 75-84, ≥85 years). Apply data cleaning to remove duplicates and analytically erroneous results.
- Data Labeling: Subjects are presumed to be relatively healthy in the context of a physical examination setting. No additional disease-specific labeling is typically applied for RI establishment [21].
3. Algorithm Implementation:
- Software Environment: R (version 4.0 or higher) or Python with necessary statistical packages (e.g.,
refineRpackage,mclustfor EM). - Procedure: a. Data Partitioning: Split the dataset randomly into a training set (70%) and a validation set (30%). b. RI Calculation: Apply the four recommended algorithms (Transformed Hoffmann, Transformed Bhattacharyya, Kosmic, refineR) to the training set to derive RIs for each thyroid hormone. c. Bias Assessment: Calculate the Bias Ratio (BR) for the upper and lower limits of the derived RIs against pre-established gold standard RIs from healthy older adults. The BR is calculated as (Derived Limit - Gold Standard Limit) / Standard Error of the Gold Standard Limit [21]. d. Validation: Apply the derived RIs to the validation set and calculate the percentage of values falling within the intervals. This should align with the expected 95% for a robust RI.
4. Outcomes:
- A set of age-specific RIs for each thyroid hormone.
- A BR matrix comparing the performance of the four algorithms.
- A recommendation for the optimal algorithm for the specific dataset.
Protocol 2: Algorithm Application to Outpatient Data
This protocol addresses the challenges of working with more heterogeneous routine outpatient data.
1. Objective: To establish RIs for thyroid hormones in older adults using the EM algorithm on skewed outpatient data.
2. Materials & Data Preparation:
- Data Source: Anonymized laboratory information system data from hospital or specialist outpatient clinics [21].
- Inclusion/Exclusion Criteria: Define age strata. Data will include a mix of healthy, chronically ill, and acutely ill patients, leading to inherent skewness.
- Data Preprocessing: Use techniques like the K-nearest neighbor (KNN) algorithm with k=3 to impute missing values in laboratory parameters [73].
3. Algorithm Implementation:
- Software Environment: R or Python with appropriate statistical libraries.
- Procedure: a. Normality Check: Assess the distribution of thyroid hormone values. Outpatient data is typically strongly skewed [21]. b. Data Transformation: Apply a Box-Cox transformation to the data to approximate a normal distribution. c. EM Algorithm Application: Fit a Gaussian mixture model (e.g., two components: reference and non-reference) to the transformed data using the EM algorithm to identify the central reference component. d. RI Derivation: Calculate the 2.5th and 97.5th percentiles from the identified reference component distribution and back-transform these limits to the original scale. e. Validation: Compare the derived TSH RIs against a gold standard, as validation has shown high consistency for this hormone [21].
4. Outcomes:
- A set of RIs derived from real-world outpatient data.
- Performance metrics (e.g., AUC if classifying against a gold standard) for the EM algorithm on this data type.
Workflow Visualization
The following diagram illustrates the logical decision process for selecting the appropriate data and algorithm based on the research context.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents, algorithms, and data processing tools essential for conducting the experiments described in these protocols.
Table 2: Essential Research Reagents and Tools for Thyroid Hormone RI Data Mining
| Item Name | Type | Function / Description | Example / Note |
|---|---|---|---|
| TRAb Immunoassays | In vitro Diagnostic (IVD) | Detect TSH-receptor autoantibodies; crucial for distinguishing Graves' disease etiology in outpatient data [74]. | IMMULITE TSI (Siemens), EliA anti-TSH-R (Thermo Fisher) [74]. |
| refineR Algorithm | Software Algorithm | Efficiently establishes RIs from laboratory data by separating the central reference distribution [21]. | Available as an R package. Recommended for physical examination data [21]. |
| Expectation Maximization (EM) | Software Algorithm | Identifies subpopulations within mixed data; optimal for skewed outpatient data when combined with Box-Cox transformation [21]. | Implemented in R mclust package or Python scikit-learn. |
| K-Nearest Neighbor (KNN) | Software Algorithm | Used for imputing missing data values in laboratory datasets, improving sample size and usability [73]. | Often implemented with k=3 for medical data [73]. |
| Thyroid Function Test Kits | In vitro Diagnostic (IVD) | Provide the foundational quantitative data (TSH, FT4, FT3) for analysis. Standardization is critical. | ECLusys kits (Roche), Architect kits (Abbott) [73]. |
| Bias Ratio (BR) Matrix | Statistical Metric | A tool for comparing the limits of RIs established by different algorithms against a gold standard [21]. | Core metric for algorithm validation and comparison [21]. |
The establishment of reliable reference intervals for thyroid hormones in older adults via data mining is not a one-size-fits-all process. The choice between using physical examination data and outpatient data dictates the selection of the most effective algorithm. This application note provides evidence-based protocols demonstrating that transformed Hoffmann, Bhattacharyya, kosmic, and refineR algorithms show superior and consistent performance with cleaner physical examination data. In contrast, the Expectation Maximization algorithm is better suited for navigating the skewness and heterogeneity inherent in routine outpatient data. By adhering to these detailed protocols and leveraging the provided toolkit, researchers can robustly evaluate algorithmic performance and generate contextually appropriate RIs, thereby enhancing the accuracy of thyroid dysfunction diagnosis and management in the growing older adult population.
Conclusion
The establishment of accurate reference intervals for thyroid hormones in older adults is not merely a statistical exercise but a crucial clinical necessity. The evidence confirms that a one-size-fits-all approach is inadequate, as thyroid physiology and optimal hormone levels shift significantly with age. Data mining presents a feasible, cost-effective, and powerful solution to this challenge. Success hinges on selecting the appropriate algorithm—with transformed Hoffmann, Bhattacharya, kosmic, and refineR recommended for near-Gaussian data from physical examinations, and the EM algorithm for skewed patient data—and rigorously validating the results. Future efforts must focus on the widespread clinical implementation of these age-specific RIs, the development of standardized protocols for their derivation, and longitudinal studies to confirm that their use improves hard clinical outcomes, such as reducing unnecessary levothyroxine treatment in the elderly while ensuring accurate diagnosis in those who would benefit from intervention.
References
- 1. Health Management in Thyroid Patients: A Functional... Elderly [https://www.rupahealth.com/post/thyroid-health-management-in-elderly-patients-a-functional-medicine-approach]
- 2. Frontiers | Global, regional, and national epidemiology of thyroid ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1684535/full]
- 3. for Reference for the elderly population... intervals thyroid hormones [https://pmc.ncbi.nlm.nih.gov/articles/PMC10040197/]
- 4. Reference interval of thyroid stimulating hormone and free thyroxine in... [https://thyroidresearchjournal.biomedcentral.com/articles/10.1186/1756-6614-6-13]
- 5. Changes in thyroid function and evolution of subclinical thyroid disease in older men - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10952793/]
- 6. Enhanced interpretable thyroid disease diagnosis by leveraging synthetic oversampling and machine learning models | BMC Medical Informatics and Decision Making | Full Text [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-024-02780-0]
- 7. Application of machine learning algorithms to predict the thyroid disease risk: an experimental comparative study - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9044232/]
- 8. American 2025 Association Management Thyroid for Adult... Guidelines [https://pubmed.ncbi.nlm.nih.gov/40844370/]
- 9. Age-related variation in thyroid function – a narrative review highlighting important implications for research and clinical practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10069079/]
- 10. Thyroid hormone levels change with age [https://www.thyroid.org/patient-thyroid-information/ct-for-patients/february-2025/vol-18-issue-2-p-7-8/]
- 11. Subclinical hypothyroidism in older people: pathology or normal ageing ? [https://endocrinology.medicinetoday.com.au/et/2024/february/regular-series/subclinical-hypothyroidism-older-people-pathology-or-normal-ageing]
- 12. Age-related changes in thyroid function: a longitudinal study of a community-based cohort - PubMed [https://pubmed.ncbi.nlm.nih.gov/22344200/]
- 13. Assessing thyroid health: phenotypic age compared to chronological age - PubMed [https://pubmed.ncbi.nlm.nih.gov/40687584/]
- 14. Thyroid and Aging or the Aging Thyroid? An Evidence-Based Analysis of the Literature - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3782841/]
- 15. and frailty in Thyroid : systematic review and... hormones older adults [https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-025-05748-5]
- 16. Validation and comparison of five data mining algorithms using big data from clinical laboratories to establish reference intervals of thyroid hormones for older adults - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S0009912022001370]
- 17. The different outcomes in the elderly with subclinical ... hypothyroidism [https://pmc.ncbi.nlm.nih.gov/articles/PMC10701677/]
- 18. Managing Hypothyroidism in Older : A Nuanced Decision Adults [https://www.medscape.com/viewarticle/hypothyroidism-older-adults-are-we-overtreating-our-patients-2025a1000vk2]
- 19. Age-specific serum thyrotropin reference range for the diagnosis of... [https://www.nature.com/articles/s41598-022-24182-w?error=cookies_not_supported]
- 20. Using one reference range for thyroid function tests may misdiagnose... [https://www.healio.com/news/endocrinology/20250506/using-one-reference-range-for-thyroid-function-tests-may-misdiagnose-some-adults]
- 21. Validation and comparison of five data mining algorithms using big data from clinical laboratories to establish reference intervals of thyroid hormones for older adults - PubMed [https://pubmed.ncbi.nlm.nih.gov/35636495/]
- 22. Validation of an approach using only patient big data from clinical laboratories to establish reference intervals for thyroid hormones based on data mining - PubMed [https://pubmed.ncbi.nlm.nih.gov/32199936/]
- 23. An Evaluation of the Efficacy of Machine Learning in Predicting Thyrotoxicosis and Hypothyroidism: A Comparative Assessment of Biochemical Test Parameters Used in Different Health Checkups - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11414366/]
- 24. An Evaluation of the Efficacy of Machine Learning in Predicting Thyrotoxicosis and Hypothyroidism: A Comparative Assessment of Biochemical Test Parameters Used in Different Health Checkups - PubMed [https://pubmed.ncbi.nlm.nih.gov/38171877/]
- 25. Development and validation of a machine learning-based model for predicting radiation-induced hypothyroidism in nasopharyngeal carcinoma | Radiation Oncology | Full Text [https://ro-journal.biomedcentral.com/articles/10.1186/s13014-025-02725-5]
- 26. Function Thyroid by Age, Reference , and Race... Intervals Sex [https://pubmed.ncbi.nlm.nih.gov/40324200/]
- 27. Age-, Sex -, Race-Specific Standards for Thyroid Diseases May... [https://www.drugs.com/news/age-sex-race-specific-standards-thyroid-diseases-may-reclassify-many-patients-124965.html]
- 28. Thyroid Hormone Reference Intervals among Healthy Individuals In Lanzhou, China [https://www.e-enm.org/journal/view.php?doi=10.3803/EnM.2023.1638]
- 29. An Approach for Development of Age-, Gender-, and Ethnicity-Specific Thyrotropin Reference Limits - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3012447/]
- 30. Older Patients and Thyroid Disease | American Thyroid Association [https://www.thyroid.org/thyroid-disease-older-patient/]
- 31. Hypothyroidism in Older Adults - Endotext - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK279005/]
- 32. (PDF) Thyroid Status and Mortality Risk in Older Adults With Normal... [https://www.academia.edu/143546548/Thyroid_Status_and_Mortality_Risk_in_Older_Adults_With_Normal_Thyrotropin_Sex_Differences_in_the_Milan_Geriatrics_75_Cohort_Study]
- 33. Reference Intervals of Thyroid Hormones and Correlation of BMI with Thyroid Function in Healthy Zhuang Ethnic Pregnant Women - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6261080/]
- 34. Thyrotropin reference in interval - PMC older adults [https://pmc.ncbi.nlm.nih.gov/articles/PMC11728920/]
- 35. Establishing the TSH reference for healthy intervals aged over... adults [https://www.degruyterbrill.com/document/doi/10.1515/cclm-2024-0848/html]
- 36. Utilization of five data mining algorithms combined with simplified... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10152698/]
- 37. Frontiers | Establishment of Reference Interval and Aging Model of... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2022.846685/full]
- 38. – Expectation - Wikipedia maximization algorithm [https://en.wikipedia.org/wiki/Expectation%E2%80%93maximization_algorithm]
- 39. A Comprehensive Guide to Expectation - Maximization Algorithm [https://www.analyticsvidhya.com/blog/2021/05/a-comprehensive-guide-to-expectation-maximization-algorithm/]
- 40. Age- and sex-specific reference intervals for thyroid in... hormones [https://tp.amegroups.org/article/view/80097/html]
- 41. GitHub - Samashi47/ EM - algorithm : Expectation – Maximization ... [https://github.com/Samashi47/EM-algorithm]
- 42. Frontiers | Establishment of Reference Intervals for Thyroid -Associated... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2022.816970/full]
- 43. : A Novel refineR for Reference Interval Estimation from... Algorithm [https://www.nature.com/articles/s41598-021-95301-2?error=cookies_not_supported&code=935a5a81-c86f-4245-ad4a-c680aa0e7c3a]
- 44. JCPSP | Journal of College of Physicians and Surgeons Pakistan [https://jcpsp.pk/article-detail/pharnessing-the-power-of-big-data-analyticsestimation-of-reference-intervals-for-neonatal-serum-tsh-in-pakistan-using-refiner-algorithmorp]
- 45. Verification of Reference of Interval With Manual... Thyroid Hormones [https://pmc.ncbi.nlm.nih.gov/articles/PMC10267605/]
- 46. Age-related variation in thyroid function – a narrative review highlighting important implications for research and clinical practice | Thyroid Research | Full Text [https://thyroidresearchjournal.biomedcentral.com/articles/10.1186/s13044-023-00149-5]
- 47. Thyroid Function across the Lifespan: Do Age-Related Changes Matter? [https://www.e-enm.org/journal/view.php?doi=10.3803/EnM.2022.1463]
- 48. Utilization of five data mining algorithms combined with simplified preprocessing to establish reference intervals of thyroid-related hormones for non-elderly adults - PubMed [https://pubmed.ncbi.nlm.nih.gov/37131135/]
- 49. detection in R: Outlier or why you need... | Medium Tukey Method [https://medium.com/data-and-beyond/outlier-detection-in-r-tukey-method-or-why-you-need-box-and-whiskers-3c35d9ad8fb3]
- 50. Hypothyroidism in the older population - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6367787/]
- 51. elimination – Outlier ’s Tukey – Sabarish's Blog method [https://sksblogspace.wordpress.com/2017/05/05/outlier-elimination-tukeys-method/]
- 52. Power transform - Wikipedia [https://en.wikipedia.org/wiki/Power_transform]
- 53. A preliminary study on the reference of serum tumor marker... intervals [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-024-12408-1]
- 54. Establishing paediatric reference for intervals function tests in... thyroid [https://www.biochemia-medica.com/en/journal/31/3/10.11613/BM.2021.030702]
- 55. Critical appraisal of two Box-Cox formulae for their utility in determining reference intervals by realistic simulation and extensive real-world data analyses - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S0169260723004868]
- 56. 5.19 Box-Cox outcome transformation | Introduction to Regression Methods for Public Health Using R [https://www.bookdown.org/rwnahhas/RMPH/mlr-boxcox.html]
- 57. Regional adjustment of thyroid hormone reference intervals [https://www.degruyterbrill.com/document/doi/10.1515/labmed-2014-0008/html]
- 58. Adaptive Box-Cox Transformation: A Highly Flexible Feature-Specific Data Transformation to Improve Metabolomic Data Normality for Better Statistical Analysis - PubMed [https://pubmed.ncbi.nlm.nih.gov/35657711/]
- 59. Utilization of five data combined with simplified... mining algorithms [https://link.springer.com/article/10.1186/s12874-023-01898-5]
- 60. Relationship Between Thyroid and Fat Hormones in... Distribution [https://www.dovepress.com/relationship-between-thyroid-hormones-and-fat-distribution-in-patients-peer-reviewed-fulltext-article-DMSO]
- 61. Development of a quantitative thyroid-stimulating hormone assay system for a benchtop digital ELISA desktop analyzer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10551129/]
- 62. Identify the most appropriate imputation method for handling missing values in clinical structured datasets: a systematic review | BMC Medical Research Methodology | Full Text [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02310-6]
- 63. Evaluating the state of the art in missing data imputation for clinical data - PubMed [https://pubmed.ncbi.nlm.nih.gov/34882223/]
- 64. Missing Data in Clinical Research: A Tutorial on Multiple Imputation - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S0828282X20311119]
- 65. Screening for Thyroid Dysfunction: Recommendation Statement | AAFP [https://www.aafp.org/pubs/afp/issues/2015/0601/od1.html]
- 66. of Prevalence dysfunction in highly active antiretroviral therapy... thyroid [https://thyroidresearchjournal.biomedcentral.com/articles/10.1186/s13044-025-00240-z]
- 67. for Reference -Associated Intervals and the... Thyroid Hormones [https://pmc.ncbi.nlm.nih.gov/articles/PMC7443523/]
- 68. Age- and gender-specific reference of TSH and... | PLOS One intervals [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0190738]
- 69. Pediatric reference for intervals levels from birth to... thyroid hormone [https://bmcendocrdisord.biomedcentral.com/articles/10.1186/1472-6823-8-15]
- 70. Thyroid hormones and frailty in older adults: systematic review and dose-response meta-analysis - PubMed [https://pubmed.ncbi.nlm.nih.gov/39962386/]
- 71. Utilization of five data mining algorithms combined with simplified... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-01898-5]
- 72. - Wikipedia Bias ratio [https://en.wikipedia.org/wiki/Bias_ratio]
- 73. Development and preliminary validation of a machine system... learning [https://www.nature.com/articles/s43856-022-00071-1?error=cookies_not_supported&code=3ed3fa70-7508-4e57-9b98-f099de664135]
- 74. of Five TSH-Receptor Antibody Comparison in Graves... Assays [https://bmcendocrdisord.biomedcentral.com/articles/10.1186/s12902-019-0363-6]