Endocrine-Disrupting Chemicals and Reproductive Health: Mechanistic Insights, Research Methodologies, and Therapeutic Implications for Infertility and Cancer
This comprehensive review synthesizes current evidence on the impact of endocrine-disrupting chemicals (EDCs) on infertility and reproductive cancers for researchers and drug development professionals.
Endocrine-Disrupting Chemicals and Reproductive Health: Mechanistic Insights, Research Methodologies, and Therapeutic Implications for Infertility and Cancer
Abstract
This comprehensive review synthesizes current evidence on the impact of endocrine-disrupting chemicals (EDCs) on infertility and reproductive cancers for researchers and drug development professionals. It explores the foundational mechanisms by which EDCs like bisphenol A, phthalates, and pesticides disrupt hormonal homeostasis and epigenetic regulation, leading to impaired fertility and carcinogenesis. The article evaluates advanced methodological approaches for studying EDC effects, addresses key challenges in risk assessment including low-dose and mixture effects, and validates findings through comparative analysis of epidemiological and experimental data. By integrating mechanistic insights with clinical implications, this review aims to inform the development of targeted diagnostic biomarkers and novel therapeutic interventions.
Unraveling the Mechanisms: How EDCs Disrupt Reproductive Biology and Promote Carcinogenesis
Endocrine-disrupting chemicals (EDCs) represent a class of exogenous substances that interfere with hormonal signaling pathways, posing a significant threat to global public health. The pervasive presence of these chemicals in modern environments has coincided with concerning trends in reproductive health and hormone-sensitive cancers. This whitepaper synthesizes current epidemiological evidence and mechanistic insights linking EDC exposure with rising rates of infertility and hormone-sensitive cancers, particularly breast and ovarian malignancies. Within the broader thesis on EDC impacts, this analysis demonstrates how these chemicals create a dual burden on reproductive and oncological health through shared molecular pathways, highlighting an urgent need for targeted research and evidence-based regulatory interventions.
Epidemiological Evidence: Quantitative Associations Between EDCs and Disease Outcomes
Global Trends in Female Infertility and EDC Exposure
Table 1: Association Between EDC Metabolites and Female Infertility (NHANES 2001-2006) [1]
| EDC Metabolite Category | Specific EDCs | Odds Ratio (OR) | 95% Confidence Interval | Study Population |
|---|---|---|---|---|
| Phthalates | DnBP | 2.10 | 1.59–2.48 | 3,982 women (463 infertile) |
| Phthalates | DEHP | 1.36 | 1.05–1.79 | 3,982 women (463 infertile) |
| Phthalates | DiNP | 1.62 | 1.31–1.97 | 3,982 women (463 infertile) |
| Phthalates | DEHTP | 1.43 | 1.22–1.78 | 3,982 women (463 infertile) |
| Phthalates | PAEs | 1.43 | 1.26–1.75 | 3,982 women (463 infertile) |
| Phytoestrogens | Equol | 1.41 | 1.17–2.35 | 3,982 women (463 infertile) |
| PFAS | PFOA | 1.34 | 1.15–2.67 | 3,982 women (463 infertile) |
| PFAS | PFUA | 1.58 | 1.08–2.03 | 3,982 women (463 infertile) |
A large-scale cross-sectional study utilizing the National Health and Nutrition Examination Survey (NHANES) database demonstrated significant associations between multiple EDC metabolites and female infertility. The research encompassed 3,982 reproductive-age women, including 463 with infertility, and revealed that increased exposure to various EDCs substantially elevated infertility risk. Subgroup analyses further indicated that advanced age and elevated body mass index may exacerbate susceptibility to EDC-related infertility, suggesting potential synergistic effects between metabolic factors and chemical exposures [1].
The global decline in fertility rates parallels increasing environmental EDC contamination. Recent analyses indicate that female reproductive disorders have risen significantly over the past five decades, with EDC exposure identified as a contributing factor. Specific trends include earlier pubertal onset, with modern girls entering breast development and menarche substantially earlier than previous generations, potentially increasing lifelong susceptibility to hormone-sensitive conditions [2].
EDCs and Hormone-Sensitive Cancers: Incidence Patterns
Table 2: EDC Associations with Female-Specific Cancers and Reproductive Outcomes [3] [4] [5]
| Health Outcome | Associated EDCs | Effect Size/Risk Increase | Evidence Source |
|---|---|---|---|
| Early-onset Breast Cancer | PCBs, PFAS, BPXs, Phthalates, Dioxins | Rising incidence in specific geographic clusters | Observational Studies |
| Ovarian Cancer | Infertility alone (no drugs) | OR: 1.35 (95% CI: 0.92–1.97) | Meta-analysis (25 studies) |
| Ovarian Cancer | Infertility drug use | OR: 1.93 (95% CI: 0.94–2.46) | Meta-analysis (25 studies) |
| Borderline Ovarian Tumors | IVF, clomiphene, human menopausal gonadotropin | OR: 1.87 (95% CI: 1.18–2.97) | Umbrella Meta-analysis |
| Premature Menopause | Pesticides, phthalates | 1.9–3.8 years earlier onset | Epidemiological Review |
| Polycystic Ovary Syndrome (PCOS) | Organochlorines, PFAS | Up to 20% prevalence in high-exposure regions | Epidemiological Studies |
Recent decades have witnessed a concerning rise in hormone-sensitive breast cancers, particularly estrogen receptor-positive (ER+) phenotypes, with an alarming increase in early-onset cases occurring in women under 50 without family history. Traditional risk factors including genetic predisposition, reproductive history, and lifestyle factors cannot fully explain these epidemiological shifts, suggesting environmental contributions [4].
Geospatial analyses reveal striking patterns in cancer distribution. Early-onset breast cancer incidence shows significant geographic disparities across the United States, with the Northeast region exhibiting the highest absolute incidence rates and significant upward trends over time. These high-incidence regions demonstrate striking overlap with areas characterized by industrial legacy pollution, PFAS contamination, and urban density. The geographic distribution of EPA Superfund sites, contaminated with PCBs, dioxins, and heavy metals, closely mirrors the geographical incidence patterns of early-onset breast cancers [4].
Mechanistic Insights: EDC Disruption of Reproductive and Oncological Pathways
Molecular Mechanisms of Endocrine Disruption
EDCs employ diverse mechanisms to disrupt physiological hormone function. The Endocrine Society has delineated ten key characteristics (KCs) of EDCs, including their ability to: (KC1) interact with or activate hormone receptors; (KC2) antagonize hormone receptors; (KC3) alter hormone receptor expression; (KC4) alter signal transduction in hormone-responsive cells; (KC5) induce epigenetic modifications; (KC6) alter hormone synthesis; (KC7) alter hormone transport; (KC8) alter hormone distribution or circulating levels; (KC9) alter hormone metabolism or clearance; and (KC10) alter the fate of hormone-producing or hormone-responsive cells [3].
These disruptions exhibit complex dose-response relationships. Unlike traditional toxicants, EDCs can produce biphasic or non-monotonic dose-response curves (NMDRs), where effects may not occur at the highest concentrations but manifest at lower exposure levels. This nonlinearity complicates risk assessment and establishes that adverse effects may occur at exposures below currently accepted thresholds [3].
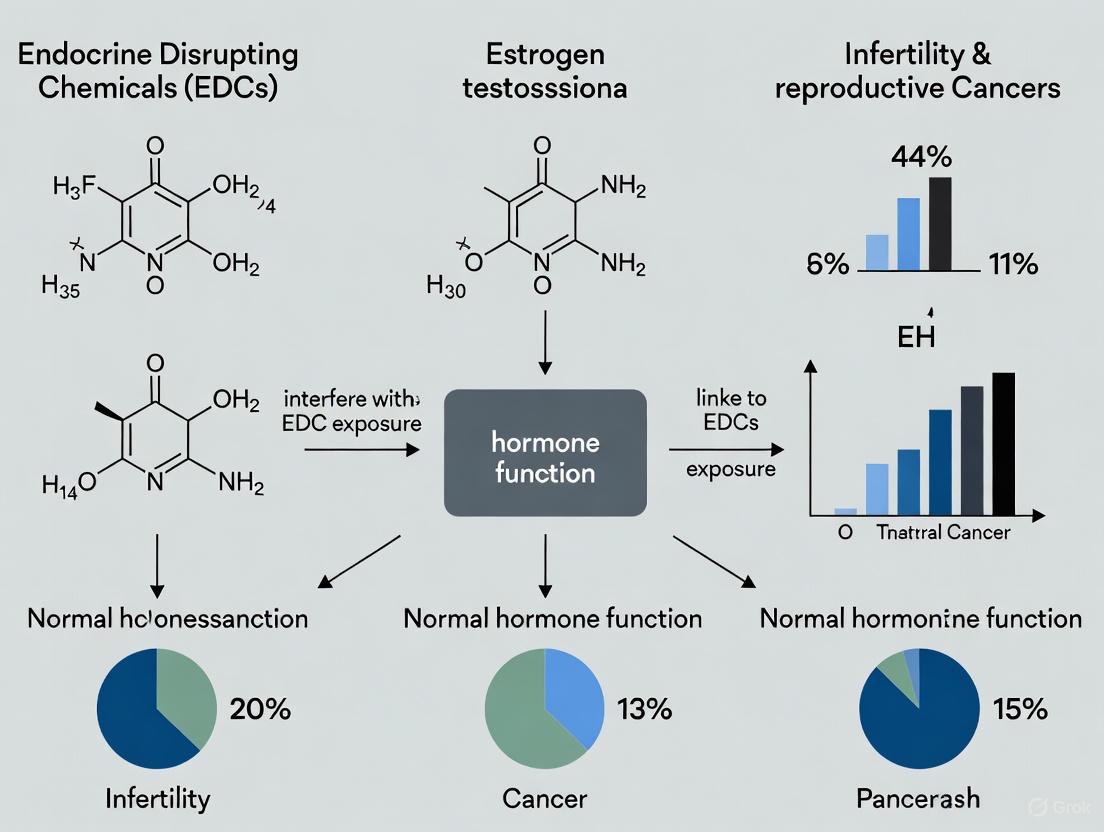
Figure 1: Integrated Pathways of EDC-Mediated Infertility and Carcinogenesis
Tissue Aging and Field Cancerization
Emerging research suggests EDCs function as accelerators of hormone-mediated tissue aging. The breast exhibits a unique aging trajectory dictated not by chronological age but by cumulative hormonal exposure. Each menstrual cycle, pregnancy, lactation period, and menopause timing contributes to hormone-driven cell proliferation, genomic stress, and epigenetic alterations. EDCs amplify this natural process by increasing cumulative hormonal load, potentially explaining the rising incidence of hormone-sensitive breast cancers among younger women [4].
The concept of "field cancerization" describes how EDC exposure remodels tissue biology before malignancy emerges. Chronic EDC exposure during developmentally susceptible windows (in utero, postnatal, peri-pubertal) can reprogram the breast epigenome, accelerate tissue-specific aging, and impair immunosurveillance mechanisms. This creates a permissive microenvironment for carcinogenesis and may explain the increasing early-onset breast cancer incidence without associated family history or genetic predisposition [4].
Methodological Approaches in EDC Research
Epidemiological Study Designs and Exposure Assessment
Table 3: Key Methodological Approaches in EDC Research [1] [6] [7]
| Method Category | Specific Approach | Application in EDC Research | Considerations |
|---|---|---|---|
| Study Designs | Cross-sectional (NHANES) | Population-level association studies | Snapshot in time, cannot establish causality |
| Cohort Studies | Longitudinal follow-up for disease incidence | Time-consuming, expensive, suitable for cumulative effects | |
| Case-Control | Compare exposure histories in cases vs controls | Susceptible to recall bias, efficient for rare outcomes | |
| Exposure Assessment | Biomonitoring (blood, urine) | Direct measurement of EDCs/metabolites | Captures recent exposure for non-persistent EDCs |
| Silicone Wristbands | Personal passive samplers for airborne EDCs | Non-invasive, captures diverse EDC classes | |
| Environmental Sampling | Air, water, dust, food contamination | Source identification, exposure route characterization | |
| Statistical Methods | Multivariate Logistic Regression | Odds ratio calculation with covariate adjustment | Controls confounding, requires careful variable selection |
| Mixture Analysis | Assess combined effects of multiple EDCs | Complex modeling, accounts for real-world exposure | |
| Subgroup Stratification | Identify vulnerable subpopulations | Reveals effect modifiers (age, BMI, ethnicity) |
Research methodologies for investigating EDC impacts have evolved to address the complexity of real-world exposure scenarios. The NHANES-based infertility study employed rigorous multivariate logistic regression adjusted for demographic, socioeconomic, lifestyle, and health-related variables including age, BMI, race, educational attainment, household income, marital status, menstrual history, smoking status, alcohol use, and history of pelvic infections, metabolic syndrome, or viral hepatitis. Sensitivity analyses excluded participants with EDC concentrations above the 99th percentile to evaluate the impact of potential outliers, confirming the robustness of the primary findings [1].
Exposure assessment technologies continue to advance. Silicone wristbands deployed as personal passive samplers have demonstrated detectable levels of EDCs across various chemical classes in nearly all samples, with organophosphate esters (OPEs) and phthalates present in 100% of samples. Crucially, extracts from these wristbands demonstrated hormonal activity in human receptor cell assays, confirming their utility in assessing biologically relevant exposures [4].
Experimental Models and Mechanistic Investigations
Figure 2: Integrated Workflow for EDC Research Methodology
Experimental approaches to elucidate EDC mechanisms include in vitro receptor binding assays, animal exposure models, and ex vivo tissue culture systems. These methodologies have demonstrated that EDCs can initiate or exacerbate cancer risks by disrupting hormone signaling and causing DNA damage. Animal studies consistently show that EDC exposure during critical developmental windows produces long-term reproductive consequences, including reduced ovarian reserve, abnormal folliculogenesis, and neuroendocrine control disruption of ovulation [4] [2].
Mechanistic investigations have revealed that persistent EDCs such as PCBs, DDT, PBDEs, organochlorine pesticides, and dioxins resist metabolic degradation and bioaccumulate in lipophilic tissues like breast fat depots. There they can remain for years or even decades, slowly releasing over time and creating prolonged endocrine disruption. Even banned substances like PCBs and DDT persist in the environment and human tissues 20-50 years after regulatory action, highlighting the persistent nature of this public health challenge [4].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for EDC Investigation [1] [3] [4]
| Research Tool Category | Specific Reagents/Materials | Research Application | Technical Function |
|---|---|---|---|
| Exposure Assessment | Silicone wristbands | Personal airborne EDC exposure monitoring | Passive sampling of volatile/semi-volatile EDCs |
| LC-MS/MS standards | Quantification of EDC metabolites | Analytical reference materials for biomonitoring | |
| Antibody-based kits (ELISA) | High-throughput EDC screening | Immunoassay detection of specific EDC classes | |
| Mechanistic Studies | Reporter gene assays (ERα, ERβ, AR) | Receptor activation profiling | Assessment of endocrine receptor pathway disruption |
| Epigenetic analysis kits | DNA methylation/histone modification | Detection of EDC-induced epigenetic alterations | |
| Primary cell cultures (ovarian granulosa, breast epithelium) | Tissue-specific response assessment | Ex vivo modeling of EDC effects on target tissues | |
| Statistical Analysis | R software with mgcv, glmmTMB | Mixture analysis and nonlinear modeling | Advanced statistical packages for complex EDC data |
| Mediation analysis macros | Pathway analysis of EDC effects | Statistical decomposition of direct/indirect effects | |
| Multiple imputation software | Handling values below detection limits | Robust approaches for left-censored exposure data |
The development of validated survey instruments represents another methodological approach to EDC research. Recent work has established reproducible questionnaires assessing reproductive health behaviors aimed at reducing EDC exposure through major routes (food, respiration, dermal absorption). Such tools enable researchers to investigate modifiable protective factors and intervention strategies across diverse populations [7].
Advanced statistical approaches for complex EDC mixture analysis continue to evolve. Methods including weighted quantile sum (WQS) regression, Bayesian kernel machine regression (BKMR), and latent variable analysis enable researchers to address the challenge of evaluating combined effects of multiple EDCs, better reflecting real-world exposure scenarios where humans encounter complex chemical mixtures rather than single compounds [6].
Knowledge Gaps and Future Research Directions
Despite substantial progress, significant knowledge gaps persist in EDC research. Current evidence relies heavily on observational studies, which face challenges related to confounding, reverse causation, and exposure misclassification. Most human studies cannot definitively establish causality between EDC exposure and disease manifestation, highlighting the need for innovative study designs that strengthen causal inference [6] [2].
Critical research priorities include better characterization of the effects of chronic low-dose EDC exposure throughout the lifespan, particularly during developmentally vulnerable windows. The potential for transgenerational effects remains inadequately explored, as does the impact of real-world chemical mixtures (the "cocktail effect"). Future studies should also focus on identifying susceptible subpopulations through advanced stratification approaches incorporating genetic, epigenetic, and metabolic biomarkers [6] [4] [2].
From a methodological perspective, developing standardized protocols for EDC assessment across matrices and establishing consensus on biomarkers of effect represent urgent needs. The integration of novel exposure assessment technologies with high-resolution health outcomes data in diverse populations will strengthen the evidence base needed to inform regulatory decision-making and public health protection [7] [2].
The accumulating epidemiological and mechanistic evidence firmly establishes EDCs as significant contributors to global trends in infertility and hormone-sensitive cancers. These chemical stressors disrupt delicate endocrine signaling through multiple pathways, with particular potency during developmental windows of susceptibility. The overlapping mechanisms underlying EDC-induced reproductive dysfunction and carcinogenesis highlight the interconnected nature of these health endpoints and suggest potential shared intervention points.
Future research addressing critical knowledge gaps—particularly regarding cumulative mixture effects, vulnerable populations, and transgenerational impacts—will strengthen the scientific foundation for evidence-based policy. As the global burden of infertility and hormone-sensitive cancers continues to rise, translational research integrating epidemiological observations with mechanistic insights offers the greatest promise for developing effective prevention strategies and mitigating the public health impact of these pervasive environmental contaminants.
Endocrine-disrupting chemicals (EDCs) represent a significant threat to human reproductive health, with growing evidence linking their exposure to rising rates of infertility and reproductive cancers. These synthetic and naturally occurring substances interfere with normal hormonal signaling pathways, predominantly through receptor-mediated mechanisms that disrupt the delicate balance of estrogenic and androgenic systems. The molecular interplay between EDCs and hormonal receptors has become a critical focus in reproductive toxicology and carcinogenesis research, providing insights into the pathogenic mechanisms underlying chemical-induced reproductive pathologies. This technical guide examines the precise molecular pathways through which EDCs disrupt estrogen and androgen signaling, with particular emphasis on implications for infertility and reproductive cancers research.
Molecular Mechanisms of Disruption
EDCs interfere with estrogen and androgen signaling through multiple interconnected mechanisms at the cellular level, primarily by mimicking or blocking endogenous hormones and altering receptor function.
Nuclear Receptor Interactions
The most extensively characterized mechanism involves direct interaction with nuclear hormone receptors. Bisphenols and phthalates demonstrate potent estrogenic agonist activity through transactivation via dimerization of both estrogen receptor alpha (ERα) and beta (ERβ). Simultaneously, these compounds exhibit androgenic antagonist activity by inhibiting dihydrotestosterone-induced transactivation through interference with androgen receptor (AR) dimerization [8]. This dual disruption creates profound imbalances in hormonal signaling critical for reproductive function.
Mechanistic Insights: At the molecular level, estrogenic EDCs compete with endogenous estradiol for binding to estrogen receptors, with their binding affinity and subsequent receptor activation potency determining the magnitude of disruption. Molecular initiating events include receptor-ligand binding, receptor dimerization, and recruitment of co-activators or co-repressors to hormone response elements on DNA [8]. The integrated assessment of these events through dimerization and transactivation assays provides a comprehensive understanding of the disruptive potential across different EDC classes.
Non-Monotonic Dose Responses
EDCs frequently exhibit non-monotonic dose-response curves (NMDRs), characterized by U-shaped or inverted U-shaped patterns rather than traditional linear dose-response relationships. This phenomenon occurs because EDCs interact with hormones and activate their receptors in a nonlinear fashion, creating complex dose-response dynamics that challenge conventional toxicological risk assessment [9]. The implications for infertility research are substantial, as low-dose exposures may produce more significant biological effects than higher concentrations, particularly during critical developmental windows.
Epigenetic Modifications
Beyond direct receptor interactions, EDCs induce heritable epigenetic modifications that can persist across generations. These include alterations in DNA methylation patterns, histone modifications, and microRNA expression that regulate gene expression without changing the underlying DNA sequence [10] [9]. The transgenerational inheritance of EDC-induced reproductive dysfunction represents a particularly concerning mechanism, with demonstrated effects on sperm quality, ovarian function, and reproductive organ development across multiple generations in animal models [10].
Quantitative Analysis of EDC Activities
The endocrine-disrupting properties of various chemical classes have been systematically quantified through integrated assessment approaches combining receptor dimerization and transactivation assays. The following tables summarize key quantitative data relevant to reproductive health research.
Table 1: Estrogenic and Androgenic Disruption Potencies of Common EDCs [8]
| Chemical Class | Specific Compound | ERα-Mediated Agonism | ERβ-Mediated Agonism | AR Antagonism | Key Findings |
|---|---|---|---|---|---|
| Bisphenols | BPA | +++ | +++ | +++ | Potent estrogenic agonist and anti-androgenic activity |
| BPS | ++ | ++ | ++ | Similar activity to BPA despite being a "substitute" | |
| BPF | ++ | ++ | ++ | Comparable disruptive profile to BPA | |
| Phthalates | DEHP | + | + | + | Demonstrates estrogenic activity and weak anti-androgenicity |
| DBP | + | + | - | Primarily estrogenic activity without significant AR antagonism | |
| BBP | + | + | + | Dual estrogenic and anti-androgenic properties | |
| Biocides | Vinclozolin | - | - | ++ | Primarily anti-androgenic through AR dimerization interference |
| p,p'-DDE | - | - | + | Weak AR dimerization mediation at high concentrations |
Table 2: Environmental Persistence and Exposure Limits of Reproductive Toxicants [10]
| Category | Substance | Environmental Persistence/Exposure | Mechanism of Reproductive Damage |
|---|---|---|---|
| Heavy Metals | Cadmium | Biological half-life: 20-30 years | Compromises blood-testis barrier; impairs sperm quality |
| Lead | Blood levels >10 μg/dL cause sperm DNA damage | Seminal accumulation (3.2 ± 0.8 μg/dL); sperm DNA damage | |
| Arsenic | Occupational exposure >0.01 mg/m³ disrupts testosterone | Metabolite DMA disrupts testosterone biosynthesis | |
| Plasticizers | Bisphenol A (BPA) | Tolerable daily intake: 50 μg/kg (US EPA) | High-affinity binding to estrogen receptors; hormonal imbalance |
| Phthalates (DEHP) | Detected in seminal plasma (0.77-1.85 μg/mL) | Reduced sperm concentration and motility | |
| Persistent Organic Pollutants | PCBs | Half-lives: 8-15 years; lipophilicity (BCF >10⁵) | Adipose tissue accumulation; sustained reproductive system effects |
| Dioxins (PCDD/Fs) | Extreme toxicity (TEF: 0.0001-1) | Severe disruption of androgen synthesis; compromised sperm development |
Table 3: Mixture Effects of Bisphenol Derivatives on Estrogen and Androgen Receptors [8]
| Chemical Combination | Effect on ER Activity | Effect on AR Activity | Implications for Risk Assessment |
|---|---|---|---|
| BPA + BPS | Additive estrogenic activity | Enhanced anti-androgenic activity | Mixtures exhibit enhanced disruption compared to individual compounds |
| BPA + BPF | Synergistic at low concentrations | Additive antagonism | Non-additive effects challenge current risk assessment models |
| Multiple phthalate combination | Potentiated estrogenic response | Variable anti-androgenic effects | Real-world exposure scenarios involve complex mixtures |
| Bisphenols + phthalates | Integrated disruptive potential | Combined receptor interference | Cumulative effects on reproductive health parameters |
Experimental Methodologies
Integrated Assessment Approach
The comprehensive evaluation of estrogenic and androgenic endocrine-disrupting properties requires an integrated methodology combining multiple assay systems to capture the full spectrum of disruptive mechanisms.
BRET-Based Receptor Dimerization Assays: Bioluminescence resonance energy transfer (BRET) technology enables real-time monitoring of receptor homodimerization (ERα, ERβ, and AR) in live cells. Test compounds are prepared as concentrated stock solutions in DMSO according to OECD Test Guideline No. 455 recommendations [8]. Cells expressing receptor fusion constructs (typically luciferase and fluorescent protein tags) are exposed to serial dilutions of EDCs, and dimerization is quantified by BRET signal following ligand addition. This approach directly measures the molecular initiating event of receptor dimerization, providing mechanistic insight into disruptive patterns.
Stably Transf Transcriptional Activation Assays: These assays measure downstream transcriptional activity following receptor activation. Cell lines (e.g., human breast cancer cells for ER, prostate cancer cells for AR) stably transfected with reporter constructs (e.g., luciferase under control of estrogen or androgen response elements) are exposed to EDCs alone (for agonist activity) or in combination with reference agonists (for antagonist activity). Following incubation (typically 16-24 hours), reporter gene activity is quantified, normalized to cell viability, and expressed relative to reference compound responses [8].
Kinetic Signaling Analysis: Time-course signaling data are analyzed using general time course equations and mechanistic model equations. Four primary curve shapes are observed: straight line, association exponential curve, rise-and-fall to zero, and rise-and-fall to steady-state [11]. The initial rate of signaling is quantified by curve-fitting to the whole time course, avoiding selection bias of the linear phase. This approach yields kτ, defining efficacy as the rate of signal generation before regulation mechanisms impact it [11].
Data Analysis Framework
Quantitative analysis of time course data utilizes curve-fitting to estimate kinetic pharmacological parameters. The four characteristic curve shapes are analyzed using corresponding equations:
- Straight line: Response = a × t
- Association exponential: Response = Plateau × (1 - e^(-K × t))
- Rise-and-fall to baseline: Response = (a/(K - k)) × (e^(-k × t) - e^(-K × t))
- Rise-and-fall to steady-state: Response = a × (e^(-k × t) - e^(-K × t)) + c [11]
This analytical framework enables quantification of signaling efficacy as the initial rate of signaling by agonist-occupied receptor (kτ), providing a biologically meaningful metric of signal transduction kinetics before regulation mechanisms introduce complexity.
Pathway Visualization
Figure 1: Molecular Pathway of Estrogenic Signaling Disruption by EDCs. EDCs mimic endogenous estrogens, binding to and activating estrogen receptors, triggering dimerization, coactivator recruitment, and altered gene transcription through estrogen response elements (EREs).
Figure 2: Molecular Pathway of Androgenic Signaling Disruption by EDCs. EDCs act as antagonists by competing with endogenous androgens like DHT, impairing receptor dimerization, promoting corepressor recruitment, and disrupting normal androgen-responsive gene transcription.
Figure 3: Integrated Experimental Workflow for Comprehensive EDC Assessment. The methodology combines dimerization assays, transactivation studies, and kinetic analysis within the Adverse Outcome Pathway framework for mechanistic risk assessment.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for EDC Signaling Studies
| Reagent/Cell Line | Application | Function in EDC Research |
|---|---|---|
| BRET-based dimerization assay systems | Receptor dimerization studies | Quantifies direct receptor-receptor interaction following EDC exposure |
| ERα/ERβ/AR transcriptional activation cell lines | Transactivation potential | Measures downstream gene expression changes from EDC-receptor interaction |
| MCF-7 (human breast adenocarcinoma) | Estrogenic activity screening | Endogenous ER expression; sensitive to estrogenic EDCs |
| MDA-MB-231 (triple-negative breast cancer) | Specific ER subtype studies | Useful for transfected receptor studies with minimal background |
| LNCaP (human prostate adenocarcinoma) | Androgenic disruption studies | Endogenous AR expression; responsive to anti-androgenic EDCs |
| CV-1 (monkey kidney fibroblast) | Transfected receptor studies | Low endogenous receptor background for clean transfection results |
| OECD reference compounds (17β-estradiol, DHT) | Assay standardization and validation | Provides benchmark responses for quantifying EDC potency |
| Li+ chloride solution | Response degradation blockade | Inhibits inositol phosphate breakdown in second messenger assays |
| Colorimetric/fluorimetric reporter gene substrates | Transactivation readout | Quantifies transcriptional activity (luciferase, SEAP, β-galactosidase) |
Implications for Reproductive Health Research
The molecular pathways of estrogenic and androgenic disruption have direct implications for understanding and addressing infertility and reproductive cancers. The receptor-mediated mechanisms described herein provide mechanistic links between EDC exposure and adverse reproductive outcomes.
In the context of infertility research, the dual disruption of both estrogen and androgen signaling explains clinical observations of reduced sperm quality, impaired oocyte maturation, and endometrial receptivity issues [10] [12]. The quantitative data on receptor activities directly correlates with epidemiological findings of declining sperm counts and increased female reproductive pathologies. Furthermore, the epigenetic modifications induced by EDC exposure provide a plausible mechanism for the transgenerational inheritance of reproductive dysfunction observed in both animal studies and human populations [9].
For reproductive cancers research, the continuous receptor activation by estrogenic EDCs and simultaneous inhibition of protective androgenic signaling creates a microenvironment conducive to cellular transformation and proliferation. The kinetic parameters of signaling disruption, particularly sustained receptor activation, mirror mechanisms employed by known carcinogens in breast, ovarian, and prostate cancer pathogenesis. The mixture effects documented in quantitative assessments reflect real-world exposure scenarios that may contribute to the increasing incidence of hormone-sensitive reproductive cancers.
The experimental methodologies and research reagents detailed in this guide provide researchers with standardized approaches for identifying and characterizing novel EDCs, screening compound libraries for endocrine activity, and developing targeted interventions to mitigate receptor-mediated disruption in susceptible populations.
Epigenetic reprogramming refers to the comprehensive erasure and re-establishment of epigenetic marks, such as DNA methylation and histone modifications, during critical developmental periods such as gametogenesis and early embryogenesis [13]. This process plays a fundamental role in regulating gene expression patterns without altering the underlying DNA sequence, serving as a key interface between environmental exposures and genomic function. Within the context of reproductive health, endocrine-disrupting chemicals (EDCs) represent a significant class of environmental exposures that can interfere with these precise epigenetic reprogramming events [14] [15]. EDCs are synthetic or natural chemicals that mimic, block, or interfere with the body's hormones, including bisphenol A (BPA), phthalates, pesticides, and polychlorinated biphenyls (PCBs) [16] [15]. A growing body of evidence indicates that exposure to EDCs, particularly during vulnerable developmental windows, can induce persistent alterations in epigenetic regulation, which in turn contribute to the pathogenesis of infertility and reproductive cancers through disrupted gene expression networks [17] [15]. This whitepaper provides an in-depth technical analysis of the core mechanisms of epigenetic reprogramming, with a specific focus on how EDC-induced disruptions manifest in transgenerational effects that impact reproductive physiology across generations.
Core Mechanisms of Epigenetic Regulation
DNA Methylation Dynamics
DNA methylation involves the covalent addition of a methyl group to the 5-carbon position of cytosine residues, primarily within CpG dinucleotides, catalyzed by DNA methyltransferases (DNMTs) [18] [13]. This epigenetic mark is dynamically regulated throughout development and plays crucial roles in genomic imprinting, X-chromosome inactivation, and transcriptional regulation.
- Molecular Machinery: The DNMT family includes maintenance methyltransferase DNMT1, which preserves methylation patterns during DNA replication, and de novo methyltransferases DNMT3A and DNMT3B, which establish new methylation patterns during development [13]. DNMT3L, a catalytically inactive cofactor, enhances the activity of DNMT3A/B. Conversely, the ten-eleven translocation (TET) family enzymes catalyze DNA demethylation through iterative oxidation of 5-methylcytosine (5mC) [13].
- Reprogramming During Germ Cell Development: The mammalian genome undergoes two waves of epigenetic reprogramming—during primordial germ cell (PGC) development and preimplantation embryogenesis [13]. In mouse PGCs, genome-wide DNA demethylation reduces 5mC levels to approximately 16.3% by embryonic day E13.5, erasing most methylation marks, including those at imprinted loci [13]. De novo methylation is subsequently established from E13.5 to E16.5, with completion by birth. Human PGCs follow a similar pattern, reaching minimal DNA methylation by weeks 10-11 of gestation [13].
Table 1: DNA Methyltransferases and Their Functions in Mammalian Systems
| Enzyme | Type | Primary Function | Consequences of Dysfunction |
|---|---|---|---|
| DNMT1 | Maintenance | Maintains methylation patterns during DNA replication; prefers hemimethylated DNA [13] | Global hypomethylation, genomic instability, spermatogenesis failure [13] |
| DNMT3A | De novo | Establishes new methylation patterns during gametogenesis and embryogenesis [13] | Embryonic lethality (in mice), imprinting disorders, aberrant methylation in spermatogonia [13] |
| DNMT3B | De novo | Works with DNMT3A to establish methylation patterns; targets specific genomic repeats [13] | ICF syndrome, centromeric instability, reduced in round spermatid arrest [13] |
| DNMT3L | Cofactor | Enhances DNMT3A/B binding and activity; essential for establishing genomic imprints [13] | Imprinting defects, impaired spermatogenesis [13] |
Histone Modifications and Chromatin Remodeling
Histone post-translational modifications represent another fundamental layer of epigenetic regulation that controls chromatin accessibility and gene expression. These modifications include methylation, acetylation, phosphorylation, and ubiquitination of specific histone residues [18] [13].
- Regulatory Complexes: Histone-modifying enzymes include histone acetyltransferases (HATs), histone deacetylases (HDACs), histone methyltransferases (HMTs), and histone demethylases (KDMs) [18]. Chromatin remodeling complexes (CRCs) such as SWI/SNF utilize ATP to nucleosomally reposition, eject, or restructure nucleosomes [13].
- Critical Roles in Spermatogenesis: The transition from histones to protamines during spermiogenesis requires extensive histone modification [13]. For example, the histone methyltransferase PRMT5 catalyzes H3R8me2 and H4R3me2, and its deficiency leads to increased H3K9me2 and H3K27me2 levels, altering the chromatin state of PLZF—a critical transcription factor for spermatogonial stem cell (SSC) self-renewal—resulting in SSC developmental defects [13]. Similarly, Suv39h null mice exhibit spermatogenic failure with nonhomologous chromosome associations [13].
Table 2: Key Histone-Modifying Enzymes in Reproductive Tissue Function
| Enzyme/Complex | Modification Catalyzed | Function in Reproduction | EDC-Induced Alterations |
|---|---|---|---|
| SIRT1 | Deacetylation | Regulates mitochondrial homeostasis, telomere function [18] | Dysregulated in aging; targeted by pharmacological interventions [18] |
| EZH2 | H3K27me3 | Polycomb repression; stem cell maintenance [18] | Participates in core aging pathways; aberrant expression in reproductive cancers [18] |
| PRMT5 | H4R3me2, H3R8me2 | SSC fate determination; regulates PLZF accessibility [13] | Deficiency alters chromatin state, leading to SSC defects and spermatogenesis disorder [13] |
| Suv39h | H3K9me3 | Heterochromatin formation; chromosome segregation [13] | Null mice show spermatogenic failure with nonhomologous chromosome associations [13] |
Figure 1: EDC Impact on Epigenetic Regulation and Reproductive Health. This diagram illustrates the pathway from EDC exposure through epigenetic disruptions to adverse reproductive outcomes, highlighting key molecular mechanisms.
Transgenerational Epigenetic Inheritance
Transgenerational epigenetic inheritance occurs when environmental exposures induce epigenetic alterations in germ cells that persist across multiple generations, potentially affecting the health of unexposed descendants [19] [20]. This phenomenon represents a significant challenge for risk assessment, as the effects of exposures may not be apparent until subsequent generations.
Mechanisms of Transgenerational Transmission
The transmission of epigenetic information across generations involves several interconnected mechanisms that can operate simultaneously or sequentially:
- DNA Methylation Patterns: Despite global epigenetic reprogramming in PGCs, certain genomic regions, including imprinted genes and specific repetitive elements, can escape erasure and maintain their methylation states [20]. For example, maternal exposure to vinclozolin during pregnancy in rats alters DNA methylation patterns in the sperm of male offspring for at least four generations, associated with increased rates of reproductive abnormalities [19].
- Histone Modifications in Germ Cells: In sperm, retained histones (approximately 1-10% in mammals) carry modifications such as H3K4me3, H3K27me3, and H3K9me3 that can potentially influence embryonic development [20]. Disruption of histone methylation in developing sperm, as demonstrated by Siklenka et al. (2015), can impair offspring health transgenerationally [20].
- Non-Coding RNAs: Sperm-borne transfer RNAs (tRNAs) and small non-coding RNAs (sncRNAs), including microRNAs (miRNAs) and PIWI-interacting RNAs (piRNAs), can serve as vectors of epigenetic information [20] [21]. For instance, trauma-induced changes in sperm miRNA profiles in mice can alter stress responses in subsequent generations [21].
EDCs and Transgenerational Inheritance of Reproductive Defects
Evidence from animal models provides compelling evidence for EDC-induced transgenerational inheritance of reproductive defects:
- Vinclozolin Exposure: Pregnant rats exposed to the fungicide vinclozolin produce male offspring with increased spermatogenic apoptosis and decreased sperm motility and concentration. These effects persist transgenerationally (F1-F4) and are associated with differential DNA methylation regions (DMRs) in sperm [19].
- BPA and Phthalates: Exposure to BPA and phthalates during critical windows of development can induce transgenerational effects, including decreased fertility, altered hormone levels, delayed puberty, and abnormal estrous cycles [19] [15]. These effects display sex-specific patterns, reflecting the complexity of epigenetic regulation in male and female reproductive systems [19].
Table 3: Evidence for Transgenerational Effects of Selected EDCs
| EDC | Model System | Exposure Window | Transgenerational Phenotypes (F1-F3+) | Associated Epigenetic Changes |
|---|---|---|---|---|
| Vinclozolin | Rat (in vivo) | Gestational [19] | Male infertility, spermatogenic defects, increased apoptosis [19] | Altered DNA methylation patterns in sperm [19] |
| Bisphenol A (BPA) | Mouse/Rat (in vivo) | Gestational or perinatal [19] [15] | Decreased fertility, ovarian defects, uterine abnormalities [19] [15] | Changes in uterine DNA methylation (e.g., HOXA10, ASCL2) [15] |
| Phthalates | Mouse (in vivo) | Prenatal [14] [19] | Reduced sperm count and motility, hormonal imbalances [14] [19] | Sperm DNA methylation changes, histone modifications [14] |
| Dioxins/PCBs | Human epidemiology & animal models | Prenatal [15] | Endometriosis, uterine disorders, reduced fertility [15] | Altered methylation of genes involved in uterine development [15] |
Methodologies for Epigenetic Analysis in EDC Research
Genome-Wide Epigenetic Profiling
Advanced high-throughput sequencing technologies enable comprehensive mapping of epigenetic modifications across the genome, providing powerful tools for identifying EDC-induced epimutations.
DNA Methylation Analysis:
- Whole Genome Bisulfite Sequencing (WGBS): Provides single-base resolution methylation maps of the entire genome. This is considered the gold standard for comprehensive DNA methylation analysis [19].
- Reduced Representation Bisulfite Sequencing (RRBS): A cost-effective method that enriches for CpG-rich regions, suitable for large-scale screening studies [19].
- Epigenome-Wide Association Studies (EWAS): Utilize microarray platforms (e.g., Illumina EPIC array) to profile methylation at >850,000 CpG sites in human population studies [20].
Histone Modification Profiling:
- Chromatin Immunoprecipitation Sequencing (ChIP-seq): Identifies genome-wide binding sites for specific histone modifications or chromatin-associated proteins [18]. Critical for mapping H3K27me3 Polycomb domains and other repressive/active marks disrupted by EDCs.
Chromatin Accessibility Assessment:
- Assay for Transposase-Accessible Chromatin using Sequencing (ATAC-seq): Maps open chromatin regions to identify accessible regulatory elements affected by EDC exposure [18].
Figure 2: Experimental Workflow for EDC Epigenetic Research. This diagram outlines a comprehensive approach from animal exposure modeling through multi-omics epigenetic analysis to functional validation of EDC-induced changes.
Table 4: Key Research Reagents for Epigenetic Studies in EDC Research
| Reagent/Resource | Category | Specific Examples | Research Application |
|---|---|---|---|
| DNMT Inhibitors | Small Molecule Inhibitors | 5-aza-2'-deoxycytidine (Decitabine) [18] | Investigate DNA methylation-dependent mechanisms; potential therapeutic applications |
| HDAC Inhibitors | Small Molecule Inhibitors | Vorinostat (SAHA) [18] | Probe role of histone acetylation in EDC toxicity; cancer therapy combinations |
| Antibodies for Histone Modifications | Immunochemical Reagents | H3K27me3, H3K4me3, H3K9ac [18] [13] | ChIP-seq, immunoblotting, immunofluorescence for histone mark detection |
| Bisulfite Conversion Kits | Molecular Biology Kits | EZ DNA Methylation kits [19] | Prepare DNA for methylation analysis by sequencing or pyrosequencing |
| Single-Cell Multi-Omics Platforms | Platform Technology | 10x Genomics Single Cell Multiome ATAC + Gene Expression [13] | Simultaneously profile chromatin accessibility and gene expression in single cells |
| Organoid Culture Systems | Biological Models | Testicular, ovarian, endometrial organoids [18] | Human-relevant in vitro models for studying EDC effects on reproductive tissues |
The intricate interplay between DNA methylation, histone modifications, and non-coding RNAs constitutes the molecular foundation of epigenetic reprogramming, a process highly vulnerable to disruption by EDCs, particularly during critical developmental windows. The evidence summarized in this technical review underscores that EDC-induced epimutations in germ cells can escape reprogramming and manifest as transgenerational inheritance of reproductive pathologies, including infertility and hormone-sensitive cancers. Future research priorities should include the systematic identification of susceptibility windows for specific EDCs, comprehensive mapping of transmitted epigenetic marks across generations using integrated multi-omics approaches, and elucidating the complex interactions between different epigenetic layers in transmitting environmental information. Furthermore, developing targeted epigenetic editing tools and pharmacological interventions to reverse or mitigate these deleterious epigenetic changes represents a promising frontier for therapeutic development in reproductive medicine. As the field advances, incorporating epigenetic endpoints into chemical risk assessment will be crucial for protecting reproductive health across generations.
The Developmental Origins of Health and Disease (DOHaD) paradigm establishes that environmental exposures during sensitive developmental periods reprogram physiological systems, increasing susceptibility to noncommunicable diseases (NCDs) in adulthood and across generations [22] [23]. This review examines the critical windows of vulnerability, emphasizing the impact of endocrine-disrupting chemicals (EDCs) on the rising incidence of infertility and reproductive cancers. During developmental plasticity phases—from preconception through adolescence—exposures to environmental stressors like EDCs can cause subtle, permanent alterations in gene expression via epigenetic reprogramming rather than genetic mutations [24]. We synthesize epidemiological and experimental evidence, detailing the mechanisms by which EDCs disrupt hormonal signaling and provide structured data, methodological protocols, and essential research tools to advance this field.
The DOHaD framework has evolved from initial observations linking low birth weight to increased coronary heart disease risk in adulthood [22] [24]. The paradigm posits that the early life environment interacts with genetic variation to shape an organism's capacity to cope with its environment later in life [22]. While early research focused on nutritional influences, it is now clear that DOHaD comprehensively includes a range of environmental factors—including EDCs, stress, and pollutants—and their relevance to disease occurrence throughout the lifespan and across generations [22].
The central mechanism involves developmental plasticity, the ability of a single genotype to produce different phenotypes in response to environmental conditions during specific critical windows [25]. When environmental cues during development mismatch the actual postnatal environment, it can lead to predictive adaptive responses that increase disease susceptibility later in life [25]. This is particularly relevant for EDCs, which can interfere with the endocrine control of development, leading to altered tissue function and increased risk of reproductive disorders, including infertility and reproductive cancers [26] [27].
Critical Windows of Developmental Vulnerability
Development is a plastic process that exhibits varying sensitivity to environmental perturbations at different life stages. These critical windows represent periods when specific tissues and organs are most susceptible to reprogramming by environmental factors.
Defining the Windows of Vulnerability
The following table summarizes the major critical windows of vulnerability, their key developmental processes, and potential consequences of EDC exposure.
Table 1: Critical Windows of Developmental Vulnerability to Environmental Exposures
| Developmental Window | Key Developmental Processes | Potential Consequences of EDC Exposure |
|---|---|---|
| Preconception (Paternal & Maternal) | Germ cell development, genomic imprinting [23] | Epimutations in sperm [23] [25]; altered fetal programming [25] |
| In Utero (Fetal period) | Organogenesis, tissue differentiation, hypothalamic-pituitary-ovarian axis establishment [22] [26] | Genital malformations (cryptorchidism, hypospadias) [26] [28]; altered reproductive tract development; increased cancer susceptibility [24] |
| Early Postnatal (Lactation, Infancy) | Immune system maturation, brain development, establishment of gut microbiome [23] | Altered immune function [23]; reprogrammed metabolic set points [23] |
| Childhood and Adolescence | Continued brain development, pubertal maturation, bone growth [22] [25] | Earlier puberty onset [29] [28]; altered neurodevelopment; entrainment of lifestyle behaviors [25] |
As illustrated, vulnerability begins prior to conception, with paternal and maternal exposures capable of influencing the germline [23] [25]. The most intense window spans the fetal period, when organ systems undergo rapid development and are exquisitely sensitive to hormonal disruption [22]. For instance, sexual differentiation is highly dependent on the fetal hormonal environment, and EDC exposure during this window can cause reproductive tract abnormalities that may not manifest until adulthood [26] [28]. Notably, vulnerability extends beyond birth for systems like the reproductive, immune, and neuroendocrine systems, which continue developing into childhood and adolescence [22] [25].
Vulnerability in the Context of EDCs and Reproductive Health
For reproductive health, EDCs such as phthalates, bisphenols, and PFAS can disrupt the tightly regulated pathways of sexual development, leading to disorders manifesting at birth (e.g., hypospadias) or later in life (e.g., reduced fertility, testicular cancer, polycystic ovary syndrome) [26] [27] [29]. These effects exhibit marked sex differences and are dependent on the timing and type of stressor [22]. The latency between developmental exposure and disease manifestation is a hallmark of DOHaD, with exposures potentially remaining clinically silent until a second "hit" or challenge occurs later in life [22] [24].
Molecular Mechanisms: Epigenetics and Pathway Disruption
The molecular basis for DOHaD effects primarily involves epigenetic reprogramming, where environmental exposures during development cause lasting changes in gene expression without altering the DNA sequence itself [23] [24].
Epigenetic Reprogramming
Environmental exposures during development can target the epigenome, leading to epimutations that increase disease susceptibility [24]. Key epigenetic mechanisms include:
- DNA methylation: The addition of methyl groups to CpG islands, typically repressing gene expression [24]. Prenatal exposure to famine has been associated with persistent DNA methylation changes at specific gene loci [24].
- Histone modifications: Methylation or acetylation of histone tails can activate or repress gene expression [24]. For example, H3K27 trimethylation typically represses gene expression [24].
- Non-coding RNAs: These can regulate gene expression post-transcriptionally and may be involved in transgenerational transmission [30].
These epigenetic modifications are particularly impactful during developmental periods when epigenetic patterns are being established and are more plastic [23] [24]. Once set, these patterns can be stable and long-lasting, potentially transmitted across generations via germline epigenetic inheritance [22] [24].
Disruption of Reproductive Endocrine Pathways
EDCs primarily interfere with the hormonal pathways critical for reproductive system development and function. The diagram below illustrates the hypothalamic-pituitary-gonadal (HPG) axis and key points of EDC disruption.
Figure 1: EDC Disruption of the Female Hypothalamic-Pituitary-Ovarian Axis
EDCs can act through multiple mechanisms to disrupt this finely tuned system:
- Hormone mimicry: Binding to and activating estrogen receptors (e.g., BPA, phthalates) or androgen receptors [27] [28].
- Receptor antagonism: Blocking hormones from binding to their receptors [28].
- Altering hormone synthesis/metabolism: Interfering with enzymes involved in hormone production or breakdown [27].
- Epigenetic modification: Reprogramming gene expression in reproductive tissues [24].
For example, phthalate exposure has been associated with elevated FSH and lower estradiol, progesterone, and testosterone in adult women [27]. PFAS exposure has been linked to longer menstrual cycles and decreased estrogen and progesterone levels [27]. These disruptions during development can permanently alter the structure and function of reproductive organs, increasing susceptibility to conditions like infertility, endometriosis, and reproductive cancers [26] [28] [24].
Transgenerational Inheritance
Epigenetic reprogramming from developmental EDC exposure can potentially be transmitted to subsequent generations through germline transmission [22] [24]. The following diagram illustrates the mechanisms of transgenerational inheritance.
Figure 2: Transgenerational Inheritance of EDC Effects
True transgenerational inheritance requires the transmission of epigenetic marks through the germline to generations never directly exposed to the original EDC [22] [24]. Experimental evidence supports this phenomenon, demonstrating that EDC exposures during development can increase disease susceptibility in multiple subsequent generations [24].
Experimental Models and Methodologies
DOHaD research utilizes diverse experimental approaches to elucidate the mechanisms linking developmental exposures to later-life disease. The following table summarizes key methodological approaches for studying EDC effects within the DOHaD framework.
Table 2: Experimental Approaches for DOHaD-EDC Research
| Method Category | Specific Method/Assay | Key Applications in DOHaD-EDC Research |
|---|---|---|
| Epidemiological Studies | Cohort studies (e.g., NHANES), cross-sectional studies, case-control studies [27] [29] | Identifying associations between early-life EDC exposure and later reproductive outcomes (e.g., infertility, early menopause) [27] [29] |
| Animal Models | Rodent (mouse, rat) developmental exposure studies [27] [30] | Controlled investigation of critical windows, mechanisms, and transgenerational inheritance [27] [30] |
| In Vitro Systems | Ovarian follicle culture, cell lines (steroidogenic cells), primordial germ cell culture [27] | High-throughput screening of EDC effects on specific cell types and pathways [27] |
| Epigenetic Analyses | Whole-genome bisulfite sequencing, ChIP-seq, histone modification profiling [24] | Identifying locus-specific and genome-wide epigenetic changes induced by EDCs [24] |
| Hormonal Assays | ELISA, LC-MS/MS, RIA for steroids (estradiol, progesterone), FSH, LH [27] | Quantifying EDC-induced alterations in endocrine profiles [27] |
Detailed Experimental Protocol: Perinatal EDC Exposure and Reproductive Assessment
This protocol outlines a comprehensive approach for assessing the effects of developmental EDC exposure on female reproductive outcomes in a rodent model, based on methodologies cited in the search results [27] [30].
1. Animal Model and Exposure Paradigm:
- Use timed-pregnant dams (e.g., Sprague-Dawley rats or C57BL/6 mice).
- Administer EDC (e.g., BPA, phthalates, or PFAS) via drinking water or oral gavage during critical windows:
- Gestational exposure: From gestational day (GD) 7 to parturition.
- Perinatal exposure: From GD7 through lactation until postnatal day (PND) 21.
- Include vehicle-control and positive control groups (e.g., known reproductive toxicant).
- Monitor dams for weight, food, and water intake.
2. Assessment of Offspring Outcomes:
- Prepubertal period (PND 1-21): Record anogenital distance, weight, and age at eye opening.
- Pubertal onset: Monitor for vaginal opening (females) daily from PND 28.
- Adult reproductive function (PND 60-90):
- Vaginal cytology: Daily smears for 3-4 weeks to assess estrous cyclicity.
- Fertility assessment: Mate exposed females with unexposed males; record time to impregnation, litter size, and offspring viability.
- Serum hormone analysis: Measure FSH, LH, estradiol, progesterone, and AMH via ELISA at different estrous stages.
- Ovarian histology: Collect ovaries at sacrifice; count primordial, primary, secondary, and antral follicles.
- Gene expression analysis: qRT-PCR or RNA-seq for ovarian steroidogenic genes (Star, Cyp11a1, Hsd3b1, Cyp19a1).
3. Transgenerational Studies:
- Breed exposed F1 females with unexposed males to generate F2 offspring.
- Continue breeding to F3 generation to assess true transgenerational effects [24].
- Assess similar reproductive endpoints in F2 and F3 generations.
This protocol allows for systematic evaluation of how developmental EDC exposure programs lifelong reproductive function and potential transgenerational impacts.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs key reagents and resources essential for investigating DOHaD mechanisms in EDC research, particularly focused on reproductive outcomes.
Table 3: Essential Research Reagents for DOHaD-EDC Studies
| Reagent/Resource | Specific Examples | Research Applications |
|---|---|---|
| Reference EDCs | Diethylstilbestrol (DES) [22], Bisphenol A (BPA) [27] [30], Di(2-ethylhexyl) phthalate (DEHP) [27], PFOS/PFOA [27] [29] | Positive controls for endocrine disruption studies; mechanistic investigations |
| Animal Models | Mouse (C57BL/6, CD-1), Rat (Sprague-Dawley, Long-Evans) [27] [30] | In vivo assessment of developmental programming and transgenerational inheritance |
| Hormone Assay Kits | ELISA kits for 17β-estradiol, progesterone, testosterone, FSH, LH, AMH [27] | Quantifying endocrine changes in serum, follicular fluid, and tissue culture media |
| Cell Culture Models | Primary ovarian follicles [27], steroidogenic cell lines (e.g., KGN, H295R), human endometrial organoids | In vitro screening of EDC effects on specific cell types and pathways |
| Epigenetic Tools | DNA methyltransferase inhibitors (5-azacytidine), histone deacetylase inhibitors (TSA), CRISPR/dCas9-epigenetic editors [24] | Mechanistic studies to establish causal relationships between epigenetic marks and phenotypes |
| Antibodies | Anti-histone modifications (H3K4me3, H3K27me3), anti-steroidogenic enzymes (CYP11A1, CYP19A1), anti-hormone receptors (ERα, AR) [27] [24] | Western blot, immunohistochemistry, and ChIP assays to assess molecular changes |
These reagents enable researchers to dissect the complex relationships between developmental EDC exposures and later-life reproductive health outcomes across multiple biological levels, from molecular epigenetics to whole-organism physiology.
Discussion and Future Directions
The DOHaD paradigm provides a crucial framework for understanding how early-life EDC exposures contribute to the growing global burden of infertility and reproductive cancers. The evidence reviewed demonstrates that developmental exposures to EDCs during critical windows of vulnerability can reprogram reproductive systems through epigenetic mechanisms, with effects potentially spanning multiple generations.
Future research should prioritize:
- Elucidating mixture effects: Humans are exposed to complex mixtures of EDCs throughout life, yet most studies examine single compounds [22] [29].
- Identifying sensitive biomarkers: Developing biomarkers that predict individual susceptibility to EDC exposure and later-life disease risk [31].
- Adolescent interventions: Targeting adolescence as a critical window for intervention, as it represents a period where lifestyle behaviors become entrained and the next generation of parents are formed [25].
- Regulatory policy translation: Incorporating DOHaD principles into chemical risk assessment and regulatory frameworks to better protect vulnerable developmental periods [29].
The DOHaD perspective underscores that prevention strategies for reproductive disorders and cancers must begin early—before conception and during key developmental windows—rather than focusing solely on adult disease treatment. By identifying mechanisms of developmental reprogramming and critical windows of vulnerability, we can develop more effective interventions to break the transgenerational cycle of reproductive disease.
Within the broader investigation into the impact of endocrine-disrupting chemicals (EDCs) on infertility and reproductive cancers, the dysregulation of cellular redox homeostasis and programmed cell death emerges as a critical pathological mechanism. EDCs, including bisphenol A (BPA), phthalates, and pesticides, induce oxidative stress and apoptosis in reproductive tissues through receptor-mediated disruption of hormonal signaling, mitochondrial dysfunction, and epigenetic modifications. This whitepaper synthesizes current mechanistic insights, details key experimental methodologies for investigating these pathways, and provides resources to advance therapeutic development. The intricate interplay between oxidative damage and apoptotic signaling not only compromises gamete quality and steroidogenesis but may also contribute to the initiation and progression of reproductive malignancies, presenting a compelling target for future pharmacologic intervention.
The decline in global fertility rates and the rising incidence of certain reproductive cancers are increasingly linked to widespread exposure to EDCs [14] [32]. These exogenous chemicals, ubiquitous in plastics, pesticides, personal care products, and industrial effluents, interfere with the synthesis, transport, and action of endogenous hormones [6]. The reproductive system is particularly vulnerable due to its heavy reliance on precise hormonal communication for development and function. A growing body of evidence positions oxidative stress and the subsequent induction of apoptosis as a convergent pathway through which diverse EDCs exert their detrimental effects on both male and female reproductive health, disrupting processes from gametogenesis to embryonic implantation [33] [34] [35]. This document details the mechanisms, measurement, and research tools relevant to this field.
Molecular Mechanisms of EDC-Induced Cellular Damage
EDCs instigate cellular damage through a network of interconnected pathways that ultimately disrupt the delicate balance between cell survival and death.
Receptor-Mediated Disruption of Redox Signaling
EDCs can directly bind to hormone receptors, initiating signaling cascades that alter redox metabolism. For instance, BPA binds to estrogen receptors (ERα/ERβ) with nanomolar affinity (Ki ≈ 5–10 nM), leading to the upregulation of estrogen-responsive genes in tissues like Sertoli cells [14]. This receptor activation can trigger rapid, non-genomic pathways, including calcium influx and activation of the MAPK/ERK signaling cascade, which in turn can promote the generation of reactive oxygen species (ROS) [14]. Similarly, phthalates and certain pesticides interfere with androgen and thyroid hormone receptors, disrupting the hormonal regulation of antioxidant defense systems and creating a pro-oxidative cellular environment [36].
Mitochondrial Dysfunction: The Epicenter of Oxidative Stress
Mitochondria, the primary source of cellular ATP, are also a major site of ROS generation and a key target for EDC toxicity. EDCs such as phthalates and pesticides impair mitochondrial electron transport chain function, leading to electron leakage and excessive production of superoxide anion (O₂⁻) [34]. This superoxide is dismutated into hydrogen peroxide (H₂O₂), which can further react to form highly damaging hydroxyl radicals (•OH). Mitochondrial DNA is especially vulnerable due to its lack of protective histones, and its damage perpetuates a cycle of metabolic dysfunction and ROS production [35]. This oxidative burden depletes crucial antioxidants like glutathione (GSH) and overwhelms enzymes like superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPx), leading to a state of sustained oxidative stress [33] [34].
The Apoptotic Cascade
Sustained oxidative stress directly activates the intrinsic (mitochondrial) apoptotic pathway. ROS promote mitochondrial membrane permeability, triggering the release of cytochrome c into the cytoplasm. This leads to the formation of the apoptosome and the sequential activation of initiator (caspase-9) and executioner caspases (caspase-3, -7) [37]. The 17 kDa active form of caspase-3, a key executioner, cleaves cellular substrates, resulting in the systematic dismantling of the cell [38]. In the male reproductive system, this process damages spermatogenic cells, while in females, it can trigger apoptosis in granulosa cells and oocytes, impairing folliculogenesis and ovarian reserve [14] [33].
The diagram below illustrates the core signaling pathway from EDC exposure to cellular damage.
Quantitative Biomarkers of Oxidative Damage and Apoptosis
Tracking oxidative stress and apoptosis requires quantifying specific molecular biomarkers. The following tables summarize key analytes and their significance.
Table 1: Key Biomarkers of Oxidative Stress and Antioxidant Capacity
| Biomarker | Description | Significance & Example Changes |
|---|---|---|
| ROS/RNS | Total levels of reactive oxygen and nitrogen species. | Direct measure of pro-oxidant load. Increased ~2.2-fold in uterine explants after octylphenol exposure [38]. |
| Malondialdehyde (MDA) | Byproduct of lipid peroxidation. | Indicator of membrane damage. Elevated in oocytes exposed to DEHP [33]. |
| 8-OHdG | 8-hydroxy-2'-deoxyguanosine, an oxidized DNA adduct. | Marker of oxidative DNA damage; found in oocytes after EDC exposure [33]. |
| GSH/GSSG Ratio | Ratio of reduced to oxidized glutathione. | Primary indicator of cellular redox status. A decreased ratio signifies oxidative stress [33]. |
| SOD, CAT, GPx Activity | Key antioxidant enzyme activities. | CAT and GPx activity increased 2-fold and 2.3-fold, respectively, in sow-fed uterine explants upon EDC exposure, indicating a compensatory response [38]. |
Table 2: Key Biomarkers of Apoptosis
| Biomarker | Description | Significance & Experimental Detection |
|---|---|---|
| Caspase-3 Activation | Cleavage of pro-caspase-3 (35 kDa) to active form (17 kDa). | Executioner caspase; increased abundance in uterine explants after antiandrogen exposure [38]. Detected by Western blot. |
| DNA Fragmentation | Cleavage of nuclear DNA. | Hallmark of late-stage apoptosis. Quantified via TUNEL assay; increased in luminal and glandular epithelium after EDC exposure [38]. |
| BCL-2 Family Proteins | Regulators of mitochondrial apoptosis (e.g., BAX pro-apoptotic, BCL-2 anti-apoptotic). | Altered expression upon EDC exposure disrupts mitochondrial membrane integrity [37]. Detected by Western blot or immunohistochemistry. |
Detailed Experimental Protocols
To ensure reproducibility in investigating EDC-induced oxidative stress and apoptosis, standardized protocols are essential.
Ex Vivo Uterine Explant Model for Assessing EDC Effects
This protocol, adapted from a 2025 study, is ideal for studying direct tissue-specific effects while controlling for systemic variables [38].
1. Tissue Collection and Preparation:
- Source: Obtain uterine tissue from a model organism (e.g., 10-day-old piglets).
- Feeding Groups: Include both naturally fed (sow-fed) and formula-fed cohorts to investigate the protective role of bioactive factors in maternal milk.
- Dissection: Aseptically dissect uterine horns and place in ice-cold, oxygenated physiological buffer (e.g., DMEM/F-12).
- Explants: Slice uterine tissue into precise, uniform explants (e.g., 2x2x2 mm³).
2. Ex Vivo EDC Exposure:
- Treatment Groups: Randomly assign explants to culture wells.
- EDC Incubation: Expose explants to relevant EDCs (e.g., 10 µM 2-hydroxyflutamide (antiandrogen), 10 µM 4-tert-octylphenol (environmental estrogen), or 10 µM HPTE (methoxychlor metabolite)) for a defined period (e.g., 24 hours) in a controlled incubator (37°C, 5% CO₂).
- Controls: Include vehicle-treated control explants (e.g., DMSO <0.1%).
3. Oxidative Stress Analysis:
- ROS/RNS Quantification: Homogenize a subset of explants. Use fluorometric assays with dichloro-dihydro-fluorescein diacetate (DCFH-DA) to measure total ROS/RNS levels.
- Antioxidant Enzyme Activity: Assay supernatants from homogenized tissue for CAT, GPx, GST, GR, and SOD activities using standardized colorimetric or kinetic assays.
4. Apoptosis and Proliferation Assessment:
- TUNEL Assay: Fix explants in 4% paraformaldehyde, embed in paraffin, section, and use a TUNEL kit to label DNA strand breaks for apoptotic cell counting via fluorescence microscopy.
- Immunohistochemistry (IHC): Perform IHC on tissue sections for proliferating cell nuclear antigen (PCNA) to quantify cell proliferation and for cleaved caspase-3 to confirm apoptosis.
- Western Blotting: Analyze total protein lysates from explants for apoptosis markers (e.g., pro/active caspase-3, BCL-2, BAX) and proliferation markers.
The workflow for this multi-faceted analysis is outlined below.
Assessing Sperm Oxidative Stress and DNA Damage
For male fertility research, analyzing sperm quality after EDC exposure is critical [34] [35].
1. Sperm Collection and EDC Exposure:
- Collect semen samples from model organisms or human donors (with consent).
- For in vitro studies, incubate motile sperm fractions with environmentally relevant concentrations of EDCs (e.g., BPA, phthalate metabolites) for several hours.
2. Sperm Quality and Redox Analysis:
- Computer-Assisted Sperm Analysis (CASA): Assess sperm concentration, motility, and kinematics.
- Chemiluminescence Assay: Use luminol or lucigenin probes to measure specific types of ROS directly from sperm suspensions.
- Lipid Peroxidation: Measure MDA levels in sperm samples via thiobarbituric acid reactive substances (TBARS) assay.
- Sperm Chromatin Dispersion Test: Evaluate DNA fragmentation by quantifying the halos of dispersed DNA following acid denaturation and protein removal.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs key reagents and their applications for studying EDC-induced oxidative stress and apoptosis.
Table 3: Research Reagent Solutions for EDC Studies
| Reagent / Assay Kit | Function & Application |
|---|---|
| DCFH-DA Probe | Cell-permeable fluorogenic dye used to quantitatively measure intracellular ROS/RNS levels in cells and tissue homogenates [38]. |
| Caspase-3 Activity Assay Kit | Colorimetric or fluorometric kit to detect and quantify the activation of the key executioner caspase, a definitive marker of apoptosis [37] [38]. |
| TUNEL Assay Kit | Fluorescence-based kit for in situ labeling of DNA fragmentation, allowing visualization and quantification of apoptotic cells within tissue sections [38]. |
| GSH/GSSG Ratio Assay Kit | Provides a sensitive method to determine the dynamic balance between reduced and oxidized glutathione, a central indicator of cellular redox state [33]. |
| Antibodies for BCL-2, BAX, PCNA | Essential for protein-level detection via Western blot or IHC to assess apoptotic signaling and cellular proliferation status [37] [38]. |
| Specific EDCs (e.g., BPA, MEHP, 4-tert-Octylphenol) | High-purity chemical standards used for in vitro and in vivo exposure studies to establish direct cause-effect relationships [14] [33] [38]. |
Endocrine-disrupting chemicals (EDCs) represent a significant concern for human reproductive health worldwide. This technical review examines the specific profiles and mechanisms of action of Bisphenol-A (BPA), phthalates, pesticides, polychlorinated biphenyls (PCBs), and diethylstilbestrol (DES) in the context of infertility and reproductive cancers. Evidence from epidemiological, clinical, and toxicological studies demonstrates that these chemicals interfere with hormonal signaling through genomic and non-genomic pathways, disrupting the hypothalamic-pituitary-gonadal axis and causing epigenetic modifications. The pervasive presence of EDCs in consumer products, environmental media, and food chains leads to ubiquitous human exposure, with particular risk for vulnerable populations. This whitepaper provides a comprehensive analysis of each EDC's reproductive toxicity profile, detailed experimental methodologies for their study, and essential research tools for advancing this critical field of environmental health science.
Chemical Profiles and Reproductive Toxicity
Bisphenol-A (BPA)
BPA is an organic synthetic compound widely used in polycarbonate plastics, epoxy resins, and thermal paper products. Global industrial production reaches billions of pounds annually, resulting in ubiquitous human exposure through food packaging, consumer goods, and environmental media [39] [40].
Table 1: BPA Reproductive Toxicity Profile
| Aspect | Details |
|---|---|
| Global Production | Billions of pounds annually [40] |
| Detection | Found in multiple human body fluids [39] |
| Male Effects | Increased sperm alterations, altered reproductive hormone levels, testicular atrophy [39] |
| Female Effects | Hormonal imbalances, reduced ovarian reserve, infertility, PCOS, endometriosis, fibroids [39] |
| Key Mechanisms | Estrogen receptor agonism, androgen receptor antagonism, HPG axis disruption [40] |
| Exposure Concern | Adverse effects observed even at low exposure levels [40] |
BPA exerts its endocrine-disrupting effects primarily through estrogen receptor agonism and androgen receptor antagonism, leading to disruption of the hypothalamic-pituitary-gonadal (HPG) axis [40]. It can cause detrimental changes to both male and female reproductive health through both genomic and non-genomic mechanisms, with epigenetic modifications playing a significant role in its long-term effects [39].
Phthalate Esters (PAEs)
Phthalates are high-production volume synthetic compounds extensively utilized as plasticizers to enhance flexibility in plastics, with global production approximately 8 million tons annually [41]. They represent 80-85% of all plasticizers produced and are found in medical devices, cosmetics, food packaging, and construction materials [41].
Table 2: Phthalate Reproductive Toxicity Profile
| Aspect | Details |
|---|---|
| Global Production | ~8 million tons annually (80-85% of plasticizers) [41] |
| Common Uses | Medical devices, cosmetics, food packaging, construction materials [41] |
| Male Effects | Testicular dysgenesis syndrome, reduced fertility capacity [41] |
| Female Effects | Disrupted follicle growth, increased oxidative stress, follicle death, faster ovarian reserve depletion [42] |
| Key Mechanisms | HPG axis dysfunction, abnormal gonadal hormone secretion, oxidative stress, apoptosis [41] [42] |
| Research Focus | Mixed exposures, dose-response relationships, toxicological mechanisms [41] |
Phthalates are recognized endocrine disruptors that interfere with the hypothalamus-pituitary-gonadal (HPG) axis, resulting in abnormal secretion of gonadal hormones and alterations in the synthesis of sex hormone receptors [41]. In females, phthalates can disrupt follicle growth patterns, increase oxidative stress, and cause follicle death, potentially leading to infertility and earlier reproductive senescence [42].
Pesticides
Pesticides encompass various chemical classes including herbicides, insecticides, and fungicides, many with endocrine-disrupting properties. Extensive evidence links pesticide exposure to numerous cancers and reproductive disorders [43] [44] [45].
Table 3: Pesticide Cancer Associations Evidence Base
| Cancer Type | Number of Studies | Studies Finding Association | Evidence Strength |
|---|---|---|---|
| Non-Hodgkin Lymphoma | 32 | 23/27 (85%) | Strong [43] |
| Leukemia | 23 | 14/16 (88%) | Strong [43] |
| Brain Cancer | 11 | 11/11 (100%) | Consistent [43] |
| Prostate Cancer | 10 | 8/8 (100%) | Consistent [43] |
| Bladder Cancer | Multiple | Positive associations | Dose-dependent [44] |
Pesticides have been associated with reproductive toxicity through multiple pathways. Recent bibliometric analyses identify "bisphenol a," "infertility," "testicular dysgenesis syndrome," "endocrine disrupting chemicals," and "oxidative stress" as research hotspots, indicating focused investigation into reproductive endpoints [41]. The association between pesticide exposure and cancer risk has been found to be comparable to smoking for some cancer types [45].
Polychlorinated Biphenyls (PCBs) and Persistent EDCs
PCBs, polybrominated diphenyl ethers (PBDEs), organochlorine pesticides (OCPs), and per- and polyfluoroalkyl substances (PFAS) constitute persistent EDCs characterized by long biological half-lives, environmental persistence, and bioaccumulation potential [46] [47]. Though many have been banned or phased out, exposure remains concerning due to environmental persistence and propensity to leach from consumer products [47].
These persistent EDCs can dysregulate the stress response by disrupting the hypothalamic-pituitary-adrenal (HPA) and hypothalamic-pituitary-thyroid (HPT) axes [46]. In studies of Black women, specific EDCs including PCB 118, PBDE 99, and perfluorodecanoic acid (PFDA) were associated with higher perceived stress scores, indicating potential disruption of neuroendocrine pathways relevant to reproductive function [46].
Diethylstilbestrol (DES)
DES was the first orally active synthetic estrogen, previously prescribed to prevent miscarriage before being linked to rare vaginal tumors in young women exposed in utero [48]. DES represents a classic case study of intergenerational endocrine disruption with profound implications for understanding EDC mechanisms.
DES-induced toxicity in mouse seminal vesicles is mediated by estrogen receptor α (ERα), which alters expression of seminal vesicle secretory protein IV (Svs4) and lactoferrin (Ltf) genes through epigenetic modifications [48]. Neonatal DES exposure causes permanent changes in DNA methylation patterns in reproductive tissues, demonstrating the ability of EDCs to program long-term reproductive dysfunction through epigenetic mechanisms [48].
Experimental Models and Methodologies
In Vivo Models
The neonatal mouse DES exposure model has been extensively utilized to study EDC effects on reproductive organs. The standard protocol involves treating pups each morning on postnatal days 1-5 with DES dissolved in dimethyl sulphoxide (DMSO) at pharmacologically relevant doses [48]. This model reproduces human reproductive tract abnormalities including uterine adenocarcinoma in females and testicular cancer, prostate, and seminal vesicle abnormalities in males [48].
Long-term follow-up studies in these models demonstrate that neonatal DES exposure results in decreased seminal vesicle weight and feminization of reproductive tissues primarily mediated through ERα [48]. These models allow for investigation of both immediate and latent effects of early-life EDC exposure on reproductive development and function.
Epidemiological Study Designs
Prospective cohort studies provide critical human evidence for EDC effects on reproductive health. The Study of Environment, Lifestyle, and Fibroids (SELF) exemplifies rigorous design for investigating EDC mixtures [46] [47]. This prospective cohort enrolled 1,693 Black women aged 23-35 years with intact uteri and no prior uterine leiomyomata diagnosis. Participants provided plasma samples at baseline which were analyzed for multiple EDC classes using high-resolution mass spectrometry techniques [47].
Key methodological considerations include:
- Cohort Retention: Follow-up visits at 20-month intervals with structured questionnaires
- Biomarker Quantification: Batch analysis with quality control protocols
- Lipid Adjustment: Enzymatic methods for lipid measurement and adjustment for lipophilic compounds
- Limit of Detection Handling: Imputation of values below LOD using batch-specific limits
- Mixture Analysis: Advanced statistical approaches including k-means clustering and principal components analysis
Biomarker Assessment Techniques
Advanced analytical methods enable comprehensive EDC biomarker quantification:
- Persistent Organic Pollutants: PCBs, PBDEs, and OCPs quantified using gas chromatography/isotope dilution high-resolution mass spectrometry [47]
- PFAS: Online solid-phase extraction-liquid chromatography-isotope dilution tandem mass spectrometry [46]
- Quality Assurance: Implementation of rigorous quality control protocols including blank samples and reference materials
Signaling Pathways and Mechanisms of Action
Hypothalamic-Pituitary-Gonadal Axis Disruption
EDCs interfere with reproductive function primarily through disruption of the HPG axis, which regulates reproduction through complex hormonal feedback loops. BPA, phthalates, and other EDCs can alter the secretion of gonadotropin-releasing hormone (GnRH) from the hypothalamus, subsequently affecting luteinizing hormone (LH) and follicle-stimulating hormone (FSH) release from the pituitary, and ultimately disrupting steroidogenesis in the gonads [41] [40].
Epigenetic Modification Mechanisms
DES provides the canonical example of EDC-induced epigenetic modifications. Neonatal DES exposure alters DNA methylation patterns in the seminal vesicle secretory protein IV (Svs4) and lactoferrin (Ltf) gene promoters in an ERα-dependent manner [48]. These changes are associated with altered gene expression that persists into adulthood, demonstrating the programming effect of early-life EDC exposure.
Oxidative Stress Pathways
Multiple EDCs including phthalates and pesticides induce oxidative stress in reproductive tissues, leading to cellular damage, apoptosis, and inflammation [41] [42]. In the ovary, phthalates can increase oxidative stress and cause follicle death, potentially accelerating ovarian reserve depletion [42]. The generation of reactive oxygen species represents a common pathway for EDC-induced damage across multiple chemical classes.
Research Reagent Solutions
Table 4: Essential Research Materials and Analytical Tools
| Reagent/Tool | Application | Technical Specifications |
|---|---|---|
| Gas Chromatography/High-Resolution Mass Spectrometry | Quantification of PCBs, PBDEs, OCPs | Isotope dilution, LOD varies by batch [47] |
| Online SPE-LC-Tandem Mass Spectrometry | PFAS quantification | LOD 0.1 ng/mL for all PFAS [46] |
| Enzymatic Lipid Quantification | Lipid adjustment for lipophilic compounds | Standardized enzymatic methods [47] |
| DNA Methylation Analysis | Bisulfite conversion sequencing | CpG site-specific methylation status [48] |
| Perceived Stress Scale (PSS-4) | Stress response assessment | 4-item scale, score range 0-16 [46] |
| Case-Cohort Study Design | EDC mixture association studies | Combines random subcohort with incident cases [47] |
The evidence for EDC-induced reproductive toxicity across multiple chemical classes underscores the urgent need for continued research and refined regulatory policies. BPA, phthalates, pesticides, PCBs, and DES each demonstrate specific profiles of reproductive harm through shared and distinct mechanisms of action, with particular concern for effects on vulnerable populations including pregnant women and children. Future research priorities should focus on understanding low-dose mixture effects, delineating epigenetic mechanisms of transgenerational inheritance, and developing targeted interventions to reduce exposure. The documented associations between EDC exposure and infertility and reproductive cancers highlight the critical importance of adopting a precautionary approach to regulation of these pervasive chemicals.
Advanced Research Models and Biomarker Discovery for EDC Risk Assessment
Endocrine-disrupting chemicals (EDCs) pose a significant threat to human well-being and the ecosystem, with particular concern for their impact on reproductive health, including infertility and reproductive cancers [49]. The U.S. Environmental Protection Agency's Endocrine Disruptor Screening Program (EDSP) utilizes a two-tiered approach combining in vitro and in vivo tests, but these traditional methods are animal-intensive, expensive, and time-consuming [49]. Completing all EDSP Tier 1 tests for a single chemical can require a minimum of 520 animals and cost between $335,100 and $964,250 [49]. These limitations have accelerated the development of advanced in vitro systems—specifically, human tissue cultures and high-throughput screening (HTS) platforms—that provide more physiologically relevant, efficient, and ethical tools for identifying and characterizing EDCs. This shift aligns with the EPA's ToxCast program and the broader Tox21 initiative, which use HTS assays and computational tools to predict chemical hazards and characterize toxicity pathways, including those related to estrogen, androgen, and thyroid hormone receptors [50].
Core In Vitro Technologies and Their Applications
Advanced Tissue Culture Models
The landscape of in vitro systems has evolved significantly from traditional two-dimensional (2D) cell cultures toward more physiologically relevant three-dimensional (3D) models. These 3D systems recapitulate in vivo morphology and functional pathways more accurately, providing a unique opportunity for estrogenic effect screening [49].
Three-Dimensional Microtissue Cultures: 3D culture technology enables the development of systems with more realistic biochemical and biomechanical microenvironments [49]. For instance, 3D microtissues formed by MCF-7 breast cancer cells in non-adhesive agarose hydrogel platforms demonstrate apical-basal polarity and luminal space formation, mirroring the human mammary gland's structure [49]. These microtissues show functional estrogenic pathways, with up-regulation of typical estrogen-responsive genes (PGR, PDZK1, and AREG) upon estradiol (E2) treatment, making them particularly valuable for studying EDCs that may influence breast cancer genesis and progression [49].
Primary Cell Culture Systems: Beyond established cell lines, primary cell cultures offer significant advantages for EDC research. Primary cultures of pituitary, testicular, and ovarian cells from model organisms like the marine medaka (Oryzias melastigma) retain tissue-specific gene expression, enabling researchers to evaluate responses of key genes along the hypothalamic-pituitary-gonadal (HPG) axis to environmental contaminants [51]. These systems allow for deciphering the specific target sites and mechanisms of EDCs by examining mRNA expression levels of gonadotropins, their receptors, and steroidogenic enzymes [51].
High-Throughput Screening Platforms
High-throughput screening technologies represent a paradigm shift in EDC identification and characterization, allowing for the rapid testing of thousands of chemical entities.
ToxCast HTS Assays: The U.S. EPA's ToxCast program utilizes HTS assays covering toxicity pathways involving estrogen, androgen, and thyroid hormone receptors, as well as steroidogenesis targets [50]. These technologies include competitive binding, reporter gene, and enzyme inhibition assays that detect chemicals capable of perturbing specific molecular initiating events in endocrine pathways [50]. When validated against EDSP Tier 1 screening assays, ToxCast estrogen receptor and androgen receptor assays demonstrated predictive balanced accuracies of 0.91 (p < 0.001) and 0.92 (p < 0.001), respectively, indicating their strong potential for prioritizing chemicals for further testing [50].
Imaging-Based Phenotypic Profiling: High-content imaging systems have emerged as powerful tools for HTS, particularly when coupled with 3D cultures [49]. These systems provide multifaceted information regarding cell-cell interactions, microtissue structure, and function, quantifying endpoints associated with cell morphology and tissue organization [49]. When combined with machine learning algorithms, this approach enables the identification of complex morphological signatures associated with EDC exposure, moving beyond single-endpoint measurements to capture integrated biological responses.
Table 1: Quantitative Performance of Selected In Vitro Assays for EDC Screening
| Assay Type | Predicted Endpoint | Balanced Accuracy | Statistical Significance | Reference |
|---|---|---|---|---|
| ToxCast ER Assays | EDSP Estrogen-related T1S | 0.91 | p < 0.001 | [50] |
| ToxCast AR Assays | EDSP Androgen-related T1S | 0.92 | p < 0.001 | [50] |
| ToxCast Models | Uterotrophic Assay | 0.89 | p < 0.001 | [50] |
| ToxCast Models | Hershberger Assay | 1.00 | p < 0.001 | [50] |
Experimental Protocols and Methodologies
Protocol for 3D Microtissue Estrogenicity Screening
Cell Culture and 3D Microtissue Formation:
- MCF-7 human breast carcinoma cells (ATCC HTB-22) are maintained in phenol-red free DMEM-F12 medium containing 10% fetal bovine serum (FBS), MEM nonessential amino acids, gentamicin, and 10 μg/mL insulin in a 5% CO2 incubator at 37°C [49].
- For 3D culture, non-adhesive agarose hydrogels are created using specialized molds (e.g., 3D Petri Dish 12-256-small spheroids molds) [49].
- Cells are trypsinized from monolayer cultures, counted, and seeded into agarose hydrogels at a density of 600,000 cells/mL [49].
- Cells are allowed to settle into recesses for 30 minutes before adding 2 mL of treatment media [49].
Chemical Treatment and Exposure:
- Treatment media consists of phenol-red free DMEM-F12 medium containing 5% dextran-coated-charcoal (DCC) stripped FBS, MEM nonessential amino acids, gentamicin, and 6 ng/mL insulin [49].
- Test compounds (EDCs) and controls (estradiol as positive control, DMSO as vehicle control) are prepared in treatment media.
- Following cell seeding, 2 mL of treatment media with test compounds or controls are added to the hydrogels.
- Plates are maintained in a 5% CO2 incubator at 37°C for up to 7 days, with treatment media changed on day 3 and day 5 [49].
Endpoint Analysis and Imaging:
- For gene expression analysis: Microtissues are collected by centrifugation, pelleted, and lysed in Tri Reagent for RNA extraction [49]. Quantitative RT-PCR is performed for estrogen-responsive genes (PDZK1, APOD, CYP1A1, TGFB3) normalized to RPLP0 as a housekeeping gene [49].
- For imaging analysis: Microtissues are rinsed in PBS, fixed in formalin for 15 minutes at room temperature, and stored in PBS at 4°C until imaging [49]. Before imaging, microtissues are incubated with ScaleS4 solution containing Hoechst 33342 for nuclear staining [49].
- High-content imaging is performed using appropriate microscope systems, capturing multiple focal planes to accommodate 3D structures [49].
Protocol for Primary Fish Cell Culture EDC Screening
Primary Cell Culture Establishment:
- Pituitary, ovarian follicular, and testicular tissues are dissected from marine medaka (Oryzias melastigma) [51].
- Tissues are dissociated using appropriate enzymatic treatments to create single-cell suspensions [51].
- Cells are seeded into culture plates with appropriate media formulations and maintained under controlled conditions [51].
EDC Exposure and Response Assessment:
- Cells are challenged with environmentally relevant concentrations of EDCs (e.g., estradiol, tetrabromodiphenyl ether, nonylphenol) [51].
- After exposure periods, cells are harvested for mRNA expression analysis of gonadotropins (luteinizing hormone, follicle-stimulating hormone), their receptors, and steroidogenic enzymes using quantitative PCR [51].
- Dose-response relationships are analyzed to determine EDC potency and efficacy [51].
Signaling Pathways and Experimental Workflows
Figure 1: EDC Impact Pathway from Molecular Initiation to Adverse Outcomes
Figure 2: High-Throughput Screening and Analysis Workflow for EDCs
Advanced Data Analysis and Artificial Intelligence
Machine Learning and High-Content Analysis
The complexity of data generated by modern in vitro systems, particularly high-content imaging, requires sophisticated computational approaches for interpretation. Machine learning algorithms have demonstrated remarkable capability in identifying EDCs based on morphological signatures.
Classification Model Performance: In studies using 3D MCF-7 microtissues, machine learning classification models built using estrogenic-associated differential imaging features successfully predicted exposure to estradiol (E2) and propyl pyrazole triol (PPT) with AUC-ROC values of 0.9528 and 0.9513, respectively [49]. These models utilized 140 common differential image features identified between E2 and PPT treatment groups, demonstrating the power of computational approaches to detect subtle, compound-specific morphological changes [49].
Deep Learning Applications: Deep learning algorithms have been developed to characterize specific morphological endpoints, such as microtissue gland lumen formation [49]. These fully automated tools can accurately quantify the number of identified lumens and the total luminal volume of each microtissue, providing robust, quantitative endpoints for estrogenic effect assessment [49].
In Vitro to In Vivo Extrapolation (IVIVE) Using AI
Translating in vitro findings to in vivo responses remains a significant challenge in toxicology. Artificial intelligence frameworks are now enhancing these extrapolations, particularly for EDC risk assessment.
AIVIVE Framework: The AIVIVE (Artificial Intelligence-aided IVIVE) framework integrates generative adversarial networks (GANs) with local optimizers guided by biologically relevant gene modules to improve prediction accuracy [52]. This approach addresses the challenge of subtle, toxicologically relevant gene expression signals that conventional GANs often miss [52]. When applied to rat liver transcriptomic data, AIVIVE demonstrated high overlap with differentially expressed genes, including Cytochrome P450 enzymes, which are often underrepresented in in vitro systems but crucial for understanding EDC metabolism [52].
Performance Metrics: Quantitative evaluation of AIVIVE using cosine similarity, root mean squared error (RMSE), and mean absolute percentage error (MAPE) demonstrated that the synthetic profiles generated were comparable to real biological replicates [52]. Notably, the model slightly outperformed real data in necrosis classification tasks, suggesting its potential for advancing toxicology predictions [52].
Table 2: Performance Metrics of AI Models in Toxicology Applications
| AI Model | Application | Key Metrics | Significance | Reference |
|---|---|---|---|---|
| Machine Learning Classifier | Estrogenic Effect Prediction | AUC-ROC: 0.9528 (E2), 0.9513 (PPT) | Accurate classification based on image features | [49] |
| AIVIVE Framework | In Vitro to In Vivo Extrapolation | High cosine similarity, Low RMSE and MAPE | Recapitulated in vivo CYP expression patterns | [52] |
| Deep Learning Algorithm | Lumen Characterization | Accurate lumen count and volume measurement | Automated high-content analysis | [49] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for In Vitro EDC Research
| Reagent/Category | Specific Examples | Function/Application | Research Context |
|---|---|---|---|
| Cell Culture Media | Phenol-red free DMEM-F12 | Base medium eliminating estrogenic interference | MCF-7 3D microtissue culture [49] |
| Serum Alternatives | DCC-stripped FBS | Removes endogenous hormones to reduce background | Estrogen signaling studies [49] |
| 3D Culture Systems | Non-adhesive agarose hydrogels | Scaffold-free 3D microtissue formation | MCF-7 mammary morphogenesis models [49] |
| Reference EDCs | 17β-estradiol (E2), Propyl pyrazole triol (PPT) | Positive controls for estrogenic activity | Assay validation and calibration [49] |
| Staining Reagents | Hoechst 33342 | Nuclear counterstaining for imaging analysis | 3D microtissue visualization [49] |
| Molecular Biology Kits | RNA extraction kits, RT2 First Strand Kit | Gene expression analysis | Estrogen-responsive gene measurement [49] |
| Primary Cell Sources | Marine medaka pituitary, testis, ovary cells | Target-specific endocrine disruption screening | HPG axis disruption studies [51] |
Advanced in vitro systems, particularly 3D human tissue cultures and high-throughput screening platforms, have transformed EDC research related to infertility and reproductive cancers. These technologies provide more physiologically relevant, efficient, and ethical approaches for identifying and characterizing endocrine disruptors, with machine learning and AI frameworks further enhancing their predictive power and translation to human health outcomes. As the global in vitro toxicology testing market continues to expand—projected to grow from USD 12.99 billion in 2025 to approximately USD 33.13 billion by 2034—continued innovation in these systems will be crucial for addressing the public health challenges posed by widespread EDC exposure [53].
Within the broader context of research on the impact of endocrine-disrupting chemicals (EDCs) on infertility and reproductive cancers, animal models are indispensable for elucidating pathogenic mechanisms and assessing long-term health risks. The Developmental Origins of Health and Disease (DOHaD) hypothesis posits that early-life environmental exposures can shape disease susceptibility later in life [54]. EDCs, a group of natural or synthetic chemicals that can interfere with the hormonal system, are of particular concern. Evidence suggests that exposure to EDCs such as bisphenol A (BPA), phthalates, and pesticides is associated with adverse reproductive health outcomes, including male and female infertility, and increased risk of hormone-sensitive cancers such as those of the breast, ovary, and prostate [12] [55] [56]. Investigating these effects requires sophisticated experimental models that can capture the nuances of transgenerational inheritance and the subtle yet impactful consequences of low-dose exposure, which are often relevant to real-world human exposure scenarios [57]. This guide synthesizes current methodologies and findings from transgenerational and low-dose exposure studies in animal models, providing a technical framework for researchers and drug development professionals working in this critical field.
Transgenerational Inheritance of EDC Effects
Experimental Design and Generational Terminology
A critical aspect of transgenerational studies is the precise definition of exposed generations, which depends on the route and timing of administration [54].
- Multigenerational vs. Transgenerational Effects: Multigenerational effects refer to phenotypes observed in directly exposed generations (F0, F1, and potentially F2 when a pregnant F0 female is exposed). In contrast, transgenerational effects are those observed in generations that were never directly exposed to the original stressor (F3 and beyond when the F0 female is exposed, or F2 and beyond when only the F0 male is exposed) [54]. This distinction is crucial for attributing effects to germline epigenetic inheritance rather than direct exposure.
- Critical Windows of Exposure: The fetus and neonate represent particularly vulnerable populations due to ongoing epigenetic reprogramming events and immature detoxification systems [54]. Exposure during gestation (F0 mother exposes the F1 embryo and its F2 germline) or during germ cell development is a common paradigm to study the origins of transgenerational phenotypes [54].
Table 1: Key EDCs Studied for Transgenerational Effects in Animal Models
| EDC Class | Example Compounds | Primary Exposure Routes in Models | Reported Transgenerational Phenotypes |
|---|---|---|---|
| Plasticizers | Bisphenol A (BPA), Phthalates (DEHP, DBP) | Dietary supplementation, oral gavage | Reproductive tract abnormalities, ovarian defects, sperm count reduction, behavioral changes [54] [57] |
| Pesticides | Vinclozolin, DDT, Methoxychlor | Dietary, subcutaneous injection | Male infertility, kidney disease, ovarian disease, prostate disease [54] [55] |
| Flame Retardants | Organophosphorus flame retardants (OPFRs) | Dietary, oral gavage | Altered hormone homeostasis, reproductive defects [58] |
Figure 1: Experimental design for assessing transgenerational effects. Exposure through the F0 female directly exposes the F1 embryo and F2 germline, making the F3 the first non-exposed generation. Exposure through the F0 male directly exposes only the F1 germline, making the F2 the first non-exposed generation [54].
Molecular Mechanisms of Epigenetic Inheritance
The prevailing hypothesis for transgenerational inheritance involves epigenetic alterations in the germline that escape reprogramming during development [54]. These mechanisms include:
- DNA Methylation: This involves the addition of a methyl group to cytosine bases in a CpG dinucleotide context, catalyzed by DNA methyltransferase (DNMT) enzymes. Promoter methylation is typically associated with transcriptional repression. EDCs can disrupt the erasure, establishment, or maintenance of these marks in primordial germ cells or developing gonads [54]. For example, vinclozolin exposure in rats has been linked to differential DNA methylation regions in sperm across multiple generations.
- Histone Post-Translational Modifications: EDCs can alter the activity of enzymes that add or remove modifications (e.g., acetylation, methylation) to histone proteins, thereby changing chromatin structure and gene accessibility [54]. Ligand-activated transcription factors like estrogen receptors, when bound by EDCs, can recruit chromatin-modifying complexes to specific genomic loci.
- Non-Coding RNAs (ncRNAs): Short and long non-coding RNAs in sperm and oocytes have been implicated as carriers of epigenetic information. These RNAs can regulate gene expression in the zygote and early embryo [54].
The interplay between these mechanisms and their stability across generations remains an active area of investigation. A cross-species review highlights that epigenetic mechanisms are the prevalent means by which EDCs mediate transgenerational effects, though the specific pathways can vary between rodents, fish, and other models [57].
Low-Dose Exposure Paradigms in Animal Models
Defining "Low-Dose" and Its Relevance
The concept of "low-dose" exposure to EDCs is a cornerstone of modern toxicology, reflecting real-world human exposure levels.
- Definition: Low doses are typically those that fall within the range of human environmental exposure or are below the traditional no-observed-adverse-effect-level (NOAEL) established in toxicological studies. These doses can induce subtle but biologically significant effects, particularly when exposure occurs during sensitive developmental windows [54].
- Non-Monotonic Dose Responses (NMDR): A hallmark of EDC action is the NMDR, where the dose-response curve is not linear. Effects at low doses can be absent or even opposite to effects observed at high doses. This phenomenon challenges traditional toxicological risk assessment, which often relies on high-dose studies and linear extrapolation [59].
Methodological Considerations for Low-Dose Studies
- Route of Exposure: It is critical to mimic human exposure routes. Common methods in rodent models include:
- Dietary Supplementation: Incorporating the EDC into the feed, which is considered a natural and sustained exposure route [54].
- Oral Gavage: Direct administration into the stomach via a tube. While it allows precise dosing, it can induce stress in animals, which may confound results [54].
- Subcutaneous Injection: Used for specific protocols, such as studies with vinclozolin [54].
- Dosage Selection: Doses should be informed by biomonitoring data from human populations (e.g., concentrations found in urine, serum, or follicular fluid) to ensure relevance [58]. For example, studies on BPA often use doses in the range of 2-50 µg/kg/day, which are below the current regulatory safe level but within the range detected in humans.
- Critical Timing: Exposure should target specific developmental windows, such as gestation, lactation, or puberty, when organisms are most susceptible to endocrine disruption [54].
Table 2: Quantitative Data from Selected Low-Dose EDC Exposure Studies
| EDC | Animal Model | Dose Range | Exposure Window | Key Reproductive or Oncogenic Findings | Source/Reference Analogue |
|---|---|---|---|---|---|
| Bisphenol A (BPA) | Rat | Low-dose (e.g., 2.5 µg/kg/day) | Perinatal (gestation + lactation) | Altered mRNA for aromatase and 5α-reductase in prefrontal cortex; altered social behavior [60] | Human epidemiological studies [12] |
| DDT | Human (Historical Cohort) | Environmental (from indoor spraying) | Early life (gestation/childhood) | Increased risk of breast cancer (aHR: 1.04), ovarian cancer (aHR: 1.06), and prostate cancer (aHR: 1.05) in adulthood [55] | Taiwan NHIRD Cohort [55] |
| Radiation (Low-dose rate) | Human (Environmental Cohort) | Protracted low-to-moderate dose (mean stomach dose 0.04 Gy) | Chronic environmental exposure | Significant linear dose-response for breast cancer incidence (ERR/Gy = 5.00) [61] | Techa River Cohort [61] |
| Organophosphorus Flame Retardants (OPFRs) | Human (Cohort Study) | Measured urinary metabolites | Adulthood | Disruption of hormone homeostasis in women undergoing IVF [58] | PKU-ERC Cohort [58] |
Signaling Pathways and Mechanisms of Action
EDCs can perturb the endocrine system through multiple pathways, leading to downstream effects on fertility and cancer pathogenesis.
Figure 2: Key signaling pathways perturbed by EDCs. EDCs can act through nuclear receptors to alter gene transcription, activate rapid non-genomic signaling cascades, directly modulate enzyme activity, and induce persistent changes to the epigenome. These initial disruptions converge on downstream effects relevant to infertility and cancer [54] [60] [59].
The Scientist's Toolkit: Research Reagent Solutions
This section details essential materials and reagents for conducting transgenerational and low-dose EDC research, as derived from cited experimental protocols.
Table 3: Essential Research Reagents for EDC Studies
| Reagent/Material | Function/Application | Example in Context |
|---|---|---|
| Certified EDC Standards | High-purity chemicals for dosing solutions and as analytical standards for quantification. | BPA (CAS 80-05-7), Di-(2-ethylhexyl) phthalate (DEHP, CAS 117-81-7), Vinclozolin (CAS 50471-44-8) [54] [59] |
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Gold-standard method for quantifying EDCs and their metabolites in biological matrices (urine, serum, follicular fluid). | Used to measure per- and polyfluoroalkyl substances (PFAS) and organophosphorus flame retardant (OPFR) metabolites in human cohort studies [58]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Quantifying protein hormones and biomarkers in serum/plasma. | Measuring Anti-Müllerian Hormone (AMH), follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol (E2) in rodent or human samples to assess ovarian function [62] [58]. |
| Antibodies for Epigenetic Marks | For chromatin immunoprecipitation (ChIP) and immunostaining to assess histone modifications and DNA methylation patterns. | Antibodies against H3K4me3, H3K27me3, 5-methylcytosine, and 5-hydroxymethylcytosine for analyzing epigenetic changes in germ cells and somatic tissues [54]. |
| RNA/DNA Extraction Kits | Isolating high-quality nucleic acids from low cell-number populations, including germ cells and early embryos. | Critical for downstream transcriptomic (RNA-seq) and epigenomic (whole-genome bisulfite sequencing) analyses [54]. |
| Specific Pathogen-Free (SPF) Animal Diets | Controlled, phytoestrogen-low diets to minimize confounding variables in EDC studies. | Open-formula diets like AIN-93G are often used to ensure consistency and control for background estrogenic activity [54]. |
Animal models employing transgenerational and low-dose exposure paradigms provide powerful, albeit complex, systems for deconstructing the link between EDC exposure and adverse health outcomes like infertility and reproductive cancers. The evidence consolidated in this guide underscores that the timing, dose, and route of exposure are critical determinants of phenotypic outcomes, which can manifest generations removed from the initial insult. The observed multigenerational and transgenerational effects, mediated largely through epigenetic mechanisms, highlight a profound and long-term threat posed by these chemicals. Future research must continue to refine these models, prioritize the testing of EDC mixtures that reflect real-world exposure, and further elucidate the precise molecular bridges between epigenetic marks in the germline and somatic disease phenotypes. The integration of these findings into regulatory science and the development of targeted therapeutic interventions is paramount for mitigating the public health impact of EDCs.
The global decline in reproductive health, including increasing rates of infertility and reproductive cancers, represents a significant public health challenge. Growing evidence suggests that exposure to endocrine-disrupting chemicals (EDCs) is a major contributing factor to this trend [63] [10]. EDCs are exogenous substances that interfere with hormone action, homeostasis, and signaling, leading to adverse health effects [63]. These compounds are pervasive in the environment, found in industrial solvents, plastics, pesticides, personal care products, and even food chains [63] [10].
The systematic identification of reliable biomarkers has become crucial for accurately assessing EDC exposure and its biological effects. Biomarkers serve as measurable indicators of exposure, effect, or susceptibility, providing critical insights into the mechanisms through which EDCs exert their toxicity [64] [65]. The emergence of sophisticated omics technologies has revolutionized this field, enabling comprehensive analysis of biological systems at multiple molecular levels [66] [67]. These technologies offer unprecedented opportunities to discover novel biomarkers, elucidate pathogenic mechanisms, and develop early warning systems for EDC-induced reproductive pathologies.
This technical guide provides an in-depth examination of omics-based approaches for biomarker identification in the context of EDC research, with particular emphasis on their application to infertility and reproductive cancers. By integrating methodologies across genomics, transcriptomics, proteomics, and metabolomics, researchers can develop a systems-level understanding of EDC toxicity, ultimately leading to improved risk assessment, diagnostic capabilities, and preventive strategies.
Major Classes of EDCs
EDCs encompass a diverse array of chemical compounds with varying structures, sources, and environmental persistence. Table 1 summarizes the primary categories of EDCs, their common sources, and documented reproductive health effects.
Table 1: Major Classes of Endocrine-Disrupting Chemicals and Reproductive Health Impacts
| Category | Examples | Primary Sources | Reproductive Health Effects |
|---|---|---|---|
| Heavy Metals | Cadmium, Lead, Mercury | Industrial processes, contaminated water, food chain bioaccumulation | Reduced sperm quality, testicular dysfunction, ovarian toxicity [10] |
| Plasticizers | Bisphenol A (BPA), Phthalates (DEHP) | Food containers, plastics, personal care products | Estrogenic activity, impaired folliculogenesis, reduced sperm count [63] [10] |
| Persistent Organic Pollutants | PCBs, Dioxins, PBDEs | Industrial byproducts, flame retardants, electrical equipment | Altered steroidogenesis, testicular development defects, sperm DNA damage [63] [10] |
| Pesticides & Herbicides | DDT, Methoxychlor, Vinclozolin | Agricultural applications, vector control | Abnormal spermatogenesis, ovarian dysfunction, epigenetic alterations [65] |
| Pharmaceuticals | Diethylstilbestrol (DES), Ketoconazole | Medical treatments, agricultural use | Vaginal clear cell carcinogenesis, reproductive tract abnormalities, impaired folliculogenesis [68] [65] |
Mechanisms of Endocrine Disruption
EDCs exert their adverse effects through multiple interconnected mechanisms. They can directly bind to hormone receptors (estrogen, androgen, thyroid receptors), mimicking or blocking the action of endogenous hormones [63] [65]. For instance, BPA demonstrates structural similarity to estradiol, enabling it to activate estrogen receptors and disrupt normal hormonal signaling [63]. EDCs can also interfere with hormone synthesis, metabolism, and transport, altering the availability of active hormones to target tissues [10]. Furthermore, emerging evidence indicates that EDCs can induce epigenetic modifications, including changes in DNA methylation and histone modifications, which can lead to transgenerational inheritance of reproductive dysfunction [66] [10].
Omics Technologies for Biomarker Discovery
Epigenomics
Epigenomics involves the comprehensive analysis of heritable changes in gene expression that occur without alterations to the DNA sequence itself [66]. Key epigenetic mechanisms include DNA methylation, histone modifications, and non-coding RNA expression. In the context of EDC research, epigenomic approaches have revealed that exposures during critical developmental windows can cause persistent changes in gene regulation that influence disease susceptibility later in life [66].
Experimental Protocol for DNA Methylation Analysis:
- DNA Extraction: Isolate genomic DNA from target tissues (e.g., ovarian cortex, testicular biopsies) or surrogate tissues (e.g., blood, semen)
- Bisulfite Conversion: Treat DNA with sodium bisulfite, which converts unmethylated cytosines to uracils while leaving methylated cytosines unchanged
- Library Preparation & Sequencing: Prepare sequencing libraries using appropriate kits (e.g., Illumina TruSeq Methylation Kit) and perform whole-genome bisulfite sequencing or reduced-representation bisulfite sequencing
- Bioinformatic Analysis: Align sequences to reference genome, identify differentially methylated regions (DMRs), and associate DMRs with gene expression changes and phenotypic outcomes [66]
Transcriptomics
Transcriptomics enables comprehensive profiling of RNA molecules, including messenger RNAs (mRNAs), microRNAs (miRNAs), and long non-coding RNAs (lncRNAs), providing insights into the functional elements of the genome and their dynamic regulation [67]. In EDC research, transcriptomic analyses have identified numerous estrogen-responsive genes that serve as sensitive biomarkers of exposure and effect [65].
Table 2: Transcriptomic Biomarkers for Estrogenic Activity of EDCs
| Biomarker | Tissue/Cell Type | Response to EDCs | Functional Significance |
|---|---|---|---|
| Vitellogenin (VTG) | Liver (fish models) | Induced in male fish by estrogenic EDCs | Classic biomarker of estrogenic exposure [65] |
| Complement C3 | Uterine endometrium | Upregulated by E2 and estrogenic compounds | Involved in immune response; sensitive parameter for estrogenicity [65] |
| pS2 | MCF-7 breast cancer cells | Induced by E2 and estrogenic EDs | Low molecular weight protein; indicator of estrogenic activity [65] |
| Mucin 1 (MUC1) | MCF-7 breast cancer cells | Regulated by E2 via ERE in promoter | Cell surface glycoprotein; breast cancer marker [65] |
| Calbindin-D9k (CaBP-9k) | Uterine tissue | Upregulated by estrogenic compounds | Calcium-binding protein; potential biomarker for uterine EDC effects [65] |
| PRM1, PRM2 | Spermatozoa | Altered expression associated with fertility | Protamine genes crucial for sperm chromatin condensation [67] |
Experimental Protocol for RNA-Sequencing:
- RNA Extraction: Isolate total RNA from tissues or cell cultures using TRIzol reagent or commercial kits; assess RNA quality (RIN > 8)
- Library Preparation: Deplete ribosomal RNA or enrich mRNA, fragment RNA, synthesize cDNA, and add sequencing adapters
- Sequencing: Perform high-throughput sequencing on platforms such as Illumina NovaSeq or NextSeq
- Bioinformatic Analysis: Quality control (FastQC), alignment (STAR, HISAT2), differential expression analysis (DESeq2, edgeR), pathway enrichment analysis (GSEA, DAVID) [68] [67]
Proteomics
Proteomics involves the large-scale study of proteins, including their structures, functions, expression levels, and modifications. Since proteins directly execute cellular functions, proteomic analyses often provide more functional insights than transcriptomic approaches alone [67]. In reproductive toxicology, proteomic studies have identified numerous protein biomarkers associated with EDC exposure and reproductive dysfunction.
Experimental Protocol for Proteomic Analysis:
- Protein Extraction: Lyse tissues or cells in appropriate buffer (e.g., RIPA buffer with protease inhibitors)
- Protein Separation: Use 1D/2D gel electrophoresis (SDS-PAGE) or liquid chromatography (LC) for separation
- Protein Digestion: Perform in-gel or in-solution tryptic digestion
- Mass Spectrometry Analysis: Utilize LC-MS/MS (e.g., Q-Exactive Orbitrap) for protein identification and quantification
- Data Analysis: Identify differentially expressed proteins using software (MaxQuant, Proteome Discoverer), perform functional annotation (GO, KEGG), and validate candidates by Western blot or ELISA [67]
Metabolomics
Metabolomics focuses on the comprehensive analysis of small-molecule metabolites, providing a direct readout of cellular activities and physiological status. As the final downstream product of gene expression, metabolomic profiles are considered closest to the actual phenotype [67]. In EDC research, metabolomic approaches have identified metabolic signatures associated with reproductive toxicity.
Experimental Protocol for Metabolomic Analysis:
- Sample Preparation: Extract metabolites from biofluids (seminal plasma, follicular fluid) or tissues using appropriate solvents (methanol, acetonitrile)
- Metabolite Separation: Employ gas chromatography (GC) or liquid chromatography (LC) coupled to mass spectrometry
- Data Acquisition: Perform untargeted or targeted metabolomic profiling using platforms such as GC-MS or LC-MS
- Data Analysis: Process raw data (XCMS, MetaboAnalyst), identify significantly altered metabolites, and map to biochemical pathways (KEGG, HMDB) [67]
Integrated Multi-Omics Approaches
The integration of multiple omics datasets provides a more comprehensive understanding of the complex biological responses to EDC exposure. Integrated multi-omics analysis enables researchers to connect molecular changes across different regulatory levels, revealing coordinated pathway alterations and network perturbations that would not be apparent from single-omics studies alone [67]. For instance, a recent multi-omics study in bull spermatozoa identified several fertility-related biomarkers, including genes (RPLP0, RPL8, RPL31), proteins (TP6V1C1, PFKL, ACADS), and metabolites (Taurine, Hypotaurine) that were consistently associated with reproductive function [67].
Diagram 1: Integrated multi-omics workflow for biomarker discovery in EDC research. This framework enables comprehensive molecular profiling and biological insight generation.
Case Studies: Omics Applications in EDC Research
Ovarian Toxicity Biomarkers
A recent study investigated the effects of EDCs on human ovarian cortex using in vitro models [68]. Ovarian tissue was exposed to diethylstilbestrol (DES) and ketoconazole (KTZ), followed by transcriptomic analysis using RNA-sequencing. The study revealed 445 and 233 differentially expressed genes in DES and KTZ exposed groups, respectively. Gene set variation analysis showed that both chemicals modulated pathways important for folliculogenesis and steroidogenesis. The researchers identified stearoyl-CoA desaturase (SCD) and 7-dehydrocholesterol reductase (DHCR7) as potential novel human-relevant biomarkers of EDC exposure and effects on ovaries, with SCD showing upregulation in growing follicles in exposed ovarian tissue [68].
Male Reproductive Health Biomarkers
In male reproduction, omics approaches have identified numerous biomarkers associated with EDC exposure and fertility status. Genomics studies have revealed fertility-associated SNPs in genes such as ETNK1, PSEN1, and USH2A [67]. Transcriptomic analyses of spermatozoa have identified differential expression of PRM1, PRM2, and EFNA1 in individuals with fertility impairments [67]. Proteomic studies have highlighted the importance of proteins such as Tektin, Annexin A5, and Calmodulin in sperm function, with altered expression linked to EDC exposure [67]. Metabolomic profiling has identified Taurine, Azelaic acid, and L-cysteine as important metabolites associated with sperm quality and fertility [67].
Diagram 2: Key events and mechanistic pathways linking EDC exposure to adverse reproductive health outcomes.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Omics-Based Biomarker Discovery
| Category | Specific Tools/Reagents | Application | Key Features |
|---|---|---|---|
| Sequencing Platforms | Illumina NovaSeq, NextSeq; PacBio Sequel | Genomics, Transcriptomics, Epigenomics | High-throughput, single-nucleotide resolution, various read lengths |
| Mass Spectrometry Systems | Q-Exactive Orbitrap, TripleTOF, GC-MS | Proteomics, Metabolomics | High mass accuracy, sensitivity, quantitative capabilities |
| Separation Techniques | 2D-PAGE, HPLC, UPLC, LC-MS | Proteomics, Metabolomics | High-resolution separation of complex mixtures |
| Bioinformatics Tools | FastQC, DESeq2, MaxQuant, XCMS, MetaboAnalyst | Data analysis across all omics domains | Quality control, statistical analysis, pathway mapping, data integration |
| Cell/Tissue Models | MCF-7 cells, primary ovarian cells, ovarian cortex culture | In vitro screening of EDCs | Human-relevant systems for mechanistic studies [68] [65] |
| Animal Models | Zebrafish, rat models | In vivo validation of biomarkers | Controlled exposure studies, tissue accessibility [63] [65] |
The application of omics technologies has fundamentally transformed our approach to biomarker discovery for EDC exposure and effect assessment. By enabling comprehensive molecular profiling at multiple biological levels, these approaches provide unprecedented insights into the mechanisms through which EDCs contribute to infertility and reproductive cancers. The integration of epigenomic, transcriptomic, proteomic, and metabolomic data offers particular promise for identifying robust biomarker signatures that reflect both exposure history and disease susceptibility.
As the field advances, key challenges remain, including the need for improved biomonitoring strategies, better understanding of mixture effects, and validation of transgenerational impacts in human populations [10]. Nevertheless, the systematic application of omics technologies, coupled with rigorous bioinformatic analysis and functional validation, holds immense potential for developing clinically relevant biomarkers that can inform risk assessment, guide regulatory decisions, and ultimately protect reproductive health across generations.
Endocrine-disrupting chemicals (EDCs) represent a class of environmental compounds that can interfere with hormonal signaling, and a growing body of evidence demonstrates that they exert profound effects on female reproductive health through epigenetic modifications, particularly DNA methylation [69] [70]. These chemicals—including bisphenol A (BPA), phthalates, dioxins, polychlorinated biphenyls (PCBs), and diethylstilbestrol (DES)—are ubiquitous in household and industrial products, leading to widespread human exposure [69]. The epigenetic framework is critically important for understanding disease etiology because it provides a mechanistic link between environmental exposures and pathological outcomes, explaining how EDCs can permanently reprogram gene expression patterns without altering the underlying DNA sequence [69] [71].
DNA methylation, the most extensively studied epigenetic mechanism, involves the addition of a methyl group to the cytosine base in CpG dinucleotides, predominantly within gene promoter regions [71]. This modification typically leads to transcriptional silencing when it occurs in promoter-associated CpG islands, effectively turning off tumor suppressor genes or developmental regulators [71]. In the context of reproductive pathologies, EDCs have been shown to disrupt normal DNA methylation patterns, leading to aberrant gene expression in uterine and ovarian tissues, which subsequently contributes to the development of endometriosis, endometrial hyperplasia, uterine fibroids, infertility, and recurrent pregnancy loss [69]. This technical guide provides a comprehensive resource for researchers investigating the intricate relationships between EDC exposure, DNA methylation alterations, and female reproductive pathologies, with a focus on methodological approaches and pathological mechanisms relevant to drug discovery and diagnostic development.
Analytical Methods for DNA Methylation Mapping
The precise mapping of DNA methylation patterns requires sophisticated technologies that can detect 5-methylcytosine (5mC) and its oxidative derivatives at base-pair resolution across the genome [72]. Several complementary approaches have been developed, each with distinct advantages, limitations, and applications in epigenetic research.
Foundational Principles of Methylation Detection
DNA methylation analysis relies on three principal strategies for distinguishing methylated from unmethylated cytosines: bisulfite conversion, restriction enzyme digestion, and affinity enrichment [73]. Bisulfite treatment remains the gold standard approach, chemically converting unmethylated cytosines to uracils while leaving methylated cytosines unchanged, thereby creating sequence differences that can be detected through subsequent PCR amplification and sequencing [72] [71]. Restriction enzyme-based methods utilize methylation-sensitive endonucleases (e.g., HpaII) that cleave only unmethylated recognition sites, or their methylation-insensitive isoschizomers (e.g., MspI) that cut regardless of methylation status, enabling comparative analysis [73]. Affinity enrichment techniques employ antibodies specific to 5mC (methylated DNA immunoprecipitation, MeDIP) or methyl-binding domain proteins (MBD-seq) to selectively capture methylated DNA fragments for downstream analysis [72].
Advanced Sequencing Technologies
Next-generation sequencing platforms have revolutionized epigenomic studies by enabling whole-genome methylation profiling at single-base resolution. As illustrated in Table 1, each method offers distinct advantages for particular research applications.
Table 1: High-Resolution DNA Methylation Sequencing Technologies
| Technology | Principle | Resolution | Advantages | Limitations |
|---|---|---|---|---|
| Whole-Genome Bisulfite Sequencing (WGBS) | Bisulfite conversion followed by whole-genome sequencing | Base-level | Comprehensive coverage; quantitative | High cost; DNA degradation during bisulfite treatment [72] |
| EM-Seq | Enzymatic conversion instead of bisulfite | Base-level | Reduced DNA damage; maintains integrity | Newer method with less established protocols [72] |
| TAPS | Chemical conversion without bisulfite | Base-level | Minimal DNA damage; high-quality libraries | Requires specialized chemistry [72] |
| MeDIP-Seq | Antibody-based enrichment of methylated DNA | ~100-300 bp | Cost-effective for large samples; no conversion needed | Lower resolution; antibody specificity issues [72] |
| Pyrosequencing | Bisulfite conversion with sequence-based quantification | Base-level for targeted regions | Highly quantitative; accurate methylation percentages | Limited to predefined genomic regions [74] [75] |
Third-generation sequencing technologies, such as single-molecule real-time (SMRT) sequencing and nanopore sequencing, offer promising alternatives by directly detecting epigenetic modifications without requiring bisulfite conversion, thereby preserving DNA integrity and providing longer read lengths that facilitate assembly of complex genomic regions [72] [71]. However, these approaches currently face challenges in achieving the accuracy and cost-effectiveness of established NGS-based methods [72].
Experimental Protocols for Targeted DNA Methylation Analysis
For researchers investigating specific candidate genes or pathological pathways, targeted methylation analysis provides a cost-effective strategy with enhanced sequencing depth for detecting subtle methylation changes. The following section outlines established protocols for locus-specific DNA methylation analysis in reproductive tissues.
Bisulfite Pyrosequencing for Quantitative Methylation Assessment
Bisulfite pyrosequencing represents a highly accurate and quantitative method for analyzing DNA methylation at multiple adjacent CpG sites within a defined genomic region [74] [75]. This technique has been successfully applied in numerous studies investigating perinatal epigenetic programming and reproductive pathologies [74] [75]. The experimental workflow proceeds through the following critical stages:
DNA Extraction and Bisulfite Conversion: Genomic DNA is isolated from target tissues (umbilical cord, endometrial biopsies, placental samples) using classical proteinase K digestion and phenol:chloroform extraction or commercial kits [74]. Subsequently, 500-1000 ng of DNA undergoes bisulfite treatment using commercial kits (e.g., EZ DNA Methylation Kit, Zymo Research), which converts unmethylated cytosines to uracils while preserving methylated cytosines [76] [75]. The conversion reaction typically involves incubation in a thermal cycler for 14-16 hours, followed by desulphonation, purification, and elution in a final volume of 10-20 μL [76].
PCR Amplification of Target Region: Bisulfite-converted DNA is amplified using sequence-specific primers designed to flank the CpG sites of interest. The PCR reaction mixture typically contains Hotstart Plus DNA polymerase, dNTPs, reaction buffer, and forward/reverse primers (one of which is biotinylated to enable subsequent immobilization) [74] [75]. Thermal cycling conditions consist of an initial activation step at 95°C for 15 minutes, followed by 40-45 cycles of denaturation (95°C for 30 seconds), annealing (primer-specific temperature for 60 seconds), and extension (72°C for 60 seconds) [76].
Pyrosequencing and Quantification: The biotinylated PCR products are immobilized on streptavidin-coated sepharose beads, denatured to yield single-stranded DNA, and incubated with a sequencing primer that is complementary to the region adjacent to the target CpG sites [74] [75]. Pyrosequencing is performed on specialized instrumentation (Pyromark MD, Qiagen) that sequentially introduces nucleotides while detecting incorporation through light emission. The resulting pyrograms provide quantitative methylation percentages for each CpG site using the formula: % methylation = C/(C+T) × 100%, where C and T represent the respective nucleotide signals at each position [74].
The following workflow diagram illustrates the key experimental steps in bisulfite pyrosequencing:
Methylation-Specific PCR (MSP) for Rapid Detection
Methylation-specific PCR provides a simpler, more rapid approach for detecting the methylation status of specific gene promoters [76]. This technique involves:
- Bisulfite Conversion: DNA is treated with sodium bisulfite as described above.
- PCR with Methylation-Specific Primers: Two parallel PCR reactions are performed using primers that specifically recognize either the methylated (containing guanine at cytosine positions) or unmethylated (containing adenine at uracil positions) sequence after bisulfite conversion.
- Detection and Analysis: Amplification products are separated by agarose gel electrophoresis, with the presence of a band in the methylated reaction indicating methylation at the target locus.
For quantitative analysis, real-time MSP utilizing SYBR Green or TaqMan chemistry can be employed, with methylation percentage calculated using the formula: Methylation % = 100/[1 + 2^ΔCT (meth-unmeth)]%, where ΔCT represents the difference in threshold cycles between methylated and unmethylated reactions [76].
Key Findings: DNA Methylation Patterns in Specific Reproductive Pathologies
Research over the past two decades has established compelling associations between aberrant DNA methylation patterns and various female reproductive disorders, with EDC exposure identified as a significant contributing factor. Table 2 summarizes key epidemiological and experimental findings linking specific EDCs, methylation changes, and reproductive pathologies.
Table 2: EDC-Associated DNA Methylation Changes in Female Reproductive Pathologies
| Reproductive Pathology | EDC Exposure | Methylation Alterations | Functional Consequences | Study Type |
|---|---|---|---|---|
| Endometriosis | BPA, phthalates (MEHP, DEHP) | Altered expression of miR-185, miR-142-3p, miR-15a-5p; hypermethylation of progesterone receptor gene | Increased matrix metalloproteinase (MMP2, MMP9) expression; reduced endometrial receptivity [69] | Human case-control studies [69] |
| Uterine Fibroids | DES, OPEs, APs, phthalates | Hypermethylation of tumor suppressor gene promoters | Increased proliferation of myometrial cells; tumor development [69] | Human prospective studies [69] |
| Recurrent Pregnancy Loss | BPA analogues (BPAF, BPAP), phthalates | Hypomethylation of imprinted genes; altered H19 methylation | Disrupted placental development; impaired embryo implantation [69] | Human case-control studies [69] |
| Female Infertility | Parabens, phthalates, BPA | Decreased methylation of ERα gene promoter; aberrant methylation of HOXA10 | Endometrial dysfunction; defective uterine receptivity [69] [70] | Human cohort studies [69] |
| Premature Ovarian Insufficiency | Pesticides, dioxins | Hypermethylation of folliculogenesis-related genes (e.g., BMP15, GDF9) | Impaired oocyte maturation; reduced ovarian reserve [70] | Animal and in vitro studies [70] |
The CDKN2A/ANRIL locus on chromosome 9p21 represents a particularly significant region where perinatal DNA methylation patterns predict later-life health outcomes [74] [75]. Research in the Southampton Women's Survey cohort demonstrated that DNA methylation at birth within the promoter of ANRIL, a long non-coding RNA, predicts markers of cardiovascular risk at 9 years of age [75]. Specifically, higher methylation at CpG5 was associated with increased pulse wave velocity (β = 0.066 m/s per 10% methylation increase, p = 0.037), while decreased methylation at CpG1 and CpG2 was associated with elevated heart rate (β = 1.93-2.30 beats/min per 10% methylation decrease, p = 0.033-0.041) [75]. Given the common developmental origins of reproductive and cardiovascular diseases and the role of ANRIL in cellular senescence, these findings suggest that similar epigenetic mechanisms may underlie reproductive pathologies [74] [77].
The following diagram illustrates the mechanistic relationship between EDC exposure, epigenetic alterations, and reproductive pathologies:
To facilitate high-quality research in epigenetic reproductive toxicology, Table 3 compiles key research reagents and methodologies employed in the field.
Table 3: Essential Research Reagents and Resources for Epigenetic Reproductive Studies
| Reagent/Resource | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| DNA Methylation Kits | EZ DNA Methylation Kit (Zymo Research); MethylEdge Bisulfite Conversion System (Promega) | Bisulfite conversion of genomic DNA for downstream methylation analysis | Conversion efficiency must be validated; DNA degradation should be minimized [74] [76] |
| Pyrosequencing Systems | PyroMark Q96 MD (Qiagen); specific assays for ANRIL, CDKN2A, HOXA10 promoters | Quantitative methylation analysis at multiple adjacent CpG sites | Requires biotinylated primers; provides quantitative data for 50-100bp regions [74] [75] |
| Methylation-Specific PCR Primers | Designed for methylated/unmethylated sequences of target genes (e.g., p14/ARF, p15INK4b, p16INK4a) | Rapid detection of methylation status in specific gene promoters | Primer specificity is critical; validation with positive controls required [77] [76] |
| Cell Line Models | SaOS-2 osteosarcoma cells (for bone density studies); Ishikawa endometrial cells; primary human endometrial stromal cells | Functional validation of epigenetic findings in relevant cellular contexts | Cell type-specific methylation patterns should be considered [74] |
| EDC Exposure Reagents | Bisphenol A (BPA); diethylstilbestrol (DES); di-(2-ethylhexyl) phthalate (DEHP) | Controlled exposure studies to establish causal relationships | Dose-response relationships should be explored; physiological relevance of concentrations [69] [70] |
Epigenetic mapping of DNA methylation patterns has revolutionized our understanding of reproductive pathology pathogenesis, particularly in elucidating the mechanistic links between EDC exposure and disease development. The methodologies outlined in this technical guide—from genome-wide bisulfite sequencing to targeted pyrosequencing—provide powerful tools for identifying novel diagnostic biomarkers and therapeutic targets. As research in this field advances, integrating multi-omics approaches that combine DNA methylation analysis with histone modification profiling and non-coding RNA expression will further enhance our ability to decipher the complex epigenetic circuitry underlying reproductive diseases. For drug development professionals, these epigenetic insights offer promising avenues for designing targeted epigenetic therapies and intervention strategies that may mitigate the adverse reproductive health effects associated with environmental EDC exposure.
Endocrine-disrupting chemicals (EDCs) represent a significant public health concern due to their ability to interfere with hormonal homeostasis and reproductive physiology [14]. The World Health Organization has recognized infertility as a public health priority, with male factors accounting for over half of all cases and female reproductive disorders showing alarming increases [14] [29]. Research confirms that EDCs contribute to declining male reproductive health, with a groundbreaking meta-analysis revealing an approximately 50% drop in sperm concentration in males from industrialized regions between 1973 and 2011 [14]. Similarly, female reproductive disorders including polycystic ovary syndrome (PCOS), premature ovarian failure, and infertility have been linked to EDC exposure, with PCOS prevalence reaching up to 20% in some regions [29].
The challenge of assessing EDC risks is compounded by several factors: EDCs act through multiple interconnected mechanisms including receptor-mediated disruption, oxidative stress, apoptosis, and epigenetic modifications; humans are exposed to complex mixtures of EDCs throughout their lifetimes, yet regulatory frameworks often fail to account for combined effects; and traditional toxicity testing methods are expensive, time-consuming, and raise ethical concerns regarding animal use [14] [78] [29]. Computational approaches have therefore become essential tools for screening chemical hazards, prioritizing compounds for further testing, and understanding the complex mechanisms through which EDCs impact reproductive health and contribute to cancers.
AI and Machine Learning Approaches for Predictive Toxicology
Advanced Deep Learning Architectures
Traditional quantitative structure-activity relationship (QSAR) models that rely on predefined molecular descriptors have limitations in capturing the complexity of reproductive and developmental toxicity [79]. Recent advances in deep learning have enabled the development of descriptor-free models that directly process molecular structures as graphs, with atoms as nodes and bonds as edges [78] [79]. The Communicative Message Passing Neural Network (CMPNN) framework incorporates a communicative kernel and message booster module to capture multi-level molecular relationships, achieving state-of-the-art performance in reproductive toxicity prediction with a mean AUC of 0.946 and accuracy of 0.857 on independent test sets [78].
Graph Convolutional Networks (GCNs) represent another significant advancement, utilizing message-passing mechanisms to aggregate feature information from neighboring nodes and edges, dynamically updating node representations to capture both local and global molecular structures [79]. Recent implementations have enhanced standard GCNs through multi-head attention mechanisms that assign varying importance to atomic contexts and gated skip-connections that preserve information flow through deep networks [79]. These architectural improvements have demonstrated exceptional performance, with one GCN model achieving 81.19% accuracy on a diverse test set of 4,514 compounds [79].
Table 1: Performance Comparison of AI Models for Reproductive Toxicity Prediction
| Model Architecture | Dataset Size | Accuracy | AUC | F1 Score | Key Advantages |
|---|---|---|---|---|---|
| CMPNN [78] | 2,154 compounds | 0.857 | 0.946 | 0.846 | Captures multi-level molecular relationships |
| GCN with Multi-head Attention [79] | 4,514 compounds | 0.812 | - | - | Identifies toxicologically relevant substructures |
| Traditional Machine Learning (RF, XGBoost) [78] | 2,154 compounds | Mediocre | - | - | Interpretable but limited performance |
Model Interpretability and Mechanistic Insights
A significant challenge in applying deep learning models for regulatory purposes has been their "black-box" nature [79]. Recent research has addressed this limitation through sophisticated interpretation techniques that identify structural alerts—chemical substructures known to be associated with toxicity. By integrating these alerts directly into model architectures, researchers have developed approaches that not only predict toxicity but also provide insights into potential mechanisms of action [79].
Advanced interpretation methods include mask optimization techniques that identify subgraphs significantly impacting model decisions and Louvain community detection algorithms that evaluate structural unit contributions to predicted toxicity [79]. These approaches help bridge the gap between model predictions and chemical interpretability, making AI tools more valuable for both screening and mechanistic studies. The identification of specific structural features associated with reproductive toxicity enables medicinal chemists to design safer chemicals and helps toxicologists generate hypotheses about molecular initiating events in adverse outcome pathways [79].
Mixture Risk Assessment of EDCs
The Complex Challenge of Chemical Mixtures
Humans are consistently exposed to complex mixtures of EDCs throughout their lifetimes, yet traditional risk assessment methods typically evaluate chemicals in isolation [29]. This represents a significant limitation because EDCs can exhibit additive, synergistic, or antagonistic effects when combined. The European RiskMix project exemplifies initiatives aiming to evaluate effects of multiple simultaneous exposures to contaminant mixtures within the exposome framework [80]. Research from Costa Rica demonstrates the real-world implications, showing reduced fertility among agricultural workers and higher prevalence of male infertility in regions with intensive pesticide use [80].
The timing of exposure is particularly critical for reproductive outcomes. Developmental windows such as fetal development, puberty, and pregnancy represent periods of heightened susceptibility to EDCs [29] [26]. Sexual differentiation is highly dependent on the fetal hormonal environment, establishing the foundation for lifelong reproductive health. EDC exposure during these sensitive windows can cause developmental disturbances that manifest as reproductive disorders at birth or later in life [26]. In females, exposure to pesticide mixtures has been associated with menopause arriving 1.9-3.8 years earlier, indicating significantly shortened reproductive lifespans [29].
Computational Approaches for Mixture Risk Assessment
While traditional mixture risk assessment has relied on in vivo and in vitro models, computational approaches are increasingly important for screening and prioritizing combinations for experimental validation [80]. The integration of biomonitoring data with AI-driven analysis enables identification of common mixture patterns in human populations and prediction of their potential effects. Computational models can incorporate data from high-throughput screening assays that measure effects on specific biological pathways, such as estrogen receptor binding or steroidogenic enzyme inhibition [14] [81].
The transition from whole-animal testing to computational approaches is being driven by both ethical considerations and regulatory mandates. The U.S. Food and Drug Administration has announced plans to assess toxicity with AI-based computational models instead of animal studies, describing this shift as "a win-win for public health and ethics" [78]. Similarly, the European Union's REACH regulation now explicitly requires justification for animal testing, effectively making computational models a regulatory necessity [78].
Table 2: Key EDC Classes and Their Impacts on Reproductive Health
| EDC Class | Common Sources | Key Reproductive Effects | Mechanisms of Action |
|---|---|---|---|
| Phthalates [14] [82] | Plastics, personal care products | Reduced sperm motility, decreased testosterone, earlier menopause [14] [29] | Androgen receptor antagonism, steroidogenic enzyme inhibition [14] |
| Bisphenol A (BPA) [14] [81] | Food and beverage containers, thermal paper | Altered ovarian function, impaired embryonic implantation, reduced sperm quality [14] [82] | Estrogen receptor binding, genomic and non-genomic signaling disruption [14] [81] |
| Organochlorine Pesticides [29] [82] | Agricultural applications, persistent environmental contaminants | Earlier puberty, PCOS, endometriosis, testicular cancer [29] [26] | Estrogen receptor activation, altered gonadotropin signaling [29] |
| Per- and Polyfluoroalkyl Substances (PFAS) [78] [29] | Non-stick coatings, water-repellent fabrics, fire-fighting foams | Impaired testicular and ovarian development, reduced birth weight, infertility [78] [29] | Thyroid hormone disruption, peroxisome proliferator-activated receptor activation [29] |
Experimental Protocols and Methodologies
Protocol: Deep Learning Model Development for Reproductive Toxicity Prediction
Objective: To develop a graph-based deep learning model for predicting reproductive and developmental toxicity potential of chemical compounds.
Data Collection and Curation:
- Source Data Extraction: Collect reproductive toxicity classifications from government databases including the European Chemicals Agency (ECHA), National Institute of Technology and Evaluation (NITE) of Japan, Hazardous Chemical Information System (HCIS) of Australia, and National Institute of Environmental Research (NIER) of Korea [79].
- Classification Harmonization: Apply the Globally Harmonized System (GHS) categories for reproductive toxicity (1A, 1B, 2) as positive cases, with conflicting classifications removed from the dataset [79].
- Data Augmentation: Address class imbalance by incorporating additional negative data from the CompTox Dashboard's Safety Chemical list (DNTPOTNEG, SCOGSLIST, SCILGREENHALFCIRCLE, SCILGREENCIRCLE) [79].
- Quality Control: Verify negative data reliability by cross-referencing GHS labels through PubChem to confirm absence of reproductive or developmental toxicity [79].
Model Architecture and Training:
- Graph Representation: Convert Simplified Molecular Input Line Entry System (SMILES) strings to molecular graphs with atoms as nodes and bonds as edges [78] [79].
- Network Configuration: Implement a Graph Convolutional Network with multi-head attention mechanisms and gated skip-connections to capture complex structural patterns [79].
- Structural Alert Integration: Incorporate known toxic substructures directly into the model to guide learning of toxicologically relevant features [79].
- Validation Framework: Employ stratified 5-fold cross-validation to assess model performance and generalizability [79].
- Interpretation Methods: Apply mask optimization and Louvain community detection to identify subgraphs influencing model predictions [79].
Protocol: In Vitro Mixture Risk Assessment Using Aquatic Models
Objective: To evaluate the effects of combined exposures to EDC mixtures on reproductive capacity using in vitro aquatic models.
Mixture Design and Preparation:
- Priority Compound Selection: Review human biomonitoring studies conducted over the past 25 years to identify frequently detected pesticides with potential reproductive health impacts [80].
- Mixture Formulation: Prepare both reference mixtures (e.g., from the European RiskMix project) and local mixtures based on prioritization of pesticides detected in human fluids [80].
- Concentration Determination: Set exposure concentrations based on environmental relevance and human biomonitoring data rather than maximum tolerated doses [80].
Experimental Assessment:
- Endpoint Selection: Focus on reproductive capacity metrics including fertilization success, embryonic development, and morphological abnormalities [80].
- Mixture Ratio Maintenance: Keep ratios of mixture components consistent with detected environmental or human tissue concentrations [80].
- Statistical Analysis: Apply appropriate mixture statistical methods to identify interactions (additive, synergistic, antagonistic) between mixture components [80].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Computational EDC Research
| Tool/Category | Specific Examples | Function/Application | Research Context |
|---|---|---|---|
| AI/ML Frameworks | CMPNN, GCN with Multi-head Attention, Gated Skip-connections [78] [79] | Prediction of reproductive toxicity from chemical structure | Deep learning model development for chemical safety screening |
| Toxicity Databases | ECHA, NITE, HCIS, NIER GHS classifications [79] | Source of curated reproductive toxicity data for model training | Building benchmark datasets for QSAR and deep learning models |
| Molecular Representations | SMILES, Molecular Graphs (Atom Nodes, Bond Edges) [78] [79] | Standardized representation of chemical structures for computational analysis | Input data preparation for graph-based neural networks |
| Structural Alert Libraries | Empirical toxicity data, Known toxic substructures [79] | Identification of chemical features associated with reproductive toxicity | Model interpretation and mechanistic hypothesis generation |
| Validation Methodologies | Stratified 5-fold Cross-validation, Repeated Nested Cross-validation [78] [79] | Robust assessment of model performance and generalizability | Ensuring predictive reliability and regulatory acceptance |
| Mixture Design Tools | Human biomonitoring data, Exposure reconstruction algorithms [80] [29] | Development of environmentally relevant mixture ratios for testing | Creating realistic exposure scenarios for cumulative risk assessment |
The integration of AI and computational approaches represents a paradigm shift in how we assess and manage risks from endocrine-disrupting chemicals. Deep learning models that directly process molecular structures as graphs have demonstrated remarkable performance in predicting reproductive toxicity, achieving accuracies exceeding 80% [78] [79]. These advances come at a critical time when global regulatory agencies are actively transitioning away from animal testing toward computational methods [78].
The future of EDC risk assessment will require increased focus on mixture effects and cumulative impacts across the lifespan. As one study notes, regulatory frameworks must move toward approaches that account for cumulative effects, which are critical in real-world exposure scenarios [29]. Computational methods will be essential for prioritizing chemical combinations for experimental validation and for understanding the complex interactions between EDCs and biological systems.
For researchers studying the impact of EDCs on infertility and reproductive cancers, these computational tools offer unprecedented opportunities to identify hazardous chemicals before widespread population exposure, generate mechanistic hypotheses about molecular initiating events in adverse outcome pathways, and design safer alternative chemicals through predictive toxicology. As the field advances, the integration of biomonitoring data, computational predictions, and targeted experimental validation will provide a more comprehensive understanding of how EDCs contribute to reproductive disorders and cancers, ultimately supporting evidence-based public health protections.
Human biomonitoring (HBM) serves as an essential tool for making evidence-based policy decisions upon assessment of human exposure to pollutants, particularly endocrine-disrupting chemicals (EDCs) linked to infertility and reproductive cancers [83]. The accurate interpretation and comparability of biomarkers of exposure and effect depend on harmonized, quality-assured sampling, processing, and analysis across studies [84]. As global chemical industry continues to expand—surpassing $5 trillion in 2017—the need for reliable HBM data to inform chemical risk assessment and protect reproductive health becomes increasingly urgent [83]. Within the context of infertility and reproductive cancers research, HBM provides critical exposure assessment data that helps elucidate the relationship between EDC body burdens and adverse reproductive outcomes, thereby strengthening the evidence base for regulatory action and clinical interventions.
The complex relationship between EDC exposure and reproductive pathologies necessitates precise exposure assessment methods. Epidemiological studies have consistently associated EDCs such as bisphenol A (BPA), phthalates, per- and polyfluoroalkyl substances (PFAS), and persistent organic pollutants (POPs) with impaired semen quality, decreased ovarian reserve, infertility, polycystic ovary syndrome (PCOS), and altered hormone levels [6]. These chemicals have been detected in human biological matrices including adipose tissue, blood, breast milk, and follicular fluid, explaining their prevalent presence in the human body and potential impact on reproductive tissues [29] [82]. By quantifying internal doses of EDCs, HBM moves beyond environmental concentration estimates to provide personalized exposure data that accounts for all exposure routes and individual metabolic differences, making it particularly valuable for investigating the impact of EDCs on susceptible clinical populations.
Fundamental Pillars of Quality Assurance in HBM
Reliable HBM data rests on three main quality assurance/quality control (QA/QC) pillars: application of validated reference methods, participation in proficiency testing (PT) schemes, and use of certified reference materials (CRMs) [83]. These components work synergistically to ensure the accuracy, precision, and comparability of data across different studies and laboratories, which is essential for pooling data, tracking temporal trends, and making valid inferences about exposure-disease relationships. The current HBM landscape faces challenges related to a limited number of established reference methods and a lack of relevant CRMs, particularly for novel biomarkers and complex matrices [83].
Table 1: Quality Assurance Pillars for HBM of EDCs
| QA Component | Current Status | Key Challenges |
|---|---|---|
| Reference Methods | Limited availability; JCTLM lists methods only for metals (Cd, Hg, Pb in blood/urine) [83] | Few standardized methods for organic EDCs (e.g., BPA, PFAS, phthalates) |
| Proficiency Testing (PT) | Multiple schemes available through EPTIS database; used to assess laboratory performance [83] | Consensus values not always metrologically traceable; multiple rounds often needed for performance improvement |
| Certified Reference Materials (CRMs) | Available for some analytes in blood, urine, serum; gaps for many EDCs in breast milk, hair [83] | Chicken-and-egg dilemma: need validated methods for CRM certification, but need CRMs for method validation |
The heterogeneity of data reliability across studies has been identified as a weakness in current HBM research [83]. To address this, initiatives like the European Partnership for the Assessment of Risks from Chemicals (PARC) include specific tasks dedicated to QA/QC [83]. Similarly, the International Society of Exposure Science HBM Working Group has established a global network to develop guidance on minimum information requirements for HBM studies (MIR-HBM), covering all phases from design to communication of results [84]. Implementation of these harmonized approaches is critical for generating data that can reliably inform clinical and public health decisions regarding EDC exposure and reproductive health risks.
HBM Matrices and Analytical Considerations for Reproductive Health Research
The selection of appropriate biological matrices is crucial for assessing EDC exposure in clinical populations focused on infertility and reproductive cancers. Different matrices provide distinct temporal exposure windows and vary in their analytical complexity, making certain matrices more suitable for specific research questions in reproductive epidemiology.
Table 2: Biological Matrices for EDC Biomonitoring in Reproductive Health Research
| Matrix | Exposure Window | Advantages | Limitations for Reproductive Studies |
|---|---|---|---|
| Urine | Recent exposure (hours to days) | Non-invasive; large volumes available; suitable for non-persistent chemicals | Requires correction for dilution; may miss peak exposures |
| Blood (serum/plasma) | Intermediate to long-term | Integrated exposure measure; suitable for persistent chemicals | Invasive; requires trained phlebotomists; ethical considerations |
| Breast Milk | Current maternal exposure; infant exposure | Non-invasive; assesses lactational transfer | Only lactating women; lipid content varies; ethical concerns |
| Follicular Fluid | Cumulative exposure | Directly relevant to oocyte development; measures target site exposure | Highly invasive; only available during ART procedures |
| Adipose Tissue | Long-term chronic exposure | Reflects body burden of lipophilic EDCs | Highly invasive; ethical constraints; not suitable for large studies |
For studies focused on infertility, follicular fluid provides particularly relevant exposure data as it constitutes the immediate microenvironment of the developing oocyte. Studies have detected various EDCs in follicular fluid, including PFAS, phthalates, and BPA, with some studies demonstrating associations between these concentrations and adverse outcomes in assisted reproductive technologies (ART), including reduced oocyte quality, impaired fertilization, and lower embryo implantation rates [6] [12]. Similarly, for research on reproductive cancers, adipose tissue biopsies can provide valuable information about long-term storage of lipophilic EDCs that may act as potential risk factors for hormone-dependent cancers, though ethical considerations limit its use to specialized studies [82].
The analytical approaches for EDC quantification continue to evolve, with liquid chromatography-tandem mass spectrometry (LC-MS/MS) representing the gold standard for most non-persistent EDCs, while gas chromatography-mass spectrometry (GC-MS) remains valuable for persistent organic pollutants. Emerging techniques including non-targeted analysis and high-resolution mass spectrometry are expanding our ability to identify novel EDCs and metabolites, though these approaches present additional QA/QC challenges related to compound identification and quantification [83].
Minimum Information Requirements for HBM Studies
The Minimum Information Requirements for Human Biomonitoring (MIR-HBM) guidance provides a framework for standardizing HBM study design, conduct, and reporting [84]. Adherence to these requirements is particularly important for studies investigating the relationship between EDC exposure and reproductive endpoints, given the complex confounding structure and potential for subtle effects that could be obscured by methodological heterogeneity.
The MIR-HBM covers all study phases from initial design to final communication of results. For the design phase, requirements include clear definition of the study objectives, target population, sampling strategy, and ethical considerations. For reproductive studies, this includes careful consideration of the critical exposure windows (e.g., in utero, peripubertal, adult) relevant to specific reproductive endpoints, as EDCs can disrupt developmental processes during sensitive windows of vulnerability, with effects that may not manifest until later in life [6] [26]. The guidance also specifies requirements for the pre-analytical phase, including sample collection, processing, storage, and transport protocols, all of which can influence measurement accuracy, particularly for labile analytes.
For the analytical phase, the MIR-HBM emphasizes the importance of documenting analytical methods, including details on instrumentation, quality control procedures, limits of detection, and measures taken to avoid contamination [84]. This is especially relevant for EDCs like BPA and phthalates, which are ubiquitous in laboratory environments and can introduce significant background contamination. Finally, for data analysis and reporting, the guidance requires transparent documentation of statistical methods, handling of values below detection limits, and approaches for dealing with co-exposure to multiple EDCs—a common scenario given that humans are routinely exposed to complex mixtures of EDCs throughout life [29].
The Scientist's Toolkit: Essential Research Reagents and Materials
Conducting rigorous HBM studies for EDCs requires access to a range of specialized research reagents and reference materials. These tools enable researchers to generate accurate, comparable data that can be reliably used to assess associations between EDC exposure and reproductive health outcomes.
Table 3: Essential Research Reagents for EDC Biomonitoring
| Reagent/Material | Function/Purpose | Examples/Sources |
|---|---|---|
| Certified Reference Materials (CRMs) | Method validation; calibration; quality control | NIST SRM 3673 (organics in urine); NIST SRM 1958 (POPs in serum) [83] |
| Isotope-Labeled Internal Standards | Correction for matrix effects and recovery; quantification | (^{13}\text{C})-BPA; (^{13}\text{C})-PFOS; (^{2}\text{H})-phthalate metabolites [83] |
| Quality Control Materials | Monitoring analytical performance over time; batch quality assessment | Commercially available pooled serum/urine; in-house prepared pools [83] |
| Solid-Phase Extraction Cartridges | Sample cleanup; analyte preconcentration; matrix interference removal | C18; HLB; mixed-mode sorbents for ion exchange |
| LC/MS-Grade Solvents | Mobile phase preparation; sample extraction; minimal background interference | Low water content; high purity; minimal plasticizer contamination |
| Stable Matrix for Calibrators | Preparation of calibration standards; avoiding analyte loss | Stripped/charcoal-treated serum or urine; artificial urine |
The availability of appropriate CRMs remains a challenge in HBM, particularly for emerging EDCs and complex matrices like breast milk and follicular fluid [83]. When CRMs are unavailable, laboratories may rely on non-certified reference materials or prepare in-house quality control materials, though these approaches provide less certainty about measurement accuracy. Participation in proficiency testing schemes, such as those organized through the European PT Information System (EPTIS), provides external validation of laboratory performance and helps identify methodological issues that could compromise data quality [83].
For reproductive health studies, matrix-matched calibrators are particularly important, as the complex composition of matrices like follicular fluid can significantly influence analyte extraction efficiency and ionization efficiency in mass spectrometry-based methods. Similarly, the use of isotope-labeled internal standards for each target analyte is essential for accurate quantification, as these standards experience similar matrix effects and procedural losses as native analytes, thereby providing a reliable correction mechanism.
Experimental Workflow for EDC Biomonitoring
A standardized experimental workflow is essential for generating reliable, comparable HBM data for EDCs in clinical populations. The following workflow outlines the key steps from study design to data interpretation, with particular emphasis on considerations relevant to infertility and reproductive cancer research.
Detailed Methodologies for Key Experimental Steps
Sample Collection and Storage Protocols: For urine collection, first-morning void samples are often preferred for EDC analysis due to higher analyte concentrations. Samples should be collected in pre-screened plastic or glass containers that have been tested for potential contamination. For clinical populations undergoing fertility treatments, follicular fluid can be obtained during oocyte retrieval procedures, with careful documentation of the aspiration technique and processing time. All samples should be immediately processed—typically by centrifugation to remove particulates—aliquoted into contaminant-free containers, and stored at -80°C until analysis to prevent analyte degradation [84].
Sample Preparation and Extraction: For urine samples, enzymatic deconjugation of phase II metabolites (glucuronides and sulfates) using β-glucuronidase/sulfatase enzymes is typically performed to measure total (free + conjugated) analyte concentrations. Solid-phase extraction (SPE) remains the most widely used cleanup and concentration technique, with various sorbent chemistries (e.g., Oasis HLB, C18, mixed-mode ion exchange) selected based on the physicochemical properties of target analytes. For complex matrices like serum or follicular fluid, protein precipitation using organic solvents or acids may be incorporated prior to SPE to improve extraction efficiency and reduce matrix effects [83].
Instrumental Analysis: Liquid chromatography coupled to tandem mass spectrometry (LC-MS/MS) is the predominant analytical technique for measuring most EDCs (e.g., BPA, phthalates, parabens) in biological matrices. Reverse-phase C18 columns with water/acetonitrile or water/methanol mobile phases are commonly used, with gradient elution programs optimized to separate isobaric compounds (e.g., different phthalate metabolites). Electrospray ionization (ESI) in negative mode is typically used for acidic compounds like PFAS and phenols, while positive mode is preferred for phthalates and other neutral EDCs. For persistent organic pollutants like organochlorine pesticides and PCBs, gas chromatography with mass spectrometry (GC-MS) remains the standard approach due to its superior separation efficiency for these semi-volatile compounds [83].
Quality Assurance Procedures: Each analytical batch should include method blanks (to monitor contamination), laboratory control samples (to assess accuracy), duplicate samples (to evaluate precision), and matrix-matched calibration standards. The use of isotope-labeled internal standards for each target analyte is critical for compensating for matrix effects and procedural losses. Ongoing participation in proficiency testing schemes provides external validation of laboratory performance [83].
Implementing comprehensive biomonitoring strategies with rigorous quality assurance is fundamental to advancing our understanding of the impact of EDCs on infertility and reproductive cancers. The Minimum Information Requirements for HBM (MIR-HBM) provide a critical framework for standardizing study design, conduct, and reporting, thereby enhancing the reliability and comparability of data across studies [84]. As research in this field evolves, several areas require continued attention and development.
First, there is a need to expand the availability of certified reference materials for emerging EDCs and complex matrices relevant to reproductive health, such as follicular fluid and breast milk [83]. Second, methodological advances are needed to better characterize exposure to EDC mixtures and their potential synergistic effects on reproductive endpoints. Finally, the integration of HBM data with other -omics technologies (e.g., metabolomics, epigenomics) holds promise for elucidating the biological pathways linking EDC exposure to adverse reproductive outcomes. By addressing these challenges and continuing to refine biomonitoring strategies, researchers can generate the high-quality evidence needed to inform clinical practice and public health policies aimed at reducing the burden of EDC-related reproductive disorders.
Addressing Research Gaps and Methodological Challenges in EDC Studies
Non-monotonic dose responses (NMDRs), characterized by a change in the direction of the effect over the dose range, represent a fundamental challenge to traditional toxicological paradigms and risk assessment models. This whitepaper examines the mechanistic basis, experimental evidence, and regulatory implications of NMDRs within the context of endocrine disrupting chemicals (EDCs) and their impact on infertility and reproductive cancers. The linear dose-response model, which assumes that lower exposures pose lesser risk, fails to accurately capture the low-dose effects and biphasic responses commonly exhibited by EDCs. Incorporating NMDR analysis into risk assessment frameworks is essential for protecting public health, particularly for reproductive outcomes that involve complex endocrine signaling pathways susceptible to disruption at minimal exposure levels.
Definition and Significance
Non-monotonic dose-response curves (NMDRCs) are mathematically defined as a change in the sign (positive/negative) of the slope of a dose-response relationship over the tested dose range [85]. Unlike monotonic responses, which consistently increase or decrease, NMDRs can manifest as biphasic (e.g., U-shaped or inverted U-shaped) curves where low doses produce effects that diverge from those observed at higher doses.
The significance of NMDRs lies in their direct challenge to a foundational principle of toxicology: the assumption that "the dose makes the poison" and that high-dose testing can reliably predict low-dose effects [85]. This assumption underpins the current practice of using high-dose studies to extrapolate to so-called "safe" low doses. When NMDRCs occur at doses within the range of human environmental exposures or below established reference doses (RfDs), they fundamentally undermine the scientific basis of current risk assessment methodologies [85].
NMDRs in the Context of Endocrine Disruption
The study of endocrine disrupting chemicals (EDCs) has brought NMDRs to the forefront of toxicological research. EDCs are exogenous substances that alter functions of the endocrine system and consequently cause adverse health effects in intact organisms [86]. The endocrine system is inherently designed to respond to low concentrations of hormones, making it particularly vulnerable to disruption by low doses of EDCs that can mimic, block, or modulate hormonal actions [87].
Evidence linking EDC exposures to male infertility continues to mount, with rising rates of male reproductive disorders coinciding with increased exposure to environmental pollutants [14]. These include declining sperm counts, reduced semen quality, and increased incidence of cryptorchidism, hypospadias, and testicular cancer – collectively termed the testicular dysgenesis syndrome [14]. Understanding NMDRs is thus critical for accurately assessing the risks posed by EDCs to reproductive health.
Mechanisms Underlying Non-Monotonic Dose Responses
Biological Foundations
NMDRs arise from the superimposition of multiple monotonic responses within complex biological systems [88]. Several mechanistic models explain how NMDRs can occur:
Receptor Systems with Multiple Subtypes: Systems with receptor subtypes having different ligand affinities and opposing downstream effects can generate NMDRs. For example, adenosine receptors A1 and A2 have different ligand affinities and mediate opposing physiological responses [88].
Mixed-Ligand Dimerization: Receptor systems requiring homodimerization for activity may exhibit decreased response when mixed-ligand dimers form at intermediate concentrations. This has been demonstrated in androgen receptor-mediated gene expression, which is driven by homodimers but not mixed-ligand dimers [88].
Induced Repair Mechanisms: At low doses, a xenobiotic may induce DNA repair enzymes that effectively repair both chemical-induced and background DNA damage. At higher doses, the damage may exceed the repair capacity, resulting in a U-shaped response for mutation frequency [88].
Cell-Specific Cytotoxicity and Compensatory Proliferation: Cytotoxic effects at high doses can trigger compensatory cellular proliferation, while lower doses may cause cell-cycle arrest without cell death, leading to complex dose-response patterns [88].
EDC-Specific Mechanisms in Reproductive Pathology
EDCs interfere with male reproductive health through multiple interrelated pathways that are particularly prone to NMDRs:
Table 1: Key Mechanisms of Endocrine Disruption in Male Reproduction
| Mechanism | Example EDCs | Mode of Action | Reproductive Consequences |
|---|---|---|---|
| Hormone receptor interaction | BPA, phthalates | Bind to estrogen/androgen receptors; inhibit steroidogenic enzymes | Altered gene expression; decreased testosterone; impaired spermatogenesis |
| HPG axis interference | Phthalates, pesticides | Disrupt GnRH, LH, and FSH signaling | Reduced Leydig/Sertoli function; low testosterone; poor sperm maturation |
| Epigenetic modifications | BPA, phthalates | DNA methylation; histone modification; altered ncRNA | Transgenerational reproductive effects; poor sperm quality |
| Oxidative stress and apoptosis | Multiple EDCs | ROS generation; mitochondrial dysfunction | Sperm DNA damage; apoptosis; infertility |
These mechanisms operate at the molecular, cellular, and systemic levels, often in a dose- and timing-dependent manner that predisposes to non-monotonicity [14]. For instance, EDCs can bind to nuclear receptors with affinities that differ from endogenous hormones, resulting in unpredictable responses across concentration ranges.
Experimental Evidence and Methodologies
Documented Cases of NMDRs in EDC Research
Substantial evidence demonstrates NMDRs occurring at environmentally relevant exposure levels:
Bisphenol A (BPA): The CLARITY-BPA study reported mammary adenocarcinomas only in rats exposed to the lowest BPA dose tested, demonstrating a NMDR below the toxicological NOAEL [85].
Phthalates: Di(2-ethylhexyl)phthalate (DEHP) showed significant effects on maternal serum testosterone at 0.5, 1, and 5 µg/kg/d and on anogenital distance at 5 µg/kg/d – all below the reference dose of 20 µg/kg/d [85].
Chlorothalonil: This fungicide exhibited NMDRs for amphibian survival at concentrations (0.0000164 to 0.0164 ppm) well below both the reference dose (0.6 ppm) and environmentally relevant concentrations [85].
Permethrin: Dopamine transport in mice was altered at 1.5 mg/kg/d, but not at higher (3 mg/kg/d) or lower (0.4, 0.8 mg/kg/d) doses, with effects occurring above the RfD (0.005 mg/kg/d) but below the NOAEL (5 mg/kg/d) [85].
Quantitative Analysis of NMDR Studies
Table 2: Examples of NMDRs Occurring Below Regulatory Thresholds
| Chemical | NMDR Effect Observed | Dose of NMDR | NOAEL | Reference Dose |
|---|---|---|---|---|
| BPA | Mammary adenocarcinomas in rats | Lowest dose tested | Higher than effect dose | Not protective |
| DEHP | Altered anogenital distance | 5 µg/kg/d | >5 µg/kg/d | 20 µg/kg/d |
| Chlorothalonil | Reduced amphibian survival | 0.0000164-0.0164 ppm | 60 ppm | 0.6 ppm |
| Permethrin | Altered dopamine transport | 1.5 mg/kg/d | 5 mg/kg/d | 0.005 mg/kg/d |
| Resveratrol | Stomach ulcer modulation | 1-2 mg/kg/d | 300 mg/kg/d | 0.3 mg/kg/d |
Experimental Protocols for NMDR Detection
In Vitro Receptor Binding Assays
Purpose: To quantify EDC interactions with hormone receptors (ER, AR, TR) and identify potential non-monotonic responses.
Methodology:
- Receptor Preparation: Isolate or express specific human hormone receptors
- Ligand Binding:
- Incubate receptors with radiolabeled native ligand and increasing concentrations of EDC
- Include full concentration range (10^-12 M to 10^-4 M) to capture potential NMDRs
- Use appropriate controls (vehicle, positive antagonist/agonist)
- Detection:
- Separate bound and free ligand via charcoal adsorption or filtration
- Measure radioactivity or fluorescence
- Data Analysis:
- Calculate percent binding relative to control
- Plot dose-response curve
- Determine Ki values for receptor affinity
Interpretation: NMDRs may manifest as enhanced binding at low concentrations that diminishes or reverses at higher concentrations.
HPG Axis Disruption Assessment
Purpose: To evaluate EDC effects on the hypothalamic-pituitary-gonadal axis using in vivo models.
Methodology:
- Animal Model: Use developing rodents (prenatal or early postnatal exposure)
- Dosing Regimen:
- Administer at least 5 different doses spanning environmental exposure range
- Include vehicle control and positive control groups
- Employ oral administration to mimic human exposure
- Tissue Collection and Analysis:
- Collect blood for hormone measurements (testosterone, LH, FSH)
- Extract hypothalami for GnRH and kisspeptin measurements
- Collect testes for histopathology and gene expression
- Endpoints:
- Hormone levels via ELISA or RIA
- Gene expression of steroidogenic enzymes (Cyp11a1, Cyp17a1, Hsd3b)
- Testicular histology and spermatogenesis scoring
- Reproductive organ weights
Interpretation: NMDRs may appear as altered hormone levels or gene expression at low doses that normalize at intermediate doses and reappear or reverse at high doses.
Figure 1: EDC Mechanisms Leading to Reproductive Pathologies. This diagram illustrates the complex pathways through which endocrine disrupting chemicals interfere with reproductive function, highlighting multiple points where non-monotonic responses may occur due to competing biological processes.
Regulatory Implications and Risk Assessment Challenges
Limitations of Current Risk Assessment Paradigms
Traditional risk assessment approaches face significant challenges in addressing NMDRs:
Inadequate Testing Protocols: Standard toxicological studies typically examine only 3-4 doses, usually at high concentrations, making detection of NMDRs unlikely [85]. The current practice of focusing on apical endpoints in guideline studies often misses sensitive endpoints and windows of exposure relevant to EDCs [89].
Problematic Extrapolation Assumptions: The linear dose-response model fails when NMDRs occur below the toxicological NOAEL or reference dose. Numerous examples demonstrate that effects observed at high doses cannot reliably predict low-dose effects for EDCs [85].
Insufficient Protection of Public Health: When NMDRs occur at or below reference doses, these regulatory thresholds become scientifically flawed and insufficiently protective [85]. This is particularly concerning for vulnerable populations, including pregnant women and developing fetuses.
Framework for Improved NMDR Assessment
The European Food Safety Authority (EFSA) has proposed a systematic framework for evaluating NMDRs consisting of six checkpoints [90]:
- Biological plausibility: Is there a credible mechanistic basis for the NMDR?
- Adequate dose spacing: Are doses appropriately spaced to detect non-monotonicity?
- Statistical robustness: Is the NMDR based on more than a single outlier?
- Reproducibility: Can the NMDR be replicated within or across studies?
- Temporal consistency: Is the effect consistent over time?
- Dose-response relationship: Does the statistical model confirm non-monotonicity?
Application of this framework to fluoxetine studies revealed that only a minority of datasets met all checkpoints, while 27% fulfilled at least five, highlighting both the occurrence of NMDRs and the need for more rigorous testing [90].
Figure 2: Systematic Evaluation Framework for NMDR Assessment. This workflow diagram outlines the stepwise approach for evaluating potential non-monotonic dose-response relationships, based on the EFSA framework with six critical checkpoints for validation [90].
The Scientist's Toolkit: Essential Research Reagents and Methods
Table 3: Key Research Reagents and Methods for NMDR Studies
| Reagent/Method | Function in NMDR Research | Application Examples |
|---|---|---|
| Receptor Binding Assays | Quantify compound affinity for hormone receptors | ERα/ERβ binding for estrogens; AR binding for anti-androgens |
| Reporter Gene Assays | Measure transcriptional activation of hormone-responsive genes | E-screen assay; androgen-responsive element assays |
| Steroidogenesis Assays | Assess hormone production in cell models | H295R adrenocortical cell line; MA-10 Leydig cells |
| qPCR Arrays | Profile expression of endocrine-related genes | Steroidogenic pathway genes; hypothalamic-pituitary genes |
| LC-MS/MS | Sensitive quantification of hormones and EDCs | Serum steroid hormones; urinary EDC metabolites |
| Chromatin Immunoprecipitation | Evaluate epigenetic modifications | Histone marks at hormone-responsive promoters |
| CRISPR/Cas9 Systems | Gene editing to validate mechanistic pathways | Knockout of specific nuclear receptors |
| Organoid Models | 3D culture systems for complex tissue modeling | Testicular organoids; mammary gland organoids |
The evidence for non-monotonic dose responses in endocrine disrupting chemicals is substantial and biologically plausible. NMDRs challenge fundamental assumptions in traditional risk assessment and necessitate revised approaches to chemical safety evaluation. For reproductive health outcomes, including infertility and reproductive cancers, failure to account for NMDRs may result in inadequate protection of public health, particularly for vulnerable populations such as pregnant women and developing fetuses.
Future directions for research and regulation should include:
Revised Testing Guidelines: Implement testing protocols that include more dose groups, particularly at low, environmentally relevant concentrations, with specific attention to sensitive developmental windows.
Integrated Assessment Frameworks: Adopt systematic review methodologies that enable transparent and objective evaluation of evidence across multiple streams (epidemiology, wildlife, laboratory animals, in vitro models) [86].
Mixture Risk Assessment: Develop approaches that address real-life exposure to complex mixtures of EDCs, as current chemical-by-chemical regulation may underestimate combined risks [91].
Precautionary Approaches: Given the potential for serious or irreversible consequences, limited evidence of NMDRs at low doses may be sufficient to justify protective measures, particularly for susceptible populations and life stages.
Addressing the challenges posed by NMDRs is essential for advancing our understanding of EDC impacts on reproductive health and for developing risk assessment models that adequately protect human health in the face of real-world exposure scenarios.
The study of Endocrine-Drupting Chemicals (EDCs) has evolved from examining single chemicals to addressing the complex reality of mixture exposures. Within the context of infertility and reproductive cancers, this paradigm shift is critical: humans are invariably exposed to multiple EDCs simultaneously, yet regulatory frameworks and traditional toxicology have predominantly relied on single-chemical risk assessments. The cumulative impact of multiple EDCs presents a formidable challenge for researchers and risk assessors alike, particularly in understanding their role in the increasing prevalence of reproductive disorders and hormone-sensitive cancers.
EDCs encompass a wide variety of substances capable of interfering with the endocrine system, including bisphenols, phthalates, polychlorinated biphenyls (PCBs), parabens, pesticides, and per- and polyfluoroalkyl substances (PFAS) [92] [93] [94]. These compounds are widely produced and used in everyday modern life and have been increasingly detected in aquatic matrices and human tissues worldwide [93]. The reproductive system is particularly vulnerable to EDC exposure due to its high expression of steroid hormone receptors in reproductive tract tissues, including the gonads, making them primary targets for EDCs [95]. Reproductive tissues are incredibly hormone-responsive by design, making them exceptionally susceptible to hormone-like compounds [95].
The concept of mixture effects acknowledges that EDCs can interact through additive, synergistic, or antagonistic mechanisms, potentially leading to significant health impacts even when individual chemicals are present at low, seemingly safe concentrations. For researchers investigating infertility and reproductive cancers, this complexity necessitates sophisticated experimental designs and analytical approaches that move beyond traditional toxicology. This technical guide provides a comprehensive framework for evaluating the cumulative impacts of EDC mixtures, with specific focus on methodologies relevant to reproductive toxicology and oncogenesis.
Mechanisms of Mixture Toxicity in Reproductive Systems
Key Molecular Pathways and Mechanisms
EDC mixtures interfere with reproductive function through multiple interconnected biological pathways. The hypothalamic-pituitary-gonadal (HPG) axis serves as a primary target, with EDCs disrupting the delicate hormonal balance required for normal reproductive function [94]. These chemicals can mimic or block hormone action through nuclear receptor interactions, particularly estrogen receptors (ERα and ERβ), androgen receptors (AR), and thyroid hormone receptors [96]. The resulting disruption affects gonadotropin-releasing hormone (GnRH) secretion, folliculogenesis, spermatogenesis, and steroidogenesis [94].
Beyond receptor-mediated effects, EDC mixtures induce epigenetic modifications that can have transgenerational consequences. Several EDCs, including bisphenol A (BPA) and phthalates, have been shown to alter DNA methylation patterns and histone modifications in female reproductive tissues [15]. These changes can lead to altered expression of genes involved in ovarian function, implantation, and placental development [15]. The developmental origins of health and disease (DOHaD) paradigm is particularly relevant here, as prenatal exposure to EDC mixtures can reprogram epigenetic marks during critical windows of development, increasing susceptibility to reproductive diseases and cancers in adulthood [97] [15].
Oxidative stress represents another critical mechanism through which EDC mixtures exert reproductive toxicity. Following exposure to EDC combinations, increased oxidative stress (OS), elevated antioxidant enzymatic activity, disrupted reproductive cycle, and reduced steroidogenesis are often reported consequences [92]. The resulting macromolecular damage contributes to mitochondrial dysfunction, impaired gamete quality, and aberrant cell signaling that can promote carcinogenic processes in hormone-sensitive tissues [94].
Figure 1: Molecular Pathways of EDC Mixtures in Reproductive Pathology. This diagram illustrates the primary mechanisms through which EDC mixtures contribute to infertility and reproductive cancers, highlighting the complexity of interacting pathways.
Sex-Specific Effects and Vulnerable Windows
A critical consideration in mixture toxicology is the sex-specific manifestation of EDC effects. Recent research has revealed that males and females exposed to the same EDC mixture can show entirely opposite outcomes [95]. For example, the same exposure might impair ovarian follicle development in females while disrupting testosterone production or spermatogenesis in males [95]. These differences extend beyond hormone levels to include variations in receptor expression, tissue architecture, detoxification capacity, and epigenetic responsiveness [95].
The timing of exposure represents another crucial variable in determining mixture toxicity. Developmental windows such as prenatal, early postnatal, and pubertal periods exhibit heightened sensitivity to EDC mixtures [97]. During pregnancy, EDCs can influence maternal metabolic adaptation, which in turn affects reproductive outcomes in offspring [95]. The concept of "latent effects" is particularly relevant – some EDC-induced changes remain dormant until triggered by physiological stressors such as metabolic conditions, inflammation, or life stage transitions like menopause [95]. This delayed manifestation complicates risk evaluation but opens new avenues for understanding disease susceptibility across the lifespan.
Experimental Models for Assessing Mixture Effects
In Vitro and In Vivo Approaches
Evaluating the cumulative impacts of EDC mixtures requires complementary experimental models that capture different aspects of toxicity. In vitro systems using human cell lines have revealed that EDC mixtures can produce effects even when each component is present at low, individually ineffective concentrations [92]. These models are particularly valuable for high-throughput screening and mechanistic studies, allowing researchers to isolate specific pathways affected by mixture exposures. For reproductive cancer research, endometrial, ovarian, and breast cancer cell lines have demonstrated increased proliferation in response to EDC mixtures, providing insights into potential carcinogenic mechanisms [94] [15].
In vivo models remain indispensable for understanding the integrated physiological responses to EDC mixtures. Animal studies have demonstrated that exposure to EDC combinations can lead to bioaccumulation, causing alterations in androgen synthesis and catabolism, impaired fertility, and multiple severe reproductive problems [92]. Recent research using female mouse models has shown that prenatal exposure to EDCs used in hydraulic fracturing (fracking) leads to adverse reproductive and developmental outcomes [28]. These models also permit examination of transgenerational effects, where exposure in one generation leads to reproductive abnormalities in subsequent, unexposed generations through epigenetic mechanisms [15].
Human Epidemiological and Clinical Studies
Human studies provide critical evidence for the real-world impacts of EDC mixtures on reproductive health. Prospective cohort designs that track individuals over time have identified associations between EDC mixtures and adverse reproductive outcomes. For instance, a recent study involving 176 women undergoing assisted reproductive technology (ART) treatment quantified 76 EDCs across five categories in follicular fluid samples [98]. The findings demonstrated that EDC mixtures were significantly associated with reduction in retrieved oocytes, mature oocytes, and biochemical pregnancy probability [98]. Among the mixtures, phthalates (PAEs) and Bisphenol S (BPS) were identified as dominant contributors to adverse conventional IVF/ICSI outcomes and biochemical pregnancy outcome, respectively [98].
Biomonitoring approaches that measure EDCs and their metabolites in human tissues and fluids have revealed the ubiquity of mixture exposures. Studies have detected multiple EDCs in follicular fluid, including phenols, parabens, phthalates (PAEs), per- and polyfluoroalkyl substances (PFASs), and synthetic phenolic antioxidants (SPAs) [98]. This internal exposure data provides a more accurate picture of the mixtures actually encountered by human reproductive systems, informing more environmentally relevant experimental designs.
Table 1: Experimental Models for EDC Mixture Assessment in Reproductive Toxicology
| Model Type | Key Applications | Advantages | Limitations |
|---|---|---|---|
| In vitro cell systems | High-throughput screening, Mechanistic pathway analysis, Receptor activity profiling | Controlled environment, High reproducibility, Cost-effective for large chemical sets | Limited metabolic competence, Does not capture integrated physiology |
| Animal models | Developmental programming effects, Transgenerational studies, Integrated physiological responses | Captures complex tissue interactions, Allows examination of latency, Controlled exposure timing | Species differences in metabolism and sensitivity, Ethical considerations |
| Human cohort studies | Real-world exposure assessment, Identification of susceptibility windows, Association with clinical endpoints | Direct human relevance, Captures actual exposure mixtures, Identifies effect modifiers | Limited causal inference, Confounding factors, Long timelines for outcomes |
| ART populations | Direct assessment of oocyte quality, Embryo development, Clinical pregnancy outcomes | Direct window into human reproduction, Multiple intermediate endpoints available | Specialized population may not represent general fertility |
Methodological Frameworks and Predictive Models
Mixture Assessment Models
The toxicological assessment of chemical mixtures requires specialized models that can predict combined effects based on individual chemical properties. The Concentration Addition (CA) model assumes that mixture components have similar mechanisms of action and act as dilutions of one another [92]. This model has proven particularly effective for predicting mixture effects of EDCs that share common receptor-mediated pathways, such as estrogenic compounds. In contrast, the Independent Action (IA) model applies to chemicals with dissimilar mechanisms of action, calculating expected mixture effects as the probability of any effect occurring [92]. Both models have demonstrated that EDC mixtures can produce significant effects even when each component is present below its individual no-observed-effect-concentration.
Recent advances in computational toxicology have incorporated Bayesian methods that better accommodate the complex, non-linear interactions characteristic of EDC mixtures. The Bayesian Kernel Machine Regression (BKMR) model has emerged as a particularly powerful tool for estimating the joint effects of chemical mixtures while accounting for non-linear relationships and interaction effects [98]. In the follicular fluid study mentioned previously, BKMR analyses revealed that EDC mixtures were significantly associated with reduction in retrieved oocytes, mature oocytes, and biochemical pregnancy probability [98]. This approach can identify key drivers of mixture toxicity and visualize exposure-response relationships for individual chemicals within the context of the mixture.
Figure 2: Experimental Workflow for EDC Mixture Assessment. This diagram outlines the strategic application of different mathematical models based on the known properties of mixture components and research questions.
Statistical Considerations for Mixture Studies
Proper evaluation of EDC mixtures requires careful attention to statistical power, confounding control, and multiple comparisons. Studies investigating complex mixtures with many components often face the curse of dimensionality, where the number of exposure variables approaches or exceeds the sample size. Dimension reduction techniques such as principal component analysis or weighted quantile sum regression can help address this challenge by creating composite exposure indices that reflect the overall mixture. Additionally, stratified analyses have revealed that susceptibility to EDC mixtures may vary by factors such as age, with one study finding stronger associations between EDCs exposure and ART outcomes among women under 33 years [98].
The non-monotonic dose-response relationships characteristic of many EDCs present another statistical challenge [15]. Unlike traditional toxicants, EDCs often exhibit U-shaped or inverted U-shaped dose-response curves, where effects at low doses differ from those at high doses [15]. This behavior contradicts standard toxicological assumptions and necessitates flexible modeling approaches that can capture non-linear patterns. Restricted cubic splines in generalized linear models represent one approach for accommodating these complex dose-response patterns without presuming a specific functional form [98].
Research Reagent Solutions for EDC Mixture Studies
Table 2: Essential Research Reagents for EDC Mixture Toxicology
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Chemical Standards | BPA, BPS, BPF, DEHP, MEHP, MECPP, PFOS, PFOA | Analytical quantification, Dose-response characterization, Mixture preparation | Purity verification, Stability testing, Solvent compatibility |
| Molecular Assays | ERα/ERβ reporter gene assays, AR bioassays, Steroidogenesis assays | Mechanism screening, Pathway identification, Potency comparisons | Cell line selection, Reference standard inclusion, Quality control criteria |
| Epigenetic Tools | Methylation-specific PCR primers, HDAC inhibitors, miRNA mimics/inhibitors | DNA methylation analysis, Histone modification assessment, Non-coding RNA functional studies | Bisulfite conversion efficiency, Antibody specificity validation, Transfection efficiency controls |
| Analytical Standards | Isotope-labeled internal standards, Certified reference materials | Mass spectrometry quantification, Method validation, Laboratory proficiency testing | Storage conditions, Shelf life monitoring, Cross-validation between laboratories |
| Biological Models | Human granulosa cell lines, Ovarian follicle cultures, Endometrial organoids | Human-relevant screening, Tissue-specific responses, Developmental toxicity assessment | Donor variability, Culture condition optimization, Phenotype stability |
Implications for Risk Assessment and Future Directions
The cumulative impact of EDC mixtures represents a significant challenge for chemical risk assessment and regulatory policy. Traditional approaches that evaluate chemicals individually may underestimate risks when multiple EDCs with similar mechanisms are present at low concentrations [92]. Future risk assessment frameworks must incorporate mixture effects and real-world exposure scenarios to adequately protect reproductive health [95] [92]. This is particularly important for vulnerable populations such as pregnant women, infants, and those with pre-existing reproductive impairments.
Research priorities identified by experts in the field include capturing the complexity of real-life exposures by moving beyond single chemicals to look at mixtures, low-dose exposures, and cumulative effects across time [95]. There is also a pressing need to "build models that include sex as a biological variable, consider genetic diversity, and examine how physiological states like pregnancy or metabolic disease affect chemical sensitivity" [95]. Integrating omics approaches and high-resolution imaging with traditional toxicology will help map mechanisms more precisely [95]. Importantly, studies need to consider sensitive windows — especially early development — as key determinants of later health outcomes [95].
For researchers focused on infertility and reproductive cancers, understanding mixture effects is not merely an academic exercise but a necessary step toward developing effective prevention strategies and clinical interventions. By adopting the methodologies and frameworks outlined in this guide, scientists can generate the robust evidence needed to inform chemical policy, clinical practice, and public health recommendations aimed at reducing the burden of reproductive disorders associated with EDC exposures.
The study of endocrine-disrupting chemicals (EDCs) presents a fundamental challenge in toxicology and public health: demonstrating adverse biological effects at low, environmentally relevant exposure levels that contradict traditional dose-response paradigms. This whitepaper examines the evidence supporting low-dose effects of EDCs, particularly within the context of infertility and reproductive cancers research. We synthesize current epidemiological and experimental findings, analyze quantitative relationships, detail methodological approaches for low-dose testing, and identify key molecular mechanisms that operate at environmentally relevant concentrations. The evidence compellingly indicates that EDCs can disrupt reproductive health at concentrations previously considered safe, necessitating a reevaluation of current risk assessment frameworks for chemical exposures.
Endocrine-disrupting chemicals (EDCs) are defined as "exogenous compounds or mixtures that alter function(s) of the endocrine system and consequently cause adverse effects in an intact organism, or its progeny, or (sub)populations" [99]. These chemicals interfere with hormonal signaling through multiple mechanisms, including receptor agonism/antagonism, altered hormone synthesis/metabolism, and epigenetic modifications. The "low-dose controversy" centers on observations that some EDCs can produce non-monotonic dose responses (NMDRs), where effects occur at low environmental exposure levels but not at higher doses, contradicting traditional toxicological principles that presume "the dose makes the poison" [12] [100].
The human body is dependent on hormones for a healthy endocrine system, which controls many biological processes like normal growth, fertility, and reproduction. Hormones act in extremely small amounts, and minor disruptions in those levels may cause significant developmental and biological effects [100]. This biological reality underpins the concern about low-dose EDC exposures, particularly regarding reproductive health outcomes such as infertility and hormonally-influenced cancers.
Mechanisms of Endocrine Disruption at Low Doses
Nuclear Receptor Interactions
EDCs frequently target nuclear hormone receptors, including estrogen receptors (ERα and ERβ), androgen receptor (AR), thyroid hormone receptors (TRs), and peroxisome proliferator-activated receptors (PPARs). At low concentrations, certain EDCs effectively compete with endogenous hormones for receptor binding due to their structural similarity and higher binding affinity. For instance, BPA mimics estradiol by binding to estrogen receptors, acting as a potent agonist at picomolar to nanomolar concentrations [12] [99]. Similarly, phthalates function as androgen receptor antagonists, disrupting normal androgen signaling at environmentally relevant exposure levels.
Epigenetic Modifications
Low-dose EDC exposures during critical developmental windows can induce epigenetic changes that alter gene expression patterns without changing DNA sequences. These modifications include DNA methylation changes, histone modifications, and microRNA expression alterations. Diethylstilbestrol (DES) provides a historical example, where prenatal exposure causes epigenetic changes in reproductive organs of mice, providing a possible explanation for how endocrine disruptors affect fertility and reproduction across generations [100]. These epigenetic alterations may persist throughout life and potentially transmit transgenerationally, contributing to increased disease susceptibility later in life.
Oxidative Stress and Cellular Damage
Several EDCs induce oxidative stress in hormonal tissues at low exposure levels. This oxidative damage can impair cellular function, promote inflammation, and damage critical cellular components including lipids, proteins, and DNA. In ovarian tissues, EDCs like BPA and phthalates generate reactive oxygen species (ROS) that disrupt follicular development and oocyte maturation, contributing to diminished ovarian reserve and reduced fertility [12] [99].
Table 1: Primary Mechanisms of Low-Dose EDC Action in Reproductive Tissues
| Mechanism | Key EDCs Involved | Biological Consequences | Effective Concentration Range |
|---|---|---|---|
| Nuclear Receptor Binding | BPA, Phthalates, PCBs, Dioxins | Altered gene transcription, Hormone mimicry/blockade | pM - nM |
| Epigenetic Modification | DES, BPA, Phthalates, PCBs | Persistent changes in gene expression, Transgenerational effects | nM - μM |
| Oxidative Stress Induction | BPA, Phthalates, Pesticides | Cellular damage, Inflammation, Apoptosis | nM - μM |
| Steroidogenesis Disruption | Phthalates, PCBs, Pesticides | Altered hormone production, Reduced steroid hormones | nM - μM |
Quantitative Evidence for Low-Dose Effects on Reproductive Health
Epidemiological Findings in Female Infertility
Growing evidence shows that endocrine disruptor chemicals (EDCs) have been considered as risk factors of infertility [12]. Their presence in our everyday life has become ubiquitous because of their universal use in food and beverage containers, personal care products, cosmetics, and phytosanitary products [12]. Recent studies suggest that women are more exposed to EDCs than men due to higher chemical products use [12].
Epidemiological studies have demonstrated significant associations between EDC exposure levels and female reproductive pathologies. Both persistent (polychlorinated biphenyls, perfluoroalkyl and polyfluoroalkyl substances) and non-persistent (phthalates) EDCs exposure could increase an overall risk of ovarian aging, leading to the diminish of ovarian reserve, decline of fertility or fecundity, irregularity of the menstrual cycle and an earlier age at menopause, and/or premature ovarian insufficiency/failure in epidemiological studies [99]. A comprehensive review of epidemiological and experimental evidence indicates that exposure to EDCs is an important environmental risk factor for ovarian aging [99].
Table 2: Epidemiological Evidence for Low-Dose EDC Effects on Female Reproduction
| EDC Class | Specific Chemicals | Reproductive Health Outcome | Effect Level | Study Population |
|---|---|---|---|---|
| Phthalates | MIBP, DEHP, DBP | Preterm birth, Diminished ovarian reserve, Earlier menopause | 0.5-5 μg/L (urine) | NHANES, Clinical cohorts |
| Bisphenols | BPA, BPS | Reduced oocyte quality, IVF failure, Altered uterine receptivity | 0.5-2 μg/L (serum) | IVF patients, General population |
| Persistent EDCs | PCBs, PFAS, Dioxins | Endometriosis, Earlier menarche, Menstrual irregularities | 1-10 ng/g (serum) | Occupational exposures, General population |
| Pesticides | DDT, Atrazine, Chlorpyrifos | Infertility, POI, Spontaneous abortion | 0.1-1 μg/L (serum) | Agricultural communities |
Experimental Evidence from Animal Studies
Animal studies provide compelling evidence for low-dose effects of EDCs on reproductive function. Experimental models in rodents have demonstrated that both persistent (polychlorinated biphenyls, perfluoroalkyl and polyfluoroalkyl substances) and non-persistent (phthalates) EDCs exposure could increase an overall risk of ovarian aging [99]. The loss of follicles has been validated in experimental studies of some EDCs, such as BPA, phthalates, parabens and PCBs [99].
The underlying mechanisms may involve the impaired ovarian follicular development by altering receptor-mediated pro-apoptotic pathways, inducing signal transduction and cell cycle arrest and epigenetic modification [99]. These findings are particularly significant because many of these effects occur at exposure levels comparable to those found in human populations, challenging traditional toxicological reference doses.
Methodological Approaches for Low-Dose EDC Research
Mixture Effect Assessment Methods
Human exposure to EDCs occurs as complex mixtures rather than isolated compounds, necessitating specialized methodological approaches to detect low-dose effects:
Weighted Quantile Sum (WQS) Regression: This statistical method evaluates the combined effect of multiple EDCs when each individual chemical is present at low concentrations. WQS regression demonstrated that each index rise in the EDC-mixture index increased the odds of preserved ratio impaired spirometry (PRISm) by 63% (OR=1.63, 95% CI: 1.25–2.13, P < 0.001) in NHANES data analysis [101].
Quantile g-computation (Qgcomp): An emerging approach that confirmed a 41% increase in odds of PRISm for each quantile increase in EDC mixture (OR=1.41, 95% CI: 1.15–1.72, P < 0.001) [101].
Bayesian Kernel Machine Regression (BKMR): This flexible modeling technique captures complex exposure-response relationships and interactions between mixture components, confirming the overall positive association between EDC mixtures and adverse health outcomes [101].
In Vitro Assays for Mechanistic Studies
High-throughput in vitro systems enable screening of low-dose EDC effects on specific molecular pathways:
Receptor Binding Assays: Luciferase reporter gene assays in cell lines expressing human nuclear receptors (ER, AR, TR, PPAR) quantify agonist/antagonist activity at low concentrations.
Steroidogenesis Assays: H295R adrenal carcinoma cell model assesses disruption of steroid hormone production pathways at environmentally relevant concentrations.
Ovarian Follicle Cultures: 3D in vitro cultures of ovarian follicles evaluate direct EDC effects on folliculogenesis and oocyte maturation without systemic compensation.
Low-Dose EDC Research Workflow
Key Signaling Pathways Disrupted by Low-Dose EDCs
Hypothalamic-Pituitary-Ovarian (HPO) Axis Disruption
The HPO axis is a prime target for EDCs, with disruption potentially occurring at multiple levels. The hypothalamic-pituitary-gonadal (HPG) axis in women is a prime target of EDCs [12]. EDCs interfere with the release and timing of Luteinizing Hormone (LH), altering the ovulation process [12]. Additionally, oxidative stress in ovarian tissues, that damages cells and impairs their function, is induced by several EDCs [12]. These molecules can also affect the epigenome causing modifications in gene expression of ovulation regulators without altering their DNA sequence [12].
HPO Axis Disruption by EDCs
Non-Monotonic Dose Response Mechanisms
Non-monotonic dose responses (NMDRs) represent a fundamental challenge in EDC risk assessment. Several biological mechanisms can generate NMDRs:
Receptor Downregulation: At high doses, EDCs may cause receptor downregulation or desensitization, diminishing biological responses that are observed at lower concentrations.
Co-receptor Competition: Different receptor isoforms with opposing functions may have varying binding affinities for EDCs, resulting in activation at low doses and inhibition at higher exposures.
Feedback Interference: EDCs can disrupt negative feedback loops in hormonal systems, producing unexpected dose-response patterns that deviate from traditional monotonic curves.
Non-Monotonic Dose Response Mechanisms
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Low-Dose EDC Studies
| Reagent/Material | Application | Key Features | Representative Examples |
|---|---|---|---|
| Recombinant Nuclear Receptors | Receptor binding assays | Human isoforms with reporter systems | ERα, ERβ, AR, TR, PPARγ |
| EDC Analytical Standards | Exposure quantification | High-purity reference materials | BPA, DEHP, PCB-153, PFOS, TCDD |
| Cell-Based Reporter Assays | Pathway activity screening | Stable transfection, low background | ER CALUX, AR CALUX, TRβ GAL4 |
| Epigenetic Analysis Kits | DNA methylation/histone modification | High sensitivity for tissue-limited samples | Methylated DNA IP, ChIP-seq kits |
| Hormone Immunoassays | Endpoint measurement in biofluids | Low cross-reactivity, high precision | ELISA for E2, T, LH, FSH, AMH |
| Animal Exposure Models | In vivo low-dose studies | Sensitive developmental stages | CD-1 mice, Sprague-Dawley rats |
| Mixture Analysis Software | Complex exposure data | Bayesian methods, interaction modeling | BKMR, WQS, g-computation packages |
The evidence for biologically relevant effects of EDCs at low environmental exposure levels continues to accumulate, with particular significance for infertility and reproductive cancers research. Traditional toxicological paradigms that assume thresholded, monotonic dose-responses are insufficient for evaluating EDCs that operate through multiple mechanisms including receptor-mediated signaling, epigenetic modifications, and oxidative stress. The demonstration of non-monotonic dose responses and mixture effects necessitates fundamental changes in chemical risk assessment approaches.
Future research should prioritize: (1) developing more sensitive biomonitoring methods for EDCs and their metabolites; (2) implementing advanced mixture analysis techniques in epidemiological studies; (3) elucidating epigenetic mechanisms of low-dose EDC effects across generations; and (4) establishing new regulatory frameworks that account for non-monotonicity and mixture effects. Addressing these challenges is essential for protecting reproductive health across populations and reducing the burden of environmentally-influenced infertility and cancers.
The translation of findings from animal studies to human clinical applications is a fundamental, yet challenging, pillar of biomedical research. This process is especially critical in fields investigating the impact of endocrine-disrupting chemicals (EDCs) on infertility and reproductive cancers. EDCs are chemicals that may interfere with the hormonal system and thereby produce harmful effects in both humans and wildlife [102]. The hormonal system regulates crucial processes including growth, development, immunity, metabolism, and reproduction, making accurate toxicological assessment paramount for public health [102]. While animal models provide invaluable insight into disease mechanisms and potential therapeutic interventions, inherent biological differences between species can lead to inaccurate predictions of human health outcomes. A quantitative analysis of therapeutic translation across various biomedical fields reveals that only 50% of therapies advance from animal studies to any human study, 40% progress to randomized controlled trials (RCTs), and a mere 5% achieve regulatory approval [103]. This low rate of final approval indicates potential deficiencies in the design of both animal studies and early clinical trials [103]. The median transition times are 5, 7, and 10 years to reach a human study, an RCT, and regulatory approval, respectively [103]. This review explores the species-specific differences that complicate the extrapolation of data from animal models to humans, with a specific focus on their implications for EDC research on reproductive pathologies.
Quantitative Landscape of Animal-to-Human Translation
Understanding the overall efficacy of translating animal research to human applications provides a critical framework for assessing its utility in EDC and reproductive toxicology. A recent umbrella review of 122 articles, describing 54 distinct human diseases and 367 therapeutic interventions, offers a sobering yet nuanced perspective on this process [103]. Contrary to some widespread assertions of extremely low translatability, the analysis found an 86% concordance between positive results in animal and clinical studies [103]. However, this high concordance must be interpreted alongside the finding that only 5% of interventions tested in animals ultimately gain regulatory approval, highlighting a significant attrition rate in the developmental pipeline [103].
Table 1: Quantitative Analysis of Animal-to-Human Translation of Therapies
| Translation Stage | Success Rate | Median Timeframe | Key Implications for EDC Research |
|---|---|---|---|
| Any Human Study | 50% | 5 years | Highlights initial feasibility but high early attrition. |
| Randomized Controlled Trial (RCT) | 40% | 7 years | Suggests many interventions fail efficacy testing in humans. |
| Regulatory Approval | 5% | 10 years | Indicates final attrition due to safety, efficacy, or design flaws. |
| Animal-Human Result Concordance | 86% | N/A | Suggests positive animal data often predicts positive human results for the interventions that do translate. |
The disconnect between high concordance and low regulatory approval suggests that the primary challenge may not be a consistent failure of animal models to predict human biological responses, but rather deficiencies in study design, including the selection of appropriate animal models that accurately recapitulate human physiology and exposure scenarios [103]. This is particularly relevant for EDC research, where effects can be subtle, delayed, and dependent on critical developmental windows of exposure. The effects caused by an EDC may only become evident long after the exposure; for example, the exposure of a fetus in the womb to an endocrine-disrupting substance may lead to effects that affect the health of the adult and possibly also future generations [102]. This complexity necessitates robust, human-relevant experimental protocols to effectively bridge the species gap.
Species Differences in EDC Mechanisms and Reproductive Toxicity
Endocrine disruption manifests through complex mechanisms that often exhibit significant species-specificity, particularly in reproductive tissues. A key mechanism is when EDCs mimic natural hormones such as estrogen and bind to their receptors, leading to hormonal disruption [12]. For instance, Bisphenol A (BPA), a widespread environmental contaminant, exerts its effects by activating membrane receptors like GPER (GPR30) in addition to the classical estrogen receptors ERα and ERβ [104]. The binding affinity and downstream signaling of these receptors can vary considerably between species, leading to divergent outcomes.
Molecular and Cellular Divergence
At the molecular level, gene expression responses to EDCs can differ. A study on human ovarian cortical tissue exposed to EDCs like diethylstilbestrol (DES) and ketoconazole (KTZ) identified hundreds of differentially expressed genes, including stearoyl-CoA desaturase (SCD), which was proposed as a novel human-relevant biomarker [68]. This highlights that molecular pathways disrupted in humans may not be accurately mirrored in standard animal models. Furthermore, toxicokinetic differences—how the body absorbs, distributes, metabolizes, and excretes a chemical—are a major source of translational failure. Metabolic rates, the presence of specific enzymes, and the efficiency of biological barriers like the placenta or blood-testis barrier can vary dramatically.
Table 2: Key Research Reagent Solutions for Investigating EDCs
| Research Reagent | Function/Application in EDC Research |
|---|---|
| Human Ovarian Cortical Tissue | Ex vivo model to study direct effects of EDCs (e.g., DES, KTZ) on human follicle survival, growth, and gene expression [68]. |
| Primary Cell Lines (e.g., Sertoli cells) | Used to assess EDC-induced cytotoxicity, oxidative stress, and barrier function disruption in reproductive tissues [105]. |
| Cancer Cell Lines (KGN, COV434) | Granulosa cell-derived lines used for RNA-sequencing and mechanistic studies on EDC impacts on steroidogenesis and gene regulation [68]. |
| Liquid-Chromatography-Mass Spectrometry (LC-MS) | Technology for precise quantification of steroid hormones (e.g., pregnenolone, progesterone) in exposed tissues [68]. |
| Zinc Oxide Nanoparticles (ZnO-NPs) | Used as a nanoscopic drug carrier and contrast agent; also studied for its own reproductive toxicity via ROS generation [105] [106]. |
Specific Examples from Reproductive Toxicology
The selective estrogen receptor modulator (SERM) lasofoxifene provides a clear example of both the utility and limitations of animal models. In female rats, lasofoxifene treatment caused a reversible cessation of the estrous cycle and inhibited implantation, effects consistent with its estrogen-modulating class [107]. While this confirms that animal models can capture gross reproductive pharmacological effects, they may not predict the full spectrum of human-specific outcomes. Similarly, studies on nanoparticles (NPs), which are increasingly present in consumer products, show that NPs like ZnO can induce reactive oxygen species (ROS) and cause DNA damage in a mouse Sertoli cell line, potentially impairing the blood-testis barrier [105]. However, the relevance of the exact molecular mechanisms and susceptibility for human testicular cells requires direct investigation using human-derived cells and tissues.
Methodological Frameworks for Enhancing Translation
To overcome species-specific differences, researchers must adopt rigorous and human-relevant experimental methodologies. The following protocols and approaches are designed to strengthen the translational value of data generated from both animal and alternative models.
Experimental Protocol for Ex Vivo Human Tissue Assessment
This protocol is critical for direct human-relevant hazard identification.
- Tissue Acquisition: Obtain human ovarian cortical tissue from consented patients (e.g., during Caesarean sections) [68].
- Tissue Culture: Divide tissue into explants and maintain in specialized culture media for 6 days.
- Chemical Exposure: Expose tissue explants to a range of environmentally relevant concentrations of the EDC under investigation (e.g., 10⁻¹⁰ M to 10⁻⁶ M for DES; 10⁻⁹ M to 10⁻⁵ M for KTZ) [68].
- Endpoint Analysis:
- Histological Analysis: Fix, section, and stain tissue to quantify follicle survival, density, and developmental stage (unilaminar, secondary).
- Steroid Profiling: Use liquid-chromatography-mass spectrometry (LC-MS) to quantify steroid hormones (pregnenolone, progesterone, etc.) in the culture media [68].
- Transcriptomic Analysis: Perform RNA-sequencing on exposed primary ovarian cells or cell lines (e.g., KGN, COV434) to identify differentially expressed genes and pathways [68].
- Biomarker Validation: Select candidate biomarkers (e.g., SCD) from transcriptomic data and validate using qPCR and in situ RNA hybridization in the original tissue [68].
Integrated Workflow for Cross-Species Comparison
The following diagram outlines a strategic workflow that integrates animal and human-derived models to systematically identify and account for species-specific differences in EDC research.
Pathway Analysis of a Model EDC: Bisphenol A (BPA)
BPA is a model endocrine disruptor whose mechanisms illustrate the complex signaling networks that can diverge between species. It promotes tumorigenesis and chemoresistance through multiple interconnected pathways.
Navigating species-specific differences is not an insurmountable obstacle but a critical factor that must be systematically addressed in the design and interpretation of research on EDCs and reproductive health. The quantitative data shows that while animal models remain a valuable component of biomedical research, their predictive power for human outcomes is constrained. The low rate of final regulatory approval for therapies developed in animals underscores the necessity for more human-relevant models and robust study designs [103]. In the specific context of EDCs, which can cause effects that are only seen long after exposure—including in future generations—the limitations of traditional animal models are particularly pronounced [102]. The future of accurate risk assessment and therapeutic development lies in the integrated use of advanced tools, such as ex vivo human tissue cultures, 'omics' technologies, and carefully designed cross-species comparative studies. By adopting these sophisticated methodological frameworks, researchers can better elucidate the complex mechanisms of EDCs, leading to improved protective strategies, more effective therapies for reproductive diseases, and ultimately, better health outcomes for humans.
The declining rates of human fertility and the rising incidence of reproductive cancers represent a significant global health challenge. A growing body of evidence implicates exposure to endocrine-disrupting chemicals (EDCs) as a key environmental driver of these conditions [29] [108]. EDCs are exogenous substances that can interfere with hormonal signaling by mimicking, blocking, or altering the synthesis, transport, and metabolism of endogenous hormones, thereby disrupting the reproductive system's normal function [108]. Research has consistently linked EDC exposure to adverse outcomes such as impaired semen quality, decreased ovarian reserve, polycystic ovary syndrome (PCOS), and infertility [29] [108]. In this context, biomarkers—defined as objective indicators of normal biological processes, pathogenic processes, or responses to an exposure or intervention—are indispensable tools [109]. They are critical for quantifying EDC exposure, understanding their mechanisms of action, identifying individuals at risk, and evaluating the efficacy of interventions. The journey of a biomarker from discovery to clinical acceptance is arduous, with only approximately 0.1% of candidate biomarkers progressing to routine clinical use [110]. This underscores the paramount importance of rigorous, systematic validation, with sensitivity and specificity serving as the foundational metrics for establishing a biomarker's clinical utility.
Biomarker Categories and the Context of Use
The first step in biomarker validation is defining its precise role. The U.S. Food and Drug Administration (FDA) emphasizes the concept of Context of Use (COU), which is a concise description of the biomarker's specified application in drug development or clinical care [109]. The COU determines the level and type of validation required. Biomarkers are categorized based on their application, and a single biomarker can fall into multiple categories depending on its COU [109]. For research on EDCs and reproductive health, several categories are particularly relevant, as summarized in Table 1.
Table 1: Key Biomarker Categories in EDC and Reproductive Health Research
| Biomarker Category | Definition and Role in EDC Research | Example in Reproductive Health |
|---|---|---|
| Susceptibility/Risk | Identifies individuals with increased susceptibility or risk of developing a condition from EDC exposure [109]. | BRCA1/2 mutations for breast/ovarian cancer risk [109]. |
| Diagnostic | Used to detect or confirm the presence of a disease or condition [109]. | Hemoglobin A1c for diabetes; Blood-based biomarkers for Alzheimer's pathology [109] [111]. |
| Monitoring | Assesses the status of a disease or medical condition over time [109]. | HCV RNA viral load for Hepatitis C infection [109]. |
| Predictive | Identifies individuals more likely to experience a favorable or unfavorable effect from a specific treatment or exposure [109]. | EGFR mutation status predicting response to targeted therapy in lung cancer [109]. |
| Pharmacodynamic/Response | Shows a biological response has occurred in an individual after an exposure or therapeutic intervention [109]. | Changes in hormone levels (e.g., LH, FSH) following EDC exposure [108]. |
| Safety | Measures the presence or extent of toxicity or adverse effects related to an exposure or intervention [109]. | Serum creatinine for monitoring kidney injury during drug treatment [109]. |
The validation pathway for a diagnostic biomarker for EDC-induced infertility, for instance, would differ significantly from that of a pharmacodynamic biomarker intended to show a biological response in a preclinical study. This principle is known as "fit-for-purpose" validation, where the extent and nature of validation are tailored to the specific COU [109] [110].
Foundational Validation Concepts: Sensitivity and Specificity
At the heart of clinical validation are the twin pillars of sensitivity and specificity. These metrics evaluate the biomarker's ability to correctly identify individuals with and without the target condition.
- Sensitivity (True Positive Rate): The proportion of individuals with the disease (or condition) who test positive. A highly sensitive test is effective at ruling out the disease when the result is negative (few false negatives).
- Specificity (True Negative Rate): The proportion of individuals without the disease who test negative. A highly specific test is effective at ruling in the disease when the result is positive (few false positives).
The required thresholds for sensitivity and specificity are dictated by the COU. For example, the Alzheimer's Association's 2025 clinical practice guideline for blood-based biomarkers stipulates that a test used as a triaging tool must have ≥90% sensitivity and ≥75% specificity, while a test serving as a confirmatory substitute for established methods must have ≥90% for both metrics [111]. This performance-based, brand-agnostic approach ensures that only adequately validated tests are integrated into clinical practice.
The Biomarker Validation Pipeline: From Discovery to Clinical Use
The journey of a biomarker from initial discovery to clinical application is a structured, multi-stage process designed to ensure robustness and reliability. The following diagram illustrates this pipeline, highlighting key stages and decision points.
Diagram 1: The Biomarker Development and Validation Pipeline
Stage 1: Analytical Validation
Analytical validation ensures that the assay used to measure the biomarker is reliable, reproducible, and accurate for its intended purpose [112]. It answers the question: "Does the test measure the biomarker correctly?" This stage involves a rigorous assessment of the assay's performance characteristics, as detailed in Table 2.
Table 2: Key Parameters for Analytical Validation of Biomarker Assays
| Parameter | Definition | Importance in EDC Research |
|---|---|---|
| Accuracy | The closeness of agreement between a measured value and a known reference value [112]. | Ensures EDC or biomarker levels are measured without bias. |
| Precision | The closeness of agreement between a series of measurements from the same sample (repeatability and reproducibility) [112]. | Guarantees consistent results across different labs and times. |
| Analytical Sensitivity | The lowest concentration of an analyte that can be reliably distinguished from zero [110]. | Critical for detecting low-abundance EDCs or hormonal changes. |
| Analytical Specificity/Selectivity | The ability to measure the analyte accurately in the presence of other components (e.g., metabolites, matrix) [112]. | Confirms the assay is not cross-reacting with other similar chemicals. |
| Dynamic Range | The range of analyte concentrations over which the assay provides accurate and precise results [110]. | Allows quantification across a wide spectrum of exposure levels. |
| Stability | The integrity of the analyte under specific storage conditions and freeze-thaw cycles [112]. | Essential for biobanked samples used in longitudinal EDC studies. |
Stage 2: Clinical Validation
Clinical validation establishes that the biomarker is consistently and accurately associated with the clinical outcome or phenotype of interest [109] [112]. It answers the question: "Is the biomarker associated with the disease or exposure?" For EDC research, this involves demonstrating a statistically significant association between the biomarker (e.g., a specific EDC level in blood or urine) and a reproductive health endpoint (e.g., reduced sperm motility, PCOS diagnosis). This is typically achieved through well-designed observational studies (cohort, case-control) and requires careful consideration of confounding factors, sample size, and population diversity [108]. The outcomes of clinical validation are the calculations of sensitivity, specificity, and predictive values in the intended-use population.
Experimental Protocols and Advanced Methodologies
The choice of technology for biomarker measurement is critical. While traditional methods like Enzyme-Linked Immunosorbent Assay (ELISA) have been the gold standard, advanced platforms offer superior performance for complex validation studies [110].
Table 3: Comparison of Biomarker Analytical Platforms
| Platform | Principle | Advantages | Considerations for EDC Research |
|---|---|---|---|
| ELISA | Antibody-based colorimetric detection. | High specificity; well-established; relatively low cost per sample for single-plex [110]. | Narrow dynamic range; potential for antibody cross-reactivity; lower throughput for multiple analytes [110]. |
| Meso Scale Discovery (MSD) | Electrochemiluminescence detection using antibody-coated spots. | Higher sensitivity (up to 100x) and broader dynamic range than ELISA; multiplexing capability saves sample and cost [110]. | Ideal for measuring panels of inflammatory or hormonal biomarkers in response to EDC exposure. |
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Physical separation followed by mass-based detection. | Unmatched specificity and sensitivity; can detect hundreds of analytes; not reliant on antibodies [110]. | The "gold standard" for directly quantifying specific EDCs (e.g., BPA, phthalates, PFAS) and their metabolites in complex biological matrices. |
A Protocol for Validating an EDC Exposure Biomarker Using LC-MS/MS
The following workflow details a typical protocol for validating a biomarker measuring a specific EDC (e.g., Bisphenol A) in human serum using LC-MS/MS, a technology increasingly favored by regulators for its precision [110].
Diagram 2: LC-MS/MS Workflow for EDC Biomarker Quantification
- Sample Collection and Pre-analytical Handling: Collect blood or urine samples from a defined cohort (e.g., fertility clinic patients). Standardize procedures: use certified chemical-free collection tubes, process samples (e.g., centrifugation) within a strict time window, and store aliquots at -80°C to preserve analyte stability [112]. Meticulous documentation of freeze-thaw cycles is essential.
- Sample Preparation (Extraction): Thaw samples on ice. Add a known quantity of isotopically labeled internal standard (e.g., ¹³C-BPA) to each sample to correct for matrix effects and recovery losses. Perform solid-phase extraction (SPE) to remove interfering compounds and concentrate the analytes.
- Instrumental Analysis (LC-MS/MS):
- Liquid Chromatography: Inject the extracted sample onto the LC system. The BPA and internal standard are separated from other components in the sample matrix using a reverse-phase C18 column and a gradient of water and organic solvent (e.g., methanol).
- Mass Spectrometry: The eluting compounds are ionized (e.g., by electrospray ionization in negative mode). Specific precursor ions for BPA and the internal standard are selected in the first mass analyzer, fragmented in a collision cell, and characteristic product ions are selected in the second mass analyzer. This multiple reaction monitoring (MRM) provides high specificity.
- Data Analysis and Quantification: Integrate the peak areas for the BPA and internal standard MRM transitions. A calibration curve is constructed by analyzing spiked standards with known concentrations. The ratio of the BPA peak area to the internal standard peak area is used to calculate the absolute concentration of BPA in the original sample with high accuracy and precision.
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Key Research Reagent Solutions for Biomarker Validation
| Reagent/Material | Function and Importance |
|---|---|
| Certified Reference Standards | Pure, well-characterized analyte (e.g., BPA, PFAS) for preparing calibration curves and quality controls. Essential for establishing accuracy [112]. |
| Stable Isotope-Labeled Internal Standards | Chemically identical analogs of the analyte labeled with ¹³C or ²H. Added to every sample to correct for matrix effects and variable extraction efficiency, dramatically improving data quality in LC-MS/MS [110]. |
| Certified Chemical-Free Collection Tubes | Specialized blood collection tubes that do not leach contaminants like phthalates or BPA, which is critical for avoiding false positives in EDC research. |
| High-Purity Solvents and Reagents | Ultra-pure grade solvents (e.g., methanol, water) are mandatory to minimize background noise and interference in sensitive assays like LC-MS/MS. |
| Validated Antibody Panels | For immunoassay-based platforms (MSD, ELISA), antibodies with high specificity and affinity are required. Validation data for the specific sample matrix (e.g., plasma, urine) is crucial [110]. |
Regulatory Frameworks and Future Trends
Regulatory acceptance is the final hurdle for biomarker qualification. In the United States, the FDA provides pathways such as the Biomarker Qualification Program (BQP), which offers a framework for developing and qualifying a biomarker for a specific COU across multiple drug development programs [109]. Early engagement with regulators via pre-IND meetings or the Critical Path Innovation Meetings is strongly encouraged to align on the validation strategy [109].
Future trends point toward:
- Multi-omics Integration: Combining data from genomics, proteomics, and metabolomics to create comprehensive biomarker signatures for complex diseases like EDC-induced infertility [113].
- Artificial Intelligence (AI): Using AI and machine learning to analyze complex datasets, identify novel biomarker patterns, and improve predictive models for disease progression and treatment response [113].
- Liquid Biopsies: Expanding the use of minimally invasive liquid biopsies beyond oncology into other areas, potentially for monitoring reproductive health status [113].
- Standardization and Real-World Evidence: Increased collaborative efforts to standardize protocols and a greater regulatory acceptance of real-world evidence to demonstrate clinical utility [113].
The establishment of sensitive and specific biomarkers is a cornerstone for advancing research on the impact of EDCs on infertility and reproductive cancers. This process, guided by a fit-for-purpose principle and a rigorous, multi-stage validation pipeline, transforms promising discoveries into reliable tools for clinical and regulatory decision-making. As technological capabilities and regulatory frameworks evolve, the continued refinement of biomarker validation practices will be essential for accurately quantifying exposure, understanding mechanisms, and ultimately mitigating the public health burden posed by endocrine-disrupting chemicals.
Within the broader investigation of the impact of endocrine-disrupting chemicals (EDCs) on infertility and reproductive cancers, understanding the temporal dimension of exposure is paramount. The concepts of critical exposure windows and latent disease manifestation explain why an exposure encountered at one life stage may not result in clinical disease until much later, a phenomenon central to the Developmental Origins of Health and Disease (DOHaD) paradigm [114]. This paradigm posits that exposures before birth and during early childhood can influence the risk of adult-onset diseases [114]. For researchers and drug development professionals, appreciating these temporal factors is crucial for designing studies, identifying biomarkers, and developing preventative strategies. This guide synthesizes current evidence and methodologies for investigating these complex exposure-disease relationships, with a specific focus on EDCs and reproductive pathologies.
Critical Windows of Susceptibility
The timing of exposure to EDCs can be as critical as the dose. Specific life stages are characterized by rapid cellular proliferation and organogenesis, making them exceptionally vulnerable to disruption.
The DOHaD Paradigm and EDCs
The DOHaD framework, originally focused on nutrition, has since expanded to include environmental chemical exposures [114]. Exposure during the first 1,000 days of life (from conception to approximately two years of age) is now recognized as a period of heightened susceptibility, programming the risk for adverse health outcomes in adulthood [12] [114]. Exposures to parents before conception can also affect a child's lifetime health, suggesting that critical windows can span generations [114].
Key Vulnerable Life Stages
The following table summarizes the primary critical windows and their associated reproductive health risks.
Table 1: Critical Windows of Susceptibility to EDCs and Associated Reproductive Health Outcomes
| Life Stage | Key Reproductive Processes | Potential Latent Outcomes (Infertility/Reproductive Cancers) | Supporting Evidence |
|---|---|---|---|
| In Utero | Formation of primordial germ cells, reproductive tract development, gonadal differentiation [12]. | Vaginal clear-cell adenocarcinoma (DES), reproductive tract abnormalities, altered ovarian follicle pool, premature ovarian insufficiency (POI), testicular dysgenesis syndrome [12] [115] [116]. | The diethylstilbestrol (DES) case study provides compelling human evidence for in utero effects [12]. |
| Early Postnatal & Childhood | Continued brain and reproductive tract maturation, prepubertal hormonal milieu establishment [114]. | Altered timing of puberty, impaired sperm quality in adulthood, subfertility [115]. | Perinatal exposure to phthalates/pesticides is linked to delayed pubertal onset and altered steroid profiles in adolescence [115]. |
| Adulthood | Cyclic ovarian function, spermatogenesis, endometrial receptivity, hormonal homeostasis [12]. | Anovulation, poor oocyte quality, endometriosis, reduced sperm parameters, implantation failure [12] [115]. | Professional and environmental EDC exposure in adults is associated with reduced IVF success and altered semen parameters [12] [115]. |
Mechanisms of Latent Disease Manifestation
The lag between EDC exposure and disease onset is mediated through several key biological mechanisms. Understanding these is essential for tracing the pathogenic pathway from a specific exposure window to a later clinical diagnosis.
Epigenetic Reprogramming
EDCs can cause epigenetic modifications, including alterations in DNA methylation, histone modifications, and non-coding RNA expression [114] [115]. These changes can alter the expression of genes critical for reproduction—such as those regulating meiosis, germ cell differentiation, and steroidogenesis—without changing the DNA sequence itself [115]. Crucially, some of these epigenetic marks can be transmitted across generations, leading to transgenerational inheritance of increased disease susceptibility [114] [115].
Oxidative Stress and Cellular Damage
Several EDCs induce oxidative stress in ovarian and testicular tissues, damaging cells and impairing their function [12] [115]. This oxidative damage can lead to a reduced ovarian follicle pool or impaired spermatogenesis, effects that may not become apparent until the individual attempts to conceive years later [12].
Alterations in the Hypothalamic-Pituitary-Gonadal (HPG) Axis
The HPG axis is a prime target for EDCs. Exposure during critical developmental windows can induce long-lasting programming effects on the HPG axis, permanently altering the set-point for hormone secretion and feedback loops [12] [115]. This can manifest in adulthood as altered LH/FSH ratios, reduced testosterone production, and delayed puberty [115].
The diagram below illustrates the core concept of how an initial EDC exposure during a critical window leads to a latent disease through key mechanistic pathways.
Experimental Models and Methodologies for Investigating Latency
Connecting early-life EDC exposure to later-life disease requires sophisticated experimental models that can capture latent effects. The following section details established protocols and a key reagent toolkit.
In Utero Exposure Rodent Models
This protocol is a cornerstone for investigating the developmental origins of disease.
- Objective: To determine the effects of gestational EDC exposure on adult reproductive function and disease risk in offspring.
- Detailed Protocol:
- Animal Housing: House timed-pregnant females (e.g., C57BL/6 or CD-1 mice) under standard conditions.
- Exposure Regimen: Randomly assign dams to treatment groups. Administer the EDC (e.g., BPA, phthalates, DES) or vehicle control via oral gavage or in drinking/diet. A critical period is often during mid-gestation (e.g., embryonic days 10-18), coinciding with reproductive tract organogenesis.
- Parturition and Litter Standardization: Allow dams to give birth. On postnatal day (PND) 1, standardize litters to a uniform size and sex ratio to minimize confounding effects of litter size and maternal care.
- Cross-Fostering (Optional): To separate in utero from lactational exposure, cross-foster pups from exposed dams to control dams at birth, and vice versa.
- Offspring Monitoring: Wean offspring at PND 21. Do not expose them further to the chemical.
- Longitudinal Endpoint Analysis:
- Puberty Assessment: Monitor for vaginal opening in females and preputial separation in males.
- Adult Tissue Collection: Sacrifice a cohort of animals in young adulthood (e.g., 3-6 months). Collect reproductive tissues (ovaries, testes, uteri, prostate), blood for hormone assays, and sperm for quality analysis (concentration, motility, morphology).
- Fertility Testing: Mate additional exposed and control animals and track time to pregnancy, litter size, and pup viability.
- Molecular Analysis: Analyze tissues for epigenetic marks (e.g., DNA methylation of key genes), transcriptomic profiles, and histopathological changes (e.g., ovarian follicle counts, testicular atrophy).
Human-Relevant In Vitro Ovarian Culture
This methodology allows for direct investigation of EDC effects on human tissue, bypassing species-specific differences.
- Objective: To identify biomarkers and mechanisms of endocrine disruption in the human ovarian cortex.
- Detailed Protocol (adapted from [68]):
- Tissue Acquisition: Obtain human ovarian cortical tissue with ethical approval from patients undergoing Caesarean sections or other surgical procedures.
- Tissue Preparation and Culture: Mince the cortical tissue into small fragments (1-2 mm³) under sterile conditions. Culture fragments in vitro for 6 days in a controlled atmosphere (37°C, 5% CO₂).
- Chemical Exposure: Explicate tissue fragments to a range of EDC concentrations (e.g., DES 10⁻¹⁰ M - 10⁻⁶ M; Ketoconazole 10⁻⁹ M - 10⁻⁵ M) or vehicle control. Refresh media containing treatments every 2-3 days.
- Endpoint Analysis:
- Histology: Fix fragments, embed in paraffin, section, and stain (e.g., H&E). Quantify follicle densities and classify follicles by developmental stage (primordial, primary, secondary).
- Steroidogenesis: Analyze culture media using liquid-chromatography-mass spectrometry (LC-MS) to quantify steroid hormone levels (e.g., pregnenolone, progesterone).
- Transcriptomics: Perform RNA-sequencing on exposed primary ovarian cells or established cell lines (e.g., KGN, COV434). Use bioinformatic analyses (e.g., Gene Set Variation Analysis - GSVA) to identify altered pathways (e.g., folliculogenesis, steroidogenesis).
- Biomarker Validation: Select candidate biomarkers (e.g., SCD, DHCR7) from RNA-seq data for validation using qPCR, in situ RNA hybridization, and immunofluorescence [68].
The Scientist's Toolkit: Key Research Reagent Solutions
The table below catalogues essential materials and their functions for the experiments described above.
Table 2: Essential Research Reagents for Investigating EDC Latent Effects
| Reagent / Material | Function / Application | Example Use-Case |
|---|---|---|
| Bisphenol A (BPA) | A model EDC; plasticizer with estrogenic activity. Used to investigate ER-mediated disruption [12] [115] [116]. | In utero exposure model to study latent effects on sperm quality and ovarian function [115]. |
| Diethylstilbestrol (DES) | A potent synthetic estrogen; positive control for estrogenic EDCs and transgenerational studies [12] [116]. | Human ovarian culture to study direct effects on follicle survival and gene expression [68]. |
| Human Ovarian Cortical Tissue | Primary ex vivo model for direct human-relevant toxicity screening and biomarker discovery [68]. | Histological analysis to quantify EDC-induced changes in follicle survival and growth [68]. |
| KGN & COV434 Cell Lines | Human granulosa cell-derived lines; models for studying steroidogenesis and gene expression in vitro [68]. | RNA-sequencing to identify differentially expressed genes and disrupted pathways after EDC exposure [68]. |
| LC-MS/MS Systems | Highly sensitive quantification of steroid hormones (e.g., progesterone, testosterone) from biological matrices [68]. | Profiling steroidogenic output from exposed ovarian cultures or serum samples [68]. |
| DNA Methylation Kits | Tools for analyzing epigenetic modifications, such as whole-genome bisulfite sequencing or targeted methylation assays. | Investigating transgenerational inheritance of epigenetic marks in sperm from exposed lineages [114] [115]. |
The following workflow diagram maps the experimental journey from a hypothesis to data generation using these key tools.
Key Characteristics of EDCs and Latent Disease Risk
The "Key Characteristics" (KCs) framework provides a systematic tool for organizing mechanistic evidence of endocrine disruption, which is vital for predicting and understanding latent risks [116].
Table 3: Key Characteristics of EDCs Relevant to Latent Effects [116]
| Key Characteristic (KC) | Description | Implication for Latent Disease |
|---|---|---|
| KC1: Interacts with or activates hormone receptors | EDCs mimic endogenous hormones (e.g., estrogen) and bind to their receptors [12] [116]. | Inappropriate receptor activation during development can permanently alter tissue programming, increasing cancer risk (e.g., vaginal, prostate) [116]. |
| KC2: Antagonizes hormone receptors | EDCs block receptors, preventing natural hormones from binding and acting [116]. | AR antagonism in utero (e.g., by vinclozolin) can cause malformations and latent reproductive dysfunction [115] [116]. |
| KC3: Alters hormone receptor expression | EDCs can change the abundance of hormone receptors in tissues [116]. | Alters the sensitivity of tissues to hormones later in life, disrupting cyclical processes like the menstrual cycle [116]. |
| KC4: Alters signal transduction in hormone-responsive cells | EDCs interfere with intracellular messaging cascades triggered by hormones [116]. | Disrupts critical cellular functions like calcium signaling, potentially leading to long-term functional deficits (e.g., in insulin secretion) [116]. |
| KC10: Alters hormone synthesis, transport, or metabolism | EDCs can affect the enzymes that produce or break down hormones [115] [116]. | Can lead to permanent hormonal imbalances after exposure has ended, affecting processes like steroidogenesis in adulthood [115]. |
The final diagram integrates the Key Characteristics into the temporal sequence of EDC action, from initial exposure to latent disease, highlighting the multifaceted mechanisms at play.
Epidemiological Correlations and Regulatory Science for EDC Risk Mitigation
The study of Endocrine-Disrupting Chemicals (EDCs) and their impact on human infertility and reproductive cancers represents a critical frontier in public health research. Establishing causal relationships between environmental exposures and complex health outcomes requires the integration of epidemiological data with mechanistic findings to build a definitive body of human evidence. Epidemiological studies reveal statistical associations between EDC exposure and health effects in human populations, while mechanistic research elucidates the biological pathways through which these chemicals exert their effects. The convergence of these evidence streams is essential not only for establishing biological plausibility but also for informing regulatory decisions and guiding therapeutic interventions [14] [117].
The integration of these disparate data types presents significant methodological challenges, including differences in study design, exposure assessment, and analytical frameworks. Traditional risk assessment approaches often struggle to fully utilize epidemiological data due to concerns about exposure misclassification, confounding, and insufficient characterization of dose-response relationships [117]. Meanwhile, mechanistic studies conducted in laboratory settings may not adequately reflect human biological complexity or real-world exposure scenarios. This technical guide provides a comprehensive framework for effectively bridging these research domains, with specific application to EDC effects on infertility and reproductive cancers, offering researchers structured methodologies for generating more actionable evidence for risk assessment and drug development [117].
Key Mechanistic Pathways Linking EDCs to Reproductive Pathologies
EDCs interfere with reproductive health through multiple interconnected biological pathways. Understanding these mechanisms is crucial for designing epidemiological studies that capture relevant biomarkers and intermediate outcomes.
Receptor-Mediated Hormone Disruption
Many EDCs directly interact with hormone receptors, mimicking or blocking endogenous hormones. Bisphenol A (BPA) exhibits nanomolar binding affinities (Ki ≈ 5-10 nM) for estrogen receptors ERα/ERβ, leading to upregulation of estrogen-responsive transcription in reproductive tissues [14]. Similarly, phthalates function as androgen receptor antagonists, with vinclozolin showing IC50 values below 1 μM. These receptor interactions disrupt delicate hormonal communication essential for reproductive processes, with epidemiological studies documenting that males in the highest quartile of urinary phthalate metabolites have 12-15% lower serum testosterone levels compared to low-exposure groups [14].
Epigenetic Modifications
EDCs can induce heritable epigenetic changes that alter gene expression without changing DNA sequence. Multiple EDCs including BPA, phthalates, and dioxins have been shown to alter DNA methylation patterns, histone modifications, and non-coding RNA expression in reproductive tissues [69]. These epigenetic disruptions can manifest as transgenerational reproductive effects, with altered imprinting of genes such as ASCL2 and HOXA10 implicated in uterine disorders and recurrent pregnancy loss [69]. The same EDC can produce diametrically opposite epigenetic effects depending on exposure timing, dose, and target tissue, highlighting the complexity of these mechanisms [69].
Oxidative Stress and Apoptosis
EDCs including heavy metals, pesticides, and plasticizers induce reactive oxygen species (ROS) generation and mitochondrial dysfunction in reproductive tissues. This oxidative stress leads to sperm DNA damage, apoptosis in testicular cells, and impaired ovarian function [14]. The resulting cellular damage compromises gamete quality and reproductive organ function, providing a mechanistic bridge between EDC exposure and clinical infertility outcomes observed in epidemiological studies [14] [108].
Table 1: Key Mechanistic Pathways of EDCs in Reproductive Pathology
| Mechanistic Pathway | Example EDCs | Molecular Targets | Reproductive Consequences |
|---|---|---|---|
| Hormone Receptor Interaction | BPA, phthalates, vinclozolin | ERα/ERβ, AR, thyroid receptors | Altered gene expression, reduced testosterone, impaired spermatogenesis |
| Epigenetic Modifications | BPA, phthalates, dioxins | DNA methyltransferases, histone modifiers | Transgenerational effects, poor sperm quality, uterine disorders |
| Oxidative Stress | Heavy metals, pesticides, BPA | Mitochondrial electron transport chain | Sperm DNA damage, apoptosis, impaired ovarian function |
| HPG Axis Disruption | Phthalates, organochlorine pesticides | GnRH, LH, FSH signaling | Reduced steroidogenesis, delayed puberty, hormonal imbalances |
Epidemiological Evidence: Quantitative Associations Between EDCs and Reproductive Outcomes
Robust epidemiological studies provide the population-level evidence linking EDC exposure to measurable reproductive health endpoints. The tables below summarize key findings from recent human studies.
Table 2: Epidemiological Evidence for EDCs and Male Reproductive Outcomes
| EDC Class | Study Design | Exposure Measure | Key Findings | Effect Size |
|---|---|---|---|---|
| Phthalates | Cross-sectional cohort | Urinary metabolites | Reduced sperm motility, lower serum testosterone | 12-15% decrease in testosterone in highest quartile |
| BPA | Multiple cohorts | Urinary BPA | Decreased sperm concentration, altered morphology | 10-15% reduction in blood testosterone |
| Organophosphate pesticides | Longitudinal birth cohort | Prenatal exposure | Delayed pubertal onset in males | 6-12 month delay |
| Multiple EDCs | Meta-analysis | Various biomarkers | Declining sperm concentration (1973-2011) | ~50% decrease in industrialized regions |
Table 3: Epidemiological Evidence for EDCs and Female Reproductive Outcomes
| EDC Class | Health Endpoint | Study Design | Key Findings | Effect Size |
|---|---|---|---|---|
| PFAS, Phthalates | Menopause timing | Cohort study | Earlier menopause with combined exposure | 1.9-3.8 years sooner |
| BPA, Phthalates | Polycystic Ovary Syndrome | Case-control | Increased PCOS prevalence | Up to 20% in high-exposure regions |
| Multiple EDCs | Infertility | Systematic review | Impaired ovarian reserve, reduced IVF success | Significant association across 14 studies |
| DES | Uterine fibroids | Prospective cohort | Increased incidence with prenatal exposure | 76% in exposed white women |
Epidemiological evidence consistently demonstrates that EDC exposure is associated with adverse reproductive outcomes in both males and females. Significant associations have been documented between EDCs and 22 cancer outcomes, 21 neonatal/infant/child-related outcomes, 18 metabolic disorder outcomes, and 11 pregnancy-related outcomes according to a comprehensive umbrella review of 67 meta-analyses [118]. The strength of these associations varies by chemical class, exposure timing, and population characteristics, but the overall pattern supports the biological plausibility of EDCs as contributors to the increasing global burden of reproductive disorders [108].
Methodological Framework: Integrating Epidemiological and Mechanistic Data
Experimental Protocols for Mechanistic Research
In Vitro Receptor Binding Assays Purpose: Quantify direct interactions between EDCs and hormone receptors. Protocol:
- Express human estrogen (ERα/ERβ) or androgen (AR) receptors in reporter cell lines
- Expose to EDCs at concentrations ranging from 0.1 nM to 10 μM
- Measure competitive displacement of radiolabeled native hormones (e.g., ³H-estradiol)
- Calculate binding affinities (Ki values) and IC50 values for receptor antagonism
- Assess transcriptional activation using reporter gene assays (luciferase) Outcome Measures: Dose-response curves, receptor binding parameters, EC50/IC50 values [14]
Epigenetic Modification Assessment Purpose: Identify EDC-induced alterations in DNA methylation and histone modifications. Protocol:
- Expose human reproductive cell lines (e.g., Sertoli cells, granulosa cells) or tissue explants to EDCs
- Extract genomic DNA and perform bisulfite sequencing for DNA methylation analysis
- Conduct chromatin immunoprecipitation (ChIP) for histone modifications (H3K4me3, H3K27ac)
- Analyze genome-wide patterns using microarray or sequencing approaches
- Validate candidate loci using pyrosequencing Outcome Measures: Differential methylation regions, histone modification patterns, correlation with gene expression [69]
Epidemiological Study Designs with Mechanistic Components
Nested Case-Control Studies with Biomarker Analysis Purpose: Integrate population-level associations with molecular measurements. Protocol:
- Establish prospective cohort with baseline biospecimen collection (blood, urine, tissue)
- Identify incident cases of reproductive disorders (infertility, cancer) during follow-up
- Select matched controls from cohort members without endpoint
- Measure EDC concentrations in baseline samples using LC-MS/MS
- Analyze epigenetic, transcriptomic, or proteomic biomarkers in same samples
- Statistically model relationships between exposure, intermediate biomarkers, and clinical endpoints Outcome Measures: Odds ratios for EDC-disease associations, mediator effects of molecular biomarkers [69] [108]
Twinned Human Population and In Vitro Models Purpose: Directly translate epidemiological findings into testable mechanistic hypotheses. Protocol:
- Identify EDC-exposure associations in human cohorts
- Culture primary human reproductive cells or use differentiated stem cell models
- Expose to same EDCs at concentrations relevant to human exposure
- Assess pathway perturbations identified in epidemiological analyses
- Validate findings using reverse translation in animal models Outcome Measures: Concordance between human biomarkers and in vitro pathways, mechanistic confirmation of observational associations [14] [69]
Advanced Integration Approaches: Artificial Intelligence and Novel Methodologies
The integration of artificial intelligence (AI) with traditional epidemiological and mechanistic approaches represents a promising frontier for EDC research. AI techniques can enhance the analysis of complex, high-dimensional data generated from both population studies and laboratory experiments [119].
Physics-Informed Neural Networks (PINNs) incorporate disease transmission mechanisms represented by differential equations directly into neural network architectures. This approach has been successfully applied to epidemiological modeling of infectious diseases and can be adapted for EDC research by encoding known endocrine disruption pathways into network loss functions [119]. Similarly, Epidemiology-Aware AI Models (EAAMs) extend standard AI architectures by assimilating epidemiological knowledge into their structures, training processes, and validation frameworks, enabling more biologically plausible integration of population data with mechanistic insights [119].
These advanced approaches address key limitations in traditional methods, including the ability to handle non-monotonic dose responses characteristic of many EDCs, model mixture effects from multiple concurrent exposures, and account for critical windows of susceptibility during development [14] [119]. The application of these methods to EDC research requires interdisciplinary collaboration between environmental epidemiologists, molecular biologists, and data scientists to ensure biological validity and translational relevance.
Visualizing Integrated Pathways and Workflows
EDC Pathogenesis and Data Integration Pathway
Integrated Research Workflow for EDC Studies
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Essential Research Reagents and Platforms for Integrated EDC Studies
| Tool Category | Specific Examples | Application in EDC Research | Key Features |
|---|---|---|---|
| Exposure Assessment | LC-MS/MS systems, ELISA kits | Quantifying EDCs and metabolites in biological samples | High sensitivity, specificity for low-concentration analyses |
| Molecular Receptors | Human ERα/ERβ, AR reporter cell lines | Assessing receptor binding and transcriptional activation | Standardized platforms for endocrine activity screening |
| Epigenetic Analysis | Bisulfite conversion kits, ChIP-grade antibodies | DNA methylation and histone modification mapping | Genome-wide and locus-specific analysis capabilities |
| Cell Models | Primary reproductive cells, organoid cultures | Mechanistic studies in relevant human cell types | Preservation of tissue-specific functions and responses |
| OMICs Platforms | Transcriptomic microarrays, DNA sequencers | High-throughput molecular profiling | Unbiased discovery of novel pathways and biomarkers |
| AI/ML Tools | Physics-Informed Neural Networks (PINNs) | Integrating mechanistic knowledge with data patterns | Combining data-driven learning with biological constraints |
The integration of epidemiological data with mechanistic findings represents the most promising approach for establishing causal relationships between EDC exposure and reproductive health outcomes. As research in this field advances, several priority areas emerge: First, there is a critical need to develop improved exposure assessment methods that capture the complexity of real-world EDC mixtures and account for non-monotonic dose responses [14] [117]. Second, researchers must expand the incorporation of epigenetic endpoints into longitudinal epidemiological studies to better understand how developmental exposures program lifelong reproductive health [69]. Finally, the field must embrace advanced computational approaches, including AI and machine learning, to overcome the limitations of traditional statistical methods when dealing with complex, high-dimensional data [119].
From a regulatory perspective, integrated approaches offer the evidence needed to support more protective chemical policies. Risk assessors have expressed dissatisfaction with the current utility of epidemiological studies, citing deficiencies in exposure assessment and insufficient characterization of uncertainty [117]. By systematically integrating mechanistic insights into epidemiological frameworks, researchers can address these limitations and provide more actionable evidence for decision-making. This is particularly urgent for protecting vulnerable populations during critical windows of development, where EDC exposures may cause permanent reproductive damage that manifests as infertility or reproductive cancers later in life [26] [118]. The methodologies outlined in this review provide a roadmap for generating the robust, convergent evidence needed to guide both clinical interventions and public health protections.
Endocrine-disrupting chemicals (EDCs) are exogenous substances that interfere with the normal function of the endocrine system by mimicking, blocking, or altering the synthesis, transport, metabolism, or elimination of endogenous hormones [6]. The reproductive system, being highly dependent on hormonal signaling, is particularly vulnerable to EDC exposure. Growing evidence suggests that EDCs are significant contributors to the increasing global incidence of reproductive disorders, including infertility and reproductive cancers [26] [28]. This review provides a comprehensive comparative analysis of the pathological effects of EDCs on male and female reproductive systems, framed within the context of their impact on infertility and reproductive cancer research. Understanding these sex-specific mechanisms is crucial for developing targeted therapeutic interventions and informed regulatory policies.
Mechanisms of Endocrine Disruption
EDCs employ multiple molecular mechanisms to disrupt reproductive endocrinology in both sexes. The primary mechanisms include:
Receptor-Mediated Actions: Many EDCs function as receptor agonists or antagonists. Estrogenic EDCs such as bisphenol A (BPA) and phthalates bind to estrogen receptors, while anti-androgenic chemicals like certain pesticides interfere with androgen receptor signaling [95] [28]. This receptor mimicry or blockade alters gene expression patterns critical for reproductive function.
Epigenetic Modifications: EDCs including BPA, phthalates, dioxins, and polychlorinated biphenyls (PCBs) can alter DNA methylation patterns, histone modifications, and microRNA expression in reproductive tissues [69]. These epigenetic changes can persist across generations and influence disease susceptibility.
Hormone Synthesis and Metabolism Interference: EDCs disrupt steroidogenic enzymes, affecting the synthesis and metabolism of sex steroids. Per- and polyfluoroalkyl substances (PFAS) and organochlorine pesticides have been shown to alter aromatase activity and other key enzymes in hormone biosynthesis pathways [29] [120].
Altered Receptor Expression: Some EDCs modulate the expression levels of hormone receptors themselves, thereby changing tissue sensitivity to hormonal signals [95].
The following diagram illustrates the core molecular mechanisms through which EDCs disrupt reproductive endocrinology:
Developmental Windows of Susceptibility
Sexual differentiation is highly dependent on the fetal hormonal environment, which guides sexual development and establishes the foundation for lifelong reproductive health [26]. Critical windows of development—including fetal life, early postnatal period, puberty, and reproductive adulthood—exhibit heightened susceptibility to EDC exposure. During these sensitive periods, EDCs can reprogram developmental trajectories through organizational effects that persist throughout life [26] [6].
The fetal period represents a particularly vulnerable window, as EDCs can cross the placental barrier and interfere with the establishment of the hypothalamic-pituitary-gonadal (HPG) axis and genital tract formation [29]. Exposure during this period can lead to permanent alterations in reproductive organ structure and function, increasing susceptibility to reproductive disorders and cancers later in life [26] [69]. The following experimental workflow outlines key methodologies for assessing developmental EDC effects:
Male Reproductive Pathology
Testicular Dysfunction and Impaired Spermatogenesis
In males, disrupted androgen signaling during fetal development is strongly linked to testicular dysgenesis syndrome (TDS), a constellation of disorders including hypospadias, cryptorchidism, reduced fertility, and testicular cancer [26]. EDCs that interfere with testosterone synthesis or action during critical developmental windows can disrupt testicular descent and masculinization of the reproductive tract. Epidemiological studies have reported declining sperm counts globally, with EDC exposure identified as a significant contributing factor [120] [28].
Adult exposure to EDCs continues to impact testicular function through multiple mechanisms. Phthalates, BPA, and PFAS have been shown to damage spermatogenic and supportive cells, leading to abnormalities in testicular development and function [120]. This damage manifests as decreased sperm count and motility, increased sperm DNA damage, and elevated numbers of morphologically abnormal spermatozoa, ultimately compromising male fertility [6] [120].
Hormonal Imbalances
Recent mixture effect analyses using weighted quantile sum (WQS) regression and Bayesian kernel machine regression (BKMR) models have confirmed that exposure to environmental EDCs negatively correlates with estradiol (E2) and total testosterone (TT) levels in adult males [120]. These analytical approaches, which better reflect real-world exposure scenarios, have identified benzophenone-3 (BP3) and specific phthalate metabolites (MECPP, MECOP) as the most influential chemicals in mixtures affecting male steroid hormones [120].
The following table summarizes key quantitative findings on EDC effects on male reproductive parameters:
Table 1: Quantitative Data on EDC Effects on Male Reproductive Health
| EDC Class | Specific Chemicals | Key Findings | Effect Size/Magnitude | Study Population/Model |
|---|---|---|---|---|
| Phthalates | DEHP, MEHP, MECPP, MECOP | Negative correlation with estradiol, total testosterone, free androgen index | WQS analysis identified these as top contributors to mixture effects | 1,262 adult men (NHANES 2013-2016) [120] |
| Phenols | BP3 (Benzophenone-3) | Most highly weighted chemical in mixture affecting sex steroid hormones | Primary contributor in WQS model | 1,262 adult men (NHANES 2013-2016) [120] |
| Plasticizers | BPA, analogs | Reduced sperm count and quality | ~50-60% decline in sperm concentration in Western countries (1973-2011) [120] | Multiple epidemiological studies [120] |
| Various EDCs | Mixed exposures | Altered hormone levels | Positive correlation with SHBG and TT/E2 ratio | 1,262 adult men (NHANES 2013-2016) [120] |
Female Reproductive Pathology
Ovarian Dysfunction and Fertility Impairment
In females, EDC exposure contributes to altered ovarian function, diminished ovarian reserve, infertility, polycystic ovary syndrome (PCOS), and premature menopause [26] [29]. The ovaries are particularly vulnerable to EDCs due to their high expression of steroid hormone receptors and the complex hormonal regulation required for folliculogenesis and ovulation. BPA and phthalates have been detected in follicular fluid and have been associated with compromised oocyte quality, reduced fertilization rates, and impaired embryo implantation [6] [69].
Epigenetic mechanisms play a crucial role in EDC-induced ovarian pathology. BPA, phthalates, dioxins, and PCBs have been shown to alter DNA methylation patterns and histone modifications in ovarian tissues, leading to changes in gene expression that negatively impact ovarian function [69]. These epigenetic alterations may explain the transgenerational effects of EDCs on female reproduction observed in animal models.
Menstrual Cycle Alterations and Lifespan Impacts
EDCs significantly impact the timing and regulation of reproductive milestones across the female lifespan. Exposure to EDCs such as DDT and PFAS has been associated with earlier breast development and menarche, lengthened menstrual cycles, and accelerated menopause [29] [28]. Women with the highest combined exposure to pesticides and phthalates experience menopause 1.9-3.8 years earlier than those with lower exposure, indicating that EDCs lead to shorter reproductive lifespans [29].
The following table summarizes key quantitative findings on EDC effects on female reproductive parameters:
Table 2: Quantitative Data on EDC Effects on Female Reproductive Health
| EDC Class | Specific Chemicals | Key Findings | Effect Size/Magnitude | Study Population/Model |
|---|---|---|---|---|
| Pesticides & Phthalates | Mixed exposures | Earlier menopause | Menopause 1.9-3.8 years sooner | Women with high combined exposure [29] |
| Organochlorine pesticides | DDT, others | Earlier puberty | Trend of earlier breast development noted | Multiple epidemiological studies [29] |
| PFAS | Various PFAS | Altered menarche and menstrual function | Significantly higher age at menarche and frequency of menstrual irregularities | Cohort studies of exposed women [29] [69] |
| Plastics additives | BPA, phthalates | PCOS prevalence | Up to 20% in some regions | Regional epidemiological data [29] |
| Various EDCs | BPA, phthalates, parabens | Infertility | 14% of women in study population | 789 individuals in cross-sectional study [69] |
Uterine Pathology and Endometrial Function
The uterus is a key target for EDCs due to its hormone-responsive nature and critical role in implantation and pregnancy maintenance. EDC exposure has been linked to several uterine pathologies, including endometriosis, uterine fibroids (leiomyomas), endometrial hyperplasia, and recurrent pregnancy loss [69]. Diethylstilbestrol (DES), a synthetic estrogen, provides a compelling historical example of EDC-induced uterine pathology, with exposed women demonstrating increased incidence of uterine malformations, fibroids, and reproductive tract cancers [69] [28].
Epigenetic mechanisms underlie many EDC-induced uterine pathologies. Studies have shown that EDCs can alter the expression of imprinted genes such as ASCL2 and HOXA10, which are critical for uterine development and endometrial receptivity [69]. The complexity of EDC effects is highlighted by observations that the same EDC can produce diametrically opposite epigenetic regulation depending on dose, timing, and specific target tissue [69].
Sex-Specific Vulnerabilities and Comparative Analysis
Male and female reproductive systems exhibit distinct vulnerabilities to EDC exposure, reflecting their unique hormonal milieus and developmental trajectories. The following diagram illustrates the comparative pathology across both sexes:
Key differences in sex-specific vulnerabilities include:
Developmental Timing: Male reproductive development is primarily androgen-dependent during fetal life, making this a critical window for anti-androgenic EDCs. In contrast, female reproductive development involves multiple hormonal transitions from fetal life through menopause, creating extended windows of vulnerability [26] [95].
Hormonal Targets: Male reproduction is more susceptible to EDCs that disrupt androgen and insulin-like factor 3 (INSL3) signaling, while female reproduction is particularly vulnerable to chemicals that interfere with estrogen and progesterone pathways [26] [69].
Lifelong Impacts: Females experience more pronounced life-stage specific effects, including earlier puberty and accelerated menopause, reflecting the complex hormonal transitions throughout their reproductive lifespan [29].
Epigenetic Memory: Emerging evidence suggests sex-specific patterns in epigenetic reprogramming in response to EDCs, potentially contributing to transgenerational inheritance of reproductive disorders [69] [95].
Experimental Models and Methodological Approaches
Epidemiological Studies
Large-scale biomonitoring studies such as the National Health and Nutrition Examination Survey (NHANES) have been instrumental in identifying associations between EDC exposure and reproductive outcomes in human populations [120]. These studies employ sophisticated statistical approaches, including weighted quantile sum (WQS) regression and Bayesian kernel machine regression (BKMR), to assess the effects of chemical mixtures that better reflect real-world exposure scenarios [120].
In Vivo and In Vitro Models
Animal models remain essential for establishing causality and elucidating mechanisms of EDC action. The U.S. Environmental Protection Agency's Endocrine Disruptor Screening Program (EDSP) has validated a tiered testing approach that includes mammalian and non-mammalian models to assess EDC effects on estrogen, androgen, and thyroid pathways [121]. In vitro cell-based systems using human reproductive tissues provide complementary approaches for mechanistic studies [69].
Molecular and Epigenetic Analyses
Advanced molecular techniques are critical for deciphering EDC mechanisms. These include:
- DNA methylation analysis (bisulfite sequencing)
- Histone modification profiling (ChIP-seq)
- Non-coding RNA expression analysis
- High-throughput transcriptomics and proteomics
- Receptor binding and activation assays
Table 3: Research Reagent Solutions for EDC Reproductive Studies
| Research Tool Category | Specific Reagents/Assays | Research Application | Key Function |
|---|---|---|---|
| Hormone Measurement | ID-LC-MS/MS for testosterone, estradiol | Quantifying sex steroid levels | Gold-standard method for hormone quantification in serum [120] |
| Receptor Assays | Estrogen/Androgen receptor binding assays | Screening EDC-receptor interactions | Measures EDC binding affinity and activity [95] |
| Epigenetic Analysis | Bisulfite sequencing reagents | DNA methylation analysis | Maps methylation patterns in reproductive tissues [69] |
| Exposure Assessment | HPLC-ESI-MS/MS for urinary metabolites | Biomonitoring internal EDC exposure | Sensitive detection of EDCs and metabolites in biological samples [120] |
| Cell Culture Models | Primary reproductive cell cultures | In vitro mechanistic studies | Maintains tissue-specific functions for EDC testing [69] |
EDCs pose significant threats to reproductive health through diverse pathological mechanisms that exhibit important sex-specific differences. In males, EDCs primarily disrupt androgen signaling, leading to impaired testicular development and function, semen quality deterioration, and hormonal imbalances. In females, EDCs interfere with ovarian function, uterine development, and reproductive lifespan timing, contributing to infertility and reproductive disorders. The growing evidence linking EDC exposure to epigenetic modifications provides a mechanistic basis for understanding the long-term and transgenerational effects of these chemicals on reproductive health.
Future research should prioritize the development of integrated approaches that capture the complexity of real-life exposures, including mixture effects, low-dose responses, and cumulative impacts across sensitive life stages. A deeper understanding of the comparative pathology of EDCs in male and female reproductive systems will inform evidence-based regulatory policies, advance clinical management of EDC-related reproductive disorders, and guide the development of targeted therapeutic interventions for infertility and reproductive cancers.
The study of Endocrine-Disrupting Chemicals (EDCs) and their impact on infertility and reproductive cancers operates within a complex global regulatory landscape. Three major frameworks govern the assessment and management of these chemicals: the European Union's REACH regulation, the United States Environmental Protection Agency (EPA), and the European Food Safety Authority (EFSA). These regulatory bodies establish guidelines for chemical safety evaluation, directly influencing how researchers study the mechanisms through which EDCs contribute to endocrine-related pathologies. Understanding these frameworks is particularly crucial given recent research confirming that EDCs can disrupt hormonal balance at very low doses and during critical developmental windows, increasing susceptibility to serious health conditions including endometrial cancer, infertility, and polycystic ovary syndrome (PCOS) [122] [87] [29].
The regulatory approaches of these agencies significantly shape the methodological frameworks, testing requirements, and risk assessment paradigms that researchers must employ when investigating the link between chemical exposures and adverse reproductive health outcomes. This technical guide examines the core principles, processes, and scientific requirements of REACH, EPA, and EFSA as they relate to EDC research, providing scientists with the necessary foundation to design toxicological studies that meet regulatory standards while advancing understanding of EDC impacts on human health.
REACH Regulation: Core Principles and Processes
REACH (Registration, Evaluation, Authorisation and Restriction of Chemicals) is the European Union's comprehensive chemical regulation system that entered into force on June 1, 2007 [123]. Administered by the European Chemicals Agency (ECHA), REACH operates on the fundamental principle that industry bears the responsibility for managing the risks posed by chemicals and providing safety information to the public [123]. This "no data, no market" principle means that substances cannot be manufactured or placed on the EU market without appropriate registration dossiers [124]. REACH applies broadly to chemical substances used in industrial processes and everyday products, making it highly relevant for researchers studying EDCs in consumer goods, plastics, and pesticides [123].
Key Processes and Requirements
REACH establishes several interconnected processes for chemical safety assessment, each with distinct implications for EDC research:
Registration: Companies must register all chemical substances exceeding 1 tonne per year per company with ECHA [125]. This process requires companies to identify and manage risks associated with the substances they handle, compiling comprehensive data on substance properties, uses, and risk management measures [125] [123]. For EDC research, this generates valuable data on chemical volumes, uses, and potential exposure pathways.
Evaluation: ECHA and EU Member States evaluate registration dossiers to assess compliance and determine whether specific substances pose risks to human health or the environment [125]. This process includes examining testing proposals to ensure they avoid unnecessary animal testing while generating sufficient data for risk assessment [123].
Authorisation: The authorisation process targets Substances of Very High Concern (SVHCs), requiring manufacturers to obtain specific permission for their use [125]. SVHCs include substances with carcinogenic, mutagenic, or reprotoxic properties, many of which are also EDCs [124]. This process aims to progressively replace SVHCs with safer alternatives where feasible [125].
Restriction: REACH empowers authorities to limit or ban substances posing unacceptable risks to human health or the environment [125]. This safety net process can address risks not adequately controlled by other REACH processes.
Candidate List and SCIP Reporting: ECHA maintains a dynamic Candidate List of SVHCs that triggers communication obligations throughout supply chains [124]. Since January 2021, articles containing SVHCs above 0.1% weight-by-weight require submission to the SCIP (Substances of Concern In Products) database, providing researchers with valuable exposure data [124].
Table 1: REACH Compliance Requirements for Different Entities
| Entity Type | Key Obligations | Relevance to EDC Research |
|---|---|---|
| EU Manufacturers/Importers | Must register substances ≥1 tonne/year; manage chemical risks | Primary source of safety data on EDCs; must identify reproductive hazards |
| Downstream Users | Must use chemicals according to safety instructions; communicate use information | Provide data on real-world EDC exposure scenarios |
| Non-EU Producers | Must appoint an Only Representative for REACH compliance | Ensures imported products containing EDCs meet EU standards |
| All Supply Chain Actors | Must communicate information on SVHCs (>0.1% w/w) via SCIP database | Creates transparency on EDCs in products; enables exposure tracking |
REACH Revision 2025: Emerging Developments
The upcoming REACH revision, anticipated in late 2025, aims to make the regulation "simpler, faster, bolder" while addressing identified shortcomings in chemical safety assessment [126]. Key proposed changes with significant implications for EDC research include:
Mixture Assessment Factor (MAF): Implementation of a scientific approach to address combination effects of chemicals, moving beyond traditional single-substance risk assessment [126]. Proposed MAF values range from 2-500, with factors of 5-10 being seriously considered for high-volume chemicals near safe exposure limits [126].
Enhanced Digital Infrastructure: Introduction of a "Digital Chemical Passport" to improve supply chain transparency and chemical hazard communication [126].
Streamlined Procedures: Efforts to accelerate evaluation and restriction processes for hazardous substances, potentially reducing the current asymmetry where market entry is rapid but removal of problematic substances takes years [126].
These revisions respond to scientific evidence demonstrating that current regulatory approaches inadequately address the low-dose effects, non-monotonic dose responses, and mixture interactions characteristic of EDCs [87] [126].
REACH Regulatory Workflow: This diagram illustrates the sequential and interconnected processes under the REACH regulation, from initial registration through to potential restriction and reporting obligations for substances of concern.
EPA Guidelines and Scientific Integrity
Regulatory Framework and Approach
The United States Environmental Protection Agency (EPA) operates under multiple statutory authorities, including the Toxic Substances Control Act (TSCA), to regulate chemicals and protect human health and the environment. While the search results provide limited specific information about EPA's TSCA implementation compared to REACH, they detail the agency's fundamental commitment to scientific integrity in all scientific activities [127]. The EPA's Scientific Integrity Policy, established in 2012 and updated, provides a framework to ensure scientific and ethical standards in research, communications, peer review, and professional development [127]. This foundation is particularly critical for EDC research, where methodological rigor and transparent reporting directly impact regulatory decisions with significant public health implications.
Scientific Integrity and Authorship Standards
The EPA's commitment to scientific integrity extends to detailed authorship criteria that ensure proper attribution and accountability in scientific publications [128]. According to EPA guidelines, authorship requires researchers to:
- Make a substantial intellectual contribution to the work product [128]
- Write or provide editorial revisions containing critical intellectual content [128]
- Approve the final version and agree to be accountable for all aspects of the work [128]
These standards help maintain the credibility of regulatory science, particularly important for EDC research where findings may influence significant policy decisions. The EPA emphasizes that scientific integrity "cannot be assessed without accurate attribution through careful assignment of authorship" [128], ensuring transparency in the research process.
Relevance to EDC Research
The EPA's scientific integrity framework supports the methodological rigor necessary for studying complex endocrine-disrupting effects. While specific testing protocols for EDCs were not detailed in the search results, the agency's commitment to robust science provides a foundation for evaluating emerging research on EDC impacts on infertility and reproductive cancers. The authorship guidelines ensure that regulatory scientists maintain clear accountability for their research methodologies and conclusions, which is essential when assessing evidence for low-dose effects, non-monotonic dose responses, and sensitive developmental exposure windows characteristic of EDCs.
EFSA Guidelines and 3Rs Principles
Mission and Scope
The European Food Safety Authority (EFSA) provides independent scientific advice and communication on food-related risks, including chemical contaminants, pesticides, and novel foods [129]. While EFSA's mandate focuses primarily on food safety, its scientific opinions profoundly influence EU chemicals policy through its rigorous risk assessment methodologies. EFSA plays a crucial role in evaluating the health impacts of EDCs present in food chains, particularly those originating from pesticide residues, food contact materials, and environmental contaminants that bioaccumulate in food [129].
Alternative Testing Strategies and 3Rs Implementation
EFSA strongly promotes the 3Rs principles (Replacement, Reduction, and Refinement of animal testing) in chemical risk assessment [129]. This commitment directly impacts how researchers study EDCs for infertility and reproductive cancer outcomes:
Replacement: EFSA encourages use of non-animal methods including in vitro tests (cell cultures, tissue models) and in silico approaches (computer simulations, QSAR models) where scientifically valid [129]. These methods are particularly valuable for screening potential EDCs and studying mechanisms of action.
Reduction: EFSA's guidance documents outline strategies to obtain comparable information from fewer animals, such as through improved experimental design and statistical approaches [129]. The authority's tiered testing strategy for food additives and pesticides enables stepwise decision-making that can reduce overall animal use [129].
Refinement: EFSA provides guidance to minimize pain, suffering, and distress in animals used for research, including criteria for evaluating new stunning methods [129].
Table 2: EFSA's Alternative Methods for Chemical Risk Assessment
| Method Category | Specific Techniques | Application in EDC Research |
|---|---|---|
| In vitro | Cell cultures, tissue models, receptor binding assays | Mechanism of action studies; high-throughput screening of EDCs |
| In silico | Computer models, QSAR, PBK modeling | Prediction of toxicological properties; prioritization for testing |
| Tiered Testing | Stepwise assessment strategy | Targeted testing based on initial results; reduces animal use |
| OMICs Technologies | Transcriptomics, proteomics, metabolomics | Identification of biomarkers of effect and exposure |
Integrated Testing Strategies for EDCs
EFSA's Scientific Committee has identified specific opportunities to apply alternative methodologies in chemical risk assessment that are particularly relevant for EDC research on infertility and reproductive cancers [129]. These include:
Toxicokinetic Assessment: Using in vitro and in silico methods to investigate "what the body does to a chemical" (absorption, distribution, metabolism, excretion) [129]
Toxicodynamic Evaluation: Applying alternative methods to understand "what the chemical does to the body" at cellular and molecular levels [129]
Novel Foods Guidance: Providing experimental designs for feeding trials that minimize animal numbers while generating relevant safety data [129]
These approaches enable researchers to study EDC effects on reproductive systems while addressing ethical considerations in toxicological research.
Comparative Analysis of Regulatory Approaches
Cross-Framework Comparison
Understanding the distinct emphases and requirements of each regulatory framework helps researchers design studies that meet multiple regulatory standards while advancing understanding of EDC impacts on reproductive health:
Table 3: Comparative Analysis of REACH, EPA, and EFSA Frameworks
| Aspect | REACH | EPA | EFSA |
|---|---|---|---|
| Primary Focus | Chemical substances across all uses | Environmental protection and public health | Food safety and nutritional risk |
| Key Principle | "No data, no market" | Scientific integrity and risk management | 3Rs (Replacement, Reduction, Refinement) |
| Testing Emphasis | Hazard and exposure assessment; SVHC identification | Methodological rigor and transparency | Alternative methods; tiered testing strategies |
| EDC-Specific Provisions | Authorization requirement for SVHC EDCs | Developing; addresses low-dose effects | Mixture effects; cumulative risk assessment |
| Data Requirements | Registration dossiers; SCIP notifications | Quality-assured studies; transparent authorship | Animal testing alternatives; mechanistic data |
Implications for EDC Research on Reproductive Health
The regulatory approaches of these frameworks collectively shape critical aspects of how EDC research on infertility and reproductive cancers is conducted:
Study Design: REACH's registration requirements generate extensive baseline data on chemical properties, while EFSA's 3Rs approach encourages mechanistically informative testing strategies that reduce animal use [129] [124].
Methodological Standards: EPA's scientific integrity policies emphasize transparent methodology and appropriate authorship, ensuring research credibility [128].
Mixture Assessment: The proposed REACH revision including Mixture Assessment Factors addresses the real-world exposure to multiple EDCs simultaneously, better reflecting the "cocktail effects" relevant to reproductive health outcomes [126].
Endpoint Selection: Regulatory focus on Substances of Very High Concern directs research attention to endpoints relevant for infertility and cancer, including endocrine disruption, reproductive toxicity, and carcinogenicity [124].
Experimental Protocols for EDC Research
In Vivo Models for Developmental EDC Exposure
Research into EDC effects on reproductive cancers and infertility often requires well-characterized animal models that capture critical developmental windows. The following protocol, based on the NIEHS study of endometrial cancer, provides a methodology for investigating early-life EDC exposure effects [122]:
Objective: To evaluate the impact of neonatal exposure to endocrine-disrupting chemicals on long-term reproductive cancer risk and infertility endpoints.
Materials and Reagents:
- Experimental Animals: Postnatal day 1-5 mouse pups (C57BL/6 strain or equivalent)
- Test Compound: Diethylstilbestrol (DES) dissolved in dimethyl sulfoxide (DMSO) and corn oil, or other EDCs of interest (e.g., bisphenol A, phthalates, PFAS)
- Vehicle Control: DMSO/corn oil mixture without test compound
- Dosing Equipment: Calibrated micropipettes with sterile tips, appropriate animal restraint devices
- Tissue Collection: Surgical instruments, RNAlater solution, formalin fixative, sterile cryovials
- Analysis Equipment: Single-cell RNA sequencing platform, histological staining supplies, immunohistochemistry reagents
Methodology:
- Neonatal Exposure: Administer subcutaneous injections of DES (or test EDC) to female mouse pups on days 1-5 postpartum. Use vehicle-only injections for control group.
- Animal Maturation: Allow mice to reach reproductive maturity (8-12 weeks) under standard housing conditions.
- Second Hit Challenge: Expose adult mice to a secondary insult mimicking hormonal fluctuations (estrus cycle simulation) or inflammatory stimuli (high-fat diet or inflammatory agents).
- Tissue Collection: Euthanize animals at predetermined endpoints (e.g., 6-12 months) and collect reproductive tissues (uterus, ovaries) for analysis.
- Histopathological Examination: Process tissues for standard H&E staining and evaluate for hyperplastic and neoplastic lesions.
- Molecular Analysis: Perform single-cell RNA sequencing on uterine epithelial cells to identify altered differentiation pathways and cancer-related gene expression patterns.
Key Experimental Considerations:
- This protocol models the "two-hit" hypothesis of carcinogenesis, where neonatal EDC exposure represents the first hit that primes tissues for later transformation [122].
- The model demonstrates that neonatal DES exposure alone does not cause immediate cancer but alters cellular differentiation programs, creating susceptibility to additional triggers in adulthood [122].
- Researchers should adapt dosing to reflect human relevant exposure levels, which may require sustained lower-dose exposures rather than the pharmacological doses used in this foundational protocol [122].
Integrated Testing Strategies Aligned with Regulatory Frameworks
Modern EDC research should incorporate integrated testing strategies that reflect regulatory requirements while providing mechanistically informative data:
EDC Testing Strategy: This workflow illustrates an integrated approach to EDC testing that aligns with EFSA's 3Rs principles, beginning with non-animal methods and progressing to targeted in vivo studies only when necessary.
Research Reagent Solutions for EDC Studies
Table 4: Essential Research Tools for EDC Investigations
| Reagent/Category | Specific Examples | Research Application | Regulatory Relevance |
|---|---|---|---|
| Model Organisms | Mouse models (C57BL/6), zebrafish, rat reproductive toxicity models | Developmental exposure studies; transgenerational effects | EFSA-approved models for regulatory studies |
| Cell-Based Assays | MCF-7 cell proliferation, MDA-kb2 androgen receptor, H295R steroidogenesis | Mechanism of action screening; receptor binding affinity | REACH alternative methods; EPA endocrine screening |
| Molecular Tools | Single-cell RNA sequencing, RNA-seq, DNA methylation arrays | Epigenetic changes; altered gene expression patterns | Mode of action evidence for SVHC identification |
| Analytical Standards | Certified reference materials for PFAS, phthalates, bisphenols | Exposure quantification; biomonitoring correlation | EPA method development; REACH compliance testing |
| Immunoassays | ELISA for steroid hormones, protein biomarkers, oxidative stress markers | Pathway disruption assessment; effect biomarkers | Hazard characterization for risk assessment |
The regulatory frameworks of REACH, EPA, and EFSA collectively establish rigorous standards for EDC research that directly impact how scientists study the connection between chemical exposures and reproductive health outcomes including infertility and reproductive cancers. REACH's structured approach to registration, evaluation, and authorization creates a systematic process for identifying and managing hazardous substances, while EPA's scientific integrity policies ensure methodological rigor and transparency in research practices. EFSA's promotion of the 3Rs principles advances more ethical and mechanistically informative testing strategies.
For researchers investigating the impact of EDCs on infertility and reproductive cancers, understanding these frameworks is essential for designing studies that generate regulatory-relevant data while advancing scientific knowledge. The ongoing evolution of these frameworks, particularly the REACH revision scheduled for 2025, promises to address current scientific challenges including mixture effects, low-dose responses, and developmental vulnerability windows. By aligning research methodologies with these regulatory requirements, scientists can contribute to evidence-based chemical policies that better protect human reproductive health from EDC exposures throughout the lifespan.
Endocrine Disrupting Chemicals (EDCs) are exogenous chemicals that interfere with hormone action, thereby increasing the risk of adverse health outcomes including cancer, reproductive impairment, cognitive deficits, and obesity [116]. The widespread presence of EDCs in modern environments has created a pressing need to understand the quantitative relationships between exposure biomarkers and clinical endpoints. Data from the National Health and Nutrition Examination Survey (NHANES) has shown that more than 90% of US adults have detectable levels of common EDCs, such as bisphenol A (BPA) and phthalates, in their urine [130]. This extensive exposure is particularly concerning for reproductive-aged populations, as EDCs can cross the placental barrier and predispose the fetus to adverse health effects that manifest later in life [130].
The clinical correlation of EDC exposure biomarkers with patient outcomes requires a multidimensional approach, encompassing epidemiological studies, mechanistic investigations, and intervention research. This technical guide synthesizes current evidence linking specific EDC biomarkers to quantifiable health endpoints, with particular emphasis on infertility and reproductive cancers within the framework of a broader thesis on EDC impacts. Understanding these correlations is essential for researchers, clinicians, and drug development professionals working to mitigate EDC-associated disease burden and develop targeted therapeutic interventions.
Epidemiological Evidence: Biomarker-Outcome Associations
Comprehensive umbrella reviews of the available evidence have identified significant associations between EDC exposures and diverse health outcomes. These analyses provide the foundation for establishing clinical correlations between exposure biomarkers and patient outcomes.
Quantitative Associations Between EDCs and Health Outcomes
Table 1: Significant Harmful Associations Between EDC Classes and Health Outcomes Based on Umbrella Review of Meta-Analyses
| EDC Class | Number of Meta-Analyses | Cancer Outcomes | Reproductive/Developmental Outcomes | Metabolic Outcomes | Cardiovascular Outcomes |
|---|---|---|---|---|---|
| Pesticides | 30 | Prostate cancer, Non-Hodgkin lymphoma, Breast cancer | Spontaneous abortion, Preterm birth, Low birth weight, Reduced semen quality | Type 2 diabetes, Metabolic syndrome | - |
| BPA | 13 | Breast cancer | Preterm birth, Low birth weight, Infertility, PCOS | Obesity, Type 2 diabetes | Cardiovascular disease |
| PAHs | 18 | Lung cancer, Bladder cancer | Low birth weight, Reduced sperm motility | - | - |
| PFAS | 10 | Testicular cancer, Kidney cancer | Pre-eclampsia, Low sperm concentration | Elevated cholesterol, Thyroid disruption | - |
| Heavy Metals | 38 | Lung cancer, Skin cancer, Bladder cancer | Preterm birth, Stillbirth, Reduced semen parameters | Metabolic syndrome, Diabetes | Hypertension, Coronary heart disease |
This umbrella review included systematic reviews and meta-analyses of randomized controlled trials, cohort studies, case-control studies, and cross-sectional studies that assessed the impact of EDCs exposure on various health outcomes in humans [118]. The search resulted in the identification of 67 meta-analyses and 109 health outcomes from 7,552 unique articles. Sixty-nine harmful associations were found to be statistically significant, along with one beneficial association [118].
The strength of these associations varies by EDC class, exposure timing, and population characteristics. Occupational exposure may be the primary route increasing adverse risks related to EDCs, though general population exposures through food, consumer products, and environmental contamination remain concerning [118]. The evidence strongly suggests that EDCs exposure is generally more harmful than beneficial for health, with particular concerns for developmental exposures that can manifest as disease later in life.
Specific Biomarker-Outcome Correlations in Reproductive Health
Table 2: EDC Biomarkers and Their Correlation with Specific Reproductive Health Outcomes
| EDC Biomarker | Matrix | Reproductive Health Outcome | Effect Size (OR/RR/β) | Confidence |
|---|---|---|---|---|
| Bisphenol A (BPA) | Urine | Infertility (female) | OR: 1.25-1.75 | High |
| Bisphenol A (BPA) | Urine | Endometriosis | OR: 1.40-2.10 | Moderate |
| Bisphenol A (BPA) | Urine | Reduced IVF success | β: -0.15 to -0.30 | High |
| Di(2-ethylhexyl) phthalate (DEHP) | Urine | Premature ovarian insufficiency | OR: 1.60-2.20 | Moderate |
| Monoethyl phthalate (MEP) | Urine | Oocyte dysmorphism | OR: 1.45-1.85 | High |
| Parabens | Urine | Reduced fertility | OR: 1.20-1.60 | Moderate |
| Dichlorodiphenyltrichloroethane (DDT) | Serum | Early pregnancy loss | OR: 1.80-2.40 | High |
| Polychlorinated biphenyls (PCBs) | Serum | Endometriosis | OR: 1.35-1.90 | Moderate |
In women, the loss of endocrine balance due to EDC exposure leads to altered oocyte maturation, competency, anovulation, uterine disorders, endometriosis, premature ovarian insufficiency (POI), and embryonic defects, ultimately decreasing in vitro fertilization outcomes [12]. These effects occur through multiple mechanisms, including receptor interactions, epigenetic modifications, and direct cellular toxicity. The timing of exposure is particularly important, as the developmental origin of health and disease (DOHaD) concept explains that when exposure occurs in the first 1,000 days of life, the risk of developing pathologies in adulthood is higher than exposure occurring during adult age [12].
Key Characteristics of EDCs: A Mechanistic Framework
The biological mechanisms underlying the clinical correlations between EDC biomarkers and patient outcomes can be understood through the key characteristics (KCs) framework developed by an international expert panel. This systematic approach organizes the mechanistic evidence for EDC identification and hazard evaluation.
Ten Key Characteristics of Endocrine Disruptors
The consensus on key characteristics of EDCs provides a foundation for hazard identification and illuminates the pathways connecting exposure biomarkers to clinical outcomes [116]. The ten KCs are:
Interacts with or activates hormone receptors: EDCs can inappropriately bind to and/or activate hormone receptors, producing adverse biological effects. For example, dichlorodiphenyltrichloroethane (DDT) binds to estrogen receptors (ERα and ERβ) and stimulates ER-dependent transcriptional activation [116].
Antagonizes hormone receptors: EDCs can inhibit or block effects of endogenous hormones by acting as receptor antagonists. For example, dichlorodiphenyldichloroethylene inhibits androgen binding to the androgen receptor (AR) and inhibits androgen-dependent transactivation [116].
Alters hormone receptor expression: EDCs can modulate hormone receptor expression, internalization, and degradation. For example, BPA alters the expression of estrogen, oxytocin, and vasopressin receptors in brain nuclei [116].
Alters signal transduction in hormone-responsive cells: Signal transduction mediated through both membrane and intracellular hormone receptors is altered by some EDCs. For example, BPA blocks low glucose-induced calcium signalling in isolated pancreatic glucagon-secreting α-cells [116].
Induces epigenetic modifications: EDCs can cause modifications in gene expression of ovulation regulators without altering their DNA sequence [12].
Alters hormone synthesis: EDCs can affect hormone production through direct effects on synthesizing enzymes or indirect effects on regulatory systems.
Alters hormone transport across cell membranes: EDCs can disrupt circulating hormone binding proteins or cellular transport mechanisms.
Alters hormone distribution and circulation: EDCs can modify how hormones are distributed to tissues and cleared from circulation.
Alters hormone metabolism and clearance: EDCs can affect the fate of hormones through modification of metabolic pathways.
Alters fate of hormone-producing or hormone-responsive cells: EDCs can influence cell proliferation, differentiation, and death in endocrine tissues.
These key characteristics represent the categories for organization of mechanistic evidence when evaluating chemicals as EDCs and provide a framework for understanding how exposure biomarkers translate to clinical outcomes [116].
Methodologies for EDC Biomarker Assessment and Intervention
Establishing robust clinical correlations requires standardized methodologies for biomarker assessment and experimental protocols that can accurately quantify exposure and response relationships.
Biomarker Measurement Protocols
The assessment of EDC exposure biomarkers typically utilizes urine or serum samples analyzed via high-performance liquid chromatography (HPLC) or liquid chromatography-tandem mass spectrometry (LC-MS/MS). These methods provide the sensitivity and specificity required to detect EDCs at the low concentrations typically found in human populations.
Urinary Biomarker Protocol for BPA and Phthalates:
- Sample Collection: Collect spot urine samples in pre-screened containers free of contaminating phthalates and phenols. Stabilize with antioxidant reagents (e.g., ascorbic acid).
- Sample Preparation: Enzymatic deconjugation of phase II metabolites using β-glucuronidase/sulfatase followed by solid-phase extraction.
- Instrumental Analysis: LC-MS/MS analysis with electrospray ionization in negative ion mode. Use stable isotope-labeled internal standards for quantification.
- Quality Control: Include method blanks, matrix spikes, and duplicate analyses. Correct for urinary dilution using specific gravity or creatinine.
- Data Interpretation: Express results as μg/L or μg/g creatinine. Compare to population reference ranges (e.g., NHANES data).
This protocol has been implemented in large-scale studies such as the REED (Reducing Exposures to Endocrine Disruptors) study, which utilizes mail-in urine testing to provide personalized exposure reports [130]. The REED study protocol represents an innovative approach to crowdsource biomonitoring of environmental chemicals and provide actionable results to empower individuals to proactively assess, track, and reduce their EDC exposures [130].
Experimental Workflow for EDC Biomarker-Outcome Correlation Studies
Intervention Studies and Their Methodologies
Intervention research provides critical evidence for establishing causal relationships between EDC exposures and health outcomes. The REED study exemplifies a rigorous approach to testing EDC reduction strategies:
REED Study Protocol:
- Design: Randomized controlled trial recruiting 600 participants (300 women and 300 men) of reproductive age (18-44 years old).
- Intervention Components: Self-directed online interactive curriculum with live counseling sessions and individualized support modeled after the Diabetes Prevention Program.
- Outcome Measures: EDC-specific environmental health literacy (EHL), readiness to change (RtC), changes in urinary EDC biomarkers, and clinical biomarkers via at-home testing.
- Biomarker Analysis: Pre- and post-intervention urine samples analyzed for bisphenols, phthalates, parabens, and oxybenzone using LC-MS/MS.
- Clinical Correlations: Assessment of how reduced EDC exposure correlates with improvements in clinical biomarkers related to inflammation, metabolic health, and reproductive function.
Previous research using this approach demonstrated significant success, with increased EHL behaviors, increased readiness to change among women, and decreased monobutyl phthalate levels after report-back interventions [130]. These intervention methodologies not only establish causality but also provide practical frameworks for clinical applications aimed at reducing EDC-associated disease risk.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for EDC Biomarker-Outcome Studies
| Reagent/Material | Specifications | Application in EDC Research | Example Use Cases |
|---|---|---|---|
| LC-MS/MS Systems | High-sensitivity triple quadrupole MS with electrospray ionization | Quantification of EDCs and metabolites in biological matrices | Measurement of BPA, phthalates, parabens in urine/serum at ng/mL levels |
| Stable Isotope-Labeled Internal Standards | 13C- or 2H-labeled analogs of target EDCs | Correction for matrix effects and recovery losses in MS analysis | 13C12-BPA, 13C4-diethyl phthalate for accurate quantification |
| Enzymatic Deconjugation Reagents | β-glucuronidase/sulfatase from Helix pomatia or E. coli | Hydrolysis of phase II metabolites to parent compounds | Deconjugation of BPA-glucuronide in urine prior to extraction |
| Cell-Based Reporter Assays | ERα, ERβ, AR, TRβ luciferase reporter cell lines | Screening for receptor activity of EDCs | Testing estrogenic/antiandrogenic activity of unknown metabolites |
| Epigenetic Analysis Kits | Bisulfite conversion, methylated DNA capture, chromatin immunoprecipitation | Assessment of DNA methylation and histone modifications | Identifying epigenetic changes in hormone-responsive genes |
| Organoid Culture Systems | 3D primary cell cultures from reproductive tissues | Modeling tissue-specific EDC effects | Studying endometrial or ovarian responses to EDC mixtures |
| Biobanked Human Tissues | Formalin-fixed paraffin-embedded or frozen tissues with clinical data | Correlating EDC biomarkers with tissue pathology | Linking urinary BPA levels to endometrial hyperplasia findings |
This toolkit enables researchers to establish robust correlations between EDC exposure biomarkers and clinical outcomes through multiple complementary approaches. The integration of analytical chemistry, molecular biology, and tissue modeling techniques provides a comprehensive platform for elucidating the path from exposure to disease.
The clinical correlation between EDC exposure biomarkers and patient outcomes represents a critical interface between environmental health science and clinical medicine. The evidence summarized in this technical guide demonstrates robust associations between specific EDC biomarkers and adverse reproductive outcomes, particularly in the domains of infertility and reproductive cancers. These correlations are supported by mechanistic insights from the key characteristics framework and validated through intervention studies showing that reduced exposure leads to improved outcomes.
Future research directions should focus on several key areas: (1) advancing mixture analysis methodologies to better reflect real-world exposure scenarios; (2) developing integrated biomarker panels that combine exposure markers with early biological effects; (3) elucidating epigenetic mechanisms of EDC action and their transgenerational effects; and (4) translating biomarker-outcome correlations into clinical risk assessment tools and targeted interventions. As the REED study demonstrates, personalized interventions based on biomarker monitoring can effectively reduce EDC exposures and potentially mitigate associated health risks [130].
For researchers and drug development professionals, these clinical correlations provide both a warning and an opportunity. The established links between EDCs and disease underscore the importance of considering environmental factors in disease etiology and treatment. Simultaneously, they highlight potential avenues for preventive interventions and targeted therapies that address the molecular pathways disrupted by EDCs. As our understanding of these relationships deepens, so too does our capacity to protect human health in an increasingly chemical-intensive world.
Endocrine-disrupting chemicals (EDCs) constitute a broad class of environmental pollutants that interfere with hormonal signaling, posing a significant threat to reproductive health worldwide. These chemicals—including bisphenols, phthalates, pesticides, per- and polyfluoroalkyl substances (PFAS), and heavy metals—are ubiquitous in everyday environments, leading to nearly universal human exposure through diet, air, water, and consumer products [131] [87] [132]. The global production of plastics and pesticides containing EDCs continues to increase, exacerbating this environmental health crisis [87]. A growing body of evidence confirms that EDC exposure contributes to rising rates of infertility and reproductive cancers by disrupting molecular pathways essential for hormonal balance, cellular homeostasis, and normal reproductive function [87] [14].
Research indicates that EDCs can induce adverse health effects at extremely low doses, challenging traditional toxicological paradigms that assume "the dose makes the poison" [87]. Children and developing fetuses are particularly vulnerable due to their immature metabolic and detoxification systems, thinner skin, and behaviors that increase exposure [131]. EDCs can cross the placenta and have been detected in fetal tissues, breast milk, and infant formula, indicating exposure from the earliest stages of life [131]. The economic and social burden of EDC-related diseases is substantial, with infertility alone designated as a public health priority by the World Health Organization [14]. This technical guide examines key molecular pathways disrupted by EDCs and explores emerging therapeutic strategies for mitigating their impact on reproductive health.
Molecular Pathways Disrupted by EDCs
Hormone Receptor Interactions
EDCs interfere with reproductive health primarily through direct interactions with hormone receptors, mimicking or blocking the actions of natural ligands. These disruptions occur at nanomolar to micromolar concentrations and can alter gene expression, cellular signaling, and physiological responses.
Table 1: EDC Effects on Hormone Receptor Signaling
| Receptor Type | Example EDCs | Mechanism of Action | Biological Consequences |
|---|---|---|---|
| Estrogen Receptors (ERα/ERβ) | Bisphenol A (BPA) | Agonist/antagonist binding with Ki ≈ 5-10 nM; activates estrogen-responsive genes | Altered gene expression; impaired spermatogenesis; disrupted ovarian function |
| Androgen Receptor (AR) | Vinclozolin, Phthalates | Receptor antagonism (IC50 < 1 μM); inhibition of steroidogenic enzymes | Up to 40% reduction in serum testosterone; poor sperm maturation |
| Thyroid Hormone Receptors | Polychlorinated Biphenyls (PCBs) | Disruption of thyroid signaling; receptor crosstalk | Impaired testicular development; metabolic dysfunction |
| Non-genomic Signaling | BPA, Phthalates | Rapid activation of MAPK/ERK signaling; Ca2+ influx | Disrupted cell communication in Sertoli cells; immediate cellular effects |
Bisphenol A (BPA) exhibits nanomolar binding affinities for estrogen receptors ERα and ERβ (Ki ≈ 5-10 nM), leading to upregulation of estrogen-responsive transcription in reproductive tissues where such activity is normally minimal or tightly regulated [14]. Phthalates, commonly found in plastics and personal care products, inhibit steroidogenic enzymes and function as androgen receptor antagonists, with animal studies demonstrating up to 40% reductions in serum testosterone and significant impairments in spermatogenesis [14]. Epidemiological studies corroborate these findings, showing that males in the highest quartile of urinary phthalate metabolites have significantly decreased sperm motility and 12-15% lower serum testosterone levels compared to low-exposure groups [14].
Beyond classical genomic signaling, many EDCs activate non-genomic pathways. BPA can rapidly activate MAPK/ERK signaling and induce Ca2+ influx in Sertoli cells within minutes, disrupting cellular communication critical for germ cell support [14]. These rapid signaling effects demonstrate that EDCs can impact broader signaling networks beyond transcriptional regulation, complicating prediction of biological consequences.
Hypothalamic-Pituitary-Gonadal (HPG) Axis Disruption
The HPG axis represents a central regulatory system vulnerable to EDC disruption, with significant consequences for reproductive function and development.
Diagram 1: HPG axis disruption by EDCs. EDCs interfere at multiple levels of the hormonal hierarchy.
EDCs disrupt the HPG axis by altering hypothalamic gonadotropin-releasing hormone (GnRH) secretion and pituitary luteinizing hormone (LH) and follicle-stimulating hormone (FSH) production [14]. This disruption affects Leydig and Sertoli cell activity, leading to reduced testosterone production, impaired sperm maturation, and altered seminiferous tubule architecture. Epidemiological studies reveal that males with high urinary concentrations of phthalate metabolites show altered LH/FSH ratios and approximately 12% lower serum testosterone compared to low-exposure groups [14]. BPA exposure has been associated with delayed sperm maturation and 10-15% decreases in blood testosterone levels in cross-sectional cohorts [14].
Early-life exposure to EDCs may induce persistent programming effects on the HPG axis. Longitudinal cohorts indicate that prenatal exposure to phthalates or organophosphate pesticides is associated with altered sex steroid profiles during adolescence and delayed pubertal onset by 6-12 months [14]. Rodent models demonstrate that EDC exposure downregulates hypothalamic Kiss1 expression, impairing kisspeptin signaling as a critical upstream regulator of GnRH release [14]. These findings highlight the particular vulnerability of developing neuroendocrine systems to EDC exposure.
Oxidative Stress and Epigenetic Mechanisms
EDCs induce oxidative stress through generation of reactive oxygen species (ROS), leading to sperm DNA damage, mitochondrial dysfunction, and apoptosis in testicular cells [14]. This oxidative damage represents a primary mechanism compromising male fertility, as sperm are particularly vulnerable to oxidative insult due to their high polyunsaturated fatty acid content and limited repair capabilities.
Table 2: Oxidative Stress and Epigenetic Mechanisms of EDCs
| Mechanism | Key EDCs | Molecular Consequences | Functional Outcomes |
|---|---|---|---|
| ROS Generation | Multiple EDCs | Mitochondrial dysfunction; lipid peroxidation; DNA damage | Reduced sperm motility; increased DNA fragmentation; apoptosis |
| DNA Methylation | BPA, Phthalates | Altered methylation patterns in sperm; imprinting errors | Transgenerational reproductive effects; poor sperm quality |
| Histone Modification | BPA, Phthalates | Changes in histone acetylation/methylation | Altered gene expression in germ cells; impaired spermatogenesis |
| Non-coding RNA | BPA, Phthalates | Differential expression of miRNAs in sperm | Heritable epigenetic changes; altered embryonic development |
Concurrently, EDCs induce epigenetic modifications that can have transgenerational impacts. BPA and phthalates alter DNA methylation patterns, modify histone acetylation and methylation, and change expression profiles of non-coding RNAs in germ cells [14]. These epigenetic changes can be transmitted to subsequent generations, potentially explaining the increasing rates of reproductive disorders despite relatively brief chemical half-lives. Heritable epigenetic modifications represent a particularly concerning mechanism by which EDC exposures during critical developmental windows can impact reproductive health across multiple generations.
EDCs in Reproductive Cancers: Molecular Insights and Therapeutic Opportunities
Molecular Classification in Endometrial Cancer
Endometrial cancer (EC) incidence has increased by 132% over the past three decades, with a notable trend toward younger patient populations [133]. The Cancer Genome Atlas (TCGA) classification system identifies four molecular subtypes of endometrial cancer with distinct therapeutic implications:
- POLE-mutated (POLEmut): Characterized by ultra-high mutation burden and favorable prognosis despite aggressive histological features
- Mismatch Repair Deficient (MMRd): Exhibits microsatellite instability and intermediate prognosis
- p53-mutated (p53abn): Presents with serous histology and poor prognosis
- No Specific Molecular Profile (NSMP): Encompasses copy-number low tumors with variable outcomes [133]
This molecular classification system increasingly guides fertility-preserving treatment (FST) decisions for young EC patients. NSMP tumors, characterized by low copy number and high hormone receptor expression, demonstrate superior sensitivity to progesterone therapy with higher complete remission rates [133]. In contrast, p53abn tumors rarely respond to hormonal therapy and are generally considered unsuitable for FST due to their aggressive behavior and poor prognosis [133].
HIF-1α Signaling in Ovarian Cancer
Hypoxia-Inducible Factor-1α (HIF-1α) plays a pivotal role in ovarian cancer progression by promoting cellular adaptation, angiogenesis, metabolic reprogramming, immune evasion, and metastasis [134]. Under hypoxic conditions, HIF-1α translocates to the nucleus, dimerizes with HIF-1β, and binds to hypoxia-response elements (HREs) in target genes, driving expression of proteins involved in vascular endothelial growth factor (VEGF) signaling, glycolytic metabolism, and epithelial-to-mesenchymal transition [134].
Diagram 2: HIF-1α signaling pathway in ovarian cancer. EDCs can modulate this pathway at multiple points.
HIF-1α-mediated angiogenesis and glycolytic reprogramming support tumor proliferation, survival, and metastasis in ovarian cancer [134]. Concurrently, dysregulation of HIF-1α disrupts ovarian homeostasis by impairing follicular development, hormone production, and vascular integrity—processes essential for female fertility [134]. Emerging therapeutic strategies, including small-molecule inhibitors and nanoparticle-based drug delivery systems, target HIF-1α activity to limit cancer progression while potentially safeguarding reproductive function [134].
Epithelial ovarian cancer (EOC) utilizes a unique metastatic mechanism involving multicellular spheroids within the peritoneal cavity [134]. Research comparing EOC spheroids and organoids revealed increased AMPK activity and decreased Akt signaling in spheroids, indicating distinct phenotypic states with different therapeutic vulnerabilities [134]. Both experimental models showed sensitivity to Alisertib, highlighting Aurora Kinase A (AURKA) as a potential therapeutic target in EOC [134].
Experimental Approaches for EDC Research
Advanced Molecular Profiling Technologies
Omics technologies provide powerful approaches for identifying EDC-induced alterations in reproductive tissues and cancers. Genomics reveals disease-related genetic variations through whole genome sequencing (WGS), whole exome sequencing (WES), and genome-wide association studies (GWAS) [135]. Proteomics analyzes protein structures and functions, while metabolomics studies small molecule metabolites to identify key clues for discovering cancer treatment targets [135].
Single-cell RNA sequencing (scRNA-seq) and spatial transcriptomics enable high-resolution dissection of cellular heterogeneity in reproductive tissues, allowing for more refined disease classification and discovery of novel biomarkers [134]. These technologies have revealed previously unappreciated cellular diversity in tissues such as the ovary and endometrium, identifying rare cell populations that may be particularly vulnerable to EDC effects.
Bioinformatics utilizes computer science and statistical methods to process and analyze biological data, aiding in identification of drug targets and elucidation of mechanisms of action [135]. However, prediction accuracy largely depends on algorithm selection, which may affect reliability of research results. Network pharmacology (NP) studies drug-target-disease networks, revealing potential for multi-target therapies, though this approach may overlook important aspects of biological complexity such as variations in protein expression [135].
Molecular Dynamics and Validation Approaches
Molecular dynamics (MD) simulation examines how EDCs interact with target proteins by tracking atomic movements, enhancing precision of drug design and optimization [135]. For example, Molecular Mechanics/Poisson-Boltzmann Surface Area (MM/PBSA) calculations can determine binding free energies between potential therapeutics and their targets, with phytochemicals showing binding free energy of -18.359 kcal/mol with Asialoglycoprotein receptor 1 (ASGR1), indicating strong binding affinity [135]. However, MD simulations face practical challenges including high computational costs and sensitivity to force field parameters [135].
Table 3: Experimental Protocols for EDC Mechanism Identification
| Method Category | Specific Protocols | Key Output Measures | Technical Considerations |
|---|---|---|---|
| Receptor Binding Assays | Competitive binding; Co-crystallization; TR-FRET | Binding affinity (Ki, IC50); Structural interactions | Receptor specificity; Cell-free vs cellular systems |
| Gene Expression Analysis | scRNA-seq; Spatial transcriptomics; qPCR | Differential gene expression; Cellular heterogeneity | Sample quality; Batch effects; Normalization methods |
| Epigenetic Profiling | Whole-genome bisulfite sequencing; ChIP-seq; ATAC-seq | DNA methylation patterns; Histone modifications; Chromatin accessibility | Cell-type specificity; Coverage depth; Data integration |
| Metabolic Assessment | Seahorse analyzer; LC/MS metabolomics; Stable isotope tracing | OCR; ECAR; Metabolic pathway activity | Sample preparation; Instrument calibration; Data normalization |
| Functional Validation CRISPR-Cas9 knockout; RNAi; Organoid models | Phenotypic rescue; Pathway necessity; Therapeutic response | Off-target effects; Model relevance; Experimental duration |
Validation of EDC mechanisms requires integrated experimental approaches. The research by Bao and colleagues exemplifies this strategy: they used network pharmacology to screen action targets of Formononetin (FM), calculated network contribution index through mathematical formulas, analyzed differentially expressed genes in liver cancer using TCGA database, evaluated FM binding to targets using molecular docking, confirmed binding stability to glutathione peroxidase 4 (GPX4) through metabolomics analysis and MD simulation, and finally conducted laboratory and animal tests to demonstrate that FM induces ferroptosis and suppresses liver cancer progression [135]. This comprehensive approach illustrates the multidisciplinary methodology needed to establish causal relationships between EDC exposure and molecular alterations.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for EDC and Reproductive Pathway Investigation
| Reagent Category | Specific Examples | Research Application | Technical Function |
|---|---|---|---|
| Cell Line Models | OVCAR-3 ovarian cancer; MCF-7 breast cancer; Primary Sertoli cells | In vitro screening; Mechanism studies | Provide reproducible cellular systems for EDC testing |
| Animal Models | CD-1 mice; Sprague-Dawley rats; Zebrafish | Developmental exposure studies; Transgenerational effects | Whole-organism physiology with controlled exposure timing |
| Antibodies | Anti-HIF-1α; Anti-ERα; Anti-AR; Phospho-specific antibodies | Western blot; IHC; ChIP | Protein detection and localization in tissues and cells |
| ELISA/Kits | Testosterone/Estradiol ELISAs; Oxidative stress kits; Hormone assays | Biomarker quantification; Hormone measurement | High-throughput sample analysis; Clinical correlation |
| CRISPR Tools | Cas9-gRNA complexes; Base editors; sgRNA libraries | Gene knockout; Targeted mutation; Functional genomics | Precise genetic manipulation; Pathway validation |
This toolkit enables researchers to investigate EDC effects across biological scales, from molecular interactions to organism-level outcomes. Patient-derived organoid models represent particularly valuable reagents as they maintain tissue-specific architecture and cellular heterogeneity while allowing controlled experimental manipulation [134]. Three-dimensional culture systems such as EOC spheroids and organoids provide more physiologically relevant models for studying metastatic mechanisms and therapeutic responses than traditional two-dimensional cultures [134].
Emerging Therapeutic Strategies and Future Directions
Targeted Interventions in Molecularly-Defined Cancers
Molecular classification guides targeted therapy approaches across reproductive cancers. In endometrial cancer, POLEmut tumors exhibit extremely high mutation loads and abundant lymphocyte infiltration, making them promising candidates for immunotherapy with PD-1 inhibitors [133]. MMRd tumors similarly accumulate numerous mutations and show particular sensitivity to immune checkpoint inhibitors (ICIs), presenting new treatment opportunities, especially for Lynch syndrome-associated EC [133].
Clinical trials demonstrate the efficacy of molecularly-targeted approaches. The KEYNOTE-B21 study showed that combining pembrolizumab with chemotherapy improved prognosis for patients with MMRd endometrial cancer [133]. Similarly, the RUBY study demonstrated significant benefits for MMRd patients receiving dostarlimab combined with chemotherapy [133]. For NSMP endometrial cancer patients, a Chinese phase II trial achieved an objective response rate of 73.9% and disease control rate of 91.3% with sintilimab plus anlotinib, suggesting that combining ICIs with tyrosine kinase inhibitors represents an effective strategy [133].
In ovarian cancer, the ROSELLA trial demonstrated improved overall survival (16 months vs. 11.5 months) and progression-free survival (6.5 months vs. 5.5 months) with relacorilant plus nab-paclitaxel in platinum-resistant disease, positioning this regimen as a potentially robust add-on therapy without requiring biomarker selection [136].
Future Research Priorities and Regulatory Considerations
Future EDC research priorities include addressing mixture effects, where combined exposures to multiple EDCs may produce synergistic toxicity unrecognized in single-chemical studies [14]. Low-dose effects and non-monotonic dose responses challenge traditional risk assessment paradigms and require more sensitive testing approaches [14]. Transgenerational impacts demand longitudinal studies spanning multiple generations to fully characterize EDC legacy effects.
Advanced technologies offer promising research avenues. Artificial intelligence (AI) and machine learning can establish standardized data integration platforms, develop multimodal analysis algorithms, and strengthen preclinical-clinical translational research [135]. High-throughput screening systems combined with organoid models enable rapid assessment of multiple EDCs across diverse genetic backgrounds [134]. Integrated multi-omics approaches will elucidate how chemical exposures interact with genetic susceptibility to influence reproductive health outcomes.
Regulatory frameworks must evolve to address EDC-specific concerns. Current regulations typically fail to protect against low-dose effects, despite evidence that even minimal EDC exposure can cause health problems [87]. Global cooperation is essential, as chemical pollution transcends national boundaries. The newly adopted Global Framework on Chemicals represents a step toward international coordination, though implementation and enforcement mechanisms remain under development [87].
EDCs disrupt molecular pathways essential for reproductive health through multiple interconnected mechanisms, including hormone receptor interactions, HPG axis disruption, oxidative stress induction, and epigenetic modifications. These disruptions contribute to increasing rates of infertility and reproductive cancers, creating an urgent need for targeted therapeutic interventions. Molecular classification systems guide precision oncology approaches, enabling fertility-preserving strategies for appropriate candidates while identifying patients who require more aggressive treatment. Advanced technologies including multi-omics profiling, bioinformatics, and molecular dynamics simulations accelerate identification of novel therapeutic targets and candidate compounds. Future research must prioritize mixture effects, low-dose responses, and transgenerational impacts while developing more protective regulatory frameworks. Through integrated multidisciplinary approaches, researchers can translate mechanistic insights into effective strategies for mitigating EDC impacts on reproductive health.
Endocrine-disrupting chemicals (EDCs) represent a paramount public health challenge of the 21st century. These exogenous substances interfere with hormone synthesis, secretion, transport, binding, action, or elimination, consequently disrupting homeostasis and developmental processes [92]. The global research output on EDCs has increased disproportionately, reflecting growing scientific concern about their widespread effects on human health, particularly on infertility and reproductive cancers [137]. Current evidence consistently links EDC exposure to declining fertility rates and increasing incidence of hormone-dependent cancers, creating an urgent imperative to translate this scientific knowledge into effective public health policy [6] [115]. This translation requires sophisticated risk communication strategies that bridge the gap between complex toxicological evidence and actionable regulatory frameworks.
The communication challenge is multifaceted: EDCs encompass structurally diverse compounds with complex mechanisms of action; exposure is ubiquitous through multiple routes including food, air, water, and consumer products; and effects may manifest years after exposure during critical developmental windows [92] [26]. Furthermore, regulatory assessment must contend with non-monotonic dose responses, mixture effects, and transgenerational epigenetic impacts that complicate traditional toxicological paradigms [115]. This technical guide provides a comprehensive framework for communicating EDC risks to inform evidence-based public health policy within the context of infertility and reproductive cancers.
Scientific Evidence: EDCs and Adverse Health Outcomes
Epidemiological Evidence on Infertility
Substantial evidence demonstrates that EDCs adversely affect reproductive health outcomes in both males and females. Recent systematic reviews of observational studies published between 2014-2024 have identified consistent associations between EDC exposure and multiple reproductive endpoints [6].
Table 1: EDC Associations with Female Reproductive Outcomes
| Health Outcome | Associated EDCs | Effect Size/Prevalence | Key Evidence |
|---|---|---|---|
| Diminished Ovarian Reserve | BPA, phthalates, PFAS | Reduced antral follicle count; decreased oocyte yield | Significant correlation in women undergoing ART [6] [138] |
| Polycystic Ovary Syndrome (PCOS) | BPA, pesticides, phthalates | PCOS prevalence up to 20% in high-exposure regions; higher serum BPA in PCOS patients (167.04 ± 9.44 vs 31.94 ± 3.57 IU/mL) [29] [138] | Altered aromatase expression in granulosa cells [138] |
| Earlier Menopause | Pesticides, phthalates | 1.9-3.8 years earlier onset [29] | Shorter reproductive lifespan with combined exposures [29] |
| Endometriosis | BPA, phthalates | Increased risk with higher urinary BPA [138] | Association with influence on epigenetics [138] |
| Impaired IVF Outcomes | BPA, PFAS, POPs | Reduced fertilization and implantation rates [6] | Dose-dependent relationship in prospective studies [6] |
For male reproductive health, evidence is equally compelling. A groundbreaking meta-analysis revealed an approximately 50% decline in sperm concentration in men from industrialized regions between 1973-2011, with declining trends continuing into the 21st century [115]. Male factors now account for over half of all infertility cases, with EDCs identified as significant contributors through multiple pathological mechanisms [115].
Table 2: EDC Associations with Male Reproductive Outcomes
| Health Outcome | Associated EDCs | Effect Size | Key Evidence |
|---|---|---|---|
| Reduced Semen Quality | Phthalates, BPA, pesticides | 12-15% decrease in sperm motility; 12% lower serum testosterone in high-exposure groups [115] | Epidemiologic studies with biomarker measurements [6] [115] |
| Altered HPG Axis | Phthalates, organophosphate pesticides | Delayed pubertal onset by 6-12 months; altered LH/FSH ratios [115] | Longitudinal cohort studies [115] |
| Testicular Dysgenesis Syndrome | Phthalates, BPA, pesticides | Increased risk of hypospadias and cryptorchidism [26] [115] | Animal models and human epidemiological studies [26] |
| Sperm DNA Damage | BPA, heavy metals, pesticides | Increased DNA fragmentation index [115] | Case-control studies [115] |
EDCs and Reproductive Cancers
The contribution of EDCs to endocrine-related neoplasia represents a significant concern in cancer etiology. A comprehensive systematic review investigating associations between EDC exposure and risk of endocrine-related tumors analyzed 237 observational studies published between 1980-2020 [139]. The findings demonstrate substantial variation in EDC-associated cancer risk across different endocrine organs.
Table 3: EDC Associations with Reproductive Cancers by Organ Site
| Cancer Site | Strongest EDC Associations | Percentage of Studies Showing Increased Risk | Key Mechanistic Insights |
|---|---|---|---|
| Thyroid | Phthalates, pesticides, particulate matter | 67% | Estrogen receptor-mediated pathways; oxidative stress [139] |
| Testis | PCBs, pesticides, heavy metals | 57% | Altered fetal gonadal development; impaired androgen signaling [139] [26] |
| Breast | Pesticides, BPA, PCBs, phthalates | 48% | Estrogen mimicry; altered mammary gland development [140] [139] |
| Ovary | Phthalates, pesticides, BPA | 43% | Chronic inflammation; oxidative stress; hormone receptor activation [139] |
| Uterus | Phthalates, pesticides | 45% | Estrogen-dependent proliferation; progesterone resistance [140] [139] |
Mammary gland and uterine tissues are particularly vulnerable to EDCs with estrogenic potential due to their hormone-dependent growth [140]. The fetal and pre-pubertal periods represent critical windows of susceptibility, with exposure during development causing morphological and functional changes that predispose to neoplasia later in life [140]. The tissue organization field theory (TOFT) provides a framework for understanding how EDCs disrupt stromal-epithelial interactions during development, creating permissive conditions for carcinogenesis [140].
Methodological Framework: Assessing EDC Risks
Experimental Models and Biomarkers
Evaluating EDC risks requires integrating evidence from multiple methodological approaches, each with distinct strengths and limitations for risk assessment.
Epidemiological Studies: Observational studies in humans provide critical evidence of real-world EDC effects but face challenges including confounding factors, exposure misclassification, and long latency periods [6]. Recent advances in biomarker-based exposure assessment have strengthened epidemiological inference. For example, measuring urinary BPA metabolites or serum PFAS concentrations provides objective exposure data that can be correlated with health outcomes [6] [138].
Animal Models: Controlled laboratory studies in rodents and other species enable examination of specific EDC effects during defined critical windows. These models have demonstrated the transgenerational epigenetic effects of EDCs, with one seminal study showing that gestational exposure to vinclozolin or methoxychlor affects male fertility across multiple generations through DNA methylation changes [137]. Standardized protocols for assessing EDC effects on female reproduction include:
- Continuous Breeding Protocols: Exposure throughout mating, gestation, and lactation to assess multi-generational effects
- Critical Window Exposure: Specific exposure during fetal development, pre-puberty, or other sensitive periods
- Uterotrophic Assay: Measurement of uterine weight changes in immature or ovariectomized females
- Estrous Cycle Monitoring: Daily vaginal cytology to detect cycle irregularities
- Ovarian Follicle Counting: Systematic quantification of follicle types and stages
In Vitro Systems: Cell-based assays provide mechanistic insights into EDC actions at molecular and cellular levels. Commonly used systems include:
- ER-positive breast cancer cell lines (e.g., MCF-7) to assess estrogenic activity
- Ovarian granulosa cell cultures to examine steroidogenic disruption
- Testicular organoids to model spermatogenesis effects
- Receptor binding assays to quantify affinity for nuclear hormone receptors
In Silico Modeling: Computational approaches include:
- Quantitative structure-activity relationship (QSAR) models to predict endocrine activity
- Pharmacokinetic modeling to estimate internal dosimetry
- Mixture toxicity prediction using concentration addition or independent action models
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for EDC Investigation
| Reagent/Category | Specific Examples | Research Application | Technical Function |
|---|---|---|---|
| EDC Standards | BPA, DEHP, BPS, PFOS, PCB-153 | Exposure treatments; analytical standards | Positive controls; dose-response studies; reference materials for analytical chemistry |
| Molecular Biology Assays | ERα/ERβ binding assays, CYP19 (aromatase) activity kits, ELISA for steroid hormones | Mechanistic studies; high-throughput screening | Quantifying receptor affinity; measuring enzymatic inhibition; endocrine profiling |
| Epigenetic Tools | Methylated DNA immunoprecipitation (MeDIP) kits, HDAC inhibitors, CRISPR/dCas9 epigenetic editors | Transgenerational studies; mechanistic investigations | DNA methylation analysis; histone modification studies; targeted epigenetic manipulation |
| Biomarker Panels | Phthalate metabolites, BPA glucuronide, oxidative stress markers, miRNA panels | Human biomonitoring; epidemiological studies | Exposure assessment; effect biomarkers; early detection of pathological changes |
| Animal Models | CD-1 mice, Sprague-Dawley rats, zebrafish, C. elegans | In vivo toxicity testing; developmental studies | Whole-organism response assessment; multi-generational studies; high-throughput screening |
| Cell-Based Reporters | ER-CALUX, AR-CALUX, steroidogenic gene reporters | Mechanism screening; high-content analysis | Specific pathway activation; receptor activity profiling; mixture effects assessment |
Risk Communication Framework
Pathway from Evidence to Policy
Translating EDC research into effective public health policy requires systematic approaches that account for scientific complexity and uncertainty while providing actionable guidance.
Key Challenges in EDC Risk Communication
Communicating EDC risks requires addressing several unique scientific challenges:
Non-Monotonic Dose Responses: Unlike traditional toxicants, EDCs often exhibit non-monotonic dose-response curves where effects may be more pronounced at low doses than at high doses [115]. This challenges conventional risk assessment paradigms that assume monotonicity. Effective communication must explain this phenomenon to policymakers without undermining scientific credibility.
Mixture Effects: Humans are exposed to complex mixtures of EDCs throughout life, yet regulation typically evaluates chemicals individually [92] [29]. The concepts of concentration addition (CA) and independent action (IA) provide models for predicting mixture effects, but regulatory frameworks have been slow to incorporate mixture risk assessment [92]. Communicating cumulative risk requires transparent discussion of methodological limitations while advocating for precautionary approaches.
Critical Windows of Susceptibility: EDC effects are strongly influenced by developmental timing, with fetal, neonatal, and pubertal periods representing heightened susceptibility [26]. Communicating these temporal dimensions requires emphasizing protective measures for vulnerable populations, particularly pregnant women and children.
Transgenerational Epigenetic Effects: Evidence from animal studies demonstrates that EDC exposure can cause epigenetic modifications that are heritable across multiple generations [137] [115]. This challenges traditional exposure-risk paradigms and necessitates communication about potential long-term population health impacts that extend beyond directly exposed individuals.
Effective Communication Strategies
Successful risk communication for EDCs involves:
Tailored Messaging for Different Audiences:
- Researchers/Scientists: Emphasize methodological rigor, mechanistic plausibility, and data limitations
- Policymakers: Focus on population health impacts, economic costs, and feasible intervention points
- Healthcare Professionals: Provide clinical guidance on patient counseling and exposure reduction
- General Public: Offer practical advice on minimizing exposures while avoiding unnecessary alarm
Visualization of Complex Concepts: Diagrams, flowcharts, and infographics can effectively communicate pathways from exposure to health outcomes, particularly for non-specialist audiences. The diagrams in this document demonstrate how complex relationships can be rendered accessible.
Uncertainty Communication: Transparent acknowledgment of methodological limitations and evidence gaps maintains scientific credibility while supporting decision-making under uncertainty. Frameworks for classifying evidence strength (e.g., IARC classifications for carcinogens) provide models for categorizing confidence in EDC health effects.
Policy-Relevant Framing: Connecting EDC science to existing policy priorities (e.g., healthcare costs, childhood development, cancer prevention) increases relevance for decision-makers. Quantifying economic impacts of EDC-related diseases strengthens the case for preventive regulation.
The substantial evidence linking EDC exposure to infertility and reproductive cancers necessitates urgent policy action guided by sophisticated risk communication. Future directions should include:
- Strengthened Testing Requirements: Mandating comprehensive endocrine disruption screening for new chemicals and prioritizing existing chemicals for evaluation based on exposure potential and structure-activity relationships [115]
- Mixture Risk Assessment: Developing regulatory frameworks that account for cumulative effects of multiple EDCs, particularly those sharing mechanisms of action [92] [29]
- Vulnerability Protection: Implementing special protections for developmental windows of heightened susceptibility, including fetal, neonatal, and pubertal stages [26]
- Global Coordination: Harmonizing EDC regulations internationally to prevent regrettable substitutions and address transboundary contamination [137]
- Biomonitoring Expansion: Supporting large-scale, longitudinal biomonitoring programs to track population exposures and identify emerging EDCs [6] [137]
Translating the compelling scientific evidence on EDCs into effective public health policy represents both an urgent necessity and a profound communication challenge. By adopting the structured approaches outlined in this technical guide, researchers, risk assessors, and public health officials can collectively advance policies that mitigate EDC impacts on infertility and reproductive cancers, safeguarding current and future generations.
Conclusion
The evidence compellingly demonstrates that EDCs pose a significant threat to reproductive health through multiple interconnected mechanisms, including receptor-mediated hormonal disruption, epigenetic reprogramming, and oxidative stress. These effects manifest as declining fertility rates and increased incidence of hormone-sensitive cancers, with particular vulnerability during developmental windows. Future research must prioritize the development of sensitive biomarkers for early detection, elucidate the health implications of EDC mixtures, and investigate transgenerational effects. For biomedical and clinical research, these findings underscore the urgent need to integrate EDC screening into reproductive healthcare and develop targeted interventions that mitigate these chemical threats. Regulatory frameworks must evolve to address non-monotonic dose responses and cumulative mixture effects, while drug development should focus on blocking EDC-receptor interactions and reversing epigenetic modifications associated with reproductive pathologies.
References
- 1. Frontiers | Association between endocrine and... disrupting chemicals [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1608861/abstract]
- 2. - Endocrine ... | Nature Reviews Endocrinology disrupting chemicals [https://www.nature.com/articles/s41574-025-01131-x?error=cookies_not_supported&code=23ff0b2e-980d-477b-a2aa-72a067d1d791]
- 3. Endocrine Disruptors and Breast Cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12649852/]
- 4. the rapid rise of hormone-sensitive and early-onset breast ... [https://www.nature.com/articles/s41523-025-00840-w]
- 5. Fertility Treatments Might Be Associated With a Higher ... [https://www.aafp.org/pubs/afp/issues/2025/0900/poems-fertility-treatments-ovarian-cancer.html]
- 6. Associations Between Endocrine-Disrupting Chemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299029/]
- 7. Development and validation of a survey on reproductive ... [https://www.frontiersin.org/journals/reproductive-health/articles/10.3389/frph.2025.1519896/full]
- 8. Integrated Assessment of Bisphenols, Phthalates, and ... [https://www.sciencedirect.com/science/article/abs/pii/S0300483X25002604]
- 9. Intergenerational and transgenerational effects of ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1571689/full]
- 10. The impact, mechanisms and prevention strategies of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12520972/]
- 11. Analyzing kinetic signaling data for G-protein-coupled ... [https://www.nature.com/articles/s41598-020-67844-3]
- 12. Endocrine disruptor chemicals exposure and female fertility ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11672798/]
- 13. Epigenetic regulation by DNA methylation, histone ... [https://link.springer.com/article/10.1007/s00018-025-05831-5]
- 14. Endocrine-Disrupting Chemicals and Male Infertility [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565704/]
- 15. Impact of endocrine disrupting chemicals (EDCs) on ... [https://rbej.biomedcentral.com/articles/10.1186/s12958-025-01413-z]
- 16. Endocrine-Disrupting Chemicals [https://www.endocrine.org/topics/edc]
- 17. Multiple Studies Link Adverse Effects on Female ... [https://beyondpesticides.org/dailynewsblog/2025/01/multiple-studies-link-assault-on-female-reproductive-health-with-endocrine-disrupting-chemical-exposure/]
- 18. Epigenetic pharmacology in aging: from mechanisms to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611946/]
- 19. of Reproductive Toxicants: Transgenerational P Effects Epigenetic [https://www.longdom.org/open-access/transgenerational-effects-of-reproductive-toxicants-epigenetic-perspectives-1103456.html]
- 20. Molecular mechanisms of transgenerational inheritance epigenetic [https://www.nature.com/articles/s41576-021-00438-5?error=cookies_not_supported&code=b1f3be1b-29ae-49dc-a578-1519acaae3a4]
- 21. Exploring the Interconnected Mechanisms of Transgenerational ... [https://www.jsr.org/hs/index.php/path/article/view/6459]
- 22. Developmental Origins of Health and Disease: Integrating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4588819/]
- 23. The Developmental Origins of Health and Disease (DOHaD) [https://pmc.ncbi.nlm.nih.gov/articles/PMC6933571/]
- 24. Developmental reprogramming of cancer susceptibility - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3820510/]
- 25. The Developmental Origins of Health and Disease [https://www.mdpi.com/1660-4601/19/10/6024]
- 26. Endocrine-disrupting chemicals and reproductive health [https://www.sciencedirect.com/science/article/pii/S0003426625001064]
- 27. Endocrine Disrupting Chemicals, Reproductive Aging, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11753258/]
- 28. Impact of EDCs on Reproductive Systems [https://www.endocrine.org/topics/edc/what-edcs-are/common-edcs/reproduction]
- 29. Endocrine Disrupting Chemicals' Effects on Reproductive ... [https://beyondpesticides.org/dailynewsblog/2025/07/endocrine-disruptors-effects-on-reproductive-health/]
- 30. Editorial – Special issue on Developmental Origins of ... [https://www.sciencedirect.com/science/article/pii/S0890623824000157]
- 31. Developmental Origins of Health and Disease (DOHaD) [https://www.sciencedirect.com/science/article/abs/pii/S1526054221000579]
- 32. Endocrine disrupting chemicals and their effects on the ... [https://www.sciencedirect.com/science/article/abs/pii/S0013935123016298]
- 33. The possible role of the endocrine disrupting chemicals on ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1081704/full]
- 34. Redox mechanisms of environmental toxicants on male ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1333845/full]
- 35. From Inflammation to Infertility: How Oxidative Stress and ... [https://www.mdpi.com/2218-1989/15/4/267]
- 36. Racial/ethnic disparities in environmental endocrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5423735/]
- 37. Disruptive environmental chemicals and cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4565614/]
- 38. Oxidative stress, apoptosis and proliferation in uterus of ... [https://www.nature.com/articles/s41598-025-09895-y]
- 39. The impact of Bisphenol-A on human reproductive health [https://www.sciencedirect.com/science/article/pii/S2214750024001562]
- 40. Bisphenol A and its potential mechanism of action for ... [https://pubmed.ncbi.nlm.nih.gov/39725262/]
- 41. Research trends and hotspots of infertility and phthalate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425914/]
- 42. Phthalates, ovarian function and fertility in adulthood [https://www.sciencedirect.com/science/article/pii/S1521690X21000695]
- 43. Cancer health effects of pesticides: Systematic review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2231435/]
- 44. Pesticide-Induced Diseases: Cancer [https://www.beyondpesticides.org/resources/pesticide-induced-diseases-database/cancer]
- 45. Comprehensive assessment of pesticide use patterns and ... [https://www.frontiersin.org/journals/cancer-control-and-society/articles/10.3389/fcacs.2024.1368086/full]
- 46. A prospective cohort study of persistent endocrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11637482/]
- 47. Correlates of Persistent Endocrine Disrupting Chemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9215200/]
- 48. Diethylstilbestrol (DES) - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3948038/]
- 49. Machine learning-assisted high-content imaging analysis ... [https://www.nature.com/articles/s41598-024-53323-6]
- 50. Using in Vitro High Throughput Screening Assays to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3546348/]
- 51. A rapid screening test for endocrine disrupting chemicals ... [https://www.sciencedirect.com/science/article/abs/pii/S0166445X1300249X]
- 52. AIVIVE: a novel AI framework for enhanced in vitro to in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469192/]
- 53. In-Vitro Toxicology Testing Market Size 2025 to 2034 [https://www.precedenceresearch.com/in-vitro-toxicology-testing-market]
- 54. Multigenerational and transgenerational effects of endocrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4662893/]
- 55. Increased reproductive cancer risks following early-life ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969725017073]
- 56. L-20 Endocrine Disruptors and Infertility [https://www.sciencedirect.com/science/article/pii/S1472648323005424]
- 57. A cross-species comparative approach to assessing multi [https://www.sciencedirect.com/science/article/pii/S001393512101358X]
- 58. Reproductive toxicology of environmental endocrine ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1335028/full]
- 59. A curated knowledgebase on endocrine disrupting ... [https://www.sciencedirect.com/science/article/abs/pii/S004896971933339X]
- 60. Endocrine Disruptor Chemicals - Endotext - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK569327/]
- 61. Breast cancer incidence following low-dose rate ... [https://www.nature.com/articles/6604775]
- 62. Exposure to radiation therapy is associated with female ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4554371/]
- 63. Endocrine-disrupting chemicals exposure: cardiometabolic ... [https://cardiab.biomedcentral.com/articles/10.1186/s12933-025-02938-8]
- 64. Standardized statistical framework for comparison of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11485401/]
- 65. Biomarker Genes for Detecting Estrogenic Activity of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3367271/]
- 66. OMICS: Current and future perspectives in reproductive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4150148/]
- 67. Omics strategies for unveiling male fertility-related ... [https://www.sciencedirect.com/science/article/abs/pii/S2452014424000517]
- 68. Identification of biomarkers and outcomes of endocrine ... [https://www.sciencedirect.com/science/article/pii/S0300483X23000100]
- 69. Impact of endocrine disrupting chemicals (EDCs) on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12105221/]
- 70. Endocrine disruptor chemicals exposure and female fertility ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2024.1466967/full]
- 71. Modern Epigenetics Methods in Biological Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7785612/]
- 72. Mapping epigenetic modifications by sequencing ... [https://www.nature.com/articles/s41418-023-01213-1]
- 73. Laboratory methods to decipher epigenetic signatures [https://cmbl.biomedcentral.com/articles/10.1186/s11658-021-00290-9]
- 74. Perinatal DNA Methylation at CDKN2A Is Associated With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5528139/]
- 75. DNA methylation at birth within the promoter of ANRIL predicts ... [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-016-0259-5]
- 76. Determinants of p14/ARF methylation in healthy females [https://jmhg.springeropen.com/articles/10.1186/s43042-019-0025-2]
- 77. Methylation of p15 INK4b and Expression of ANRIL on ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0047193]
- 78. A deep-learning approach to predict reproductive toxicity of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12321834/]
- 79. Prediction of reproductive and developmental toxicity using ... [https://www.nature.com/articles/s41598-025-02590-y]
- 80. P28-28 Reproductive Impact Assessment of Endocrine ... [https://www.sciencedirect.com/science/article/abs/pii/S0378427425024166]
- 81. Molecular mechanism(s) of endocrine-disrupting chemicals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3823132/]
- 82. Endocrine disruptors: Unravelling the link between ... [https://www.sciencedirect.com/science/article/abs/pii/S0013935123021898]
- 83. Quality assurance and quality control for human biomonitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12206187/]
- 84. Guidance on minimum information requirements (MIR ... [https://www.sciencedirect.com/science/article/pii/S0160412025003526]
- 85. Nonmonotonic Dose–Response Curves Occur in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6137554/]
- 86. A proposed framework for the systematic review and ... [https://ehjournal.biomedcentral.com/articles/10.1186/s12940-016-0156-6]
- 87. Latest Science Shows Endocrine Disrupting Chemicals in ... [https://www.endocrine.org/news-and-advocacy/news-room/2024/latest-science-shows-endocrine-disrupting-chemicals-in-pose-health-threats-globally]
- 88. Nonmonotonic dose-response relationships [https://pubmed.ncbi.nlm.nih.gov/14600281/]
- 89. Using systematic reviews for hazard and risk assessment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4803521/]
- 90. Evaluating non-monotonic dose-response relationships in ... [https://www.sciencedirect.com/science/article/pii/S0045653524017132]
- 91. Acting on uncertainty: real-life mixtures of endocrine ... [https://link.springer.com/article/10.1057/s41292-020-00192-7]
- 92. Reproductive toxicity of combined effects of endocrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10214012/]
- 93. The evolution of endocrine disruptor chemical ... [https://www.sciencedirect.com/science/article/abs/pii/S0025326X23011621]
- 94. The adverse role of endocrine in the... disrupting chemicals [https://pmc.ncbi.nlm.nih.gov/articles/PMC10832042/]
- 95. Easy Targets: How Endocrine - Disrupting ... Chemicals Affect [https://endocrinenews.endocrine.org/easy-targets-how-endocrine-disrupting-chemicals-affect-reproductive-endocrinology/]
- 96. Frontiers | Role of personal care products as endocrine disruptors... [https://www.frontiersin.org/journals/reproductive-health/articles/10.3389/frph.2025.1514060/full]
- 97. Prenatal Dietary Exposure to Endocrine Disruptors and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568251/]
- 98. Exposure to endocrine-disrupting chemicals in follicular fluid [https://www.sciencedirect.com/science/article/abs/pii/S1472648325005486]
- 99. Endocrine disrupting chemicals impact on ovarian aging [https://www.sciencedirect.com/science/article/abs/pii/S0269749122004833]
- 100. Endocrine Disruptors [https://www.niehs.nih.gov/health/topics/agents/endocrine]
- 101. Potential effects of endocrine-disrupting chemicals on ... [https://www.sciencedirect.com/science/article/pii/S0147651325010462]
- 102. Endocrine disruptors - ECHA - European Union [https://echa.europa.eu/hot-topics/endocrine-disruptors]
- 103. Analysis of animal-to-human translation shows that only 5 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11175415/]
- 104. The Endocrine Disruptor Bisphenol A (BPA) Exerts a Wide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6864600/]
- 105. Potential adverse effects of nanoparticles on the reproductive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6294055/]
- 106. ZnO-Based Nanoparticles for Targeted Cancer Chemotherapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428772/]
- 107. Reproductive toxicity assessment of lasofoxifene, a ... [https://pubmed.ncbi.nlm.nih.gov/15282736/]
- 108. Associations Between Endocrine-Disrupting Chemical ... [https://www.mdpi.com/2075-1729/15/7/993]
- 109. Use of Biomarkers in Drug Development for Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12489174/]
- 110. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 111. New Clinical Practice Guideline for Blood-Based Biomarkers [https://aaic.alz.org/releases-2025/clinical-practice-guideline-blood-based-biomarkers.asp]
- 112. From Biomarker Discovery to Clinical Use [https://www.nordicbioscience.com/why-biomarkers/from-biomarker-discovery-to-clinical-use/]
- 113. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 114. Understanding exposures and latent disease risk within the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9014525/]
- 115. Endocrine-Disrupting Chemicals and Male Infertility [https://www.mdpi.com/2039-4713/15/5/165]
- 116. Consensus on the key characteristics of endocrine ... [https://www.nature.com/articles/s41574-019-0273-8]
- 117. Improving the integration of epidemiological data into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11492098/]
- 118. Review Endocrine disrupting chemicals exposure and health [https://www.sciencedirect.com/science/article/pii/S0147651325009194]
- 119. Integrating artificial intelligence with mechanistic ... [https://www.nature.com/articles/s41467-024-55461-x]
- 120. a comparison of different statistical models [https://www.nature.com/articles/s41598-024-76972-z]
- 121. Endocrine Disruptor Screening Program Federal Register ... [https://www.epa.gov/endocrine-disruption/endocrine-disruptor-screening-program-federal-register-notices]
- 122. Risk for female reproductive cancer may increase after early ... [https://www.niehs.nih.gov/news/factor/2023/11/papers/endocrine-disruptors-alter-cell-differentiation]
- 123. Understanding REACH - ECHA - European Union [https://echa.europa.eu/regulations/reach/understanding-reach]
- 124. EU REACH Regulation: Reporting & Compliance | IPOINT [https://go.ipoint-systems.com/blog/eu-reach-regulation]
- 125. REACH Regulation - Environment - European Commission [https://environment.ec.europa.eu/topics/chemicals/reach-regulation_en]
- 126. REACH Revision 2025: A Critical Moment for European ... [https://www.setac.org/resource/reach-revision-2025-a-critical-moment-for-european-chemical-safety.html]
- 127. EPA's Scientific Integrity Policy [https://www.epa.gov/scientific-integrity/epas-scientific-integrity-policy]
- 128. Authorship Best Practices | US EPA [https://www.epa.gov/scientific-integrity/authorship-best-practices]
- 129. Alternatives to animal testing - EFSA [https://www.efsa.europa.eu/en/topics/topic/alternatives-animal-testing]
- 130. Reducing Exposures to Endocrine Disruptors (REED) study, a ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-024-08627-3]
- 131. Bibliometric and visual analysis of global research on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12532360/]
- 132. What do people need to know about endocrine disrupting ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-025-25561-4]
- 133. Research Progress of Molecular Classification Guiding ... [https://www.scientificarchives.com/article/research-progress-of-molecular-classification-guiding-targeted-therapy-combined-with-fertility-preserving-treatment-for-endometrial-cancer]
- 134. Uncovering the Cellular and Molecular Landscape of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427882/]
- 135. Strategies for the drug development of cancer therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518319/]
- 136. ASCO 2025 highlights new treatment paradigms in oncology [https://www.drugdiscoverytrends.com/new-treatment-paradigms-in-oncology-highlights-from-the-asco-2025-annual-meeting/]
- 137. Global research on endocrine disruptors as emerging hazards ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12240779/]
- 138. Advances in understanding the reproductive toxicity of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1390247/full]
- 139. Review article Endocrine-disrupting chemicals and ... [https://www.sciencedirect.com/science/article/pii/S001393512202196X]
- 140. Endocrine disrupting chemicals (EDCs) and female cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC4801991/]