Endocrine Regulation of Circadian Rhythms: Molecular Mechanisms, Systemic Impacts, and Therapeutic Applications
This article provides a comprehensive synthesis for researchers, scientists, and drug development professionals on the intricate bidirectional relationship between the endocrine system and circadian biology.
Endocrine Regulation of Circadian Rhythms: Molecular Mechanisms, Systemic Impacts, and Therapeutic Applications
Abstract
This article provides a comprehensive synthesis for researchers, scientists, and drug development professionals on the intricate bidirectional relationship between the endocrine system and circadian biology. It explores the foundational molecular architecture of circadian clocks and their systemic synchronization by hormonal signals. The content delves into advanced methodologies for monitoring circadian endocrine rhythms and investigates the profound health consequences of circadian disruption, including metabolic syndrome, cardiometabolic disorders, and cognitive impairments. Furthermore, it evaluates emerging therapeutic strategies such as chronotherapy and time-restricted eating, which leverage circadian principles for optimized drug efficacy and metabolic health. By integrating genetic, physiological, and clinical perspectives, this review aims to bridge fundamental circadian science with translational applications for novel disease interventions and therapeutic development.
The Molecular Clockwork: Unraveling Core Mechanisms and Hormonal Synchronization
The suprachiasmatic nucleus (SCN) of the hypothalamus is the master circadian pacemaker in mammals, responsible for generating and coordinating daily ~24-hour cycles of physiology and behavior [1] [2]. This bilateral structure, containing approximately 20,000 neurons in mice and humans, synchronizes virtually all bodily processes—from sleep-wake cycles to hormone secretion and metabolism—with the external environment [3] [4] [5]. Its unique ability to generate autonomous, precise circadian rhythms while remaining responsive to environmental time cues makes it a critical regulator of organismal function. Within the broader context of endocrine regulation research, understanding SCN architecture is paramount, as this central clock exerts profound control over hormonal rhythms, including those of cortisol, melatonin, and reproductive hormones [6] [7]. This whitepaper provides an in-depth technical analysis of SCN organization, from its molecular mechanisms to its network-level properties, and details experimental approaches for its study, offering researchers a comprehensive resource for investigating circadian neuroendocrinology.
Anatomical and Neurochemical Organization
The SCN exhibits a sophisticated heterogeneous structure that underlies its function as a precise timekeeper. Located in the anterior hypothalamus directly above the optic chiasm, the nucleus is divided into two primary subregions: the ventrolateral "core" and the dorsomedial "shell" [1] [2] [7]. This anatomical specialization is consistent across mammalian species, though subtle morphological differences exist [2] [7].
Table: Key Neurochemical Subregions of the SCN
| Subregion | Primary Neuropeptides | Afferent Inputs | Functional Specialization |
|---|---|---|---|
| Core (Ventrolateral) | Vasoactive intestinal peptide (VIP), Gastrin-releasing peptide (GRP) [1] [7] | Retinohypothalamic tract (RHT), Geniculohypothalamic tract (GHT) [1] [2] | Receives and processes direct photic input; mediates entrainment to light-dark cycles [1] [3] |
| Shell (Dorsomedial) | Arginine vasopressin (AVP) [1] [7] | Primarily from SCN core; other hypothalamic areas [2] [7] | Generates autonomous rhythmicity; projects to hypothalamic targets for rhythm output [1] [7] |
This neuroanatomical organization creates a functional processing pathway where photic information received by the core is integrated and communicated to the shell, which in turn generates coherent rhythmic outputs to downstream systems [2] [7]. The core region is essential for producing rhythmic output signals, as its destruction abolishes circadian rhythms in hormone secretion, body temperature, and locomotor activity [7].
Molecular Mechanisms of Circadian Timekeeping
The SCN generates circadian rhythms through a core transcriptional-translational feedback loop (TTFL) that operates within individual SCN neurons [2] [4]. This cell-autonomous molecular clock consists of interlocking feedback loops that create approximately 24-hour oscillations in clock gene expression.
The core feedback loop begins with CLOCK and BMAL1 proteins forming heterodimers that activate transcription of Period (Per1, Per2, Per3) and Cryptochrome (Cry1, Cry2) genes by binding to E-box elements in their promoters [2] [4]. Following translation, PER and CRY proteins gradually accumulate in the cytoplasm, form heterodimers, and translocate to the nucleus where they inhibit CLOCK:BMAL1-mediated transcription, thereby repressing their own expression [2]. This negative feedback loop spans approximately 24 hours due to strategic delays in transcription, translation, and protein nuclear translocation. Subsequent degradation of PER and CRY proteins by ubiquitin ligase complexes (including β-TrCP1 and FBXL3) relieves the transcriptional inhibition, allowing the cycle to begin anew [2].
Additional stability is provided by auxiliary feedback loops, most notably through REV-ERBα, which inhibits Bmal1 transcription by binding to ROR elements, creating an interlocking loop that enhances rhythm robustness and precision [2] [4]. Recent evidence indicates that post-transcriptional and metabolic mechanisms also contribute to circadian timing, with membrane depolarization, intracellular calcium, and cAMP acting as both inputs to and outputs of the transcriptional clock, potentially forming reinforcing loops that stabilize rhythmicity [2].
Network Properties and Synchronization
While individual SCN neurons can generate circadian oscillations in isolation, the network properties of the intact SCN are essential for its precision and robustness as a master pacemaker [2] [4]. The SCN network synchronizes its cellular oscillators, reinforces their rhythms, responds to environmental inputs, increases robustness to genetic perturbations, and enhances temporal precision [2].
Communication within the SCN network involves multiple neurotransmitter and signaling systems. GABA serves as the primary fast neurotransmitter, with most SCN neurons being GABAergic [2]. The effects of GABA vary across the circadian cycle, exhibiting excitatory actions by day and inhibitory effects by night, though the mechanisms underlying this dual effect remain under investigation [1]. Neuropeptides play crucial roles in intra-SCN communication, with VIP-VPAC2 signaling in the core serving as a key synchronizer of cellular oscillations [1] [2]. This peptide signaling is particularly important for maintaining internal synchrony within the nucleus.
The SCN exhibits spatial and temporal waves of activity across the nucleus, with neurons in the dorsomedial shell typically phase-advanced relative to those in the ventrolateral core [7] [5]. This ordered pattern of activation was demonstrated in studies showing that Per1 expression begins in the shell and spreads slowly through the nucleus over approximately 12 hours before receding [7]. The phase distribution across the SCN network is not fixed but can be reconfigured in response to environmental changes, such as seasonal variations in day length, enabling the SCN to encode temporal information beyond the 24-hour cycle [2].
Table: SCN Network Characteristics and Functional Consequences
| Network Property | Mechanistic Basis | Functional Outcome |
|---|---|---|
| Synchronization | VIP/VPAC2 signaling; GABAergic transmission [1] [2] | Coherent rhythmic output across the entire nucleus [2] |
| Phase Wave | Topographically organized circuitry; differential phasing of regional activation [7] [5] | Temporal expansion of SCN output signals; seasonal encoding [2] |
| Robustness | Intercellular coupling; redundant signaling systems [2] [4] | Resistance to genetic and environmental perturbations [2] |
| Precision | Network-level averaging of cellular oscillations [2] [4] | Higher temporal accuracy than individual cellular oscillators [2] |
Connectivity along the caudal-to-rostral axis appears particularly important for maintaining proper network function, with computational modeling suggesting that coronal slicing (which disrupts this axis) has the most detrimental effect on oscillatory dynamics, while horizontal slicing has the least impact [5].
Endocrine Regulation and Output Pathways
The SCN regulates endocrine function through multiple efferent pathways that convey temporal information to peripheral tissues. The major monosynaptic efferents from the SCN project to hypothalamic nuclei including the subparaventricular zone, medial preoptic nucleus, dorsomedial hypothalamus, and paraventricular nucleus [1] [8]. These projections ultimately regulate the secretion of hormones including melatonin, cortisol, and reproductive hormones [1] [6] [7].
The SCN regulates the hypothalamic-pituitary-adrenal (HPA) axis through AVP projections from the shell to the PVN, which generates the circadian rhythm in corticotropin-releasing hormone release and ultimately cortisol secretion [6] [7]. Additionally, the SCN influences adrenal sensitivity to ACTH via autonomic innervation through the splanchnic nerve, and the adrenal gland's intrinsic circadian clock gates its response to ACTH [6]. This multilayered regulation creates a robust circadian rhythm in glucocorticoid secretion that peaks just before the active phase [6].
The melatonin rhythm is generated through a polysynaptic pathway from the SCN to the pineal gland. During the night, SCN efferents ultimately trigger norepinephrine release in the pineal, stimulating melatonin production through β-1 and α-1 adrenergic receptors on pinealocytes [1] [6]. Melatonin serves as a hormonal signal of darkness duration, with production prolonged during long winter nights and shortened in summer, thus communicating seasonal information to tissues throughout the body [1] [6].
The SCN also regulates metabolic hormones through both direct and indirect pathways. The dorsomedial hypothalamus, a major recipient of SCN output, is crucial for generating circadian rhythms in feeding behavior, thereby influencing insulin, leptin, ghrelin, and other metabolic hormones [6] [8]. The timing of food intake can itself reset peripheral clocks, creating a feedback loop between metabolic state and circadian timing [6].
Experimental Models and Methodologies
Monitoring SCN Oscillations
Advanced techniques enable real-time monitoring of SCN molecular rhythms. The PER2::LUCIFERASE (PER2::LUC) system is a cornerstone method, using SCN tissue slices from genetically modified mice expressing a PER2-luciferase fusion protein [5]. When cultured with luciferin, bioluminescence intensity reflects PER2 expression levels, allowing long-term, real-time monitoring of circadian gene expression in intact SCN slices [5]. This approach revealed spatiotemporal waves of PER2 expression across the SCN but is limited by tissue slicing, which disrupts intrinsic connectivity and alters network dynamics [5].
Emerging volumetric imaging techniques address this limitation. Intact, unsliced SCN can be studied using light-sheet microscopy combined with tissue clearing methods such as iDISCO, enabling visualization of PER2 expression throughout the entire nucleus without disrupting its native circuitry [5]. This approach preserves the complex three-dimensional architecture of the SCN and provides a more complete picture of its network dynamics.
Table: Essential Research Reagents for SCN Circadian Research
| Research Tool | Composition/Type | Primary Research Application |
|---|---|---|
| PER2::LUC Mouse Model | Transgenic mouse expressing PER2-luciferase fusion protein [5] | Real-time monitoring of molecular clock function in SCN slices via bioluminescence [5] |
| Luciferin | D-luciferin substrate | Culture medium additive for bioluminescence imaging in PER2::LUC systems [5] |
| iDISCO Protocol | Tissue clearing reagents | Preparation of intact SCN for volumetric imaging using light-sheet microscopy [5] |
| Calcium Indicators | Genetically encoded or chemical fluorescent dyes | Monitoring rhythmic neuronal activity in SCN slices or in vivo [2] |
| VIP/AVP Receptor Antagonists | Pharmacological inhibitors | Investigating neuropeptide signaling in SCN network synchronization [1] [2] |
Experimental Protocol: PER2::LUC Rhythm Monitoring in SCN Slices
Objective: To characterize circadian rhythms of gene expression in SCN explants from PER2::LUC mice [5].
Tissue Preparation:
- Sacrifice PER2::LUC reporter mice during the light phase under appropriate anesthesia.
- Rapidly dissect brain and prepare coronal hypothalamic slices (150-250 μm thickness) using a vibratome in ice-cold, oxygenated artificial cerebrospinal fluid.
- Microdissect the SCN region from surrounding hypothalamic tissue.
Culture Establishment:
- Place SCN explants on culture membrane inserts in 35mm dishes containing 1.2mL of culture medium (e.g., DMEM with HEPES, B27 supplement, and 0.1mM luciferin).
- Seal dishes with coverslips using silicone grease to prevent evaporation and maintain sterility.
Data Acquisition:
- Transfer cultures to a light-tight chamber maintained at 36°C.
- Collect bioluminescence signals using photomultiplier tubes or cooled CCD cameras at 10-60 minute intervals for 5-10 days.
- Maintain constant temperature and darkness throughout imaging.
Data Analysis:
- Subtract baseline drift using 24-hour moving averages.
- Fit damped cosine curves or use FFT-NLLS algorithms to determine period, phase, and amplitude of rhythms.
- Generate phase maps from image data to visualize spatiotemporal wave patterns.
This protocol yields precise measurements of circadian period and amplitude in SCN tissue, though it should be noted that slicing orientation affects results due to disruption of specific connectivity axes [5].
Clinical and Therapeutic Implications
SCN dysfunction has significant clinical consequences, with circadian disruption implicated in various mood disorders, sleep disorders, and metabolic conditions [1] [6]. Patients with major depressive disorder frequently show phase-delayed circadian rhythms and disrupted sleep architecture, while bipolar disorder exhibits contrasting phase abnormalities—phase-advanced during manic episodes and phase-delayed during depressive episodes [1]. Seasonal affective disorder is strongly linked to dysfunctional serotonergic pathways and abnormal melatonin rhythms [1] [6].
Chronopharmacology represents a promising therapeutic approach that leverages knowledge of circadian regulation to optimize drug timing [1]. Because the absorption, metabolism, and excretion of many pharmaceuticals vary across the circadian cycle, coordinating drug administration with internal biological time can enhance efficacy and reduce side effects [1]. This is particularly relevant for endocrine therapies, given the robust circadian rhythms in hormone secretion and receptor expression [6].
The SCN also mediates the health consequences of modern lifestyle challenges, including shift work, jet lag, and artificial light exposure at night [1] [6]. These conditions create misalignment between the central SCN clock and peripheral tissue clocks, as well as between internal circadian rhythms and external environmental demands. Such misalignment is associated with increased risks of metabolic syndrome, cardiovascular disease, and certain cancers, highlighting the importance of maintaining proper circadian alignment for human health [6].
The suprachiasmatic nucleus represents a remarkable integration of molecular precision and network-level computation. Its sophisticated architecture—from the cell-autonomous transcriptional-translational feedback loops to the carefully orchestrated neurochemical and temporal organization across its core and shell subregions—enables it to function as the body's master circadian pacemaker. The SCN's ability to synchronize with environmental light-dark cycles while maintaining robust internal timekeeping allows it to coordinate endocrine rhythms essential for health and homeostasis. Ongoing research continues to reveal how SCN network properties emerge from its constituent cellular oscillators and how these properties enable the encoding of seasonal and other temporal information. For researchers and drug development professionals, understanding SCN architecture provides not only fundamental insights into circadian biology but also promising avenues for therapeutic intervention through chronopharmacological approaches that align treatments with the body's internal temporal architecture.
Circadian rhythms are endogenous, ~24-hour oscillations in physiological processes that allow organisms to anticipate and adapt to daily environmental changes. These rhythms are governed by a cell-autonomous molecular clockwork present in nearly every cell, which is hierarchically coordinated by a master pacemaker in the suprachiasmatic nucleus (SCN) of the hypothalamus [9] [10]. The SCN receives light input from the retina and synchronizes peripheral oscillators throughout the body via neurohumoral signals, including endocrine pathways [9] [11]. This master clock integrates external environmental changes and internal physiological signals to generate natural oscillations of secreted endocrine signals such as melatonin, cortisol, and thyrotropin, which in turn regulate diverse biological processes [12] [10]. The core molecular mechanism generating these rhythms consists of interlocked transcriptional-translational feedback loops (TTFLs) involving several core clock components: the activators CLOCK and BMAL1, the repressors PER and CRY, and the stabilizing nuclear receptors REV-ERB and ROR [9] [13] [10]. This molecular oscillator not only drives circadian rhythmicity but also temporally gates endocrine function, creating a crucial bidirectional relationship between the circadian system and endocrine regulation [12] [14].
Molecular Architecture of the Core Circadian Clock
The Primary Negative Feedback Loop
The core negative feedback loop consists of the transcriptional activators CLOCK (or its paralog NPAS2 in some tissues) and BMAL1, which form a heterodimer that binds to E-box enhancer elements (CACGTG) in the promoter regions of target genes [10]. This CLOCK-BMAL1 complex drives the transcription of period (Per1, Per2, Per3) and cryptochrome (Cry1, Cry2) genes [9] [10]. After translation, PER and CRY proteins form multimeric complexes in the cytoplasm that translocate back into the nucleus to inhibit CLOCK-BMAL1-mediated transcription, thus completing a 24-hour feedback cycle [9] [10]. The timing of this loop is regulated by post-translational modifications, particularly phosphorylation by casein kinase 1ε/δ (CK1ε/δ) and adenosine monophosphate kinase (AMPK), which tag PER and CRY proteins for ubiquitination and degradation by the 26S proteasome complex [10].
The Stabilizing Auxiliary Loop
A crucial auxiliary feedback loop involves the nuclear receptors REV-ERB (α and β) and ROR (α, β, and γ), which regulate Bmal1 transcription and provide stability to the core oscillator [9] [13] [15]. The CLOCK-BMAL1 heterodimer activates transcription of Rev-erbα and Rev-erbβ genes [9]. REV-ERB proteins then compete with ROR activators for binding to ROR response elements (ROREs) in the Bmal1 promoter [9] [15]. While RORs activate Bmal1 transcription, REV-ERBs function as transcriptional repressors by recruiting the nuclear receptor corepressor (NCoR)-histone deacetylase 3 (HDAC3) complex [9] [13]. This competing activation and repression creates precisely timed anti-phase oscillations of Bmal1 transcription relative to Per and Cry expression [9] [15].
Table 1: Core Components of the Mammalian Circadian Clock Mechanism
| Component | Type | Function | Role in Feedback Loop |
|---|---|---|---|
| CLOCK | Transcription factor | Forms heterodimer with BMAL1; histone acetyltransferase activity | Positive element; activates Per, Cry, Rev-erb transcription |
| BMAL1 | Transcription factor | Forms heterodimer with CLOCK; binds E-box elements | Positive element; essential for rhythm generation |
| PER | Repressor protein | Forms complex with CRY; inhibits CLOCK-BMAL1 activity | Negative element; rhythm period determination |
| CRY | Repressor protein | Forms complex with PER; inhibits CLOCK-BMAL1 activity | Negative element; strong transcriptional repression |
| REV-ERB | Nuclear receptor | Represses Bmal1 transcription; competes with ROR | Negative element in auxiliary loop; stabilizes rhythms |
| ROR | Nuclear receptor | Activates Bmal1 transcription; competes with REV-ERB | Positive element in auxiliary loop; regulates rhythm amplitude |
Tissue-Specific Variations in Clock Architecture
While the core clock mechanism is present in nearly all cells, tissue-specific variations exist in the relative importance of different feedback loops. Computational modeling of circadian gene expression across different tissues has revealed that the essential feedback loops differ between tissues, pointing to specific design principles within the hierarchy of mammalian tissue clocks [16]. For example, self-inhibitions of Per and Cry genes are characteristic for models of SCN clocks, whereas in liver models, multiple loops act in synergy and are connected by a repressilator motif (a system of three mutually repressing genes) [16]. In heart tissue, Bmal1–Rev-erb-α loops appear to be particularly important, while repressilator motifs are rarely found in brain, heart, and muscle tissues due to the earlier phases and small amplitudes of Cry1 in these tissues [16]. This tissue-specific use of a network of co-existing synergistic feedback loops could account for functional differences between organs and their specific endocrine relationships.
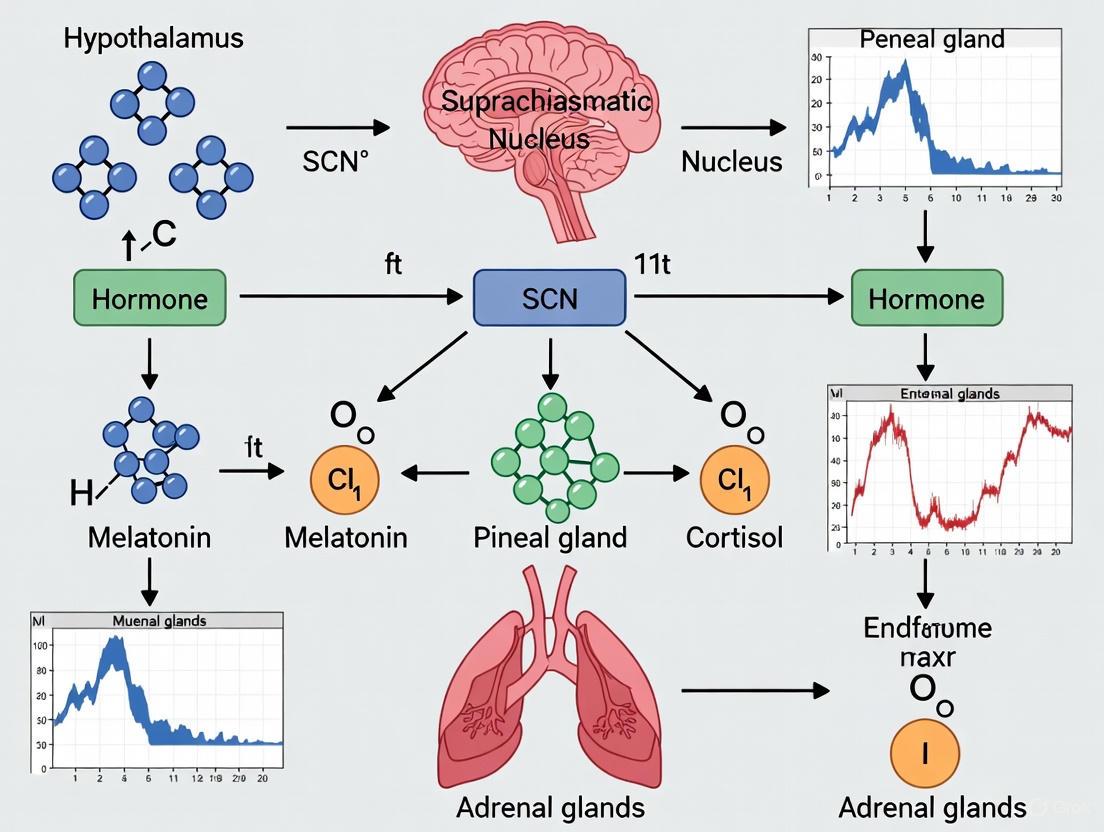
Diagram 1: Core transcriptional-translational feedback loops of the mammalian circadian clock. The core negative feedback loop (blue/red) and auxiliary stabilizing loop (gray/green) interact to generate robust ~24-hour oscillations. REV-ERB and ROR compete for binding to ROR response elements (ROREs) in the BMAL1 promoter.
Experimental Analysis of Circadian Clock Mechanisms
Genetic Manipulation Approaches
Understanding the hierarchical importance of clock components has required sophisticated genetic approaches. Functional redundancy between REV-ERBα and REV-ERBβ was demonstrated through combined gene knockout and RNA interference, showing that both are required for rhythmic Bmal1 expression but are functionally redundant [17]. In contrast, the RORs contribute to Bmal1 amplitude but are dispensable for Bmal1 rhythm [17]. Importantly, cells deficient in both REV-ERBα and β function, or those expressing constitutive BMAL1, were still able to generate and maintain normal Per2 rhythmicity, underscoring the resilience of the intracellular clock mechanism [17]. This demonstrates that while the auxiliary loop contributes to fine-tuning of the core loop, its primary function is to provide discrete waveforms of clock gene expression for control of local physiology rather than being absolutely essential for rhythm generation [17].
Table 2: Key Genetic Manipulation Studies in Circadian Rhythm Research
| Genetic Approach | Key Findings | Experimental Model | Reference |
|---|---|---|---|
| REV-ERBα/β double knockout | REV-ERBα and β are functionally redundant; required for rhythmic Bmal1 expression but not essential for core clock function | Fibroblast cell culture | [17] |
| ROR knockdown | RORs contribute to Bmal1 amplitude but are dispensable for Bmal1 rhythm | Cell culture models | [17] |
| Constitutive BMAL1 expression | Bmal1 mRNA/protein cycling not necessary for basic clock function; core PER/CRY loop sufficient for rhythm generation | Fibroblast cell culture; Bmal1-/- mice | [17] |
| Tissue-specific modeling | Essential feedback loops differ between tissues; Per/Cry auto-inhibition dominant in SCN, repressilator motifs in liver | Computational modeling of multiple tissues | [16] |
Real-Time Monitoring of Circadian Rhythms
Longitudinal monitoring of circadian rhythms in real-time has been crucial for understanding clock dynamics. Real-time bioluminescence monitoring of gene expression using reporters such as Per2-luciferase has allowed researchers to assess the persistence of circadian rhythmicity in various genetic backgrounds [17]. This approach circumvents the limitations of behavioral analysis, which may not faithfully reflect intracellular clock function due to pleiotropic effects and functional redundancy [17]. For endocrine research, engineered cells with genomically integrated switch components using transposase-based systems have enabled the establishment of clonal cell populations with robust circadian characteristics [12]. Single cell clones can be isolated via fluorescence-activated cell sorting (FACS), and high-performing clones can be identified based on transgene expression and fold induction (e.g., up to 40-fold induction in response to circadian signals) [12].
Diagram 2: Experimental workflow for analyzing core clock components and their therapeutic applications. The process begins with genetic manipulation, proceeds through circadian rhythm assessment, and culminates in therapeutic development.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Circadian Rhythm Studies
| Reagent/Category | Specific Examples | Function/Application | Experimental Use |
|---|---|---|---|
| Bioluminescence Reporters | Per2-luciferase, Bmal1-luciferase | Real-time monitoring of promoter activity | Longitudinal tracking of circadian rhythms in living cells and tissues |
| Gene Editing Tools | CRISPR-Cas9, RNA interference | Targeted knockout/knockdown of clock genes | Functional analysis of specific clock components |
| Cell Line Models | HEK293T, CHO, hMSC, primary fibroblasts | In vitro testing of circadian mechanisms | Screening of genetic manipulations and drug effects |
| Nuclear Receptor Ligands | REV-ERB agonists (SR9009), ROR inverse agonists | Pharmacological modulation of auxiliary loop | Testing stability and resilience of circadian oscillations |
| Hormonal Sensors | Melatonin receptor assays, cortisol measurements | Monitoring endocrine-circadian interactions | Studying bidirectional clock-endocrine relationships |
| Computational Tools | Global optimization algorithms, tissue-specific models | Analysis of complex circadian networks | Identifying essential feedback loops in different tissues |
Circadian-Endocrine Integration and Therapeutic Implications
Endocrine Regulation of Circadian Rhythms
The circadian system exhibits profound bidirectional relationships with endocrine pathways. The SCN controls peripheral oscillators through autonomic innervation of peripheral tissues, endocrine signaling (glucocorticoids), body temperature, and feeding-related cues [10]. Glucocorticoids in particular serve as humoral entraining signals for peripheral oscillators, as glucocorticoid-response elements (GREs) are present in promoter regions of core clock components, enabling glucocorticoids to regulate transcriptional activation of clock genes and clock-related genes [10]. Additionally, circadian regulation of host-microbiota crosstalk has emerged as an important factor in systemic physiology, with microbial-derived metabolites (short-chain fatty acids, bile acids, indoles) acting as circadian cues, while host clock genes modulate microbial ecology and intestinal barrier integrity [14]. This establishes a dynamic circadian-microbiota axis that synchronizes nutrient processing, hormonal secretion, immune surveillance, and neural signaling [14].
Chronotherapy and Circadian-Targeted Therapeutics
The growing understanding of circadian biology has spurred development of therapeutic approaches targeting the molecular clock. Chronotherapy involves aligning treatments with circadian rhythms to maximize efficacy and minimize side effects, while direct circadian modulation aims to correct underlying rhythm disturbances using chronobiotics [11]. REV-ERB has emerged as a particularly promising therapeutic target, as it regulates glucose and lipid metabolism, inflammation, autophagy, ferroptosis, and mitochondrial function in addition to its circadian functions [9]. Pharmacological activation of REV-ERB has shown promise in reducing pathological gene expression and improving outcomes in myocardial infarction and heart failure preclinical models [9]. For endocrine applications, synthetic biology approaches have engineered melatonin-responsive gene switches that can translate circadian inputs into therapeutic outputs, demonstrating potential for cell-based therapies for obesity-dependent type-2 diabetes through circadian-regulated GLP-1 expression [12]. Nanomaterial-enabled drug delivery systems are also being developed for circadian medicine, leveraging liposomes, polymeric nanoparticles, and mesoporous silica nanoparticles to deliver drugs to specific targets over sustained periods aligned with circadian biology [11].
The core transcriptional-translational feedback loops comprising CLOCK, BMAL1, PER, CRY, REV-ERB, and ROR represent a fundamental biological mechanism that orchestrates ~24-hour rhythms in virtually all physiological processes, with particularly profound implications for endocrine regulation. The hierarchical organization of this system, with the SCN as master pacemaker coordinating peripheral oscillators through endocrine and neural pathways, ensures temporal coordination across tissues and systems. The resilience of the core PER/CRY feedback loop, stabilized by the auxiliary REV-ERB/ROR loop, provides both robustness and flexibility to adapt to changing environmental conditions. From a therapeutic perspective, targeting core clock components—particularly REV-ERB—holds significant promise for treating metabolic, cardiovascular, and endocrine disorders, while chronotherapeutic approaches leverage circadian timing to optimize drug efficacy and safety. Future research will continue to elucidate tissue-specific clock variations and their implications for endocrine health, potentially leading to more personalized circadian medicine approaches.
The suprachiasmatic nucleus (SCN) serves as the master circadian pacemaker, coordinating daily rhythms in physiology and behavior. This whitepaper details the neural and endocrine output pathways through which the SCN synchronizes peripheral clocks throughout the body. The SCN achieves temporal coordination via autonomic nervous system outputs and hormonal signaling cascades, including regulation of glucocorticoids and melatonin. Disruption of these pathways contributes to metabolic disorders, cardiovascular disease, and neurodegeneration. Emerging chronotherapeutic strategies that target these synchronization mechanisms offer promising avenues for optimizing drug efficacy and developing novel treatments for circadian-related disorders. Understanding these systemic synchronizers provides a critical foundation for advancing circadian medicine in clinical practice and drug development.
The suprachiasmatic nucleus (SCN) of the hypothalamus functions as the central circadian pacemaker in mammals, coordinating a network of peripheral clocks located throughout the brain and body [18] [19]. This approximately 20,000-neuron structure in rodents generates endogenous ~24-hour rhythms through cell-autonomous transcriptional-translational feedback loops (TTFLs) involving core clock genes such as CLOCK, BMAL1, PER, and CRY [19]. While individual SCN neurons can generate independent circadian oscillations, network interactions within the SCN enhance rhythm amplitude and robustness through synaptic signaling involving gamma-aminobutyric acid (GABA) and vasoactive intestinal peptide (VIP) [19].
The SCN receives photic input directly from the retina via the retinohypothalamic tract, aligning internal circadian time with the external light-dark cycle [18]. However, the SCN also integrates non-photic cues, including metabolic and hormonal signals, to maintain optimal temporal coordination [19]. The primary function of the SCN is to synchronize peripheral oscillators in organs and tissues, which it accomplishes through two principal output pathways: direct neural projections and systemic endocrine signals [18] [20]. These synchronized outputs regulate daily rhythms in physiology, including sleep-wake cycles, hormone secretion, metabolism, and cardiovascular function.
Table 1: Core Clock Genes and Proteins in the SCN TTFL
| Gene/Protein | Function in TTFL | Role in Rhythm Generation |
|---|---|---|
| CLOCK | Transcriptional activator | Forms heterodimer with BMAL1; binds E-box elements |
| BMAL1 | Transcriptional activator | Forms heterodimer with CLOCK; initiates transcription of Per and Cry genes |
| PER1-3 | Transcriptional repressors | Accumulate, form complexes with CRY proteins, inhibit CLOCK:BMAL1 activity |
| CRY1/2 | Transcriptional repressors | Stabilize PER proteins, facilitate nuclear translocation, suppress transcription |
| REV-ERBα/β | Auxiliary loop regulator | Suppresses Bmal1 transcription by competing for RORE elements |
| RORα/β | Auxiliary loop regulator | Activates Bmal1 transcription by competing for RORE elements |
Neural Output Pathways from the SCN
The SCN coordinates peripheral circadian rhythms through direct neural projections to key hypothalamic nuclei, which subsequently regulate autonomic outflow to peripheral organs and endocrine systems [19]. These hard-wired neural networks form the primary pathway for immediate SCN control over physiological rhythms.
Central Neural Circuitry
SCN efferent projections are largely confined to hypothalamic and midline thalamic regions, with the most prominent projections targeting the subparaventricular zone (SPZ) and dorsomedial hypothalamic nucleus (DMH) [19]. The SPZ serves as an intermediate relay station that amplifies and distributes SCN signals to other brain regions. Lesion studies indicate that the SPZ contributes significantly to the regulation of daily rhythms in sleep, locomotor activity, and body temperature [19].
The DMH, in turn, projects to multiple nuclei governing specific physiological functions:
- Ventrolateral preoptic nucleus (VLPO): Regulates sleep-wake cycles
- Lateral hypothalamic area (LHA): Coordinates energy balance and arousal
- Paraventricular nucleus of the hypothalamus (PVN): Modulates stress response and autonomic tone [19]
This multi-synaptic pathway allows the SCN to indirectly influence diverse functions including neuroendocrine secretion, autonomic nervous system activity, and behavior.
Autonomic Regulation of Peripheral Organs
The SCN regulates peripheral circadian clocks via autonomic nervous system outputs. SCN projections to the PVN initiate sympathetic and parasympathetic pathways that synchronize peripheral oscillators in organs such as the liver, heart, and pancreas [18]. This neural synchronization enables rapid, tissue-specific regulation of circadian physiology without relying on systemic cues.
The adrenal gland exemplifies this neural control mechanism. The SCN influences glucocorticoid secretion not only through the hypothalamic-pituitary-adrenal (HPA) axis but also via direct innervation through the splanchnic nerve, which modulates adrenal sensitivity to adrenocorticotropic hormone (ACTH) [6] [20]. This autonomic connection transmits photic information directly from the SCN to the adrenal cortex, contributing to the robust circadian rhythm of glucocorticoid release [6].
Endocrine Output Pathways from the SCN
In addition to direct neural control, the SCN regulates systemic synchronizers through neuroendocrine pathways that rhythmically release hormones into circulation. These hormonal signals serve as potent zeitgebers for peripheral clocks throughout the body.
Glucocorticoid Rhythms
Circulating glucocorticoids (cortisol in humans, corticosterone in rodents) exhibit robust circadian rhythms that are critically dependent on SCN regulation. The SCN generates this rhythm through three distinct mechanisms:
- Circadian control of the HPA axis via arginine-vasopressin (AVP) projections from the SCN to the PVN, generating rhythmic firing patterns in downstream regions [6]
- Autonomic regulation of adrenal sensitivity via the splanchnic nerve, which modulates adrenal responsiveness to ACTH [6] [20]
- Gating of adrenal sensitivity by the intrinsic adrenal circadian clock, which further contributes to robust glucocorticoid rhythm generation [6]
Glucocorticoids function as systemic synchronizers by binding to glucocorticoid receptors (GR) and mineralocorticoid receptors (MR) that directly regulate clock gene expression, particularly Per1 and Per2, in peripheral tissues [6]. Through this mechanism, the daily glucocorticoid rhythm entrains peripheral clocks throughout the body.
Table 2: Endocrine Synchronizers Regulated by the SCN
| Hormone | Rhythm Characteristics | Primary Targets | Function as Zeitgeber |
|---|---|---|---|
| Glucocorticoids | Peak before active phase; ultradian pulsatility | Liver, heart, adipose, muscle | Resets peripheral clocks via GREs in clock genes |
| Melatonin | Nocturnal peak; duration encodes night length | SCN, pituitary, immune cells | Provides feedback to SCN; synchronizes peripheral tissues |
| Vasopressin | Diurnal rhythm from SCN neurons | SPZ, DMH, PVN | Regulates HPA axis; coordinates neural outputs |
| Prokineticin 2 | Highest expression during subjective night | DMH, LHA | Reduces locomotor activity; regulates circadian behavior |
Melatonin Rhythms
Melatonin secretion from the pineal gland represents another key endocrine output of the SCN. The SCN generates the melatonin rhythm through two regulatory signals:
- A clock-coupled signal that restricts melatonin synthesis to the nocturnal phase
- An inhibitory signal that transmits incidental nighttime light exposure to acutely suppress melatonin production [6]
Melatonin acts as both a rhythm driver and zeitgeber by:
- Providing feedback to the SCN via MT1 and MT2 receptors to fine-tune circadian phase
- Synchronizing peripheral clocks in various tissues through receptor-mediated signaling pathways
- Refining the amplitude and robustness of circadian rhythms throughout the body [6]
The duration of melatonin secretion encodes night length, providing a seasonal timing signal that regulates photoperiodic responses in mammals.
Other Hormonal Outputs
The SCN also regulates the circadian rhythms of several other hormones through direct and indirect pathways:
- Growth hormone: Secretion peaks at sleep onset and correlates with renin levels [6]
- Thyroid-stimulating hormone: Exhibits a circadian rhythm that is influenced by sleep-wake state
- Metabolic hormones: Including leptin, adiponectin, ghrelin, insulin, and glucagon, whose rhythms are influenced by both circadian timing and feeding behavior [6]
These endocrine rhythms collectively coordinate temporal organization across metabolic, immune, and cardiovascular systems.
Experimental Protocols for Studying SCN Output Pathways
Multi-Modal Data Acquisition and Synchronization
Investigating SCN output pathways requires precise temporal alignment of data from multiple recording modalities. The Syntalos platform provides an open-source solution for synchronized multi-modal data acquisition [21].
Protocol: Synchronized Neural and Endocrine Recording
- System Setup: Configure Syntalos with modules for electrophysiology (Intan RHX), calcium imaging (UCLA Miniscope), video tracking, and endocrine sampling apparatus
- Timing Synchronization: Implement continuous timestamp alignment to a global master clock with statistical analysis and correction of individual device timestamp divergences
- Data Acquisition: Simultaneously record neuronal activity (spike patterns, calcium dynamics), behavioral parameters (locomotor activity, feeding), and endocrine samples (blood collection for hormone assay)
- Closed-Loop Interventions: Program Arduino-based I/O interfaces for state-dependent sampling with 2-6 ms latency
- Data Integration: Store all data in structured formats with unified timestamps for subsequent correlation analysis
Validation: Temporal misalignment >1 ms/sec between high-speed video and electrophysiological signals can reduce stimulus classification accuracy from 100% to chance levels in sensory discrimination tasks, highlighting the critical importance of precise synchronization [21].
SCN Neural Circuit Mapping
Protocol: Anterograde and Retrograde Tract Tracing
- Stereotaxic Surgery: Inject recombinant AAV-expressing fluorescent reporters (e.g., GFP) under cell-specific promoters into the SCN of anesthetized mice
- Neural Pathway Visualization: Process brain sections for immunohistochemistry to identify projection targets (SPZ, DMH, PVN)
- Functional Connectivity Assessment: Combine tract tracing with immediate early gene (c-Fos) expression during specific circadian phases
- Circuit Manipulation: Employ optogenetic or chemogenetic approaches to selectively activate or inhibit SCN output pathways
- Output Measurement: Quantify changes in peripheral gene expression, hormone levels, and physiological parameters
Endocrine Rhythm Characterization
Protocol: Hormonal Sampling and Analysis
- Serial Blood Collection: Implement automated sampling systems or manual collection at 2-4 hour intervals across the 24-hour cycle
- Hormone Assay: Utilize ELISA or RIA for melatonin, corticosterone, and other hormones of interest
- Rhythm Analysis: Apply Cosinor analysis or similar mathematical models to determine rhythm parameters (mesor, amplitude, acrophase)
- Peripheral Clock Assessment: Measure clock gene expression rhythms (Per2::Luciferase reporters) in peripheral tissues
- Intervention Studies: Test effects of SCN lesions, timed feeding, or light exposure manipulations on endocrine rhythms
Signaling Pathway Diagrams
SCN Neural Output Pathway
SCN Neural Output Pathway: This diagram illustrates the multi-synaptic neural pathways through which the SCN regulates physiological and behavioral rhythms. The SCN projects primarily to hypothalamic nuclei (SPZ, DMH, PVN), which then relay signals to regulatory centers controlling sleep, feeding, and neuroendocrine function.
Endocrine Synchronization of Peripheral Clocks
Endocrine Synchronization Pathway: This diagram shows the endocrine pathways through which the SCN regulates melatonin and glucocorticoid secretion, which in turn synchronize peripheral clocks in tissues throughout the body. Dashed lines represent hormonal actions on peripheral tissues.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Studying SCN Output Pathways
| Reagent/Tool | Function/Application | Example Use Cases |
|---|---|---|
| Syntalos Platform | Multi-modal data acquisition and synchronization | Simultaneous recording of electrophysiology, imaging, and behavior with precise temporal alignment [21] |
| AAV Vectors | Anterograde and retrograde neural tracing | Mapping SCN neural connectivity to SPZ, DMH, and PVN targets |
| Per2::Luciferase Reporters | Real-time monitoring of circadian rhythms in tissues | Assessing peripheral clock synchronization by SCN outputs |
| Optogenetic Tools (Channelrhodopsin, Archaerhodopsin) | Cell-specific activation/inhibition of SCN neurons | Testing necessity and sufficiency of specific SCN output pathways |
| Chemogenetic Tools (DREADDs) | Remote control of neuronal activity | Chronic manipulation of SCN circuits without implanted hardware |
| ELISA/RIA Kits | Hormone quantification | Measuring circadian rhythms in melatonin, glucocorticoids |
| c-Fos Antibodies | Neural activity mapping | Identifying recently activated neurons in output regions |
| Clock Gene Antibodies | Immunohistochemistry and Western blotting | Localizing and quantifying clock protein expression |
Implications for Drug Development and Chronotherapy
Understanding SCN output pathways has profound implications for pharmaceutical development and therapeutic optimization. Chronotherapy—the timing of drug administration to align with biological rhythms—can significantly enhance efficacy and reduce adverse effects [18].
Cardiovascular Chronotherapy
The circadian regulation of cardiovascular function creates time-dependent windows of vulnerability and therapeutic opportunity:
- Morning surge in blood pressure and sympathetic tone coincides with peak incidence of myocardial infarction and stroke [18] [22]
- Coagulation factors like plasminogen activator inhibitor-1 (PAI-1) peak in the early morning, creating a prothrombotic state [18]
- Antihypertensive medications show improved efficacy when timed to target morning blood pressure surge [18]
- Antiplatelet agents may provide superior protection when aligned with circadian peaks in platelet aggregability [18]
Endocrine-Targeted Therapeutics
The endocrine outputs of the SCN provide opportunities for novel therapeutic approaches:
- Melatonin agonists (ramelteon, agomelatine) can reset circadian phase in sleep disorders and depression [6]
- Glucocorticoid receptor modulators timed to circadian rhythms may improve metabolic outcomes while minimizing side effects [6]
- REV-ERB agonists show promise for enhancing circadian amplitude and treating metabolic disorders [18]
Experimental Chronopharmacology Protocols
Protocol: Drug Timing Studies
- Rhythm Characterization: First establish circadian rhythms in target pathways (enzyme activity, receptor expression, metabolic processes)
- Dosing Time Optimization: Administer drug candidates at multiple circadian times using controlled lighting conditions
- PK/PD Analysis: Compare pharmacokinetics and pharmacodynamics across circadian phases
- Mechanistic Studies: Investigate molecular clock components regulating drug target rhythms
- Therapeutic Optimization: Identify optimal dosing schedules that align with biological rhythms for maximum efficacy and minimum toxicity
The SCN functions as the master circadian coordinator through precisely regulated neural and endocrine output pathways. These systemic synchronizers maintain temporal alignment across brain regions and peripheral organs, optimizing physiological function. Disruption of these pathways—through genetic mutations, environmental misalignment (shift work, jet lag), or aging—contributes to numerous pathological conditions.
Future research should focus on:
- Developing more sophisticated models of multi-oscillator network interactions
- Identifying novel synchronizing factors that mediate SCN-peripheral communication
- Advancing chronotherapeutic approaches for circadian-related disorders
- Exploring personalized circadian medicine based on individual circadian phenotypes
The continued elucidation of SCN output mechanisms will provide critical insights for developing novel treatments that restore circadian alignment and promote optimal health throughout the lifespan.
This whitepaper provides a comprehensive analysis of three pivotal oscillating hormone systems—melatonin, glucocorticoids, and metabolic hormones—that govern circadian rhythmicity in mammalian physiology. We examine the molecular mechanisms, regulatory functions, and interdisciplinary connections of these hormonal oscillators within the framework of endocrine regulation of circadian rhythms. The content synthesizes current research on how these hormones synchronize central and peripheral clocks, their roles in maintaining temporal homeostasis, and the pathological consequences of circadian disruption. Targeted to researchers, scientists, and drug development professionals, this review integrates foundational knowledge with emerging therapeutic strategies that target circadian biology for metabolic, neurological, and sleep-related disorders.
Circadian rhythms are endogenous 24-hour oscillations in physiology, metabolism, and behavior that persist in the absence of external cues, allowing organisms to anticipate and adapt to daily environmental changes. These rhythms are generated and maintained by a hierarchical network of molecular clocks, with the suprachiasmatic nucleus (SCN) in the hypothalamus serving as the central pacemaker that synchronizes peripheral oscillators in virtually all tissues and organs [23] [24]. The circadian system functions as a multistage processor that integrates environmental time cues (zeitgebers), primarily light-dark cycles, with internal metabolic signals to optimize the temporal organization of biological processes [23].
The molecular clockwork consists of interlocking transcription-translation feedback loops (TTFLs) involving core clock genes including CLOCK, BMAL1, PER, CRY, REV-ERB, and ROR. The CLOCK-BMAL1 heterodimer activates transcription of PER and CRY genes, whose protein products eventually repress CLOCK-BMAL1 activity, creating a approximately 24-hour oscillation [24]. This molecular oscillator regulates the rhythmic expression of thousands of genes in a tissue-specific manner, with nearly the entire primate genome showing daily rhythms in expression [24].
Endocrine systems serve as crucial mediators between the central circadian pacemaker and peripheral tissues, with several key hormones exhibiting robust circadian oscillations that coordinate physiological processes across the body. This whitpaper focuses on three fundamental oscillating hormone systems: melatonin, which conveys photic information; glucocorticoids, which integrate stress and metabolic responses; and metabolic hormones that coordinate energy homeostasis. Understanding the intricate regulation and functions of these hormonal oscillators provides critical insights for developing chronotherapeutic interventions for various disorders.
Melatonin: The Chronobiotic Regulator
Biosynthesis and Circadian Regulation
Melatonin (N-acetyl-5-methoxytryptamine) is an indoleamine hormone primarily synthesized and secreted by the pineal gland during the dark phase in both diurnal and nocturnal animals [25] [26]. Its production follows a robust circadian rhythm controlled by the SCN through a multisynaptic pathway involving the paraventricular nucleus of the hypothalamus, intermediolateral cell column of the spinal cord, and superior cervical ganglion [26]. The synthesis begins with the uptake of the essential amino acid tryptophan, which is converted to serotonin through hydroxylation and decarboxylation. The key enzymatic steps in melatonin synthesis involve N-acetylation of serotonin by arylalkylamine N-acetyltransferase (AA-NAT) followed by O-methylation by hydroxyindole-O-methyltransferase (HIOMT) [26].
Light serves as the primary environmental cue that suppresses melatonin synthesis through retinal photoreceptors, particularly melanopsin-expressing intrinsically photosensitive retinal ganglion cells (ipRGCs) that project directly to the SCN [24] [25]. The SCN relays this light information to the pineal gland, resulting in inhibition of melatonin production during daylight hours. Conversely, the absence of light input disinhibits the SCN, allowing norepinephrine release from sympathetic nerve terminals that stimulates beta-adrenergic receptors on pinealocytes, triggering a cAMP-mediated signaling cascade that activates AA-NAT and dramatically increases melatonin synthesis [26]. This light-regulated mechanism creates the characteristic diurnal rhythm of melatonin secretion, with plasma levels typically low during the day, beginning to rise around 9-10 PM, peaking between 2-4 AM, and declining toward morning [25].
Table 1: Melatonin Oscillation Characteristics
| Parameter | Characteristics | Regulating Factors |
|---|---|---|
| Daily Peak Time | 2-4 AM | Suprachiasmatic nucleus (SCN) control, darkness |
| Amplitude Range | 3-10 times nighttime vs. daytime levels | Age, retinal light exposure, pineal health |
| Phase Marker | Dim Light Melatonin Onset (DLMO) | Light exposure timing, circadian phase |
| Primary Zeitgeber | Light-dark cycle | Intensity, wavelength, duration of light exposure |
| Half-life | 20-50 minutes | Hepatic metabolism (CYP1A2, CYP2C19) |
| Secretory Pattern | Pulsatile | Sympathetic tone (norepinephrine) |
Receptor-Mediated and Non-Receptor-Mediated Mechanisms
Melatonin exerts its effects through both receptor-mediated and non-receptor-mediated mechanisms. There are two high-affinity G-protein-coupled membrane receptors identified in mammals: MT1 (Mel1a) and MT2 (Mel1b) [25] [26]. MT1 receptors primarily mediate sleep onset and vasoconstriction, while MT2 receptors are involved in phase-shifting circadian rhythms and regulating retinal and cardiovascular functions [25]. Both receptor subtypes are highly expressed in the SCN, with MT1 receptors inhibiting neuronal firing in response to melatonin and MT2 receptors mediating phase advances of circadian rhythms [23] [25]. Beyond the SCN, melatonin receptors are distributed throughout various tissues including the pituitary, retina, blood vessels, immune cells, and reproductive organs, indicating diverse physiological roles [26].
In addition to membrane receptors, melatonin acts through nuclear receptors, potentially including ROR/RZR retinoid orphan receptors, though this mechanism remains controversial [26]. Melatonin also exhibits non-receptor-mediated actions due to its amphiphilic nature, allowing it to cross cellular membranes easily and function as a broad-spectrum antioxidant and free radical scavenger [26]. It can directly neutralize reactive oxygen and nitrogen species, stimulate antioxidant enzymes (glutathione peroxidase, superoxide dismutase, catalase), and inhibit pro-oxidant enzymes, contributing to cytoprotection across various tissues [26]. Mitochondria represent a key target for melatonin's direct actions, where it helps maintain electron transport chain efficiency, reduce oxidative damage, and inhibit mitochondrial permeability transition pore opening [26].
Regulatory Functions in Sleep and Circadian Rhythms
Melatonin plays a fundamental role in regulating sleep and circadian rhythms through multiple interconnected mechanisms. As a "chronobiotic" molecule, it adjusts the timing of internal biological rhythms, primarily by phase-shifting the central circadian pacemaker in the SCN [23] [25]. Administration of melatonin during the biological day (when endogenous levels are low) typically induces phase advances, while evening administration can phase-delay rhythms, depending on the timing relative to the individual's circadian phase [25]. These phase-resetting properties form the basis for melatonin's therapeutic applications in circadian rhythm sleep disorders.
Melatonin also functions as a "hypnotic" agent that directly promotes sleep initiation and maintenance, particularly when administered during the day or in individuals with low endogenous production [23] [25]. The sleep-promoting effects emerge approximately 2 hours after intake, mirroring the physiological sequence at night, and are attributed to the attenuation of the SCN's wake-promoting signal rather than a sedative effect [23]. Functional MRI studies demonstrate that melatonin reduces activation in the precuneus region of the default mode network, correlating with increased subjective fatigue and sleep propensity [23]. This effect on brain activity patterns highlights melatonin's role in modulating neural circuits involved in arousal and consciousness.
Table 2: Research Reagent Solutions for Melatonin Studies
| Reagent/Category | Specific Examples | Research Applications |
|---|---|---|
| Receptor Agonists/Antagonists | Ramelteon (MT1/MT2 agonist), Luzindole (MT2 antagonist), S20928 (MT1 antagonist) | Receptor-specific pathway analysis, sleep architecture studies |
| Antibodies | Anti-AA-NAT, Anti-ASMT/HIOMT, Anti-MT1/MT2 receptors | Enzyme expression analysis, receptor localization, immunohistochemistry |
| ELISA/Kits | Salivary Melatonin ELISA, Plasma/Serum Melatonin RIA, Urinary 6-sulfatoxymelatonin EIA | Circadian phase assessment, rhythm amplitude measurement |
| Enzyme Inhibitors | Beta-adrenergic blockers (propranolol), cAMP pathway modulators | Melatonin synthesis pathway analysis, sympathetic regulation studies |
| Cell Lines | Pinealocyte cultures, MT1/MT2 transfected HEK293 cells | Receptor signaling studies, high-throughput screening |
| Animal Models | C57BL/6J melatonin-proficient, Pinealectomized rodents, MT1/MT2 knockout mice | In vivo rhythm studies, receptor function analysis |
Experimental Protocols for Melatonin Research
Melatonin Phase Response Curve (PRC) Determination: To establish the phase-shifting effects of melatonin, collect blood or saliva samples every 30-60 minutes under dim light conditions (<10 lux) to assess dim-light melatonin onset (DLMO) before and after melatonin administration at different circadian times. The protocol involves administering 0.5-5 mg melatonin at 6-8 different time points across the 24-hour cycle to healthy volunteers or animal subjects, with precise control of light exposure. Calculate phase shifts by comparing the timing of DLMO or other circadian markers (e.g., core body temperature minimum) before and after treatment [23] [25].
Melatonin Receptor Signaling Assay: Transfert MT1 or MT2 receptors into CHO or HEK293 cells and measure cAMP inhibition (for MT1) or phosphoinositide hydrolysis (for MT2) following melatonin stimulation. Pre-treat cells with pertussis toxin (100 ng/mL, 16-24 hours) to confirm Gi/o protein coupling. For competitive binding assays, incubate membrane preparations with [³H]-melatonin (0.1-5 nM) and increasing concentrations of test compounds for 60-120 minutes at 25-37°C, then separate bound and free ligand by rapid filtration through GF/B filters [25] [26].
Sleep Architecture Analysis with Melatonin: Administer extended-release melatonin (2 mg) or placebo to subjects (particularly aged ≥55 years) 30-60 minutes before bedtime for 4-6 weeks in a crossover design. Perform polysomnography (PSG) recordings including electroencephalography (EEG), electrooculography (EOG), and electromyography (EMG) to assess sleep latency, wake after sleep onset (WASO), total sleep time, and sleep stage distribution (N1, N2, N3, REM). Compare power spectral analysis of EEG frequencies, particularly in the delta (0.5-4 Hz) range, to evaluate sleep intensity [23] [25].
Glucocorticoids: The Stress-Responsive Oscillators
HPA Axis Dynamics and Circadian Regulation
Glucocorticoids (primarily cortisol in humans and corticosterone in rodents) are steroid hormones produced in the adrenal cortex that exhibit a robust circadian rhythm essential for metabolic homeostasis and stress adaptation [27] [28]. The secretory activity of the hypothalamic-pituitary-adrenal (HPA) axis follows a distinct 24-hour pattern characterized by a nadir around midnight, an abrupt increase 2-3 hours after sleep onset, a peak approximately at waking (around 8-9 AM), and a progressive decline throughout the day [27] [28]. This circadian rhythm originates from the interaction between the SCN and the HPA axis, with vasopressin-containing SCN neurons projecting to corticotropin-releasing hormone (CRH) neurons in the paraventricular nucleus (PVN) to impose circadian information onto HPA activity [28].
The HPA axis operates through a classic endocrine cascade: CRH released from the hypothalamus stimulates adrenocorticotropic hormone (ACTH) secretion from the anterior pituitary, which in turn triggers glucocorticoid production from the adrenal cortex [27]. Glucocorticoids exert negative feedback at multiple levels (hypothalamus, pituitary, hippocampus) to regulate their own secretion, maintaining appropriate circulating levels and preventing excessive activation [27] [29]. The circadian rhythm of glucocorticoid secretion is modulated by the sleep-wake cycle, with sleep onset potentiating the declining phase of cortisol and awakening contributing to the morning peak [28].
Molecular Mechanisms of Glucocorticoid Signaling
Glucocorticoids exert their effects primarily through the glucocorticoid receptor (GR), a ligand-activated transcription factor belonging to the nuclear hormone receptor superfamily [29]. The GR consists of several functional domains: an N-terminal transactivation domain (AF1), a central DNA-binding domain (DBD) containing two zinc fingers, and a C-terminal ligand-binding domain (LBD) with a second transactivation function (AF2) [29]. In the absence of ligand, the GR resides in the cytoplasm as part of a multiprotein complex containing heat shock proteins (Hsp90, Hsp70) and immunophilins. Upon glucocorticoid binding, the receptor undergoes conformational changes, dissociates from chaperone proteins, homodimerizes, and translocates to the nucleus where it regulates gene expression through several mechanisms [27] [29].
The classical mechanism of GR action involves direct binding to glucocorticoid response elements (GREs) in the promoter regions of target genes, leading to transactivation or transrepression depending on the sequence context and cofactor recruitment [27] [29]. Negative GREs (nGREs) mediate direct repression of gene transcription. Additionally, GR can modulate gene expression without direct DNA binding through protein-protein interactions with other transcription factors such as AP-1, NF-κB, and STATs (tethering mechanism), or by binding to composite elements together with other DNA-bound factors (composite mechanism) [29]. These diverse mechanisms allow glucocorticoids to regulate a wide range of physiological processes, with transrepression primarily mediating anti-inflammatory effects and transactivation responsible for metabolic effects [27].
Figure 1: Glucocorticoid Signaling Pathway - This diagram illustrates the HPA axis activation, glucocorticoid receptor (GR) transformation, and subsequent genomic regulation through transactivation and transrepression mechanisms.
Circadian Integration and Systemic Effects
Glucocorticoids serve as key systemic synchronizers that help coordinate circadian rhythms throughout the body. The circulating glucocorticoid rhythm not only reflects SCN control but also participates in entraining peripheral clocks in various tissues including liver, muscle, and adipose tissue [28] [29]. This synchronizing function occurs through GR-mediated regulation of core clock gene expression, particularly Per1 and Per2, in peripheral tissues. The importance of this glucocorticoid-mediated entrainment becomes evident in shift work and jet lag scenarios, where misalignment between the central SCN clock and peripheral oscillators can disrupt metabolic homeostasis [28] [24].
The metabolic effects of glucocorticoids are extensive and include stimulation of gluconeogenesis, glycogenolysis, and lipolysis while antagonizing insulin action [27]. These actions mobilize energy substrates during the active phase (wakefulness for diurnal species) to meet metabolic demands. Glucocorticoids increase blood glucose levels by promoting hepatic gluconeogenesis through induction of phosphoenolpyruvate carboxykinase (PEPCK) and glucose-6-phosphatase expression, while simultaneously decreasing glucose uptake in peripheral tissues by downregulating GLUT4 transporters [27]. In adipose tissue, glucocorticoids activate hormone-sensitive lipase (HSL), increasing free fatty acid availability for beta-oxidation [27]. Chronic glucocorticoid excess leads to characteristic metabolic alterations including muscle wasting, skin thinning, central fat redistribution (moon face, buffalo hump), and hyperglycemia [27].
Table 3: Glucocorticoid Oscillation Characteristics
| Parameter | Characteristics | Regulating Factors |
|---|---|---|
| Daily Peak Time | ~8-9 AM | SCN regulation, wake time, HPA axis activity |
| Amplitude | 5-10 times morning peak vs. nighttime nadir | Stress, sleep quality, circadian alignment |
| Nadir Timing | Between midnight-4 AM | Sleep consolidation, HPA axis quiescence |
| Primary Regulator | HPA axis | SCN input, stress, negative feedback |
| Half-life | 60-90 minutes | Hepatic metabolism, renal excretion |
| Ultradian Pattern | Pulsatile (~hourly) | Hypothalamic pulse generator |
Experimental Protocols for Glucocorticoid Research
Diurnal Cortisol Rhythm Assessment: Collect saliva or blood samples at multiple time points across the 24-hour cycle (e.g., upon waking, 30 minutes post-waking, midday, late afternoon, bedtime) for 1-2 consecutive days. For saliva sampling, instruct participants not to eat, drink, or brush teeth 30 minutes before collection. For plasma measurements, use an indwelling catheter to minimize stress from repeated venipuncture. Assay samples using ELISA, RIA, or LC-MS/MS with appropriate quality controls. Calculate the cortisol awakening response (CAR) as the difference between waking and 30-minute post-waking values, and the diurnal slope as the rate of decline from peak to nadir [27] [28].
GR Nuclear Translocation Assay: Culture cells expressing GR-GFP fusion protein in chambered coverslips. Treat with dexamethasone (100 nM) or vehicle for various durations (15 minutes to 2 hours). Fix cells with 4% paraformaldehyde, counterstain nuclei with DAPI, and visualize using confocal microscopy. Quantify nuclear translocation by calculating the ratio of nuclear to cytoplasmic fluorescence intensity using image analysis software. For higher throughput, use a cell line stably expressing GR-luciferase and measure nuclear and cytoplasmic fractions separately using a luminometer [29].
Glucocorticoid Sensitivity Testing: Isolate peripheral blood mononuclear cells (PBMCs) from fresh blood samples using density gradient centrifugation. Culture cells in RPMI 1640 medium with 10% charcoal-stripped FCS. Treat with increasing concentrations of dexamethasone (10^-10 to 10^-6 M) for 1 hour prior to stimulation with phytohemagglutinin (PHA) or lipopolysaccharide (LPS) for 24 hours. Measure lymphocyte proliferation using [³H]-thymidine incorporation or cytokine production (e.g., IL-6, TNF-α) by ELISA. Calculate IC50 values to determine glucocorticoid sensitivity [29].
Metabolic Hormones: Integrating Energy Homeostasis
Growth Hormone and Prolactin Rhythms
Growth hormone (GH) and prolactin (PRL) exhibit distinct sleep-dependent rhythms that coordinate metabolic processes and energy homeostasis. GH secretion demonstrates a strong association with slow-wave sleep (SWS), with a major secretory burst occurring approximately 90 minutes after sleep onset during the first SWS period [30]. This pulsatile release pattern is significantly diminished during sleep deprivation, indicating a crucial relationship between SWS and GH secretion [30]. The sleep-related GH surge mediates important anabolic functions including tissue repair, muscle development, and growth processes, highlighting the metabolic restoration that occurs during sleep.
Prolactin secretion follows a different pattern, characterized by increasing levels throughout the night with peak concentrations occurring during the early morning hours [30]. Unlike GH, prolactin rhythm is more closely tied to the sleep-wake cycle than to specific sleep stages, with secretion enhanced during sleep regardless of the time of day. This rhythm is regulated by complex interactions between hypothalamic dopamine (the primary prolactin-inhibiting factor), thyrotropin-releasing hormone (TRH), vasoactive intestinal peptide (VIP), and serotonin [30]. Beyond its classical role in lactation, prolactin influences various metabolic processes including pancreatic function, hepatic steatosis, and adipose tissue metabolism through receptors widely distributed in metabolic tissues [30].
Sex Steroid Oscillations
Testosterone (TT) in males exhibits a robust circadian rhythm characterized by increasing levels with prolonged sleep duration and peak levels in the early morning hours [30]. This rhythm is closely associated with REM sleep, with young men typically reaching peak levels during the first REM episode and maintaining elevated levels until awakening [30]. The tight coupling between REM sleep and testosterone secretion means that disruptions in sleep architecture, particularly reductions in REM sleep frequency or efficiency, directly impact testosterone levels. Conversely, low testosterone levels can further disrupt sleep quality, creating a potential vicious cycle characterized by increased awakenings and decreased SWS [30].
Estradiol (E2), the primary estrogen during female reproductive years, demonstrates complex relationships with sleep architecture that vary across different populations and physiological states [30]. Estrogen appears to lessen the homeostatic sleep need, potentially through its actions on the median preoptic nucleus (MnPO), a key sleep-regulatory region. E2 attenuates the action of adenosine A2A receptors on the MnPO, resulting in increased arousal episodes and significant inhibition of NREM sleep, particularly during the dark phase in diurnal species [30]. These interactions between sex steroids and sleep regulation contribute to the gender differences observed in sleep architecture and the prevalence of sleep disorders.
Thyroid Axis Rhythms
The hypothalamic-pituitary-thyroid (HPT) axis exhibits complex circadian regulation that interacts with sleep-wake processes. Thyroid-stimulating hormone (TSH) demonstrates a distinct circadian rhythm characterized by a rise prior to sleep onset, reaching peak concentrations during the night, and declining upon morning awakening [30]. This rhythm is modulated by both circadian influences and sleep itself, with sleep deprivation resulting in enhanced and prolonged TSH secretion [30]. Interestingly, different types of sleep disruption produce distinct effects on the thyroid axis—REM sleep deprivation induces central hypothyroidism with decreased TSH secretion and reduced circulating thyroxine (T4) levels, while total sleep deprivation suppresses TRH secretion [30].
The interplay between thyroid hormones and sleep regulation represents a bidirectional relationship. Thyroid hormones influence sleep architecture, with hyperthyroidism typically associated with sleep fragmentation and reduced sleep efficiency, while hypothyroidism may contribute to excessive daytime sleepiness and fatigue. Meanwhile, sleep disturbances can significantly impact thyroid axis function, potentially contributing to the metabolic consequences commonly observed in sleep disorders. These interconnected relationships highlight the importance of considering circadian and sleep-wake influences when assessing thyroid function and implementing thyroid-related therapies [30].
Table 4: Metabolic Hormone Oscillations and Sleep Relationships
| Hormone | Peak Secretion Time | Primary Sleep Relationship | Major Metabolic Functions |
|---|---|---|---|
| Growth Hormone (GH) | First SWS period (N3) | Strongly linked to slow-wave sleep | Tissue repair, muscle development, growth mediation |
| Prolactin (PRL) | Early morning hours | Sleep-dependent (not stage-specific) | Lactation, reproduction, energy metabolism |
| Testosterone (TT) | Early morning | Associated with REM sleep | Sperm production, sexual characteristics, muscle mass |
| Thyroid-Stimulating Hormone (TSH) | During night | Rise before sleep, decline after awakening | Metabolism, thermogenesis, growth, development |
| Follicle-Stimulating Hormone (FSH) | Varies by cycle | Positive correlation with sleep duration | Follicular growth, estrogen production, sperm production |
Interdisciplinary Connections and Therapeutic Implications
Bidirectional Relationships Between Sleep and Hormonal Systems
The relationships between sleep and hormonal systems are fundamentally bidirectional, with sleep architecture influencing hormonal secretion patterns and hormones reciprocally modulating sleep structure and quality. The HPA axis exemplifies this bidirectional relationship—sleep deprivation, sleep disruption, and circadian misalignment activate the HPA axis, leading to elevated cortisol levels that can further disrupt sleep architecture [28] [30]. This creates a potential vicious cycle wherein sleep loss begets HPA dysregulation which in turn perpetuates poor sleep. Specifically, sleep restriction to 4 hours per night for 6 consecutive nights results in increased cortisol levels in the afternoon and early evening, with a delayed onset of the quiescent period by approximately 1.5 hours [28].
Different sleep stages exert distinct influences on hormonal secretion. Slow-wave sleep (SWS) is associated with inhibition of thyroid-stimulating hormone (TSH) secretion, activation of the vagus nerve, promotion of growth hormone (GH) release, and reduction of cortisol levels, collectively contributing to improved glucose metabolism [30]. In contrast, REM sleep regulates testosterone secretion rhythms and activates the sympathetic nervous system, resulting in elevated blood pressure, disrupted insulin secretion, and increased diabetes risk [30]. The proportional distribution of sleep stages throughout the night therefore creates a complex temporal pattern of hormonal regulation that optimizes metabolic functioning when properly aligned with circadian phase.
Metabolic Consequences of Circadian Disruption
Circadian disruption, whether from shift work, jet lag, social jet lag, or genetic alterations in clock components, produces significant metabolic consequences that increase disease risk. Modern society poses two primary types of circadian challenge: extended light exposure at night that suppresses melatonin and delays sleep onset, and early waking demands that reduce sleep duration [24]. This misalignment between endogenous circadian rhythms and behavioral cycles disrupts the temporal coordination of metabolic processes, leading to impaired glucose tolerance, decreased insulin sensitivity, dyslipidemia, and increased adiposity [28] [24] [30].
The mechanisms underlying these metabolic consequences involve dysregulation across multiple hormonal systems. Circadian misalignment alters the normal rhythmicity of cortisol secretion, with shifted sleep-wake cycles causing profound disruptions in the 24-hour cortisol rhythm characterized by higher nadir values and altered acrophase timing [28]. Similarly, melatonin secretion is suppressed by light exposure at night, eliminating its important regulatory effects on insulin secretion and glucose metabolism [23] [26]. These hormonal disturbances, combined with mistimed feeding behavior, create a metabolic environment conducive to the development of obesity, metabolic syndrome, and type 2 diabetes [28] [24] [30].
Figure 2: Circadian Disruption Pathway - This diagram illustrates how modern lifestyle factors disrupt circadian rhythms, leading to hormonal dysregulation and increased metabolic disease risk through multiple interconnected pathways.
Chronotherapeutic Approaches
Chronotherapy represents a promising approach for optimizing treatment outcomes by aligning therapeutic interventions with biological rhythms. For circadian rhythm sleep disorders, strategically timed melatonin administration can help reset the central pacemaker and realign sleep-wake cycles with desired schedules [23] [25]. The phase-shifting effects of melatonin follow a phase-response curve (PRC) wherein administration during the biological afternoon/evening produces phase advances, while administration during the biological night/early morning causes phase delays [25]. This principle can be applied therapeutically for conditions like delayed sleep phase syndrome (advancing evening melatonin) or advanced sleep phase syndrome (delaying early morning melatonin).
The timing of medication administration for endocrine and metabolic disorders can significantly impact both efficacy and side effect profiles. For glucocorticoid therapies, morning administration typically produces less HPA axis suppression than evening dosing, as it more closely mimics the physiological cortisol rhythm [27] [29]. Similarly, the metabolic effects of many medications vary according to circadian timing—statins are often more effective when taken in the evening due to the nocturnal peak in cholesterol synthesis, while certain antihypertensive medications may be more beneficial when taken at bedtime [24]. These chronotherapeutic principles highlight the importance of considering biological timing in treatment regimen design.
The oscillating hormones melatonin, glucocorticoids, and metabolic hormones form an integrated network that coordinates circadian physiology and maintains metabolic homeostasis. These hormonal systems function as both outputs of the central circadian pacemaker and as regulatory inputs that fine-tune peripheral clocks throughout the body. Their complex interactions create a temporal organization of physiological processes that optimizes energy utilization, repair mechanisms, and adaptive responses to environmental challenges. Disruption of these hormonal oscillations through modern lifestyle factors, sleep disorders, or circadian misalignment contributes significantly to the pathogenesis of metabolic, cardiovascular, and neuropsychiatric disorders.
Future research directions should focus on elucidating the precise molecular mechanisms through which these hormonal oscillators regulate circadian gene expression in target tissues, developing more targeted chronotherapeutic interventions with improved specificity and reduced side effects, and exploring personalized chronomedicine approaches that account for individual differences in circadian phase and hormonal sensitivity. A deeper understanding of how these key oscillating hormones coordinate circadian rhythms will provide critical insights for preventing and treating the numerous disorders associated with circadian disruption in our increasingly 24-hour society.
The endocrine system and circadian clocks engage in a complex, bidirectional dialogue that is fundamental to temporal physiology. Hormones function as key zeitgebers (time-givers), internal time cues that synchronize and shape circadian rhythms through distinct mechanistic roles: as phasic drivers of physiological outputs, as resetters of molecular clock phase, and as tonic tuners of rhythmic amplitude and precision. This review dissects these roles through the lens of specific endocrine factors—melatonin, glucocorticoids, and thyroid hormones—detailing their mechanisms of action, presenting quantitative physiological data, and providing experimental protocols for their study. Understanding these hierarchical interactions provides a framework for developing chronotherapeutic strategies for metabolic, psychiatric, and sleep disorders.
The mammalian circadian system is organized hierarchically, with a master pacemaker in the suprachiasmatic nucleus (SCN) coordinating peripheral clocks in virtually every tissue and cell [6] [31]. This coordination ensures that physiological processes—from sleep-wake cycles to metabolism—are optimally timed with the 24-hour solar day. The molecular clockwork consists of interlocked transcriptional-translational feedback loops (TTFLs) driven by core clock genes (e.g., CLOCK, BMAL1, PER, CRY) [31] [32].
While the SCN is primarily entrained by light, peripheral clocks respond strongly to non-photic cues, with endocrine signals representing a primary mechanism for system-wide synchronization [6] [33]. Hormones exhibit robust circadian oscillations and can influence circadian timing through multiple conceptual frameworks: (1) as phasic drivers, where their rhythmic secretion directly drives rhythmic physiological processes without altering the core clock; (2) as clock resetters (zeitgebers proper), where they phase-shift the molecular TTFL; and (3) as rhythm tuners, where their tonic levels modulate the amplitude or robustness of circadian outputs without necessarily altering phase [6]. This review systematically examines these roles through specific endocrine examples, providing mechanistic insights and methodological approaches for researchers.
Conceptual Framework: Three Modes of Hormonal Regulation
Phasic Drivers of Physiological Rhythms
A hormone acts as a phasic driver when its own rhythmic production and secretion directly creates rhythmicity in downstream physiological processes. This effect is independent of the core clock machinery in target tissues and instead relies on direct hormone-receptor interactions activating rhythmic gene expression programs. The classic example is glucocorticoid secretion, which, through its receptor binding to glucocorticoid response elements (GREs) in target genes, drives daily rhythms in glucose metabolism, immune function, and cardiovascular tone [6].
Clock Resetters (Zeitgebers)
Hormones function as resetters when they directly interact with components of the molecular TTFL to alter its phase. This requires that the hormone receptor signaling pathway converges on clock gene regulatory elements (e.g., E-boxes, D-boxes). Melatonin exemplifies this role, capable of phase-advancing or delaying SCN neuronal activity and peripheral clock gene expression through MT1/MT2 receptor-mediated signaling that ultimately affects PER transcription [6] [34].
Rhythm Tuners
The most recently characterized role, tuning, refers to hormones that modulate the amplitude or robustness of circadian output rhythms without drastically altering the phase or period of the core oscillator. This often involves more chronic, tonic signaling that sets the sensitivity of tissues to other circadian signals. Thyroid hormones have been proposed to act as tuners in the liver, where they modulate the amplitude of circadian gene expression without resetting the core clock [6].
Table 1: Conceptual Framework of Hormonal Zeitgeber Roles
| Role | Mechanism | Temporal Profile | Key Example |
|---|---|---|---|
| Phasic Driver | Direct hormone-target interaction via response elements | Rhythmic (phasic) | Glucocorticoids via GREs |
| Clock Resetter | Alters phase/period of TTFL via clock gene elements | Rhythmic (phasic) | Melatonin via E-box regulation |
| Rhythm Tuner | Modulates amplitude of output rhythms without core clock reset | Tonic (non-rhythmic) | Thyroid hormones in liver |
Melatonin: A Master Circadian Resetter and Seasonal Timer
Rhythmic Secretion and Light-Dependent Regulation
Melatonin synthesis in the pineal gland is strictly controlled by the SCN, which integrates light information from the retina. Secretion is confined to the dark phase, with peak levels occurring at night in both diurnal and nocturnal species [6] [35]. This robust rhythm makes melatonin a reliable internal time cue for the entire organism.
Molecular and Signaling Pathways
Melatonin exerts its resetting effects primarily through two G-protein-coupled receptors, MT1 and MT2. Their activation triggers several intracellular signaling cascades, including:
- Inhibition of adenylyl cyclase and reduction of cAMP
- Activation of protein kinase C (PKC)
- Modulation of ion channel activity
- In the SCN, MT1 receptor activation reduces GABAergic neuronal firing, while MT2 receptor activation phase-shifts circadian rhythmicity through PKC-mediated regulation of PER expression [6].
The seasonal timing (photoperiodic) function of melatonin deserves special attention. In the pars tuberalis (PT) of the pituitary, the duration of the nocturnal melatonin signal acts as a proxy for day length. This signal is decoded through a molecular coincidence timer involving circadian genes. Long photoperiods induce the circadian transcription factor BMAL2, which triggers summer biology through the EYA3/TSH pathway. Conversely, long-duration melatonin signals on short photoperiods induce circadian repressors like DEC1, suppressing this pathway and triggering winter biology [34]. This mechanism involves progressive genome-wide changes in chromatin state (e.g., H3K4me3 marks), elaborating the effect of the circadian coincidence timer [34].
Figure 1: Melatonin Signaling and Circadian Reset Mechanism. Light information reaches the SCN via the retinohypothalamic tract (RHT), which regulates melatonin synthesis in the pineal gland via a multisynaptic sympathetic pathway. Melatonin binding to MT1/MT2 receptors modulates intracellular cAMP and PKC signaling, ultimately altering clock gene expression and producing a phase shift in the transcriptional-translational feedback loop (TTFL).
Experimental Protocol: Assessing Melatonin's Resetting Capacity
Objective: To determine the phase-shifting effects of melatonin on the circadian clock in vivo and in vitro.
In Vivo Wheel-Running Assay in Nocturnal Rodents:
- Animal Housing: House mice (C57BL/6J) or Syrian hamsters individually in cages equipped with running wheels.
- Baseline Recording: Maintain animals in constant darkness (DD) for at least 10 days to establish a stable free-running rhythm of locomotor activity.
- Melatonin Administration: At a predetermined circadian time (CT; where CT12 is activity onset), subcutaneously inject melatonin (0.5-5 mg/kg in saline with 1% ethanol) or vehicle.
- Data Analysis: Plot actograms and calculate the phase shift by comparing the regression line of activity onset for 7-10 days pre- and post-injection.
In Vitro Phase-Shift in SCN Slice Cultures:
- SCN Explant Preparation: Prepare 300-400 μm thick coronal hypothalamic slices from PER2::LUCIFERASE reporter mice during the day (ZT 4-6).
- Culture and Recording: Culture slices on membrane inserts and record bioluminescence rhythm in real-time for several days.
- Treatment: Apply melatonin (100 nM-1 μM) or vehicle to the culture medium at different circadian times.
- Phase Analysis: Determine the peak time of the PER2::LUC rhythm before and after treatment to quantify the phase shift.
Table 2: Quantitative Data on Melatonin Rhythms and Effects
| Parameter | Species | Value/Range | Conditions | Citation |
|---|---|---|---|---|
| Peak Secretion Time | Human | 01:00 - 04:00 | Nocturnal, in darkness | [35] |
| Circulating Concentration (Peak) | Human | 60-200 pg/mL | Nocturnal, in darkness | [35] |
| Phase Advance Capacity | Human | Up to 60-90 minutes | Timed evening administration | [6] |
| EC50 for MT2 Receptor | In vitro | ~160 pM | Cell-based assay | [6] |
Glucocorticoids: Dual Roles as Phasic Drivers and Clock Resetters
Complex Regulation of Rhythmic Secretion
Glucocorticoids (cortisol in humans, corticosterone in rodents) exhibit a robust circadian rhythm with a peak around the onset of the active phase (morning in humans, evening in rodents). This rhythm is governed by three interconnected mechanisms:
- SCN Control of HPA Axis: The SCN provides rhythmic vasopressinergic and glutamatergic input to the paraventricular nucleus (PVN), driving corticotropin-releasing hormone (CRH) and arginine vasopressin (AVP) release, which subsequently stimulate pituitary ACTH secretion [6].
- Adrenal Innervation: The SCN also transmits timing signals via the autonomic nervous system (splanchnic nerve) to the adrenal cortex, modulating its sensitivity to ACTH [6] [35].
- Local Adrenal Clock: The intrinsic circadian clock in the adrenal cortex gates glucocorticoid production by rhythmically regulating the expression of steroidogenic enzymes and the response to ACTH [6] [35]. Superimposed on the circadian rhythm is an ultradian rhythm of approximately 90-minute pulses, whose physiological significance is increasingly recognized [6].
Molecular Mechanisms of Action
Glucocorticoids exert their effects through two nuclear receptors: the high-affinity mineralocorticoid receptor (MR) and the lower-affinity glucocorticoid receptor (GR). The GR mediates most phasic circadian effects and functions as both a driver and resetter through distinct mechanisms:
- As a Phasic Driver: GR binding to glucocorticoid response elements (GREs) directly drives the rhythmic transcription of numerous metabolic and immune genes [6].
- As a Clock Resetter: Several clock genes, including Per1 and Per2, contain GREs in their regulatory regions. Glucocorticoid activation can directly reset peripheral clocks by inducing Per expression [6]. This is particularly evident in the liver, where glucocorticoid administration can rapidly shift the phase of circadian gene expression.
Figure 2: Glucocorticoid Regulation and Signaling. The SCN regulates glucocorticoid (GC) secretion through the HPA axis (PVN → Pituitary → ACTH) and via direct autonomic innervation of the adrenal. Circulating GCs bind to the glucocorticoid receptor (GR), which translocates to the nucleus and binds glucocorticoid response elements (GREs) to act as a phasic driver of metabolic genes or as a clock resetter when GREs are located in clock gene promoters.
Experimental Protocol: Dissecting Driver vs. Resetter Functions
Objective: To determine whether a metabolic effect of glucocorticoids is mediated through direct driver activity or indirect clock resetting.
Chromatin Immunoprecipitation (ChIP) Assay:
- Cell/Tissue Treatment: Treat synchronized hepatocytes or adrenal cells with dexamethasone (100 nM) or vehicle at two different circadian times (e.g., CT6 and CT18).
- Cross-linking and Shearing: At 1-hour post-treatment, cross-link proteins to DNA with formaldehyde. Lyse cells and sonicate chromatin to shear DNA to 200-500 bp fragments.
- Immunoprecipitation: Incubate chromatin with antibody against GR or control IgG. Capture antibody-DNA complexes.
- qPCR Analysis: Analyze immunoprecipitated DNA by qPCR using primers for:
- Known GREs in metabolic genes (e.g., PEPCK)
- GREs in clock gene promoters (e.g., Per1, Per2)
- Control genomic regions without GREs
Interpretation: Time-dependent GR binding to metabolic gene GREs indicates phasic driver function. GR binding to clock gene GREs supports a resetter role, especially if binding patterns differ by circadian time.
The Scientist's Toolkit: Key Research Reagents and Models
Table 3: Essential Research Reagents for Studying Endocrine Zeitgebers
| Reagent / Model | Category | Key Application | Example Use |
|---|---|---|---|
| PER2::LUCIFERASE | Reporter Mouse | Real-time clock phase monitoring | Tracking phase shifts in SCN/explant cultures [6] |
| Corticosterone ELISA | Assay Kit | Quantifying glucocorticoid levels | Measuring circadian hormone profiles in serum [33] |
| MT1/MT2 Agonists/Antagonists | Pharmacological Tools | Dissecting melatonin receptor function | Determining receptor-specific phase-shifting effects [6] |
| ChIP-grade GR Antibody | Research Antibody | Mapping GR-DNA interactions | Identifying direct GR targets in driver vs. resetter roles [6] |
| siRNA/shRNA for Clock Genes | Gene Knockdown | Functional analysis of clock components | Testing necessity of specific genes in hormone signaling [36] |
| Adrenalectomized (ADX) Rodents | Animal Model | Studying glucocorticoid-independent rhythms | Isolating direct vs. GC-mediated circadian effects [6] |
| uORF-Mutant Drosophila | Genetic Model | Studying translational clock regulation | Investigating post-transcriptional control of CLOCK [37] |
Emerging Concepts and Therapeutic Implications
Post-Translational and Epigenetic Regulation
Beyond transcriptional control, recent research highlights the importance of post-translational and epigenetic mechanisms in hormone-clock interactions. For example, upstream open reading frames (uORFs) in the Clock mRNA rhythmically attenuate CLK protein translation in Drosophila, with uORF deletion leading to shortened circadian periods and altered sleep patterns [37]. This represents a novel layer of regulation where hormonal signals might interact with translational control mechanisms to fine-tune circadian outputs.
Histone modifications also play a critical role. In the pars tuberalis, photoperiod-driven changes in melatonin duration induce genome-wide alterations in H3K4me3 marks, associated with seasonal changes in chromatin accessibility and gene expression [34]. This epigenetic remodeling represents a mechanism for long-term hormonal timing information storage.
Chronodisruption and Disease
Misalignment between hormonal rhythms and behavioral cycles (e.g., during shift work) disrupts circadian coordination, promoting metabolic disease, mood disorders, and cancer [33] [31] [32]. Experimental zeitgeber desynchrony (ZD) paradigms in mice, where light-dark cycles and feeding-fasting cycles are out of phase, demonstrate tissue-specific dissociation of peripheral clocks from the SCN, with associated metabolic dysfunction [33]. These models provide insight into the pathophysiology of shift work disorders and suggest that realigning hormonal rhythms may offer therapeutic benefit.
Chronotherapeutic Opportunities
Understanding hormonal zeitgeber mechanisms opens avenues for timed interventions (chronotherapeutics). Potential strategies include:
- Timed Hormone Administration: Using melatonin or synthetic analogs to reset circadian phase in shift workers or jet lag patients.
- Timed Corticosteroid Therapy: Aligning glucocorticoid administration with the endogenous peak to minimize metabolic side effects.
- Hormone Receptor-Targeted Drugs: Developing specific receptor modulators that selectively enhance or suppress particular zeitgeber functions.
The endocrine system regulates circadian physiology through a sophisticated division of labor, with hormones acting as phasic drivers, clock resetters, and rhythm tuners. These roles are mediated through distinct molecular mechanisms—from direct transcriptional activation to epigenetic remodeling—that operate across different timescales. Future research should focus on developing more precise tools to dissect these mechanisms, particularly in human models, and translating this knowledge into chronotherapeutic strategies that restore circadian harmony in various disease states. The integration of hormonal timing signals into a coherent physiological output represents a fundamental principle of temporal biology with far-reaching implications for human health and disease management.
Advanced Tools and Models: Monitoring Rhythms and Informing Drug Discovery
Circadian rhythms are intrinsic 24-hour biological cycles that govern numerous physiological processes, from sleep-wake patterns to metabolic homeostasis. The endocrine system plays a pivotal role in regulating these rhythms, with cortisol and melatonin serving as key hormonal mediators. The suprachiasmatic nucleus (SCN) in the hypothalamus acts as the master pacemaker, synchronizing peripheral clocks throughout the body via neuronal and endocrine pathways [6] [38]. This synchronization ensures temporal coordination of physiological functions, enabling organisms to anticipate and adapt to daily environmental changes.
The molecular architecture of the circadian clock consists of interlocking transcription-translation feedback loops. The core loop involves CLOCK and BMAL1 proteins forming heterodimers that activate transcription of Period (Per) and Cryptochrome (Cry) genes. PER and CRY proteins then accumulate and suppress CLOCK:BMAL1 activity, completing the negative feedback cycle [38]. An auxiliary loop involves REV-ERB and ROR proteins that competitively bind to ROR response elements on the Bmal1 promoter, providing additional regulatory precision. This molecular oscillator generates rhythmic gene expression that governs endocrine secretion patterns.
Within this framework, cortisol and melatonin emerge as crucial hormonal outputs and regulators of circadian timing. Melatonin, produced by the pineal gland, exhibits nocturnal secretion patterns that are directly inhibited by light exposure via the retinohypothalamic tract [6]. Cortisol, secreted by the adrenal cortex, follows a diurnal rhythm with peak levels around awakening that decline throughout the day [6] [39]. Both hormones serve as hands of the circadian clock, translating central timing signals into peripheral physiological responses, while also providing feedback regulation to fine-tune circadian phase and amplitude.
Current Biomarker Detection Methods and Methodological Challenges
Traditional approaches for monitoring cortisol and melatonin rhythms have relied on invasive or discontinuous sampling methods. Blood serum measurements provide the gold standard for hormone quantification but are unsuitable for frequent sampling due to their invasive nature. Salivary sampling offers a less invasive alternative and correlates well with free hormone concentrations in blood, but requires strict protocol adherence regarding sampling time and contamination risks [39]. Urinary measurements integrate hormone secretion over several hours but cannot capture rapid fluctuations, while hair cortisol analysis reflects chronic exposure over months but lacks temporal resolution for circadian assessment [39].
Each biofluid presents distinct advantages and limitations for hormone monitoring, as summarized in Table 1. These methodological constraints have historically impeded comprehensive understanding of circadian hormone dynamics, particularly the ultradian (hourly) pulsatility that characterizes cortisol secretion and the precise onset timing of melatonin secretion.
Table 1: Comparison of Biofluids for Cortisol and Melatonin Monitoring
| Biofluid | Analytes Detected | Temporal Resolution | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Blood Serum | Total cortisol, melatonin | Point measurement | Gold standard quantification, high accuracy | Invasive, requires clinical setting, discontinuous |
| Saliva | Free cortisol, melatonin | 15-30 min resolution | Non-invasive, correlates with free hormone levels | Sensitive to collection protocol, contamination risk |
| Urine | Cortisol metabolites, 6-sulfatoxymelatonin | 4-12 hour integrated | Non-invasive, integrated measure | Poor temporal resolution, influenced by renal function |
| Sweat | Cortisol, melatonin | Continuous (minutes) | Continuous monitoring, non-invasive | Low analyte concentration, variable secretion rates |
| Interstitial Fluid | Cortisol (theoretical) | Continuous (minutes) | Continuous monitoring, good correlation with blood | Requires microneedles, validation ongoing |
The emergence of non-invasive biosensing technologies addresses critical limitations of conventional methods by enabling continuous, real-time monitoring of hormonal fluctuations. These platforms facilitate collection of high-density temporal data essential for characterizing circadian phase, amplitude, and ultradian pulsatility under real-world conditions [40] [41]. Furthermore, they minimize interference with natural sleep-wake patterns and hormone secretion, thereby providing more ecologically valid assessments of circadian function.
Innovative Biosensing Platforms for Continuous Hormone Monitoring
Sweat-Based Wearable Sensors
Recent technological advances have established passive perspiration as a viable biofluid for continuous hormone monitoring. The CIRCA study (Circadian inference of rhythmicity using comparative analysis) demonstrated a wearable sensor for simultaneous measurement of cortisol and melatonin in sweat [42] [43]. This platform utilizes a skin-conformal microfluidic system that interfaces with eccrine sweat glands via capillary action, continuously wicking minute volumes of perspiration (0.5-5 µL/min) to embedded sensing electrodes [41].
The sensing mechanism employs electrochemical detection with molecularly imprinted polymers (MIPs) or aptamer-based receptors that provide high specificity despite the complex sweat matrix [40]. For cortisol detection, anti-cortisol antibodies immobilized on working electrodes generate current signals proportional to hormone concentration through competitive immunoassays. Similarly, melatonin detection utilizes electrophymerized MIPs with cavities complementary to melatonin's molecular structure, enabling selective recognition amid structurally similar tryptophan metabolites [40].
Validation against established salivary measures demonstrated strong correlations for both cortisol (Pearson r = 0.92) and melatonin (r = 0.90) [42]. Bland-Altman analysis further confirmed matrix agreement with mean bias close to zero and narrow limits of agreement (-6.09 to 5.94 ng/mL for cortisol; -7.54 to 10.77 pg/mL for melatonin) [42]. This analytical performance supports sweat as a valid alternative to saliva for endocrine monitoring while offering superior temporal resolution through continuous sampling.
Microfluidic Integration and Autonomous Operation
Capillary microfluidics enables autonomous, power-free operation of wearable hormone sensors through engineered wettability and channel geometries [41]. These systems employ hydrophilic microchannels that passively transport sweat from skin interfaces to sensing reservoirs via capillary forces, eliminating the need for mechanical pumps. Multilayer architectures incorporate burst valves and evaporative disposal regions that manage flow sequencing and prevent backflow contamination [41].
Advanced implementations feature chrono-sampling designs that compartmentalize sequential samples for discrete analysis, enabling reconstruction of concentration profiles while minimizing carryover effects [41]. Transduction modalities include electrochemical systems with flexible working electrodes (carbon, gold, or graphene-based) that detect hormone-induced current or potential changes, and optical systems that measure colorimetric or fluorescence signals from hormone-sensitive dyes [40] [41].
Sensor calibration presents significant challenges due to inter-individual variations in sweat rates, pH, and electrolyte composition. Innovative approaches incorporate internal standards such as conductivity measurements that normalize hormone concentrations to sweat extraction rates [40]. Some platforms implement multi-analyte capability by integrating separate sensing channels for cortisol, melatonin, and reference biomarkers (e.g., sodium, chloride), enhancing measurement reliability under dynamic physiological conditions [41].
Experimental Protocols and Analytical Frameworks
Sensor Fabrication and Characterization Protocol
The development of non-invasive biosensors for cortisol and melatonin monitoring follows a rigorous fabrication and validation workflow:
Electrode Fabrication: Pattern flexible electrodes (typically gold or carbon) onto polyethylene terephthalate (PET) substrates using screen printing or vapor deposition techniques. Functionalize working electrodes with cortisol/melatonin capture elements (antibodies, aptamers, or MIPs) through covalent coupling using crosslinkers like EDC-NHS [40].
Microfluidic Integration: Bond polydimethylsiloxane (PDMS) microchannels to electrode substrates using oxygen plasma treatment. Hydrophilic surface treatment ensures spontaneous capillary flow. Incorporate cellulose membranes or hydrogel interfaces at skin contact points to enhance wicking efficiency [41].
Electrochemical Characterization: Perform cyclic voltammetry in standard solutions (e.g., potassium ferricyanide) to verify electrode functionality. Calibrate sensors in synthetic sweat matrix with hormone concentrations spanning physiological ranges (cortisol: 1-50 ng/mL; melatonin: 1-100 pg/mL) [42] [40].
Selectivity Testing: Evaluate cross-reactivity against structurally similar compounds (cortisone for cortisol; tryptophan, serotonin for melatonin) using solutions with 10-fold higher concentrations of potential interferents [40].
On-Body Validation: Conduct controlled studies with simultaneous sweat and saliva collection across circadian cycles. Sample saliva at 60-minute intervals while continuously collecting sweat. Correlate temporal profiles using cosinor analysis or similar rhythmicity algorithms [42].
Circadian Rhythm Analysis Using CircaCompare
The CIRCA study employed CircaCompare, a robust statistical framework implemented in R, to characterize circadian parameters from continuous hormone data [42]. The analytical protocol includes:
Data Preprocessing: Normalize raw sensor signals using internal standards (e.g., conductivity). Remove motion artifacts using wavelet transformation or median filtering. Align data timestamps to dim light melatonin onset (DLMO) or wake time for phase referencing.
Rhythm Parameterization: Fit cosine functions with 24-hour period to hormone concentration time series:
Y(t) = M + Acos(2πt/τ + φ) + ε, where M is mesor (mean level), A is amplitude (peak-trough difference), φ is acrophase (peak time), and ε represents residuals [42].Group Comparisons: Implement CircaCompare's differential rhythmicity analysis to test for significant differences in mesor, amplitude, and phase between demographic groups (e.g., age, sex) or experimental conditions. This method uses nonlinear mixed-effects models to account within-subject correlations across sampling intervals [42].
Phase Relationship Assessment: Calculate cross-correlation functions between cortisol and melatonin rhythms within individuals. Determine phase angle differences between hormone peaks relative to sleep onset or wake time.
Statistical Validation: Apply false discovery rate correction for multiple comparisons. Report effect sizes with 95% confidence intervals for rhythm parameter differences between groups.
Table 2: Representative Circadian Parameters for Cortisol and Melatonin from Continuous Sweat Monitoring
| Parameter | Young Adults (18-30) | Older Adults (50-70) | Sex Differences | Measurement Units |
|---|---|---|---|---|
| Cortisol Acrophase | 08:15 ± 30 min | 07:45 ± 40 min | Males: 08:00 ± 35 min Females: 08:30 ± 25 min | Time of day (hh:mm) |
| Cortisol Amplitude | 8.5 ± 2.1 ng/mL | 5.2 ± 1.8 ng/mL | Males: 7.8 ± 2.3 ng/mL Females: 9.1 ± 1.9 ng/mL | Concentration (ng/mL) |
| Melatonin Acrophase | 02:30 ± 25 min | 01:45 ± 35 min | Males: 02:15 ± 30 min Females: 02:45 ± 20 min | Time of day (hh:mm) |
| Melatonin Amplitude | 12.3 ± 3.2 pg/mL | 7.8 ± 2.5 pg/mL | Males: 10.9 ± 3.1 pg/mL Females: 13.6 ± 2.8 pg/mL | Concentration (pg/mL) |
| Cortisol-Melatonin Phase Angle | 5.75 ± 0.8 hours | 6.0 ± 1.1 hours | Males: 5.8 ± 0.9 hours Females: 5.7 ± 0.7 hours | Duration (hours) |
Note: Data synthesized from CIRCA study findings [42]. Phase angle represents time difference between cortisol peak and melatonin peak.
Signaling Pathways and Hormonal Regulation of Circadian Rhythms
The endocrine regulation of circadian rhythms involves complex interactions between hormonal signaling and molecular clock mechanisms. Cortisol and melatonin exert complementary effects on peripheral clocks through distinct receptor-mediated pathways, as illustrated in Figure 1.
Figure 1: Endocrine Regulation of Circadian Rhythms. The suprachiasmatic nucleus (SCN) coordinates hormonal signals through neural pathways to the pineal gland (melatonin) and adrenal cortex (cortisol). These hormones feedback on peripheral clocks via specific receptors to regulate clock gene expression and physiological outputs.
Melatonin synchronizes circadian rhythms through G protein-coupled MT1 and MT2 receptors that modulate multiple signaling cascades. MT1 receptor activation inhibits adenylate cyclase and reduces cAMP formation, while MT2 receptor coupling affects protein kinase C and cGMP pathways [6]. In the SCN, melatonin phase-shifts neuronal firing rhythms and reduces light-induced phase shifts, thereby stabilizing the master clock. In peripheral tissues, melatonin receptor signaling influences the expression of core clock genes, particularly by enhancing Per1 and Cry1 transcription, which reinforces circadian phase alignment [6].
Cortisol exerts widespread effects on circadian gene regulation through glucocorticoid receptors (GR) that function as ligand-activated transcription factors. Upon cortisol binding, GR translocates to the nucleus and binds glucocorticoid response elements (GREs) in regulatory regions of target genes, including core clock components [6]. Notably, the Per1 and Per2 genes contain functional GREs, allowing cortisol to directly reset peripheral clocks [6]. This mechanism enables cortisol to synchronize metabolic and immune functions with the central SCN rhythm, particularly in liver, muscle, and adipose tissue.
The interplay between cortisol and melatonin creates a coordinated temporal framework that aligns physiological processes with the light-dark cycle. Melatonin promotes sleep-related functions during the biological night, while cortisol facilitates awakening and activity readiness during the biological day. Disruption of this balance, as occurs in shift work or chronic stress, degrades circadian amplitude and perturbs metabolic, immune, and cognitive processes [44] [45].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Circadian Hormone Biosensing
| Reagent/Category | Specific Examples | Research Function | Technical Considerations |
|---|---|---|---|
| Molecular Recognition Elements | Anti-cortisol monoclonal antibodies, Melatonin aptamers, Molecularly imprinted polymers (MIPs) | Target capture and specificity | Cross-reactivity testing required; MIPs offer superior stability over antibodies |
| Electrode Materials | Screen-printed carbon electrodes, Gold nanowires, Graphene oxide composites | Signal transduction platform | Flexible substrates enable wearability; Nanomaterials enhance sensitivity |
| Microfluidic Components | PDMS channels, Hydrogel interfaces, Cellulose membranes, Burst valves | Autonomous fluid handling | Hydrophilic coatings ensure capillary flow; Evaporative regions prevent backflow |
| Electrochemical Mediators | Ferrocene derivatives, Prussian blue, Methylen blue | Signal amplification | Reversibility essential for continuous monitoring; Must be biocompatible |
| Calibration Standards | Synthetic sweat formulations, Certified reference materials | Sensor calibration and validation | Must match ionic composition of native biofluid; Include pH buffers |
| Data Analysis Tools | CircaCompare R package, Cosinor analysis, Lomb-Scargle periodogram | Circadian parameter estimation | Handles unequally spaced time series; Provides confidence intervals for rhythm parameters |
Applications in Chronotherapy and Circadian Medicine
Continuous hormone monitoring enables personalized chronotherapy approaches that optimize treatment timing according to individual circadian rhythms. In oncology, coordinating chemotherapy with circadian cycles has demonstrated reduced toxicity and improved efficacy in clinical trials [38]. Wearable hormone sensors provide objective data for identifying optimal treatment windows based on individual cortisol rhythms rather than population averages.
In psychiatric disorders, circadian disruption represents a core feature of conditions like major depressive disorder and bipolar disorder [45]. Continuous melatonin monitoring facilitates precise assessment of dim light melatonin onset (DLMO), a key marker of circadian phase that guides light therapy and melatonin supplementation for mood disorders [45]. Similarly, cortisol rhythm assessment identifies HPA axis dysregulation in burnout and stress-related disorders, enabling targeted interventions [45].
The integration of continuous hormone data with other physiological metrics (sleep, activity, heart rate variability) through multimodal sensing platforms provides comprehensive circadian phenotyping. This approach supports early detection of circadian disruption before manifest pathology develops, creating opportunities for preventive interventions. Machine learning algorithms applied to these rich longitudinal datasets can identify subtle rhythm alterations that predict disease susceptibility or treatment response [40].
Non-invasive biosensing of cortisol and melatonin represents a transformative approach for circadian endocrine research. Sweat-based wearable platforms address critical limitations of conventional methods by enabling continuous, real-time hormone monitoring in ecological settings. The strong correlation between sweat and saliva matrices (r = 0.90-0.92) validates this methodology for circadian rhythm assessment while providing superior temporal resolution [42].
Future developments will focus on enhancing sensor longevity through improved antifouling materials and regeneration protocols. Multi-analyte capability expansion to include metabolic markers (glucose, lactate) and inflammatory cytokines will provide systems-level insights into circadian physiology [40] [41]. Clinical translation requires standardization of measurement protocols and establishment of sweat hormone reference ranges across diverse populations.
These technological advances will accelerate precision medicine approaches that account for individual circadian variability in disease manifestation and treatment response. Large-scale population studies using wearable hormone sensors will define the spectrum of circadian phenotypes and their relationship to health outcomes. Ultimately, continuous circadian endocrine monitoring promises to advance fundamental understanding of temporal biological organization while enabling novel diagnostic and therapeutic strategies for circadian disruption.
Circadian rhythms are endogenous 24-hour cycles that govern a vast array of physiological and behavioral processes in virtually all eukaryotic organisms [38]. These rhythms are regulated by a transcriptional-translational feedback loop (TTFL) composed of core circadian clock genes, including CLOCK, BMAL1 (also known as ARNTL), Period (PER1, PER2, PER3), and Cryptochrome (CRY1, CRY2) [6] [38]. The BMAL1:CLOCK heterodimer acts as the primary transcriptional activator, driving the expression of PER and CRY genes. Subsequently, PER:CRY protein complexes form and translocate back to the nucleus to inhibit BMAL1:CLOCK activity, completing the core feedback loop [38]. An auxiliary loop involving REV-ERB and ROR proteins provides additional stability by rhythmically regulating Bmal1 transcription [38].
In mammalian systems, the suprachiasmatic nucleus (SCN) of the hypothalamus serves as the master pacemaker, synchronizing peripheral clocks located in various tissues throughout the body [6] [38]. These peripheral clocks regulate tissue-specific rhythmic gene expression, with transcriptomic studies revealing that a substantial proportion of the mammalian genome—up to half of all genes in some tissues—exhibits circadian oscillations [46] [47]. The endocrine system plays a crucial role in communicating timing signals from the SCN to peripheral tissues, with hormones such as melatonin, glucocorticoids, and others serving as key systemic synchronizers [6] [44].
Profiling circadian gene expression requires specialized genomic and transcriptomic approaches capable of capturing dynamic changes across the 24-hour cycle. This technical guide provides an in-depth examination of current methodologies, analytical frameworks, and experimental considerations for comprehensive circadian gene expression profiling, with particular emphasis on their application within endocrine research contexts.
Experimental Design Considerations
Temporal Sampling Strategies
Robust circadian profiling requires dense temporal sampling across at least 24 hours to adequately capture expression peaks and troughs. Studies in rodent models typically collect samples at 2-4 hour intervals under constant environmental conditions (e.g., constant darkness) to distinguish endogenous rhythms from light-induced responses [46]. For human studies, the practical challenges are greater, but similar principles apply. The number of biological replicates required depends on the expected effect size and rhythmicity characteristics, with statistical power analyses suggesting that two biological replicates per time point can detect approximately 89% of truly rhythmic genes in well-controlled experiments [46].
When designing sampling schedules, researchers must account for the internal circadian time (ICT) of each subject, which may be offset from the external Zeitgeber time (ZT) due to individual differences in circadian phase [48]. The gold-standard biomarker for determining this offset in humans is the dim-light melatonin onset (DLMO), though its measurement requires controlled dim-light conditions and frequent sample collection, adding substantial cost and complexity to studies [48].
Cell-Type-Specific Approaches
Traditional bulk tissue transcriptomics obscures cell-type-specific circadian rhythms, potentially missing important biological signals. Recent methodological advances enable cell-type-specific circadian profiling through genetic labeling techniques. The Translating Ribosome Affinity Purification (TRAP) and RiboTag methods allow isolation and sequencing of ribosome-associated mRNA from specific cell populations in complex tissues [46].
For example, astrocyte-specific TRAP mice (Aldh1l1-RPL10aeGFP, termed AstroTRAP) and microglia-specific RiboTag mice (Cx3cr1-CreERT2;LSL-Rpl22HA, termed mgRiboTag) have been used to elucidate cell-specific circadian "translatomes" in the mouse brain [46]. These approaches have revealed that glial circadian translatomes are highly cell-type-specific and exhibit profound, context-dependent reprogramming in response to challenges such as amyloid pathology or aging [46]. Similar cell-type-specific approaches are applicable to endocrine tissues, allowing researchers to investigate circadian function in specific hormone-producing cell populations.
Table 1: Key Considerations for Circadian Sampling Design
| Factor | Consideration | Recommendation |
|---|---|---|
| Sampling Frequency | Sufficient to capture waveform | Every 2-4 hours over ≥24 hours |
| Biological Replicates | Statistical power for rhythm detection | Minimum 2 per time point |
| Experimental Conditions | Control of external cues | Constant darkness for rodent studies |
| Phase Determination | Individual variation | DLMO measurement for human studies |
| Cell-Type Resolution | Cellular heterogeneity | TRAP, RiboTag, or single-cell approaches |
Methodological Approaches
Transcriptomic Profiling Technologies
RNA sequencing (RNA-seq) has become the standard method for comprehensive circadian transcriptomic profiling due to its sensitivity, dynamic range, and ability to detect novel transcripts. Both conventional RNA-seq and ribosome profiling (Ribo-seq) approaches provide valuable insights, with the latter capturing actively translated mRNAs that may more closely reflect rhythmic protein expression [46].
Specialized computational platforms have been developed to facilitate circadian data analysis. BioDare2 is an online repository and analysis platform specifically designed for rhythmic biological data, providing access to multiple analysis methods including FFT-NLLS, MESA, MFourFit, and various periodogram approaches [49]. These tools enable researchers to perform rhythm detection and characterization without requiring extensive bioinformatics expertise.
For large-scale studies involving multiple experimental conditions, TRAP-RNA-seq combined with cell-type-specific labeling enables decomposition of circadian regulation across different cell populations. This approach has revealed that approximately half of all Alzheimer's disease risk genes display circadian oscillations in glial cells, many of which are altered by pathology [46].
Analytical Frameworks and Algorithms
Multiple computational algorithms have been developed specifically for detecting circadian rhythms in transcriptomic data. These can be broadly categorized as parametric (e.g., cosinor-based models) and nonparametric (e.g., JTK_CYCLE, RAIN) approaches [50]. The cosinor model assumes gene expression follows a sine or cosine function of circadian time and offers biological interpretability with accurate statistical inferences under Gaussian assumptions [50] [48].
Recent methodological advances include BayesCircRhy, a novel Bayesian framework that incorporates prior biological knowledge to enhance detection of circadian genes [50]. This approach uses a hierarchical model and reverse jump Markov chain Monte Carlo (rjMCMC) technique for model selection, demonstrating favorable false discovery rate control and robustness against heavier-tailed error distributions compared to existing methods [50].
For analyzing population-level data with individual phase variations, mixed-effects cosinor models have been developed that account for the offset between each person's internal circadian time and external Zeitgeber time [48]. These approaches help mitigate attenuation bias that can occur when individual phase differences are not considered.
Table 2: Computational Methods for Circadian Rhythm Detection
| Method | Approach | Key Features | Applications |
|---|---|---|---|
| JTK_CYCLE | Nonparametric | Robust to non-sinusoidal waveforms | General transcriptomic screening |
| RAIN | Nonparametric | Detects asymmetric waveforms | Bulk and cell-type-specific transcriptomics |
| Cosinor | Parametric | Biologically interpretable parameters | Hypothesis-driven rhythm characterization |
| BayesCircRhy | Bayesian | Incorporates prior knowledge | Enhanced power for known circadian genes |
| Mixed-Effects Cosinor | Parametric | Accounts for individual phase differences | Human population studies |
Single-Timepoint and Multi-omic Integration
When traditional time-course sampling is impractical, novel computational approaches can infer circadian information from single timepoint samples. The COFE (Circadian Omics Feature Extraction) algorithm uses unsupervised machine learning to reconstruct circadian rhythms from single omics samples across cohorts, simultaneously assigning time labels to samples and identifying rhythmic features [51]. This approach has revealed widespread circadian gene expression rhythms in human cancers using data from The Cancer Genome Atlas [51].
Integration across multiple omics layers (transcriptomics, proteomics, metabolomics) provides a more comprehensive view of circadian regulation. For example, rhythmic genes and proteins common to multiple cancer types are predominantly involved in metabolism and the cell cycle, suggesting core circadian processes that may be therapeutic targets [51].
Experimental Protocols
Cell-Type-Specific Circadian Translational Profiling Using TRAP
Purpose: To isolate and sequence ribosome-associated mRNA from specific cell types in complex tissues at high temporal resolution to characterize cell-type-specific circadian translatomes.
Materials:
- Cell-type-specific TRAP or RiboTag mouse lines (e.g., Aldh1l1-RPL10aeGFP for astrocytes, Cx3cr1-CreERT2;LSL-Rpl22HA for microglia)
- Control: Pre-IP bulk tissue
- Cycloheximide solution (to halt ribosomal activity during tissue collection)
- Standard RNA extraction and sequencing reagents
- Immunoprecipitation antibodies and reagents
Procedure:
- Animal entrainment: House mice under 12-hour light/12-hour dark cycles for at least two weeks prior to experiment.
- Constant conditions: Transfer mice to constant darkness for 24 hours before and during sample collection to measure endogenous rhythms.
- Temporal sampling: Euthanize mice at 2-4 hour intervals over a 24-hour period in duplicate (minimum 2 biological replicates per time point).
- Perfusion and tissue collection: Perfuse mice with cycloheximide (100 µg/mL in PBS) to immobilize ribosomes, then rapidly dissect tissue of interest.
- Immunoprecipitation: Homogenize tissue and perform immunoprecipitation using antibodies against the tagged ribosomes (e.g., GFP for AstroTRAP, HA for mgRiboTag).
- RNA extraction: Isolate RNA from both immunoprecipitated and pre-IP samples.
- Library preparation and sequencing: Prepare RNA-seq libraries using standard protocols and sequence on an appropriate platform.
- Bioinformatic analysis: Align sequences, quantify gene expression, and identify rhythmic transcripts using algorithms such as RAIN or JTK_CYCLE.
Validation: Enrichment of cell-type-specific markers should be confirmed in IP samples compared to pre-IP (typically 5-10-fold for astrocytes, 10-20-fold for microglia) [46]. Principal component analysis should show clustering by cell type rather than genotype or other variables.
Circadian Reprogramming Analysis in Disease Models
Purpose: To identify changes in circadian gene expression patterns (circadian reprogramming) in response to disease pathology, aging, or other experimental manipulations.
Materials:
- Appropriate disease model (e.g., APP/PS1-21 mice for amyloid pathology)
- Age-matched wild-type controls
- Reagents for transcriptomic profiling (as above)
- Computational tools for differential rhythm analysis (e.g., compareRhythms)
Procedure:
- Experimental groups: Establish experimental and control groups with appropriate sample sizes based on power calculations.
- Temporal sampling: Collect samples across the circadian cycle as described in Protocol 4.1.
- Transcriptomic profiling: Perform RNA-seq on all samples.
- Rhythm detection: Identify rhythmically expressed genes in both experimental and control conditions using a consistent statistical threshold (e.g., RAIN adjusted p-value < 0.01 and FDR < 0.15).
- Comparative analysis: Use the compareRhythms algorithm to classify genes into categories:
- Consistently rhythmic: Rhythmic in both conditions with consistent phase
- Rhythm loss: Rhythmic in control but not in experimental condition
- Rhythm gain: Rhythmic in experimental but not in control condition
- Phase-shifted: Rhythmic in both conditions but with significantly different phases
- Pathway analysis: Perform KEGG pathway enrichment analysis on each category of genes to identify biological processes affected by circadian reprogramming.
Application Example: In APP/PS1-21 mouse cortex, this approach identified 2,563 transcripts that lost rhythmicity and 591 that gained rhythmicity compared to wild-type, with core clock genes remaining rhythmic in both conditions [46]. Pathway analysis revealed loss of rhythms in autophagy and lysosomal genes, with gain of rhythmicity in inflammatory pathways.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Circadian Transcriptomics
| Reagent/Tool | Function | Application Notes |
|---|---|---|
| TRAP/RiboTag Mouse Lines | Cell-type-specific ribosomal tagging | Enables translatome analysis from specific cell types in complex tissues |
| Cycloheximide | Ribosome immobilization | Preserves in vivo ribosome positioning during tissue collection |
| RNA Stabilization Reagents | RNA integrity preservation | Critical for accurate transcript quantification during temporal sampling |
| Phase Determination Assays | Individual circadian time assessment | Melatonin assay kits for DLMO determination in human studies |
| BioDare2 Platform | Rhythm analysis and data sharing | Online resource for multiple circadian analysis methods [49] |
| BayesCircRhy R Package | Bayesian circadian detection | Incorporates prior knowledge for enhanced rhythm detection [50] |
Integration with Endocrine Research
The genomic and transcriptomic approaches described above have profound implications for understanding endocrine regulation of circadian rhythms. Hormones function as rhythm drivers, zeitgebers, and tuners of circadian processes in target tissues [6]. For example, glucocorticoids not only exhibit robust circadian rhythms but also regulate circadian gene expression by binding to glucocorticoid response elements (GREs) in clock genes and clock-controlled genes [6].
Cell-type-specific circadian profiling approaches are particularly relevant for endocrine tissues, which often contain multiple cell types with distinct functions. Applying TRAP or similar methods to pituitary, adrenal, pancreatic, or other endocrine tissues could reveal how circadian regulation differs across hormone-producing cell populations. This is especially important given that endocrine disruption is a common feature of circadian disruption-related diseases [44].
Circadian transcriptomic analyses have revealed that many endocrine pathways are under circadian control. In astrocyte circadian translatomes, transcripts involved in metabolic pathways and insulin signaling show robust rhythms that are altered in disease models [46]. Similarly, human cancers exhibit rhythms in metabolic pathways that may be coordinated with endocrine signals [51].
The relationship between circadian gene expression and endocrine function is bidirectional. While hormones regulate circadian rhythms in target tissues, the circadian clock also gates hormonal responses. For example, the adrenal clock gates glucocorticoid release in response to ACTH stimulation, and the pancreatic clock influences glucose-stimulated insulin secretion [6]. This bidirectional relationship creates complex feedback systems that can be dissected using the transcriptomic approaches described in this guide.
Diagram 1: Endocrine-Circadian Integration. This diagram illustrates the bidirectional relationship between the central circadian pacemaker in the suprachiasmatic nucleus (SCN), endocrine signals, peripheral tissue clocks, and physiological responses. The SCN regulates hormone secretion through neural and humoral pathways. Hormones act as zeitgebers and tuners for peripheral clocks. Peripheral clocks regulate clock-controlled genes (CCGs) that drive tissue-specific rhythmic responses, which in turn provide feedback to the endocrine system.
Genomic and transcriptomic approaches for profiling circadian gene expression have evolved from bulk tissue analyses to sophisticated cell-type-specific and multi-omic methods. These technical advances have revealed the remarkable complexity of circadian organization across different cell types and physiological contexts. The integration of these approaches with endocrine research is particularly powerful, given the fundamental role of hormones as both regulators and outputs of circadian clocks.
Future directions in the field will likely include increased spatial resolution through single-cell circadian transcriptomics, enhanced multi-omic integration, and refined computational methods that better account for individual differences in circadian phase. As these methodologies continue to advance, they will provide deeper insights into how circadian disruption contributes to disease and how temporal considerations might be incorporated into therapeutic strategies for endocrine and metabolic disorders.
In Vitro and Animal Models for Studying Peripheral Tissue Clocks
The mammalian circadian system is a hierarchical network of biological clocks that orchestrates near-24-hour rhythms in physiology and behavior. While the suprachiasmatic nucleus (SCN) in the hypothalamus serves as the central pacemaker, autonomous circadian clocks exist in virtually all peripheral tissues, including the liver, heart, kidneys, adipose tissue, and skeletal muscle [18] [22]. These peripheral clocks operate through transcriptional-translational feedback loops (TTFLs) involving core clock genes such as CLOCK, BMAL1, PER, CRY, REV-ERB, and ROR [22]. Unlike the light-entrained SCN, peripheral oscillators can be synchronized by local cues including feeding patterns, body temperature, hormonal fluctuations, and metabolic signals [18] [22].
Investigating peripheral clocks requires specialized experimental models that capture their autonomous nature while accounting for systemic influences. This technical guide provides an in-depth overview of current in vitro and in vivo models, detailing their applications, methodological considerations, and relevance to endocrine research. Understanding these clocks is particularly crucial in endocrine regulation, as they govern daily fluctuations in hormone secretion and tissue responsiveness to hormonal signals [18] [52]. Disruption of peripheral circadian rhythms is increasingly implicated in metabolic diseases, cardiovascular dysfunction, cancer, and neurodegenerative disorders, highlighting the importance of robust experimental models for both basic research and therapeutic development [18] [22] [53].
Molecular Basis of Peripheral Circadian Clocks
Core Clock Machinery
The molecular architecture of peripheral clocks centers on TTFLs that generate approximately 24-hour oscillations in gene expression. The core loop involves the CLOCK-BMAL1 heterodimer activating transcription of Per and Cry genes via E-box enhancer elements. PER and CRY proteins then form complexes that translocate back to the nucleus to repress CLOCK-BMAL1 activity, completing the approximately 24-hour cycle [22]. Stabilizing loops involving nuclear receptors REV-ERBα/β and RORα/β/γ provide additional regulation by competing for ROR response elements (RREs) in the Bmal1 promoter, with REV-ERBs repressing and RORs activating transcription [22] [54].
This molecular oscillator regulates the rhythmic expression of clock-controlled genes (CCGs), which govern tissue-specific functions. In the liver, approximately 6-10% of transcripts show circadian oscillation, influencing processes such as glucose metabolism, lipid homeostasis, and xenobiotic detoxification [18]. Similarly, cardiac clocks regulate daily patterns in metabolism, contractile function, and electrophysiology [18] [22]. The system's robustness allows peripheral tissues to maintain rhythmicity even when isolated from the SCN, though with eventual desynchronization without external timing cues.
Signaling Pathways in Peripheral Clock Regulation
The following diagram illustrates the key signaling pathways that synchronize peripheral clocks with external and internal cues:
Figure 1: Signaling pathways regulating peripheral circadian clocks. External and internal zeitgebers synchronize peripheral oscillators through multiple signaling cascades that ultimately converge on the core clock machinery.
In Vitro Model Systems
Primary Cell Cultures
Primary cells isolated from peripheral tissues provide a robust model for studying autonomous circadian rhythms while maintaining tissue-specific characteristics. Protocols typically involve isolating cells from transgenic reporter mice expressing luciferase under control of clock gene promoters (e.g., Per2::Luc), enabling real-time monitoring of circadian rhythms through bioluminescence recording [55].
Hepatocyte isolation protocol:
- Perform hepatic perfusion with collagenase solution via the portal vein
- Dissociate liver tissue in Hanks' Balanced Salt Solution (HBSS)
- Filter cell suspension through 70μm nylon mesh
- Centrifuge at 50×g for 3 minutes to separate hepatocytes from non-parenchymal cells
- Plate cells on collagen-coated 35mm dishes at 2.5×10⁵ cells/dish in DMEM with 10% FBS
- After confluence, synchronize with 100nM dexamethasone for 30 minutes
- Record bioluminescence rhythms in air-controlled incubators at 36°C [55]
Primary cultures maintain tissue-specific gene expression and metabolic functions but have limited lifespan and may lose circadian amplitude after several days in culture. The dexamethasone synchronization mimics glucocorticoid signaling, a key endocrine mechanism for peripheral clock entrainment [18] [52].
Immortalized Cell Lines
Established cell lines offer reproducibility, scalability, and genetic tractability for circadian studies. Popular models include:
- NIH3T3 mouse fibroblasts: Widely used for circadian mechanistic studies and chemical screening
- U2OS human osteosarcoma cells: Human model with robust circadian oscillations
- C2C12 mouse myoblasts: For skeletal muscle circadian biology
Circadian monitoring protocol:
- Culture cells in appropriate medium with 10% FBS
- Transfect with circadian reporter constructs if not endogenously expressing
- Synchronize rhythms using 100nM dexamethasone, 50% horse serum, or forskolin
- Transfer to recording medium (phenol-red free medium with 0.1mM luciferin and 10mM HEPES)
- Measure bioluminescence rhythms in real-time using photomultiplier tube systems or cooled CCD cameras [55]
Immortalized cells provide unlimited material but may have altered signaling pathways due to transformation. Serum shock synchronization reveals the innate circadian oscillatory capacity of peripheral cells without neural or hormonal inputs.
Animal Models
Genetic Mouse Models
Genetic models are indispensable for studying peripheral clocks in physiological context. The table below summarizes key mouse models used in peripheral circadian research:
Table 1: Genetic Mouse Models for Studying Peripheral Clocks
| Model Name | Genetic Manipulation | Key Features | Applications | Limitations |
|---|---|---|---|---|
| Per2::Luc | Luciferase knocked into Per2 locus | Real-time bioluminescence monitoring of PER2 expression rhythms | Ex vivo culture rhythm measurements; Tissue-specific oscillations | Requires specialized imaging equipment |
| Per1/2/3 Triple KO | Global deletion of all Per genes | Arrhythmic in constant darkness; Reveals extra-SCN pacemakers | Studying TTFL-independent rhythms; Pacemaker localization | Compensatory mechanisms may develop |
| BMAL1 KO | Global or tissue-specific Bmal1 deletion | Disrupted molecular oscillator; Metabolic and physiological deficits | Clock function in specific tissues; Metabolic phenotyping | Developmental effects in global KO |
| CRY1/2 Double KO | Global deletion of both Cry genes | Arrhythmic in constant conditions; Altered light responses | Molecular clock mechanism studies | Potential pleiotropic effects |
The Per triple knockout model is particularly valuable for studying non-canonical circadian rhythms. These mice exhibit arrhythmic behavior in constant darkness but can express robust circadian rhythms under constant light conditions or in response to methamphetamine administration, revealing the existence of extra-SCN pacemakers [55]. This model demonstrates that circadian-like behaviors can occur independent of the canonical PER/CRY-based TTFL.
Environmental Manipulation Models
Environmental disruption models recapitulate human conditions like shift work or social jet lag that disrupt peripheral clocks:
Chronic phase shift protocol (mimicking shift work):
- House mice in light-tight cabinets with programmable lighting
- Advance or delay light-dark cycle by 8 hours every 2-3 days
- Maintain disruption for 4-8 weeks depending on experimental goals
- Assess peripheral clock function through tissue collection at multiple time points [56]
Social jet lag model (for adolescent mice):
- Use adolescent mice (4-6 weeks old)
- Expose to alternating light-dark cycles: 4 days of 12:12 LD, then 3 days of 8:16 LD
- Repeat cycle for 4-8 weeks during adolescent development
- Evaluate cognitive and metabolic outcomes alongside molecular rhythms [56]
These models effectively disrupt the phase relationship between central and peripheral oscillators, leading to internal desynchronization that mimics human pathology. Studies using these approaches have revealed that chronic circadian disruption during adolescence impairs hippocampal memory and disrupts gene expression oscillations in both hypothalamus and hippocampus [56].
Experimental Protocols and Methodologies
Rhythm Monitoring and Analysis
Tissue explant culture enables assessment of autonomous peripheral rhythms:
- Sacrifice reporter mice (e.g., Per2::Luc) at designated time points
- Rapidly dissect tissues and place in cold, sterile HBSS
- Slice tissues into 1-2mm sections using vibratome or manual slicing
- Place explants on culture membranes in 35mm dishes with 1.5ml recording medium
- Record bioluminescence in LumiCycle or similar apparatus for 5-7 days
- Analyze data using cosine fitting or JTK_CYCLE algorithm to determine period, phase, and amplitude [55]
Salivary circadian assessment (human translational approach):
- Collect saliva samples at 3-4 time points daily for 2 consecutive days
- Preserve samples in RNAprotect at 1:1 ratio
- Extract RNA and analyze core clock gene expression (ARNTL1, NR1D1, PER2)
- Correlate gene acrophase with cortisol rhythms and behavioral timing [57]
This non-invasive approach demonstrates phase synchronization of clock genes across peripheral tissues and offers potential for clinical circadian monitoring [57].
Behavioral and Cognitive Assessment
For animal models, comprehensive behavioral testing contextualizes molecular findings:
Spatial memory assessment (Reference memory test):
- Use Y- or T-maze with three identical arms
- During training, block one arm and allow exploration of other two for 10 minutes
- After 1-hour inter-trial interval, test by allowing access to all three arms
- Measure time spent in novel arm versus familiar arms
- Calculate discrimination index: (time in novel - time in familiar)/(total time) [56]
Social recognition test:
- House test mouse individually for 30 minutes before testing
- Place unfamiliar "stimulus" mouse under inverted wire cup in test arena
- Allow 10-minute exploration, then return to home cage
- After 1-hour interval, repeat with familiar and novel stimulus mice
- Measure time investigating each stimulus mouse [56]
Circadian disruption models consistently show deficits in these tasks, with disrupted mice showing impaired novel object recognition and reduced social recognition discrimination indices compared to controls [56].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Peripheral Clock Studies
| Reagent Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Synchronizing Agents | Dexamethasone (100nM), Forskolin (10μM), Horse serum (50%) | Reset cellular clocks in culture; Enable rhythm analysis | Different agents may induce varying phase responses |
| Circadian Reporters | PER2::LUC fibroblasts, Bmal1-dLuc constructs | Real-time monitoring of molecular clock function | Requires specialized detection equipment |
| Clock Gene Antibodies | Anti-BMAL1, Anti-PER1/2, Anti-CRY1/2, Anti-REV-ERBα | Immunodetection of clock proteins in tissues | Validate for specific applications (IHC, WB) |
| qPCR Assays | Primer sets for Bmal1, Per1/2, Cry1/2, Rev-erbα, Dbp | Quantify circadian gene expression | Include multiple reference genes for normalization |
| Bioluminescence Substrates | D-Luciferin potassium salt (0.1-1mM) | Sustained luminescence for long-term recording | Concentration affects signal duration and intensity |
Data Analysis and Interpretation
Circadian data requires specialized analytical approaches:
Period and phase analysis:
- Chi-square periodogram: Identifies dominant periodic components in time-series data
- Fast Fourier Transform (FFT): Decomposes rhythmic data into frequency components
- Cosine fitting: Determines acrophase (peak time), amplitude, and mesor (mean) using equation: y = mesor + amplitudecos(2π(x-acrophase)/period)
Statistical testing for rhythmicity:
- JTK_CYCLE: Non-parametric algorithm robust to noise and outliers
- RAIN: Detects non-sinusoidal rhythms in large datasets
For animal behavior studies, appropriate statistical tests include two-way ANOVA with time and genotype/treatment as factors, followed by post-hoc tests with multiple comparison corrections. Sample sizes should be determined by power analysis based on expected effect sizes, typically n=6-12 animals per group for mouse studies [56] [54].
In vitro and animal models for studying peripheral clocks have revealed the fundamental principles of circadian organization in mammalian physiology. The continuing development of more sophisticated genetic tools, including tissue-specific inducible knockout systems and multi-modal reporters, will further enhance our ability to dissect peripheral clock functions. The integration of human cell-based models, including organoid systems, represents a promising frontier for translational applications.
Research in this area has profound implications for chronotherapy - the timing of treatments to align with biological rhythms - which is emerging as a promising approach for optimizing drug efficacy and minimizing side effects [18] [57]. This is particularly relevant in endocrine-related disorders, where circadian disruption both contributes to and results from disease pathogenesis. Future work will continue to elucidate how peripheral clocks integrate systemic and local signals to maintain physiological homeostasis, informing novel therapeutic strategies for the range of disorders associated with circadian disruption.
Circadian disruption is a pervasive feature of modern life, emerging from lifestyles such as shift work and transmeridian travel. In experimental research, simulating these human conditions in model organisms is crucial for understanding the underlying pathophysiology of associated metabolic, gastrointestinal, and cognitive disorders. This guide provides an in-depth examination of the principal experimental paradigms—chronic jet lag and shift work models—used to study circadian disruption, with a specific focus on their implications for endocrine regulation. These models are foundational for investigating how misalignment between the central circadian clock in the suprachiasmatic nucleus (SCN) and peripheral oscillators (e.g., in the liver, adrenal gland, and gut) leads to systemic physiological dysfunction. The choice of paradigm, including the frequency and direction of phase shifts, is critical, as it determines the nature and severity of the resulting misalignment and metabolic phenotypes [58] [59].
Chronic Jet Lag Models
Chronic jet lag (CJL) paradigms are experimental tools designed to emulate the repeated circadian disruption experienced during frequent transmeridian travel or rotating shift work. These models aim to induce a state of internal desynchronization, where different bodily rhythms fall out of alignment with each other and with the external environment.
Paradigm Design and Key Parameters
The core principle of CJL involves periodically shifting the timing of the light-dark (LD) cycle to which experimental animals are exposed. The specific physiological and molecular outcomes are highly sensitive to several key parameters [58]:
- Shift Direction and Frequency: Advances (phase advances) of the light schedule are generally more disruptive to circadian rhythms and associated with more severe metabolic and cognitive impairments than delays (phase delays). Shifts are applied every 2-4 days to prevent full re-entrainment.
- Shift Magnitude: An 8-hour shift is commonly used as it represents a substantial challenge to the circadian system, similar to traveling across eight time zones.
- "Every Other Day" Shifts: This intense protocol can eventually uncouple peripheral organ rhythms from the central light cycle, creating a state reminiscent of free-running conditions [58].
Table 1: Comparison of Chronic Jet Lag Paradigms and Their Outcomes
| Paradigm Parameter | Protocol Description | Key Physiological Outcomes | Molecular/Cellular Findings |
|---|---|---|---|
| Frequent 8-h Advances [58] | 8-hour phase advance of the LD cycle applied frequently (e.g., every 2-4 days). | Severe circadian misalignment; non-fasted hyperglycemia. | Distinct effects on liver rhythmicity; misalignment without arrthythmicity. |
| "Every Other Day" Shifts [58] | Extreme shifting protocol preventing stable entrainment. | Uncoupling of behavioral and hepatic rhythms from the light cycle. | Liver rhythms become reminiscent of free-running conditions. |
| Phase Advances vs. Delays [59] | Comparing 8-hour advances against 8-hour delays every 4th day for 6 cycles. | Advances cause more pronounced desynchronization and cognitive impairment. | Greater dysregulation of clock gene expression (Per1, Cry1, Bmal1) in the hippocampus and prefrontal cortex. |
Detailed Experimental Protocol
A typical CJL protocol for studying metabolic dysfunction in rodents is as follows [58]:
- Animal Acclimation: House mice (e.g., C57BL/6J males) under a standard 12:12 hour LD cycle for at least two weeks to establish stable baseline rhythms.
- Chronic Jet Lag Induction: Subject the experimental group to a series of 8-hour phase advances in the LD cycle. For example, shift the lights-on and lights-off times 8 hours earlier every second day for a duration of 2-3 weeks.
- Control Group: Maintain a control group under the original, stable LD cycle.
- Monitoring: Continuously monitor voluntary locomotor activity (e.g., via running wheels) throughout the experiment to assess rhythm disruption and re-entrainment kinetics.
- Sample Collection: Conduct tissue collection (e.g., liver, serum, brain regions) in a time-dependent manner (every 4-6 hours over a 24-hour cycle) at the end of the paradigm to assess circadian phasing of gene expression, hormone levels, and metabolites.
- Functional Assessment: Perform metabolic tests, such as glucose tolerance tests (GTT) and insulin tolerance tests (ITT), in the final days of the experiment.
Simulated Shift Work Models
Shift work models aim to replicate the chronic, irregular sleep-wake schedules common in human populations, often incorporating additional environmental stressors to model the real-world context of shift workers.
Paradigm Design and Key Parameters
These models go beyond simple light schedule manipulation to include factors like social isolation, which is a common correlate of shift work [59].
- Light Schedule Manipulation: Involves inverting the LD cycle for night-shift simulation or implementing rotating shifts (e.g., advancing or delaying the LD cycle by 8 hours every few days).
- Social Isolation as an Amplifier: Social isolation is a powerful non-photic stressor that can exacerbate the circadian disruption caused by shifting light schedules. It acts by removing social cues, which are potent non-photic zeitgebers that normally help maintain rhythm coherence [59].
- Housing Condition: Grouped housing can confer resilience and protect against severe rhythm disruption, whereas isolated housing potentiates circadian desynchrony [59].
Table 2: Simulated Shift Work Paradigms and Interactive Effects
| Experimental Factor | Protocol Description | Impact on Circadian Rhythms | Combined Effect with Phase Shifts |
|---|---|---|---|
| Phase Advances (Rotating Shifts) [59] | Successive 8-hour advances of the LD cycle every 4th day for 6 cycles. | Pronounced behavioral desynchronization and rhythm fragmentation. | Considered the most disruptive protocol. |
| Social Isolation [59] | Single-housing of mice for the experiment duration. | Marked rhythm fragmentation, phase misalignment, and delayed re-entrainment. | Amplifies disruption from phase shifts; leads to marked clock gene dysregulation. |
| Group Housing [59] | Housing multiple mice together during the experiment. | Promotes stable behavioral rhythms and normal clock gene expression. | Confers resilience and preserves circadian stability under shifting schedules. |
Detailed Experimental Protocol
A protocol investigating the combined impact of shift work and social isolation includes [59]:
- Animal Assignment: Assign male AKR mice to grouped or isolated housing conditions.
- Lighting Regimens: Expose mice to one of three lighting regimens:
- Stable 12:12 LD cycle (control).
- Successive 8-hour phase delays every 4th day for 6 cycles.
- Successive 8-hour phase advances every 4th day for 6 cycles.
- Activity Monitoring: Assess locomotor activity rhythms using wheel-running apparatus throughout the experiment.
- Tissue Collection: At the end of the protocol, collect brain regions critical for cognition and circadian regulation (e.g., prefrontal cortex and hippocampus) at a designated time point.
- Molecular Analysis: Quantify transcript levels of core clock genes (Per1, Cry1, Bmal1, Clock) using RT-qPCR.
Endocrine and Systemic Pathophysiological Outcomes
Circadian disruption models consistently recapitulate key features of human disease, with the endocrine system playing a central role in mediating systemic effects.
Metabolic Dysregulation and the Liver
A core finding is that chronic circadian misalignment, rather than a complete loss of rhythm, drives metabolic dysfunction. Frequent shifts can uncouple liver rhythms from the central light cycle, leading to a misaligned state that impairs glucose homeostasis and results in non-fasted hyperglycemia [58]. The liver clock, when desynchronized, fails to optimally coordinate metabolic processes with nutrient intake.
The Brain and Cognitive Function
The hippocampus and prefrontal cortex, brain regions critical for memory and executive function, possess their own peripheral clocks and are highly vulnerable to disruption. Social isolation combined with phase advances causes significant dysregulation of clock genes (Per1, Cry1, Bmal1) in these regions, with the hippocampus showing particular sensitivity. This molecular desynchrony is a proposed mechanism for the cognitive impairments observed in shift workers [59].
The Gut Microbiota Axis: "Gut Jet Lag"
A novel pathogenic mechanism emerging from these models is "gut jet lag," a state of desynchronization between the host's circadian system and the rhythmic gut microbiota. This concept is formalized in the Chrono-Microbiota-Motility axis [60] [61].
- Disruption: Irregular feeding times and nocturnal light exposure disrupt the peripheral clocks in the gut, leading to dysbiosis and altered rhythmicity of microbial metabolites like short-chain fatty acids (SCFAs).
- Consequences: Disrupted SCFA rhythms impair intestinal propulsive motility and weaken the intestinal barrier, contributing to the development of functional constipation and low-grade inflammation [60] [61].
Endocrine Rhythms as Mediators
Hormones are key mediators between the central clock and peripheral tissues.
- Glucocorticoids: These steroid hormones exhibit a robust circadian rhythm regulated by the SCN, the HPA axis, and the adrenal gland's intrinsic clock. Glucocorticoids act as potent zeitgebers for peripheral clocks; their rhythmic release helps synchronize organs like the liver. Disruption of their rhythm is a key pathway for systemic metabolic effects [6].
- Melatonin: This hormone, secreted rhythmically by the pineal gland in response to darkness, is a direct circadian rhythm driver and zeitgeber. It helps synchronize the SCN and peripheral tissues. Its secretion is acutely suppressed by light at night, a common feature in shift work models, which contributes to the misalignment of downstream physiological processes [6].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for Circadian Disruption Research
| Reagent/Tool | Specific Example | Research Application |
|---|---|---|
| Genetically Modified Mouse Models | Muscle stem cell-specific NAD+ boosters [62]; global/peripheral tissue-specific clock gene knockouts. | To investigate cell-type-specific mechanisms of circadian function and regeneration. |
| Single-Cell RNA Sequencing | 10X Genomics Chromium Platform. | To profile time-dependent inflammatory responses and cell-cell signaling in tissues like muscle after injury [62]. |
| RT-qPCR Assays | TaqMan assays for core clock genes (Per1, Cry1, Bmal1, Clock, Rev-erbα). | To quantify circadian gene expression rhythms in tissue samples (e.g., brain, liver) [59]. |
| Metabolic Assay Kits | Glucose Assay Kit, Insulin ELISA. | To assess metabolic dysfunction (hyperglycemia, insulin resistance) in vivo and ex vivo [58]. |
| Hormone Measurement | Corticosterone/Cortisol ELISA, Melatonin ELISA. | To monitor circadian endocrine rhythms as readouts of central and peripheral clock function [6]. |
| Activity Monitoring Software | ClockLab (Actimetrics). | To analyze locomotor activity and sleep-wake rhythms from wheel-running or infrared beam data. |
Chronic jet lag and shift work models are indispensable for deconstructing the complex pathophysiology arising from circadian misalignment. The evidence demonstrates that the specific design of the paradigm—the direction, frequency, and magnitude of shifts, coupled with environmental factors like social isolation—profoundly influences the physiological outcome, from metabolic and gastrointestinal dysfunction to cognitive impairment. A central insight is that misalignment, not arrhythmicity, is the primary disturbance underlying metabolic dysfunction. The endocrine system, through hormones like glucocorticoids and melatonin, serves as a critical conduit for this misalignment, synchronizing peripheral clocks and coordinating systemic physiology. Future research employing these models, particularly with single-cell technologies and tissue-specific genetic tools, will continue to elucidate the intricate network of communication between the brain, body, and gut microbiota in circadian disorders.
Chronopharmacology represents a critical frontier in precision medicine, investigating how biological rhythms influence drug efficacy, toxicity, and metabolism [63]. This discipline recognizes that physiological processes exhibit predictable temporal variations governed by the circadian system, which profoundly modulates drug pharmacokinetics and pharmacodynamics [64]. Within endocrine research, circadian rhythms regulate hormone secretion, receptor sensitivity, and metabolic pathways, creating optimal temporal windows for therapeutic interventions [65] [66]. The suprachiasmatic nucleus (SCN) of the hypothalamus serves as the master circadian pacemaker, synchronizing peripheral clocks in virtually all tissues through neural and hormonal signals [38] [11]. This hierarchical organization ensures temporal coordination of physiological systems, including endocrine function, metabolism, and cellular proliferation [67]. Understanding these circadian regulatory networks is transforming drug development and administration paradigms, moving beyond "what" to administer to "when" to administer for optimized therapeutic outcomes [63] [68].
Molecular Foundations of Circadian Rhythms
The circadian system operates through cell-autonomous molecular clocks that generate approximately 24-hour rhythms via transcription-translation feedback loops (TTFLs) [38].
Core Clock Machinery
At the molecular level, circadian rhythms are generated by a core group of clock genes and their protein products that form interlocking feedback loops [38]:
- Positive Limb: The BMAL1 (brain and muscle ARNT-like protein-1) and CLOCK (circadian locomotor output cycles kaput) proteins form a heterodimer that activates transcription of target genes by binding to E-box elements in their promoter regions [38].
- Negative Limb: The PERIOD (PER) and CRYPTOCHROME (CRY) proteins accumulate, form complexes, and translocate to the nucleus to inhibit CLOCK-BMAL1 transcriptional activity [38].
- Stabilizing Loop: Nuclear receptors REV-ERBα/β and RORα/β/γ compete for ROR response elements (RREs) in the BMAL1 promoter, creating an additional feedback loop that stabilizes the core oscillator [38].
This molecular clockwork regulates the rhythmic expression of clock-controlled genes (CCGs), estimated at 5-20% of the transcriptome in various tissues, including those governing drug metabolism, hormone signaling, and cellular stress responses [64] [68].
Figure 1: Core Circadian Clock Feedback Loops. The molecular clock consists of interlocked transcriptional-translational feedback loops that generate ~24-hour rhythms.
Endocrine Regulation of Circadian Rhythms
The circadian and endocrine systems exhibit bidirectional regulation, with clock genes modulating hormone secretion and hormonal signals influencing circadian timing [65] [66]. Key endocrine-circadian interactions include:
- Glucocorticoid Rhythms: The hypothalamic-pituitary-adrenal (HPA) axis exhibits robust circadian and ultradian rhythms, with glucocorticoid levels peaking before the active phase [67]. The SCN regulates this rhythm through differential inhibition of the paraventricular nucleus, with glucocorticoids in turn phase-shifting peripheral clocks [67].
- Melatonin Regulation: Pineal melatonin secretion exhibits a marked diurnal rhythm, with elevated levels during the dark phase serving as a chronobiotic signal that entrains circadian rhythms [65] [11].
- Glucose Homeostasis: Insulin sensitivity, pancreatic β-cell function, and glucose tolerance display circadian rhythms regulated by clock genes in metabolic tissues [66]. Rev-erbα regulates insulin sensitivity rhythms in skeletal muscle and adipose tissue [66].
- Sex Hormones: The hypothalamic-pituitary-gonadal axis exhibits circadian regulation, with sex hormones influencing clock gene expression in various tissues [67].
Chronopharmacological Principles
Circadian Influences on Pharmacokinetics
Drug absorption, distribution, metabolism, and excretion (ADME) exhibit significant circadian variations [64]. These fluctuations arise from rhythmic changes in physiological processes and expression of drug-metabolizing enzymes [64].
Table 1: Circadian Regulation of Pharmacokinetic Processes
| Process | Circadian Influence | Molecular/Physiological Basis |
|---|---|---|
| Absorption | Gastric pH, motility, and blood flow to GI tract vary daily [64] | Higher gastric acid secretion during active phase; circadian regulation of transporters [69] |
| Distribution | Plasma protein binding shows circadian variation [64] | Circadian oscillations in albumin and α1-acid glycoprotein synthesis [64] |
| Metabolism | Hepatic enzyme activity and expression fluctuate rhythmically [64] | PAR bZip transcription factors (DBP, TEF, HLF) regulate cytochrome P450 enzymes and conjugating enzymes [64] |
| Excretion | Renal blood flow, glomerular filtration rate, and urine pH vary daily [64] | Circadian regulation of renal transporters and electrolyte handling; lower urine pH at night [64] |
Chronopharmacodynamics
The circadian system regulates drug targets including receptors, enzymes, and ion channels, creating temporal variations in drug efficacy [64]. Key mechanisms include:
- Receptor Rhythmicity: The expression and sensitivity of numerous drug targets oscillate circadianly, including G-protein coupled receptors, nuclear receptors, and ion channels [64].
- Signal Transduction Pathways: Intracellular signaling cascades exhibit circadian regulation, modulating cellular responses to pharmacological interventions [68].
- Cell Cycle Regulation: The circadian clock gates cell cycle progression, influencing the efficacy of chemotherapeutic agents that target specific cell cycle phases [68].
Experimental Approaches in Chronopharmacology
Methodologies for Circadian Parameter Assessment
Table 2: Experimental Models and Methodologies in Chronopharmacology Research
| Model System | Key Methodologies | Applications in Chronopharmacology |
|---|---|---|
| In Vitro Models | Real-time bioluminescence imaging of reporter genes (PER2::LUC), live-cell imaging of circadian parameters, mathematical modeling of oscillatory systems [68] | Screening for circadian drug effects, investigating cell-autonomous clock influences on drug sensitivity [68] |
| Rodent Models | Jet lag models, shift work paradigms, genetic clock gene mutations, metabolic cages for sampling, telemetry for physiological monitoring [64] | Preclinical assessment of chronotherapeutic efficacy, toxicity rhythm evaluation, mechanistic studies [64] |
| Human Studies | Actigraphy, dim-light melatonin onset (DLMO) assessment, forced desynchrony protocols, repeated sampling for hormone/metabolite measurements [70] | Clinical chronotherapy trials, biomarker discovery, personalized chronotype assessment [70] |
Mathematical Modeling of Time-of-Day Drug Sensitivity
Mathematical approaches provide powerful tools for dissecting factors influencing circadian drug responses [68]. A combined experimental and modeling framework can simulate how circadian and drug properties shape time-of-day efficacy profiles:
- Circadian Parameters: Amplitude, period, and decay rate of circadian oscillations significantly influence time-of-day drug response curves [68].
- Drug Characteristics: Pharmacodynamic properties, including mechanism of action and dose-response relationships, interact with circadian modulation [68].
- Cellular Context: Proliferation rate and cellular fitness rhythms further modulate drug sensitivity patterns [68].
Figure 2: Experimental Workflow for Chronopharmacology Screening. Integrated approach combining cellular models, circadian monitoring, and mathematical modeling.
Research Reagent Solutions for Chronopharmacology Studies
Table 3: Essential Research Tools for Chronopharmacology Investigations
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Circadian Reporters | PER2::LUC, BMAL1::LUC knock-in cells and animals [68] | Real-time monitoring of circadian phase and amplitude in living systems |
| Clock-Modifying Agents | REV-ERB agonists (SR9009), Casein kinase inhibitors [38] | Pharmacological manipulation of core clock components to establish causality |
| Metabolomic Platforms | UPLC-Q-TOF mass spectrometry, LC-MS/MS [69] | Comprehensive profiling of time-dependent drug metabolism and endogenous metabolites |
| Chronotherapeutic Formulations | Programmable infusion pumps, pulsatile release systems, light-sensitive nanoparticles [11] | Testing time-specific drug delivery in preclinical models |
Chronotherapeutic Applications in Endocrine Disorders
Diabetes and Metabolic Diseases
Circadian medicine offers promising approaches for diabetes management through chronotherapeutic strategies [66]:
- Timed Medication: Aligning insulin sensitizers and secretagogues with circadian peaks in insulin resistance and β-cell responsiveness [66].
- Meal Timing: Restricting food intake to active phases to align with endogenous metabolic rhythms [66].
- Chronotype Assessment: Personalizing intervention timing based on individual circadian phase (morningness/eveningness) [66].
Clinical evidence demonstrates that glucose tolerance and insulin sensitivity exhibit diurnal variations, with reduced efficacy in the evening compared to morning [66]. Pancreatic β-cell function shows intrinsic circadian regulation, with clock disruption accelerating β-cell decline in type 2 diabetes [66].
Endocrine Cancer Chronotherapies
The circadian clock influences multiple processes relevant to cancer therapy, including drug metabolism, cell cycle progression, and DNA repair mechanisms [68]. Chronotherapy approaches aim to align anticancer drug administration with circadian rhythms to maximize efficacy and minimize toxicity:
- Temporal Targeting: Administering chemotherapeutic agents during phases of maximal tumor vulnerability and normal tissue resistance [68].
- Hormonal Timing: Aligning endocrine therapies (e.g., aromatase inhibitors, antiestrogens) with circadian rhythms in hormone receptor expression and signaling [68].
- Personalized Chronotherapy: Adapting treatment schedules to individual circadian parameters measured through biomarker assessment [70].
Emerging Frontiers and Technologies
Nanomaterial-Enabled Chronotherapy
Advanced drug delivery systems represent a promising approach for implementing chronotherapeutic principles [11]:
- Stimuli-Responsive Nanocarriers: Liposomes, polymeric nanoparticles, and mesoporous silica designed to release payloads in response to circadian cues such as temperature, pH, or enzyme activity [11].
- Sustained Release Systems: Formulations that maintain therapeutic levels aligned with circadian rhythms in drug sensitivity [11].
- Targeted Delivery: Nanocarriers functionalized with ligands to specific tissues for site-specific chronotherapy [11].
Circadian Biomarker Discovery
Identification of robust circadian biomarkers enables precise assessment of internal time and individual chronotypes for personalized chronotherapy [70]:
- Hormonal Markers: Dim-light melatonin onset (DLMO), cortisol rhythm characteristics [70].
- Metabolic Biomarkers: Rhythmic metabolites identified through targeted metabolomics [69].
- Transcriptional Signatures: Clock gene expression patterns in easily accessible tissues [70].
Chronopharmacology represents a paradigm shift in pharmaceutical sciences, recognizing that biological timing is a critical determinant of therapeutic outcomes. The integration of circadian biology with endocrine research reveals complex temporal regulation of hormonal pathways, metabolic processes, and cellular functions that profoundly influence drug action. As chronotherapeutic approaches advance, they promise more effective, personalized treatments aligned with individual circadian rhythms, ultimately improving patient care across numerous disease domains, particularly in endocrine and metabolic disorders. Future research should focus on developing practical biomarkers of circadian phase, refining chronotherapeutic formulations, and implementing personalized timing strategies in clinical practice.
Circadian Disruption Pathologies and Intervention Strategies
The endocrine system plays a fundamental role in the orchestration of circadian rhythms, serving as a critical interface between the central nervous system and peripheral physiology. Within the context of a broader thesis on endocrine regulation, this review examines how desynchrony of these biological clocks contributes to the pathophysiology of three major conditions: metabolic syndrome, cardiovascular disease, and mood disorders. The circadian timing system is hierarchically organized, with a master pacemaker in the suprachiasmatic nucleus (SCN) of the hypothalamus synchronizing peripheral oscillators in virtually every tissue and organ system [6] [38]. This synchronization occurs through complex neuroendocrine pathways that regulate hormone secretion, metabolic processes, and cardiovascular function across the 24-hour cycle [6]. Disruption of this precise temporal organization—through factors such as shift work, artificial light at night, mistimed eating, and sleep deprivation—induces desynchrony between central and peripheral clocks, creating a state of internal physiological conflict that manifests in significant health impairments [71] [72] [73]. By examining the mechanistic links between circadian disruption and these pathological states, this review aims to provide researchers and drug development professionals with a comprehensive framework for understanding these connections and developing chronotherapeutic interventions.
Molecular Mechanisms of Circadian Timekeeping
Core Clock Machinery
The cellular circadian clock operates through interlocked transcriptional-translational feedback loops (TTFLs) that generate approximately 24-hour rhythms in gene expression. The core positive regulators BMAL1 (brain and muscle ARNT-like protein-1) and CLOCK (circadian locomotor output cycles kaput) form a heterodimer that activates transcription of Period (Per1, Per2, Per3) and Cryptochrome (Cry1, Cry2) genes by binding to E-box elements in their promoter regions [38] [72] [74]. Following translation, PER and CRY proteins progressively accumulate in the cytoplasm, form complexes, and translocate to the nucleus where they suppress CLOCK:BMAL1-mediated transcription, constituting the core negative feedback loop [38] [72]. This oscillation is stabilized by an auxiliary loop involving nuclear receptors REV-ERBα/β (NR1D1/2) and RORα/β/γ, which competitively bind ROR response elements (ROREs) in the Bmal1 promoter, with REV-ERBs repressing and RORs activating transcription [38] [74]. This molecular framework is expressed not only in the SCN but throughout peripheral tissues, where it governs tissue-specific transcriptional programs that coordinate physiological processes with anticipated daily demands [72].
Endocrine Regulation of Circadian Rhythms
Hormones serve as key mediators in the synchronization of circadian rhythms throughout the body. They function through three principal mechanisms: as phasic drivers of physiological rhythms, as zeitgebers resetting tissue clock phase, and as tuners that modify downstream rhythms without directly affecting the core clock [6]. The SCN regulates hormonal secretion through both neural outputs and indirect influence on peripheral oscillators, creating a complex network of temporal regulation [6] [38].
Table 1: Endocrine Regulation of Circadian Rhythms
| Hormone | Secretion Pattern | Primary Role in Circadian System | Target Tissues |
|---|---|---|---|
| Melatonin | Nocturnal peak (2:00-4:00 a.m.) | Zeitgeber; synchronizes peripheral oscillators; promotes sleep | SCN, retina, cardiovascular system, metabolic tissues |
| Glucocorticoids | Peak before active phase; ultradian pulses | Rhythm driver and zeitgeber; regulates metabolic and immune genes | Liver, adipose tissue, muscle, brain, cardiovascular system |
| Sex Hormones | Pulsatile with circadian variation | Rhythm tuner; modulates clock gene expression | Reproductive tissues, brain, bone, liver |
| Leptin/Ghrelin | Leptin: nocturnal peak; Ghrelin: pre-meal rises | Metabolic synchronizers; link nutrient status to clock function | Hypothalamus, liver, adipose tissue |
Melatonin, synthesized primarily by the pineal gland during darkness, functions as a potent chronobiotic signal that phase-shifts the SCN and synchronizes peripheral oscillators through MT1 and MT2 receptors [6] [71]. Its secretion is tightly regulated by the SCN via a multisynaptic pathway, with light exposure during night suppressing production [6] [71]. Glucocorticoids exhibit robust circadian rhythmicity with a peak preceding the active phase, and serve dual roles as both drivers of rhythmic gene expression through glucocorticoid response elements (GREs) and as zeitgebers for peripheral clocks by regulating Per expression [6]. The circadian release of glucocorticoids is governed by a tripartite regulatory system involving SCN signaling to the hypothalamic-pituitary-adrenal (HPA) axis, adrenal innervation, and local adrenal clock gating of sensitivity to adrenocorticotropic hormone (ACTH) [6]. Metabolic hormones including insulin, leptin, ghrelin, and adiponectin also display circadian oscillations and participate in nutrient sensing pathways that feedback on clock function, creating intricate loops between metabolic state and circadian timing [6] [73].
Figure 1: Endocrine Regulation of Circadian Rhythms. The suprachiasmatic nucleus (SCN) coordinates peripheral clocks through neural and hormonal pathways, including melatonin from the pineal gland and glucocorticoids from the adrenal cortex. Bidirectional communication between metabolic tissues (liver, adipose, pancreas) further synchronizes peripheral oscillators.
Metabolic Syndrome
Epidemiological and Clinical Evidence
Circadian disruption has emerged as a significant risk factor for metabolic syndrome, a cluster of conditions including central obesity, dyslipidemia, hypertension, insulin resistance, oxidative stress, and chronic inflammation that collectively increase cardiovascular disease risk [75]. Approximately 25% of the working population engages in shift work, which is associated with increased prevalence of obesity, type 2 diabetes, and metabolic syndrome [73]. The "social jet lag" experienced by approximately 70% of working adults—characterized by shifting sleep timing between workdays and free days—further contributes to metabolic dysregulation [72]. Experimental studies demonstrate that circadian misalignment induced by forced desynchrony protocols or simulated shift work rapidly induces insulin resistance, dyslipidemia, and elevated blood pressure in previously healthy individuals [72] [73]. These effects are mediated through direct impacts of desynchrony on endocrine regulation, with misaligned behavioral cycles disrupting the precise temporal coordination of glucose metabolism, lipid handling, and energy homeostasis [73].
Molecular Mechanisms
At the molecular level, circadian desynchrony disrupts metabolic homeostasis through multiple interconnected pathways. In white adipose tissue, approximately 4% of transcripts (856 genes) exhibit circadian expression patterns, including key regulators of adipogenesis, lipogenesis, and lipolysis [73]. Diet-induced obesity in mouse models disrupts cycling of clock genes and metabolic genes in adipose tissue and causes phase shifts in food intake, with animals consuming more calories during their normal rest period [73]. This disruption includes altered BMAL1 DNA binding and subsequent changes in rhythmic transcription of metabolic pathway genes [73]. The brown adipose tissue clock also regulates thermogenic capacity, with rhythmic genes controlling adipogenesis, lipogenesis, and lipid catabolism to optimize energy dissipation during appropriate circadian phases [73]. Human studies reveal attenuated circadian clock function in omental and subcutaneous adipose tissue of obese, insulin-resistant individuals, associated with reduced amplitude in non-esterified fatty acid rhythms and altered expression of inflammatory and fibrotic markers [73]. Weight loss interventions restore rhythm amplitude in clock gene expression and improve metabolic parameters, demonstrating plasticity in this system [73].
Table 2: Circadian Disruption and Metabolic Parameters
| Metabolic Parameter | Effect of Circadian Disruption | Proposed Mechanism | Experimental Evidence |
|---|---|---|---|
| Body Weight | Increased adiposity, particularly visceral fat | Reduced energy expenditure; mistimed eating | HFD-fed mice show 25-30% greater weight gain with circadian disruption |
| Glucose Homeostasis | Insulin resistance; elevated fasting glucose | Disrupted hepatic glucose production; impaired insulin secretion | 27% reduction in insulin sensitivity after 3 days of circadian misalignment in humans |
| Lipid Metabolism | Elevated triglycerides; reduced HDL | Altered expression of lipogenic and lipolytic genes | Shift workers show 20-40% higher triglyceride levels compared to day workers |
| Blood Pressure | Loss of nocturnal dipping; hypertension | Altered autonomic balance; endothelial dysfunction | 75% of shift workers show non-dipping BP pattern vs. 25% of day workers |
Experimental Models and Methodologies
Animal models have been instrumental in elucidating the causal relationships between circadian disruption and metabolic dysfunction. Key methodologies include:
Genetic Manipulation Models: Tissue-specific knockout of core clock genes (Bmal1, Clock, Per, Cry) in metabolic tissues (liver, adipose, pancreas) reveals tissue-specific contributions to systemic metabolism. For example, Bmal1 knockout in the liver disrupts glucose homeostasis and lipid metabolism, while adipose-specific deletion impairs lipid storage and adipokine secretion [72] [73].
Environmental Disruption Models: Experimental chronodisruption through altered light-dark cycles (e.g., chronic jet lag models) or timed feeding during normal rest periods recapitulates shift work conditions. These models demonstrate that mistimed food intake alone can decouple peripheral clocks from the central pacemaker, leading to metabolic dysregulation even without genetic manipulation [73].
High-Fat Diet Feeding: Providing high-fat diet ad libitum to mice disrupts circadian organization of feeding behavior and metabolic gene expression, creating a vicious cycle where metabolic dysfunction begets further circadian disruption [73].
Table 3: Research Reagent Solutions for Circadian Metabolic Studies
| Reagent/Catalog Number | Application | Experimental Function |
|---|---|---|
| Anti-BMAL1 Antibody | Immunoblotting, IHC, ChIP | Detection and quantification of core clock protein expression and localization |
| Corticosterone/EIA Kit | Hormone profiling | Measurement of circadian HPA axis rhythmicity in serum/plasma |
| CLOCK:BMAL1 Transcriptional Activity Assay | Functional screening | Assessment of molecular clock function in cell-based systems |
| Prolumi Melatonin Assay Kit | Phase determination | Sensitive detection of melatonin rhythm phase markers |
| Circadian Metabolomics Panel | Metabolic profiling | Comprehensive analysis of circadian metabolites in biofluids/tissues |
Cardiovascular Disease
Circadian Regulation of Cardiovascular System
The cardiovascular system exhibits profound circadian rhythms in function, with blood pressure, heart rate, vascular tone, and endothelial function all displaying significant time-of-day variations [71] [74]. Blood pressure typically follows a biphasic pattern with nocturnal dipping during sleep and a morning surge upon waking, while heart rate peaks during daytime activity and declines during nocturnal rest [71] [74]. These rhythms are not merely responses to behavioral cycles but reflect endogenous circadian regulation, as demonstrated by constant routine protocols that eliminate environmental influences [71]. At the molecular level, core clock genes in cardiovascular tissues regulate the expression of key determinants of vascular function, including nitric oxide (NO) and endothelin-1 (ET-1), which exhibit opposing circadian profiles that modulate vascular tone [71]. The autonomic nervous system also shows circadian variation, with sympathetic dominance during daytime and parasympathetic dominance at night, further contributing to cardiovascular rhythms [71].
Mechanisms Linking Circadian Disruption to Cardiovascular Pathophysiology
Chronic circadian disruption promotes cardiovascular disease through multiple interconnected pathways, with shift workers demonstrating a 20-40% increased risk of developing cardiovascular diseases including hypertension, atherosclerosis, and myocardial infarction [71] [76] [74]. The mechanisms include:
Endothelial Dysfunction: Circadian misalignment impairs endothelial function by reducing nitric oxide bioavailability and increasing oxidative stress. Melatonin, whose secretion is suppressed by artificial light at night, normally exerts antioxidant and anti-inflammatory effects on the endothelium; its reduction exacerbates vascular inflammation [71].
Autonomic Imbalance: Disruption of normal sleep-wake cycles causes sympathetic overactivity with reduced parasympathetic tone, promoting hypertension, cardiac arrhythmias, and increased myocardial oxygen demand [71] [74].
Metabolic Dysregulation: As described in Section 3, circadian disruption promotes insulin resistance and dyslipidemia, which accelerate atherosclerosis and increase cardiovascular risk [75] [71].
Coagulation and Fibrinolysis: Circadian clocks regulate platelet aggregability and fibrinolytic activity, with misalignment predisposing to a prothrombotic state that elevates risk for myocardial infarction and stroke [71].
Figure 2: Pathophysiological Pathways from Circadian Disruption to Cardiovascular Disease. Circadian disruption promotes cardiovascular disease through multiple interconnected mechanisms including endothelial dysfunction, autonomic imbalance, metabolic dysregulation, and prothrombotic states.
Chronotherapeutic Approaches
The growing understanding of circadian cardiovascular regulation has informed chronotherapeutic strategies aimed at optimizing treatment timing relative to biological rhythms. These include:
Timed Antihypertensive Administration: Dosing time significantly influences the efficacy of antihypertensive medications, with bedtime administration of at least one blood pressure medication resulting in better nocturnal blood pressure control and reduced cardiovascular event rates compared to morning dosing [71].
Time-Restricted Eating: Limiting food intake to an 8-12 hour window aligned with daytime activity improves cardiovascular risk factors including blood pressure, lipid profiles, and endothelial function, particularly when the feeding window occurs earlier in the day [71] [73].
Melatonin Supplementation: Exogenous melatonin administration in the evening can restore circadian alignment and improve blood pressure control in individuals with circadian disruption, though optimal dosing and timing require further investigation [71].
Mood Disorders
Bidirectional Relationship Between Circadian Rhythms and Mood
Mood disorders, including major depressive disorder, bipolar disorder, and seasonal affective disorder, exhibit significant heterogeneity but share common disturbances in biological rhythms that contribute to their onset, progression, and recurrence [77] [78]. Longitudinal studies reveal a bidirectional relationship between circadian dysregulation and mood disorders, suggesting that biological clock abnormalities may both signal and predispose individuals to mood episodes [77]. Insomnia and hypersomnia are both diagnostic criteria for major depressive disorder, and the degree of circadian misalignment correlates with symptom severity [78]. Genetic studies have identified associations between mood disorders and polymorphisms in core clock genes, including PER2, BMAL1, and CLOCK, providing a molecular basis for this relationship [78]. Additionally, circadian disruption by shift work is associated with a 20-30% increased risk of developing depression, while blunted circadian activity rhythms predict future mood instability and depressive episodes [78].
Neurobiological Mechanisms
The mechanisms linking circadian disruption to mood disorders involve complex interactions between the circadian system, stress response pathways, and neural circuits regulating emotion:
HPA Axis Dysregulation: The hypothalamic-pituitary-adrenal axis exhibits robust circadian rhythmicity, with cortisol typically peaking in the morning and reaching a nadir at night [6] [78]. In depression, this rhythm is flattened, with elevated evening cortisol and reduced amplitude [78]. Circadian disruption can directly cause HPA axis abnormalities, while stress-induced glucocorticoid secretion can feedback to disrupt circadian timekeeping, creating a vicious cycle [78].
Monoaminergic Signaling: Circadian clocks regulate the expression and function of monoamine transporters and receptors, with disruption altering serotonin, dopamine, and norepinephrine signaling in brain regions critical for mood regulation [77] [78].
Neuroplasticity and Neurogenesis: Circadian clocks regulate rhythms in hippocampal neurogenesis and synaptic plasticity, processes impaired in depression and modulated by antidepressant treatments [78]. Circadian disruption reduces neurotrophic factor expression and impairs neuronal connectivity in prefrontal-limbic circuits [78].
Developmental Programming: Early-life circadian disruption, including prenatal stress and glucocorticoid exposure, can permanently alter the development of circadian and stress response systems, increasing vulnerability to mood disorders later in life [78].
Chronobiological Interventions
The intimate connection between circadian rhythms and mood has inspired the development of chronobiological interventions for mood disorders:
Light Therapy: Timed bright light exposure is a well-established treatment for seasonal affective disorder and shows efficacy for non-seasonal depression, with morning light typically producing the greatest phase-advancing effects and antidepressant benefits [77].
Dark Therapy/Sleep Phase Advancement: Controlled darkness and strategic sleep scheduling can help realign circadian phase in bipolar disorder, with evidence supporting their role in stabilizing mood and preventing manic episodes [77].
Melatonin Agonists: Melatonin and melatonin receptor agonists (e.g., ramelteon, agomelatine) can help reset circadian phase and have demonstrated antidepressant effects, particularly in individuals with documented circadian disruption [77] [6].
Timed Pharmacotherapy: Administration of certain antidepressants at specific times of day may enhance efficacy and reduce side effects, though optimal timing varies by medication mechanism and individual circadian phenotype [77].
The evidence reviewed demonstrates that circadian desynchrony represents a significant risk factor for metabolic syndrome, cardiovascular disease, and mood disorders through complex interactions between environmental disruptors, genetic susceptibility, and dysregulated endocrine signaling. The bidirectional relationships between circadian disruption and these conditions create vicious cycles that accelerate disease progression and complicate treatment. Future research should focus on developing precise circadian biomarkers for diagnostic and prognostic applications, refining chronotherapeutic protocols for individualized medicine, and identifying novel targets that modulate clock function for therapeutic benefit. The integration of circadian biology into clinical practice represents a promising frontier for preventing and treating these prevalent conditions, with potential for significant public health impact. As our understanding of the intricate connections between circadian rhythms and health continues to deepen, so too will opportunities for innovative interventions that restore temporal harmony to physiological systems.
The regulation of circadian rhythms represents a fundamental biological process that synchronizes physiological functions with the 24-hour light-dark cycle. Within this complex regulatory network, the endocrine system serves as both a clock-controlled output and a feedback modulator of circadian timing. Sleep disorders disrupt this precise coordination, leading to hormonal imbalances that further exacerbate circadian disruption, creating a self-perpetuating cycle of physiological dysregulation. Understanding these bidirectional relationships is critical for developing targeted chronotherapeutic interventions for metabolic, cardiovascular, and neuropsychiatric conditions.
The suprachiasmatic nucleus (SCN) of the hypothalamus functions as the central pacemaker, coordinating peripheral clocks throughout the body via neural, hormonal, and behavioral outputs [6]. This master clock regulates the timing of hormone release, while hormonal signals in turn provide feedback to fine-tune circadian phase and amplitude. Sleep architecture, specifically the alternation between non-rapid eye movement (NREM) and rapid eye movement (REM) sleep stages, plays a crucial role in organizing the temporal secretion patterns of various hormones [30]. The disruption of this delicate interplay forms the pathophysiological basis for the relationship between sleep disorders and endocrine dysfunction.
Molecular Mechanisms of Circadian-Hormonal Crosstalk
Core Clock Machinery and Hormonal Regulation
The molecular circadian clock consists of interlocking transcription-translation feedback loops that generate approximately 24-hour rhythms in gene expression. The core loop involves the heterodimerization of BMAL1 and CLOCK proteins, which activate transcription of Period (Per1-3) and Cryptochrome (Cry1/2) genes [6] [74]. PER and CRY proteins subsequently form complexes that inhibit BMAL1:CLOCK activity, completing the negative feedback loop. Auxiliary loops involving REV-ERBs and RORs provide additional stability and regulatory input.
Table 1: Core Clock Components and Their Hormonal Interactions
| Clock Component | Function | Hormonal Influences |
|---|---|---|
| BMAL1:CLOCK | Core transcriptional activators | Glucocorticoid response elements (GREs) in promoter regions |
| PER/CRY | Transcriptional repressors | Insulin affects nuclear translocation |
| REV-ERBα/β | Transcriptional repressors | Regulated by thyroid hormones; target for nuclear receptor drugs |
| RORα/β/γ | Transcriptional activators | Altered by estrogen signaling |
Hormones can influence circadian rhythms through three principal mechanisms: as rhythm drivers that directly regulate rhythmic gene expression through hormone-response elements; as zeitgebers that reset tissue clock phase; and as tuners that modify downstream rhythms without directly affecting the core clock [6]. For example, glucocorticoids function as both rhythm drivers through glucocorticoid response elements (GREs) in target genes and as zeitgebers through GREs in Per gene promoters.
Sleep Architecture and Hormonal Secretion Patterns
Sleep is organized into cyclic alternations between NREM (stages N1-N3) and REM sleep, with each stage exerting distinct effects on hormonal secretion. NREM sleep, particularly slow-wave sleep (SWS), is associated with increased growth hormone (GH) release, suppressed thyroid-stimulating hormone (TSH) secretion, and reduced cortisol levels [30]. In contrast, REM sleep influences the timing of testosterone secretion and activates the sympathetic nervous system, which can disrupt insulin secretion and increase diabetes risk.
The progression through sleep stages follows a predictable architecture across the night, with SWS dominating the first half and REM sleep concentrated in the latter half. This organization creates a temporal framework for hormonal release, with pulsatile secretion of many hormones locked to specific sleep stages rather than simply following a circadian pattern [30]. The first SWS period, occurring approximately 90 minutes after sleep onset, is associated with the largest GH pulse, while testosterone levels peak during REM sleep episodes in the early morning hours.
Impact of Sleep Disorders on Specific Hormonal Axes
Hypothalamic-Pituitary-Adrenal (HPA) Axis
The HPA axis exhibits a robust circadian rhythm, with cortisol levels typically lowest around midnight, rising in the early morning hours, peaking within the first hour after waking (cortisol awakening response), and gradually declining throughout the day [30] [6]. Sleep disorders significantly disrupt this pattern, with insomnia and sleep deprivation associated with elevated evening cortisol levels, flattened diurnal rhythm, and heightened HPA axis activation [30]. This hypercortisolemia contributes to insulin resistance, increased inflammatory responses, and potentially accelerates neurodegenerative processes.
Table 2: Sleep Disorder Effects on Major Hormonal Axes
| Hormonal Axis | Normal Sleep-Associated Secretion | Effect of Sleep Disorders |
|---|---|---|
| HPA Axis (Cortisol) | Nadir during early sleep, peak at awakening | Elevated evening levels, flattened rhythm, increased overall secretion |
| HPT Axis (TSH, T3/T4) | Nocturnal TSH rise, daytime decline | Blunted TSH rhythm, altered peripheral conversion of T4 to T3 |
| HPG Axis (Gonadal Hormones) | Testosterone peak during REM sleep; sleep-dependent prolactin release | Reduced testosterone, lower FSH, disrupted LH pulsatility |
| Somatotropic Axis (GH) | Major pulse during first SWS period | Reduced GH secretion, impaired tissue repair |
Experimental protocols for assessing HPA axis function in sleep disorders typically involve frequent blood sampling (every 15-30 minutes) over 24 hours under controlled conditions, with simultaneous polysomnographic recording to correlate hormonal measures with sleep architecture. Salivary cortisol measurements provide a less invasive alternative for assessing diurnal rhythm, particularly when measuring the cortisol awakening response.
Hypothalamic-Pituitary-Thyroid (HPT) Axis
Thyroid-stimulating hormone (TSH) demonstrates a characteristic circadian pattern, with levels increasing prior to sleep, reaching peak concentrations at night, and declining upon waking [30]. Total sleep deprivation induces central hypothyroidism by suppressing thyrotropin-releasing hormone (TRH) secretion, while REM sleep deprivation specifically decreases TSH secretion and reduces circulating thyroxine (T4) levels [30]. Interestingly, sleep deprivation also enhances deiodinase type 2 (D2) activity in brown adipose tissue, increasing conversion of T4 to the more biologically active T3, suggesting complex regulation across different tissue compartments.
Methodological considerations for studying HPT axis in sleep disorders must account for pulsatile TSH secretion, with sampling intervals of at least 20 minutes required to accurately characterize rhythm parameters. The timing of blood sampling relative to sleep-wake transitions is critical, as the TSH rhythm is more closely linked to sleep onset than to the light-dark cycle.
Hypothalamic-Pituitary-Gonadal (HPG) Axis
Sleep significantly influences reproductive hormone secretion, with distinct patterns observed in males and females. In men, testosterone levels increase with prolonged sleep duration, peaking during the early morning hours in association with REM sleep episodes [30]. Disruption of sleep architecture, particularly reduced REM sleep, directly impairs testosterone secretion. In women, follicle-stimulating hormone (FSH) levels correlate positively with sleep duration, with short sleep duration (<8 hours) associated with 20% lower FSH levels after adjusting for age and BMI [30].
Prolactin secretion follows a sleep-dependent pattern, with higher levels during sleep and lower levels during wakefulness [30]. Sleep deprivation consequently reduces prolactin levels, potentially affecting its diverse functions in reproduction, metabolism, and immune regulation. Research methodologies for investigating HPG axis in sleep disorders must account for menstrual cycle phase in premenopausal women and consider the pulsatile nature of gonadotropin-releasing hormone (GnRH) secretion.
Metabolic Hormones and Appetite Regulation
Sleep duration and quality significantly impact hormones regulating appetite and energy homeostasis. Leptin, which signals satiety, typically increases during sleep, while ghrelin, which stimulates appetite, decreases. Sleep restriction reverses these patterns, reducing leptin and increasing ghrelin levels, potentially promoting weight gain and insulin resistance [30]. The sympathetic nervous system activation during disrupted sleep further contributes to metabolic dysregulation, particularly during REM sleep when significant cardiovascular and respiratory fluctuations occur.
Research methodologies for metabolic hormone assessment typically involve frequent sampling (hourly or more frequently) under controlled nutritional conditions, with careful standardization of meal timing and composition. Hyperinsulinemic-euglycemic clamps and oral glucose tolerance tests provide complementary measures of insulin sensitivity that correlate with sleep architecture parameters, particularly SWS duration.
Consequences of Sleep-Related Hormonal Disruption
Metabolic Dysregulation and Disease Risk
The hormonal alterations induced by sleep disorders create a metabolic milieu conducive to disease development. Insulin resistance, decreased glucose tolerance, and hepatic steatosis represent direct consequences of sleep-related endocrine changes [30]. Experimental evidence demonstrates that even short-term sleep restriction (4-5 hours/night for one week) significantly impairs insulin sensitivity to a degree comparable to established diabetes risk factors.
Longitudinal studies indicate that sleep disorders accelerate the development of diabetes, obesity, and metabolic syndrome [30]. The combination of elevated cortisol, reduced GH, altered thyroid function, and appetite dysregulation creates a synergistic metabolic burden that promotes adiposity, dyslipidemia, and cardiovascular complications. Shift workers, who experience chronic circadian misalignment, demonstrate particularly high risks for these conditions, highlighting the importance of temporal organization in metabolic health.
Cardiovascular Implications
Circadian disruption directly impacts cardiovascular function through multiple hormonal mechanisms. Blood pressure and heart rate exhibit robust diurnal variations, with a morning surge mediated by cortisol increases and adrenergic stimulation [74]. Sleep disorders disrupt this pattern, leading to non-dipping blood pressure (absence of the normal nighttime decline) and increased cardiovascular event risk. Core clock genes regulate the expression of cardiovascular genes including Hcn4 (pacemaker current) and Scn5a (cardiac sodium channel), providing direct molecular links between circadian disruption and arrhythmogenesis [74].
Table 3: Quantitative Risks of Sleep Disorder-Associated Conditions
| Condition | Risk Associated with Sleep Disorders | Key Hormonal Mediators |
|---|---|---|
| All-Cause Dementia | RR = 1.13-1.43 [79] | Cortisol, melatonin |
| Alzheimer's Disease | RR = 1.24-1.66 [79] | Melatonin, cortisol |
| Vascular Dementia | RR = 1.85-2.53 [79] | Cortisol, catecholamines |
| Diabetes/Obesity | Significantly increased risk [30] | Insulin, cortisol, leptin, ghrelin |
| Depression/Anxiety | Significant reduction with sleep improvement [80] | Cortisol, GABA, monoamines |
Neurocognitive and Mental Health Consequences
Sleep disorders substantially increase the risk of cognitive decline and dementia, with meta-analyses revealing relative risks of 1.13 for all-cause dementia, 1.24-1.66 for Alzheimer's disease, and 1.85-2.53 for vascular dementia [79]. The mechanisms linking sleep disruption to neurodegeneration involve multiple hormonal pathways, including cortisol-mediated hippocampal toxicity, reduced melatonin-mediated antioxidant activity, and impaired glymphatic clearance of beta-amyloid during deep sleep.
Mental health is profoundly influenced by sleep-related hormonal changes. Meta-analyses demonstrate that improving sleep quality significantly reduces symptoms of depression (mean difference: -2.92) and anxiety (mean difference: -1.14) compared to standard care [80]. The HPA axis dysfunction commonly observed in insomnia contributes to emotional dysregulation and negative affective states, while restoration of normal sleep architecture promotes emotional resilience.
Experimental Methodologies and Research Approaches
Assessing Circadian Hormonal Profiles
Comprehensive evaluation of circadian hormonal regulation requires specialized protocols that control for confounding factors:
Constant Routine Protocol: Participants remain awake in constant dim light, semi-recumbent position, with identical small snacks evenly distributed across the 24-hour cycle. This methodology eliminates environmental and behavioral cues, revealing endogenous circadian rhythms.
Forced Desynchrony Protocol: Subjects live on sleep-wake cycles substantially longer or shorter than 24 hours (typically 20-28 hours) in dim light conditions. This approach separates endogenous circadian rhythms from homeostatic sleep processes.
Frequent Sampling Techniques: Blood sampling at 10-60 minute intervals via indwelling catheters to characterize pulsatile hormone secretion. Less invasive salivary and urinary measurements provide alternatives for field studies.
These protocols typically incorporate polysomnography to correlate hormonal measures with sleep architecture parameters, including sleep stages, arousal frequency, and spectral characteristics of the EEG.
Molecular and Genetic Approaches
Advanced techniques enable investigation of molecular mechanisms underlying circadian-hormonal interactions:
Tissue-Specific Clock Gene Expression: Assessment of clock gene rhythms in peripheral tissues using biopsies collected across the circadian cycle, with careful attention to collection time documentation.
Epigenetic Analyses: Investigation of DNA methylation and histone modifications in clock gene promoters and hormone response elements in response to sleep disruption.
Chromatin Immunoprecipitation: Determination of BMAL1:CLOCK binding to hormone gene promoters and nuclear hormone receptor binding to clock gene regulatory elements.
These molecular approaches complement physiological measures to provide integrated understanding of mechanisms linking sleep disorders to hormonal imbalance.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Circadian-Hormonal Investigations
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Hormone Assays | ELISA, RIA, LC-MS/MS kits for cortisol, melatonin, GH | Quantitative hormone measurement in blood, saliva, urine |
| Sleep Staging | Polysomnography systems, EEG/EMG/EOG electrodes | Objective sleep architecture assessment |
| Actigraphy | Wrist-worn activity monitors with light sensors | Long-term circadian rhythm monitoring in natural environment |
| Core Clock Reporters | PER2::LUCIFERASE, Bmal1-ELuc transgenic cells/systems | Real-time monitoring of molecular clock function |
| Hormone Modulators | Mifepristone (GR antagonist), Luzindole (MT2 antagonist) | Mechanistic dissection of specific hormonal pathways |
| Genetic Models | Clock mutant mice, Bmal1 knockout, tissue-specific deletions | Determining causal relationships in hormonal regulation |
Chronotherapeutic Implications and Future Directions
The intricate relationship between sleep disorders and hormonal imbalance presents compelling opportunities for chronotherapeutic interventions. Timing of hormonal replacement therapies to align with endogenous secretory patterns can enhance efficacy and reduce side effects [81]. For example, evening administration of melatonin synergizes with its physiological rise to improve sleep initiation, while morning glucocorticoid replacement more closely mimics the cortisol awakening response.
Future research directions should focus on:
Personalized Chronotherapy: Individualizing treatment timing based on chronotype, genetic polymorphisms in clock genes, and hormonal rhythm characteristics.
Tissue-Specific Clock Targeting: Developing interventions that selectively reset pathological circadian rhythms in specific tissues without disrupting overall synchrony.
Digital Health Integration: Utilizing wearable technology to continuously monitor sleep and physiological parameters, enabling dynamic adjustment of therapeutic interventions.
Multi-omics Approaches: Integrating transcriptomic, proteomic, and metabolomic data to comprehensively characterize the impact of sleep disorders on endocrine function.
Understanding the bidirectional relationship between sleep disorders and hormonal imbalance provides not only insight into fundamental physiological regulation but also opens innovative avenues for treating the growing spectrum of circadian rhythm-related disorders. As research in this field advances, the integration of circadian biology into endocrine practice promises more physiological and effective approaches to restoring metabolic health.
The endocrine system serves as a crucial mediator between the central circadian clock in the suprachiasmatic nucleus (SCN) and peripheral tissue functions, coordinating metabolic homeostasis with the 24-hour light-dark cycle. Circadian rhythms are ~24-hour biological cycles in behavior, metabolism, and physiology governed by the SCN, which receives photic input from the retina and synchronizes peripheral oscillators throughout the body [82] [83]. The SCN regulates endocrine functions through humoral and autonomic nervous system outputs, notably controlling melatonin secretion from the pineal gland during the biological night and modulating cortisol rhythms and other metabolic hormones [82] [83]. Disruption of these circadian-endocrine axes—through artificial light exposure, irregular eating patterns, or shift work—increases risk for metabolic diseases, mental health disorders, and cancer [82] [84] [68]. Time-restricted eating (TRE) and light therapy represent potent behavioral interventions that target these circadian-endocrine pathways to restore rhythmicity and improve health outcomes.
Time-Restricted Eating: Mechanisms and Protocols
Molecular Mechanisms Linking TRE to Endocrine Function
Time-restricted eating synchronizes the circadian timing of food intake to protect against metabolic diseases by aligning nutrient sensing with circadian gene expression [84]. At a molecular level, TRE coordinates the circadian clock system with nutrient-sensing pathways through several key mechanisms:
Circadian Clock Gene Regulation: TRE influences core clock components (CLOCK, BMAL1, PER, CRY) that coordinate metabolic processes with the light-dark cycle [84]. This regulation ensures that anabolic and catabolic pathways are active at appropriate times.
Nutrient-Sensing Pathway Integration: TRE activates key nutrient sensors including AMPK, SIRT1, and mTOR, which interact with circadian proteins to optimize metabolic efficiency [85] [84]. AMPK activation during fasting periods promotes mitochondrial biogenesis and autophagy, while mTOR signaling during feeding windows supports protein synthesis and cell growth.
Endocrine Hormone Regulation: TRE modulates insulin sensitivity, leptin signaling, and ghrelin secretion [86] [84]. Early TRE (eTRE) particularly enhances insulin sensitivity during morning hours when insulin responsiveness is naturally highest, leading to improved glucose control [86].
Hepatic Metabolic Function: In the liver, TRE synchronizes the expression of genes involved in glucose metabolism, lipid processing, and cholesterol homeostasis through regulation of transcriptional factors like PPARγ, LXR, and RXR [84].
The coordination between these systems optimizes metabolic homeostasis by ensuring that feeding-fasting cycles align with endogenous circadian rhythms in endocrine function.
Experimental Protocols and Clinical Evidence
Table 1: Key Clinical Studies on Time-Restricted Eating
| Study Reference | Participant Characteristics | Intervention Protocol | Primary Endocrine/Metabolic Outcomes |
|---|---|---|---|
| [86] | N=90; BMI 25-35 kg/m² with metabolic syndrome features | 3-month RCT: eTRE+ER (8h window, 8:00-16:00), lTRE+ER (12:00-20:00), or ER alone (12h window) | eTRE+ER showed greater reductions in fat mass, BMI, fasting glucose, and leptin levels compared to other groups |
| [87] | N=90 with obesity and T2D; mean age 36.8, HbA1c 7.42% | 16-week RCT: IER (5:2), TRE (10h window), or CER | IER showed advantages in reducing fasting glucose, improving insulin sensitivity (Matsuda index), and lowering triglycerides; all groups improved HbA1c |
Standardized TRE Research Protocol:
Participant Screening and Chronotype Assessment:
Intervention Randomization and Design:
- Randomize participants based on chronotype: morning types to eTRE or control groups; evening types to lTRE or control [86]
- Define eating windows: eTRE (e.g., 8:00-16:00), lTRE (e.g., 12:00-20:00), control (12-hour window) [86]
- Isocaloric design: match daily caloric intake and macronutrient distribution across groups [86]
Outcome Measurements and Adherence Monitoring:
- Primary endpoints: body weight, body composition, fasting glucose, insulin sensitivity indices [86]
- Secondary endpoints: lipid profile, liver enzymes, appetite hormones (leptin, ghrelin, adiponectin) [86]
- Adherence tracking: Food diaries, time-stamped photographs of meals, or digital platform reporting [86]
Research Reagent Solutions for TRE Studies
Table 2: Essential Research Materials for TRE Investigations
| Reagent/Material | Specific Application | Research Function |
|---|---|---|
| Morningness-Eveningness Questionnaire (MEQ) | Participant screening | Chronotype classification for appropriate intervention assignment |
| ELISA Kits (Leptin, Ghrelin, Adiponectin) | Plasma/serum analysis | Quantification of appetite and metabolic hormones |
| Continuous Glucose Monitoring Systems | Interstitial glucose measurement | Assessment of 24-hour glycemic patterns and variability |
| Indirect Calorimetry Systems | Metabolic rate assessment | Measurement of resting energy expenditure and substrate utilization |
| Actigraphy Devices | Physical activity and sleep tracking | Objective monitoring of activity rhythms and sleep-wake cycles |
| Dual-Energy X-ray Absorptiometry (DEXA) | Body composition analysis | Precise measurement of fat mass, lean mass, and bone density |
Light Therapy: Mechanisms and Protocols
Neuroendocrine Pathways of Light Action
Light therapy exerts its effects through specialized photoreceptors in the retina that project to circadian and neuroendocrine centers in the brain:
Retinal Photoreceptors: Intrinsically photosensitive retinal ganglion cells (ipRGCs) containing melanopsin are primarily responsible for circadian phototransduction, with peak sensitivity around 480 nm (blue light) [82]. These ipRGCs also receive input from rods and cones, integrating light signals across the visual spectrum [82].
Central Circadian Pathway: The retinohypothalamic tract projects directly from ipRGCs to the SCN, the master circadian pacemaker [82]. The SCN then regulates pineal melatonin secretion via a multisynaptic pathway, with light exposure suppressing melatonin during daytime hours [82] [89].
Neuroendocrine Outputs: The SCN coordinates endocrine function through several pathways: (1) autonomic projections regulating pineal melatonin synthesis; (2) paraventricular nucleus projections controlling cortisol rhythm via the HPA axis; and (3) direct and indirect regulation of other neuroendocrine systems [82].
Non-Vinal Pathways: Emerging evidence suggests retinal projections to the habenula may mediate mood-related effects of light, providing a potential pathway for light therapy's antidepressant effects [82].
The timing, intensity, duration, and spectral characteristics of light exposure determine its phase-shifting properties, with morning light typically producing phase advances and evening light producing phase delays.
Experimental Protocols and Clinical Applications
Table 3: Light Therapy Parameters for Circadian Rhythm Alignment
| Disorder | Timing | Intensity | Duration | Evidence Level |
|---|---|---|---|---|
| Delayed Sleep Phase Syndrome | Upon awakening or gradually advancing before awakening | 10,000 lux | 30-90 minutes | Well-established [90] |
| Advanced Sleep Phase Syndrome | Evening | 10,000 lux | 30-90 minutes | Moderate [90] |
| Non-24-Hour Sleep-Wake Rhythm | Morning | 10,000 lux | 30-90 minutes | Clinical support [90] |
| Dementia-Related Circadian Disruption | Morning (phase delay) or Evening (phase advance) based on individual phase | 2,500 lux | 2 hours | Clinical trials [89] |
Standardized Light Therapy Research Protocol:
Pre-Intervention Assessment:
Intervention Parameters:
- Light source: Full-spectrum fluorescent light boxes with UV filtration [90] [89]
- Intensity: 2,500-10,000 lux at eye level [90] [89]
- Timing: Based on desired phase shift and individual circadian phase [90]
- Duration: 30 minutes to 2 hours daily, depending on intensity [90] [89]
- Positioning: Approximately 1 meter from participant at a 45° visual angle [89]
Outcome Measures:
Research Reagent Solutions for Light Therapy Studies
Table 4: Essential Research Materials for Light Therapy Investigations
| Reagent/Material | Specific Application | Research Function |
|---|---|---|
| Actigraphy Devices | Sleep-wake pattern monitoring | Objective measurement of rest-activity rhythms and sleep parameters |
| Melatonin ELISA/Saliva Kits | Dim Light Melatonin Onset (DLMO) | Gold standard assessment of circadian phase position |
| Portable Light Meters | Ambient light measurement | Quantification of personal light exposure in lux and circadian-effective irradiance |
| Dedicated Light Therapy Lamps | Light intervention delivery | Controlled administration of specific light intensities and spectra |
| Validated Mood Scales (HAM-D, SPAQ) | Affective state assessment | Measurement of depressive symptoms and seasonal pattern variations |
Circadian-Endocrine Integration in Drug Development
The circadian system significantly influences drug efficacy and toxicity through circadian regulation of drug metabolism, target pathways, and elimination processes. Understanding these temporal patterns creates opportunities for chronotherapy approaches in pharmaceutical development:
Circadian Pharmacokinetics: Cytochrome P450 enzymes, drug transporters, and metabolic pathways show circadian oscillations, leading to time-dependent drug clearance [68]. For instance, enzymes like CYP3A4 display circadian expression patterns in the liver, potentially creating optimal timing windows for drug administration.
Cellular Pathway Regulation: Core circadian genes regulate up to 60% of protein-coding genes in various cell types, including those involved in DNA repair, cell cycle progression, and apoptosis [68]. This creates temporal windows of vulnerability for cancer cells to chemotherapeutic agents.
Experimental Approaches: Recent combined mathematical and experimental frameworks systematically investigate factors influencing time-of-day drug sensitivity, including circadian properties (amplitude, period) and drug characteristics (half-life, mechanism) [68]. These models simulate how circadian modulation affects effective drug concentration and treatment outcomes.
Translation to Clinical Practice: While promising, chronotherapy approaches require deeper mechanistic insights and stringent clinical validation before widespread implementation [68]. Current research focuses on identifying biomarkers of circadian timing to personalize drug administration schedules.
Time-restricted eating and light therapy represent scientifically grounded behavioral interventions that target fundamental circadian-endocrine pathways. TRE optimizes metabolic health by aligning nutrient intake with circadian rhythms in endocrine function and metabolic processing, while light therapy directly modulates the central circadian pacemaker to restore appropriate neuroendocrine timing. For researchers and drug development professionals, understanding these mechanisms provides opportunities for developing novel chronotherapeutic approaches that optimize treatment timing for metabolic diseases, mental health disorders, and cancer. Future research should focus on personalized application of these interventions based on individual circadian phenotypes and genetic profiles, ultimately enhancing precision medicine approaches through circadian optimization.
The circadian rhythm, a nearly 24-hour internal biological clock, is a fundamental physiological process that enables organisms to anticipate and adapt to daily environmental changes. [6] [91] This rhythm is governed by a cell-autonomous molecular oscillator present in most cells, consisting of interlocking transcription-translation feedback loops (TTFLs). [24] The core positive limb of this loop involves the heterodimerization of the transcription factors CLOCK (or NPAS2) and BMAL1, which activate the expression of period (Per1-3) and cryptochrome (Cry1/2) genes. [6] [24] The PER and CRY proteins then form complexes that suppress CLOCK-BMAL1 activity, completing the negative feedback loop. [24]
The endocrine system plays a crucial role in the temporal coordination of physiological processes, with many hormones exhibiting robust circadian oscillations. [6] [35] These include melatonin, cortisol, growth hormone, adiponectin, and insulin. [35] Hormones can influence circadian rhythms in three principal ways: (1) as rhythm drivers by directly regulating rhythmic gene expression in target tissues independent of the local clock; (2) as zeitgebers (time-givers) that reset the phase of local circadian clocks; and (3) as tuners that modulate the amplitude of circadian output rhythms without affecting the core clock mechanism. [6] This intricate interaction positions the endocrine system as a key mediator of circadian organization and a promising target for therapeutic interventions aimed at circadian-related disorders.
REV-ERB: A Core Circadian Repressor
Molecular Structure and Function
REV-ERBα (NR1D1) and REV-ERBβ (NR1D2) are nuclear receptors that function as transcriptional repressors and are integral components of the auxiliary feedback loop that stabilizes the core circadian oscillator. [91] [24] Unlike most nuclear receptors, REV-ERBs lack the C-terminal activation function-2 (AF2) domain, which prevents them from recruiting co-activators and limits their function to transcriptional repression. [92] [91] [93] REV-ERBs exert their repressive function by binding to ROR response elements (ROREs) in the promoter regions of target genes and recruiting the nuclear receptor corepressor (NCoR)/histone deacetylase 3 (HDAC3) complex, leading to chromatin condensation and suppression of transcription. [92] [91]
The endogenous ligand for REV-ERB is heme, which binds to its ligand-binding domain and modulates its interaction with corepressors. [91] The discovery of heme as a natural ligand revealed that REV-ERB serves as a metabolic sensor, linking cellular energy status with circadian gene expression. [91]
Role in the Circadian Network
Within the circadian clock network, the CLOCK-BMAL1 heterodimer activates the transcription of Rev-erbα and Rev-erbβ. [24] In turn, REV-ERB proteins repress the expression of Bmal1 and Clock, thereby creating a stabilizing feedback loop that reinforces circadian rhythmicity. [24] This regulatory dynamic makes REV-ERB a critical node for pharmacological manipulation of the circadian clock, as modulating its activity can directly influence the period and phase of circadian rhythms.
Development of REV-ERB Agonists: From Proof-of-Concept to Clinical Candidates
The development of synthetic REV-ERB ligands has progressed significantly, with successive generations showing improved potency, specificity, and pharmacokinetic profiles.
Table 1: Evolution of Key REV-ERB Agonists
| Compound | Discovery/Report Year | Key Characteristics | Therapeutic Potential | Limitations |
|---|---|---|---|---|
| GSK4112 | 2008 [92] | First synthetic REV-ERB agonist identified via FRET screening. [92] | Reduces IL-6 in macrophages; reduces fibrosis in human lung fibroblasts. [92] [94] | Poor pharmacokinetic profile, limiting preclinical use. [92] |
| SR9009 & SR9011 | ~2012 [92] | Show better potency and bioavailability than GSK4112. [92] | Reduces fat mass in obese mice; improves dyslipidemia; inhibits Th17 cell differentiation. [92] [95] | Reports of nonspecific binding or REV-ERB-independent effects. [92] |
| SR12418 | ~Post SR9009 [92] | Improved pharmacokinetic profile. [92] | Suppresses Th17-driven autoimmunity and colitis in mice. [92] | Limited data on full pharmacological profile. |
| Tetrahydroiso-quinolines (THIQ1-4) | ~Post SR12418 [92] | Longer half-life and lower plasma clearance. [92] | Promising scaffold for further development. [92] | Poor oral bioavailability. [92] |
| STL1267 | 2022 [92] | Non-porphyrin-based, high-affinity and specificity; 10x greater potency than SR9009; improved cell viability. [92] | Enhances fatty acid oxidation and mitochondrial function genes; reduced Bmal1 expression in mouse liver. [92] | Specificity for serotonin transporter and kappa opioid receptor requires evaluation. [92] |
Recent Advancements: STL1267
The recently developed agonist STL1267 represents a significant step forward. It is a non-porphyrin-based synthetic agonist that binds REV-ERB with very high specificity and regulates target genes more efficiently than SR9009. [92] Its binding mode is distinct from the natural heme ligand, which may contribute to its specificity. [92] In vitro, STL1267 was nearly twice as effective as SR9009 at recruiting NCoR to REV-ERBα and showed 10-fold greater potency. [92] It also demonstrated improved cell viability in C2C12 and HepG2 cells and enhanced the expression of genes related to fatty acid oxidation and mitochondrial biogenesis more prominently than SR9009. [92] Furthermore, STL1267 exhibited improved pharmacokinetics and bioavailability in key metabolic tissues (liver, skeletal muscle, adipose tissue) and the brain in mice. [92]
Signaling Pathways and Therapeutic Mechanisms
REV-ERB agonists influence a wide array of physiological processes through direct transcriptional repression of key target genes. The diagram below illustrates the core circadian feedback loop and the primary signaling pathways through which REV-ERB activation exerts its therapeutic effects.
Key Therapeutic Applications
Inflammation and Pain: REV-ERB agonists directly repress the transcription of pivotal pro-inflammatory mediators, including NLRP3 and IL-1β. [93] This suppression underlies their efficacy in models of inflammatory pain, where agonists like SR9009 and STL1267 reduced inflammatory signaling in human monocytes and microglia. [93]
Metabolic Disorders: Agonists such as SR9009 and the newer STL1267 alter the expression of metabolic genes in the liver, skeletal muscle, and adipose tissue. [92] This results in increased energy expenditure, reduced fat mass, improved glucose homeostasis, and lowered plasma lipids in diet-induced obese mice. [92] [95]
Sleep and Anxiety: Pharmacological activation of REV-ERB with SR9011 or SR9009 administered during the sleep phase increases wakefulness and reduces both REM and non-REM sleep in mice. [95] Interestingly, these agonists also reduce anxiety-like behavior, suggesting potential for treating sleep and anxiety disorders. [95]
Fibrosis: In pulmonary fibrosis models, the REV-ERB agonist GSK4112 reduces the expression of collagen, fibronectin, and α-smooth muscle actin in human lung fibroblasts. [92] [94] Genetic deletion of REV-ERBα in mouse lungs exacerbates bleomycin-induced fibrosis, confirming its protective role. [92]
Experimental Protocols for Evaluating REV-ERB Agonists
In Vitro Assessment of Inflammatory Marker Suppression
This protocol is used to validate the anti-inflammatory efficacy of REV-ERB agonists in human cell lines. [93]
Cell Culture and Differentiation:
- Culture human monocyte THP-1 cells in RPMI-1640 media with 10% FBS.
- Differentiate into macrophages by treating with phorbol 12-myristate 13-acetate (PMA, 100 nM) for 24 hours.
- Wash cells and allow to recover in PMA-free media for 72 hours.
Compound Pre-treatment:
- Pre-treat differentiated THP-1 cells with the REV-ERB agonist (e.g., 10 µM SR9009 or STL1267) or vehicle control (DMSO) for 24 hours.
Inflammatory Challenge:
- Replace media with fresh media containing an inflammatory stimulus such as lipopolysaccharide (LPS, 250 ng/mL) and interferon-gamma (IFNγ, 20 ng/mL) for 48 hours. The agonist or vehicle should remain present.
Downstream Analysis:
- Gene Expression: Harvest cells for RNA extraction. Perform quantitative PCR (qPCR) to measure mRNA levels of target genes (e.g., NLRP3, IL-1β, IL-18). Normalize data to a housekeeping gene (e.g., 36B4). [93]
- Protein Secretion: Collect cell culture media. Use an enzyme-linked immunosorbent assay (ELISA) to quantify the secretion of pro-inflammatory cytokines like IL-1β. [93]
In Vivo Assessment of Circadian Period and Metabolic Function
This methodology outlines the evaluation of REV-ERB agonists in animal models. [92] [95]
Animal Models:
- Use wild-type or disease-specific mouse models (e.g., diet-induced obese mice). Rev-erbβ-null mice serve as a control to confirm on-target effects. [95]
Compound Administration:
Phenotypic Readouts:
- Circadian Gene Expression: Sacrifice animals at various time points post-injection. Isolate tissues (e.g., liver) and analyze RNA or protein. A key metric is the repression of the REV-ERB target gene Bmal1. [92]
- Sleep Architecture: Implant mice with EEG/EMG transmitters. Administer compound during the rest phase (ZT6) and monitor sleep-wake states (wakefulness, slow-wave sleep, REM sleep) for 24-48 hours. [95]
- Metabolic Phenotyping: Monitor body composition (fat mass), plasma lipids, glucose tolerance, and locomotor activity over a treatment period.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for REV-ERB Agonist Research
| Reagent / Model | Function/Application | Example Use Case | Reference |
|---|---|---|---|
| SR9009 | First-generation in vivo REV-ERB agonist. | Used to establish effects on metabolism, sleep, and inflammation in vivo. [95] [93] | [92] |
| STL1267 | Novel high-affinity, high-specificity REV-ERB agonist. | Used for proof-of-concept studies requiring high potency and reduced off-target effects. [92] [93] | [92] |
| GSK4112 | First synthetic REV-ERB agonist (proof-of-concept). | Used in early in vitro studies to elucidate REV-ERB biology. [92] [94] | [92] |
| Nr1d1-/- (KO) Mice | REV-ERBα knockout model. | Essential for validating the specificity of agonists and studying receptor function in isolation. [93] | [93] |
| THP-1 Human Monocyte Cell Line | In vitro model for human immunology. | Used to test agonist effects on inflammatory pathways (NLRP3, IL-1β) in human-derived cells. [93] | [93] |
| Bmal1-dLuc Reporter Cell Line | Real-time monitoring of circadian clock function. | Used in bioluminescence recording assays to measure changes in circadian period length in response to compounds. [96] | [96] |
Pharmacological targeting of the circadian clock, particularly through REV-ERB agonists, represents a promising frontier for treating a broad spectrum of disorders, including metabolic syndrome, chronic inflammation, sleep disorders, and fibrosis. The evolution from initial tool compounds like GSK4112 to more potent and specific agents like STL1267 underscores the growing therapeutic potential of this approach. [92] Future efforts should focus on further optimizing the pharmacokinetic profiles of these agonists, particularly their oral bioavailability and tissue-specific targeting. [92] The integration of circadian biology and pharmacology holds the key to developing novel, effective therapies that work in harmony with the body's intrinsic temporal rhythms.
Optimizing Sleep Hygiene and Environmental Cues for Circadian Alignment
Circadian rhythms are endogenous, roughly 24-hour cycles that regulate virtually all physiological processes, from cellular function to organism-level behavior. In mammals, the master circadian pacemaker is located in the suprachiasmatic nucleus (SCN) of the hypothalamus, which synchronizes peripheral clocks found in virtually every tissue and organ throughout the body [97] [98]. This hierarchical clock system ensures temporal coordination of physiological processes, including endocrine function, metabolism, and sleep-wake cycles. The regulation of sleep is processed by the homeostatic physiology of the circadian rhythm, which interacts closely with the endocrine system [97]. Levels of numerous hormones—including melatonin, cortisol, sex hormones, thyroid-stimulating hormone, and metabolic factors like leptin and ghrelin—vary significantly across the 24-hour day [6]. These hormonal rhythms are not merely outputs of the circadian system but also provide critical feedback, acting as internal time cues that reinforce circadian organization throughout the body. Understanding this intricate bidirectional relationship between circadian rhythms and endocrine function provides a scientific foundation for developing targeted interventions to optimize circadian alignment and overall health.
Molecular and Neural Mechanisms of Circadian Timekeeping
Core Molecular Clock Machinery
At the cellular level, circadian rhythms are generated by a conserved transcriptional-translational feedback loop (TTFL) comprising core clock genes and their protein products. The core clock operates as a feedback loop where CLOCK and BMAL1 proteins heterodimerize and activate the transcription of Period (Per1, Per2, Per3) and Cryptochrome (Cry1, Cry2) genes [98]. PER and CRY protein products accumulate, form complexes in the cytoplasm, and translocate back to the nucleus to inhibit CLOCK:BMAL1-mediated transcription, thus repressing their own expression [6] [98]. This cycle takes approximately 24 hours to complete. Post-translational modifications, including phosphorylation of core clock proteins by kinases such as CK1δ/ε, lead to their degradation, allowing the cycle to begin anew [97]. This molecular oscillator is autonomous and present in most cells, enabling them to maintain their own circadian rhythms.
The Suprachiasmatic Nucleus (SCN) as Master Pacemaker
The SCN serves as the master conductor of the body's circadian rhythms. It receives direct photic input from intrinsically photosensitive retinal ganglion cells (ipRGCs) via the retinohypothalamic tract, aligning the internal clock with the external light-dark cycle [97] [6]. The SCN then coordinates peripheral clocks through multiple output signals, including neuronal, hormonal, and behavioral rhythms [6]. While the SCN is entrained primarily by light, peripheral oscillators in organs like the liver, heart, and kidneys can be reset by other cues, notably feeding-fasting cycles and temperature fluctuations [6] [99]. This hierarchical organization ensures coherent timing across the organism while allowing peripheral tissues to respond to local environmental conditions.
The following diagram illustrates the core molecular feedback loop of the circadian clock:
Endocrine Regulation of Circadian Rhythms
The endocrine system and circadian rhythms engage in a sophisticated bidirectional dialogue. Hormones serve as key signaling molecules that communicate temporal information from the SCN to peripheral tissues, and in turn, provide feedback to the central clock. Hormones can regulate circadian physiology through three principal modes: as rhythm drivers, zeitgebers, and tuners [6].
Melatonin: The Photoperiodic Messenger
Melatonin, synthesized and secreted by the pineal gland during the dark phase, is a crucial hormonal signal of the circadian night. Its production is tightly controlled by the SCN via a multisynaptic pathway [6]. Light exposure at night potently suppresses melatonin release, making it a key mediator of light-dark information. Melatonin acts as both a rhythm driver and zeitgeber:
- Phase-Resetting Capability: Exogenous melatonin administration can phase-shift circadian rhythms, making it therapeutic for conditions like jet lag and shift work disorder [6].
- Receptor-Mediated Signaling: Melatonin exerts its effects primarily through two G-protein coupled receptors, MT1 and MT2, which are expressed in the SCN and various peripheral tissues [6].
- Amplitude Enhancement: Melatonin reinforces the amplitude and robustness of circadian rhythms, potentially stabilizing the entire circadian system against disruptive influences [6].
Glucocorticoids: Metabolic and Immune Coordinators
Glucocorticoids (cortisol in humans, corticosterone in rodents) exhibit a robust circadian rhythm with a peak concentration around the onset of the active phase (morning in humans). This rhythm results from the integrated control by the SCN via three mechanisms [6]:
- Circadian HPA Axis Regulation: The SCN projects to the paraventricular nucleus (PVN) of the hypothalamus, generating rhythmic corticotropin-releasing hormone (CRH) and arginine-vasopressin (AVP) release, which drive pituitary ACTH secretion.
- Adrenal Innervation: SCN signals via the autonomic nervous system modulate adrenal sensitivity to ACTH.
- Adrenal Clock Gating: The local circadian clock in the adrenal cortex gates its responsiveness to ACTH, contributing to the robust glucocorticoid rhythm [6].
Glucocorticoids function as potent zeitgebers for peripheral clocks. They bind to glucocorticoid receptors (GR) and mineralocorticoid receptors (MR), which translocate to the nucleus and regulate the transcription of numerous genes, including core clock genes such as Per1 and Per2 [6]. This enables glucocorticoids to synchronize metabolic and immune processes throughout the body.
Metabolic Hormones: Integrators of Nutrient Status
Circulating levels of metabolic hormones, including insulin, leptin, ghrelin, and adiponectin, display significant circadian rhythms [6]. While these rhythms are influenced by behavioral cycles like feeding-fasting, they are also under direct circadian control. These hormones can in turn feed back on the circadian system:
- Insulin has been shown to phase-shift peripheral clocks, potentially mediating the entraining effects of meal timing [6].
- Leptin and Ghrelin not only regulate appetite and energy balance but also interact with sleep-wake regulation and circadian processes.
Table 1: Circadian Profiles of Key Hormones in Humans
| Hormone | Peak Time | Trough Time | Primary Function in Circadian Regulation |
|---|---|---|---|
| Melatonin | 02:00-04:00 | 08:00-10:00 | Signals circadian night; promotes sleep; synchronizes peripheral clocks |
| Cortisol | 06:00-09:00 | 00:00-02:00 | Facilitates awakening; synchronizes peripheral metabolic clocks |
| Growth Hormone | Early sleep (SWS) | Daytime | Primarily sleep-dependent; promotes tissue repair |
| Testosterone | Early morning | Evening | Links reproductive function with sleep-wake cycle |
| TSH | Evening (before sleep) | Morning | Regulates thyroid axis with circadian variation |
Assessing Circadian and Sleep Parameters: Methodological Approaches
Comprehensive assessment of circadian rhythms and sleep requires a multimodal approach combining subjective reports, objective monitoring, and physiological biomarkers. The choice of methodology depends on the research question, with each technique offering distinct advantages and limitations.
Circadian Biomarker Assessment
Gold-standard assessment of the central circadian pacemaker requires rigorous protocols that minimize masking effects from sleep, activity, posture, and food intake. The primary circadian biomarkers include:
- Dim Light Melatonin Onset (DLMO): The gold standard for assessing circadian phase, DLMO measures the time at which melatonin levels begin to rise under dim light conditions (<10-30 lux) [98].
- Core Body Temperature (CBT): The circadian rhythm of CBT shows a nadir during the biological night and a rise before awakening, providing a reliable phase marker when measured continuously [97] [98].
- Cortisol Awakening Response (CAR): The sharp increase in cortisol levels occurring 30-45 minutes after morning awakening provides insight into HPA axis rhythmicity, though it is influenced by both circadian and sleep-related processes [6].
These biomarkers are typically measured during constant routine or forced desynchrony protocols that control for environmental influences, though such protocols are burdensome and costly [98].
Sleep Measurement Techniques
Sleep is a multidimensional construct encompassing regularity, satisfaction, alertness, timing, efficiency, and duration [98]. Assessment approaches include:
- Polysomnography (PSG): The gold standard for objective sleep assessment, PSG measures electroencephalogram (EEG), electrooculogram (EOG), electromyogram (EMG), and other physiological parameters to determine sleep stages and architecture [98] [100].
- Actigraphy: Wrist-worn devices that measure movement are widely used for long-term monitoring of sleep-wake patterns in naturalistic settings. While offering high sensitivity for sleep detection, they typically have moderate specificity for wake detection [98] [100].
- Sleep Diaries and Questionnaires: Subjective measures provide complementary information about sleep perception, satisfaction, and timing. Commonly used instruments include the Pittsburgh Sleep Quality Index (PSQI), Insomnia Severity Index (ISI), and Morningness-Eveningness Questionnaire (MEQ) [98].
Table 2: Methods for Assessing Circadian Rhythms and Sleep
| Assessment Method | Measured Parameters | Advantages | Limitations |
|---|---|---|---|
| DLMO Protocol | Circadian phase (melatonin onset) | Gold standard for central clock phase | Requires controlled dim light conditions; resource-intensive |
| Core Body Temperature | Circadian phase (temperature nadir) | Reliable physiological marker | Continuous measurement is intrusive; masked by activity and posture |
| Actigraphy | Sleep-wake patterns, rest-activity cycles | Suitable for long-term monitoring in natural environment | Lower specificity for wake detection; algorithm-dependent |
| Polysomnography (PSG) | Sleep stages, architecture, disorders | Comprehensive assessment of sleep physiology | Laboratory setting; not for long-term use; expensive |
| Sleep Diaries | Subjective sleep timing, quality, disturbances | Low cost; captures perception | Subject to recall and reporting bias |
The following workflow diagram outlines a protocol for comprehensive circadian phase assessment:
Environmental Cues and Circadian Disruption
Light: The Primary Zeitgeber
Light is the most potent environmental time cue for the central circadian pacemaker in the SCN. Specialized intrinsically photosensitive retinal ganglion cells (ipRGCs) containing the photopigment melanopsin are particularly sensitive to short-wavelength (blue) light and project directly to the SCN via the retinohypothalamic tract [101] [97]. The timing, intensity, duration, and spectral composition of light exposure determine its effect on the circadian phase:
- Morning Light: Exposure to bright light in the morning causes a phase advance of the circadian clock.
- Evening Light: Exposure to bright light in the evening and early night causes a phase delay.
- Nighttime Light: Exposure during the biological night (typically ~2-4 am) can cause maximal phase disruption and suppress melatonin production [101].
Modern lifestyles with abundant artificial light, particularly from electronic devices emitting blue-enriched light in the evening, contribute to widespread circadian misalignment [97].
Non-Photic Zeitgebers: Temperature, Feeding, and Activity
While light is the primary synchronizer of the central clock, peripheral oscillators are highly responsive to other environmental cues:
- Temperature Cycles: Daily temperature oscillations can entrain circadian rhythms, particularly in peripheral tissues. This appears to be especially relevant for timing emergence in some insect species, suggesting evolutionary conservation of this pathway [99].
- Feeding-Fasting Cycles: The timing of food intake is a potent zeitgeber for peripheral clocks in metabolic tissues such as the liver, pancreas, and gastrointestinal system [6]. Mistimed eating can desynchronize peripheral from central clocks.
- Physical Activity and Social Cues: Exercise can induce phase shifts in the human circadian clock, while social interactions may provide additional time cues, though their potency is less than that of light [102].
Circadian Disruptors and Health Implications
Various environmental factors can disrupt circadian rhythms, with significant health consequences:
- Shift Work and Jet Lag: These conditions create misalignment between the internal circadian clock and the external environment, associated with increased risks of metabolic disorders, cardiovascular disease, and cognitive impairment [97] [98].
- Environmental Chemicals: Emerging evidence indicates that certain environmental compounds, including steroid hormones, metals, pesticides, and bisphenol A, can disrupt circadian rhythms in animal models, though understanding of their effects in humans remains limited [103].
- Social Jet Lag: The mismatch between biological time (determined by the internal clock) and social time (determined by work/school schedules) is prevalent in modern societies and associated with metabolic and mental health deficits [100].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Circadian and Sleep Investigations
| Reagent/Technology | Primary Application | Key Function in Research |
|---|---|---|
| Melatonin Assays (Salivary, Plasma) | Circadian phase mapping (DLMO) | Quantifies melatonin for precise determination of circadian phase |
| Cortisol Immunoassays | HPA axis rhythm assessment | Measures cortisol rhythm and awakening response |
| Gene Expression Analysis (qPCR, RNA-Seq) | Clock gene oscillation profiling | Quantifies rhythmic expression of core clock genes (BMAL1, CLOCK, PER, CRY) |
| Luciferase Reporter Systems | Real-time clock gene activity monitoring | Tracks promoter activity of clock genes in live cells or tissues |
| Wireless Actigraphy Systems | Long-term sleep-wake monitoring | Provides objective measurement of rest-activity cycles in naturalistic settings |
| Polysomnography (PSG) Systems | Comprehensive sleep architecture analysis | Gold-standard assessment of sleep stages and disorders |
| Core Body Temperature Sensors (Ingestible, Skin) | Circadian rhythm monitoring | Tracks core body temperature rhythm as circadian phase marker |
| Controlled Light Exposure Systems | Photic entrainment studies | Delivers precise light intensity, spectrum, and timing for entrainment experiments |
Optimizing Circadian Alignment: Research-Backed Strategies
Light Exposure Management
Strategic light exposure represents the most powerful intervention for circadian alignment:
- Morning Light Enhancement: Seek bright light, particularly blue-enriched light, for 30-60 minutes upon waking to promote phase advances and morning alertness [101] [102].
- Evening Light Restriction: Minimize exposure to blue-enriched light from electronic devices 2-3 hours before bedtime. Use blue-blocking glasses or software applications that reduce blue light emission in the evening [101].
- Workplace Lighting: Implement dynamic lighting systems that provide brighter, blue-enriched light during morning and daytime hours, with warmer, dimmer light toward the end of the day [102].
Sleep-Wake Schedule Regularity
Maintaining consistent sleep-wake times across all days, including weekends, strengthens circadian rhythms and improves sleep quality:
- Fixed Scheduling: Establish consistent bed and wake times that align with natural circadian preferences (chronotype) as much as possible [101] [104].
- Gradual Adjustments: When schedule changes are necessary, implement gradual shifts of 15-30 minutes per day to allow the circadian system to adapt [104].
- Social Jet Lag Reduction: Minimize differences between workday and free-day sleep schedules to reduce circadian misalignment [100].
Meal Timing and Composition
The timing of food intake serves as a potent zeitgeber for peripheral clocks:
- Time-Restricted Feeding: Consume calories within a consistent 8-12 hour window during the active phase of the day to synchronize metabolic rhythms [6].
- Morning-Loaded Energy Intake: Front-load calorie consumption to earlier in the day, with a smaller evening meal, to align with natural metabolic rhythms [6].
- Avoid Late-Night Eating: Refrain from food consumption for 2-3 hours before bedtime to prevent disruption of circadian metabolism and sleep [104].
Chronotherapeutic Interventions
Targeted timing of interventions can enhance their efficacy and minimize side effects:
- Melatonin Supplementation: Appropriately timed low-dose melatonin (0.3-5 mg) can phase-shift circadian rhythms. Evening administration typically advances the clock, while morning administration may cause phase delays [6].
- Timed Exercise: Morning exercise may promote phase advances, while late afternoon or early evening exercise has minimal phase-shifting effects for most individuals [104].
- Medication Chronotherapy: Consider the circadian timing of drug administration to align with rhythms in drug metabolism, target sensitivity, and disease symptoms [102].
The intricate interplay between circadian rhythms, environmental cues, and endocrine function represents a critical frontier in biomedical research. Optimizing circadian alignment through strategic manipulation of sleep hygiene and environmental time cues offers a powerful, non-pharmacological approach to enhancing health and preventing disease. Future research directions should focus on:
- Personalized Chronotherapy: Developing individualized circadian interventions based on genetic profiling, chronotype assessment, and real-time physiological monitoring [102] [100].
- AI-Driven Circadian Health Monitoring: Leveraging artificial intelligence to analyze data from wearable devices for early detection of circadian disruption and automated intervention [102] [100].
- Circadian-Targeted Pharmacotherapy: Designing therapeutics that specifically target clock components or are timed to align with circadian rhythms in disease processes [105] [102].
- Environmental Engineering: Designing built environments that support, rather than disrupt, natural circadian rhythms through optimized lighting, temperature, and acoustic profiles [102].
As our understanding of circadian biology deepens, integrating these principles into clinical practice and public health policy holds immense promise for enhancing physical and mental well-being across populations.
Evaluating Evidence and Comparative Analysis of Chronotherapeutic Approaches
Chronotherapy represents a transformative approach in medical treatment, founded on the principle of aligning therapeutic interventions with the body's endogenous circadian rhythms. This strategy is profoundly influenced by the endocrine system, which governs key circadian rhythms through the systematic release of hormones such as cortisol, melatonin, and others that fluctuate over the 24-hour cycle [6]. These hormonal oscillations act as critical zeitgebers (time-givers), rhythm drivers, and tuners for peripheral tissue clocks, thereby orchestrating a complex temporal order in physiological processes ranging from metabolic cycles to cellular repair mechanisms [6]. The strategic scheduling of medication administration to coincide with specific circadian phases can significantly enhance drug efficacy and minimize adverse effects, particularly for therapeutics with narrow therapeutic indices. This in-depth review synthesizes evidence from clinical trials, focusing on cardiology and oncology, to evaluate the impact of chronotherapy on hard clinical endpoints and to delineate the underlying molecular mechanisms governed by endocrine-circadian interactions.
Synthesis of Clinical Evidence from Major Chronotherapy Trials
The clinical validation of chronotherapy is supported by several pivotal trials demonstrating that the timing of medication administration is a critical determinant of therapeutic outcomes. The evidence spans cardiovascular disease prevention and oncology, revealing a consistent pattern of improved efficacy and reduced toxicity with circadian-timed treatments.
2.1 The Hygia Chronotherapy Trial in Hypertension The Hygia Chronotherapy Trial, a large-scale, controlled, prospective endpoint trial conducted within a primary care setting, represents a landmark study in the field. It investigated whether bedtime ingestion of hypertension medications improved cardiovascular risk reduction compared to upon-awakening dosing [106].
- Study Population & Protocol: The trial enrolled 19,084 hypertensive patients (10,614 men and 8,470 women, average age 60.5 years). Participants were assigned 1:1 to ingest their entire daily dose of one or more hypertension medications at bedtime (n=9,552) or all of them upon awakening (n=9,532). At inclusion and at least annually thereafter, 48-hour ambulatory blood pressure (ABP) monitoring was performed [106].
- Primary Outcomes: Over a median follow-up of 6.3 years, 1,752 participants experienced the primary CVD outcome (a composite of CVD death, myocardial infarction, coronary revascularization, heart failure, or stroke). The study found that patients in the bedtime treatment group exhibited a significantly lower adjusted hazard ratio for the primary CVD outcome (0.55; 95% CI 0.50–0.61; P < 0.001). This risk reduction was consistent across all individual components of the primary outcome [106]:
- CVD death: 0.44 (0.34–0.56)
- Myocardial infarction: 0.66 (0.52–0.84)
- Coronary revascularization: 0.60 (0.47–0.75)
- Heart failure: 0.58 (0.49–0.70)
- Stroke: 0.51 (0.41–0.63)
- Mechanistic Insights: The superior outcomes were linked to improved ABP control, specifically a significantly enhanced decrease in asleep systolic blood pressure and an increased sleep-time relative systolic BP decline (nocturnal dipping). This finding underscores the role of circadian blood pressure regulation, which is partly under the control of the hypothalamic-pituitary-adrenal (HPA) axis and its circadian cortisol rhythm [106] [6].
Table 1: Cardiovascular Risk Reduction in the Hygia Chronotherapy Trial
| Outcome Measure | Adjusted Hazard Ratio (Bedtime vs. Awakening) | 95% Confidence Interval |
|---|---|---|
| Primary Composite CVD Outcome | 0.55 | 0.50 – 0.61 |
| Cardiovascular Death | 0.44 | 0.34 – 0.56 |
| Myocardial Infarction | 0.66 | 0.52 – 0.84 |
| Coronary Revascularization | 0.60 | 0.47 – 0.75 |
| Heart Failure | 0.58 | 0.49 – 0.70 |
| Stroke | 0.51 | 0.41 – 0.63 |
2.2 Chronomodulated Anthracycline Chemotherapy Anthracyclines are highly effective chemotherapeutic agents whose use is limited by dose-dependent cardiotoxicity. A systematic review of chronotherapeutic strategies for anthracycline administration summarized evidence from 3 in vitro studies, 12 animal studies, and 9 clinical studies [107].
- Proposed Optimal Timing: Based on extrapolation from animal studies, a hypothesized optimal time frame for anthracycline administration in humans was identified as being from 3 to 11 AM [107]. In nocturnal rodents (which are active at night, opposite to humans), administration during the rest phase was associated with reduced cardiotoxicity.
- Efficacy and Toxicity Outcomes: The review concluded that chronomodulated chemotherapy led to toxicity reduction in most trials, while anticancer efficacy was maintained in all studies, compared to non-circadian-based protocols [107].
- Endocrine-Circadian Mechanistic Basis: The circadian variation in cardiotoxicity is linked to the endogenous rhythms of cardiomyocytes. Key mechanistic explanations include:
- Oxidative Stress Regulation: The cardiomyocyte circadian clock regulates the activity of NAD+-dependent deacetylases SIRT1 and SIRT3, which are involved in mitochondrial function and reactive oxygen species (ROS) clearance. The activity of these enzymes oscillates, leading to a peak in ROS clearance capacity during the catabolic phase, thereby offering greater protection against anthracycline-induced oxidative stress at certain times of the day [107].
- DNA Damage Repair: Core clock components like CLOCK and PER2 regulate the expression of genes involved in DNA double-strand break repair (e.g., RAD50, BRCA1, p53, p21). The circadian variation in the efficiency of this repair machinery influences the extent of DNA damage caused by anthracyclines [107].
- Systemic & Intracellular Pharmacokinetics: Circadian fluctuations in body temperature, liver metabolism, and renal excretion can alter the pharmacokinetics of anthracyclines, while the expression of drug transporters in cells may also follow a circadian pattern [107].
Table 2: Summary of Evidence for Chronomodulated Anthracycline Therapy
| Evidence Category | Number of Studies | Key Findings Related to Chronotherapy |
|---|---|---|
| In Vitro Studies | 3 | Apoptosis rates in cardiomyocytes were lowest between Circadian Time (CT) 36-45 and highest between CT 18-27 post-synchronization [107]. |
| Animal Studies | 12 | Informed the hypothesized optimal administration window and provided evidence for reduced cardiotoxicity with timing aligned to the rest phase [107]. |
| Clinical Studies | 9 | Most trials showed a reduction in toxicity while maintaining oncological efficacy [107]. |
Molecular Mechanisms: The Endocrine-Circadian Interface in Therapeutics
The efficacy of chronotherapy is rooted in the molecular architecture of the circadian clock and its intricate regulation by endocrine signals. This system creates predictable daily variations in drug metabolism, target availability, and tissue susceptibility.
3.1 The Core Circadian Clock Machinery The mammalian circadian system is organized hierarchically. The master pacemaker in the suprachiasmatic nucleus (SCN) synchronizes peripheral clocks in virtually every cell, including cardiomyocytes, hepatocytes, and vascular endothelial cells [107] [6]. On a molecular level, these clocks are composed of interlocking transcriptional-translational feedback loops. The core loop involves the activation of Period (Per1-3) and Cryptochrome (Cry1/2) genes by the CLOCK-BMAL1 heterodimer. PER and CRY proteins then accumulate, form complexes, and translocate back to the nucleus to repress their own transcription, completing a cycle that takes approximately 24 hours [6].
3.2 Endocrine Regulation of Circadian Rhythms Hormones function as key mediators that synchronize peripheral clocks with the central SCN pacemaker and with environmental cues. The primary endocrine regulators include:
- Melatonin: Secreted by the pineal gland during the night, melatonin is a potent zeitgeber for the SCN and peripheral tissues. It signals the "biological night," helping to entrain sleep-wake cycles and other physiological rhythms. It acts via MT1 and MT2 receptors to influence phase and amplitude of circadian rhythms [6].
- Glucocorticoids (e.g., Cortisol): These steroids exhibit a robust circadian rhythm with a peak around wake-up time. They act as rhythm drivers by binding to glucocorticoid response elements (GREs) in the genome to regulate the expression of numerous genes. Simultaneously, they function as zeitgebers for peripheral clocks, as clock genes like Per1 and Per2 contain GREs and are directly induced by glucocorticoids [6]. The adrenal clock itself gates the organ's sensitivity to ACTH, contributing to the robustness of the cortisol rhythm [6].
- Other Metabolic Hormones: Rhythms in insulin, glucagon, leptin, and ghrelin, influenced by both the central clock and feeding-fasting cycles, help synchronize metabolic processes in tissues like the liver, thereby acting as tuners of circadian metabolism [6].
Diagram 1: Endocrine Regulation of Circadian Therapeutics. This diagram illustrates how the central clock (SCN) integrates light input to regulate the rhythmic secretion of melatonin and cortisol, which in turn act as zeitgebers and rhythm drivers for peripheral clocks in organs like the heart and liver, ultimately influencing drug metabolism and tissue susceptibility to toxicity.
3.3 Chronopharmacology of Anthracycline-Induced Cardiotoxicity The circadian timing of anthracycline administration interacts directly with the molecular clock of the cardiomyocyte to modulate cardiotoxicity through several key pathways.
Diagram 2: Circadian Regulation of Anthracycline Cardiotoxicity. The core circadian clock in cardiomyocytes regulates protective pathways. CLOCK-BMAL1 activates SIRT1/SIRT3, which enhance mitochondrial function and mitigate doxorubicin-induced ROS. CLOCK-BMAL1 also activates DNA repair genes. Anthracyclines cause ROS and DNA damage, leading to apoptosis. The circadian variation in the protective pathways explains the time-dependent sensitivity to cardiotoxicity.
Experimental Protocols for Chronotherapy Research
Robust experimental design is paramount for generating reliable data in chronotherapy research. The following protocols detail key methodologies for both clinical and preclinical investigations.
4.1 Clinical Trial Protocol: Randomized Controlled Trial of Antihypertensive Chronotherapy
- Objective: To compare the effect of bedtime versus upon-awakening administration of antihypertensive medication on major cardiovascular events.
- Primary Endpoint: Composite of cardiovascular death, myocardial infarction, coronary revascularization, heart failure, or stroke.
- Design:
- Randomization: Multicenter, prospective, randomized, controlled trial with 1:1 allocation to bedtime or upon-awakening treatment arms. Stratification by site, sex, and diabetes status is recommended.
- Blinding: While true blinding of administration time is challenging, endpoint adjudication committees should be blinded to treatment allocation.
- Ambulatory Blood Pressure Monitoring (ABPM): ABPM for 48 hours should be performed at baseline and at scheduled annual visits. Key parameters include 24-hour, daytime, and nighttime systolic and diastolic BP, as well as the nocturnal BP dipping percentage [106].
- Sample Size & Follow-up: A large sample size (e.g., >10,000 patients) and long-term follow-up (median >5 years) are required to accrue a sufficient number of hard clinical endpoints [106].
- Considerations: The protocol should account for potential confounders such as age, sex, chronotype, comorbidities (e.g., type 2 diabetes, chronic kidney disease), and concomitant medications [107].
4.2 Preclinical In Vitro Protocol: Circadian Timing of Doxorubicin Exposure in Cardiomyocytes
- Objective: To investigate 24-hour variation in apoptotic response to doxorubicin in synchronized cardiomyocytes.
- Cell Model: Human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs) or neonatal rat ventricular myocytes.
- Synchronization: Cells are synchronized using a high-concentration serum shock (e.g., 50% horse serum for 2 hours) or dexamethasone treatment to align their circadian clocks. The start of synchronization is defined as Circadian Time (CT) 0 [107].
- Doxorubicin Treatment: At defined CT points throughout the circadian cycle (e.g., every 3-4 hours), cells are exposed to a standardized concentration of doxorubicin (e.g., 10 μM) for a set duration (e.g., 6 hours) [107].
- Outcome Assessment:
- Apoptosis Assay: The primary readout is the rate of apoptosis, measured 24-48 hours post-exposure via flow cytometry using Annexin V/propidium iodide staining or caspase-3/7 activity assays.
- Gene Expression Analysis: Quantitative PCR (qPCR) is performed to examine the expression of core clock genes (Bmal1, Per2, Rev-erbα), stress-response genes (HSPH1, DNAJA1), and DNA damage markers in samples collected at different CTs [107].
- Data Analysis: Apoptosis rates are plotted against CT to identify phases of high and low susceptibility. Correlation analysis with gene expression profiles can reveal potential mechanistic links.
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagents for Chronotherapy Investigations
| Reagent / Material | Function in Chronotherapy Research |
|---|---|
| Ambulatory Blood Pressure Monitor (ABPM) | A portable device for measuring blood pressure at regular intervals over 24-48 hours, essential for assessing circadian BP profiles and nocturnal dipping in clinical trials [106]. |
| Synchronization Agents (e.g., Dexamethasone, High Serum) | Pharmacological tools used in in vitro studies to align the circadian phases of cells in culture, enabling the study of circadian variation in drug response [107]. |
| Human iPSC-Derived Cardiomyocytes | A physiologically relevant and genetically manipulable human cell model for studying circadian mechanisms of drug-induced cardiotoxicity in vitro [107]. |
| qPCR Assays for Clock Genes | Used to quantify the mRNA expression of core circadian clock components (e.g., BMAL1, CLOCK, PER1/2/3, CRY1/2, REV-ERBα) to verify synchronization and assess clock function [107]. |
| Apoptosis Detection Kits (e.g., Annexin V) | Reagents for flow cytometry or fluorescence microscopy to quantify programmed cell death, a key endpoint for assessing time-dependent toxicity of chemotherapeutics [107]. |
| Cosinor Analysis Software | A statistical package for analyzing circadian rhythms by fitting time-series data to a cosine curve, allowing for the determination of rhythm period, amplitude, and phase [108]. |
The endocrine system and circadian rhythms are inextricably linked in a complex, bidirectional relationship that governs physiological timing across the body. While the suprachiasmatic nucleus (SCN) in the hypothalamus acts as the central pacemaker, peripheral clocks in tissues such as the brain, liver, and adrenal glands exhibit significant autonomy and specialized functions [22] [18]. These tissue-specific clocks are synchronized by both the SCN and local zeitgebers—environmental and physiological time-giving signals—including light, feeding schedules, and hormonal fluctuations [6] [18]. Understanding the distinct molecular architectures, regulatory mechanisms, and functional outputs of these clocks is crucial for elucidating their roles in health and disease. This comparative analysis examines the unique characteristics of endocrine clocks in the brain, liver, and adrenal glands, highlighting their specialized functions, regulatory inputs, and pathological consequences when disrupted. The intricate interplay between these clocks enables precise temporal coordination of physiology, from metabolism and stress response to cognition and behavior [6] [22] [109].
Molecular Architecture of Circadian Clocks
The molecular machinery governing circadian rhythms consists of evolutionarily conserved transcriptional-translational feedback loops (TTFLs) that generate approximately 24-hour oscillations in clock gene expression [38] [22]. While this core mechanism is shared across tissues, its implementation and regulation exhibit significant tissue-specific variations.
The core negative feedback loop involves heterodimers of BMAL1 (Brain and muscle ARNT-like protein-1) and CLOCK (Circadian locomotor output cycles kaput) proteins that activate transcription of Period (Per1-3) and Cryptochrome (Cry1/2) genes by binding to E-box elements in their promoter regions [6] [38]. Following translation, PER and CRY proteins form complexes that translocate back to the nucleus to inhibit CLOCK:BMAL1 transcriptional activity, thereby repressing their own expression [38]. This cycle takes approximately 24 hours to complete.
An auxiliary feedback loop involves the nuclear receptors REV-ERBα and RORα, which compete for binding to ROR response elements (ROREs) in the Bmal1 promoter [38]. REV-ERBα represses while RORα activates Bmal1 transcription, adding stability and robustness to the core oscillator [38]. Post-translational modifications, including phosphorylation and ubiquitination, regulate the stability, localization, and degradation of core clock components, fine-tuning the clock's period and precision [38].
This molecular framework is expressed in virtually all cells throughout the body, but tissue-specific factors—including epigenetic modifications, transcriptional co-regulators, and metabolic conditions—modulate its operation to generate specialized circadian outputs in different organs [110].
Figure 1: Core molecular mechanism of circadian clocks. The transcriptional-translational feedback loop (TTFL) consists of a core negative feedback loop (gold, green, red) and an auxiliary stabilizing loop (blue). This conserved mechanism operates in all mammalian cells but is modulated differently across tissues.
Brain Clocks
Suprachiasmatic Nucleus (SCN): The Central Pacemaker
The SCN serves as the master circadian pacemaker, coordinating timing throughout the body by integrating light information received via intrinsically photosensitive retinal ganglion cells (ipRGCs) and the retinohypothalamic tract [6] [111]. The SCN contains approximately 20,000 neurons, including distinct populations of vasoactive intestinal peptide (VIP) and arginine-vasopressin (AVP)-expressing cells that mediate intercellular synchronization and broadcast timing signals to peripheral tissues [22] [18]. Unlike peripheral oscillators, the SCN maintains robust circadian rhythms even in the absence of external timing cues, demonstrating its self-sustaining nature [111].
The SCN synchronizes peripheral clocks through multiple output pathways: (1) neural connections via the autonomic nervous system; (2) neuroendocrine signaling, including regulation of melatonin and cortisol secretion; and (3) indirect behavioral cues such as feeding-fasting cycles [38] [22]. Light serves as the primary zeitgeber for the SCN, inducing phase shifts that vary in magnitude and direction depending on the circadian phase of exposure [111]. The human circadian pacemaker exhibits an intrinsic period averaging 24.18 hours, which is tightly regulated genetically and precisely synchronized to the 24-hour solar day by light exposure [111].
Extra-SCN Brain Clocks
Beyond the SCN, autonomous circadian oscillators exist in various brain regions, including the hippocampus, amygdala, cortex, and olfactory bulb [22] [18]. These extra-SCN clocks operate via the same core TTFL mechanism but regulate region-specific functions. Hippocampal clocks modulate long-term potentiation and synaptic plasticity, processes critical for memory formation [22] [18]. Cortical clocks influence cognitive functions, while amygdala clocks contribute to emotional regulation [18].
Desynchronization between hippocampal and SCN rhythms impairs learning and memory in rodent models [22]. Similarly, disruptions in cortical and amygdala circadian regulation are associated with psychiatric and neurodegenerative disorders in both animal models and human clinical studies [22] [18]. The brain's circadian system also extends its influence to neuroendocrine axes, particularly the hypothalamic-pituitary-adrenal (HPA) axis, which regulates stress responses [22] [18].
Liver Clocks
The hepatic circadian clock operates as a key peripheral oscillator that regulates metabolic processes, including glucose homeostasis, lipid metabolism, and xenobiotic detoxification [22] [110]. Unlike the SCN, which is primarily entrained by light, the liver clock is strongly influenced by feeding-fasting cycles [22] [109]. When feeding schedules are shifted, the liver clock can rapidly recalibrate its phase independent of the SCN, demonstrating its metabolic flexibility [109].
Approximately 10-15% of the hepatic transcriptome exhibits circadian oscillations, including genes involved in glycolysis, gluconeogenesis, cholesterol synthesis, and bile acid metabolism [110]. This temporal organization enables the liver to anticipate periodic changes in nutrient availability and optimize metabolic efficiency. For instance, genes promoting glucose utilization are upregulated during active periods, while those enhancing glycogen synthesis and storage peak during rest phases [110].
The liver clock also regulates drug metabolism and detoxification pathways, with enzymes such as cytochrome P450s exhibiting robust circadian expression [110]. This temporal variation significantly influences drug pharmacokinetics and efficacy, forming the basis for chronotherapeutic approaches [110]. Disruption of hepatic circadian rhythms, as occurs in shift work or jet lag, contributes to metabolic diseases including non-alcoholic fatty liver disease (NAFLD), insulin resistance, and obesity [110].
Adrenal Clocks
The adrenal gland contains an autonomous circadian clock that gates glucocorticoid production and secretion, creating a robust circadian rhythm in circulating cortisol (in humans) and corticosterone (in rodents) levels [6] [109]. This endocrine rhythm peaks shortly before the active phase (dawn in diurnal humans, dusk in nocturnal rodents), preparing the body for anticipated activity and stress [6]. Superimposed on this circadian rhythm is an ultradian rhythm of approximately 90-minute pulses, although these vary in frequency and amplitude [6].
Three distinct mechanisms coordinate rhythmic glucocorticoid secretion: (1) Circadian control of the hypothalamic-pituitary-adrenal (HPA) axis via arginine-vasopressin (AVP) projections from the SCN to the paraventricular nucleus (PVN) [6]; (2) Direct autonomic innervation of the adrenal gland via the splanchnic nerve, which transmits light information from the SCN and modulates adrenal sensitivity to adrenocorticotropic hormone (ACTH) [6]; (3) The intrinsic adrenal clock, which gates the organ's responsiveness to ACTH and contributes to generating a robust glucocorticoid rhythm [6].
Once released, glucocorticoids act as potent zeitgebers for peripheral clocks throughout the body by binding to glucocorticoid response elements (GREs) in the regulatory regions of clock genes such as Per1 and Per2 [6]. This creates a feedback loop wherein the SCN regulates glucocorticoid secretion, which in turn synchronizes peripheral oscillators. The adrenal clock also influences the production of catecholamines and other steroid hormones, extending its regulatory reach beyond glucocorticoids alone [6] [109].
Comparative Analysis
Table 1: Comparative characteristics of endocrine clocks across tissues
| Parameter | Brain (SCN) | Liver | Adrenal |
|---|---|---|---|
| Primary Function | Master pacemaker, coordination of peripheral clocks | Metabolic regulation, detoxification | Glucocorticoid and stress hormone production |
| Core Clock Components | BMAL1, CLOCK, PER1-3, CRY1-2, REV-ERB, ROR | BMAL1, CLOCK, PER1-3, CRY1-2, REV-ERB, ROR | BMAL1, CLOCK, PER1-3, CRY1-2, REV-ERB, ROR |
| Key Entrainment Signals | Light via retinohypothalamic tract | Feeding-fasting cycles, nutrients | Light (via SCN-HPA axis), ACTH |
| Phase Relationship to SCN | Master pacemaker (reference) | ~4-6 hour delay | ~2-4 hour delay |
| Primary Output Signals | Neural, endocrine, behavioral | Metabolic (glucose, lipids), detoxification | Hormonal (cortisol, catecholamines) |
| Key Regulatory Hormones | Melatonin, AVP, VIP | Insulin, glucagon | ACTH, cortisol |
| Impact of Disruption | Sleep disorders, cognitive impairment, mood disorders | Metabolic syndrome, NAFLD, obesity | HPA axis dysfunction, stress disorders |
Table 2: Disease associations and clinical implications of circadian disruption
| Tissue | Associated Diseases | Key Pathogenic Mechanisms | Potential Chronotherapeutic Approaches |
|---|---|---|---|
| Brain | Alzheimer's disease, Parkinson's disease, depression, bipolar disorder, sleep disorders | Neuroinflammation, oxidative stress, impaired neurogenesis, synaptic dysfunction | Timed light therapy, melatonin supplementation, timed sleep-wake schedules |
| Liver | Non-alcoholic fatty liver disease (NAFLD), type 2 diabetes, obesity, metabolic syndrome | Dysregulated glucose and lipid metabolism, impaired insulin signaling, oxidative stress | Time-restricted feeding, chronopharmacology for metabolic drugs |
| Adrenal | Cushing's syndrome, adrenal insufficiency, metabolic syndrome, cardiovascular disease | HPA axis dysregulation, glucocorticoid resistance, inflammatory signaling | Chronotherapy with glucocorticoid replacement, timed antihypertensive medications |
The brain, liver, and adrenal clocks exhibit distinct entrainment mechanisms, physiological functions, and disease associations despite sharing a common molecular framework. The SCN shows remarkable autonomy and resilience, maintaining rhythmicity even in isolation, while peripheral clocks in the liver and adrenal glands depend more heavily on external signals—feeding cycles and ACTH, respectively [6] [22] [109]. This hierarchical organization ensures coherent timing across tissues while allowing flexibility for local adaptation.
From a translational perspective, these tissue-specific differences have important implications for chronotherapy. The timing of drug administration can be optimized based on the target tissue's circadian rhythms to maximize efficacy and minimize side effects [110]. For instance, cardiovascular medications may be most effective when aligned with the morning surge in blood pressure and cortisol, while chemotherapy agents might be timed to coincide with peaks in metabolic activity of target tissues [110].
Figure 2: Hierarchical organization of endocrine clocks. The SCN serves as the central pacemaker, entrained primarily by light. Peripheral clocks in the liver and adrenal glands are synchronized by both the SCN and local zeitgebers (feeding cycles, ACTH), creating a coordinated temporal network. Hormonal outputs (cortisol) provide additional feedback, reinforcing system-wide synchronization.
Experimental Protocols and Methodologies
Assessing Circadian Rhythms in Human Studies
Studying endocrine clocks in humans requires specialized methodologies that account for individual variability while capturing robust circadian parameters. Saliva sampling has emerged as a non-invasive approach for assessing peripheral clock rhythms, offering practical advantages for clinical applications [57]. The protocol involves collecting saliva at 3-4 time points per day over 2 consecutive days, using RNAprotect preservative in a 1:1 ratio with 1.5 mL saliva to ensure RNA stability [57]. This method enables analysis of core clock gene expression rhythms (ARNTL1, NR1D1, PER2) that show phase synchronization across peripheral tissues [57].
Dim Light Melatonin Onset (DLMO) remains the gold standard for circadian phase assessment in humans, though molecular markers like β-Arrestin (ARRB1) show promise for tracking phase shifts, potentially offering advantages over DLMO in certain contexts [57]. The Morningness-Eveningness Questionnaire (MEQ) provides a practical estimate of chronotype, though it lacks the complexity of direct physiological measurements [57].
For tissue-specific analysis, proteomic aging clocks have been developed using plasma proteomics and machine learning approaches [112]. These models quantify organ-specific biological aging by measuring tissue-enriched proteins, revealing that different organs age at different rates and that accelerated organ aging predicts disease onset and mortality beyond chronological age [112]. This approach has been validated across diverse populations, with brain aging showing the strongest association with mortality and neurodegenerative diseases [112].
Animal Models and Tissue-Specific Manipulations
Animal studies, primarily in rodents, have been instrumental in elucidating the molecular mechanisms of tissue-specific circadian clocks. Key approaches include:
Tissue-specific knockout models: Cre-loxP systems enable selective deletion of core clock genes (e.g., Bmal1, Clock) in specific tissues, revealing their distinct functions [22] [18]. For example, cardiomyocyte-specific Bmal1 knockout impairs cardiac contractility and metabolic function, while liver-specific knockout disrupts glucose homeostasis [22].
Forced desynchrony protocols: These paradigms dissociate the central SCN pacemaker from peripheral clocks by manipulating feeding schedules or light exposure, enabling study of their independent contributions [109].
Real-time bioluminescence imaging: Tissues from transgenic mice expressing luciferase under control of clock gene promoters (e.g., Per2::Luc) allow direct visualization of circadian rhythms in explants [109].
Viral vector-mediated gene transfer: Enables tissue-specific rescue or perturbation of clock components in adult animals, circumventing developmental compensation effects [22].
Table 3: Essential research reagents and methodologies for circadian studies
| Reagent/Method | Application | Key Features | Considerations |
|---|---|---|---|
| Per2::Luc reporter mice | Real-time monitoring of circadian rhythms in tissues | Non-invasive, high-temporal resolution | Requires specialized imaging equipment |
| Tissue-specific Cre lines | Selective genetic manipulation of clocks in target tissues | Cell-type specificity, temporal control (with inducible systems) | Potential for off-target effects, developmental compensation |
| TimeTeller methodology | Assessing circadian rhythms from human saliva | Non-invasive, clinically applicable, measures multiple clock genes | Requires multiple sampling time points |
| Plasma proteomics (Olink) | Quantifying organ-specific biological age | Measures ~3000 proteins, validated across populations | Cost, specialized equipment required |
| Dim Light Melatonin Onset (DLMO) | Gold standard for human phase assessment | High accuracy, established protocols | Requires controlled light conditions, multiple samples |
The comparative analysis of endocrine clocks across brain, liver, and adrenal tissues reveals a sophisticated temporal architecture that optimizes physiological function through specialized, tissue-specific timing mechanisms. While sharing a common molecular framework, these clocks have evolved distinct regulatory inputs and physiological outputs tailored to their unique roles in the organism. The SCN operates as the central coordinator, entrained primarily by light and maintaining temporal coherence across tissues. The liver clock serves as a metabolic integrator, finely tuned by feeding-fasting cycles to optimize energy utilization and storage. The adrenal clock functions as a key endocrine regulator, generating glucocorticoid rhythms that synchronize peripheral tissues while preparing the organism for daily stressors.
Disruption of this coordinated timing system—through genetic alterations, environmental misalignment, or lifestyle factors—contributes significantly to disease pathogenesis across multiple organ systems. Understanding the unique properties of tissue-specific clocks provides a foundation for developing targeted chronotherapeutic interventions that restore circadian alignment and optimize treatment outcomes. Future research should focus on elucidating the communication mechanisms between different tissue clocks and developing precise methods for assessing and modulating their function in human health and disease.
The translation of circadian biology from nocturnal rodent models to diurnal humans presents a fundamental challenge in biomedical research. While the core molecular machinery of the circadian clock is conserved across mammalian species, critical differences in the phase relationships of subordinate oscillators and opposite responses to environmental cues create significant translational gaps. This whitepaper examines the neural, endocrine, and molecular mechanisms underlying these chronotype differences and provides a framework for researchers to contextualize findings from nocturnal models within human physiology. By integrating recent advances in diurnal modeling and chronotherapy approaches, we offer methodological guidance for optimizing translational success in circadian research and drug development.
The predominant use of nocturnal rodents in biomedical research has created a significant translational challenge for understanding human circadian biology. While humans are diurnal, approximately 70% of modern mammals are nocturnal, with only about 20% sharing our day-active pattern [113]. This fundamental difference in temporal organization means that physiological and neurological processes in diurnal mammals during the day are not equivalent to those of nocturnal ones at night [114] [113]. The circadian system orchestrates temporal organization of behavior and physiology through a hierarchical structure, with the suprachiasmatic nucleus (SCN) serving as the master pacemaker that coordinates subordinate oscillators throughout the body and peripheral tissues [115] [10]. Although the molecular machinery of this system is largely conserved between diurnal and nocturnal species, the phase relationships between principal and subordinate oscillators exhibit chronotype-specific patterns that complicate direct translation of research findings [114] [113].
Understanding these differences is particularly crucial within the context of endocrine regulation of circadian rhythms, as many hormones exhibit robust daily oscillations that synchronize physiological processes across body systems. The endocrine system serves as a key communication channel between the SCN and peripheral clocks, with hormonal rhythms both influencing and being influenced by circadian regulation [6]. This review examines the mechanisms underlying chronotype differences, explores their implications for translational research, and provides experimental frameworks for bridging this translational gap.
Molecular Circadian Machinery: Conservation and Divergence
Core Clock Mechanisms
The molecular foundation of circadian rhythms consists of interlocked transcriptional/translational feedback loops (TTFLs) that are remarkably conserved across mammalian species, regardless of chronotype [115] [10] [113]. At the core of this system, the CLOCK and BMAL1 proteins form heterodimers that activate transcription of Period (Per1, Per2, Per3) and Cryptochrome (Cry1, Cry2) genes by binding to E-box enhancer elements in their promoters [115] [116] [10]. The resulting PER and CRY proteins accumulate, form complexes, and translocate back to the nucleus to inhibit CLOCK:BMAL1 transcriptional activity, completing the primary negative feedback loop with a period of approximately 24 hours [115] [10].
This core oscillation is stabilized by auxiliary feedback loops involving nuclear receptors REV-ERBα/β and RORα/γ, which rhythmically regulate Bmal1 expression by competing for ROR response elements (ROREs) [10] [117]. Post-translational modifications, particularly phosphorylation by casein kinases 1δ/ε (CK1δ/ε) and ubiquitination by F-box proteins such as FBXL3, regulate the stability and degradation of core clock components, providing critical fine-tuning of clock speed and precision [115] [117]. Recent research has revealed additional regulatory layers, including SUMOylation, which modulates CLOCK:BMAL1 transcriptional activity and stability [117].
Phase Relationships in Central and Peripheral Clocks
Despite conservation of molecular components, diurnal and nocturnal mammals exhibit significant differences in the phase relationships between central and peripheral oscillators. In the SCN itself, rhythms in clock gene expression, electrical activity, and metabolism are similarly phased relative to the light-dark cycle in both chronotypes, with peak activity occurring during the daytime [113]. This indicates that the SCN serves primarily as a light-tracker rather than directly determining activity phase.
However, in extra-SCN brain regions and peripheral tissues, complex phase differences emerge between diurnal and nocturnal species. While some tissues exhibit simple 12-hour anti-phase relationships, others show more complex phase shifts of 6-15 hours depending on tissue type [113]. Transcriptomic studies comparing diurnal non-human primates (olive baboons) with nocturnal laboratory mice have revealed that while core clock genes are in phase within the SCN, they are approximately 12 hours out of phase in many other brain regions and peripheral tissues [113]. This complex patterning suggests that no single simple switch determines chronotype; rather, it likely involves distributed differences in neural circuitry and gene regulatory networks downstream of the SCN [113].
Table 1: Comparative Analysis of Circadian Systems in Diurnal vs. Nocturnal Mammals
| Feature | Nocturnal Rodents | Diurnal Humans | Translational Implications |
|---|---|---|---|
| Activity Pattern | Active at night, sleep during day | Active during day, sleep at night | Fundamental reversal in behavioral and physiological rhythms |
| SCN Molecular Rhythm | High electrical activity and metabolism during day | High electrical activity and metabolism during day | SCN phase conserved despite opposite activity patterns |
| Light Response | Induces sleep and melatonin synthesis | Promotes arousal and wakefulness | Opposite behavioral and endocrine responses to light |
| Melatonin Secretion | Peaks during active phase (night) | Peaks during rest phase (night) | Same phase relative to dark, but opposite to activity state |
| Peripheral Clocks | Various phase relationships to SCN | ~12h phase shift in many tissues | Complex translation required for peripheral physiology |
Endocrine Regulation of Circadian Rhythms
Hormones as Rhythm Drivers, Zeitgebers, and Tuners
The endocrine system plays a crucial role in circadian regulation, with hormones functioning as rhythm drivers, zeitgebers (time-givers), and tuners of circadian rhythms [6]. Several key hormones exhibit robust daily oscillations that influence circadian organization throughout the body:
Melatonin, synthesized primarily by the pineal gland, displays opposite functional roles relative to activity phase between chronotypes. While melatonin peaks during the rest phase in both diurnal and nocturnal mammals, it functions as a hypnotic in diurnal humans but is secreted during the active phase in nocturnal rodents [114] [6] [113]. Melatonin acts on the SCN through MT1 and MT2 receptors to help synchronize circadian rhythms and refine their amplitude [6]. Its production is tightly regulated by the SCN, which transmits signals that restrict melatonin synthesis to the nocturnal phase while also providing inhibitory signals in response to incidental nighttime light exposure [6].
Glucocorticoids (cortisol in humans, corticosterone in rodents) exhibit a robust circadian rhythm with peak secretion anticipating the active phase (morning for humans, evening for nocturnal rodents) [6]. This rhythm is regulated through multiple mechanisms: (1) circadian control of the HPA axis via SCN projections to the paraventricular nucleus; (2) autonomic innervation of the adrenal gland modulating sensitivity to ACTH; and (3) an intrinsic adrenal clock that gates glucocorticoid release [6]. Glucocorticoids function as both rhythm drivers, regulating rhythmic gene expression through glucocorticoid response elements (GREs), and zeitgebers, affecting peripheral clocks by influencing Per expression [6].
Gonadotropin-releasing hormone (GnRH) and luteinizing hormone (LH) exhibit reversed circadian patterns in diurnal versus nocturnal species. Research comparing diurnal Nile grass rats (Arvicanthis niloticus) with nocturnal laboratory rats (Rattus norvegicus) has demonstrated 12-hour anti-phase rhythms in GnRH neuronal activity and the preovulatory LH surge, which persist under constant darkness, indicating endogenous circadian control [118]. These findings highlight the crucial role of circadian timing in reproductive endocrinology and its differential regulation across chronotypes.
Metabolic Hormones and Feeding-Fasting Cycles
Metabolic hormones including insulin, glucagon, leptin, ghrelin, and adiponectin also display circadian rhythms that are influenced by both the central clock and feeding-fasting cycles [6]. The timing of food intake can reset peripheral clocks independently of the SCN, creating complex interactions between circadian and metabolic systems [119] [6]. These relationships have important implications for understanding metabolic disorders and developing chronotherapeutic approaches for their treatment.
Table 2: Endocrine Rhythms and Their Chronotype-Specific Regulation
| Hormone | Source | Peak Phase in Humans | Peak Phase in Nocturnal Rodents | Primary Circadian Functions |
|---|---|---|---|---|
| Melatonin | Pineal gland | Night (sleep phase) | Night (active phase) | Sleep promotion, SCN phase resetting, antioxidant effects |
| Cortisol/Corticosterone | Adrenal cortex | Morning (pre-waking) | Evening (pre-active) | Metabolic preparation for activity, immune modulation, peripheral clock entrainment |
| LH | Anterior pituitary | Variable across cycle | Variable across cycle | Timing of preovulatory surge, reproductive cycle regulation |
| Insulin | Pancreatic β-cells | Day (feeding phase) | Night (feeding phase) | Glucose regulation, metabolic rhythm coordination |
| Ghrelin | Stomach | Day (pre-meal) | Night (pre-meal) | Appetite regulation, meal initiation |
Experimental Approaches for Cross-Species Translation
Diurnal Rodent Models
The development and characterization of diurnal rodent models represents a significant advancement for circadian translational research. Species such as the Nile grass rat (Arvicanthis niloticus) and degu (Octodon degus) provide valuable alternatives to nocturnal models, particularly for studying conditions where circadian rhythm disruption, altered photic response, or melatonin secretion is involved [114] [118] [113]. These models enable researchers to investigate diurnal physiology directly while maintaining the practical advantages of rodent studies.
Recent research utilizing these models has revealed important insights into chronotype differences. For example, a study comparing GnRH neuronal activity and LH surges in diurnal grass rats versus nocturnal laboratory rats demonstrated that the 12-hour phase difference in these reproductive events is driven by endogenous circadian mechanisms rather than simply being a response to the light-dark cycle [118]. Such findings highlight the value of diurnal models for understanding human-relevant circadian physiology.
Molecular and Genomic Approaches
Advanced molecular and genomic techniques provide powerful tools for investigating cross-species circadian biology. Transcriptomic analyses across multiple tissues in both diurnal and nocturnal species have revealed that 45-80% of protein-coding genes show circadian expression in at least one organ [113]. These comprehensive datasets enable researchers to identify conserved and divergent rhythmic genes across chronotypes.
Single-nucleotide polymorphism (SNP) analyses and genome-wide association studies have identified links between clock genes and human disorders. For example, polymorphisms in CLOCK, CRY1, NPAS2, and VIP genes have been associated with bipolar disorder, while TIMELESS and PER3 variants have been linked to schizophrenia and bipolar disorder [116]. Similar approaches in rodent models can help validate these associations and elucidate underlying mechanisms.
Chronopharmacology and Experimental Design
Chronopharmacology research has revealed that up to 60% of FDA-approved drug targets exhibit circadian oscillations, contributing to time-dependent drug effects [119] [68]. Mathematical modeling combined with experimental approaches has helped characterize how circadian and drug properties interact to shape time-of-day drug sensitivity profiles [68]. These models incorporate factors such as circadian amplitude, period, amplitude decay rate, and drug-specific characteristics to predict optimal timing for drug administration.
When designing translational circadian studies, researchers should consider:
- Zeitgeber alignment: Properly aligning experimental timing with species-specific activity phases
- Tissue-specific rhythms: Accounting for differential phase relationships across tissues
- Endocrine profiling: Comprehensive monitoring of hormonal rhythms throughout experiments
- Chronotype-appropriate endpoints: Selecting outcome measures relevant to human physiology
Diagram Title: Cross-Species Circadian Translation Framework
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Circadian Translation Studies
| Reagent/Category | Specific Examples | Research Application | Chronotype Considerations |
|---|---|---|---|
| Diurnal Rodent Models | Arvicanthis niloticus (Nile grass rat), Octodon degus | Direct modeling of diurnal physiology | Natural diurnal pattern enables human-relevant timing studies |
| Circadian Reporter Systems | PER2::LUC, BMAL1::LUC knock-in lines | Real-time monitoring of circadian rhythms in vitro and in vivo | Conserved molecular machinery enables cross-species comparison |
| Clock Gene Targeting Tools | CRISPR/Cas9 systems, siRNA/shRNA constructs | Functional analysis of clock gene variants | Polymorphism-specific reagents needed for human vs. rodent studies |
| Hormone Assays | ELISA, RIA, LC-MS/MS kits for melatonin, cortisol | Endocrine rhythm characterization | Timing of sampling must account for opposite activity phases |
| Neuromodulator Receptors | MT1/MT2 agonists/antagonists, GR/MR modulators | Analysis of endocrine-circadian interactions | Receptor distribution and sensitivity may differ between chronotypes |
| Transcriptomic Tools | RNA-seq, single-cell RNA-seq, spatial transcriptomics | Systems-level analysis of rhythmic gene expression | 45-80% of genes show tissue-specific circadian expression |
Implications for Drug Development and Chronotherapeutics
Circadian Regulation of Drug Metabolism
Circadian rhythms significantly influence drug metabolism and efficacy through rhythmic expression of drug-metabolizing enzymes. Research has identified two primary modes for generation of diurnal rhythmicity in these enzymes: (1) a general mode where core clock genes generate rhythms via transcriptional actions on E-box, D-box, and Rev-RE/RORE cis-elements; and (2) an alternative mode involving cycling nuclear receptors such as HNF4α and PPARγ [119]. These mechanisms create time-dependent variations in enzyme activity that can affect drug efficacy and toxicity.
For example, mouse Cyp3a11 (analogous to human CYP3A4) shows higher expression at night, leading to increased detoxification of substrates such as aconitine, triptolide, and brucine during this period [119]. This temporal variation results in significantly different toxicity profiles based on administration time, with higher toxicity observed during daytime hours when detoxification capacity is reduced [119]. Similar patterns have been documented for over 300 medications, with variability in effects of up to 10-fold depending on dosing time [119].
Chronotherapy Approaches
Chronotherapy—the strategic timing of medication administration to align with biological rhythms—has demonstrated significant potential for optimizing therapeutic outcomes. Clinical studies have shown that chronotherapy can improve drug efficacy by approximately 2-fold and enhance tolerability by up to 5-fold compared to conventional dosing regimens [119]. This approach is particularly relevant for medications with narrow therapeutic windows and significant time-dependent pharmacokinetics.
Mathematical modeling approaches have helped characterize the factors influencing time-of-day drug sensitivity, including circadian properties (amplitude, period, decay rate) and drug-specific characteristics [68]. These models reveal that the amplitude of circadian oscillations in effective drug concentration proportionally increases the maximum range of time-of-day responses, while longer circadian periods (up to approximately 32 hours) maintain relatively stable response ranges before gradually decreasing [68]. Such modeling provides valuable insights for designing chronotherapy regimens tailored to specific drug and disease characteristics.
Circadian Genes as Therapeutic Targets
Beyond influencing drug metabolism, core clock components themselves represent promising therapeutic targets. Clock-controlled genes include many druggable targets, with 82.2% of genes coding for FDA-approved drug targets showing cyclic oscillations in transcription [10]. Synthetic ligands for clock components such as REV-ERBα/β have shown potential for modulating circadian amplitude and phase, offering novel approaches for treating circadian rhythm disorders and associated conditions [117].
The relationship between clock gene polymorphisms and psychiatric disorders further supports the therapeutic potential of circadian targets. Genetic variations in CLOCK, BMAL1, PER, and CRY genes have been associated with mood disorders, schizophrenia, and substance abuse, suggesting that circadian-targeted therapies may benefit these conditions [116] [117]. Additionally, traditional medicine formulations have been found to exert multi-pathway regulatory effects on clock gene expression, providing potential leads for novel chronotherapeutic development [117].
Diagram Title: Circadian Influence on Drug Response
The translation of circadian insights from nocturnal rodent models to diurnal humans requires careful consideration of chronotype-specific differences in physiological organization. While the core molecular clock machinery is conserved across species, critical differences in phase relationships between central and peripheral oscillators, opposite responses to environmental cues such as light, and distinct endocrine rhythms create significant translational challenges. By utilizing diurnal animal models, employing advanced molecular techniques, incorporating chronotherapeutic principles in drug development, and applying appropriate experimental design considerations, researchers can enhance the translational validity of circadian research. As our understanding of chronotype differences continues to grow, so too does the potential for developing more effective, circadian-optimized therapies for human disease.
The endocrine system plays a pivotal role as both a regulator and output of the circadian system, creating a complex feedback network that maintains temporal homeostasis [6]. This whitepaper evaluates the robustness of circadian rhythms by comparing two fundamental manipulation strategies: genetic interventions that target the core molecular clockwork and environmental approaches that alter zeitgebers (time-giving cues). For researchers and drug development professionals, understanding the distinct resilience and vulnerabilities of these systems is crucial for developing chronotherapeutic strategies that can withstand biological variability and real-world challenges [120] [117]. The robustness of circadian rhythms—their ability to maintain stable period and phase against perturbations—varies significantly depending on whether manipulations target genetic components or environmental inputs, with implications for treating metabolic, psychiatric, and sleep disorders [6] [117] [121].
Molecular Foundations of Circadian Rhythms
Core Clock Machinery
The mammalian circadian clock operates through autoregulatory transcription-translation feedback loops (TTFLs) that generate approximately 24-hour oscillations [38] [117]. At its core, the BMAL1/CLOCK heterodimer activates transcription of Period (Per1, Per2, Per3) and Cryptochrome (Cry1, Cry2) genes by binding to E-box elements in their promoter regions [38] [117]. Following translation and complex post-translational modifications, PER/CRY protein complexes accumulate in the nucleus to inhibit BMAL1/CLOCK activity, completing the primary negative feedback loop [38].
An auxiliary loop involves REV-ERBα/β and RORα/γ, which competitively bind to ROR response elements (ROREs) on the Bmal1 promoter, creating rhythmic expression of BMAL1 [38] [117]. This multi-loop architecture enhances system robustness by providing compensatory mechanisms when individual components are disrupted [120] [122].
Post-Translational Regulation
Post-translational modifications (PTMs) critically regulate clock protein stability, localization, and activity, serving as key mechanisms that determine circadian robustness [38] [117]. Phosphorylation of PER proteins by casein kinase 1δ/ε (CK1δ/ε) marks them for ubiquitination and proteasomal degradation, while F-Box and Leucine-Rich Repeat Protein 3 (FBXL3)-mediated ubiquitination targets CRY proteins [117]. Recent research has identified SUMOylation as a novel regulatory layer that modulates CLOCK-BMAL1 transcriptional activity and stability [117]. These PTMs provide precise control over the timing and amplitude of circadian rhythms, allowing for rapid adjustments without requiring new protein synthesis.
Systemic Synchronization
The suprachiasmatic nucleus (SCN) serves as the master pacemaker, integrating light information from the retina and synchronizing peripheral clocks throughout the body [111] [38]. The SCN communicates timing signals via neural pathways and endocrine pathways, particularly through rhythmic secretion of melatonin and glucocorticoids [6] [38]. This hierarchical organization allows both systemic coordination and tissue-specific circadian programming, with peripheral clocks in organs like the liver, heart, and adrenal glands responding to local environmental cues such as feeding-fasting cycles [6] [44].
Quantitative Analysis of Manipulation Robustness
Genetic Manipulation Approaches
Table 1: Genetic Manipulation Methods and Their Effects on Circadian Robustness
| Method | Molecular Target | Effect on Period | Effect on Amplitude | Robustness Assessment |
|---|---|---|---|---|
| Bmal1 Knockout | Core clock gene | Complete arrhythmia [117] | Zero amplitude [117] | Low - Complete loss of circadian function |
| Clock Mutation | Core clock gene | Reduced sleep time, advanced phase [117] | Altered rhythm stability [117] | Low-Moderate - Severe behavioral disruptions |
| Per1/2 Knockout | Negative limb of core loop | Shortened period (~22h) [117] | Reduced amplitude [117] | Moderate - Maintains rhythmicity with altered parameters |
| Cry1/2 Knockout | Negative limb of core loop | Altered period length [117] | Increased NREM sleep time [117] | Moderate - Compensatory mechanisms maintain some function |
| Per3 VNTR Polymorphism | Circadian stability | Altered phase timing [117] | Changes in sleep architecture [117] | High - Modifications rather than disruptions |
| REV-ERBα/β Agonists | Auxiliary loop | Phase-dependent period modulation [117] | Enhanced rhythm amplitude [117] | High - Therapeutic enhancement of existing rhythms |
Genetic manipulations demonstrate a threshold effect where core component disruption (BMAL1, CLOCK) causes complete rhythm loss, while modifications to auxiliary components (PER3, REV-ERB) yield more graduated effects [117]. Mathematical models reveal that the core TTFL exhibits parameter sensitivity, requiring unrealistically tight binding constants (K_d ≤ 0.04 nM) to sustain oscillations in basic models [120]. However, incorporating multistep posttranslational modifications and nonlinear degradation kinetics increases permissible parameter ranges, reflecting the biological system's inherent robustness [120].
Environmental Manipulation Approaches
Table 2: Environmental Manipulations and Their Effects on Circadian Robustness
| Method | Target System | Phase Response | Amplitude Effect | Recovery Time |
|---|---|---|---|---|
| Light Exposure (Night) | SCN photoreception | Phase delay up to 2-3h [111] | Acute suppression [6] | 1-3 days [111] |
| Melatonin Administration | MT1/MT2 receptors | Phase advance (~1h) [6] | Enhanced rhythm stability [6] | <24h [6] |
| Scheduled Feeding | Peripheral clocks | Food-entrainable oscillator alignment [6] | Tissue-specific amplitude changes [6] | 3-5 cycles [6] |
| Shift Work Protocols | Entire circadian system | Progressive misalignment [117] | Rhythm dissociation [117] | Weeks [117] |
| Jet Lag Protocol | Entrainment system | Transient desynchronization [111] | Temporary amplitude reduction [111] | ~1 day/time zone [111] |
| Chemical Disruptors (PCBs, metals) [103] | Multiple cellular targets | Variable, compound-dependent [103] | Concentration-dependent suppression [103] | Poorly characterized [103] |
Environmental manipulations typically exhibit dose-response relationships and phase-dependent effects [111] [6]. The SCN demonstrates remarkable entrainment flexibility, adjusting to gradually changing zeitgeber cycles while resisting abrupt changes—a property quantified as "circadian resilience" [122]. However, chronic environmental disruption (e.g., shift work) induces maladaptive plasticity that can lead to permanent circadian misalignment and associated health consequences [117] [121].
Experimental Protocols for Robustness Assessment
Genetic Perturbation Protocol
Gene Editing Using CRISPR-Cas9 in Model Organisms
- Objective: To assess robustness through targeted disruption of core clock genes.
- Materials: CRISPR-Cas9 system, guide RNAs targeting Bmal1, Per2, or Cry1; model organism embryos (zebrafish, mice); genotyping reagents; locomotor activity monitoring system [120] [117].
- Procedure:
- Design and validate guide RNAs with high efficiency and minimal off-target effects.
- Microinject CRISPR components into single-cell embryos.
- Raise founders and establish mutant lines through breeding.
- Validate mutations using sequencing and Western blotting.
- Monitor locomotor activity in constant darkness (DD) to assess endogenous period.
- Challenge with light pulses at different circadian times to measure phase-response curves.
- Analyze period stability, rhythm power, and inter-tissue synchrony using Lomb-Scargle periodogram analysis [120].
- Robustness Metrics: Coefficient of variation for period length, rhythm amplitude, phase coherence across tissues, and recovery time after perturbation [120] [122].
Environmental Perturbation Protocol
Shift Work Simulation in Human Participants
- Objective: To quantify robustness against misalignment between environmental and endogenous cycles.
- Materials: Saliva collection kits (Salivettes), actigraphy monitors, dim-light melatonin onset (DLMO) assessment equipment, cortisol assay kits, RNA extraction reagents for transcriptomic analysis [57].
- Procedure:
- Recruit participants with confirmed morning or evening chronotypes using the Morningness-Eveningness Questionnaire (MEQ) [57].
- Establish baseline circadian phase through DLMO measurement.
- Implement 7-day simulated shift work protocol with sleep/wake cycle inversion.
- Collect saliva samples at 3-4 hour intervals over 24-hour periods pre-, during, and post-protocol.
- Isolve RNA from saliva and analyze core clock gene expression (ARNTL1, PER2, NR1D1) using qPCR or TimeTeller methodology [57].
- Assay cortisol and melatonin levels from saliva samples using ELISA.
- Monitor rest-activity rhythms using wrist actigraphy.
- Robustness Metrics: Phase shift magnitude, amplitude reduction, internal desynchronization measures, transcriptomic resilience index, and recovery rate to baseline [57] [117].
Mathematical Modeling Approach
Bifurcation Analysis of Circuit Robustness
- Objective: To computationally assess the parameter sensitivities of circadian clock models.
- Materials: Kim & Forger-style ordinary differential equation models, XPPAUT or MATLAB bifurcation software, parameter estimation algorithms [120].
- Procedure:
- Implement the core single negative feedback (SNF) model with appropriate kinetic parameters.
- Systematically vary key parameters (e.g., PER:BMAL1 binding affinity, transcription rates, degradation rates).
- Identify oscillatory parameter ranges using continuation algorithms.
- Compute Floquet multipliers to determine structural stability.
- Extend analysis to dual-loop models incorporating REV-ERB and ROR feedback.
- Compare robustness between model architectures using parametric sensitivity indices [120].
- Robustness Metrics: Oscillatory parameter space volume, tolerance to parameter variation, period stability across parameter changes [120] [122].
Signaling Pathways in Circadian Manipulation
The molecular pathways governing circadian responses to genetic and environmental manipulations involve complex interactions between core clock components and endocrine signals.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Circadian Rhythm Manipulation Studies
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Gene Editing Tools | CRISPR-Cas9 systems, siRNA against clock genes [117] | Targeted genetic disruption | Off-target effects; temporal control of knockdown |
| Chemical Agonists/Antagonists | REV-ERB agonists (SR9009), CK1δ/ε inhibitors [117] | Pharmacological manipulation of clock components | Specificity; dose-response characterization |
| Hormone Assays | Salivary cortisol/melatonin ELISA kits [57] | Non-invasive endocrine rhythm assessment | Sampling frequency; dim light conditions for melatonin |
| Transcriptomics | TimeTeller kits, qPCR reagents for core clock genes [57] | Molecular rhythm profiling in human saliva | RNA stability; reference gene selection |
| Activity Monitoring | Actigraphy devices, running wheels for rodents [57] | Behavioral rhythm analysis in free-living conditions | Data density; appropriate analysis algorithms |
| Mathematical Modeling | Bifurcation analysis software (XPPAUT) [120] | In silico robustness assessment | Parameter estimation; model validation |
Discussion and Research Implications
Comparative Robustness Analysis
The circadian system demonstrates hierarchical robustness, with the core SCN pacemaker exhibiting greater stability against genetic and environmental perturbations than peripheral oscillators [111] [38]. Genetic manipulations reveal that the multi-loop architecture of the circadian clock provides built-in redundancy, where auxiliary feedback loops can partially compensate when core components are compromised [120] [122]. Environmental manipulations demonstrate that the system maintains entrainment flexibility while resisting complete arrhythmia, though chronic misalignment can overwhelm homeostatic mechanisms [6] [117].
From a therapeutic perspective, the superior robustness of environmental interventions like timed light exposure and melatonin administration explains their clinical efficacy for conditions like delayed sleep phase disorder and jet lag [6] [117]. However, genetic approaches offer greater specificity for targeting pathological processes in particular tissues, such as REV-ERB agonists for metabolic disorders [117].
Future Research Directions
Key challenges remain in understanding tissue-specific robustness variations and developing personalized chronotherapies based on individual circadian phenotypes [57] [117]. The emerging recognition of epigenetic regulation of clock genes suggests another layer of plasticity that modulates robustness across the lifespan [117]. Future research should focus on:
- Developing more comprehensive mathematical models that incorporate tissue-specific parameters and endocrine interactions [120].
- Establishing standardized robustness metrics that enable cross-study comparisons [57] [122].
- Exploring the role of novel post-translational modifications like SUMOylation in modulating circadian stability [117].
- Investigating the impact of environmental circadian disruptors (e.g., pesticides, heavy metals) on system robustness [103].
Understanding the differential robustness to genetic versus environmental manipulation will accelerate the development of effective chronotherapeutics for the range of metabolic, psychiatric, and sleep disorders linked to circadian disruption [117] [121].
Circadian rhythms, the endogenous 24-hour biological cycles governing diverse physiological processes, are fundamentally regulated by endocrine signaling. The suprachiasmatic nucleus (SCN) of the hypothalamus serves as the master circadian pacemaker, integrating environmental light cues and coordinating peripheral clocks throughout the body via neural and hormonal pathways [38]. This circadian system regulates the rhythmic secretion of key endocrine signals including melatonin, cortisol, and thyroid-stimulating hormone (TSH), which in turn synchronize cellular and tissue-level rhythms across organ systems [38] [123]. Disruptions to this precise temporal organization—whether through genetic mutation, environmental misalignment (e.g., shift work), or lifestyle factors—are increasingly implicated in disease pathogenesis across multiple domains including metabolic disorders, neurodegenerative conditions, and cancer [38] [124].
Within this context, the assessment of circadian rhythm restoration represents a critical frontier in therapeutic development. The endocrine system provides both targets for intervention and biomarkers for monitoring therapeutic efficacy. This technical guide examines current biomarker modalities and methodologies for quantifying circadian recovery, with particular emphasis on their application in endocrine-focused circadian medicine. We present a structured framework for biomarker classification, detailed experimental protocols for biomarker assessment, and emerging technologies that are advancing the precision of circadian rhythm evaluation in both research and clinical settings.
Classification and Characteristics of Circadian Biomarkers
Circadian biomarkers can be categorized into molecular, physiological, and endocrine classes, each with distinct characteristics, measurement methodologies, and applications. The following table summarizes the primary biomarker classes used in circadian rhythm assessment.
Table 1: Classification and Characteristics of Circadian Biomarkers
| Biomarker Class | Specific Markers | Biological Source | Measurement Approach | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|
| Endocrine | Melatonin (DLMO), Cortisol | Plasma, Saliva | Immunoassays, LC-MS | Direct SCN output; strong rhythmicity | Requires controlled conditions; sampling frequency |
| Molecular | Core Clock Genes (PER, CRY, BMAL1), Circadian-Related Output Genes (ABCC2, FBXW7) | Blood, Tissue biopsies | RNA sequencing, RT-qPCR | Mechanistic insight; high specificity | Invasive sampling; tissue-specific expression |
| Physiological | Skin temperature, Heart rate, Activity rhythms | Wearable sensors | Continuous monitoring (e.g., Fitbit) | Non-invasive; continuous data | Subject to behavioral masking |
| Metabolic | Bone Turnover Markers (BTMs), Glucose, Insulin | Blood | Immunoassays, Biochemical assays | Functional output; clinical relevance | Influenced by diet and activity |
The establishment of circadian phase, particularly through the dim-light melatonin onset (DLMO) in plasma or saliva, remains the gold standard for assessing the timing of the central SCN pacemaker [125] [126]. Meanwhile, rhythmic expression of core clock genes and their outputs (e.g., ABCC2, FBXW7) in peripheral blood mononuclear cells (PBMCs) or tissues provides a window into the molecular clockwork in specific cell types [127] [128]. Emerging research has identified specific circadian rhythm-related differentially expressed genes (CRRDEGs)—such as ECE1, FLT3, and APPL1 in osteoporosis, and ABCC2 and FBXW7 in melanoma—as potential diagnostic and prognostic biomarkers, revealing the intersection between circadian disruption and specific disease pathologies [127] [128].
Physiological rhythms in heart rate and activity, monitored via wearable devices, offer a non-invasive method for estimating circadian phase over extended periods in naturalistic environments. Recent advances have introduced novel computational biomarkers from wearable data, such as the continuous wavelet circadian rhythm energy (CCE) and relative amplitude of heart rate, which have shown strong associations with metabolic syndrome [129]. These physiological rhythms, however, are subject to "behavioral masking," where the direct effects of activity and sleep obscure the endogenous circadian signal, necessitating analytical approaches that can disentangle these influences [125].
Methodologies for Circadian Biomarker Assessment
Protocol 1: Assessing Molecular Circadian Rhythmicity in Human Blood
Objective: To quantify circadian gene expression rhythms in human peripheral blood mononuclear cells (PBMCs) and identify circadian rhythm-related differentially expressed genes (CRRDEGs) for diagnostic biomarker discovery.
Materials and Reagents:
- PAXgene Blood RNA tubes or similar collection system
- RNA extraction kit (e.g., Qiagen RNeasy)
- cDNA synthesis kit
- Quantitative PCR system with reagents or RNA-seq preparation kit
- Primer sets for core clock genes (BMAL1, PER1-3, CRY1-2, REV-ERBα) and candidate output genes
- Bioinformatics software (R, limma package, WGCNA, machine learning packages)
Procedure:
- Participant Preparation and Sampling: Recruit participants according to protocol (e.g., healthy controls vs. patients). For precise phase assessment, collect serial blood samples over a 24-48 hour period under controlled conditions. A minimum of 8 timepoints at 3-hour intervals is recommended. Record precise collection times.
- RNA Extraction and Quality Control: Isolate total RNA from PBMCs using standard procedures. Assess RNA integrity and concentration using spectrophotometry or bioanalyzer systems. Only samples with RNA Integrity Number (RIN) >7.0 should proceed.
- Gene Expression Analysis: Convert RNA to cDNA. Perform quantitative PCR using validated primer sets or prepare libraries for RNA sequencing. For transcriptomic analysis, utilize platforms such as Affymetrix Human Genome U133 Plus 2.0 Array or RNA-seq.
- Bioinformatic and Machine Learning Analysis:
- Differential Expression: Use R package "limma" to identify differentially expressed genes (DEGs) between case and control groups (e.g., |logFC| > 0.1-1.2, p < 0.05) [127] [128].
- CRRDEG Identification: Intersect DEGs with a database of known circadian rhythm-related genes (e.g., from CGDB, MSigDB, or GeneCards) to identify circadian rhythm-related differentially expressed genes [127] [128].
- Functional Enrichment: Perform Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analysis on CRRDEGs using "clusterProfiler" in R [127].
- Machine Learning Biomarker Selection: Apply multiple machine learning algorithms (Support Vector Machine (SVM), Random Forest, Generalized Linear Model, Extreme Gradient Boosting) to identify top predictor genes from CRRDEGs. Validate key genes (e.g., top 5 from SVM) using independent datasets [127].
Analysis: Key outputs include phase and amplitude of core clock gene expression, identification of disease-specific CRRDEGs, and diagnostic performance (AUC) of machine learning models based on key circadian genes.
Protocol 2: Determining Dim-Light Melatonin Onset (DLMO)
Objective: To establish the phase of the central circadian pacemaker by measuring the onset of melatonin secretion under dim-light conditions.
Materials and Reagents:
- Dim red light source (<10 lux)
- Salivettes or plasma collection tubes
- Radioimmunoassay (RIA) or ELISA kits for melatonin
- Controlled environment facility
Procedure:
- Participant Preparation: Participants should avoid caffeine, alcohol, and nicotine for 24 hours prior. Maintain a regular sleep-wake schedule for at least one week beforehand.
- Light Control: Begin dim-light conditions (<10 lux) at least 2 hours before expected melatonin onset. Use dim red light for sample collection and necessary activities.
- Sample Collection: Collect saliva or blood plasma samples hourly beginning 7 hours before habitual bedtime until 1 hour after bedtime [126].
- Melatonin Assay: Process samples using established RIA or ELISA protocols. Determine DLMO as the time when melatonin concentration consistently exceeds a threshold (typically 3-4 pg/mL in saliva) [126].
Analysis: Plot melatonin concentration against clock time. DLMO is typically defined as the point where melatonin levels cross and remain above a predetermined threshold (e.g., 3-4 pg/mL for saliva).
Protocol 3: Wearable-Based Circadian Biomarker Derivation
Objective: To extract circadian rhythm biomarkers from continuous wearable sensor data for metabolic disease assessment.
Materials and Reagents:
- Wearable device with heart rate and accelerometer sensors (e.g., Fitbit Versa/Inspire 2)
- Data analysis software (R, Python) with signal processing capabilities
Procedure:
- Data Collection: Participants wear devices for a minimum of 5-7 consecutive days, including weekdays and weekends. Collect minute-level heart rate and step count data [129].
- Preprocessing: Remove periods of non-wear (e.g., >6 hours of consecutive zero steps). Impute short missing segments if necessary.
- Circadian Marker Calculation:
- Parametric Analysis: Fit 24-hour cosine curves to heart rate data to calculate Mesor (mean), Amplitude (peak-trough difference), and Acrophase (peak time).
- Non-Parametric Analysis: Calculate Interdaily Stability (IS), Intradaily Variability (IV), and Relative Amplitude (RA) from activity data.
- Novel Biomarkers: Compute Continuous Wavelet Circadian Energy (CCE) using continuous wavelet transform on heart rate signals to quantify rhythm strength [129].
- Statistical Analysis and Machine Learning: Compare circadian metrics between groups (e.g., Metabolic Syndrome vs. healthy) using t-tests/Wilcoxon tests. Apply explainable AI (XAI) models (SHAP, Explainable Boosting Machine) to determine feature importance for disease classification [129].
Analysis: Key outcomes include significant differences in circadian parameters between clinical groups, and importance metrics from XAI models highlighting the most predictive circadian biomarkers.
Signaling Pathways and Molecular Mechanisms
The molecular circadian clock operates through cell-autonomous transcription-translation feedback loops (TTFLs). The core loop involves the activators BMAL1 and CLOCK, which form a heterodimer that binds to E-box elements in the promoters of Period (PER) and Cryptochrome (CRY) genes, driving their transcription. PER and CRY proteins accumulate, form complexes, and translocate back to the nucleus to repress BMAL1:CLOCK activity, completing the approximately 24-hour cycle [38].
A stabilizing auxiliary loop involves the nuclear receptors REV-ERBα and RORα, which compete for ROR response elements (ROREs) in the BMAL1 promoter. REV-ERB suppresses while ROR activates BMAL1 transcription, adding robustness to the oscillator [38]. This molecular clockwork regulates the rhythmic expression of clock-controlled genes (CCGs), which in turn coordinate endocrine secretion, metabolic fluxes, and immune function.
The following diagram illustrates the core transcriptional feedback loops and their connection to endocrine outputs:
Diagram Title: Core Circadian Clock Feedback Loops
Post-translational modifications, including phosphorylation and ubiquitination, critically regulate the timing, stability, and nuclear translocation of core clock components. For instance, the phosphorylation of BMAL1 at specific residues (e.g., Ser42) enables it to exert non-transcriptional effects at synapses, while rhythmic ubiquitination of PER and CRY controls their degradation and thus the period length of the clock [38].
Advanced Applications and Therapeutic Targeting
Chronotherapy and Circadian Biomarker Applications
Chronotherapy—the timing of drug administration to coincide with rhythms in drug metabolism, target susceptibility, and therapeutic index—represents a major translational application of circadian biology. In hematological malignancies, for example, circadian clock genes serve as diagnostic and prognostic biomarkers, and treatment timing can significantly impact efficacy and toxicity [124]. The following diagram outlines a workflow for developing circadian biomarker-informed therapies:
Diagram Title: Circadian Biomarker Therapeutic Workflow
Engineered Circadian Therapies
Cutting-edge approaches are leveraging synthetic biology to create therapies that respond directly to circadian biomarkers. One pioneering example is a melatonin-inducible gene switch for type-2 diabetes therapy. This system uses ectopically expressed melatonin receptor 1A (MTNR1A) linked to a cAMP-mediated signaling cascade that drives transgene expression from a synthetic promoter containing cAMP response elements (CRE) [123].
The system is engineered to be responsive specifically to night-time physiological concentrations of melatonin (peaking at ~700 pM), while remaining inactive during daytime low levels, creating a closed-loop, circadian-regulated therapeutic. When implanted in mouse models, engineered cells with this switch secreted therapeutic peptides like glucagon-like peptide-1 (GLP-1) exclusively during the night, effectively restoring normoglycemia [123]. This demonstrates the potential of using endogenous circadian hormones as inputs to control the timing and level of therapeutic transgene expression.
Simultaneously, advanced drug delivery platforms are being developed for circadian medicine. Nanomaterial-based systems (e.g., liposomes, polymeric nanoparticles) enable sustained and targeted drug release, and can be designed as "smart" systems that respond to physiological cues such as temperature or pH changes, allowing for timing-specific drug release aligned with circadian rhythms [130].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for Circadian Biomarker Investigation
| Reagent / Material | Primary Function | Example Application | Technical Notes |
|---|---|---|---|
| PAXgene Blood RNA Tubes | RNA stabilization in whole blood | Molecular rhythm analysis from blood draws | Enables multi-timepoint sampling from single subjects; critical for gene expression time series |
| Melatonin RIA/ELISA Kits | Quantification of melatonin in saliva/plasma | Determination of DLMO | Saliva collection allows for at-home sampling; requires strict dim-light conditions pre-collection |
| cDNA Synthesis & qPCR Kits | Gene expression analysis from RNA | Quantifying clock gene expression rhythms | Pre-validated primer-probe sets for human clock genes (e.g., ARNTL, PER1-3) are commercially available |
| Circadian Reporter Cell Lines | Real-time monitoring of cellular circadian rhythms | In vitro chronotherapy screening | Often use luciferase reporters under control of clock gene promoters (e.g., Bmal1:luc) |
| Wearable Activity Monitors | Continuous physiological monitoring (HR, activity) | Deriving non-parametric circadian metrics | Devices like Actiwatch or Fitbit; require consistent wear (≥5 days) and data processing pipelines |
| Machine Learning Algorithms (SVM, RF) | Feature selection & diagnostic model building | Identifying key CRRDEGs from high-dimensional data | Implementable in R/Python (e.g., 'caret', 'DALEX' packages in R) [127] |
| Nanomaterial Carriers (Liposomes, PNPs) | Timed drug delivery | Chronotherapy for improved efficacy/toxicity ratio | Can be engineered for triggered release in response to circadian physiological cues [130] |
The precise assessment of circadian rhythm restoration requires a multimodal approach, integrating gold-standard endocrine measures like DLMO with emerging molecular and physiological biomarkers. The field is rapidly advancing toward methodologies that can accurately determine internal circadian time from minimal samples, enabling practical application in clinical trials and personalized medicine. As our understanding of the intricate relationship between endocrine signaling and circadian organization deepens, so too will our ability to develop and monitor targeted therapies that restore healthy circadian function, ultimately improving outcomes across a broad spectrum of diseases.
Conclusion
The intricate crosstalk between the endocrine system and circadian clocks is fundamental to physiological homeostasis, and its disruption presents a significant pathophysiological trigger for numerous chronic diseases. The key takeaway is the transition from viewing hormones as mere outputs of the circadian system to recognizing their active role as critical zeitgebers and tuners of peripheral clocks. Future research must focus on elucidating tissue-specific clock mechanisms and developing sophisticated, targeted chronotherapeutics. For biomedical and clinical research, this promises a new frontier in personalized medicine, where treatment strategies are synchronized with an individual's internal time to maximize efficacy and minimize adverse effects. The integration of circadian biology into drug development pipelines and public health recommendations holds immense potential for preventing and managing the growing burden of circadian rhythm-related diseases.
References
- 1. Neuroanatomy, Nucleus Suprachiasmatic - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK546664/]
- 2. Suprachiasmatic Nucleus: Cell Autonomy and Network ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3758475/]
- 3. Suprachiasmatic nucleus - Wikipedia [https://en.wikipedia.org/wiki/Suprachiasmatic_nucleus]
- 4. Generation of circadian rhythms in the suprachiasmatic ... [https://www.nature.com/articles/s41583-018-0026-z]
- 5. Suprachiasmatic nucleus-wide estimation of oscillatory ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1012855]
- 6. Endocrine regulation of circadian rhythms [https://www.nature.com/articles/s44323-025-00024-6]
- 7. Minireview: The Neuroendocrinology of the Suprachiasmatic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3423957/]
- 8. Suprachiasmatic Nucleus - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/suprachiasmatic-nucleus]
- 9. Role of circadian transcription factor REV-ERB in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12006074/]
- 10. Molecular regulations of circadian rhythm and implications ... [https://www.nature.com/articles/s41392-022-00899-y]
- 11. Nanomaterial-enabled drug delivery systems for circadian ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra04137f]
- 12. Regulation of therapeutic protein release in response to ... [https://www.nature.com/articles/s41467-025-64761-9]
- 13. The REV-ERBs and RORs: molecular links between circadian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3134326/]
- 14. circadian regulation of host-microbiota crosstalk in ... [https://pubmed.ncbi.nlm.nih.gov/41262263/]
- 15. A Rhythmic Ror [https://www.sciencedirect.com/science/article/pii/S089662730400491X]
- 16. Co-existing feedback loops generate tissue-specific ... [https://www.life-science-alliance.org/content/1/3/e201800078]
- 17. Redundant Function of REV-ERBα and β and Non-Essential ... [https://journals.plos.org/plosgenetics/article?id=10.1371/journal.pgen.1000023]
- 18. Frontiers | Peripheral clocks and systemic zeitgeber interactions: from molecular mechanisms to circadian precision medicine [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1606242/full]
- 19. Suprachiasmatic Nucleus Neuron - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/immunology-and-microbiology/suprachiasmatic-nucleus-neuron]
- 20. Frontiers | Mutual Shaping of Circadian Body-Wide Synchronization by the Suprachiasmatic Nucleus and Circulating Steroids [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2022.877256/full]
- 21. Syntalos: a software for precise synchronization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11736130/]
- 22. Peripheral clocks and systemic zeitgeber interactions [https://pmc.ncbi.nlm.nih.gov/articles/PMC12158691/]
- 23. New perspectives on the role of melatonin in human sleep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6057895/]
- 24. Training the circadian clock, clocking the drugs and drugging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7249726/]
- 25. The Role of Melatonin in the Circadian Rhythm Sleep ... [https://www.psychiatrictimes.com/view/role-melatonin-circadian-rhythm-sleep-wake-cycle]
- 26. Melatonin: beyond circadian regulation - exploring its ... [https://www.sciencedirect.com/science/article/abs/pii/S1087079225000760]
- 27. Physiology, Glucocorticoids - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK560897/]
- 28. Interactions between sleep, stress, and metabolism [https://pmc.ncbi.nlm.nih.gov/articles/PMC4688585/]
- 29. Regulatory and Mechanistic Actions of Glucocorticoids on ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2018.00235/full]
- 30. Sleep disorders impact hormonal regulation: unravelling the ... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-025-01871-w]
- 31. Multi-Modal Regulation of Circadian Physiology by Interactive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8772734/]
- 32. Genomics of circadian rhythms in health and disease [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-019-0704-0]
- 33. Differentiating external zeitgeber impact on peripheral circadian clock resetting | Scientific Reports [https://www.nature.com/articles/s41598-019-56323-z]
- 34. Circadian clock mechanism driving mammalian ... [https://www.nature.com/articles/s41467-020-18061-z]
- 35. Circadian Clock Control of Endocrine Factors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4304769/]
- 36. CLOCK and NPAS2 have overlapping roles in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2950611/]
- 37. Upstream open reading frames dynamically modulate CLOCK ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12121920/]
- 38. Circadian Rhythm: Biological Functions, Diseases, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547082/]
- 39. Cortisol Detection Methods and the Hormone's Role in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12470794/]
- 40. Emerging trends in wearable and non-invasive cortisol ... [https://pubs.rsc.org/en/content/articlelanding/2025/tb/d5tb01519g]
- 41. Autonomous wearable sensing enabled by capillary ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00536a]
- 42. Circadian inference of rhythmicity using comparative ... [https://www.sciencedirect.com/science/article/pii/S2590137025000834]
- 43. New study: Sweat-based wearable sensor for cortisol and ... [https://www.linkedin.com/posts/shalini-prasad-87040aa_biosensors-bioelectronicsx-research-activity-7362989499330527232-Elil]
- 44. Editorial: Circadian rhythm in adrenal endocrinology [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1620570/full]
- 45. Melatonin and Cortisol Suppression and Circadian Rhythm ... [https://www.mdpi.com/2039-7283/15/11/199]
- 46. A glial circadian gene expression atlas reveals cell-type ... [https://www.nature.com/articles/s41593-025-02067-1]
- 47. Transcriptome profiling revealed multiple circadian rhythm ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1422122/full]
- 48. A mixed-effects cosinor modelling framework for circadian ... [https://www.sciencedirect.com/science/article/abs/pii/S0022519325002851]
- 49. BioDare2 - circadian period analysis [https://biodare2.ed.ac.uk/]
- 50. A Bayesian framework for genome-wide circadian rhythmicity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560793/]
- 51. Rhythm profiling using COFE reveals multi-omic circadian ... [https://pubmed.ncbi.nlm.nih.gov/40424435/]
- 52. Environmental endocrine disrupting chemicals: Disruptors ... [https://www.sciencedirect.com/science/article/abs/pii/S0149763425003719]
- 53. New research will map the impact of sleep and circadian ... [https://www.rdm.ox.ac.uk/news/new-research-will-map-the-impact-of-sleep-and-circadian-rhythm-disruption-on-cardiometabolic-disease]
- 54. Voluntary wheel running exercise improves sleep disorder ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12187974/]
- 55. A novel circadian behavior rhythm in arrhythmic Period triple ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12396279/]
- 56. Chronic circadian disruption in adolescent mice impairs ... [https://www.nature.com/articles/s41598-025-12237-7]
- 57. Comprehensive integrative analysis of circadian rhythms in ... [https://www.nature.com/articles/s44323-025-00035-3]
- 58. Frequent Shifts During Chronic Jet Lag Uncouple Liver ... [https://pubmed.ncbi.nlm.nih.gov/39773136/]
- 59. Impact of Social Isolation on Circadian Rhythmicity and ... [https://www.sciencedirect.com/science/article/abs/pii/S0031938425003804]
- 60. Gut jet lag: how circadian rhythm disruption undermines ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1678482/full]
- 61. Gut jet lag: how circadian rhythm disruption undermines the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12528175/]
- 62. Circadian Rhythms Play a Role in Muscle Repair - News Center [https://news.feinberg.northwestern.edu/2025/03/10/circadian-rhythms-play-a-role-in-muscle-repair/]
- 63. The clinical impact of chronopharmacology on current ... [https://pubmed.ncbi.nlm.nih.gov/39792169/]
- 64. The importance of determining circadian parameters in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6637036/]
- 65. Editorial: Circadian rhythm in metabolism and endocrinology [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1263823/full]
- 66. Leveraging Circadian Rhythms in Diabetes Treatment [https://chronobiologyinmedicine.org/m/journal/view.php?number=214]
- 67. Rhythmicity as an important regulatory factor in complex ... [https://arh.amegroups.org/article/view/4616/html]
- 68. A combined mathematical and experimental approach ... [https://www.nature.com/articles/s42003-025-07931-1]
- 69. Chronopharmacology of diuresis via metabolic profiling ... [https://www.sciencedirect.com/science/article/abs/pii/S0944711323006189]
- 70. Circadian rhythm homeostasis biomarkers [https://www.sciopen.com/article/10.26599/OSHM.2025.9610028]
- 71. Circadian Rhythm Disruptions and Cardiovascular Disease Risk [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384635/]
- 72. Circadian disruption, clock genes, and metabolic health [https://www.jci.org/articles/view/170998]
- 73. Circadian Disruption and the Risk of Developing Obesity [https://link.springer.com/article/10.1007/s13679-025-00610-6]
- 74. Circadian rhythms in cardiovascular (dys)function [https://www.nature.com/articles/s44325-024-00024-8]
- 75. Metabolic syndrome: epidemiology, mechanisms, and ... [https://pubmed.ncbi.nlm.nih.gov/40969606/]
- 76. Study finds disruptions to circadian rhythm increase risk of ... [https://www.aha.org/news/headline/2025-10-28-study-finds-disruptions-circadian-rhythm-increase-risk-heart-disease-other-conditions]
- 77. The Role of the Biological Clock in Depression and Bipolar ... [https://www.sciencedirect.com/science/article/pii/S0006322325011898]
- 78. Translational implications of circadian activity alterations in an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12457307/]
- 79. Sleep disorders and the risk of cognitive decline or dementia [https://link.springer.com/article/10.1007/s00415-025-13372-x]
- 80. A meta-analysis study evaluating the effects of sleep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12400548/]
- 81. The Chronobiology of Hormone Administration [https://www.endocrine.org/journals/endocrine-reviews/chronobiology-of-hormone-administration]
- 82. Effects of light on human circadian rhythms, sleep and mood [https://pmc.ncbi.nlm.nih.gov/articles/PMC6751071/]
- 83. Keeping an eye on circadian time in clinical research and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9790849/]
- 84. Time-restricted feeding regulates molecular mechanisms ... [https://www.sciencedirect.com/science/article/abs/pii/S0899900721001064]
- 85. Fasting, circadian rhythms, and time restricted feeding in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5388543/]
- 86. per-protocol analysis of a 3-month randomized clinical trial [https://pmc.ncbi.nlm.nih.gov/articles/PMC12309031/]
- 87. Intermittent energy restriction may improve outcomes in ... [https://www.endocrine.org/news-and-advocacy/news-room/endo-annual-meeting/endo-2025-press-releases/zhang-press-release]
- 88. Human circadian rhythm studies: Practical guidelines for ... [https://www.sciencedirect.com/science/article/pii/S2451994422000062]
- 89. Effect of Light Treatment on Sleep and Circadian Rhythms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2764401/]
- 90. Bright Light Therapy [https://stanfordhealthcare.org/medical-conditions/sleep/advanced-sleep-phase-syndrome/treatments/bright-light-therapy.html]
- 91. Nuclear receptor protein: REV-ERB - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12051005/]
- 92. Regulating the Clock : REV - ERB as Promising Therapeutic... Agonists [https://pmc.ncbi.nlm.nih.gov/articles/PMC10623616/]
- 93. REV-ERB activation as a novel pharmacological approach ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1171931/full]
- 94. Rev-Erbα: A Chronobiological Approach to Inflammation ... [https://ijopp.org/10.5530/ijopp.20250293]
- 95. of the mammalian Pharmacological regulates sleep... targeting clock [https://www.nature.com/articles/ncomms6759?error=cookies_not_supported&code=1cdd968e-a8c5-4752-b081-503e9327a18c]
- 96. Structure-based design and classifications of small ... [https://www.nature.com/articles/s41598-021-97962-5]
- 97. Physiology, Circadian Rhythm - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK519507/]
- 98. Methods for Assessment of Sleep and Circadian Rhythms in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540570/]
- 99. The circadian clock uses different environmental time cues ... [https://www.nature.com/articles/s41598-019-54111-3]
- 100. Preventive circadian medicine: improving health with sleep ... [https://www.nature.com/articles/s44323-025-00047-z]
- 101. Optimize Sleep: Decoding Your Circadian Rhythm (2025) [https://agurgentcare.com/decoding-sleep-cycle-circadian-rhythm-optimal-sleep/]
- 102. "Circadian rhythms and health: Chronobiological strategies ... [https://pubmed.ncbi.nlm.nih.gov/40393257/]
- 103. Environmental chemicals affect circadian rhythms [https://www.sciencedirect.com/science/article/pii/S0160412020321140]
- 104. Sleep hygiene: Simple practices for better rest [https://www.health.harvard.edu/staying-healthy/sleep-hygiene-simple-practices-for-better-rest]
- 105. Mini review: Bidirectional Regulation of Circadian Rhythm ... [https://pubmed.ncbi.nlm.nih.gov/40225034/]
- 106. the Hygia Chronotherapy Trial [https://pubmed.ncbi.nlm.nih.gov/31641769/]
- 107. Chronotherapy as a novel strategy to limit anthracycline ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638736/]
- 108. 10. Synthesis: visualisations [https://systematicreviewmethods.github.io/synthesis1.html]
- 109. Chronobiology in the endocrine system [https://www.sciencedirect.com/science/article/abs/pii/S0169409X07001123]
- 110. Circadian Clock Deregulation and Metabolic Reprogramming [https://pubmed.ncbi.nlm.nih.gov/40650041/]
- 111. Circadian rhythms revealed: unraveling the genetic, ... [https://www.frontiersin.org/journals/sleep/articles/10.3389/frsle.2025.1544945/full]
- 112. Organ-specific proteomic aging clocks predict disease and ... [https://www.nature.com/articles/s43587-025-01016-8]
- 113. Circadian Regulation in Diurnal Mammals: Neural ... [https://www.mdpi.com/2079-7737/13/12/958]
- 114. Circadian Regulation in Diurnal Mammals: Neural Mechanisms and Implications in Translational Research - PubMed [https://pubmed.ncbi.nlm.nih.gov/39765625/]
- 115. Molecular components of the mammalian circadian clock - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3762864/]
- 116. The Impact of Circadian Rhythms on Medication Timing and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11586979/]
- 117. Circadian clock genes and insomnia: molecular mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12548078/]
- 118. Circadian regulation of gonadotropin-releasing hormone neurons and the preovulatory surge in luteinizing hormone in the diurnal rodent, Arvicanthis niloticus, and in a nocturnal rodent, Rattus norvegicus - PubMed [https://pubmed.ncbi.nlm.nih.gov/14668212/]
- 119. Circadian Clock–Controlled Drug Metabolism: Implications ... [https://www.sciencedirect.com/science/article/abs/pii/S0090955624079777]
- 120. Mathematical analysis of robustness of oscillations in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8979472/]
- 121. Circadian rhythms in metabolism and mental health [https://www.sciencedirect.com/science/article/pii/S2468867325000240]
- 122. Robustness from flexibility in the fungal circadian clock [https://pmc.ncbi.nlm.nih.gov/articles/PMC2913929/]
- 123. Regulation of therapeutic protein release in response to circadian ... [https://www.nature.com/articles/s41467-025-64761-9?error=cookies_not_supported&code=1932a0fc-d68b-44b5-b010-193853926afe]
- 124. in haematological malignancies: Circadian ... rhythms therapeutic [https://pubmed.ncbi.nlm.nih.gov/39566400/]
- 125. Novel Approaches for Assessing Circadian Rhythmicity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7543025/]
- 126. Validation of Circadian Biomarkers in Patients With Sleep ... [https://www.centerwatch.com/clinical-trials/listings/NCT04690504/validation-of-circadian-biomarkers-in-patients-with-sleep-disorders]
- 127. Frontiers | Exploring the association between circadian and... rhythms [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1614221/full]
- 128. Identifying novel circadian rhythm biomarkers for diagnosis ... [https://www.aging-us.com/article/205961/text]
- 129. Detection and Analysis of Circadian Biomarkers for Metabolic ... [https://medinform.jmir.org/2025/1/e69328]
- 130. Nanomaterial-enabled drug delivery systems for circadian medicine... [https://pubs.rsc.org/en/content/articlelanding/2025/ra/d5ra04137f]