Controlling Methodologic Variance in Endocrine Research: A Comprehensive Guide to Accurate Hormone Measurement
This article provides a systematic framework for researchers and drug development professionals to manage the biologic and procedural-analytic factors that introduce variance into endocrine measurements.
Controlling Methodologic Variance in Endocrine Research: A Comprehensive Guide to Accurate Hormone Measurement
Abstract
This article provides a systematic framework for researchers and drug development professionals to manage the biologic and procedural-analytic factors that introduce variance into endocrine measurements. Covering foundational concepts from participant selection to pre-analytical protocols, it details methodological applications for standardization, troubleshooting strategies for common pitfalls like circadian rhythms and endocrine disruptors, and validation techniques for emerging technologies. By synthesizing current guidelines and recent research, this guide aims to enhance the validity, reliability, and interpretability of endocrine data in both basic and clinical research settings.
Understanding the Core Biologic and Procedural Sources of Endocrine Variance
Accurate endocrine research requires rigorous control over non-methodologic biologic factors that introduce variance in hormonal measurements. Sex, age, and circadian rhythms represent three fundamental biologic variables that systematically influence endocrine parameters independently of experimental manipulations. These factors affect virtually all endocrine systems from basal hormone levels to dynamic responses to challenges. Research that fails to adequately control, measure, or account for these factors risks generating confounded results with limited validity and reproducibility. This document provides application notes and experimental protocols for investigating and controlling these key biologic factors within endocrine research paradigms, with particular emphasis on their implications for drug development and translational science.
Quantitative Data Synthesis
Table 1: Global Burden of Endocrine, Metabolic, Blood, and Immune Disorders (EMBID) by Sex and Age
| Parameter | Overall Global Burden (2021) | Sex Differences | Age Differences |
|---|---|---|---|
| Incidence | 79.47 million (95% UI: 63.34-98.63 million) [1] | Higher in females [1] | Highest in ≥70 years age group [1] |
| Prevalence | 475.78 million (95% UI: 381.23-591.19 million) [1] | Higher in females [1] | Highest in ≥70 years age group [1] |
| Mortality | 175,902 deaths (95% UI: 154,306-190,755) [1] | Higher in males [1] | Highest in ≥70 years age group [1] |
| DALYs | 12.86 million (95% UI: 9.94-16.98 million) [1] | Not specified | Highest in ≥70 years age group [1] |
| Age-Standardized Incidence Rate | 957.58 per 100,000 (95% UI: 766.99-1,183.95) [1] | Not specified | Not specified |
Table 2: Methodologic Considerations for Biologic Factors in Endocrine Research
| Factor | Key Considerations | Impact on Endocrine Measurements |
|---|---|---|
| Sex | Differences manifest at puberty; distinct hormonal profiles in males vs. females; sex-specific exercise responses [2] | Increased androgen production in males; pulsatile gonadotrophin/sex steroid release in females; differential growth hormone responses [2] |
| Age | Prepubertal vs. postpubertal differences; menopausal/andropausal changes; decreased growth hormone/testosterone with aging [2] | Increased insulin resistance during puberty; altered hormonal responses to exercise and training; increased cortisol with age [2] |
| Circadian Rhythms | Endogenous ~24-hour cycles; affects hormone secretion and sensitivity; differs between sexes [3] [2] | Fluctuating hormonal levels throughout day/night cycle; circadian variation in drug responses; sex differences in circadian parameters [3] [2] |
| Menstrual Cycle | Phases (follicular, ovulation, luteal) with dramatic hormone fluctuations; oral contraceptive effects [2] | 2-to 10-fold hormone increases in ovulatory/luteal phases; influences non-reproductive hormone responses [2] |
Table 3: Circadian Cardiac Autonomic Function by Sex and Age
| Parameter | Sex Differences | Aging Effects |
|---|---|---|
| Heart Rate Variability (HRV) | Women exhibit higher vagal oscillatory activity [4] | Diminished fluctuations across all parameters [4] |
| Parasympathetic Activity | Increased oscillatory activity in females [4] | Reduced vagal influence [4] |
| Circadian Rhythmicity | Differential entrainment of melatonin, temperature, and heart rate [4] | Chronodisruption of cardiac autonomic markers [4] |
| System Complexity | Not specified | Reduced complexity and adaptability [4] |
Experimental Protocols
Protocol 1: Controlling for Sex Differences in Endocrine Studies
Background: Sexual dimorphism affects endocrine systems through chromosomal, hormonal, and organizational differences that persist throughout the lifespan. Each cell contains sex chromosomes that influence function independently of reproductive processes, creating fundamental biological differences in endocrine systems [3].
Materials:
- Animal subjects or human participants of both sexes
- Appropriate hormonal assay platforms (ELISA, RIA, MS)
- Data collection forms for sex-specific variables
Procedure:
- Stratified Recruitment: Intentionally recruit both male and female participants in approximately equal numbers. For animal studies, include both sexes in experimental designs.
- Documentation Stage: Record biological sex at enrollment. For human studies, additionally document gender identity where relevant to study objectives.
- Hormonal Status Assessment: In post-pubertal subjects, establish baseline sex hormone status (testosterone, estradiol, progesterone) prior to experimental interventions.
- Data Collection: Collect all endocrine measurements using consistent methodologies across both sexes.
- Statistical Analysis: Analyze data with sex as a biological variable, using appropriate statistical models to test for main effects of sex and sex-by-treatment interactions.
Interpretation: Significant main effects of sex indicate different absolute hormone levels between males and females. Significant interactions indicate that experimental manipulations affect endocrine parameters differently in each sex. Both outcomes have important implications for basic science and drug development.
Protocol 2: Accounting for Age-Related Endocrine Changes
Background: Aging systematically alters endocrine function through multiple mechanisms including changes in hormone production, receptor sensitivity, and feedback regulation. These changes create distinct endocrine environments across the lifespan that must be considered in research design [2].
Materials:
- Age-appropriate recruitment strategies
- Age-specific reference ranges for hormonal parameters
- Adjustment protocols for age-related comorbidities
Procedure:
- A Priori Age Group Definition: Define specific age categories relevant to the research question (e.g., pre-pubertal, reproductive age, post-menopausal/andropausal, advanced age).
- Stratified Enrollment: Recruit participants within specified age ranges or intentionally across the lifespan as dictated by study objectives.
- Maturation Documentation: For pediatric populations, document Tanner stage or other maturation indices beyond chronological age.
- Age-Matching: For case-control studies, implement rigorous age-matching between groups (±3-5 years for adults).
- Statistical Control: In analyses of continuously distributed age, include age as a covariate in statistical models to adjust for its effects.
Interpretation: Age-related differences in endocrine parameters may reflect normal developmental changes or pathological alterations. Reference to established age-specific normative ranges is essential for proper interpretation. In intervention studies, age may modify treatment effects, necessitating stratified analyses.
Protocol 3: Circadian Rhythm Monitoring in Endocrine Research
Background: The circadian timing system regulates endocrine function through central neural clocks in the suprachiasmatic nucleus (SCN) and peripheral clocks in endocrine tissues. These systems create predictable 24-hour oscillations in hormone secretion and sensitivity that must be controlled in research designs [3].
Materials:
- Time-stamped sample collection systems
- Diary tools for sleep/wake cycle documentation
- Appropriate sample storage facilities for batch analysis
Procedure:
- Timing Standardization: Fix the timing of all experimental procedures and sample collections relative to each participant's wake time or to a standardized clock time.
- Sleep/Wake Documentation: Record sleep onset, wake time, and sleep quality for at least 72 hours prior to testing.
- Multiple Sampling: For comprehensive circadian assessment, collect serial samples across the 24-hour cycle (e.g., every 2-4 hours).
- Constant Routine Protocol: For precise circadian assessment, implement constant routine conditions with controlled posture, wakefulness, light exposure, and nutrient intake.
- Time-Stamped Analysis: Process and analyze all samples with documentation of collection time.
Interpretation: Circadian rhythms affect both baseline hormone levels and responses to interventions. Time-of-day effects can be as large as experimental effects. Proper control requires either testing all participants at the same circadian time or intentionally mapping responses across the circadian cycle.
Protocol 4: 24-Hour Heart Rate Variability (HRV) Monitoring for Autonomic Circadian Assessment
Background: Cardiac autonomic function exhibits robust circadian rhythmicity regulated by both central and peripheral clocks. HRV parameters provide non-invasive indicators of autonomic balance that fluctuate predictably across the 24-hour cycle and are differentially affected by sex and age [4].
Materials:
- Digital Holter recorder (e.g., SpaceLab-Burdick) [4]
- Three leads with pseudoorthogonal configuration (X, Y, Z) [4]
- Kubios HRV Scientific software or equivalent [4]
- Artifact identification and correction tools
Procedure:
- Participant Preparation: Apply Holter monitor with three leads in pseudoorthogonal configuration after 20 minutes of supine rest [4].
- Data Collection: Conduct 24-hour ambulatory monitoring during normal daily activities with sampling frequency ≥200 Hz [4].
- Data Preprocessing: Identify RR intervals and select artifact-free 5-minute windows per hour using threshold-based beat correction (<5% correction acceptable) [4].
- Stationarity Assessment: Apply smoothness prior detrending method; retain only stationary segments based on respiratory rate estimation [4].
- Analysis Domains:
- Time Domain: Calculate SDNN, SDANN, RMSSD, pNN50 [4]
- Frequency Domain: Apply fast Fourier transformation with 5-minute Blackman-Harris windows; integrate power spectral density in VLF, LF, and HF bands [4]
- Nonlinear Parameters: Analyze fractal and multifractal properties, Poincare plot parameters [4]
- Circadian Analysis: Calculate MESOR, amplitude, and acrophase for each parameter across the 24-hour cycle [4].
Interpretation: Healthy adults typically show increased parasympathetic activity (higher HF, RMSSD, pNN50) during nighttime. Women exhibit higher vagal oscillatory activity than men. Aging diminishes circadian fluctuations and reduces overall HRV complexity. Chronodisruption manifests as altered amplitude, phase, or periodicity of rhythms.
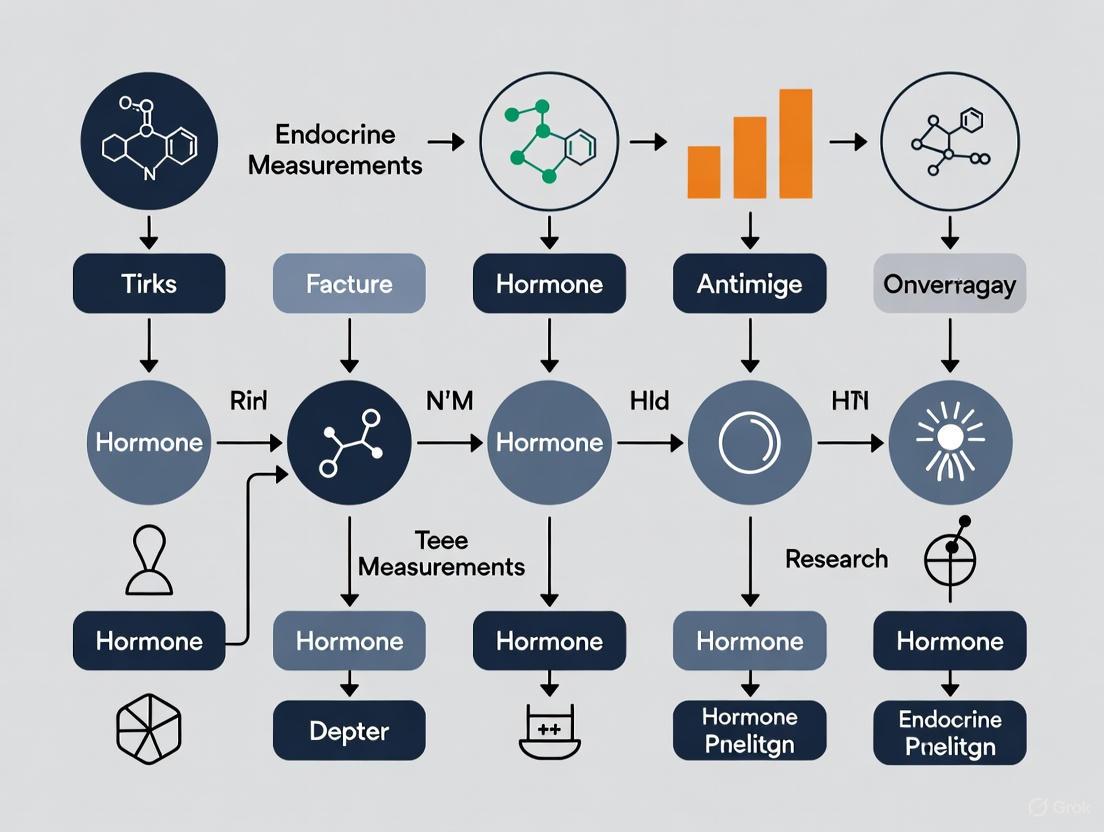
Signaling Pathways and Experimental Workflows
Diagram 1: Neuroendocrine underpinnings of sex differences and circadian regulation
Diagram 2: Endocrine research workflow integrating biologic factor controls
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for Investigating Biologic Factors in Endocrinology
| Item | Function/Application | Specific Examples/Considerations |
|---|---|---|
| Digital Holter Recorder | 24-hour ambulatory monitoring of cardiac autonomic function [4] | SpaceLab-Burdick digital Holter recorder with pseudoorthogonal lead configuration (X, Y, Z); 200 Hz sampling frequency [4] |
| HRV Analysis Software | Analysis of time-domain, frequency-domain, and nonlinear heart rate variability parameters [4] | Kubios HRV Scientific software (v.4.2.0+) with artifact correction, fast Fourier transformation, and nonlinear parameter calculation capabilities [4] |
| Hormonal Assay Platforms | Quantification of endocrine parameters from biological samples | ELISA, RIA, LC-MS/MS platforms validated for specific hormones with appropriate sensitivity ranges for expected concentrations |
| Standardized Data Repositories | Access to large datasets for examining population-level patterns | Korean NHID, Global Health Data Exchange (GHDx), CDC Data & Statistics, NHANES, ClinicalTrials.gov [5] [1] [6] |
| Common Data Elements (CDE) | Standardized data collection across studies | NIH Common Data Elements Repository for endocrine research variables and outcomes [5] |
| REDCap (Research Electronic Data Capture) | Web-based data management for clinical endocrine research | Customizable databases for capturing sex, age, circadian timing, and endocrine parameters with export capabilities for statistical analysis [5] |
The Impact of Body Composition and Adiposity on Hormone Levels
The recognition of adipose tissue as a dynamic endocrine organ has fundamentally altered our understanding of how body composition influences physiological function. Adiposity—particularly its quantity and distribution—directly modulates the secretion and function of various hormones, creating complex endocrine interactions that impact metabolic health, inflammatory status, and disease risk. This relationship presents critical methodological considerations for researchers investigating endocrine parameters, as body composition represents a significant confounding variable that must be accounted for in study design and data interpretation. This document provides application notes and experimental protocols for investigating these relationships within a rigorous methodological framework, specifically contextualized for research on methodological factors influencing endocrine measurements.
Scientific Background and Key Concepts
Adipose Tissue as an Endocrine Organ
White adipose tissue (WAT) functions beyond passive energy storage, actively secreting bioactive molecules known as adipokines that regulate essential metabolic processes including glucose homeostasis, lipid metabolism, energy balance, and immune responses [7]. The dysregulation of these adipokines in states of excess adiposity forms a core mechanism linking body composition to endocrine dysfunction [7] [8].
Critical Body Composition Indices
While Body Mass Index (BMI) provides a general anthropometric classification, it fails to distinguish between fat and muscle mass, leading to misclassification of metabolic health status [9]. More precise indices are essential for endocrine research:
- Body Fat Percentage (PBF): A more accurate indicator of metabolic risk than BMI; a cut-off point of 35.78% has been established for identifying increased cardiometabolic risk in young women with normal BMI (a condition termed Normal Weight Obesity, NWO) [9].
- Android-to-Gynoid (A/G) Fat Ratio: A significant predictor of cardiometabolic risk, correlating positively with insulin resistance and negatively with HDL-C levels [9].
- Visceral Adipose Tissue (VAT): Though not directly measured in all studies, VAT is highly metabolically active and strongly associated with adverse endocrine profiles.
Table 1: Key Adipokines and Their Metabolic Roles
| Adipokine | Primary Secretion Source | Function | Dysregulation in Obesity | Clinical Implications |
|---|---|---|---|---|
| Leptin | White Adipose Tissue | Regulates appetite, energy expenditure, and satiety [7] | Elevated levels with leptin resistance [7] [10] | Contributes to weight gain and metabolic dysregulation [7] |
| Adiponectin | White Adipose Tissue | Enhances insulin sensitivity, anti-inflammatory [7] [11] | Reduced levels [7] [11] | Increased risk of T2DM and cardiovascular disease [7] [11] |
| Resistin | Macrophages in adipose tissue [7] | Promotes insulin resistance and inflammation [7] | Increased levels [7] | Associated with chronic inflammation and reduced insulin sensitivity [7] |
| Lipocalin-2 (LCN-2) | Adipocytes, Neutrophils | Involved in inflammation, glucose homeostasis, insulin sensitivity [8] | Elevated levels in obesity [8] | Positively correlates with resistin and adiponectin in obesity; potential biomarker for metabolic dysregulation [8] |
Methodological Considerations for Endocrine Research
Investigating adiposity-hormone relationships requires strict control of confounding variables to ensure valid and reproducible results. The following factors must be considered in study design.
Biological Factors Influencing Measurements
Multiple participant-related factors introduce variance in endocrine outcomes and must be either controlled or documented [2]:
- Sex and Sex Hormones: Post-puberty, significant differences exist in resting hormonal profiles between males and females, particularly in leptin levels and sex steroid hormones [2]. Females show characteristic menstrual cycle variations in gonadotrophin and sex steroid hormones that influence other hormonal responses [2].
- Age and Life Stage: Prepubertal and postpubertal individuals display different hormonal responses [2]. Similarly, postmenopausal women and andropausal men show altered hormonal profiles compared to their premenopausal counterparts [2].
- Body Composition: Varying levels of adiposity significantly influence cytokines and hormones; resting insulin and leptin levels are typically elevated in obesity [2]. The hormonal response to exercise differs between normal-weight and obese individuals [2].
- Circadian Rhythms: Many hormones exhibit significant fluctuations throughout the day, necessitating standardized timing for specimen collection [2].
Table 2: Methodological Factors Affecting Endocrine Measurements
| Factor Category | Specific Considerations | Recommended Controls |
|---|---|---|
| Participant Biological Factors | Sex, age, race, body composition, mental health, menstrual status, circadian rhythms [2] | Match participants by sex, age, adiposity; control for menstrual cycle phase; standardize testing time |
| Procedural-Analytic Factors | Blood collection timing, processing methods, assay variability, sample storage conditions [2] | Standardize collection procedures; fasted morning sampling; uniform processing protocols; validated assays |
| Body Composition Assessment | BMI limitations, fat distribution patterns, lean mass contribution [9] | Use DXA or other precise methods; report PBF and fat distribution indices; avoid relying solely on BMI |
Experimental Protocols
Protocol 1: Comprehensive Body Composition and Endocrine Profiling
Objective: To assess relationships between detailed body composition parameters and circulating hormone levels in adults.
Materials:
- Dual-energy X-ray absorptiometry (DXA) scanner [9] [12]
- Phlebotomy supplies (vacutainer tubes, including EDTA for plasma and clot activator for serum) [9]
- Centrifuge capable of 3000 rpm at 4°C [9]
- -80°C freezer for sample storage [9]
- Validated hormone assay kits (e.g., for leptin, adiponectin, insulin, etc.) [8]
Procedure:
- Participant Preparation: Participants should fast overnight (10-12 hours), abstain from strenuous exercise for 24 hours, and avoid alcohol and caffeine for 12 hours prior to testing [9].
- Blood Collection: Between 6:00-8:00 a.m. after 10 minutes of seated rest, collect ~15mL venous blood [9]. Process within 30 minutes of collection.
- Sample Processing: Centrifuge at 3000 rpm for 15 minutes at 4°C [9]. Aliquot plasma/serum and store at -70°C until analysis [9].
- Body Composition Assessment: Perform DXA scan to determine total body fat percentage, android-to-gynoid ratio, and lean mass [9] [12].
- Hormonal Analysis: Use validated immunoassays according to manufacturer protocols for target hormones. Include appropriate controls and standards.
- Data Analysis: Correlate body composition indices with hormone levels using appropriate statistical methods (e.g., Pearson/Spearman correlations, multiple regression adjusting for potential confounders).
Protocol 2: Intervention Study on Exercise-Induced Changes
Objective: To evaluate the effects of structured exercise on adipokine profiles in relation to body composition changes.
Materials:
- DXA or other body composition tool [12] [13]
- Exercise equipment appropriate for intervention
- Phlebotomy and sample processing supplies [9]
- Validated adipokine assay kits [11] [13]
Procedure:
- Baseline Assessment: Perform body composition analysis and fasted blood collection as in Protocol 1.
- Exercise Intervention: Implement a structured program (e.g., 16 weeks of combined aerobic and resistance exercise, 3-5 sessions/week) [13]. The systematic review by [11] suggests effective doses of approximately 800-1300 MET-min/week.
- Post-Intervention Assessment: Repeat body composition and blood collection 48-72 hours after the final exercise session to avoid acute effects.
- Sample Analysis: Measure leptin, adiponectin, and other target hormones using standardized assays.
- Data Analysis: Compare pre-post changes using paired t-tests or Wilcoxon tests; analyze correlations between body composition changes and hormonal changes.
Data Presentation Standards
Quantitative Data Tables
Table 3: Body Composition and Adipokine Response to Exercise Interventions (Sample Data)
| Parameter | Pre-Intervention Mean ± SD | Post-Intervention Mean ± SD | % Change | P-value |
|---|---|---|---|---|
| Body Fat Percentage | 37.61 ± 3.2% [13] | 29.16 ± 2.8% [13] | -22.5% | <0.001 |
| Leptin (ng/mL) | 14.05 ± 2.1 [13] | 11.06 ± 1.8 [13] | -21.3% | <0.001 |
| Adiponectin (μg/mL) | 5.2 ± 1.1 [11] | 6.8 ± 1.3 [11] | +30.8% | <0.01 |
| C-peptide (ng/mL) | 4.58 ± 0.7 [13] | 2.96 ± 0.5 [13] | -35.4% | <0.001 |
| IGF-1 (ng/mL) | 224.74 ± 25 [13] | 272.89 ± 28 [13] | +21.4% | <0.001 |
Table 4: Optimal Exercise Dosages for Adipokine Improvement (from Network Meta-Analysis)
| Exercise Modality | Effect on Adiponectin (SMD) | Effect on Leptin (SMD) | Optimal Weekly Dose (MET-min/week) |
|---|---|---|---|
| HIIT | ++ (0.85) [11] | - (-0.45) [11] | 800-1000 |
| Combined Exercise | + (0.62) [11] | ++ (-0.99) [11] | 900-1100 |
| Aerobic Exercise | + (0.58) [11] | + (-0.75) [11] | 800-1000 |
| Resistance Training | + (0.65) [11] | NS [11] | 1000-1300 |
SMD = Standardized Mean Difference; HIIT = High-Intensity Interval Training; NS = Not Significant
Signaling Pathways and Metabolic Relationships
Figure 1: Adiposity-Endocrine Pathway Mapping
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Materials for Body Composition-Endocrine Research
| Item | Specification/Example | Research Application |
|---|---|---|
| DXA Scanner | GE HealthCare Lunar iDXA or equivalent [12] | Gold-standard body composition assessment; provides regional fat distribution analysis [9] [12] |
| Blood Collection System | Vacutainer system with EDTA tubes (plasma) and serum separator tubes [9] | Standardized blood sample acquisition for hormone analysis |
| Low-Temperature Freezer | -70°C to -80°C capacity (e.g., Eppendorf CryoCube F570) [9] | Preservation of hormone integrity in stored samples |
| Centrifuge | Refrigerated centrifuge capable of 3000 rpm (e.g., MPW-260R) [9] | Proper processing of blood samples for plasma/serum separation |
| Adipokine Assay Kits | Validated ELISA kits for leptin, adiponectin, resistin | Quantification of specific adipokine levels in serum/plasma |
| Hormone Analysis Platform | Multiplex immunoassay systems (e.g., Luminex) or standard ELISA readers | Simultaneous measurement of multiple hormones with efficiency |
| Physical Activity Monitoring | Objective accelerometry (e.g., SenseWear Armband) [12] | Quantification of physical activity levels and energy expenditure |
The intricate relationship between body composition and hormone levels represents a critical area of investigation with significant implications for metabolic health and chronic disease risk. Methodologically rigorous research in this field requires precise body composition assessment beyond BMI, controlled experimental conditions that account for biological variability, and standardized protocols for endocrine measurement. The application notes and protocols provided herein offer a framework for generating reliable, reproducible data that advances our understanding of how adiposity influences endocrine function, ultimately contributing to improved strategies for preventing and treating obesity-related metabolic disorders.
Mental Health and Menstrual Cycle Status as Confounding Variables
In endocrine research, accurate measurement of hormone levels is paramount. However, unaccounted-for confounding variables can significantly distort these measurements, leading to erroneous conclusions. Mental health status and phase of the menstrual cycle represent two potent, frequently overlooked confounding factors. Confounding occurs when an extraneous variable systematically differs between study groups and independently influences the outcome of interest [14]. In studies of medical interventions, this often arises from the complex factors influencing physician treatment decisions and patient medication use, which are also independent determinants of health outcomes [14]. Failure to adequately control for mental health and menstrual cycle status can introduce bias, obscuring true causal relationships in endocrine and pharmacodynamic studies. This document outlines standardized protocols to identify, measure, and control for these critical confounders.
Quantitative Evidence of Association
The following tables summarize key empirical findings demonstrating the associations between menstrual cycle phases, mental health, and physiological parameters, underscoring their potential as confounders.
Table 1: Summary of Key Studies on Menstrual Cycle, Mental Health, and Physiological Correlates
| Study Focus | Study Design & Population | Key Findings | Implications for Endocrine Research |
|---|---|---|---|
| Premenstrual Exacerbation (PME) of Mood Symptoms [15] | Cohort study (N=352 women with depression); Ecological Momentary Assessment (EMA). | - Gradual decline in mood beginning 14 days pre-menstruation until 3 days before next period (β=0.0004, p<0.001). - Lowest mood ratings from 3 days before until 2 days after menstruation onset. - Mood was significantly associated with Heart Rate Variability (HRV) on the same day (β=-0.0022, p=0.005). | Endocrine measurements during the luteal phase may be confounded by cyclical mood deterioration and associated autonomic nervous system changes (HRV). |
| Menstrual Health and Mental Health Problems [16] | Longitudinal analysis (N=2,829 Ugandan adolescents); Mixed-effects linear regression. | Multiple dimensions of poor menstrual health were associated with subsequent mental health problems: - Lack of social support: aMD=0.74 (95% CI 0.26–1.21) - Lower self-efficacy: aMD=0.60 (95% CI 0.15–1.05) - Unmet practice needs: aMD=1.11 (95% CI 0.61–1.60) | Psychosocial stressors related to menstruation are independent risk factors for poor mental health, which can act as a confounder. |
| Predicting PMS with Anxiety and Depression [17] | Cross-sectional study (N=624 female students); Ordinal Logistic Regression (OLR). | - Depression and anxiety were significant predictors of PMS severity. - For each increase in depression severity, odds of more severe PMS increased by 41% (OR=1.41, 95% CI [1.21, 1.65]). - For anxiety, the odds increased by 51% (OR=1.51, 95% CI [1.29, 1.76]). | The strong, bidirectional relationship between mental health and premenstrual symptoms necessitates concurrent assessment of both. |
Table 2: Common Types of Confounding Biases in Observational Research [14]
| Type of Bias | Description | Example in Endocrine Research |
|---|---|---|
| Confounding by Indication/Severity | Treatment is prescribed based on disease severity or prognosis, which itself influences the outcome. | A drug may appear less effective because it is prescribed to patients with more severe, treatment-resistant hormonal imbalances. |
| Confounding by Functional Status | Patients with impaired physical or cognitive function have different exposure and outcome patterns. | Functionally impaired patients may have worse endocrine outcomes due to stress and poor care access, not the treatment under study. |
| Healthy User/Adherer Bias | Patients who initiate or adhere to preventive medications engage in other health-promoting behaviors. | Patients who adhere to a study drug may also have lifestyles that positively impact endocrine function, inflating the drug's apparent benefit. |
Detailed Experimental Protocols
Protocol for Tracking Menstrual Cycle and Related Symptoms
This protocol utilizes Ecological Momentary Assessment (EMA) to minimize recall bias and capture real-time fluctuations [15].
Aim: To accurately determine the menstrual cycle phase at the time of endocrine sampling and quantify premenstrual symptomatology.
Materials:
- Mobile health platform or EMA-compatible smartphone application.
- Validated symptom tracking questionnaire (e.g., Premenstrual Symptoms Screening Tool, PSST) [17].
Methodology:
- Participant Enrollment: Recruit participants with confirmed regular menstrual cycles (21-35 days). Record baseline characteristics.
- Cycle Tracking: Participants track their menstrual cycles for a minimum of two consecutive cycles [15]. The first day of menstruation is designated as cycle day 1.
- Symptom Assessment: Participants receive daily push notifications to record:
- Mood and Energy: Using a digital circumplex model or 7-point Likert scale [15].
- Physical Symptoms: Based on PSST or similar criteria.
- Cycle Phase Alignment: Retrospectively align cycles using the luteal phase (consistently ~14 days post-ovulation). Define key phases:
- Data Integration: Synchronize symptom data with cycle phase for each participant at the time of biological sampling.
Protocol for Assessing Mental Health Status
Aim: To screen for and quantify symptoms of depression and anxiety that may confound endocrine measurements.
Materials:
- Patient Health Questionnaire (PHQ-8 or PHQ-9) [15].
- Depression, Anxiety, and Stress Scales (DASS-42) or similar validated instrument [17].
Methodology:
- Baseline Screening: Administer the PHQ-8 and a anxiety scale (e.g., GAD-7 or DASS-anxiety subscale) during study enrollment. A PHQ-8 score ≥10 indicates a high likelihood of major depressive disorder [15].
- Longitudinal Monitoring: For studies extending beyond two weeks, readminister mental health scales every two weeks to capture fluctuations [15].
- Statistical Control: In analysis, include mental health scores as continuous covariates or use cutoff scores to stratify the study population.
Protocol for Measuring Heart Rate Variability (HRV)
HRV serves as an objective, physiological correlate of autonomic nervous system function, which is linked to both mental state and menstrual cycle [15].
Aim: To obtain a standardized measure of HRV as a potential biomarker for the physiological stress state.
Materials:
- FDA-cleared or CE-marked smart device or HRV monitor capable of measuring inter-beat intervals (e.g., chest strap monitor, smartwatch).
- Standardized operating procedure for measurement.
Methodology:
- Standardization: Measure HRV upon waking, in a sitting position, after a 5-minute rest period to control for diurnal variation and activity [15].
- Measurement: Record for a minimum of 5 minutes. Use the SD of the inter-beat intervals (SDNN) as the primary metric, as it reflects overall HRV and is less susceptible to measurement method differences [15].
- Frequency: Measure HRV on the same day as endocrine sampling and mental health assessments.
Experimental Workflow and Data Analysis
The following diagram illustrates the integrated workflow for controlling these confounding variables in a research study.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Confounder Control
| Item / Tool | Function / Rationale | Example / Specification |
|---|---|---|
| Ecological Momentary Assessment (EMA) Platform | Captures real-time data on mood, energy, and symptoms in the participant's natural environment, reducing recall bias. | Custom mobile apps (e.g., Juli platform [15]); Commercial survey tools (e.g., Ethica Data). |
| Validated Mental Health Questionnaires | Quantifies depression and anxiety symptoms for use as covariates or stratification variables in statistical models. | PHQ-8/9: For depression severity [15].DASS-42: For depression, anxiety, and stress [17]. |
| HRV Monitoring Device | Provides an objective, physiological measure of autonomic nervous system state, correlated with mood. | FDA-cleared smartwatches (e.g., Apple Watch, Fitbit); Medical-grade chest strap monitors (e.g., Polar H10). Report SDNN in milliseconds (ms) [15]. |
| Statistical Analysis Software with Ordinal Regression Capabilities | Fits sophisticated models to account for ordered categorical outcomes (e.g., PMS severity) and continuous confounders. | R (package MASS), Python (statsmodels), SAS (PROC LOGISTIC). Essential for implementing Ordinal Logistic Regression [17]. |
| Color-Accessible Data Visualization Tools | Ensures research findings are communicated clearly and accessibly to all audiences, including those with color vision deficiencies. | ColorBrewer 2.0: For selecting colorblind-safe palettes [18].APCA Contrast Calculator: To check contrast ratios per WCAG guidelines [18]. |
The validity of endocrine research is fundamentally dependent on the accuracy of hormone measurements. Methodologic errors can be broadly categorized as either biologic (originating from the physiologic status of the subject) or procedural-analytic (arising from specimen handling and laboratory analysis) [2]. A lack of control for these factors introduces significant variance, leading to inconsistent and contradictory research findings [2]. This document provides a detailed framework for identifying, controlling, and mitigating these error sources to enhance the scientific rigor of endocrine studies in both human and rodent models.
Biologic sources of error are endogenous factors related to the subject's physiologic status at the time of specimen collection. These factors introduce variance by altering true hormone concentrations prior to sampling.
Table 1: Common Biologic Sources of Error and Control Strategies
| Biologic Factor | Impact on Hormonal Measurements | Recommended Control Strategies |
|---|---|---|
| Circadian Rhythm | Pronounced diurnal variation in cortisol, ACTH, GH, prolactin, and TSH [19]. Testosterone peaks in the morning in men [19]. | Standardize blood sampling times, typically in the early morning for cortisol and ACTH [19]. Document time of sampling for interpretation [19]. |
| Sex & Menstrual Cycle | Post-puberty, males and females have distinct resting hormonal profiles [2]. In females, menstrual cycle phase dramatically affects estradiol, progesterone, LH, and FSH [2]. | Match participants by sex for studies where hormones are sex-influenced [2]. For female participants, document menstrual status and test in a specific cycle phase or match by phase [2]. |
| Age | Prepubertal and postpubertal individuals show different hormonal responses [2]. Growth hormone and testosterone decrease with age, while cortisol and insulin resistance increase [2]. | Match participants by chronologic age and maturation level, unless studying age-related changes [2]. |
| Body Composition | Adiposity influences cytokines (e.g., leptin, IL-6), which in turn affect metabolic and reproductive hormones [2]. Obesity can blunt or elevate exercise-induced hormonal responses [2]. | Match participants by adiposity (e.g., BMI categories) rather than body weight alone [2]. |
| Acute Stress & Illness | Physical and psychological stress elevates catecholamines, ACTH, cortisol, GH, and prolactin [19]. Acute illness is a significant stressor [19]. | Implement a quiet, standardized resting period (e.g., 30 minutes seated) prior to blood sampling [19]. Document health status and recent stressors. |
| Medication & Supplements | Various prescription drugs, over-the-counter medications, and illicit substances can suppress or stimulate hormone secretion (e.g., opioids suppress gonadotropins; steroids suppress ACTH) [19]. | Perform thorough documentation of all current medication, including topical and over-the-counter products [19]. |
Experimental Protocol: Standardizing Blood Collection for Circadian Hormones
Aim: To minimize pre-analytical variability from circadian rhythms in a study measuring cortisol.
- Participant Preparation: Instruct participants to maintain a regular sleep-wake cycle for 3 days prior to sampling. Avoid strenuous exercise, alcohol, and caffeine for 24 hours.
- Sampling Setup: The sampling environment should be quiet and relaxed.
- Rest Period: Upon arrival, the participant rests in a seated position for 30 minutes [19].
- Blood Draw: Precisely at 8:00 AM, collect the blood sample via venipuncture.
- Documentation: Record the exact time of blood collection and any deviations from the protocol.
Procedural-analytic errors are determined by the investigator and occur during specimen collection, processing, storage, and laboratory analysis. It is estimated that the pre-analytical phase accounts for up to 93% of total errors in the diagnostic process [20].
Table 2: Common Procedural-Analytic Sources of Error and Mitigation Strategies
| Procedural-Analytic Factor | Impact on Hormonal Measurements | Recommended Mitigation Strategies |
|---|---|---|
| Blood Sampling Site & Method | In rodents, sampling site (e.g., retrobulbar vs. tail vein) and anesthesia (e.g., isoflurane) can significantly alter measured concentrations of insulin and stress hormones [20]. | Maintain absolute consistency in sampling site and method within a single experiment [20]. Document the procedure in detail. |
| Sample Processing & Storage | Delay in processing, improper temperature during storage or transport, and repeated freeze-thaw cycles can degrade hormones and alter measurable concentrations [21]. | Centrifuge samples promptly after collection. Aliquot plasma/serum and freeze at -80°C. Avoid repeated freeze-thaw cycles. |
| Immunoassay Interference | Biotin: High doses (>5 mg/day) can cause dramatic interference in biotin-streptavidin based immunoassays, leading to falsely high or low results [22] [19].Heterophile Antibodies/HAMAs: Cause false elevation or suppression of results [23] [22].Hook Effect: In sandwich immunoassays, extremely high analyte concentrations (e.g., prolactin in macroprolactinoma) saturate antibodies, causing a falsely low result [23] [22].Macroprolactin: Falsely elevates prolactin levels due to accumulation of biologically inactive prolactin-IgG complexes [23] [22]. | Inquire about biotin supplementation and request a wash-out period [19]. For large tumors with discrepant lab values, request sample dilution to rule out the hook effect [23] [22]. Screen for macroprolactin via PEG precipitation [23]. |
| Assay Standardization | Different immunoassays for the same hormone (e.g., GH, cortisol) may use different antibodies, standards, and show poor harmonization, leading to method-specific results and reference ranges [24]. | Use the same laboratory and assay method for all samples within a study. Report the specific assay used and reference standards. |
| Sample Matrix | Hemolysis, icterus, and lipemia can interfere with various immunoassays, leading to over- or underestimation of analytes like ferritin, TSH, and Vitamin B12 [25]. | Inspect samples for hemolysis/lipemia. Use clear, non-hemolyzed samples for analysis. |
Experimental Protocol: Validating a Novel Immunoassay for Rodent Samples
Aim: To perform a basic validation of a commercial immunoassay for measuring a metabolic hormone in mouse plasma [20].
- Parallelism (Linearity) Test: Serially dilute a pooled mouse plasma sample with high analyte concentration with the assay's zero calibrator or recommended buffer. The diluted samples should produce a curve parallel to the standard curve. Non-parallelism indicates matrix interference.
- Spike-and-Recovery Test: Spike a known amount of the pure standard analyte into a pooled mouse plasma sample with a known baseline concentration. Calculate the percentage of the added analyte that is recovered. Recovery should typically be between 85-115%.
- Intra- and Inter-Assay Precision: Run multiple replicates of quality control samples (low, medium, high) within the same assay plate (intra-assay) and across different plates/days (inter-assay) to calculate the coefficient of variation (CV).
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Endocrine Research
| Item | Function/Application |
|---|---|
| EDTA or Heparin Tubes | Anticoagulants for plasma collection. The choice of tube must be validated for the specific analyte, as additives can interfere with some immunoassays [25]. |
| Serum Separator Tubes (SST) | For serum collection. Allows for easy separation of serum after clotting and centrifugation. |
| Protease Inhibitor Cocktails | Added to collection tubes to prevent proteolytic degradation of protein and peptide hormones during processing. |
| PEG (Polyethylene Glycol) | Used in the precipitation test to screen for macroprolactin, which helps distinguish true hyperprolactinemia from macroprolactinemia [23]. |
| International Hormone Standards | Certified reference materials (e.g., IS 98/574 for GH) that allow for harmonization and comparison of results across different laboratories and studies [24]. |
| Species-Specific Immunoassays | Immunoassays whose antibodies have been validated for the specific species under study (e.g., rat vs. human). Using non-validated assays is a major source of error [20]. |
Workflow and Relationship Diagrams
Endocrine Error Categorization
Pre-Analytical Phase Workflow
The Critical Role of Participant Screening and Homogeneity
In endocrine research, the validity of hormonal measurements is critically dependent on the rigorous control of methodologic factors. These factors can be broadly categorized as those affecting biologic variation, originating from the physiologic status of the participant, and those affecting procedural-analytic variation, determined by the investigators [2]. Inadequately controlled, these sources of variance produce research outcomes that are inconsistent, contradictory, and difficult to interpret, thereby compromising scientific quality [2]. Participant screening and homogeneity form the foundational strategy to minimize biologic variance, ensuring that the studied cohort is sufficiently uniform to allow for the detection of true physiologic signals against a background of inherent individual variability.
The free hormone hypothesis, a cornerstone of modern endocrinology, posits that a hormone's physiological effects are correlated with its free (non-protein-bound) concentration, not the total hormone concentration [26]. This principle underscores a significant challenge in endocrine measurements: hormones like thyroxine (T4) and testosterone are extensively bound to plasma proteins such as albumin and sex hormone-binding globulin (SHBG) [26]. Factors that alter the concentration or binding affinity of these proteins—including age, sex, and health status—can profoundly impact measured free hormone levels, even if the underlying endocrine physiology is unchanged. Consequently, failure to ensure participant homogeneity for these key biologic factors can lead to erroneous data interpretation.
Key Biologic Factors Influencing Endocrine Measurements
A comprehensive screening protocol must account for several intrinsic participant factors to establish a homogeneous research cohort. The following variables are paramount, as they are known to significantly influence hormonal profiles at rest and in response to interventions.
Sex and Menstrual Cycle Status
Until puberty, males and females exhibit minimal differences in resting hormonal profiles. Post-puberty, significant divergences emerge, with males demonstrating increased androgen production and females exhibiting the characteristic pulsatile release of gonadotrophin and sex steroid hormones [2]. The menstrual cycle phase (follicular, ovulation, or luteal) in eumenorrheic females produces large and dramatic basal changes in key reproductive hormones like estradiol-β-17 and progesterone, which can, in turn, influence non-reproductive hormones [2]. Research involving pre-menopausal females must, therefore, account for menstrual status and cycle phase during testing to avoid confounding results.
Age and Maturation Level
Hormonal responses are not uniform across the lifespan. Prepubertal and postpubertal children of the same sex do not typically display identical hormonal responses, a phenomenon illustrated by the well-documented increase in insulin resistance observed during puberty [2]. At the other end of the age spectrum, postmenopausal women and andropausal men exhibit drastically different hormonal responses (e.g., decreased growth hormone and testosterone) compared to their pre-pausal counterparts [2]. Participants should be matched by chronologic age or maturation level to increase response homogeneity.
Body Composition
Adipose tissue is an active endocrine organ that releases cytokines with autocrine, paracrine, and endocrine-like actions. Varying levels of adiposity can greatly influence hormones and cytokines such as leptin and interleukin-6 [2]. Furthermore, the hormonal response to exercise is often altered in obese individuals; for instance, the catecholamine and growth hormone response to exercise is reduced [2]. Matching participants for adiposity (e.g., by body mass index categories) rather than simply body weight is crucial for many study outcomes.
Additional Critical Factors
- Circadian Rhythms: Many hormones, such as cortisol, exhibit strong diurnal variations. Standardizing the time of day for specimen collection is essential for comparative analysis [2].
- Mental Health: Conditions like high anxiety or depression can lead to altered resting levels of circulating catecholamines, cortisol, and thyroid hormones, which may subsequently modify the hormonal response to an intervention [2].
- Race: Although less studied, certain hormonal differences exist across races (e.g., resting parathyroid hormone levels tend to be higher in Blacks than Whites) and should be considered in cohort design [2].
Table 1: Key Biologic Factors and Their Documented Impact on Endocrine Measurements
| Biologic Factor | Documented Impact on Hormonal Measures | Recommendation for Screening/Homogenization |
|---|---|---|
| Sex | Post-puberty, differences in androgen production (males) and menstrual cycle hormones (females) [2]. | Stratify groups by sex post-puberty. |
| Menstrual Cycle | Large fluctuations in estradiol-β-17, progesterone, LH, and FSH across phases [2]. | Test females in a similar phase or account for cycle phase in analysis. |
| Age & Maturation | Differing responses in prepubertal vs. postpubertal individuals; declining GH and testosterone with age [2]. | Match participants by chronologic age and maturation level. |
| Body Composition | Adiposity influences cytokines (leptin, IL-6) and hormones (insulin, cortisol) [2]. | Match for adiposity (e.g., BMI, body fat %) rather than body weight alone. |
| Circadian Rhythm | Diurnal variation in hormones like cortisol [2]. | Standardize time of day for specimen collection. |
| Mental Health | Altered resting levels of catecholamines and cortisol in anxiety/depression [2]. | Utilize mental health screening questionnaires. |
Principles and Protocols for Homogeneity Assessment
The principle of homogeneity—defined as the degree of uniformity distributed throughout a quantity of a material or solution—is not only applicable to patient cohorts but also to the reagents and formulations used in research [27]. In the context of pharmaceutical development, demonstrating dose formulation homogeneity is a regulatory requirement to ensure that the test system is being administered the appropriate amount of an active ingredient [28].
Experimental Protocol: Assessing Preclinical Dose Formulation Homogeneity
This protocol is adapted from standard practices in regulated preclinical safety studies [28].
1. Principle: Homogeneity is assessed by sampling a prepared formulation at various strata within its container, followed by analysis using a validated method. Establishing homogeneity ensures the formulation preparation procedure is adequate for the study.
2. Materials:
- Prepared dose formulation (e.g., solution, suspension, solid-dose)
- Appropriate analytical instrument (e.g., HPLC, UV-Vis Spectrophotometer) with validated method
- Calibrated pipettes and sample containers
3. Procedure:
- Step 1: Preparation. Prepare the dosing formulation according to the study's standard operating procedure. Factors such as batch size, mixing method, and vehicle composition must be documented and kept consistent [28].
- Step 2: Sampling. Sample the prepared formulation from the top, middle, and bottom strata of the container. For each stratum, collect two samples, resulting in a total of n=6 samples for analysis [28].
- Step 3: Analysis. Analyze all samples using the validated analytical method to determine the concentration of the active ingredient.
- Step 4: Calculation and Acceptance Criteria. Calculate the mean, standard deviation (SD), and percent relative standard deviation (%RSD) of the six concentration values. Typical acceptance criteria are %RSD ≤ 3% for solutions and %RSD ≤ 5% for suspensions and solid formulations [28].
4. Troubleshooting: Failed homogeneity assessments often relate to particle size or mixing efficiency. Modifications may include:
- Grinding and Sieving: Grinding the test article with a mortar and pestle, followed by sieving to ensure uniform particle size prior to formulation [28].
- Enhanced Mixing: Increasing homogenization or sonication time, or using specialized equipment like a Silverson homogenizer to achieve a smooth, uniform mixture [28].
The following workflow diagram illustrates the key steps in the homogeneity assessment protocol:
Statistical Assessment of Homogeneity
A more advanced statistical approach for homogeneity assessment, suitable for both formulations and biologic samples, can be employed. The standard uncertainty due to homogeneity (uhom) can be estimated using data from a one-way analysis of variance (ANOVA) [27].
The formula for calculation is:
u_hom = sqrt( MS_within / n ) * sqrt( 2 / f_within^4 )
Where:
- MSwithin represents the mean square within groups from the ANOVA
- n represents the number of replicate measurements
- fwithin represents the degrees of freedom of MSwithin
This calculated uncertainty component can then be incorporated into a comprehensive measurement uncertainty budget for the analytical procedure, strengthening the metrological traceability of the results [27].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Endocrine and Homogeneity Studies
| Item | Function/Application | Key Considerations |
|---|---|---|
| PVP-Iodine Complex | A broad-spectrum antiseptic used in clinical trials (e.g., for oro-nasal application). Serves as a model formulation for stability/homogeneity studies [27]. | Requires stability and homogeneity testing under ICH guidelines; assessment of available iodine content is critical [27]. |
| Sodium Thiosulfate | A titrant used in official USP analytical methods for determining the concentration of available iodine in PVP-I solutions [27]. | Must be of known concentration (e.g., 0.1 M); purity should be ≥99.5% [27]. |
| Binding Protein Assays | Kits or components for measuring free hormones (e.g., free T4, free testosterone) based on equilibrium principles [26]. | Susceptible to bias from alterations in binding proteins; candidate reference methods use ultrafiltration and ID-LC/tandem MS [26]. |
| Ultrafiltration Devices | Used in reference measurement procedures to separate free hormone from protein-bound hormone in serum prior to quantification by mass spectrometry [26]. | Essential for validating routine free hormone immunoassays and ensuring accuracy despite binding protein variations [26]. |
| Enzyme Immunoassay Kits | Multiplex or cell-based assays for detecting and quantifying hormones, cytokines, or autoantibodies (e.g., antibodies to interferon) [29]. | Different methods have varying specificities; a cell-based assay can determine neutralizing activity, while a microarray is useful for screening [29]. |
Integrated Workflow: From Participant Screening to Data Integrity
A robust endocrine study integrates careful participant screening with rigorous procedural controls. The following diagram maps the complete workflow, highlighting the critical control points that safeguard data integrity from cohort assembly to final analysis.
The pursuit of valid and reproducible findings in endocrine research is inextricably linked to the meticulous management of methodologic variance. As outlined in this document, a dual-pronged strategy is essential: first, the implementation of comprehensive participant screening to control for biologic factors such as sex, age, body composition, and menstrual cycle status; and second, the application of rigorous homogeneity assessment protocols for both the study cohort and the reagents or formulations used. By adhering to these structured protocols and understanding the principles underpinning endocrine measurements—such as the free hormone hypothesis—researchers and drug development professionals can significantly reduce experimental noise, enhance the detection of true physiologic effects, and ultimately advance the development of reliable diagnostic and therapeutic interventions.
Implementing Rigorous Pre-Analytical and Analytical Protocols
Methodologic factors in blood collection represent a critical yet often underestimated source of pre-analytical variation in endocrine research. Standardized protocols for patient preparation, sample timing, handling procedures, and storage conditions are paramount for generating reliable, reproducible data in scientific studies and drug development programs. Even with advanced analytical technologies, inconsistent pre-analytical practices can compromise data integrity, leading to erroneous conclusions about endocrine function, biomarker discovery, and therapeutic efficacy. This document establishes detailed application notes and protocols to standardize blood collection specifically for endocrine measurements, providing researchers with a framework to minimize pre-analytical variability.
Patient Preparation Protocols
Proper patient preparation is fundamental to obtaining biologically representative blood specimens for endocrine assessment. Numerous extrinsic factors can alter hormone concentrations, potentially confounding research outcomes.
Fasting Requirements and Dietary Restrictions
Table 1: Common Dietary Preparation Requirements for Endocrine Tests
| Test Name | Fasting Duration | Specific Dietary Restrictions | Rationale |
|---|---|---|---|
| Basic & Comprehensive Metabolic Panel | 8-12 hours [30] | Water only; no other beverages or food | Prevents interference from lipidemia and ensures accurate glucose and electrolyte measurements |
| Lipid Profile (Cholesterol, Triglycerides) | 9-12 hours [30] | Avoid alcohol for 24-48 hours; maintain consistent fat intake prior to fast | Minimizes postprandial effects on triglyceride levels and lipid metabolism |
| Glucose & Insulin Tests | 8-12 hours [30] | Water only; avoid caffeine | Establishes baseline glucose and insulin levels without dietary influence |
| 5-HIAA Test (Serotonin Metabolite) | Not typically required | Avoid avocados, bananas, pineapples, walnuts, eggplants 24-48 hours before test [30] | Prevents false elevation from serotonin-rich foods interfering with metabolite measurement |
Behavioral and Pharmacological Considerations
Beyond dietary factors, researchers must control for behavioral and pharmacological influences:
- Medication and Supplements: Document all prescription medications, over-the-counter drugs, vitamins, and supplements [30]. Endocrine researchers should establish washout periods for interfering substances when scientifically justified and ethically permissible.
- Physical Activity: Avoid strenuous exercise for 24-48 hours before blood collection, as physical exertion can acutely alter cortisol, growth hormone, and other stress-responsive hormones [30].
- Sleep Patterns: Encourage a good night's sleep prior to sampling [31], as sleep deprivation disrupts circadian hormone rhythms including cortisol and melatonin.
- Stress Minimization: Implement relaxation protocols before venipuncture, as anxiety can elevate cortisol, catecholamines, and prolactin [31].
- Tobacco and Alcohol: Refrain from smoking and alcohol consumption for specified periods before sampling, as both can influence endocrine parameters.
Timing Considerations for Circadian Rhythms
Many endocrine biomarkers exhibit significant circadian, ultradian, and seasonal rhythmicity:
- Standardize Collection Times: Collect samples at consistent times of day within and across studies, particularly for cortisol, TSH, and sex hormones which have known diurnal variation.
- Document Collection Time: Record exact phlebotomy time [32] to enable statistical adjustment for circadian effects.
- Consider Menstrual Cycle Phase: For sex hormone assessments in premenopausal women, document and standardize collection according to menstrual cycle phase.
Figure 1: Comprehensive patient preparation workflow for endocrine research.
Blood Collection Procedures
Standardized venipuncture techniques are essential to prevent in vitro alterations that compromise endocrine measurements.
Order of Draw
Table 2: CLSI Order of Draw for Blood Collection Tubes
| Order | Tube Type | Additive | Common Uses in Endocrine Research |
|---|---|---|---|
| 1 | Blood culture bottles | Culture media | Rule out infection in endocrine studies (rarely used) |
| 2 | Sodium citrate (blue closure) | Sodium citrate | Coagulation studies (not typically endocrine) |
| 3 | Serum tubes (red, red-speckled, gold closures) | Clot activator ± gel separator | Thyroid hormones, steroid hormones, prolactin |
| 4 | Heparin (green closure) | Lithium/sodium heparin ± gel | Electrolytes, insulin, cortisol (plasma) |
| 5 | EDTA (lavender, pearl, pink closures) | K₂/K₃ EDTA | Renin, aldosterone, plasma catecholamines |
| 6 | Sodium fluoride/potassium oxalate (gray closure) | Glycolytic inhibitors | Glucose, lactate (preserves unstable analytes) |
The Clinical and Laboratory Standards Institute (CLSI) established this specific order of draw to prevent cross-contamination of tube additives [33]. For endocrine research, particular attention should be paid to:
- Serum Tubes: Allow complete clot formation (30-45 minutes) before processing for thyroid and steroid hormones.
- EDTA Tubes: Use for peptide hormones like PTH and catecholamines; invert gently 8-10 times immediately after collection.
- Glycolytic Inhibitors: Essential for accurate glucose measurements in studies of glucose metabolism.
Venipuncture Protocol
Step 1: Equipment Assembly Collect all necessary equipment: appropriate vacuum tubes, safety-engineered blood collection devices, non-sterile well-fitting gloves, tourniquet, alcohol-based disinfectant (70% isopropyl alcohol or chlorhexidine-alcohol combination), gauze, bandages, and specimen labels [34].
Step 2: Patient Identification and Site Selection
- Confirm patient identity using at least two unique identifiers [32].
- Position patient comfortably, preferably supine for endocrine assessments affected by posture (e.g., renin-aldosterone).
- Inspect antecubital fossa to locate visible, straight veins; median cubital vein is preferred [34].
- Apply tourniquet 4-5 finger widths above intended venipuncture site [34].
Step 3: Aseptic Technique and Venipuncture
- Perform hand hygiene and don gloves [34] [35].
- Disinfect venipuncture site using appropriate antiseptic in a back-and-forth motion for 30 seconds, allowing complete drying (30-60 seconds) [32].
- Disinfect blood culture bottle septa or tube tops with 70% isopropyl alcohol if used [32].
- Anchor vein and perform venipuncture using safety-engineered device.
- Collect blood in correct order of draw [33].
- Release tourniquet within one minute of application to prevent hemoconcentration.
Step 4: Post-Collection Procedures
- Apply gauze and gentle pressure after needle withdrawal; secure with bandage.
- Discard used needles and blood collection devices immediately in puncture-resistant sharps container [34] [35].
- Label all tubes at the patient bedside with required information [32].
Sample Handling and Storage Protocols
Proper post-collection handling is critical for preserving labile endocrine analytes.
Temperature Management and Processing Timelines
Table 3: Sample Handling Conditions for Endocrine Analytes
| Analyte Category | Processing Temperature | Processing Timeline | Storage Temperature | Special Considerations |
|---|---|---|---|---|
| Peptide Hormones (Insulin, PTH, GH) | Room temperature or 4°C | Centrifuge within 1 hour | -20°C to -80°C | Avoid repeated freeze-thaw cycles; use protease inhibitors for some peptides |
| Steroid Hormones (Cortisol, Estradiol, Testosterone) | Room temperature | Centrifuge within 2 hours | -20°C to -80°C | Generally stable but temperature-sensitive for long-term storage |
| Catecholamines (Epinephrine, Norepinephrine) | 4°C (on ice) | Centrifuge within 30 minutes | -70°C or lower | Use special preservative; extremely labile at room temperature |
| Thyroid Hormones (TSH, T4, T3) | Room temperature | Centrifuge within 2 hours | -20°C | Generally stable but follow specific assay requirements |
Sample Processing Workflow
Figure 2: Endocrine sample handling and processing workflow.
Quality Assurance Measures
- Sample Identification: Implement a system using at least two unique patient-specific identifiers on all samples and requisition forms [32].
- Hemolysis Assessment: Inspect serum/plasma for hemolysis; note and report hemolyzed samples as they interfere with many endocrine assays.
- Documentation: Maintain accurate records of collection time, processing time, freeze-thaw cycles, and storage conditions [36].
- Transportation: Use temperature-monitored transport with appropriate packaging to maintain sample integrity [36].
Research Reagent Solutions
Table 4: Essential Materials for Endocrine Blood Collection
| Item | Function | Application Notes |
|---|---|---|
| Serum Separation Tubes (SST) | Allows clot formation and serum separation via gel barrier | Ideal for most steroid and thyroid hormones; invert 5 times after collection |
| K₂EDTA Tubes | Preserves whole blood for plasma separation; chelates calcium | Preferred for peptide hormones like PTH, renin; invert 8-10 times immediately |
| Sodium Heparin Tubes | Anticoagulant for plasma samples; preserves certain enzymes | Alternative to EDTA for some hormone assays; check assay compatibility |
| PAXgene Blood RNA Tubes | Stabilizes intracellular RNA for gene expression studies | For transcriptomic studies in endocrine research; requires specific handling |
| Protease Inhibitor Cocktails | Inhibits protein degradation in blood samples | Essential for proteomic approaches in hormone discovery |
| Cryogenic Vials | Long-term storage at ultra-low temperatures | Use internally-threaded vials to prevent contamination during storage |
| Temperature Monitoring Devices | Tracks sample temperature during storage and transport | Critical for validating sample integrity for regulatory submissions |
Standardization of blood collection protocols represents a fundamental requirement for generating valid, reproducible data in endocrine research. By implementing these detailed protocols for patient preparation, venipuncture technique, sample handling, and storage, researchers can significantly reduce pre-analytical variability—a persistent confounder in endocrine measurements. Consistency across these methodological factors ensures that biological signals rather than procedural artifacts drive research findings, ultimately enhancing the reliability of endocrine studies and accelerating drug development processes.
The selection between immunoassay and liquid chromatography-tandem mass spectrometry (LC-MS/MS) is a critical methodological consideration in endocrine research. Immunoassays have served as the gold standard for decades, but LC-MS/MS is increasingly recognized for its superior specificity and multiplexing capabilities [37] [38]. The fundamental distinction lies in their detection principles: immunoassays rely on antibody-antigen binding, while LC-MS/MS separates and identifies molecules based on their mass-to-charge ratio [37] [39]. This technical difference translates to significant practical implications for sensitivity, specificity, and applicability in research and drug development.
The following table summarizes the core comparative characteristics of these two methodological approaches.
Table 1: Core Comparative Characteristics of Immunoassay and LC-MS/MS
| Characteristic | Immunoassay | LC-MS/MS |
|---|---|---|
| Principle of Detection | Antibody-antigen binding and signal detection (colorimetric, fluorescent, etc.) [37] | Physical separation followed by mass-based identification [37] [39] |
| Specificity | Susceptible to cross-reactivity with structurally similar compounds or matrix interferents [40] [41] | High inherent specificity; can distinguish between structurally similar analytes (e.g., steroid hormones) [40] [42] |
| Multiplexing Capability | Possible with technologies like Luminex and MSD, but can be challenging with antibody cross-reactivity [37] | High; can simultaneously quantify dozens of analytes in a single run (e.g., 19 steroids) [40] [42] |
| Sensitivity | Generally high (e.g., pico-gram level for MSD) [37] | Comparable or superior; suitable for low-concentration analytes in complex matrices [37] [40] |
| Dynamic Range | Typically 3-4 orders of magnitude; up to 5 with advanced platforms like MSD [37] | Wide, often 4-5 orders of magnitude [37] [40] |
| Development Timeline | Can be lengthy due to antibody production and optimization [37] | Generally faster development, less reliant on specific protein reagents [39] [38] |
| Sample Volume | Can be low, but depends on the format | Requires low sample volumes (e.g., 25 μL plasma) [43] |
| Throughput | High for established kits | High, especially with automated sample preparation [37] [40] |
Detailed Experimental Protocols
Protocol for LC-MS/MS Analysis of Steroid Hormones
This protocol is adapted from a validated method for quantifying 17 steroid hormones and 2 synthetic drugs in plasma or serum, demonstrating the application of LC-MS/MS for complex endocrine panels [40] [42].
Sample Preparation:
- Protein Precipitation: Add 300 µL of a cold organic solvent mixture (e.g., methanol:acetonitrile) to 25 µL of plasma or serum in a microcentrifuge tube [40] [43].
- Vortex and Centrifuge: Vortex the mixture vigorously for 1 minute and incubate on ice for 30 minutes. Centrifuge at 12,000-15,000 rpm for 10 minutes at 4°C to pellet precipitated proteins [40].
- Solid-Phase Extraction (SPE): Transfer the supernatant to a pre-conditioned SPE µElution plate (e.g., Oasis HLB). Wash and elute the analytes according to the optimized protocol for the specific steroid panel. This step purifies the sample and reduces matrix effects [40] [42].
- Reconstitution: Evaporate the eluent to dryness under a gentle stream of nitrogen or using a centrifugal vacuum concentrator. Reconstitute the dry residue in an appropriate volume of initial mobile phase for LC-MS/MS injection [40].
Liquid Chromatography:
- Column: Utilize a reversed-phase UPLC column (e.g., ACQUITY UPLC BEH C18, 2.1 mm × 100 mm, 1.7 µm) maintained at a constant temperature (e.g., 40°C) [40].
- Mobile Phase: Employ a binary gradient system. Mobile Phase A is often an aqueous solution (e.g., 10 mM ammonium formate with 0.1% formic acid), and Mobile Phase B is an organic solvent (e.g., acetonitrile with 0.1% formic acid) [40] [43].
- Gradient and Flow: Use a optimized gradient elution program. For example, start at 5% Mobile Phase A, ramp to 60% over 10 minutes, with a constant flow rate of 0.4 mL/min [43].
- Injection Volume: A typical injection volume is 5-10 µL [40].
Mass Spectrometry:
- Ionization: Employ Electrospray Ionization (ESI) in positive or negative mode, depending on the analytes. Key parameters include an ion spray voltage (e.g., 4.5 kV) and source temperature (e.g., 425°C) [40] [43].
- Analysis: Operate the triple quadrupole mass spectrometer in Multiple Reaction Monitoring (MRM) mode. This involves selecting the precursor ion of the target analyte in the first quadrupole, fragmenting it in the second, and monitoring one or more specific product ions in the third quadrupole. This provides high specificity [39] [40].
- Quantification: Use a stable isotope-labeled (SIL) internal standard for each analyte to correct for variability in sample preparation and ionization. Quantify analytes by interpolating the analyte-to-internal standard peak area ratio against a linear calibration curve [39] [40].
Figure 1: LC-MS/MS Workflow for Endocrine Analytics
Protocol for a Multiplex Immunoassay (e.g., Meso Scale Discovery - MSD)
This protocol outlines the steps for a multiplex electrochemiluminescent immunoassay, suitable for quantifying multiple proteins simultaneously, such as appetite-related hormones or cytokines [37].
Assay Procedure:
- Plate Preparation: Use an MSD multi-spot plate pre-coated with capture antibodies specific to the target proteins in each spot. Block any remaining binding sites with a blocking buffer [37].
- Standard and Sample Addition: Prepare a serial dilution of the purified protein standard to generate a calibration curve. Add standards and prepared samples (e.g., saliva or plasma supernatants) to the designated wells. Incubate with shaking to allow the target analytes to bind to the capture antibodies [37] [44].
- Washing: After incubation, decant the plate contents and wash the plate several times with a wash buffer to remove unbound proteins and matrix components.
- Detection Antibody Addition: Add a mixture of detection antibodies, each conjugated to an SULFO-TAG label (an electrochemiluminescent compound), specific to the captured analytes. Incubate to form a sandwich complex: capture antibody-analyte-detection antibody [37].
- Final Wash and Reading: Wash the plate again to remove unbound detection antibodies. Add a read buffer to the plate. The MSD instrument applies an electrical potential to the plate electrodes, which stimulates the SULFO-TAG labels to emit light. The intensity of the emitted light at each spot is measured and is proportional to the amount of analyte bound [37].
Data Analysis:
- Curve Fitting: Generate a calibration curve for each analyte using the standard data, typically with a non-linear 4- or 5-parameter logistic (4PL/5PL) model [39].
- Concentration Interpolation: Interpolate the concentration of analytes in unknown samples from their respective calibration curves.
Figure 2: Multiplex Electrochemiluminescent Immunoassay Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of either methodology requires specific, high-quality reagents. The following table details essential materials and their functions.
Table 2: Essential Reagents for Immunoassay and LC-MS/MS
| Reagent / Material | Function | Application |
|---|---|---|
| Capture & Detection Antibodies | Bind specifically to the target protein analyte for isolation and signal generation. Critical for specificity [37]. | Immunoassay |
| SULFO-TAG Label | An electrochemiluminescent label conjugated to detection antibodies. Emits light upon electrical stimulation for detection [37]. | MSD Immunoassay |
| Stable Isotope-Labeled (SIL) Internal Standards | Chemically identical analogs of the analyte with heavier isotopes (e.g., ^13^C, ^15^N). Corrects for sample loss and ion suppression, ensuring accuracy and precision [39]. | LC-MS/MS |
| Solid-Phase Extraction (SPE) Plates | Microwell plates containing sorbent material for purifying and concentrating analytes from biological samples, reducing matrix effects [40]. | LC-MS/MS |
| UPLC BEH C18 Column | A reversed-phase chromatography column with small, durable particles for high-resolution separation of complex mixtures prior to MS detection [40]. | LC-MS/MS |
| Stable Protein Standard | A purified and well-characterized protein used to create the calibration curve for quantitative analysis [37]. | Immunoassay, Protein LC-MS/MS |
Method Selection and Validation Framework
Choosing between immunoassay and LC-MS/MS depends on the research question's specific requirements. Key decision factors include:
- Required Specificity: For measuring specific analytes within a class of structurally similar molecules (e.g., individual steroid hormones, free vs. total concentrations), LC-MS/MS is often necessary due to its high specificity and low cross-reactivity [40] [41].
- Multiplexing Needs: If the study requires simultaneous measurement of a large panel of biomarkers (e.g., a multi-steroid panel or a broad metabolomic profile), LC-MS/MS is the most efficient platform [40] [45]. For a smaller set of protein biomarkers, multiplex immunoassays can be effective [37].
- Throughput and Cost: While LC-MS/MS instrumentation has a higher initial cost, it can offer a lower cost per sample for multiplexed analyses and faster development times compared to developing multiple individual immunoassays [38].
- Sample Matrix: Complex matrices like saliva require careful method development due to potential interferents. LC-MS/MS's separation step can provide an advantage in overcoming matrix effects compared to some immunoassays [44] [41].
Validation Considerations: For regulated bioanalysis, method validation is crucial. For LC-MS/MS protein/steroid methods, key parameters to validate include accuracy and precision (within ±20-25%), sensitivity (LLOQ), and demonstration of selectivity against matrix interferences using 6-10 individual matrix lots [39]. It is also critical to assess matrix effects on ionization and ensure the stability of the analytes throughout the sample processing and storage lifecycle [39].
Establishing Personalized Reference Intervals for Diverse Populations
The interpretation of laboratory results is fundamental to endocrine research and clinical diagnostics. Traditionally, this relies on population-based reference intervals (popRIs), which define a "normal" range based on the central 95% of values from a reference population [46]. However, a significant methodological limitation exists: popRIs are designed for population-level interpretation and perform poorly when assessing individual patient results [47] [48]. A test result that falls within the broad popRI may nonetheless represent a significant pathological change for that specific individual, a change that remains hidden without an individual context for comparison.
Personalized reference intervals (prRIs) represent a paradigm shift, moving from a population-centric to an individual-centric model. Founded on the homeostatic model, a prRI is a statistically derived range specific to a single person, calculated from their previous results and estimates of analytical and biological variation [47]. This approach is particularly powerful in endocrinology, where hormone levels exhibit significant individual biological variation and are influenced by factors such as sex, age, body composition, and circadian rhythms [2]. By providing a tailored baseline, prRIs enhance the sensitivity for detecting clinically significant changes in an individual, thereby addressing a critical methodological gap in longitudinal endocrine research and patient monitoring.
Theoretical Foundation: From Population to Personal
Limitations of Population-Based Reference Intervals
The use of popRIs for individual patient care and research has several inherent weaknesses. PopRIs assume that the individual's biological variation is equivalent to the variation seen between individuals in a population, which is often not the case [47]. The appropriateness of a popRI is quantified by the index of individuality (II), calculated as the ratio of within-subject biological variation (CVI) to between-subject biological variation (CVG) [48]. An II of less than 0.6 indicates low individuality, meaning that the population reference interval is often insensitive to detecting significant changes within an individual [47]. Many endocrine biomarkers fall into this category, making the case for personalization particularly strong.
The Concept of Biological Variation
Biological variation (BV) is the natural fluctuation of an analyte around an individual's homeostatic set point (HSP) and is composed of two elements:
- Within-subject biological variation (CVI): The variation observed in a single individual over time.
- Between-subject biological variation (CVG): The variation in the average values of different individuals.
The prRI concept leverages these principles to create a prediction interval for an individual's future test results based on their own historical data [47]. This interval is calculated by incorporating the CVI and the analytical variation (CVA) of the measurement method, providing a much tighter and more relevant range for monitoring.
Key Calculations for Personalized Reference Intervals
The core of establishing a prRI involves calculating the Reference Change Value (RCV) and the prRI itself. The RCV, also known as the critical difference, is the minimum difference between two consecutive test results that can be considered statistically significant [48]. The formulas for a prRI based on population BV data are:
Reference Change Value (RCV):
RCV = z × √2 × √(CVA² + CVI²)
Where z is the z-score (e.g., 1.96 for a 95% confidence level).
Personalized Reference Interval (prRI):
prRI = HSP ± (z × √(CVA² + CVI²))
Where HSP is the individual's homeostatic set point, estimated from their previous measurements [48].
The following diagram illustrates the logical workflow for determining and applying the appropriate reference interval method.
The practical advantage of prRIs is demonstrated by their ability to detect pathological changes that popRIs miss. A recent case study observing a patient through SARS-CoV-2 reinfection provided a direct comparison of these methods.
Table 1: Performance Comparison of Reference Interval Methods in a Clinical Case (N=110 tests) [48]
| Method Type | Number of Potential Abnormal Values Identified | Ratio of Abnormal to Total Tests |
|---|---|---|
| Population-Based Reference Intervals (popRIs) | 2 | 2/110 |
| Personalized RIs (from Population BV data) | 22 | 22/110 |
| Reference Change Value (from Population BV data) | 25 | 25/110 |
Table 2: Calculated Parameters for Personalized Reference Intervals in a Case Study [48]
| Analyte | Homeostatic Set Point (HSP) | CVI (%) | popRI | prRI_pop. | RCV_pop. (%) |
|---|---|---|---|---|---|
| Leukocytes (x 10⁹/L) | 4.8 ± 0.5 | 11.10 | 3.5 ~ 9.5 | 3.7 ~ 6.0 | 30.96 |
| Neutrophils (x 10⁹/L) | 3.0 ± 0.3 | 14.10 | 1.8 ~ 6.3 | 2.0 ~ 3.9 | 39.29 |
| Lymphocytes (x 10⁹/L) | 1.4 ± 0.1 | 10.80 | 1.1 ~ 3.2 | 1.0 ~ 1.7 | 31.51 |
| Hemoglobin (g/L) | 141 ± 5 | 2.70 | 115 ~ 150 | 132 ~ 149 | 7.52 |
| Platelets (x 10⁹/L) | 217 ± 25 | 6.40 | 125 ~ 350 | 185 ~ 249 | 18.06 |
As shown in Table 2, the prRI is consistently narrower than the popRI for these parameters, creating a more precise "normal" range for the individual. This increased precision directly translates to the enhanced sensitivity for detecting abnormality demonstrated in Table 1.
The Scientist's Toolkit: Research Reagent Solutions
The successful implementation of prRIs in endocrine research requires careful attention to methodological consistency. The following reagents and materials are critical for ensuring data quality.
Table 3: Essential Research Reagents and Materials for Endocrine Studies
| Item | Function/Application | Methodological Considerations |
|---|---|---|
| Certified Reference Materials | Calibrate analytical instruments and assays to ensure accuracy and traceability. | Source from National Metrology Institutes; verify commutability with patient samples [47]. |
| Quality Control (QC) Pools | Monitor analytical performance (precision and drift) over time. | Use at least two different concentration levels; determine CVA from QC data [48]. |
| Stable Isotope-Labeled Internal Standards | Correct for sample-specific matrix effects and losses in sample preparation (e.g., in MS assays). | Essential for liquid chromatography-mass spectrometry (LC-MS/MS) methods to achieve high precision. |
| Specialized Collection Tubes | Maintain sample integrity for specific analytes (e.g., proteases, chelators). | Use prescribed tubes (e.g., EDTA, heparin, serum); follow strict sample handling protocols [2]. |
| Automated Immunoassay/LC-MS Platforms | Perform high-throughput, precise quantification of hormone levels. | Select platform based on required sensitivity and specificity; CVA is a key input for prRI calculations [47] [48]. |
Methodologic Factors in Endocrine Research
The accurate establishment of prRIs is highly dependent on controlling pre-analytical and biological variables that contribute to variance in endocrine measurements [2]. Key factors to control in study design include:
- Biological Factors: Sex, age, race, body composition, and mental health status can significantly influence baseline hormone levels [2]. For example, the menstrual cycle phase in females causes large, predictable fluctuations in reproductive hormones, requiring careful timing of sample collection for establishing a reliable HSP [2].
- Procedural-Analytic Factors: Time of day (circadian rhythms), fasting status, and posture during blood draw are critical. Standardizing these procedures across all sample collections is essential to minimize unnecessary variance that could widen the prRI and reduce its clinical sensitivity [2].
Experimental Protocols
Protocol 1: Establishing a Personalized Reference Interval
This protocol outlines the steps for calculating a prRI for an endocrine biomarker using population biological variation data.
1. Define the Analyte and Gather Prerequisites:
- Select the endocrine biomarker (e.g., cortisol, TSH, testosterone).
- Obtain the population-derived within-subject biological variation (CVI) for the analyte from a reliable source such as the European Federation of Clinical Chemistry and Laboratory Medicine (EFLM) Biological Variation database.
- Determine the analytical variation (CVA) of your measurement method from internal quality control data.
2. Estimate the Individual's Homeostatic Set Point (HSP):
- Collect a minimum of three serial samples from the individual under steady-state conditions (e.g., same time of day, fasting status).
- Ensure the individual is free from acute illness during this baseline period.
- Calculate the mean value of these measurements. This mean serves as the best estimate for the HSP.
3. Calculate the prRI and RCV:
- Apply the formulas from Section 2.3.
- For a 95% probability interval, use
z = 1.96. - Example Calculation for Cortisol:
- Assume:
HSP = 12.5 μg/dL,CVI = 10.2%,CVA = 5.0%. - prRI Calculation:
Width = 1.96 * √(5.0² + 10.2²) = 1.96 * √(127.04) = 1.96 * 11.27 = 22.09% - prRI =
12.5 μg/dL ± 22.09%=9.7 - 15.3 μg/dL - RCV Calculation:
RCV = 1.96 * √2 * √(5.0² + 10.2²) = 1.96 * 1.414 * 11.27 ≈ 31.2%
- Assume:
4. Validate and Implement:
- Report the calculated prRI and RCV alongside subsequent test results.
- Flag a result as significantly changed if it falls outside the prRI or if the difference from the previous value exceeds the RCV.
The following workflow summarizes this multi-step protocol for practical application in a research setting.
Protocol 2: Monitoring with Reference Change Value in an Intervention Study
This protocol is designed for monitoring individual responses to an intervention, such as a new drug therapy or exercise program.
1. Baseline Phase:
- Collect two baseline samples from the study participant, separated by a short, standardized time interval (e.g., 24-48 hours) to minimize biological variation not related to the intervention.
- Analyze samples using the same validated method.
2. Pre-Calculate RCV:
- Prior to the intervention, calculate the RCV for the target biomarker(s) using the formula in Protocol 1.
3. Intervention Phase:
- Administer the intervention according to the study protocol.
- Collect post-intervention samples at predefined time points.
4. Assessment of Change:
- For each post-intervention result, calculate the percentage difference from the baseline average.
- A change is considered statistically significant if the percentage difference exceeds the pre-calculated RCV.
- This method helps distinguish true treatment effects from random analytical and biological noise.
The establishment of personalized reference intervals represents a significant methodological advancement in endocrine research. By accounting for an individual's unique homeostatic set point and biological variation, prRIs offer a more precise and powerful tool for detecting clinically relevant changes than traditional population-based ranges. The successful application of this approach requires rigorous control of pre-analytical variables, precise analytical methods, and the use of reliable biological variation data. As the field moves towards more personalized medicine, the integration of prRIs into research protocols and clinical practice will enhance our ability to understand individual physiological responses and optimize therapeutic interventions.
The EndoCompass Project Roadmap for Laboratory Medicine
The EndoCompass Research Roadmap, a major initiative by the European Society of Endocrinology (ESE) and the European Society for Paediatric Endocrinology (ESPE), provides a strategic framework to advance endocrine science over the next decade [49] [50]. Developed by 228 clinical and scientific experts across Europe alongside patient advocacy groups, this roadmap addresses the critical gap between the societal impact of endocrine disorders and their chronic underfunding in research programs, which accounted for less than 4% of Horizon 2020 biomedical and health research funding [50]. For laboratory medicine, the roadmap establishes evidence-based priorities to enhance the quality, standardization, and innovation of hormonal measurements, which are fundamental to both research validity and clinical care [51].
Accurate endocrine measurement is fundamentally challenged by numerous methodological factors that introduce variance and can compromise data validity [2]. These influences can be categorized into biologic variation (stemming from the physiologic status of the participant) and procedural-analytic variation (determined by investigative procedures) [2]. The EndoCompass laboratory medicine chapter directly addresses these challenges by calling for strategic investment in quality assurance, standardization of endocrine tests, and the implementation of innovative technologies [51]. This application note details the experimental protocols and methodologies necessary to operationalize this roadmap, ensuring reliable and reproducible endocrine data.
Quantitative Analysis of Methodologic Variance in Endocrine Research
Key Biologic Factors Influencing Hormonal Measurements
Biologic factors are endogenous to the participant's physiologic status at the time of specimen collection. The following table summarizes the primary biologic factors, their specific influences on hormonal measurements, and recommended control strategies for research design [2].
Table 1: Key Biologic Factors and Their Influence on Endocrine Measurements
| Biologic Factor | Impact on Hormonal Measurements | Exemplary Hormones Affected | Recommended Control Strategies |
|---|---|---|---|
| Sex | Marked differences post-puberty; influences exercise response. | Testosterone, Growth Hormone, Leptin | Match participant groups by sex; account for sex-specific responses. |
| Age & Maturation | Alters resting levels, exercise response, and training adaptation. | Growth Hormone, Testosterone, Cortisol, Insulin Resistance | Match participants by chronologic age and/or maturation level. |
| Body Composition | Adiposity influences cytokines and metabolic hormones. | Insulin, Leptin, Cortisol, Catecholamines | Match volunteers for adiposity (e.g., BMI categories) rather than body weight alone. |
| Menstrual Cycle | Causes large, dramatic fluctuations in reproductive and other hormones. | Estradiol-β-17, Progesterone, Luteinizing Hormone (LH), Follicle-Stimulating Hormone (FSH) | Test females of similar menstrual status or in the same cycle phase; account for oral contraceptive use. |
| Circadian Rhythms | Causes predictable daily fluctuations in hormone levels. | Cortisol, Growth Hormone, Thyroid-Stimulating Hormone (TSH) | Standardize time of day for specimen collection across all participants. |
| Mental Health | Conditions like anxiety and depression can elevate or suppress basal levels. | Catecholamines, ACTH, β-endorphin, Cortisol, Thyroid hormones | Utilize mental health screening questionnaires administered by qualified personnel. |
Procedural-Analytic Research Priorities from the EndoCompass Roadmap
The EndoCompass project for laboratory medicine translates current challenges into strategic research priorities. These priorities are designed to minimize procedural-analytic variance and leverage new technologies [51].
Table 2: EndoCompass Procedural-Analytic Research Priorities and Methodologic Implications
| Research Priority Area | Specific Goals & Methodologic Implications | Key Outcomes for Research Quality |
|---|---|---|
| Pre-Analytical Process Optimization | Define and standardize conditions from specimen collection to analysis (e.g., time of day, posture, tourniquet use, sample handling). | Reduced introduced variance, improved inter-study comparability. |
| Standardization & Harmonization | Develop common standards and reference measurement procedures for endocrine tests across platforms (e.g., LC-MS/MS vs. immunoassay). | Equitable result interpretation, reliable multi-center research data. |
| Personalized Reference Intervals | Establish reference intervals and clinical decision limits that consider diversity, biological variation, and environmental factors. | More accurate clinical interpretation and participant stratification in research. |
| Biomarker Innovation & Point-of-Care Testing (POCT) | Discover and validate new biomarkers; develop robust, accurate POCT technologies for decentralized testing. | Novel research endpoints and increased accessibility of endocrine testing. |
| Sustainable Laboratory Practices | Implement eco-friendly laboratory workflows without compromising analytical quality. | Reduced environmental impact of endocrine research. |
| Leveraging Artificial Intelligence (AI) | Apply AI for data analysis, pattern recognition, and improving diagnostic accuracy from complex datasets. | Enhanced data interpretation, identification of novel biomarkers and associations. |
Experimental Protocols for Advanced Endocrine Laboratory Analysis
Protocol 1: Standardized Pre-Analytical Workflow for Blood-Based Hormone Assessment
This protocol is designed to minimize pre-analytical variance, a cornerstone of the EndoCompass roadmap [51], by controlling key biologic and procedural factors [2].
1.0 Principal Investigator and Personnel: Certified phlebotomists, trained research nurses, and laboratory technicians. 2.0 Reagent Solutions and Materials:
- Tourniquet: Standard clinical single-use.
- Blood Collection Tubes: Serum separator tubes (SST), EDTA plasma tubes, specialized tubes (e.g., containing protease inhibitors for labile analytes).
- Centrifuge: Refrigerated bench-top centrifuge capable of 1500 × g.
- Storage Vessels: Cryogenic vials (e.g., 2.0 mL).
- Low-Temperature Storage: -80°C Freezer, liquid nitrogen for long-term storage.
- Labelling System: Barcode labels and scanner.
- Data Management System: Electronic Case Report Form (eCRF) or Laboratory Information Management System (LIMS).
3.0 Procedural Steps:
- Participant Preparation & Scheduling: Schedule all blood draws to control for circadian rhythms, ideally between 7:00-9:00 AM. Instruct participants to fast for 8-12 hours, avoid strenuous exercise and alcohol for 24 hours, and arrive well-hydrated.
- Pre-Collection Rest: Upon arrival, have the participant rest in a seated or supine position for 20 minutes before venipuncture to stabilize hormone levels affected by posture and recent activity.
- Standardized Venipuncture: Perform venipuncture using minimal tourniquet time (ideally < 1 minute) to avoid hemoconcentration. Document the exact time of collection.
- Sample Handling & Processing: Gently invert collection tubes as per manufacturer's instructions. Allow serum tubes to clot for exactly 30 minutes at room temperature. Centrifuge all tubes at 1500 × g for 15 minutes at 4°C within 1 hour of collection.
- Aliquoting & Storage: Immediately aliquot the supernatant (serum/plasma) into pre-labeled cryogenic vials. Flash-freeze aliquots in a mixture of dry ice and ethanol or place directly in a -80°C freezer. Avoid multiple freeze-thaw cycles.
- Data Annotation: Record all critical pre-analytical data in the eCRF/LIMS: participant ID, collection date/time, processing time, freezer location, and any protocol deviations.
Protocol 2: Method Comparison for Hormone Assay Harmonization
This protocol addresses the EndoCompass priority of standardization and harmonization [51] by systematically comparing a novel or routine immunoassay with a gold-standard Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) method.
1.0 Principal Investigator and Personnel: Mass spectrometry specialist, clinical chemist, biostatistician. 2.0 Reagent Solutions and Materials:
- Test Samples: A minimum of 100 residual clinical serum/plasma samples covering the assay's measuring interval (low, medium, high).
- Reference Method: Validated LC-MS/MS platform.
- Comparative Method: Automated immunoassay platform.
- Quality Controls (QCs): Commercial QC materials at multiple levels.
- Calibrators: Manufacturer-provided calibrators for both methods.
- Data Analysis Software: Statistical software package (e.g., R, MedCalc, EP Evaluator).
3.0 Procedural Steps:
- Sample Selection & Aliquoting: Select and thaw samples. Create two identical aliquots for each sample, one for each method. Ensure all samples are processed in a single batch to minimize drift.
- Calibration & Quality Control: Calibrate both the LC-MS/MS and immunoassay systems according to manufacturer protocols. Run QCs at the beginning, middle, and end of the batch to ensure analytical performance.
- Sample Analysis: Analyze all sample aliquots in a randomized order on both platforms within the same working day to minimize the effect of sample degradation.
- Data Collection & Management: Record raw results from both instruments. Anonymize data and prepare for statistical analysis.
- Statistical Analysis for Method Comparison:
- Perform Passing-Bablok regression and Bland-Altman analysis to assess systematic and proportional bias.
- Calculate the Pearson or Spearman correlation coefficient.
- Analyze bias at critical medical decision points.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and reagents essential for implementing high-quality endocrine research protocols, aligning with the push for improved analytical quality and innovation [51].
Table 3: Key Research Reagent Solutions for Endocrine Laboratory Medicine
| Item/Category | Function & Application in Endocrine Research |
|---|---|
| LC-MS/MS Systems | Gold-standard for hormone quantification due to high specificity and sensitivity; crucial for developing reference measurement procedures and harmonization studies [51]. |
| High-Affinity/Specific Antibodies | Core components of immunoassays and immunohistochemistry; their quality directly determines assay specificity, sensitivity, and cross-reactivity for proteins and peptide hormones. |
| Stable Isotope-Labeled Internal Standards | Used in LC-MS/MS to correct for sample matrix effects and losses during preparation; essential for achieving high accuracy and precision in mass spectrometric quantification. |
| Certified Reference Materials | Well-characterized materials with assigned analyte values; used for calibrating measurement procedures and ensuring traceability, a key aspect of standardization [51]. |
| Specialized Collection Tubes | Tubes containing specific additives (e.g., protease inhibitors, anticoagulants) to stabilize labile hormones (e.g., ACTH, glucagon) during the pre-analytical phase [2] [51]. |
| Multiplex Immunoassay Panels | Allow simultaneous measurement of multiple hormones/cytokines from a single small-volume sample; useful for exploratory research and assessing complex endocrine axes. |
| Point-of-Care Testing (POCT) Devices | Enable rapid hormone measurement near the participant (e.g., glucose, HbA1c); research focuses on improving their accuracy and expanding the menu of measurable hormones [51]. |
The EndoCompass Project Roadmap for Laboratory Medicine provides an essential strategic framework for elevating the quality and impact of endocrine research. By implementing the detailed experimental protocols for pre-analytical control and method harmonization, researchers can directly address the critical methodological factors—both biologic and procedural-analytic—that introduce variance and compromise data validity [2] [51]. The integration of advanced technologies like LC-MS/MS and AI, coupled with a rigorous focus on standardization and quality assurance, will enable the generation of more reliable, reproducible, and clinically translatable endocrine data. This disciplined methodological approach is fundamental to realizing the EndoCompass vision of aligning research with the highest priority questions in endocrine health, ultimately leading to improved patient outcomes.
The validity of endocrine research is fundamentally dependent on the rigorous control of methodological variables. Among these, lifestyle factors—diet, exercise, and sleep—represent significant sources of biological variance that can dramatically compromise the accuracy and validity of physiological data if not properly monitored and adjusted for [2]. The decline in testosterone levels among young males, for instance, is increasingly linked to modern lifestyle shifts rather than aging alone, highlighting the need to account for these variables in study designs [52]. This protocol provides detailed methodologies for controlling these lifestyle factors to reduce experimental variance and increase the scientific soundness of endocrine research.
Quantitative Impact of Lifestyle Factors on Endocrine Outcomes
Key Predictors of Testosterone Levels in Young Adults
Emerging evidence quantifies the specific effects of various lifestyle factors on endocrine parameters. An exploratory cross-sectional study investigating 50 males aged 18-22 years revealed distinct positive and negative correlates of serum testosterone levels, measured via chemiluminescent immunoassay [52].
Table 1: Lifestyle Factors as Predictors of Testosterone Levels
| Lifestyle Factor | Category/Exposure | Regression Coefficient (β) | P-value |
|---|---|---|---|
| Exercise Type | Hypertrophy training | +20.3 | <0.001 |
| Sunlight Exposure | >60 minutes daily | +10.3 | 0.03 |
| Supplement Use | Yes | +20.5 | <0.001 |
| Diet Type | Non-vegetarian | +8.7 | 0.03 |
| Carbonated Beverages | Daily consumption | -10.2 | 0.01 |
| Tobacco Use | Yes | -15.6 | <0.001 |
| Sleep Deprivation | Yes | -18.2 | <0.001 |
This data underscores the multifactorial nature of testosterone regulation and emphasizes that holistic lifestyle interventions—rather than single-factor approaches—are critical for endocrine health in research populations [52].
Interventional Outcomes on Metabolic and Sleep Parameters
Research in populations with endocrine-related conditions like Type 2 Diabetes Mellitus (T2DM) further demonstrates the measurable effects of controlled exercise interventions. A 12-week randomized controlled trial with 100 T2DM patients compared different exercise regimens, revealing distinct outcomes on abdominal fat and sleep quality [53].
Table 2: Effects of 12-Week Exercise Interventions in T2DM Patients
| Outcome Measure | Control Group | Aerobic Exercise (AEX) | Resistance Exercise (REX) | Combined Exercise (COMB) |
|---|---|---|---|---|
| PSQI Score (Sleep Quality) | Minimal improvement | Improved | Improved | Greatest improvement |
| Total Sleep Time | No significant change | No significant change | No significant change | Significantly increased |
| Sleep Efficiency | No significant change | No significant change | No significant change | Significantly improved |
| Visceral Adipose Tissue | No significant change | Reduced | Reduced | Most reduced |
| Wake After Sleep Onset | No significant change | No significant change | No significant change | Significantly reduced |
The combined exercise protocol emerged as the most effective intervention, demonstrating that synergistic approaches yield the most significant improvements in both metabolic and sleep parameters [53].
Experimental Protocols for Lifestyle Factor Control
Protocol for Controlling Biological Variation in Endocrine Studies
Objective: To standardize participant selection and monitoring procedures to minimize biologic variation in endocrine outcome measures.
Participant Selection Criteria:
- Age and Maturation Matching: Participants must be matched by chronologic age or maturation level unless studying age-related changes. Prepubertal, postpubertal, and postmenopausal individuals demonstrate drastically different hormonal responses [2].
- Body Composition Assessment: Match volunteers for adiposity using BMI categorization and additional measures like DXA scans rather than body weight alone. Group normal-weight (BMI <25.0 kg·m²), overweight (BMI ≥25.0 ≤30.0 kg·m²), and obese (BMI >30.0 kg·m²) individuals separately [2].
- Mental Health Screening: Administer validated mental health screening questionnaires (e.g., Beck Depression Inventory, State-Trait Anxiety Inventory) conducted by trained professionals to identify conditions that may alter hypothalamic-pituitary-adrenal axis activity [2].
- Circadian Rhythm Control: Schedule all blood collections consistently between 7:30 AM and 9:00 AM to coincide with known peak testosterone secretion periods in young adult men [52] [2].
Implementation Notes: This protocol requires preliminary screening sessions 2-4 weeks before data collection to properly categorize participants and establish baseline measures.
Protocol for Combined Exercise Intervention in Metabolic Studies
Objective: To implement a standardized 12-week combined exercise regimen that improves endocrine and metabolic parameters while controlling for confounding variables.
Intervention Structure:
- Program Duration: 12 weeks
- Session Frequency: 3 times per week
- Session Duration: 60-90 minutes, including 15 minutes of warm-up and cool-down
- Exercise Composition: Combination of aerobic exercise (Tai Chi) and resistance training (elastic band exercises)
- Energy Expenditure Standardization: 41.8 kilojoules (kcal) per kg body weight per week allocated to aerobic exercise component [53]
Exercise Prescription Details:
- Aerobic Component: Tai Chi sessions focused on continuous movement, balance, and controlled breathing
- Resistance Component: Elastic band training exercises including chest clamps, deep squat push-ups, and standing lateral flexion
- Intensity Monitoring: Maintain exercise intensity at level 3-5 on the Borg Physical Exertion Scale to standardize perceived exertion across participants [53]
- Supervision Requirements: All sessions supervised by qualified exercise physiologists to ensure proper form and adherence to protocol
Outcome Assessment: Measure visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT) via magnetic resonance imaging at the L4-L5 disc plane, analyzed using Slice Omatic 5.0 software. Assess sleep quality using both objective (sleep monitoring bracelets) and subjective (Pittsburgh Sleep Quality Index) measures [53].
Dietary Control and Assessment Protocol
Objective: To categorize and monitor dietary patterns that influence endocrine parameters while controlling for nutritional confounders.
Dietary Categorization Framework:
- Lacto-Vegan (Vegetarian): Excludes all animal products except dairy
- Eggetarian: Vegetarian diet incorporating eggs and egg products
- Non-Vegetarian: Includes all animal products [52]
Dietary Monitoring Procedures:
- Data Collection: Use previously validated food frequency questionnaires or 24-hour dietary recalls
- Timing Controls: Prohibit food and caffeine consumption for at least 3 hours before blood collection to minimize acute metabolic effects
- Carbonated Beverage Tracking: Record frequency of carbonated beverage consumption as a separate variable due to its significant negative correlation with testosterone levels (β=-10.2, p=0.01) [52]
Implementation Notes: While categorization provides general trends, future studies should collect nutrient-level data (zinc, vitamin D, omega-3) to elucidate mechanistic pathways.
Visual Experimental Workflows
Endocrine Research Lifestyle Control Workflow
Exercise Intervention Decision Pathway
The Researcher's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Materials for Endocrine Lifestyle Studies
| Category | Item/Reagent | Specification/Application | Key Function |
|---|---|---|---|
| Hormone Assessment | Chemiluminescent Immunoassay (CLIA) System | Roche Diagnostics; sensitivity 0.1 ng/dL | Quantification of serum testosterone levels [52] |
| Body Composition | Magnetic Resonance Imaging (MRI) | 1.5T HDxt system with standard array coil | Measurement of visceral (VAT) and subcutaneous (SAT) adipose tissue [53] |
| Body Composition | Dual-energy X-ray Absorptiometry (DXA) | Discovery W Bone Densitometer (Hologic) | Assessment of whole-body lean body mass (LBM) [53] |
| Sleep Monitoring | Pittsburgh Sleep Quality Index (PSQI) | Chinese version (C-PSQI, Cronbach's α=0.77) | Subjective sleep quality assessment across 7 domains [53] |
| Sleep Monitoring | Sleep Monitoring Bracelet | Validated wearable technology | Objective measurement of sleep duration and efficiency [53] |
| Exercise Monitoring | Borg Physical Exertion Scale | 10-point rating system (3-5 for moderate intensity) | Standardization of exercise intensity across participants [53] |
| Statistical Analysis | Python & R Packages | Statsmodels, pandas, numpy, car, ggplot2, psych, lmtest | Multiple regression analysis with VIF assessment for multicollinearity [52] |
Controlling for diet, exercise, and sleep factors is not merely a methodological consideration but a fundamental requirement for valid endocrine research. The protocols outlined herein provide researchers with standardized approaches to minimize biological variance and enhance the reliability of endocrine outcome measures. By implementing these detailed methodologies—including participant selection criteria, intervention protocols, and assessment techniques—researchers can significantly improve the scientific quality of their investigations into endocrine function and its relationship with modifiable lifestyle factors. Future studies should continue to refine these protocols, particularly through the inclusion of nutrient-level dietary assessments and the development of standardized composite lifestyle scores that can better capture the synergistic effects of these interconnected factors on endocrine health.
Identifying and Mitigating Common Pitfalls in Endocrine Studies
Managing Circadian and Pulsatile Hormone Secretion
The accurate assessment of endocrine function is fundamental to both physiological research and clinical diagnostics. Hormonal secretion is governed by two principal temporal patterns: circadian rhythms, which are approximately 24-hour cycles driven by an internal biological clock, and pulsatile secretion, characterized by brief, recurrent secretory bursts. These patterns are not merely incidental; they are essential for normal physiology, and their disruption is implicated in a wide range of pathologies [54] [55]. A comprehensive understanding and rigorous assessment of these dynamics are often complicated by numerous methodological factors. These factors can be categorized as biologic variation, stemming from the physiologic status of the subject, and procedural-analytic variation, introduced by the investigator's choices and technical procedures [2]. This document outlines key analytical frameworks, assessment protocols, and essential methodological considerations for managing the complexities of circadian and pulsatile hormone secretion in a research setting.
Analytical Frameworks for Hormone Secretion Dynamics
The Circadian System and its Outputs
The mammalian circadian system is organized in a hierarchical manner. The master pacemaker, located in the suprachiasmatic nucleus (SCN) of the hypothalamus, synchronizes peripheral clocks in virtually every cell and tissue throughout the body [56] [57]. This synchronization occurs via neuronal and endocrine pathways, ensuring that local physiological processes are aligned with the external environment [56]. The molecular clock within cells is driven by a network of clock genes, including Bmal1, Clock, Per, and Cry, which engage in transcription-translation feedback loops to generate ~24-hour rhythmicity [56].
Hormones serve as crucial signaling molecules for this system. They can act in three primary ways to regulate circadian rhythms in target tissues [57]:
- Rhythm Drivers: The hormone itself is rhythmic and directly drives rhythmic gene expression in target tissues via hormone-specific response elements (e.g., glucocorticoids acting through glucocorticoid response elements, GREs).
- Zeitgebers: The rhythmic hormone signal can reset or entrain the phase of peripheral clocks (e.g., melatonin acting on the SCN, glucocorticoids affecting Per gene expression).
- Tuners: A largely arrhythmic hormonal signal can be interpreted rhythmically by the target tissue, thereby modifying the amplitude or phase of tissue output rhythms without directly affecting the core clock (e.g., as proposed for thyroid hormones in the liver).
Table 1: Key Hormones with Prominent Circadian and Pulsatile Characteristics
| Hormone | Circadian Pattern | Pulsatile Pattern | Primary Regulatory Role |
|---|---|---|---|
| Cortisol | Peak at awakening (circadian); Cortisol Awakening Response (CAR) [57] | ~90-minute ultradian pulses [57] | Metabolism, immune function, stress response |
| Melatonin | High during night, low during day [57] | -- | Sleep-wake cycle regulation, SCN zeitgeber |
| Luteinizing Hormone (LH) | Diurnal variation [55] | Circhoral (~hourly) pulses [55] [58] | Reproductive axis regulation |
| Growth Hormone (GH) | Major secretory pulse at sleep onset [57] | Volleys of pulses every 35-60 min [55] | Growth, metabolism |
| Insulin | Influenced by meal timing [57] | Rapid pulses every 4-7 min [55] | Glucose homeostasis |
The following diagram illustrates the core molecular feedback loops of the circadian clock and its systemic regulation.
Diagram 1: Circadian System Architecture. The core molecular clock (center) consists of interlocking transcription-translation feedback loops. The SCN (Suprachiasmatic Nucleus) acts as the master pacemaker, synchronizing peripheral clocks via neural, endocrine (e.g., melatonin, cortisol), and behavioral outputs. HPA: Hypothalamic-Pituitary-Adrenal.
Quantifying Pulsatile Secretion
Pulsatile secretion is a fundamental property of many hormones, including LH, GH, ACTH, and insulin [55]. Analytical goals include quantifying the number, size, shape, and uniformity of pulses, as well as distinguishing pulsatile from basal (non-pulsatile) secretion and modeling elimination kinetics [55]. The following diagram outlines a generalized workflow for assessing pulsatile hormone secretion.
Diagram 2: Workflow for Pulsatile Hormone Analysis. The process involves intensive blood sampling, sensitive hormone measurement, and computational analysis to reconstruct underlying secretory events.
Several computational methods have been developed to analyze these complex time-series data:
- Deconvolution Analysis: This is a gold-standard method that mathematically separates the measured hormone concentration-time series into its underlying secretion and elimination components [55] [58]. It provides estimates of secretory-burst mass, waveform, basal secretion, and hormone half-life.
- Approximate Entropy (ApEn): A model-free statistic used to quantify the regularity or orderliness of hormone release. More irregular patterns have higher ApEn and are associated with various pathophysiological states [55].
- Bayesian Frameworks: Newer approaches, such as the HormoneBayes framework, utilize Bayesian statistics and Monte-Carlo methods to infer key parameters like inter-pulse interval, secretion rate, and clearance rate, while also providing a quantification of estimation uncertainty [59].
Table 2: Comparison of Computational Methods for Pulse Analysis
| Method | Primary Approach | Key Outputs | Advantages | Limitations |
|---|---|---|---|---|
| Deconvolution Analysis [55] [58] | Mathematically resolves secretion and elimination from concentration data. | Pulse times, secretory-burst mass and waveform, basal secretion, half-life. | Considered the gold standard; provides detailed secretory parameters. | Requires assumptions about elimination kinetics; complex implementation. |
| Approximate Entropy (ApEn) [55] | Model-free measure of pattern regularity. | Single unitless statistic; higher ApEn = greater irregularity. | Useful for quantifying system feedback and control without a specific model. | Does not provide specific pulse characteristics (mass, frequency). |
| HormoneBayes [59] | Bayesian inference of a stochastic model of pulsatile dynamics. | Posterior distributions for IPI, secretion/clearance rates, latent signal. | Quantifies uncertainty; open-access graphical interface. | Requires prior knowledge for parameter priors; newer, less established method. |
| Threshold Methods [55] | Identifies peaks exceeding a threshold based on assay variance. | Pulse frequency, amplitude. | Simple, intuitive. | Does not account for hormone clearance; can miss broader pulses. |
Critical Methodologic Factors Influencing Endocrine Measurements
Research design must account for numerous factors that contribute to variance in hormonal outcomes. Failure to control these can lead to inconsistent and uninterpretable data [2].
Biologic Factors (Endogenous)
These factors are intrinsic to the research participant and must be carefully documented and controlled.
- Sex and Age: Post-pubertal males and females exhibit significant differences in sex steroid and leptin profiles. Age impacts hormonal levels, such as the decline of GH and testosterone with aging and increased insulin resistance during puberty [2].
- Menstrual Cycle: In eumenorrheic females, phases of the menstrual cycle (follicular, ovulation, luteal) cause large, dramatic fluctuations in reproductive hormones (e.g., estradiol, progesterone, LH), which can also influence other non-reproductive hormones [2]. Testing should be standardized to a specific cycle phase or account for this variation.
- Circadian and Ultradian Rhythms: Hormone levels fluctuate profoundly throughout the day and night. Single time-point measurements can be highly misleading. Sampling time must be strictly controlled and reported [2] [57].
- Body Composition: Adiposity levels influence cytokines (e.g., leptin, interleukin-6) and hormones like insulin and cortisol. Grouping normal-weight, overweight, and obese individuals can confound outcomes [2].
- Mental Health: Conditions like high anxiety or depression can alter basal levels of catecholamines, ACTH, and cortisol, thereby modifying the hormonal response to experimental stimuli [2].
Procedural-Analytic Factors (Exogenous)
These factors are determined by the investigator and must be standardized across a study.
- Blood Sampling Protocol: The frequency and duration of sampling are critical. Capturing rapid insulin pulses requires 1-5 minute sampling, while LH pulses can be assessed with 10-minute sampling. Longer sampling durations are needed to accurately determine pulse frequency [55] [59].
- Assay Sensitivity and Specificity: The assay must be sensitive enough to detect hormone levels at the physiological range, including at nadir concentrations. Cross-reactivity with other hormones must be minimal to ensure accurate measurement [2] [58].
- Sample Type and Handling: Whether serum, plasma, or whole blood is used, along with processing time, storage temperature, and freeze-thaw cycles, can affect hormone stability and must be consistent [2] [58].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Hormone Secretion Studies
| Item | Specific Example(s) | Function/Application |
|---|---|---|
| High-Sensitivity Immunoassays | ELISA [58], RIA [58], Chemiluminescent Immunoassay (CLIA) [59] | Quantification of hormone concentrations in blood/serum/plasma samples. Sensitivity is paramount for detecting nadir levels. |
| Capture & Detection Antibodies | Monoclonal anti-bovine LHβ (518B7); Polyclonal rabbit LH antiserum (AFP240580Rb) [58] | Form the core of sandwich immunoassays. High specificity is required to avoid cross-reactivity with similar hormones (e.g., FSH, TSH). |
| Reference Preparations (Standards) | Mouse LH (AFP-5306A) from NIDDK-NHPP [58] | Calibrate assays and generate standard curves for accurate interpolation of unknown sample concentrations. |
| Cell Lines for In Vitro Studies | H295R adrenocortical cell line [60] | Model for studying cell-autonomous circadian clock properties and hormone regulation in adrenal cells. |
| Deconvolution Software | MATLAB-based algorithms [58], HormoneBayes graphical interface [59] | Computational tools to analyze pulsatile hormone data and estimate secretion and elimination parameters. |
| Frequent Blood Sampling Kit | Customized protocols for small-volume serial sampling in mice [58] | Enables high-resolution hormone profiling in small animal models without the need for fluid replacement. |
Detailed Experimental Protocols
Protocol for Assessing Pulsatile LH Secretion in a Mouse Model
This protocol, adapted from a 2013 study, details a method for high-resolution LH profiling in mice [58].
Application: To characterize the pulsatile pattern of Luteinizing Hormone (LH) secretion in pre-pubertal and adult mice, revealing changes across development and in genetic knockout models.
Materials and Reagents:
- Animals: Wild-type C57BL/6 mice and relevant genetic models (e.g., Gpr54 KO).
- LH Sandwich ELISA Reagents:
- Coating Buffer: 1x PBS.
- Capture Antibody: Monoclonal anti-bovine LHβ subunit (e.g., 518B7), diluted 1:1000.
- Blocking Buffer: 5% (w/v) skim milk powder in 1x PBS-T.
- LH Standard: Mouse LH reference preparation (e.g., AFP-5306A from NIDDK-NHPP), serially diluted in 0.2% BSA–1x PBS-T.
- Detection Antibody: Polyclonal rabbit LH antiserum (e.g., AFP240580Rb), diluted 1:10,000.
- Secondary Antibody: Horseradish peroxidase (HRP)-conjugated goat anti-rabbit IgG, diluted 1:2000.
- Substrate: o-phenylenediamine (OPD) with 0.1% H₂O₂.
- Stop Solution: 3 M HCl.
- Equipment: Frequent blood sampling setup, high-affinity binding 96-well microplates, plate reader.
Procedure:
- Animal Preparation and Sampling: House mice under a standardized 12-hour light/12-hour dark cycle. For sampling, use a validated frequent blood collection procedure (e.g., sampling every 5-10 minutes for 360 minutes) from a suitable vessel without volume replacement [58].
- Sample Collection: Collect small-volume whole blood fractions (e.g., 2 μL) into heparinized tubes. Centrifuge briefly if plasma is required, or use whole blood directly if validated.
- ELISA Execution:
- Coating: Coat wells with 50 μL of capture antibody overnight at 4°C.
- Blocking: Wash plates, then add 200 μL blocking buffer per well for 2 hours at room temperature (RT).
- Incubation with Samples/Standard: Add 50 μL of LH standards and unknown blood samples to wells. Simultaneously add 50 μL of detection antibody to each well. Incubate for 1.5 hours at RT.
- Incubation with Secondary Antibody: Wash plates. Add 50 μL of HRP-conjugated secondary antibody to each well. Incubate for 1.5 hours at RT.
- Detection: Wash plates. Add 100 μL of OPD substrate solution to each well. Incubate in the dark for 30 minutes at RT.
- Stop and Read: Add 50 μL of 3 M HCl to stop the reaction. Read the absorbance immediately at 490 nm.
- Data Analysis:
- Concentration Interpolation: Calculate LH concentrations in unknowns by interpolating OD values against the non-linear regression of the LH standard curve.
- Pulse Analysis with Deconvolution: Analyze the LH concentration-time series using a validated deconvolution algorithm (e.g., a MATLAB-based method) [58]. This will detrend the data, identify pulse times, and simultaneously estimate parameters such as:
- Basal secretion (
β0) - Secretory-burst mass (
η0, η1) - Secretory-burst waveform (
β1, β2, β3) - Slow half-life of LH
- Basal secretion (
- Regularity Analysis: Calculate the Approximate Entropy (ApEn) of the LH profile to quantify pattern regularity [55].
Methodological Notes:
- Assay Validation: It is critical to fully validate the ELISA for use with whole blood, including tests for spike recovery, linearity of dilution, and intra- and inter-assay precision [58].
- Control Groups: Include age- and sex-matched wild-type controls, especially when using genetic models. For developmental studies, perform longitudinal assessments in the same animals where possible.
Protocol for Human Circadian Rhythm Biomarker Assessment
Application: To evaluate the integrity of the circadian system in human subjects by measuring key circadian biomarker rhythms for research on sleep disorders, shift work, or metabolic disease.
Materials and Reagents:
- Hormone Assays: Validated commercial immunoassays for Melatonin and Cortisol.
- Collection Tubes: Appropriate tubes for serum or plasma separation (e.g., EDTA for plasma cortisol).
- Saliva Collection Kits (if using salivary cortisol).
- Actigraphy Monitors.
- Core Body Temperature Sensors (if applicable).
Procedure:
- Subject Preparation and Standardization: Instruct participants to maintain a regular sleep-wake schedule (e.g., 11 pm - 7 am) for at least one week prior to the study. Verify compliance using actigraphy or sleep diaries. On the test day, control light exposure, meal timing, and physical activity.
- Biomarker Sampling:
- Dim-Light Melatonin Onset (DLMO): Place subjects in dim light (<10 lux) starting in the early evening (e.g., 6 pm). Collect blood or saliva samples every 30-60 minutes from, for example, 7 pm until 11 pm. The DLMO is defined as the time when melatonin concentration consistently exceeds a threshold (e.g., 3 or 4 pg/mL in saliva) [54] [57].
- Cortisol Awakening Response (CAR): Provide subjects with saliva collection kits and detailed instructions. Upon waking, subjects collect saliva immediately (S1), then at 30 minutes (S2), 45 minutes (S3), and 60 minutes (S4) post-awakening. Record exact wake and sampling times. This captures the characteristic sharp rise in cortisol upon awakening [57].
- Data Analysis:
- DLMO Calculation: Plot melatonin concentration against clock time. The DLMO is the interpolated time at which the rising melatonin curve crosses the predefined threshold.
- CAR Analysis: Calculate the area under the curve (AUC) with respect to ground (AUCG) and with respect to increase (AUCI) for the four samples to capture the total cortisol output and the dynamic change, respectively.
- Actigraphy Analysis: Analyze actigraphy data to determine sleep onset, offset, and fragmentation indices, which serve as behavioral correlates of circadian phase and amplitude.
Methodological Notes:
- Control of Confounders: Strictly control for the biologic factors outlined in Section 3.1, including age, sex, menstrual cycle phase, and mental health status. For the CAR, subjects must not eat, drink (except water), or smoke between samples.
- Assay Consistency: Use the same validated assay for all samples within a study to minimize procedural-analytic variance.
Addressing the Impact of Endocrine-Disrupting Chemicals (EDCs)
Endocrine-disrupting chemicals (EDCs) represent a class of exogenous substances that interfere with the normal function of the endocrine system, potentially causing adverse health effects in intact organisms or their progeny [61] [62]. The global production of chemical products has increased dramatically in recent decades, leading to widespread environmental contamination and human exposure through various routes including ingestion, inhalation, and dermal contact [63] [62]. EDCs encompass diverse chemical structures including phthalates, bisphenol A (BPA), per- and polyfluoroalkyl substances (PFAS), pesticides, heavy metals, and industrial chemicals used in petroleum manufacturing [61] [64] [62].
The concern regarding EDCs stems from their capacity to mimic or block natural hormones, alter hormone synthesis and metabolism, and modify hormone receptor expression even at very low concentrations [61] [62]. Recent umbrella reviews evaluating numerous meta-analyses have identified significant harmful associations between EDC exposure and 22 cancer outcomes, 21 neonatal/infant/child-related outcomes, 18 metabolic disorder outcomes, 17 cardiovascular disease outcomes, and multiple other health conditions [64]. Given the widespread presence of these pollutants and their potential health impacts, robust methodological approaches for their detection and characterization are essential for both environmental monitoring and public health protection.
Analytical Methodologies for EDC Detection
Advanced Instrumentation Approaches
The analysis of EDCs presents significant challenges due to their occurrence at trace-level concentrations in complex environmental and biological matrices. Mass spectrometry coupled with chromatography has emerged as the dominant analytical technique for EDC determination, providing the necessary sensitivity and selectivity for reliable quantification [65] [63].
Table 1: Analytical Techniques for EDC Determination
| Technique | Applications | Sensitivity | Key Advantages |
|---|---|---|---|
| GC-MS | Analysis of non-polar EDCs [65] | High (ng·L⁻¹) | Excellent for volatile and semi-volatile compounds |
| LC-MS/MS | Analysis of more polar EDCs; PFAS and phthalates [65] [62] | Very High (ng·L⁻¹ to pg·L⁻¹) | Broad applicability; does not require derivatization |
| QqQ-MS | Complex matrices; operated in SRM mode [63] | High | Improved selectivity and unequivocal identification |
| Qq-TOF-MS | Structural elucidation of unknowns; identification of target compounds [63] | High | Accurate mass of product ions |
| ICP-MS | Metal EDCs (arsenic, lead) [62] | Very High | Specific for elemental analysis |
Recent advances in sample preparation have focused on reducing solvent use, time, and cost while maintaining analytical performance [65]. The choice between GC-MS and LC-MS/MS primarily depends on the polarity of the target EDCs, with GC-MS being preferred for non-polar compounds and LC-MS/MS for more polar substances [65]. The development of high-throughput analysis using monolithic columns, high-temperature liquid chromatography, and ultra-high-pressure liquid chromatography with sub-2-micron particles has significantly reduced analytical run times without compromising resolution and separation efficiency [63].
Emerging Sensing Technologies
While conventional instrumentation provides excellent sensitivity, there is growing interest in portable sensing technologies for field-deployable EDC monitoring. These advanced sensing systems offer rapid, portable, and eco-friendly alternatives to traditional laboratory-based methods [62].
Table 2: Emerging Sensor Technologies for EDC Detection
| Sensor Type | Detection Principle | Target EDCs | Key Features |
|---|---|---|---|
| Electrochemical | Redox reactions at electrode surfaces | Various EDCs | Portable, low cost, rapid results |
| Optical | Light-matter interaction | BPA, pesticides | High sensitivity, real-time monitoring |
| Aptamer-based | Molecular recognition | Specific EDC classes | High specificity, tunable recognition |
| Microbial | Whole-cell biosensors | Broad-spectrum | Biological relevance, functional assessment |
Sensor technologies represent a complementary approach to traditional analytical methods, particularly useful for rapid screening and onsite monitoring applications where laboratory instrumentation is not accessible or practical [62].
Methodological Framework for EDC Testing and Assessment
OECD Conceptual Framework
The Organisation for Economic Co-operation and Development (OECD) has established a comprehensive conceptual framework for the testing and assessment of endocrine disruptors, providing standardized methodologies for hazard identification and characterization [66]. This framework employs a tiered approach that progresses from initial screening to comprehensive in vivo studies.
In Vitro Screening Assays
Level 2 of the OECD framework encompasses in vitro assays designed to identify endocrine mechanism(s) and pathway(s). Key standardized test guidelines include:
- Estrogen Receptor Transactivation Assay (OECD TG 455): Detects chemicals acting as agonists or antagonists of the estrogen receptor
- Androgen Receptor Transactivation Assay (OECD TG 458): Identifies chemicals that interact with the androgen receptor
- Steroidogenesis Assay (OECD TG 456): Detects chemicals that disrupt steroid hormone synthesis
- Aromatase Assay (US EPA TG OPPTS 890.1200): Measures inhibition of aromatase enzyme activity
These in vitro assays provide crucial mechanistic data while reducing animal use and allowing higher throughput screening of potential endocrine activity [66].
Experimental Protocol: Estrogen Receptor Activity Assessment
Ishikawa Cell-Based Gene Expression Assay
This protocol evaluates the estrogenic activity of test chemicals using ER-positive immortalized human uterine Ishikawa cells, measuring changes in endogenous gene expression of estrogen-responsive markers [61].
Materials and Reagents
Table 3: Research Reagent Solutions for ER Activity Assessment
| Reagent/Material | Specifications | Function | Supplier Example |
|---|---|---|---|
| Ishikawa Cells | ER-positive, immortalized human uterine cell line | Model system for uterine endocrine responses | ATCC/Commercial |
| RPMI-1640 Medium | Phenol red-free | Cell culture base medium | Gibco/Thermo Fisher |
| Charcoal-Dextran Treated FBS | Steroid-stripped | Removes endogenous hormones | Gemini Bio-Products |
| Test Chemicals | ≥97-99% purity | EDCs for evaluation | Sigma-Aldrich |
| 17β-Estradiol (E2) | ≥98% pure | Positive control | Sigma-Aldrich |
| TRIzol Reagent | - | RNA isolation | Invitrogen |
| TaqMan PCR Probes | Specific for PGR, NPPC, GREB1 | Gene expression quantification | Applied Biosystems |
Step-by-Step Procedure
Day 1: Cell Seeding
- Culture Ishikawa cells in RPMI-1640 medium supplemented with 10% charcoal-dextran treated FBS under standard conditions (37°C, 5% CO₂).
- At 70-80% confluence, detach cells using trypsin-EDTA and prepare single-cell suspension.
- Seed cells in 6-well plates at a density of 2.5 × 10⁵ cells/well in steroid-stripped medium.
- Incubate for 24 hours to allow cell attachment and equilibration.
Day 2: Chemical Treatment
- Prepare fresh treatment solutions in steroid-stripped medium:
- Vehicle control (0.1% DMSO or ethanol)
- Positive control (10 nM 17β-estradiol)
- Test chemicals at concentrations below reported toxicity limits (e.g., 0.1-10 μM)
- Combination treatments for additive effect assessment
- Replace medium with treatment solutions in triplicate wells.
- Incubate cells for 24 hours under standard conditions.
Day 3: RNA Isolation and Analysis
- Aspirate treatment media and wash cells with cold PBS.
- Extract total RNA using TRIzol reagent according to manufacturer's protocol.
- Quantify RNA concentration and purity using spectrophotometry.
- Reverse transcribe 1 μg RNA to cDNA using high-capacity cDNA reverse transcription kit.
- Perform quantitative real-time PCR using TaqMan probes for estrogen-responsive genes (PGR, NPPC, GREB1) and housekeeping genes.
- Analyze data using the 2^(-ΔΔCt) method to calculate fold changes in gene expression.
Data Interpretation
- Estrogenic Agonists: Significant induction of PGR, NPPC, and GREB1 expression similar to 17β-estradiol
- Estrogenic Antagonists: Significant repression of basal expression or inhibition of 17β-estradiol-mediated induction
- Non-Estrogenic: No significant effect on gene expression patterns
This protocol successfully identified 2,6-di-tert-butyl-p-cresol (BHT) and diethanolamine (DEA) as repressors of estrogen-responsive genes, while tetrachloroethylene (PCE) and 2,2'-methyliminodiethanol (MDEA) induced these genes, demonstrating previously unappreciated endocrine disrupting effects [61].
Molecular Docking Analysis
To complement experimental findings, computational molecular docking can be performed to visualize potential binding interactions between EDCs and the ligand binding domain of ERα [61].
Methodologic Factors in Endocrine Measurements
Accurate assessment of endocrine disruption requires careful control of methodological factors that can introduce variance and compromise data validity. These factors can be categorized as biologic and procedural-analytic sources of variation [2].
Biological Factors Influencing Endocrine Measurements
Table 4: Biological Factors Affecting Endocrine Measurements
| Factor | Impact on Hormonal Measurements | Methodological Control Recommendations |
|---|---|---|
| Sex | Post-puberty hormonal profiles differ significantly; sex-specific exercise responses [2] | Match participant sex or analyze separately; account for hormonal status |
| Age | Pre/post-pubertal differences; menopausal/andropausal changes [2] | Match participants by chronological age or maturation level |
| Menstrual Cycle | Large fluctuations in reproductive hormones across phases [2] | Test females in similar menstrual phases; document oral contraceptive use |
| Circadian Rhythms | Diurnal variations in many hormones [2] | Standardize sampling times across experimental conditions |
| Body Composition | Adiposity influences cytokines and hormones; obesity alters exercise responses [2] | Match for adiposity rather than just body weight; use BMI categories |
| Mental Health | Anxiety and depression alter hypothalamic-pituitary-adrenal axis activity [2] | Implement mental health screening with qualified professionals |
Procedural-Analytic Considerations
Procedural factors determined by investigators can significantly influence hormonal measurement outcomes and must be carefully controlled [2] [67]:
- Pre-testing Conditions: Standardize environmental temperature, relative humidity, and control intake of alcohol, caffeine, nicotine, and medications
- Sleep and Nutrition: Control for sleep deprivation, prandial state, and previous exercise
- Specimen Collection: Minimize tourniquet-induced stasis effects and control for postural changes affecting plasma volume
- Sample Processing: Standardize specimen selection (plasma, serum, urine), collection protocols, storage conditions, and analysis procedures
- Analytical Variation: Monitor both analytical and biological variation, including magnitude of hemolysis when relevant
Exercise-related hormone evaluations require additional controls for exercise intensity, duration, mode, frequency, volume, and training status of participants, as each of these variables can specifically affect endocrine responses [67].
Computational Approaches for EDC Identification
Advanced computational methods are increasingly valuable for predicting endocrine disruption potential, especially for the large number of chemicals in commercial use without adequate safety testing.
Machine Learning-Based Toxic Alert Identification
Recent research has applied explainable machine learning algorithms to identify specific chemical substructures ("toxic alerts") associated with endocrine disruption across multiple nuclear receptors [68].
Protocol: Toxic Alert Identification Using LIME
- Data Curation: Collect and curate large chemical datasets (TOX21, EDC, EDKB-FDA) with known endocrine activity
- Feature Engineering: Generate extended-connectivity fingerprints (ECFPs) for molecular characterization
- Model Training: Implement random forest classifiers with hyperparameter optimization using cross-validation
- Model Interpretation: Apply Local Interpretable Model-agnostic Explanations (LIME) to identify substructures driving predictions
- Validation: Statistically analyze substructure weights and map to visual representations
This approach has identified specific substructures including thiophosphate, sulfamate, anilide, carbamate, sulfamide, and thiocyanate as toxic alerts for endocrine disruption across multiple receptor targets (androgen receptor, estrogen receptor, aryl hydrocarbon receptors, aromatase receptors, and peroxisome proliferator-activated receptors) [68].
The methodological approaches outlined in this document provide a comprehensive framework for addressing the impact of endocrine-disrupting chemicals through advanced analytical techniques, standardized testing protocols, and computational predictions. The integration of these methodologies enables researchers to better characterize EDC hazards, understand mechanisms of action, and prioritize chemicals for further investigation.
Future directions in EDC research include the development of high-throughput screening methods, advanced sensor technologies for environmental monitoring [62], non-targeted analysis to expand the number of EDCs monitored [65], and improved understanding of low-dose mixture effects [61]. Additionally, there is growing recognition of the need to address knowledge gaps in public understanding of EDC exposure routes and regulatory limitations [69].
By implementing robust methodological approaches and controlling for key factors influencing endocrine measurements, researchers can generate more reliable, reproducible data to support evidence-based decision-making for chemical regulation and public health protection.
Incorporating endocrinologic measurements into research on special populations requires meticulous methodological control to ensure data validity and reliability. Numerous biologic and procedural-analytic factors introduce variance into hormonal outcomes, potentially compromising research accuracy [2]. This document provides detailed application notes and experimental protocols for conducting rigorous endocrine research within pediatric, elderly, and athletic populations, framed within the context of a broader thesis on methodological factors influencing endocrine measurements. The recommendations address population-specific physiological characteristics, confounding variables, and standardized assessment techniques to optimize protocol design for these distinct groups.
Methodologic Factors Influencing Endocrine Measurements
Endocrine research is particularly susceptible to methodological variance arising from both biologic (participant-derived) and procedural-analytic (investigator-derived) factors. The table below summarizes key considerations that researchers must address during study design.
Table 1: Key Methodologic Factors Influencing Endocrine Measurements in Special Populations
| Factor Category | Specific Consideration | Impact on Endocrine Measurements | Population-Specific Concerns |
|---|---|---|---|
| Biologic Factors | Sex Differences | Post-puberty hormonal profiles diverge significantly; females exhibit menstrual cycle pulsatility [2]. | Athletes: training response variations; Pediatrics: maturation timing |
| Age & Maturation | Prepubertal/postpubertal differences; age-related hormonal declines (e.g., GH, testosterone) [2]. | Elderly: hormonal senescence; Pediatrics: pubertal staging | |
| Body Composition | Adiposity influences cytokines (leptin, IL-6) and hormones (insulin, cortisol) [2]. | All populations: obesity comorbidities; Athletes: lean mass focus | |
| Circadian Rhythms | Hormonal levels exhibit diurnal fluctuations (e.g., cortisol) [2]. | All populations: standardized timing critical | |
| Menstrual Cycle | Cycle phase dramatically affects reproductive hormones and interacting systems [2]. | Female athletes: oral contraceptive considerations | |
| Procedural-Analytic Factors | Dehydration Assessment | Single-method assessment is unreliable; requires multi-modal approach [70]. | Athletes: exercise-induced fluid shifts |
| Hydration Terminology | Must distinguish between "dehydration" (water deficit) and "underhydration" (low intake) [70]. | Research clarity: hypertonic vs. isotonic dehydration | |
| Intrinsic Capacity Tracking | Comprehensive monitoring of physical/mental capacities in aging populations [71]. | Elderly: functional status connection to endocrine health |
Population-Specific Protocols and Application Notes
Pediatric Population Protocols
Key Methodological Considerations: Pediatric endocrine research must account for rapid developmental changes, puberty progression, and age-appropriate assessment techniques. Researchers should match participants by both chronologic age and maturation level (Tanner staging) to reduce interindividual variability [2]. The dynamic nature of hormonal systems during growth necessitates longitudinal designs with careful attention to minimal risk procedures.
Experimental Protocol: Assessing Pubertal Development and Endocrine Function
Participant Recruitment and Screening:
- Inclusion Criteria: Clearly define age ranges (e.g., 6-18 years) and pubertal status (prepubertal, peripubertal, postpubertal) based on Tanner stages assessed by trained clinicians.
- Exclusion Criteria: Chronic diseases affecting growth, endocrine disorders, medications influencing hormonal axes, and mental health conditions that could confound measures (assessed via standardized screening tools) [2].
Baseline Assessments:
- Anthropometrics: Measure height, weight, BMI, and body composition via DEXA or bioelectrical impedance. Calculate BMI Z-scores using age- and sex-specific references [2].
- Pubertal Staging: Document Tanner stages for breast/genitalia and pubic hair development.
- Maturation Assessment: Obtain bone age radiographs (left hand and wrist) for precise biological age determination.
Biological Sampling Protocol:
- Timing: Standardize blood draw times to control for circadian rhythms. For longitudinal studies, conduct follow-up assessments at the same time of day as baseline.
- Procedure: Collect blood samples for relevant hormones (e.g., LH, FSH, estradiol, testosterone, IGF-1, cortisol). Consider less-invasive methods (saliva, urine) where validated for pediatric use.
- Pre-analytical Processing: Follow strict protocols for sample handling: immediate centrifugation, proper aliquotting, and storage at -80°C to maintain hormone integrity.
Data Analysis:
- Stratify analyses by pubertal status and biological age (bone age) rather than chronological age alone.
- Use appropriate statistical models (e.g., mixed-effects models) to account for repeated measures and varying maturation trajectories.
Elderly Population Protocols
Key Methodological Considerations: Research involving elderly populations must address age-related hormonal changes (e.g., growth hormone and testosterone decrease, cortisol and insulin resistance increase), multimorbidity, polypharmacy, and functional status [2] [71]. The World Health Organization's Intrinsic Capacity (IC) framework provides a comprehensive approach to capturing the multidimensional health of older adults, encompassing locomotion, vitality, cognition, psychological, and sensory domains [71].
Experimental Protocol: Evaluating Endocrine Function with Intrinsic Capacity Assessment
Participant Characterization:
- Comprehensive Health Assessment: Document all comorbidities, medications, and cognitive status (using Mini-Mental State Examination or Montreal Cognitive Assessment).
- Intrinsic Capacity Evaluation: Assess all IC domains:
- Locomotion: Gait speed, chair rise test
- Vitality: Nutritional status (Mini Nutritional Assessment), fatigue scales
- Cognition: Memory, executive function tests
- Psychological: Geriatric Depression Scale, anxiety inventories
- Sensory: Visual acuity, hearing tests [71]
Biological Sampling Protocol:
- Timing and Control: Account for altered circadian rhythms in older adults. Strictly document medication timing as many drugs affect endocrine parameters.
- Hormonal Panels: Target hormones relevant to aging: cortisol, DHEA-S, testosterone, estradiol, IGF-1, thyroid hormones, and vitamin D.
- Special Handling: Some age-related hormones may require specialized stabilization techniques; follow assay-specific guidelines.
Longitudinal Trajectory Analysis:
- Implement Group-Based Trajectory Modeling (GBTM) to identify distinct patterns of IC and endocrine change over time [71].
- Collect data at multiple time points (minimum 3) to adequately model trajectories.
Data Interpretation:
- Control for confounding factors like inflammation (measure CRP, IL-6) and body composition changes (sarcopenia).
- Analyze associations between hormonal changes and specific IC domain trajectories.
Table 2: Intrinsic Capacity Domains and Assessment Methods for Elderly Research
| IC Domain | Key Components | Recommended Assessment Tools | Endocrine Correlations |
|---|---|---|---|
| Locomotion | Mobility, balance, strength | Gait speed, grip strength, SPPB | Cortisol, Vitamin D, Testosterone |
| Vitality | Energy metabolism, nutrition | MNA, fatigue scales, body composition | Thyroid hormones, IGF-1, Leptin |
| Cognition | Memory, executive function | MoCA, MMSE | Cortisol, Thyroid hormones, Estradiol |
| Psychological | Mood, motivational state | GDS, anxiety inventories | Cortisol, Serotonin metabolites |
| Sensory | Vision, hearing | Visual acuity, audiometry | Cortisol (stress response) |
Athletic Population Protocols
Key Methodological Considerations: Endocrine research in athletes must account for training load, nutritional status, and sport-specific demands. The International Consensus Conference on optimizing elite athlete performance emphasizes individualized, sport-specific approaches and careful monitoring of hormonal status, particularly in female athletes [72]. Dehydration protocols require particular methodological rigor, as fluid losses exceeding 2% body mass can impair performance and affect hormonal measurements [70].
Experimental Protocol: Investigating Exercise-Induced Dehydration and Endocrine Response
Pre-Test Standardization:
- Participant Control: Match athletes by sex, adiposity (not just body weight), and training status. For females, document menstrual status (eumenorrheic vs. amenorrheic), cycle phase, and oral contraceptive use [2] [72].
- Hydration Baseline: Ensure euhydration before testing (verified via urine specific gravity <1.020 and normal plasma osmolality) [70].
- Diet/Exercise Control: Standardize nutritional intake and avoid strenuous exercise 24-48 hours prior to testing.
Dehydration Induction:
- Protocol: Implement exercise-in-heat or passive dehydration to achieve 2-5% body mass loss.
- Monitoring: Measure body mass changes every 15-30 minutes using a scale accurate to 10g [70].
Multi-Modal Hydration Assessment:
- WUT Approach: Combine Weight (body mass change), Urine (USG >1.020 or color >5), and Thirst (subjective rating) [70].
- Blood Biomarkers: Analyze plasma osmolality (>290 mmol/kg indicates dehydration), sodium, and regulatory hormones (AVP/copeptin) [70].
- Avoid Single-Method Reliance: No single hydration biomarker is universally applicable; use at least two complementary methods [70].
Hormonal Response Analysis:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Endocrine Studies
| Reagent/Material | Application | Specific Considerations |
|---|---|---|
| EDTA/Lithium Heparin Tubes | Blood collection for hormone analysis | Choose appropriate anticoagulant for specific assays (e.g., EDTA for renin) |
| Protease Inhibitors | Stabilize protein hormones during processing | Essential for peptide hormones like GH, IGF-1, PTH |
| Steroid Assay Kits | Quantitative analysis of steroid hormones | Consider cross-reactivity issues; LC-MS/MS preferred for specific measurements |
| ELISA Kits for Cytokines | Measure inflammatory markers (IL-6, TNF-α) | Important for obesity-related research and exercise-induced inflammation |
| Cryogenic Vials | Long-term sample storage at -80°C | Ensure low-temperature stability for all analytes |
| Deuterated Isotopes | Gold-standard dilution techniques for TBW measurement | Critical for validation of hydration assessment methods [70] |
| Salivary Collection Devices | Non-invasive hormone sampling | Useful for pediatric populations and circadian rhythm studies (cortisol) |
| Point-of-Care Analyzers | Immediate analysis of glucose, electrolytes | Enable rapid assessment during dehydration protocols |
Optimizing endocrine research protocols for special populations requires meticulous attention to population-specific physiological characteristics and methodological rigor. By implementing the detailed application notes and experimental protocols outlined above—including standardized biological sampling, comprehensive participant characterization, appropriate assessment methodologies, and multi-modal hydration evaluation—researchers can significantly reduce variance in hormonal outcomes and increase the validity of their findings. These approaches provide a framework for generating reliable, reproducible endocrine data that accounts for the unique aspects of pediatric, elderly, and athletic populations, ultimately advancing our understanding of endocrine function across the human lifespan and performance spectrum.
Correcting for Medication and Supplement Use
Accurate endocrine measurement is fundamental to biomedical research, yet it is frequently complicated by the influence of medications and nutritional supplements. These exogenous substances can directly interfere with assay methodologies or indirectly alter physiological hormone pathways, potentially leading to erroneous data interpretation. Within the context of a broader thesis on methodological factors in endocrine research, this protocol details systematic approaches to identify, account for, and correct for the effects of common medications and supplements, thereby enhancing the validity of research findings.
Established Clinical Impacts and Corrections
Clinical and preclinical studies have consistently documented the significant effects that various interventions can have on endocrine physiology. The table below summarizes key findings and the established corrections or considerations for researchers.
Table 1: Documented Endocrine Effects of Medications and Supplements and Research Corrections
| Intervention | Documented Endocrine Effect | Recommended Research Correction/Methodological Consideration |
|---|---|---|
| Anti-Obesity Medications (e.g., GLP-1 RAs) | Significantly raises total and free testosterone levels in men with obesity or type 2 diabetes. A study showed the proportion of men with normal testosterone levels rose from 53% to 77% alongside a 10% weight loss [73]. | Consider medications as a key independent variable. Stratify analysis based on medication use. Monitor body composition, as ~40% of weight loss can be lean mass, which itself correlates with glycemic improvement [74]. |
| Vitamin D Supplementation | Bioavailability is significantly influenced by body composition. Individuals with high trunk fat mass require substantially higher doses to achieve sufficient serum 25(OH)D levels [75]. | In studies assessing vitamin D status, measure and account for body fat distribution (e.g., using DXA scans) rather than relying solely on BMI. Intramuscular administration can standardize for compliance and sunlight exposure [75]. |
| Dietary Composition during Pharmacotherapy | During semaglutide treatment, lower protein intake is associated with greater loss of lean mass. This muscle loss can attenuate improvements in glucose homeostasis (HbA1c) [74]. | Standardize or meticulously record protein and caloric intake in nutritional intervention studies. Prescribe adequate protein (>1.0 g/kg/day) to protect against lean mass loss during weight loss interventions [74]. |
| Endocrine-Disrupting Chemicals (EDCs) | Early-life exposure in rats led to sex-specific alterations in brain gene expression related to reward pathways, influencing long-term food preference (high-fat in females, high-sucrose in males) and hormone levels (reduced testosterone in males) [74]. | In animal or observational studies, control for and document exposure to known EDCs. Use in silico protocols (e.g., OECD QSARs) for initial screening and prioritization of chemicals for endocrine activity assessment [76]. |
Critical Methodological Protocol: Accurate Testosterone Measurement
Inaccurate laboratory testing is a profound methodological pitfall that can invalidate research findings, particularly for sex hormones like testosterone.
The Problem
Most commercially available immunoassays are designed for the high testosterone levels found in men and lack the sensitivity and specificity for accurate measurement in women, children, or hypogonadal men, where levels are much lower. The direct free testosterone assay is widely used but has been demonstrated to be "totally inaccurate" [77].
The Verified Method
The Endocrine Society and CDC recommend a specific methodology for reliable results [77]:
- Total Testosterone Measurement: Use liquid chromatography-tandem mass spectrometry (LC-MS/MS).
- Free/Bioavailable Testosterone Calculation: Calculate free and non-SHBG-bound (bioavailable) testosterone using validated equations from the accurately measured total testosterone, SHBG, and serum albumin concentrations. The "direct free testosterone" assay must be avoided.
Research Application
Investigators must verify the assay methodology used in their studies and explicitly state the use of LC-MS/MS and calculated free testosterone in their publications. Journals and peer reviewers are encouraged to mandate this as a prerequisite for publication [77].
Experimental Protocol: Assessing Vitamin D Bioavailability in Different Body Compositions
The following detailed protocol, adapted from a 2025 study, provides a framework for investigating how a physiological factor (body composition) modifies the effect of a supplement (Vitamin D) [75].
Objective
To determine which specific body components (e.g., fat mass, lean mass) affect the bioavailability of intramuscularly administered vitamin D2 in healthy adults with vitamin D deficiency.
Materials and Reagents
Table 2: Research Reagent Solutions for Vitamin D Bioavailability Studies
| Item | Function/Description |
|---|---|
| Vitamin D2 (Ergocalciferol) | Pharmaceutical grade (e.g., 200,000 IU/mL). The study used "Futai" from Jiangxi Gannan Haixin Pharmaceutical. Content should be verified via HPLC [75]. |
| Liquid Chromatography Tandem Mass Spectrometry (LC-MS/MS) | Gold-standard method for precise quantification of serum 25-hydroxyvitamin D2 [25(OH)D2] and D3 [25(OH)D3] levels [75]. |
| Dual-Energy X-ray Absorptiometry (DXA) | To accurately measure body composition components: total fat mass, trunk fat mass, visceral adipose tissue, and lean mass [75]. |
| Body Fat Mass Index (FMI) | A derived metric calculated as total fat mass (kg) / height (m²). Used to normalize fat mass for body size [75]. |
Procedure
- Screening & Recruitment: Recruit adults (e.g., 18-60 years) with vitamin D deficiency (serum 25(OH)D < 20 ng/mL). Exclude individuals with conditions or on medications known to affect vitamin D metabolism.
- Baseline Assessment: Collect baseline blood for 25(OH)D measurement via LC-MS/MS. Perform full body composition analysis using DXA.
- Intervention & Dose Adjustment:
- Initial Dose: Administer a single intramuscular injection of 600,000 IU vitamin D2.
- Second Dose: Administer a second 600,000 IU injection two weeks later.
- Monitoring & Titration: Measure serum 25(OH)D every 6 weeks. If levels are < 30 ng/mL, administer another two injections of 600,000 IU (spaced two weeks apart). Repeat until sufficiency (≥ 30 ng/mL) is achieved.
- Group Stratification: Upon completion, stratify participants based on the total cumulative dose required to achieve sufficiency (e.g., ≤ 1,200,000 IU group vs. ≥ 2,400,000 IU group).
- Data Analysis: Correlate the total vitamin D2 dose required with various body composition metrics (FMI, trunk fat, lean mass, BMI) to identify the primary determining factor.
The workflow for this experimental protocol is as follows:
In Silico Protocol for Predicting Endocrine Activity
For chemical screening in drug development, integrated computational approaches provide a rapid means to assess potential endocrine activity.
Objective
To define a transparent, reproducible in silico protocol for assessing potential chemical interactions with key endocrine modalities (Estrogen, Androgen, Thyroid, Steroidogenesis - EATS) using (Q)SAR models and existing experimental data [76].
Procedure
- Define Hypothesis: Focus the assessment on a specific EATS modality (e.g., Estrogen Receptor (ER) agonism/antagonism).
- Gather Existing Data: Collect all available in vitro and in vivo data from sources like ToxCast/Tox21 and OECD guidelines (e.g., TG 455 for ER).
- Perform In Silico Predictions: Use (Q)SAR models and expert alerts to predict activity related to the Molecular Initiating Event (MIE) and Key Events (KEs).
- Integrate Evidence via Pathway Models: For ER and AR, utilize integrated pathway models (e.g., ER/AR Pathway Model) that generate an Area Under the Curve (AUC) score from multiple assay outputs. A score > 0.1 indicates activity [76].
- Apply Weight-of-Evidence (WoE): Combine in silico predictions, in vitro data, and any in vivo data (e.g., Uterotrophic assay for ER) to form a WoE conclusion on endocrine activity.
- Refine Testing Strategy: Use the in silico assessment to prioritize chemicals for higher-tier, targeted in vivo testing.
The logical flow of this assessment, which aligns with the OECD conceptual framework, is shown below:
Strategies for Multi-Center Study Harmonization
Multi-center studies are fundamental to advancing clinical and translational research, enabling larger sample sizes, increased statistical power, and improved generalizability of findings [78] [79]. However, the integration of data from multiple sites introduces significant methodological challenges, particularly from non-biological variations related to differences in scanners, acquisition protocols, and analytical techniques [78] [79] [80]. These inconsistencies can produce systematic biases that obscure genuine biological effects and compromise the reproducibility and validity of research outcomes [79] [81]. Within endocrinology, where precise hormone measurement is critical, these challenges are compounded by inherent biological variances and specific methodological factors influencing assay accuracy [2] [82]. This document outlines standardized protocols and application notes for the harmonization of multi-center studies, with specific consideration for endocrine research.
Foundational Concepts and Challenges
The variance in multi-center studies can be categorized into two primary sources, both of which are highly relevant to endocrine investigations:
- Procedural-Analytic Variance: Determined by the investigators and includes:
- Imaging Heterogeneity: Differences in scanner hardware (vendor, model, field strength), acquisition protocols, and reconstruction algorithms [78] [79] [80]. This is a primary concern for radiomics but also affects medical imaging used in some endocrine research (e.g., adrenal or pituitary imaging).
- Data Handling: Inconsistent variable definitions, naming conventions, and data collection methods across sites [81] [83].
- Analytical Techniques: Use of different assay kits, platforms (e.g., immunoassay vs. mass spectrometry), and laboratory protocols for hormone measurement [2] [82].
- Biological Variance: Affiliated with the physiologic status of the participant and is a major focus in endocrine research [2]:
- Subject-Specific Factors: Sex, age, race, body composition, and mental health status [2]. For instance, resting hormonal profiles differ significantly post-puberty and with advancing age [2] [82].
- Temporal Dynamics: Circadian and, in females, menstrual cycle rhythms can cause substantial fluctuations in hormone levels [2].
- Health Status: Conditions like obesity can alter hormonal levels and responses, such as reducing growth hormone response to exercise [2].
The Impact of Variance on Endocrine Measurements
In endocrine research, a failure to control for the sources of variance listed above can lead to inconsistent, contradictory, and difficult-to-interpret results [2]. For example, the accuracy and validity of testosterone measurements are notoriously challenged by factors including assay technique, diurnal variation, age-dependent decreases, and confounding by sex hormone-binding globulin (SHBG) levels [82]. Without harmonization strategies, the signal of true biological effect can be lost in the noise of technical and uncontrolled biological variation.
Strategic Approaches to Harmonization
Harmonization strategies can be broadly classified into prospective (implemented before data collection) and retrospective (applied after data collection).
Prospective Harmonization
Prospective harmonization involves standardizing procedures before a study begins and is considered the gold standard for minimizing variability.
- Common Data Elements (CDEs): Developing and implementing a library of standardized definitions for data items. The Translational Outcomes Project in Neurotrauma (TOP-NT) consortium, for instance, aligned 481 pre-clinical and clinical CDEs and generated 272 new ones to ensure consistent data collection across centers [81].
- Standard Operating Procedures (SOPs): Establishing detailed SOPs for all aspects of the study protocol, including participant recruitment, sample collection, processing, assay techniques, and imaging acquisition [81]. For endocrine studies, this is critical for controlling pre-analytical factors.
- Centralized Training and Quality Control: Ensuring all personnel across sites are trained on the SOPs and implementing centralized quality control checks for ongoing monitoring of protocol adherence [81].
Retrospective Harmonization
When prospective harmonization is not fully achievable, statistical and computational methods can be applied to existing datasets to remove non-biological variability.
- ComBat Harmonization: A powerful empirical Bayesian method widely used to remove batch effects (e.g., site, scanner vendor) from high-dimensional data [78] [80]. It models the data as a combination of biological signals and batch-specific effects, effectively adjusting for the latter while preserving the former. It has been successfully applied to harmonize radiomic features from multi-center PET and MRI datasets [78] [80].
- Machine Learning and Domain Adaptation: These techniques can map data from different sources (domains) into a common feature space, reducing domain-specific biases [79].
- Natural Language Processing (NLP): Automated methods using models like BioBERT can harmonize disparate variable names and descriptions across datasets into unified medical concepts, addressing a major bottleneck in data integration [83].
Table 1: Comparison of Harmonization Methods for Multi-Center Studies
| Method | Type | Key Principle | Example Application |
|---|---|---|---|
| Common Data Elements (CDEs) | Prospective | Standardizes definitions and protocols before data collection | TOP-NT consortium for TBI research [81] |
| ComBat | Retrospective | Empirical Bayes framework to remove batch effects | Harmonizing radiomic features from multi-center PET/MRI [78] [80] |
| Machine Learning Domain Adaptation | Retrospective | Maps data from different domains into a common feature space | Harmonization of DTI data [79] |
| NLP with BioBERT | Retrospective | Uses language models to standardize variable descriptions | Harmonizing cardiovascular risk variables across cohorts [83] |
Experimental Protocols for Harmonization
Protocol: ComBat Harmonization for Quantitative Features
This protocol is adapted from multi-center radiomics studies [78] [80] and can be conceptually applied to standardized endocrine measures.
1. Objective: To remove site- or scanner-specific biases (batch effects) from quantitative feature data (e.g., radiomic features, hormone levels from different assay batches) in a multi-center study.
2. Materials and Software:
- Dataset with quantitative features and associated metadata (Site, Scanner, Age, Sex, etc.).
- Statistical software with ComBat implementation (e.g., R or Python with
neuroCombatorcombatlibraries).
3. Procedure: 1. Data Preparation: Organize the feature data into a matrix (features x subjects). Assemble covariates matrix (e.g., patient age, sex, clinical group) and a batch vector (e.g., site or scanner identifier). 2. Data Splitting: If using the data for model development, split the dataset into training and testing sets (e.g., 90%/10%) to avoid information leakage during harmonization. The ComBat parameters are estimated only on the training set [78]. 3. Model Estimation: On the training set, fit the ComBat model. The model estimates the additive (({\gamma}{if})) and multiplicative (({\delta}{if})) batch effects for each feature [80]. 4. Harmonization: Apply the estimated parameters to adjust the training data. The harmonized feature ( {Y}{ijf}^{*} ) is calculated as: ( {Y}{ijf}^{*} = \frac{{Y}{ijf} - \widehat{{\alpha}{f}} - \widehat{{\gamma}{if}} - X\widehat{{\beta}{f}}}{\widehat{{\delta}{if}}} + \widehat{{\alpha}{f}} + X\widehat{{\beta}{f}} ) where ( {Y}{ijf} ) is the original value, and ( \widehat{{\alpha}{f}}, \widehat{{\gamma}{if}}, \widehat{{\delta}{if}}, \widehat{{\beta}{f}} ) are the estimated parameters [80]. 5. Application to Test Set: Apply the parameters learned from the training set to harmonize the held-out test set, ensuring a unbiased evaluation of model performance [78].
4. Outcome Assessment:
- Use statistical tests (t-test, ANOVA) to confirm the reduction of significant differences in features between batches before and after harmonization.
- Evaluate the effect size using metrics like Cohen's F, which should be reduced post-harmonization [80].
Figure 1: ComBat Harmonization Workflow. A schematic of the key steps for applying ComBat harmonization to a multi-center dataset, highlighting the critical separation of training and testing data.
Protocol: Controlling Biological Variance in Endocrine Studies
This protocol is based on established methodological guidelines for endocrinologic measurements [2].
1. Objective: To minimize the contribution of biological variance to the overall variance of endocrine outcome measures in a clinical study.
2. Materials:
- Study protocol and participant screening tools.
- Mental health screening questionnaire (e.g., for anxiety or depression) [2].
- Facilities for standardized blood sample collection and processing.
3. Procedure: 1. Participant Screening and Matching: * Screen for mental health conditions that may alter basal hormone levels (e.g., elevated cortisol in anxiety) [2]. * Match participants by sex, age, and maturation level. For mixed-sex studies, confirm that the hormonal outcomes are not sex-influenced [2]. * Match participants by body composition (e.g., body mass index) rather than body weight alone, as adiposity influences cytokines and hormones like leptin and insulin [2]. 2. Standardization of Timing: * Schedule all testing and sample collections to account for circadian rhythms. For hormones with a strong diurnal pattern (e.g., cortisol), collect samples at a consistent time of day for all participants [2]. * For studies involving pre-menopausal females, record menstrual status (eumenorrheic vs. amenorrheic) and phase (follicular, ovulatory, luteal). Conduct exercise testing or sample collection with females in the same menstrual phase or account for phase in the statistical analysis. This also applies to females using oral contraceptives [2]. 3. Sample Collection and Assay: * Use standardized protocols for blood collection, processing, and storage across all study sites. * Where possible, analyze all samples from a multi-center study in a single, centralized laboratory using the same assay platform to minimize procedural-analytic variance [2] [82].
4. Outcome Assessment:
- Reduced inter-individual variability in baseline hormonal measures.
- Increased statistical power and validity of the study's physiologic data [2].
Figure 2: Controlling Biological Variance in Endocrinology. Key sources of biological variance in hormone measurements and corresponding strategies for their control in research study design.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for Multi-Center Harmonization
| Item/Tool | Function | Application Notes |
|---|---|---|
| PyRadiomics (Python) | Open-source platform for extraction of standardized radiomic features from medical images. | Ensures reproducibility of image-based feature extraction across sites; compliant with Image Biomarkers Standardization Initiative (IBSI) [78] [80]. |
| ComBat Libraries (R/Python) | Statistical tool for removing batch effects from high-dimensional data. | Critical for retrospective harmonization of data from different scanners or assay batches. Parameters must be estimated on a training set [78] [80]. |
| BioBERT Model | Domain-specific language model for biomedical natural language processing. | Automates the harmonization of variable names and descriptions across different cohort datasets into unified concepts [83]. |
| Standardized Assay Kits | Pre-packaged reagents for hormone measurement (e.g., testosterone). | Reduces analytic variance. For critical applications, mass spectrometry is preferred over immunoassay for its superior accuracy and specificity [82]. |
| Common Data Elements (CDEs) | Standardized definitions for data items. | The foundation of prospective harmonization, ensuring all sites collect data in a consistent, interoperable manner [81]. |
| Traveling Subjects/Phantoms | Healthy subjects or physical objects scanned across all sites. | Provides gold-standard data for directly quantifying and correcting for site-specific biases in imaging studies [79]. |
The success of multi-center research hinges on robust harmonization strategies that mitigate both technical and biological sources of variance. A combined approach of prospective standardization, using CDEs and SOPs, and retrospective statistical adjustment, using methods like ComBat, provides the most powerful framework for generating valid, reproducible, and generalizable data. In endocrine research, where measurements are acutely sensitive to methodological and physiological confounders, the rigorous application of these harmonization protocols is not merely beneficial but essential for producing scientifically sound and clinically meaningful results.
Advancing Validation Frameworks and Embracing Emerging Technologies
Method validation is a critical process in research that ensures analytical techniques produce reliable, accurate, and reproducible data. Within endocrine research, the accurate measurement of hormones is particularly challenging due to their low concentrations, structural similarities, and complex physiological variations [84]. The validation parameters of sensitivity, specificity, and reproducibility form the foundation for establishing method credibility, directly impacting the validity of scientific conclusions and the direction of subsequent studies [84]. This document provides detailed application notes and protocols for the validation of methods used in endocrine measurements, framed within the broader context of methodological factors influencing hormone analysis in research settings.
Defining Key Validation Parameters
Understanding the precise definitions and distinctions between validation parameters is paramount. It is crucial to differentiate between analytical and diagnostic performance characteristics, as these terms are often misused, leading to confusion in interpreting results [85].
Sensitivity
- Analytical Sensitivity: This refers to the lowest concentration of an analyte that an assay can reliably detect. It is a quantitative measure of an assay's detection capability, often expressed as the Limit of Detection (LOD) [86] [85]. A higher analytical sensitivity means the assay can detect smaller amounts of the target hormone.
- Diagnostic Sensitivity: This describes the ability of a test to correctly identify individuals who have the disease or condition of interest. It is the proportion of true positives correctly identified by the test [87] [88]. A highly diagnostically sensitive test is critical for "ruling out" disease, as it minimizes false negatives.
Specificity
- Analytical Specificity: This parameter indicates an assay's ability to measure solely the target analyte without cross-reacting with or being interfered by other substances in the sample [86] [85]. It encompasses cross-reactivity (e.g., an antibody binding to similar hormones) and interference from substances like medications or endogenous compounds [84] [85].
- Diagnostic Specificity: This refers to the ability of a test to correctly identify individuals who do not have the disease or condition. It is the proportion of true negatives correctly identified by the test [87] [88]. A highly diagnostically specific test is valuable for "ruling in" a disease, as it minimizes false positives.
Reproducibility
Reproducibility, sometimes referred to as precision, measures the closeness of agreement between independent results obtained under stipulated conditions. It is typically assessed at multiple levels:
- Repeatability: Precision under the same operating conditions over a short interval (within-run).
- Intermediate Precision: Precision within laboratories, accounting for variations like different days, analysts, or equipment.
- Reproducibility: Precision between different laboratories.
The relationship and differences between these core parameters are summarized in the diagram below.
Figure 1: Core Method Validation Parameters and Their Definitions
Methodologies for Parameter Assessment
Experimental Protocol for Determining Analytical Sensitivity (LOD)
Principle: The Limit of Detection (LOD) is the lowest concentration of an analyte that can be consistently distinguished from a blank sample [86].
Procedure:
- Sample Preparation: Prepare a series of samples (n ≥ 20) at concentrations near the expected detection limit. This should include the zero analyte (blank) sample and samples at, above, and below the likely LOD [86]. For hormone assays, use a matrix that matches the study samples (e.g., charcoal-stripped serum).
- Measurement: Analyze all samples in multiple replicates across different runs.
- Data Analysis:
- Calculate the mean and standard deviation (SD) of the responses for the blank samples.
- The LOD is frequently determined as the concentration corresponding to the mean blank response plus 2 or 3 standard deviations.
Best Practices:
- For assays involving nucleic acid extraction (e.g., in molecular diagnostics for endocrine genes), always include a control to monitor extraction efficiency [86].
- Use whole viruses or bacteria as control material if relevant to the isolation process.
Experimental Protocol for Determining Analytical Specificity
Principle: Assess the assay's ability to detect only the target hormone and distinguish it from structurally similar compounds (cross-reactivity) and its resilience to interfering substances [86] [85].
Procedure:
- Cross-reactivity Studies:
- Compile a panel of related hormones and metabolites (e.g., for a testosterone assay, include DHEAS, androstenedione, and cortisol) [84].
- Spike these compounds individually into the sample matrix at physiologically relevant high concentrations.
- Analyze the samples and calculate the apparent concentration of the target hormone. Significant measured signal indicates cross-reactivity.
- Interference Studies:
- Identify potential interfering substances common in the study population (e.g., bilirubin, hemoglobin, lipids, or common medications) [85].
- Prepare samples spiked with the target hormone at low and high concentrations, along with the interfering substance at a high concentration.
- Compare the results with those from control samples (without the interferent). A clinically significant difference indicates interference.
Best Practices:
- Conduct specificity studies for each specimen matrix (e.g., serum, plasma, urine) approved for use with the assay [86].
- For immunoassays, be particularly vigilant about steroid hormone cross-reactivity, a well-documented issue that can lead to falsely elevated results [84].
Experimental Protocol for Assessing Reproducibility (Precision)
Principle: Quantify the random variation in measurement results under defined conditions.
Procedure:
- Sample Preparation: Select at least two quality control (QC) samples with concentrations spanning the clinically relevant range (e.g., low, medium, high).
- Experimental Design:
- Perform multiple replicates (e.g., n=20) of each QC level in a single run for within-run precision (repeatability).
- Analyze each QC level in duplicate or triplicate over at least 10-20 different days, using different lots of reagents and different analysts if possible, for between-run precision (intermediate precision).
- Data Analysis:
- For each level, calculate the mean, standard deviation (SD), and coefficient of variation (CV = SD/mean × 100%).
- The CV is the primary metric for precision, with a lower CV indicating higher reproducibility.
Best Practices:
- Internal quality controls should always accompany study samples and must be independent of the assay kit's proprietary controls to objectively monitor assay performance over time [84].
- Precision profiles (CV vs. concentration) can help understand performance across the assay's measuring range.
Table 1: Summary of Key Validation Experiments
| Parameter | Experimental Goal | Key Procedure | Acceptance Criteria |
|---|---|---|---|
| Analytical Sensitivity (LOD) | Determine the lowest detectable concentration. | Measure low-level samples & blanks (n≥20). | LOD established with defined confidence (e.g., mean blank + 3SD). |
| Analytical Specificity | Verify measurement of only the target analyte. | Test for cross-reactivity & interference. | No significant cross-reactivity or interference from listed substances. |
| Reproducibility (Precision) | Quantify random measurement error. | Analyze QC samples over multiple runs/days. | CV (%) meets pre-defined goals based on biological variation. |
Critical Considerations in Endocrine Research
The validation of methods for hormone measurement presents unique challenges that must be addressed to ensure data quality.
Technique Selection: Immunoassay vs. Mass Spectrometry
The choice of analytical platform significantly impacts method performance, particularly regarding specificity.
- Immunoassays: These are widely used but rely on antibody binding and are susceptible to cross-reactivity with structurally similar hormones [84]. For example, DHEAS cross-reacts in several testosterone immunoassays, leading to falsely high results, especially in women and children [84]. They can also be affected by matrix effects and varying concentrations of binding proteins (e.g., SHBG, CBG) [84].
- Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS): This technique is generally superior for measuring steroid hormones due to its high analytical specificity and ability to measure multiple analytes simultaneously [84]. However, its performance is dependent on laboratory expertise, thorough development, and validation [84].
Table 2: Comparison of Common Techniques for Hormone Measurement
| Feature | Immunoassay | Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) |
|---|---|---|
| Principle | Antibody-antigen binding | Physical separation and mass-based detection |
| Analytical Specificity | Lower; prone to cross-reactivity | Higher; can distinguish closely related isomers |
| Throughput | Typically high | Variable; can be high with modern systems |
| Multiplexing | Limited; usually single analyte or small panels | High; multiple hormones in a single run |
| Sample Volume | Usually low | Can be higher, but technology is improving |
| Expertise & Cost | Generally lower | High expertise required; higher instrumentation cost |
| Key Limitation | Cross-reactivity, matrix effects | Not always superior if not properly validated [84] |
Pre-Analytical and Biological Factors
Method validation must account for real-world biological and handling variables that affect reproducibility.
- Matrix Effects: The performance of an assay can differ significantly between serum, plasma, saliva, and other matrices. Validation should be performed in the intended matrix [84].
- Binding Proteins: For steroid and thyroid hormones, the concentration of binding proteins (e.g., SHBG, TBG) can interfere in some immunoassays, leading to inaccurate measurements of total hormone concentration, particularly in special populations like pregnant women or patients with liver disease [84].
- Timing and Storage: Hormone levels can fluctuate diurnally and across menstrual cycles [89]. Standardizing sample collection timing and storage conditions (e.g., freeze-thaw cycles) is critical for reproducible results [84].
A Case Study in Reproductive Endocrinology
The following workflow integrates these validation principles into a practical research scenario, such as developing an assay panel for polycystic ovary syndrome (PCOS) [89].
Figure 2: Endocrine Method Validation and Application Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagent Solutions for Endocrine Method Validation
| Reagent / Material | Function in Validation | Application Notes |
|---|---|---|
| Charcoal-Stripped Serum | Provides a hormone-free matrix for preparing calibration standards and spike-recovery samples. | Essential for creating a blank and for analytical sensitivity/specificity experiments. Must match the sample type (e.g., human, animal). |
| Pure Hormone Standards | Used to prepare calibrators and for spiking experiments to determine recovery, linearity, and cross-reactivity. | Source from certified reference material providers. Purity is critical for accurate calibration. |
| Cross-Reactant Panel | A mixture of structurally similar hormones and metabolites to challenge the assay's analytical specificity. | For a testosterone assay, include DHEAS, androstenedione, cortisol, and progesterone [84]. |
| Independent Quality Controls | Non-kit controls used to monitor assay reproducibility over time across multiple runs [84]. | Should be independent of the assay manufacturer and have concentrations at key medical decision points. |
| Interference Stock Solutions | Solutions of common interferents (bilirubin, hemoglobin, intralipids) to test analytical specificity. | Spike into patient samples at high concentrations to simulate pathological or atypical conditions [85]. |
| Stable Isotope-Labeled Internal Standards (for LC-MS/MS) | Used to correct for sample preparation losses and matrix effects in mass spectrometry-based methods. | Critical for achieving high accuracy and reproducibility in quantitative LC-MS/MS workflows. |
Rigorous method validation is not a mere formality but a fundamental component of robust endocrine research. The careful determination of sensitivity, specificity, and reproducibility provides the necessary confidence in hormone data, preventing false conclusions and ensuring that valuable resources are not wasted on misguided follow-up studies [84]. As research progresses, with increasing focus on complex endocrine dynamics and the effects of endocrine-disrupting chemicals, the principles outlined in these application notes and protocols will continue to underpin the generation of reliable and meaningful scientific evidence.
Comparative Analysis of Hormone Measurement Platforms
The accurate quantification of hormonal biomarkers is fundamental to advancing both clinical diagnostics and research in exercise science, drug development, and sports medicine. Hormone measurement platforms have evolved significantly, incorporating advanced technologies to address the complex methodological factors that influence endocrine outcomes. These factors can be broadly categorized as biologic variation (originating from the physiologic status of the participant) and procedural-analytic variation (determined by investigative procedures) [2]. Uncontrolled variance from either source can compromise data validity, making the selection of appropriate measurement platforms a critical consideration for researchers [2] [90].
This document provides a detailed comparative analysis of current hormone measurement technologies, framed within the context of methodological best practices. It includes structured protocols, technical specifications, and analytical workflows designed to assist researchers in selecting and implementing the most appropriate platforms for their specific investigative contexts, from traditional immunoassays to emerging continuous monitoring systems.
Key Methodologic Factors Influencing Hormone Measurements
Research design must account for numerous biologic factors that introduce variance into hormonal measurements. These include participant sex, age, race, body composition, mental health status, menstrual cycle phase, and circadian rhythms [2]. For instance, until puberty, males and females exhibit similar resting hormonal profiles, but significant differences manifest post-puberty and persist through adulthood [2]. Similarly, the menstrual status and cycle phase in females can produce dramatic basal changes in key reproductive hormones, potentially influencing exercise and training responses [2].
Procedural-analytic factors represent another major source of variance, largely determined by the investigators' choice of platform and methodology. A 2025 scoping review highlighted significant inconsistencies in definitions and a scarcity of reported hormone values for menstrual cycle phases, making cross-study comparisons challenging despite the inclusion of intra-assay coefficient reporting in many studies [91]. These findings underscore the necessity for rigorous validation and standardized reporting in endocrine research.
Platform Selection by Research Scenario
The choice of measurement platform should be guided by the specific research context, including sample type, required throughput, sensitivity, and intended application.
- Large Hospitals/Reference Labs: High-throughput, scalable solutions from companies like Abbott, Roche, or Siemens offer extensive validation and are ideal for high-volume settings [92].
- Smaller Clinics/Research Labs: Bio-Rad, Euroimmun, or Abbexa provide cost-effective, specialized options suitable for more focused or exploratory research [92].
- Biotech Firms/Basic Research: Thermo Fisher or Hologic are often preferred for their advanced detection technologies and extensive customization capabilities for novel assay development [92].
For fertility applications, which are projected to dominate the continuous hormone monitoring market with a 65% share in 2025, urinary and salivary methods have gained traction due to their non-invasive nature and feasibility for field settings, though their validity compared to gold-standard serum testing requires careful consideration [93] [91].
Quantitative Platform Comparison and Market Analysis
Table 1: Comparative Analysis of Major Hormone Measurement Platforms
| Platform Category | Example Vendors/Products | Typical Sample Types | Key Strengths | Throughput | Best Application Fit |
|---|---|---|---|---|---|
| Automated Immunoassay Analyzers | Abbott, Roche, Siemens Healthineers | Serum, Plasma | High precision, Extensive validation, Scalability | High | Large-scale clinical diagnostics, High-volume research |
| LC-MS/MS Systems | Shimadzu LC-MS 8060, Agilent ZORBAX columns | Serum, Plasma, Plant Matrices, Saliva | High specificity, Multi-analyte profiling, Broad dynamic range | Medium | Phytohormone research, Metabolomics, Method development |
| Continuous Monitoring Systems | OOVA Inc., Eli Health Hormometer, Level Zero Health wearable patch | Urine, Saliva, Interstitial Fluid | Real-time data, Remote monitoring, High user compliance | Continuous Data Stream | Fertility tracking, Dynamic hormone profiling |
| Rapid/POC Test Kits | Mira, Inito, Everlywell (DTC) | Urine, Saliva | Ease of use, At-home testing, Rapid results | Low | Consumer self-testing, Preliminary screening |
Table 2: Global Market Outlook for Hormone Monitoring (2025-2035)
| Market Segment | Projected 2025 Market Size | Projected 2035 Market Size | CAGR (%) | Dominant Segment (2025) | Key Growth Driver |
|---|---|---|---|---|---|
| Continuous Hormone Monitoring | USD 325.7 Million [93] | USD 716.2 Million [93] | 8.2% [93] | Fertility (65% share) [93] | Wearable tech, Personalized medicine |
| Hormone Therapy Market | USD 30.53 Billion [94] | USD 45.06 Billion [94] | 5.72% [94] | Estrogen Therapy (30.1% share) [94] | Aging population, Bioidentical hormones |
| Direct-to-Consumer Sales Channel | 62.7% share of Continuous Monitoring Market [93] | - | - | Urine Samples (81% share) [93] | Consumer demand for convenience and privacy |
The hormone measurement market is characterized by robust growth and technological diversification. The direct-to-consumer (DTC) sales channel is expected to hold a 62.7% share of the continuous hormone monitoring market in 2025, reflecting a significant shift toward patient-driven health monitoring [93]. Urine samples are projected to dominate this segment with an 81% market share in 2025, driven by non-invasive collection methods suitable for at-home testing, particularly for fertility and pregnancy monitoring [93].
Geographically, the Asia-Pacific region is anticipated to be the fastest-growing market for hormone therapies, with a 23.5% share in 2025, while North America continues to lead with a 39.3% share due to mature healthcare infrastructure and high patient awareness [94]. Within the continuous monitoring segment, China is identified as a key growth region, with a projected CAGR of 10.4% through 2035, driven by rapid industrialization and government healthcare initiatives [93].
Detailed Experimental Protocols
Protocol 1: Unified LC-MS/MS for Phytohormone Profiling
This protocol provides a standardized approach for profiling phytohormones across diverse plant matrices using Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS), demonstrating the application of advanced separation and detection techniques for complex biological samples [95].
4.1.1 Workflow Diagram: LC-MS/MS Phytohormone Analysis
4.1.2 Materials and Reagents
- Plant Matrices: 1.0 g ± 0.1 g of homogenized tissue (e.g., cardamom, dates, tomato, Mexican mint, aloe vera) [95]
- Internal Standard: Salicylic acid D4 (Sigma-Aldrich) [95]
- Extraction Solvents: LC-MS grade Methanol, Formic acid, Acetic acid (Fluka, Supelco) [95]
- Equipment: SHIMADZU LC-30AD Nexera X2 system coupled with LC-MS 8060 mass spectrometer; ZORBAX Eclipse Plus C18 column (4.6 x 100 mm, 3.5 μm) [95]
4.1.3 Procedure
- Sample Preparation: Homogenize plant tissues with mortar and pestle under liquid nitrogen to preserve integrity [95].
- Matrix-Specific Extraction: Weigh approximately 1.0 g of plant material and extract with solvent mixtures tailored to each matrix. For high-sugar content matrices like dates, use a two-step procedure with acetic acid followed by 2% HCl in ethanol [95].
- Internal Standard Addition: Add salicylic acid D4 to all samples for normalization across analyses [95].
- Centrifugation and Filtration: Centrifuge at 3000 × g for 10 minutes at 4°C. Filter supernatant through 0.22 µm syringe filter [95].
- LC-MS/MS Analysis: Inject filtered extract into the LC-MS/MS system using consistent chromatographic and mass spectrometric conditions across all matrices [95].
- Validation: Validate method for sensitivity, reproducibility, and matrix adaptability to ensure robust performance [95].
Protocol 2: Salivary and Urinary Hormone Detection for Menstrual Cycle Tracking
This protocol addresses the complexities of non-invasive hormone monitoring for menstrual cycle phase detection, with applications in sports medicine and reproductive health research [91].
4.2.1 Workflow Diagram: Menstrual Cycle Hormone Detection
4.2.2 Materials and Reagents
- Salivary Collection Kits: Commercially available kits for estradiol and progesterone detection [91]
- Urinary LH Kits: Qualitative or quantitative luteinizing hormone test strips or kits [91]
- Reference Standards: Gold-standard serum testing and transvaginal ultrasound for cycle phase confirmation [91]
4.2.3 Procedure
- Participant Screening: Recruit healthy, naturally cycling premenopausal women. Document menstrual cycle characteristics and exclude participants with hormonal contraception or endocrine disorders [91].
- Sample Collection: Collect saliva or urine samples at specified cycle phases based on participant-reported cycle days or confirmed by basal body temperature [91].
- Phase Definition: Define menstrual phases according to established criteria (e.g., early follicular phase: day 3 ±1 day; peri-ovulatory: ultrasound day of ovulation ±1 day; luteal phase: ultrasound day of ovulation +5, +7, +9 days) [91].
- Assay Procedure: Follow manufacturer instructions for salivary estradiol/progesterone or urinary LH assays. Include appropriate controls and standards in each run [91].
- Data Analysis: Compare salivary and urinary results against gold-standard measures (serum hormone levels, transvaginal ultrasound). Calculate validity parameters (sensitivity, specificity) and precision measures (intra- and inter-assay coefficients of variation) [91].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents for Endocrine Measurements
| Reagent Category | Specific Examples | Function & Application | Technical Notes |
|---|---|---|---|
| Internal Standards | Salicylic acid D4 [95] | Normalization for LC-MS/MS analysis; corrects for extraction and ionization variance | Use isotope-labeled analogs for each target analyte when highest precision required |
| Chromatography Columns | ZORBAX Eclipse Plus C18 (4.6 x 100 mm, 3.5 μm) [95] | Reverse-phase separation of phytohormones prior to MS detection | Optimize mobile phase gradients for each hormone class |
| Mass Spectrometry Reference Kits | Indole-3-acetic acid, Gibberellic acid, Abscisic acid (Sigma-Aldrich) [95] | Quantification standards for phytohormone profiling | Prepare fresh calibration curves with each analysis batch |
| Salivary Collection Devices | Passive drool kits, Synthetic swabs | Collection of saliva for cortisol, estradiol, progesterone measurement | Avoid cotton swabs that can interfere with immunoassays |
| Urinary LH Assays | Qualitative and quantitative LH test strips | Detection of luteinizing hormone surge for ovulation prediction | Standardize time of collection; first morning urine typically recommended |
| Automated Immunoassay Reagents | Abbott, Roche, Siemens analyte-specific kits | High-throughput clinical hormone testing on automated platforms | Strict lot-to-lot validation required for longitudinal studies |
Emerging Technologies and Future Outlook
The field of hormone measurement is rapidly evolving, with several key trends shaping its future trajectory. Continuous monitoring systems represent one of the most significant advancements, with the market projected to grow from USD 325.7 million in 2025 to USD 716.2 million by 2035, registering a CAGR of 8.2% [93]. Recent innovations include Level Zero Health's wearable patch utilizing DNA-based sensors for continuous hormone monitoring, which secured €6.6 million in pre-seed funding in February 2025 to advance its technology [93].
The integration of AI and advanced analytics is another transformative trend, enabling more precise, personalized treatment plans based on individual genetic and hormonal profiles [96]. This is particularly relevant for the interpretation of complex hormonal dynamics, such as those described in mathematical models of glucocorticoid regulation [97]. These models investigate how the speed of endocrine regulation affects baseline and stress-induced hormone levels, highlighting the importance of temporal resolution in hormone measurement [97].
The direct-to-consumer channel continues to expand, with 62.7% of the continuous hormone monitoring market share expected to be held by this channel in 2025 [93]. Companies like Everlywell and Modern Fertility are leveraging this model by offering hormone tests directly to consumers, empowering individuals to monitor their health independently [93].
Looking ahead to 2025 and beyond, the market is expected to see increased consolidation among vendors through M&A activity aimed at expanding technological capabilities [92]. Pricing strategies will likely shift toward flexible, subscription-based models, while manufacturers will focus on enhancing assay sensitivity, reducing costs, and expanding automation to meet rising global demand [92]. These advancements will provide researchers with an increasingly sophisticated toolkit for exploring the complex dynamics of endocrine function across diverse physiological and pathological states.
The Role of Artificial Intelligence in Data Analysis and Quality Control
The accurate measurement of endocrine biomarkers is foundational to advancing research in metabolism, growth, and hormonal disorders. Methodologic factors—from pre-analytical sample handling to data interpretation—introduce significant variability that can compromise research validity and drug development outcomes. This document outlines Application Notes and Protocols for integrating Artificial Intelligence (AI) into endocrine research workflows. Adherence to these methodologies enhances data integrity, automates quality control, and ensures reproducible measurement of endocrine parameters.
Quantitative Performance Benchmarks of AI in Research
AI methodologies are demonstrating transformative potential across various research domains. The following tables summarize key quantitative benchmarks relevant to data analysis and quality control tasks.
Table 1: AI Performance on Demanding Technical Benchmarks (2023-2024)
| Benchmark Name | Domain | Performance Improvement (2023-2024) |
|---|---|---|
| MMMU [98] | Multidisciplinary Reasoning | +18.8 percentage points |
| GPQA [98] | Graduate-Level Q&A | +48.9 percentage points |
| SWE-bench [98] | Software Engineering | +67.3 percentage points |
Table 2: AI Adoption and Impact in Business and Industry (2024 Data)
| Metric | Value | Context/Impact |
|---|---|---|
| Organizations using AI [98] | 78% | Up from 55% in 2023 |
| Global Private AI Investment [98] | $109.1B (US) | Leading other regions |
| Cost Reduction for AI Inference [98] | >280-fold | For GPT-3.5 level performance since 2022 |
| AI's Potential Global Economic Impact [99] | $2.6-4.4T annually | Across 63 use cases |
Table 3: AI in Quality Control and Clinical Research
| Application Area | Reported Impact | Source/Context |
|---|---|---|
| Defect Detection in Manufacturing [100] | 30% improvement | Gartner prediction for 2025 |
| Spectral Data Generation (SpectroGen) [101] | 99% accuracy | vs. physical instrument measurement |
| AI-Generated Spectral Data Speed [101] | <1 minute | vs. hours/days for traditional methods |
Application Notes & Experimental Protocols
Protocol: AI-Assisted Pre-Analytical Quality Control for Endocrine Samples
Objective: To automate the detection of pre-analytical errors in endocrine biospecimens (e.g., serum, plasma) using AI-powered computer vision and metadata analysis, ensuring only samples meeting quality thresholds proceed to expensive endocrine assays.
Background: The integrity of endocrine measurements (e.g., cortisol, HbA1c, growth hormone) is highly sensitive to pre-analytical variables. AI can standardize this critical, often subjective, workflow stage.
Materials & Workflow:
- Input Data:
- Digital Images: High-resolution images of sample tubes (e.g., centrifuged serum/plasma).
- Sample Metadata: Time from collection to processing, storage temperature, freeze-thaw cycles.
- AI Model & Training:
- Technique: Supervised Deep Learning (Convolutional Neural Network - CNN).
- Training Data: A curated dataset of sample images labeled by expert technicians as "Acceptable" or "Unacceptable" based on criteria like hemolysis, lipemia, icterus, fibrin clots, and sample volume.
- Validation: The model is validated against a hold-out test set of labeled images, with performance metrics including AUROC (Area Under the Receiver Operating Characteristic Curve), sensitivity, and specificity calculated [102].
- Execution:
- Sample tubes are automatically imaged upon arrival.
- Images are processed by the trained CNN model.
- The model outputs a quality score and a classification flag.
- Decision & Action:
- "Acceptable": Sample proceeds to the analytical platform.
- "Unacceptable - Critical": Sample is rejected, and a recollection is requested.
- "Unacceptable - Non-Critical": A flag is appended to the sample's data file for potential covariate adjustment during statistical analysis.
AI-Driven Pre-Analytical QC Workflow
Protocol: Predictive Analytics for Subject Cohort Selection in Endocrine Clinical Trials
Objective: To leverage ML models on Electronic Health Record (EHR) data to identify and predict eligible patients for endocrine clinical trials who are most likely to adhere to the protocol and exhibit a treatment response, thereby improving recruitment efficiency and trial success rates.
Background: Participant recruitment and retention are major bottlenecks. ML can phenotype patients from unstructured EHR data, moving beyond simple diagnostic codes to identify ideal candidates [103].
Materials & Workflow:
- Input Data (Structured & Unstructured):
- EHR Data: Demographics, lab results (e.g., HbA1c, hormone panels), medication lists, diagnosis codes.
- Clinical Notes: Physician and nursing notes, progress reports.
- Historical Trial Data: Past recruitment outcomes and adherence patterns.
- AI Model & Training:
- Technique: Natural Language Processing (NLP) for note analysis combined with supervised ML (e.g., Gradient Boosting or Random Forest) for prediction.
- Training: The model is trained on historical data to predict two key outcomes: a) the probability a patient meets complex trial eligibility criteria, and b) the likelihood of protocol adherence.
- Validation: Model performance is evaluated using AUROC and AUPR (Area Under the Precision-Recall Curve), the latter being critical for imbalanced datasets where eligible patients are rare [102] [103].
- Execution:
- The trained model screens a live or historical EHR database.
- It outputs a ranked list of potential candidates with a predicted eligibility and adherence score.
- Decision & Action:
- Clinical research coordinators focus outreach efforts on the highest-probability candidates.
- This data-driven approach refines recruitment strategy and resource allocation.
Predictive Analytics for Trial Recruitment
Protocol: Generative AI for Spectral Data Augmentation in Endocrine Assay Development
Objective: To use generative AI models as a "virtual spectrometer" to augment analytical datasets for endocrine assay validation, reducing reliance on costly and time-consuming physical instrument runs.
Background: Verifying the performance of a new endocrine assay (e.g., Mass Spectrometry) requires extensive calibration and validation runs. Generative AI can create high-fidelity synthetic spectral data, accelerating this process [101].
Materials & Workflow:
- Input Data:
- A foundational dataset of paired spectral measurements. For example, infrared spectra and their corresponding X-ray diffraction or mass spectrometry profiles for known endocrine biomarkers (e.g., steroid hormones).
- AI Model & Training:
- Technique: Physics-informed Generative AI (e.g., a modified Generative Adversarial Network - GAN).
- Training: The model learns the mathematical mappings between different spectral modalities from the paired training data. The "physics-informed" component incorporates known mathematical representations of spectral waveforms (e.g., Gaussian, Lorentzian distributions) [101].
- Validation: The model's output is validated by comparing AI-generated spectra for a hold-out compound against its real, physically obtained spectra, with accuracy measured by correlation (e.g., R²) or structural similarity index [101].
- Execution:
- Researchers input a spectral measurement from a single, cheaper modality (e.g., infrared).
- The generative model outputs the predicted spectrum in the target, more complex modality (e.g., mass spectrometry).
- Decision & Action:
- Generated data is used to supplement experimental data during the assay development and calibration phase.
- This protocol is for research and development acceleration and must be followed by final validation using physical instruments on a subset of samples.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential AI and Data Solutions for Endocrine Research
| Solution / Tool Category | Function in Endocrine Research | Specific Examples / Notes |
|---|---|---|
| Generative BI & NLP Platforms | Enables conversational querying of complex datasets. Allows analysis of unstructured clinical notes for patient phenotyping [103] [99]. | Tools like Luzmo's AI Chart Generator; Allows researchers to ask questions of their data in plain language [99]. |
| AI-Powered Data Cleaning Tools | Automates the identification and handling of outliers, missing values, and data normalization in large endocrine datasets [99]. | Critical for ensuring data quality; frees up to 90% of data analysts' time from manual cleaning tasks [99]. |
| SPIRIT-AI / CONSORT-AI Guidelines | Provides a structured framework for reporting clinical trials involving AI interventions, ensuring transparency and reproducibility [104]. | Mandatory for publishing AI-integrated clinical research; includes 15 new protocol items specific to AI [104]. |
| Virtual Spectrometer (SpectroGen) | Acts as a generative AI tool to predict complex spectral data (e.g., Mass Spec) from simpler, cheaper inputs (e.g., IR), accelerating assay development [101]. | MIT-developed tool; demonstrated 99% accuracy and a >1000x speed increase for generating spectral data [101]. |
| AI Agent Platforms | Capable of planning and executing multi-step research workflows, such as literature review, data extraction, and preliminary analysis [105]. | 23% of organizations are scaling AI agents, with high use in IT and knowledge management for deep research tasks [105]. |
The integration of AI into endocrine research methodology is no longer a future prospect but a present-day necessity for ensuring data quality and accelerating discovery. The protocols outlined—for pre-analytical QC, intelligent cohort selection, and data augmentation—provide a concrete roadmap for researchers to harness these tools. Adherence to emerging standards like SPIRIT-AI is critical for methodological rigor. By adopting these AI-driven Application Notes and Protocols, the endocrine research community can significantly mitigate pre-analytical and analytical variances, leading to more robust, reproducible, and impactful scientific outcomes.
Biomarker Discovery and the Future of Point-of-Care Testing
The field of biomarker discovery is undergoing a transformative shift, driven by technological advances that are simultaneously making biomarkers more powerful and more accessible. Biomarkers—measurable indicators of biological processes, pathogenic processes, or pharmacological responses to therapeutic intervention—represent a transformative framework in modern healthcare, offering powerful insights into human biology and disease [106]. The global biomarkers market reflects this importance, having reached approximately $62.39 billion in 2025 and projected to grow at a compound annual growth rate of 10.8% to $104.15 billion by 2030 [107].
Parallel to these developments, point-of-care testing (POCT) is evolving from a convenience tool to a critical component of diagnostic infrastructure. POCT is defined as testing carried out at or near the site of patient care by a specially trained medical professional, with the ultimate goal of obtaining accurate results conveniently for patients [108]. The convergence of sophisticated biomarker panels with advanced POCT platforms represents a paradigm shift toward decentralized, personalized, and proactive healthcare delivery, particularly relevant for endocrine and metabolic disorders where continuous monitoring provides significant clinical benefits.
Table: Key Market and Technology Drivers in Biomarker and POCT Integration (2025)
| Area | Current Status | Projected Growth/Metrics |
|---|---|---|
| Global Biomarkers Market | $62.39 Billion (2025) | $104.15 Billion by 2030 (10.8% CAGR) [107] |
| Liquid Biopsy Technologies | Real-time disease monitoring & MRD detection | Emerging $16+ Billion market by 2030 [106] |
| AI in Biomarker Discovery | Predictive analytics & automated data interpretation | Accelerating discovery and validation cycles [109] |
| POCT Clinical Impact | Rapid results enabling faster clinical decisions | Decreased overall cost of care [108] |
| Multi-omics Integration | Genomics, proteomics, metabolomics, transcriptomics | Holistic understanding of disease mechanisms [109] |
Methodologic Factors in Endocrine Research: A Foundation for Biomarker Validation
The successful discovery and implementation of biomarkers, particularly for endocrine applications, hinge on rigorous methodological control. Numerous methodological factors influence human endocrine (hormonal) measurements and can dramatically compromise the accuracy and validity of research if not properly addressed [2]. These factors can be categorized as biologic variation (affiliated with the physiologic function or status of the participant) and procedural-analytic variation (determined by the investigators conducting the research) [2].
Critical Biologic Factors Influencing Endocrine Measurements
Biologic factors are endogenous in nature and must be accounted for in both research design and clinical interpretation [2]:
- Sex and Age: Until puberty, males and females exhibit little difference in resting hormonal profiles, but significant differences manifest thereafter and persist through adulthood. Prepubertal and postpubertal individuals do not typically display the same hormonal responses, and age-related differences exist at the other end of the spectrum, with growth hormone and testosterone typically decreasing with age, while cortisol and insulin resistance increase [2].
- Circadian Rhythms: Many hormonal levels fluctuate and display circadian variations due to endogenous pulse generators, meaning time of day for sample collection is a critical experimental control [2].
- Menstrual Cycle Status: In females, menstrual status (eumenorrheic vs. amenorrheic) and cycle phase (follicular, ovulation, or luteal) can produce large and dramatic basal changes in key reproductive hormones like estradiol-β-17, progesterone, luteinizing hormone, and follicle-stimulating hormone [2].
- Body Composition and Mental Health: Varying levels of adiposity can greatly influence cytokines released by adipose tissue, which in turn have autocrine, paracrine, and endocrine-like actions. Furthermore, conditions like high anxiety or depression can lead to altered resting levels of catecholamines, cortisol, and thyroid hormones [2].
Procedural-Analytic Considerations for Reliable Assays
Procedural factors introduce analytic variance that can obscure true biological signals [2]. Key considerations include:
- Sample Collection and Handling: Variations in phlebotomy technique, sample processing time, and storage conditions can artificially alter measured hormone levels.
- Assay Precision and Accuracy: Utilizing assays with appropriate sensitivity and specificity for the target analyte is fundamental. Cross-reactivity with similar molecules must be characterized.
- Data Normalization and Analysis: Choosing appropriate reference standards and statistical methods is crucial for accurate interpretation. Failure to control for these biologic and procedural-analytic factors introduces variance that reduces the validity of hormonal outcomes and complicates the development of robust biomarkers [2].
Diagram 1: Methodologic factors influencing endocrine measurements. Controlling for these biologic and procedural-analytic sources of variance is fundamental to developing reliable biomarkers.
Emerging Biomarker Classes and Technologies: Applications in Endocrinology
Multi-Omics and Digital Biomarkers
The biomarker landscape is experiencing remarkable transformation through collaborative innovation. Advanced analytical methods, including next-generation sequencing (NGS), proteomics, and metabolomics, have become cornerstone technologies in research laboratories [106]. The trend toward multi-omics integration is gaining momentum, enabling researchers to leverage data from genomics, proteomics, metabolomics, and transcriptomics to achieve a holistic understanding of disease mechanisms [109]. This is particularly relevant for endocrine disorders, which often involve complex, multifactorial mechanisms [110].
Digital biomarkers represent another frontier. These are objective health indicators derived from data collected by digital devices like smartwatches, smartphones, or other biometric monitoring technologies [111]. Unlike a one-time blood test, digital biomarkers provide continuous data streams on parameters like heart rate, sleep patterns, and activity levels, ushering in an era of proactive healthcare. For endocrine conditions such as diabetes, this enables detection of subtle changes that signal dysregulation long before acute symptoms appear [111].
Liquid Biopsy and Non-Invasive Monitoring
Liquid biopsy technologies have emerged as a groundbreaking advancement, offering non-invasive methods for disease monitoring and treatment response assessment [106]. These technologies analyze circulating biomarkers in blood, such as circulating tumor DNA (ctDNA), exosomes, and circulating tumor cells. By 2025, advancements are expected to enhance the sensitivity and specificity of liquid biopsies, making them more reliable for early disease detection and monitoring, and facilitating real-time monitoring of disease progression [109]. While prominent in oncology, the principles of liquid biopsy are expanding into endocrine applications, offering a non-invasive window into metabolic and hormonal status.
Table: Emerging Biomarker Classes and Their Endocrine Applications
| Biomarker Class | Core Technology | Representative Endocrine Applications |
|---|---|---|
| Genomic Biomarkers | Next-Generation Sequencing (NGS) | Identification of hereditary endocrine cancer syndromes (e.g., MEN1, MEN2); monogenic diabetes variants [106] [112] |
| Proteomic Biomarkers | Mass Spectrometry, Immunoassays | Quantification of peptide hormones (e.g., insulin, GLP-1); parathyroid hormone (PTH) assays [110] |
| Metabolomic Biomarkers | MS, NMR Spectroscopy | Discovery of metabolite signatures for GDM; monitoring of inborn errors of metabolism [110] |
| Digital Biomarkers | Wearables, Biosensors | Continuous glucose monitoring (CGM); physical activity tracking in obesity; sleep pattern analysis in Cushing's [111] |
| Liquid Biopsy Biomarkers | ctDNA/exosome analysis | Monitoring of endocrine tumor recurrence (e.g., neuroendocrine tumors); prenatal endocrine diagnostics [109] |
Advanced Experimental Protocols for Biomarker Discovery and Validation
Protocol: A Multi-Omics Workflow for Discovering Metabolic Biomarkers in Gestational Diabetes Mellitus (GDM)
This protocol outlines an MS-based untargeted metabolomics approach to identify a distinctive metabolic signature for GDM, as exemplified by recent research [110].
1.0 Sample Collection and Preparation
- Participants: Recruit pregnant women at 24–28 weeks of gestation. Screen using the standard oral glucose tolerance test (OGTT), classifying participants into GDM-positive and healthy control groups (e.g., n=20 per group) [110].
- Sample Type: Collect fasting venous blood serum.
- Preprocessing: Allow blood to clot, then centrifuge to isolate serum. Aliquot and store at -80°C until analysis. Importantly, match participants for potential confounding biologic factors such as gestational age, BMI, and time of sample collection [2].
2.0 Metabolite Extraction and Analysis
- Metabolite Extraction: Thaw serum aliquots on ice. Precipitate proteins using cold methanol or acetonitrile (e.g., 3:1 ratio of solvent to serum). Vortex, incubate at -20°C, then centrifuge to pellet proteins. Transfer the supernatant containing metabolites to new vials and dry under a gentle nitrogen stream [110].
- Instrumentation: Reconstitute samples in a suitable mobile phase for analysis by High-Resolution Mass Spectrometry (HR-MS) coupled with Liquid Chromatography (LC).
- Data Acquisition: Run samples in randomized order to avoid batch effects. Use quality control (QC) samples (a pooled mixture of all samples) throughout the sequence to monitor instrument stability.
3.0 Data Processing and Biomarker Candidate Identification
- Feature Detection: Process raw LC-MS data using bioinformatics software (e.g., XCMS, MS-DIAL) for peak picking, alignment, and retention time correction.
- Metabolite Identification: Annotate detected features by comparing their mass-to-charge ratios (m/z) and fragmentation spectra (MS/MS) against public databases (e.g., HMDB, MetLin).
- Statistical Analysis: Perform multivariate statistical analysis, such as Partial Least Squares-Discriminant Analysis (PLS-DA), to visualize group separation. Use univariate tests (e.g., t-tests with false discovery rate correction) to identify metabolites with significantly different abundances between GDM and control groups. In the referenced study, this revealed a significant number of dysregulated metabolites in GDM serum [110].
4.0 Biomarker Validation and Panel Selection
- Pathway Analysis: Input significantly altered metabolites into pathway analysis tools (e.g., MetaboAnalyst) to identify disturbed biological pathways (e.g., tryptophan metabolism, inositol phosphate metabolism) [110].
- Panel Construction: Apply machine learning algorithms (e.g., Random Forest, LASSO regression) to select a minimal set of metabolites that best differentiate GDM from controls. The referenced study selected a combination of 10 metabolites, including N-acetylproline and serylmethionine [110].
- Performance Assessment: Evaluate the diagnostic performance of the biomarker panel by calculating the Area Under the Receiver Operating Characteristic Curve (AUC). The 10-metabolite panel achieved an AUC of 0.978, indicating high diagnostic importance [110].
Diagram 2: A multi-omics workflow for GDM biomarker discovery. This protocol from recent research identifies a metabolic signature as a potential alternative to standard OGTT [110].
Protocol: Developing a Point-of-Care Platform for Endocrine Biomarkers
This protocol describes a generalized framework for translating a validated laboratory-based endocrine biomarker assay into a robust POCT device, considering the critical regulatory and clinical workflow requirements.
1.0 Analytical Technique Selection and Assay Miniaturization
- Core Technology: Choose a detection method appropriate for the target biomarker (e.g., immunoassay for proteins/peptides, electrochemical sensing for metabolites). The technology must be amenable to miniaturization and provide reliable results in a shortened time frame.
- Device Design Principles: The device must be fit for its intended purpose, easy to operate, and maintainable in a safe and reliable condition [108]. Adhere to guidelines such as the WHO "ASSURED" criteria (Affordable, Sensitive, Specific, User-friendly, Rapid, Robust, Equipment-free, and Delivered) [108].
- Sample Introduction: Implement a simple, foolproof sample handling system (e.g., capillary action for blood, dipstick for urine) that requires minimal user steps.
2.0 Assay Optimization for POCT Conditions
- Reagent Stability: Formulate dry reagents that are stable at room temperature for extended periods. Integrate them into a single-use cartridge or test strip.
- Signal Generation and Readout: Optimize the assay chemistry for speed and clarity of signal (e.g., colorimetric, fluorescent, electrochemical). Integrate a reader (e.g., a compact optical sensor or potentiostat) that provides a quantitative or semi-quantitative result.
- Connectivity: Ensure the device can transmit results to electronic health records (EHRs) or central laboratories via Bluetooth or other standard protocols to support data traceability [112].
3.0 Analytical and Clinical Performance Validation
- Precision and Accuracy: Evaluate the POC device's performance against the gold-standard laboratory method using clinical samples. Assess intra-assay and inter-assay precision.
- Sensitivity and Specificity: Determine the clinical sensitivity and specificity of the test in the intended-use population.
- Reference Intervals: Establish or verify reference intervals specific to the POC platform.
4.0 Integration into Clinical Workflow and Value Assessment
- Workflow Mapping: Collaborate with clinical end-users to integrate the test into the existing patient care pathway without causing disruption. A clinical needs-driven approach is essential for adoption [113].
- Operator Training: Develop a simple, standardized training program for potential users (e.g., nurses, community health workers, pharmacists).
- Value Proposition Assessment: Generate evidence not just of clinical performance, but of clinical utility (e.g., reduced time to diagnosis, improved patient outcomes, cost savings) to address the needs of payers and provider organizations [113].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of the protocols above requires high-quality, reliable reagents and platforms. The following table details key materials and their functions in modern biomarker research and POCT development.
Table: Research Reagent Solutions for Biomarker Discovery and POCT Development
| Reagent/Material | Function and Critical Features | Application Examples |
|---|---|---|
| High-Affinity Monoclonal Antibodies | Specific molecular recognition for immunoassay development; low cross-reactivity is critical. | Quantifying specific protein hormones (e.g., insulin, cortisol) in POC immunoassays [108]. |
| Stable Isotope-Labeled Internal Standards | Absolute quantification and normalization in mass spectrometry-based assays. | Precise measurement of metabolite or peptide concentrations in multiplexed biomarker panels [110]. |
| Next-Generation Sequencing Kits | Targeted gene panels or whole-exome/genome sequencing for genomic biomarker discovery. | Identifying genetic variants associated with endocrine disorders (e.g., thyroid cancer, monogenic diabetes) [106] [112]. |
| Digital Biomarker Software Suites (e.g., DBDP) | Open-source pipelines (e.g., Digital Biomarker Discovery Pipeline) for processing mHealth data; promotes standardization and reproducibility [111]. | Analyzing continuous glucose monitor (CGM) or accelerometer data to derive digital endpoints for clinical trials [111]. |
| Point-of-Care Test Strips/Cartridges | Integrated, single-use platforms containing stabilized reagents for decentralized testing. | Consumer and professional glucose meters; emerging rapid tests for HbA1c or other endocrine markers [108]. |
The integration of sophisticated biomarker discovery with decentralized testing platforms is poised to redefine diagnostic and therapeutic paradigms in endocrinology. For researchers and drug development professionals, success will depend on a multi-faceted strategy that embraces multi-omics integration, leverages AI and machine learning for discovery and validation, and prioritizes clinical needs-driven development for POCT devices [109] [113].
Future trajectories will see biomarker pipelines shift from single analytes to composite, multi-modal signatures, with AI-native discovery accelerating the volume of validated candidates [107]. The convergence of wearables and biosensors with traditional biomarker science will enable continuous, real-time monitoring of endocrine health, moving medicine from a reactive to a proactive and deeply personalized model [111] [107]. By building robust, methodologically sound discovery pipelines and simultaneously addressing the practical challenges of implementation, the scientific community can fully realize the potential of biomarkers to revolutionize point-of-care testing and patient care.
The choice of study design is a fundamental methodological factor that profoundly influences the validity, interpretation, and causal inference of endocrine measurements in research. Observational studies, which do not manipulate the study environment, primarily fall into two categories: cross-sectional and longitudinal designs [114]. The decision to employ one over the other hinges on the research question, with each offering distinct advantages and limitations for investigating the complex, dynamic nature of endocrine systems. Cross-sectional studies provide a snapshot of hormone levels and their associations at a single point in time, allowing researchers to compare different population groups simultaneously [114]. In contrast, longitudinal studies involve repeated observations of the same subjects over prolonged periods—years or even decades—enabling researchers to track individual changes and establish sequences of events [114] [115]. Within the specific context of endocrine research, where many processes such as pubertal development unfold over time, longitudinal designs are particularly valuable for disentangling the effects of age, endocrine events, and other confounding variables [116]. This article delineates the strategic progression from initial cross-sectional investigations to definitive prospective longitudinal studies, providing detailed protocols to enhance the rigor of endocrine measurement in research and drug development.
Comparative Analysis: Study Designs at a Glance
Table 1: Key Characteristics of Cross-Sectional and Longitudinal Designs in Endocrine Research
| Feature | Cross-Sectional Design | Prospective Longitudinal Design |
|---|---|---|
| Temporal Framework | Single time point; "snapshot" [114] | Multiple time points over a prolonged period [115] |
| Primary Utility | Identifying associations and generating hypotheses [114] | Establishing sequences of events and studying cause-and-effect [114] [115] |
| Data on Individual Change | No | Yes [115] |
| Ability to Correct for Cohort Effects | Limited | Yes [115] |
| Key Advantage | Speed, lower cost, and ability to compare many variables [114] | Detects development and change at group and individual levels [114] |
| Key Limitation | Cannot establish causality [114] | Subject to attrition, time-consuming, and financially demanding [115] |
| Risk of Recall Bias | Possible | Minimized in prospective designs [115] |
| Inference on Causality | Limited | Stronger [114] |
Experimental Protocols for Endocrine Research
Protocol 1: Conducting a Cross-Sectional Endocrine Survey
This protocol is designed for the initial investigation of associations between endocrine measures and variables of interest.
1. Aims: To compare hormone concentrations across different population groups (e.g., by age, gender, BMI, or exposure status) at a single point in time and to identify potential associations for further investigation.
2. Key Materials and Reagents:
- Biological Sample Collection Kits: For standardized collection of serum, plasma, saliva, or urine.
- Validated Immunoassay Kits: Such as ELISA or RIA, with known cross-reactivity profiles for the target analyte (e.g., sex steroids, cortisol, TSH).
- Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) System: For high-specificity measurement of steroid hormones, if available.
- Demographic and Health Questionnaire: To capture potential confounders (e.g., age, time of sample collection, medication use, menopausal status).
3. Detailed Methodology:
- Step 1: Participant Recruitment and Sampling. Define and recruit distinct population groups of interest. Ensure groups are sufficiently powered to detect a clinically meaningful difference. Collect biological samples in a standardized manner,严格控制样本采集时间以控制昼夜节律影响.
- Step 2: Biochemical Analysis. Process and aliquot samples according to established SOPs to prevent analyte degradation. Analyze all samples for the endocrine measures of interest within the same batch, or if batched, include appropriate internal quality controls across batches to minimize inter-assay variability.
- Step 3: Data Collection and Harmonization. Administer questionnaires. Create a derived variable for, as an example, "biologically active testosterone" from total testosterone and SHBG measurements, if required [117]. Clean and harmonize all data prior to analysis.
- Step 4: Statistical Analysis. Use analysis of variance (ANOVA) or multivariate analysis (MANOVA) to compare mean hormone levels across groups. Employ linear or logistic regression models to examine associations between exposures and hormone outcomes while adjusting for identified confounders (e.g., age, BMI).
Protocol 2: Implementing a Prospective Longitudinal Endocrine Cohort Study
This protocol outlines the design for an ongoing, long-term study to understand the temporal dynamics of endocrine function, such as the NIMH Longitudinal Study of Puberty [116].
1. Aims: To measure changes in endocrine parameters and related health outcomes within individuals over time; to establish the temporal sequence between endocrine changes and physiological or neurodevelopmental outcomes.
2. Key Materials and Reagents:
- Longitudinal Biobank: A -80°C freezer system with a robust inventory management system for long-term storage of serial biological samples.
- Multimodal Assessment Suite: Tools for repeated measures beyond endocrinology, which may include neuroimaging, cognitive assessments, and physical exams [116].
- Data Linkage Infrastructure: Secure systems for linking repeated participant data using unique codes and for potentially linking to administrative health records [115] [117].
- Mixed-Effect Regression Model (MRM) Software: Statistical software (e.g., R, Stata) capable of analyzing hierarchical longitudinal data.
3. Detailed Methodology:
- Step 1: Baseline Characterization. Recruit a well-characterized cohort at a baseline state (e.g., prepubertal children [116]). Collect comprehensive baseline data, including biosamples, neuroimaging, and clinical phenotypes.
- Step 2: Longitudinal Follow-up and Wave Planning. Establish a pre-planned schedule of follow-up visits at defined intervals (e.g., 8-10 months [116]). The frequency should be informed by the expected rate of change in the endocrine system under investigation. Use consistent methods and assays at all timepoints.
- Step 3: Contemporaneous Data Collection. At each follow-up wave, collect endocrine, phenotypic, and omics data contemporaneously. For example, measure sex steroids, adrenal androgens, and GnRH agonists/antagonists at each visit alongside neuroimaging measures [116].
- Step 4: Longitudinal Data Analysis and Attrition Management. Employ statistical methods like Mixed-Effect Regression Models (MRM) or Generalized Estimating Equations (GEE) that account for within-individual correlation, unequal time intervals, and missing data [115]. Implement strategies to maximize retention, such as exit interviews to understand reasons for dropout [115].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Longitudinal Endocrine Investigations
| Item | Function | Application Example |
|---|---|---|
| LC-MS/MS Assays | High-specificity quantification of multiple steroid hormones from a single sample, minimizing cross-reactivity. | Precisely measuring low levels of estradiol in children or postmenopausal women [116]. |
| Multiplex Immunoassay Panels | Simultaneous measurement of multiple analytes (e.g., hormone panels, cytokines) from a small sample volume. | Profiling the hypothalamic-pituitary-gonadal (HPG) and hypothalamic-pituitary-adrenal (HPA) axes in parallel. |
| Stable Isotope-Labeled Internal Standards | Correct for analyte loss during sample preparation and matrix effects in mass spectrometry. | Ensuring quantitative accuracy in longitudinal hormone measurements across thousands of samples. |
| Biospecimen Inventory Management System | Track aliquot location, freeze-thaw cycles, and sample quality for a longitudinal biobank. | Maintaining sample integrity and chain-of-custody over a decade-long study. |
| Data Harmonization Tools | Retrospectively adjust data collected using different methods or instruments to enable comparison. | Combining endocrine data from multiple study waves or different cohorts [117]. |
Visualizing the Research Workflow
The following diagram illustrates the logical progression and key decision points in a research program moving from cross-sectional to longitudinal design.
Conclusion
Accurate endocrine measurement is foundational to producing valid, reproducible research and enabling effective clinical decision-making. Success hinges on a holistic strategy that rigorously controls for biologic variability through careful participant selection, standardizes pre-analytical and analytical procedures in line with initiatives like the EndoCompass project, and proactively troubleshoots for environmental factors such as endocrine disruptors. Future progress depends on strategic investment in harmonizing laboratory standards, leveraging artificial intelligence for data analysis, and fostering collaborative research to establish robust, personalized reference intervals. By adopting this comprehensive framework, researchers and drug development professionals can significantly reduce methodological variance, thereby enhancing the scientific quality and impact of their work in endocrinology.
References
- 1. a systematic analysis of the global burden of disease study [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1631123/full]
- 2. Research Methodology: Endocrinologic Measurements in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2582556/]
- 3. Neuroendocrine underpinnings of sex differences in circadian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4841755/]
- 4. Age and sex affect circadian patterns of cardiac autonomic ... [https://www.nature.com/articles/s41598-025-18525-6]
- 5. Endocrinology, Diabetes & Metabolism: Statistics, Data, and ... [https://guides.uflib.ufl.edu/endocrine/data]
- 6. Big Data Research in the Field of Endocrine Diseases ... [https://www.e-enm.org/journal/view.php?number=2368]
- 7. The Interplay Between Adipokines and Body Composition in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11863173/]
- 8. Prospective changes in lipocalin-2 and adipocytokines ... [https://www.nature.com/articles/s41598-025-14091-z]
- 9. Diagnostic and prognostic value of adipose tissue content ... [https://www.nature.com/articles/s41598-025-12262-6]
- 10. The Role of Adipokines and Gene Polymorphisms in ... [https://link.springer.com/article/10.1007/s13679-025-00652-w]
- 11. exercise modalities and dosages to ameliorate adipokine ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1653449/full]
- 12. Relationship of Physical Activity Levels and Body ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346752/]
- 13. Exercise improves body composition, physical fitness, and ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2024.1451427/full]
- 14. Confounding control in healthcare database research [https://pmc.ncbi.nlm.nih.gov/articles/PMC4024462/]
- 15. Tracking mood symptoms across the menstrual cycle in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12198828/]
- 16. The Association of Mental Health With Menstrual ... [https://www.sciencedirect.com/science/article/pii/S1054139X25001648]
- 17. Prediction premenstrual syndrome (PMS) with anxiety, and ... [https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-025-07250-z]
- 18. 5 pitfalls to avoid when working with color in data ... [https://flourish.studio/blog/color-in-data-visualization/]
- 19. Pitfalls in the lab assessment of hypopituitarism [https://link.springer.com/article/10.1007/s11154-024-09881-1]
- 20. Control of (pre)-analytical aspects in immunoassay measurements of metabolic hormones in rodents [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5881432/]
- 21. Use of biomarkers in epidemiologic studies: minimizing the influence of measurement error in the study design and analysis | Cancer Causes & Control [https://link.springer.com/article/10.1007/s10552-006-0035-5]
- 22. Interpretation of common endocrine laboratory tests: technical pitfalls, their mechanisms and practical considerations - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6657094/]
- 23. Common Pitfalls in the Interpretation of Endocrine Tests - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8453144/]
- 24. An Evidence-base for Laboratory Endocrinology? - PMC [https://ncbi.nlm.nih.gov/pmc/articles/PMC2605414]
- 25. Causes of Preanalytical Interferences on Laboratory Immunoassays – A Critical Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7109499/]
- 26. Principles and pitfalls of free hormone measurements [https://www.sciencedirect.com/science/article/abs/pii/S1521690X13000936]
- 27. Stability, homogeneity and measurement uncertainty ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10973327/]
- 28. How to Assess Preclinical Dose Formulation Homogeneity [https://www.pharmtech.com/view/how-assess-preclinical-dose-formulation-homogeneity]
- 29. Materials of the 2nd Conference with International ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12028731/]
- 30. How to Prepare for a Lab Test [https://medlineplus.gov/lab-tests/how-to-prepare-for-a-lab-test/]
- 31. Having Your Blood Drawn? Here is How to Prepare [https://www.bannerhealth.com/healthcareblog/advise-me/need-to-have-blood-drawn-here-is-the-best-way-to-prepare]
- 32. Collect Adult Blood Culture Sets | Laboratory Quality [https://www.cdc.gov/lab-quality/php/preventing-adult-blood-culture-contamination/collect.html]
- 33. Order of Blood Draw Tubes and Additives [https://clsi.org/resources/insights/order-of-blood-draw-tubes-and-additives/]
- 34. Best practices in phlebotomy - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK138665/]
- 35. DPDx - Diagnostic Procedures - Blood Specimens [https://www.cdc.gov/dpdx/diagnosticprocedures/blood/safety.html]
- 36. Best Practices for Handling Blood Samples [https://www.solomon.org/best-practices-for-handling-blood-samples/]
- 37. Immunoassays and Mass Spectrometry for Determination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11046482/]
- 38. Should LC-MS Replace Immunoassay? [https://www.thermofisher.com/us/en/home/products-and-services/promotions/industrial/should-lc-lcms-replace-immunoassay.html]
- 39. Recommendations for Validation of LC-MS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4287296/]
- 40. Reliable in-house LC-MS/MS method for steroid hormone ... [https://www.sciencedirect.com/science/article/pii/S0009898125004899]
- 41. Comparing immunoassay and mass spectrometry ... [https://www.sciencedirect.com/science/article/pii/S0306453025001027]
- 42. Reliable in-house LC-MS/MS method for steroid hormone ... [https://pubmed.ncbi.nlm.nih.gov/40946765/]
- 43. LC-MS-based conventional metabolomics combined with ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1588718/full]
- 44. Methodological Considerations in Saliva‐Based Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560811/]
- 45. Metabolomics in Endocrinology: The Way Forward - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12410955/]
- 46. Reference intervals: past, present, and future - PubMed [https://pubmed.ncbi.nlm.nih.gov/37036018/]
- 47. Personalized reference intervals: from theory to practice - PubMed [https://pubmed.ncbi.nlm.nih.gov/35579539/]
- 48. Perspective and consideration in the application of personalized reference intervals based on biological variation: a four-month observation of a woman with SARS-CoV-2 reinfection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12334944/]
- 49. The EndoCompass Project: Research Roadmap for Better ... [https://www.ese-hormones.org/what-we-do/research/the-endocompass-project/]
- 50. Press release: New EndoCompass Research Roadmap ... [https://www.ese-hormones.org/news/press-release-new-endocompass-research-roadmap-calls-for-coordinated-investment-to-tackle-europe-s-hormone-health-challenge/]
- 51. EndoCompass project: endocrine laboratory medicine [https://pubmed.ncbi.nlm.nih.gov/41104467/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=0eobfQRcBgAaZcq5tGJ-h_C66iXogjZx_r9ngKsF4u0&fc=None&ff=20251023104426&v=2.18.0.post22+67771e2]
- 52. Lifestyle in flux: urbanization, dietary shifts, and endocrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12372347/]
- 53. The relationship between abdominal fat and sleep quality ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1471608/full]
- 54. Circadian rhythm homeostasis biomarkers [https://www.sciopen.com/article/10.26599/OSHM.2025.9610028]
- 55. Motivations and Methods for Analyzing Pulsatile Hormone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2647703/]
- 56. Circadian Rhythm: Biological Functions, Diseases, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547082/]
- 57. Endocrine regulation of circadian rhythms [https://www.nature.com/articles/s44323-025-00024-6]
- 58. Development of a Methodology for and Assessment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5398599/]
- 59. HormoneBayes: A novel Bayesian framework for the analysis ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1011928]
- 60. Editorial: Circadian rhythm in adrenal endocrinology [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1620570/full]
- 61. Determining the Endocrine Disruption Potential of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6728168/]
- 62. Sensor technologies for the detection and monitoring of ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1141523/full]
- 63. Analytical Methodologies for the Determination of Endocrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3662172/]
- 64. Review Endocrine disrupting chemicals exposure and health [https://www.sciencedirect.com/science/article/pii/S0147651325009194]
- 65. Methods for the analysis of endocrine disrupting chemicals ... [https://www.sciencedirect.com/science/article/pii/S0013935121019174]
- 66. Endocrine disrupters [https://www.oecd.org/en/topics/sub-issues/testing-of-chemicals/endocrine-disrupters.html]
- 67. Methodological and statistical considerations for exercise ... [https://pubmed.ncbi.nlm.nih.gov/7481285/]
- 68. Toxic Alerts of Endocrine Disruption Revealed by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11934200/]
- 69. What do people need to know about endocrine disrupting ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-025-25561-4]
- 70. Recommendations for Optimizing Research Regarding the ... [https://link.springer.com/article/10.1007/s40279-025-02310-6]
- 71. The trajectory of intrinsic capacity and its related factors ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1539982/full]
- 72. Consensus Statements—Optimizing Performance of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12334928/]
- 73. Anti-obesity medications can normalize testosterone levels ... [https://www.endocrine.org/news-and-advocacy/news-room/endo-annual-meeting/endo-2025-press-releases/portillo-canales-press-release]
- 74. ENDO 2025: The Gold Standard - Endocrine News [https://endocrinenews.endocrine.org/endo-2025-the-gold-standard/]
- 75. Impact of body composition on vitamin D requirements in ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1421663/full]
- 76. An in silico protocol for endocrine activity assessment [https://www.sciencedirect.com/science/article/abs/pii/S2468111325000246]
- 77. Initiative Calls for Updated Standards in Testing ... [https://reports.mountsinai.org/article/endo2025-_2_testing-standards]
- 78. Impact of harmonization and oversampling methods on radiomics analysis of multi-center imbalanced datasets: application to PET-based prediction of lung cancer subtypes | EJNMMI Physics | Full Text [https://ejnmmiphys.springeropen.com/articles/10.1186/s40658-025-00750-7]
- 79. Harmonization of Multi-Center Diffusion Tensor Imaging Data: Challenges and Solutions [https://www.alliedacademies.org/articles/harmonization-of-multicenter-diffusion-tensor-imaging-data-challenges-and-solutions-32702.html]
- 80. Investigation of ComBat Harmonization on Radiomic and Deep Features from Multi-Center Abdominal MRI Data | Journal of Imaging Informatics in Medicine [https://link.springer.com/article/10.1007/s10278-024-01253-0]
- 81. Prospective Harmonization, Common Data Elements, and Sharing Strategies for Multicenter Pre-Clinical Traumatic Brain Injury Research in the Translational Outcomes Project in Neurotrauma Consortium - PubMed [https://pubmed.ncbi.nlm.nih.gov/39831841/]
- 82. Review Challenges in Testosterone Measurement, Data ... [https://www.sciencedirect.com/science/article/abs/pii/S1743609516301709]
- 83. JMIR Formative Research - Automated Data Harmonization in Clinical Research: Natural Language Processing Approach [https://formative.jmir.org/2025/1/e75608]
- 84. Improving Science by Overcoming Laboratory Pitfalls With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7993596/]
- 85. Analytical vs Diagnostic Sensitivity and Specificity [https://www.immqas.org.uk/news/analytical-vs-clinical-sensitivity-and-specificity/]
- 86. Molecular Diagnostics - Part 5: Analytical Sensitivity and ... [https://blog.seracare.com/molecular-serology-blog/verification-part5]
- 87. Sensitivity and specificity [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]
- 88. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 89. A semi-mechanistic mathematical framework for simulating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12395073/]
- 90. Research methodology: endocrinologic measurements in ... [https://pubmed.ncbi.nlm.nih.gov/19030142/]
- 91. Complexities in salivary and urinary methodology for ... [https://gremjournal.com/journal/01-2025/complexities-in-salivary-and-urinary-methodology-for-ovulation-and-menstrual-cycle-hormone-detection-a-scoping-review/]
- 92. Top Endocrine Testing Companies & How to Compare ... [https://www.linkedin.com/pulse/top-endocrine-testing-companies-how-compare-them-2025-axenth-labs-w5fzf/]
- 93. Continuous Hormone Monitoring Market Growth 2025-2035 [https://www.futuremarketinsights.com/reports/continuous-hormone-monitoring-market]
- 94. Hormone Therapy Market Size & Opportunities, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/hormone-therapy-market]
- 95. Comparative LC-MS/MS-based profiling of phytohormones [https://www.frontiersin.org/journals/plant-science/articles/10.3389/fpls.2025.1670979/full]
- 96. hormone analyzer trends 2025: AI & Wearable Tech [https://www.accio.com/t-v2/business/hormone-analyzer-trends]
- 97. Mathematical modeling reveals how the speed of ... [https://www.sciencedirect.com/science/article/abs/pii/S0018506X21001380]
- 98. The 2025 AI Index Report | Stanford HAI [https://hai.stanford.edu/ai-index/2025-ai-index-report]
- 99. Using AI for Data Analysis: The Ultimate Guide (2025) [https://www.luzmo.com/blog/ai-data-analysis]
- 100. How is AI revolutionizing Quality Control in manufacturing? [https://www.koerber.com/en/insights-and-events/supply-chain-insights/ai-quality-control-manufacturing]
- 101. Checking the quality of materials just got easier with a new ... [https://news.mit.edu/2025/checking-quality-materials-just-got-easier-new-ai-tool-1014]
- 102. Machine Learning in Clinical Trials: A Primer with Applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10228463/]
- 103. The role of machine learning in clinical research - Trials [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-021-05489-x]
- 104. Guidelines for clinical trial protocols for interventions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8212701/]
- 105. The State of AI: Global Survey 2025 [https://www.mckinsey.com/capabilities/quantumblack/our-insights/the-state-of-ai]
- 106. What Are Biomarkers? Definition, Applications and ... [https://blog.omni-inc.com/blog/what-are-biomarkers-and-whats-new-in-2025]
- 107. Biomarkers in 2025: From Liquid Biopsy to AI-Driven ... [https://www.barchart.com/story/news/35377423/biomarkers-in-2025-from-liquid-biopsy-to-ai-driven-discovery-what-business-leaders-must-know]
- 108. Faster results, better care: The rising importance of point ... [https://diagnostics.roche.com/global/en/article-listing/lab-leaders/article/importance-point-of-care-testing.html]
- 109. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 110. Editorial: Omics in endocrinology: from biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11865747/]
- 111. Biomarker discovery pipeline: 3 Critical Steps 2025 [https://lifebit.ai/blog/biomarker-discovery-pipeline/]
- 112. Insights from Biomarkers & Precision Medicine 2025 [https://www.signifyresearch.net/insights/biomarkers-billions-and-breakthroughs-insights-from-biomarkers-precision-medicine-2025/]
- 113. Overcoming Challenges with the Adoption of Point-of-Care ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7751984/]
- 114. Cross-sectional vs. longitudinal studies [https://www.iwh.on.ca/what-researchers-mean-by/cross-sectional-vs-longitudinal-studies]
- 115. Longitudinal studies - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4669300/]
- 116. The NIMH Intramural Longitudinal Study of the Endocrine and ... [https://pubmed.ncbi.nlm.nih.gov/33771694/]
- 117. Longitudinal vs cross-sectional studies [https://learning.closer.ac.uk/learning-modules/introduction/types-of-longitudinal-research/longitudinal-versus-cross-sectional-studies/]