Chronopharmacology in Drug Development: Mitigating Medication Interference in Circadian Hormone Sampling
This article addresses the critical challenge of medication-induced circadian disruption in biomedical research and drug development.
Chronopharmacology in Drug Development: Mitigating Medication Interference in Circadian Hormone Sampling
Abstract
This article addresses the critical challenge of medication-induced circadian disruption in biomedical research and drug development. It explores the foundational mechanisms by which therapeutics interfere with endocrine circadian rhythms, provides methodological frameworks for accurate hormone sampling in clinical trials, offers troubleshooting strategies for optimizing protocol design, and discusses validation techniques for distinguishing drug-induced effects from endogenous rhythms. Aimed at researchers, scientists, and drug development professionals, this comprehensive review synthesizes current chronobiological principles with practical applications to enhance data reliability, improve drug safety profiling, and advance personalized chronotherapy approaches.
The Circadian-Hormone Axis: Understanding Fundamental Interference Mechanisms
Core Principles of Circadian Clock Organization and Hormonal Regulation
Troubleshooting Guide: Circadian Hormone Sampling and Analysis
This guide addresses common challenges researchers face when investigating circadian rhythms in hormonal systems, particularly in the context of medication interference studies.
FAQ: Pre-Analytical Phase
Q: My hormonal assay results, particularly for melatonin, show high variability between participants. What could be the cause?
- A: Uncontrolled light exposure is a primary culprit. Light is the most potent zeitgeber (time-giver) and can acutely suppress melatonin production [1]. Ensure participants are in dim light conditions for several hours before and during sample collection for melatonin assessment. The use of "Dim Light Melatonin Onset" (DLMO) protocols is the gold standard for phase determination [2].
Q: I am observing inconsistent cortisol rhythms in my cohort. What pre-analytical factors should I verify?
- A: Inconsistent rhythms can stem from poor control of wake-up times and the cortisol awakening response (CAR). Cortisol secretion has a strong circadian rhythm with its highest pulse around wake-up time [1]. Standardize wake-up times across study participants and document the exact time of each sample. Also, control for stress, as it can activate the HPA axis independently of the circadian clock.
Q: How can I account for the effects of investigational medications on core clock gene expression?
- A: Many drugs can directly or indirectly influence the molecular clock. When possible, analyze the 24-hour expression profile of core clock genes (e.g., ARNTL1, PER2, NR1D1) in the target tissue alongside hormone measurements [2]. This allows you to distinguish whether a drug alters hormonal rhythms by directly resetting the local tissue clock (a zeitgeber effect) or by affecting downstream hormonal pathways without changing the core clock phase (a rhythm driver or tuning effect) [1].
FAQ: Analytical and Interpretation Phase
Q: Blood sampling is invasive and limits frequency. What is a robust alternative for circadian phase assessment?
- A: Saliva is a validated, non-invasive biological material for circadian rhythm analysis [2]. It allows for high-frequency, at-home sampling and can be used to measure both hormonal levels (cortisol, melatonin) and core clock gene expression rhythms from the same sample, providing a multi-modal assessment of circadian phase [2].
Q: How many timepoints are needed to reliably determine a participant's circadian phase?
- A: While more timepoints provide a higher-resolution rhythm, studies have shown that protocols sampling at 3-4 time points per day over 2 consecutive days can yield robust and stable circadian profiles for core clock genes in saliva [2]. This balance between practical feasibility and data robustness is suitable for clinical applications.
Q: My data shows a disconnect between the central SCN clock phase and a peripheral hormone rhythm. Is this possible?
- A: Yes. While the SCN is the master pacemaker, peripheral clocks in organs like the liver, adrenal gland, and pineal gland can be reset by non-photic cues. The most potent cue is the feeding-fasting cycle [1] [3]. An investigational drug that alters meal timing or composition could therefore dissociate peripheral hormonal rhythms from the central light-entrained SCN rhythm.
Experimental Protocols for Circadian Hormone Research
Protocol 1: Assessing Circadian Phase via Salivary Biomarkers
This non-invasive protocol is ideal for human studies, especially those investigating medication effects on circadian timing.
- Participant Preparation: Instruct participants to maintain a consistent sleep-wake schedule for at least one week prior to sampling. During the sampling period, enforce dim light conditions (<10 lux) from 2 hours before the first sample until the end of the protocol.
- Sample Collection: Collect saliva samples at 3-4 pre-defined time points per day (e.g., upon waking, 30 minutes post-waking, afternoon, before bed) for 2 consecutive days. Use a standardized preservative like RNAprotect at a 1:1 ratio with saliva to stabilize RNA for gene expression analysis [2].
- Sample Processing:
- Centrifuge samples to separate cellular material from supernatant.
- Aliquot supernatant for hormone analysis (melatonin, cortisol) via ELISA or LC-MS.
- Extract total RNA from the cell pellet for gene expression analysis of core clock genes (e.g., ARNTL1, PER2, NR1D1) via qRT-PCR.
- Data Analysis: Determine the acrophase (time of peak) for each analyte. Correlate the acrophases of hormone levels and gene expression to understand the coupling between the local clock and hormonal output.
Protocol 2: Investigating Drug-Induced Circadian Disruption in Cell Models
This in vitro protocol helps determine if a medication directly interferes with the core molecular clockwork.
- Cell Culture and Synchronization: Culture cells containing a functional circadian clock (e.g., primary fibroblasts, engineered reporter cell lines). Synchronize the cellular clocks by treating with a high concentration of dexamethasone (100 nM) or serum shock for 2 hours [1].
- Drug Treatment: After synchronization, wash out the synchronizing agent and apply the investigational medication at physiologically relevant concentrations. Include vehicle-only controls.
- Sample Harvesting: Collect cell lysates every 4-6 hours over a period of at least 48 hours post-synchronization.
- Readouts:
- Gene Expression: Analyze mRNA levels of core clock genes (Bmal1, Per2, Rev-Erbα) via qRT-PCR.
- Protein Expression: Analyze oscillation of clock proteins (e.g., BMAL1, PER2) via western blotting or immunocytochemistry.
- Analysis: Compare the period, phase, and amplitude of oscillations between drug-treated and control cells to quantify the drug's impact on the core clock.
Quantitative Data on Circadian Hormonal Rhythms
The following table summarizes key hormonal rhythms relevant to medication interference studies.
Circadian Hormone Profiles and Their Regulation
| Hormone | Source Organ | Peak Phase (in Diurnal Humans) | Primary Regulator | Potential for Medication Interference |
|---|---|---|---|---|
| Melatonin | Pineal Gland | Night (during sleep) [1] | SCN via light input; acutely suppressed by light [1] | High (e.g., via beta-blockers, SSRIs) |
| Cortisol | Adrenal Cortex | Early morning, around wake-time (Cortisol Awakening Response) [1] | SCN (via HPA axis); adrenal clock gating [1] | High (e.g., via corticosteroids, anti-inflammatories) |
| Growth Hormone (GH) | Pituitary Gland | Early during sleep [1] | Sleep stage (non-REM sleep) [1] | Moderate (e.g., via GABA-ergic drugs) |
| Leptin | Adipose Tissue | Night [4] | Feeding-fasting cycle; sleep-wake cycle [4] | High (e.g., via drugs affecting appetite or metabolism) |
| Ghrelin | Stomach | Before meal times [4] | Feeding-fasting cycle [4] | High (e.g., via drugs affecting appetite or motility) |
Signaling Pathways and Experimental Workflows
Core Molecular Clock Feedback Loop
The following diagram illustrates the primary transcriptional-translational feedback loop of the mammalian circadian clock, which can be a direct target of pharmacological intervention.
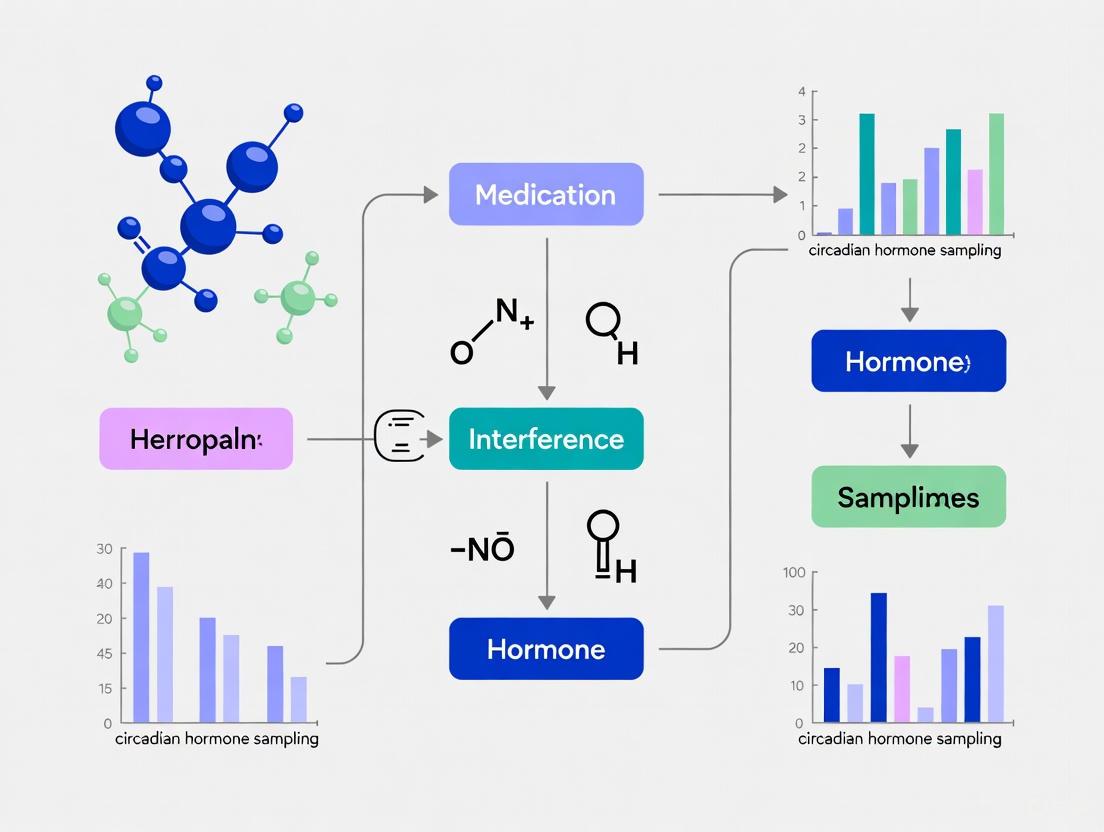
Circadian Hormone Sampling Workflow
This diagram outlines the integrated experimental workflow for non-invasive circadian phase assessment in human subjects, suitable for drug study cohorts.
The Scientist's Toolkit: Research Reagent Solutions
Essential Materials for Circadian Hormone Sampling Research
| Item | Function & Application | Example Use Case |
|---|---|---|
| Saliva Collection Kit (with RNA stabilizer) | Non-invasive collection and stabilization of RNA from saliva for gene expression studies. | High-frequency, at-home sampling of circadian phase in human subjects [2]. |
| Light Therapy Box / Metered Light Glasses | Provides controlled, bright light exposure for entrainment studies or as a standardized light stimulus. | Testing how a drug affects circadian phase shifts in response to light [5] [6]. |
| Melatonin ELISA or LC-MS Kit | Quantifies melatonin levels in saliva or plasma. Essential for determining DLMO, the gold standard phase marker. | Precisely measuring the timing of the circadian signal for sleep onset in medication trials [2]. |
| Cortisol ELISA Kit | Quantifies cortisol levels in saliva, serum, or plasma. | Assessing HPA axis rhythmicity and the impact of stress-related medications on circadian cortisol peaks [1] [2]. |
| qRT-PCR Assays for Core Clock Genes | Measures the expression rhythm of genes like ARNTL1 (BMAL1), PER2, and NR1D1 (REV-ERBα). | Determining if a drug acts directly on the molecular clockwork in peripheral tissues [2]. |
| Dexamethasone | A synthetic glucocorticoid used to synchronize cellular clocks in in vitro models. | Establishing a synchronized rhythm in fibroblast or cell-line cultures to test drug effects on period and phase [1]. |
Molecular Mechanisms of Medication Interference with Clock Gene Expression
The mammalian circadian clock is a cell-autonomous system governed by a network of core clock genes that form transcriptional-translational feedback loops (TTFLs) with a near-24-hour periodicity [7] [8]. The central pacemaker in the suprachiasmatic nucleus (SCN) coordinates rhythms throughout the body, but peripheral clocks exist in virtually all tissues [9]. These molecular clocks regulate the timing of physiological processes, including sleep-wake cycles, metabolism, hormone secretion, and immune function [8] [10].
Medications can interfere with clock gene expression through multiple molecular mechanisms: by directly binding to core clock components, altering post-translational modifications of clock proteins, affecting epigenetic regulation of clock genes, or disrupting the synchronizing signals that entrain circadian rhythms [11] [12]. Understanding these interference mechanisms is crucial for both predicting chronopharmacological interactions and developing novel circadian-targeted therapies.
Key Molecular Targets for Medication Interference
Core Clock Transcription Factors
The BMAL1-CLOCK heterodimer serves as the primary activator of circadian transcription, making it a prime target for pharmacological intervention [12].
Table 1: Core Clock Proteins as Direct Drug Targets
| Target Protein | Function in Circadian Clock | Known Pharmacological Modulators | Mechanism of Interference |
|---|---|---|---|
| BMAL1 | Forms heterodimer with CLOCK; binds E-box elements to drive transcription of PER, CRY, REV-ERB, ROR genes | CCM (Core Circadian Modulator) [12] | Binds PAS-B domain, causing conformational changes that alter transcriptional activity |
| CLOCK | Heterodimerizes with BMAL1; histone acetyltransferase activity | CLK8 [12] | Binds bHLH segment, modulating transcriptional activity |
| REV-ERBα/β | Nuclear receptors that repress BMAL1 transcription | Synthetic ligands (e.g., SR9009, SR9011) [11] | Agonism enhances repression of BMAL1 transcription |
| RORα/γ | Nuclear receptors that activate BMAL1 transcription | Inverse agonists [11] | Suppress transcriptional activation of BMAL1 |
Recent research has demonstrated that the BMAL1 protein architecture is inherently configured to enable small molecule binding [12]. The development of CCM (Core Circadian Modulator), which targets the cavity in the PAS-B domain of BMAL1, represents a breakthrough in directly targeting core clock components. CCM binding causes the cavity to expand, leading to conformational changes in the PAS-B domain and altering BMAL1's function as a transcription factor [12].
Post-Translational Regulation Machinery
Casein kinase 1δ/ε (CK1δ/ε) regulates the stability and nuclear localization of PER proteins through phosphorylation [11] [8]. CK1δ/ε-mediated phosphorylation marks PER proteins for degradation via the ubiquitin-proteasome system [11]. The F-Box proteins FBXL3 and FBXL21 target CRY proteins for proteasomal turnover [7] [8]. Mutations in human CK1δ (T44A) and PER2 (S662G) have been linked to Familial Advanced Sleep Phase Disorder (FASPD), highlighting the clinical importance of this regulatory mechanism [8].
Recent research has also identified SUMOylation as a novel layer of circadian regulation. SUMO modification of BMAL1 can enhance its transcriptional activation, while excessive SUMOylation promotes degradation through crosstalk with ubiquitination pathways [11]. SUMOylation of CLOCK influences its nuclear localization and stability, thereby fine-tuning circadian oscillations [11].
Figure 1: Core Circadian Clock Mechanism and Pharmacological Intervention Points. The diagram illustrates the transcriptional-translational feedback loop with key targets for medication interference.
Experimental Protocols for Assessing Medication Interference
Protocol 1: Measuring Circadian Gene Expression in Peripheral Clocks
Objective: To evaluate the effects of test compounds on circadian gene expression rhythms in peripheral tissues or cultured cells.
Materials:
- CD14+ monocytes or other relevant cell types [13]
- RNA isolation kit (e.g., NucleoSpin RNA, Mini Kit) [13]
- Reverse transcription quantitative PCR (RT-qPCR) system
- Primers for core clock genes (PER1, PER2, PER3, NR1D1, NR1D2, CRY1, BMAL1, CLOCK) [13]
- Cell culture equipment and synchronization agents (dexamethasone, forskolin)
Methodology:
- Cell Isolation and Synchronization: Isolate CD14+ monocytes from whole blood using CD14+ microbeads and AutoMACS Pro separator [13]. Synchronize cells using 100 nM dexamethasone or 10 μM forskolin for 2 hours.
- Compound Treatment: Apply test compounds at various concentrations immediately after synchronization. Include vehicle controls.
- Time-Series Sampling: Collect samples every 4-6 hours over a 48-hour period. For human studies, multiple sampling timepoints are critical as single timepoint measurements may not detect phase shifts [13].
- RNA Extraction and Quality Control: Extract total RNA following manufacturer protocols. Assess RNA quality and concentration using spectrophotometry.
- RT-qPCR Analysis: Perform reverse transcription followed by quantitative PCR using validated primer sets for core clock genes. Normalize to reference genes (GAPDH, ACTB).
- Data Analysis: Calculate relative expression using the 2^(-ΔΔCt) method. Analyze rhythmic parameters (period, amplitude, phase) using specialized software (e.g., BioDare2, CircaCompare).
Troubleshooting: If rhythms are dampened quickly, consider lower compound concentrations or different application timing relative to synchronization.
Protocol 2: High-Throughput Screening for BMAL1-Binding Compounds
Objective: To identify and characterize compounds that directly bind to core clock proteins.
Materials:
- Recombinant human BMAL1(PASB) protein [12]
- Fragment libraries for screening
- Protein thermal shift (PTS) assay reagents [12]
- Isothermal titration calorimetry (ITC) system
- Surface plasmon resonance (SPR) system
- Cellular thermal shift assay (CETSA) reagents
Methodology:
- Primary Screening: Use PTS assays to screen fragment libraries for compounds that stabilize BMAL1(PASB). Measure melting temperature (Tm) shifts ≥2°C as initial hits [12].
- Binding Affinity Determination: Confirm direct binding of hits using ITC and SPR. For CCM, Kd values of 1.99±0.38 μM (ITC) and 4 μM (SPR) were observed [12].
- Cellular Target Engagement: Validate binding in cellular contexts using CETSA with HiBiT-tagged BMAL1(PASB). CCM showed EC50 of 10.3 μM in cells [12].
- Selectivity Assessment: Evaluate binding selectivity against related PAS domains (BMAL2, ARNT, ARNT2) using CETSA [12].
- Functional Characterization: Assess effects on circadian oscillations using PER2::Luc reporter systems in U2OS cells. CCM induced dose-dependent alterations in PER2-Luc rhythms [12].
Troubleshooting: If cellular activity doesn't match biochemical binding affinity, check compound permeability and metabolic stability.
Troubleshooting Guides and FAQs
FAQ 1: Why don't we observe consistent clock gene expression changes in our human study samples?
Answer: Clock gene expression oscillates throughout the day, so single timepoint measurements may miss significant effects. Recent research demonstrates that individuals with early and late chronotypes may show similar gene expression at 7 a.m., despite having different circadian phases [13]. This suggests that:
- Multiple sampling timepoints are essential for detecting phase shifts or amplitude changes
- Chronotype assessment should be incorporated into study design using validated questionnaires (MCTQ, MEQ)
- Cell-type specific effects must be considered - analyze specific immune cell populations separately when possible
Solution: Implement a serial sampling design with at least 4 timepoints over 24 hours, stratify analysis by chronotype, and use cosinor analysis to detect rhythm parameter changes.
FAQ 2: How can we distinguish direct clock gene targeting from indirect effects?
Answer: Many medications affect circadian rhythms indirectly through neurotransmitter systems (melatonin, serotonin, GABA, dopamine) or metabolic pathways [11]. To establish direct mechanisms:
- Use in vitro binding assays (ITC, SPR) with recombinant clock proteins
- Perform cellular thermal shift assays (CETSA) to demonstrate target engagement in living cells
- Test effects in genetic knockouts - if a compound requires specific clock genes for its effects, it likely acts directly on the clock machinery
- Evaluate phase-response curves - direct clock targets typically produce characteristic phase-dependent effects
Solution: Implement a tiered approach starting with binding assays, followed by target engagement studies, and finally functional assays in genetically modified systems.
FAQ 3: Our test compound affects circadian behavior in mice but not in cellular models. What could explain this discrepancy?
Answer: This common issue can arise from several factors:
- Metabolic activation: The compound may require metabolic conversion not occurring in cell culture
- Multi-tissue integration: Circadian behaviors emerge from SCN-peripheral clock interactions absent in isolated cells
- Neurohormonal pathways: The compound might act indirectly via glucocorticoid, melatonin, or autonomic signaling
- Concentration differences: Tissue distribution may result in different effective concentrations
Solution: Test metabolites in cellular assays, measure compound concentrations in brain tissue, use SCN slice cultures or organoid models that preserve tissue organization, and assess neuroendocrine markers.
Figure 2: Troubleshooting Workflow for Medication Interference Studies. This decision tree helps diagnose common experimental challenges.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Studying Medication Interference with Clock Genes
| Reagent/Cell Line | Specific Application | Key Features | Experimental Considerations |
|---|---|---|---|
| U2OS PER2::Luc cells | Reporter assay for circadian oscillations [12] | Stable PER2-promoter driven luciferase expression; robust rhythms | Requires serum shock or dexamethasone synchronization; measure bioluminescence for 5+ days |
| Recombinant BMAL1(PASB) | Direct binding studies [12] | Isolated PAS-B domain for structural and binding studies | May not fully recapitulate full-length protein behavior in cells |
| CEMs (Circadian Expression Microarrays) | Transcriptome-wide profiling of circadian gene expression [8] | Capture cycling transcripts beyond core clock genes | Requires 4+ timepoints over 48 hours for reliable rhythm detection |
| CD14+ monocytes | Human peripheral clock studies [13] | Accessible human peripheral clock model; relevant for immune-related drug effects | Expression levels vary by chronotype and sampling time; requires immediate processing |
| Synthetic REV-ERB ligands | Positive control for nuclear receptor targeting [11] | Well-characterized circadian period and phase effects | Can produce off-target effects at high concentrations |
| CK1δ/ε inhibitors | Positive control for post-translational regulation [8] | Modulate PER stability and degradation | Can affect multiple cellular pathways beyond circadian regulation |
Advanced Methodologies and Emerging Technologies
Nanomaterial-Enabled Drug Delivery for Circadian Medicine
Recent advances in nanotechnology offer innovative approaches for targeting circadian clocks. Various nanomaterials, including liposomes, polymeric nanoparticles, and mesoporous silica nanoparticles, enable sustained, targeted delivery of chronobiotics [10]. These systems address key challenges in circadian medicine:
- Temporal targeting: Programmed release at specific circadian times
- Tissue specificity: Functionalized nanoparticles can target specific peripheral clocks
- Combination therapy: Co-delivery of multiple compounds targeting different clock components
Smart drug delivery systems (SDDSs) that respond to physiological cues (temperature, pH, enzyme activity) represent a promising frontier for circadian medicine [10]. These systems could automatically deliver anti-inflammatory medications before daily inflammation peaks, as demonstrated in a mouse model of rheumatoid arthritis using genetically engineered stem cell implants [14].
Chronogenetic Approaches
The emerging field of "chronogenetics" involves engineering cells to respond to circadian signals for therapeutic purposes. Recent work has demonstrated that tissue implants incorporating genetically engineered stem cells can automatically deliver anti-inflammatory medications in response to circadian signals [14]. These implants effectively treated inflammatory flare-ups for up to a month in mice and rapidly resynchronized when the sleep schedule was reversed [14].
Single-Cell Circadian Analysis
Traditional circadian experiments measure population-level rhythms, potentially masking important cell-to-cell heterogeneity. Emerging single-cell technologies enable:
- Detection of circadian phase distributions in heterogeneous cell populations
- Identification of rare cell states with altered circadian parameters
- Characterization of circadian gene expression noise
These approaches are particularly valuable for understanding how medications might selectively affect specific subpopulations of cells within tissues.
Data Analysis and Interpretation Framework
Quantitative Analysis of Circadian Parameters
When assessing medication interference with clock genes, quantify these key parameters:
- Period: The duration of one complete cycle (typically near 24 hours)
- Amplitude: The peak-to-trough difference in expression levels
- Phase: The timing of expression peaks relative to a reference point
- Damping rate: The rate at which rhythms diminish over time in constant conditions
Table 3: Statistical Methods for Analyzing Circadian Drug Effects
| Analysis Method | Application | Software Tools | Interpretation Guidelines |
|---|---|---|---|
| Cosinor Analysis | Detecting rhythmicity in time-series data [13] | Cosinor, CircaCompare | Significant rhythm detected when p < 0.05 for cosine fit |
| JTK_CYCLE | Non-parametric rhythm detection | MetaCycle, BioDare2 | Robust to outliers; appropriate for noisy data |
| Oscillator Models | Modeling complex interactions between clock components | BioDare2, CellWare | Can predict effects of perturbations on system dynamics |
| Principal Component Analysis | Identifying patterns in high-dimensional circadian data | R, Python | Reveals compound-specific signatures of clock interference |
Integration with Omics Data
Modern circadian studies increasingly incorporate multiple data types:
- Transcriptomics: RNA-seq across multiple timepoints
- Proteomics: Assessment of clock protein abundance and modifications
- Phosphoproteomics: Analysis of rhythmic phosphorylation events
- Metabolomics: Measurement of circadian metabolites
Integrative analysis can reveal how medication interference at the clock gene level propagates through downstream regulatory networks to affect physiological outputs.
Impact of Drug Timing (Chronopharmacology) on Endocrine Rhythm Phase and Amplitude
Core Concepts in Chronopharmacology and Endocrine Rhythms
What are the fundamental principles of chronopharmacology that I must understand for endocrine research? Chronopharmacology is the study of how the effects of drugs vary with biological timing and endogenous periodicities, primarily the circadian rhythm. It is divided into two main areas: chronopharmacokinetics (how timing affects drug absorption, distribution, metabolism, and excretion) and chronopharmacodynamics (how timing affects a drug's biochemical and physiological effects on the body) [15]. The endocrine system is under the control of central and peripheral circadian clocks, and its rhythmic secretions are influenced by both endogenous and environmental factors. Administering a drug can disrupt this delicate chrono-organization, altering the phase (timing of peaks/troughs) and amplitude (strength of oscillation) of hormonal rhythms, which is a critical source of interference in circadian hormone sampling research [16].
How is the circadian clock system hierarchically organized? The system is organized as a hierarchical network [17]:
- Master Clock: Located in the suprachiasmatic nucleus (SCN) of the hypothalamus. It is entrained primarily by the light-dark cycle and generates self-sustaining circadian rhythms [15] [18].
- Peripheral Clocks: Found in most cells throughout the body, including endocrine glands and target tissues. These are synchronized by the SCN through various signals, including autonomic nervous system output, hormonal rhythms (e.g., glucocorticoids, melatonin), and behavioral rhythms (e.g., feeding-fasting cycles) [17] [19]. Under normal conditions, these clocks are in phase harmony, but external perturbations like shift work or mistimed drug administration can cause internal desynchronization [17].
What is the molecular mechanism of the circadian clock? The core mechanism is a transcriptional-translational feedback loop involving key clock genes and proteins [17] [20] [19]:
- Activation: The CLOCK and BMAL1 proteins form a heterodimer that binds to E-box elements in the DNA, promoting the transcription of Period (Per) and Cryptochrome (Cry) genes.
- Repression: PER and CRY proteins accumulate, multimerize, and translocate back to the nucleus to inhibit the CLOCK:BMAL1 complex, repressing their own transcription.
- Cycle Renewal: The degradation of PER and CRY proteins allows the cycle to begin anew, with a period of approximately 24 hours. Auxiliary feedback loops involving genes like Rev-Erbα further stabilize this core oscillator [17].
The diagram below illustrates this core molecular machinery.
Troubleshooting Experimental Challenges
FAQ: My hormone assay results are highly variable despite controlled conditions. Could drug timing be a factor? Yes, this is a classic sign of unaccounted-for chronopharmacological interference. Variability can arise from:
- Chronopharmacokinetics: The absorption, distribution, metabolism, and excretion (ADME) of your drug may vary with circadian time. For example, gastric pH and motility, liver enzyme activity (e.g., cytochrome P450 family), and renal blood flow all exhibit circadian rhythms, leading to time-dependent differences in drug concentration at the target site [15] [21].
- Chronesthesy: This refers to rhythmic changes in the susceptibility of a target system (e.g., a hormone-producing cell) to a drug. This can be due to circadian oscillation in receptor number/conformation, secondary messengers, or downstream metabolic pathways, independent of drug pharmacokinetics [21].
- Troubleshooting Action: Standardize the time of drug administration across all experimental subjects and ensure it is documented relative to the light-dark cycle or other synchronizing cues (e.g., feeding time).
FAQ: I have confirmed a drug alters cortisol rhythm. How can I determine if it's a direct effect on the adrenal gland versus an effect on the central SCN clock? Disentangling central vs. peripheral effects is a common challenge. The following experimental workflow can help you systematically identify the site of action.
FAQ: My animal model shows a blunted amplitude for a hormone rhythm after chronic drug treatment. Is this reversible? The reversibility of rhythm disruption depends on the drug, dose, and treatment duration. Amplitude dampening suggests a weakening of the underlying oscillatory system [20]. To assess reversibility:
- Implement a Drug Washout Period: Cease drug administration and continue to monitor hormonal profiles over multiple cycles.
- Reinforce Zeitgebers: During the washout, ensure a strong and consistent light-dark cycle and control feeding times, as these are potent synchronizers for peripheral clocks [16].
- Evaluate Recovery: Compare the mesor (average level), amplitude, and phase of the hormone rhythm post-washout to pre-treatment baselines. Full recovery suggests transient disruption, while persistent blunting may indicate more profound clock dysfunction that may require active chronotherapeutic intervention to reset [16].
Quantitative Data & Experimental Protocols
Table 1: Circadian Rhythm Parameters for Key Hormones Monitoring these parameters is essential for quantifying drug-induced interference.
| Hormone | Phase (Acrophase) | Amplitude (Representative) | Key Regulator / Driver |
|---|---|---|---|
| Cortisol | Early morning, around wake-time (in diurnal humans) [19] | Peak-to-trough variation of 5-10 μg/dL (approx.) | HPA Axis; SCN via AVP; adrenal clock gating [19] |
| Melatonin | Night-time (peaks ~2-4 AM in darkness) [19] | Can increase >10-fold from daytime baseline [19] | SCN (light-inhibited, dark-activated) [19] |
| Growth Hormone (GH) | Major pulse at sleep onset [19] | - | Sleep-stage dependent (non-REM sleep) [19] |
| Testosterone | Early morning peak [16] | - | Hypothalamic-Pituitary-Gonadal (HPG) Axis [16] |
Table 2: Examples of Drug Chronopharmacodynamics Affecting Endocrine Parameters This table provides documented examples of how timing affects drug action.
| Drug Class / Example | Administration Time | Observed Chronopharmacodynamic Effect | Experimental Context |
|---|---|---|---|
| Statins (HMG-CoA Reductase Inhibitors) [15] [22] | Evening / Night | Increased efficacy in lowering cholesterol | Human clinical practice; cholesterol synthesis peaks at night. |
| Beta-Blocker (Propranolol) [21] | 8 AM - 2 PM | Greater reduction in heart rate | Human study; aligns with high daytime sympathetic tone. |
| Immunotherapy (anti-PD-1/PD-L1) [23] [22] | Morning | Improved patient outcomes | Clinical trials; linked to circadian entry of lymphocytes into tumors in the morning. |
Detailed Experimental Protocol: Assessing Drug Impact on Corticosterone Rhythm in Rodents
This protocol is designed to systematically evaluate how a novel compound affects the phase and amplitude of a key glucocorticoid rhythm.
1. Objective To determine the effects of chronic administration of Drug X on the phase, amplitude, and mesor of the circadian corticosterone rhythm in a murine model.
2. Materials
- Animals: Adult male/female C57BL/6 mice (n=8-12 per group).
- Equipment: Standard light-controlled housing, HPLC-MS/MS system or ELISA kit for corticosterone, automated blood sampling system or equipment for serial saphenous vein sampling.
- Reagents: Drug X and vehicle control.
3. Methodology
- Animal Housing and Synchronization: House mice under a strict 12-hour light/12-hour dark (LD 12:12) cycle for at least two weeks prior to experimentation. Provide food and water ad libitum.
- Experimental Groups:
- Group 1 (Control): Administer vehicle at ZT (Zeitgeber Time) 2.
- Group 2 (Drug A.M.): Administer Drug X at ZT 2.
- Group 3 (Drug P.M.): Administer Drug X at ZT 14.
- Note: ZT0 is lights-on, ZT12 is lights-off.
- Dosing and Sampling: Administer drugs intraperitoneally for 7 consecutive days. On day 8, collect blood samples (e.g., ~20 μL via saphenous vein) from each animal at 4-hour intervals across the 24-hour cycle (e.g., ZT0, 4, 8, 12, 16, 20). Use a cross-sectional design (different animals at each time point) to avoid stress from repeated sampling.
- Hormone Measurement: Process blood samples to plasma and measure corticosterone levels using a validated ELISA or MS/MS method according to manufacturer protocols.
- Data Analysis:
- Cosinor Analysis: Fit the 24-hour corticosterone data for each group to a cosine curve using the formula:
C(t) = M + A*cos(2π(t-φ)/τ), whereMis the mesor,Ais the amplitude,φis the acrophase, andτis the period (fixed at 24 hours). - Statistics: Compare the mesor, amplitude, and acrophase between groups using appropriate statistical tests (e.g., one-way ANOVA with post-hoc tests).
- Cosinor Analysis: Fit the 24-hour corticosterone data for each group to a cosine curve using the formula:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Chrono-Endocrine Research
| Item | Function / Application in Research | Example / Note |
|---|---|---|
| Corticosterone / Cortisol ELISA Kit | Quantifies glucocorticoid levels in serum/plasma to assess HPA axis rhythm. | A high-sensitivity kit is crucial for detecting low trough levels. |
| Melatonin ELISA Kit / RIA | Measures melatonin in plasma/saliva to assess rhythm phase and amplitude; a marker of SCN function. | Requires careful handling due to melatonin's light sensitivity. |
| Antibodies (for IHC/WB): anti-BMAL1, anti-PER2 | Visualizes and quantifies core clock protein expression and localization in tissues (e.g., SCN, liver, adrenal). | Phospho-specific antibodies can assess post-translational regulation. |
| Bmal1-dLuc Reporter Cell Line | Real-time monitoring of molecular clock function in live cells after drug treatment. | Allows for high-throughput screening of clock-modifying compounds. |
| RNA Isolation Kit (Trizol-based) | Extracts high-quality RNA from tissues for qPCR analysis of clock gene expression (e.g., Per2, Rev-Erbα). | Ensure RNase-free conditions for rhythmic gene expression studies. |
| SYBR Green qPCR Master Mix | Quantifies rhythmic mRNA expression of clock-controlled genes (CCGs) in target endocrine tissues. | Use geometric mean of multiple housekeeping genes for stable normalization. |
This guide provides technical support for researchers investigating how common drug classes disrupt circadian hormone rhythms. It covers documented case studies, core experimental methodologies, and troubleshooting for common challenges in this field.
Core Disruption Mechanism: Many drugs interfere with the Transcriptional-Translational Feedback Loop (TTFL) of the core circadian clock [4]. This molecular clock, governed by genes like CLOCK, BMAL1, PER, and CRY, regulates the rhythmic release of hormones such as cortisol and melatonin [24] [4]. Drug-induced disruption can alter the timing, amplitude, and phase of these hormonal rhythms, complicating research and therapeutic outcomes.
The diagram below illustrates this core molecular circuitry and the points where drug classes are known to cause interference.
Documented Case Studies & Data
The following table summarizes quantitative findings from studies on how common drug classes disrupt circadian hormone profiles.
Table 1: Documented Circadian Hormone Disruption by Drug Class
| Drug Class | Specific Drug(s) | Documented Circadian Disruption & Key Findings | Magnitude of Effect / Key Metrics | Primary Research Method |
|---|---|---|---|---|
| Antipsychotics | Various (General class) | Alters expression of core clock genes (CLOCK, Bmal1, Per); linked to treatment-emergent circadian side effects [24]. | - CRY1, NPAS2: Assoc. with unipolar depression [24].- CLOCK, VIP: Assoc. with bipolar disorder [24]. | Genetic association studies (SNP analysis), postmortem brain transcriptome analysis [24]. |
| Cholesterol-Lowering Agents | Atorvastatin | Circadian metabolism by liver enzyme CYP3A4 leads to varying production of toxic metabolites depending on administration time [25]. | Toxicity of atorvastatin was found to be significantly higher at specific times of day [25]. | In vitro testing using engineered human liver models [25]. |
| Analgesics | Acetaminophen (Tylenol) | Metabolism by CYP3A4 and other enzymes follows a circadian rhythm, affecting the production of the toxic metabolite NAPQI [25]. | Production of NAPQI varied by up to 50% based on the time of drug administration [25]. | In vitro testing using engineered human liver models [25]. |
| Calcium Channel Blockers | Nifedipine GITS, Verapamil COER/CODAS | Bedtime dosing demonstrated enhanced efficacy on blood pressure control and reduced side effects compared to morning dosing [26]. | Bedtime dosing was "more effective" for 24-hour BP control, with a "greater reduction in nocturnal BP" in non-dippers [26]. | Multicenter, double-blind, randomized clinical trials [26]. |
| Immunosuppressants / Chemotherapeutics | (Theoretical for many) | Drug metabolism pathways (e.g., involving CYP3A4) are under circadian control, suggesting a widespread potential for time-dependent efficacy/toxicity [25]. | The enzyme CYP3A4 metabolizes ~50% of all drugs and shows a clear circadian cycle [25]. | Gene expression analysis in engineered human livers; >300 liver genes identified with circadian rhythms [25]. |
Essential Experimental Protocols
Protocol 1: Assessing Circadian Phase in Human Subjects
This is the gold-standard method for establishing an individual's endogenous circadian phase in a clinical or research setting.
- Objective: To determine the timing of an individual's circadian pacemaker by measuring the Dim Light Melatonin Onset (DLMO) [27].
- Equipment & Reagents:
- Dim Light Melatonin Onset (DLMO) testing kit (saliva collection kits).
- Salivary melatonin enzyme immunoassay (EIA) or radioimmunoassay (RIA).
- Access to a -20°C freezer for sample storage.
- FedEx or equivalent courier service for sample transport to a CLIA-certified lab [27].
- Pre-Test Conditions: Participants must avoid bright light for at least 2 hours prior to and throughout sample collection. They should refrain from using melatonin supplements for a period (consult lab guidelines) and avoid caffeine, alcohol, and brushing teeth immediately before sampling [27].
- Procedure:
- Begin collection in the early evening, approximately 4-6 hours before habitual bedtime.
- Collect 7 to 9 saliva samples at regular intervals (e.g., every 30 minutes).
- Participants must remain in dim light (< 10-30 lux) during the entire collection period.
- Samples are immediately frozen and shipped overnight on dry ice to the analytical lab.
- Data Analysis: The lab will provide a DLMO profile. The onset is typically defined as the time when melatonin concentration crosses a predetermined threshold (e.g., 3-4 pg/mL) or 2 standard deviations above the mean of the first three baseline samples [27].
Protocol 2: Longitudinal Monitoring of Sleep-Wake Patterns
This protocol is critical for diagnosing circadian rhythm sleep-wake disorders like Non-24 and for monitoring the effects of drugs on rest-activity cycles.
- Objective: To objectively track sleep-wake patterns over extended periods (weeks to months) to identify circadian periodicity and disruptions [28].
- Equipment: Actigraph – a wrist-worn, accelerometer-based device.
- Procedure:
- The actigraph is worn continuously on the non-dominant wrist for a minimum of 14 days, though 4-7 weeks may be necessary to observe the drifting pattern of Non-24 [28].
- Participants simultaneously maintain a sleep diary to record subjective sleep times, wake times, sleep quality, and daytime alertness. This diary is used to validate and calibrate the actigraphy data.
- Data Analysis:
- Actigraphy data is processed using specialized software to calculate sleep onset, offset, duration, and fragmentation.
- The data is plotted over time to visualize the sleep-wake cycle. A diagnosis of Non-24 is supported by a pattern where sleep onset and wake time progressively delay each day (e.g., by 1-2 hours), creating a cycle that rotates around the clock [28].
Protocol 3: Profiling Circadian Gene Expression in Models
This in vitro approach is used to mechanistically study how drugs directly interfere with the molecular clock.
- Objective: To quantify the rhythmic expression of core clock genes and clock-controlled genes (e.g., Bmal1, Per2, Cry1, CYP3A4) in response to drug treatment.
- Model System: Engineered human livers [25], primary cell cultures, or animal tissues.
- Synchronization: Cells or tissues must first be synchronized. This can be achieved with a pulse of a corticosteroid (e.g., dexamethasone) or by manipulating the serum concentration in the culture medium.
- Drug Treatment & Sampling:
- Apply the drug of interest at different circadian times (e.g., at the peak vs. trough of a target gene's expression).
- Collect samples (e.g., for RNA or protein extraction) at regular intervals (e.g., every 3-6 hours) over a period of at least 48 hours [25].
- Downstream Analysis:
- qRT-PCR: To measure mRNA expression levels of target genes.
- RNA-Seq: For an unbiased, genome-wide transcriptomic analysis to identify all cycling genes and affected pathways [25].
- Western Blot / Immunoassays: To confirm changes at the protein level (e.g., for metabolic enzymes like CYP3A4).
Frequently Asked Questions (FAQs)
Q1: Our clinical study results on a drug's effect on cortisol rhythm are inconsistent. What could be the cause? A: Inconsistencies often stem from uncontrolled biological variables.
- Cause 1: Unaccounted for Circadian Time. The effect of a drug can vary dramatically based on the circadian time of administration [26] [25]. Administering a drug at different times across your cohort can introduce significant noise.
- Troubleshooting: Standardize drug administration time for all participants relative to their DLMO or wake time. In animal studies, control for Zeitgeber Time (ZT).
- Cause 2: Underlying Circadian Phase Differences. Participants with advanced, delayed, or misaligned circadian phases will show different hormonal responses [27].
- Troubleshooting: Measure and account for the baseline circadian phase (e.g., via DLMO) of each subject before starting the drug intervention.
Q2: We suspect our drug candidate causes circadian disruption in our animal model. What is the first experiment to confirm this? A: Begin with longitudinal actigraphy monitoring.
- Protocol: House animals with running wheels and monitor their voluntary activity under constant darkness (DD) conditions before, during, and after drug treatment [29].
- Expected Outcome: In DD, the animal's endogenous circadian period (tau) will manifest. A drug that directly perturbs the core clock mechanism will cause a measurable change in the free-running period (tau) or a reduction in the robustness (amplitude) of the activity rhythm.
Q3: How can we determine the best time of day to administer a drug to minimize toxicity? A: Employ in vitro models that recapitulate human circadian metabolism.
- Protocol: Use engineered human liver models that exhibit robust circadian rhythms in drug-metabolizing enzymes like CYP3A4 [25].
- Procedure: Treat these models with your drug at different circadian time points (simulated by the in vitro cycle) and measure the production of toxic metabolites or markers of cellular stress (e.g., NAPQI for acetaminophen) [25]. This approach can identify a toxicity window and a safer administration window.
Q4: How do we distinguish a drug's direct effect on the clockwork versus its indirect effect through altering behavior (e.g., sleep)? A: This requires a carefully designed experimental separation.
- For direct effects: Use in vitro systems (synchronized cells). Any change in the rhythmicity of clock gene expression is a direct effect on the cellular molecular clock [25].
- For indirect effects: In in vivo studies, control for behavioral confounders. For example, if a drug causes sedation, it might disrupt sleep, which in turn can shift the circadian clock. Using pair-fed controls or controlling for activity levels can help isolate the drug's direct effect.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Reagents and Materials for Circadian Disruption Research
| Item / Reagent | Critical Function / Application | Example Use Case |
|---|---|---|
| Salivary Melatonin Assay Kits | Quantifying melatonin concentration in saliva samples for DLMO phase assessment [27]. | Determining the circadian phase of human subjects before and after a drug intervention. |
| Actigraph Devices | Objective, long-term monitoring of rest-activity and sleep-wake cycles in vivo [28]. | Diagnosing Non-24 Sleep-Wake Disorder or monitoring the stability of circadian behavior in animal models and humans. |
| Circadian Reporter Cell Lines | Real-time, non-invasive monitoring of molecular clock activity in live cells (e.g., Bmal1-luciferase). | Screening for drugs that directly alter the period, phase, or amplitude of the core circadian oscillator in vitro. |
| Engineered Human Liver Models | Studying human-specific circadian metabolism and time-dependent drug toxicity in vitro [25]. | Identifying the time of day when metabolism of a drug candidate produces the highest level of toxic metabolites. |
| qPCR Assays for Clock Genes | Profiling the expression levels of core clock genes (e.g., Bmal1, Per1/2, Cry1/2, Rev-erbα). | Validating that a drug treatment alters the molecular clockwork in tissues or cells. |
| Dexamethasone | A synthetic corticosteroid used to synchronize the circadian clocks in cell cultures for in vitro studies. | Creating a synchronized population of cells to study the direct, cell-autonomous effects of a drug on the molecular clock. |
Key Signaling Pathways & Workflow Diagram
The following diagram integrates the core circadian pathway with the experimental workflows for assessing drug-induced disruption, highlighting the logical relationship between molecular mechanisms, investigative methods, and observed outcomes.
Light-Dark Cycles, Feeding Patterns, and Sleep as Confounding Variables in Hormone Sampling
FAQ: Understanding Confounding Variables
What are confounding variables in the context of circadian hormone research?
A confounding variable is a factor other than the one being studied that is associated with both the exposure (e.g., an experimental medication) and the outcome (e.g., hormone levels) [30]. In circadian hormone sampling, if a factor like sleep timing influences both the drug's metabolism and the natural hormone rhythm, it can distort or mask the true relationship between the medication and the hormonal outcome [31] [30].
Why are light-dark cycles considered a major confounder in hormone studies?
The body's master clock, the suprachiasmatic nucleus (SCN), uses light-dark cues to synchronize circadian rhythms [32]. Light exposure directly regulates the secretion of hormones like melatonin [32] [33]. Artificial Light at Night (ALAN) can suppress nocturnal melatonin synthesis, disrupting circadian homeostasis and introducing significant variability in hormone measurements if not controlled [32]. This is a critical consideration when assessing a drug's potential impact on melatonin-related pathways.
How can feeding patterns confound hormone sampling?
Meal timing is a powerful "zeitgeber" (time cue) for peripheral clocks in metabolic tissues like the liver [34]. Consuming meals during the circadian night (when melatonin is high) has been correlated with impaired glucose tolerance [34]. In research, if a medication alters appetite or feeding behavior, or if feeding schedules are inconsistent across study subjects, it becomes nearly impossible to disentangle the drug's direct effects from the metabolic consequences of mistimed feeding on hormones like insulin, ghrelin, and leptin [34] [33].
What is the specific risk of uncontrolled sleep patterns?
Sleep directly regulates the secretion of numerous hormones. For example, growth hormone (GH) release is strongly linked to slow-wave sleep (SWS), and cortisol follows a circadian pattern that is influenced by sleep-wake cycles [33] [35]. Sleep deprivation or disruption activates the hypothalamic-pituitary-adrenal (HPA) axis, leading to elevated cortisol levels [35]. Uncontrolled sleep patterns can therefore be a potent confounder, making it appear that a medication is affecting cortisol or GH levels when the effect is actually due to poor sleep hygiene among participants.
What is "time-varying confounding" and when does it occur?
A time-varying confounder is a factor that changes over the course of a study and continues to influence both the likelihood of an outcome and the exposure status at different time points [36]. In a longitudinal study where participants may start or stop a medication, a variable like stress level is a classic example. Stress can influence the decision to take a medication, is affected by prior medication use, and is independently a risk factor for the outcome (e.g., a specific hormone level). Standard statistical adjustment fails in this scenario because the confounder is also a mediator on the causal pathway [36].
Troubleshooting Guides
Problem: Inconsistent Hormone Measurements Across Study Cohorts
Potential Cause: Uncontrolled light exposure among participants, leading to misaligned central circadian clocks and hormone rhythms [32].
Solutions:
- Protocol Design: Implement a strict "constant routine" protocol in a lab setting to control for light, posture, and feeding [32]. For field studies, provide participants with actigraphs with light sensors to monitor compliance.
- Participant Guidance: Issue standardized instructions mandating avoidance of bright light, especially blue-wavelength light, for 2-3 hours before target bedtime and during nocturnal samplings.
- Statistical Control: Measure and record the timing of light exposure for use as a covariate in statistical models.
Problem: High Variability in Metabolic Hormone Readouts (e.g., Insulin, Glucose)
Potential Cause: Unstandardized feeding patterns and meal timing relative to participants' sleep-wake cycles [34].
Solutions:
- Standardize Meals: Provide all participants with identical, pre-packaged meals for a defined period (e.g., 24-72 hours) prior to sampling.
- Implement Time-Restricted Feeding (TRF): Confine all caloric intake to a specific and biologically appropriate window, such as an 8-10 hour period during the daytime. Early time-restricted eating has been shown to improve glucose levels and substrate oxidation [34].
- Document Thoroughly: Meticulously record the clock time, macronutrient composition, and size of every meal consumed before and during the sampling period.
Problem: Hormone Levels Do Not Follow Expected Circadian Patterns
Potential Cause: Poorly controlled or documented sleep-wake schedules, leading to circadian disruption or misalignment [33] [35].
Solutions:
- Verify Sleep: Use polysomnography (PSG) or actigraphy to objectively verify sleep timing, duration, and architecture (e.g., SWS, REM) during the study period, rather than relying on self-report [33].
- Stabilize Schedules: Require participants to maintain a fixed sleep-wake schedule (e.g., +/- 30 minutes) for at least one week prior to sampling, verified by actigraphy and sleep diaries.
- Account for Chronotype: Assess participants' innate chronotype (morningness/eveningness) using standardized questionnaires and consider it as a stratifying variable in the analysis [37] [38].
Problem: Suspected Confounding by an Unmeasured Variable
Potential Cause: A factor that influences both the independent and dependent variable was not identified or recorded, making statistical control impossible [31] [30].
Solutions:
- Design Phase: Use restriction by enrolling a homogenous population (e.g., narrow age range, same sex) to eliminate confounding by those factors [31]. For drug studies, use an active comparator design instead of a placebo/no-treatment group to mitigate confounding by indication [31].
- Analysis Phase: Employ propensity score methods (matching or weighting) to create a balanced pseudo-population where treated and untreated subjects have similar distributions of measured confounders [31]. For complex time-varying confounding, advanced methods like G-methods (e.g., inverse probability of treatment weighting) may be necessary [31] [36].
Experimental Protocols for Controlling Confounders
Protocol 1: Controlled Laboratory Sampling for Circadian Hormone Profiles
This protocol is designed to isolate endogenous circadian rhythms from masking effects.
1. Pre-Study Stabilization (7-10 Days at Home): * Participants maintain a fixed 8-hour sleep schedule aligned with their habitual timing. * Adherence is monitored via wrist actigraphy and call-in time stamps. * Meals are standardized and consumed at the same clock times each day.
2. Laboratory Admission (≥ 24 Hours Before Sampling): * Participants enter a laboratory environment free from time cues ("temporal isolation"). * The light-dark cycle is controlled and set to the participant's habitual schedule.
3. Constant Routine Protocol (Initiated for ≥ 18 Hours): * Participants remain in a semi-recumbent posture. * Wakefulness is maintained under dim light conditions (< 10 lux). * Nutritional intake is distributed evenly across the protocol in the form of small, isocaloric snacks every hour. * This protocol unmasking the endogenous circadian rhythm by holding constant the behavioral and environmental factors that normally mask it [32].
4. Hormone Sampling: * Blood samples are drawn frequently (e.g., every 60 minutes) via an indwelling catheter. * Key hormones to assay: Melatonin, Cortisol, GH, TSH, Leptin, Ghrelin [33].
Protocol 2: Standardized Field-Based Sampling for Medication Studies
This protocol maximizes ecological validity while imposing key controls to minimize confounding.
1. Participant Selection and Stratification: * Recruit participants based on similar chronotypes (e.g., intermediate types only) [38]. * Stratify randomization by age, sex, and BMI.
2. Pre-Sampling Control Period (5-7 Days): * Sleep: Fixed sleep-wake schedule (± 1 hour), verified by actigraphy. * Light: Instructions to avoid bright light after sunset and use blue-light blocking glasses if using electronic devices. * Feeding: Consume all calories within a consistent 10-12 hour daytime window (e.g., 08:00 a.m. to 07:00 p.m.). The final meal before sampling should be standardized.
3. Sampling Day: * Time Stamping: Record the exact clock time of every sample. * Context Recording: Document recent activity, posture, and food intake prior to each sample. * Wake-Time Sampling: For morning cortisol, sample immediately upon waking (while still in bed) and again at 30-minute intervals.
Data Presentation: Circadian Hormone Reference Ranges
Table 1: Peak Secretion Timing of Key Hormones Under Controlled Conditions This table summarizes the typical circadian phase of hormone peaks, which serves as a baseline for detecting deviations caused by experimental manipulations or confounders. [33]
| Hormone | Typical Peak Time (Circadian Phase) | Primary Regulator (Circadian/Sleep) | Key Confounding Variables to Control |
|---|---|---|---|
| Melatonin | 02:00 - 04:00 a.m. (Biological night) | Circadian (Darkness) | Light exposure, posture |
| Cortisol | ~30 mins after wake-time (Biological morning) | Circadian (ACTH surge) | Sleep timing, stress, wake time |
| Growth Hormone (GH) | Early part of nocturnal sleep | Slow-Wave Sleep (SWS) | Sleep depth/architecture, age |
| Thyroid-Stimulating Hormone (TSH) | Middle of the biological night | Circadian | Sleep deprivation, SWS |
| Testosterone (TT) | Early morning hours | REM Sleep | Sleep structure, age |
| Leptin | Biological night | Circadian/Sleep | Meal timing, energy balance |
| Prolactin (PRL) | During sleep | Sleep-Wake Cycle | Sleep duration |
Table 2: Common Confounding Variables and Methodological Controls
| Confounding Variable | Impact on Hormone Sampling | Recommended Control Methods |
|---|---|---|
| Light at Night | Suppresses melatonin; disrupts central clock timing [32]. | Dim light conditions before/during sampling; actigraphs with light sensors. |
| Irregular Meal Timing | Desynchronizes peripheral clocks; alters glucose, insulin, ghrelin [34]. | Time-restricted feeding; standardized meal composition. |
| Sleep Deprivation / Disruption | Elevates cortisol; blunts GH amplitude; alters TSH [33] [35]. | Actigraphy/PSG; fixed sleep schedules; controlled lab environment. |
| Posture & Activity | Affects plasma volume and hormone concentration. | Controlled posture (semi-recumbent) during sampling in lab studies. |
| Chronotype | Causes phase shifts in rhythms (e.g., earlier in morning types) [38]. | Chronotype assessment; stratification in analysis. |
Signaling Pathways and Experimental Workflows
Diagram 1: Hypothalamic-Pituitary-Adrenal (HPA) Axis and Key Confounders
This diagram illustrates the pathway of cortisol regulation and where major confounding variables can interfere, potentially creating the illusion of medication interference.
Diagram 2: Experimental Workflow for Controlling Confounders
This flowchart outlines a systematic experimental workflow to identify and control for key confounding variables in circadian hormone sampling research.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Materials for Confounder-Controlled Circadian Research
| Item | Function & Importance in Controlling Confounders |
|---|---|
| Actigraphs | Worn like a watch to objectively monitor sleep-wake cycles, rest/activity patterns, and (if equipped with light sensors) ambient light exposure. Critical for verifying participant compliance with stabilization protocols outside the lab [37]. |
| Portable Polysomnography (PSG) | The gold standard for objective measurement of sleep architecture (SWS, REM). Essential for studies where the outcome hormone is tightly linked to a specific sleep stage (e.g., GH and SWS) [33] [35]. |
| Dim-Light Melatonin Onset (DLMO) Kit | A standardized protocol to assess the timing of the central circadian clock. Involves serial saliva or plasma sampling under dim light conditions. Used to establish a baseline circadian phase for each participant [32]. |
| Chronotype Questionnaires (e.g., MEQ) | Self-report tools like the Morningness-Eveningness Questionnaire (MEQ) to categorize participants' innate circadian phase preferences. Allows for stratification in analysis to avoid confounding by phase differences [37] [38]. |
| Controlled Light Environments/Boxes | Light boxes that can deliver specific light intensities and spectra. Used in lab studies to provide a standardized light stimulus or to create a controlled photoperiod, eliminating confounding from variable environmental light [32]. |
| Standardized Meal Kits | Pre-portioned, nutritionally defined meals and snacks. Eliminates confounding from variations in meal size, composition, and timing, ensuring that feeding is a controlled variable, not a confounder [34]. |
| Radioimmunoassay (RIA) / ELISA Kits | Specific kits for assaying hormone levels from blood, saliva, or urine. High-sensitivity and low-cross-reactivity kits are essential for accurately measuring the low concentrations and pulsatile secretion of many circadian hormones [33]. |
Protocol Design and Sampling Strategies for Reliable Circadian Data
Gold-Standard Biomarkers for Circadian Phase Assessment in Clinical Trials
Biomarker Comparison Table
The following table summarizes the key characteristics of established and emerging biomarkers for circadian phase assessment.
Table 1: Gold-Standard and Emerging Biomarkers for Circadian Phase Assessment
| Biomarker | Biological Matrix | Key Measured Analytes | Key Advantages | Key Limitations & Sources of Interference |
|---|---|---|---|---|
| Dim Light Melatonin Onset (DLMO) [18] [27] | Saliva, Plasma | Melatonin | Considered the gold standard; directly reflects the timing signal from the central pacemaker (SCN) [18]. | Requires strict dim-light conditions and frequent sampling over 5-6 hours; inconvenient for large-scale studies [39] [18]. |
| Core Body Temperature (CBT) [18] | Rectal, Gastrointestinal | Core Body Temperature | Robust rhythm generated by the SCN [18]. | Rhythm is easily masked by activity, sleep-wake cycles, and food intake [18]. |
| Transcriptomic Biomarkers (e.g., BodyTime) [39] | Blood (Monocytes) | Expression of a small gene set (e.g., 12 genes) | Requires only a single blood sample; high accuracy comparable to DLMO [39]. | Performance can be affected by the specific training set and experimental conditions used for development [40]. |
| Blood Clock Correlation Distance (BloodCCD) [41] | Blood (Whole Blood) | Expression correlation of 42 circadian-related genes | Provides a single score for circadian disruption; not dependent on time of sample collection [41]. | Novel method requiring further validation; performance in various disease and medication contexts is under investigation [41]. |
Detailed Experimental Protocols
Dim Light Melatonin Onset (DLMO) Assessment
This protocol outlines the standard procedure for determining DLMO from saliva, which is critical for defining an individual's circadian phase in research and clinical trials [18] [27].
- Primary Materials: Saliva collection kits (salivettes), freezer (-20°C or lower), portable cooler, pre-paid shipping materials [27].
- Sample Collection:
- Begin collection 6-8 hours before habitual bedtime [27].
- Collect 7 to 9 saliva samples at regular intervals (e.g., every 30-60 minutes) [18] [27].
- Maintain strict dim-light conditions (<10-30 lux) before and during the entire collection period. Participants should avoid overhead lights and use dim, indirect light if necessary.
- Participants should refrain from eating, drinking (except water), brushing teeth, or smoking for at least 30 minutes before each sample.
- Sample Handling:
- Freeze samples immediately after collection.
- Ship frozen on dry ice to a CLIA-certified laboratory for analysis [27].
- Data Analysis:
- Melatonin concentration is typically determined by immunoassay.
- DLMO is calculated as the time point when melatonin concentration crosses a predefined threshold (often 3-4 pg/mL) or a certain percentage above the baseline mean [18].
Blood-Based Transcriptomic Phase Assessment (BodyTime Assay)
This protocol describes a method for estimating internal circadian time from a single blood draw using a targeted gene expression panel [39].
- Primary Materials: PAXgene Blood RNA tubes, RNA extraction kit (e.g., Qiagen PAXgene Blood RNA Kit), globin RNA depletion kit (e.g., GLOBINclear), NanoString nCounter platform and reagents, multiplexed gene expression codeset for the target genes [39] [41].
- Sample Collection and Processing:
- Gene Expression Profiling:
- Use the NanoString nCounter platform for multiplexed gene expression analysis without the need for reverse transcription or amplification [39].
- Hybridize the extracted RNA to the reporter codeset for the specific biomarker genes (e.g., the 12-gene panel from the BodyTime assay) and the capture probeset overnight.
- Data Analysis and Phase Prediction:
- Count the fluorescent barcodes on the nCounter system.
- Normalize the raw data using internal positive controls and housekeeping genes.
- Input the normalized gene expression data into a pre-trained algorithm (e.g., based on ZeitZeiger) to compute the predicted internal circadian time [39].
Diagram 1: Transcriptomic biomarker workflow from sample to result.
Troubleshooting Common Experimental Issues
Immunoassay and Multiplex Assay Performance
Problem: High variability or low signal in immunoassays (e.g., melatonin or cytokine detection).
- Cause & Solution: Improper sample handling and preparation.
- Action: Always vortex and centrifuge thawed samples at 10,000 × g for 5-10 minutes to remove debris and lipids. For viscous samples like plasma, repeat centrifugation if needed [42].
- Cause & Solution: Inconsistent pipetting technique.
- Action: Use calibrated pipettes, hold the pipette at a consistent angle, and employ reverse pipetting for more precise fluid additions [42].
- Cause & Solution: Incomplete or inconsistent plate washing.
- Action: Use a magnetic separation block and ensure the plate is firmly attached. For manual washing, decant and blot the plate gently. Use the wash buffer provided in the kit [42].
- Cause & Solution: Low bead counts in multiplex bead-based assays (e.g., Luminex).
- Action: Resuspend beads in Wash Buffer (instead of Sheath Fluid) just before reading to prevent clumping. Ensure the instrument is regularly cleaned and calibrated [42].
Problem: Suspected medication interference with hormone (e.g., melatonin) immunoassay.
- Cause & Solution: Cross-reactivity of the drug or its metabolites with the assay antibody.
- Action: Consult the assay manufacturer's data sheet for known cross-reactivities. If possible, use a more specific method like LC-MS/MS for confirmation. Note the medication and dosing schedule of participants as a potential confounding variable.
Transcriptomic Assay Performance
Problem: Poor performance of a transcriptomic biomarker when applied to a new study cohort.
- Cause & Solution: The biomarker was trained on data from experimental conditions (e.g., baseline sleep) that do not match the new study's conditions (e.g., sleep deprivation, shift work).
- Action: Ensure the biomarker has been validated for the specific population and condition of your study. Performance can be significantly degraded when applied to protocols that mimic real-world scenarios like shift work [40].
- Cause & Solution: Overfitting due to a small training set size during biomarker development.
- Action: Select biomarkers developed with established validation concepts and large, diverse training sets to ensure generalizability [40].
Medication Interference in Circadian Hormone Sampling
Many classes of drugs can directly or indirectly interfere with the accurate measurement of circadian hormones, potentially confounding research results.
Table 2: Common Medication Interferences with Circadian Biomarkers
| Medication Class | Example Drugs | Target Circadian Biomarker | Nature of Interference |
|---|---|---|---|
| Beta-Blockers | Propranolol, Atenolol | Melatonin | Suppresses nocturnal melatonin production by blocking adrenergic receptors in the pineal gland [43]. |
| Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) | Ibuprofen, Aspirin | Melatonin | May suppress melatonin synthesis by inhibiting the enzyme N-acetyltransferase [43]. |
| Selective Serotonin Reuptake Inhibitors (SSRIs) | Fluoxetine, Sertraline | Melatonin, Cortisol | Can alter melatonin synthesis and secretion rhythms; impacts HPA axis and cortisol dynamics [43] [44]. |
| Benzodiazepines | Lorazepam, Diazepam | Cortisol | Can blunt the cortisol awakening response and suppress HPA axis activity [43]. |
| Exogenous Glucocorticoids | Prednisone, Dexamethasone | Cortisol | Directly suppresses endogenous cortisol production via negative feedback on the HPA axis [43]. |
| Catecholamines | --- | Core Clock Genes | Can directly reset peripheral clocks (e.g., in the liver) through signaling pathways, altering circadian gene expression [43]. |
Diagram 2: Mechanisms of medication interference with circadian biomarkers.
Frequently Asked Questions (FAQs)
Q1: Why is DLMO considered the gold standard when it is so burdensome?
DLMO is considered the gold standard because melatonin secretion is directly controlled by the central circadian pacemaker, the SCN, and is less susceptible to masking by non-circadian factors like sleep or posture compared to other markers like core body temperature [18]. It provides a direct readout of the central clock's phase.
Q2: Can I use a transcriptomic biomarker to assess circadian phase in shift workers or individuals with irregular sleep schedules?
Caution is advised. The performance of blood-based biomarkers depends heavily on the conditions of the training data. Biomarkers developed under baseline conditions may not translate accurately to protocols involving sleep restriction or desynchronization, such as shift work [40]. Always check the validation scope of the specific biomarker.
Q3: What is the most critical step in the DLMO protocol to ensure accurate results?
Maintaining strict dim-light conditions is paramount. Even brief exposure to ordinary room light can suppress melatonin secretion and dramatically shift or obscure the DLMO, leading to incorrect phase assessment [27].
Q4: How can I control for the effects of medications in my circadian research?
- Documentation: Meticulously record all medications, including dosage and timing, for all participants.
- Exclusion Criteria: Consider excluding participants on medications known to strongly interfere with your primary circadian biomarkers (see Table 2).
- Statistical Control: For medications that cannot be excluded, plan to include them as covariates in your statistical models.
- Pilot Testing: If a participant is on a critical medication, consider running a pilot assay to check for obvious interference.
Q5: Are there emerging biomarkers that could replace DLMO in the future?
Yes, methods like the BodyTime assay (transcriptomic) [39] and BloodCCD (correlation-based) [41] show great promise. Their key advantage is requiring only one or a few samples, greatly reducing participant burden. However, they are still being validated across diverse populations and conditions and are not yet considered a universal replacement for DLMO [40].
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for Circadian Phase Assessment Experiments
| Item | Function/Application | Example(s) |
|---|---|---|
| Salivettes | Hygienic collection and stabilization of saliva samples for hormone (melatonin, cortisol) analysis [27]. | Sarstedt Salivette |
| PAXgene Blood RNA Tubes | Collect and stabilize intracellular RNA from whole blood for transcriptomic biomarker analysis [39] [41]. | BD PAXgene Blood RNA Tubes |
| RNA Extraction Kit | Purify high-quality total RNA from stabilized blood samples. | Qiagen PAXgene Blood RNA Kit [41] |
| Globin RNA Depletion Kit | Improve detection of non-globin transcripts in whole blood RNA-seq by removing highly abundant globin mRNAs [41]. | Thermo Scientific GLOBINclear Kit |
| NanoString nCounter Platform | Multiplexed digital quantification of gene expression without amplification, used in validated transcriptomic assays [39]. | NanoString nCounter SPRINT/FLEX |
| Luminex xMAP Technology | Multiplexed quantification of soluble analytes (e.g., cytokines) using magnetic beads and fluorescent detection [42]. | MILLIPLEX MAP Assays |
| Handheld Magnetic Separator | Efficiently separate magnetic beads from solution during wash steps in immunoassays [42]. | EMD Millipore Magnetic Separator Block |
| Chloronaphthol (4-CN) | Substrate for horseradish peroxidase (HRP) used in enzymatic signal enhancement assays on some biosensor platforms [45]. | 4-Chloro-1-naphthol |
Optimal Sampling Frequencies and Timing for Capturing Endocrine Rhythms
Troubleshooting Guides
Guide 1: Resolving Inconsistent Circadian Phase Estimates
Problem: Measurements from different biomarkers (e.g., melatonin vs. cortisol) provide conflicting estimates of a subject's circadian phase.
Explanation: Different circadian outputs can be influenced by varying masking factors. For instance, cortisol is strongly affected by stress and posture, while melatonin is more robust but requires strict dim light conditions [46] [2]. The peripheral clocks in different tissues may also show slight phase variations [47] [2].
Solution:
- Prioritize Dim Light Melatonin Onset (DLMO): When possible, use DLMO as the primary phase marker, as it is considered the gold standard and is less susceptible to non-photic masking [46].
- Control conditions strictly: For all biomarkers, implement strict protocols regarding posture, light exposure, and meal timing during sampling [46].
- Use a constant routine protocol: If feasible and ethically permissible, use a constant routine protocol to unmask the endogenous circadian rhythm by keeping participants in a constant environment of wakefulness, posture, and caloric intake [46].
- Cross-validate with a second marker: In clinical settings, if DLMO is not possible, use a combination of markers (e.g., wrist temperature and cortisol) and compare the results to identify potential masking effects [48] [2].
Guide 2: Addressing High Participant Burden in Dense Sampling
Problem: Frequent sampling over a 24-48 hour period leads to poor participant compliance and increased dropout rates.
Explanation: Capturing the full profile of a circadian rhythm traditionally requires sampling every 1-2 hours for at least 24 hours, which is burdensome [2]. This is often necessary for robust curve fitting and accurate determination of rhythm parameters like acrophase (peak time) and amplitude.
Solution:
- Optimize sampling strategy: Recent research suggests that with advanced computational methods, fewer time points may be sufficient. One study indicates that as few as 3-4 strategic time points per day over 2 days can be used to assess circadian gene expression in saliva [2].
- Choose less invasive methods: Utilize non-invasive sampling materials like saliva, which participants can collect themselves at home, rather than repeated blood draws [2].
- Implement careful timing: Schedule sampling times to capture key phases of the rhythm, such as the anticipated rise, peak, and decline of the hormone of interest, rather than equidistant intervals [46].
Guide 3: Mitigating Medication Interference on Circadian Biomarkers
Problem: The very medications being studied are suspected of altering the circadian rhythms you are trying to measure.
Explanation: Many medications, including antipsychotics and antidepressants, can directly or indirectly affect the circadian system. They may alter the expression of core clock genes (e.g., CLOCK, BMAL1, PER), shift sleep-wake cycles, or modify the levels of circadian hormones like melatonin and cortisol [24]. This creates a confounding loop in research.
Solution:
- Establish a baseline: If ethically possible, measure circadian parameters (e.g., DLMO, actigraphy) in a medication-free baseline period before administering the drug [24] [46].
- Monitor clock gene expression: In addition to hormones, track the expression of core clock genes in accessible tissues like saliva or blood cells. This can provide a more direct measure of the medication's impact on the molecular clock [24] [2].
- Use a control group: Include a matched control group that does not receive the medication but undergoes identical sampling and monitoring procedures.
- Longitudinal sampling: Design studies with multiple sampling time points over weeks to track the evolution of circadian changes in response to medication, rather than relying on a single snapshot [24].
Frequently Asked Questions (FAQs)
Q1: What is the minimum number of sampling time points needed to reliably estimate a circadian rhythm?
A: While 24-hour profiling with sampling every 1-2 hours is ideal, emerging methods show promise with fewer points. For salivary gene expression, 3-4 time points per day over 2 consecutive days can provide a reliable circadian profile. The exact minimum depends on the biomarker and the computational model used for analysis [2]. For DLMO, 4-6 samples in the evening (e.g., every 30-60 minutes before habitual bedtime) are typically sufficient [46].
Q2: How does the choice of biomarker impact the required sampling frequency and timing?
A: The optimal schedule is entirely biomarker-dependent. The table below summarizes the key requirements for common circadian biomarkers.
| Biomarker | Recommended Sampling Frequency | Critical Timing Windows | Key Considerations |
|---|---|---|---|
| Dim Light Melatonin Onset (DLMO) | Every 30-60 minutes in the evening [46] | 5-7 hours before to 1 hour after habitual bedtime [46] | Must be collected under dim light (<10 lux) [46]. |
| Cortisol | Every 1-2 hours, with higher density around the wake-up time [2] | First hour after waking (cortisol awakening response) and the subsequent decline [2] | Highly sensitive to stress, posture, and time of waking [2]. |
| Core Body Temperature (CBT) | Continuous or every 5-10 minutes [48] | Entire 24-hour cycle, with focus on identifying the temperature minimum [46] | Requires a constant routine protocol to unmask the endogenous rhythm from activity effects [46]. |
| Core Clock Gene Expression | Every 3-4 hours or 3-4 strategic time points per day [2] | Should cover anticipated peak and trough times (e.g., morning, afternoon, evening, night) [47] [2] | Tissue-specific (e.g., saliva, blood, buccal mucosa). Rhythm may be dampened or phased-shifted in patient populations [24] [2]. |
Q3: My research involves shift workers. How should I adapt sampling protocols for this population?
A: Sampling in shift workers requires accounting for their misaligned schedule.
- Schedule Sampling by Shift Cycle: Plan sampling across both day and night shifts, or during rest days, to capture the degree of misalignment [46].
- Measure Social Jetlag: Use tools like the Munich Chronotype Questionnaire (MCTQ) to quantify the difference between sleep timing on workdays and free days, which is a key metric in this population [46].
- Focus on Ease of Collection: Prioritize robust and participant-friendly methods like actigraphy and salivary hormones that can be collected in their natural environment [48] [2].
Q4: What are the best practices for at-home self-collection of saliva samples?
A: To ensure high-quality data from self-collected saliva:
- Provide Detailed Training: Give clear, written, and visual instructions on how to collect the sample without contamination.
- Use Stabilization Reagents: Provide containers with RNA-stabilizing agents (e.g., RNAprotect) if measuring gene expression to prevent degradation [2].
- Standardize Collection Procedure: Specify if saliva should be unstimulated or stimulated, as this can affect composition [2].
- Record Exact Timestamps: Require participants to record the precise time of each sample collection.
- Control Light Exposure: For evening melatonin sampling, provide participants with a lux meter or clear instructions to remain in dim light before and during sampling [46].
Experimental Protocols & Methodologies
Protocol 1: Determining Dim Light Melatonin Onset (DLMO)
Principle: DLMO is the gold standard for assessing circadian phase in humans and is defined as the time when melatonin concentration in saliva (or plasma) begins to steadily rise in the evening [46].
Materials:
- Salivette collection tubes
- Freezer (-20°C or -80°C) for sample storage
- Lux meter
- Radioimmunoassay (RIA) or Enzyme-Linked Immunosorbent Assay (ELISA) kits for melatonin
Step-by-Step Method:
- Preparation (1 week before):
- Instruct participants to maintain a consistent sleep-wake schedule.
- Avoid alcohol, caffeine, and nicotine for 24 hours prior to sampling.
- Sampling Day:
- Dim Light Conditions: Beginning at least 5 hours before the participant's habitual bedtime, ensure they are in dim light (<10 lux, verified with a lux meter). They should avoid screens or use blue-light-blocking glasses [46].
- Sample Collection: Every 30 minutes, starting 5-7 hours before bedtime and continuing until 1 hour after bedtime, collect a saliva sample.
- Pre-collection: Participants should not eat or drink anything except water for 15 minutes before each sample. They must rinse their mouth with water 5 minutes before collection.
- Storage: Immediately freeze samples at -20°C or lower.
- Data Analysis:
- Assay melatonin concentrations.
- Plot concentration against clock time.
- Calculate DLMO using a threshold method (e.g., the time when melatonin concentration crosses a fixed threshold, often 3-4 pg/mL, or 2 standard deviations above the average daytime baseline) [46].
Protocol 2: Assessing Circadian Gene Expression in Saliva
Principle: The expression of core clock genes (e.g., ARNTL1 (BMAL1), PER2, NR1D1) oscillates in a circadian manner in peripheral tissues, including salivary cells. This protocol provides a non-invasive method for assessing the molecular clock phase [2].
Materials:
- Standard saliva collection tubes
- RNA-stabilizing solution (e.g., RNAprotect)
- RNA extraction kit
- Reverse Transcription and Quantitative PCR (RT-qPCR) equipment and reagents
- Primers for core clock genes and housekeeping genes
Step-by-Step Method:
- Sample Collection:
- Collect saliva samples (e.g., 1.5 mL) at 3-4 strategic time points per day (e.g., 8:00, 14:00, 20:00, 02:00) for 2 consecutive days [2].
- Immediately mix saliva with an equal volume of RNA-stabilizing solution (1:1 ratio) to preserve RNA integrity [2].
- Record exact collection time and store samples at -80°C.
- RNA Extraction and Analysis:
- Extract total RNA from the saliva samples following the manufacturer's protocol.
- Check RNA concentration and purity (e.g., A260/280 ratio ~1.8-2.0).
- Perform RT-qPCR for target core clock genes and a reference housekeeping gene.
- Data Analysis:
Signaling Pathways and Experimental Workflows
Circadian Clock Molecular Feedback Loop
This diagram illustrates the core transcriptional-translational feedback loop of the mammalian molecular clock, which governs circadian rhythms in the SCN and peripheral tissues.
Circadian Biomarker Sampling Workflow
This workflow outlines the key decision points and methods for designing a study to capture human endocrine rhythms.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function/Application | Technical Notes |
|---|---|---|
| Salivette Tubes | Collection of clean saliva samples for hormone (melatonin, cortisol) or RNA analysis. | Inert polyester swab or passive drool format minimizes contamination [2]. |
| RNA Stabilizing Reagent | Preserves RNA integrity in saliva samples immediately upon collection, preventing degradation prior to extraction. | Products like RNAprotect are used at a 1:1 ratio with saliva [2]. |
| Lux Meter | Quantifies ambient light intensity to ensure adherence to dim light conditions (<10 lux) required for accurate DLMO assessment [46]. | Critical for validating at-home collection protocols. |
| Melatonin ELISA/RIA Kit | Quantifies melatonin concentration in saliva or plasma samples for DLMO calculation. | Requires high sensitivity to detect low pg/mL levels in saliva [46]. |
| RNA Extraction Kit | Isolates high-quality total RNA from saliva samples for subsequent gene expression analysis. | Must be optimized for viscous saliva samples and compatible with stabilizers [2]. |
| qPCR Reagents & Primers | Measures mRNA expression levels of core clock genes (e.g., ARNTL1, PER2, NR1D1). | Primers must be validated for specificity and efficiency in saliva cDNA [2]. |
| Actigraph Device | A wearable sensor that continuously monitors rest and activity cycles, used to estimate sleep patterns and circadian rhythm stability. | Multi-sensor devices that also track light and temperature provide richer data [18] [48]. |
Standardized Protocols for Controlling Masking Factors During Hormone Collection
This technical support center provides troubleshooting guides and frequently asked questions for researchers conducting circadian hormone sampling research. The guidance focuses on controlling masking factors—variables that can obscure true circadian rhythmicity—during the collection, handling, and analysis of hormonal biomarkers such as melatonin and cortisol. Adherence to these standardized protocols is essential for generating reliable, reproducible data in studies investigating medication interference with circadian hormone rhythms.
Troubleshooting Guides
Guide 1: Addressing Pre-Analytical Errors in Hormone Sampling
Pre-analytical errors occur before the sample reaches the laboratory and are a major source of unreliable data [49].
| Error Type | Common Causes | Impact on Hormone Results | Corrective & Preventive Actions |
|---|---|---|---|
| Incorrect Timing | Non-adherence to circadian-driven collection schedules [50]. | Misrepresentation of circadian phase (e.g., DLMO, CAR) [50]. | - Standardize collection times relative to the individual's wake time.- For cortisol, collect immediately upon waking, then at 30, and 45 minutes post-awakening for CAR [50].- For melatonin, use a 4-6 hour sampling window before habitual bedtime for DLMO assessment [50]. |
| Improper Sample Handling | - Clotting: Failure to invert tubes gently after collection [51].- Haemolysis: Vigorous shaking, squeezing fingerpricks [51] [49]. | - Clotted samples cannot be analyzed [51].- Haemolysis can alter potassium, AST, LDH, and hormone levels [49]. | - Invert collection tubes 5-10 times gently; do not shake [51].- For fingerpricks, let blood drip naturally; avoid squeezing [51]. |
| Patient Preparation Errors | - Incorrect posture [49].- Non-fasting when required.- Recent medication/supplement intake [49]. | - Posture changes affect renin, aldosterone, catecholamines [49].- Biotin supplements (>1 week washout) interfere with immunoassays [49]. | - Supine rest for 30 mins pre-collection for catecholamines [49].- Verify fasting status.- Document and standardize medication/supplement washout periods. |
Guide 2: Managing Medication and Substance Interference
Many medications and substances are known to alter circadian hormone secretion profiles [50] [49].
| Interfering Substance | Affected Hormone(s) | Direction of Interference | Recommended Protocol |
|---|---|---|---|
| Beta-Blockers | Melatonin | Suppresses secretion [50]. | Document usage; consider washout period if clinically safe. |
| Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) | Melatonin | Suppresses secretion [50]. | Document usage; standardize timing of administration relative to sampling. |
| Antidepressants | Melatonin | Artificially elevates levels [50]. | Document type and dosage; crucial for psychiatric circadian research. |
| Oral Contraceptives | Cortisol, Melatonin | Alters binding protein levels, can artificially elevate cortisol [50] [52]. | Record usage; consider measuring free hormone levels via LC-MS/MS [52]. |
| Biotin (Vitamin B7) | Various (via immunoassay interference) | Falsely high or low results depending on assay [49]. | Mandatory washout period of at least 1 week before testing [49]. |
Frequently Asked Questions (FAQs)
FAQ 1: What is the gold-standard method for analyzing circadian hormones like melatonin and cortisol to minimize analytical interference?
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) is considered superior for circadian hormone analysis [50] [52]. Compared to immunoassays, LC-MS/MS offers enhanced specificity, sensitivity, and reproducibility, with less susceptibility to cross-reactivity from structurally similar compounds or interfering medications [50] [52]. This is particularly crucial for measuring low-abundance analytes in saliva [50].
FAQ 2: How should we handle the collection of salivary hormones for circadian phase assessment like Dim Light Melatonin Onset (DLMO)?
Salivary DLMO is a reliable, non-invasive marker of circadian phase [50]. Key protocols include:
- Dim Light Conditions: Samples must be collected under dim light (<10-30 lux) to prevent suppression of melatonin secretion [50].
- Sampling Window: A 4-6 hour window before and up to 1 hour after habitual bedtime is typically sufficient [50].
- Sample Integrity: Use salivettes or approved collection devices. Avoid citric acid-stimulated samples if they interfere with the assay. After collection, samples should be frozen at -20°C or lower as soon as possible [50].
FAQ 3: Our study involves patients on multiple medications. How can we account for drug-induced circadian hormone disruption?
- Documentation: Meticulously record all medications, including dose and administration time [49].
- Standardization: Standardize the timing of medication administration relative to hormone collection across all participants where possible.
- Statistical Adjustment: In your statistical analysis plan, include medication use as a potential covariate.
- Consult Resources: Refer to databases and literature on drug-hormone interactions when interpreting results [24].
FAQ 4: What are the most critical factors to control when assessing the Cortisol Awakening Response (CAR)?
- Supervised Timing: The first sample must be taken immediately upon waking (time "0"). Subsequent samples should be collected at precisely 30 and 45 minutes post-awakening [50].
- Patient Compliance: Train participants thoroughly on the protocol. Use electronic monitoring caps for tubes to verify timing compliance.
- Documentation: Record exact sampling times and wake-up time. Note factors like sleep quality the previous night and stress levels, as these can influence CAR [50].
Experimental Workflows & Signaling Pathways
Hormone Sampling Workflow
Analytical Method Decision Pathway
The Scientist's Toolkit: Research Reagent Solutions
| Essential Material | Function in Hormone Collection & Analysis |
|---|---|
| LC-MS/MS System | Provides high-specificity measurement of melatonin, cortisol, and other hormones, minimizing cross-reactivity issues common in immunoassays [50] [52]. |
| Salivettes | Specialized devices for hygienic and standardized collection of saliva samples for hormone analysis. |
| Dim Light Spectrometer | Verifies ambient light levels are below the melatonin suppression threshold (e.g., <10 lux) during DLMO sampling [50]. |
| EDTA or Serum Gel Tubes | Appropriate blood collection tubes for hormone stability. Follow correct order of draw to avoid cross-contamination [49]. |
| Electronic Monitoring Caps | Track the precise timing of sample collection (e.g., for CAR) to verify participant compliance. |
| High-Quality Freezers (-80°C) | Ensure long-term stability of hormone samples prior to batch analysis. |
Incorporating Chronotherapy Principles into Drug Dosing Schedule Design
Frequently Asked Questions (FAQs)
FAQ 1: What is the fundamental rationale for applying chronotherapy in drug development? The fundamental rationale is that the physiology of the human body, including metabolism, hormone secretion, immune function, and cellular proliferation, is governed by 24-hour circadian rhythms. These rhythms are regulated by a central pacemaker in the suprachiasmatic nucleus (SCN) and peripheral clocks in virtually every cell. Consequently, drug pharmacokinetics (how the body processes a drug) and pharmacodynamics (how a drug affects the body) can vary significantly depending on the time of administration. Aligning drug dosing with these intrinsic biological rhythms can maximize efficacy and minimize toxicity [53] [54] [55].
FAQ 2: How can a researcher account for inter-individual differences in circadian timing? Individual circadian timing, known as chronotype, can vary by several hours between people. To account for this in studies, researchers should stratify participants by chronotype. Assessment methods include:
- Validated Questionnaires: The Morningness-Eveningness Questionnaire (MEQ) or the Munich Chronotype Questionnaire (MCTQ) can determine diurnal preference [56] [37].
- Wearable Biosensors: Devices that continuously monitor locomotor activity, body temperature, or heart rate can provide objective phase markers [56] [57].
- Biomolecular Snapshot Methods: Novel assays can estimate an individual's circadian phase from one or two biosamples (e.g., blood, saliva) by analyzing circadian transcripts, proteins, or metabolites [56].
FAQ 3: What are the primary challenges in implementing chronotherapy in clinical practice? Despite a strong mechanistic foundation, several challenges hinder broad clinical implementation:
- Lack of Prospective Trials: Most evidence comes from retrospective studies, which are susceptible to bias. There is a scarcity of large, prospective, randomized clinical trials [56] [53].
- Protocol Complexity: Moving away from a "one-size-fits-all" dosing schedule requires personalized timing, which can be logistically challenging [56].
- Defining "Time": The difference between biological ("internal") time and "wall clock" time must be considered, especially in individuals with misaligned rhythms [56].
- Drug Formulation: Conventional drug formulations lack temporal control, making it difficult to achieve precise release profiles aligned with circadian biology [58].
FAQ 4: How does circadian rhythm disruption, common in modern life, affect medication efficacy? Circadian disruption—caused by factors like artificial light, shift work, and irregular eating patterns—can desynchronize the central and peripheral clocks. This misalignment is linked to various pathologies, including metabolic syndrome, cancer, and cardiovascular diseases. From a therapeutic standpoint, disruption can alter the optimal timing for drug administration, potentially reducing efficacy and increasing adverse effects. Therefore, restoring rhythmicity or timing drug administration to the patient's altered rhythm may be necessary [37] [54] [58].
Troubleshooting Guides
Issue 1: High Variability in Drug Response Despite Time-Stamped Dosing
Potential Cause: Unaccounted-for differences in participant chronotypes may be obscuring the time-dependent efficacy of the drug.
Solution:
- Stratify Participants by Chronotype: Incorporate chronotype assessment during participant screening using the Munich Chronotype Questionnaire (MCTQ) [56].
- Implement Protocol: Recruit cohorts of distinct chronotypes (e.g., "larks" vs. "owls"). Administer the drug at the same clock time for all participants initially, then analyze results stratified by chronotype. For evening types ("owls"), a later administration time may prove more effective, while for morning types ("larks"), an earlier time may be optimal [56].
Issue 2: Inconsistent Results in Measuring Circadian Phase in a Cohort
Potential Cause: Uncontrolled lifestyle factors during the study are masking or confounding the endogenous circadian rhythm.
Solution: Implement strict participant guidelines and screening based on best practices for circadian studies [57].
- Screening: Exclude individuals with recent shift work, jet lag, significant sleep complaints, or extreme chronotypes unless they are the focus of the study.
- Protocol Control: For biomarker sampling (e.g., melatonin), control posture, exercise, and dietary intake. Ideally, samples should be collected in dim light conditions to prevent light-induced phase shifts.
- Substance Restrictions: Instruct participants to avoid caffeine, alcohol, and nicotine for a sufficient washout period prior to and during sampling, as these can alter circadian phase and sleep architecture [57].
Issue 3: Difficulty in Translating Preclinical Chronotherapy Findings to Humans
Potential Cause: The inbred animal models used in preclinical studies have highly synchronized circadian rhythms, unlike the large inter-individual variability found in human populations.
Solution:
- Incorporate Chronotype in Trial Design: When designing prospective clinical trials, use biomarker stratification or adaptive enrichment designs that account for patient chronotypes. This can improve the trial's ability to detect a significant chronotherapeutic effect that might be diluted in an unstratified population [56].
- Focus on Molecular Targets: Ensure preclinical work investigates the circadian regulation of the specific drug target or pathway in the relevant tissue, as this molecular timing may be more conserved across species than behavioral outputs [56] [58].
Experimental Protocols for Key Chronotherapy Assessments
Protocol 1: Assessing the Time-Dependent Efficacy of a Drug
Objective: To determine the optimal time of day for drug administration that yields the highest efficacy and lowest toxicity.
Materials:
- Animal model or human cohort.
- Equipment for drug administration and effect monitoring.
- Facilities with controlled light-dark cycles.
Methodology:
- Acclimatization: House subjects under standardized 12-hour light/12-hour dark (LD 12:12) conditions for at least two weeks prior to the experiment.
- Group Allocation: Randomly assign subjects to different drug administration time groups (e.g., at ZT4, ZT8, ZT12, ZT16, ZT20, where ZT0 is lights-on and ZT12 is lights-off).
- Drug Administration: Administer the drug at the designated Zeitgeber Time (ZT) for each group.
- Monitoring: Measure primary efficacy endpoints (e.g., tumor size reduction, biomarker change) and toxicity markers (e.g., body weight, organ function tests, survival) at regular intervals.
- Data Analysis: Plot efficacy and toxicity outcomes against administration time to identify peaks and troughs. Statistical analysis (e.g., cosinor analysis) can be used to fit a rhythmic pattern to the data [55].
Protocol 2: Determining an Individual's Circadian Phase in a Clinical Study
Objective: To accurately characterize the circadian phase of human participants for stratification in a chronotherapy trial.
Materials:
- Dim red light for sample collection.
- Saliva or blood collection kits.
- Radioimmunoassay or ELISA kits for melatonin/cortisol.
- Actigraphy watches (optional).
- Munich Chronotype Questionnaire (MCTQ).
Methodology:
- Pre-Screening: Administer the MCTQ to recruit participants with a range of chronotypes or to characterize the study population.
- Salivary Melatonin Collection (Dim Light Melatonin Onset - DLMO):
- On the test day, participants should avoid caffeine, heavy exercise, and bright light after 6 PM.
- Starting 5 hours before and until 2 hours after habitual sleep time, collect saliva samples every 30 minutes in dim light (<10 lux).
- Immediately freeze samples at -20°C.
- Analysis: Assay samples for melatonin concentration. The DLMO is calculated as the time when melatonin concentration continuously exceeds a threshold (e.g., 3 or 4 pg/mL) [57].
- Actigraphy: Participants wear an actigraphy watch for 1-2 weeks before sampling to confirm their rest-activity cycle aligns with the study requirements [56] [57].
Research Reagent Solutions
Table: Essential Materials for Circadian Rhythm and Chronotherapy Research
| Item | Function/Benefit |
|---|---|
| Munich Chronotype Questionnaire (MCTQ) | A validated tool to assess an individual's chronotype based on their sleep behavior on free days, corrected for sleep debt. It is a practical and non-invasive method for participant stratification [56]. |
| Actigraphy Watch | A wearable device that continuously monitors locomotor activity and rest. It provides an objective, long-term measure of the rest-activity rhythm, a reliable marker of circadian system function [56] [57]. |
| Dim Light Melatonin Onset (DLMO) Kit | Radioimmunoassay or ELISA kits for measuring melatonin in saliva or plasma. DLMO is the gold standard biomarker for assessing the phase of the central circadian clock in the SCN [56] [57]. |
| Validated Gene Panels | Pre-designed panels for qPCR or RNA-Seq to analyze the expression of core clock genes (e.g., BMAL1, CLOCK, PER1/2, CRY1/2, NR1D1/2) and clock-controlled output genes in human samples [37]. |
| TimeTeller or Similar Algorithms | A machine learning-based tool that can estimate an individual's molecular circadian phase from a single blood sample, making large-scale clinical trials more feasible [56]. |
Circadian Rhythm Molecular Feedback Loop
Circadian Clock Core Mechanism
Chronotherapy Experimental Workflow
Chronotherapy Study Design
Data Analysis Techniques for Deconvoluting Endogenous vs. Drug-Induced Rhythmicity
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary computational methods for identifying whether a rhythmic signal is endogenous or drug-induced? The primary methods involve a combination of differential rhythmicity analysis and mathematical modeling. Tools like CircaCompare are specifically designed for differential rhythmicity analysis, allowing you to compare rhythmic parameters (phase, amplitude, period) between two conditions—such as pre- and post-drug treatment [59]. Furthermore, mathematical models can simulate how a drug might alter an existing circadian signal. These models treat the circadian clock as an oscillatory modulator of drug concentration, helping to isolate the drug's effect from the underlying endogenous rhythm [60].
FAQ 2: Which non-invasive sampling methods are emerging for continuous circadian hormone monitoring? Passive perspiration (sweat)-based wearable biosensors are a cutting-edge method for the continuous, dynamic monitoring of key circadian hormones like cortisol and melatonin. Studies have shown strong agreement between hormone levels measured in sweat and saliva, validating sweat as a reliable matrix for endocrine monitoring. This technology enables real-time tracking of circadian phase shifts and is suitable for long-term, personalized chronotherapy [59].
FAQ 3: How can AI and machine learning be applied to deconvolute complex circadian drug responses? AI-driven deep learning frameworks can be built to integrate multi-omics network analysis with mechanistic learning. For instance, a Pathway and Transcriptome-Driven Drug Efficacy Predictor (PTD-DEP) can systematically identify candidate compounds that target shared pathological pathways. These models use a dual-modality architecture, combining biological pathway prediction with transcriptomic profiling to evaluate a drug's therapeutic potential and its interaction with core circadian mechanisms [61]. Machine learning can also predict a patient's internal circadian time from easier-to-obtain samples (e.g., a single blood draw), which is crucial for personalizing chronotherapy [62].
FAQ 4: What are the key properties of a circadian rhythm that must be analyzed? A circadian rhythm is defined by three key parameters that must be quantified and compared across conditions [62] [63]:
- Period: The time required to complete one cycle of oscillation (approximately 24 hours).
- Amplitude: The intensity or magnitude of the oscillation, measured as the difference between the peak and the midpoint (or trough) of the rhythm.
- Phase: The timing of a specific reference point in the cycle, such as the peak or trough, relative to a fixed time (e.g., time of day or another marker).
FAQ 5: Our in vitro drug sensitivity assays show high variability. Could time-of-day be a factor? Yes, the time of day (ToD) of drug application is a critical and often overlooked factor in in vitro studies. Research shows that drug sensitivity in human cell lines can fluctuate dramatically throughout the day due to the cell's endogenous circadian clock. To ensure reproducible results, it is essential to synchronize cell cultures (e.g., using a dexamethasone pulse) and carefully document the circadian time at which drugs are applied and assays are read out [60] [64].
Troubleshooting Guides
Issue 1: High Variability in Circadian Phase Estimates from Hormone Measurements
Problem: Measurements of melatonin or cortisol from patient samples yield inconsistent phase estimates, making it difficult to determine the true endogenous rhythm.
Solutions:
- Implement Continuous Monitoring: Replace single-time-point or sparse sampling with continuous monitoring using wearable biosensors [59]. This provides a dense data stream that is more robust for rhythm analysis.
- Use Robust Differential Analysis Software: Employ specialized statistical packages like CircaCompare to fit and compare circadian parameters. This method is more reliable than simple peak-picking, especially for noisy biological data [59].
- Control for Confounding Factors: Age and sex significantly influence circadian phase and amplitude. Stratify your data analysis by these demographic factors to reduce variability and reveal true biological signals [59].
Issue 2: Differentiating Direct Drug Effects on the Clock from Indirect Physiological Effects
Problem: It is challenging to determine if a drug is directly targeting the core circadian clockwork or merely inducing rhythmicity through indirect physiological changes (e.g., altering sleep patterns).
Solutions:
- Employ Target Deconvolution Techniques: Use experimental methods like PROTAC (Proteolysis Targeting Chimera)-guided chemoproteomics to identify the direct molecular target of a drug. This approach was successfully used to identify the histone acetyltransferase p300 as a direct target of melatonin, linking it directly to circadian control [61].
- Conduct Multi-Omics Integration: Combine transcriptomic, metabolomic, and lipidomic data from treated samples. Analyze this data for enrichment in core circadian pathways (e.g., CLOCK/BMAL1, PER, CRY) to establish a direct link to the clock machinery [64].
- Leverage Mathematical Modeling: Use in silico models to simulate the contribution of direct vs. indirect effects. A model that treats the circadian clock as a modulator of effective drug concentration can help you test hypotheses about the site of drug action [60].
Issue 3: Translating In Vitro Chronotherapy Findings to In Vivo Models
Problem: Promising time-of-day drug effects observed in cell cultures fail to replicate in animal models or human trials.
Solutions:
- Characterize the Circadian Properties of Your Model: Before testing drugs, quantify the amplitude, period, and damping rate of the circadian clock in your specific cell line or animal model. The mathematical model shows that these properties dramatically shape the time-of-day drug response profile [60].
- Align Treatment with the Resistant Phase: Model simulations indicate that administering drugs a few hours before the endogenous peak of a relevant pathway (e.g., dopamine) can prolong the treatment's effects and avoid sharp spikes and crashes in biomarkers [65].
- Account for Species-Specific Differences: Be aware that the phase of core clock gene expression can be shifted by up to 12 hours between nocturnal (e.g., mice) and diurnal (e.g., humans, baboons) species. Always confirm that the circadian time of treatment is aligned correctly for your model [66].
The following table summarizes core techniques for deconvoluting rhythmic signals.
Table 1: Core Data Analysis Techniques for Circadian Deconvolution
| Technique | Primary Function | Key Metrics Output | Applicable Data Source |
|---|---|---|---|
| Differential Rhythmicity Analysis (e.g., CircaCompare) [59] | Statistically compares rhythmic parameters between two conditions (e.g., control vs. drug-treated). | Phase shift, change in amplitude, difference in period. | Hormone levels (melatonin, cortisol), gene expression data. |
| Mathematical Modeling of ToD Sensitivity [60] | Simulates how circadian properties and drug kinetics interact to produce time-of-day effects. | Predicted optimal treatment time, maximum range of ToD response. | In vitro drug sensitivity data, known circadian parameters of a cell line. |
| AI/Deep Learning (e.g., PTD-DEP) [61] | Predicts drug efficacy and identifies compounds that target shared aging/circadian pathways. | Compound-pathway interaction scores, pharmacological profile predictions. | Transcriptomic data, compound libraries, biological pathway databases. |
| Multi-Omics Integration [64] | Provides a holistic view of drug effects by correlating changes across gene expression, metabolites, and lipids. | Enrichment of circadian pathways, identification of key biomarker genes (e.g., NPAS2, PER2). | RNA-seq, metabolomics, and lipidomics datasets from treated samples. |
Experimental Protocols for Key Cited Methodologies
Protocol 1: Differential Rhythmicity Analysis for Hormonal Data
This protocol is adapted from the methodology used to analyze cortisol and melatonin rhythms from wearable sensor data [59].
1. Sample Collection:
- Method: Use a continuous, non-invasive biosensor that collects passive perspiration, or perform frequent salivary sampling (e.g., every 30-60 minutes over a 24-48 hour period).
- Controls: Record precise collection times and subject demographics (age, sex).
2. Hormone Quantification:
- Analyze samples using standardized immunoassays (ELISA) or mass spectrometry to determine cortisol and melatonin concentrations.
3. Data Analysis with CircaCompare:
- Input: A dataset of hormone concentrations with corresponding timepoints for each subject/group.
- Process: Use the CircaCompare package in R to fit a nonlinear model that estimates the mesor (mean level), amplitude, and phase for each group.
- Output: The software will provide statistical comparisons (p-values) for differences in amplitude and phase between groups, allowing you to conclude if the drug has significantly altered the endogenous rhythm.
Protocol 2: In Vitro Assessment of Time-of-Day Drug Sensitivity
This protocol is based on the combined mathematical and experimental approach used to define drivers of time-of-day drug sensitivity [60].
1. Cell Culture and Circadian Synchronization:
- Cell Line: Use a relevant human cell line (e.g., cancer cell line, primary fibroblasts).
- Synchronization: Treat cells with 100 nM dexamethasone (DEX) or another synchronizing agent (e.g., serum shock) for 1 hour to align the cellular clocks [64]. Replace with fresh medium after synchronization.
2. Time-of-Day Drug Application:
- After synchronization, apply the drug of interest at different circadian times (e.g., every 4 hours over a 24-48 hour period).
- Include vehicle control treatments at each corresponding time point.
3. Cell Viability/Proliferation Assay:
- At a predetermined endpoint, measure cell viability using a standardized assay like WST-1 [64].
- Normalize absorbance values to untreated control cells at each time point.
4. Data Modeling:
- Input: Cell viability data and the corresponding circadian time of drug application.
- Process: Fit a mathematical model that treats the circadian clock as an oscillatory modulator of the effective drug concentration. The model can simulate how clock properties (amplitude, period) shape the time-of-day response curve.
- Output: Identification of the circadian time window of maximum drug sensitivity (or resistance) for that specific cell line and drug combination.
Research Reagent Solutions
The following table lists key reagents and tools essential for experiments in this field.
Table 2: Essential Research Reagents and Materials
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Dexamethasone (DEX) [64] | A synthetic glucocorticoid used for in vitro synchronization of peripheral circadian clocks in cell cultures. | Synchronizing the circadian phase of BMAT-MSCs prior to RNA extraction or drug treatment. |
| StemRegenin 1 (SR1) [64] | A potent and selective antagonist of the Aryl Hydrocarbon Receptor (AhR). Used to probe the crosstalk between AhR signaling and circadian rhythms. | Treating bone marrow-derived MSCs to study the interplay between AhR, circadian clock, and leukemia microenvironment. |
| PROTAC Molecules [61] | (Proteolysis Targeting Chimeras) are bifunctional molecules used for target deconvolution. They bind to a protein of interest and recruit an E3 ubiquitin ligase, leading to the protein's degradation. | Identifying the histone acetyltransferase p300 as a direct target of the drug melatonin through chemoproteomic analysis. |
| WST-1 Cell Proliferation Assay [64] | A colorimetric assay for the non-radioactive, high-throughput quantification of cell viability and proliferation. | Evaluating the proliferation of BMAT-MSCs after treatment with different concentrations of an AhR antagonist. |
| CircaCompare Software [59] | An R package for differential rhythmicity analysis. It fits and compares circadian parameters between two groups of rhythmic data. | Establishing differential rhythmicity of cortisol and melatonin between young and older adults from wearable sensor data. |
Signaling Pathways and Experimental Workflows
Diagram 1: Molecular Crosstalk Between Circadian Clock and Drug Response
Diagram 2: Experimental Workflow for Deconvolution Analysis
Troubleshooting Experimental Noise and Optimizing Data Quality
Frequently Asked Questions
Q1: What are the most common sources of circadian disruption in a laboratory or clinical research setting? The most common sources include irregular light/dark cycles, especially exposure to blue light at night from computer screens and other devices [67] [68]. Other key disruptors are the timing of meals (particularly eating late at night), shift-work-like schedules for animal models or human participants, and inconsistent timing of experimental procedures like drug administration [67] [26] [24]. Many prescription sleep aids and stimulants only address symptoms and may further disrupt the underlying circadian system [67].
Q2: How can I control for circadian phase when collecting hormone samples? Strictly standardize the time of sample collection for all subjects relative to their known sleep/wake cycle or a fixed environmental zeitgeber like light onset [24]. Monitor and record key phase markers such as the timing of melatonin onset or the cortisol awakening response to align sampling with individual circadian phases [24]. Control lighting conditions meticulously in the hours leading up to and during sampling, as light exposure can immediately suppress melatonin and alter cortisol rhythms [67] [24].
Q3: What are the best practices for designing a study that investigates chronopharmacology? Incorporate time of day as a fundamental biological variable in your research design, similar to sex or age [26]. When testing a drug, include multiple dosing-time groups (e.g., morning vs. evening) rather than defaulting to a single time point [26]. Furthermore, monitor circadian rhythms in your study subjects (e.g., via actigraphy or melatonin sampling) instead of assuming a normal rhythm [24]. Finally, align drug administration with the rhythmic expression of the drug's target and metabolizing enzymes [67] [26].
Q4: How does aging affect the circadian system, and how should this be considered in studies with aged models? Aging progressively weakens the circadian system, leading to blunted and fragmented rhythms in activity, sleep, and core body temperature [67]. The suprachiasmatic nucleus (SCN) shows reduced output of neuropeptides and a diminished ability to coordinate peripheral tissues, even if core molecular clocks remain intact [67]. Aged organisms also show a slower adaptation to new light/dark cycles and an increased vulnerability to the detrimental health effects of circadian disruption [67]. Studies using aged models must account for this inherent circadian weakness and avoid protocols that young models can tolerate but that may be fatal to older ones [67].
Troubleshooting Guide
| Problem | Possible Cause | Solution |
|---|---|---|
| High variability in hormone assay results | Uncontrolled circadian phase of subjects; samples collected at different biological times. | Standardize collection time to a precise circadian anchor (e.g., 2 hours after wake-up); assess individual phase via dim-light melatonin onset (DLMO). |
| Unexpected lack of drug efficacy | Drug administered at a circadian time when the target pathway is inactive or drug metabolism is high. | Review literature for circadian expression of drug target and metabolizing enzymes; redesign study to include a time-of-day factor [26]. |
| Disrupted sleep-wake cycles in animal models | Uncontrolled light exposure during the dark phase (light pollution); improper cage placement; noisy environment at night. | Implement strict light-tight housing; use red light for dark-phase work; ensure consistent timing of animal facility maintenance. |
| Inconsistent gene expression data from peripheral tissues | Tissues collected without considering circadian time; misalignment between central (SCN) and peripheral clocks. | Sacrifice animals at multiple, defined Zeitgeber Times (ZTs); control for the effects of fasting and feeding time on peripheral clocks [67]. |
Quantitative Data on Circadian Disruption and Mitigation
Table 1: Impact of Common Zeitgebers on Circadian Phase
| Zeitgeber | Effect on Circadian Phase | Key Considerations for Study Design |
|---|---|---|
| Light (Blue spectrum) | Strongest phase-resetting signal. Morning light advances the clock; evening light delays it [68]. | Control all light exposure in the lab. Use darkness or amber glasses to block blue light before nocturnal hormone sampling. |
| Scheduled Feeding | Potent entrainer for peripheral clocks (e.g., liver). Can decouple peripheral clocks from the SCN if timed incorrectly [67]. | Fix feeding schedules and record meal times. For metabolic studies, time-restricted feeding can be a powerful intervention. |
| Exercise | Can phase-shift the circadian clock. Morning exercise may help advance the phase [68]. | Record the timing of physical activity for human subjects. Standardize exercise timing in animal studies. |
| Melatonin Administration | Chronobiotic effect; can phase-shift the clock. Evening melatonin advances the clock; morning melatonin delays it. | Can be used as an experimental tool to manipulate phase. Note that light exposure can suppress endogenous melatonin production [24]. |
Table 2: Example Chronopharmacology Findings for Common Drug Classes
| Drug Class | Example Drug | Suggested Optimal Dosing Time | Rationale & Effect |
|---|---|---|---|
| Calcium Channel Blockers | Nifedipine GITS | Bedtime [26] | More effective at lowering blood pressure and associated with fewer side effects when taken at night. |
| Calcium Channel Blockers | Isradipine SR | Night (2000 h) [26] | Evening administration showed a more pronounced effect on nocturnal blood pressure in non-dipping chronic renal failure patients. |
| Statins | (Various) | Evening [67] | Cholesterol production in the liver is rhythmic, with peak activity at night. Timing administration to the evening increases efficacy. |
Experimental Protocols
Protocol 1: Assessing Circadian Rhythmicity in Animal Models
Objective: To characterize the circadian period and rhythm stability in a rodent model under standard and disrupted conditions.
- Materials: Running wheels and activity monitoring system, light-tight housing, data analysis software.
- Methodology:
- House animals in individual cages with access to a running wheel under a standard 12:12 hour Light/Dark (LD) cycle for two weeks to establish baseline activity.
- Transfer animals to constant darkness (DD) for at least two weeks to observe the free-running period (tau) of their circadian rhythm.
- To test rhythm stability, subject a separate cohort to a "jet lag" paradigm by advancing or delaying the LD cycle by 6-8 hours and monitor the number of days required to re-entrain.
- Analyze actograms and periodograms using appropriate software to quantify activity onset, period length, and rhythm strength.
Protocol 2: Minimizing Circadian Disruption During Nocturnal Blood Sampling
Objective: To collect serial blood samples for hormone analysis (e.g., melatonin, cortisol) with minimal perturbation to the subject's circadian rhythm.
- Materials: Long intravenous catheter (for remote sampling), dim red light source, shielded collection setup, comfortable recliner for human subjects.
- Methodology:
- Pre-study habituation: Subjects should maintain a strict sleep/wake schedule for at least one week prior to the study. Wrist actigraphy can confirm compliance.
- Lighting control: During the sampling session, all work must be conducted under dim red light, which does not suppress melatonin [24].
- Remote sampling: For frequent sampling, use a long catheter passed through a port in the wall to an adjacent room. This allows collection without entering the subject's room, preventing disturbance from light, noise, and researcher presence.
- Sample processing: Immediately centrifuge samples in a dimly lit lab and store plasma at -80°C until assay.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Circadian Rhythm Research
| Item | Function | Example Application |
|---|---|---|
| Luciferase Reporter Constructs | Real-time monitoring of clock gene expression. | Generate transgenic animals (e.g., PER2::LUC) to track circadian gene activity in explants or live cells. |
| ELISA/Kits for Melatonin & Cortisol | Quantify hormone levels in serum, saliva, or plasma. | Determine circadian phase (DLMO) and assess rhythm strength in human or animal subjects. |
| siRNA/shRNA for Core Clock Genes | Knock down expression of specific clock components (e.g., BMAL1, CLOCK, PER). | Investigate the function of specific clock genes in cellular or animal models of disease. |
| Pharmacological Agents (e.g., REV-ERB agonists/antagonists) | Manipulate the circadian clock component. | Experimentally shift circadian phase or modulate clock-controlled gene networks. |
Signaling Pathways and Experimental Workflows
Circadian System & Disruption Pathways
Chronopharmacology Workflow
Strategies for Participant Screening and Chronotype Assessment in Trials
FAQs: Participant Screening and Chronotype Assessment
What is the minimum set of variables needed for robust chronotype classification in clinical trials?
A comprehensive chronotype assessment should integrate both subjective and objective measures across multiple dimensions. The minimal recommended set includes:
- Subjective Questionnaires: Munich Chronotype Questionnaire (MCTQ) or Morningness-Eveningness Questionnaire (MEQ)
- Objective Behavioral Monitoring: At least 7 days of actigraphy
- Sleep Diaries: Concurrent with actigraphy to provide context
- Biological Sampling: Dim Light Melatonin Onset (DLMO) or core body temperature rhythm where feasible [18] [69] [70]
Using only a single dimension (e.g., just questionnaires) fails to capture the complexity of chronotype, which encompasses biological, social, and environmental components [70].
How can we reduce participant burden in longitudinal circadian trials while maintaining data quality?
Implement tiered assessment strategies:
- Core Continuous Monitoring: Use ambulatory circadian monitoring (ACM) devices that simultaneously track wrist temperature, motor activity, body position, and light exposure [69]
- Targeted Intensive Assessments: Schedule biomarker sampling (e.g., saliva for melatonin/cortisol) during critical windows rather than continuously
- Experience Sampling Method (ESM): Deploy brief, real-time surveys triggered by specific activity patterns detected by accelerometers [71]
- Salivary Biomarkers: Utilize emerging methods like TimeTeller that require only 3-4 timepoints per day over 2 consecutive days for circadian phase assessment [2]
Our study involves medication known to affect circadian rhythms. How should we adjust our chronotype assessment protocol?
For medications with potential circadian disruption (e.g., chemotherapeutic agents like paclitaxel):
- Increase Assessment Frequency: Conduct pre-treatment, during treatment, and post-treatment assessments
- Expand Biomarker Panels: Include molecular clock gene expression analysis where feasible
- Monitor SCN Function: Implement phase response curve (PRC) assessments to detect central clock disruptions [72]
- Control for Confounders: Include measures of sleep disturbances, fatigue, and light exposure patterns that may mediate drug effects on circadian rhythms [72]
What objective biomarkers provide the most reliable chronotype assessment with minimal invasiveness?
The following table summarizes optimal biomarkers balancing reliability and practicality:
| Biomarker | Protocol Requirements | Phase Reliability | Participant Burden |
|---|---|---|---|
| Dim Light Melatonin Onset (DLMO) | Saliva/blood sampling in dim light (<10-20 lux) every 30-60 min for 6-8 h before sleep | Gold standard [2] | High [18] |
| Wrist Temperature Rhythm | Continuous ACM monitoring for ≥7 days [69] | High (validated against PSG) [69] | Low [69] |
| Core Body Temperature | Ingestible pills or rectal probes; continuous 24-48 h monitoring | High | Moderate-High [18] |
| Salivary Clock Genes | 3-4 timepoints/day over 2 days (e.g., ARNTL1, PER2) [2] | Emerging evidence [2] | Low [2] |
| Integrated TAP Variable | ACM-derived composite (Temperature, Activity, Position) [69] | High (correlates with MCTQ) [69] | Low [69] |
How do we handle discordance between subjective and objective chronotype measures?
Discordance between subjective and objective measures reflects distinct constructs rather than measurement error:
- Analyze Patterns: Determine if discordance follows predictable patterns (e.g., older adults underestimating sleep duration)
- Contextual Factors: Examine environmental influences (e.g., social jetlag, work schedules) that may explain discrepancies [70]
- Statistical Approaches: Use both measures as separate variables in models or create composite scores weighted by reliability
- Clinical Interpretation: Subjective measures may better predict treatment adherence, while objective measures may better predict biological outcomes [18]
Experimental Protocols for Chronotype Assessment
Comprehensive Chronotyping Protocol (14 Days)
Day 1-7: Baseline actigraphy with concurrent sleep diaries Day 8: DLMO assessment (saliva sampling every 30-60 minutes in dim light for 6-8 hours before habitual sleep time) [18] Day 9-14: Continued actigraphy to assess stability Data Integration: Calculate mid-sleep on free days corrected for sleep debt (MSFsc) from MCTQ, compare with objective phase markers
Abbreviated Protocol for Large Cohorts (7 Days)
Days 1-7: Continuous ACM monitoring with TAP variable calculation [69] Days 3-4: Saliva sampling at 4 strategic timepoints (e.g., waking, +2h, +6h, before bed) for circadian gene expression (ARNTL1, PER2) [2] Calculation: Night phase marker (NPM) of TAP variable provides objective chronotype classification strongly correlating with MCTQ (β = 0.531; p < 0.001) [69]
The Scientist's Toolkit: Essential Research Reagents & Materials
| Tool Category | Specific Products/Assays | Primary Application | Key Considerations |
|---|---|---|---|
| Subjective Measures | Munich Chronotype Questionnaire (MCTQ) [70], Morningness-Eveningness Questionnaire (MEQ) [70], Insomnia Severity Index [18] | Behavioral preference assessment | MCTQ better for objective timing; MEQ for preference [70] |
| Objective Monitors | Actigraphy devices, Ambulatory Circadian Monitoring (ACM) sensors [69], iButton temperature loggers [69] | Continuous rhythm assessment | ACM provides multi-parameter data (TAP variable) [69] |
| Biomarker Assays | Salivary melatonin ELISA kits [2], Salivary cortisol assays [2], RNA extraction kits for gene expression [2] | Phase marker quantification | Salivary melatonin correlates with plasma levels [2] |
| Molecular Tools | TimeTeller kits [2], qPCR assays for clock genes (ARNTL1, PER2, NR1D1) [2] | Peripheral clock assessment | Requires RNA stabilization (e.g., RNAprotect) [2] |
| Data Analysis | Non-parametric circadian analysis (NPCRA), Cosinor analysis, Phase response curve (PRC) modeling [72] | Rhythm parameter calculation | PRC essential for detecting SCN dysfunction [72] |
Troubleshooting Common Experimental Challenges
Low Amplitude Rhythms in Actigraphy Data
Problem: Weak or disrupted rest-activity cycles reducing chronotype classification accuracy.
Solutions:
- Extend Monitoring: Increase from 7 to 10-14 days to capture more stable patterns
- Check Device Compliance: Use tamper-resistant wearables and verify continuous wear
- Environmental Controls: Instruct participants to maintain regular light-dark schedules during monitoring
- Data Processing: Apply Lomb-Scargle periodogram analysis for noisy data rather than cosinor fits
High Participant Dropout in Longitudinal Biomarker Sampling
Problem: Attrition in studies requiring repeated biological sampling (e.g., salivary melatonin curves).
Mitigation Strategies:
- Tiered Compensation: Provide incremental payment for each completed timepoint
- Sampling Optimization: Use the minimal effective sampling frequency (3-4 timepoints/day for salivary genes) [2]
- Home-Based Protocols: Implement dried saliva spots or home saliva collection kits to reduce clinic visits
- Participant Education: Clearly explain the scientific importance of complete data collection
Discordance Between Physiological and Behavioral Phase Markers
Problem: Significant differences between DLMO and self-reported sleep timing.
Interpretation Framework:
- Assess Social Jetlag: Calculate difference between mid-sleep on workdays vs. free days
- Evaluate Light Exposure: Examine ACM light data for phase-delaying evening light exposure
- Consider Medication Effects: Review known circadian impacts of participant medications [72]
- Statistical Handling: Treat as separate constructs in analysis rather than attempting forced alignment
Budget Constraints Limiting Comprehensive Assessment
Cost-Effective Alternatives:
- Prioritize MCTQ + 7-Day Actigraphy: Provides reasonable accuracy for most applications
- Targeted Biomarker Sampling: Instead of full DLMO curves, use salivary cortisol awakening response or 2-point melatonin sampling
- Pooled Analysis: For genetic studies, pool samples across extreme chronotype groups rather than whole-sample analysis
- Public Datasets: Incorporate data from repositories like GEO or ArrayExpress for validation cohorts [2]
Advanced Technical Considerations
Nanotechnology-Enabled Assessment Methods
Emerging approaches leverage nanomaterials for enhanced circadian monitoring:
- Smart Drug Delivery Systems: Nanoparticles that release chronobiotics in phase-dependent manner [10]
- Biosensing Platforms: Nanomaterial-based sensors for continuous hormone monitoring
- Blood-Brain Barrier Penetration: Intranasal delivery systems for direct central clock assessment [73]
Chemotherapy-Induced Circadian Disruption Assessment
For studies involving circadian-disrupting medications:
- SCN Function Tests: Implement phase response curves to light (PRC) [72]
- Molecular Clock Analysis: Assess SCN clock gene expression rhythms (Bmal1, Per2, Nr1d1) [72]
- Peripheral vs Central Disruption: Differentiate through simultaneous SCN and peripheral tissue sampling
- Recovery Timeline: Monitor circadian parameters for extended periods post-treatment (weeks to months) [72]
Approaches for Differentiating Direct Drug Effects from Circadian Modulation
Troubleshooting Guide: Common Experimental Challenges
Problem: Unclear whether a change in hormone level is a direct drug effect or an indirect effect via circadian clock modulation.
- Potential Cause 1: The drug targets a receptor or pathway that is part of the circadian clock system (e.g., a clock gene or a neurotransmitter that phase-shifts the SCN).
- Solution: Measure core circadian clock components. If the drug alters the expression rhythm of core clock genes (e.g., Per1/2, Bmal1, Clock) or the phase of clock-controlled genes, it suggests circadian modulation [24] [10]. A direct effect would show hormone changes without this systematic shift in clock gene expression.
- Solution: Conduct a phase-response curve experiment. Administer the drug at different circadian times and monitor shifts in the timing of a reliable circadian biomarker, such as melatonin or cortisol onset [18] [74]. A phase-dependent response indicates direct clock interaction.
Problem: High variability in drug response metrics between subjects, obscuring circadian patterns.
- Potential Cause: Individual differences in circadian chronotype (e.g., morningness/eveningness) or irregular sleep-wake cycles are not controlled for, leading to misaligned internal rhythms during testing.
- Solution: Characterize and control for subject chronotype using standardized questionnaires like the Morningness-Eveningness Questionnaire (MEQ) or Munich ChronoType Questionnaire (MCTQ) [18]. For animal studies, ensure a strict and consistent light-dark cycle.
- Solution: Implement constant routine or forced desynchrony protocols in human studies. These methods minimize masking effects from sleep, activity, and meals, allowing a clearer assessment of the endogenous circadian rhythm and its interaction with the drug [18].
Problem: Difficulty determining if a drug's effect on a circadian biomarker is primary or secondary to its impact on sleep.
- Potential Cause: Many drugs that affect circadian rhythms also alter sleep architecture (e.g., antipsychotics, antidepressants). Changes in sleep can, in turn, influence hormone secretion.
- Solution: Use polysomnography (PSG) or actigraphy concurrently with circadian biomarker sampling. This allows you to correlate changes in the hormone profile (e.g., melatonin amplitude, cortisol timing) with objective sleep metrics (e.g., sleep onset latency, wake after sleep onset) [18].
- Solution: Sample hormones under conditions of sleep deprivation or during a constant routine protocol to isolate the circadian component from the sleep-homeostatic influence.
Problem: In animal studies, distinguishing a direct pharmacological effect from a general disruption of locomotor activity.
- Potential Cause: The drug may cause sedation or stimulate hyperactivity, which can mask or be mistaken for a true resetting of the central circadian pacemaker.
- Solution: Measure circadian rhythms in SCN tissue explants or PER2::LUCIFERASE reporter lines in vitro. This removes the confounds of locomotor activity and allows direct assessment of the drug's effect on the molecular clockwork [10] [75].
- Solution: Analyze the period and phase of the rest-activity rhythm using chi-square periodogram analysis or similar methods on actigraphy data. A stable new period/phase suggests true entrainment, while a fragmented rhythm suggests general disruption [76].
Frequently Asked Questions (FAQs)
Q1: What are the key molecular targets I should examine to confirm a drug is directly modulating the circadian clock? The primary targets are components of the core circadian transcriptional-translational feedback loop [24] [10]. This includes:
- Core Clock Genes and Proteins: Clock, Bmal1, Per1/2/3, Cry1/2, Rev-erbα/β, Rorα/β/γ.
- Methodology: Monitor the rhythmic expression (mRNA and protein) of these targets in relevant tissues (e.g., SCN, liver) over a 24-hour period after drug administration. A significant change in period, phase, or amplitude confirms direct circadian modulation [24].
Q2: Which biomarkers are most reliable for assessing circadian phase in hormone sampling research? The gold-standard biomarkers, best measured under controlled conditions, are:
- Melatonin: The timing of dim-light melatonin onset (DLMO) is the most reliable marker of central circadian phase in humans [18] [74].
- Cortisol: The circadian rhythm of cortisol secretion, with its characteristic morning peak, is a robust phase marker, though it is more susceptible to stress-induced masking [24] [74].
- Core Body Temperature (CBT): The daily trough of CBT is a stable circadian phase marker, but requires continuous monitoring [18].
Q3: How can I design a dosing-time experiment (chronotoxicity/efficacy) to separate circadian from direct effects? Administer the same dose of the drug at different circadian times (e.g., at 4-6 hour intervals across the 24-hour cycle) and monitor two key sets of outcomes [65] [77]:
- Pharmacokinetic (PK) Parameters: (Absorption, Distribution, Metabolism, Excretion).
- Pharmacodynamic (PD) Parameters: (Efficacy/Toxicity endpoints, target engagement). A significant time-dependent variation in PK indicates circadian influence on the body's processing of the drug. A time-dependent variation in PD, even after correcting for PK differences, suggests circadian regulation of the drug's target pathway [77].
Q4: Our drug shows circadian-timed efficacy. How can we prove this is driven by the target organ's local clock and not just the central SCN clock? This requires a tissue-specific approach:
- Animal Models: Use tissue-specific clock gene knockout mice. If the drug's time-dependent efficacy is abolished in the target organ's knockout model, it demonstrates reliance on that local peripheral clock [10].
- In Vitro Models: Treat synchronized cell cultures or tissue explants from the target organ with the drug. If the response varies based on the circadian phase of the culture, it provides direct evidence for local clock control, independent of the SCN [10].
Signaling Pathways and Experimental Workflows
Diagram 1: Core Circadian Clock Mechanism
This diagram illustrates the core transcriptional-translational feedback loop of the mammalian circadian clock, showing key components that drugs may target for direct modulation [24] [10].
Diagram 2: Experimental Differentiation Workflow
This flowchart outlines a systematic experimental approach to differentiate direct drug effects from circadian modulation.
Research Reagent Solutions Toolkit
Table 1: Essential Reagents and Tools for Circadian-Drug Interaction Studies
| Item Name | Function/Brief Explanation | Example Use Case |
|---|---|---|
| BioDare2 [75] [76] | An online resource for circadian data analysis and sharing. Uses multiple algorithms (e.g., FFT-NLLS, MESA) to determine period, phase, and amplitude from timeseries data. | Analyzing rhythmic bioluminescence data from PER2::LUC tissue explants treated with a drug candidate. |
| ChronobioticsDB [78] | A curated database of drugs and compounds known to modulate circadian rhythms. | Screening for known chronobiotic properties of a drug or its analogs during experimental design. |
| Actigraphy System | A watch-like device that measures gross motor activity to infer sleep-wake cycles and rest-activity rhythms. | Objectively monitoring circadian activity patterns in humans or animals in response to chronic drug treatment. |
| PER2::LUCIFERASE Reporter Line | A genetically modified cell or animal model where the expression of the Per2 clock gene is linked to luciferase production, allowing real-time monitoring of circadian rhythms via bioluminescence. | Visualizing and quantifying the direct effect of a drug on the molecular clock in live cells or tissues. |
| Dim-Light Melatonin Onset (DLMO) Protocol [18] [74] | A standardized method for assessing the central circadian phase by frequently sampling melatonin levels under dim light conditions. | Establishing a baseline circadian phase in human subjects before testing a drug's phase-shifting potential. |
| MetaCycle / JTK_Cycle [76] | R-based software packages for detecting rhythmic signals from large-scale timeseries data (e.g., transcriptomics). | Identifying rhythmically expressed genes in omics datasets from drug-treated vs. control samples. |
| Constant Routine Protocol [18] | A rigorous research design involving prolonged wakefulness in a constant posture under dim light to unmask the endogenous circadian rhythm. | Precisely measuring the effect of a drug on core body temperature, melatonin, or cortisol rhythms, free from masking effects. |
Detailed Experimental Protocols
Protocol 1: Assessing Direct Circadian Clock Modulation Using a Reporter Gene System In Vitro
- Cell Culture and Synchronization: Culture cells carrying a circadian reporter (e.g., U2OS-PER2::Luc) [75]. Synchronize the cellular clocks by treating with a high-concentration serum shock (e.g., 50% horse serum for 2 hours) or a dexamethasone pulse (e.g., 100 nM for 30 minutes).
- Drug Treatment: After synchronization, replace the medium with a recording medium (e.g., phenol-red free DMEM with Luciferin). Add your test drug at a range of physiologically relevant concentrations. Include vehicle-only controls. For chronotherapy analysis, apply the drug at different phases of the circadian cycle (e.g., CT0, CT6, CT12, CT18).
- Bioluminescence Recording: Place the culture plates in a luminometer or an incubator with an integrated light-sealing detector. Record bioluminescence counts continuously for at least 5-7 days.
- Data Analysis: Export the timeseries data and analyze it using a platform like BioDare2 [75] [76]. Key parameters to assess:
- Period: Changes in the free-running period (e.g., shortening or lengthening from ~24 hours).
- Phase: Shifts in the peak time of the bioluminescence rhythm.
- Amplitude: Dampening or increase in the rhythm's robustness.
- A significant change in any of these parameters indicates direct modulation of the core circadian oscillator.
Protocol 2: Differentiating Circadian PK from Circadian PD in an Animal Model
- Experimental Design: Divide animals into several groups based on planned sacrifice times. Administer a single dose of the drug to all animals at one of multiple Zeitgeber Times (ZTs, e.g., ZT0, ZT6, ZT12, ZT18), representing different circadian phases [77].
- Sample Collection: At predetermined time points post-dosing, collect blood plasma to measure drug concentration (for PK) and tissue samples from the target organ (for PD and biomarker analysis).
- Pharmacokinetic Analysis:
- Use HPLC-MS/MS or similar to determine plasma drug concentration over time for each dosing-time group.
- Calculate PK parameters: ( C{max} ) (maximum concentration), ( T{max} ) (time to ( C{max} )), and ( AUC{0-\infty} ) (area under the concentration-time curve).
- Interpretation: If ( AUC ) or ( C_{max} ) varies significantly with dosing time, this is evidence of circadian PK (e.g., due to rhythms in metabolic enzymes) [77].
- Pharmacodynamic & Biomarker Analysis:
- Analyze target engagement in the tissue (e.g., receptor occupancy, downstream signaling pathway activation).
- Measure the expression of key clock genes (Per2, Bmal1) in the target tissue via qPCR.
- Interpretation: If the drug's effect on the target pathway varies with dosing time, even after normalizing for drug concentration (from step 3), this indicates circadian PD. If clock gene expression is also altered, it suggests the PD effect may be mediated via circadian modulation [24] [77].
This technical support center provides troubleshooting guides and FAQs for researchers conducting medication interference studies within circadian hormone sampling research. The content addresses specific issues you might encounter during experimental and computational workflows.
Frequently Asked Questions (FAQs)
Q1: Our in vitro chronotherapy model shows inconsistent time-of-day drug effects across cell lines. What are the key factors to optimize? A: Inconsistencies often arise from variations in circadian clock properties and experimental conditions between cell lines. Focus on these key parameters [60]:
- Circadian Amplitude: Cell lines with stronger circadian rhythms (higher amplitude) produce more pronounced time-of-day drug responses.
- Circadian Period: The period length shifts and broadens the window of drug sensitivity. Models show that periods up to ~32 hours maintain a robust time-of-day effect range.
- Amplitude Decay Rate (Dampening): A slow decay rate is crucial. Rapid dampening of the circadian signal leads to an exponential decline in time-of-day efficacy.
- Assay Duration: Ensure experiments run long enough to capture multiple circadian cycles to observe stable rhythms and drug effects.
Q2: How can we model the interaction between a patient's circadian rhythm and a drug's pharmacokinetics? A: A Physiologically Based Pharmacokinetic (PBPK) model is a powerful top-down approach. It integrates the drug's properties with the patient's physiology and can be tailored for circadian research by [79]:
- Incorporating circadian parameters for metabolic enzymes (e.g., CYP450 family) and drug transporters (e.g., P-glycoprotein).
- Using the model to predict drug concentration-time profiles not just in plasma, but also in target tissues, which is vital for assessing hormone modulation.
- Quantifying drug-drug interactions and their circadian variation, which is critical for medication interference studies.
Q3: We have sparse clinical data. Can we still build a predictive model for time-of-day dosing? A: Yes. A Population Pharmacokinetic (PPK) approach is designed for this. It uses sparse, clinically collected blood concentration data from a population to identify key sources of variability [79].
- Key Covariates: In drugs like tacrolimus, factors such as body weight, time post-transplant, CYP3A5 genotype, and hematocrit are common covariates that significantly impact drug clearance and volume of distribution.
- Bayesian Estimation: Once a population model is built, you can use a Maximum A Posteriori (MAP) Bayesian estimator to fit the model to just a few data points from a new patient, thereby individualizing their dosing schedule.
Q4: What are the core components of a mathematical model for circadian drug sensitivity? A: A generic but powerful model treats the circadian clock as an oscillatory modulator of the effective drug concentration [60]. The core components include:
- A reference drug concentration (the baseline dose).
- A circadian modulation function that boosts or attenuates the reference concentration over time.
- A cell growth model (exponential for control, inhibited for drug conditions).
- A dose-response relationship that translates the modulated effective concentration into a biological effect (e.g., cell death).
Table 1: Key Parameters for In Vitro Time-of-Day Drug Sensitivity Assays [60]
| Parameter | Description | Impact on Time-of-Day Response | Recommended Validation Approach |
|---|---|---|---|
| Circadian Amplitude | Strength of the oscillatory signal. | Higher amplitude increases the range of sensitivity/resistance. | Real-time luciferase reporting of core clock genes (e.g., PER2::LUC). |
| Circadian Period | Length of one complete cycle. | Alters the timing and width of sensitive windows. | Period analysis of bioluminescence data. |
| Amplitude Decay Rate | How quickly the oscillation damps over time. | Slow decay is essential for sustained time-of-day effects. | Fit a damping curve to the amplitude data over time. |
| Drug EC₅₀/IC₅₀ | Potency of the drug. | The shape of the dose-response curve influences the asymmetry of the time-of-day effect. | Perform a full dose-response curve prior to time-of-day experiments. |
| Cell Growth Rate | Doubling time of the cell population. | Impacts the dynamic range of the assay readout. | Use live-cell imaging to track confluence over time. |
Protocol 1: Developing a Circadian-Modulated Pharmacodynamic Model This protocol outlines a combined mathematical and experimental approach to define time-of-day drug sensitivity profiles [60].
- Characterize the Circadian Clock:
- Transduce your cell model with a circadian reporter (e.g., PER2::LUC).
- Record bioluminescence over at least 3-5 days to quantify the endogenous period, amplitude, and damping rate.
- Establish Baseline Drug Response:
- Perform a classic dose-response assay to determine the EC₅₀ or IC₅₀ of the drug of interest.
- Conduct Time-of-Day Dosing Experiments:
- Synchronize cells and apply a fixed concentration of the drug at different circadian phases (e.g., every 4 hours over a 24-48 hour period).
- Use a scalable assay (e.g., live-cell imaging for confluence) to measure the drug's effect over time.
- Mathematical Modeling:
- Build a model where the effective drug concentration ( C{eff}(t) ) is modulated by the circadian signal: ( C{eff}(t) = C_{ref} \times (1 + A \cdot \sin(2\pi t/T + \phi)) ), where ( A ) is amplitude and ( T ) is period.
- Fit the model output to your experimental growth curves to simulate and predict the optimal timing for drug administration.
Protocol 2: Integrating Circadian Rhythms into a PBPK Model This methodology helps predict tissue-level drug exposure and its circadian variation [79].
- System Characterization:
- Drug Parameters: Collect physicochemical properties (e.g., log P, pKa), binding data, and in vitro metabolic clearance rates.
- Physiological Parameters: Use literature values for human organ weights, blood flows, and tissue compositions. Incorporate known circadian oscillations in enzyme activity (e.g., CYP3A4) and hormone levels (e.g., cortisol).
- Model Construction:
- Use a PBPK software platform to build a model comprising compartments representing key organs (liver, gut, kidney, brain).
- Program the circadian variation in metabolic pathways and transporters as time-dependent functions.
- Model Verification and Application:
- Verify the model by comparing its predictions of plasma concentration-time profiles to existing clinical data.
- Use the validated model to simulate drug-hormone interference scenarios, such as how a drug's tissue concentration rhythm interacts with the secretion rhythm of a hormone like cortisol or melatonin.
The Scientist's Toolkit
Table 2: Essential Research Reagents and Solutions
| Reagent / Solution | Function in Research | Example Application |
|---|---|---|
| Real-time Luciferase Reporter (e.g., PER2::LUC) | Visualizing and quantifying circadian rhythms in living cells or tissues. | Characterizing the circadian period and amplitude of a novel cancer cell line [60]. |
| Dopamine Reuptake Inhibitors (e.g., Modafinil) | Pharmacological tools to probe circadian-pharmacology interactions. | Testing the principle that dosing during circadian troughs yields more stable neurotransmitter elevation [80]. |
| CYP3A5 Genotyping Assay | Identifying genetic covariates for PPK model development. | Personalizing the starting dose of tacrolimus in transplant patients to account for metabolic differences [79]. |
| Active Pharmaceutical Ingredient (API) | The core compound for in vitro and in silico modeling. | Determining the drug-specific parameters (IC₅₀, half-life) for a circadian PBPK/PD model. |
Modeling and Pathway Visualizations
The following diagrams, generated using DOT language, illustrate core concepts and workflows for managing medication interference in circadian research.
Circadian Medication Interference Modeling Framework
Experimental Workflow for Chronotherapy Research
Mechanism of Medication-Circadian System Interference
Adaptive Protocol Designs for Populations with Pre-existing Circadian Disruption
FAQ: Foundational Concepts and Rationale
Q1: Why do populations with pre-existing circadian disruption require specialized adaptive trial designs?
Populations with conditions like shift work disorder or circadian rhythm sleep-wake disorders exhibit fundamental physiological alterations that standard clinical trial designs fail to address. These alterations include misaligned central and peripheral circadian clocks and blunted hormonal rhythms, which can modify drug pharmacokinetics and pharmacodynamics [32] [81]. Adaptive designs are necessary to account for this altered physiological baseline, which can obscure true efficacy signals or confound safety assessments. By prospectively planning for protocol adjustments based on interim data, researchers can enhance the trial's sensitivity to detect genuine treatment effects in this unique subpopulation [82] [83].
Q2: What are the primary forms of circadian disruption I must account for in my trial protocol?
You should design your protocol to measure and account for three primary forms of disruption [44]:
- Internal Misalignment: A state where the central circadian clock (SCN) and peripheral clocks (e.g., in the heart, liver) are desynchronized [32] [44].
- Behavioral Misalignment: A mismatch between the sleep-wake cycle and the timing of the internal central circadian clock (CRCO-sleep misalignment) [44].
- Systemic Circadian Disruption: This encompasses a loss of rhythm amplitude (reduced peak-to-trough difference), abnormal phase (timing of peaks/troughs), and period instability [81] [84].
FAQ: Protocol Design and Troubleshooting
Q3: Our initial data shows high variability in circadian phase. How can we adapt patient enrollment?
This is a common challenge. Implement a prescreening phase using objective markers to categorize participants by their circadian phenotype prior to randomization.
- Solution: Use a run-in period with actigraphy and sleep diaries for at least 7 days to establish individual sleep-wake patterns [57] [85]. You can then stratify randomization based on key metrics like sleep midpoint or actigraphy-derived regularity. For more precise assessment, measure the Dim Light Melatonin Onset (DLMO) in a subset of participants to confirm circadian phase [57] [84]. This stratification ensures balanced allocation of different circadian phenotypes across treatment arms, reducing noise in your endpoint assessment [83].
Q4: We are concerned that our primary endpoint is being masked by circadian hormone variation. How can we resolve this?
This risk necessitates a protocol that controls for time-of-day effects on your biomarker.
- Solution: Standardize the timing of all biological sample collections relative to each participant's individual waking time or circadian phase, not to a fixed clock hour [84]. For example, schedule blood draws for hormone sampling at 2, 6, and 10 hours after waking. If your endpoint is a single daily measure, conduct sensitivity analyses to confirm the result is not driven solely by a subgroup sampled at a specific circadian phase. Furthermore, consider adapting the statistical analysis plan to include circadian phase as a covariate [82] [85].
Q5: Our interim analysis suggests drug efficacy is confined to a subgroup with severe circadian misalignment. What are our options?
This scenario is a key use-case for an adaptive enrichment design [83] [86].
- Solution: Prospectively define criteria for "severe circadian misalignment" in your protocol (e.g., CRCO-sleep misalignment >4 hours [44]). In a pre-planned interim analysis, if a pre-specified threshold of evidence is met, you can adapt the trial to:
- Re-allocate future randomization to enrich for this subgroup.
- Re-estimate the sample size to ensure the subgroup analysis is adequately powered.
- Drop the non-responsive subgroup and continue the trial exclusively in the enriched population, while statistically controlling the Type I error to maintain trial validity [83].
Quantitative Data on Circadian Disruption Markers
The table below summarizes key digital and biochemical markers used to quantify circadian disruption in clinical studies, based on recent large-scale research.
Table 1: Key Markers for Quantifying Circadian Disruption in Clinical Research
| Marker Category | Specific Measure | Typical Value in Healthy Adults | Value in Circadian Disruption (e.g., Shift Work) | Associated Clinical Risk |
|---|---|---|---|---|
| Digital (Wearable-Derived) [44] | CRCO-Sleep Misalignment | ~1.7 hours | Increases to ~2.2 hours* | Most significant negative impact on next-day mood [44] |
| CRPO-Sleep Misalignment | ~4.1 hours | Increases to ~4.6 hours* | Associated with depressive symptoms [44] | |
| Internal Misalignment (CRCO vs. CRPO) | Lower score | Significantly increases* | Most pronounced impact from poor mood on previous day [44] | |
| Biochemical (Gold Standard) [57] [84] | Dim Light Melatonin Onset (DLMO) | Stable timing, high nocturnal amplitude | Timing shift, suppressed amplitude | Independent risk factor for metabolic and cardiovascular disease [32] |
| Cardiovascular Rhythms [32] [85] | Nocturnal Blood Pressure Dipping | 10-20% drop at night | Blunted or reversed dipping ("non-dipper") | Strongly associated with target organ damage and cardiovascular events [32] |
*Statistically significant increase (p < 0.001) observed in a cohort of over 800 first-year physicians after starting shift work [44].
Experimental Protocols for Circadian Assessment
Protocol 1: Core Assessment for Stratification and Endpoint Adjustment
This protocol is designed for integration into clinical trial run-in periods or as a baseline assessment.
- Objective: To characterize the central circadian phase and sleep-wake patterns of each participant.
- Materials: Actigraphy device, sleep diary, saliva collection kits (for DLMO).
- Duration: 7-14 days under habitual conditions [85].
- Procedures:
- Actigraphy: Participants wear an actigraph on the non-dominant wrist 24/7 to monitor rest-activity cycles [57] [85].
- Sleep Diary: Participants complete a daily sleep diary (e.g., Consensus Sleep Diary) each morning, reporting time into bed, sleep onset latency, wake time, and sleep quality [85].
- DLMO Assessment (if required): On one evening, participants provide saliva samples in dim light (<10 lux) every 30-60 minutes for 6-8 hours before their habitual sleep time. Samples are assayed for melatonin concentration to determine the time of onset [57] [84].
- Analysis: Calculate sleep midpoint, sleep regularity, and DLMO phase. Use these to derive misalignment metrics (e.g., sleep midpoint - DLMO) [44].
Protocol 2: The Constant Routine for Unmasking Endogenous Rhythms
This is a rigorous, highly controlled inpatient protocol to isolate the endogenous circadian component from behavioral and environmental effects.
- Objective: To measure the pure endogenous circadian rhythm of hormones (e.g., cortisol, melatonin) and other physiological variables without the confounding effects of sleep, activity, and meals [84].
- Key Controls: Participants remain awake in a semi-recumbent posture for at least 24 hours under very dim light conditions. They receive identical hourly snacks or small meals to eliminate fasting/feeding cycles [57] [84].
- Measurements: Core body temperature (via rectal probe or ingested pill), hormone levels via frequent blood or saliva sampling, and subjective alertness are measured throughout the protocol.
- Output: The data reveals the true period, phase, and amplitude of the underlying circadian pacemaker, providing a gold-standard baseline for assessing circadian disruption in a research setting [84].
Signaling Pathways and Experimental Workflows
Circadian Clock Molecular Feedback Loop
Adaptive Trial Workflow for Circadian Populations
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Circadian Hormone Sampling Research
| Item | Function/Brief Explanation | Key Considerations |
|---|---|---|
| Actigraphy Device | Objective, long-term measurement of rest-activity cycles, a behavioral correlate of the circadian rhythm. | Choose devices with validated algorithms for sleep-wake detection and light logging capabilities [57] [44]. |
| Portable Polysomnography (PSG) | Gold-standard for objective sleep staging; essential if sleep architecture is a secondary endpoint. | Use home-based systems to measure sleep in the participant's natural environment and minimize the "first-night effect" [85]. |
| Salivary Melatonin Kits | For non-invasive assessment of DLMO, the gold-standard marker for central circadian phase. | Must be used under strict dim light conditions (<10-15 lux). Requires an assay with high sensitivity for low hormone concentrations [57] [84]. |
| Core Body Temperature Sensor | Measuring the circadian rhythm of core body temperature (CBT) is a classic marker of the endogenous pacemaker. | Rectal probes or ingestible telemetry pills provide the most reliable data. Wrist skin temperature is a less invasive proxy [57]. |
| Validated Sleep Diaries | Prospective, subjective assessment of sleep timing and quality. Critical for interpreting actigraphy data. | The Consensus Sleep Diary is a standardized tool that improves consistency across studies [85]. |
| Controlled Light Environments | To perform DLMO assessments or constant routine protocols without light masking the circadian signal. | Use light meters to verify ambient light levels. Light-proof rooms or dim red light (which minimally suppresses melatonin) are required [57] [84]. |
Biomarker Validation and Comparative Analytical Approaches
Validation of Novel Circadian Biomarkers Resistant to Medication Interference
For researchers in drug development, accurately measuring circadian hormones is critical for assessing drug efficacy, toxicity, and chronotherapy. However, many common medications are known to interfere with the secretion and measurement of key circadian biomarkers like melatonin and cortisol, potentially compromising study validity. This technical support center provides targeted guidance for troubleshooting this specific experimental challenge, framed within the broader context of medication interference in circadian hormone sampling research.
Frequently Asked Questions (FAQs)
Q1: Which common medications are known to interfere with melatonin and cortisol assays?
Numerous medications can alter the natural secretion patterns or interfere with the analytical detection of key circadian hormones. The table below summarizes common interferents.
Table 1: Common Medication Interferents with Circadian Biomarkers
| Biomarker | Class of Medication | Effect on Biomarker | Impact on Assay |
|---|---|---|---|
| Melatonin [87] | Beta-blockers, Non-steroidal Anti-inflammatory Drugs (NSAIDs) | Suppresses endogenous production | Alters physiological concentration |
| Melatonin [87] | Certain Antidepressants, Exogenous Melatonin, Contraceptives | Artificially elevates levels | Masks true endogenous rhythm |
| Cortisol [87] | Corticosteroids, Sex Hormones | Suppresses or alters rhythm | Cross-reactivity in immunoassays |
Q2: What analytical methods can minimize pharmacological interference in hormone measurement?
The choice of analytical platform is crucial. While immunoassays are widely used, they are prone to cross-reactivity with drug metabolites. Liquid chromatography-tandem mass spectrometry (LC-MS/MS) is a superior alternative, offering enhanced specificity, sensitivity, and reproducibility for both salivary and serum melatonin and cortisol by distinguishing the target hormone from structurally similar interferents [87].
Q3: How can we control for medication interference during participant screening?
Implementing strict screening protocols is the first line of defense. For a stringent protocol, participants using any medication known to interfere with melatonin or cortisol should be excluded [57]. In studies where this is not feasible, a moderate approach is to require a stable medication regimen for a defined period (e.g., the past month) and to document all medications for post-hoc analysis [88] [89].
Q4: My study population requires chronic medication. How can I validate a circadian biomarker under these conditions?
The core of your research involves developing biomarkers resistant to these confounders. The strategy involves using advanced statistical and machine learning models to identify biomarker panels that remain robust. Feature-selection methods like Elastic Net can build multivariate models from transcripts or proteins that accurately predict circadian phase (e.g., Dim Light Melatonin Onset - DLMO) even when traditional single-hormone measurements are compromised [40]. The key is to validate any novel biomarker panel against the gold-standard DLMO in both medicated and non-medicated cohorts [40] [88].
Troubleshooting Guides
Problem: Inconsistent Circadian Phase Estimates in Participants on Medication
Potential Cause: The medication is directly suppressing melatonin secretion (e.g., beta-blockers) or interfering with the immunoassay through cross-reactivity.
Solutions:
- Switch to LC-MS/MS: Confirm all hormone measurements using this specific method to rule out analytical interference [87].
- Develop a Multivariate Biomarker: Move beyond a single hormone. Use machine learning (e.g., Elastic Net, Partial Least Squares Regression) on transcriptomic or proteomic data from blood samples to build a predictive model of circadian phase that is less susceptible to the effects of any single compound [40].
- Implement a Robust Protocol: For gold-standard phase assessment like DLMO, ensure sampling occurs under dim light conditions, control participant posture, and standardize meal times to minimize non-medication confounders [57] [87].
Problem: Unable to Recruit a Medication-Naive Cohort for a Clinical Trial
Potential Cause: The target patient population for the drug under development typically requires concomitant medications.
Solutions:
- Document and Stratify: Meticulously document all concomitant medications. Use statistical stratification or include medication as a covariate in the final analysis to account for its effects.
- Use a Predictive Tool: Employ a tool like predictDLMO.com, which uses actigraphy data to estimate circadian phase. This can serve as a non-invasive secondary validation method, though it should be correlated with biochemical measures initially [90].
- Validate with At-Home DLMO: If blood draws are challenging, implement an at-home saliva DLMO protocol. This expands your recruitment pool and, with proper instruction (dim light, sample timing), can provide a reliable phase estimate against which to validate your novel biomarker [90].
Experimental Protocols & Workflows
Protocol 1: Validating a Novel Biomarker Against Gold-Standard DLMO
This protocol is adapted from current clinical trials validating circadian biomarkers in patients with sleep disorders [88] [89] [91].
1. Objective: To validate a single-sample transcriptomic or proteomic biomarker for estimating circadian phase against the gold-standard DLMO in participants with and without medication use.
2. Participant Screening & Inclusion:
- Recruit adults (e.g., 18-65) meeting study criteria.
- Inclusion: Target populations with known circadian disorders (e.g., Delayed Sleep-Wake Phase Disorder) or healthy controls.
- Exclusion: (Stringent) History of drug/alcohol dependency, use of interfering medications (e.g., beta-blockers, melatonin agonists) within the past month, night shift work, recent transmeridian travel [88] [57] [89].
3. Experimental Procedure:
- Pre-Study Monitoring: Participants wear a wrist actigraph and complete a sleep diary for at least 7 days to determine habitual sleep patterns [89].
- Clinic Visit (Day): A single blood draw is performed for the novel biomarker analysis (e.g., whole blood for transcriptomics or plasma for proteomics) [88].
- DLMO Assessment (Evening): Participants collect saliva samples every 30-60 minutes for 6-8 hours, starting 5-7 hours before their habitual bedtime and ending 1 hour after. This must be done under dim light conditions (<10 lux) [87] [90]. Samples are immediately frozen.
- Alternative Lab Protocol: Participants can complete the blood draw and saliva sampling in a single extended visit to the lab/clinic under controlled dim light conditions [91].
4. Data Analysis:
- DLMO Calculation: Calculate DLMO from saliva melatonin using a fixed threshold (e.g., 3-4 pg/mL for saliva) or a variable threshold (2 standard deviations above the mean of baseline samples) [87].
- Biomarker Model Building: Using the training dataset, apply feature-selection methods (e.g., Elastic Net) to the transcriptomic/proteomic data to build a model that predicts the DLMO phase.
- Validation: Test the model's phase prediction accuracy against the actual DLMO in a separate validation cohort. Compare performance between medicated and non-medicated subgroups.
Experimental Workflow for Biomarker Validation
Protocol 2: At-Home Saliva DLMO Collection for Biomarker Validation
This protocol is suitable for larger, more decentralized studies [90].
1. Kit Provision: Provide participants with a kit containing salivettes, a dim light flashlight, a detailed instruction sheet, a sample log, and pre-labeled freezer bags.
2. Sampling Schedule: Instruct participants to collect saliva samples hourly, beginning 5-7 hours before habitual bedtime and ending 1 hour after, while maintaining dim light conditions.
3. Sample Handling: Participants log the time of each sample and store them immediately in their home freezer. The next day, samples are shipped on cold packs to the central lab for analysis [90].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Circadian Biomarker Research
| Item | Function/Benefit | Key Considerations |
|---|---|---|
| LC-MS/MS Instrumentation | High-specificity measurement of melatonin/cortisol; minimizes medication assay interference [87]. | Superior specificity over immunoassays; allows for multiplexing. |
| Wrist Actigraph | Objective monitoring of rest-activity cycles and sleep patterns prior to sampling [57] [90]. | Can be used with predictive models (e.g., predictDLMO.com) for phase estimation. |
| Saliva Collection Kit (Salivettes) | Non-invasive collection for DLMO assessment; ideal for at-home and frequent sampling [87] [90]. | Must be used with strict dim light protocols for reliable results. |
| Feature-Selection Algorithms (Elastic Net) | Identifies the most predictive molecular features for circadian phase from high-dimensional data (e.g., transcripts) [40]. | Resists overfitting; creates robust, multi-feature biomarker panels. |
| Dim Light Flashlight / Light Meter | Ensures ambient light during evening sampling is <10 lux to prevent melatonin suppression [87]. | Critical for obtaining a valid DLMO measurement. |
Signaling Pathways and Logical Workflows
The following diagram illustrates the logic of how medication interference can confound single-marker measurements and how a multivariate biomarker approach offers a solution.
Biomarker Strategy Overcoming Interference
Comparative Analysis of Sampling Methodologies Across Research Settings
Frequently Asked Questions
1. What is the core difference between probability and non-probability sampling? Probability sampling gives all members of the target population an equal chance of being selected, making the sample more representative. Non-probability sampling selects participants based on accessibility or researcher judgment, which is faster but less representative [92].
2. How do I choose a sampling method for a clinical trial? The choice depends on your research goals, population accessibility, and required generalizability. For rigorous clinical trials, probability methods like stratified random sampling are preferred. For early-stage exploratory research, convenience sampling may be appropriate [92] [93].
3. What sampling considerations are unique to circadian rhythm research? Circadian research requires careful timing of sample collection to account for daily hormonal fluctuations. Key considerations include mapping samples to cortisol/melatonin rhythms, controlling for light exposure, and considering menstrual cycle phases in female participants [24] [37].
4. How can I optimize sampling in vulnerable populations like pediatrics? Use sparse sampling strategies, micro-volume assays, dried blood spots, and population PK modeling. These approaches minimize blood volume while maintaining data quality through advanced statistical methods [94].
5. What are common pitfalls in pharmacokinetic sampling? Common errors include insufficient sampling around Tmax (peak concentration), ending sampling too early to characterize elimination, and not collecting samples across a complete dosing interval [94].
6. How does sampling differ across drug development phases? Phase 1 studies typically use extensive sampling (12-18 samples per subject) for detailed PK profiling. Phase 2/3 studies employ sparser sampling (1-2 samples per visit) focused on safety and efficacy in larger patient populations [94].
Troubleshooting Guides
Problem: Inconsistent Hormonal Measurements in Circadian Studies
Potential Causes and Solutions:
Cause: Improper sampling timing relative to individual circadian phases
Cause: Medication interference with circadian rhythms
- Solution: Map drug administration times relative to endogenous hormone secretion patterns and consider chronotherapy approaches [24]
Cause: Inadequate sampling frequency to capture ultradian rhythms
- Solution: Increase sampling density during critical windows (e.g., every 30-60 minutes during circadian phase transitions) [37]
Problem: Insufficient Statistical Power in Sampling Strategy
Potential Causes and Solutions:
Cause: Sample size too small for population heterogeneity
Cause: High variability in measured parameters
- Solution: Increase sample size or implement measurement controls; use crossover designs where participants serve as their own controls [93]
Cause: Missing data at critical timepoints
- Solution: Implement adaptive sampling designs; use population statistical models that can handle sparse, unevenly spaced data [94]
Problem: Practical Constraints in Special Populations
Potential Causes and Solutions:
Cause: Blood volume limitations in pediatric studies
- Solution: Implement dried blood spot (DBS) sampling, use population PK approaches with sparse sampling across subjects [94]
Cause: Participant burden in long-term circadian studies
- Solution: Use wearable technology for continuous monitoring, implement home-based sampling with clear protocols [37]
Cause: Shift workers or irregular sleep patterns
- Solution: Characterize individual sleep-wake cycles before study entry; use actigraphy to verify timing [24]
Sampling Methodologies Comparison Table
Comparison of Major Sampling Approaches
| Sampling Method | Best Use Cases | Advantages | Limitations | Example Applications |
|---|---|---|---|---|
| Simple Random Sampling [92] | Homogeneous populations, probability-based studies | Minimal bias, simple implementation | Requires complete sampling frame, may miss rare subgroups | Phase 1 healthy volunteer studies |
| Stratified Random Sampling [92] | Populations with important subgroups | Ensures subgroup representation, improves precision | Requires knowledge of population strata | Studies requiring gender/age balance |
| Convenience Sampling [92] | Early exploratory research, pilot studies | Quick, inexpensive, easy to implement | High selection bias, limited generalizability | Preclinical feasibility studies |
| Systematic Sampling [92] | Large populations with sequential access | Even coverage of population, simple implementation | Vulnerable to periodic patterns | Electronic health record-based studies |
| Cluster Sampling [92] | Geographically dispersed populations | Cost-effective for large areas, practical implementation | Higher sampling error, complex analysis | Multi-center clinical trials |
Pharmacokinetic Sampling Optimization Across Development Phases
| Development Phase | Typical Sample Frequency | Key Objectives | Matrix Considerations | Regulatory Guidance |
|---|---|---|---|---|
| Phase 1 (First-in-Human) [94] | Extensive (12-18 samples per subject) | Complete ADME characterization, safety profiling | Plasma/serum preferred; whole blood if needed | FDA recommends sampling over ≥3 elimination half-lives |
| Phase 2 (Proof of Concept) [94] | Sparse (1-6 samples per subject) | Exposure-response relationships, dose justification | Alignment with clinical routine samples | Population PK modeling encouraged |
| Phase 3 (Pivotal Trial) [94] | Sparse (1-2 samples per visit) | Confirmatory efficacy, special population assessment | Integration with safety laboratory timepoints | Representative sampling across populations |
| Food Effect Studies [94] | 12-18 samples per period | Bioavailability comparison under fed/fasted conditions | Consistent matrix across conditions | Different sampling may be needed for each state |
Experimental Protocols
Protocol 1: Circadian Hormone Sampling in Medication Studies
Purpose: To characterize circadian hormone profiles while accounting for medication interference [24] [37]
Materials:
- Salivary cortisol collection kits (for frequent home sampling)
- Melatonin assay kits
- Actigraphy devices for sleep-wake monitoring
- Temperature loggers (for circadian phase markers)
- Electronic medication adherence monitoring
Procedure:
- Participant Screening: Recruit participants with stable sleep-wake cycles (±1 hour variation for 2 weeks)
- Baseline Characterization:
- Measure dim-light melatonin onset (DLMO) for phase assessment
- Collect salivary cortisol every 2 hours for 24 hours to establish baseline
- Record core body temperature continuously for 48 hours
- Medication Administration:
- Randomize participants to different dosing times (e.g., morning vs. evening)
- Monitor adherence with electronic caps
- Maintain for 2 weeks to establish steady-state concentrations
- Post-Intervention Sampling:
- Repeat 24-hour cortisol sampling
- Measure melatonin profile under dim light conditions
- Collect frequent PK samples around dosing (pre-dose, 0.5, 1, 2, 4, 6, 8, 12 hours post-dose)
- Data Integration:
- Align hormone measurements with drug concentration data
- Analyze phase shifts in circadian markers
- Correlate with reported side effects and symptoms
Protocol 2: Population PK Sampling in Special Populations
Purpose: To characterize drug disposition with minimal sampling burden [94]
Materials:
- Dried blood spot collection cards
- Micro-sampling devices (e.g., Mitra devices)
- Population PK modeling software
- Electronic data capture for precise timing documentation
Procedure:
- Sampling Scheme Design:
- Identify optimal sampling windows through simulation
- Stratify sampling times across population (different times for different subjects)
- Limit blood volume to <100 μL per sample in pediatric studies
- Sample Collection:
- Train participants/caregivers on home sampling technique
- Document exact sampling times relative to dosing
- Include paired clinical laboratory samples when available
- Sample Processing:
- Process DBS samples according to analytical method requirements
- Document hematocrit for DBS corrections
- Store samples appropriately until analysis
- Population Modeling:
- Develop structural PK model using all available data
- Identify covariate relationships (age, weight, renal function)
- Validate model using visual predictive checks
- Model Application:
- Simulate exposure profiles for various dosing regimens
- Identify outliers for further evaluation
- Refine sampling for future studies
Research Reagent Solutions
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Dried Blood Spot (DBS) Cards [94] | Micro-volume blood collection | Enables sparse sampling; requires hematocrit monitoring |
| Salivary Cortisol Kits [37] | Non-invasive stress hormone measurement | Ideal for frequent home sampling; correlates with plasma free cortisol |
| Melatonin ELISA Kits [24] [37] | Circadian phase assessment | Critical for dim-light melatonin onset (DLMO) determination |
| Portable Actigraphy Devices [37] | Sleep-wake cycle monitoring | Provides objective activity/rest patterns for circadian analysis |
| Population PK Software [94] | Sparse data analysis | Enables parameter estimation from limited samples per subject |
| Electronic Medication Monitors | Dosing adherence tracking | Documents exact administration times for accurate PK modeling |
| Stabilization Tubes [94] | Sample preservation | Maintains analyte stability during storage/transport |
Sampling Methodology Diagrams
Sampling Strategy Decision Tree
Circadian Medication Sampling Timeline
Pharmacokinetic Sampling Strategy Evolution
Assessing Robustness of Endocrine Markers Under Different Drug Regimens
Technical Support Center
Troubleshooting Guides & FAQs
FAQ 1: My experimental results show an unexpectedly low SETER/PR index. What could be the cause?
- A: An unexpectedly low SETER/PR index can stem from several issues. First, review your sample quality and handling. While the SETER/PR index is robust to preanalytical conditions like sample preservation method (RNAlater vs. snap frozen) and ex vivo ischemic time [95], significant RNA degradation will affect results. Second, verify the accuracy of your reference transcripts measurement, as the index calculation relies on the normalized expression of 18 informative genes against 10 stable reference genes [95]. Finally, ensure your patient cohort is correctly classified; the index is designed to predict sensitivity specifically in metastatic HR+/HER2− breast cancer patients receiving endocrine therapy [95].
FAQ 2: I have detected a high SETER/PR index, yet the patient showed poor response to endocrine therapy. How should I interpret this?
- A: A high SETER/PR index generally indicates prolonged sensitivity to endocrine therapy [95]. However, a key confounding factor is the presence of constitutively activating mutations in the ligand-binding domain (LBD) of the ESR1 gene. These mutations can cause high ER-related transcription but are associated with resistance to aromatase inhibitors [95]. It is recommended to sequence the ESR1 LBD in your sample. In one study, 15% of metastases harbored such mutations, which can explain the discordance between a high index and poor treatment response [95].
FAQ 3: How can I improve the consistency of my immunohistochemistry (IHC) results for protein validation?
- A: Consistency in IHC is critical. Follow these steps [96] [97]:
- Appropriate Controls: Always include positive and negative controls. A positive control (a tissue known to express the target protein) confirms your protocol works. A negative control (omitting the primary antibody) helps identify non-specific binding.
- Optimize Antibody Concentration: Titrate your primary and secondary antibodies. Too high a concentration can cause high background; too low can lead to a dim signal [96].
- Standardize Fixation and Antigen Retrieval: Under-fixation or over-fixation can mask epitopes. For formalin-fixed paraffin-embedded (FFPE) tissues, heat-induced epitope retrieval (HIER) is often necessary and must be optimized for time and buffer pH [97].
- Check Reagents: Ensure all reagents are fresh and stored correctly. Visually inspect solutions for cloudiness or precipitation [96].
FAQ 4: Does the timing of drug administration in animal studies or patient dosing affect endocrine marker assessments?
- A: Yes, circadian rhythms can significantly influence drug pharmacokinetics and pharmacodynamics [26] [98]. The molecular clock, governed by genes like CLOCK, BMAL1, PER, and CRY, regulates virtually all physiological processes, including those targeted by therapies [26]. For instance, studies on antihypertensive medications show that dosing time can alter a drug's effectiveness and side-effect profile [26]. Therefore, it is crucial to standardize and report the time of day for all drug administrations in your experimental design, as this is a key biological variable that can impact the interpretation and reproducibility of your results on endocrine marker robustness [26] [98].
Table 1: Prognostic Performance of the SETER/PR Index in Metastatic Breast Cancer
This table summarizes the association between the continuous SETER/PR index and patient survival outcomes, based on a study of 140 patients with HR+/HER2− metastatic breast cancer [95].
| Treatment Group | Sample Size (N) | Outcome Measure | Hazard Ratio (HR) | 95% Confidence Interval | p-value |
|---|---|---|---|---|---|
| Endocrine Therapy | 97 | Progression-Free Survival (PFS) | 0.51 | 0.41 – 0.74 | < 0.001 |
| Endocrine Therapy | 97 | Overall Survival (OS) | 0.40 | 0.26 – 0.62 | < 0.001 |
| Chemotherapy | 33 | Progression-Free Survival (PFS) | 0.76 | 0.45 – 1.27 | 0.290 |
Table 2: Impact of Dosing Time for Selected Calcium Channel Blockers
This table illustrates the principle of chronopharmacology, showing how dosing time can influence drug efficacy, which is a critical consideration for designing drug regimens [26].
| Drug | Study Population | Suggested Optimal Dosing Time | Observed Effect |
|---|---|---|---|
| Nifedipine GITS | Hypertensive patients | Bedtime | More effective blood pressure control and fewer side effects [26]. |
| Isradipine SR | Non-dipping chronic renal failure patients | Night (2000 h) | More pronounced reduction of nocturnal blood pressure [26]. |
| Diltiazem | Non-dipper hypertensive patients | Evening | Most pronounced antihypertensive effects during nightly rest [26]. |
Detailed Experimental Protocol: Targeted RNAseq for SETER/PR Index andESR1LBD Mutation Detection
This protocol is customized for measuring both the phenotypic SETER/PR index and the genotypic ESR1 status from metastatic biopsy samples [95].
1. Sample Preparation and RNA Extraction
- Input: Biopsies of metastatic HR+/HER2− breast cancer.
- Extraction: Extract total RNA using a standardized method (e.g., column-based kits). Assess RNA integrity (RIN > 7.0 is recommended) and quantity using an instrument like a Bioanalyzer or spectrophotometer.
2. Targeted RNA Sequencing Library Preparation
- Custom Panel: Design a targeted RNAseq panel to include:
- 18 Informative Transcripts: Genes whose expression is correlated with both ESR1 and PGR but not associated with proliferation.
- 10 Reference Transcripts: Stable, minimally variable genes for normalization.
- ESR1 Ligand-Binding Domain (LBD): Region where constitutive activating mutations commonly occur.
- Library Construction: Use a droplet-based targeted RNAseq system. Convert RNA into a sequencing library according to the manufacturer's instructions, incorporating unique molecular identifiers (UMIs) to correct for PCR duplicates and improve quantification accuracy.
3. Sequencing and Data Analysis
- Sequencing: Run the library on a high-throughput sequencer to achieve sufficient depth for accurate transcript quantification and variant calling.
- SETER/PR Index Calculation:
- Calculate the normalized expression:
(Average of 18 informative transcripts) - (Average of 10 reference transcripts) + 2. - The "+2" scaling factor ensures most HR+/HER2− cancers score above zero. Scores below zero are set to zero.
- A dichotomized index (e.g., using the median value of 0.82 as a cut-off) can be used to classify samples as "High" or "Low" [95].
- Calculate the normalized expression:
- ESR1 Mutation Detection:
- Align sequences to the human genome.
- Call variants in the ESR1 LBD using a robust variant-calling pipeline.
- Report the percentage of mutated ESR1 transcripts. Mutations present in as low as 1% of transcripts can be detected [95].
4. Interpretation
- High SETER/PR Index: Predicts longer progression-free and overall survival with endocrine therapy.
- Low SETER/PR Index: Suggests intrinsic resistance to endocrine therapy.
- ESR1 LBD Mutation Present: Indicates a likely mechanism of acquired resistance, even in the context of a high SETER/PR index.
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions
| Item | Function/Application |
|---|---|
| SETER/PR Targeted RNAseq Panel | A custom panel to simultaneously quantify the 18-gene signature and sequence the ESR1 LBD for a comprehensive sensitivity and resistance profile [95]. |
| Stable Reference Genes | A set of 10 validated reference transcripts (e.g., from the SETER/PR assay) used to normalize gene expression data and control for technical variability [95]. |
| Primary & Secondary Antibodies (IHC/ICC) | For protein-level validation of hormone receptors (ER/PR) and other markers. Selecting compatible and specific antibody pairs is crucial for signal detection [96] [97]. |
| Antigen Retrieval Buffers | Solutions (e.g., citrate-based) used in Heat-Induced Epitope Retrieval (HIER) to unmask antigens in FFPE tissue sections, which is critical for successful antibody binding [97]. |
| Cell Line & Tissue Controls | Positive and negative control cell lines or tissue sections that are essential for troubleshooting IHC, ICC, and molecular assays to ensure protocol validity [96] [97]. |
Experimental Workflow & Signaling Pathways
Cross-Species Considerations in Translational Circadian Research
Frequently Asked Questions & Troubleshooting Guides
Model System Considerations
Q: Why might my preclinical findings on circadian drug metabolism not translate to human trials?
A: A primary cause is the disregard for the fact that mice and rats are nocturnal animals, while humans are diurnal. Most behavioral testing in rodents is conducted during the day, which is their normal rest phase [99]. This is analogous to waking a human at 3 a.m. to perform complex tasks, leading to data that does not reflect the organism's optimal function [99]. This discrepancy can affect a wide range of physiological processes, including drug metabolism, immune function, and learning/memory.
- Troubleshooting Guide:
- Problem: Low effect size or inconsistent results in rodent studies.
- Solution: Reverse the light/dark cycle for your animal colony. House the animals in total darkness during the day and turn on the lights at night. This allows researchers to observe and test the animals during their active phase without disrupting their own schedules [99].
- Problem: Needing to check on animals or perform minor procedures during their active (dark) phase.
- Solution: Use dim red lighting instead of standard white light. Rodents cannot see red light, so it will not disrupt their circadian rhythms. This can be achieved with red overhead lights, a miner's light with a red LED, or night-vision goggles [99].
- Critical Step: Always record these environmental conditions in detail in your methods section to ensure reproducibility [99].
Q: How does the circadian system differ in organization between species?
A: While the core transcriptional-translational feedback loop (TTFL) of the circadian clock is conserved, the overall system architecture varies [100] [37].
- Mammals: Have a hierarchically organized system with a master pacemaker in the suprachiasmatic nucleus (SCN) that synchronizes peripheral clocks in other tissues [101] [37].
- Birds: Possess a multi-oscillatory system. In addition to the SCN, the pineal gland and retina also synthesize and release melatonin in a circadian manner [100].
- Other Organisms: Some, like cyanobacteria and marine dinoflagellates, can have circadian rhythms that operate with minimal or no transcription, placing a greater emphasis on post-translational and translational regulation [102].
Experimental Design & Confounding Variables
Q: What are the major pathways of circadian translational control I should consider in my research?
A: Circadian rhythms regulate mRNA translation at multiple levels, with translation initiation being a key control point [101]. The major pathways include:
- mTOR Signaling: The mTORC1 complex rhythmically phosphorylates key translation factors. It phosphorylates 4E-BP, freeing eIF4E to bind the 5' cap of mRNA and initiate cap-dependent translation. mTOR also regulates other factors like S6K and eIF4B [101] [102].
- Integrated Stress Response (ISR): This pathway can modulate translation initiation in response to cellular stress, which may interact with circadian cues [101].
- Ribosome Biogenesis: The very process of creating ribosomes is under circadian control. In mouse livers, the transcription of ribosomal RNA (rRNA), synthesis of ribosomal proteins, and final ribosome assembly occur in sequential, rhythmic waves throughout the 24-hour day [101].
The following diagram illustrates the core signaling pathways involved in the circadian regulation of translation initiation:
Q: My research involves hormone sampling. How can artificial light confound my results?
A: Artificial Light at Night (ALAN) is a potent disruptor of circadian hormonal rhythms [100]. Even low levels of ALAN (2-5 lux) can:
- Attenuate the molecular clock mechanism in the SCN [100].
- Eliminate rhythmic changes in key hormones like melatonin, testosterone, and vasopressin [100].
- Interfere with the circadian rhythm of glucocorticoids (e.g., corticosterone) [100].
- This chronodisruption is associated with disturbed daily patterns of metabolism and behavior [100].
- Troubleshooting Guide:
- Problem: Dampened or absent hormonal rhythms in animal studies.
- Solution: Scrutinize the light environment. Ensure dark phases are truly dark, with no light leaks from equipment, hallway lights, or under doors. Use light-tight housing and consider monitoring light levels with sensors.
- Best Practice: For research specifically investigating circadian hormones, validate your sampling protocols by collecting data across multiple time points throughout the 24-hour cycle to accurately capture rhythm parameters like amplitude, phase, and mesor [100].
Methodologies & Protocols
Q: What are some key experimental protocols for studying circadian translation?
A: The field employs a combination of molecular, cellular, and systems-level approaches.
Protocol 1: Assessing Rhythmic Protein Synthesis and Ribosome Biogenesis
- Objective: To characterize diurnal rhythms in global translation and the synthesis of ribosomal components.
- Methodology:
- Animal Housing: House mice under a controlled 12-hour light/12-hour dark cycle for at least two weeks before the experiment. For sampling during the active phase, implement a reversed light-dark cycle.
- Tissue Collection: Collect liver (or other tissue of interest) at multiple Zeitgeber Times (ZT) across the 24-hour cycle (e.g., every 4-6 hours). ZT0 is defined as lights-on.
- Ribosome Biogenesis Analysis:
- rRNA Transcription: Analyze the expression of RNA polymerase I subunits and transcription factors like UBF1 via qPCR or Western blot. Peak expression in mouse liver is around ZT6 [101].
- Ribosomal Protein Translation: Measure the mRNA and protein levels of ribosomal proteins (e.g., Rpl, Rps genes). Their translation peaks around ZT18 in mouse liver [101].
- Ribosome Assembly: Monitor the nuclear entry of pre-ribosomal subunits, which peaks near ZT22 [101].
- Translation Initiation Analysis: Examine the phosphorylation status of key translation factors by Western blot (e.g., 4E-BP1, RpS6, eIF4E, eIF4G). These often show robust diurnal phosphorylation patterns [101].
Protocol 2: Utilizing Engineered Human Liver Models for Chronopharmacology
- Objective: To study human-specific circadian drug metabolism without the confounding factors of cross-species translation.
- Methodology (based on [25]):
- Model System: Use engineered, miniaturized human livers derived from human hepatocytes.
- Circadian Synchronization: Establish culture conditions that support the circadian expression of core clock genes (e.g., by supporting synchronization of the BMAL1 gene).
- Gene Expression Profiling: Perform transcriptomic analysis (e.g., RNA-seq) every 3-6 hours over 48 hours to identify rhythmically expressed genes.
- Drug Exposure: Administer the drug of interest at different circadian times (e.g., corresponding to peak vs. trough expression of metabolizing enzymes).
- Metabolite Assessment: Quantify drug metabolites and toxicity. For example, the production of the toxic Tylenol metabolite NAPQI can vary by up to 50% depending on the time of administration [25].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential research tools for translational circadian research.
| Reagent / Material | Function / Application | Example & Notes |
|---|---|---|
| Engineered Human Liver Models | Studying human-specific circadian drug metabolism and toxicity. | Identified >300 rhythmically expressed liver genes; revealed time-dependent toxicity of acetaminophen and atorvastatin [25]. |
| Ribosome Profiling (Ribo-seq) | Genome-wide mapping of translated mRNAs; identifies rhythms in translation efficiency. | Revealed that in mouse liver, a sizable number of transcripts undergo diurnal rhythms in translation independent of mRNA abundance [102]. |
| Circadian-Controlled Luciferase Reporters | Real-time monitoring of circadian clock function and gene expression in live cells/tissues. | Used to track circadian phase and period in engineered liver models and other cell types. |
| Phospho-Specific Antibodies | Detecting rhythmic post-translational modifications in signaling pathways. | Essential for assessing activation of mTOR pathway components (p-4E-BP1, p-RpS6) and other kinases [101]. |
| Dim Red Lighting / Night Vision | Allows researcher access to nocturnal animals during their active phase without circadian disruption. | A miner's light with a red LED or night-vision goggles are practical solutions [99]. |
| siRNA/shRNA for Clock Genes | Functional validation of core clock components (e.g., BMAL1, CLOCK, PER, CRY) in translational regulation. | Knockdown of CRY1/2 or BMAL1 disrupts rhythmic ribosome biogenesis [101]. |
Table 1: Impact of Testing Time on Rodent Behavioral Studies. This table summarizes the findings from a survey of highly-cited behavioral neuroscience papers, highlighting the common oversight of circadian timing [99].
| Behavioral Testing Time | Percentage of Studies | Implication for Translational Relevance |
|---|---|---|
| Daytime (inactive phase) | 17% | Low; data collected when animal performance is suboptimal. |
| Nighttime (active phase) | 20% | High; data reflects the animal's natural state. |
| Both Day & Night | 7.5% | Allows for internal comparison of circadian effects. |
| Not Mentioned | 42% | Major flaw for reproducibility and interpretation. |
| Ambiguous Reporting | 13.5% | Hinders accurate replication of the study. |
Table 2: Effects of Dim Artificial Light at Night (ALAN) on Hormonal Rhythms in Rodents. This table synthesizes data from multiple studies on the chronodisruptive effects of light pollution [100].
| Hormone | Species | Effect of dim ALAN (≈5 lux) |
|---|---|---|
| Melatonin | Sprague-Dawley Rats | ↓ Nocturnal levels; suppressed amplitude [100]. |
| Corticosterone | Siberian Hamsters | Suppressed amplitude (lower at peak time) [100]. |
| Corticosterone | Grass Rats | ↑ Levels at ZT6 [100]. |
| Hypothalamic Gene Expression | Siberian Hamsters | ↑ Mel1, Tshr, GnRH, GnIH mRNA [100]. |
The following diagram outlines a general workflow for designing a robust circadian study that accounts for cross-species considerations:
Establishing Best Practice Guidelines for Circadian Hormone Assessment in Drug Development
Frequently Asked Questions (FAQs)
FAQ 1: What are the most critical participant screening factors to ensure reliable circadian hormone data? The most critical factors are a stable sleep-wake cycle, strict avoidance of confounding substances, and screening for medical or lifestyle conditions that disrupt circadian rhythms. Participants should maintain a consistent sleep schedule for at least one week prior to sampling. You must screen for and exclude individuals who work night shifts, have traveled across time zones recently, or have conditions like delayed sleep phase syndrome. Substance use, including caffeine, alcohol, and nicotine, should be restricted prior to and during the study, as they can directly affect central circadian pacemakers and hormone levels [57].
FAQ 2: Which hormones are most relevant for assessing circadian phase in clinical trials? The primary markers are melatonin and cortisol. Melatonin is considered the gold standard for assessing circadian phase in humans. Its secretion by the pineal gland is a direct output of the Suprachiasmatic Nucleus (SCN) and is highly sensitive to light. Cortisol rhythms are also a robust marker, with a characteristic peak in the morning and a trough around midnight. These hormones are preferable because their rhythms are clearly defined and their collection (via saliva or blood) is feasible in clinical settings [24] [57].
FAQ 3: How can we minimize the impact of medication interference on circadian hormone sampling? First, conduct a thorough literature review on the drug's known effects on the circadian system (e.g., on clock gene expression or melatonin secretion). If possible, include a washout period. If the investigational drug must be administered, use a constant routine or forced desynchrony protocol to separate endogenous rhythms from maskers. Always measure and account for baseline circadian phase before drug administration begins. Be aware that many psychotropic drugs, as well as beta-blockers and anti-inflammatory medications, can interfere with melatonin and cortisol rhythms [24] [57].
FAQ 4: What is the recommended protocol for collecting melatonin samples? Salivary or plasma Dim Light Melatonin Onset (DLMO) is the standard. Sampling should begin at least 3 hours before expected onset and continue every 30-60 minutes until at least 1 hour after onset.
- Lighting: Maintain dim light (< 10-30 lux) before and during collection.
- Posture: Participants should remain in a semi-recumbent position.
- Diet: Avoid eating large meals during sampling; standardize a small, caffeine-free snack if necessary.
- Sample Handling: Saliva samples should be stored frozen at -20°C or -80°C immediately after collection [57].
Troubleshooting Guides
Problem 1: High Variability in Hormone Measurements Between Subjects
Potential Causes and Solutions:
| Problem Area | Potential Cause | Recommended Solution |
|---|---|---|
| Participant Screening | Undetected circadian rhythm disorders or non-compliance with pre-study protocols. | Implement stricter screening using sleep logs and actigraphy for ≥1 week prior to the study [57]. |
| Environmental Control | Uncontrolled light exposure, posture, or meal timing during sampling. | Enforce a "constant routine" protocol or, at minimum, strictly control light (<30 lux), maintain semi-recumbent posture, and standardize meal timings [57]. |
| Assay Methodology | Inconsistent sample handling or assay techniques across different study sites. | Use a single, centralized laboratory for all hormone assays. Standardize and validate all kits and procedures beforehand [57]. |
Problem 2: Inability to Detect a Clear Circadian Rhythm
Potential Causes and Solutions:
| Problem Area | Potential Cause | Recommended Solution |
|---|---|---|
| Sampling Density | Infrequent sampling misses the peak or trough of the hormone rhythm. | Increase sampling frequency. For cortisol, sample hourly or bi-hourly over 24-48 hours. For DLMO, sample every 30 minutes in the evening [57]. |
| Participant Rhythm | Underlying weak or disrupted circadian rhythm in the participant. | Use actigraphy to confirm a robust rest-activity cycle before the study. Consider that the drug itself may be disrupting the clock, which is a valid finding [103] [37]. |
| Data Analysis | Inappropriate curve-fitting or analysis method for noisy data. | Use specialized circadian analysis software that employs robust algorithms like non-orthogonal spectral analysis or cosine fitting. Visually inspect raw data alongside fitted curves [104]. |
Problem 3: Suspected Masking of Rhythms by Drug or Food
Potential Causes and Solutions:
- Cause: The drug may directly affect the HPA axis (altering cortisol) or the synthesis of melatonin. Food intake can also acutely suppress melatonin.
- Solution: If a constant routine is not feasible, schedule all sampling and drug administration relative to each participant's individual wake-up time, rather than clock time. Conduct a baseline (pre-drug) assessment on all participants to use as an internal control. For food, enforce a fasting period before and during critical sampling windows (e.g., for DLMO) [24] [57].
Detailed Experimental Protocol: Core Body Temperature (CBT) and Melatonin Assessment
Objective: To simultaneously assess circadian phase using Core Body Temperature and Dim Light Melatonin Onset in a controlled clinical setting.
Materials:
- Ingestible telemetric temperature pill (e.g., VitalSense) and data recorder.
- Salivary melatonin collection kits (salivettes).
- Dim red light source (< 10 lux).
- Freezer (-20°C or -80°C) for sample storage.
- Actiwatch or similar device for activity monitoring.
Procedure:
- Pre-Study (≥1 week): Participants wear an actiwatch and complete a sleep diary to confirm a stable sleep-wake cycle. They avoid caffeine, alcohol, and night-time light exposure.
- Study Day:
- The participant swallows the temperature pill at a standardized time in the morning.
- The participant arrives at the lab 5-7 hours before their habitual bedtime.
- The CBT monitor is initialized, and the participant is settled in a private, sound-attenuated room under dim light (< 10 lux).
- Constant Routine Protocol (24-36 hours):
- The participant remains awake in a semi-recumbent posture.
- Nutritional intake is divided into small isocaloric snacks provided at regular intervals (e.g., hourly).
- Ambient temperature and light levels are kept constant.
- Sample Collection (for DLMO):
- Starting 3 hours before expected sleep onset, collect saliva samples every 30 minutes until the participant's scheduled bedtime.
- Label each tube with time, date, and participant ID.
- Centrifuge salivettes and freeze saliva at -20°C or lower immediately.
- Data Analysis:
- CBT: The CBT time series is analyzed to identify the time of the CBT minimum, which typically occurs in the later part of the sleep period.
- Melatonin: Salivary melatonin concentrations are plotted. DLMO is calculated as the time when melatonin levels continuously exceed a threshold (e.g., 3 pg/mL or 2 standard deviations above the average daytime baseline) [57].
Circadian Hormone Signaling Pathway
Experimental Workflow for Circadian Assessment
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Primary Function in Circadian Assessment |
|---|---|
| Salivary Melatonin Kits (e.g., Salivette) | Non-invasive collection of saliva for radioimmunoassay (RIA) or enzyme-linked immunosorbent assay (ELISA) to determine Dim Light Melatonin Onset (DLMO) [57]. |
| Actigraphy Watch | Worn on the wrist to continuously monitor rest-activity cycles, used to verify participant compliance with sleep protocols and to calculate rest-activity rhythm metrics [57]. |
| Ingestible Telemetric Pill & Receiver | Measures core body temperature (CBT), a reliable physiological marker of circadian phase. The CBT minimum is a key phase reference point [57]. |
| Dim Red Light Source | Provides safe illumination for participants during saliva sample collection in the dark, as red light does not suppress melatonin secretion like white/blue light [57]. |
| Circadian Reporter Cell Lines | Engineered cells (e.g., with BMAL1 or PER2 luciferase reporters) used in vitro to screen drug compounds for direct effects on molecular clock function [104]. |
Conclusion
Integrating circadian biology into drug development is essential for accurate hormone assessment and therapeutic optimization. The bidirectional relationship between medications and circadian rhythms necessitates rigorous sampling protocols, sophisticated analytical approaches, and chronotherapy-informed study designs. Future directions should focus on developing medication-resistant circadian biomarkers, establishing standardized guidelines for circadian data collection in clinical trials, and advancing personalized chronotherapeutic approaches that account for individual circadian phenotypes. Embracing these principles will enhance drug safety evaluation, improve efficacy outcomes, and pave the way for circadian medicine to become mainstream in pharmaceutical development and clinical practice.
References
- 1. Endocrine regulation of circadian rhythms | npj Biological Timing and... [https://www.nature.com/articles/s44323-025-00024-6?error=cookies_not_supported&code=c3dc03f0-b9ee-4cd0-bb06-76811c9556c7]
- 2. Comprehensive integrative analysis of circadian rhythms in ... [https://www.nature.com/articles/s44323-025-00035-3]
- 3. Rhythms and Circadian Homeostasis: Pathophysiological... Hormonal [https://pmc.ncbi.nlm.nih.gov/articles/PMC5372003/]
- 4. Circadian Rhythm: Biological Functions, Diseases, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547082/]
- 5. Circadian Rhythm Disorders - Treatment - NHLBI - NIH [https://www.nhlbi.nih.gov/health/circadian-rhythm-disorders/treatment]
- 6. How to Fix & Reset Your Circadian Rhythm in 8 Simple Steps [https://goayo.com/blogs/news/how-to-fix-reset-your-circadian-rhythm-in-8-simple-steps]
- 7. Circadian Clock Genes and the Transcriptional Architecture of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6872945/]
- 8. Genomics of circadian rhythms in health and disease [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-019-0704-0]
- 9. Peripheral clocks and systemic zeitgeber interactions [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1606242/full]
- 10. Nanomaterial-enabled drug delivery systems for circadian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12412127/]
- 11. Circadian clock genes and insomnia: molecular mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12548078/]
- 12. Pharmacological targeting of BMAL1 modulates circadian ... [https://www.nature.com/articles/s41589-025-01863-x]
- 13. Morning clock gene expression in young adults of early ... [https://www.nature.com/articles/s41598-025-12423-7]
- 14. Study uses body's clock to deliver medication precisely when ... [https://source.washu.edu/2025/04/study-uses-bodys-clock-to-deliver-medication-precisely-when-needed/]
- 15. The clinical impact of chronopharmacology on current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12125046/]
- 16. Chrono-Endocrinology in Clinical Practice - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11121809/]
- 17. Chronopharmacology: New Insights and Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3885389/]
- 18. Methods for Assessment of Sleep and Circadian Rhythms in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540570/]
- 19. Endocrine regulation of circadian rhythms [https://www.nature.com/articles/s44323-025-00024-6]
- 20. The Impact of Circadian Rhythms on Medication Timing ... [https://www.mdpi.com/2624-5175/6/4/43]
- 21. Chronopharmacodynamics of drugs in toxicological aspects [https://pmc.ncbi.nlm.nih.gov/articles/PMC4076864/]
- 22. Cancer treatments based on our internal clock could improve ... [https://hub.jhu.edu/2025/10/06/circadian-rhythms-and-cancer-treatments/]
- 23. Chronopharmacology of immune-related diseases [https://www.sciencedirect.com/science/article/pii/S1323893022000752]
- 24. The Impact of Circadian Rhythms on Medication Timing and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11586979/]
- 25. Circadian rhythms can influence drugs' effectiveness [https://news.mit.edu/2024/circadian-rhythms-can-influence-drugs-effectiveness-0424]
- 26. Circadian Variation in Efficacy of Medications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8268638/]
- 27. Circadian DLMO Test Information Guide - Biology of Sleep [https://biologyofsleep.com/circadian-phase-information-guide/]
- 28. How to Test for Non-24-Hour Sleep-Wake Disorder [https://gwinnettsleep.com/how-do-you-test-for-non-24-hour-sleep-wake-disorder-a-comprehensive-diagnostic-guide/]
- 29. Training the circadian clock, clocking the drugs and drugging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7249726/]
- 30. Confounding Variable - an overview [https://www.sciencedirect.com/topics/nursing-and-health-professions/confounding-variable]
- 31. Confounding in Observational Studies Evaluating the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8786092/]
- 32. Circadian Rhythm Disruptions and Cardiovascular Disease Risk [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384635/]
- 33. The Impact of Sleep and Circadian Disturbance on Hormones ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4377487/]
- 34. The Interplay between Early Mealtime, Circadian Rhythms ... [https://www.mdpi.com/2624-5175/5/3/34]
- 35. Sleep disorders impact hormonal regulation: unravelling the ... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-025-01871-w]
- 36. Confounding in longitudinal studies in addiction treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5360166/]
- 37. A prospective study to investigate circadian rhythms as ... [https://www.nature.com/articles/s44294-025-00057-z]
- 38. Optimizing Hormone Therapy With Circadian Rhythms [https://www.medscape.com/viewarticle/optimizing-hormone-therapy-circadian-rhythms-2025a1000nnn]
- 39. High-accuracy determination of internal circadian time from a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6118629/]
- 40. Performance of Blood-Based Biomarkers for Human Circadian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572356/]
- 41. Blood Clock Correlation Distance (BloodCCD) as a novel ... [https://www.nature.com/articles/s44276-025-00176-9]
- 42. Tips & Tricks | Immunoassay Protocols & Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/product-supporting/milliplex/tips-tricks-immunoassay-protocol-troubleshooting-advice?srsltid=AfmBOoqIoV4cvwJmNhkn37ZWI68JCBsNze4xKcoVbQkoZazCmqwXURZp]
- 43. Chronobiome medicine: circadian regulation of host ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623188/]
- 44. The real-world association between digital markers of ... [https://www.nature.com/articles/s41746-024-01348-6]
- 45. A Guide to Quantitative Biomarker Assay Development using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5657521/]
- 46. Assessment of Circadian Rhythms - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6857846/]
- 47. An Optimal Time for Treatment—Predicting Circadian Time by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7690897/]
- 48. Common Mistakes in Sleep & Circadian Research [https://web.fibion.com/articles/sleep-circadian-research-mistakes/]
- 49. Preparation for blood tests: what can go wrong before the ... [https://australianprescriber.tg.org.au/articles/preparation-for-blood-tests-what-can-go-wrong-before-the-sample-reaches-the-lab.html]
- 50. Circadian Biomarkers in Humans: Methodological Insights into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293921/]
- 51. What Has Caused My Blood Sample Error? [https://www.medichecks.com/blogs/blood-testing/what-causes-blood-sample-errors?srsltid=AfmBOooz3Zctmw10FBYwvc9PWXTRCAM2KlhuA_fD_UrRW64_h29V7HuX]
- 52. Improving Science by Overcoming Laboratory Pitfalls With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7993596/]
- 53. Chronotherapy: Intuitive, Sound, Founded…But Not Broadly ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5082589/]
- 54. Pioneering new frontiers in circadian medicine ... [https://www.sciencedirect.com/science/article/pii/S1043276024000407]
- 55. Cancer chronotherapy: principles, applications, and ... [https://pubmed.ncbi.nlm.nih.gov/12491517/]
- 56. Personalizing chronotherapy of immune checkpoint blockade [https://pmc.ncbi.nlm.nih.gov/articles/PMC12581061/]
- 57. Human circadian rhythm studies: Practical guidelines for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9382328/]
- 58. Nanomaterial-enabled drug delivery systems for circadian ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra04137f]
- 59. Circadian inference of rhythmicity using comparative ... [https://www.sciencedirect.com/science/article/pii/S2590137025000834]
- 60. A combined mathematical and experimental approach ... [https://www.nature.com/articles/s42003-025-07931-1]
- 61. AI-driven discovery of dual antiaging and anti-AD therapeutics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12629202/]
- 62. An Optimal Time for Treatment—Predicting Circadian ... [https://www.mdpi.com/2072-6694/12/11/3103]
- 63. Circadian rhythms revealed: unraveling the genetic ... [https://www.frontiersin.org/journals/sleep/articles/10.3389/frsle.2025.1544945/full]
- 64. Circadian rhythm and aryl hydrocarbon receptor crosstalk ... [https://www.nature.com/articles/s41598-025-93169-0]
- 65. New research could help boost drug efficacy by getting ... [https://news.umich.edu/new-research-could-help-boost-drug-efficacy-by-getting-dosing-in-rhythm-with-circadian-clocks/]
- 66. Circadian rhythms in cardiovascular (dys)function [https://www.nature.com/articles/s44325-024-00024-8]
- 67. How to fix a broken clock - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3856231/]
- 68. How to Fix Your Circadian Rhythm: 6 Easy Steps [https://www.sleepfoundation.org/circadian-rhythm/can-you-change-your-circadian-rhythm]
- 69. Assessing Chronotypes by Ambulatory Circadian Monitoring [https://pmc.ncbi.nlm.nih.gov/articles/PMC6879660/]
- 70. Assessing Chronotype: A Complex and Multifaceted ... [https://www.chronobiologyinmedicine.org/journal/view.php?number=197]
- 71. Experience Sampling Method (ESM) in Circadian Rhythm ... [https://web.fibion.com/articles/esm-circadian-research/]
- 72. Paclitaxel Chemotherapy Disrupts Circadian Gene ... [https://www.eneuro.org/content/12/9/ENEURO.0061-25.2025]
- 73. Intranasal and inhaled delivery systems for targeting ... [https://www.sciencedirect.com/science/article/pii/S0169409X25000602]
- 74. Circadian rhythm homeostasis biomarkers [https://www.sciopen.com/article/10.26599/OSHM.2025.9610028]
- 75. BioDare2 - circadian period analysis [https://biodare2.ed.ac.uk/]
- 76. Research tools [https://srbr.org/education-outreach/research-tools/]
- 77. Circadian rhythm in pharmacokinetics and its relevance to ... [https://www.sciencedirect.com/science/article/abs/pii/S0006295220302793]
- 78. ChronobioticsDB: The Database of Drugs and Compounds ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12286229/]
- 79. Page 135 - 《中国药房》2025年1期 [http://net.china-pharmacy.com/2025/202501/files/basic-html/page135.html]
- 80. New Study Reveals How Aligning Drug Dosing with ... [https://bioengineer.org/new-study-reveals-how-aligning-drug-dosing-with-circadian-rhythms-can-enhance-treatment-effectiveness/]
- 81. Circadian disruption: What do we actually mean? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6504624/]
- 82. E20 Adaptive Designs for Clinical Trials September 2025 [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/e20-adaptive-designs-clinical-trials]
- 83. Improving phase 2/3 trials with an enhanced 2-in-1 ... [https://pubmed.ncbi.nlm.nih.gov/40822703/]
- 84. Keeping an eye on circadian time in clinical research and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9790849/]
- 85. Methods for Assessment of Sleep and Circadian Rhythms ... [https://link.springer.com/article/10.1007/s11906-025-01345-4]
- 86. Adaptive Trial Design: A Guide to Flexible Clinical Trials [https://intuitionlabs.ai/articles/adaptive-clinical-trial-design]
- 87. Circadian Biomarkers in Humans: Methodological Insights ... [https://www.mdpi.com/2218-273X/15/7/1006]
- 88. Validation of Circadian Biomarkers in Patients With Sleep ... [https://www.centerwatch.com/clinical-trials/listings/NCT04690504/validation-of-circadian-biomarkers-in-patients-with-sleep-disorders]
- 89. Validation of Circadian Biomarkers in Patients With Sleep ... [https://mentalhealth.networkofcare.org/Lake/CommunityResources/ClinicalTrials/Detail/NCT04690504?keyword=%22Advanced%20Sleep%20Phase%20Syndrome%22]
- 90. Integrating Assessment of Circadian Rhythmicity to Improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11832606/]
- 91. Validation of Circadian Biomarkers in Patients With Sleep ... [https://ctv.veeva.com/study/validation-of-circadian-biomarkers-in-patients-with-sleep-disorders]
- 92. Sampling methods in Clinical Research; an Educational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5325924/]
- 93. Developing Representative Sampling Plans for ... [https://www.biopharminternational.com/view/developing-representative-sampling-plans-development-problem-solving-and-validation]
- 94. PK Sampling Optimization: Importance, Schedule & ... [https://www.allucent.com/resources/blog/why-pk-sampling-optimization-matters]
- 95. SETER/PR: a robust 18-gene predictor for sensitivity to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6542807/]
- 96. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 97. Protocols & Troubleshooting Guides [https://www.rndsystems.com/resources/protocols-troubleshooting-guides]
- 98. Pharmacogenomics and circadian rhythms as mediators of ... [https://www.sciencedirect.com/science/article/pii/S2590257121000122]
- 99. Like night and day: Animal studies may not translate to ... [https://www.sciencedaily.com/releases/2021/06/210610144505.htm]
- 100. Disturbances of Hormonal Circadian Rhythms by Light Pollution [https://pmc.ncbi.nlm.nih.gov/articles/PMC10138516/]
- 101. Circadian regulation of translation - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11441039/]
- 102. Emerging Roles of Translational Control in Circadian ... [https://www.sciencedirect.com/science/article/abs/pii/S0022283620302564]
- 103. Molecular Links Between Circadian Rhythm Disruption ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12073486/]
- 104. Time-of-day effects of cancer drugs revealed by high- ... [https://www.nature.com/articles/s41467-024-51611-3]