Beyond the Calendar: Addressing Methodological Challenges in Menstrual Cycle Endpoint Measurement for Robust Clinical Research
This article synthesizes current evidence and consensus recommendations to address the critical methodological challenges in measuring menstrual cycle endpoints for clinical and research applications.
Beyond the Calendar: Addressing Methodological Challenges in Menstrual Cycle Endpoint Measurement for Robust Clinical Research
Abstract
This article synthesizes current evidence and consensus recommendations to address the critical methodological challenges in measuring menstrual cycle endpoints for clinical and research applications. Aimed at researchers, scientists, and drug development professionals, it explores the foundational need for standardized measurement, critiques common methodological pitfalls like phase estimation, and presents rigorous verification tools from hormonal assays to wearable technology. It further provides a troubleshooting guide for optimizing study design and a comparative analysis of validation frameworks. The goal is to advance the quality and reliability of female-specific health research by promoting methodological rigor and transdisciplinary standardization in menstrual cycle science.
The Imperative for Precision: Why Standardized Menstrual Cycle Measurement is a Research Priority
FAQs: Methodological Challenges in Menstrual Cycle Research
FAQ 1: Why is it methodologically unsound to assume menstrual cycle phases based on calendar counting alone?
Assuming cycle phases based solely on the calendar day is considered "guessing" and lacks validity and reliability [1]. This approach fails to account for the high prevalence (up to 66% in exercising females) of subtle menstrual disturbances, such as anovulatory or luteal phase deficient cycles, which present with meaningfully different hormonal profiles despite normal cycle length [1]. Relying on a calendar-based method without hormonal confirmation risks linking research data to an incorrect hormonal milieu, leading to invalid conclusions about cycle-phase-dependent effects on health, training, or performance [1].
FAQ 2: What is the critical distinction between a 'eumenorrheic' cycle and a 'naturally menstruating' individual in research?
Terminology is critical [1]. A eumenorrheic cycle is confirmed through advanced testing (e.g., evidence of a luteinizing hormone surge and a sufficient progesterone profile in the luteal phase) and represents an ovulatory cycle with a characteristic hormonal profile [1]. In contrast, the term naturally menstruating should be applied when cycle regularity (21-35 days) is established through calendar-based counting, but no advanced testing confirms the hormonal profile [1]. In this case, the cycle can only be reliably split into menstruation and non-menstruation days, not into specific hormonal phases [1].
FAQ 3: What is the gold standard design for studying within-person effects of the menstrual cycle?
The menstrual cycle is fundamentally a within-person process [2] [3]. Therefore, repeated measures studies are the gold standard [2]. Treating the cycle or its phases as a between-subject variable conflates within-person variance with between-subject variance and lacks validity [2] [3]. For reliable estimation, a minimum of three observations per person across one cycle is suggested, though three or more observations across two cycles provides greater confidence in the reliability of between-person differences in within-person changes [2].
FAQ 4: How can researchers accurately identify the periovulatory and luteal phases for lab testing?
Scheduling lab visits for specific phases requires forward planning based on physiological markers, not just the calendar [2] [3].
- Predicting Ovulation: Use at-home urinary luteinizing hormone (LH) test kits. A positive test indicates the LH surge, with ovulation typically occurring 24-36 hours later [2] [3].
- Confirming the Luteal Phase: The luteal phase can be confirmed after ovulation via a rise in progesterone. This can be measured retrospectively from serum samples or quantitatively from urine as pregnanediol glucuronide (PDG) [2] [4]. The rise in basal body temperature (BBT) also provides a retrospective confirmation of ovulation [2] [5].
Troubleshooting Common Experimental Issues
Problem 1: Inconsistent or conflicting findings in cycle phase literature.
- Potential Cause: Use of assumed or estimated menstrual cycle phases without hormonal verification, leading to misclassification of participants' true hormonal status [1].
- Solution: Implement direct measurement of key hormonal endpoints to characterize cycle phases. For example, confirm ovulation via urinary LH surge kits and verify luteal phase viability with serum progesterone or urinary PDG [1] [2] [4]. Transparently report all methods and their limitations.
Problem 2: High variability in outcome measures within the same presumed cycle phase.
- Potential Cause: Failure to account for substantial between-person differences in sensitivity to hormonal changes (e.g., individuals with Premenstrual Dysphoric Disorder (PMDD)) or naturally occurring variations in follicular phase length [2] [3].
- Solution: Treat the cycle as a within-person variable and use study designs that allow for the assessment of individual differences. Increase the density of sampling (e.g., daily hormone measures) and use statistical models like multilevel modeling that can separate within-person and between-person effects [2] [3].
Problem 3: Participant drop-out due to the burden of intensive monitoring.
- Potential Cause: Traditional serum-based hormone monitoring is invasive and requires clinic visits, which can be burdensome [4].
- Solution: Leverage validated, quantitative at-home urine hormone monitors (e.g., Mira monitor) that track hormones like FSH, E1G, LH, and PDG [4]. These tools facilitate dense, longitudinal data collection in ecologically valid settings while providing research-grade information.
Standardized Experimental Protocols for Phase Verification
Protocol for Confirming Ovulation and Luteal Phase Function
Objective: To prospectively identify the ovulatory phase and retrospectively confirm a viable luteal phase. Materials: Urinary LH test kits, materials for serum collection (venipuncture), or a quantitative urinary hormone monitor capable of measuring PDG [2] [4].
| Step | Procedure | Measurement Endpoint |
|---|---|---|
| 1. | Starting on ~cycle day 8-10, instruct participants to perform daily urinary LH tests each morning. | A positive LH test, indicated by a test line as dark as or darker than the control line. |
| 2. | Schedule a lab visit for 5-7 days after a positive LH test. | Collect a serum sample for progesterone analysis. |
| 3. | (Alternative) Use a quantitative urinary hormone monitor for daily tracking from cycle start. | Identify the LH peak and the subsequent sustained rise in PDG levels. |
Validation Criteria: A serum progesterone level of > 16 nmol/L (or ~5 ng/mL) is a common threshold to confirm that ovulation has occurred [1] [2]. For urinary PDG, the specific threshold should be validated against serum or ultrasound, but a sustained rise is indicative of luteal activity [4].
Protocol for Quantifying Hormonal Profiles Across the Cycle
Objective: To characterize the full hormonal trajectory of the menstrual cycle for precise phase classification. Materials: Quantitative at-home urine hormone monitor (e.g., Mira) and corresponding test wands (e.g., Mira Plus wands measuring FSH, E1G, LH, PDG) [4].
| Step | Procedure | Measurement Endpoint |
|---|---|---|
| 1. | From the first day of menstruation (cycle day 1), participants use the monitor to test first-morning urine daily. | The device provides quantitative values for FSH, E1G, LH, and PDG. |
| 2. | Data is synced to a companion app and/or research database. | Hormone profiles are plotted over time. |
| 3. | Phase determination is based on hormone patterns: - Late Follicular: Rising E1G, low PDG. - Ovulatory: LH surge, peak E1G. - Luteal: Sustained rise in PDG, followed by a perimenstrual decline. | The specific day of ovulation can be estimated from the LH peak, and luteal phase function is assessed via PDG levels. |
Gold Standard Validation: This protocol is currently being validated in research against serial transvaginal ultrasound (the gold standard for pinpointing ovulation) and serum hormone levels to establish its accuracy [4].
Flowchart for Phase Verification
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key materials required for rigorous menstrual cycle phase determination in research settings [2] [3] [4].
Table: Essential Materials for Menstrual Cycle Phase Determination Research
| Item | Function in Research | Key Considerations |
|---|---|---|
| Urinary LH Test Kits | Predicts ovulation by detecting the luteinizing hormone surge in urine. | Cost-effective and practical for field-based or remote studies. Ideal for scheduling lab visits around the periovulatory phase. |
| Quantitative Urinary Hormone Monitor (e.g., Mira) | Provides quantitative daily values for FSH, E1G, LH, and PDG from urine to map the entire hormonal profile. | Enables dense, longitudinal data collection at home. Validated against serum and ultrasound is ongoing [4]. |
| ELISA Kits for Serum Progesterone | Precisely measures serum progesterone concentration to confirm ovulation and luteal phase function. | Considered a standard; requires a clinic visit for blood draw. A level >16 nmol/L is a common threshold for confirming ovulation [1] [2]. |
| Basal Body Temperature (BBT) Thermometer | Tracks the slight, sustained rise in resting body temperature that occurs after ovulation. | A low-cost method, but only provides retrospective confirmation of ovulation. Subject to confounding by illness, poor sleep, and alcohol [2] [5]. |
| Validated Daily Symptom Logs/Apps | Tracks participant-reported outcomes (mood, pain, bleeding) prospectively to avoid recall bias. | Critical for diagnosing conditions like PMDD. Retrospective recall of symptoms is highly unreliable and not recommended [2] [3]. |
Methodology and Outcome Relationship
In health research, particularly in the methodologically complex field of menstrual cycle science, measurement neglect poses a substantial threat to both scientific validity and public health. The systematic failure to implement rigorous measurement protocols generates cascading effects that compromise data quality, distort research findings, and ultimately erode public trust in scientific institutions. This technical support center document addresses these challenges within the specific context of menstrual cycle endpoint measurement, where biological complexity intersects with pressing clinical and research needs.
The menstrual cycle represents a fundamental indicator of health and physiological function, often described as the "fifth vital sign" for individuals who menstruate [4]. Despite its significance, research in this domain remains fractured across disciplines and hampered by inconsistent methodologies [6]. This article provides researchers, scientists, and drug development professionals with targeted troubleshooting guidance to identify, diagnose, and resolve common measurement challenges in menstrual health research.
The Impact of Measurement Neglect: Evidence and Consequences
Documented Consequences of Poor Data Quality
Inadequate attention to measurement quality and data integrity produces demonstrable harm across multiple dimensions of health research and practice. The following table summarizes key documented impacts:
| Impact Area | Documented Consequence | Example from Literature |
|---|---|---|
| Public Health Policy | Misguided interventions based on inaccurate prevalence data | CDC's false COVID-19 cleaning practices report led to unnecessary public health recommendations [7] |
| Clinical Research Validity | Compromised findings from unvetted respondents | Inattentive respondents inflated dangerous behavior reports by nearly 20% in replication studies [7] |
| Menstrual Research Specificity | Limited generalizability and selection bias | Studies focusing only on women trying to conceive or with regular cycles miss critical population variability [8] |
| Measurement Precision | Inability to detect true physiological signals | Subjective "light" vs. "heavy" bleeding classifications show poor correlation with quantitative measures [8] |
| Trust in Institutions | Erosion of public confidence in scientific bodies | Media amplification of flawed data damages institutional credibility [7] |
Methodological Challenges in Menstrual Cycle Research
Menstrual cycle research faces particular methodological vulnerabilities that amplify the consequences of measurement neglect:
- Selection Bias: Studies frequently overrepresent White populations, women with regular cycles, and those attempting conception, limiting generalizability [8].
- Informative Cluster Size: In fertility studies, women with less fertile cycles contribute more data, potentially skewing characterizations of "normal" cycle patterns [8].
- Definitional Inconsistency: Variations in defining menses onset, bleeding intensity, and cycle parameters hinder cross-study comparisons [8] [6].
- Endpoint Measurement: Subjective assessments of bleeding intensity lack precision, with 40% of women with heavy menstruation considering it normal [8].
Troubleshooting Guides for Common Measurement Challenges
Guide 1: Addressing Data Quality and Respondent Vetting Issues
Problem: Suspect data quality from inattentive or fraudulent survey respondents.
Symptoms:
- Unexpectedly high prevalence rates for rare behaviors
- Inconsistent response patterns within subjects
- Aberrant data distributions contradicting established literature
Diagnostic Steps:
- Implement attention checks: Incorporate instructional attention checks (e.g., "Select 'sometimes' for this item") and patterned responses to identify inattentive respondents [7].
- Analyze response distributions: Examine data for statistically improbable responses that may indicate fraudulent or inattentive participants.
- Compare with established benchmarks: Check findings against previously validated population estimates to identify significant deviations.
Resolution Protocols:
- Pre-study vetting: Implement behavioral and technical screening tools like Sentry to prevent problematic respondents from entering studies [7].
- Multi-measure validation: Combine attention checks with open-ended responses and analysis of response tendencies to identify quality issues [7].
- Provider accountability: Require sample providers to supply evidence of their screening methodologies and effectiveness data [7].
Guide 2: Resolving Menstrual Cycle Endpoint Measurement Errors
Problem: Inaccurate characterization of menstrual cycle parameters (bleeding, blood, pain, perceptions).
Symptoms:
- High within-woman variability in cycle phase length reporting
- Discrepancies between subjective bleeding assessments and quantitative measures
- Inability to compare findings across studies due to definitional differences
Diagnostic Steps:
- Audit measurement instruments: Review whether data collection tools have been validated against gold standards like quantitative blood loss measurement or urinary hormone monitoring [6] [4].
- Assess temporal precision: Evaluate how precisely cycle start dates and symptom onset are recorded, as participant recall introduces significant error [8].
- Check for objective correlates: Determine whether subjective measures are supplemented with objective indicators (e.g., product saturation, hormone levels) [8].
Resolution Protocols:
- Adopt standardized frameworks: Implement FIGO criteria for normal uterine bleeding parameters (frequency: 24-38 days; duration: ≤8 days; regularity: ±4 days) [6].
- Implement quantitative tools: Utilize validated instruments like the Mansfield-Voda-Jorgensen Menstrual Bleeding Scale for bleeding assessment [4].
- Incorporate hormonal verification: Where feasible, employ quantitative urine hormone monitors (e.g., Mira monitor measuring FSH, E13G, LH, PDG) to confirm ovulation and cycle phase [4].
Guide 3: Correcting Selection Bias and Generalizability Limitations
Problem: Research findings that cannot be generalized beyond the immediate study population.
Symptoms:
- Homogeneous participant demographics not representing target population
- Exclusion of participants with irregular cycles or specific health conditions
- Volunteer bias from participants with particular interest in menstrual cycle tracking
Diagnostic Steps:
- Analyze participant demographics: Compare study population characteristics with broader target population metrics.
- Review exclusion criteria: Assess whether exclusion criteria unnecessarily restrict participant diversity (e.g., limiting to "regular cycles" when studying cycle variability).
- Evaluate recruitment methods: Determine whether recruitment strategies systematically exclude certain subgroups.
Resolution Protocols:
- Purposive sampling: Implement strategies to ensure ethnically diverse samples reflective of target populations [4].
- Broad inclusion criteria: Where scientifically justified, include participants with irregular cycles, diverse ages, and varying pregnancy intentions [8].
- App-based data collection: Consider menstrual tracking apps to expand beyond typical volunteer populations, while acknowledging their limitations [8].
Frequently Asked Questions (FAQs)
Q1: What defines an adequate sample size for menstrual cycle research? A: Avoid rules of thumb; calculate sample size based on specific parameters of interest. One ultrasound validation study targeted 50 participants over 3 cycles (150 total cycles) to detect differences of 0.5 days in ovulation timing with 80% power [4]. Always conduct power analyses specific to your research questions and account for anticipated dropout rates.
Q2: How can we accurately capture subjective menstrual experiences like pain and bleeding intensity? A: Use validated instruments that combine subjective reports with objective correlates. For bleeding intensity, implement pictorial blood loss assessment charts alongside qualitative descriptions. For pain, utilize standardized scales with clear anchors. Always document the specific instruments used to enable cross-study comparisons [6].
Q3: What are the ethical considerations in menstrual cycle app data collection? A: Key considerations include data privacy and security (several major apps have experienced data breaches), transparent informed consent regarding data usage, and appropriate representation of diverse populations in algorithm development. Ensure compliance with relevant regulations and consider implementing data anonymization protocols [4].
Q4: How does the "mere-measurement effect" impact menstrual cycle research? A: The mere-measurement effect describes how the act of measurement itself can influence participants' perceptions and behaviors. In menstrual research, repeatedly asking about symptoms may heighten awareness or change tracking behaviors. Mitigate this by considering control groups without intensive measurement and documenting potential measurement effects in limitations [9].
Q5: What strategies exist for handling missing menstrual cycle data? A: Methods like multiple imputation make strong assumptions but are often preferable to complete-case analysis, which makes even stronger assumptions. Choose handling methods based on the missing data mechanism (MCAR, MAR, MNAR) and conduct sensitivity analyses to assess robustness of findings to different approaches [10].
Essential Research Reagents and Methodological Tools
The following table outlines key methodological approaches and their applications for robust menstrual cycle research:
| Tool Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Urinary Hormone Monitors | Mira monitor (FSH, E13G, LH, PDG) [4] | At-home ovulation prediction and confirmation | Correlate with serum values and ultrasound for validation |
| Bleeding Assessment Tools | Mansfield-Voda-Jorgensen Menstrual Bleeding Scale [4] | Standardized quantification of blood loss | Validated against direct measurement of fluid loss |
| Cycle Tracking Apps | Customized research applications with privacy protections [4] | Longitudinal data collection on multiple parameters | Ensure data security and validate against gold standards |
| Ultrasound Verification | Serial follicular tracking via endovaginal ultrasound [4] | Gold standard for ovulation confirmation | Resource-intensive but provides definitive phase identification |
| Serum Hormone Correlates | Anti-Müllerian Hormone (AMH) for ovarian reserve [4] | Contextualizing cycle characteristics | Single values less valuable than dynamic patterns |
Visualizing the Trust Erosion Pathway in Data Quality Failures
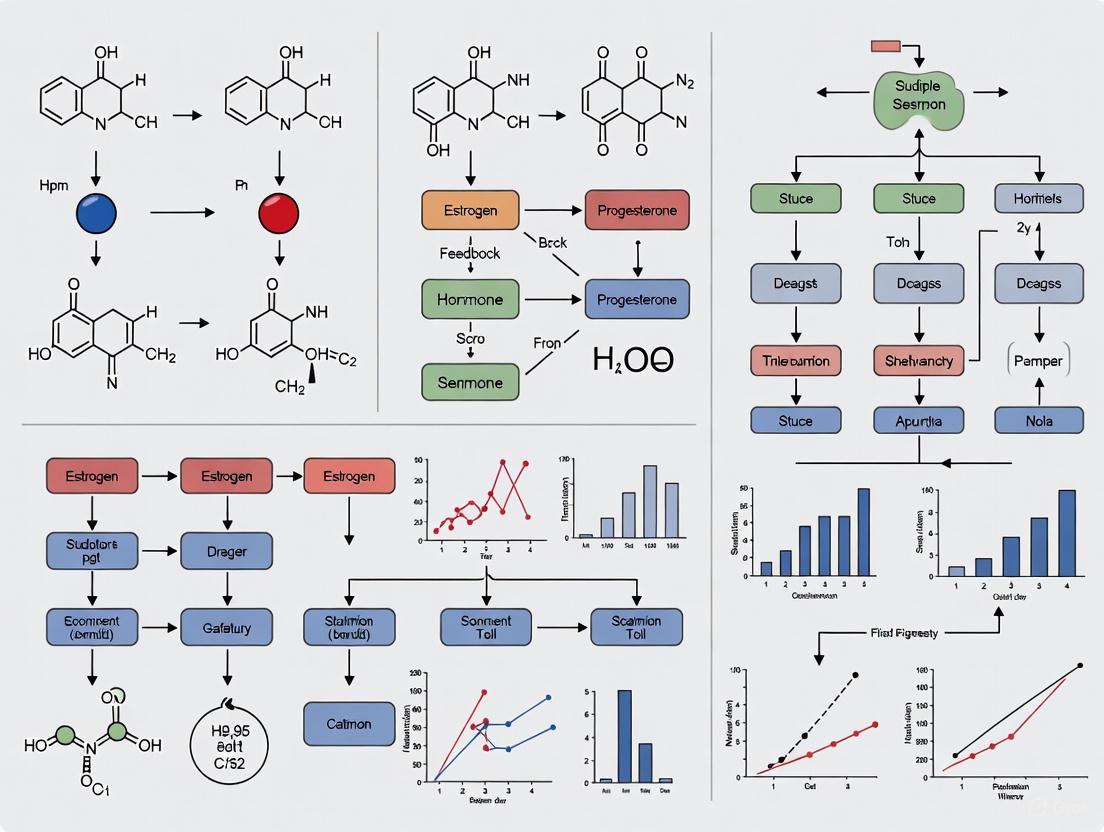
The following diagram illustrates how measurement neglect triggers a cascade of effects culminating in institutional trust erosion:
Visualizing the Menstrual Cycle Research Validation Pathway
This workflow depicts the integration of multiple validation methods for robust menstrual cycle measurement:
Addressing measurement neglect in menstrual cycle research requires concerted implementation of validated methodologies, vigilant data quality practices, and inclusive study designs. By adopting the troubleshooting approaches outlined in this technical support document, researchers can enhance the validity and impact of their work while contributing to the restoration of scientific trust. The development of transdisciplinary standards for menstrual cycle assessment represents a critical frontier in reproductive health research—one that demands methodological rigor equal to the biological complexity and societal importance of this fundamental physiological process.
The study of the menstrual cycle is inherently transdisciplinary, spanning fields from gynecology and sports physiology to psychology and public health. Despite its profound importance as a key indicator of health and wellbeing, research remains fractured across numerous disciplines, each with its own methodologies and terminologies. A recent systematic review highlighted this issue, finding that of 94 identified instruments for measuring menstrual changes, only three had good scores for both quality and utility for clinical trials [6]. This lack of standardization creates significant challenges for comparing results across studies, conducting systematic reviews, and accumulating knowledge about menstrual cycle function [2] [3]. The consequences extend beyond academic circles—during the introduction of COVID-19 vaccinations, the absence of systematic data collection on menstrual changes in vaccine trials led to confusion and eroded trust when people experienced cycle alterations [6]. This technical support center aims to bridge this disciplinary divide by providing standardized troubleshooting guides, methodologies, and frameworks for researchers across all fields studying menstrual endpoints.
Foundational Concepts: Understanding Menstrual Cycle Parameters
Defining Core Menstrual Cycle Characteristics
A eumenorrheic (healthy) menstrual cycle is characterized by predictable fluctuations in ovarian hormones, primarily estradiol (E2) and progesterone (P4), which drive both reproductive and systemic effects throughout the body [2]. The International Federation of Gynecology and Obstetrics (FIGO) establishes four key parameters for normal uterine bleeding: frequency (every 24-38 days), duration (up to 8 days), regularity (cycle length variation of ± 4 days), and volume (defined as "normal" by the patient without quality of life interference) [6]. The average menstrual cycle lasts 28 days, but healthy cycles can vary between 21-37 days [2]. The follicular phase (day 1 until ovulation) typically lasts 15.7 days but shows considerable variability, while the luteal phase (post-ovulation until menstruation) is more consistent at approximately 13.3 days [2].
Hormonal Dynamics Across Cycle Phases
The menstrual cycle features complex hormonal interactions that can be divided into six distinct phases based on hormonal fluctuations: early follicular, late follicular, ovulation, early luteal, mid-luteal, and late luteal [11]. Estradiol rises gradually through the mid-follicular phase, spikes dramatically before ovulation, and exhibits a secondary peak during the mid-luteal phase. Progesterone remains low during the follicular phase but rises gradually after ovulation, peaking during the mid-luteal phase before declining rapidly if no fertilization occurs [2]. These hormonal fluctuations have systemic effects beyond reproduction, influencing metabolism, immune function, neural processing, and cardiovascular regulation [11] [2].
Table 1: Key Hormonal Fluctuations Across the Menstrual Cycle Phases
| Cycle Phase | Estradiol (E2) | Progesterone (P4) | Other Key Hormones |
|---|---|---|---|
| Early Follicular | Low and stable | Low and stable | FSH begins to rise |
| Late Follicular | Rapid rise and peak | Low and stable | LH surge triggers ovulation |
| Ovulation | Sharp decline post-surge | Begins to rise | LH and FSH peak |
| Early Luteal | Secondary rise | Gradual increase | - |
| Mid-Luteal | Secondary peak | Peaks | - |
| Late Luteal | Decline | Sharp decline | - |
Common Methodological Challenges & Troubleshooting Guides
FAQ: Determining Menstrual Cycle Phase
Q: What is the most accurate method for determining menstrual cycle phase in research settings?
A: The most rigorous approach involves a combination of methods rather than relying on a single indicator. The gold standard includes: (1) Forward-count and backward-count methods for cycle day calculation using menstrual start dates as anchor points; (2) Urinary luteinizing hormone (LH) testing to identify the pre-ovulatory surge; (3) Serum or salivary hormone measurement of estradiol and progesterone; and (4) Basal body temperature (BBT) tracking to confirm ovulation through the biphasic pattern [2] [3]. Quantitative urine hormone monitors that measure multiple hormones (FSH, E1G, LH, PDG) show promise for at-home monitoring while maintaining accuracy comparable to serum measurements [4].
Q: Why can't I rely solely on calendar counting or period-tracking apps for phase determination?
A: Calendar counting alone is insufficient because menstrual cycle length variability is primarily attributable to follicular phase variation [2]. Additionally, a significant percentage of cycles that appear regular by calendar tracking actually exhibit subtle menstrual disturbances such as anovulation or luteal phase deficiency [12]. One study found that when cycles are assessed solely based on regular menstruation, up to 66% of exercising females had undetected menstrual disturbances despite normal cycle lengths [12]. Most menstrual tracking apps have been shown to be inaccurate, with additional concerns about data privacy and security [4].
FAQ: Participant Selection and Characterization
Q: What criteria should I use to characterize participants as "eumenorrheic" in my study?
A: A eumenorrheic menstrual cycle should be characterized by: (1) cycle lengths ≥21 days and ≤35 days; (2) nine or more consecutive periods per year; (3) evidence of an LH surge; and (4) the correct hormonal profile with confirmed ovulation and sufficient progesterone during the luteal phase [12]. The term "naturally menstruating" should be used when cycle length criteria are met but no advanced testing confirms the hormonal profile. Transparent reporting of which criteria were used for participant characterization is essential for study interpretation and replication [12].
Q: How can I account for between-person differences in hormone sensitivity?
A: Between-person differences in hormone sensitivity are substantial and clinically meaningful. Approximately 3-8% of reproductive-aged people meet diagnostic criteria for Premenstrual Dysphoric Disorder (PMDD), indicating abnormal sensitivity to normal hormone changes [2]. Research demonstrates that beliefs about premenstrual symptoms can influence retrospective reports, so prospective daily monitoring for at least two consecutive cycles is required for accurate PMDD diagnosis [2]. The Carolina Premenstrual Assessment Scoring System (C-PASS) provides a standardized system for diagnosing PMDD and premenstrual exacerbation of underlying disorders based on daily symptom ratings [2].
Troubleshooting Guide: Common Methodological Errors
Table 2: Troubleshooting Common Methodological Challenges in Menstrual Cycle Research
| Problem | Potential Consequences | Recommended Solutions |
|---|---|---|
| Assuming/estimating cycle phases without hormonal verification | Misattribution of phase; inclusion of anovulatory cycles; inaccurate conclusions about hormone-outcome relationships | Implement multi-method verification (LH testing, BBT, hormonal assays); clearly report verification methods and limitations [12] |
| Between-subjects designs treating cycle as between-person variable | Conflating within-person and between-person variance; inability to detect true cycle effects | Use repeated measures designs with at least 3 observations per participant across the cycle; employ multilevel modeling [2] |
| Inconsistent endpoint measurement across studies | Inability to compare findings; limited utility for systematic reviews and meta-analyses | Adopt FIGO standards for bleeding parameters; use validated instruments with good quality and utility scores [6] |
| Failure to account for contraceptive use | Confounding of natural cycle patterns; inappropriate grouping of participants | Screen for and document all hormonal contraceptive use; consider contraceptive users as a separate group [8] |
| Retrospective symptom reporting | Recall bias; false positive reports of premenstrual symptoms | Implement prospective daily monitoring; use validated daily symptom rating tools [2] |
Standardized Experimental Protocols
Protocol: Quantitative Menstrual Cycle Monitoring With Hormone Verification
Objective: To precisely track menstrual cycle phases using a combination of hormonal verification methods and bleeding patterns.
Materials:
- Urinary luteinizing hormone (LH) test strips
- Basal body thermometer (digital preferred)
- Menstrual cycle tracking app or diary
- Optional: quantitative urine hormone monitor (e.g., Mira monitor)
- Optional: salivary or serum hormone testing kits
Procedure:
- Participant Training: Train participants in proper LH testing technique, BBT measurement (upon waking, before rising), and bleeding documentation.
- Cycle Day 1 Identification: Instruct participants to mark the first day of menstrual bleeding (full red flow) as Cycle Day 1.
- LH Surge Monitoring: Begin daily LH testing from approximately cycle day 7-10 until surge is detected. Testing should occur at similar times each day, with limited fluid intake beforehand.
- BBT Tracking: Measure and record BBT daily upon waking throughout the entire cycle.
- Bleeding Documentation: Record bleeding patterns daily using standardized categories (spotting, light, medium, heavy).
- Hormonal Verification: For increased precision, schedule laboratory visits during key phases (early follicular, periovulatory, mid-luteal) for serum hormone confirmation or use quantitative urine hormone monitors.
Validation Criteria:
- Ovulation Confirmation: Detected LH surge followed by sustained BBT elevation within 1-3 days that remains elevated for at least 10 days.
- Follicular Phase: From menstruation onset (Cycle Day 1) until day before LH surge.
- Luteal Phase: From day after LH surge until day before next menstruation.
This protocol combines the accessibility of at-home tracking with the precision of hormonal verification, balancing practical concerns with scientific rigor [4] [3].
Protocol: Standardized Menstrual Bleeding Assessment
Objective: To quantitatively and qualitatively assess menstrual bleeding patterns using validated instruments.
Materials:
- Validated pictorial blood loss assessment chart (PBLAC)
- Mansfield-Voda-Jorgensen Menstrual Bleeding Scale (MVJ)
- Daily bleeding diary
- Menstrual products for saturation assessment (if applicable)
Procedure:
- Bleeding Volume Assessment:
- Distribute PBLAC to participants at beginning of study
- Instruct participants to record number of sanitary products used each day and degree of saturation
- Provide standardized pictorial guides for saturation estimation
- Bleeding Pattern Documentation:
- Implement daily bleeding diaries using categorical ratings (none, spotting, light, medium, heavy)
- Use validated scales such as MVJ for consistent categorization
- Cycle Parameter Calculation:
- Calculate cycle length from Day 1 of bleeding to Day 1 of subsequent bleeding
- Document bleeding duration in days
- Assess regularity through cycle length variation across multiple cycles
Analysis:
- Apply FIGO standards for normal uterine bleeding parameters
- Calculate intermenstrual bleeding episodes separately from menstrual bleeding
- Document impact on quality of life and activities of daily living [6] [4]
Visualization: Experimental Workflows and Methodological Relationships
Diagram 1: Comprehensive Workflow for Menstrual Cycle Research Methodology
The Researcher's Toolkit: Essential Materials and Instruments
Table 3: Essential Research Tools for Standardized Menstrual Endpoint Measurement
| Tool Category | Specific Instruments/Assays | Primary Function | Key Considerations |
|---|---|---|---|
| Hormone Verification | Urinary LH test strips | Detection of LH surge predicting ovulation | Test timing critical; false surges possible |
| Quantitative urine hormone monitors (e.g., Mira) | Measures multiple hormones (FSH, E1G, LH, PDG) | Emerging technology; requires validation [4] | |
| Serum hormone assays (E2, P4) | Gold standard hormone quantification | Resource-intensive; limited sampling frequency | |
| Salivary hormone kits | Non-invasive hormone measurement | Validation against serum required [3] | |
| Cycle Tracking | Basal body thermometer | Detection of post-ovulatory temperature shift | Requires consistent morning measurement |
| Menstrual bleeding diaries | Documentation of timing and intensity | Use validated scales (e.g., MVJ) [4] | |
| Pictorial blood loss assessment | Quantitative bleeding measurement | Correlates with actual blood loss [6] | |
| Symptom Assessment | Daily symptom rating scales | Prospective symptom monitoring | Essential for PMDD/PME diagnosis [2] |
| Carolina Premenstrual Assessment Scoring System (C-PASS) | Standardized PMDD/PME diagnosis | Available as worksheet, Excel, R, SAS macros [2] | |
| Data Analysis | Multilevel modeling software | Appropriate statistical analysis for repeated measures | Accounts for within-person variability [2] |
Standardizing menstrual endpoint measurement across disciplines requires concerted effort to adopt common methodologies, terminologies, and validation criteria. By implementing the troubleshooting guides, experimental protocols, and methodological frameworks outlined in this technical support center, researchers across diverse fields can contribute to a more coherent and cumulative science of menstrual health. The transdisciplinary need for standardized menstrual endpoints extends beyond academic consistency—it represents a fundamental requirement for advancing understanding of a key physiological process that influences nearly every aspect of health and wellbeing for half the global population. As research in this area accelerates, particularly in elite sport and pharmaceutical development, maintaining methodological rigor while developing pragmatic approaches for diverse research settings will be essential for generating valid, reliable, and actionable knowledge.
The study of the menstrual cycle is fraught with methodological inconsistencies that have significantly impeded scientific progress and the development of safe, effective treatments for people who menstruate. Despite decades of research, laboratories worldwide have failed to adopt consistent methods for operationalizing the menstrual cycle, leading to substantial confusion in the literature and frustrating attempts at systematic reviews and meta-analyses [2]. This problem is particularly acute in clinical trials, where the recent introduction of COVID-19 vaccinations highlighted critical gaps in data collection when vaccinated individuals reported menstrual changes that hadn't been systematically assessed during development [6]. The menstrual cycle represents a complex, dynamic system with profound implications for health, human rights, and sociocultural and economic wellbeing [6]. This technical support document establishes core parameters requiring quantification and provides standardized methodologies to advance rigorous, reproducible research on menstrual cycle endpoints.
Core Parameters for Quantification
Cycle Length and Regularity Parameters
The International Federation of Gynecology and Obstetrics (FIGO) has established clinical standards defining normal and abnormal uterine bleeding, providing a critical foundation for research parameterization [6] [13]. These parameters should form the baseline for all clinical and research assessments.
Table 1: Core Menstrual Cycle Parameters and FIGO Definitions
| Parameter | FIGO Normal Range | Abnormal Classification | Measurement Method |
|---|---|---|---|
| Cycle Frequency | Every 24-38 days | Short (<24 days) or long (>38 days) cycles | First day of one menses to first day of next |
| Bleeding Duration | ≤8 days | >8 days | Self-reported bleeding days |
| Cycle Regularity | Variation of ≤7-9 days between cycles | Variation >7-9 days | Standard deviation of consecutive cycle lengths |
| Bleeding Volume | "Normal" per patient assessment; no quality of life interference | Heavy (increases anemia risk) or light | Qualitative assessment; pictorial blood loss charts |
The follicular phase demonstrates substantially greater variability (15.7 ± 3 days; 95% CI: 10-22 days) compared to the luteal phase (13.3 ± 2.1 days; 95% CI: 9-18 days) [2]. Research indicates that 69% of variance in total cycle length is attributable to follicular phase variance, while only 3% stems from luteal phase variance [2]. This variability has profound implications for study design, particularly when testing interventions hypothesized to have phase-dependent effects.
Hormonal Parameters
Hormonal fluctuations represent the primary drivers of menstrual cycle changes, yet their measurement presents significant methodological challenges. The characteristic patterns of estradiol (E2) and progesterone (P4) across phases provide the biochemical foundation for cycle phase determination.
Table 2: Hormonal Parameters Across Menstrual Cycle Phases
| Cycle Phase | Estradiol (E2) Profile | Progesterone (P4) Profile | LH/FSH Status | Key Physiological Markers |
|---|---|---|---|---|
| Early Follicular | Low and stable | Consistently low | Baseline FSH | Menstrual bleeding |
| Late Follicular | Gradual rise then pre-ovulatory spike | Remains low | LH surge initiation | Cervical mucus changes |
| Ovulation | Dramatic peak | Begins gradual rise | LH peak, ovulation | Temperature shift onset |
| Early Luteal | Initial drop then gradual rise | Gradually rising | Post-surge decline | Sustained temperature elevation |
| Mid-Luteal | Secondary peak | Peaking levels | Low levels | Peak progesterone effects |
| Late Luteal | Rapid decline | Rapid decline | Low levels | Premenstrual symptoms |
Recent technological advances now enable more precise hormone monitoring through at-home urine tests that quantitatively track luteinizing hormone (LH) and pregnanediol-3-glucuronide (PdG), a urinary progesterone metabolite [14]. These methods represent significant improvements over traditional qualitative ovulation predictor kits.
Experimental Protocols and Methodologies
Phase Verification and Ovulation Confirmation
Gold Standard Protocol for Phase Determination
For research requiring precise phase identification, the following multi-modal approach is recommended:
Initial Cycle Day Tracking: Document first day of menstruation (Cycle Day 1) through daily self-report.
Urinary Hormone Monitoring:
- Collect daily first-morning urine samples
- Quantify LH to detect the preovulatory surge (threshold: ≥2.5 times baseline)
- Measure PdG to confirm ovulation (threshold: ≥5 μg/mL for 3 consecutive days post-LH peak) [14]
Basal Body Temperature (BBT) Tracking:
- Measure immediately upon waking before any physical activity
- Document sustained temperature rise (≥0.3°C) for 3+ days confirming ovulation
Serum Hormone Validation (Optional):
- Draw serum samples 7-9 days post-LH surge for progesterone
- Threshold: P4 ≥10 nmol/L confirms ovulatory cycle [11]
Emerging Automated Methods
Machine learning approaches using wearable device data show promise for reducing participant burden in phase tracking. One recent methodology achieved 87% accuracy classifying three phases (period, ovulation, luteal) using random forest models with physiological signals including skin temperature, electrodermal activity, interbeat interval, and heart rate [15]. Another approach utilizing circadian rhythm-based heart rate (minHR) with XGBoost algorithms demonstrated particular robustness in individuals with high variability in sleep timing, outperforming BBT-based methods by reducing ovulation detection errors by 2 days [16].
Statistical Considerations for Menstrual Cycle Data
The menstrual cycle represents a fundamentally within-person process that must be treated as such in statistical modeling. Between-subject designs comparing groups in different cycle phases conflate within-subject variance (attributable to changing hormone levels) with between-subject variance (attributable to each person's baseline symptoms), producing invalid results [2].
Minimum Design Standards:
- Repeated Measures: At least 3 observations per person across one cycle to estimate random effects
- Multi-Cycle Assessment: 3+ observations across two cycles for reliable estimation of between-person differences in within-person changes
- Phase-Specific Sampling: Strategic assessment timing based on hormonal hypotheses (e.g., mid-follicular, periovulatory, mid-luteal for E2/P4 interaction effects)
Recommended Analytical Approaches:
- Multilevel modeling (random effects modeling) to account for nested data structure
- Circular statistics or harmonic regression for cyclic patterns
- Time-varying effect models for dynamic hormone-outcome relationships
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents and Technologies for Menstrual Cycle Research
| Reagent/Technology | Function | Application Notes | Evidence Quality |
|---|---|---|---|
| Urinary LH Test Strips | Qualitative detection of LH surge | Inexpensive; limited to surge detection only | Well-validated for ovulation timing |
| Quantitative Urine Hormone Monitors (e.g., Oova, Mira) | Measures actual LH/PdG concentrations | Provides continuous hormone data; requires validation | Emerging evidence [14] [17] |
| Basal Body Temperature (BBT) Devices | Detects post-ovulatory progesterone rise | Affordable; confounded by sleep disturbances | Established but limited reliability |
| Wearable Sensors (e.g., Oura Ring, Empatica) | Continuous physiological monitoring (HR, HRV, temperature) | Reduces participant burden; machine learning analysis | Validation ongoing [15] |
| Menstrual Cycle Tracking Apps | Digital symptom and cycle day logging | Variable accuracy; depends on algorithm quality | Mixed validation results [17] |
| FIGO Bleeding Assessment Tool | Standardized bleeding characteristic documentation | Critical for uniform parameter assessment | Clinical gold standard [6] |
| Carolina Premenstrual Assessment Scoring System (C-PASS) | Diagnoses PMDD/PME from daily ratings | Eliminates retrospective recall bias | Validated against DSM-5 criteria [2] |
Troubleshooting Guide: Frequently Asked Questions
Q1: How do we accurately identify menstrual cycle phases in participants with irregular cycles?
Irregular cycles present significant methodological challenges. The recommended approach involves:
- Extending the data collection period to capture multiple cycles
- Implementing frequent (daily) hormone monitoring rather than phase-based sampling
- Using within-person standard deviations of cycle length to quantify irregularity
- Considering machine learning approaches that may be more adaptable to irregular patterns [15]
- Documenting potential causes of irregularity (energy balance, stress, medical conditions) [11]
Q2: What is the minimum number of cycles we should assess for reliable data?
The optimal number depends on research questions and outcome variability:
- For between-person differences in within-person changes: ≥2 cycles with 3+ observations each [2]
- For cycle characteristic stability (e.g., cycle length): ≥3 cycles to establish patterns
- For premenstrual disorder diagnosis: ≥2 symptomatic cycles required by DSM-5 [2]
Q3: How can we mitigate participant burden in intensive longitudinal designs?
- Utilize wearable technologies that passively collect physiological data [15]
- Implement smart notification systems rather than fixed-interval assessments
- Provide clear rationales for intensive sampling to enhance adherence
- Consider measurement-burst designs with intensive periods followed by rest
Q4: What validation methods are recommended for emerging menstrual tracking technologies?
- Conduct correlation studies with serum hormone measurements
- Compare phase identification against the multi-method gold standard
- Assess accuracy in diverse populations (including those with irregular cycles)
- Evaluate performance across the lifespan and in various health conditions [17]
Q5: How should we handle the confounding effects of hormonal contraceptives?
- Clearly document contraceptive type, formulation, and duration of use
- Consider excluding combined oral contraceptive users for studies of endogenous hormones
- For progestin-only methods, assess bleeding patterns rather than cycle phases
- Stratify analyses by contraceptive status when appropriate
Substantial methodological challenges persist in menstrual cycle research, including selection bias in study populations, measurement inconsistencies across studies, and insufficient attention to the within-person nature of cycle effects [8]. The parameters and methodologies outlined in this document provide a foundation for standardized approaches that will enhance cross-study comparability and accelerate knowledge generation. As the field advances, researchers must prioritize transparent reporting of methodological decisions, validation of emerging technologies, and inclusion of diverse populations to ensure findings generalize across the spectrum of menstrual experiences. Only through rigorous, standardized quantification of core menstrual cycle parameters can we overcome historical research gaps and advance both scientific understanding and clinical care for people who menstruate.
From Assumptions to Assays: A Toolkit for Direct Menstrual Cycle Phase Verification
Technical Support Center
Troubleshooting Guides & FAQs
Category 1: Ultrasonography Challenges
Q: During follicle tracking, what does it mean if a dominant follicle is identified but then regresses without rupture?
- A: This is a classic sign of Luteinized Unruptured Follicle (LUF) Syndrome, a known methodological challenge in endpoint confirmation. The follicle matures and even begins luteinization (as evidenced by a subsequent progesterone rise) but fails to release the oocyte. This can lead to false-positive ovulation calls if relying solely on hormone data. Confirm with serum progesterone and ensure the ultrasound protocol continues until a corpus luteum (with its characteristic "ring of fire" on color Doppler) is visualized or menstruation occurs.
Q: Our ultrasound measurements of follicle size are inconsistent between operators. How can we standardize this?
- A: Inter-operator variability is a significant source of error. Implement this protocol:
- Training: Ensure all sonographers are trained to measure the mean diameter in the sagittal and transverse planes.
- Blinding: Operators should be blinded to the participant's cycle day and previous measurements when performing a scan.
- Calibration: Regularly calibrate ultrasound equipment.
- SOP: Use a strict Standard Operating Procedure (SOP) stating that follicle size is the average of three perpendicular diameters (longitudinal, anteroposterior, and transverse).
- A: Inter-operator variability is a significant source of error. Implement this protocol:
Category 2: Serum Hormone Profiling Issues
Q: We see an LH surge in our serum profiles, but no subsequent rise in progesterone. What is the likely cause?
- A: This pattern suggests an inadequate luteal phase or an anovulatory cycle. The hypothalamic-pituitary axis triggered an LH surge, but the resulting corpus luteum is failing to produce sufficient progesterone. This highlights the critical need for multi-parameter confirmation; an LH surge alone is not a definitive endpoint for a fertile ovulatory event. Review the entire hormone profile in context.
Q: Our assay for progesterone is producing high inter-assay coefficients of variation (CV), making it hard to define the post-ovulatory rise. How can we improve reliability?
- A: High CVs undermine data integrity. Troubleshoot as follows:
- Reagent Stability: Ensure all reagents, calibrators, and controls are within their expiration dates and have been stored correctly.
- Plate Layout: Use a randomized plate layout to avoid systematic bias. Include multiple internal controls across the plate.
- Sample Integrity: Confirm samples are not repeatedly thawed and refrozen. Use single-use aliquots.
- Assay Validation: Prior to the study, validate the assay for the specific matrix (e.g., serum) and expected concentration range.
- A: High CVs undermine data integrity. Troubleshoot as follows:
Category 3: Data Integration & Endpoint Definition
- Q: How do we definitively assign the day of ovulation (DOO) when hormone and ultrasound data are slightly discordant?
- A: There is no universal consensus, which is a core methodological challenge. You must pre-define a primary endpoint in your statistical analysis plan. The most common integrated definition is:
- The day of follicle disappearance (or a sudden decrease in size) is assigned as the DOO, provided it occurs within 24-48 hours after the LH peak. If the follicle disappears before the LH peak or more than 48 hours after, the cycle may be considered anovulatory or LUF for the study's purposes.
- A: There is no universal consensus, which is a core methodological challenge. You must pre-define a primary endpoint in your statistical analysis plan. The most common integrated definition is:
Table 1: Expected Hormone Levels Across the Peri-Ovulatory Period
| Cycle Phase | Luteinizing Hormone (LH) | Follicle-Stimulating Hormone (FSH) | Estradiol (E2) | Progesterone (P4) |
|---|---|---|---|---|
| Late Follicular | Baseline (5-15 IU/L) | Baseline (5-10 IU/L) | Peak (>200 pg/mL) | Low (<1 ng/mL) |
| LH Surge | Surge (>25 IU/L) | Small parallel surge | Sharp decline | Begins to rise |
| Post-Ovulation | Drops to baseline | Drops to baseline | Low | Sustained rise (>3 ng/mL) |
Table 2: Follicular Growth and Morphological Changes via Ultrasonography
| Structure | Typical Size & Characteristics | Timing Relative to Ovulation |
|---|---|---|
| Dominant Follicle | Grows ~1.5-2.5 mm/day, reaches 17-28 mm before ovulation | -5 to -1 days before |
| Pre-Ovulatory Follicle | "Cumulus complex" may be visible on the wall. | -1 to 0 days before |
| Ovulation | Follicle suddenly collapses or disappears. Free fluid in pouch of Douglas may be seen. | Day 0 |
| Corpus Luteum | Irregular, cystic structure with "ring of fire" on color Doppler. | +1 to +2 days after |
Experimental Protocols
Protocol 1: Serial Transvaginal Ultrasonography for Follicle Tracking
- Participant Preparation: Participants should have an empty bladder for optimal visualization. Obtain informed consent.
- Equipment: Use a high-frequency transvaginal transducer (e.g., 5-9 MHz). Set machine to pre-defined gynecological settings.
- Scanning Procedure:
- Perform a systematic survey of the uterus and adnexa in both the sagittal and coronal planes.
- Identify and measure all follicles >10 mm in diameter in both ovaries.
- Measure each follicle in three perpendicular dimensions (longitudinal, anteroposterior, transverse). Record the mean diameter.
- Document the appearance of the follicle wall and the presence of any internal echoes or cumulus oophorus.
- Note the presence of free fluid in the pouch of Douglas.
- Frequency: Begin scans on cycle day ~8-10. Continue daily once a dominant follicle (>14 mm) is identified, until follicle rupture is confirmed.
Protocol 2: Serum Hormone Profiling via Electrochemiluminescence Immunoassay (ECLIA)
- Sample Collection: Collect venous blood samples daily, synchronized with ultrasound scans. Allow blood to clot, then centrifuge to separate serum. Aliquot and freeze at -80°C.
- Assay Principle: The assay uses a biotinylated monoclonal antibody and a ruthenium-complex-labeled monoclonal antibody against the target hormone (e.g., LH, FSH, P4, E2). Streptavidin-coated magnetic beads capture the complex.
- Procedure:
- Thaw samples and reagents, bring to room temperature.
- Pipette 20 µL of calibrator, control, or sample into designated wells.
- Add the specific reagent mixture (biotinylated antibody + labeled antibody).
- Incubate for 9-18 minutes (time is assay-dependent).
- Apply a voltage to the electrode, inducing electrochemiluminescence.
- Measure light emission with a photomultiplier. Intensity is proportional to hormone concentration.
- Data Analysis: Use a 4- or 5-parameter logistic curve to interpolate concentrations from the calibrators.
Visualizations
Diagram 1: HPO Axis & Ovulation Pathway
Diagram 2: Ovulation Confirmation Workflow
The Scientist's Toolkit
Table 3: Essential Research Reagents & Materials
| Item | Function & Application |
|---|---|
| Transvaginal Ultrasound Probe | High-frequency transducer for high-resolution imaging of ovarian follicles and endometrial lining. |
| ECLIA Reagent Kits (LH, FSH, P4, E2) | Ready-to-use kits for quantitative hormone analysis in serum, known for high sensitivity and wide dynamic range. |
| Biotinylated & Ruthenium-labeled Antibodies | Core components of the ECLIA; form the immunocomplex for specific hormone detection. |
| Streptavidin-coated Magnetic Beads | Solid phase for capturing the biotinylated antibody-hormone complex in the ECLIA. |
| Serum Separator Tubes (SST) | Tubes for blood collection that contain a gel separator for efficient serum recovery after centrifugation. |
| Hormone Calibrators & Controls | Essential for assay calibration and quality control to ensure inter-assay precision and accuracy. |
FAQ: Why use urinary metabolites like LH and PdG instead of serum hormones for menstrual cycle research?
Urinary hormone metabolites offer a non-invasive, practical method for field-based and at-home testing, enabling longer-term studies with higher compliance. Luteinizing Hormone (LH) in urine reliably detects the pre-ovulatory surge, while Pregnanediol Glucuronide (PdG), the primary urinary metabolite of progesterone, confirms ovulation has occurred [18]. Quantitative home-use devices can predict urinary hormone values that show high correlation with serum concentrations, providing a valid proxy for serum measurements in research settings [19].
FAQ: What are the primary methodological challenges in validating at-home hormone tests?
Key challenges include ensuring test-retest reliability and managing unexpected instrumentation failure [20]. Furthermore, menstrual cycle research itself faces inherent methodological issues such as selection bias (e.g., over-representation of women trying to conceive), cycle phase misclassification when using self-report alone, and a lack of standardization in endpoint measurements across studies [8] [21]. Validation requires demonstrating that the at-home tool can accurately capture hormone trends and defined cycle endpoints despite this variability.
Validation Data & Performance Tables
Independent studies have validated the performance of various at-home hormone monitoring systems. The data below summarizes key quantitative findings from recent research.
Table 1: Correlation between Urinary Metabolites and Serum Hormones [19]
| Urinary Metabolite | Serum Hormone | Correlation (R²) | Sample Size (Data Points) |
|---|---|---|---|
| Estrone-3-glucuronide (E3G) | Estradiol (E2) | 0.96 | 73 |
| Pregnanediol Glucuronide (PdG) | Progesterone (P4) | 0.95 | 73 |
| Luteinizing Hormone (LH) | Serum LH | 0.98 | 73 |
Table 2: Ovulation Detection Rates in a Pilot Comparative Study [22]
| Monitoring System | Cycles with Detected LH Surge | Correlation with CBFM Peak Fertility |
|---|---|---|
| Clearblue Fertility Monitor (CBFM) | 94% | Benchmark |
| Premom LH Test System | 82% | R = 0.99 |
| Easy@Home (EAH) LH Test System | 95% | R = 0.99 |
Table 3: Assay Precision of a Novel Smartphone-Based Reader [23]
| Analyte | Average Coefficient of Variation (CV) |
|---|---|
| Pregnanediol Glucuronide (PdG) | 5.05% |
| Estrone-3-glucuronide (E3G) | 4.95% |
| Luteinizing Hormone (LH) | 5.57% |
Detailed Experimental Protocols
Objective: To establish correlation between urinary metabolite concentrations measured by a home-use device and serum hormone levels.
Methodology:
- Participants: Recruit women of reproductive age (21-45) with regular cycle lengths (23-45 days). Exclude users of hormonal contraception, infertility medications, or those who are recently pregnant/breastfeeding.
- Sample Collection:
- Blood: Collect 2 ml venous blood samples in EDTA-coated vacutainers during assigned phases (early follicular, late follicular, luteal). Maintain a 10-12 hour fasting period prior. Analyze serum E2, P4, and LH using chemiluminescent immunoassays.
- Urine: Participants test first-morning urine at home using the fertility monitor on the same day as blood collection. Record test timings precisely.
- Data Analysis: Perform linear regression analysis to correlate serum hormone levels with device-predicted urinary metabolite values.
Objective: To compare the beginning, peak, and length of the fertile window as determined by a new LH tracking app versus an established fertility monitor.
Methodology:
- Design: Prospective, randomized pilot study.
- Participants: Women aged 18-42 with regular cycles, not using hormonal contraception or known to have fertility problems.
- Procedure:
- Randomize participants into groups using different LH test strips (e.g., quantitative Premom vs. qualitative Easy@Home).
- Instruct participants to test first-morning urine from cycle day 6 for 20 days over three cycles.
- On each test day, consecutively test urine with the CBFM test strip followed by the assigned LH test strip.
- Record results (low/high/peak for CBFM; quantitative/ratio for app-based strips) on a charting sheet.
- Analysis: Use Pearson correlation to compare the peak fertility day identified by the app systems with the CBFM peak day.
Troubleshooting Common Experimental Issues
Problem: Inconsistent or Erratic Hormone Readings
- Action 1 (Gather Information): Thoroughly document the unexpected readings. Check for participant compliance with testing protocols (e.g., first-morning urine, proper strip dipping time). Review any error logs or messages from the device [20].
- Action 2 (Identify Root Cause): Analyze potential sources. Common causes include diluted urine samples, improper test strip storage, device software glitches, or user error in reading results [22] [20].
- Action 3 (Resolve):
- Re-train participants on standardized collection procedures.
- Ensure test strips are stored in a cool, dry place and are not expired.
- Update device firmware or application software.
- For visual test strips, use a smartphone app for objective quantification to reduce user interpretation error [22].
Problem: Failure to Detect an LH Surge or PdG Rise
- Action 1 (Gather Information): Confirm the participant's cycle length and testing window. Review the complete cycle's data for any subtle shifts. Check if the participant has conditions like PCOS, which can cause multiple LH surges or anovulation [18].
- Action 2 (Identify Root Cause): The root cause could be a short LH surge that was missed between tests, an anovulatory cycle, or a PdG rise that is below the detection threshold of the test [18] [21].
- Action 3 (Resolve):
- Recommend testing twice daily (mid-morning and evening) as the LH surge approaches.
- Use a combination of methods (LH, PdG, BBT) to build a complete picture. A sustained BBT rise may indicate ovulation even if PdG is low, or a positive PdG test can confirm ovulation even if the LH surge was missed [18].
- If anovulation is suspected across multiple cycles, recommend clinical evaluation.
Problem: Suspected Instrument Malfunction
- Action 1 (Gather Information): Replicate the problem with a new test strip and a control solution if available. Document any error codes [24].
- Action 2 (Identify Root Cause): Follow a step-by-step approach. Isolate variables: try a different smartphone (for app-based devices), different batch of test strips, or different user [20] [24].
- Action 3 (Resolve):
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Validating Urinary Hormone Metabolites
| Item | Function in Research |
|---|---|
| Quantitative LH Test Strips | Measures the surge of Luteinizing Hormone in urine to predict impending ovulation. Provides quantitative data for trend analysis [22]. |
| PdG (Pregnanediol Glucuronide) Test Strips | Confirms ovulation by detecting the rise in the primary urinary metabolite of progesterone during the luteal phase [23] [18]. |
| E3G (Estrone-3-glucuronide) Test Strips | Tracks the rise of estrogen in the follicular phase, helping to identify the start of the fertile window [23]. |
| Smartphone-Connected Reader / App | Provides objective, quantitative readouts of test strips, reducing user interpretation error and enabling digital data collection for analysis [22] [23]. |
| Electronic Hormonal Fertility Monitor (e.g., CBFM) | An established research tool that measures E3G and LH to provide "low," "high," and "peak" fertility readings, used as a benchmark for validation studies [22]. |
| Reference Standards (for E3G, PdG, LH) | Purified metabolites used to generate calibration curves for assay validation and to determine the accuracy and recovery percentage of testing systems [23]. |
Workflow and Troubleshooting Diagrams
Research Troubleshooting Logic Flow
Urinary Hormone Validation Workflow
For researchers and drug development professionals, the accurate measurement of menstrual cycle endpoints presents a significant methodological challenge. The menstrual cycle is a dynamic process characterized by complex, individual-specific hormonal fluctuations. Relying on assumed or estimated cycle phases, rather than direct physiological measurements, introduces substantial variability and risks generating low-quality evidence [1]. This technical resource center outlines how wearable devices and apps can provide objective, continuous data to overcome these challenges, while also addressing the practical troubleshooting issues that arise in a research setting.
Technical Support & FAQs for Research-Grade Wearables
Q1: Our research team is encountering low signal quality from wrist-worn PPG sensors. What steps can we take to improve data fidelity?
- A: Low photoplethysmography (PPG) signal quality is a common issue that can compromise heart rate and heart rate variability data. Implement the following protocol:
- Device Fit: Ensure the device is snug but not constricting. It should not slide on the wrist. For studies involving prolonged wear, use adjustable, hypoallergenic bands.
- Sensor Placement: The sensor must maintain consistent skin contact. Position it on the top of the wrist, proximal to the ulnar styloid process. Provide participants with clear pictorial guides.
- Activity Logging: Instruct participants to log periods of high-motion activity (e.g., typing, vigorous exercise) as these can introduce motion artifact. This metadata is crucial for post-processing and data cleaning.
- Data Quality Checks: Implement automated checks for signal-to-noise ratio. Define exclusion criteria a priori, such as segments where more than 20% of data is lost to artifact.
Q2: How can we validate that a wearable is accurately capturing menstrual cycle phases and not just sleep/wake cycles or activity patterns?
- A: Validation is a multi-step process requiring a combination of device data and gold-standard references:
- Multi-Modal Sensing: Utilize devices that capture multiple parameters (e.g., resting heart rate, heart rate variability, skin temperature, sleep data). Correlated fluctuations across several parameters strengthen the phase prediction [25] [15].
- Ground Truthing: For a subset of your cohort or a validation cycle, correlate wearable data with direct hormonal assays. This includes urinary luteinizing hormone (LH) tests to pinpoint ovulation and serum (or validated salivary) progesterone levels to confirm luteal phase status [1].
- Algorithm Transparency: When selecting a device or platform, inquire about the machine learning model used for phase prediction (e.g., Random Forest, XGBoost) and the features it relies on. Models using a combination of circadian-based heart rate features and cycle day have shown high accuracy [16].
Q3: What is the best practice for handling data from participants with irregular sleep patterns or shift work?
- A: Irregular sleep timing is a known confounder for metrics like Basal Body Temperature (BBT). Wearables can offer more robust solutions.
- Circadian Metrics: Leverage features that are less dependent on sleep timing. One study developed a model using the heart rate at the circadian rhythm nadir (
minHR), which significantly outperformed BBT in participants with high sleep timing variability, reducing ovulation day detection errors by two days [16]. - Sleep Stage Data: Use the device's sleep staging (awake, light, deep, REM) to identify the most quiescent periods for analysis, rather than relying on arbitrary clock times.
- Stratified Analysis: Plan to stratify your analysis based on sleep regularity metrics, which can be derived from the wearable data itself.
- Circadian Metrics: Leverage features that are less dependent on sleep timing. One study developed a model using the heart rate at the circadian rhythm nadir (
The following tables summarize key quantitative findings from recent large-scale studies on cardiovascular fluctuations across the menstrual cycle, providing reference values for researchers.
Table 1: Population-Level Cardiovascular Metrics Across the Menstrual Cycle in Naturally Cycling Individuals (n=11,590) [25]
| Metric | Nadir (Lowest Point) | Offset from Cycle Mean | Peak (Highest Point) | Offset from Cycle Mean | Average Amplitude (Peak-Nadir) |
|---|---|---|---|---|---|
| Resting Heart Rate (RHR) | Day 4.81 | -1.83 BPM | Day 26.44 | +1.64 BPM | 2.73 BPM |
| HRV (RMSSD) | Day 27.13 | -3.22 ms | Day 4.81 | +3.57 ms | 4.65 ms |
Table 2: Performance of Machine Learning Models in Menstrual Phase Classification [16] [15]
| Study Model | Input Features | Classification Task | Accuracy | Key Validation Note |
|---|---|---|---|---|
| XGBoost [16] | Cycle day + Heart Rate at Circadian Nadir (minHR) |
Luteal Phase vs. Follicular Phase | High (Specifics not given) | Outperformed BBT in high sleep variability; reduced ovulation error by ~2 days. |
| Random Forest (Fixed Window) [15] | HR, IBI, EDA, Temperature | 3 Phases (Period, Ovulation, Luteal) | 87% | AUC-ROC: 0.96; Leave-last-cycle-out cross-validation. |
| Random Forest (Sliding Window) [15] | HR, IBI, EDA, Temperature | 4 Phases (Period, Follicular, Ovulation, Luteal) | 68% | AUC-ROC: 0.77; Simulates real-world daily tracking. |
Experimental Protocols for Wearable-Based Endpoint Measurement
Protocol 1: Validating Menstrual Cycle Phase Classification
Objective: To establish a robust methodology for classifying menstrual cycle phases in a research cohort using wearable-derived data, validated against hormonal markers.
Materials: Research-grade wearable devices (e.g., Oura Ring, Empatica Embrace, Garmin watch) capable of continuous PPG and skin temperature monitoring; urinary LH test kits; saliva collection kits for progesterone assay; a digital platform for participant symptom logging.
Methodology:
- Participant Onboarding: Recruit participants meeting inclusion criteria (e.g., premenopausal, naturally menstruating). Define "naturally menstruating" as cycle lengths of 21-35 days, with no confirmed hormonal status, and "eumenorrheic" as meeting the same criteria with confirmed ovulation and sufficient progesterone [1].
- Data Collection: Continuous physiological data is collected via the wearable device for the duration of the study (minimum two complete cycles). Participants self-administer urinary LH tests daily from cycle day 10 until a surge is detected. Saliva samples for progesterone assay are collected in the mid-luteal phase (e.g., days 19-22).
- Phase Determination:
- Ovulation: The day after the positive urinary LH test is designated as ovulation day.
- Luteal Phase: Defined as the period from post-ovulation to the onset of next menses, confirmed by elevated progesterone levels in saliva.
- Follicular Phase: Defined as the period from menses onset to ovulation.
- Data Analysis: Machine learning models (e.g., Random Forest) are trained using features extracted from the wearable data (e.g.,
minHR, nightly average skin temperature, HRV). The model's phase classification output is validated against the ground-truth hormonal phase labels.
Protocol 2: Calculating Cardiovascular Amplitude as a Novel Endpoint
Objective: To derive and analyze the "cardiovascular amplitude" metric for investigating the magnitude of physiological fluctuation and its association with factors like age and hormonal birth control use.
Materials: Wrist-worn wearable device with PPG capabilities; a validated menstrual cycle tracking app.
Methodology:
- Data Acquisition: Collect continuous RHR and RMSSD data across multiple complete menstrual cycles.
- Cycle Alignment: Align all cycle data to a standardized length (e.g., 28 days) or use the participant's actual cycle length, clearly stating the method.
- Amplitude Calculation:
- RHR Amplitude (RHRamp): For each cycle, calculate the mean RHR during the early cycle window (days 2-8, centered on the population nadir at day 5). Subtract this from the mean RHR during the late luteal window (the final 7 days of the cycle) [25].
- RMSSD Amplitude (RMSSDamp): Perform the same calculation for RMSSD (mean days 2-8 minus mean final 7 days).
- Cohort Analysis: Calculate the average RHRamp and RMSSDamp for each participant. Use generalized linear models to test for associations with age, BMI, and birth control status. As demonstrated, birth control pill use is associated with a significant attenuation of cardiovascular amplitude [25].
Research Reagent Solutions: Essential Materials for Wearable-Based Studies
Table 3: Key Materials and Tools for Menstrual Cycle Research Using Digital Technology
| Item | Function in Research | Example Products / Models |
|---|---|---|
| Research-Grade Wearables | Continuous, raw data collection of physiological signals (PPG, accelerometry, EDA, temperature). | Empatica EmbracePlus, E4 Wristband [15], Oura Ring [26] |
| Medical-Grade Wearables | FDA-approved devices for clinical endpoint monitoring (ECG, respiratory rate). | VitalPatch [26], BioBeat wearables [26] |
| Hormonal Assay Kits | Provide gold-standard validation for ovulation (LH) and luteal phase confirmation (Progesterone). | Urinary LH test kits (OTC), Salivary Progesterone ELISA Kits |
| Digital Logging Platforms | Secure collection of participant-reported outcomes (symptoms, medication) and ground-truth labels (menses onset). | Custom REDCap surveys, Commercial FDA-cleared apps |
| Data Analysis Software | Machine learning model training, statistical analysis, and data visualization. | Python (scikit-learn, XGBoost), R, MATLAB |
Workflow and System Diagrams
Research Workflow for Wearable-Based Endpoint Measurement
Wearable Data Processing for Research Endpoints
Frequently Asked Questions (FAQs)
Q1: What is the core terminology change recommended for discussing menstrual changes in clinical trials? The consensus recommends a shift to patient-centered and accessible language. The term "Contraceptive-Induced Menstrual Changes (CIMCs)" should be prioritized to accurately describe the full range of user experiences, moving away from technical or potentially stigmatizing terms like "bleeding patterns." This ensures the language in trial protocols, data collection tools, and eventual product labeling is clear and meaningful to patients [27] [28].
Q2: How should we select a Patient-Reported Outcome Measure (PROM) for CIMCs? The selection process must be scientifically rigorous. The chosen PROM must be a validated instrument designed to measure a specific concept, such as symptoms or impacts on daily life [29]. For CIMCs, a disease-specific (in this case, condition-specific) PROM is strongly recommended over a generic one. This ensures the tool is relevant and responsive to the specific changes caused by contraceptives, includes items that matter to users, and avoids irrelevant questions that can lead to poor data quality [29]. The instrument should have evidence of proper development, validation, and testing for the intended population [29].
Q3: What are the key considerations for designing the data collection strategy? The consensus emphasizes standardized data collection of primary CIMC and acceptability outcomes [28]. Key recommendations include:
- Accounting for Confounders: The study design and recruitment strategy must consider intrinsic (e.g., age, BMI) and extrinsic factors (e.g., concomitant medications) that could influence menstrual outcomes [28].
- Harmonized Analysis: Pre-specify statistical analysis plans that use harmonized approaches, including how to handle the common challenge of missing data [28].
- Standardized Data Elements: Using Common Data Elements (CDEs), as demonstrated in other fields like circadian rhythm and stroke research, provides a framework for aggregation and comparison across studies [30].
Q4: Our trial uses electronic data capture. Are there standards for structuring this data? Yes. For regulatory submissions, implementing CDISC Foundational and Therapeutic Area Standards is often required. These standards provide models and specifications for data representation, facilitating data sharing, improving quality, and streamlining regulatory review [31]. This ensures your data on CIMCs and PROs is structured in a consistent, predictable format.
Troubleshooting Guides
Issue 1: Inconsistent Endpoint Reporting Across Trial Sites
Problem: Investigator-reported events of abnormal bleeding or other CIMCs are inconsistent, with varying interpretations of definitions across different clinical sites, potentially introducing bias.
Solution: Implement a Central Endpoint Adjudication Committee (CAC).
- Background: Central adjudication is a standardized process for the independent, blinded assessment of safety and efficacy endpoints in clinical trials. It aims to achieve consistency and accuracy, reducing variability from site-based assessments [32].
- Procedure:
- Develop a Charter: Create a detailed charter that specifies the CAC's composition (e.g., clinical specialists in gynecology), operating procedures, and, most critically, the precise endpoint definitions for all CIMCs [32].
- Define Endpoints: Establish clear, objective criteria for different types of menstrual changes (e.g., amenorrhea, frequent bleeding, heavy bleeding) based on the consensus recommendations [28].
- Collect Source Documents: The Endpoint Office (EPO) collects relevant source documents (e.g., patient diaries, PRO questionnaires, clinical notes) for each potential event [32].
- Blinded Review: Two independent, blinded reviewers assess each event package. If they agree, the event is classified. Disagreements are resolved through a pre-defined consensus process or a third reviewer [32].
Workflow for Central Adjudication of Endpoints
Issue 2: High Rates of Missing PRO Data
Problem: Patients are failing to complete daily diaries or electronic PRO (ePRO) questionnaires about their bleeding, leading to significant missing data.
Solution: Enhance PRO instrument selection and patient-centric procedures.
- Background: Missing PRO data often stems from patient burden, irrelevant questions, or complex interfaces [29].
- Procedure:
- Validate the Instrument: Ensure the chosen PRO is a validated, condition-specific measure developed with direct patient input to maximize relevance and acceptability [29] [28].
- Simplify and Train: Use simplified terminology as per consensus and provide comprehensive training to patients on how to use the diary or ePRO device [28].
- Implement Reminders: Configure automated reminders within the ePRO system.
- Plan for Analysis: Pre-specify in the statistical analysis plan the methods for handling missing data (e.g., multiple imputation) to minimize bias [28].
Issue 3: Difficulty Aggregating or Comparing Results with Other Studies
Problem: The data collected on CIMCs cannot be easily compared or aggregated with findings from other trials, limiting its broader scientific value.
Solution: Adopt standardized data elements and implement regulatory data standards.
- Background: Lack of standardization in definitions, collection methods, and data structure prevents meaningful cross-trial comparison [30] [28].
- Procedure:
- Adopt Common Data Elements (CDEs): Follow the consensus recommendations to implement standardized data elements for CIMCs, similar to approaches in other fields like circadian rhythm research [30] [28].
- Use Controlled Terminology: Apply standardized terminologies (e.g., for bleeding intensity or duration) as outlined in the consensus to ensure consistency [28] [31].
- Implement CDISC Standards: Structure the final trial data using CDISC standards, including SDTM for tabulation and ADaM for analysis, to meet regulatory requirements and enable pooling with other studies [31].
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key resources for implementing consensus standards in CIMC research.
| Item | Function in CIMC Research |
|---|---|
| Validated PRO Instrument | A condition-specific, psychometrically validated questionnaire to quantitatively measure the patient's experience of menstrual changes and their impact [29] [28]. |
| Central Adjudication Committee (CAC) | A panel of independent clinical experts who apply standardized definitions to consistently classify reported CIMC events across all trial sites, reducing bias [32]. |
| Common Data Elements (CDEs) | Standardized definitions and formats for collecting key data points (e.g., "amenorrhea," "heavy bleeding duration"), enabling data aggregation and cross-study comparison [30] [28]. |
| CDISC Standards | A suite of data standards (e.g., SDTM, ADaM) required by many regulators for submission. They provide a consistent structure for organizing CIMC and PRO data, ensuring traceability and interoperability [31]. |
| Electronic Data Capture (EDC) & ePRO System | A secure, compliant digital platform for direct capture of site data and patient-reported outcomes in real-time, which can be configured with reminders to reduce missing data [29]. |
Navigating Pitfalls: Strategies to Overcome Common Methodological Errors in Cycle Research
In menstrual cycle research, the common practice of assuming or estimating cycle phases based on calendar counting presents a fundamental scientific problem. This approach, often adopted for pragmatic reasons in field-based research, lacks the methodological rigor necessary to produce valid and reliable data [1]. Replacing direct hormonal measurements with calendar-based assumptions amounts to guessing the occurrence and timing of critical ovarian hormone fluctuations, which can have significant implications for understanding female athlete health, training adaptations, performance outcomes, and injury risk [1] [33].
The physiological complexity of the menstrual cycle makes assumption-based approaches particularly problematic. A eumenorrheic (healthy) menstrual cycle is characterized not just by cycle length (21-35 days) and regular menstruation, but by specific hormonal events: a luteinizing hormone (LH) surge prior to ovulation and sufficient luteal phase progesterone [1]. Studies relying solely on calendar-based counting cannot detect subtle menstrual disturbances, such as anovulatory or luteal phase deficient cycles, which research shows can affect up to 66% of exercising females [1]. These disturbances are often asymptomatic but represent meaningful deviations from normal hormonal profiles that assumption-based methodologies inevitably miss.
FAQs: Understanding Direct Hormonal Measurement
Why is calendar-based counting insufficient for phase determination in research?
Calendar-based counting (counting days between periods) only establishes that a participant is "naturally menstruating" but provides no information about hormonal status [1]. This approach cannot detect anovulatory cycles or luteal phase deficiencies, as regular bleeding and cycle length do not guarantee normal hormonal profiles [1]. The variability in follicular and luteal phase length further complicates calendar-based approaches - within-woman follicular phase length varies by more than 7 days in 42% of women, and luteal phase length varies by more than 3 days in 59% of women [8].
What are the key hormonal events that must be confirmed through direct measurement?
The two most critical hormonal events requiring confirmation are:
- The LH surge preceding ovulation, detectable via urine tests
- Adequate luteal phase progesterone, measurable through blood or saliva sampling [1] [33]
These direct measurements provide objective confirmation of ovulatory cycles and appropriate hormonal environments for each cycle phase, eliminating guesswork in phase determination [1].
What methodological considerations are crucial when implementing direct hormone measurement?
Researchers must decide a priori on their hormonal phase-based boundaries and clearly define these in their methodology [1]. Additionally, attention should be paid to the accuracy, sensitivity, and variability of the hormonal analyses used, as these factors critically impact research reliability [1]. When using mass spectrometry methods, considerations include potential interference from substances that co-elute in preparatory columns and from epimers and structural isomers [34].
How do technological advancements support more accurate phase determination?
Menstrual cycle tracking applications present promising research tools that can overcome past study limitations when combined with validation sub-studies [8]. For hormone analysis, tandem mass spectrometry (TMS) has emerged as a method superior to immunoassays for steroid hormone measurement, offering enhanced sensitivity and specificity [35] [34]. The Journal of Clinical Endocrinology & Metabolism now only accepts papers using TMS methods for steroid analysis [34].
Troubleshooting Common Implementation Challenges
Problem: High Variability in Hormone Measurement Results
Possible Causes and Solutions:
- Cause: Interference in immunoassays from molecules structurally similar to target analytes
- Solution: Implement tandem mass spectrometry (TMS) methods which provide superior specificity for steroid hormone measurement [35] [34]
- Cause: Inadequate sample timing relative to hormonal fluctuations
- Solution: Establish standardized sampling protocols based on detected LH surge rather than calendar days
- Cause: Participant factors affecting hormone binding or metabolism
- Solution: Use equilibrium dialysis or ultrafiltration coupled with TMS to measure free hormone concentrations in cases of altered binding protein states [35]
Problem: Participant Recruitment and Retention Challenges
Possible Causes and Solutions:
- Cause: Burden of frequent laboratory visits for sample collection
- Solution: Implement field-friendly sampling methods (saliva, urine, dried blood spots) and consider at-home testing kits with proper validation
- Cause: Exclusion of diverse populations leading to selection bias
- Solution: Expand recruitment beyond traditional cohorts (e.g., beyond women trying to conceive) and ensure racial/ethnic diversity, as cycle characteristics may differ across groups [8]
- Cause: Hormonal contraceptive use confounding natural cycle assessment
- Solution: Establish clear inclusion criteria requiring absence of hormonal contraception for sufficient duration (typically ≥3 months) before testing [36]
Method Comparison Tables
Table 1: Comparison of Hormone Measurement Techniques
| Method | Applications | Advantages | Limitations |
|---|---|---|---|
| Immunoassays | Peptide hormones (LH, FSH); historical steroid measurement | Widely available; established protocols; high throughput | Potential antibody interference (∼1:200 samples); limited specificity for steroids; cross-reactivity concerns [34] |
| Tandem Mass Spectrometry (TMS) | Steroid hormones (estrogen, progesterone, testosterone) | High specificity and sensitivity; gold standard for steroids; measures multiple analytes simultaneously | Requires specialized equipment and expertise; higher initial costs [35] [34] |
| Equilibrium Dialysis + TMS | Free (bioactive) hormone measurement | Direct measurement of physiologically active hormone fraction | Technically challenging; low concentrations require high sensitivity [35] |
Table 2: Menstrual Cycle Phase Determination Methods
| Method | Data Collected | Validity for Phase Determination | Practical Considerations |
|---|---|---|---|
| Calendar-Based Counting | Cycle start dates, cycle length | Low: Cannot confirm ovulation or hormonal status; misses subtle disturbances | Minimal participant burden; low cost; suitable only for establishing "natural menstruation" [1] |
| Urinary LH Monitoring | LH surge detection | High: Confirms impending ovulation | Home testing possible; requires daily testing during fertile window; ∼97% accuracy for ovulation detection |
| Serum Progesterone | Luteal phase progesterone levels | High: Confirms ovulatory cycle and luteal function | Requires blood draws; timing critical (mid-luteal phase); establishes sufficient progesterone production [1] |
| Combined Direct Methods | LH surge + progesterone | Highest: Comprehensive ovulatory cycle confirmation | Maximum methodological rigor; higher participant burden; ideal for laboratory-based studies [1] |
Experimental Protocols for Direct Hormonal Measurement
Protocol 1: Confirmatory Ovulatory Cycle Testing
Purpose: To objectively confirm ovulation and adequate luteal phase function through direct hormonal measurement.
Materials:
- Urinary LH detection kits (qualitative or quantitative)
- Venipuncture supplies or saliva collection devices
- Laboratory equipment for progesterone analysis (preferably TMS)
Procedure:
- Cycle Day Tracking: Participants record first day of menstruation (Cycle Day 1)
- LH Surge Detection: Beginning cycle day 8-10, participants test daily first morning urine with LH detection kits until surge is detected
- Ovulation Confirmation: LH surge designated as "ovulation day" for cycle phase alignment
- Luteal Phase Verification: Serum or saliva progesterone measured 5-9 days post-LH surge
- Adequacy Threshold: Progesterone levels ≥10 nmol/L (3 ng/mL) in serum confirm adequate luteal phase [1]
Troubleshooting Notes:
- If no clear LH surge detected, consider anovulatory cycle and exclude from phase-based analysis
- If progesterone levels inadequate despite detected LH surge, classify as luteal phase defect
- For field-based studies, explore validated saliva progesterone tests or capillary blood sampling
Protocol 2: Mass Spectrometry-Based Steroid Hormone Profiling
Purpose: To simultaneously quantify multiple steroid hormones with high specificity for comprehensive cycle phase characterization.
Materials:
- LC-TMS system with appropriate analytical columns
- Steroid reference standards for calibration
- Sample preparation equipment (including equilibrium dialysis apparatus if measuring free hormones)
Procedure:
- Sample Collection: Blood samples collected at predetermined cycle phases (based on confirmed LH surge)
- Sample Preparation: Protein precipitation or solid-phase extraction; for free hormones, equilibrium dialysis or ultrafiltration separation [35]
- Chromatographic Separation: Reverse-phase LC separation optimized for steroid hormones
- Mass Spectrometric Detection: Multiple reaction monitoring (MRM) for target hormones (estradiol, progesterone, testosterone)
- Data Analysis: Quantification against calibration curves; quality control samples to ensure accuracy [35] [34]
Methodological Considerations:
- Carefully validate for potential isomeric interference (e.g., 17α-estradiol vs 17β-estradiol)
- Implement appropriate internal standards (preferably stable isotope-labeled)
- Establish laboratory-specific reference ranges for each cycle phase
Research Reagent Solutions
Table 3: Essential Research Reagents for Direct Hormonal Measurement
| Reagent/Kit | Application | Key Features | Considerations |
|---|---|---|---|
| Urinary LH Detection Kits | Ovulation confirmation | Qualitative or quantitative results; home testing capability | Choose FDA-cleared tests for research; establish laboratory-specific cutoff values |
| Mass Spectrometry Calibration Standards | Steroid hormone quantification | Certified reference materials; isotope-labeled internal standards | Source from reputable suppliers; verify purity and concentration |
| Equilibrium Dialysis Devices | Free hormone measurement | Physiologically relevant measurement; TMS compatibility | Optimize temperature and timing; account for non-specific binding |
| Sample Preparation Kits | Steroid extraction prior to TMS | Solid-phase extraction; protein precipitation | Evaluate recovery rates for each analyte; minimize matrix effects |
Visual Workflows and Methodologies
Diagram 1: Direct Measurement Experimental Workflow
Diagram 2: Hormone Measurement Methodology Decision Tree
Transitioning from assumption-based to measurement-based menstrual cycle research requires commitment to methodological rigor but is essential for generating valid, reliable data. The scientific limitations of calendar-based approaches - including inability to detect anovulatory cycles and luteal phase defects - fundamentally undermine research validity [1]. By implementing direct hormonal measurement protocols, researchers can advance our understanding of menstrual cycle impacts on health, performance, and disease.
The research community must prioritize appropriate methodology selection based on research context, whether in laboratory or field settings. While resource constraints in applied environments present real challenges, field-appropriate direct measurement methods (urinary LH detection, saliva progesterone) offer viable alternatives to assumption-based approaches [1]. Through consistent implementation of direct measurement methodologies and transparent reporting of limitations, menstrual cycle research can achieve the scientific rigor necessary to advance female-specific research and innovation across sports medicine, pharmacology, and women's health.
Mitigating Selection and Participation Bias in Study Cohort Recruitment
Technical Support Center: Troubleshooting Guides and FAQs
This technical support resource addresses common methodological challenges in recruiting study cohorts for research on menstrual cycle endpoints. The following guides and FAQs provide targeted solutions for mitigating selection and participation bias.
Frequently Asked Questions
Q1: Our study on cognitive performance across the menstrual cycle achieved only a 30% participation rate. Could this introduce selection bias?
Yes, low participation rates can significantly threaten validity. Studies with low baseline participation (e.g., 31%) demonstrate that participants often systematically differ from the target population. They are frequently more health-conscious, have higher social status, and report better health than nonparticipants [37]. In menstrual research, this could mean your participants have less symptomatic cycles, potentially underestimating the true effect of menstrual phases on cognitive performance.
- Troubleshooting Steps:
- Compare Participants to Target Population: Use available demographics (age, education, health status) to identify systematic differences [37].
- Analyze Non-Responders: Implement a short questionnaire for nonparticipants to gather core health and demographic data [37].
- Statistical Adjustment: Use methods like inverse probability weighting to correct for identified biases [38].
Q2: We are designing a longitudinal study tracking menstrual cycles. What is the most critical error to avoid in participant selection?
A critical error is assuming or estimating menstrual cycle phases without direct measurement. Using calendar-based counting alone is unreliable and amounts to guessing complex hormonal status [1]. This misclassification can introduce severe selection bias by incorrectly grouping participants into hormonal phases.
- Troubleshooting Steps:
- Implement Direct Hormonal Measurement: Use quantitative urine hormone monitors (tracking LH, E1G, PDG) or serum tests to confirm ovulation and phase [4].
- Define "Eumenorrheic" Rigorously: Beyond self-reported cycle regularity, confirm ovulation and sufficient progesterone production in the luteal phase [1].
- Report Methods Transparently: Clearly distinguish between "naturally menstruating" (cycle length 21-35 days) and "eumenorrheic" (hormonally confirmed) participants [1].
Q3: Our female athletes report that menstruation affects their training, but our objective data doesn't show a performance difference. What could explain this discrepancy?
This is a known phenomenon. Participants often perceive that symptoms negatively impact performance during menstruation, but objective cognitive and performance measures may not show this detriment [39]. This disconnect can stem from societal biases and individual symptomology not directly translating to measurable performance loss.
- Troubleshooting Steps:
- Acknowledge the Disconnect: Recognize that perceived impact is a valid outcome influencing participation and quality of life [40] [41].
- Investigate Barriers: Explore non-performance barriers like fear of leaking, lack of coach understanding, or inadequate facilities, which can affect participation and create bias in who continues the study [40] [41].
- Use Multidimensional Outcomes: Combine objective performance metrics with validated self-report tools on symptoms, mood, and barriers [39].
Quantitative Data on Participation Bias
The table below summarizes findings from a population-based cohort study, illustrating systematic differences between participants and nonparticipants [37].
Table 1: Characteristics Associated with Selective Study Participation
| Characteristic | Direction of Effect in Participants | Example Magnitude of Difference |
|---|---|---|
| Education Level | Higher | In men aged 50-69, high education was 1.5x more frequent than in the general population [37]. |
| Health Status | Better (Less Disease) | Frequency of myocardial infarction was half that of nonparticipants [37]. |
| Employment Status | More Often Employed | Participants were more likely to be employed compared to nonparticipants [37]. |
| Smoking Status | Healthier Lifestyle | Participants were more often current nonsmokers [37]. |
| Marital Status | More Often Married | Participants were more frequently married than the source population [37]. |
Experimental Protocols for Mitigating Bias
Protocol 1: Standardized Method for Menstrual Cycle Phase Verification in Research
This protocol ensures accurate, hormonally-defined participant grouping, minimizing selection bias from phase misclassification [1] [4].
- Primary Objective: To confirm ovulation and define hormonally discrete menstrual cycle phases (early follicular, late follicular, ovulation, mid-luteal) for research participation criteria.
- Participant Inclusion Criteria:
- Aged 18-40 years.
- Self-report of regular menstrual cycles (21-35 days) for the last 3 cycles.
- Not using hormonal contraception or other hormonal medication in the previous 3 months.
- Phase Verification Workflow:
- Hormonal Tracking: Participants use a quantitative at-home urine hormone monitor (e.g., Mira monitor) to track follicle-stimulating hormone (FSH), estrone-3-glucuronide (E1G), luteinizing hormone (LH), and pregnanediol glucuronide (PDG) daily [4].
- Ovulation Confirmation: A detected LH surge (>30 IU/L) followed by a sustained rise in PDG (>5 μg/mL) confirms ovulation [4].
- Phase Assignment:
- Early Follicular/Menstruation: First 1-3 days of menstrual bleeding.
- Late Follicular: 2-3 days after bleeding ceases, with rising E1G but low PDG.
- Ovulation: Day of detected LH surge.
- Mid-Luteal: 5-7 days after confirmed ovulation, with elevated PDG.
- Exclusion from "Eumenorrheic" Group: Participants with anovulatory cycles, short luteal phases (<10 days), or no clear hormonal profiles are classified as "naturally menstruating" and analyzed separately or excluded, depending on the research question [1].
Protocol 2: Active Non-Responder Analysis for Observational Studies
This protocol assesses the potential for participation bias by characterizing those who choose not to participate [37].
- Primary Objective: To compare core characteristics of study participants and nonparticipants to quantify selection bias.
- Procedure:
- Short Questionnaire: A brief, anonymous questionnaire is enclosed with all invitation and reminder letters sent to potential participants.
- Core Data Collection: The questionnaire collects minimal data on key socio-demographics (e.g., age, education), lifestyle factors (e.g., smoking status), and health (e.g., self-rated health, major diagnosed conditions) [37].
- Reasons for Nonparticipation: Includes questions on primary reasons for declining (e.g., lack of time, health problems, lack of interest) [37].
- Data Analysis:
- Use descriptive statistics and logistic regression to compare participants and nonparticipants.
- Quantify differences in the distribution of key variables (see Table 1).
- Use findings to inform statistical weighting or sensitivity analyses.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Menstrual Cycle and Bias Mitigation Research
| Item | Function/Application |
|---|---|
| Quantitative Urine Hormone Monitor (e.g., Mira) | At-home measurement of FSH, E1G, LH, and PDG to objectively track hormone dynamics and confirm ovulation for accurate phase classification [4]. |
| Urinary LH Surge Kits | Semi-quantitative detection of the pre-ovulatory LH surge to pinpoint ovulation [1]. |
| Short Non-Responder Questionnaire | A standardized, minimal-data tool to collect core information from individuals who decline full study participation, enabling bias analysis [37]. |
| Salivary Progesterone Test Kits | Non-invasive method to assess luteal phase progesterone sufficiency, confirming ovulatory cycles [1]. |
| Validated Menstrual Symptom Diary | A structured tool (e.g., Mansfield-Voda-Jorgensen Bleeding Scale) to consistently capture self-reported symptoms, bleeding patterns, and barriers [4]. |
Workflow and Relationship Diagrams
Bias Mitigation Workflow
Phase Verification Methods
Addressing High Intra- and Inter-Individual Variability in Cycle Length and Hormone Profiles
Frequently Asked Questions (FAQs)
Q1: What are the primary sources of variability I need to consider when designing a menstrual cycle study? You must account for multiple, interacting sources of variability. These include:
- Intra-individual variability: Cycle length can vary by approximately 5 days from cycle to cycle in the same individual [42].
- Inter-individual variability: Normal cycle lengths can range from 21 to 35 days across a population [43] [44].
- Hormonal variability: Hormone levels exhibit pulsatile secretion, diurnal variation, and can be affected by food intake. For instance, a single luteinizing hormone (LH) measurement has a high coefficient of variation (CV) of 28%, while estradiol (E2) and progesterone (P4) are more stable (CV ~12-13%) [45] [46].
- Demographic variability: Cycle length and variability are significantly influenced by age, BMI, and ethnicity [47] [48].
Q2: How can I accurately define and code menstrual cycle phases given the variability in follicular phase length? The luteal phase is more consistent in length (average 13.3 days, SD = 2.1 days) than the follicular phase (average 15.7 days, SD = 3.0 days) [2]. Therefore, the gold-standard method is to define cycle phases relative to a confirmed ovulation event, not solely by cycle day. Using the "reverse cycle day" method, where the onset of subsequent menses is day -1, provides a more reliable alignment of the luteal phase across subjects [2].
Q3: What is the minimum number of sampling timepoints required per cycle to reliably model within-person effects? For basic multilevel modeling, a minimum of three observations per person per cycle is required to estimate random effects [2]. However, for reliable estimation of between-person differences in within-person changes (e.g., identifying hormone-sensitive individuals), collecting three or more observations across two consecutive cycles is strongly recommended [2].
Q4: When is the most reliable time of day to collect blood samples for reproductive hormone assessment? Reproductive hormone levels show diurnal variation. Initial morning values are typically higher than the daily mean. For the most consistent baseline, collect samples in the morning after an overnight fast, as feeding—particularly a mixed meal—can significantly suppress hormone levels like testosterone (up to 34.3% reduction) [45] [46].
Troubleshooting Guides
Problem: Inability to detect a statistically significant cycle effect. Potential Causes and Solutions:
- Cause: Underpowered sampling design.
- Solution: Increase sampling density. Move from a sparse, phase-based design (e.g., 2 timepoints) to a repeated-measures design with at least 3-5 timepoints per cycle, ideally across two cycles [2].
- Cause: Misaligned cycle phases.
- Solution: Incorporate ovulation confirmation (e.g., urinary LH surge kits) and define the luteal phase based on the subsequent menses (reverse cycle day) instead of estimating ovulation as cycle day 14 [2].
- Cause: High between-subject variability is masking within-subject effects.
- Solution: Use multilevel statistical models (mixed effects models) that explicitly partition within-person and between-person variance components. Ensure your hypothesis is framed as a within-person effect [2].
Problem: Participant cycle lengths are highly irregular, complicating visit scheduling. Potential Causes and Solutions:
- Cause: Natural variation, especially in perimenopausal or adolescent populations.
- Solution: Anticipate and plan for this. For example, cycles in individuals under 20 vary by an average of 5.3 days, and for those over 50, variability can be 11.2 days [47] [48]. Use a flexible scheduling protocol that triggers assessments based on participant-reported menses onset or ovulation, not fixed calendar dates.
- Cause: Underlying medical conditions (e.g., PCOS, obesity) or hormonal contraceptive use.
Quantitative Data on Variability
Table 1: Variation in Menstrual Cycle Length by Age [47] [48]
| Age Group | Average Cycle Length (Days) | Difference from Ref. (35-39 yrs) (Days) | Cycle Variability (Days) |
|---|---|---|---|
| < 20 | 30.3 | +1.6 | 5.3 |
| 20-24 | 30.1 | +1.4 | 4.5 |
| 25-29 | 29.8 | +1.1 | 4.1 |
| 30-34 | 29.3 | +0.6 | 3.9 |
| 35-39 (Ref.) | 28.7 | - | 3.8 |
| 40-44 | 28.2 | -0.5 | 4.0 |
| 45-49 | 28.4 | -0.3 | 5.1 |
| ≥ 50 | 30.8 | +2.0 | 11.2 |
Table 2: Variation in Menstrual Cycle Length by Ethnicity [47] [48] Reference group: White, non-Hispanic.
| Ethnicity | Average Cycle Length (Days) | Difference from Ref. (Days) |
|---|---|---|
| White (Ref.) | 29.1 | - |
| Asian | 30.7 | +1.6 |
| Hispanic | 29.8 | +0.7 |
| Black | 28.9 | -0.2 |
Table 3: Variability of Single Hormone Measurements [45] [46]
| Hormone | Coefficient of Variation (CV) | Diurnal Change (9am to 5pm) | Effect of Mixed Meal |
|---|---|---|---|
| Luteinizing Hormone (LH) | 28% | Information Missing | Information Missing |
| Estradiol (E2) | 13% | Information Missing | Information Missing |
| Testosterone (T) | 12% | -14.9% | -34.3% |
| Follicle-Stimulating Hormone (FSH) | 8% | Information Missing | Information Missing |
Standardized Experimental Protocols
Protocol 1: Determining Menstrual Cycle Phase with Ovulation Confirmation This protocol provides a robust method for aligning participants' cycles based on biological markers rather than population averages [2].
- Track Menses: Participant reports first day of menstrual bleeding (Cycle Day 1).
- Predict Ovulation: Estimate ovulation window (typically ~CD10-14 in a 28-day cycle).
- Confirm Ovulation: Use at-home urinary luteinizing hormone (LH) kits. Instruct participants to test daily until a surge is detected. The day of the first positive test is designated as ovulation day (OD).
- Define Phases:
- Follicular Phase: Cycle Day 1 to OD.
- Luteal Phase: Day after OD to the day before next menses. For analysis, use "reverse cycle day" (day before next menses = -1).
Protocol 2: Timing and Collection of Hormone Samples This protocol minimizes pre-analytical variability in hormone assessment [45] [46].
- Schedule Timing: Schedule all blood draws during a consistent morning window (e.g., 8:00 - 10:00 AM).
- Fasting State: Require participants to fast overnight for a minimum of 8 hours prior to sampling.
- Sample Processing: Centrifuge blood samples within 2 hours of collection to separate serum or plasma. Aliquot and freeze samples at -80°C until batch analysis to reduce inter-assay variability.
Visualizing Variability and Workflows
Diagram 1: Conceptual framework for addressing variability.
Diagram 2: Workflow for phase determination with ovulation confirmation.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Menstrual Cycle Research
| Item | Function in Research | Key Consideration |
|---|---|---|
| Urinary LH Surge Kits | Confirms occurrence and timing of ovulation for accurate phase alignment [2]. | Prefer kits with digital readouts to reduce user interpretation error. |
| Validated Hormone Assays | Quantifies estradiol, progesterone, LH, and FSH levels in serum, plasma, or saliva. | Use highly specific assays (e.g., LC-MS/MS for steroids) and always batch analyze samples per participant. |
| Electronic Daily Diaries | Enables prospective tracking of menses onset, symptoms, and protocol adherence (e.g., LH testing) [2]. | Reduces recall bias; provides time-stamped, high-quality longitudinal data. |
| Carolina Premenstrual Assessment Scoring System (C-PASS) | Standardized tool for diagnosing PMDD and PME from daily symptom ratings, identifying potential confounding participants [2]. | Requires prospective daily symptom monitoring for at least two cycles. |
| Multilevel Modeling Software (R, SAS, etc.) | Statistically models nested data (observations within cycles within persons) to separate within-person from between-person effects [2]. | Requires sufficient density of observations (≥3 per person) to estimate random effects reliably. |
A technical guide for researchers navigating the methodological intricacies of menstrual cycle research.
Frequently Asked Questions (FAQs)
Q1: Why is a within-subject design strongly recommended for menstrual cycle research?
The menstrual cycle is a fundamentally within-person process [2]. Using a between-subject design to study cycle effects conflates variance from hormonal changes with variance from inherent differences between individuals, potentially leading to invalid results [2]. The repeated-measures approach of a within-subject design offers key advantages:
- Controls for Individual Differences: Each participant acts as their own control, accounting for baseline traits like genetics, metabolism, and personality that could confound results [49] [50].
- Increased Statistical Power: Requires fewer participants to detect an effect of the same size, making studies more cost-effective and feasible [49] [2].
- Reduces Random Noise: Participant-specific factors (e.g., a bad night's sleep) affect all tested conditions equally, making it easier to detect the true signal of the menstrual phase effect [49].
Q2: My participants believe their cognitive performance is worst during menstruation. How should I design a study to investigate this?
This question addresses a key challenge: the discrepancy between self-perception and objectively measured performance [51]. A well-designed within-subject study can objectively test this assumption.
- Design: Use a within-subject design where each participant completes a cognitive battery at multiple, verified menstrual cycle phases.
- Key Consideration: A recent study found that while participants perceived their cognitive performance to be negatively impacted during menstruation, no objective detriment was found in reaction times or errors on cognitive tasks. This highlights the importance of objective measurement and the potential influence of societal biases [51].
Q3: What is the minimal number of observations per participant needed for a robust within-subject cycle study?
For statistical reliability, a minimum of three observations per participant across one cycle is required to estimate within-person effects using multilevel modeling [2]. However, for greater confidence, especially when aiming to understand differences between individuals in their within-person changes, three or more observations across two menstrual cycles is the gold standard [2].
Q4: How can I accurately time my experimental sessions to specific menstrual cycle phases?
Rigorous phase timing is critical. Relying on self-reported cycle day alone is insufficient due to high inter-individual variability.
- Follicular Phase Length: Accounts for ~69% of the variance in total cycle length [2].
- Luteal Phase Length: More consistent, averaging 13.3 days (SD = 2.1 days) [2].
The table below outlines a robust protocol for phase timing, moving beyond a simple calendar-based approach.
| Target Phase | Recommended Timing Method | Key Hormonal Signature |
|---|---|---|
| Menstruation / Early Follicular | Day 1 of heavy menstrual bleeding (cycle day 1) [52]. | Low estrogen and progesterone [2]. |
| Late Follicular | ~2 days after bleeding has ceased [51]. | High and rising estrogen, low progesterone [2]. |
| Ovulation | Detected via urinary luteinizing hormone (LH) surge kits [51] [2]. | LH surge, estrogen peak followed by a drop [2] [53]. |
| Mid-Luteal | ~7 days after a detected ovulation [51]. | High progesterone and a secondary peak in estrogen [2]. |
Troubleshooting Guides
Problem: I'm concerned about order and learning effects in my within-subject design. Solution:
- Counterbalancing: Randomize or systematically vary the order in which conditions (e.g., cognitive tests) are presented across participants [49]. For example, with two sites (A and B), randomly assign 50% of participants to experience A then B, and the other 50% to experience B then A.
- Practice Trials: Incorporate a full practice session of the cognitive battery before the actual data collection begins to minimize learning effects during the test phases [51].
Problem: My participant pool has individuals with irregular cycles or premenstrual disorders. How do I control for this? Solution:
- Inclusion/Exclusion Criteria: Screen for and include only individuals who self-report a regular cycle (e.g., 21-35 days) and have tracked it for several months [51]. Exclude those using hormonal contraception or with conditions like PMDD, which can be a confounding variable [2].
- Prospective Symptom Monitoring: Use standardized systems like the Carolina Premenstrual Assessment Scoring System (C-PASS) to identify hormone-sensitive individuals based on prospective daily ratings, as retrospective self-reports are highly unreliable [2].
Problem: The budgetary and participant burden of a within-subject design is high. Solution:
- Leverage Technology: Use online platforms for data collection (e.g., cognitive test batteries administered from home) to reduce the need for frequent lab visits [51].
- Strategic Sampling: Focus on key hormonal contrasts. For instance, if you are testing the effect of progesterone, sampling during the mid-follicular (low progesterone) and mid-luteal (high progesterone) phases may be sufficient [2].
Experimental Protocols & Workflows
Detailed Methodology: A Model Within-Subject Study on Cognitive Performance
This protocol is adapted from a recent study investigating cognitive performance across the menstrual cycle [51].
- Objective: To determine whether cognitive performance (attention, inhibition, spatial anticipation) fluctuates across the menstrual cycle and if these fluctuations are influenced by athletic participation level.
- Participants: 54 naturally menstruating females, aged 18-40, with regular cycles, not using hormonal contraception.
- Study Design: A within-subject (repeated measures) design where each participant was tested at four key menstrual phases.
- Phase Verification: Phases were verified using a combination of first-day-of-bleed reporting and urinary ovulation (LH) kits [51].
- Procedure:
- Initial Lab Session: Participants provided informed consent, were trained on the cognitive battery, and received urinary kits for ovulation testing.
- Cognitive Battery: Participants completed a 10-15 minute online cognitive battery at home at four time points:
- Timepoint 1: First day of menstrual bleed.
- Timepoint 2: Two days after bleeding ceased.
- Timepoint 3: Day of a detected LH surge (ovulation).
- Timepoint 4: Seven days after ovulation (mid-luteal phase).
- Counterbalancing: Participants were randomly assigned to one of four groups, each starting the testing sequence at a different phase to control for order effects [51].
- Data Collected: Reaction times, error rates on cognitive tasks, and self-reported mood and symptoms.
The following diagram illustrates the experimental workflow and participant journey through the study.
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item / Solution | Function in Menstrual Cycle Research |
|---|---|
| Urinary Luteinizing Hormone (LH) Kits | Critical for objective, at-home confirmation of ovulation to accurately define the peri-ovulatory and subsequent luteal phases [51] [2]. |
| Standardized Cognitive Test Battery | A validated set of computerized tasks (e.g., Go/No-Go, spatial anticipation) to objectively measure performance changes across domains like attention and inhibition [51]. |
| Multilevel Modeling (MLM) Software | Statistical software (e.g., R, SAS) capable of running MLM (aka hierarchical linear models) to appropriately analyze nested, repeated-measures data [2]. |
| Daily Symptom Tracking App/Diary | A tool for prospective monitoring of menstrual bleeding dates and symptoms, which is more reliable than retrospective recall and essential for screening [2]. |
| Hormone Assay Kits | For directly quantifying serum or salivary levels of estradiol and progesterone to provide biochemical validation of menstrual phase in addition to timing [2]. |
Benchmarking Best Practices: Validating Novel Tools and Comparative Analysis of Measurement Frameworks
Validating Quantitative At-Home Hormone Monitors Against Serum and Ultrasound Gold Standards
The integration of quantitative at-home hormone monitors into menstrual cycle research requires rigorous validation against established clinical gold standards. These devices, which measure key reproductive hormones like luteinizing hormone (LH), estrone-3-glucuronide (E3G), pregnanediol glucuronide (PdG), and follicle-stimulating hormone (FSH) in urine, represent a significant advancement for decentralized clinical trials and longitudinal studies [54] [55]. However, their research application demands systematic verification to ensure data reliability comparable to serum measurements and transvaginal ultrasound follicular tracking [54].
The methodological challenges in menstrual cycle endpoint measurement are substantial, particularly when translating between different biological matrices (serum vs. urine) and measurement technologies [54] [56]. This technical support center provides validation protocols, troubleshooting guidance, and methodological frameworks to support researchers in generating evidence-quality data using these emerging technologies.
Key Research Reagent Solutions
The following table details essential materials and their specific functions in validation study protocols:
| Item Name | Function/Application in Research |
|---|---|
| Quantitative Hormone Monitors (Mira, Inito, Proov, Oova) | At-home devices measuring urinary hormone metabolites (E3G, LH, PdG, FSH) via lateral flow assays [57] [58] [59]. |
| ClearBlue Fertility Monitor (CBFM) | Qualitative benchmark device providing "Low," "High," and "Peak" readings for E3G and LH; serves as comparison standard in validation studies [60] [58]. |
| Serum Hormone Immunoassays | Gold standard blood measurements for estradiol, progesterone, LH, and FSH to correlate with urinary metabolite levels [54] [56]. |
| Transvaginal Ultrasound | Gold standard for tracking follicular development and confirming ovulation day [54]. |
| Urine Collection Cups | Standardized containers for first-morning urine samples to ensure consistent sample quality [57] [61]. |
| Lateral Flow Test Strips/Wands | Disposable immunoassay strips specific to each device for detecting urinary hormone metabolites [57] [59] [61]. |
Experimental Validation Protocols
Core Study Design for Device Validation
Objective: To characterize quantitative urine hormone patterns using at-home monitors and validate them against serum hormonal measurements and the ultrasound day of ovulation [54].
Population Groups:
- Group 1: Participants with consistent regular cycle lengths (24-38 days)
- Group 2: Participants with polycystic ovarian syndrome (PCOS) with irregular cycles
- Group 3: Athletes or individuals with high exercise levels with irregular cycles [54]
Inclusion Criteria: Participants aged 18-45, ability to travel to clinic for serial ultrasounds, negative pregnancy test at cycle beginning and end [54].
Exclusion Criteria: Medications affecting ovulation in previous 3 months (contraceptives, ovulation stimulants), known conditions impairing ovulation (PCOS, endometriosis, pituitary adenomas), pregnancy, breastfeeding, or surgeries impacting menstrual cycle (hysterectomy, bilateral oophorectomy) [54].
Longitudinal Tracking: Participants track menstrual cycles for 3 months with daily first-morning urine testing using the at-home monitor, serial ultrasounds for follicular tracking, and periodic serum hormone measurements [54].
Statistical Analysis Protocol
Primary Outcome Measures:
- Correlation between urine hormone values and serum levels
- Agreement between monitor-predicted ovulation and ultrasound-confirmed ovulation
- Sensitivity and specificity for detecting fertile window [54]
Analytical Methods:
- Bland-Altman analysis: Assess agreement between devices measuring same phenomenon [60]
- Hormone range values: Calculate thresholds predictive of ovulation events [60]
- Pattern recognition: Identify characteristic hormone profiles for different cycle types [58]
Comparative Device Accuracy Studies
Table 2.1: LH Surge Correlation Between Quantitative Monitors and CBFM
| Study Population | Cycles (n) | Correlation Coefficient (R) | p-value | Outliers | Agreement within ±1 day |
|---|---|---|---|---|---|
| Postpartum | 24 | 0.94 | <0.001 | 29% | 71% |
| Perimenopause | 33 | 0.83 | <0.001 | 18% | 82% |
| Regular Cycles (Pilot) | 57 | 0.98 | <0.001 | 5% | 95% |
Data compiled from [60]
Table 2.2: Hormone Threshold Validation in Postpartum and Perimenopause Transitions
| Hormone | CBFM Reading | Mira Monitor Levels | Statistical Significance |
|---|---|---|---|
| E3G | "High" vs. "Low" | Significantly higher for "High" reading | p < 0.001 |
| LH | "Peak" vs. "High" | Significantly higher for "Peak" reading | p < 0.001 |
Data from [60]
Multi-Hormone Detection Capabilities
Table 2.3: Analytical Capabilities of Current Quantitative Hormone Monitors
| Device | Hormones Measured | Sample Type | Technology | Ovulation Confirmation |
|---|---|---|---|---|
| Mira Monitor | E3G, LH, PdG, FSH | Urine | Fluorescence assay | PdG rise post-ovulation |
| Inito Monitor | Estrogen, LH, PdG, FSH | Urine | Smartphone camera + LFA | PdG steady rise |
| Proov Complete | E1G, LH, PdG, FSH | Urine | Lateral flow reader | PdG >5 μg/mL |
| Oova Monitor | LH, PdG | Urine | Lateral flow assay | PdG pattern |
| ClearBlue (CBFM) | E3G, LH | Urine | Optical intensity | LH surge only |
Data compiled from [57] [58] [59]
Technical Troubleshooting Guide
Frequently Asked Questions (FAQs)
Q1: What are the optimal sampling procedures for first-morning urine collection?
A: Always use first-morning urine for testing, as hormones are most concentrated after a long, uninterrupted collection period [57] [61]. Collect urine in a clean, dry cup rather than dipping the test wand directly into the toilet to control urine volume absorption [57]. Test immediately after collection, as hormone levels break down rapidly in urine samples [57].
Q2: How should researchers handle error messages or incomplete tests from automated readers?
A: Ensure the sampling end of the wand points downward at all times after dipping to prevent urine backflow, which causes incomplete tests [57]. Place the analyzer on a flat surface and avoid movement during the analysis countdown (typically 16 minutes), as movement interferes with reading [57]. For connectivity issues with Bluetooth-enabled devices, try resetting both the phone and analyzer, or push the "reset" pinhole on the device [57].
Q3: What validation approach is recommended for special populations like postpartum or perimenopausal participants?
A: In postpartum and perimenopause transitions, establish population-specific hormone thresholds, as standard thresholds may not apply [60]. For example, triggering ovulation before the first postpartum period often requires higher LH thresholds than regularly cycling women [60]. Use Bland-Altman analysis to assess agreement between new monitors and established methods in these populations [60].
Q4: How can researchers verify proper device function throughout a longitudinal study?
A: Implement regular quality control checks using control solutions if available. Monitor for consistent baseline readings at cycle start. Track individual participant patterns across multiple cycles to identify anomalous readings. Maintain detailed device usage logs including error messages and performance issues [57] [58].
Q5: What methodology effectively correlates urinary PdG with serum progesterone for luteal phase assessment?
A: Establish a urinary PdG threshold of ≥5 μg/mL to correlate with serum progesterone >5 ng/mL, which confirms ovulation [59]. Track PdG patterns through the implantation window (7-10 days post-LH surge), as sustained elevation correlates with significantly higher pregnancy rates [59]. Pattern recognition is more valuable than single measurements for assessing luteal phase adequacy [58].
Methodological Considerations for Research Applications
Addressing Matrix and Technology Discrepancies
The translation between serum hormones and urinary metabolites presents analytical challenges that must be accounted for in research design. Serum measurements capture active hormones, while urine tests measure hormone metabolites (E3G for estrogen, PdG for progesterone) [62]. These metabolites accurately reflect hormone production but require understanding of metabolic pathways and clearance rates [56].
Different monitoring technologies employ various detection methods - Mira uses fluorescence assays [60], while Inito uses smartphone cameras to measure lateral flow assay intensity [58]. These technological differences can yield varying absolute values while maintaining similar pattern recognition capabilities [58]. Researchers should focus on hormone trends and thresholds rather than absolute values when comparing across platforms.
Emerging Technologies and Future Directions
Wearable biosensors represent the next frontier in hormone monitoring, potentially enabling continuous estradiol measurement in sweat [56]. These nanobiosensors use synthetic aptamers specific to estradiol's secondary structure and demonstrate sub-picomolar sensitivity [56]. While currently in development, this technology addresses key limitations of current methods by enabling non-invasive, continuous monitoring without sample preparation [56].
The field continues to evolve with ongoing studies validating new monitors and establishing population-specific reference ranges. Researchers should monitor publications from specialized resources such as the "Quantitative Hormone Monitoring of the Menstrual Cycle" special issue for the latest validation studies and methodological advances [55].
Comparative Analysis of Menstrual Cycle Phase Definitions and Terminology Across Disciplines
Why is there confusion in menstrual cycle terminology, and why does it matter for research?
The study of the menstrual cycle is fractured across numerous disciplines, including physiology, clinical medicine, epidemiology, and sports science. Historically, this has led to the use of inconsistent and poorly defined terms to describe both normal and abnormal menstrual cycle characteristics [63]. This lack of standardization hampers clinical management, makes comparing research findings across studies challenging, and can obscure important biological signals [8] [63]. For instance, the term "menorrhagia" has been used in published literature to describe a symptom, a diagnosis, and a patient complaint, often without being clearly defined [63]. This variability creates significant methodological challenges for researchers and drug development professionals seeking to establish reliable menstrual cycle endpoints.
The FIGO Standardization Initiative To address this problem, the International Federation of Gynecology and Obstetrics (FIGO) established a standardized system for terminology through an international consensus process [52] [63]. The FIGO system defines normal uterine bleeding using four key parameters [52] [6]:
- Frequency: Every 24 to 38 days
- Regularity: Variation of ≤ 7-9 days (depending on age) between cycles
- Duration: Up to 8 days
- Volume: Not explicitly quantified by volume, but defined as blood loss that does not interfere with physical, social, emotional, and/or material quality of life. For research purposes, heavy menstrual bleeding is often defined as >80 mL per cycle [52].
This framework provides a critical foundation for comparative analysis, which is essential for designing robust experimental protocols and interpreting data consistently across trials.
Comparative Analysis Tables: Phase Definitions & Measurement Techniques
Table 1: Comparative Analysis of Menstrual Cycle Phase Definitions
| Discipline/System | Phase Name | Key Hormonal Drivers | Physiological Endpoints | Typical Duration (Days) | Key Variability Considerations |
|---|---|---|---|---|---|
| Reproductive Physiology [52] [42] [64] | Follicular Phase | Rising FSH, Rising Estradiol | Follicle growth, Endometrial proliferation | ~17 (10-16 days of high variability) [64] | Highly variable; primary source of cycle length differences [64]. |
| Ovulation | LH Surge, FSH Surge | Release of oocyte from ovary | ~1 day | Timing is not fixed at day 14; occurs ~14 days before next menses [42]. | |
| Luteal Phase | Rising Progesterone, Estradiol | Endometrial secretion, preparation for implantation | ~12.4 (± 2.4) [42] | Relatively constant across individuals and cycles [64]. | |
| Clinical Medicine (FIGO) [52] | Proliferative Phase | Rising Estradiol | Endometrial thickening | Variable (overlaps with menses and follicular phase) | Corresponds with the ovarian follicular phase. |
| Secretory Phase | Progesterone | Endometrial maturation | Variable | Corresponds with the ovarian luteal phase. | |
| Menstrual Phase | Withdrawal of Progesterone, Estradiol | Shedding of endometrial lining | 3-7 days (up to 8 normal) [52] | Volume and duration are critical clinical parameters. | |
| Metabolomics Research [65] | Menstrual (M) | Low Estradiol, Low Progesterone | - | Defined by bleeding | Characterized by higher levels of Vitamin D and pyridoxic acid [65]. |
| Follicular (F) | Rising Estradiol | - | Defined by hormone levels | - | |
| Peri-Ovulatory (O) | LH/FSH Surge | - | Defined by hormone levels | Increase in plasma and urine acylcarnitines [65]. | |
| Luteal (L) | High Progesterone, High Estradiol | - | Defined by hormone levels | Decrease in plasma amino acids, biogenic amines, and phospholipids [65]. | |
| Pre-Menstrual (P) | Falling Progesterone, Falling Estradiol | - | Defined by hormone levels | - |
Table 2: Comparison of Methodologies for Measuring Cycle Parameters
| Parameter | Gold Standard & Clinical Methods | Research-Grade & Emerging Technologies | Methodological Challenges & Considerations |
|---|---|---|---|
| Ovulation Confirmation | Serial transvaginal ultrasound for follicular tracking [4]. | Urinary LH surge detection (qualitative); Quantitative urinary hormone monitors (e.g., Mira monitor measuring LH, PDG) [4]. | Ultrasound is labor-intensive and expensive. Urinary LH predicts but does not confirm ovulation. PDG rise in urine confirms ovulation has occurred [4]. |
| Cycle Phase Tracking | Luteinizing Hormone (LH) testing, basal body temperature (BBT) charting [42]. | Quantitative tracking of FSH, E1G, LH, PDG in urine [4]. Multi-omics profiling (e.g., metabolomics) [65]. | BBT only confirms ovulation post-hoc and has low reliability [42]. Metabolomics shows phase-specific patterns but is not yet practical for routine use [65]. |
| Bleeding Volume Assessment | Alkaline hematin method (objective, research-only) [52]. | Pictorial Blood Loss Assessment Chart (PBLAC); Patient-completed bleeding diaries; Validated bleeding scales (e.g., Mansfield-Voda-Jorgensen) [4] [6]. | Objective measurement is impractical clinically. Self-reported measures are subjective; 40% with heavy loss consider it normal, and 14% with mild loss consider it heavy [8]. |
| Endpoint Definition | FIGO criteria for normal/abnormal bleeding [52] [63]. | App-based cycle tracking; Fertility awareness methods (FAM) [8]. | App algorithms are often inaccurate [4]. FAMs may be designed for regular cycles, excluding those with irregular cycles from research [8]. |
Troubleshooting Guides & FAQs: Addressing Methodological Challenges
FAQ 1: A significant number of cycles in our healthy study cohort are anovulatory. Is this normal?
Answer: Yes, this is a normal biological occurrence and must be accounted for in your experimental design. In healthy, cycling individuals, up to 12% of cycles can be anovulatory (without egg release) [42]. Anovulation rates are higher at the extremes of reproductive age (adolescence and perimenopause) but occur throughout the reproductive lifespan. Relying on calendar dates alone to define phases will misclassify these cycles.
Troubleshooting Guide: Do not assume ovulation occurs on day 14.
- For high-precision studies: Use quantitative urinary progesterone metabolite (pregnanediol glucuronide, PDG) tracking to biochemically confirm ovulation [4].
- For larger cohort studies: Incorporate urinary luteinizing hormone (LH) surge kits to estimate ovulation timing, acknowledging this is a prediction and not confirmation.
- In data analysis: Plan for a sensitivity analysis that excludes anovulatory cycles if they are not the focus of your research.
FAQ 2: Our study participants are reporting highly variable cycle lengths. How do we define "regular" versus "irregular" for inclusion/exclusion criteria?
Answer: Use the standardized FIGO definitions for regularity, which are age-dependent [52]:
- Ages 18-25 and 42-45: Cycles are considered regular if the variation between the shortest and longest cycle is ≤ 9 days.
- Ages 26-41: Cycles are considered regular if the variation is ≤ 7 days. A cycle is considered irregular if the variation exceeds 8 days (for age 26-41) or 10 days (for ages 18-25 or 42-45) [52].
Troubleshooting Guide:
- Baseline Data Collection: Require participants to prospectively track at least one cycle before enrollment to establish their individual variability.
- Avoid Selection Bias: Be aware that studies requiring "regular cycles" may exclude a significant portion of the population and limit the generalizability of your findings [8]. Clearly report your criteria.
FAQ 3: We are seeing discrepancies between self-reported menstrual bleeding and objective measures. How should we handle this in data collection?
Answer: This is a common and expected challenge. Self-reported bleeding intensity is highly subjective. FIGO now defines heavy menstrual bleeding not by a specific volume, but as "excessive menstrual bleeding that interferes with a person's physical, social, emotional, and/or material quality of life" [52].
Troubleshooting Guide:
- Use Validated Tools: Employ validated pictorial charts (e.g., PBAC) or scales (e.g., Mansfield-Voda-Jorgensen Menstrual Bleeding Scale) that are more correlated with objective loss than simple descriptors [4] [6].
- Combine Measures: Collect both quantitative data (e.g., number of saturated pads/tampons) and qualitative data (impact on quality of life). This provides a more comprehensive picture [6].
- Account for Intermenstrual Bleeding: Bleeding between periods can cause participants to misidentify the true start of menses. Clear instructions in daily diaries can help mitigate this [8].
Experimental Protocols for Endpoint Measurement
Protocol 1: Validating Ovulation and Phase Length with Urinary Hormones and Ultrasound
This protocol is adapted from contemporary validation studies aiming to establish a gold standard for at-home cycle monitoring [4].
Objective: To characterize quantitative urinary hormone patterns and validate them against the gold standard of serial ultrasound for determining the day of ovulation and calculating follicular/luteal phase lengths.
Materials:
- Quantitative urinary hormone monitor (e.g., Mira monitor) and corresponding test strips (FSH, E1G, LH, PDG).
- Access to transvaginal ultrasound.
- Customized app or diary for tracking bleeding and symptoms.
Methodology:
- Screening & Recruitment: Recruit participants across a range of cycle regularity. Group 1: Regular cycles (24-38 days). Group 2: Irregular cycles (e.g., PCOS). Group 3: Irregular cycles (e.g., athletes) [4].
- Cycle Tracking: Participants track cycles for 3 months. Starting from the end of menses, they use the urine monitor daily.
- Ultrasound Confirmation: When urinary hormones suggest the approach of ovulation (rising E1G, initial LH rise), participants undergo serial transvaginal ultrasounds every 1-2 days until follicle rupture (ovulation) is confirmed.
- Serum Correlation: On the day of the LH surge and the day of confirmed ovulation, serum samples are collected for correlation with urinary hormone levels.
- Data Analysis:
- The estimated day of ovulation from the urinary LH peak and PDG rise is compared to the ultrasound day of ovulation.
- Follicular phase length is calculated as (Ovulation Day - Day 1 of menses).
- Luteal phase length is calculated as (Day 1 of next cycle - Ovulation Day).
Protocol 2: Capturing Metabolic Patterns Across the Cycle Phases
This protocol is based on metabolomics research that reveals profound biochemical rhythmicity across the menstrual cycle [65].
Objective: To identify and characterize phase-specific metabolic patterns in plasma and urine throughout the menstrual cycle.
Materials:
- LC-MS and GC-MS platforms for metabolomics and lipidomics.
- HPLC-FLD for B vitamin analysis.
- Serum for clinical chemistries.
- Daily urine or serum for LH testing to define phase transitions.
Methodology:
- Phase Classification: Use serum hormones (estradiol, progesterone, FSH, LH) and urinary LH to classify cycles into 5 distinct phases: Menstrual, Follicular, Periovulatory, Luteal, and Premenstrual [65].
- Sample Collection: Collect biofluids (plasma, urine, serum) at each of the five defined phase timepoints over a single cycle.
- Laboratory Analysis:
- Analyze samples using mass spectrometry-based metabolomics to quantify amino acids, lipids, organic acids, and acylcarnitines.
- Perform targeted analysis of micronutrients (e.g., B vitamins, Vitamin D).
- Statistical Analysis: Use linear mixed-models to test for statistically significant differences in metabolite concentrations between phases, controlling for false discovery rate (e.g., FDR < 0.20). This identifies metabolites with significant rhythmicity [65].
Visualization: The Hypothalamic-Pituitary-Ovarian (HPO) Axis
Diagram 1: HPO Axis Feedback Mechanisms. This diagram illustrates the core hormonal feedback loops that govern the menstrual cycle. The switch from negative to positive feedback of estradiol (E2) at the hypothalamus and pituitary triggers the mid-cycle LH surge, which is essential for ovulation.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for Menstrual Cycle Studies
| Item | Function & Application in Research | Key Considerations |
|---|---|---|
| Quantitative Urine Hormone Monitor (e.g., Mira) [4] | At-home measurement of FSH, E1G (estrogen metabolite), LH, and PDG (progesterone metabolite). Used to predict and confirm ovulation and define phase lengths. | Provides numerical hormone values for pattern analysis. Emerging technology; requires validation against serum and ultrasound for specific research contexts. |
| Transvaginal Ultrasound | Gold standard for visualizing follicular development, measuring follicle size, and confirming the day of ovulation [4]. | Essential for validating other methods. Resource-intensive (cost, time, expertise), limiting use in large cohort studies. |
| Luteinizing Hormone (LH) Immunoassay Kits | Detects the urinary LH surge, which predicts impending ovulation (~24-36 hours prior). | Widely available and relatively inexpensive. Does not confirm that ovulation actually occurred. |
| Validated Bleeding Scale (e.g., Mansfield-Voda-Jorgensen) [4] | A standardized pictorial tool for participants to self-report volume of menstrual blood loss. | More objective than unstructured diaries. Correlates better with actual blood loss than verbal descriptors alone. |
| LC-MS / GC-MS Platforms [65] | High-throughput metabolomic and lipidomic profiling to identify and quantify hundreds of small molecules in biofluids. | Used to discover phase-specific metabolic patterns (e.g., decreased amino acids in luteal phase). Requires advanced bioinformatics for data analysis. |
| Anti-Müllerian Hormone (AMH) ELISA | Serum marker of ovarian reserve. Used to contextualize ovarian response and follicular development within a cohort [4]. | Provides information on an individual's ovarian follicular pool, which can influence cycle characteristics. |
Assessing the Utility and Quality of Existing Menstrual Cycle Measurement Instruments for Clinical Trials
Accurately measuring menstrual cycle endpoints presents a core methodological challenge in clinical trials focused on female health. Many traditional approaches rely on assumed or estimated menstrual cycle phases, an approach criticized for guessing rather than directly measuring complex hormonal fluctuations [1]. Furthermore, the proliferation of digital tracking technologies introduces new questions regarding their validation, functionality, and appropriateness for rigorous clinical research [66] [4]. This technical support guide addresses these challenges by providing troubleshooting guidance and standardized protocols for researchers navigating this complex landscape.
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: What is the primary pitfall in current methodologies for defining menstrual cycle phases in research?
The most significant pitfall is relying on assumed or estimated cycle phases without direct hormonal measurement. This approach lacks scientific rigor, as it guesses the occurrence and timing of key ovarian hormone fluctuations [1]. Calendar-based counting alone cannot detect subtle menstrual disturbances like anovulation or luteal phase deficiency, which are common in study populations and can profoundly impact trial outcomes [1]. For valid phase determination, direct measurement of hormones like luteinizing hormone (LH) and progesterone is essential.
Q2: How can I evaluate the quality of a commercial menstrual cycle tracking app for use in a clinical trial setting?
Evaluating a commercial app requires a multi-faceted assessment of its functionality, inclusiveness, and scientific basis. The table below summarizes key evaluation criteria, drawing from recent research [66]:
Table: Evaluation Framework for Menstrual Cycle Tracking Apps in Clinical Research
| Evaluation Dimension | Key Criteria | What to Look For | Common Issues |
|---|---|---|---|
| Functionality & Data Quality | Symptom Tracking | Number and relevance of tracked symptoms; use of validated measurement tools. | Mean of 17.5 relevant symptoms tracked; none used validated tools [66]. |
| Prediction Method | Algorithm basis (e.g., calendar, basal body temperature, hormonal). | Calendar-based algorithms are often inaccurate for ovulation [67]. | |
| Privacy & Security | Transparency of privacy policy; data sharing with third parties. | 71.4% of apps shared user data with third parties [66]. | |
| Inclusiveness | Gender & Sexuality | Options for neutral pronouns and diverse user identities. | 50% of apps offered neutral or no pronouns [66]. |
| Cycle Variability | Ability to accommodate irregular cycle lengths and patterns. | All evaluated apps could be tailored to non-28-day cycles [66]. | |
| Scientific Validity | Evidence Base | Citation of medical literature; clinical validation of algorithms. | Only 42.9% of apps cited medical literature [66]. |
| Educational Content | Credibility and comprehensiveness of health information provided. | Variable quality; often lacks information on when to seek care [66]. |
Q3: What are the ethical considerations regarding algorithm-driven tracking technologies?
Algorithm-driven technologies raise several nuanced ethical concerns beyond basic data privacy [68]. These include:
- Inconclusive/Inscrutable Evidence: Algorithms may present predictions based on incomplete data or use "black box" logic that users and researchers cannot scrutinize.
- Misguided Evidence & Unfair Outcomes: Algorithms can perpetuate biases, leading to inaccurate predictions for underrepresented groups (e.g., those with PCOS or diverse gender identities) and potentially causing harm, such as stress or unintended pregnancy [67] [68].
- Transformative Effects: These technologies can shape how users understand their bodies, potentially creating an over-reliance on app predictions over bodily awareness [68].
Q4: Can at-home quantitative hormone monitors be considered a viable tool for clinical trials?
Yes, at-home quantitative hormone monitors represent a promising tool for decentralizing and objectifying cycle phase measurement. Devices like the Mira monitor, which measures urinary FSH, E1G, LH, and PdG, are undergoing validation against the gold standard of serial ultrasound and serum hormone levels [4]. The primary workflow for their validation in a study setting is illustrated below.
Diagram: Protocol for Validating At-Home Hormone Monitors in Clinical Research
Experimental Protocols & Methodologies
Gold Standard Protocol for Quantitative Menstrual Cycle Monitoring
The following protocol, adapted from a prospective cohort study design, outlines the methodology for establishing a validated, quantitative approach to menstrual cycle monitoring [4].
Primary Objective: To characterize quantitative urine hormone patterns and validate them against serum hormone measurements and the ultrasound-defined day of ovulation in participants with both regular and irregular cycles.
Study Design:
- Cohort: Prospective cohort with longitudinal follow-up over three menstrual cycles.
- Groups:
- Group 1 (Control): Participants with consistent regular cycle lengths (24-38 days).
- Group 2 (PCOS): Participants with diagnosed Polycystic Ovary Syndrome and irregular cycles.
- Group 3 (Athletes): Participants engaged in high levels of exercise with irregular cycles.
Materials & Procedures:
- At-Home Hormone Monitoring: Participants use an at-home quantitative urine hormone monitor (e.g., Mira monitor) to measure FSH, E1G, LH, and PdG daily.
- Gold Standard Ovulation Confirmation: Participants undergo serial transvaginal ultrasounds at a clinical site to track follicular development and confirm the day of ovulation.
- Serum Correlation: Serum samples are collected periodically for correlation with urinary hormone levels.
- Ancillary Data: Bleeding patterns and temperature changes are recorded using a customized study app.
Key Outcome Measures: Correlation between urine hormone surge (LH) and ovulation, confirmation of luteal phase via PdG rise, and accuracy of cycle phase prediction compared to ultrasound.
Decision Framework for Instrument Selection
The diagram below provides a logical pathway for researchers to select the most appropriate menstrual cycle measurement instrument based on their trial's requirements, budget, and need for precision.
Diagram: Decision Framework for Selecting Menstrual Cycle Instruments
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Materials and Tools for Menstrual Cycle Endpoint Research
| Item | Function/Description | Utility in Clinical Trials |
|---|---|---|
| Quantitative Urine Hormone Monitor (e.g., Mira) | At-home device measuring FSH, E1G, LH, and PdG in urine. | Enables decentralized, daily hormone tracking to objectively predict and confirm ovulation and define cycle phases [4]. |
| Serum Hormone Assays | Gold-standard blood measurements of reproductive hormones (e.g., Progesterone, Oestradiol). | Provides definitive reference for validating at-home urine monitors and confirming hormonal status [4]. |
| Serial Follicular Ultrasound | Transvaginal ultrasound to visually track follicular growth and confirm ovulation day. | Serves as the ultimate gold standard for timing ovulation in validation studies [4]. |
| Validated Bleeding Scale (e.g., Mansfield–Voda–Jorgensen) | Standardized tool for quantifying menstrual blood loss. | Critical for objective assessment of bleeding patterns, a key endpoint in contraceptive and therapeutic trials [4]. |
| Temperature Tracking Wearables (e.g., Tempdrop) | Wearable sensors that track basal body temperature (BBT) with minimal user error. | Provides data for detecting the post-ovulatory temperature shift; useful for fertility awareness-based endpoints [69]. |
| Customized Study App | A purpose-built application for data collection on bleeding, symptoms, and other user-input metrics. | Ensures consistent, structured data collection across the trial population and improves participant compliance [4]. |
Research on menstrual cycle endpoints faces a significant scientific hurdle: the lack of consistent, validated methods for operationalizing the cycle across different populations [2]. This challenge is particularly acute when studying two distinct groups: athletes and individuals with Polycystic Ovarian Syndrome (PCOS). The absence of standardized approaches frustrates attempts at systematic reviews and meta-analyses, limiting the accumulation of reliable knowledge on cycle effects [2] [6].
This case study examines the specific methodological challenges in applying rigorous validation techniques when measuring menstrual cycle endpoints in these populations with irregular cycles. We explore practical troubleshooting guidance and experimental protocols to enhance the reliability and validity of future research.
Understanding the Populations: Athletic and PCOS Cycles
Polycystic Ovarian Syndrome (PCOS)
PCOS is the most common endocrine disorder among females of reproductive age worldwide, affecting between 5% and 26% of this population [70]. The pathophysiology is complex and multifactorial, characterized by:
- Chronic anovulation: Irregular or absent ovulation leading to unpredictable cycle timing and length [70]
- Hyperandrogenism: Elevated androgen levels that can disrupt normal follicular development [70]
- Insulin resistance: Present in approximately 70% of cases, independent of adiposity, further contributing to hormonal dysregulation [70]
- Altered steroidogenesis: Theca cells exhibit overexpression of steroidogenic enzymes, increasing androgen production [70]
Athletic Menstrual Cycles
Eumenorrheic cycles (regular 21-35 day cycles) occur in 67%-91% of elite female athletes [71]. However, athletic participation can influence hormonal fluctuations through:
- Energy availability: Insufficient caloric intake relative to expenditure can suppress the hypothalamic-pituitary-ovarian axis [71]
- Exercise stress: Impact on pulsatile gonadotropin-releasing hormone release [71]
- Body composition changes: Though evidence is mixed, fluctuations in total body water across phases may occur [71]
Table 1: Characteristics of Menstrual Cycles in Study Populations
| Characteristic | PCOS Population | Athletic Population | Eumenorrheic Reference |
|---|---|---|---|
| Cycle Regularity | Irregular (diagnostic criterion) [70] | Typically regular, but susceptible to exercise-induced disruptions [71] | Regular (21-35 days) [2] |
| Primary Challenge | Chronic anovulation, hyperandrogenism [70] | Potential for luteal phase defects, anovulation with intense training [71] | Normal hormonal fluctuations |
| Ovulation Prediction | Highly challenging due to irregular hormone patterns [72] | Generally reliable with confirmation recommended [39] | Predictable with standard methods [2] |
| Key Hormonal Features | Elevated androgens, LH:FSH ratio disruption [70] | Varies with training load; generally normal patterns [71] | Characteristic estradiol and progesterone patterns [2] |
Experimental Protocols and Validation Frameworks
Foundational Study Design Considerations
When investigating menstrual cycles in these populations, several methodological considerations are critical:
Study Design Selection
- Repeated measures designs are the gold standard as the menstrual cycle is fundamentally a within-person process [2]
- A minimum of three observations per person is required to estimate random effects in multilevel modeling [2]
- For reliable estimation of between-person differences in within-person changes, three or more observations across two cycles provides greater confidence [2]
Cycle Phase Categorization
- Move beyond simple follicular/luteal division to account for distinct hormonal milieus [71]
- Recommended phases: early follicular (menstruation), late follicular, ovulatory, early luteal, mid-luteal, and late luteal [71]
- The luteal phase has a more consistent length (average 13.3 days, SD=2.1) than the follicular phase (average 15.7 days, SD=3.0) [2]
Participant Recruitment and Screening
- For PCOS populations: Apply established diagnostic criteria (at least 2 of: chronic anovulation, hyperandrogenism, polycystic ovaries) [70]
- For athletic populations: Document training load, energy availability, and athletic participation level using standardized frameworks [39]
- Exclude: Hormonal contraceptive use in previous 3 months, pregnancy/breastfeeding in previous 6 months [39]
Cycle Validation and Phase Confirmation Protocols
Accurately identifying menstrual cycle phases is particularly challenging in populations with irregular cycles. The following protocol provides a rigorous approach:
Protocol: Menstrual Cycle Phase Validation for Irregular Cycles
Objective: To confirm menstrual cycle phase and ovulation in populations with irregular cycles (PCOS and athletes).
Materials:
- Urinary luteinizing hormone (LH) test kits
- Salivary ferning microscope (for PCOS populations)
- Basal body thermometer
- Standardized daily symptom tracking tool
- Venipuncture supplies for serum hormone testing (where feasible)
Procedure:
- Baseline Assessment:
Daily Monitoring:
Ovulation Detection:
- Begin urinary LH testing from cycle day 10 (or adjusted based on individual history)
- Test twice daily until LH surge detected
- Confirm ovulation with sustained basal body temperature elevation
- In PCOS populations with unreliable LH testing: Utilize salivary ferning with AI interpretation where available [72]
Phase-Specific Testing:
- Schedule experimental assessments for confirmed:
- Early follicular phase (menstruation: days 1-5 of confirmed bleeding)
- Late follicular phase (2 days after bleeding cessation, pre-ovulation)
- Ovulatory phase (within 24 hours of detected LH surge)
- Mid-luteal phase (7 days post-ovulation) [39]
- Schedule experimental assessments for confirmed:
Hormonal Validation:
- Where feasible, obtain serum progesterone during mid-luteal phase (>3 ng/mL confirms ovulation) [2]
- For multi-cycle studies: Repeat validation each cycle
Troubleshooting:
- If no LH surge detected by cycle day 25, consider anovulatory cycle and exclude from phase-based analysis
- If hormonal markers conflict with calendar-based estimates, prioritize hormonal data
- For ambiguous results, utilize transvaginal ultrasound for follicular tracking (clinical settings)
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Materials for Menstrual Cycle Endpoint Studies
| Research Tool | Primary Function | Population-Specific Considerations | Validation Evidence |
|---|---|---|---|
| Urinary LH Test Kits | Detection of LH surge predicting ovulation | Limited reliability in PCOS due to chronically elevated LH [72] | High for regular cycles; variable for PCOS [72] |
| Salivary Ferning Microscopes | Detection of estrogen-driven ferning patterns indicating fertility | Promising alternative for PCOS; requires AI interpretation for reliability [72] | Emerging evidence for irregular cycles [72] |
| Serum Hormone Panels | Gold standard quantification of estradiol, progesterone, LH, FSH, testosterone | Essential for PCOS diagnosis and cycle confirmation in both populations [70] | Well-established for cycle phase confirmation [2] |
| Standardized Daily Symptom Trackers | Prospective monitoring of physical, cognitive, and emotional symptoms | Critical for distinguishing perceived vs. measured performance [39] | Variable quality; select instruments with proven responsiveness [6] |
| Basal Body Thermometers | Tracking post-ovulatory temperature rise | Useful adjunct but insufficient alone for irregular cycles | Moderate; confounded by other factors [2] |
Troubleshooting Guides and FAQs
FAQ 1: How can we reliably detect ovulation in PCOS patients with chronically elevated LH levels?
Challenge: Traditional urinary LH kits have limited utility in PCOS due to persistently elevated LH levels, making surge detection difficult [72].
Solutions:
- Implement multi-modal detection combining salivary ferning patterns with basal body temperature tracking [72]
- Utilize emerging AI-interpreted salivary ferning technology that shows promise for irregular cycles [72]
- Employ serial transvaginal ultrasonography in clinical research settings to visualize follicular development
- Use algorithm-based approaches that integrate multiple biomarkers rather than relying on single indicators
Protocol Adjustment:
- Allocate additional budget for more sophisticated ovulation detection methods when studying PCOS populations
- Extend testing timelines to account for cycle irregularity and potential anovulatory cycles
- Collect additional serum progesterone measurements to retrospectively confirm ovulation
FAQ 2: How should we handle the high dropout rates common in multi-cycle studies of irregular populations?
Challenge: Studies requiring multi-cycle participation show high dropout rates, particularly in populations with irregular cycles where study timelines become extended [72].
Mitigation Strategies:
- Simplify study requirements to reduce participant burden [72]
- Implement flexible scheduling that accommodates unpredictable cycle lengths
- Enhance participant compensation for extended time commitments
- Incorporate remote monitoring technologies to reduce in-person visit requirements
- Refine recruitment messaging to clearly communicate timeline expectations [72]
Statistical Considerations:
- Oversample initially to account for anticipated attrition
- Implement intention-to-treat analyses to preserve randomization
- Collect reason-for-dropout data to assess potential bias
FAQ 3: What are the best practices for distinguishing between perceived versus measured performance changes across cycles?
Challenge: Research consistently shows discordance between self-reported perception of cycle impacts and objectively measured performance [39].
Methodological Approach:
- Implement blinded testing where participants are unaware of hypothesis regarding cycle phase effects
- Collect both objective performance metrics (reaction time, accuracy, strength measures) and subjective ratings of performance simultaneously [39]
- Use validated cognitive batteries specifically designed to detect subtle cycle-related fluctuations [39]
- Control for expectancy effects through careful participant briefing that avoids suggesting expected patterns
Analysis Framework:
- Calculate discrepancy scores between perceived and actual performance
- Test for systematic biases in self-assessment across cycle phases
- Include potential moderators such as athletic experience level or premenstrual symptom severity
FAQ 4: How can we address the substantial inter-individual variability in cycle characteristics and hormone sensitivity?
Challenge: There is high variability in both cycle characteristics and individual sensitivity to hormonal fluctuations, potentially obscuring group-level effects [2].
Individual-Differences Approach:
- Implement within-subject designs with adequate repeated measures to model individual response trajectories [2]
- Collect detailed cycle history including typical symptoms, regularity patterns, and hormonal sensitivity
- Test for moderator effects of factors such as athletic level, PCOS phenotype, or hormone baseline levels [39]
- Consider person-centered analyses such as cluster analysis to identify response subtypes
Reporting Standards:
- Document inter-individual variability metrics rather than focusing exclusively on central tendency
- Include individual response patterns in data visualizations
- Report proportion of participants showing clinically meaningful changes in addition to statistical significance
Data Validation and Statistical Considerations
Validation Techniques for Menstrual Cycle Endpoints
Implement rigorous validation approaches tailored to menstrual cycle research:
Temporal Validation:
- Collect data across multiple cycles to establish within-person stability of measures [2]
- Use intraclass correlation coefficients to quantify consistency across cycles
- Implement split-half reliability testing where appropriate
Cross-Method Validation:
- Correlate subjective symptom reports with objective hormone measures [6]
- Validate simplified assessment methods against gold-standard approaches
- Test concordance between different ovulation detection methods in irregular cycles
Statistical Modeling Considerations:
- Use multilevel modeling to account for nested data (observations within cycles within persons) [2]
- Model cycle phases as random effects to account for variability in phase timing between individuals
- Consider circular statistics or functional data analysis approaches that respect the cyclic nature of menstrual data
- Account for non-independent errors in repeated measures designs
Addressing Missing Data in Irregular Cycles
Missing data is particularly problematic in irregular cycles where phase timing is unpredictable:
Prevention Strategies:
- Implement flexible scheduling systems that accommodate cycle unpredictability
- Use remote data collection methods for symptoms and self-report measures
- Provide multiple reminder systems for scheduled assessments
Analytical Approaches:
- Use maximum likelihood estimation or multiple imputation that accommodates time-series data
- Conduct sensitivity analyses to test robustness of findings to missing data assumptions
- Document patterns of missingness by cycle phase and participant characteristics
The methodological challenges in studying menstrual cycle endpoints in athletic and PCOS populations are substantial but not insurmountable. By implementing the rigorous validation frameworks, troubleshooting protocols, and methodological adaptations outlined in this technical guide, researchers can generate more reliable, valid, and clinically meaningful evidence.
Future research directions should prioritize:
- Development and validation of population-specific assessment tools
- Refined statistical approaches that accommodate cycle irregularity
- Integration of digital health technologies for remote monitoring
- Larger-scale studies that can adequately capture inter-individual variability
- Standardized reporting guidelines to enhance cross-study comparability
Through continued methodological innovation and rigorous validation practices, the field can overcome current limitations and provide robust evidence to support the health and performance of individuals with varied menstrual cycle characteristics.
Conclusion
The synthesis of evidence underscores a critical juncture in menstrual cycle research: the field must decisively shift from convenient estimation to rigorous, direct measurement. Key takeaways emphasize that assumptions of cycle phases lack scientific validity, while a suite of validated tools—from hormonal assays to wearables—is now available for precise endpoint quantification. Future progress hinges on the widespread adoption of standardized terminology, transparent reporting of methodological limitations, and the development of accessible, high-quality instruments. For biomedical and clinical research, this methodological evolution is not merely an academic exercise but a fundamental prerequisite for generating valid, reliable data that truly advances female health, ensures drug safety, and builds participant trust. The future of the field depends on its commitment to this new standard of rigor.
References
- 1. Why We Must Stop Assuming and Estimating Menstrual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12152053/]
- 2. How to study the menstrual cycle - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC8363181/]
- 3. How to study the menstrual cycle: Practical tools and ... [https://www.sciencedirect.com/science/article/abs/pii/S0306453020303188]
- 4. Establishing a Gold Standard for Quantitative Menstrual ... [https://www.mdpi.com/1648-9144/59/9/1513]
- 5. A Guide to Tracking Your Menstrual Cycle [https://bwhealth.com.au/blog/a-guide-to-tracking-your-menstrual-cycle/]
- 6. Measurement of changes to the menstrual cycle [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0306491]
- 7. The Consequences and Embarrassment of Bad Data Quality [https://www.cloudresearch.com/resources/blog/the-consequences-of-bad-data-quality/]
- 8. Challenges and future directions in menstrual cycle research [https://pmc.ncbi.nlm.nih.gov/articles/PMC7192772/]
- 9. The mere-measurement effect of patient-reported outcomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12064450/]
- 10. A Very Short List of Common Pitfalls in Research Design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9477699/]
- 11. Menstrual Cycle Tracking in Sports Research [https://www.mdpi.com/2673-9488/3/4/44]
- 12. Why We Must Stop Assuming and Estimating Menstrual ... [https://link.springer.com/article/10.1007/s40279-025-02189-3]
- 13. The menstrual cycle as a vital sign: a comprehensive review [https://www.sciencedirect.com/science/article/abs/pii/S2666571924000380]
- 14. Using Hormone Data and Age to Pinpoint Cycle Day within ... [https://www.mdpi.com/1648-9144/59/7/1348]
- 15. Machine learning-based menstrual phase identification ... [https://www.nature.com/articles/s44294-025-00078-8]
- 16. Machine learning model for menstrual cycle phase ... [https://www.sciencedirect.com/science/article/pii/S0010482525000551]
- 17. Survey Analysis of Quantitative and Qualitative Menstrual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10534579/]
- 18. Using PdG Tests to Identify Fertility and Ovulation [https://premom.com/how-progesterone-pdg-tests-can-help-you-get-pregnant/]
- 19. Predicting serum hormone concentration by estimation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9838318/]
- 20. Common Research Instrumentation Problems and ... [https://merkel.co.il/research-instrumentation-troubleshooting/]
- 21. Determining Menstrual Phase: An Empirical Examination of... Cycle [https://pmc.ncbi.nlm.nih.gov/articles/PMC10714354/]
- 22. A Comparison of Two Hormonal Fertility Monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9960263/]
- 23. Validation of urinary reproductive hormone measurements ... [https://www.nature.com/articles/s41598-023-36539-w]
- 24. Here's how you can troubleshoot effectively in a research lab. [https://www.linkedin.com/advice/1/heres-how-you-can-troubleshoot-effectively-research-lab-uehaf]
- 25. A Novel method for quantifying fluctuations in wearable derived daily cardiovascular parameters across the menstrual cycle | npj Digital Medicine [https://www.nature.com/articles/s41746-024-01394-0]
- 26. Wearable health devices: Examples & 2025 technology ... [https://www.sermo.com/resources/wearable-devices-for-healthcare/]
- 27. Consensus recommendations for measuring the impact of ... [https://www.sciencedirect.com/science/article/pii/S0010782425000204]
- 28. Consensus recommendations for measuring the impact of ... [https://pubmed.ncbi.nlm.nih.gov/39864646/]
- 29. Measuring patient-reported outcomes - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3170214/]
- 30. Consensus Recommendations for Standardized Data ... [https://pubmed.ncbi.nlm.nih.gov/37272394/]
- 31. Standards [https://www.cdisc.org/standards]
- 32. When do we need clinical endpoint adjudication in clinical trials? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6454409/]
- 33. Why We Must Stop Assuming and Estimating Menstrual ... [https://pubmed.ncbi.nlm.nih.gov/40085421/]
- 34. HOW ARE HORMONES MEASURED? A JOURNEY IN ... [https://www.endocrinology.org/endocrinologist/140-summer-2021/features/how-are-hormones-measured-a-journey-in-endocrinology/]
- 35. Clinical Utility and Analytical Aspects of Direct ... [https://pubmed.ncbi.nlm.nih.gov/35296890/]
- 36. Thinking About Hormone Testing? 7 Things to Know [https://livehealthy.muhealth.org/stories/thinking-about-getting-your-hormone-levels-tested-7-things-know]
- 37. Evaluating selection bias in a population-based cohort ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6604357/]
- 38. Selection bias [https://catalogofbias.org/biases/selection-bias/]
- 39. Menstrual Cycle and Athletic Status Interact to Influence ... [https://sportsmedicine-open.springeropen.com/articles/10.1186/s40798-025-00924-8]
- 40. Impact of the menstrual cycle and barriers to football and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11965649/]
- 41. “What are my options here? I don't want to stop training or ... [https://www.sciencedirect.com/science/article/pii/S1440244025001963]
- 42. Menstrual Cycles: Normal Variability and Clinical Terms [https://ditki.com/course/physiology/glossary/physiological-process/menstrual-cycles-normal-variability-and-clinical-terms]
- 43. Menstrual Cycle (Normal Menstruation): Overview & Phases [https://my.clevelandclinic.org/health/articles/10132-menstrual-cycle]
- 44. Menstrual cycle: What's normal, what's not [https://www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/menstrual-cycle/art-20047186]
- 45. Quantifying the variability in the assessment of ... [https://pubmed.ncbi.nlm.nih.gov/37977226/]
- 46. Quantifying the variability in the assessment of ... [https://www.sciencedirect.com/science/article/pii/S0015028223019994]
- 47. Menstrual cycle length variation by demographic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10226714/]
- 48. how menstrual cycles vary by age, weight, race, and ethnicity [https://hsph.harvard.edu/research/apple-womens-health-study/study-updates/menstrual-cycles-today-how-menstrual-cycles-vary-by-age-weight-race-and-ethnicity/]
- 49. Between-Subjects vs. Within-Subjects Study Design [https://www.nngroup.com/articles/between-within-subjects/]
- 50. Within-Subjects vs Between-Subjects Design - Innerview [https://innerview.co/blog/within-subjects-vs-between-subjects-design-choosing-the-right-experimental-approach]
- 51. Menstrual Cycle and Athletic Status Interact to Influence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511478/]
- 52. Physiology, Menstrual Cycle - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK500020/]
- 53. Understanding the Phases of the Menstrual Cycle [https://helloclue.com/articles/cycle-a-z/the-menstrual-cycle-more-than-just-the-period]
- 54. Establishing a Gold Standard for Quantitative Menstrual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10533176/]
- 55. Quantitative Hormone Monitoring of the Menstrual Cycle [https://www.mdpi.com/journal/medicina/special_issues/quantitative_hormone_monitoring]
- 56. Personalized reproductive hormone monitoring in sweat [https://myadlm.org/science-and-research/clinical-chemistry/clinical-chemistry-podcasts/2024/personalized-reproductive-hormone-monitoring-in-sweat]
- 57. A Complete Guide to Testing with Mira Fertility [https://shop.miracare.com/blogs/resources/how-to-test-with-mira-fertility-plus?srsltid=AfmBOopaCWdqrlrsTeC-QbaHXJdL6hj44G6iYPBCEnQXayhpCLE_j6XS]
- 58. Using Quantitative Hormonal Fertility Monitors to Evaluate the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9866173/]
- 59. Complete Cycle Mapping Using a Quantitative At-Home ... [https://www.mdpi.com/1648-9144/58/12/1853]
- 60. Validating At-Home Urinary Hormone Measurements in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12040536/]
- 61. A Complete Guide to Testing with the Inito Fertility Monitor [https://blog.inito.com/a-complete-guide-to-testing-with-the-inito-fertility-monitor/]
- 62. How to Test Estrogen Levels at Home [https://www.oova.life/blog/how-test-estrogen-levels-home?srsltid=AfmBOooQfJn_QA7Ubt0n-S18IKanEfX1IB3c_Uq1Gfrs5MbR5-I5MsOk]
- 63. Historical Perspectives and Evolution of Menstrual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9580747/]
- 64. The Normal Menstrual Cycle and the Control of Ovulation - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK279054/]
- 65. Menstrual cycle rhythmicity: metabolic patterns in healthy ... [https://www.nature.com/articles/s41598-018-32647-0]
- 66. An evaluation of menstrual health apps' functionality ... [https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-025-03812-1]
- 67. A survey of women's experiences of using period tracker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9047811/]
- 68. Mapping ethical concerns in algorithm-driven period and ... [https://www.sciencedirect.com/science/article/pii/S0010782425000289]
- 69. Survey Analysis of Quantitative and Qualitative Menstrual ... [https://www.mdpi.com/1648-9144/59/9/1509?utm_source=chatgpt.com]
- 70. Polycystic Ovarian Syndrome - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK459251/]
- 71. The Impact of Menstrual Cycle Phase on Athletes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7916245/]
- 72. Challenges in AI-Based Ovulation Testing For PCOS And ... [https://www.emjreviews.com/innovations/news/challenges-in-ai-based-ovulation-testing-for-pcos-and-irregular-cycles/]