Assessing Public Awareness of Bisphenols, Phthalates, and Parabens: A Scientific Review for Research and Drug Development
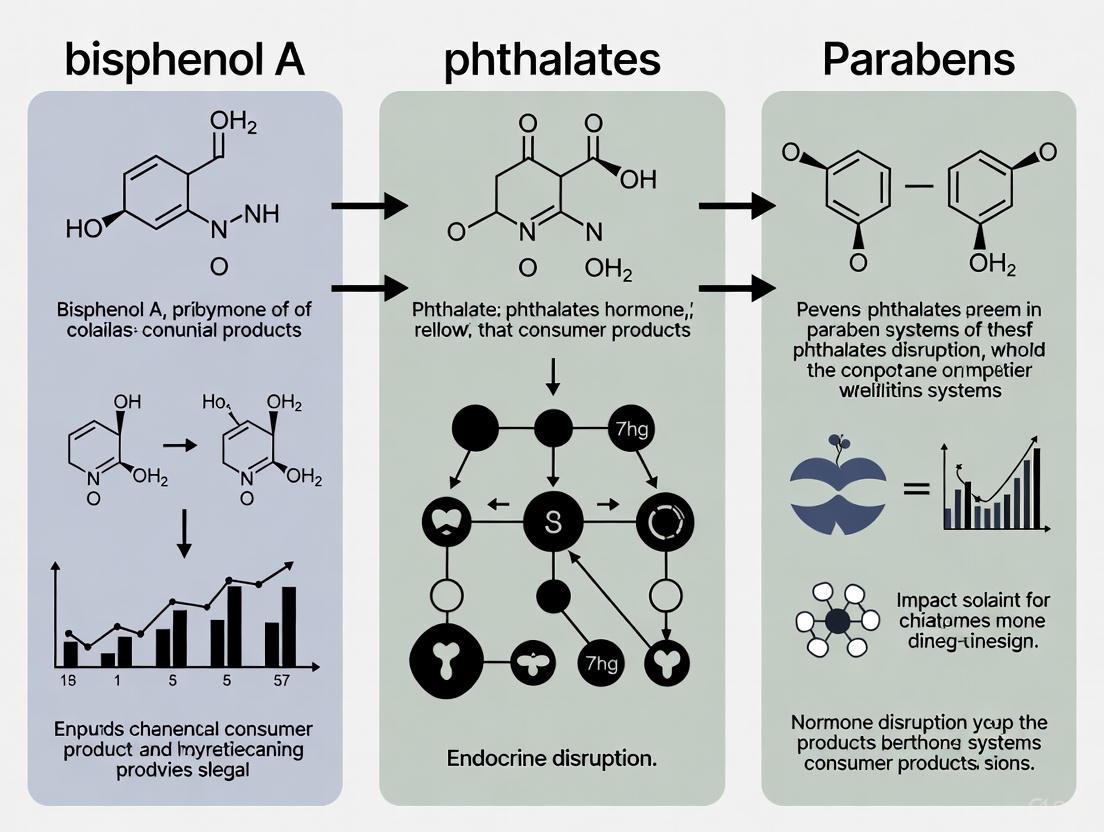
This article synthesizes current scientific evidence on public awareness and exposure to prevalent endocrine-disrupting chemicals (EDCs)—bisphenols, phthalates, and parabens.
Assessing Public Awareness of Bisphenols, Phthalates, and Parabens: A Scientific Review for Research and Drug Development
Abstract
This article synthesizes current scientific evidence on public awareness and exposure to prevalent endocrine-disrupting chemicals (EDCs)—bisphenols, phthalates, and parabens. Tailored for researchers, scientists, and drug development professionals, it explores the foundational science behind these compounds, methodologies for assessing public awareness and exposure, strategies for improving risk communication, and comparative analyses of regulatory and health outcome data. The review highlights significant awareness gaps despite widespread exposure, underscores the role of human biomonitoring (HBM) in exposure assessment, and discusses the implications of emerging substitutes and mixture toxicity for future biomedical research and public health policy.
The Unseen Exposure: Foundational Science and Population Awareness of Common EDCs
Bisphenols, phthalates, and parabens represent three classes of synthetic chemicals that have become ubiquitous in modern industrial and consumer applications. Their widespread use as plasticizers, preservatives, and additives has led to pervasive environmental contamination and human exposure, raising significant concerns within the scientific and public health communities. Framed within a broader thesis on public awareness, this technical guide provides a comprehensive examination of these compounds, detailing their primary sources, environmental prevalence, analytical methodologies for their detection, and the molecular mechanisms underpinning their health impacts. Understanding the ubiquity and characteristics of these chemicals is a fundamental prerequisite for informed risk assessment and the development of effective mitigation strategies.
The following table delineates the core characteristics and common applications of bisphenols, phthalates, and parabens.
Table 1: Defining Bisphenols, Phthalates, and Parabens
| Chemical Class | Chemical Structure & Properties | Primary Functions & Uses | Common Example Compounds |
|---|---|---|---|
| Bisphenols | Two hydroxyphenyl groups; key component in polycarbonate plastics and epoxy resins [1]. | Production of polycarbonate plastics, epoxy resin linings for food/drink cans, thermal paper, medical devices, and dental sealants [2] [1]. | Bisphenol A (BPA), Bisphenol S (BPS), Bisphenol F (BPF), Bisphenol AF (BPAF), Bisphenol B (BPB), Bisphenol E (BPE) [1]. |
| Phthalates | Diesters of phthalic acid; not chemically bound to plastics, enabling leaching [3]. | Plasticizers to enhance flexibility, durability, and transparency of plastics (esp. PVC); also used as solvents and fragrance carriers [4] [5] [3]. | Di(2-ethylhexyl) phthalate (DEHP), Di-n-butyl phthalate (DBP), Diethyl phthalate (DEP), Di-isobutyl phthalate (DIBP), Benzyl butyl phthalate (BBP) [4] [3]. |
| Parabens | Esters of para-hydroxybenzoic acid; broad-spectrum antimicrobial activity [6] [7]. | Preservatives in cosmetics, pharmaceuticals, food products, and personal care products to extend shelf-life [6] [7]. | Methylparaben (MeP), Ethylparaben (EtP), Propylparaben (PrP), Butylparaben (BuP) [6] [7] [8]. |
Environmental Ubiquity and Concentrations
The extensive use of these chemicals has resulted in their detection across diverse environmental matrices. The following tables summarize reported concentrations in aquatic environments, sediments, and human exposure markers.
Table 2: Environmental Concentrations of Bisphenols and Phthalates
| Matrix | Location | Chemical | Concentration Range | Citation |
|---|---|---|---|---|
| Surface Water | European freshwaters | Bisphenol A (BPA) | <0.03 ng/L - 588,000 ng/L (Median: 36 ng/L) | [9] |
| European saline waters | Bisphenol A (BPA) | <0.03 ng/L - 4,800 ng/L (Median: 22.2 ng/L) | [9] | |
| Turag River, Bangladesh (Rainy) | Bisphenol F (BPF) | 1.3950 - 7.2352 μg/L | [1] | |
| Turag River, Bangladesh (Winter) | Bisphenol F (BPF) | 1.1186 - 7.3094 μg/L | [1] | |
| Coastal Bushehr, Iran (Wastewater) | Di(2-ethylhexyl) phthalate (DEHP) | 19.67 - 39.75 μg/L | [4] | |
| Sediment | European freshwater | Bisphenol A (BPA) | <0.01 - 8,067 ng/g dry weight (Median: 78.5 ng/g) | [9] |
| Turag River, Bangladesh | Bisphenol F (BPF) | 27.2740 - 234.4540 μg/g dry weight | [1] | |
| Human Exposure | Urine Samples (General Population) | Bisphenol A (BPA) | [2] | |
| Urine Samples (General Population) | Bisphenol S (BPS) | [2] |
Table 3: Environmental Concentrations and Exposure of Parabens
| Matrix | Location | Chemical | Concentration / Level | Citation |
|---|---|---|---|---|
| Wastewater Influent | Various (Literature Review) | Total Parabens | 5460 - 10,000 ng/L (up to 79.6 μg/L) | [6] [7] |
| Groundwater | Rural Nigeria | Butylparaben (BuP) | Up to 400 μg/L | [8] |
| Human Exposure | Personal Care Product Users | Paraben Metabolites | Urinary levels 28-80% higher than non-users | [7] |
Detailed Analytical Methodologies
Accurate assessment of these contaminants requires robust and sensitive analytical protocols. The following section details specific experimental workflows cited in recent literature.
Analysis of Phthalate Esters (PAEs) and BPA in Wastewater
A study investigating contaminants in coastal wastewater employed the following protocol [4]:
- Sample Collection: Raw urban wastewater samples were collected in 100 mL pre-cleaned amber glass bottles and filtered through 0.45 μm nylon membrane filters to remove suspended particles.
- Extraction - Liquid-Liquid Extraction (LLE): For PAEs, 100 mL of filtered seawater was combined with 20 mL of dichloromethane and 20 μL of benzyl benzoate (internal standard) in a separatory funnel. The mixture was shaken vigorously to transfer PAEs into the organic phase.
- Extraction - Solid Phase Extraction (SPE): For BPA, 100 mL of acidified seawater (pH 2–3) was spiked with BPA-d16 (internal standard) and passed through pre-conditioned C18 cartridges.
- Instrumental Analysis - Gas Chromatography-Mass Spectrometry (GC-MS): Analysis was performed using an Agilent 7890 GC/5975 MSD system with a J&W-5MS column. The oven temperature was programmed from 70°C (1 min hold) to 300°C at 10°C/min, with a 7 min final hold. Helium was used as the carrier gas at 1 mL/min.
Analysis of Bisphenol Analogues in River Water and Sediment
Research on an urban river system used this methodology for bisphenols [1]:
- Water Sample Extraction: A 500 mL water sample was salted with 150 g NaCl, acidified with HCl, and extracted with 20 mL of dichloromethane via mechanical shaking. The organic extract was dried with anhydrous sodium sulfate, filtered, and derivatized with BSTFA + 1% TMCS at 45°C for 30 minutes before GC-MS analysis.
- Sediment Sample Extraction: 10 g of homogenized sediment was extracted with 20 mL of DCM on an orbital shaker at 250 rpm for 60 minutes.
- Instrumental Analysis: The extracts were analyzed using GC-MS, with quantification performed against calibration curves of known bisphenol analogue standards.
Diagram 1: Experimental workflow for analyzing environmental contaminants.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 4: Essential Reagents and Materials for Environmental Analysis
| Item | Function / Application | Specific Examples |
|---|---|---|
| Amber Glass Bottles | Sample collection and storage; prevents photodegradation of target analytes. | Pre-cleaned with acetone, hexane, and methanol [4]. |
| Solid Phase Extraction (SPE) Cartridges | Extract and concentrate analytes from liquid samples. | C18 cartridges for BPA extraction [4]. |
| Derivatization Reagents | Chemically modify target analytes to improve volatility and detection for GC-MS. | BSTFA with 1% TMCS [1]. |
| Internal Standards | Correct for variability in extraction and analysis; enable accurate quantification. | Benzyl benzoate for PAEs; BPA-d16 for BPA [4] [1]. |
| Chromatography Columns | Separate complex mixtures of compounds within the instrument. | J&W-5MS ultra inert column (30 m × 0.25 mm I.D., 0.25 μm film) for GC-MS [4]. |
| Organic Solvents | Extraction and cleaning of samples. | Dichloromethane (DCM), acetone, hexane, methanol [4] [1]. |
Molecular Pathways and Health Significance
Epidemiological and toxicological studies have linked exposure to these chemicals with various adverse health outcomes, mediated through specific molecular pathways.
- Endocrine Disruption: Bisphenols and parabens can mimic natural estrogen by binding to estrogen receptors (ER), disrupting hormonal signaling [6] [7]. Phthalates are known to disrupt testosterone synthesis, which is a predictor of cardiovascular disease [5].
- Oxidative Stress and Inflammation: BPA exposure has been linked to childhood obesity by disrupting lipid metabolism, oxidative stress, and inflammatory pathways [10]. Phthalates like DEHP contribute to heart disease by promoting inflammation in the coronary arteries [5].
- Specific Organ Toxicity: Phthalates accumulate in the kidneys, potentially causing renal inflammation, fibrosis, and cancer through mechanisms involving oxidative stress and activation of the PPARγ pathway [3]. Parabens have been detected in breast tumor tissues and are investigated for their potential role in breast cancer, possibly by interacting with the HER2 pathway [7].
Diagram 2: Key molecular pathways and health outcomes of chemical exposure.
Bisphenols, phthalates, and parabens are definitively established as ubiquitous environmental contaminants due to their extensive industrial and commercial applications. While European data suggests declining trends for BPA in some regions, the continued high levels found in other parts of the world and the increasing use of substitute compounds underscore a persistent and evolving issue. The health implications, driven by mechanisms such as endocrine disruption, oxidative stress, and inflammation, are supported by a growing body of scientific evidence. Enhancing public and professional awareness of the sources and prevalence of these chemicals is a critical first step toward mitigating exposure and informing future regulatory and research priorities.
Endocrine-disrupting chemicals (EDCs), including bisphenols, phthalates, and parabens, have become ubiquitous in environment due to their widespread use in consumer products. Human exposure to these compounds is virtually unavoidable, occurring through ingestion, inhalation, and dermal absorption [11]. These chemicals can interfere with the normal functioning of the endocrine system by mimicking, blocking, or altering the synthesis, transport, metabolism, or elimination of endogenous hormones such as estrogens, androgens, and thyroid hormones [12]. Understanding the routes of exposure and metabolic fate of these compounds is crucial for assessing health risks and developing public health strategies. This technical guide synthesizes current scientific knowledge on exposure pathways and bio-metabolism of these EDCs, providing researchers and public health professionals with essential information to advance both scientific understanding and public awareness.
Exposure Routes and Mechanisms
Dermal Absorption
Dermal exposure occurs when chemicals come into contact with skin and are absorbed into the bloodstream. The skin structure and chemical properties determine absorption efficiency.
- Mechanism: Dermal absorption is a two-step process involving contact between contaminant and skin, followed by absorption into the body. The amount absorbed represents what is available for interaction with target tissues or organs [13].
- Key Parameters: Dermal exposure depends on contaminant concentration in the contacted medium, timeframe of exposure, skin surface area exposed, and compound-specific permeability coefficients [13].
- Calculating Absorbed Dose: For inorganics in water, the internal absorbed dose can be calculated as: DAevent = Kp × C × t, where Kp is the permeability coefficient (cm/hr), C is the chemical concentration (mg/cm³), and t is contact time (hours/event) [13].
- Real-World Exposure: Feminine hygiene products have been identified as significant sources of EDC exposure in women, with panty liners containing the highest concentrations of dimethyl phthalate (median: 249 ng/g), diethyl phthalate (386 ng/g), dibutyl phthalate (393 ng/g), and di-iso-butyl phthalate (299 ng/g) [14]. Parabens are also frequently detected in bactericidal creams and solutions at parts per million levels [14].
Ingestion
Ingestion involves chemical absorption through the digestive tract, occurring both directly and indirectly.
- Direct Ingestion: Accidentally eating or drinking a chemical [15].
- Indirect Ingestion: Higher probability exposure occurs when food or drink is brought into contaminated environments or when people handle chemicals and then eat, drink, or smoke without proper hygiene [15].
- Primary Exposure Sources: Humans are mainly exposed to bisphenols through the diet, particularly from food packaging and canned food linings [16]. Some dairy products, fish, seafood, and oils have been found to contain high levels of phthalates [11].
- Vulnerable Populations: Infants are exposed to phthalates through breast milk from mothers exposed to DEHP and DiNP, and by sucking on toys containing DEHP, DBP, and BBP [11]. Phthalates can also cross the placenta-blood barrier, representing a major exposure route for the fetus [11].
Inhalation
Inhalation occurs when chemicals are absorbed through the respiratory tract (lungs), after which they can enter the bloodstream for distribution throughout the body.
- Forms Inhaled: Chemicals can be inhaled as vapors, fumes, mists, aerosols, and fine dust [15].
- Exposure Settings: Phthalates are semi-volatile organic compounds, with DEHP and DBP being the main compounds found in both indoor and outdoor air [11]. Residents living near phthalate manufacturing industries are particularly at risk through absorption of polluted air [11].
- Protection Measures: Laboratory workers can protect themselves through proper use of functioning fume hoods, dust masks, and respirators when fume hoods are not available [15].
Table 1: Comparative Analysis of Exposure Routes for Selected EDCs
| Chemical Class | Primary Exposure Routes | Common Sources | Vulnerable Populations |
|---|---|---|---|
| Phthalates | Ingestion, Dermal, Inhalation | Plastic products, Personal care products, Food packaging, Medical devices | Fetuses, Infants, Children, Reproductive age adults [11] |
| Bisphenols | Primarily Ingestion | Canned food linings, Polycarbonate plastics, Thermal receipts | Pregnant women, Developing fetuses [16] |
| Parabens | Dermal, Ingestion | Cosmetics, Personal care products, Food packaging, Pharmaceuticals | Women (higher use of PCPs), Elderly [17] [16] |
Table 2: Concentration Ranges of EDCs in Various Exposure Media
| Exposure Medium | Phthalates | Parabens | Bisphenols |
|---|---|---|---|
| Feminine Hygiene Products | DMP: 249 ng/g (median in panty liners); DEHP: 267 ng/g (median in tampons) [14] | MeP: 2840 ng/g; EtP: 734 ng/g; PrP: 278 ng/g (median in bactericidal creams) [14] | Not quantified in available studies |
| Human Serum | Not specified | MeP: 3.4 ng/mL (median in elderly) [17] | Not specified |
| Indoor Air | DEHP, DBP as main compounds [11] | Not specified | Not specified |
Metabolic Pathways and Fate
Phthalate Metabolism
Phthalates undergo rapid bio-metabolism in the human body, with short biological half-lives of approximately 12 hours [11]. The metabolic process occurs in two primary phases:
- Phase I Metabolism: The first step involves hydrolyzation after absorption into cells, where parent phthalate diesters are converted to their corresponding monoester metabolites [11].
- Phase II Metabolism: The second step is conjugation to form hydrophilic glucuronide conjugates, catalyzed by the enzyme uridine 5′-diphosphoglucuronyl transferase [11].
- Metabolic Patterns: Metabolic pathways differ by phthalate type. Short-branched phthalates are typically hydrolyzed to monoester phthalates and excreted in urine, while long-branched phthalates undergo more complex transformations including hydroxylation and oxidation before excretion in urine and feces as phase 2 conjugated compounds [11].
- DEHP Metabolism: As an example of complex metabolism, DEHP is hydrolyzed to mono(2-ethylhexyl) phthalate (MEHP), which can then be further metabolized to mono(2-ethyl-5-hydroxyhexyl) phthalate, mono(2-ethyl-5-oxohexyl) phthalate, mono(2-ethyl-5-carboxypentyl) phthalate (MECPP), mono(2-carboxymethylhexyl) phthalate (MCMHP), and other metabolites [11].
- Excretion: Most phthalates and their metabolites are excreted in urine and feces, though some compounds (e.g., DEHP) and metabolites can also be excreted in sweat [11].
- Age-Related Differences: Research indicates that oxidative metabolism of DEHP is age-related, with younger children (6-7 years) excreting more oxidative DEHP metabolites compared to adults [11].
Bisphenol and Paraben Metabolism
Bisphenols and parabens are also rapidly metabolized, contributing to continuous exposure needs to maintain body burdens.
- Rapid Metabolism: Like phthalates, bisphenols and parabens are quickly metabolized in the body and do not bioaccumulate, with most metabolites excreted within 24 hours [18].
- Measurement Challenges: Due to this rapid metabolism, studies relying on single spot urine analyses may not accurately reflect exposure, as concentrations vary throughout a day and over longer periods [18].
- Enzymatic Transformation: Parabens (alkyl esters of p-hydroxybenzoic acid) undergo metabolic hydrolysis and conjugation similar to phthalates [16].
- Interindividual Variability: Metabolic efficiency varies between individuals, potentially explaining differential susceptibility to EDC effects.
Figure 1: Integrated Exposure and Metabolic Pathway of EDCs
Experimental Methods for Exposure Assessment
Biomarker Measurement in Biological Samples
Accurate assessment of EDC exposure relies on sophisticated analytical methods to measure chemicals or their metabolites in biological samples.
- Sample Collection: Studies typically collect urine samples as the primary matrix for assessing exposure to non-persistent EDCs. The Environment and Reproductive Health (EARTH) Study protocol asked participants to collect all voids over a 24-hour period, with samples kept cool and frozen at −80°C within 36 hours of collection [19] [18].
- Analytical Techniques: Advanced chromatographic methods are employed:
- BPA Analysis: Total BPA (free plus conjugated) measured after enzymatic hydrolysis of urine samples, with derivation using pentafluorobenzyl bromide, extraction with hexane/dichloromethane mixture, and analysis by gas chromatography coupled with mass spectrometry operating in negative chemical ionization mode [18].
- Phthalate Metabolite Analysis: Urine samples enzymatically hydrolyzed, with resulting phthalate monoesters extracted by anion exchange solid phase or liquid-liquid technique using hexane/ethyl acetate mixture, followed by analysis using tandem mass spectrometry with electrospray ion source in negative mode [18].
- Paraben Analysis: Measured using online solid-phase extraction coupled with isotope dilution–high-performance liquid chromatography–tandem mass spectrometry [19].
- Quality Control: Implementation of strict quality controls including blank samples, low/medium/high concentration quality control samples, and careful treatment of labware to eliminate contamination [18].
- Specific Gravity Adjustment: Urine dilution is accounted for using specific gravity measurements with digital refractometers, with adjusted concentrations calculated using the formula: Pc = Pi × [(SGm - 1)/(SGi - 1)], where Pc is the adjusted concentration, Pi is the observed concentration, SGi is the sample specific gravity, and SGm is the median specific gravity for the cohort [18].
Dermal Exposure Assessment Protocol
The U.S. Environmental Protection Agency has established standardized approaches for assessing dermal exposure [13].
- Exposure Calculation: The average daily dermal dose (ADD) is calculated as: ADDabs = DAevent × SA × EF × ED / (BW × AT), where:
- DAevent = Absorbed dose per event (mg/cm²-event)
- SA = Skin surface area available for contact (cm²)
- EF = Exposure frequency (events/year)
- ED = Exposure duration (years)
- BW = Body weight (kg)
- AT = Averaging time (days)
- Dose Characterization: Differentiation between:
- Potential dose: Amount applied to skin
- Applied dose: Amount at absorption barrier
- Internal dose: Amount absorbed into bloodstream
- Biologically effective dose: Amount interacting with target tissues
- Permeability Coefficients: Use of empirically derived Kp values specific to chemical and vehicle matrix.
Table 3: Key Parameters for Dermal Exposure Assessment
| Parameter | Symbol | Units | Description | Source Example |
|---|---|---|---|---|
| Permeability Coefficient | Kp | cm/hour | Chemical-specific skin permeability constant | Chemical-specific literature |
| Skin Surface Area | SA | cm² | Body region-specific surface area values | EPA Exposure Factors Handbook |
| Exposure Frequency | EF | events/year | How often exposure occurs | Product use surveys |
| Exposure Duration | ED | years | Length of exposure period | Study population characteristics |
| Body Weight | BW | kg | Body weight of exposed individual | Cohort measurements |
Figure 2: Experimental Workflow for EDC Exposure Assessment
Research Reagent Solutions and Essential Materials
Table 4: Essential Research Materials for EDC Analysis
| Reagent/Material | Function | Application Example |
|---|---|---|
| Isotope-labeled Standards | Internal standards for quantification | Deuterated phthalate metabolites for mass spectrometry [18] |
| Enzymes for Hydrolysis | Deconjugation of metabolites | β-glucuronidase for hydrolyzing phase II metabolites [18] |
| Solid Phase Extraction Cartridges | Sample clean-up and concentration | Anion exchange SPE for phthalate metabolite extraction [18] |
| UPLC-MS/MS Systems | High-sensitivity analyte detection | Quantification of phenol and phthalate biomarkers [19] |
| Digital Refractometer | Specific gravity measurement | Urine dilution adjustment for exposure quantification [18] |
| Certified Reference Materials | Quality assurance and method validation | Quality control samples at low, medium, high concentrations [18] |
Implications for Public Awareness and Regulatory Science
The scientific evidence summarized in this review has significant implications for public awareness and regulatory policy. Understanding exposure routes and metabolic handling of EDCs provides the foundation for:
- Targeted Exposure Reduction: Identifying primary exposure routes enables development of specific intervention strategies, such as reducing use of certain personal care products or modifying food packaging materials.
- Biomonitoring Programs: Data on metabolic patterns informs selection of appropriate biomarkers for population surveillance studies.
- Risk Assessment Refinement: Quantitative exposure data and metabolic fate information support more accurate risk assessment and establishment of evidence-based safety guidelines.
- Public Health Communication: Clear understanding of exposure pathways enables more effective communication of practical risk reduction strategies to the public.
Future research should address critical knowledge gaps regarding cumulative effects of mixture exposures, sensitive windows of vulnerability, and interindividual differences in metabolism that may affect susceptibility to EDC-mediated health effects.
Biomonitoring Evidence of Widespread Exposure in General and Vulnerable Populations
Biomonitoring studies reveal widespread human exposure to endocrine-disrupting chemicals (EDCs)—particularly bisphenols, phthalates, and parabens—across general and vulnerable populations. Recent national research demonstrates that 96 different chemicals were detected in US preschoolers, with 34 compounds found in over 90% of children [20]. These exposures are linked to potentially serious health implications, including disrupted reproductive function, altered hormonal balance, and adverse developmental outcomes [12] [21] [22]. Vulnerable populations such as children, pregnant women, and adolescents face disproportionate exposure and susceptibility due to their unique physiological characteristics and exposure patterns [20] [23] [24]. This technical review synthesizes current biomonitoring evidence, detailed methodological approaches, and emerging health associations to inform researchers, scientists, and drug development professionals working in toxicology and public health.
Population-Specific Biomonitoring Data
General Population Exposure Profiles
Table 1: Biomonitoring Evidence of Widespread Exposure in General and Vulnerable Populations
| Population Group | Sample Size & Source | Key Chemicals Detected | Detection Frequency & Concentrations | Primary Exposure Routes |
|---|---|---|---|---|
| US Preschoolers (2-4 years) | 201 children from ECHO Cohort [20] | 111 chemicals including phthalates, bisphenols, parabens, pesticides, OPEs, PAHs | 96 chemicals in ≥5 children; 48 in >50%; 34 in >90%; 9 not in NHANES [20] | Hand-to-mouth contact, indoor dust, food packaging, personal care products [20] |
| Adults (NHANES) | 4,455 US women (2005-2014) [25] | BPA, triclosan, benzophenone-3, methyl/ethyl/propyl/butyl paraben | BPA detected in >70% population; Triclosan Q2: OR=2.33 (1.45-3.75) for breast cancer [25] | Personal care products, food containers, pharmaceuticals [25] |
| Women Undergoing ART | 144 follicular fluid samples [21] | Phthalate metabolites (mPAEs), bisphenols, parabens, OH-PAHs | mPAEs highest (6.14 ng/mL), parabens (2.17 ng/mL), bisphenols (1.33 ng/mL), OH-PAHs lowest [21] | Dietary ingestion, dermal absorption, respiratory inhalation [21] |
| Pregnant Taiwanese Women | TMICS Cohort (2012-2016) [24] | Methylparaben, ethylparaben, propylparaben, BPA | Positive association makeup use & paraben levels; Higher BPA in lowest income group [24] | Leave-on PCPs (makeup, lotion), rinse-off products, food packaging [24] |
| Korean Adolescent Girls | 112 participants (13-17 years) [23] [26] | Methyl/ethyl/propyl parabens, BPA, benzophenones | Frequent PCP use → higher paraben levels; BPA reduced 32.7% post-intervention [23] | Skincare, sunscreen, cosmetics, lip products [23] |
Temporal Trends and Demographic Disparities
Longitudinal data from 2010-2021 reveals concerning exposure trends. While levels of triclosan, parabens, polycyclic aromatic hydrocarbons (PAHs), and most phthalates have decreased, alternative plasticizers and emerging pesticides show significant upward trends [20]. Di-iso-nonyl-cyclohexane-1,2-dicarboxylic acid (DINCH), neonicotinoid acetamiprid, pyrethroid pesticides, and the herbicide 2,4-D have all demonstrated increasing detection frequencies [20].
Substantial demographic disparities exist in EDC exposure. Research indicates that firstborn children have significantly lower chemical levels than their younger siblings, and chemical concentrations are typically higher in 2-year-olds compared to 3- or 4-year-olds [20]. Importantly, children from racial and ethnic minority groups demonstrate higher levels of parabens, several phthalates, and PAHs, highlighting environmental justice concerns [20].
Socioeconomic status significantly modifies exposure patterns. Research with pregnant Taiwanese women found that lower income groups had higher BPA concentrations, particularly with frequent product use [24]. Conversely, the strongest associations between personal care product use and paraben concentrations were observed in the highest education group (postgraduate), suggesting product use patterns may vary by socioeconomic factors [24].
Detailed Experimental Protocols and Methodologies
Biomonitoring Workflow and Analytical Techniques
The following diagram illustrates the comprehensive workflow for biomonitoring studies of endocrine-disrupting chemicals:
Biomonitoring Workflow for EDC Assessment
Specific Analytical Methodologies
Sample Preparation and Extraction
For follicular fluid analysis, researchers employed rigorous sample preparation protocols. Internal standards were added to 200μL follicular fluid samples, followed by enzymatic hydrolysis using β-glucuronidase at 37°C for 180 minutes to deconjugate phase II metabolites [21]. The mixture was subsequently loaded onto MAX solid-phase extraction (SPE) cartridges, with target compounds eluted using 1 mL of 2% formic acid in methanol [21]. This protocol achieved recovery rates of 77%-109% for phthalate metabolites (mPAEs), 74%-97% for parabens, 63%-108% for bisphenols, and 64%-105% for hydroxylated PAHs (OH-PAHs) [21].
Instrumental Analysis
Separation and quantification employed ultra-performance liquid chromatography coupled with tandem mass spectrometry (UPLC-MS/MS). Specific analytical conditions varied by compound class:
- Parabens and phthalate metabolites were analyzed using a gradient of Milli-Q water and acetonitrile
- Bisphenols and OH-PAHs were analyzed using a gradient of 2 mM ammonium acetate and methanol [21]
Chromatographic separation utilized a Poroshell 120 EC-C18 column (100 mm × 4.6 mm, 2.7 μm particle diameter) [21]. This methodology enabled precise quantification of compounds at concentrations as low as 0.1-2.3 ng/mL, depending on the specific analyte [25].
Quality Assurance and Quality Control
Each sample batch included procedural blanks, reagent blanks, and matrix-spiked samples for recovery assessment and background contamination evaluation [21]. For measurements below the limit of detection (LOD), values were assigned using established protocols: concentrations below LOD were treated as half the LOD value, while values between LOD and LOQ were calculated as one-fourth of the LOQ when detection frequencies were below 50%, or as one-half of the LOQ when detection frequencies exceeded 50% [21] [24].
Molecular Mechanisms and Health Implications
Endocrine Disruption Pathways
The following diagram illustrates the molecular mechanisms through which bisphenols, phthalates, and parabens disrupt endocrine function:
Molecular Mechanisms of EDC Action
Key Health Endpoints and Epidemiological Evidence
Reproductive Health Outcomes
Substantial evidence links EDC exposure to impaired reproductive function in both males and females. Systematic reviews of epidemiological studies demonstrate consistent associations between EDC exposure and multiple adverse reproductive endpoints, including impaired semen quality, decreased ovarian reserve, infertility, polycystic ovary syndrome (PCOS), and altered hormone levels [12]. Research involving women undergoing assisted reproductive technologies (ART) reveals that EDCs measured in follicular fluid—the microenvironment surrounding developing oocytes—directly associate with alterations in critical reproductive hormones including estradiol (E2) and progesterone [21].
The specific mechanisms underlying these reproductive effects include:
- Disruption of Steroidogenesis: BPA exposure downregulates genes involved in ovarian steroidogenesis, disrupting hormone production and ovarian function [22]
- Oxidative Stress and Inflammation: BPA-induced oxidative stress damages reproductive tissues, while inflammation disrupts normal physiological processes in ovaries and testes [22]
- Epigenetic Modifications: BPA exposure induces DNA methylation changes in genes critical for ovarian function and follicular development, potentially contributing to transgenerational effects [22]
Developmental and Long-Term Health Risks
Early-life exposure to EDCs presents particular concern due to the heightened vulnerability during critical developmental windows. Research demonstrates that children have higher levels of several chemicals than their mothers during pregnancy, including two phthalates, bisphenol S (BPS), and pesticide biomarkers 3-PBA and trans-DCCA [20]. These early exposures may have lifelong consequences, as developmental exposure to EDCs has been linked to increased susceptibility to disease later in life, including hormone-sensitive cancers [25] and metabolic disorders [12].
Research Reagents and Methodological Toolkit
Table 2: Essential Research Reagents and Analytical Tools for EDC Biomonitoring
| Reagent/Category | Specific Examples | Application in Research | Technical Specifications |
|---|---|---|---|
| Analytical Standards | Parabens (MeP, EtP, PrP, BuP, HeP, BzP); Bisphenols (BPA, BPS, BPF, BPB, BPAF, BPZ, BPP, BPAP); OH-PAHs (1-hydroxynathalene, 2-hydroxynathalene, etc.); Phthalate metabolites (mPAEs) | Quantification and identification in biological matrices; Quality control and calibration | Purity ≥95%; Isotope-labeled internal standards for accurate quantification [21] |
| Sample Preparation | β-glucuronidase enzyme; MAX solid-phase extraction cartridges; Formic acid; Methanol, acetonitrile; Ammonium acetate | Enzymatic deconjugation; Sample purification and concentration; Mobile phase components | SPE recovery: 63%-109% depending on analyte; Enzymatic hydrolysis at 37°C for 180 min [21] |
| Chromatography | Poroshell 120 EC-C18 column (100 mm × 4.6 mm, 2.7 μm); UPLC systems; C18 guard columns | Compound separation; Analytical separation with high resolution | Particle size: 2.7μm; Gradient elution with water/acetonitrile or ammonium acetate/methanol [21] |
| Mass Spectrometry | Triple quadrupole mass spectrometers; Electrospray ionization sources; Tandem mass spectrometry | Compound detection and quantification; High sensitivity detection | Multiple reaction monitoring (MRM) mode; LODs: 0.1-2.3 ng/mL depending on analyte [21] [25] |
| Quality Control | Certified reference materials; Pooled quality control samples; Matrix-spiked samples | Method validation; Accuracy and precision assessment | Background contamination monitoring; Batch-to-batch reproducibility [21] |
Emerging Research Frontiers and Methodological Innovations
Novel Exposure Assessment Approaches
Recent studies demonstrate innovative methodologies for capturing complex exposure scenarios. Research integrating 7-day time-activity diaries with individualized urinary biomonitoring identified previously overlooked exposure sources, including medical plasters, sheer tights, wallpapering, vinyl flooring installation, and food preparation with gloves [2]. This approach revealed that standard questionnaires alone miss capturing diverse bisphenol exposure pathways, highlighting the need for more comprehensive exposure assessment strategies.
Mixture Effects and Advanced Statistical Models
Growing recognition of the "cocktail effect" of chemical mixtures has driven the development of advanced statistical approaches. Studies increasingly employ Bayesian Kernel Machine Regression (BKMR), Weighted Quantile Sum (WQS) regression, and Quantile g-computation to assess the combined effects of multiple EDCs [21] [27] [25]. These methods help identify the most influential chemicals in mixtures and characterize potential synergistic or antagonistic interactions.
BKMR analysis generates posterior inclusion probabilities (PIPs) to quantify individual chemical contributions, with a PIP threshold of 0.50 considered statistically significant [21]. Complementary analysis using Quantile g-computation models determines chemical-specific weight contributions, providing robust assessment of mixture effects that more accurately reflects real-world exposure scenarios.
Intervention Studies and Exposure Reduction Strategies
Intervention research demonstrates the efficacy of exposure reduction approaches. A 2-day cosmetic restriction intervention among Korean adolescent girls resulted in substantial reductions in BPA (32.7%) and benzophenones (11.9%-22.8%) after excluding participants with no baseline personal care product use [23]. This highlights the importance of targeted behavioral interventions for reducing EDC exposure in vulnerable populations, while also revealing the challenges in achieving significant reductions across all participants.
Endocrine-disrupting chemicals (EDCs) are exogenous compounds that interfere with the normal functioning of the hormonal system by mimicking, blocking, or altering the synthesis, transport, metabolism, or elimination of natural hormones [28]. The endocrine system is exceptionally vulnerable to disruption during critical developmental windows, and even low doses of EDCs can precipitate significant developmental and biological effects due to the hormone-sensitive nature of physiological processes [28]. Bisphenols (including BPA, BPS, and BPF), phthalates, and parabens represent some of the most pervasive EDCs in our environment, found in countless consumer products from food packaging and cosmetics to pharmaceuticals and toys [29] [28]. This technical review synthesizes current evidence linking these chemical classes to endocrine disruption, inflammatory responses, and subsequent chronic disease risks, providing researchers and drug development professionals with a comprehensive analysis of mechanisms, outcomes, and methodological approaches.
Global Burden and Key Epidemiological Data
The global health burden attributable to EDC exposure has reached alarming proportions. A temporal and cross-country comparative analysis from 2000 to 2024 revealed a dramatic increase in metabolic diseases linked to bisphenol exposure alone, with cases rising from 68 million in 2000 to 127 million in 2024 [30]. This total includes 72 million cases of obesity, 24 million cases of type 2 diabetes mellitus (T2DM), and 31 million cases of metabolic syndrome (MetS), with corresponding global economic costs projected to exceed $1.1 trillion USD in 2024 [30]. The distribution of this burden is not uniform, with Asia bearing 45% of the global bisphenol-related disease burden, followed by North America and Europe [30].
Table 1: Global Burden of Bisphenol-Attributable Metabolic Disease (2024)
| Health Outcome | Attributable Cases (Millions) | Primary Contributors |
|---|---|---|
| Obesity | 72 | BPS, BPF, BPA |
| Type 2 Diabetes | 24 | BPA, BPS |
| Metabolic Syndrome | 31 | BPA, BPF |
| Total | 127 |
Regulatory actions targeting specific EDCs have demonstrated complex outcomes. BPA-specific bans in Europe successfully reduced BPA exposure by 33%, but this achievement was offset by a 47% increase in BPS levels and a 22% increase in BPF exposure due to analog substitution [30]. Consequently, BPS and BPF now account for 76% of the global bisphenol-related disease burden, highlighting the phenomenon of "regrettable substitution" and the limitations of chemical-specific rather than class-based regulation [30].
Bisphenols: Metabolic and Reproductive Toxicity
Mechanisms of Action and Health Outcomes
Bisphenol A (BPA) and its analogs (BPS, BPF) primarily exert their endocrine-disrupting effects through interaction with estrogen receptors, particularly ESR1 and ESR2 [31] [32]. These interactions can alter gene expression related to steroidogenesis and metabolic homeostasis. The hypothalamic-pituitary-gonadal (HPG) axis represents a key target for bisphenol disruption, with downstream effects on reproductive function and development [31].
Recent research has revealed that co-exposure to bisphenols and other environmental contaminants can produce synergistic effects that exceed the toxicity of individual compounds. A 2025 study demonstrated that polyethylene microplastics (PE-MPs) can adsorb BPA, enhancing its bioavailability and environmental persistence [31]. When combined, PE-MPs and BPA induced significantly greater toxicity in MLTC-1 cells (mouse Leydig tumor cells) and zebrafish models compared to single exposures, decreasing cell viability, increasing apoptosis rates, inducing G2/M cell cycle arrest, and reducing mitochondrial membrane potential [31].
Gene Expression Alterations
In vivo studies using zebrafish models have documented sex-specific transcriptional changes following co-exposure to PE-MPs and BPA. In male zebrafish brains, genes including Gnrh2, Esr1, and Ar were downregulated, while in female brains, Gnrh3, Esr1, and Ar also exhibited downregulation [31]. In male testes, Star, Cyp11a1, and Hsd11b2 were upregulated, whereas Cyp19a1a, Hsd3b, Hsd20b, and Hsd17b3 were downregulated. Female ovaries showed upregulation of Cyp11a1, Cyp17, Cyp11b, Hsd3b, Hsd20b, and Hsd17b3, while Cyp19a1a was downregulated [31]. These findings demonstrate the capacity of bisphenols to disrupt critical reproductive pathways in a sex-specific manner.
Phthalates: Inflammatory Pathways and Immune Dysregulation
Metabolites and Systemic Inflammation
Phthalate metabolites (mPAEs) have emerged as significant modulators of inflammatory responses, with recent evidence pointing to their association with novel systemic inflammatory indices. A 2025 cross-sectional analysis of NHANES data from 2013-2018, encompassing 2,763 U.S. adults, employed multiple analytical models (generalized linear models, weighted quantile sum regression, Bayesian kernel machine regression, and restricted cubic splines) to investigate relationships between nine urinary phthalate metabolites and systemic immune inflammation index (SII) and systemic inflammatory response index (SIRI) [33].
The study identified mono-n-butyl phthalate (MnBP), mono-ethyl phthalate (MEP), and monobenzyl phthalate (MBzP) as being positively associated with SII/SIRI in single-exposure analyses [33]. In mixed-exposure models, mPAEs collectively showed a positive association with SII/SIRI, with MBzP identified as the most significant contributor [33]. These inflammatory indices integrate multidimensional information from neutrophils (pro-inflammatory), lymphocytes (immune regulation), platelets (coagulation/inflammation), and monocytes (chronic inflammation), providing a more systematic assessment of immune-inflammatory balance compared to conventional single-marker approaches [33].
Susceptible Populations
Subgroup analyses revealed that associations between mPAEs and SII/SIRI were more pronounced in specific demographic groups: females, overweight/obese populations, young/middle-aged adults, and individuals with high intake of ultra-processed foods (UPFs) [33]. This pattern highlights the importance of considering effect modification by lifestyle and demographic factors in EDC risk assessment.
Parabens: Metabolic Disruption and Carcinogenic Potential
Metabolic Perturbations
Parabens, commonly used as preservatives in cosmetics, pharmaceuticals, and food products, demonstrate significant potential for metabolic disruption, particularly in vulnerable populations. A 2025 nontargeted metabolomics study investigating paraben exposure in geriatric serum found that methyl paraben (MeP) and propyl paraben (PrP) were detected at high rates and concentrations in elderly individuals, with median MeP concentrations reaching 3.4 ng/mL [17]. The analysis identified 160 metabolites associated with paraben exposure, with steroid hormone biosynthesis and fatty acid metabolism emerging as the most significantly enriched pathways [17].
Molecular docking studies provided mechanistic insights into these metabolic disruptions, revealing that parabens can bind to and potentially inhibit 3α-hydroxysteroid dehydrogenase (3α-HSD), a key enzyme in steroid metabolism [17]. This interaction represents a plausible molecular initiating event in paraben-induced metabolic syndrome and reproductive toxicity.
Estrogenic Activity and Breast Cancer Risk
Network toxicology approaches integrating molecular docking have elucidated potential mechanisms linking paraben exposure to breast carcinogenesis. Parabens exhibit estrogenic activity by binding to estrogen receptors (ESR1 and ESR2), potentially disrupting hormonal homeostasis and increasing breast cancer risk [32]. Additional analyses identified SERPINE1 as another core target in paraben-associated breast cancer pathogenesis [32].
Immune infiltration analyses further revealed that in breast cancer contexts, ESR1 expression was negatively correlated with CD8+ T cells and macrophages, while ESR2 and SERPINE1 expressions showed positive correlations with these immune populations [32]. Molecular docking confirmed strong binding activities between parabens and these core targets, suggesting a multifactorial mechanism involving direct receptor binding and immune modulation [32].
Methodological Approaches and Experimental Protocols
Research Reagent Solutions
Table 2: Essential Research Reagents for EDC Investigation
| Reagent/Resource | Application | Example Use |
|---|---|---|
| MLTC-1 Cells (Mouse Leydig Tumor Cells) | In vitro steroidogenesis assessment | Evaluating combined toxicity of PE-MPs and BPA [31] |
| Zebrafish (Danio rerio) Model | In vivo endocrine disruption studies | HPG axis gene expression analysis after 28-day exposure [31] |
| NHANES Biomonitoring Data | Epidemiological studies | Cross-sectional analysis of phthalate metabolites and inflammation indexes [33] |
| Raman Spectrometry | Microplastic characterization | Physical characterization of PE-MPs [31] |
| Non-targeted Metabolomics | Metabolic pathway disruption screening | Identifying paraben-associated metabolic changes in geriatric serum [17] |
| Molecular Docking Software | Mechanistic binding studies | Predicting paraben interactions with ESR1, ESR2 [32] |
| CCK-8 Assay Kit | Cell viability assessment | Measuring cytotoxicity of BPA and PE-MPs in MLTC-1 cells [31] |
Detailed Experimental Protocol: Combined Toxicity Assessment
A comprehensive protocol for assessing the combined toxicity of microplastics and bisphenols exemplifies contemporary approaches to EDC research [31]:
Cell Culture and Treatment:
- Maintain MLTC-1 cells in RPMI 1640 medium supplemented with 10% FBS and 1% penicillin-streptomycin at 37°C in a 5% CO2 incubator.
- Prepare stock solutions of PE-MPs (average diameter 20 μm) and BPA, with working solutions diluted in culture media.
- Ensure uniform distribution of PE-MPs by vortex mixing and brief sonication of stock solution prior to dilution.
- Maintain DMSO concentration below 0.1% in all treatments and include vehicle control with equivalent DMSO concentration.
Viability Assay:
- Seed cells at density of 1 × 10^5 cells/well in 96-well plates.
- Expose cells to varying concentrations of BPA (0, 1, 10, 100, 150, 200, and 250 μmol/L) and PE-MPs (0, 10, 100, 1000 μg/mL) for 24, 48, and 72 hours.
- Add 10 μL of CCK-8 reagent to each well and incubate for additional 2 hours.
- Measure absorbance at 450 nm using plate reader, normalizing relative optical density against untreated controls.
Gene Expression Analysis:
- Extract total RNA from treated cells or harvested zebrafish tissues using appropriate isolation kits.
- Conduct reverse transcription followed by quantitative real-time PCR.
- Analyze expression of key genes related to steroidogenesis (Star, Cyp11a1, Hsd3b) and hormonal receptors (Ar, Esr1, Esr2).
- Normalize expression to appropriate housekeeping genes and calculate relative expression using 2^(-ΔΔCt) method.
Statistical Analysis Framework for Epidemiological Studies
Recent phthalate research demonstrates sophisticated analytical approaches for complex EDC mixture data [33]:
- Employ generalized linear models (GLM) to assess single-chemical associations between phthalate metabolites and inflammatory indices.
- Utilize weighted quantile sum (WQS) regression to evaluate the overall effect of phthalate mixtures and identify major contributors.
- Implement Bayesian kernel machine regression (BKMR) to capture potential nonlinear and interaction effects in mixed exposures.
- Apply restricted cubic splines (RCS) to visualize dose-response relationships.
- Conduct extensive sensitivity analyses and subgroup analyses to assess robustness of findings across demographic and lifestyle factors.
Visualizing Molecular Pathways and Experimental Workflows
EDC Mechanisms and Inflammatory Signaling
Integrated EDC Research Workflow
The accumulating evidence unequivocally demonstrates that bisphenols, phthalates, and parabens contribute significantly to endocrine disruption, inflammatory pathogenesis, and chronic disease risk through multiple interconnected mechanisms. The global health burden attributable to these chemicals is substantial and continues to grow, with recent data indicating 127 million cases of metabolic disease linked to bisphenol exposure alone in 2024 [30]. Future research directions should prioritize the development of class-based regulatory strategies that address all bisphenol analogues rather than individual compounds [30], increased focus on mixture effects and synergistic interactions [31], implementation of advanced biomonitoring and epidemiological designs to capture long-term exposure effects, and translation of mechanistic insights into targeted therapeutic approaches for EDC-associated conditions. For drug development professionals, understanding these pathways creates opportunities for interventions that might mitigate EDC effects, particularly for populations with high exposure burden.
Identifying Critical Knowledge Gaps in Public Understanding
Endocrine-disrupting chemicals (EDCs), including bisphenol A (BPA), phthalates, and parabens, constitute a significant public health concern due to their pervasive presence in consumer products and potential to interfere with hormonal systems. A comprehensive thesis on public awareness must acknowledge that while scientific evidence linking these chemicals to adverse health outcomes continues to grow, significant disparities exist between scientific understanding and public knowledge. This technical guide systematically identifies and characterizes the critical gaps in public understanding of BPA, phthalates, and parabens, providing a structured framework for researchers and public health professionals to develop targeted interventions. The analysis presented herein is synthesized from current epidemiological studies, social science surveys, and experimental research, offering a multi-dimensional perspective on the public awareness landscape.
Quantitative Assessment of Public Knowledge Gaps
Recent studies across multiple countries have quantified awareness levels for specific EDCs, revealing substantial knowledge gaps within the general public and vulnerable populations. The data demonstrates significant variability in recognition of different chemical substances, with historical contaminants better recognized than those prevalent in personal care products.
Table 1: Public Awareness Levels for Specific EDCs Across Populations
| Chemical | Population Studied | Awareness Level | Study |
|---|---|---|---|
| Lead | Women in Toronto (age 18-35) | Among most recognized EDCs | [34] |
| Parabens | Women in Toronto (age 18-35) | Among most recognized EDCs | [34] |
| Triclosan | Women in Toronto (age 18-35) | Among least recognized EDCs | [34] |
| Perchloroethylene | Women in Toronto (age 18-35) | Among least recognized EDCs | [34] |
| EDCs (general) | Pregnant women/new mothers, Türkiye | 59.2% unfamiliar | [35] |
| Bisphenol A (BPA) | Pregnant women/new mothers, Türkiye | Significant portion never heard | [35] |
| Phthalates | Pregnant women/new mothers, Türkiye | Significant portion never heard | [35] |
| Parabens | Pregnant women/new mothers, Türkiye | Relatively higher awareness | [35] |
| Phthalates | Irish residents (non-experts) | Lower perceived harmfulness | [36] |
| Parabens | Irish residents (non-experts) | Lower perceived harmfulness | [36] |
| PFAS | Irish residents (non-experts) | Lower perceived harmfulness | [36] |
Table 2: Relationships Between Knowledge, Demographics, and Behavioral Outcomes
| Factor | Impact on Awareness/Behavior | Population | Study |
|---|---|---|---|
| Higher Education | More likely to avoid lead | Women with chemical sensitivities | [34] |
| Greater Knowledge of Specific EDCs | Significantly predicted chemical avoidance | Women (preconception/conception) | [34] |
| Higher Risk Perceptions | Predicted greater avoidance of parabens, phthalates | Women in Toronto | [34] |
| Label Reading | Associated with mitigated exposure | Reproductive-aged women | [34] |
| Awareness of Health Risks | Did not consistently translate to avoidance | Reproductive-aged women (only 29% adopted avoidance) | [34] |
Critical Knowledge Domains with Significant Gaps
Understanding of Regulatory Frameworks and Exposure Pathways
A fundamental gap identified in recent research concerns public misunderstanding of chemical regulations and exposure mechanisms. A U.S. survey revealed that most participants held significant misconceptions about regulatory oversight, with 82% incorrectly believing that chemicals must be safety-tested before being used in products, 73% wrongly assuming that product ingredients must be fully disclosed, and 63% mistakenly thinking that restricted chemicals cannot be replaced by similar substitutes [37]. This "false security" perception creates a critical barrier to informed consumer decision-making and public support for stronger regulatory measures.
Additionally, understanding of exposure pathways remains incomplete. While participants demonstrated some awareness of exposure routes (58-86%), comprehensive knowledge of how EDCs migrate from products to the human body remains limited [37]. This includes insufficient understanding of dermal absorption from personal care products, leaching from food packaging, and indoor air contamination from household goods.
Awareness of Health Implications and Vulnerable Populations
The public demonstrates partial understanding of the health implications associated with EDC exposure. While major health effects like impaired fertility (90% awareness), cancer risk (90%), and child brain development impacts (84%) were reasonably recognized [37], knowledge of specific mechanistic pathways and endocrine disruption mechanisms remains limited.
Critical gaps exist in understanding the heightened vulnerability during specific life stages, including fetal development, puberty, and reproductive years. Although pregnant women and new mothers represent a particularly vulnerable population, 59.2% of these women in one study were unfamiliar with EDCs generally [35]. This is especially concerning given evidence that EDCs can disrupt reproductive function by altering hormone levels, including estradiol (E2), luteinizing hormone (LH), and follicle-stimulating hormone (FSH) [12] [21].
Disconnect Between Awareness and Behavioral Change
Perhaps the most significant gap identified is the disconnect between awareness and protective action. Research indicates that even when individuals possess knowledge of EDC risks, this infrequently translates into consistent avoidance behaviors. Among reproductive-aged women aware of risks, only 29% adopted avoidance behaviors [34]. This intention-behavior gap represents a critical challenge for public health interventions.
Consumer behavior research indicates that avoidance strategies are more effective for certain chemicals than others. Individuals who reported avoiding specific ingredient groups (parabens, triclosan, bisphenols, and fragrances) were twice as likely to be in the lowest quartile of cumulative exposure [38]. However, avoiding BPA alone was not effective for reducing overall bisphenol exposure, likely due to substitution with analogous chemicals like BPS and BPF [38].
Methodological Approaches for Assessing Knowledge Gaps
Survey-Based Assessment Protocols
Standardized questionnaires represent the primary methodology for quantifying public knowledge gaps. The Health Belief Model (HBM) has been effectively employed to structure assessments of knowledge, health risk perceptions, beliefs, and avoidance behaviors [34]. A typical implementation includes:
Instrument Design: Developing structured questionnaires with sections on:
- Sociodemographic characteristics
- Knowledge assessment (access to resources, perceived sufficiency of knowledge)
- Health risk perceptions (perceived susceptibility and severity)
- Beliefs about health impacts
- Avoidance behaviors and purchasing practices
Measurement Scales: Utilizing Likert scales (typically 5- or 6-point) ranging from "Strongly Agree" to "Strongly Disagree" for knowledge, perceptions, and beliefs, and frequency scales ("Always" to "Never") for avoidance behaviors [34].
Sampling Strategy: Targeting specific populations (e.g., women aged 18-35 for reproductive health studies) with inclusion/exclusion criteria based on age, gender, and language proficiency [34]. Sample sizes should be calculated for adequate statistical power, with typical studies requiring 300-400 participants to detect awareness frequencies with 95% power and 5% alpha [35].
Implementation: Administration through both in-person recruitment (e.g., at relevant public events) and online platforms (e.g., Google Forms) to enhance participation diversity [34].
Biomonitoring-Coupled Behavioral Assessment
Innovative methodologies combine biological exposure monitoring with behavioral surveys to objectively measure the effectiveness of avoidance behaviors:
Study Design: Crowdsourced biomonitoring approaches recruit participants through open enrollment, targeting diverse populations without restrictive criteria [38].
Exposure Assessment: Collection of urine samples analyzed using:
- Solid-phase extraction combined with high-performance liquid chromatography and tandem mass spectrometry (UPLC-MS/MS)
- Creatinine correction to normalize metabolite concentrations
- Lower limits of detection (LLODs) typically ranging from 0.10-2.30 ng/mL depending on the compound and analytical year [25]
Behavioral Correlation: Survey instruments capturing:
- Consumer product usage patterns
- Cleaning habits
- Specific chemical avoidance behaviors
- Ingredient label reading practices
Data Analysis: Multivariable regression models examining associations between 68+ self-reported exposure behaviors and urinary concentrations of ten+ target chemicals [38]. Evaluation of whether associations are modified by intention to avoid exposures.
Focus Group and Mental Models Approach
Qualitative methodologies provide depth and context to quantitative findings:
Focus Group Convening: Assembling community-engaged research teams (n=38) to define targets for public understanding [37].
Mental Models Approach: Structured facilitation including:
- Transcript coding and thematic analysis
- Causal pathway mapping of factors influencing EDC exposures and health outcomes
- Identification of key communication priorities based on expert consensus
Knowledge Gap Identification: Comparison between expert mental models and public knowledge through subsequent quantitative surveys to identify specific misconceptions and understanding gaps [37].
Experimental Workflows and Analytical Techniques
Biomarker Analysis in Biological Matrices
Advanced analytical techniques enable quantification of EDCs and their metabolites in various biological matrices to assess exposure levels:
Table 3: Research Reagent Solutions for EDC Analysis
| Reagent/Equipment | Function/Application | Specification Example |
|---|---|---|
| MAX Solid-Phase Extraction (SPE) Cartridges | Extract and purify target analytes from complex biological matrices | 10 mg/1 mL capacity [21] |
| UPLC-Tandem Mass Spectrometry | Separate, identify, and quantify chemical concentrations | Poroshell 120 EC-C18 column (100 mm × 4.6 mm, 2.7 μm) [21] |
| β-glucuronidase | Enzymatic deconjugation of phase II metabolites | Incubation at 37°C for 180 min [21] |
| Internal Standards | Isotope-labeled analogs for quantification accuracy | Deuterated compounds for each analyte class [21] |
| Mobile Phases | Chromatographic separation | Milli-Q water, acetonitrile, 2mM ammonium acetate, methanol [21] |
Sample Preparation Protocol:
- Addition of Internal Standards: Spike samples with isotope-labeled internal standards for quantification accuracy [21]
- Enzymatic Hydrolysis: Incubate with β-glucuronidase at 37°C for 180 minutes to deconjugate metabolites [21]
- Solid-Phase Extraction: Load samples onto MAX SPE cartridges, elute targets using 1 mL of 2% formic acid in methanol [21]
- Chromatographic Separation: Utilize gradient elution with specific mobile phase combinations tailored to analyte classes [21]
- Mass Spectrometric Detection: Employ multiple reaction monitoring (MRM) for sensitive and specific quantification [21]
Quality Assurance/Control Measures:
- Include procedural blanks, reagent blanks, and matrix-spiked samples in each batch
- Acceptable recovery rates: 63%-109% depending on analyte class [21]
- Values below LOD handled through standardized imputation protocols [25]
Mixture Risk Assessment Methodologies
Modern exposure science has developed sophisticated approaches to assess the effects of chemical mixtures:
Bayesian Kernel Machine Regression (BKMR):
- Models complex exposure-response relationships for mixtures
- Generates posterior inclusion probabilities (PIPs) to quantify individual chemical contributions (PIP > 0.50 significant) [21]
- Allows visualization of multivariable exposure relationships
Quantile g-Computation (Qgcomp):
- Determines chemical-specific weight contributions in mixtures
- Estimates overall mixture effect direction and magnitude [27]
Weighted Quantile Sum (WQS) Regression:
- Identifies potentially influential chemicals in mixtures
- Handles high correlation between exposures [27]
Figure 1: EDC Mixture Risk Assessment Workflow
Implications for Public Health Intervention and Research
The identified knowledge gaps present both challenges and opportunities for public health initiatives. Research indicates that current regulatory labeling practices insufficiently protect consumers, as terms like "fragrance" or "parfum" can mask dozens to hundreds of undisclosed chemical ingredients, even in products marketed as "green" or "eco-friendly" [34]. This underscores the need for enhanced ingredient transparency alongside educational efforts.
Effective intervention strategies should address the specific gaps identified in this analysis:
- Targeted Educational Campaigns: Focus on chemicals with lowest recognition (triclosan, perchloroethylene) and populations with identified vulnerabilities [34]
- Regulatory Knowledge Integration: Address misconceptions about chemical regulation and safety testing [37]
- Behavioral Implementation Strategies: Bridge the awareness-behavior gap through practical guidance on effective avoidance strategies [38]
- Knowledge Translation Tools: Develop mobile applications and educational toolkits with features including accessibility, information simplicity, personalization, and clear knowledge sharing [39]
Future research directions should prioritize longitudinal studies to assess knowledge evolution over time, evaluation of intervention effectiveness, and investigation of knowledge-behavior relationships across diverse socioeconomic and cultural contexts. Furthermore, integration of public perception data into chemical prioritization processes for biomonitoring programs represents a promising approach for aligning scientific and public health priorities [36].
From Urine to Survey: Methodological Approaches in Exposure and Awareness Assessment
Human Biomonitoring (HBM) serves as a gold-standard method for assessing human exposure to environmental chemicals by quantitatively measuring the parent compounds, their metabolites, or reaction products in biological tissues and fluids. For endocrine-disrupting chemicals (EDCs) such as bisphenols, phthalates, and parabens—substances of significant public concern due to their prevalence in personal care products and food packaging—HBM provides critical data for linking exposure to health risks. This technical guide details the advanced analytical techniques, including liquid chromatography-tandem mass spectrometry (LC-MS/MS) and gas chromatography-mass spectrometry (GC-MS), that enable the precise identification and quantification of these compounds at trace levels. It further explores the role of HBM data in elevating public awareness by translating complex exposure science into actionable evidence for policymakers and consumers, thereby informing risk assessment and regulatory strategies aimed at protecting vulnerable populations.
Human Biomonitoring (HBM) is a critical public health tool that directly measures the concentration of environmental chemicals or their metabolites in human biological specimens, such as urine, blood, and serum. By providing an integrated measure of exposure from all routes—including ingestion, inhalation, and dermal absorption—HBM offers an accurate and individualized assessment of a person's or population's internal dose of specific chemicals [40] [36]. This approach is widely regarded as the gold standard for exposure assessment because it accounts for variations in physiology, behavior, and multiple exposure pathways that indirect environmental monitoring cannot capture.
The application of HBM is particularly vital for assessing exposure to endocrine-disrupting chemicals (EDCs), such as bisphenols, phthalates, and parabens. Public awareness of the potential health risks from these chemicals, which are ubiquitous in consumer products, has grown significantly. HBM data transforms this awareness from a theoretical concern into an evidence-based one. For instance, national surveys like the U.S. National Health and Nutrition Examination Survey (NHANES) have detected numerous EDCs in a majority of participants, providing tangible proof of widespread exposure that commands public and regulatory attention [20] [25]. Furthermore, HBM initiatives such as the European HBM4EU project have prioritized these substance groups, systematically evaluating exposure biomarkers and analytical methods to generate comparable data across borders, which is essential for effective public health policy [41].
Analytical Techniques for Major EDC Classes
The accurate quantification of EDCs and their metabolites in complex biological matrices requires sophisticated instrumentation and meticulously optimized methods. The following sections and tables detail the standard analytical approaches for the major classes of EDCs, highlighting the targeted biomarkers, preferred biological matrices, and key instrumental parameters.
Table 1: Analytical Techniques for Bisphenols, Phthalates, and Parabens
| EDC Class | Primary Biomarkers | Preferred Biological Matrix | Core Analytical Technique | Key Technical Notes |
|---|---|---|---|---|
| Bisphenols | BPA, BPS, BPF (parent compounds) | Urine | High-Performance Liquid Chromatography-Tandem Mass Spectrometry (HPLC-MS/MS) | Often requires enzymatic deconjugation of glucuronidated metabolites; high sensitivity required for low ng/mL levels [41] [25]. |
| Phthalates | Monoester metabolites (e.g., MEP, MnBP, MEHHP, MEOHP) | Urine | LC-MS/MS | Measures metabolites to avoid contamination; specific metabolites like MEP are key biomarkers for personal care product exposure [41] [42]. |
| Parabens | Methylparaben (MPB), Ethylparaben (EPB), Propylparaben (PPB), Butylparaben (BUP) | Urine | LC-MS/MS | Typically analyzed as free compounds; creatinine correction is essential for normalizing urinary dilution [25] [24]. |
Table 2: Analytical Techniques for Other Priority Chemicals
| EDC / Chemical Class | Primary Biomarkers | Preferred Biological Matrix | Core Analytical Technique | Key Technical Notes |
|---|---|---|---|---|
| Per- and Polyfluoroalkyl Substances (PFASs) | Parent compounds (e.g., PFOA, PFOS) | Serum | LC-MS/MS | Protein-binding chemicals require serum; methods require high sensitivity to detect pg/mL to ng/mL levels [41]. |
| Organophosphate Flame Retardants (OPFRs) | Metabolites (e.g., BDCPP from TDCPP) | Urine | LC-MS/MS with APCI or ESI | Metabolite measurement is specific for exposure assessment; BDCPP is a unique biomarker for TDCPP [41] [43]. |
| Metals (e.g., Cd, Cr) | Cadmium (Cd), Chromium (Cr) | Blood, Urine, Erythrocytes | Inductively Coupled Plasma Mass Spectrometry (ICP-MS) | Measurement in erythrocytes is preferred for Cr(VI) exposure; requires careful method optimization to avoid interferences for Cd [41]. |
| Halogenated Flame Retardants (HFRs) | Parent compounds (e.g., HBCDD) | Serum | GC-MS with ECNI or LC-MS/MS | Technique selection depends on the specific compound; GC-MS/MS is an emerging alternative [41]. |
Detailed Experimental Protocol: LC-MS/MS Analysis of Urinary Parabens and Bisphenols
The following protocol, adapted from NHANES and cohort study methodologies, outlines a standard procedure for the simultaneous quantification of parabens and bisphenols in urine [25] [24].
1. Sample Collection and Preparation:
- Collect spot urine samples in pre-cleaned containers without preservatives.
- Freeze samples at -20°C or lower immediately after collection and maintain this temperature until analysis to prevent degradation.
- Thaw samples overnight at 4°C and vortex thoroughly to ensure homogeneity.
2. Hydrolysis and Deconjugation:
- Pipette 1 mL of urine into a centrifuge tube.
- Add an appropriate volume of an enzyme solution containing β-glucuronidase/sulfatase (e.g., from Helix pomatia) to hydrolyze the conjugated metabolites back to their free forms.
- Incubate the mixture for several hours (e.g., 12-16 hours) at 37°C in a shaking water bath.
3. Solid-Phase Extraction (SPE):
- Dilute the hydrolyzed urine sample with a buffer (e.g., ammonium acetate, pH 6.5).
- Condition a reversed-phase C18 SPE cartridge sequentially with methanol and the dilution buffer.
- Load the diluted urine sample onto the cartridge, wash with a water/methanol mixture, and elute the target analytes with pure methanol.
- Evaporate the eluent to dryness under a gentle stream of nitrogen and reconstitute the residue in a mobile phase compatible with LC-MS/MS (e.g., water/methanol).
4. Instrumental Analysis via LC-MS/MS:
- Chromatography: Separate the analytes using a reversed-phase UHPLC system. A C18 column (e.g., 2.1 x 100 mm, 1.8 µm) is typically used. The mobile phase consists of (A) water and (B) methanol, both with 0.1% formic acid, using a gradient elution from 20% B to 95% B over 10-15 minutes.
- Mass Spectrometry: Utilize an electrospray ionization (ESI) source operating in negative ion mode. Detection is performed via multiple reaction monitoring (MRM). Example transitions include:
- Methylparaben: 151 → 136
- Bisphenol A: 227 → 212
- Quantification is achieved using isotope-labeled internal standards (e.g., ¹³C-BPA, D4-Methylparaben) for each analyte to correct for matrix effects and recovery losses.
5. Quality Assurance/Quality Control (QA/QC):
- Include calibration standards, reagent blanks, and quality control materials (pooled urine spiked at low and high concentrations) in each analytical batch.
- Report results with creatinine correction to account for urinary dilution.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful HBM analysis relies on a suite of high-purity reagents and specialized materials. The following table details the essential components of a researcher's toolkit for quantifying EDCs.
Table 3: Key Research Reagent Solutions for HBM of EDCs
| Reagent/Material | Function/Application | Technical Notes |
|---|---|---|
| Isotope-Labeled Internal Standards | Quantification and correction for matrix effects. | Examples: ¹³C-Bisphenol A, D4-Monoethyl phthalate (D4-MEP). Crucial for achieving high accuracy in mass spectrometry [43] [44]. |
| β-Glucuronidase/Sulfatase Enzyme | Enzymatic deconjugation of phase-II metabolites in urine. | Releases the free, aglycone form of the analyte for measurement, essential for assessing total body burden [25]. |
| Solid-Phase Extraction (SPE) Cartridges | Sample clean-up and pre-concentration of analytes. | Reversed-phase C18 or mixed-mode sorbents are commonly used to remove interfering compounds from the biological matrix [25]. |
| Chromatography Columns | Separation of analytes prior to mass spectrometric detection. | UHPLC columns with sub-2µm particle size (e.g., C18, 100 mm x 2.1 mm) provide high-resolution separation, reducing ion suppression [43]. |
| Certified Reference Materials | Method validation and quality control. | Used to establish accuracy and traceability of measurements; available from organizations like NIST [40]. |
HBM Workflow: From Sample to Public Awareness
The journey of HBM from a biological sample to a catalyst for public awareness and policy involves a meticulously structured workflow. The following diagram illustrates the key stages of this process.
Human Biomonitoring stands as an indispensable scientific tool, providing the most direct and definitive evidence of human exposure to bisphenols, phthalates, parabens, and other EDCs. The sophistication of analytical techniques like LC-MS/MS and GC-MS/MS enables the precise quantification of these chemicals at trace levels, generating the robust data required for credible health risk assessments. This technical capability is the foundation upon which public awareness is built and validated. By translating abstract concerns about "chemicals in the environment" into concrete, measurable data on "chemicals in our bodies," HBM empowers individuals, informs public discourse, and provides policymakers with the evidence needed to enact protective regulations. As analytical methods continue to advance towards greater sensitivity and efficiency, HBM will undoubtedly play an even more critical role in bridging the gap between scientific evidence and public health action, ensuring that awareness leads to tangible reductions in exposure and risk.
Within the context of public awareness research on endocrine-disrupting chemicals (EDCs) such as bisphenol A (BPA), phthalates, and parabens, the ability to accurately measure public perceptions is paramount [28] [12]. These environmental contaminants, prevalent in consumer products and linked to adverse health outcomes including reproductive issues and metabolic disorders, represent a significant public health concern [12] [45]. Social surveys employing well-designed questionnaires and Likert scales serve as critical methodological tools for quantifying public understanding, risk perception, and perceived harmfulness of these chemicals [36]. This technical guide provides researchers and scientists with a comprehensive framework for developing, implementing, and analyzing surveys aimed at capturing reliable data on chemical risk perceptions, with specific application to EDC research.
Likert Scale Fundamentals and Design Considerations
A Likert scale is a psychometric measurement tool used to quantify attitudes, opinions, or perceptions through a series of structured response options [46] [47]. Typically, respondents indicate their level of agreement or disagreement with a specific statement along a symmetric continuum, often with five or seven points [48]. The fundamental strength of Likert scales lies in their ability to transform subjective qualitative perceptions into quantifiable ordinal data suitable for statistical analysis [47].
Scale Structure and Response Options
The design of response options significantly impacts data quality and respondent experience. Key considerations include the number of scale points and the framing of responses [46] [48].
- Number of Scale Points: While 5-point and 7-point scales are most common, the optimal choice depends on the desired balance between granularity and respondent burden [48]. Odd-numbered scales typically include a neutral midpoint, while even-numbered scales force respondents toward a positive or negative direction [46].
- Bipolar vs. Unipolar Scales: Bipolar scales measure two opposing attributes along a single continuum (e.g., "Extremely harmful" to "Not at all harmful"), whereas unipolar scales measure the intensity of a single attribute (e.g., "Not at all harmful" to "Extremely harmful") [46]. For perceived harmfulness, a unipolar approach often provides more precise measurement.
Table 1: Common Likert Response Formats for Measuring Perceived Harmfulness
| Scale Type | Number of Points | Response Options | Best Use Cases |
|---|---|---|---|
| Agreement | 5 or 7 | Strongly Disagree to Strongly Agree | Assessing agreement with specific risk statements |
| Perceived Harm | 5 | Not at all harmful, Slightly harmful, Moderately harmful, Very harmful, Extremely harmful | Direct measurement of harm perceptions |
| Frequency | 5 | Never, Rarely, Sometimes, Often, Always | Measuring frequency of risk-avoidance behaviors |
| Importance | 5 | Not at all important to Extremely important | Gauging importance of regulatory actions |
Crafting Effective Likert Items
Item construction is critical for obtaining valid and reliable data. The following principles should guide question development [46] [47]:
- Focus on a Single Construct: Each item should assess only one aspect of the topic. Avoid double-barreled questions that combine multiple concepts, such as "How harmful are BPA and phthalates?" which conflates two distinct chemical groups [46].
- Clarity and Simplicity: Use clear, unambiguous language accessible to the target population. Avoid technical jargon where possible, or provide brief definitions [46]. For example, instead of "Are you aware of the endocrine-disrupting properties of phthalates?", consider "How harmful do you think chemicals called 'phthalates' (often found in plastics and cosmetics) are to human health?"
- Balanced Framing: Include both positively and negatively framed statements to control for acquiescence bias (the tendency to agree with statements regardless of content) [47]. For instance, follow a statement like "BPA in food packaging is a serious health threat" with a reverse-coded item such as "The health risks of BPA exposure are exaggerated."
- Avoid Leading Questions: Phrasing should not suggest a particular response or assume a level of knowledge. Instead of "Don't you agree that parabens are dangerous?", use "To what extent do you agree or disagree that parabens pose a health risk?"
Application to EDC Awareness Research
Research reveals significant gaps in public knowledge regarding EDCs. A 2025 study among Turkish healthcare professionals found critically low awareness levels, with only 23.7% having previously encountered information about bisphenols and 82.6% classified as having inadequate knowledge [45]. This underscores the need for precise measurement tools to identify specific knowledge gaps and inform public health communication strategies.
Domain-Specific Questionnaire Design
When researching public awareness of BPA, phthalates, and parabens, surveys should encompass multiple knowledge domains to provide a comprehensive assessment [45] [36]:
- Awareness and Recognition: Measure basic familiarity with the chemical names and their common sources (e.g., "Before this survey, had you heard of bisphenol A (BPA)?") [36].
- Perceived Harmfulness: Assess beliefs about health risks using Likert scales (e.g., "How harmful do you believe exposure to parabens in personal care products is?") [36].
- Knowledge of Exposure Routes: Evaluate understanding of how exposure occurs (e.g., "To what extent do you agree that food packaging is a significant source of BPA exposure?") [37].
- Regulatory Knowledge: Gauge awareness of regulatory status and safety testing requirements (e.g., "To what extent do you agree that chemicals must be proven safe before they are used in consumer products in the U.S.?") [37].
- Preventive Behaviors: Measure self-reported avoidance behaviors and their frequency (e.g., "How often do you try to avoid plastics with recycling code 7 to reduce BPA exposure?") [48].
The following workflow outlines the systematic process of developing and validating a survey instrument for this research context.
Experimental Protocols from Recent Studies
Recent research provides validated methodological approaches for surveying EDC awareness:
Healthcare Professional Survey Protocol: A 2025 cross-sectional study implemented a standardized 13-item bisphenol knowledge assessment questionnaire administered via in-person interviews [45]. The protocol involved:
- Participant Recruitment: Convenience sampling of physicians, nurses, midwives, and health technicians from a tertiary care hospital.
- Instrument Validation: The questionnaire was developed through expert consultation with environmental health specialists and content validation by three public health academics.
- Pilot Testing: A preliminary test with 20 healthcare professionals (excluded from final analysis) to refine question clarity and relevance.
- Data Analysis: Utilization of descriptive statistics, ANOVA, chi-square tests, and decision tree analysis to identify knowledge predictors [45].
Public Perception Survey Methodology: The HBM4IRE feasibility study (2025) employed a social survey adapted from the European HBM4EU framework to assess awareness and perceived harmfulness of 24 chemical groups [36]. The methodology featured:
- Two-Stage Questioning: For each chemical group, participants were first asked about prior awareness ("Known/Unknown"), followed by a Likert-scale assessment of perceived harmfulness for those indicating familiarity.
- Digital Distribution: The survey was disseminated via SurveyMonkey through institutional email lists, websites, and social media channels.
- Comparative Analysis: Data were stratified to compare perceptions between expert (those involved in chemical management) and non-expert groups, revealing significant awareness gaps for phthalates, parabens, and PFAS among non-experts [36].
Psychometric Validation and Scale Evaluation
Ensuring the reliability and validity of Likert scale instruments is essential for producing scientifically rigorous findings [47].
Reliability Assessment
- Internal Consistency: Measured using Cronbach's alpha, which assesses how closely related a set of items are as a group [47]. A value greater than 0.7 is generally considered acceptable, while values greater than 0.8 are good. For multi-item scales measuring EDC knowledge, target internal consistency should exceed 0.8 [47].
- Test-Retest Reliability: Administering the same instrument to the same participants at two different time points to evaluate score stability, particularly important for measuring traits presumed to be stable over time [47].
Validity Assessment
- Content Validity: Ensures the survey adequately covers all relevant aspects of EDC knowledge [47]. This is typically established through expert review by environmental health specialists and public health researchers.
- Construct Validity: Evaluates whether the instrument truly measures the theoretical construct of "EDC awareness" [47]. Factor analysis is the primary statistical method used to verify that items load onto intended theoretical dimensions.
- Criterion Validity: Assesses how well the survey correlates with other established measures of environmental health literacy or related constructs [47].
Data Analysis and Interpretation
The analysis of Likert-derived data requires careful consideration of its ordinal nature, where responses have a rank order but the distances between categories may not be mathematically equal [47] [49].
Analytical Approaches
Table 2: Statistical Methods for Analyzing Likert Scale Data
| Analysis Type | Recommended Methods | Application Example |
|---|---|---|
| Descriptive Statistics | Frequency distributions, percentages, mode, median [47] [49] | "65% of respondents rated phthalates as 'very harmful'" |
| Group Comparisons | Mann-Whitney U test, Kruskal-Wallis test [49] | Comparing harm ratings between experts and non-experts |
| Relationship Analysis | Spearman's rank-order correlation [46] [49] | Correlation between knowledge scores and preventive behaviors |
| Multi-item Scale Analysis | Summated scales, mean scores, parametric tests (t-tests, ANOVA) [49] | Creating a composite "EDC concern" score from multiple items |
While Likert data is technically ordinal, a body of research supports the use of parametric statistics (e.g., t-tests, ANOVA, Pearson correlations) with Likert-derived data, particularly when using multi-item summated scales, the data approximate a normal distribution, and sample sizes are sufficient [49]. However, it is crucial to explicitly state and justify the analytical approach in methodological sections [49].
Visualization and Reporting
Effective data presentation enhances interpretability:
- Frequency Bar Charts: Visualize the distribution of responses for each item, clearly showing the proportion of respondents selecting each Likert point [46] [47].
- Stacked Bar Charts: Compare response distributions across different demographic or professional groups (e.g., healthcare providers vs. general public) [36].
- Summary Tables: Present composite scores (means, medians) for multi-item scales across different participant subgroups [45].
The table below outlines key materials and their functions for implementing EDC awareness surveys.
Table 3: Research Reagent Solutions for EDC Awareness Surveys
| Research Tool | Function | Implementation Example |
|---|---|---|
| Validated Knowledge Questionnaire | Measures objective knowledge of EDC sources, health effects, and regulations | 13-item bisphenol knowledge assessment [45] |
| Perceived Harmfulness Scale | Quantifies subjective risk perceptions for specific chemicals | 5-point Likert scale from "Not at all harmful" to "Extremely harmful" [36] |
| Demographic Module | Captures participant characteristics for subgroup analysis | Items on profession, education, age, gender, and prior EDC awareness [45] |
| Statistical Analysis Software | Performs reliability tests and statistical comparisons | SPSS, R, or Python with appropriate statistical packages [45] |
Well-designed social surveys utilizing rigorously developed Likert scales are indispensable for accurately measuring public awareness and perceived harmfulness of endocrine-disrupting chemicals like BPA, phthalates, and parabens. By adhering to established psychometric principles—including careful item construction, systematic validation, and appropriate analytical techniques—researchers can generate robust, actionable evidence regarding public knowledge gaps and risk perceptions. Such evidence is foundational for developing targeted public health interventions, effective risk communication strategies, and informed regulatory policies aimed at mitigating the health impacts of widespread EDC exposure. Future research should continue to refine these methodological approaches, particularly in addressing emerging chemical substitutes and their public perception.
Correlating Biomarker Levels with Consumer Behavior and Product Use
The pervasive use of synthetic chemicals in consumer products represents a significant public health consideration within modern environmental epidemiology. Chemicals such as bisphenol A (BPA), phthalates, and parabens are established endocrine-disrupting chemicals (EDCs) with demonstrated potential to interfere with hormonal homeostasis [12]. Despite growing scientific evidence linking these compounds to adverse health outcomes, including impaired reproductive function, metabolic disorders, and increased cancer risk, public awareness remains limited, particularly regarding exposure sources and risk mitigation strategies [50] [36]. This technical guide provides methodological frameworks for researchers investigating correlations between biomarker levels and consumer product use, with particular emphasis on study design, analytical techniques, and data interpretation within the context of public awareness research.
The detection of EDCs in biological matrices confirms systemic absorption and potential for biological activity. Recent studies have consistently demonstrated that personal care product (PCP) use significantly predicts urinary concentrations of phthalates, parabens, and phenols across diverse populations [23] [51]. For instance, a nationally representative Korean study found that females used all categories of PCPs more frequently than males, with correspondingly higher urinary concentrations of methylparaben (MeP), ethylparaben (EtP), and propylparaben (PrP) [51]. Similarly, intervention studies have shown that restricting cosmetic use can substantially reduce urinary concentrations of BPA and benzophenones within days [23]. These findings underscore the value of biomonitoring data in both exposure assessment and evaluation of public health interventions.
Analytical Methodologies for Biomarker Quantification
Sample Collection and Storage Protocols
Proper sample collection and storage conditions are fundamental to preserving biomarker integrity. For phenols, phthalates, and parabens, spot urine samples represent the preferred matrix due to non-invasive collection and relatively high biomarker concentrations. Based on NHANES protocols, participants should provide at least 5mL of urine in standardized collection cups [25]. While first-morning voids are preferable for their higher concentration, random spot samples are acceptable for population studies. Immediately following collection, samples should be frozen at -20°C until analysis to prevent degradation [25]. For biobanking purposes, long-term storage at -80°C is recommended to maintain biomarker stability over extended periods [52].
Chemical Analysis Techniques
High-performance liquid chromatography coupled with tandem mass spectrometry (HPLC-MS/MS) represents the gold standard for quantifying EDCs in biological matrices due to its superior sensitivity and specificity. The methodological approach developed for NHANES employs solid-phase extraction (SPE) followed by HPLC separation and MS/MS detection [25]. This protocol enables simultaneous quantification of multiple analyte classes, including bisphenols, parabens, benzophenones, and phthalate metabolites.
Detailed analytical parameters should include:
- Chromatographic separation: Poroshell 120 EC-C18 column (100mm × 4.6mm, 2.7μm)
- Mobile phase: Gradient elution using Milli-Q water and acetonitrile for parabens and phthalates; 2mM ammonium acetate and methanol for bisphenols and OH-PAHs
- Ionization source: Electrospray ionization (ESI) in negative mode
- Mass detection: Multiple reaction monitoring (MRM) for enhanced specificity [21]
Quality assurance/quality control (QA/QC) measures must include procedural blanks, reagent blanks, and matrix-spiked samples for recovery assessment. Method validation should establish limits of detection (LOD), precision, accuracy, and linear dynamic ranges. Values below the LOD require appropriate imputation strategies, typically LOD/√2 [25] [52].
Table 1: Quality Assurance Parameters for EDC Biomarker Analysis
| Parameter | mPAEs | Parabens | Bisphenols | OH-PAHs |
|---|---|---|---|---|
| Recovery (%) | 77-109 | 74-97 | 63-108 | 64-105 |
| Background (ng/mL) | 4.14-8.91 | 12.19 | 0.26-0.94 | 0.01-0.17 |
| LOD Range (ng/mL) | 0.10-0.40 | 0.10-1.00 | 0.20-0.40 | Compound-specific |
Creatinine Correction and Lipid Adjustment
To account for urinary dilution, creatinine correction is essential for normalizing biomarker concentrations. Urinary creatinine should be measured using automated clinical chemistry analyzers based on the Jaffe reaction. Creatinine-adjusted values (μg/g creatinine) provide more reliable exposure estimates than uncorrected volumetric concentrations [53] [25]. For lipophilic compounds in serum or follicular fluid, lipid adjustment (ng/g lipid) may be necessary to account for varying lipid content between samples.
Study Designs for Linking Behavior and Exposure
Cross-Sectional Surveys with Biomonitoring
Questionnaire development represents a critical component in exposure-behavior correlation studies. Instruments should capture detailed information on:
- Product usage frequency (daily, weekly, monthly)
- Product categories (skincare, cosmetics, fragrances, hair products)
- Application areas and surface coverage
- Temporal patterns relative to biological sampling
Validated surveys, such as those implemented in the Korean National Environmental Health Survey, effectively associate specific product categories with elevated biomarker levels [51]. For example, fragrance product use was significantly associated with ethyl paraben exposure in preschoolers, while makeup use predicted methyl paraben levels across age groups [51].
Table 2: Consumer Behavior Variables and Associated Biomarkers
| Product Category | Chemical Class | Key Biomarkers | Population with Strongest Association |
|---|---|---|---|
| Skincare products | Parabens | MeP, EtP, PrP | Female adolescents [23] |
| Sunscreens | Benzophenones | BP-3, BP-1 | Korean adolescent girls [23] |
| Cosmetics/makeup | Phthalates | MCPP, MEP | Preschoolers, adults [51] |
| Fragrances | Parabens | EtP | Preschoolers [51] |
| Antimicrobial soaps | Phenols | Triclosan | Adults [25] |
| Nail polishes | Phthalates | MCPP | Preschoolers, adults [51] |
Intervention Studies
Controlled intervention designs provide the most compelling evidence for causal relationships between product use and biomarker levels. The fundamental approach involves baseline biomonitoring followed by a period of product use restriction with subsequent biomarker measurement.
A rigorous intervention protocol should include:
- Baseline assessment: Urine collection and product use inventory
- Intervention phase: Provision of verified low-EDC alternative products or complete product abstinence for a defined period (typically 2-7 days)
- Follow-up assessment: Post-intervention urine collection under identical conditions
A study of Korean adolescent girls demonstrated that a two-day cosmetic intervention significantly reduced urinary concentrations of BPA (32.7%) and benzophenones (11.9-22.8%) among regular product users [23]. Interestingly, the reduction was not significant when including participants with no baseline product use, highlighting the importance of stratified analysis by usage patterns [23].
Mixture Analysis Approaches
Human exposure to EDCs occurs as complex mixtures rather than isolated compounds, necessitating advanced statistical methods for evaluating combined effects. Three principal methodologies have emerged for mixture analysis:
Weighted Quantile Sum (WQS) Regression: Identifies a weighted index of mixture components most associated with health outcomes. WQS has successfully identified triclosan as the predominant driver in phenol/paraben mixtures associated with breast cancer risk [25].
Bayesian Kernel Machine Regression (BKMR): A flexible approach for modeling complex exposure-response relationships and interactions. BKMR generates posterior inclusion probabilities (PIPs) to quantify individual chemical contributions, with a PIP >0.50 indicating significant influence [27] [21].
Quantile g-Computation: Estimates the joint effect of increasing all mixture components by one quantile simultaneously. This method identified overall positive associations between PCP-related chemical mixtures and osteoarthritis prevalence [27].
Statistical Analysis and Data Interpretation
Handling Non-Detects and Extreme Values
Biomarker data typically contain substantial left-censored observations (values below LOD). Recommended approaches for non-detects include substitution methods (LOD/√2) [25] or multiple imputation techniques. For right-skewed distributions, log10 transformation improves normality and reduces the influence of extreme values [25].
Confounder Adjustment
Covariate selection should be based on established associations with both exposure and outcome. Essential confounders include:
- Demographic factors: Age, race/ethnicity, socioeconomic status (PIR)
- Anthropometric measures: Body mass index (BMI)
- Lifestyle factors: Smoking status, alcohol consumption, physical activity
- Physiological parameters: Renal function (for urinary biomarkers), menopausal status
Stratified analysis by potential effect modifiers (e.g., BMI, age groups) is recommended to identify susceptible subpopulations. For instance, associations between triclosan and breast cancer risk were more pronounced among overweight individuals (BMI ≥25 kg/m²) and those aged <60 years [25].
Complex Survey Design Analysis
Nationally representative surveys (e.g., NHANES, KNEHS) employ multistage probability sampling requiring specialized analytical approaches. Analysis must incorporate sample weights, strata, and cluster variables to account for complex survey design and produce population-representative estimates [25].
The Researcher's Toolkit
Table 3: Essential Research Reagents and Materials
| Reagent/Material | Specification | Application | Reference |
|---|---|---|---|
| MAX SPE cartridges | 10mg/1mL | Solid-phase extraction of phenols, parabens | [21] |
| β-glucuronidase | Helix pomatia type | Enzymatic deconjugation of phase II metabolites | [21] |
| Isotope-labeled internal standards | ¹³C or deuterated analogs | Quantification by isotope dilution | [52] |
| UPLC-QToF-MS system | Quadrupole time-of-flight mass spectrometry | High-resolution biomarker quantification | [53] |
| Creatinine assay kits | Jaffe reaction-based | Urine dilution correction | [53] [25] |
| Stable isotope tracers | ¹³C-labeled compounds | Recovery assessment during extraction | [21] |
Experimental Workflow and Signaling Pathways
The following diagrams illustrate key experimental workflows and biological pathways relevant to EDC biomarker research.
Biomarker Analysis Workflow
EDC Signaling Pathways in Disease Pathogenesis
The methodologies outlined in this technical guide provide a robust framework for investigating correlations between consumer product use and biomarker levels of EDCs. As research continues to elucidate the health implications of chronic low-dose EDC exposure, the integration of precise biomonitoring, detailed behavioral assessment, and advanced mixture analysis will be crucial for informing evidence-based public health policies and targeted risk communication strategies. Future research directions should prioritize longitudinal designs to capture exposure variability over time, harmonized protocols for cross-study comparisons, and sensitive population studies to identify vulnerable subgroups requiring tailored protection measures.
The pervasive presence of endocrine-disrupting chemicals (EDCs)—including phthalates, parabens, and bisphenols—in consumer products has raised significant public health concerns due to their documented adverse effects on human health. These compounds, commonly found in plastics, personal care products, and food packaging, are known to interfere with hormonal signaling and have been linked to developmental, reproductive, and metabolic disorders [54] [42]. Within the broader context of research on public awareness of bisphenol A, phthalates, and parabens, this case study examines the efficacy of structured awareness campaigns as an intervention strategy for reducing internal exposure levels, as measured through urinary biomarkers.
Human biomonitoring (HBM) studies provide a critical tool for assessing exposure to EDCs by quantifying specific chemical metabolites or parent compounds in biological samples. The measurement of urinary biomarker levels serves as a validated approach for evaluating population-wide exposure and the effectiveness of exposure-reduction interventions [55] [56]. This technical analysis synthesizes evidence from recent studies to evaluate whether educational initiatives and public awareness campaigns successfully translate into measurable reductions in EDC exposure biomarkers, with particular focus on the methodologies employed, observed outcomes, and implications for future public health strategies.
Key Studies and Quantitative Evidence
Belgian Population Time-Trend Study
A pivotal human biomonitoring study conducted in Liège, Belgium, tracked exposure trends in an adult population between 2015 and 2018, coinciding with a provincial awareness campaign [55] [57]. The investigation revealed significant changes in urinary biomarker concentrations over the three-year period, as summarized in Table 1.
Table 1: Urinary Biomarker Trends in Belgian Population (2015-2018)
| Chemical Class | Specific Compounds | Trend (2015-2018) | Magnitude of Change | Detection Frequency |
|---|---|---|---|---|
| Parabens | Methylparaben, Ethylparaben | Significant decrease | 1.3 to 2.5-fold reduction | High (>89% for most metabolites) |
| Phthalates | Multiple metabolites (except monoethyl phthalate) | Significant decrease | 1.3 to 2.5-fold reduction | High (89-98% for most metabolites) |
| Phthalate Substitute | DINCH metabolites | Significant increase | Higher concentrations in 2018 | Increasing detection |
| Bisphenol Alternatives | BPS, BPF, BPZ, BPP | Significant increase | Higher concentrations in 2018 | Increasing detection |
| Bisphenol A | BPA | No significant change | Stable levels | High |
The study authors noted that while paraben and phthalate exposures decreased likely due to regulatory actions and formulation changes, it was not feasible to unequivocally attribute these reductions to the awareness campaign alone [55]. The concomitant rise in substitute chemicals (DINCH and bisphenol alternatives) highlights the complex dynamics of chemical exposure patterns, where reductions in regulated compounds are often offset by increased use of replacement chemicals whose toxicological profiles may be less thoroughly characterized.
Intervention Studies on Behavioral Modification
Targeted intervention studies provide more direct evidence of causality between awareness campaigns and biomarker reduction. A review of mitigation strategies highlighted that switching to phthalate-free personal care products significantly reduced urinary monoethyl phthalate (MEP) levels by 27.4% within just three days [42]. This finding demonstrates that conscious consumer substitution can rapidly alter internal exposure measures.
Similarly, a U.S. study utilizing direct-to-consumer biomarker reporting found that providing individuals with their personal EDC metabolite levels alongside actionable recommendations led to increased environmental health literacy and corresponding reductions in urinary biomarkers [56]. This "report-back" intervention approach demonstrates that personalized data coupled with specific guidance effectively motivates exposure-reducing behaviors.
Table 2: Effectiveness of Different Intervention Strategies
| Intervention Type | Study Population | Key Outcomes | Implementation Challenges |
|---|---|---|---|
| Product Substitution | Adolescent girls | Significant decreases in phthalates, parabens, and phenols within 3 days | Requires access to and identification of safer alternatives |
| Biomarker Report-Back | Adults of reproductive age | Increased environmental health literacy; reduced EDC exposure | Individual burden of behavior change; cost of testing |
| Public Awareness Campaign | General adult population | Mixed results; decreased phthalates/parabens but increased alternatives | Difficult to isolate campaign effects from regulatory impacts |
| Healthcare Provider Counseling | Pregnant women | Limited implementation despite professional recommendations | Poor EDC-specific environmental health literacy among providers |
Methodological Approaches in Awareness Research
Study Design Considerations
Research evaluating awareness campaigns employs distinct methodological frameworks. The pre-post study design,
as implemented in the Belgian study, involves biomarker measurement in the same population before and after an intervention period [55]. This approach controls for inter-individual variability but faces challenges in isolating the campaign effects from concurrent regulatory changes and market trends.
Randomized controlled interventions offer more rigorous evidence of causality. In these studies, participants are assigned to intervention groups (receiving education and alternative products) or control groups (maintaining usual practices). The aforementioned study with adolescent girls exemplifies this approach, demonstrating that providing phthalate-free personal care products significantly reduced urinary metabolite levels [42]. These studies typically incorporate standardized urine collection protocols, with first-morning void samples preferred to capture concentrated metabolite levels, and strict temperature control during storage and transport to preserve sample integrity [56].
Biomarker Quantification Techniques
Advanced analytical techniques are essential for accurate biomarker assessment. The Belgian study and NHANES protocols utilize solid-phase extraction (SPE) combined with high-performance liquid chromatography tandem mass spectrometry (HPLC-MS/MS) [55] [25]. This methodology offers high sensitivity and specificity for quantifying EDC metabolites at the low concentrations typical in general population exposure.
Liquid chromatography-mass spectrometry operations require careful method validation, including determination of limits of detection (LOD) and quantification (LOQ). For values below LOD, imputation strategies (e.g., LOD/√2) are standardly applied [25]. Additionally, creatinine correction is essential to account for urine dilution, typically measured using enzymatic methods on a separate portion of the urine sample [25] [56].
Covariate Assessment and Statistical Analysis
Comprehensive studies collect extensive data on potential confounding factors, including age, body mass index, residential characteristics (urban vs. rural), and product usage patterns [55] [56]. Multivariate regression models identify significant predictors of exposure, though determination coefficients often remain low, indicating that known covariates explain only a small portion of biomarker variance [55].
Emerging statistical approaches for mixture analysis, including Bayesian Kernel Machine Regression (BKMR) and quantile g-computation, enable investigation of combined effects of multiple chemicals [21] [25]. These methods are particularly relevant for real-world exposure scenarios where individuals encounter complex chemical mixtures simultaneously.
Experimental Workflow
The following diagram illustrates the standard experimental workflow for conducting awareness campaign intervention studies and measuring urinary biomarkers:
Diagram 1: Experimental workflow for awareness campaign studies
Signaling Pathways of Target Chemicals
The biological activity of the chemicals measured in urinary biomarker studies involves complex endocrine disruption pathways. The following diagram illustrates the primary mechanisms through which these compounds exert their effects:
Diagram 2: Signaling pathways of endocrine-disrupting chemicals
Research Reagent Solutions
The following table details essential research reagents and materials used in the featured studies for quantifying urinary biomarkers of EDC exposure:
Table 3: Essential Research Reagents for EDC Biomarker Analysis
| Reagent/Material | Function in Research | Application Example | Technical Specifications |
|---|---|---|---|
| Solid-Phase Extraction (SPE) Cartridges | Extract and concentrate target analytes from urine matrix | MAX SPE cartridges (10 mg/1 mL) for phenolic compounds | Mixed-mode anion exchange; conditioned with methanol and water |
| β-Glucuronidase | Enzymatic deconjugation of phase II metabolites | Hydrolysis of glucuronidated phthalate metabolites | Incubation at 37°C for 180 min to release free forms |
| HPLC-MS/MS System | Separation and quantification of target biomarkers | Poroshell 120 EC-C18 column for paraben separation | 100 mm × 4.6 mm, 2.7 μm particle diameter; gradient elution |
| Isotope-Labeled Internal Standards | Correct for matrix effects and recovery variations | 13C- or D4-labeled phthalate metabolites | Added prior to extraction to monitor analytical variability |
| Certified Reference Materials | Method validation and quality assurance | NIST standard reference materials for urine biomarkers | Verify accuracy and participate in interlaboratory comparisons |
| Creatinine Assay Kits | Normalize for urine dilution | Enzymatic creatinine determination on clinical analyzers | Essential for standardizing biomarker concentrations |
Discussion and Research Gaps
Interpretation of Campaign Effectiveness
The evidence regarding awareness campaign effectiveness presents a complex picture. While several studies demonstrate significant reductions in urinary biomarkers following targeted interventions, the Belgian study highlights the challenge of attributing population-level changes specifically to awareness activities amidst concurrent regulatory changes [55]. This suggests that awareness campaigns may be most effective when implemented as part of a comprehensive strategy including regulation, market shifts, and public education.
The consistent observation that substitute chemicals increase as traditional phthalates and parabens decrease raises important questions about the net public health benefit of chemical substitution without thorough safety assessment. Future awareness campaigns should educate consumers about both traditional EDCs and their emerging alternatives to prevent regrettable substitutions.
Methodological Considerations and Limitations
Current research faces several methodological challenges. The predominantly observational nature of many awareness campaign studies limits causal inference. Additionally, most interventions focus on short-term biomarker reduction, leaving open questions about the sustainability of behavior changes and exposure reductions over extended periods.
Significant demographic disparities in EDC exposure highlight another limitation. Research indicates that racial and ethnic minority groups often demonstrate higher levels of certain parabens, phthalates, and PAHs [20]. Similarly, individuals with lower socioeconomic status may face barriers to implementing exposure-reduction recommendations due to the higher cost of "safer" products and limited access to information. Future campaigns require targeted approaches to address these inequities.
Future Research Directions
Promising research directions include developing more sophisticated chemical mixture analysis methods to better understand real-world exposure scenarios [21]. Additionally, investigation of sensitive exposure windows—particularly during early development and pregnancy—remains a priority, as these periods may represent critical opportunities for intervention impact [42] [35].
Expanding research on behavioral drivers and barriers to exposure reduction would strengthen future campaign design. The finding that women showed increased readiness to reduce exposures after biomarker report-back while men demonstrated the opposite response suggests the need for demographic-tailored communication strategies [56]. Furthermore, integrating environmental health literacy into healthcare provider education could leverage clinical encounters for exposure reduction counseling.
This case study demonstrates that while awareness campaigns and educational interventions show promise for reducing exposure to phthalates, parabens, and bisphenols—as measured through urinary biomarkers—their effectiveness is influenced by multiple factors including concurrent regulations, market availability of safer alternatives, and socioeconomic considerations. The consistent decrease in traditional phthalate and paraben biomarkers in intervention studies confirms that conscious consumer choices can meaningfully reduce internal exposure doses.
However, the parallel increase in substitute chemicals underscores the dynamic nature of chemical exposures and the need for comprehensive approaches that address entire chemical classes rather than individual substances. Future efforts should integrate awareness campaigns with broader policy initiatives, corporate responsibility, and continued biomonitoring to track both intended and unintended consequences of intervention strategies.
For researchers and public health professionals, this analysis highlights the importance of rigorous study designs, standardized biomarker measurements, and equity-focused implementation to maximize the public health impact of awareness campaigns aimed at reducing EDC exposure across diverse populations.
Human biomonitoring (HBM) has emerged as a gold-standard method for assessing population-wide exposure to environmental chemicals by measuring the chemicals or their metabolites in human biological samples like urine, blood, and tissues [36]. Two pioneering programs have fundamentally advanced this field: the U.S. National Health and Nutrition Examination Survey (NHANES) and the European Human Biomonitoring Initiative (HBM4EU). These programs provide critical insights into exposure patterns, trends, and potential health effects of endocrine-disrupting chemicals (EDCs) such as bisphenol A (BPA), phthalates, and parabens across diverse populations.
NHANES employs a complex, multistage probability sampling design to represent the civilian, non-institutionalized U.S. population, collecting comprehensive data through interviews, physical examinations, and biological samples [25]. Similarly, HBM4EU represents a coordinated effort across 30 European countries to harmonize HBM data collection and analysis, enabling comparable chemical exposure assessment across Europe [58]. Together, these programs address growing public and scientific concern about EDCs, which are known to interfere with hormonal signaling and have been linked to adverse reproductive, developmental, and metabolic effects even at low exposure levels [59] [21].
Quantitative Insights on Exposure and Health Effects
Large-scale biomonitoring data from these cohorts have revealed widespread exposure to EDCs and provided crucial quantitative insights into exposure levels, demographic patterns, and health associations.
Population Exposure Patterns
Table 1: Detection Frequency of EDCs in Various Populations
| Population Group | Chemical Class | Detection Frequency | Key Metabolites/Compounds | Data Source |
|---|---|---|---|---|
| U.S. reproductive-age women | Parabens | MP/PP: 99%; BP: 46%; EP: 96% | Methyl, propyl, butyl, ethyl paraben | NHANES 2013-2016 [59] |
| U.S. reproductive-age women | Other EDCs | BPA: 94%; BP-3: 96%; TCS: 73% | Bisphenol A, Benzophenone-3, Triclosan | NHANES 2013-2016 [59] |
| Spanish children (5-12 years) | Phthalates | 100% exposed to ≥1 phthalate | Monoethyl phthalate, DEHP metabolites | BIOVAL Program [60] |
| Spanish children (5-12 years) | Bisphenols & Parabens | >75% exposed | BPA, methyl paraben, propyl paraben | BIOVAL Program [60] |
| U.S. preschoolers (2-4 years) | Multiple | 48 chemicals in >50% children | Phthalates, parabens, bisphenols, pesticides | ECHO Cohort [20] |
Table 2: Geometric Mean Concentrations of EDCs in Urine
| Population Group | Chemical | Geometric Mean | Units | Data Source |
|---|---|---|---|---|
| Spanish children | Monoethyl phthalate | 55.0 | ng/mL | BIOVAL [60] |
| Spanish children | DEHP metabolites | 60.6 | ng/mL | BIOVAL [60] |
| Spanish children | Bisphenol A | 0.9 | ng/mL | BIOVAL [60] |
| Spanish children | Methyl paraben | 1.4 | ng/mL | BIOVAL [60] |
| Spanish children | Propyl paraben | 0.39 | ng/mL | BIOVAL [60] |
| Swedish mothers | ΣDEHP metabolites | 38.4 | μg/L | [61] |
| Swedish children | ΣDEHP metabolites | 65.5 | μg/L | [61] |
Analysis of NHANES data reveals that ubiquitous exposure to multiple EDCs is common among U.S. women of reproductive age, with methyl and propyl parabens detected in 99% of urine samples, and benzophenone-3 (BP-3), ethyl paraben (EP), and BPA detected in over 94% of samples [59]. Similarly, European data through HBM4EU shows that phthalate exposure is nearly universal among children, with 100% of studied children in Spain exposed to at least one phthalate compound [60].
Demographic analyses reveal important patterns in exposure levels. Children often exhibit higher exposures to certain phthalates compared to adults, while women show higher levels of parabens and certain phthalates used in personal care products compared to children [61]. Significant disparities in exposure have been observed across racial, ethnic, and socioeconomic groups, with children from racial and ethnic minority groups having higher levels of parabens, several phthalates, and polycyclic aromatic hydrocarbons (PAHs) [20].
Health Risk Associations
Table 3: Association Between EDC Exposure and Health Outcomes
| Health Outcome | Chemical Exposure | Association Measure | Population | Data Source |
|---|---|---|---|---|
| Self-reported infertility | Combined BP-3, BPA, TCS | PR = 1.13, p = 0.007 | U.S. women 18-45y | NHANES [59] |
| Self-reported infertility | Ethyl paraben above detection | PR = 1.57, p = 0.025 | U.S. women 18-45y | NHANES [59] |
| Breast cancer | Triclosan (Q2 vs Q1) | OR = 2.33, p < 0.001 | U.S. women ≥20y | NHANES [25] |
| Breast cancer | Triclosan (Q3 vs Q1) | OR = 1.94, p = 0.006 | U.S. women ≥20y | NHANES [25] |
| Hormone disruption | EDCs in follicular fluid | Altered E2, progesterone | Women undergoing ART | [21] |
Analysis of NHANES data demonstrates that EDC exposures are associated with meaningful health risks. A study of U.S. women aged 18-45 years found that self-reported infertility was significantly associated with a combined exposure score of BP-3, BPA, and triclosan (Prevalence Ratio [PR] = 1.13, p = 0.007) and with ethyl paraben levels above the detection limit (PR = 1.57, p = 0.025) after adjusting for potential confounders [59].
Notably, when assessed individually, triclosan, BP-3, and BPA were not associated with self-reported infertility, highlighting the importance of evaluating mixture effects rather than single chemicals in isolation [59]. This finding is particularly relevant given that real-world exposure invariably involves complex mixtures of chemicals.
Research leveraging NHANES data has also identified significant associations between EDC exposure and breast cancer risk. Analysis of 2005-2014 NHANES data revealed that elevated concentrations of triclosan increased breast cancer risk by 2.33 times (95% CI = 1.45-3.75) in the second quartile and 1.94 times (95% CI = 1.21-3.09) in the third quartile compared to the lowest exposure quartile [25]. This association displayed a nonlinear relationship, with an inverted U-shape curve, and was more pronounced among overweight individuals, those aged <60 years, and White individuals [25].
Methodological Frameworks and Experimental Protocols
The scientific value of NHANES and HBM4EU data stems from their rigorous methodological frameworks and standardized protocols, which enable valid comparisons across populations and time periods.
Study Design and Sampling Protocols
NHANES employs a cross-sectional survey design with a complex, multistage probability sampling methodology to represent the civilian, noninstitutionalized U.S. population [25]. The survey collects data in two-year cycles, allowing for examination of temporal trends. Critical to its utility for EDC research is the inclusion of urinary concentrations of phenols, parabens, and other EDCs in subsamples of participants, along with comprehensive health and demographic data.
HBM4EU has implemented a harmonized approach across European countries, with standardized protocols for data collection, chemical analysis, and statistical aggregation [58]. The initiative developed a standardized data template and R-script for aggregating individual data with consistently calculated statistical measures, enabling meaningful comparisons across diverse European studies conducted between 2005 and 2019 [58]. This harmonization is particularly valuable given that existing HBM studies differ widely in their sample collection methods, time periods, study samples, geographical coverage, analytical methodologies, and quality assurance levels.
Diagram 1: HBM study workflow from sampling to policy
Analytical Methodologies for EDC Quantification
The core laboratory methodologies employed in these programs enable precise quantification of EDCs and their metabolites at low concentrations relevant to population exposures.
NHANES Laboratory Protocol: Urine samples are collected in standard urine collection cups (minimum 5 mL), labeled, and frozen at -20°C until transport to the National Center for Environmental Health for analysis [25]. The analysis employs solid-phase extraction combined with high-performance liquid chromatography and tandem mass spectrometry (HPLC-MS/MS), a highly accurate method sufficient for measuring urinary phenols, parabens, and triclosan in non-occupationally exposed subjects [25]. To account for urine dilution, concentrations are typically creatinine-corrected.
Key parameters for NHANES methods include:
- Lower Limits of Detection (LLODs): Vary by chemical and survey cycle (e.g., for 2013-2014: BPA 0.20 ng/mL, triclosan 1.70 ng/mL, methyl paraben 1.00 ng/mL) [25]
- Quality Control: Includes routine blanks, spikes, and duplicate samples
- Values Below LLOD: Assigned a value of LLOD/√2 as per NHANES protocols
Follicular Fluid Analysis Protocol: Recent research has expanded beyond urine to matrices like follicular fluid, which may better reflect target organ exposure for reproductive health outcomes. A 2025 study by Dou et al. details a sophisticated protocol for analyzing EDCs in follicular fluid [21]:
- Sample Preparation: 200 μL follicular fluid mixed with internal standards and hydrolyzed with β-glucuronidase at 37°C for 180 minutes
- Extraction: Processed through MAX solid-phase extraction cartridges
- Elution: Target compounds eluted using 1 mL of 2% formic acid in methanol
- Separation and Detection: Compounds separated using a Poroshell 120 EC-C18 column and detected by UPLC-MS/MS
- Quality Assurance: Recoveries ranged 63%-109% across compound classes; blank samples used to assess background contamination
This method demonstrates the evolution of HBM techniques toward more complex matrices and lower detection limits to better understand target organ exposure.
Statistical Approaches for Complex Data
Both NHANES and HBM4EU employ specialized statistical methods to address the challenges inherent in HBM data, including complex sampling designs, values below detection limits, and mixture effects.
NHANES Analysis Requirements: Analysis of NHANES data must account for the complex survey design by incorporating stratum and primary sampling unit variables (SDMVSTRA and SDMVPSU) and applying appropriate survey weights according to NHANES analytical guidelines [25]. These weights compensate for unequal selection probabilities and nonresponse, enabling population-representative estimates.
Advanced Mixture Analysis Methods: Recent studies have employed sophisticated statistical approaches to address chemical mixture effects:
- Bayesian Kernel Machine Regression (BKMR): Used to evaluate joint effects of chemical mixtures and identify interactions, generating posterior inclusion probabilities to quantify individual chemical contributions [25] [21]
- Weighted Quantile Sum (WQS) Regression: Identifies potentially important chemicals in a mixture and estimates their relative weights
- Quantile g-computation: A generalized method for estimating mixture effects that does not assume a single direction of effect for all components
These methods represent significant advances beyond traditional multiple regression approaches that may fail to capture complex, non-linear mixture effects.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for EDC Biomonitoring
| Reagent/Material | Application | Function | Example Sources |
|---|---|---|---|
| β-glucuronidase | Sample preparation | Deconjugation of metabolites | Sigma Aldrich [21] |
| MAX solid-phase extraction cartridges | Sample cleanup | Retention and purification of analytes | CNW Technologies [21] |
| HPLC/MS-MS grade solvents | Mobile phase | Chromatographic separation | Various suppliers [21] |
| Isotope-labeled internal standards | Quantification | Correction for recovery and matrix effects | LGC Standards [62] [21] |
| Poroshell 120 EC-C18 column | Separation | UPLC separation of compounds | Agilent [21] |
| Certified reference materials | Quality assurance | Method validation and accuracy control | NIST, LGC Standards [21] |
The analytical core of HBM research relies on specialized reagents and materials that enable precise quantification of EDCs at trace levels in complex biological matrices. Isotope-labeled internal standards are particularly critical for accurate quantification, as they account for matrix effects and variations in extraction efficiency [62] [21]. For bisphenol analysis, these typically include Bisphenol A D14, while for parabens, deuterated analogs like 4-hydroxybenzoic acid-propyl ester D7 are employed.
Solid-phase extraction (SPE) cartridges, particularly mixed-mode anion exchange (MAX) cartridges, are essential for sample cleanup and pre-concentration of analytes from biological matrices [21]. This step is crucial for removing interfering compounds and achieving the low detection limits required for population biomonitoring where exposure levels are typically in the ng/mL range.
Enzymatic deconjugation using β-glucuronidase/sulfatase enzymes is a critical step in quantifying total (free + conjugated) concentrations of EDC metabolites [21]. This hydrolysis step is typically performed at 37°C for several hours to ensure complete cleavage of glucuronide and sulfate conjugates, which often represent the majority of excreted metabolites for many EDCs.
Diagram 2: Analytical workflow for EDC biomonitoring
The NHANES and HBM4EU programs represent paradigm-shifting approaches to understanding population exposure to EDCs and their potential health impacts. Through their harmonized methodologies, comprehensive biomarker panels, and sophisticated statistical approaches, these initiatives have revealed the ubiquitous nature of exposure to bisphenol A, phthalates, parabens, and other EDCs across diverse populations.
The data generated by these programs have provided critical evidence for public health policy, including chemical restrictions and exposure reduction guidelines. As research continues to evolve, focusing on complex mixture effects, sensitive windows of exposure, and vulnerable populations, these large-scale cohorts will remain indispensable resources for linking environmental exposures to human health outcomes and guiding evidence-based public health interventions.
Bridging the Awareness Gap: Strategies for Effective Communication and Exposure Reduction
This whitepaper provides an in-depth analysis of the demographic and socioeconomic disparities in both exposure to and awareness of synthetic endocrine-disrupting chemicals (EDCs), specifically bisphenols, phthalates, and parabens. Within the context of a broader thesis on public awareness, this review synthesizes current scientific evidence to illuminate how race, ethnicity, income, and education levels create unequal burdens of chemical exposure and significant gaps in knowledge among both the public and healthcare professionals. A comprehensive understanding of these disparities is crucial for researchers, scientists, and drug development professionals to accurately assess population risks, design targeted public health interventions, and develop strategies to mitigate exposure among vulnerable subgroups.
Quantitative Disparities in Exposure and Awareness
Empirical data from recent international studies consistently reveal clear demographic and socioeconomic gradients in exposure to EDCs. The tables below summarize key quantitative findings on exposure disparities and awareness gaps.
Table 1: Demographic and Socioeconomic Disparities in EDC Exposure
| Demographic Factor | Chemical Class | Key Finding | Population Studied | Citation |
|---|---|---|---|---|
| Race/Ethnicity | Parabens (MePb, EtPb, PrPb) | ~2 to 3-fold higher concentrations in Non-Hispanic Black participants vs. Non-Hispanic White | Pregnant people in U.S. (ECHO Cohort) | [63] |
| Race/Ethnicity | Dichlorophenols (2,4-DCP, 2,5-DCP) | 2 to 4-fold higher concentrations in Hispanic, Non-Hispanic Black, and Non-Hispanic Other participants | Pregnant people in U.S. (ECHO Cohort) | [63] |
| Socioeconomic Status | Bisphenol A (BPA) | Significantly higher predicted concentrations in the lowest income group, especially with high PCP use | Pregnant women in Taiwan | [64] [24] |
| Infant/Caregiver Status | Parabens (MP, EP, PP) | Urinary paraben levels 355% higher in infants with recent lotion use | 1-3 month-old infants | [65] [66] |
| Caregiver Education | Parabens | Higher exposure in infants whose parents had lower education levels | 1-3 month-old infants | [66] |
Table 2: Disparities in Awareness and Knowledge of EDCs
| Awareness Factor | Study Population | Key Finding | Citation |
|---|---|---|---|
| Overall Knowledge | Turkish Healthcare Professionals | 82.6% classified as having inadequate knowledge (mean score: 3.90/13) | [45] |
| Professional Title | Turkish Healthcare Professionals | Physicians scored highest in knowledge; significant difference by professional title | [45] |
| Prior Awareness | Turkish Healthcare Professionals | Only 23.7% had previously encountered information on bisphenols | [45] |
Detailed Experimental Protocols in Disparity Research
To ensure reproducibility and critical evaluation of the data presented, this section outlines the core methodological approaches used in the cited research on exposure and awareness disparities.
Biomarker-Based Exposure Assessment in Cohort Studies
The assessment of internal chemical exposure via urinary biomonitoring follows a standardized workflow. The following diagram illustrates the primary steps involved in this process, from cohort recruitment to data analysis.
Diagram 1: Urinary Biomonitoring Workflow
Cohort Recruitment and Sampling: Studies such as the Taiwan Maternal and Infant Cohort Study (TMICS) and the U.S.-based ECHO program enroll specific populations (e.g., pregnant women) during routine clinical visits [64] [63]. Participants provide informed consent and complete detailed questionnaires on demographics, lifestyle, and product use. Single or multiple spot urine samples are collected in chemically-free containers and stored at -80°C until analysis.
Laboratory Analysis (Chemical Quantification): Urinary metabolites are quantified using highly sensitive techniques like ultra-performance liquid chromatography coupled with tandem mass spectrometry (UPLC-MS/MS) [67]. Solid-phase extraction is commonly used for sample clean-up and analyte concentration. Methods are validated with strict quality control procedures, including the use of blanks, spikes with internal standards (often isotopically labeled), and reference materials to ensure accuracy and precision [66].
Data Processing and Statistical Analysis: To account for urinary dilution, analyte concentrations are typically corrected for creatinine or specific gravity [63]. Values below the limit of detection (LOD) are imputed (e.g., LOD/√2) [64]. Complex statistical models, including linear mixed-regression models with a censored normal distribution, are employed to handle repeated measures and varying LODs across cohorts [63]. A key step is the stratification of results by socioeconomic and demographic variables to identify disparities.
Cross-Sectional Assessment of Awareness
The evaluation of knowledge gaps, particularly among healthcare professionals, follows a structured survey methodology.
Study Design and Instrument Development: A descriptive, cross-sectional design is used, as seen in the Turkish healthcare worker study [45]. Knowledge assessment questionnaires are developed through a literature review, expert consultation, and content validation by public health academics. The final instrument is pilot-tested for clarity and reliability.
Participant Recruitment and Data Collection: A target sample size is calculated based on power analysis. Participants from relevant professional groups (e.g., physicians, nurses, midwives, health technicians) are recruited via convenience sampling during active work hours. Data is collected through standardized, in-person interviews using a validated questionnaire that covers domains of knowledge, such as sources of exposure, health risks, and protective measures [45].
Data Analysis: Responses are analyzed using statistical software (e.g., SPSS). Descriptive statistics summarize the overall knowledge scores. Inferential statistics, including one-way ANOVA, t-tests, chi-square tests, and correlation analyses, are used to determine significant differences in knowledge levels based on professional title, years of experience, and other demographic factors [45].
The Scientist's Toolkit: Research Reagent Solutions
This section details essential materials and reagents used in the featured research, providing a resource for scientists aiming to replicate or extend these studies.
Table 3: Key Research Reagents and Materials
| Reagent/Material | Function in Research | Specific Examples & Notes |
|---|---|---|
| Certified Reference Standards | Quantification and method calibration | Pure methylparaben, ethylparaben, propylparaben, butylparaben, BPA, and specific phthalate metabolites (e.g., MnBP, MEHP). Isotopically labeled internal standards (e.g., 13C-BPA) are critical for MS-based quantification. |
| LC-MS/MS Grade Solvents | Mobile phase for chromatographic separation | High-purity methanol, acetonitrile, and water to minimize background noise and ion suppression. |
| Solid-Phase Extraction (SPE) Cartridges | Sample clean-up and analyte pre-concentration | Reversed-phase C18 cartridges are commonly used for extracting phenolic EDCs and their metabolites from urine matrix. |
| Creatinine Assay Kits | Urinary dilution correction | Enzymatic or Jaffe method kits. Essential for standardizing urinary biomarker concentrations across spot samples. |
| Validated Questionnaires | Assessing product use frequency and awareness | Standardized questions on rinse-off/leave-on PCP use [64]; 13-item bisphenol knowledge assessment tools [45]. |
Underlying Mechanisms and Pathways
The observed disparities are not random but are driven by a complex interplay of social, commercial, and biological factors. The following diagram maps the logical pathway from root causes to ultimate health outcomes.
Diagram 2: Pathways from Root Causes to Health Outcomes
Systemic and Commercial Drivers: Disparities are propelled by the targeted marketing of specific product types to racial and ethnic minorities. For example, certain personal care products like skin lighteners or hair relaxers, which are marketed heavily to Black communities, have been identified as sources of higher chemical exposures [68]. This is compounded by socioeconomic barriers that limit access to and the affordability of paraben- or phthalate-free alternatives, creating a disproportionate toxic burden for lower-income and minoritized groups [63] [68].
The Amplifying Role of Psychosocial Stress: Research highlights that the effects of chemical exposures can be amplified by non-chemical stressors. In the Atlanta African American Maternal-Child Cohort, the association between a mixture of phthalates/BPA and reduced birthweight became more pronounced when psychosocial stressors (e.g., experiences of discrimination, depression) were included in the exposure model [68]. This suggests that chronic stress may increase biological susceptibility to the adverse effects of EDCs, creating a "double jeopardy" effect.
Biological Plausibility of Long-Term Effects: Animal studies provide mechanistic insights into how low-dose developmental exposure can program long-term health effects. Developmental exposure to BPA in rats leads to extensive sex-specific transcriptome changes in the bone marrow later in life, described as "female masculinization and male feminization," and promotes a metabolic profile overlapping with human metabolic syndrome [69]. Furthermore, longitudinal studies in children link early-life paraben exposure to biological markers like advanced glycation end products (AGEs) and blood pressure, indicating a potential pathway for influencing cardiovascular health from a young age [67].
The evidence synthesized in this whitepaper unequivocally demonstrates that exposure to bisphenols, phthalates, and parabens is not uniformly distributed across populations, nor is the knowledge required to mitigate such exposure. Systemic factors, including race, ethnicity, and socioeconomic status, are major determinants of both exposure burden and awareness. For researchers and public health professionals, these findings underscore the critical need to move beyond population-wide averages and integrate demographic and socioeconomic stratification into risk assessment models. Future efforts must focus on rectifying the imbalance in environmental health literacy, particularly among healthcare providers, and on developing targeted public health strategies that address the root causes of these exposure disparities, ultimately working towards environmental justice in chemical safety.
In response to growing public awareness and conclusive research on the health risks of endocrine-disrupting chemicals (EDCs) such as bisphenol A (BPA) and certain phthalates, regulatory bodies worldwide have implemented significant restrictions. The European Union, for instance, has progressively banned BPA in infant feeding bottles, food containers for young children, and thermal paper receipts [70]. Similarly, in the United States, the Environmental Protection Agency (EPA) has released draft risk evaluations for phthalates like DBP and DEHP, preliminarily determining they present unreasonable risks to human health [71]. This regulatory landscape has pressured manufacturers to seek alternative compounds—notably bisphenol S (BPS), bisphenol F (BPF), and di-isononyl-cyclohexane-1,2-dicarboxylate (DINCH)—to maintain product functionality while achieving "phthalate-free" or "BPA-free" marketing claims. However, within the context of increasing public and scientific scrutiny on environmental chemicals, this whitepaper examines whether these substitutes represent genuinely safer alternatives or merely constitute "regrettable substitutions" that pose similar, or potentially greater, health concerns.
Chemical Profiles and Usage of Common Substitutes
The structural similarities of common substitutes to the original compounds they replace raise immediate concerns about their biological activity.
- BPS (Bisphenol S): A primary replacement for BPA in thermal paper, plastics, and food contact materials, valued for its perceived higher stability [72] [73].
- BPF (Bisphenol F): Used in epoxy resins, coatings, food packaging, and dental sealants, and also occurs naturally in some foods like mustard [70] [72].
- DINCH (Di-isononyl-cyclohexane-1,2-dicarboxylate): A non-phthalate plasticizer designed to replace ortho-phthalates like DEHP in PVC and other flexible plastics, especially in applications close to humans such as medical devices and toys [70] [20].
Human exposure to these compounds is now widespread. A 2025 national study in the U.S. found that preschoolers are routinely exposed to a broad range of potentially harmful chemicals, with emerging substitutes like DINCH showing an upward trend in exposure levels [20]. Furthermore, children often exhibit higher levels of certain substitutes, such as BPS, compared to their mothers, indicating significant early-life exposure during critical developmental windows [20].
Table 1: Detection of Substitute Chemicals in Human Populations and Products
| Chemical | Detection Frequency & Levels | Common Sources of Exposure |
|---|---|---|
| BPS | Detected in urine of 78% of American adults (up to 12.3 ng/mL); found in 79% of tested foods [72] [74] | Thermal paper receipts, canned foods, personal care products, dust |
| BPF | Detected in urine of 55% of American adults (up to 212 ng/mL) [72] | Food packaging, coatings, water pipes, dental sealants, some foods |
| DINCH | Median urinary concentration of 3.1 µg/L in Polish children; showing upward exposure trend in U.S. [70] [20] | PVC plastics, medical devices, toys, food packaging |
Health Impacts and Endocrine Disruption Potential
Endocrine Disruption by Bisphenol Substitutes
A substantial body of evidence indicates that BPS and BPF exhibit endocrine-disrupting properties similar to BPA. A systematic review from 2015 concluded that the hormonal potency of BPS and BPF is in the same order of magnitude and of similar action as BPA (estrogenic, antiestrogenic, androgenic, and antiandrogenic) in both in vitro and in vivo studies [72]. BPS, in particular, has potencies similar to estradiol in membrane-mediated pathways, which are critical for cellular processes like proliferation, differentiation, and death [72].
More recent research has quantified the significant global health burden associated with these substitutes. A 2025 analysis projected that the total global burden of bisphenol-attributable metabolic disease would exceed 127 million cases in 2024, with associated costs projected to surpass $1.1 trillion USD. Notably, while BPA-specific bans in Europe successfully reduced BPA exposure by 33%, they resulted in a 47% increase in BPS levels and a 22% increase in BPF. Consequently, 76% of the bisphenol-related disease burden is now attributed to BPS and BPF [75].
Neurodevelopmental and Behavioral Effects
Emerging research links exposure to these substitutes with behavioral problems in children, with effects often showing sex-specific patterns. A 2025 cross-sectional study of the REPRO_PL cohort in Poland found that childhood exposure to several replacement compounds was associated with adverse effects on school-age children's behavior [70]. Key findings included:
- Among girls, DiBP (a phthalate) was associated with mental health problems, including emotional symptoms, hyperactivity/inattention, and externalizing behaviors.
- BPF was associated with emotional problems and internalizing behavior among boys.
- Exposure to the alternative plasticizer DEHTP was also linked to behavioral issues in boys [70].
These findings are particularly concerning given that early childhood represents a critical window for brain development, and exposures during this period may have lifelong consequences [20].
Metabolic and Reproductive Toxicity
Experimental studies directly comparing the impacts of BPA substitutes have found concerning effects on metabolic and reproductive health:
- A 2025 28-day oral exposure study in male rats comparing BPA, BPF, and BPS found that all three bisphenols shared similarities with the estrogenic positive control (17α-ethinylestradiol), but also presented noticeable differences in their impacts on serum hormone levels and endocrine-responsive tissues. This suggests they may interfere with endocrine functions through slightly different molecular mechanisms [76].
- Academic studies have identified adverse effects of BPS on specific target organs/systems at much lower doses (0.5–10 μg/kg bw/day) than those used in regulatory studies, which are performed in the mg/kg bw/day range. Endpoints affected include male and female reproduction, mammary gland development, neurobehavior, and metabolism/obesity [73].
- Toxicokinetic studies reveal that BPS has a 100-fold higher oral bioavailability compared to BPA in pig models, suggesting that replacement of BPA with BPS may lead to higher internal exposure to the active parent compound [73].
Table 2: Comparison of Health Endpoints for BPA and Its Substitutes
| Health Endpoint | BPA | BPS | BPF | DINCH |
|---|---|---|---|---|
| Estrogenic Activity | Established | Similar potency to BPA | Similar potency to BPA | Considerably less potent |
| Metabolic Effects | Linked to obesity, diabetes | Linked to obesity, diabetes | Linked to obesity, diabetes | Limited data |
| Neurobehavioral Effects | Evidence in humans and animals | Evidence in humans (sex-specific) | Evidence in humans (sex-specific) | Limited human data |
| Reproductive Toxicity | Established concern | Adverse effects at low doses | Adverse effects at low doses | Less potent than phthalates |
| Bioavailability | High | 100x higher than BPA (pig model) | Data still emerging | Data still emerging |
Experimental Evidence and Methodologies
Key Experimental Protocols
Research on the health impacts of chemical substitutes employs rigorous methodological approaches:
HPLC-MS/MS Quantification in Biological Samples:
- Protocol: Urine samples are stored at -80°C after aliquoting. For analysis, 300 µl of urine is transferred into vials, with isotopically-labeled standards and ammonium acetate buffer added. To hydrolyze glucuronide conjugated metabolites, β-glucuronidase from E. coli is used. High-performance liquid chromatography coupled with tandem mass spectrometry (HPLC-MS/MS) is then employed for quantification [70].
- Application: This method was used to quantify BPA, 21 phthalate metabolites, and substitutes including BPF, BPS, DEHTP, and DINCH metabolites in the REPRO_PL cohort study [70].
28-Day Oral Exposure Study in Rodent Models:
- Protocol: In a 2025 study comparing BPA, BPF, and BPS, 8-week-old male Fischer rats were exposed to one of the bisphenols at five different doses, or to 17α-ethinylestradiol (positive control), by gavage for 28 consecutive days. Researchers monitored rat health, dietary intakes, and weight gains, collected 24-hour urine samples, and harvested blood and tissues at terminal necropsy for analysis [76].
- Endpoints Measured: Organ weights and histology, liver enzymatic activities, hematology, clinical chemistry, and serum hormone levels [76].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for Studying Substitute Chemicals
| Reagent/Material | Function in Research | Example Application |
|---|---|---|
| Isotopically-labeled standards | Internal standards for quantification | Correcting for matrix effects in mass spectrometry [70] |
| β-glucuronidase (E. coli K-12) | Enzyme hydrolysis of conjugated metabolites | Releasing free phenols for accurate measurement of total concentrations [70] |
| HPLC-MS/MS systems | High-sensitivity chemical quantification | Detecting low ng/L concentrations of biomarkers in urine [70] |
| Strengths and Difficulties Questionnaire (SDQ) | Behavioral assessment tool | Evaluating emotional symptoms, conduct problems, hyperactivity in children [70] |
| C18 solid-phase extraction cartridges | Sample clean-up and concentration | Isolating analytes from complex urine matrix prior to analysis |
Regulatory and Public Health Implications
The current regulatory framework for EDCs remains fragmented and largely reactive. The European Chemicals Strategy for Sustainability has committed to minimizing and substituting harmful chemicals, particularly in consumer products, but implementation has been slow [77]. The fundamental challenge is that most regulations focus on individual chemicals rather than classes of chemicals with similar properties or structures.
This chemical-by-chemical approach has created a "whack-a-mole" problem where restricting one chemical of concern (e.g., BPA) leads to its replacement with structurally similar analogs (e.g., BPS, BPF) that have not been adequately assessed for safety [72] [75]. As noted in one review, "policy which reduces or removes EDC in manufacturing and processing across multiple sectors, rather than individual behavior change, may have the greatest impact on population exposure" [77].
The disparity between regulatory toxicology studies and academic research further complicates risk assessment. Regulatory studies often follow OECD Test Guidelines and are performed at high dose levels (mg/kg bw/day range), while academic studies investigating specific endocrine-sensitive endpoints frequently find adverse effects at much lower doses (μg/kg bw/day range) [73]. This discrepancy suggests that current regulatory testing protocols may be insufficiently sensitive to detect the endocrine-mediated effects of these chemicals, particularly at environmentally relevant exposure levels.
The scientific evidence compiled in this review indicates that BPS, BPF, and DINCH cannot be considered unequivocally safer alternatives to the chemicals they replace. While DINCH appears to be considerably less potent in its reproductive toxicity compared to ortho-phthalates [70], the bisphenol substitutes BPS and BPF demonstrate endocrine-disrupting properties comparable to, and in some aspects potentially more concerning than, BPA. Their widespread detection in human biomonitoring studies, combined with evidence linking them to metabolic, reproductive, and neurobehavioral effects, underscores the inadequacy of the current substitution-based approach to chemical regulation.
Addressing this problem will require a fundamental shift from current practices:
- Class-Based Regulation: Regulatory frameworks must evolve to evaluate and regulate chemicals based on their structural and functional similarities, rather than proceeding with a chemical-by-chemical approach that facilitates regrettable substitution.
- Advanced Testing Protocols: Pre-market safety assessment should include more sensitive endocrine-disrupting endpoints and non-monotonic dose responses at environmentally relevant exposure levels.
- Green Chemistry Solutions: Ultimately, the development of truly safer alternatives requires investment in green chemistry principles that design chemicals with minimal hazard from the outset, rather than seeking structural analogs with potentially similar biological activities.
For researchers and public health professionals, these findings highlight the critical need to consider the entire class of bisphenols and plasticizers when assessing exposure risks and health impacts, rather than focusing solely on individual chemicals that happen to be subject to current regulatory scrutiny.
Developing Targeted Risk Communication for Vulnerable Groups (e.g., Pregnant Women, Parents)
Bisphenol A (BPA), phthalates, and parabens represent significant public health concerns due to their ubiquitous presence in consumer products and documented associations with adverse health outcomes. Current research confirms that vulnerable groups, including pregnant women, infants, and children, experience disproportionate exposure and increased susceptibility to the effects of these endocrine-disrupting chemicals (EDCs). This whitepaper synthesizes the most recent scientific evidence on exposure sources, health impacts, and biomarker detection methodologies to inform the development of targeted risk communication strategies for these populations. The findings underscore the urgent need for evidence-based communication that translates complex exposure science into actionable guidance for healthcare professionals and at-risk communities.
Quantitative Evidence of Exposure and Health Risks in Vulnerable Groups
Epidemiological studies consistently demonstrate that vulnerability to EDCs is influenced by life stage, with specific windows of development such as in utero, neonatal, and early childhood periods being particularly critical. The data presented below quantify these disparities.
Table 1: Documented Exposure Levels and Health Outcomes in Vulnerable Populations
| Vulnerable Group | Documented Exposure Levels & Disparities | Associated Health Outcomes | Primary Exposure Sources |
|---|---|---|---|
| Pregnant Women | Higher urinary levels of parabens (Methylparaben: 37.8 μg/L) and MEP (43.4 μg/L) compared to their children [61]. Use of fragranced products and cosmetics is a significant predictor of phthalate biomarker levels [78]. | In women undergoing IVF, higher DEHP metabolite mixtures were associated with a 38% lower probability of live birth in earlier study years (2006-2012) [79]. Associations with increased systemic oxidant stress [80]. | Personal care products, cosmetics, fragrances, diet [78] [80]. |
| Children (General Population) | Generally higher levels of certain phthalates than their mothers (ΣDEHP 65.5 μg/L; MnBP 76.9 μg/L) [61]. Exposure is linked to consumption of specific foods like chocolate and ice cream [61]. | Increased oxidant stress (F2-isoprostane), insulin resistance (HOMA-IR), and disturbances in vascular function (decreased brachial artery distensibility) [80]. | Diet, indoor dust, PVC in flooring and wall coverings [61]. |
| Very Low Birth Weight (VLBW) Infants | Estimated Daily Intake (EDI) higher than TDI for multiple chemicals: 100% for BPA, 75% for DEHP, and 25-50% for Propylparaben in the first week of life [81]. EDI is higher in infants with lower gestational age or birth weight [81]. | Hazard Quotient (HQ) >1 indicates increased risk of adverse health effects. Associated with conditions like late-onset septicaemia (LOS) and bronchopulmonary dysplasia (BPD) [81]. | Medical devices (e.g., intravenous tubing), hospital environment [81] [80]. |
| Infants & Young Children via Textiles | BPA detected in 91% of children's socks (up to 3736 ng/g). Ethyl-paraben found in 100% of samples [82]. | Sock extracts demonstrated estrogenic (41% of samples) and anti-androgenic (19%) activity [82]. | Dermal absorption from clothing and textiles [82]. |
Experimental Protocols for Biomarker Assessment
Understanding the methodological backbone of exposure science is crucial for interpreting data and designing future studies. The following section details standard operating procedures for quantifying exposure biomarkers.
Urine Sample Collection and Handling Protocol
Objective: To collect, process, and store urine samples for the analysis of non-persistent EDCs, including phthalate metabolites, phenols, and parabens.
- Sample Collection: Participants provide spot urine samples in sterile polypropylene specimen cups. For studies requiring temporal assessment, first-morning void samples are often collected. To avoid contamination, participants are instructed not to use any wipes prior to sampling [78].
- Specific Gravity Measurement: Urine dilution is measured immediately using a handheld refractometer (e.g., PAL-10S) calibrated with deionized water. Specific Gravity (SG) is used to correct for urinary dilution in subsequent analyses [79].
- Aliquoting and Storage: Urine is aliquoted into cryogenic vials and frozen at -80°C until shipment. Shipments to analytical laboratories are conducted on dry ice to maintain sample integrity [78] [79].
- Quality Control: Blank samples (e.g., deionized water) are processed alongside patient samples to monitor for potential background contamination during handling and analysis.
Chemical Quantification via LC-MS/MS
Objective: To accurately quantify the concentrations of target biomarkers in urine using isotope-dilution tandem mass spectrometry, the gold-standard method.
- Sample Preparation: Enzymatic hydrolysis of glucuronidated/sulfated metabolites is performed using enzymes like β-glucuronidase from E. coli K12 [78]. This step deconjugates the metabolites back to their free forms for accurate measurement.
- Solid Phase Extraction (SPE): An automated online SPE system is used to isolate and concentrate the target analytes from the urine matrix, reducing interference and enhancing sensitivity [78] [79].
- Chromatographic Separation: Analytes are separated using High-Performance Liquid Chromatography (HPLC) with a C18 reverse-phase column. A gradient elution with methanol and water is typically employed [78].
- Mass Spectrometric Detection: Detection is performed using tandem mass spectrometry (MS/MS) in multiple reaction monitoring (MRM) mode. Isotope-labeled internal standards (e.g., 13C- or D4-labeled analogs of each analyte) are added to the samples prior to processing to correct for matrix effects and recovery losses [79].
- Data Processing: Concentrations below the Limit of Detection (LOD) are imputed as LOD/√2 [78] [79]. Metabolite concentrations are adjusted for specific gravity using the formula:
Pc = P[(1.015 – 1)/(SG - 1)], where Pc is the SG-corrected concentration (μg/L) and 1.015 is the mean SG in the study population [79].
Pathway Visualization and Experimental Workflow
The following diagrams map the conceptual pathway from exposure to health outcome and the technical workflow for biomarker assessment, providing a visual tool for understanding the complex relationships and processes.
Diagram 1: Exposure-Health Outcome Pathway
Diagram 2: Biomarker Analysis Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
This table catalogs critical reagents and materials required for conducting robust biomonitoring and toxicological research on BPA, phthalates, and parabens.
Table 2: Key Research Reagent Solutions
| Reagent / Material | Function / Application | Technical Notes |
|---|---|---|
| Isotope-Labeled Internal Standards (e.g., D4-BPA, 13C-Phthalate Metabolites) | Quantification of target analytes via isotope-dilution mass spectrometry, correcting for matrix effects and analyte loss. | Essential for achieving high analytical accuracy and precision. Must be added to samples prior to the extraction step [79]. |
| β-Glucuronidase/Sulfatase Enzymes | Enzymatic deconjugation of phase-II metabolites (glucuronides/sulfates) in urine to free analytes for accurate measurement. | Often sourced from E. coli K12 or Helix pomatia. Incubation time and temperature must be optimized [78]. |
| Certified Reference Materials | Method validation and quality assurance. Used to establish accuracy, precision, and recovery rates of the analytical method. | Available from institutions like NIST (e.g., SRM 3672 - Organic Contaminants in Non-Smoker's Urine) [79]. |
| Solid Phase Extraction (SPE) Cartridges | Clean-up and pre-concentration of target analytes from complex urine matrix, reducing ion suppression in MS. | Automated online SPE systems are commonly used for high-throughput analyses [78] [79]. |
| LC-MS/MS Grade Solvents | Mobile phase preparation for HPLC to ensure minimal background noise, high signal-to-noise ratio, and reproducible chromatography. | Low particulate and high-purity methanol, acetonitrile, and water are required. |
| Polypropylene Labware | Sample collection cups, storage vials, and pipette tips. | Prevents leaching of contaminants and absorption of target analytes. Glass should be avoided for phthalate analysis due to adsorption issues [78] [79]. |
The evidence synthesized in this document highlights critical pathways and disparities in exposure to BPA, phthalates, and parabens. Effective risk communication must be tailored to the specific vulnerabilities and exposure sources of each group. The following strategic recommendations are proposed:
- For Pregnant Women: Messages should focus on reducing use of fragranced personal care products and cosmetics, as these are modifiable sources of phthalates and parabens [78]. Guidance should also include opting for fresh over packaged foods to reduce BPA and DEHP exposure [61] [80].
- For Parents of Infants and Children: Communication should emphasize the choice of clothing and textiles, as studies show these can be a source of BPA and parabens with hormonal activity [82]. Further, dietary advice to limit certain processed foods (e.g., chocolate, ice cream) linked to higher phthalate levels is warranted [61].
- For Healthcare Professionals Serving VLBW Infants: Awareness must be raised about the exceptionally high EDI of these chemicals in the NICU setting. Advocacy for the use of alternative medical devices that are DEHP- and BPA-free is a critical intervention point [81].
- For Researchers: Future studies must continue to investigate the health implications of chemical mixtures and the toxicity of replacement chemicals like BPS and DiNP, which are increasingly common but poorly understood [81] [80]. Integrating biomarker assessment with measures of inflammatory and oxidative stress pathways will further elucidate the mechanisms linking exposure to disease [16] [83] [80].
Endocrine-disrupting chemicals (EDCs) such as bisphenol A (BPA), phthalates, and parabens are ubiquitous in consumer products, leading to widespread human exposure with potential implications for reproductive, developmental, and long-term health [84] [85]. This whitepaper synthesizes current intervention research to provide evidence-based, practical checklists for researchers and public health professionals. Evidence confirms that targeted behavioral interventions, including product substitution and dietary modification, can significantly reduce urinary concentrations of these compounds within days [84] [42]. However, individual action must be coupled with broader policy initiatives to achieve equitable and substantial reductions in exposure population-wide [86].
The pervasive use of EDCs in modern industrial society presents a critical challenge for public health. Phthalates, used as plasticizers and solvents, and phenols/parabens, used in plastics and as preservatives, are encountered daily through diet, personal care products (PCPs), and the built environment [85]. Their status as non-persistent chemicals (with half-lives of approximately 6-12 hours) is counterbalanced by continuous, chronic exposure, making the general population consistently vulnerable [85].
Of particular concern are exposure windows during sensitive periods of the reproductive life cycle, from menarche to menopause in women and after pubertal onset in men [85]. During these windows, EDCs can interfere with hormone action through multiple mechanisms, including receptor binding and epigenetic modifications, potentially leading to adverse reproductive outcomes, metabolic disorders, and other health effects [85]. A 2023 scoping review identified 26 interventions demonstrating that exposure can be actively altered, underscoring the feasibility of personal intervention strategies while also highlighting systemic barriers like product availability and unintentional contamination [84].
Quantitative Evidence for Exposure Reduction
Intervention studies provide quantitative data on the efficacy of exposure reduction strategies. The following tables summarize key findings from dietary and PCP-focused interventions.
Table 1: Efficacy of Dietary Intervention Strategies
| Intervention Strategy | Target Chemical(s) | Reported Reduction in Urinary Biomarkers | Study Duration |
|---|---|---|---|
| Replacement of packaged foods with fresh, organic alternatives [84] | BPA, Phthalates | Significant reductions reported; specific magnitude varies [84] | Several days to weeks |
| Avoidance of canned foods and polycarbonate plastics [84] | BPA | Significant reductions reported [84] | Several days |
Table 2: Efficacy of Personal Care Product (PCP) Intervention Strategies
| Intervention Strategy | Target Chemical(s) | Reported Reduction in Urinary Biomarkers | Study Population |
|---|---|---|---|
| Using phthalate-free PCPs [42] | Diethyl phthalate (DEP), Di-n-butyl phthalate (DBP) | MEP ↓ 27.4%; MnBP ↓ 11% over 3 days [42] | Adolescent girls |
| Selecting fragrance-free products [86] [87] | Diethyl phthalate (DEP) | MEP ↓ >50% (geometric mean 95 ng/mL vs. 276 ng/mL in avoiders vs. non-avoiders) [87] | Black Women |
| Avoiding products with oxybenzone [86] | Benzophenone-3 (BP-3) | Significantly lower BP-3 levels [86] | Latinas |
| Avoiding products with parabens [86] | Methyl and Propyl Paraben | 2-fold lower concentrations [86] | Black Women & Latinas |
Experimental Protocols for Intervention Studies
To validate and build upon the findings summarized above, researchers require robust methodological frameworks. The following outlines a standardized protocol for a PCP replacement intervention study.
Protocol: Short-Term PCP Replacement Trial
Participant Recruitment and Baseline Assessment:
- Cohort: Recruit a defined population (e.g., adults of reproductive age, pregnant women). Obtain informed consent.
- Baseline Biomarker Sampling: Collect first-morning void urine samples for analysis of target metabolites (e.g., MEP, MnBP, methylparaben, propylparaben, BP-3) [42].
- Baseline Product Inventory: Use a smartphone application or structured interview to document all PCPs used by participants in the preceding 24-48 hours. This establishes baseline use patterns [87].
Intervention Phase:
- Product Provision/Guide: Provide participants with a kit of pre-screened PCPs verified to be free of the target chemicals (e.g., free of phthalates, parabens, triclosan, and specified UV filters). Alternatively, provide a detailed guide and resources for procuring such products independently [84] [86].
- Duration: A minimum of 3 days has been shown to be effective for observing significant reductions in urinary metabolites for chemicals with short half-lives [84] [42].
- Compliance Monitoring: Maintain daily contact via text message or phone call. Use a dedicated app for participants to log product use and report any deviations or adverse reactions [87].
Post-Intervention Assessment:
- Endpoint Biomarker Sampling: Collect first-morning void urine samples on the final day of the intervention.
- Exit Interview: Conduct a qualitative assessment of participant experience, perceived barriers, and feasibility of long-term adherence.
Biomarker Analysis:
- Laboratory Methodology: Urine samples are analyzed using high-performance liquid chromatography coupled with tandem mass spectrometry (HPLC-MS/MS). This method is highly accurate for measuring phenol, paraben, and phthalate metabolites in non-occupationally exposed subjects [25].
- Data Correction: Normalize urinary metabolite concentrations for dilution using creatinine values [25].
Diagram 1: PCP replacement trial workflow.
Mechanistic Pathways of Exposure and Intervention
Understanding the biological pathways of EDCs is crucial for contextualizing biomarker data and health outcomes. The following diagram illustrates the pathway from product use to potential health effects and the points of intervention.
Diagram 2: Exposure pathway and intervention points.
The primary molecular mechanisms include endocrine disruption via binding to hormone receptors (e.g., estrogen, androgen, thyroid) and the induction of oxidative stress, which can lead to cellular damage [42] [88]. Phthalates, for example, can disrupt hormonal balance by interfering with the secretion and function of hormones like gonadotropin-releasing hormone (GnRH) and estrogen [42]. The exploration of antioxidant strategies as a mitigating intervention targets this oxidative stress pathway, potentially providing a protective effect at the cellular level [88].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Exposure Assessment Research
| Reagent / Material | Function in Research | Technical Notes |
|---|---|---|
| Certified Reference Standards (e.g., BPA, MEP, MnBP, Methyl Paraben) | Quantification of target analytes in biological matrices via calibration curves. | Essential for ensuring analytical accuracy and precision in HPLC-MS/MS. |
| Solid-Phase Extraction (SPE) Cartridges | Pre-concentration and purification of urinary metabolites prior to analysis. | Reduces matrix effects and improves assay sensitivity and reliability [25]. |
| β-Glucuronidase/Sulfatase Enzymes | Enzymatic deconjugation of phase-II metabolites in urine to free analytes for measurement. | Critical for measuring total metabolite burden, as EDCs are extensively conjugated. |
| Creatinine Assay Kits | Normalization of urinary analyte concentrations for urine dilution. | A mandatory step for accurate data interpretation in spot urine samples [25]. |
| Pre-screened Personal Care Products | Intervention materials verified to be free of target EDCs. | Used as provided replacements in controlled trials to ensure exposure reduction [84] [86]. |
| High-Performance Liquid Chromatography with Tandem Mass Spectrometry (HPLC-MS/MS) | Gold-standard instrumentation for sensitive and specific quantification of EDC metabolites. | Allows for multi-analyte panels from a single sample with low limits of detection (e.g., 0.1-2.3 ng/mL) [25]. |
Practical Checklists for Daily Life
The following checklists translate experimental evidence into actionable guidance for reducing personal exposure.
Checklist 1: Reducing Dietary Exposure
- Prioritize Fresh and Frozen Foods: Choose fresh or frozen produce over canned goods to minimize exposure to BPA and other chemicals from can linings [84].
- Avoid Plastic Food Containers: Do not microwave food in plastic containers or use plastic wrap for hot foods, as heat can increase leaching of phthalates and BPA [84].
- Consume a Balanced Diet Rich in Antioxidants: Increase intake of fruits and vegetables. Emerging research suggests antioxidants may help mitigate the oxidative stress effects induced by phthalate exposure [88].
Checklist 2: Selecting Safer Personal Care Products
- Eliminate Synthetic Fragrance: Choose products labeled "fragrance-free" or those that use essential oils for scent. "Fragrance" is a common hiding spot for phthalates like DEP [86] [87].
- Scrutinize Preservatives: Avoid products containing parabens (methylparaben, propylparaben, etc.) by reading the ingredient list [86].
- Choose Physical Sunscreens: Use sunscreens with zinc oxide or titanium dioxide instead of those containing chemical UV filters like oxybenzone (BP-3) [86].
- Use Resources Wisely: Leverage online databases and tools from reputable research institutions (e.g., Silent Spring Institute) to identify safer products [86].
The evidence is clear: practical, short-term interventions utilizing the provided checklists can effectively reduce individual body burden of EDCs like BPA, phthalates, and parabens. However, the onus for exposure reduction must not rest solely on the consumer. As noted by researchers from the Taking Stock Study, "The burden to protect oneself from risky products should not be on the consumer" [87].
Significant research gaps remain. Future studies should focus on interventions tailored for men during their reproductive years, a currently understudied population [85]. Furthermore, research must move beyond exposure reduction to explicitly link these reductions to improved health outcomes in the long term. Finally, the efficacy of adjunct strategies, such as antioxidant supplementation, requires further validation through clinical trials [88]. Ultimately, empowering individuals with knowledge must be paralleled by robust policy changes that prioritize the removal of harmful chemicals from consumer products, ensuring health equity and comprehensive public health protection [84] [86].
The Role of Healthcare Providers in Educating Patients on EDC Risks
Endocrine-disrupting chemicals (EDCs) represent a class of exogenous substances that can interfere with the normal function of the hormonal system, posing significant threats to human health. Bisphenol A (BPA), phthalates, and parabens are among the most prevalent EDCs in everyday consumer products, leading to widespread and continuous human exposure through ingestion, inhalation, and dermal absorption [89] [90]. The endocrine system is particularly vulnerable during critical developmental windows, such as fetal development and early childhood, rendering these periods of special concern [12]. Healthcare providers occupy a pivotal position at the intersection of scientific research and patient care. This whitepaper details the quantitative evidence of exposure, elucidates the mechanistic pathways of toxicity, and provides a toolkit of experimental protocols, thereby empowering researchers and clinicians to translate emerging data into actionable patient education and improved public health outcomes.
Quantitative Evidence of Exposure and Health Impacts
Robust biomonitoring data is fundamental for healthcare providers to contextualize patient exposure. The following tables summarize key quantitative findings from recent human studies, illustrating the ubiquity of EDCs and their association with adverse health outcomes.
Table 1: Documented Concentrations of EDCs in Human Matrices
| Biological Matrix | Population | EDC Class | Detection Frequency | Median Concentration | Citation |
|---|---|---|---|---|---|
| Hair | 97 Spanish children (4-12 years) | Total Bisphenols | 100% | 311.33 ng/g | [91] [92] |
| Hair | 97 Spanish children (4-12 years) | Total Parabens | 100% | 1904.11 ng/g | [91] [92] |
| Follicular Fluid | 144 women undergoing ART | Phthalate metabolites (mPAEs) | High | 6.14 ng/mL | [21] |
| Follicular Fluid | 144 women undergoing ART | Parabens | High | 2.17 ng/mL | [21] |
| Follicular Fluid | 144 women undergoing ART | Bisphenols | High | 1.33 ng/mL | [21] |
Table 2: Selected Health Outcomes Associated with EDC Exposure in Epidemiological Studies
| Health Outcome | Associated EDC(s) | Study Population | Key Finding | Citation |
|---|---|---|---|---|
| Breast Cancer | Triclosan (TRS) | 4,455 subjects (NHANES) | Elevated TRS concentrations increased risk by 2.33 times (Q2) and 1.94 times (Q3). | [25] |
| Altered Gut Microbiota | Bisphenol S (BPS) | 97 children | BPS was negatively associated with a microbial pathway for methionine metabolism. | [91] [92] |
| Predictive Biomarker | Propylparaben | 97 children | Lachnospiraceae_UCG-001 identified as a predictive genus for exposure. | [91] [92] |
| Impaired Female Reproduction | Phthalates, Bisphenols, Parabens | Women in ART | Co-exposure in follicular fluid associated with altered reproductive hormone levels. | [21] [12] |
Mechanistic Insights: From Molecular Disruption to Clinical Disease
Understanding the mechanisms by which EDCs exert their effects is crucial for explaining health risks to patients and fellow researchers. Bisphenols, phthalates, and parabens can act through multiple, often overlapping, pathways.
A primary mechanism is hormone receptor interaction. BPA, for instance, is a xenoestrogen that can bind to estrogen receptors, acting as an agonist or antagonist and disrupting the normal estrogen-signaling pathway [89]. Similarly, phthalates and parabens have been shown to exhibit estrogenic and anti-androgenic properties, interfering with the feedback mechanisms of the hypothalamic-pituitary-gonadal (HPG) axis [89] [93].
Emerging research highlights the role of neuroinflammation as a novel pathway. EDCs such as phthalates and BPA can cross the blood-brain barrier, potentially causing inflammation in the hypothalamus [93]. This is critically important because the hypothalamus plays a central role in regulating reproduction. Inflammation in these hypothalamic centers can disrupt the release of gonadotropin-releasing hormone (GnRH), leading to downstream dysregulation of the entire reproductive axis [93].
Furthermore, EDCs can influence cellular and metabolic pathways beyond direct receptor binding. For example, dioxins act through the aryl hydrocarbon receptor (AhR), which dysregulates gene expression [89]. Recent evidence also points to EDCs disrupting metabolic functions of the gut microbiota, as seen with BPS's negative association with methionine biosynthesis [91] [92].
The diagram below synthesizes these key mechanistic pathways into a unified visual model.
Figure 1: Multisystem Mechanisms of EDC Toxicity. This diagram illustrates the primary pathways—hormonal disruption, neuroinflammation, and gut microbiome alteration—through which EDCs like BPA, phthalates, and parabens lead to adverse health outcomes.
Analytical Methodologies for EDC Quantification
Accurate measurement of EDCs is a cornerstone of exposure assessment in research. Advanced chromatographic techniques coupled with mass spectrometry are the gold standard. The following workflow details a representative protocol for quantifying EDCs in complex biological matrices like follicular fluid or urine [94] [21].
The process begins with Sample Collection, such as follicular fluid, urine, or hair, followed by Hydrolysis using enzymes like β-glucuronidase to free conjugated metabolites. The next critical step is Extraction and Clean-up, increasingly performed via modern microextraction techniques (e.g., Solid-Phase Extraction - SPE) to isolate and pre-concentrate target analytes from the complex matrix. The extracted samples are then Analyzed typically using Ultra-Performance Liquid Chromatography coupled with tandem Mass Spectrometry (UHPLC-MS/MS), which provides the high sensitivity and selectivity needed to detect low ng/mL concentrations. Finally, Data Analysis is performed using rigorous quality controls and statistical models to ensure reliability.
Figure 2: EDC Analysis Workflow. This chart outlines the key steps in the analytical protocol for quantifying EDCs in biological samples, from collection to data analysis.
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagents for EDC Analysis
| Reagent/Material | Function in Protocol | Specific Example |
|---|---|---|
| β-glucuronidase Enzyme | Hydrolyzes phase-II metabolites (glucuronides) to free the parent EDC for measurement. | From Sigma Aldrich Corp [21]. |
| Solid-Phase Extraction (SPE) Cartridges | Isolate, clean-up, and pre-concentrate target analytes from the complex biological matrix. | MAX SPE cartridges (CNW Technologies) [21]. |
| Chromatography Column | Separates the complex mixture of analytes prior to detection. | Poroshell 120 EC-C18 column (Agilent) [21]. |
| Isotope-Labeled Internal Standards | Correct for matrix effects and losses during sample preparation, ensuring quantification accuracy. | e.g., 13C-labeled BPA, Phthalates [21]. |
| UHPLC-MS/MS System | Provides high-resolution separation (UPLC) and highly sensitive & selective detection (MS/MS). | Ultra-performance liquid chromatography-tandem mass spectrometry [91] [94] [21]. |
The evidence is compelling and unequivocal: chronic exposure to prevalent EDCs like bisphenols, phthalates, and parabens is a significant environmental health risk factor with demonstrable impacts on reproduction, metabolic function, and long-term disease susceptibility. The quantitative data, elucidated mechanisms, and refined analytical protocols detailed in this whitepaper provide a scientific foundation for action. For healthcare providers, this translates to an urgent responsibility to integrate assessment of EDC exposure into patient care and to provide evidence-based guidance on exposure reduction. The research community must continue to advance the field by elucidating the "cocktail effect" of mixed exposures, conducting longitudinal studies to understand chronic impacts, and developing even more sensitive and accessible biomonitoring techniques. Through a concerted effort between researchers, clinicians, and public health officials, we can mitigate the risks posed by these ubiquitous chemicals and safeguard public health.
Validating the Risk: Correlating Exposure with Health Outcomes and Regulatory Landscapes
Endocrine-disrupting chemicals (EDCs) are exogenous substances that interfere with the normal functioning of the endocrine system by mimicking, blocking, or altering the synthesis, transport, metabolism, or elimination of endogenous hormones [12]. The most commonly studied EDCs include bisphenol A (BPA) and its analogs, phthalates, parabens, per- and polyfluoroalkyl substances (PFAS), and persistent organic pollutants (POPs) [12]. These chemicals are pervasive in everyday materials and consumer products, including plastics, food packaging, cosmetics, personal care products, and children's toys, leading to widespread and continuous human exposure through ingestion, inhalation, and dermal absorption [12].
This review synthesizes current epidemiological evidence linking EDC exposure to specific health endpoints, particularly breast cancer and developmental effects. The assessment is framed within the critical context of public awareness and scientific concern regarding bisphenols, phthalates, and parabens. As global regulatory guidelines largely lack updates despite mounting evidence of harmful effects from low-dose exposure, this analysis aims to inform researchers, scientists, and drug development professionals about the urgent need for enhanced biomonitoring, stricter regulations, and further mechanistic studies [95].
Epidemiological Evidence on Breast Cancer
Current Trends and EDC Involvement
Breast cancer remains the most common malignancy among women worldwide, with recent decades witnessing a steady rise in incidence, particularly for estrogen receptor-positive (ER+) phenotypes and early-onset cases occurring in individuals without a family history [96]. While traditional risk factors include genetic mutations, hormonal dynamics, and tissue aging, these elements alone cannot fully account for epidemiological studies showing that each new generation carries a slightly higher risk of breast cancer than the prior one [96].
A growing body of evidence suggests that chronic, cumulative environmental exposures to EDCs profoundly alter breast tissue biology. The continuous exposure to EDCs during highly plastic and susceptible stages of breast development (in utero, post-natal, peri-pubertal, and pubertal) can remodel the breast epigenome, accelerate tissue-specific aging, and impair immunosurveillance, leading to increased cancer development [96]. The geographic distribution of high-incidence early-onset breast cancer regions in the United States shows a striking overlap with states having a legacy of industrial pollution, PFAS contamination, and urban living, further supporting this potential link [96].
Table 1: Epidemiological Evidence Linking EDCs to Breast Cancer
| EDC Class | Specific Chemicals Studied | Key Epidemiological Findings | Study Details |
|---|---|---|---|
| Phthalates | DEHP, BBP, DBP, Di-ethyl phthalate [97] | Significant positive association with breast cancer incidence; higher serum concentrations in women with breast cancer vs. without [97] | Cohort of 102 women; phthalates detected in all participants |
| Persistent EDCs | PCBs, DDT, PBDEs, dioxins [96] | Associated with increased cancer risk; can remain in body for decades despite bans [96] | Lipophilic properties lead to bioaccumulation in breast adipose tissue |
| Non-Persistent EDCs | Phthalates, parabens, bisphenols [96] | Nearly continuous total hormonal load exceeding natural range due to ubiquitous exposure [96] | Measured in blood and urine of nearly all children and adults |
Mechanisms of Carcinogenesis
EDCs contribute to breast carcinogenesis through multiple interconnected mechanisms. As hormone mimics, they can activate estrogen receptor signaling, driving proliferation in hormone-responsive breast tissue [97] [98]. They also promote activation of oncogenic pathways, induction of cancer stemness, and development of therapy resistance [97]. Furthermore, EDCs can cause epigenetic modifications and alter the immune microenvironment, facilitating tumor development and progression [96] [98].
The classification of breast cancer into molecular subtypes (Luminal A, Luminal B, HER2-enriched, and Triple-Negative) is crucial for understanding EDC mechanisms, as these chemicals predominantly influence hormone receptor-positive subtypes through their interaction with estrogen and progesterone signaling pathways [98].
Diagram 1: EDC Mechanisms in Breast Cancer Pathogenesis. EDCs promote breast cancer through multiple interconnected pathways at cellular, molecular, and tissue levels, culminating in increased cancer initiation and progression.
Epidemiological Evidence on Developmental Effects
Early Childhood Exposure and Vulnerabilities
Early childhood represents a critical window of vulnerability for EDC exposure due to rapid brain and body development. A recent national study published in Environmental Science & Technology analyzed urine samples from 201 children aged 2 to 4 years across the United States, finding widespread exposure to potentially harmful chemicals [20] [99]. The study tested for 111 chemicals and detected 96 compounds in at least five children, with 48 chemicals found in over half of the children and 34 chemicals detected in more than 90% of children [20] [99]. Alarmingly, nine of these chemicals are not currently tracked in national health surveys like the National Health and Nutrition Examination Survey (NHANES) [20].
Children are particularly vulnerable to chemical exposure due to frequent hand-to-mouth contact, playing close to the ground, and higher intake rates relative to their smaller body size [20]. These exposures occur through everyday activities such as eating, drinking, breathing indoor and outdoor air, and touching contaminated surfaces [20]. The chemicals identified include phthalates and their alternatives, parabens, bisphenols, benzophenones, pesticides, organophosphate esters (OPEs), polycyclic aromatic hydrocarbons (PAHs), and bactericides [20] [99].
Table 2: Childhood EDC Exposure Patterns and Associated Health Risks
| Exposure Pattern | Chemical Trends | Associated Health Risks | Population Disparities |
|---|---|---|---|
| Widespread Exposure | 96 chemicals detected in toddlers; 34 found in >90% of children [20] [99] | Developmental delays, hormone disruption, impaired immune function [20] | Higher levels in racial/ethnic minority groups for parabens, phthalates, PAHs [20] |
| Changing Trends | Legacy compounds (triclosan, some parabens, PAHs, phthalates) decreasing; replacements (DINCH, neonicotinoids) increasing [20] [99] | Long-term health implications largely unknown for newer replacement chemicals [20] | Firstborn children have lower levels than younger siblings; higher levels in youngest children (age 2) [20] |
| Generational Comparison | Children had higher levels of several chemicals than their mothers during pregnancy [20] | Potential for increased susceptibility to health impacts compared to previous generations [20] | Includes two phthalates, bisphenol S, and pesticide biomarkers [20] |
Long-Term Developmental Consequences
Exposure to EDCs during critical developmental windows has been linked to numerous adverse health outcomes that may manifest across the lifespan. These include impaired nervous system function, learning disabilities, immune system dysfunction, and metabolic issues such as obesity and diabetes [100]. The developing endocrine system is especially sensitive to perturbation, which can lead to permanent changes in physiology and increased disease susceptibility later in life [12].
The concept of "early origins of adult disease" is particularly relevant to EDC exposure, as subtle disruptions during organogenesis and development can program physiological systems for altered function and disease predisposition in adulthood [101]. This is compounded by evidence that children often have higher levels of certain EDCs than their parents, suggesting increasing environmental exposures and potential health burdens for future generations [20].
Research Methodologies and Experimental Approaches
Biomonitoring and Exposure Assessment
Modern epidemiological studies employ sophisticated biomonitoring techniques to assess EDC exposure and internal dose. The analysis of urine samples for chemical biomarkers or their metabolites represents the gold standard for assessing recent exposure to non-persistent EDCs like phthalates and parabens [20] [12]. This approach was utilized in the ECHO Cohort study which examined samples from 201 children across four states [20].
For broader exposure assessment, silicone wristbands have emerged as a passive sampling technology that can detect a wide range of EDCs, including organophosphate esters (OPEs), phthalates, PAHs, brominated flame retardants (BFRs), PCBs, and bisphenols [96]. Studies using this technology have detected hormonally active levels of EDCs in nearly all samples across various chemical classes [96].
Long-term exposure assessment for persistent EDCs (e.g., PCBs, DDT, PBDEs, dioxins) may involve adipose tissue sampling or retrospective exposure modeling, as these lipophilic compounds can accumulate in body fat and remain for years to decades [96].
Study Designs in EDC Epidemiology
Epidemiological research on EDCs utilizes various study designs, each with distinct strengths and limitations:
- Cohort Studies: Longitudinal designs that follow participants over time, assessing exposure levels and health outcomes. The ECHO Cohort represents a prominent example examining early environmental exposures on child health and development [20].
- Case-Control Studies: Compare EDC exposure levels between individuals with a specific health condition (cases) and those without (controls). This design has been frequently used in breast cancer studies [97] [12].
- Cross-Sectional Studies: Assess exposure and outcome at a single time point, providing prevalence data but limited causal inference [12].
A recent systematic review on EDCs and reproductive outcomes included 14 observational studies (6 case-control, 5 cohort, and 3 cross-sectional studies) published between 2014 and 2024, demonstrating the application of these various designs [12].
Diagram 2: EDC Research Workflow. Comprehensive epidemiological assessment of EDCs involves multiple methodological approaches from exposure assessment to health outcome evaluation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for EDC Studies
| Reagent/Material | Function/Application | Examples of Use |
|---|---|---|
| Chromatography-Mass Spectrometry Systems (LC-MS/MS, GC-MS) | Gold standard for precise quantification of EDCs and their metabolites in biological and environmental samples [12] | Measurement of phthalate metabolites, parabens, and bisphenols in urine samples [20] [12] |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | High-throughput screening for specific EDCs or biomarkers in biological samples [12] | Analysis of hormone levels (estradiol, testosterone) as biomarkers of effect [12] |
| Silicone Wristbands | Passive samplers for monitoring personal exposure to multiple EDC classes in real-world settings [96] | Detection of OPEs, phthalates, PAHs, BFRs, PCBs, and bisphenols in community exposure studies [96] |
| Cell-Based Reporter Assays | Assessment of receptor activation (estrogen, androgen, thyroid) by EDCs and their mixtures [96] [98] | Determination of hormonal activity of environmental samples; testing for "cocktail effects" [96] |
| Certified Reference Materials | Quality control and method validation for analytical chemistry measurements [12] | Ensuring accuracy and comparability of EDC measurements across different laboratories and studies [12] |
| DNA Methylation & Epigenetic Analysis Kits | Investigation of epigenetic modifications induced by EDC exposure [96] [98] | Analysis of DNA methylation patterns in genes relevant to breast development and cancer [96] |
Public Health Implications and Future Directions
Risk Assessment and Regulatory Gaps
Current risk assessment paradigms for EDCs face significant challenges, including the non-monotonic dose responses demonstrated by many EDCs, where effects may occur at low doses but not at higher doses [98]. Additionally, the "cocktail effect" of simultaneous exposure to multiple EDCs presents complications for traditional single-chemical risk assessment approaches [12].
Despite mounting evidence of harmful effects from low-dose EDC exposure, most regulatory guidelines have not been updated accordingly [95]. A worldwide risk assessment of phthalates and BPA revealed that while exposure daily intake (EDI) values of phthalates range up to 3,700 µg kg bw⁻¹ d⁻¹ (and up to 5,100 µg kg bw⁻¹ d⁻¹ considering dose-additive effects), many regulations do not reflect these exposure levels or the associated health risks [95]. The hazard quotient (HQ) values for phthalates reach up to 3.66, indicating potential concern, while carcinogenic risk (CR) values for DEHP are notably high [95].
Recommendations for Research and Policy
Based on the current evidence, several key actions are warranted:
Expanded Biomonitoring: Implementation of more comprehensive biomonitoring programs that include emerging EDCs and their replacements, particularly focusing on vulnerable populations like children and pregnant women [20] [99].
Updated Regulatory Guidelines: Revision of safety thresholds and regulatory standards based on the latest evidence of low-dose effects and mixture toxicity [95].
Longitudinal Studies: Initiation of long-term cohort studies following children from gestation through adulthood to better understand the lifelong consequences of early-life EDC exposure [20] [12].
Mechanistic Research: Increased investment in research elucidating the precise molecular mechanisms by which EDCs contribute to disease pathogenesis, particularly through epigenetic modifications and effects on the immune microenvironment [97] [96].
Public Awareness and Product Labeling: Enhancement of public awareness campaigns and clear labeling of products containing EDCs to enable informed consumer choices [20].
The epidemiological evidence linking EDC exposure to specific health endpoints such as breast cancer and developmental effects has substantially strengthened in recent years. The widespread exposure to these chemicals, particularly during critical developmental windows, combined with their potent biological activities at low doses, presents a significant public health concern. Future research must address knowledge gaps regarding chronic low-dose exposure, mixture effects, and the mechanisms underlying EDC-mediated diseases. Simultaneously, regulatory frameworks require urgent updating to reflect the current state of scientific evidence and protect vulnerable populations from these ubiquitous environmental contaminants.
Within the broader context of public awareness of chemical safety, the regulatory approaches to substances like bisphenol A (BPA), phthalates, and parabens reveal fundamental philosophical differences in how societies manage potential health risks. These chemicals, prevalent in food contact materials, cosmetics, and consumer products, have become subjects of intense scientific scrutiny and public concern. Researchers, scientists, and drug development professionals must navigate this complex regulatory landscape, which is characterized by divergent risk assessment methodologies, legal frameworks, and public protection standards. This analysis examines the current regulatory stances of the U.S. Food and Drug Administration (FDA), the European Union, and other international bodies, providing a technical comparison of their scientific approaches, regulatory actions, and the underlying principles guiding their decisions. The evolving nature of these regulations reflects the continuous integration of new scientific evidence into public health policy, highlighting the critical interface between emerging research and regulatory decision-making.
Regulatory Frameworks and Key Agencies
United States Regulatory Framework
In the United States, chemical regulation is characterized by a multi-agency approach with jurisdiction divided by product category. The Food and Drug Administration (FDA) serves as the primary regulator for chemicals in food, food contact substances, drugs, and cosmetics. The FDA's authority derives from the Federal Food, Drug, and Cosmetic Act (FD&C Act), which provides the legal foundation for ensuring product safety. For food contact substances specifically, the FDA employs a pre-market review process through its Food Contact Notification (FCN) program, evaluating potential chemical migration and cumulative dietary exposure [102]. The FDA maintains a dynamic list of chemicals under post-market assessment, recently adding butylated hydroxyanisole (BHA), butylated hydroxytoluene (BHT), azodicarbonamide (ADA), several synthetic color additives, and opiate alkaloids on poppy seeds to its review agenda [103].
The Environmental Protection Agency (EPA) regulates environmental chemicals and pesticides under authorities such as the Toxic Substances Control Act (TSCA), which requires risk evaluation of chemicals in commerce. Recently, the EPA released draft TSCA risk evaluations for phthalates BBP and DIBP, preliminarily determining they "pose unreasonable risk to health and the environment" [104]. The Consumer Product Safety Commission (CPSC) rounds out the primary U.S. regulatory framework by focusing on general consumer products outside the FDA's and EPA's jurisdictions.
European Union Regulatory Framework
The European Union employs a more centralized, precautionary approach to chemical regulation, characterized by comprehensive horizontal legislation. The European Chemicals Agency (ECHA) administers the Registration, Evaluation, Authorisation and Restriction of Chemicals (REACH) regulation, which requires manufacturers to register and demonstrate the safe use of chemicals. For specific product categories, the EU maintains detailed vertical regulations: Regulation (EC) No 1223/2009 for cosmetic products establishes stringent safety requirements, central notification, and serious undesirable effects reporting [105], while various regulations govern food contact materials, including recent bans on BPA [106].
Scientific risk assessment in the EU is primarily conducted by the European Food Safety Authority (EFSA), which provides independent scientific advice to support regulatory decisions. This separation of risk assessment from risk management creates a distinct regulatory dynamic compared to the U.S. model. The EU frequently updates its chemical regulations through commission regulations, recently expanding fragrance allergen labelling requirements and restricting substances in cosmetics based on classification as carcinogenic, mutagenic, or toxic for reproduction [105] [107].
Comparative Analysis of Specific Chemical Regulations
Bisphenol A (BPA) Regulations
Table 1: Comparative Regulatory Stances on Bisphenol A (BPA)
| Region | Regulatory Status | Key Actions & Dates | Scientific Basis | Scope of Restrictions |
|---|---|---|---|---|
| United States | Safety reassessment ongoing | Food Contact Notification program; FDA review initiated July 2023; Food Additive Petition under review (filed May 2022) [108] [102] | FDA's current perspective: "BPA is safe at current levels occurring in foods"; CLARITY Core Study found no clear adverse effects at typical exposure levels [102] | No comprehensive ban; focus on voluntary market phase-outs for certain applications (e.g., BPA in baby bottles) |
| European Union | Comprehensive ban implemented | Commission Regulation (EU) 2024/3190 bans use and trade in FCMs from January 2025; phased implementation through 2028 [106] | 2023 EFSA report concluded current exposure levels pose risk to consumers across all age groups; harmful to reproductive and endocrine systems [106] | Bans BPA, its salts, and derivatives in adhesives, rubbers, plastics, printing inks, varnishes and coatings; limited exceptions (e.g., plastic filtration membranes) [106] |
| Canada | Restricted | Recognized as toxic substance; banned in baby bottles | Assessment of developmental and reproductive toxicity | Specific product category restrictions |
The transatlantic divergence in BPA regulation represents a case study in contrasting risk management philosophies. The U.S. FDA maintains that "BPA is safe at the current levels occurring in foods" based on its ongoing safety assessments, including the extensive CLARITY (Consortium Linking Academic and Regulatory Insights on BPA Toxicity) study, whose principal investigator stated that "BPA did not elicit clear, biologically plausible, adverse effects" at typical consumer exposure levels [102]. The FDA continues to authorize BPA uses in food containers and packaging while conducting post-market assessments.
Conversely, the European Union has implemented a comprehensive ban on BPA in food contact materials effective January 2025, based on EFSA's 2023 conclusion that "current levels of BPA exposure posed a risk to consumers across all age groups" with specific concerns about harm to "reproductive and endocrine systems" [106]. The EU prohibition encompasses BPA, its salts, and other hazardous bisphenols and derivatives across multiple material categories including plastics, varnishes, coatings, and printing inks, with transitional provisions extending through 2028 for certain applications [106].
This regulatory divergence reflects fundamentally different interpretations of the scientific evidence and applications of the precautionary principle. While the EU has prioritized preventive action based on potential endocrine-disrupting effects, the U.S. has maintained that current exposure levels from authorized uses do not pose a demonstrated health risk, highlighting how identical scientific data can yield different regulatory outcomes based on risk tolerance and policy frameworks.
Phthalates Regulations
Table 2: Comparative Regulatory Stances on Phthalates
| Region | Regulatory Status | Key Actions & Dates | Scientific Basis | Specific Restricted Compounds |
|---|---|---|---|---|
| United States | Risk evaluation ongoing | EPA draft TSCA risk evaluations for BBP and DIBP (August 2025); FDA reviewing phthalates as food contact substances [108] [104] | EPA preliminarily found BBP and DIBP pose "unreasonable risk to health and environment"; concerns about reproductive toxicity and endocrine disruption [104] | BBP, DIBP, DEHP, DBP under assessment; focus on conditions of use presenting unreasonable risk |
| European Union | Comprehensive restrictions implemented | REACH regulation restrictions; Plastics Regulation (EU) 10/2011 for FCMs; specific phthalates prohibited in cosmetics [109] [105] | EFSA assessment: may damage fertility, harm unborn children, cause endocrine disruption; classified as reproductive toxicants [109] | DEHP, BBP, DBP, DIBP restricted to 0.1% in consumer articles; DINP, DIDP, DNOP restricted in toys; multiple phthalates banned in cosmetics |
The regulatory approach to phthalates demonstrates both convergence in concern and divergence in implementation between the U.S. and EU. In the United States, the EPA is currently conducting TSCA risk evaluations for butyl benzyl phthalate (BBP) and diisobutyl phthalate (DIBP), with draft evaluations released in August 2025 preliminarily determining these substances "pose unreasonable risk to health and the environment" [104]. The FDA is simultaneously conducting post-market assessments of phthalates as food contact substances, indicating heightened regulatory attention across multiple agencies [108].
The European Union maintains more established and comprehensive restrictions on phthalates through multiple regulatory frameworks. Under REACH, DEHP, DBP, BBP, and DIBP are restricted to a maximum concentration of 0.1% by weight in most consumer articles [109]. The Plastics Regulation (EU) 10/2011 establishes specific migration limits for authorized phthalates in food contact materials, particularly restricting use with fatty foods or foods for infants and young children [109]. Furthermore, the EU Cosmetics Regulation explicitly prohibits multiple phthalates including DBP, DEHP, and DIBP from cosmetic products [109] [105].
The scientific concerns driving regulatory action on both sides of the Atlantic are similar, focusing on reproductive toxicity, endocrine disruption, and potential effects on fertility and fetal development. However, the EU has implemented more sweeping preventative restrictions, while the U.S. is proceeding through chemical-specific risk evaluations that may lead to targeted restrictions on conditions of use determined to present unreasonable risk.
Parabens and Other Chemicals
Table 3: Regulatory Approaches to Other Select Chemicals
| Chemical | U.S. FDA Approach | European Union Approach | Key Regulatory Differences |
|---|---|---|---|
| Parabens | No current ban; considers parabens safe as used in cosmetics; continues to review new data [110] | Multiple parabens prohibited in cosmetics (Regulation (EC) No 1223/2009) [107] | Fundamental difference in precautionary approach; EU prioritizes prevention of potential endocrine disruption |
| PFAS | Market phase-out completed for grease-proofing agents in food contact paper/board (February 2024); research continues on health effects [108] | Comprehensive restriction under REACH; various member state initiatives; EU-wide ban proposed | FDA focused on specific applications; EU pursuing broader regulatory approach |
| FD&C Red No. 3 | Order issued to revoke use in food and ingested drugs (January 2025) based on Delaney Clause [108] | Subject to authorization and labeling requirements | Rare case of similar restrictive action, though based on different legal frameworks |
For parabens, the transatlantic regulatory divergence is particularly striking. The U.S. FDA states it does "not have information showing that parabens as they are used in cosmetics have an effect on human health" and continues to permit their use as preservatives while monitoring emerging science [110]. By contrast, the European Union has prohibited multiple parabens in cosmetics through Regulation (EC) No 1223/2009, reflecting the application of the precautionary principle to potential endocrine-disrupting properties [107].
This pattern of divergent approaches extends to other chemical categories as well. For per- and polyfluoroalkyl substances (PFAS), the FDA has facilitated a market phase-out of specific applications (grease-proofing agents in food contact paper and board) while continuing to research health effects [108]. Meanwhile, the EU is advancing toward more comprehensive PFAS restrictions under REACH. With color additives like FD&C Red No. 3, the U.S. has taken restrictive action based on the Delaney Clause's statutory requirement, demonstrating how specific legal mandates can compel regulatory action even amidst general philosophical differences [108].
Experimental Protocols and Risk Assessment Methodologies
Chemical-Specific Risk Assessment Protocols
The divergent regulatory outcomes for BPA, phthalates, and parabens stem in part from differences in risk assessment methodologies and the interpretation of toxicological data. For BPA, the FDA's CLARITY (Consortium Linking Academic and Regulatory Insights on BPA Toxicity) study represents a comprehensive approach to resolving scientific uncertainties. This multi-year research program combined a core guideline study conducted according to standardized protocols with supplemental investigations from academic institutions. The study design included:
- Chronic toxicity assessment following OECD Test Guidelines 452
- Developmental and reproductive toxicity studies using OECD Guidelines 414, 415, and 421
- Dose-response characterization across multiple life stages
- Systemic exposure quantification through biomonitoring and pharmacokinetic modeling
- Mechanistic studies on potential endocrine activity
The European Food Safety Authority's (EFSA) 2023 assessment that prompted the EU BPA ban employed a different methodological framework, placing greater weight on:
- Low-dose endocrine disruption studies not conducted according to standardized protocols
- Biomarker-based exposure assessment across susceptible populations
- Hazard-based identification of endocrine disrupting properties
- Application of uncertainty factors to address data gaps
For phthalates, the EPA's TSCA risk evaluation process follows a structured framework focusing on conditions of use across the chemical lifecycle. Key methodological elements include:
- Systematic literature review and study quality evaluation
- Hazard identification using established toxicological endpoints
- Exposure assessment across multiple pathways and populations
- Risk characterization integrating hazard and exposure data
- Unreasonable risk determination considering susceptible subpopulations
The EPA's draft risk evaluations for BBP and DIBP specifically seek input on dermal occupational exposure scenarios, inhalation exposure monitoring data, environmental release information, and approaches for estimating chemical migration rates [104].
The Scientist's Toolkit: Essential Research Reagents and Methods
Table 4: Essential Research Materials and Methods for Chemical Safety Assessment
| Research Tool Category | Specific Examples | Function in Safety Assessment | Regulatory Application |
|---|---|---|---|
| Analytical Standards | Deuterated BPA (BPA-d16); (^{13})C-labeled phthalates; Paraben metabolite standards | Quantification of analyte recovery; Method validation; Internal standardization for precise measurement | FDA Total Diet Study; EFSA monitoring data; Compliance testing |
| In Vitro Assay Systems | MCF-7 breast cancer cells (estrogenicity); H295R steroidogenesis assay; Yeast estrogen screen (YES) | Mechanism-based screening for endocrine activity; High-throughput hazard identification | EPA Endocrine Disruptor Screening Program; REACH requirements |
| Animal Models | Sprague-Dawley rats (chronic toxicity); CD-1 mice (developmental studies); Zebrafish (developmental screening) | Traditional hazard identification; Dose-response characterization; Multigenerational effects | OECD guideline studies; CLARITY Core Study; EFSA risk assessment |
| Chromatography Systems | GC-MS/MS for phthalates; LC-MS/MS for BPA and parabens; HPLC with fluorescence detection | Sensitive quantification in complex matrices; Confirmation of chemical identity; Metabolite profiling | FDA food testing; Migration testing for FCMs; Biomonitoring studies |
| Biomarkers of Exposure | BPA glucuronide in urine; Monoethyl phthalate (MEP); p-hydroxybenzoic acid (paraben metabolite) | Internal dose measurement; Aggregate exposure assessment; Trend monitoring | NHANES biomonitoring; HBM4EU program; Exposure modeling validation |
The sophisticated methodologies employed in chemical risk assessment require specialized research tools and analytical approaches. Gas chromatography-tandem mass spectrometry (GC-MS/MS) has emerged as the gold standard for phthalate analysis due to its sensitivity and specificity, particularly important for measuring these ubiquitous contaminants at low concentrations in biological matrices [109]. For BPA and paraben analysis, liquid chromatography-tandem mass spectrometry (LC-MS/MS) provides the necessary sensitivity for detecting these compounds and their metabolites in urine and other biological samples at parts-per-billion levels.
In vitro bioassays have become increasingly important for screening endocrine-disrupting properties, with the MCF-7 cell proliferation assay and yeast estrogen screen serving as well-validated tools for detecting estrogenic activity. These mechanism-based approaches complement traditional toxicological testing by providing insights into potential modes of action at environmentally relevant concentrations.
The selection of appropriate analytical standards is critical for method validation and accurate quantification. Deuterated internal standards for BPA and phthalates correct for matrix effects and analyte recovery variations, ensuring measurement accuracy essential for regulatory decision-making. Certified reference materials further validate analytical methods used in compliance testing and monitoring programs.
The comparative analysis of regulatory stances on BPA, phthalates, and parabens reveals fundamental philosophical differences in how the FDA, EU, and international bodies approach chemical risk management. The United States generally employs a risk-based framework that requires substantial evidence of harm at expected exposure levels before implementing restrictions, while the European Union more frequently applies the precautionary principle, restricting chemicals based on hazard properties and potential risk. These divergent approaches result in markedly different regulatory outcomes for identical substances, creating challenges for global chemical management and product distribution.
For researchers and drug development professionals, understanding these regulatory divergences is essential for designing testing strategies that meet multiple jurisdictional requirements. The ongoing scientific dialogue between regulatory bodies, particularly through initiatives like the FDA's CLARITY study and EFSA's continuing reassessments, provides valuable insights into evolving safety paradigms. As public awareness of chemical exposures grows and scientific methodologies advance, regulatory frameworks will continue to evolve, likely increasing the emphasis on endocrine disruption, cumulative risk assessment, and susceptible population protection. Navigating this complex landscape requires both rigorous scientific investigation and nuanced understanding of the policy contexts that transform toxicological data into public health protection.
The alignment between public perception and scientific evidence regarding the harmfulness of chemicals in consumer products is a critical public health issue. This whitepaper examines three ubiquitous chemical classes—bisphenol A (BPA), phthalates, and parabens—synthesizing current exposure data, mechanistic toxicology, and health outcome studies. Analysis reveals that public concern over these substances is largely validated by emerging scientific evidence, particularly for endocrine-disrupting effects at low exposure levels. Recent biomonitoring studies confirm widespread exposure across populations, including vulnerable subgroups, while mechanistic studies elucidate plausible biological pathways for observed health effects. Regulatory actions are evolving to address these risks, though significant scientific and regulatory challenges remain. This assessment provides researchers and drug development professionals with a technical foundation for understanding exposure risks and developing mitigation strategies.
The pervasive presence of synthetic chemicals in consumer products has generated significant public concern and scientific scrutiny. Bisphenol A (BPA), phthalates, and parabens represent three high-volume production chemicals with demonstrated endocrine-disrupting properties. Understanding the alignment between perceived risks and established toxicological profiles requires systematic evaluation of exposure data, mechanistic studies, and epidemiological evidence.
Table 1: Detection Frequency of Select Chemicals in U.S. Preschoolers (Ages 2-4) [20]
| Chemical Class | Specific Compounds | Detection Frequency |
|---|---|---|
| Phthalates & Alternatives | Multiple metabolites | 48 chemicals found in >50% of children |
| Parabens | Methylparaben, Propylparaben | >90% of children (among 34 frequently detected chemicals) |
| Bisphenols | BPA, BPS | Widespread detection; BPS higher in children than mothers |
| Pesticides | 3-PBA, trans-DCCA | Higher levels in children than mothers |
| Organophosphate Esters (OPEs) | Multiple compounds | Widespread detection |
Recent biomonitoring data reveals concerning exposure patterns, particularly in vulnerable populations. A 2025 national study found that U.S. preschoolers (ages 2-4) are routinely exposed to a broad range of potentially harmful chemicals, with 48 chemicals detected in over half of the children studied [20]. This widespread exposure during critical developmental windows is alarming, as early childhood represents a sensitive period for brain and body development where chemical exposures may have lifelong health consequences.
Global plastic production and chemical use continue to drive environmental contamination and human exposure. Plastics contain over 16,000 chemicals, with potential hazards unknown for more than two-thirds of these substances [111]. The economic impact is substantial, with plastic-related health costs estimated at $1.5 trillion annually [111].
Quantitative Exposure Assessment and Health Benchmarks
Understanding the disconnect between established safety thresholds and observed low-dose effects is fundamental to validating public concern. Traditional toxicological risk assessment has often failed to capture the nuanced effects of endocrine-disrupting chemicals (EDCs), particularly at exposure levels previously considered safe.
Table 2: Comparative Toxicity Thresholds for Bisphenol A [112] [69]
| Reference Point | Dose | Biological Significance |
|---|---|---|
| US-EPA Reference Dose (Historical) | 50 µg/kg/day | Based on high-dose studies from 1980s |
| EFSA Tolerable Daily Intake (2015) | 50 µg/kg/day | Considered safe in 2015 |
| EFSA Temporary TDI (2025) | 4 µg/kg/day | Revised based on new evidence of T-cell effects |
| "Low Dose" Definition | <50 µg/kg/day | Doses below traditional toxicological studies |
| Observed Effects Level | 0.5 µg/kg/day (~8× lower than EFSA TDI) | Extensive transcriptome feminization/masculinization in rats |
The evolution of safety standards for BPA demonstrates how scientific understanding has progressed to validate public concern. The Chapel Hill expert panel consensus statement noted that "adverse effects are occurring in animals within the range of exposure to BPA of the typical human living in a developed country" [112]. This concern is supported by experimental evidence showing effects at doses approximately eight times lower than the recent temporary European Food Safety Authority (EFSA) tolerable daily intake [69].
For parabens, the disconnect between regulation and emerging science is equally notable. While the European Union has prohibited certain parabens like isopropylparaben and isobutylparaben, regulations in the United States and Canada remain less stringent, with no specific laws pertaining to paraben use in cosmetics despite scientific concerns [6]. This regulatory gap persists despite evidence that paraben-free product use can reduce urinary paraben concentrations by at least 43% [39].
Mechanistic Insights: Molecular Pathways and Disruption Mechanisms
Endocrine Disruption Pathways
The primary mechanism of action for BPA, phthalates, and parabens involves interference with endocrine signaling pathways. While initially considered a "weak" estrogen based on its affinity for estrogen receptor alpha, research shows BPA is equipotent with estradiol in its ability to activate responses via estrogen receptors associated with the cell membrane [112]. These receptors mediate rapid physiological responses at low picogram per milliliter concentrations (parts per trillion).
BPA also exhibits multiple modes of endocrine disruption beyond estrogen receptor binding, including:
- Alterations in endogenous hormone synthesis
- Hormone metabolism and blood concentration changes
- Modulation of tissue enzymes and hormone receptors
- Interaction with androgen and thyroid hormone receptor signaling systems [112]
Parabens demonstrate similar endocrine-disrupting capabilities, with mechanistic studies implicating oxidative stress, mitochondrial dysfunction, apoptosis, and inflammation in mediating genotoxic, immunotoxic, and neurotoxic effects [6]. Their chemical structure as esters of p-hydroxybenzoic acid enables interaction with multiple hormonal pathways.
Transcriptomic and Metabolic Consequences
Recent investigations reveal that developmental low-dose BPA exposure produces extensive sex-specific effects on the transcriptome later in life. A 2025 study demonstrated that BPA exposure induces "extensive female masculinization and male feminization of the bone marrow transcriptome" at doses eight times lower than the recent temporary EFSA tolerable daily intake [69]. These molecular changes manifest as a hypometabolic cancer-like state in females and a hypermetabolic autoimmunity-like state in males, with blood metabolic profiles significantly overlapping with human metabolic syndrome.
The Consortium Linking Academic and Regulatory Insights on Toxicity of BPA (CLARITY-BPA) confirmed that lower doses of BPA (2.5–250 µg/kg body weight/day) elicited more significant biological effects compared to higher doses (2500–25,000 µg/kg body weight/day) [69]. This non-monotonic dose response represents a fundamental challenge to traditional toxicological paradigms and validates public concern about low-level environmental exposures.
Experimental Evidence and Methodologies
Key Experimental Protocols
Developmental BPA Exposure Model [69]
- Animal Model: Female Fischer 344 rats, with dosing initiation on gestational day 3.5
- Dosing Regimen: 0 (control), 0.5, or 50 μg BPA/kg body weight per day via drinking water
- Exposure Window: Gestational day 3.5 through lactation until weaning (postnatal day 22)
- Housing Conditions: Polysulfone cages with glass water bottles to minimize background BPA exposure
- Endpoint Analysis: Bone marrow transcriptome analysis and blood metabolic profiling at >48 weeks post-exposure
- Statistical Design: Block design with dose groups evenly distributed across seven temporal blocks
Human Biomonitoring and Health Outcome Assessment [25]
- Study Design: Cross-sectional analysis of NHANES data (2005-2014 cycles)
- Population: 4,455 subjects with complete exposure and outcome data
- Exposure Measurement: Urinary concentrations of phenols (BPA, triclosan, benzophenone-3) and parabens (methyl-, ethyl-, propyl-, butylparaben) via solid-phase extraction with HPLC and tandem mass spectrometry
- Outcome Assessment: Breast cancer diagnosis via Medical Conditions Questionnaire
- Confounder Adjustment: Age, race, poverty income ratio, education, BMI, smoking, drinking, and comorbidities
- Statistical Analysis: Weighted multivariable regression, weighted quantile sum (WQS), and Bayesian Kernel Machine Regression (BKMR) for mixture effects
Research Reagent Solutions Toolkit
Table 3: Essential Research Materials and Methodologies
| Reagent/Method | Function/Application | Technical Specifications |
|---|---|---|
| Solid-Phase Extraction with HPLC-MS/MS | Quantification of urinary phenol and paraben metabolites | LLOD for BPA: 0.2-0.4 ng/mL; Parabens: 0.1-1.0 ng/mL depending on compound [25] |
| Fischer 344/DuCrl Rat Model | Developmental origins of health and disease (DOHaD) studies | Inbred strain with consistent response to endocrine disruption [69] |
| RNA Sequencing Transcriptomics | Unbiased assessment of gene expression changes | Identifies sex-specific feminization/masculinization patterns [69] |
| Extreme Gradient Boosting (XGBoost) Classifier | Machine learning analysis of cognitive impairment risk | Identifies key exposure contributors from multiple variables [113] |
| Bone Marrow Isolation Protocol | Assessment of hematopoietic and metabolic effects | Evaluates long-term programming of bone marrow niche [69] |
| Bayesian Kernel Machine Regression (BKMR) | Mixture effect estimation in epidemiological studies | Accounts for complex correlated exposures [25] |
Regulatory Landscape and Scientific Consensus
The regulatory environment for EDCs is evolving rapidly as scientific evidence accumulates. The U.S. Environmental Protection Agency (EPA) recently released draft risk evaluations for phthalates DBP and DEHP, preliminarily determining that both present unreasonable risks to human health, particularly for workers under certain conditions of use [71]. This represents a significant shift in regulatory posture based on updated risk assessment.
Internationally, the European Union has implemented more restrictive regulations on parabens, prohibiting specific compounds like isopropylparaben, isobutylparaben, phenylparaben, benzylparaben, and pentylparaben, while setting strict limits on others like methylparaben and ethylparaben [6]. This precautionary approach contrasts with the more fragmented regulatory framework in the United States.
The scientific consensus, as exemplified by the Chapel Hill expert panel, acknowledges that "BPA causes a wide range of adverse effects at 'low doses' that are below the US-EPA reference dose in animals" and that "there is evidence from in vitro mechanistic studies that indicates the potential for disruption of human and animal cell function at concentrations of BPA far below unconjugated levels typically found in human blood and tissues" [112]. This consensus has strengthened with recent evidence, validating long-standing public concerns.
The alignment between public perception and scientifically established harmfulness for BPA, phthalates, and parabens is remarkably strong. Scientific evidence confirms that public concerns about these chemicals are valid and supported by robust mechanistic and epidemiological data. Key findings include:
- Widespread human exposure to these chemicals, with detectable levels in >90% of preschoolers for some compounds
- Endocrine-disrupting effects at doses significantly below established safety thresholds
- Long-term health consequences from developmental exposure, including metabolic, reproductive, and immune effects
- Evolving regulatory assessments that increasingly acknowledge previously underestimated risks
For researchers and drug development professionals, these findings highlight the importance of considering endocrine-disrupting chemicals as potential confounding factors in disease etiology and therapeutic development. Future research should prioritize:
- Elucidation of mixture effects and real-world exposure scenarios
- Identification of sensitive developmental windows for chemical exposure
- Development of improved mechanistic biomarkers of effect and susceptibility
- Translation of mechanistic data into refined risk assessment paradigms
The scientific evidence now clearly supports the conclusion that public concern about these chemicals is not misplaced but rather reflects an intuitive understanding of risks that science has subsequently validated through rigorous investigation.
This whitepaper synthesizes current evidence on temporal trends in exposure to synthetic chemicals, focusing on bisphenols and phthalates. Biomonitoring data reveals a significant global shift: while regulatory actions have successfully reduced exposure to legacy compounds like Bisphenol A (BPA) in some regions, this has been paralleled by a rapid increase in exposure to their substitutes, such as Bisphenol S (BPS) and various phthalate replacements. Mounting toxicological evidence indicates that many of these alternatives exhibit similar endocrine-disrupting properties to the chemicals they replace, creating a "regrettable substitution" cycle. This analysis underscores the critical need for updated risk assessment frameworks that account for low-dose effects and mixture exposures, as well as for regulatory approaches that transition from hazard substitution to functional "safe-by-design" strategies.
The widespread use of synthetic chemicals in consumer products has made human exposure to compounds like bisphenols, phthalates, and parabens a significant public health concern. These chemicals are known for their endocrine-disrupting properties, with potential links to reproductive, metabolic, developmental, and neurological disorders [114] [95]. Over the past decade, increasing public awareness and scientific evidence have driven regulatory actions aimed at restricting certain high-volume chemicals like Bisphenol A (BPA) and specific phthalates.
However, these regulatory shifts have triggered substantial market changes, primarily through the substitution of regulated chemicals with structurally similar alternatives. This whitepaper evaluates the temporal trends in human exposure levels in the context of these regulations and market shifts. It frames this analysis within a broader thesis on public awareness, arguing that while scientific research and public concern have successfully driven policy changes, the resulting "regrettable substitutions" highlight critical gaps in chemical regulation and public understanding of cumulative risks.
Global Temporal Trends in Bisphenol Exposure
Quantitative Analysis of Bisphenol Trends
Table 1: Global Temporal Trends in Urinary Bisphenol Concentrations
| Region | Time Period | BPA Trend | BPS Trend | BPF Trend | Key Statistics | Study Source |
|---|---|---|---|---|---|---|
| United States & Canada | 2010-2014 | Significant decrease | Significant increase | Increasing | BPA GM decreased from 2.07 to 0.36 µg/L; BPS detection >70% | [114] |
| Czech Population | 2011-2012 vs. 2019-2020 | Significant decrease | Significant increase | Not dominant | BPA ↓28.6% (adults), ↓47.5% (children); BPS ↑121.1% (adults), ↑90.0% (children) | [115] |
| Eastern & Pacific Asia | 2000-2023 | Non-linear increase | Data limited | Data limited | Positive non-linear association (beta: 0.03 ng/mL/year²) | [116] |
| Middle East & South Asia | 2000-2023 | Non-linear increase | Non-linear increase | Data limited | BPA (beta: 0.13 ng/mL/year²); BPS (beta: 0.29 ng/mL/year²) | [116] |
| European Populations | 2015-2018 | Decreasing | Significant increase | Increasing | 2018 concentrations significantly higher than 2015 for alternatives | [114] |
| Australia | 2012-2017 | Decreasing | Increasing | Data limited | Urinary and wastewater levels show diverging trends | [114] |
A comprehensive meta-analysis of 164 studies published between 2000-2023 revealed complex global patterns in bisphenol exposure [116]. The analysis demonstrated positive non-linear associations between time and BPA concentration internationally (beta: 0.02 ng/mL/year², 95% CI: [0.01, 0.03]), with particularly strong trends in Eastern and Pacific Asia (beta: 0.03 ng/mL/year², 95% CI: [0.02, 0.05]) [116]. These trends highlight the uneven effectiveness of regulatory measures across different geographic and economic contexts.
Data from the Czech population provides one of the most detailed longitudinal views of these shifting exposure patterns. Between 2011-2012 and 2019-2020, BPA concentrations decreased significantly by 28.6% in adults and 47.5% in children [115]. Conversely, BPS concentrations increased dramatically by 121.1% in adults and 90.0% in children during the same period [115]. This inverse relationship provides compelling evidence that regulatory targeting of specific chemicals drives substitution with structural analogues.
Regulatory Framework and Market Response
The regulatory landscape for bisphenols has evolved significantly. The European Union implemented its first ban on BPA in baby bottles through Directive 2011/8/EU in 2011 [114]. More recently, BPA was added to the SVHC list under Regulation (EU) 2024/3190 and completely banned in food-contact materials in 2024 [114]. These regulatory changes have directly influenced market dynamics, with global production and import volumes of BPS in the European Economic Area rising from 1,000-10,000 tons in 2014 to 10,000-100,000 tons by 2023 [114].
The phenomenon of "regrettable substitutions" is now well-documented in the scientific literature. As Yang and Yu (2025) note, "With the restriction of bisphenol A (BPA) in certain consumer products due to its endocrine-disrupting properties, structurally analogous alternatives such as bisphenol S (BPS) and bisphenol F (BPF) have rapidly entered the market" [114]. This shift has led to a wave of substitutions where replacement chemicals may pose comparable or even unforeseen risks.
Phthalate Replacement Dynamics and Exposure Trends
Market Shift to Phthalate Alternatives
The North American phthalate replacements market exemplifies the industrial response to regulatory pressures and consumer demand. This market is experiencing strong growth driven by "growing regulatory pressures and increasing consumer demand for non-toxic, environmentally friendly plasticizers" [117]. Manufacturers across various sectors, including healthcare, automotive, construction, and consumer goods, are transitioning toward compliant and safer formulations [117].
Table 2: Phthalate Replacement Market Dynamics and Key Alternatives
| Market Aspect | Current Status | Projected Trends | Primary Drivers | |
|---|---|---|---|---|
| Overall Market Size | Substantial growth by 2025 | Projected CAGR of ~7.5% (2025-2033); reaching ~$15B by 2025 | Regulatory scrutiny, consumer awareness | [118] |
| Key Replacement Types | DINP, DINCH, bio-based alternatives | Innovation in adipates, trimellitates, terephthalates | Performance parity, toxicological profile | [117] [118] |
| Application Sectors | Flooring, consumer goods, films, cables | Healthcare and medical devices gaining prominence | FDA requirements, safety standards | [117] |
| Regional Adoption | North America and Europe leading | Asia-Pacific emerging as crucial market | Regulatory harmonization, manufacturing volume | [118] |
| Technical Challenges | Higher cost, performance gaps in some applications | Improved performance through advanced polymer science | Cost-performance optimization, green chemistry | [117] |
The most promising phthalate replacements include citrates, adipates, terephthalates, and bio-based plasticizers, with DINP (Diisononyl phthalate) and DINCH (Diisononyl cyclohexane-1,2-dicarboxylate) leading the market in terms of adoption and established safety profiles [118]. DINCH, in particular, has gained traction due to its extensive toxicological evaluation and approval for use in sensitive applications, including children's toys and medical devices [118].
Impact of Regulations on Industry Practices
Regulatory bodies including the U.S. Environmental Protection Agency (EPA), Food and Drug Administration (FDA), and Health Canada have implemented increasingly stringent restrictions on certain phthalates, particularly in products intended for children and food contact applications [119]. These regulations have compelled manufacturers to reformulate products, redesign packaging, and alter supply chains.
The economic impact of these transitions is significant. Compliance costs include substantial investments in research and development of alternative formulations, with many companies heavily investing in "bio-based and non-toxic plasticizer alternatives to expand their portfolios and comply with regulations such as California Proposition 65 and the REACH directive" [117]. Despite these challenges, the regulatory environment has driven innovation, with companies leveraging "machine learning models to predict performance outcomes and toxicological profiles of new phthalate alternatives" to accelerate development cycles [117].
Experimental Methodologies for Exposure Assessment
Biomonitoring Protocols
Human biomonitoring represents the gold standard for assessing temporal trends in chemical exposure. The Czech longitudinal study implemented a robust methodology where "urinary bisphenol metabolite biomarkers (bisphenol A, bisphenol S and bisphenol F) were analyzed in samples from mothers and children in the DEMOCOPHES project (2011-2012), and from children, teenagers, and young adults in the CELSPAC cohorts (2019-2020)" [115]. All samples were analyzed by the same method at the RECETOX Trace analytical laboratory to ensure consistency, with first-morning urine samples collected and creatinine-adjusted concentrations used for comparison [115].
A novel comprehensive approach integrated "7-day time-activity diaries with individualized urinary biomonitoring to capture overlooked BP exposure sources" [2]. This study involved twelve adult participants who meticulously documented their daily activities, including food intake, across seven consecutive days while providing all urine voids for analysis. A total of 401 urine samples were collected and analyzed individually to assess temporal variations and exposure associations [2]. This method successfully identified both well-known sources and previously underexplored exposure routes, including medical plasters, sheer tights, wallpapering, and food preparation with gloves [2].
Analytical Techniques
Advanced analytical methods are critical for accurate exposure assessment. The Brazilian children's study employed "high-performance liquid chromatography coupled to high-resolution mass spectrometry" for urinary BPA quantification, with a detection limit of 0.03 ng/mL [120]. Similar sophisticated methodologies were applied across the cited studies, with quality control measures including creatinine adjustment to account for urine dilution and the use of standardized protocols to enable cross-study comparisons.
Figure 1: Comprehensive Biomonitoring Workflow for Exposure Assessment
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for Bisphenol and Phthalate Analysis
| Research Tool | Function/Application | Technical Specifications | Representative Use |
|---|---|---|---|
| HPLC-MS/MS Systems | Quantitative analysis of urinary biomarkers | High-resolution mass spectrometry; detection limit ~0.03 ng/mL | BPA, BPS, BPF quantification in urine matrices [120] |
| Creatinine Assay Kits | Urine normalization for dilution adjustment | Enzymatic or Jaffe method; standardized protocols | Adjusting urinary bisphenol concentrations for comparative analysis [115] |
| Certified Reference Materials | Quality control and method validation | Matrix-matched materials with certified concentrations | Ensuring analytical accuracy and inter-laboratory comparability [115] |
| BMDS Software | Dose-response modeling and reference dose derivation | Benchmark Dose Software; BMDL calculation | Deriving RfDs for novel bisphenols based on epidemiological data [114] |
| Stable Isotope-Labeled Standards | Internal standards for quantification | ¹³C or deuterium-labeled analogs; recovery correction | Compensating for matrix effects and extraction efficiency in LC-MS [2] |
Toxicological Implications of Alternative Chemicals
Health Risk Assessment of Substitutes
Emerging evidence indicates that many bisphenol and phthalate alternatives exhibit similar toxicological profiles to the chemicals they replace. A critical perspective highlights that "most mainstream BPA alternatives exhibit estrogenic/anti-androgenic activity, metabolic disruption potential, reproductive toxicity, and neurodevelopmental effects similar to those of BPA" [114]. For instance, a recent study derived reference doses (RfDs) of 0.37 and 8.09 ng/kg-bw/day for BPS and BPF, respectively, based on epidemiological evidence of declining male semen quality [114]. These values are orders of magnitude lower than the original BPA RfD of 50 μg/kg-bw/day established by the USEPA in 1988 [114].
The worldwide risk assessment of these chemicals reveals concerning exposure levels. The estimated daily intake (EDI) values of phthalates and BPA reported worldwide range from 1.11 × 10⁻⁷ to 3,700 μg kg bw⁻¹ d⁻¹ and from 3.00 × 10⁻⁵ to 6.56 μg kg bw⁻¹ d⁻¹, respectively [95]. When considering the dose-additive effect of phthalate mixtures, the EDI can increase up to 5,100 μg kg bw⁻¹ d⁻¹, representing a high risk in terms of noncarcinogenic (HQ) and carcinogenic (CR) effects [95].
The Mixture Exposure Challenge
A critical limitation in current risk assessment approaches is their focus on individual chemicals rather than real-world mixture exposures. As noted in recent research, "human exposure typically involves complex mixtures of multiple bisphenol analogues, other EDCs, and environmental stressors" [114]. A study on co-exposure to bisphenols and other EDCs in follicular fluid revealed that these mixtures primarily influence hormone levels through combined effects, with BPS and bisphenol P (BPP) identified as key contributors to adverse effects on reproductive hormones [114].
The interaction between different chemicals further complicates risk assessment. BPS and BPF exhibit synergistic effects when co-exposed with each other, with BPA, or with other environmental factors, contradicting simple dose-additive predictions [114]. These findings demonstrate that current "safe threshold" assessment models, based on single-chemical evaluations, systematically underestimate the combined health risks of mixed exposures.
Figure 2: Regulatory Impact Pathway and Unintended Consequences
The evaluation of temporal trends in exposure to bisphenols, phthalates, and their alternatives reveals a complex narrative of regulatory impact and market adaptation. While targeted restrictions have successfully reduced population-level exposure to specific chemicals like BPA in regulated regions, this success has been tempered by the rapid emergence of substitute chemicals with similar toxicological concerns. The phenomenon of "regrettable substitution" underscores fundamental limitations in current chemical management approaches that focus on individual substances rather than classes of chemicals with similar properties or functions.
Future strategies must embrace a more comprehensive framework that integrates several key elements:
Class-Based Regulation: Moving beyond chemical-by-chemical regulation to group-based assessments that consider shared properties and modes of action [114]
Advanced Screening Methods: Implementing high-throughput in vitro and in silico methods to identify endocrine-disrupting properties early in chemical development [114]
Mixture Risk Assessment: Developing robust methodologies to evaluate cumulative exposure and synergistic effects [95]
Functional "Safe-by-Design" Approach: Shifting from hazard substitution to designing chemicals and materials with inherently safer properties [114]
The continued monitoring of temporal trends through biomonitoring programs remains essential for evaluating the effectiveness of regulatory interventions and identifying emerging exposure concerns. As production volumes of alternative chemicals continue to rise globally, particularly in regions with less stringent regulations, the public health community must maintain vigilance and advocate for science-based policies that truly protect human health across the lifespan.
Endocrine-disrupting chemicals (EDCs) are synthetic compounds that mimic, block, or interfere with hormones in the body's endocrine system, with documented adverse effects on reproduction, neurodevelopment, metabolism, and immune function [121]. The modern environment exposes humans to complex mixtures of EDCs daily, including bisphenols, phthalates, parabens, and other compounds found in food packaging, cosmetics, household products, and water systems [122] [123] [124]. While substantial research exists on the health impacts of individual EDCs, a significant scientific challenge emerges when attempting to assess the combined effects of multiple EDCs—a phenomenon known as "the mixture effect."
The mixture effect problem is particularly complex because EDCs do not follow the classic dose-response principle of toxicology. Their effects are non-monotonic, meaning they may not increase proportionally with dose, and they can exhibit potentiated toxicity when several EDCs are present simultaneously, creating a "cocktail effect" that complicates risk assessment [125]. This technical guide examines the methodological challenges, advanced analytical approaches, and public health implications of assessing combined EDC exposures, with particular focus on bisphenol A (BPA) and phthalates as representative compounds of significant public concern.
Methodological Frameworks for Mixture Analysis
Advanced Statistical Models for Mixture Effects
Researchers have developed sophisticated statistical approaches to disentangle the complex relationships between EDC mixtures and health outcomes. These methodologies move beyond traditional single-chemical risk assessment to capture the reality of combined exposure.
Weighted Quantile Sum (WQS) Regression: This statistical method constructs a weighted index of chemical mixtures to identify the most influential compounds while assessing their overall effect. In a study investigating preserved ratio impaired spirometry (PRISm), a precursor to chronic obstructive pulmonary disease, WQS regression demonstrated that each index rise in the EDC-mixture increased the odds of PRISm by 63% (OR=1.63, 95% CI: 1.25–2.13, P < 0.001) [126].
Quantile g-computation (Qgcomp): This approach estimates the effect of increasing all mixture components simultaneously by one quantile. In the same PRISm study, Qgcomp showed a 41% increase in odds (OR=1.41, 95% CI: 1.15–1.72, P < 0.001) for each quartile increase in the EDC mixture [126].
Bayesian Kernel Machine Regression (BKMR): This flexible modeling technique captures complex exposure-response relationships and interactions between mixture components. BKMR analysis confirmed the overall positive association between EDC mixtures and PRISm prevalence, particularly when all chemical concentrations were at or above their 55th percentile compared to the median [126] [127].
Latent Class Growth Analysis (LCGA): Used in longitudinal studies, this method identifies distinct trajectories of health outcomes over time. A study on preschoolers' hyperactivity used LCGA to classify children into "high hyperactivity trajectory" and "low hyperactivity trajectory" groups, then examined how EDC exposures predicted membership in these groups [127].
Table 1: Statistical Methods for EDC Mixture Analysis
| Method | Key Features | Application Example | Strengths |
|---|---|---|---|
| WQS Regression | Creates weighted index of mixture | PRISm study: OR=1.63 for EDC mixture [126] | Identifies key drivers within mixture |
| Qgcomp | Estimates effect of simultaneous increase in all components | PRISm study: OR=1.41 per quartile increase [126] | Straightforward interpretation of overall mixture effect |
| BKMR | Flexible non-parametric approach | Hyperactivity in preschoolers [127] | Captures complex interactions and non-linearities |
| LCGA | Identifies patterns in longitudinal data | Hyperactivity trajectories over time [127] | Models development of outcomes over time |
Experimental Protocols for Mixture Assessment
Research into EDC mixture effects requires carefully designed protocols that account for real-world exposure scenarios. The following methodologies represent current best practices in the field:
Cohort Study Design for Neurodevelopmental Outcomes: A recent study on EDCs and hyperactivity in preschoolers exemplifies rigorous mixture assessment. The protocol involved recruiting 823 preschoolers, collecting baseline urine samples to measure concentrations of 22 different EDCs, and conducting follow-up assessments every six months. Mothers completed standardized hyperactivity questionnaires at all time points, allowing researchers to track behavioral trajectories in relation to EDC exposure patterns [127].
NHANES-Based Analysis of Pulmonary Effects: Research on PRISm utilized data from 1,363 participants in the National Health and Nutrition Examination Survey (NHANES) 2007-2012 dataset. The protocol included multiple logistic regression to investigate associations between individual EDCs and PRISm, followed by application of three mixture analysis models (WQS, Qgcomp, BKMR) to assess combined effects. Additionally, researchers examined potential mediators including systemic inflammation and uric acid through mediation analysis [126].
Biomonitoring and Exposure Assessment: The European HBM4EU initiative established standardized protocols for measuring EDCs in human populations. This program collected urine samples from 2,756 adults across 11 European countries, analyzing them for BPA and its substitutes (bisphenol S and F). The detection of BPA in 92% of participants demonstrated near-ubiquitous exposure, with levels exceeding the newly established European Safety Authority safety threshold in most cases [122].
Key Scientific Findings on EDC Mixture Effects
Health Impacts Across Biological Systems
Research on EDC mixtures has revealed significant health concerns across multiple organ systems and developmental stages:
Respiratory System Effects: Research has demonstrated that EDC mixtures significantly impact respiratory health. In the PRISm study, the overall mixture effect was primarily attributable to mono-isobutyl phthalate (MIBP), which yielded the largest single-chemical odds ratio in multivariable logistic regression (OR=2.29, 95% CI: 1.71–3.07, P < 0.001). Mediation analysis revealed that systemic inflammation (as measured by the Systemic Immune-Inflammation Index) and uric acid mediated 15.8% and 15.6% of the association between mixed EDCs and PRISm, respectively [126].
Neurodevelopmental and Behavioral Effects: A cohort study of preschoolers found that exposure to EDC mixtures was positively associated with hyperactivity trajectories, with notable gender-specific effects. When all EDCs in the mixture were at or above their 55th percentile compared to the median, a significant positive relationship with high hyperactivity trajectories was observed. Importantly, this association was stronger in girls, highlighting the importance of considering gender specificity in EDC effects [127].
Transgenerational and Epigenetic Effects: EDCs can act through epigenetic mechanisms, including alterations in DNA and/or RNA methylation, histone modifications, chromatin structure, and non-coding RNA functions. These mechanisms facilitate the multigenerational and potentially transgenerational transmission of EDC effects, with consequences that may not manifest until adulthood despite fetal exposure [125].
Cancer and Chemoresistance: BPA exposure has been associated with increased risk of hormone-related cancers (breast, ovarian, prostate, colon) and can induce resistance to various chemotherapeutics including doxorubicin, cisplatin, tamoxifen, and vinblastine. Proposed mechanisms include evasion of apoptosis via downregulation of p53, p21 and BAX; activation of mTOR pathway; increased ERα/ERβ ratio; and upregulation of anti-apoptotic proteins [128].
Table 2: Documented Health Effects of EDC Mixtures
| Health Domain | Key Findings | Principal EDCs Implicated | Potential Mechanisms |
|---|---|---|---|
| Respiratory Health | 63% increased odds of PRISm per EDC mixture index [126] | MIBP, BPA, multiple phthalates | Systemic inflammation, uric acid mediation |
| Neurodevelopment | 2.13x odds of high hyperactivity trajectory [127] | Various EDCs in mixture | Hormone disruption, thyroid interference |
| Cancer Risk & Treatment | Chemoresistance to multiple agents [128] | BPA | Altered apoptosis, receptor signaling pathways |
| Transgenerational Effects | Psychiatric disorders in adulthood from fetal exposure [125] | DES, synthetic estrogens/progestins | Epigenetic modifications |
Public Exposure Levels and Real-World Mixtures
Understanding real-world exposure patterns is crucial for contextualizing experimental findings:
Near-Ubiquitous BPA Exposure: The HBM4EU initiative found BPA in 92% of adult participants from 11 European countries, with 71-100% of participants across countries exceeding the newly established human biomonitoring guidance value of 11.5 ng/L of total urinary BPA [122].
Multiple Exposure Routes: Exposure to EDC mixtures occurs through diverse pathways including diet (the most significant route for BPA, particularly from canned foods), personal care products, household dust, and occupational settings. Cosmetic products contribute significantly to phthalate exposure, with one study finding phthalates, BPA, and triclosan in 88-100% of urine samples tested [123].
Complex Mixture Profiles: Individuals are typically exposed to complex EDC combinations rather than single compounds. Analysis of consumer cosmetic products reveals that individuals using multiple products are exposed to phthalates, parabens, and other EDCs simultaneously, creating unique mixture profiles that vary by product use patterns [123] [124].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for EDC Mixture Studies
| Research Reagent | Function/Application | Example Use |
|---|---|---|
| LC-MS/MS Systems | Quantification of EDCs in biological samples | Measuring BPA, phthalate metabolites in urine [126] |
| ELISA Kits | Biomarker analysis | Measuring inflammatory mediators, uric acid in mediation studies [126] |
| Standardized Urine Collection Kits | Biomonitoring sample integrity | HBM4EU biomonitoring initiative [122] |
| Cell Culture Models (H295R) | Steroidogenesis assessment | Evaluating effects on adrenocortical function [129] |
| Laccase/Peroxidase Enzymes | Biodegradation studies | BPA removal in wastewater treatment systems [129] |
| Behavioral Assessment Tools | Neurodevelopmental outcome measures | Hyperactivity questionnaires in preschool cohort [127] |
Visualizing Experimental Workflows and Biological Pathways
EDC Mixture Analysis Workflow
The following diagram illustrates a comprehensive workflow for assessing EDC mixture effects in epidemiological studies, from participant recruitment through data analysis and interpretation:
EDC Mechanisms and Signaling Pathways
This diagram outlines the key molecular mechanisms through which EDCs like BPA exert their effects, including receptor interactions and downstream signaling pathways:
The assessment of mixture effects represents both a formidable challenge and an essential evolution in environmental health science. Traditional single-chemical risk assessment paradigms are inadequate for protecting public health given the demonstrated mixture effects observed at real-world exposure levels. The scientific evidence clearly indicates that EDC mixtures can produce adverse health outcomes even when individual components are present at seemingly safe levels.
Future research priorities should include:
- Development of standardized mixture testing protocols that reflect real-world exposure scenarios
- Enhanced understanding of the epigenetic mechanisms underlying EDC effects
- Longitudinal studies tracking health outcomes across the lifespan following early-life exposures
- Refined statistical approaches that can handle the complex interactions in high-dimensional mixture data
Regulatory frameworks must evolve to address the mixture effect, moving beyond single-chemical risk assessment toward cumulative impact evaluation that acknowledges the reality of simultaneous exposure to multiple EDCs. This paradigm shift is essential for meaningful public health protection in the context of modern environmental chemical exposures.
Conclusion
Synthesis of the evidence reveals a critical disconnect: while human biomonitoring confirms widespread and often concerning exposure to bisphenols, phthalates, and parabens across populations, significant gaps persist in public awareness, particularly regarding newer substitutes and specific health risks. For researchers and drug development professionals, this underscores the necessity of integrating robust HBM data with sophisticated social science methodologies to accurately assess and address public perception. Future efforts must prioritize the development of clear, targeted communication strategies to translate scientific evidence into actionable public knowledge. Furthermore, biomedical research must urgently address the challenges posed by chemical mixtures and the safety of emerging alternatives. Closing this awareness gap is not merely an educational imperative but a foundational step for informing effective regulatory policies, guiding the development of safer products, and ultimately mitigating the public health burden of endocrine-disrupting chemicals.
References
- 1. Assessment of bisphenol A analogues in water and sediment ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra04861c?page=search]
- 2. Exploring overlooked bisphenol exposure sources through ... [https://www.sciencedirect.com/science/article/pii/S0147651325009376]
- 3. A narrative review of phthalates: From environmental ... [https://www.sciencedirect.com/science/article/abs/pii/S0269749125007535]
- 4. Occurrence, fate and ecological risks of phthalate esters ... [https://www.nature.com/articles/s41598-025-25697-8]
- 5. Common household plastics linked to thousands of global... | CNN [https://www.cnn.com/2025/04/29/health/phthalates-heart-disease-wellness]
- 6. Ecotoxicological impacts of parabens on flora and fauna [https://www.nature.com/articles/s44454-025-00012-2]
- 7. Parabens as the double-edged sword [https://www.sciencedirect.com/science/article/abs/pii/S0048969724067032]
- 8. Occurrence and Exposure Assessment of Antibiotics, ... [https://pubmed.ncbi.nlm.nih.gov/40674573/]
- 9. Trend analysis of environmental concentrations ... [https://www.sciencedirect.com/science/article/pii/S0013935125011971]
- 10. Bisphenol A exposure and its impact on childhood obesity [https://pubmed.ncbi.nlm.nih.gov/40884426/]
- 11. Phthalates and Their Impacts on Human Health - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8157593/]
- 12. Associations Between Endocrine-Disrupting Chemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299029/]
- 13. Exposure Assessment Tools by Routes - Dermal [https://www.epa.gov/expobox/exposure-assessment-tools-routes-dermal]
- 14. Phthalates, bisphenols, parabens, and triclocarban in ... [https://www.sciencedirect.com/science/article/pii/S0160412019333859]
- 15. 7.4 Routes of Chemical Entry - Cornell EHS [https://ehs.cornell.edu/book/export/html/1381]
- 16. Human Exposure to Bisphenols, Parabens, and ... [https://www.mdpi.com/1422-0067/24/8/7325]
- 17. Metabolic effects of paraben exposure in geriatric serum ... [https://www.sciencedirect.com/science/article/pii/S0160412025006531]
- 18. Bisphenol A and phthalate metabolite urinary concentrations [https://www.nature.com/articles/jes201465]
- 19. Mixtures of Urinary Phenol and Phthalate Metabolite ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11359712/]
- 20. New study: U.S. preschoolers exposed to broad range of ... [https://health.ucdavis.edu/news/headlines/new-study-us-preschoolers-exposed-to-broad-range-of-potentially-harmful-chemicals/2025/07]
- 21. Co-exposure of phthalates, bisphenols, parabens, and ... [https://www.oaepublish.com/articles/jeea.2025.07]
- 22. Its Pervasive Presence and Impact on Reproductive Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC12206273/]
- 23. Parabens, bisphenols, and other environmental phenols ... [https://www.sciencedirect.com/science/article/abs/pii/S0013935125012903]
- 24. Socioeconomic status in the association between use of ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1537669/full]
- 25. Associations between phenol and paraben exposure ... [https://www.nature.com/articles/s41598-025-88765-z]
- 26. Parabens, bisphenols, and other environmental phenols ... [https://pubmed.ncbi.nlm.nih.gov/40451416/]
- 27. Associations of phenols, parabens, and phthalate ... [https://www.sciencedirect.com/science/article/pii/S0160412025005471]
- 28. Endocrine Disruptors [https://www.niehs.nih.gov/health/topics/agents/endocrine]
- 29. Endocrine-Disrupting Chemicals [https://www.endocrine.org/advocacy/priorities-and-positions/edc]
- 30. Quantifying the metabolic health burden of increased BPA ... [https://www.sciencedirect.com/science/article/pii/S0048969725025379]
- 31. Synergistic endocrine disruption and cellular toxicity of ... [https://www.nature.com/articles/s41598-025-94902-5]
- 32. A network toxicology approach to decipher paraben-induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12165941/]
- 33. Associations between phthalate metabolites and two novel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12024508/]
- 34. Analysis of Women's Knowledge, Health Risk Perceptions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12116110/]
- 35. Awareness and Knowledge of Endocrine-Disrupting ... [https://www.mdpi.com/2305-6304/12/12/890]
- 36. A Social Survey to Capture the Public Awareness and ... [https://www.mdpi.com/2076-3298/12/11/410]
- 37. What do people need to know about endocrine disrupting ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-025-25561-4]
- 38. Consumer behavior and exposure to parabens, bisphenols ... [https://www.sciencedirect.com/science/article/pii/S1438463920305708]
- 39. Risk perception of personal care products: A scoping review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623616/]
- 40. Human biomonitoring and environmental health: a critical ... [https://pubmed.ncbi.nlm.nih.gov/40635229/]
- 41. Biomarkers, matrices and analytical methods targeting ... [https://www.sciencedirect.com/science/article/pii/S0160412020320377]
- 42. Exposure risks to phthalates by cosmetics and personal ... [https://www.sciencedirect.com/science/article/abs/pii/S0009279725004168]
- 43. Analytical human biomonitoring method for the ... [https://pubmed.ncbi.nlm.nih.gov/30927662/]
- 44. References for Biomonitoring Analytical Methods | NER [https://www.cdc.gov/environmental-exposure-report/php/resources/references-for-biomonitoring-analytical-methods.html]
- 45. Assessment of bisphenol-related knowledge and awareness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463856/]
- 46. What Is a Likert Scale? | Guide & Examples [https://www.scribbr.com/methodology/likert-scale/]
- 47. Likert Scale Questionnaire: Examples & Analysis [https://www.simplypsychology.org/likert-scale.html]
- 48. Likert Scales: Definition & Questions [https://www.surveymonkey.com/mp/likert-scale/]
- 49. Analyzing and Interpreting Data From Likert-Type Scales - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3886444/]
- 50. Awareness and Knowledge of Endocrine-Disrupting ... [https://pubmed.ncbi.nlm.nih.gov/39771105/]
- 51. The associations between personal care products use and ... [https://www.sciencedirect.com/science/article/pii/S0048969720341620]
- 52. Exposure to Phenols, Phthalates, and Parabens and ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2021.620769/full]
- 53. Analysis of Paraben and Bisphenol A Exposure in Relation ... [https://pubmed.ncbi.nlm.nih.gov/41164939/]
- 54. The impact of perfumes and cosmetic products on human health [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425936/]
- 55. Urinary levels of parabens, phthalate metabolites ... [https://www.sciencedirect.com/science/article/abs/pii/S0013935122011793]
- 56. Associations Between Daily-Use Products and Urinary ... [https://www.mdpi.com/1660-4601/22/1/99]
- 57. Urinary levels of parabens, phthalate metabolites ... [https://pubmed.ncbi.nlm.nih.gov/35820649/]
- 58. Exposure to Phthalates in European Children, Adolescents ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10057641/]
- 59. Exposure of U.S. population to endocrine disruptive ... [https://www.sciencedirect.com/science/article/abs/pii/S026974912030717X]
- 60. Biomonitoring of Phthalates, Bisphenols and Parabens in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8431397/]
- 61. Exposure determinants of phthalates, parabens, bisphenol ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4207945/]
- 62. Evaluation of EDCs (phthalates, bisphenols, parabens, and ... [https://www.sciencedirect.com/science/article/abs/pii/S0308814625037173]
- 63. Racial and ethnic differences in prenatal exposure to ... [https://www.nature.com/articles/s41370-025-00750-w]
- 64. Socioeconomic status in the association between use of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12019293/]
- 65. Infants are exposed to higher levels of parabens via lotions ... [https://www.ehn.org/baby-parabens-exposure]
- 66. Young infants' exposure to parabens: lotion use as a ... [https://pubmed.ncbi.nlm.nih.gov/39955433/]
- 67. Urinary parabens, advanced glycation end products and ... [https://www.sciencedirect.com/science/article/pii/S001393512501480X]
- 68. Exposure to phthalate metabolites, bisphenol A, and ... [https://www.sciencedirect.com/science/article/abs/pii/S0013935123012689]
- 69. Developmental low-dose bisphenol A exposure leads to ... [https://www.nature.com/articles/s43856-025-01119-8]
- 70. Impact of plastic-related chemicals on emotional and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523086/]
- 71. EPA Releases Draft TSCA Risk Evaluations for Phthalates ... [https://www.epa.gov/chemicals-under-tsca/epa-releases-draft-tsca-risk-evaluations-phthalates-dbp-and-dehp-public]
- 72. Bisphenol S and F: A Systematic Review and Comparison of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4492270/]
- 73. Regulatory and academic studies to derive reference ... [https://www.sciencedirect.com/science/article/abs/pii/S0013935121015346]
- 74. The Plastic Chemicals Hiding in Your Food [https://www.consumerreports.org/health/food-contaminants/the-plastic-chemicals-hiding-in-your-food-a7358224781/]
- 75. Quantifying the metabolic health burden of increased BPA ... [https://pubmed.ncbi.nlm.nih.gov/41232288/]
- 76. Direct Comparison of the Impacts of Bisphenol A, ... [https://pubmed.ncbi.nlm.nih.gov/40966161/]
- 77. Interventions to Reduce Exposure to Synthetic Phenols ... [https://link.springer.com/article/10.1007/s40572-023-00394-8]
- 78. Personal care product use patterns in association with ... [https://www.nature.com/articles/s41370-023-00627-w]
- 79. Urinary concentrations of bisphenol A, parabens and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6469504/]
- 80. Exposure to Bisphenols and Phthalates and Association with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5618435/]
- 81. Estimated daily intake of phthalates, parabens, and ... [https://www.sciencedirect.com/science/article/pii/S0045653522031800]
- 82. Concentrations of bisphenol A and parabens in socks for ... [https://www.sciencedirect.com/science/article/pii/S0160412019307287]
- 83. Associations between phenols, parabens, and phthalates ... [https://www.sciencedirect.com/science/article/pii/S0147651324012673]
- 84. Interventions to Reduce Exposure to Synthetic Phenols ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10300154/]
- 85. Lifestyle interventions to reduce endocrine-disrupting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9890927/]
- 86. Choosing safer personal care products can lower ... [https://silentspring.org/news/choosing-safer-personal-care-products-can-lower-exposures-risky-chemicals]
- 87. Ingredient-aware product choices linked to reduced ... [https://www.contemporaryobgyn.net/view/ingredient-aware-product-choices-linked-to-reduced-chemical-exposure]
- 88. Preventive antioxidant strategies to reduce the effects of ... [https://link.springer.com/article/10.1007/s44274-025-00257-z]
- 89. Role of personal care products as endocrine disruptors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289576/]
- 90. Endocrine disruptors: Unravelling the link between ... [https://www.sciencedirect.com/science/article/abs/pii/S0013935123021898]
- 91. Associations between chronic exposure to bisphenols and ... [https://pubmed.ncbi.nlm.nih.gov/40849015/]
- 92. Associations between chronic exposure to bisphenols and ... [https://www.sciencedirect.com/science/article/pii/S001393512501895X]
- 93. Endocrine-Disrupting Chemicals, Hypothalamic ... [https://www.mdpi.com/1422-0067/25/21/11344]
- 94. Endocrine disruptors in personal care products and ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25011233]
- 95. Worldwide risk assessment of phthalates and bisphenol A ... [https://www.sciencedirect.com/science/article/pii/S0160412023005676]
- 96. the rapid rise of hormone-sensitive and early-onset breast ... [https://www.nature.com/articles/s41523-025-00840-w]
- 97. How phthalates promote breast carcinogenesis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466654/]
- 98. Endocrine Disruptors and Breast Cancer [https://www.mdpi.com/2227-9059/13/11/2774]
- 99. Researchers tested 200 toddlers — 96 chemicals were ... [https://www.sciencedaily.com/releases/2025/07/250701234739.htm]
- 100. - Endocrine Chemicals (EDCs) | Disrupting Society Endocrine [https://www.endocrine.org/patient-engagement/endocrine-library/edcs]
- 101. Human endocrine : an updated review of toxicological... disruption [https://link.springer.com/article/10.1007/s13530-025-00264-w]
- 102. Government Regulation and Research on Safe Use of BPA ... [https://www.americanchemistry.com/chemistry-in-america/news-trends/blog-post/2025/government-regulation-and-research-on-safe-use-of-bpa-in-food-and-packaging]
- 103. FDA Update on Post-market Assessment of Chemicals in ... [https://www.fda.gov/food/hfp-constituent-updates/fda-update-post-market-assessment-chemicals-food-supply-0]
- 104. EPA Releases Draft TSCA Risk Evaluations for Phthalates ... [https://www.lawbc.com/epa-releases-draft-tsca-risk-evaluations-for-phthalates-bbp-and-dibp-for-public-comment/]
- 105. Legislation - Internal Market, Industry, Entrepreneurship and ... [https://single-market-economy.ec.europa.eu/sectors/cosmetics/legislation_en]
- 106. EU prohibition on the use and trade of Bisphenol A from 20 ... [https://trade.ec.europa.eu/access-to-markets/en/news/eu-prohibition-use-and-trade-bisphenol-20-january-2025]
- 107. Cosmetic Regulations 2025: What's Changing in the EU ... [https://www.gcrs.co.uk/cosmetic-regulations-2025/]
- 108. List of Select Chemicals in the Food Supply Under ... [https://www.fda.gov/food/food-chemical-safety/list-select-chemicals-food-supply-under-fda-review]
- 109. Phthalates Testing according to EU Regulations [https://measurlabs.com/blog/phthalates-testing-by-eu-regulations/]
- 110. Parabens in Cosmetics [https://www.fda.gov/cosmetics/cosmetic-ingredients/parabens-cosmetics]
- 111. New report calls plastics a “grave” danger to health as ... [https://www.thenewlede.org/2025/08/lancet-plastic-health-impacts-global-treaty-geneva/]
- 112. Chapel Hill bisphenol A expert panel consensus statement [https://pmc.ncbi.nlm.nih.gov/articles/PMC2967230/]
- 113. Exposure to bisphenol A and its analogs provides ... [https://www.sciencedirect.com/science/article/pii/S2405665025000083]
- 114. A health conundrum of bisphenol A and its alternatives [https://www.oaepublish.com/articles/jeea.2025.39]
- 115. Temporal patterns of bisphenol exposure in the Czech ... [https://enveurope.springeropen.com/articles/10.1186/s12302-025-01244-0]
- 116. Temporal and geographic variability of bisphenol levels in ... [https://www.sciencedirect.com/science/article/pii/S0013935124022485]
- 117. North America Phthalate Replacements Market Forecast ... [https://www.linkedin.com/pulse/north-america-phthalate-replacements-market-forecast-l0xaf/]
- 118. Phthalate Replacements Dynamics and Forecasts: 2025- ... [https://www.datainsightsmarket.com/reports/phthalate-replacements-1134858]
- 119. North America Phthalates and Bisphenol A Market ... [https://www.linkedin.com/pulse/north-america-phthalates-bisphenol-market-size-wtapf]
- 120. Exposure of elementary school-aged Brazilian children to ... [https://www.nature.com/articles/s41598-024-67267-4]
- 121. Endocrine-Disrupting Chemicals [https://www.endocrine.org/topics/edc]
- 122. Human exposure to Bisphenol A in Europe | Publications [https://www.eea.europa.eu/en/analysis/publications/human-exposure-to-bisphenol-a]
- 123. The dark side of beauty: an in-depth analysis of the health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11381309/]
- 124. Phthalates in Cosmetics [https://www.fda.gov/cosmetics/cosmetic-ingredients/phthalates-cosmetics]
- 125. Effects of Endocrine-Disrupting Chemicals in the Brain [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565183/]
- 126. Potential effects of endocrine-disrupting chemicals on ... [https://www.sciencedirect.com/science/article/pii/S0147651325010462]
- 127. Effects of single and multiple endocrine-disrupting ... [https://www.sciencedirect.com/science/article/pii/S0160412025005768]
- 128. The Endocrine Disruptor Bisphenol A (BPA) Exerts a Wide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6864600/]
- 129. Endocrine disrupting effects of bisphenol A exposure and ... [https://www.sciencedirect.com/science/article/pii/S2468227619306969]