Advancing Reproductive Health: Behavioral Strategies for Endocrine-Disrupting Chemical Avoidance and Intervention
This article synthesizes current scientific evidence and methodological approaches for understanding and promoting reproductive health behaviors aimed at reducing exposure to endocrine-disrupting chemicals (EDCs).
Advancing Reproductive Health: Behavioral Strategies for Endocrine-Disrupting Chemical Avoidance and Intervention
Abstract
This article synthesizes current scientific evidence and methodological approaches for understanding and promoting reproductive health behaviors aimed at reducing exposure to endocrine-disrupting chemicals (EDCs). Targeting researchers, scientists, and drug development professionals, it explores the mechanistic foundations of EDC effects on reproductive systems, evaluates validated assessment tools and behavioral intervention strategies, addresses implementation challenges and knowledge gaps, and examines comparative effectiveness of different intervention models. The review emphasizes the critical importance of evidence-based behavioral interventions alongside pharmaceutical and regulatory approaches for protecting reproductive health across the lifespan.
Understanding the Threat: EDC Mechanisms and Reproductive Health Consequences
Environmental endocrine-disrupting chemicals (EDCs) represent a broad class of synthetic and naturally occurring compounds that can interfere with the normal function of the endocrine system, posing a significant threat to reproductive health globally [1] [2]. These substances infiltrate our environment through industrial, agricultural, and consumer sources, leading to widespread human exposure through diet, inhalation, and dermal contact [1] [3]. The molecular mechanisms by which EDCs exert their effects are complex and multifaceted, involving direct receptor interactions, epigenetic modifications, and induction of cellular stress pathways [1]. Understanding these fundamental mechanisms is crucial for developing evidence-based avoidance behaviors and intervention strategies to mitigate the risks EDCs pose to reproductive health. This technical guide synthesizes current knowledge on the molecular underpinnings of endocrine disruption, with a specific focus on implications for reproductive health and the theoretical foundations for avoidance behaviors.
Core Molecular Mechanisms of Action
Endocrine-disrupting chemicals employ diverse strategies to interfere with hormonal signaling. The primary molecular mechanisms can be categorized into four key areas, each with distinct pathways and consequences.
Nuclear Receptor Interference
The most characterized mechanism of EDCs involves direct interaction with nuclear hormone receptors, particularly estrogen receptors (ERs) and androgen receptors (ARs). These interactions can either mimic or block the actions of endogenous hormones.
Receptor Agonism/Antagonism: EDCs such as bisphenol A (BPA) and phthalates structurally mimic natural hormones like 17β-estradiol, enabling them to bind to estrogen receptors with high affinity [1]. This binding can initiate transcription of estrogen-responsive genes, leading to inappropriate activation of estrogenic pathways. Conversely, compounds like vinclozolin act as androgen receptor antagonists, blocking normal androgen signaling and impairing masculinization and reproductive development [1].
Receptor Cross-Talk: Beyond direct binding, EDCs can modulate receptor activity through cross-talk with other signaling pathways. For instance, certain EDCs activate membrane-associated estrogen receptors (e.g., GPER), which trigger rapid non-genomic signaling cascades that ultimately influence nuclear transcription [1] [4]. This cross-talk creates complex signaling networks that extend the disruptive potential of EDCs beyond classical receptor pathways.
Non-Receptor Mediated Pathways
EDCs also disrupt endocrine function through mechanisms that do not involve direct receptor binding, primarily by inducing oxidative stress and disrupting metabolic pathways.
Oxidative Stress Induction: Heavy metals like cadmium and lead, as well as various organic pollutants, promote excessive generation of reactive oxygen species (ROS) [1]. This oxidative stress damages cellular macromolecules including lipids, proteins, and DNA, particularly affecting sperm membranes and viability. Titanium dioxide nanoparticles, for instance, induce ROS production with an ED50 of 150 mg/kg, resulting in significant sperm membrane damage [1].
Mitochondrial Dysfunction: Many EDCs specifically target mitochondrial function, impairing energy production and further exacerbating oxidative stress. Zinc oxide nanoparticles (ZnO-NPs) penetrate the blood-testis barrier and trigger inflammatory cascades that substantially impair sperm motility by compromising mitochondrial ATP production [1].
Epigenetic Modifications
Perhaps the most concerning aspect of EDC exposure is their ability to induce heritable changes through epigenetic mechanisms, potentially affecting multiple generations.
DNA Methylation Alterations: EDCs including BPA, phthalates, and persistent organic pollutants can alter DNA methylation patterns at critical gene regulatory regions [1]. These changes can silence or activate genes involved in hormonal signaling, gametogenesis, and reproductive development.
Transgenerational Inheritance: Animal studies provide compelling evidence that EDC-induced epigenetic modifications can be transmitted to subsequent generations without additional exposure [1]. For example, ancestral exposure to vinclozolin has been shown to impair fertility across multiple generations through stable changes in sperm DNA methylation patterns [1].
Table 1: Classification of Major Endocrine-Disrupting Chemicals and Their Primary Molecular Targets
| Chemical Category | Representative EDCs | Primary Molecular Targets | Exposure Routes |
|---|---|---|---|
| Heavy Metals | Cadmium, Lead, Arsenic | Blood-testis barrier, Antioxidant systems, DNA integrity | Contaminated food/water, Occupational exposure |
| Synthetic Organics | BPA, Phthalates (DEHP) | Estrogen receptors, Androgen receptors, Epigenetic regulators | Food packaging, Personal care products, Plastics |
| Persistent Organic Pollutants | PCBs, Dioxins, PBDEs | Aryl hydrocarbon receptor, Thyroid hormone receptors, Androgen synthesis enzymes | Animal fats, Contaminated fish, Environmental persistence |
| Fluorinated Pesticides | Various fluorinated compounds | Estrogen receptors, Multiple nuclear receptors | Agricultural runoff, Food residues, Environmental contamination |
Experimental Models and Methodologies
Advancements in research methodologies have been crucial for elucidating the complex mechanisms of endocrine disruption and identifying novel EDCs.
Traditional Toxicology Approaches
Traditional toxicological methods have established foundational knowledge about EDC effects through standardized testing protocols.
In Vivo Animal Studies: Rodent models have been extensively used to assess the reproductive effects of EDCs across the lifespan. These studies measure endpoints such as sperm quality, hormone levels, organ weights, and morphological changes [1]. For example, studies exposing rats to a common mixture of EDCs during gestation or infancy found altered food preferences and weight gain in adulthood, accompanied by physical changes in brain regions controlling food intake and reward [5].
Cell-Based Assays: Established cell lines provide controlled systems for investigating specific molecular pathways. These assays can examine receptor binding affinity, gene expression changes, and cellular responses to EDC exposure [4]. Cell models are particularly valuable for high-throughput screening of potential endocrine activity and for elucidating specific mechanisms of action at the cellular level [4].
Advanced Mechanistic Approaches
Emerging technologies are transforming EDC research by enabling more comprehensive and human-relevant assessments.
Transcriptomics and Adverse Outcome Pathways (AOPs): A novel approach combines RNA-sequencing of zebrafish embryos with structured AOP networks to predict endocrine-disrupting potential without traditional animal testing [6]. This method identifies gene expression changes following chemical exposure and links these molecular initiating events to potential adverse outcomes through established biological pathways [6]. The automated, data-driven approach helps structure and interpret complex transcriptomic data, connecting early molecular changes to potential health effects.
Epigenetic Mapping: Advanced sequencing technologies enable genome-wide mapping of epigenetic modifications induced by EDCs. These approaches can identify specific regions of the genome susceptible to EDC-induced methylation changes and correlate these alterations with functional outcomes [1].
Table 2: Key Experimental Models for Studying Endocrine Disruption Mechanisms
| Model System | Key Applications | Advantages | Limitations |
|---|---|---|---|
| In Vivo (Rodent) | Developmental exposure studies, Transgenerational effects, Integrated physiological responses | Captures complex systemic interactions, Whole-organism context | Species differences, Time and cost intensive, Ethical considerations |
| Cell Lines | High-throughput screening, Specific pathway analysis, Receptor binding studies | Controlled environment, Mechanistic studies, Human cells possible | Limited tissue complexity, Does not capture systemic effects |
| Zebrafish Embryos | Rapid screening, Developmental toxicity, Transcriptomic analysis | Transparent embryos, High fecundity, Genetic tractability | Evolutionary distance from mammals, Different metabolic pathways |
| Computational/AOP Networks | Data integration, Predictive toxicology, Pathway analysis | Reduces animal use, Integrates diverse data types, Framework for prediction | Limited by existing knowledge, Validation challenges |
Research Reagent Solutions
Cutting-edge research on endocrine disruption mechanisms relies on specialized reagents and tools that enable precise investigation of molecular pathways.
Molecular Profiling Tools
RNA-Sequencing Kits: Comprehensive transcriptomic analysis kits are essential for identifying gene expression changes in response to EDC exposure. These tools were used in the zebrafish model study to analyze which genes were affected by cadmium and PCB-126 exposure and predict the biological processes involved [6].
Epigenetic Modification Kits: Commercial kits for assessing DNA methylation patterns (e.g., bisulfite sequencing kits) and histone modifications enable researchers to map EDC-induced epigenetic changes across the genome, providing insights into potential transgenerational effects [1].
Specialized Assay Systems
Receptor Binding Assays: Fluorescence-based and radio-labeled ligand binding assays allow quantitative assessment of EDC interactions with nuclear receptors (ERα, ERβ, AR, TR). These assays provide critical data on binding affinity and potency for prioritization and risk assessment [4].
Oxidative Stress Detection Kits: Commercial kits for measuring reactive oxygen species, antioxidant capacity, and oxidative damage products (e.g., lipid peroxidation, 8-oxo-dG) are crucial for quantifying EDC-induced cellular stress [1].
Visualization of Molecular Mechanisms
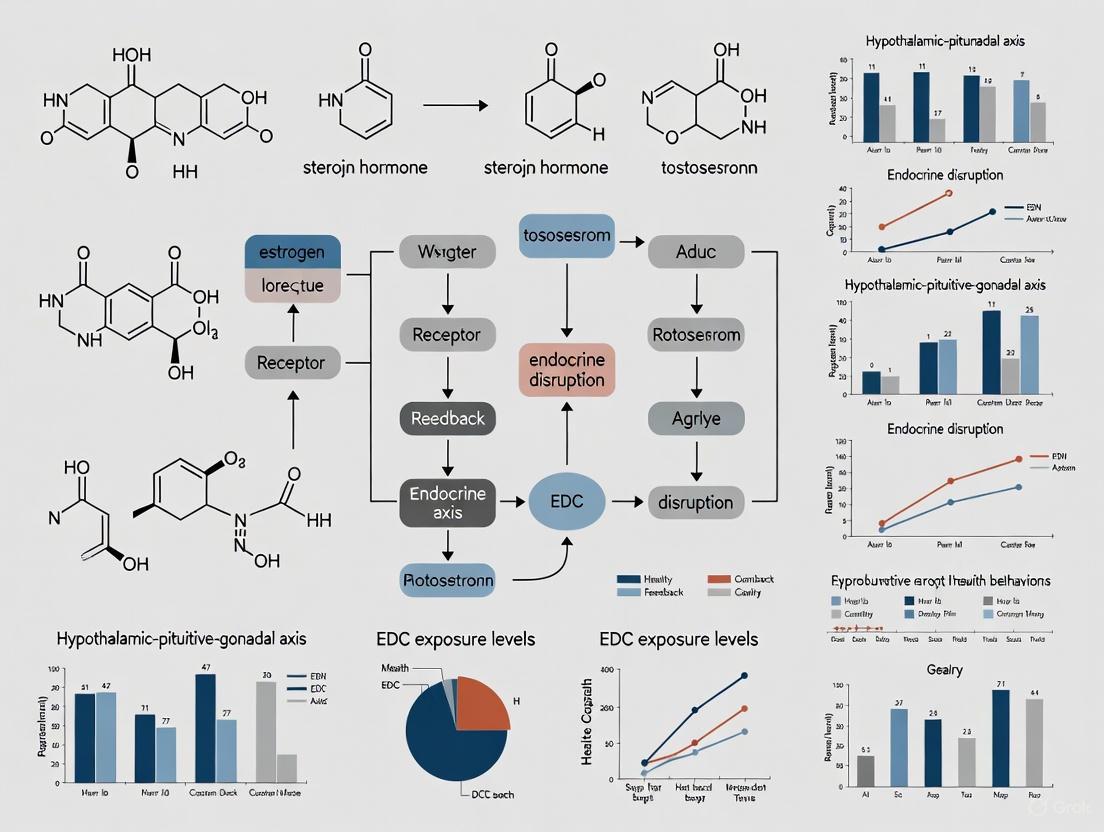
The following diagrams illustrate key signaling pathways and experimental workflows for studying endocrine disruption mechanisms.
Molecular Interference Pathways
Experimental Workflow for EDC Identification
The molecular mechanisms underlying endocrine disruption involve complex interactions at multiple biological levels, from direct receptor binding to epigenetic reprogramming. Understanding these mechanisms provides the scientific foundation for developing targeted avoidance behaviors and intervention strategies to protect reproductive health. Advanced research methods, particularly those integrating omics technologies with adverse outcome pathway frameworks, offer promising approaches for identifying EDCs and elucidating their mechanisms without exclusive reliance on animal testing. As research continues to uncover the subtle yet profound ways in which EDCs alter hormonal signaling, this knowledge must inform both public health recommendations and regulatory policies to reduce exposure and mitigate the risks to current and future generations.
The concept of "critical windows of vulnerability" posits that specific periods during development exhibit heightened sensitivity to environmental insults, with consequences that can persist across the lifespan. Exposure to endocrine-disrupting chemicals (EDCs), nutritional deficiencies, and other stressors during these precise developmental phases can disrupt organogenesis, programming, and maturation processes, leading to long-term functional deficits and increased disease risk. Understanding the temporal specificity of these exposures is paramount for developing targeted intervention strategies, particularly within the framework of reproductive health behaviors and EDC avoidance theory. This review synthesizes evidence on critical windows from fetal development through adulthood, emphasizing quantitative data, experimental methodologies, and implications for public health and clinical practice.
Theoretical Framework: Critical Windows and Developmental Origins of Health and Disease
The Developmental Origins of Health and Disease (DOHaD) hypothesis provides a foundational framework for understanding how environmental factors during sensitive developmental periods influence long-term health trajectories. Critical windows represent specific temporal phases when developing systems exhibit maximal susceptibility to perturbation due to rapid cell division, differentiation, and morphogenetic events. Exposure to stressors during these windows can induce permanent alterations in tissue structure and function through epigenetic reprogramming, changes in stem cell populations, and disruption of hormonal signaling.
Within reproductive health behavior research, EDC avoidance theory seeks to identify modifiable behaviors that reduce exposure during these critically vulnerable periods. The theory posits that knowledge of critical windows, combined with understanding of exposure routes and sources, can motivate and guide protective behaviors among vulnerable populations, particularly during preconception and gestational periods.
Table 1: Characteristics of Major Critical Windows Across the Lifespan
| Developmental Stage | Critical Windows | Key Vulnerable Systems | Primary Environmental Stressors |
|---|---|---|---|
| Fetal Development | Weeks 1-13 (Organogenesis) | Neural tube, cardiac system, foundational structures | Nutritional deficiencies (e.g., iron), EDCs, temperature extremes |
| Weeks 10-37 (System-specific maturation) | Auditory system, metabolic programming, growth | EDCs, temperature extremes, nutritional deficits | |
| Childhood | Early postnatal period | Brain maturation, immune system | EDCs, infectious agents, psychosocial stress |
| Adolescence | Pubertal transition | Reproductive system, brain remodeling | EDCs, psychosocial stress, substance use |
| Adulthood | Preconception period | Germ cell quality (sperm/oocyte) | EDCs, nutritional status, oxidative stress |
Critical Windows in Fetal Development: Experimental Evidence
Nutritional Insufficiencies: The Case of Iron Deficiency
Iron deficiency during pregnancy represents a well-characterized model for understanding critical windows of vulnerability. Animal models with precise dietary manipulation have demonstrated that the timing of iron restriction produces differential effects on fetal development.
Experimental Protocol: In a seminal rat model study, researchers established four distinct dietary-feeding protocols to induce iron deficiency during specific gestational stages [7]. Dams were provided a customized iron-deficient diet either prior to conception or during specific trimesters. Functional outcomes in offspring were assessed using Auditory Brainstem Response (ABR) measurements at postnatal days 40-45, when the auditory system is fully developed.
Key Findings: Maternal iron restriction initiated prior to conception and during the first trimester was associated with profound neural impairment in offspring, evidenced by significantly increased ABR interpeak latencies across all frequencies tested (0.25±0.18 ms to 0.49±0.034 ms, p<0.0001) [7]. Iron restriction later in pregnancy produced less severe effects. Importantly, these impairments occurred even in the absence of severe maternal anemia, indicating that iron deficiency without anemia during critical windows can disrupt fetal CNS development.
Table 2: Effects of Timing of Iron Deficiency on Fetal Development in a Rat Model
| Timing of Iron Restriction | Embryonic Iron Concentration | Fetal Weight (E19) | ABR Interpeak Latency | Neural Impairment Severity |
|---|---|---|---|---|
| Pre-conception + 1st trimester | 44% of control at E15 | ~40% lighter at E15 | Significantly increased | Profound |
| Later gestation only | Progressive decrease from E15 | Moderately reduced | Moderately increased | Moderate |
| Adequate iron throughout | Normal developmental increase | Normal developmental pattern | Normal range | Minimal |
Temperature Extremes During Gestation
Ambient temperature exposure during pregnancy represents another environmental factor with time-dependent effects on fetal development.
Experimental Protocol: A retrospective cohort study of 1,129,572 singleton births in Wuhan, China (2011-2022) linked daily ambient temperature data at 1-km² resolution to maternal residential coordinates [8]. Researchers used extended distributed lag non-linear models combined with logistic regression to examine associations between weekly temperature exposure and small vulnerable newborn (SVN) outcomes, including preterm birth (PTB), small for gestational age (SGA), and low birth weight (LBW).
Key Findings: The research identified distinct critical windows for heat and cold exposure with remarkable weekly resolution. Heat exposure during weeks 10-23 and 34-37 increased PTB risk, peaking at week 37 (OR: 1.11, 95% CI: 1.09-1.13) [8]. Cold exposure during weeks 1-13 and 22-33 increased PTB risk, most notably at week 28 (OR: 1.09, 95% CI: 1.07-1.10). For LBW, heat exposure during weeks 9-24 and 37-42 increased risks, strongest at week 42 (OR: 1.19, 95% CI: 1.16-1.21). The exposure-response relationship exhibited U-shaped, J-shaped, or L-shaped patterns depending on the gestational week, demonstrating substantial heterogeneity in temperature sensitivity across development.
Endocrine-Disrupting Chemical Exposures
EDCs present a particularly insidious threat during critical developmental windows due to their ability to interfere with hormonal signaling at extremely low concentrations.
Experimental Protocol: The Reducing Exposures to Endocrine Disruptors (REED) study protocol outlines a randomized controlled trial testing a self-directed online interactive curriculum with live counseling sessions and individualized support to reduce EDC exposure among reproductive-aged men and women [9]. Participants provide urine samples before and after the intervention for biomonitoring of phthalates, bisphenols, parabens, and oxybenzone.
Key Findings: While longitudinal outcome data are forthcoming, baseline observations confirm the ubiquitous exposure to EDCs in reproductive-aged populations. Previous intervention studies demonstrate that personalized feedback on exposure levels combined with educational resources can significantly reduce urinary concentrations of certain phthalates (monobutyl phthalate decreased with p<0.001) and increase avoidance behaviors [9].
Methodological Approaches for Identifying Critical Windows
Animal Models for Precise Temporal Manipulation
Animal models remain indispensable for identifying critical windows due to the ability to precisely control the timing and intensity of exposures. The rat model of iron deficiency exemplifies this approach, with carefully controlled dietary regimens administered during specific gestational windows [7]. Key methodological considerations include:
- Dietary Control: Customized iron-deficient diets administered during precise gestational days
- Functional Assessment: ABR measurements as a sensitive functional readout of neural development
- Tissue Analysis: Atomic absorption spectroscopy for quantifying iron concentrations in embryonic tissues
Large-Scale Epidemiological Studies with Temporal Resolution
Large retrospective cohort studies with detailed exposure data enable the identification of critical windows in human populations. The temperature exposure study exemplifies this approach with several methodological strengths [8]:
- High-Resolution Exposure Data: Daily ambient temperature data at 1-km² resolution linked to maternal residential coordinates
- Weekly Analytical Framework: Extended distributed lag non-linear models examining associations with weekly resolution
- Population Scale: Over 1 million births providing substantial statistical power for detecting associations
Intervention Studies for Modifiable Behaviors
Randomized controlled trials of behavioral interventions provide evidence for reducing exposures during critical windows. The REED study incorporates several innovative methodological elements [9]:
- Personalized Report-Back: Individualized exposure reports with urinary levels, health effect information, and personalized recommendations
- Interactive Curriculum: Self-directed online modules with live counseling sessions
- Biomonitoring: Pre- and post-intervention urine testing to quantify exposure reduction
Diagram 1: Critical Windows of Vulnerability Across Gestation. Different developmental stages exhibit specific sensitivity to environmental stressors, with the timing of exposure determining potential adverse outcomes.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Methodologies for Studying Critical Windows
| Reagent/Methodology | Primary Application | Key Function in Vulnerability Research | Example Use |
|---|---|---|---|
| Atomic Absorption Spectroscopy | Quantification of elemental concentrations | Measures tissue iron levels in embryonic and postnatal tissues | Determining embryonic iron concentration in rat models [7] |
| Auditory Brainstem Response (ABR) | Functional assessment of neural development | Non-invasive measurement of nerve conduction velocity in auditory system | Detecting neural impairment in iron-deficient offspring [7] |
| Distortion-Product Otoacoustic Emissions (DPOAE) | Assessment of peripheral auditory function | Exclusion of hair cell dysfunction as confounder for ABR measurements | Confirming central rather than peripheral neural deficits [7] |
| Liquid Chromatography-Mass Spectrometry | Biomonitoring of EDCs | Quantification of urinary phthalate, phenol, and paraben metabolites | Measuring intervention effectiveness in EDC reduction studies [9] |
| Distributed Lag Non-Linear Models | Statistical analysis of time-varying exposures | Identification of critical exposure windows with high temporal resolution | Determining weekly temperature susceptibility windows [8] |
Implications for Public Health and Clinical Practice
Understanding critical windows of vulnerability has profound implications for developing targeted interventions and public health recommendations. The evidence suggests that:
- Preconception and Early Pregnancy Interventions may be most effective for preventing certain developmental impairments, as demonstrated by the profound effects of first-trimester iron deficiency [7].
- Time-Specific Recommendations for avoiding temperature extremes could potentially reduce adverse birth outcomes, with precise weekly guidance possible based on identified critical windows [8].
- Personalized EDC Reduction Strategies that provide specific, actionable recommendations based on individual exposure profiles can effectively reduce body burden of these chemicals during vulnerable life stages [9].
Educational interventions targeting reproductive-aged populations have shown promise in increasing knowledge and promoting avoidance behaviors. Studies demonstrate that greater knowledge of specific EDCs like phthalates and parabens significantly predicts chemical avoidance in personal care products [10]. However, significant knowledge gaps remain, with chemicals like triclosan and perchloroethylene being poorly recognized even among educated populations [10].
Diagram 2: Framework for Targeted Interventions Based on Critical Windows. Effective public health interventions require identification of exposure timing, development of targeted strategies, and rigorous evaluation of outcomes.
Critical windows of vulnerability represent discrete temporal phases during which developing systems exhibit heightened sensitivity to environmental perturbations. Evidence from studies of nutritional deficiencies, temperature extremes, and EDC exposures demonstrates that the timing of insult is often as important as the dose in determining long-term outcomes. The fetal period, particularly during organogenesis and system-specific maturation, presents multiple critical windows with potential lifelong consequences.
Future research directions should include: (1) refined temporal mapping of critical windows using high-resolution exposure assessment and modeling approaches; (2) elucidation of molecular mechanisms underlying developmental vulnerability, including epigenetic reprogramming and stem cell susceptibility; and (3) development of targeted interventions based on identified critical windows to maximize protective effects during the most vulnerable developmental periods. Integration of this knowledge into clinical practice and public health policy offers the promise of more effective strategies for protecting developmental health across the lifespan.
Reproductive health encompasses physical, mental, and social well-being in all matters relating to the reproductive system, not merely the absence of disease or disorders [11]. In recent decades, a growing body of evidence has identified concerning trends in reproductive health outcomes, including rising rates of infertility, polycystic ovary syndrome (PCOS), early puberty, and menopause acceleration. These conditions represent significant challenges to individual well-being, public health systems, and global demographic patterns.
This technical guide examines the complex interplay between environmental exposures, particularly to endocrine-disrupting chemicals (EDCs), and their role in the pathogenesis of these reproductive health outcomes. Framed within the context of reproductive health behaviors and EDC avoidance theory, this review synthesizes current scientific evidence, provides detailed methodological approaches for studying these relationships, and offers a toolkit for researchers and drug development professionals working in this rapidly evolving field. The comprehensive analysis presented here aims to bridge laboratory research, clinical practice, and public health policy by providing mechanistic insights, standardized protocols, and evidence-based intervention strategies.
Reproductive Health Outcomes: Prevalence and Pathophysiology
Polycystic Ovary Syndrome (PCOS)
PCOS represents one of the most common endocrine disorders affecting women of reproductive age, with an estimated global prevalence of 6-13% [12]. Despite its prevalence, up to 70% of affected women remain undiagnosed worldwide, creating a significant public health gap [12]. The condition is characterized by three cardinal features: oligo- or anovulation, clinical or biochemical signs of hyperandrogenism, and polycystic ovarian morphology [13]. PCOS remains a leading cause of anovulatory infertility and represents the most common endocrine disturbance in reproductive-aged women [13] [12].
The pathophysiology of PCOS manifests across the female lifespan, beginning with early markers in infancy and continuing through menopause. Daughters of women with PCOS show increased anti-Müllerian hormone (AMH) levels in infancy, early childhood, and prepubertally, suggesting an increased follicle complement and mild metabolic abnormalities compared with controls [14]. During adolescence, PCOS often presents with premature pubarche (development of pubic/axillary hair before age 8 years) and a wider age range at menarche [13] [14]. The transition through reproductive years is marked by a gradual decrease in the severity of PCOS features, though hyperandrogenism and menstrual irregularities often persist [14]. In menopause, women with a history of PCOS continue to manifest cardiovascular risk factors, though longitudinal studies on long-term outcomes remain limited [14].
Table 1: Diagnostic Features and Prevalence of PCOS Across the Lifespan
| Life Stage | Key Features | Prevalence/Notes | References |
|---|---|---|---|
| Infancy/Childhood | Increased AMH levels (proxy for follicle number); mild metabolic abnormalities | Studied in daughters of women with PCOS; strong heritability component | [14] |
| Puberty/Adolescence | Premature pubarche; wider age range at menarche; hyperandrogenism; irregular menses | Diagnosis challenging due to overlap with normal puberty; hyperandrogenemia most reliable diagnostic criterion | [13] [14] |
| Reproductive Years | Oligo/anovulation; hyperandrogenism; polycystic ovarian morphology; insulin resistance | 6-13% of reproductive-aged women; leading cause of anovulatory infertility | [13] [12] |
| Menopause | Higher Ferriman-Gallwey scores; increased cardiovascular risk factors; possible later menopause | Limited longitudinal data; metabolic features may persist | [14] |
Infertility and Menstrual Dysfunction
Infertility represents a significant consequence of multiple reproductive health disorders, with PCOS being a predominant cause. Approximately 75-85% of women with PCOS experience irregular menstrual cycles due to ovulatory dysfunction [13]. The mechanisms of anovulation in PCOS involve disordered follicle development from the earliest phases through to the antral stages, with persistence and assumed arrest of larger antral follicles [13]. These "arrested" follicles comprise those that have already undergone terminal differentiation together with healthy follicles that have stopped growing due to suboptimal FSH stimulation [13].
The impact of PCOS on fertility varies with age. While pregnancy rates are similar amongst younger women with and without PCOS, older women with PCOS have been found to have lower numbers of deliveries overall, lower average number of children, and higher rates of infertility [13]. Pregnancy in women with PCOS is associated with higher risks of complications including miscarriage, pre-eclampsia, low birth weight, and gestational diabetes mellitus, particularly in those with obesity [13].
Early Puberty and Menopause Acceleration
Emerging evidence suggests that environmental factors, including EDC exposure, may influence the timing of pubertal onset and reproductive senescence. Early life exposures to EDCs have been associated with premature pubarche, which may be an early sign of PCOS and later reproductive dysfunction [13] [14]. The relationship between birth weight and pubertal timing appears complex, with both low and high birth weight associated with higher AMH levels in infancy, suggesting alterations in follicular development that may influence reproductive lifespan [14].
Women with PCOS appear to have a later age of menopause, though longitudinal studies are lacking and the experience of women with PCOS in peri/postmenopause remains poorly studied [13]. The benefits and risks associated with menopausal hormone replacement therapy in women with PCOS represent a significant knowledge gap in current literature.
EDCs and Reproductive Health
Endocrine-disrupting chemicals are synthetic compounds that interfere with the normal function of the endocrine system through multiple mechanisms. Some EDCs directly bind to hormone receptors, such as estrogen, androgen, and thyroid hormone receptors, either mimicking or blocking their functions, thereby disrupting the body's normal physiological processes [11]. The reproductive system is particularly vulnerable to EDC exposure, as many EDCs exert estrogenic or anti-estrogenic effects that can lead to reduced sperm count, smaller male reproductive organs, abnormal reproductive behaviors, and decreased fertility rates [11].
EDCs enter the body through various exposure routes, including food, air, and skin absorption, making them nearly unavoidable in daily life [11]. Women are disproportionately exposed to EDCs through personal care and household products (PCHPs), encountering an estimated 168 different chemicals daily [3]. This heightened exposure is particularly concerning during vulnerable life stages such as preconception, pregnancy, and lactation, when EDC exposures can have transgenerational effects.
Table 2: Common Endocrine-Disrupting Chemicals, Sources, and Reproductive Health Impacts
| EDC | Common Sources | Primary Functions | Reproductive Health Impacts | References |
|---|---|---|---|---|
| Phthalates | Scented PCHPs; hair care products; lotions; cosmetics; household cleaners | Plasticizer, preservative | Estrogen mimicking/hormonal imbalances; reproductive effects/impaired fertility; antiandrogenic effects | [3] [9] |
| Parabens | Shampoos & conditioners; lotions; cosmetics; antiperspirants; household cleaners | Preservative | Carcinogenic potential; estrogen mimicking/hormonal imbalances; reproductive effects/impaired fertility | [3] |
| Bisphenol A (BPA) and analogs | Plastic packaging of PCHP; antiperspirants; detergents; conditioners; lotions | Plasticizer | Fetal disruptions/placental abnormalities; reproductive effects; mammary carcinogen | [3] [9] |
| Lead | Cosmetics (lipsticks, eyeliner); household cleaners | Color enhancer | Infertility; menstrual disorders; disturbances to fetal development; possibly carcinogenic | [3] |
| Triclosan | Toothpaste/mouth wash; body washes; dish soaps; bathroom cleaners | Antimicrobial | Miscarriage; impaired fertility; fetal developmental effects | [3] |
| Perchloroethylene (PERC) | Spot removers; floor cleaners; furniture cleaners; dry cleaning | Solvent | Probable carcinogen; reproductive effects/impaired fertility | [3] |
Mechanistic Insights: EDC Disruption of Reproductive Pathways
EDCs interfere with reproductive physiology through multiple interconnected mechanisms. The following diagram illustrates key pathways through which EDCs disrupt normal reproductive function:
Diagram 1: Mechanisms of EDC Disruption in Reproductive Health. EDCs interfere with multiple physiological pathways including the HPO axis, hormone receptor signaling, follicular development, and metabolic function, leading to diverse reproductive pathologies.
Methodological Approaches: Assessing EDC Exposure and Reproductive Outcomes
EDC Exposure Assessment Methodologies
Accurate assessment of EDC exposure represents a critical component of research on reproductive health outcomes. The following diagram illustrates a comprehensive workflow for EDC exposure assessment and intervention evaluation:
Diagram 2: Comprehensive Workflow for EDC Exposure and Reproductive Health Research. This methodology integrates exposure assessment, health outcome measurement, intervention components, and statistical analysis to evaluate EDC-reproductive health relationships.
Validated Survey Instruments for EDC Exposure and Reproductive Health Behaviors
Several validated survey instruments have been developed to assess EDC-related knowledge, risk perceptions, and avoidance behaviors. Kim et al. (2025) developed and validated a 19-item survey assessing reproductive health behaviors to reduce EDC exposure through four factors: health behaviors through food, health behaviors through breathing, health behaviors through skin, and health promotion behaviors [11]. This instrument utilizes a 5-point Likert scale and has demonstrated acceptable reliability (Cronbach's alpha = 0.80) [11].
The Health Belief Model (HBM) has been successfully applied to understand and predict EDC avoidance behaviors. A Toronto-based study of 200 women in preconception and conception periods utilized a researcher-designed questionnaire based on the HBM to assess knowledge, health risk perceptions, beliefs, and avoidance behaviors regarding EDCs in personal care and household products [3]. The questionnaire demonstrated acceptable reliability in preliminary analyses and identified that greater knowledge of specific EDCs (lead, parabens, bisphenol A, and phthalates) significantly predicted chemical avoidance in PCHPs [3].
Biomarker Assessment in EDC Research
Biomonitoring represents the gold standard for assessing internal EDC exposure. Phthalates, parabens, bisphenols, and other EDCs can be measured in urine, blood, saliva, and other biological matrices. The Million Marker program has pioneered mail-in urine testing kits for EDC biomonitoring, making exposure assessment more accessible for research and clinical applications [9]. These methods are particularly valuable given the short half-lives of many EDCs (6 hours to 3 days), which reflects recent exposure and enables researchers to track changes in exposure following interventions [9].
Recent advances have integrated clinical biomarker assessment with EDC intervention studies. The Reducing Exposures to Endocrine Disruptors (REED) study protocol includes testing for clinical biomarkers (via at-home Siphox tests) to evaluate whether EDC reduction interventions lead to improvements in health parameters such as metabolic markers, hormone levels, and inflammatory markers [9]. This approach addresses a critical gap in connecting EDC exposure reduction with measurable health improvements.
Research Reagent Solutions and Technical Toolkit
Table 3: Essential Research Reagents and Materials for EDC and Reproductive Health Research
| Category | Specific Reagents/Materials | Application/Function | Technical Notes | References |
|---|---|---|---|---|
| Biomonitoring | Urine collection kits; LC-MS/MS systems; ELISA kits; SPE cartridges | Quantification of EDCs and metabolites in biological samples | Consider short half-lives; measure multiple analogs; account for specific gravity | [9] |
| Clinical Biomarkers | Hormone panels (testosterone, estrogen, LH, FSH, AMH); metabolic panels (glucose, insulin, lipids); inflammatory markers (CRP, cytokines) | Assessment of reproductive and metabolic health status | AMH correlates with antral follicle count; consider menstrual cycle timing | [13] [9] |
| Survey Instruments | Validated EDC knowledge scales; Health Belief Model questionnaires; Readiness to Change assessments; Product use inventories | Measure knowledge, perceptions, behaviors related to EDC exposure | Ensure cultural adaptation; validate in specific populations; use consistent scaling | [3] [11] |
| Intervention Materials | Educational curricula on EDC sources; Product replacement kits; Counseling protocols; Digital health platforms | Implement and test EDC exposure reduction strategies | Personalized approaches show greater efficacy; combine with biomonitoring feedback | [9] [15] |
| Data Analysis | Statistical software (R, SPSS); Structural equation modeling; Mixed-effects models; Mediation analysis packages | Analyze complex exposure-outcome relationships; model behavioral change | Account for multiple comparisons; adjust for key covariates; consider non-monotonic dose responses | [3] [11] |
EDC Avoidance Theory and Intervention Strategies
Theoretical Frameworks for Behavior Change
The Health Belief Model has demonstrated utility in understanding and promoting EDC avoidance behaviors. According to this framework, women who perceive a heightened risk of health impacts from EDC exposure and understand the health implications become more concerned about chemical-based products [3]. If they believe that choosing EDC-free products can lower their risk, they are more likely to adjust their purchasing behavior accordingly [3]. Research has confirmed that higher risk perceptions of parabens and phthalates predict greater avoidance behaviors [3].
Educational interventions that increase EDC-related health literacy (EHL) have shown promising results in promoting behavior change. A previous intervention study found that after report-back of personal EDC exposure results, participants demonstrated increased EHL behaviors and women showed increased readiness to change their exposure behaviors [9]. Participants reported subsequently using non-toxic personal products (50%), using non-toxic household products (44%), dining out less (20%), eating less packaged food (32%), using less plastic (40%), and reading product labels more (48%) [9].
Effective Intervention Components
Evidence-based EDC reduction interventions typically incorporate several key components. Accessible web-based educational resources, targeted replacement of known toxic products, and personalization of the intervention through meetings and support groups represent the most promising strategies for reducing EDC concentrations [15]. The REED study protocol incorporates an online interactive curriculum with live counseling sessions and individualized support modeled after the Diabetes Prevention Program [9].
Product replacement represents a particularly effective intervention strategy. Research has demonstrated that providing participants with alternatives to high-EDC products leads to significant reductions in urinary biomarkers of exposure. For example, replacing conventional personal care products with certified low-EDC alternatives for as little as three days can reduce urinary concentrations of certain phthalates, parabens, and phenols by 27-45% [15].
Global Family Planning and Reproductive Health Context
Reproductive health outcomes, including infertility and PCOS, must be understood within the broader context of global family planning needs. Current data indicate that 928 million women in low- and middle-income countries want to avoid pregnancy, yet 214 million are not using modern contraception [16]. Among those with unmet needs, 78 million women intend to use or would be open to using contraception in the future, representing a strategic target for family planning interventions [16].
Meeting the global need for sexual and reproductive health services requires significant investment. An estimated $104 billion annually is needed to meet all sexual and reproductive health needs in low- and middle-income countries, with $14 billion needed annually specifically to close the contraceptive gap alone [16]. These investments yield significant returns, with every additional $1 spent on contraceptive services saving $2.48 in maternal, newborn, and abortion care costs [16].
Family planning interventions also demonstrate important economic benefits beyond health outcomes. In Kenya and Nigeria, women's use of contraception led to a 10-12% increase in doing paid work the following year and a nearly 15% increase in control over use of wages [16]. In Burkina Faso, Kenya, and Niger, longer duration of contraceptive use was associated with women experiencing more years of paid employment with control over use of their earnings [16].
The intricate relationships between EDC exposure, reproductive health behaviors, and adverse reproductive outcomes represent a critical area of scientific inquiry with significant implications for clinical practice and public health policy. The evidence synthesized in this review demonstrates that EDCs contribute to the pathogenesis of infertility, PCOS, early puberty, and potentially menopause acceleration through multiple mechanistic pathways. Framed within the context of EDC avoidance theory, this guide provides researchers and drug development professionals with comprehensive methodological approaches, validated assessment tools, and evidence-based intervention strategies to advance this field.
Significant knowledge gaps remain that warrant further investigation. Future research should prioritize longitudinal studies tracking EDC exposures and reproductive outcomes across the lifespan, intervention trials testing the efficacy of EDC reduction strategies on clinical endpoints, and mechanistic studies elucidating the precise pathways through which EDCs disrupt reproductive function. Additionally, research should explore potential ethnic variations in EDC metabolism and susceptibility, develop more sensitive biomarkers of effect, and validate brief assessment tools for clinical identification of high-risk individuals.
As the field advances, collaboration across disciplines—including environmental health, reproductive endocrinology, epidemiology, and behavioral science—will be essential to translate scientific evidence into effective clinical and public health interventions. By integrating EDC exposure reduction strategies into reproductive healthcare and family planning services, we may mitigate the burden of adverse reproductive outcomes and improve health across generations.
Transgenerational Effects and Epigenetic Modifications from EDC Exposure
Environmental endocrine disruptors (EDCs) represent a class of widespread chemical contaminants that interfere with normal hormonal signaling, with growing evidence indicating they can induce heritable epigenetic changes affecting multiple generations [17]. The transgenerational inheritance of EDC-induced phenotypes represents a paradigm shift in understanding environmental impacts on health, moving beyond direct toxic effects to encompass germline epigenetic reprogramming that can manifest as disease susceptibility in subsequent generations. While epidemiological associations between EDC exposure and reproductive dysfunction are well-established, the mechanistic underpinnings of transgenerational epigenetic inheritance remain an area of intense investigation [17] [18].
This technical guide synthesizes current evidence on EDC-mediated transgenerational epigenetic effects, focusing on molecular mechanisms, experimental methodologies, and implications for reproductive health across generations. The content is framed within the broader context of reproductive health behaviors and EDC avoidance theory, providing researchers with the conceptual frameworks and technical tools necessary to advance this critically important field.
Molecular Mechanisms of EDC-Induced Epigenetic Modifications
EDCs disrupt normal epigenetic programming through multiple interconnected pathways that can become permanently encoded in the germline, leading to transgenerational inheritance of reproductive abnormalities [17]. The primary molecular mechanisms include:
DNA Methylation Alterations
DNA methylation patterns, particularly at imprinted gene loci and metastable epialleles, are highly vulnerable to disruption by EDC exposure during critical developmental windows. The establishment and maintenance of DNA methylation marks during embryogenesis and germ cell development represent key periods of epigenetic vulnerability [17]. EDCs including bisphenol A (BPA), phthalates, and persistent organic pollutants have been demonstrated to induce hypermethylation or hypomethylation at specific genomic regions that control the expression of genes critical for reproductive development and function. These altered methylation patterns can be transmitted through the germline and maintained across generations, even in the absence of continued exposure [17].
Histone Modifications
EDC exposure can profoundly alter the post-translational modification landscape of histones, including methylation, acetylation, and phosphorylation changes that regulate chromatin accessibility and gene expression. These histone modifications serve as epigenetic marks that can be propagated during cell division and potentially transmitted across generations. Specific EDCs have been shown to modulate the activity and expression of histone-modifying enzymes such as histone deacetylases (HDACs) and histone methyltransferases, leading to lasting changes in chromatin states that influence gene expression programs in reproductive tissues [17].
Non-Coding RNA Regulation
Small non-coding RNAs, including microRNAs and piwi-interacting RNAs, have emerged as important mediators of EDC-induced transgenerational epigenetic effects. These regulatory RNAs can be altered in the germline following EDC exposure and contribute to the transmission of epigenetic information across generations. The dysregulation of non-coding RNA networks can result in persistent changes in gene expression that manifest as reproductive pathologies in subsequent generations, even without direct exposure [17].
Table 1: Primary Epigenetic Mechanisms of EDC Action
| Mechanism | Key EDCs Involved | Molecular Consequences | Transgenerational Evidence |
|---|---|---|---|
| DNA Methylation Alterations | BPA, Phthalates, Vinclozolin | Hypermethylation of hormone response genes; Hypomethylation of repetitive elements | Confirmed in animal models across multiple generations [17] |
| Histone Modifications | Persistent Organic Pollutants, Heavy Metals | Altered histone acetylation/methylation patterns at promoters of steroidogenic genes | Demonstrated in animal studies; human evidence emerging |
| Non-Coding RNA Regulation | Plasticizers, Pesticides | Dysregulation of miRNA expression profiles in sperm and germ cells | Experimental evidence in animal models |
The following diagram illustrates the interconnected molecular pathways through which EDC exposure leads to transgenerational epigenetic effects:
Experimental Evidence for Transgenerational Inheritance
Animal Model Studies
Compelling evidence for EDC-induced transgenerational epigenetic effects comes from well-controlled animal studies that have demonstrated the inheritance of reproductive abnormalities across multiple generations. These studies typically expose pregnant females during critical periods of germline epigenetic reprogramming in the developing fetus, then track phenotypic and epigenetic changes in subsequent generations (F1-F3) without additional exposure [17]. The F3 generation represents the first truly transgenerational cohort when exposure occurs during gestation, as the F1 generation fetus and F2 generation germline are directly exposed, while the F3 generation is the first without direct exposure [17].
Research has shown that EDCs including vinclozolin, methoxychlor, BPA, and phthalates can induce transgenerational inheritance of disease states, particularly affecting male reproductive function. Documented effects include reduced sperm motility and concentration, increased sperm apoptosis, and morphological abnormalities in reproductive tissues [17]. These phenotypic changes are associated with transcriptional alterations in the testis and specific epigenetic modifications in sperm, including differential DNA methylation regions and changes in non-coding RNA expression [17].
Human Evidence and Epidemiological Studies
While animal studies provide compelling mechanistic evidence for transgenerational epigenetic inheritance, human evidence remains limited due to the extended timeframes required for multigenerational studies and practical challenges of maintaining long-term cohorts across decades [17]. However, some epidemiological studies have suggested transgenerational effects through analysis of generational exposures and disease incidence patterns.
The available human evidence primarily comes from retrospective cohort studies and analysis of historical exposure events, which suggest potential transgenerational effects of EDCs on reproductive health. These studies face significant methodological challenges, including accurate exposure assessment across generations, controlling for confounding factors, and the long latency between exposure and phenotypic manifestation [17].
Table 2: Transgenerational Effects of Select EDCs in Animal Models
| EDC Class | Specific Compound | Exposure Window | F1 Generation Effects | F3 Generation Effects |
|---|---|---|---|---|
| Fungicide | Vinclozolin | Gestational days 8-15 | 20% reduction in sperm motility; 30% increase in apoptosis | 50% reduction in sperm motility; 70% of males infertile |
| Plasticizer | BPA | Gestational days 10-18 | 15% decrease in sperm concentration; altered sexual behavior | 25% decrease in sperm concentration; social behavior deficits |
| Phthalate | DEHP | Gestational days 10- birth | 18% reduction in testosterone; testicular abnormalities | 30% reduction in sperm count; 40% increase in pubertal abnormalities |
| Insecticide | Methoxychlor | Gestational days 8-15 | 25% reduction in sperm viability; kidney disease | 60% disease incidence; 90% of males have spermatogenic defects |
Methodological Approaches for Transgenerational EDC Research
Experimental Design Considerations
Robust investigation of transgenerational epigenetic effects requires carefully controlled experimental designs that account for the unique challenges of multigenerational studies. Key considerations include:
Exposure Timing: The developmental stage during EDC exposure is critical, as windows of germline epigenetic reprogramming represent periods of heightened vulnerability. In mammalian models, gestational exposure during primordial germ cell development and gonadal sex determination is particularly effective at inducing transgenerational effects [17].
Dose Selection: Environmental relevance of exposure doses should be prioritized, with consideration of non-monotonic dose responses that are characteristic of many EDCs. Studies should include multiple dose levels when possible, including human-relevant exposure levels [17].
Generational Analysis: Proper experimental design must distinguish between direct multigenerational effects (F0-F2) and true transgenerational inheritance (F3 and beyond) when exposure occurs during gestation [17].
Epigenetic Analysis Techniques
Comprehensive assessment of EDC-induced epigenetic changes requires multimodal approaches that capture different layers of epigenetic regulation:
DNA Methylation Analysis: Genome-wide approaches include whole-genome bisulfite sequencing for comprehensive methylation mapping and reduced representation bisulfite sequencing for cost-effective assessment of CpG-rich regions. Locus-specific methods such as pyrosequencing provide high-precision quantification of methylation at candidate regions [17].
Histone Modification Profiling: Chromatin immunoprecipitation followed by sequencing (ChIP-seq) enables genome-wide mapping of histone modifications and transcription factor binding sites. Antibody specificity and chromatin quality are critical factors for reproducible results [17].
Non-Coding RNA Analysis: Small RNA sequencing provides comprehensive profiling of miRNA and other small non-coding RNAs, with special considerations for the unique biogenesis and stability of different RNA classes [17].
The following diagram outlines a standardized experimental workflow for transgenerational EDC research:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Transgenerational EDC Research
| Reagent/Material Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| EDC Reference Standards | Bisphenol A (BPA), Di(2-ethylhexyl) phthalate (DEHP), Vinclozolin | Controlled exposure studies; analytical standard for exposure verification | Purity >99%; stable isotope-labeled versions for exposure quantification |
| Epigenetic Analysis Kits | EZ DNA Methylation-Gold Kit, EpiQuik HDAC Activity Assay, Magna ChIP Kit | DNA methylation analysis; histone modification assessment; chromatin immunoprecipitation | Batch-to-batch consistency; minimal DNA degradation during processing |
| Antibodies for Histone Modifications | H3K4me3, H3K27me3, H3K9ac, H3K27ac | ChIP-seq; immunohistochemistry; western blotting | Specificity validation for species; lot-to-lot consistency |
| Next-Generation Sequencing Kits | TruSeq DNA Methylation, Small RNA Library Prep, ChIP-seq Library Prep | Genome-wide epigenetic profiling | Compatibility with sequencing platform; optimization for input material |
| Germ Cell Isolation Reagents | Collagenase IV, Trypsin-EDTA, Percoll gradients, Fluorescent-activated cell sorting buffers | Isolation of specific germ cell populations | Maintenance of cell viability; preservation of epigenetic marks |
| Quality Control Assays | Bioanalyzer/Tapestation, Qubit Fluorometric Quantitation, Bisulfite Conversion Efficiency | Assessment of nucleic acid quality and quantity | Accurate quantification of low-input samples; verification of complete bisulfite conversion |
Implications for Reproductive Health and EDC Avoidance Theory
The transgenerational epigenetic effects of EDCs have profound implications for reproductive health behaviors and public policy. Understanding that current exposures may impact multiple future generations strengthens the imperative for preventative approaches to EDC exposure [17] [9]. This evidence supports the development of comprehensive EDC avoidance strategies targeting susceptible populations, particularly during critical developmental windows such as pregnancy and early childhood [9].
Recent intervention studies demonstrate that personalized exposure reduction programs can significantly decrease body burdens of EDCs, supporting the potential for breaking cycles of transgenerational epigenetic inheritance [9]. These interventions combine biomonitoring approaches with educational components to empower individuals to reduce exposures through behavioral modifications, demonstrating significant reductions in EDC metabolites following targeted interventions [9].
Research Gaps and Future Directions
Despite significant advances, critical knowledge gaps remain in understanding EDC-induced transgenerational epigenetic effects. Key research priorities include:
Mixture Toxicology: Most studies examine individual EDCs, while real-world exposure involves complex mixtures. Research on interactive effects of EDC mixtures on epigenetic programming is needed [17].
Human Translation: Bridging the gap between compelling animal model data and human evidence requires innovative epidemiological approaches and potential analysis of human germline epigenetic changes [17].
Mechanistic Resolution: Deeper understanding of how specific epigenetic marks are established, maintained, and transmitted across generations will clarify the fundamental principles of transgenerational epigenetic inheritance [17].
Intervention Strategies: Development of evidence-based interventions to prevent or reverse EDC-induced epigenetic changes represents a critical frontier for protecting reproductive health across generations [9].
The emerging evidence for transgenerational epigenetic effects of EDCs underscores the urgency of addressing environmental chemical exposures as a matter of intergenerational justice, with implications for regulatory policy, clinical practice, and individual lifestyle choices aimed at preserving reproductive health for future generations.
Endocrine-disrupting chemicals (EDCs) represent a significant and growing concern in public health, particularly regarding reproductive outcomes. This whitepaper provides a technical overview of five major EDC classes—bisphenols, phthalates, parabens, pesticides, and per- and polyfluoroalkyl substances (PFAS)—focusing on their mechanisms of action, reproductive toxicity, and methodologies for their study. Mounting epidemiological and experimental evidence links exposure to these compounds with adverse reproductive health effects in both males and females, including reduced sperm quality, altered steroidogenesis, diminished ovarian reserve, and increased risk of conditions like endometriosis and polycystic ovary syndrome. Understanding the specific pathways through which these chemicals exert their effects is crucial for developing targeted therapeutic interventions and informing public health policies aimed at exposure reduction. This document serves as a technical primer for researchers and drug development professionals working at the intersection of environmental toxicology and reproductive medicine.
Endocrine-disrupting chemicals are exogenous substances or mixtures that alter function(s) of the endocrine system and consequently cause adverse health effects in an intact organism, or its progeny, or (sub)populations [19]. The global decline in human fertility rates has occurred concurrently with increased production and environmental release of synthetic chemicals, suggesting a potential link that has prompted intensive research efforts [19]. EDCs can interfere with hormonal action through multiple mechanisms, including mimicking natural hormones, blocking hormone receptors, and altering the production, transport, metabolism, or elimination of natural hormones [19]. The reproductive system is particularly vulnerable to EDC exposure during critical developmental windows, such as fetal development, puberty, and reproductive adulthood, with effects that may manifest immediately or decades later [19].
Bisphenols
Bisphenol-A (BPA) is a high-production-volume chemical primarily used in the manufacture of polycarbonate plastics and epoxy resins. These materials are found in numerous consumer goods, including food and beverage containers, dental materials, and thermal receipt paper [20] [21]. BPA monomers can leach from these products, especially when heated or damaged, leading to widespread human exposure through dietary intake, dermal absorption, and inhalation [21].
Mechanisms of Reproductive Toxicity
BPA exerts its endocrine-disrupting effects through both genomic and non-genomic pathways. Structurally similar to estradiol, BPA can bind to estrogen receptors (ERα and ERβ), acting as a xenoestrogen and mimicking the effects of natural estrogens [20] [21]. Additionally, BPA can interfere with other nuclear receptors, including androgen and thyroid hormone receptors [21]. Non-genomic effects include interference with cellular signaling pathways and epigenetic modifications that can alter gene expression patterns critical for reproductive development and function [21].
Bisphenol-A (BPA) Signaling Interference Pathways
Experimental Approaches for BPA Research
In vitro models utilizing cell lines derived from reproductive tissues (e.g., granulosa cells, Sertoli cells) are employed to study the direct effects of BPA on cellular function. Typical experimental protocols involve exposing these cells to varying concentrations of BPA (ranging from nM to μM) across different time courses, followed by assessment of gene expression, hormone production, and cell viability [22]. For endocrine disruption screening, reporter gene assays in ER-transfected cell lines quantify the estrogenic activity of BPA. In vivo studies often utilize perinatal exposure paradigms in rodent models to examine the long-term reproductive effects of developmental BPA exposure. These studies administer BPA via drinking water or diet at environmentally relevant doses (2-50 μg/kg/day) and assess outcomes including pubertal onset, ovarian follicle counts, sperm parameters, and hormone levels throughout the lifespan [20] [21].
Key Research Reagents for BPA Studies
| Research Reagent | Application | Function in Experimental Design |
|---|---|---|
| ERα/ERβ Reporter Cell Lines | In vitro screening | Detect estrogenic activity via luciferase expression |
| Anti-17β-HSD1 Antibody | Enzyme activity assays | Quantify expression of estrogen-activating enzyme |
| BPA Molecularly Imprinted Polymers | Sample purification | Selective extraction of BPA from biological matrices |
| LC-MS/MS Standards (deuterated BPA) | Analytical quantification | Internal standard for precise biomonitoring |
| DNA Methylation Kits | Epigenetic analysis | Assess BPA-induced changes in methylation patterns |
Phthalates
Phthalates are a class of chemicals primarily used as plasticizers to increase the flexibility and durability of polyvinyl chloride (PVC) plastics. Common phthalates include diethylhexyl phthalate (DEHP), dibutyl phthalate (DBP), diethyl phthalate (DEP), di-isononyl phthalate (DiNP), and di-iso-decyl phthalate (DiDP) [23]. These compounds are not covalently bound to the plastic matrix and can readily leach into the environment. Human exposure occurs primarily through ingestion of contaminated food and water, inhalation of indoor air, and dermal absorption from personal care products and medical devices [23]. Phthalates are rapidly metabolized in the human body, with monoester metabolites and secondary oxidative metabolites excreted in urine and feces, making these metabolites useful biomarkers for exposure assessment [23].
Mechanisms of Reproductive Toxicity
Phthalates exert anti-androgenic effects through multiple mechanisms, primarily by reducing testosterone synthesis in Leydig cells through suppression of gene expression encoding steroidogenic enzymes [23]. They also induce oxidative stress in germ cells and disrupt the blood-testis barrier by degrading intercellular junctions between Sertoli cells [23] [24]. In females, phthalates can interfere with folliculogenesis and steroid hormone production, potentially leading to reduced ovarian reserve and hormonal imbalances [19]. Some phthalates have also been shown to affect gene expression through epigenetic modifications, including altered DNA methylation status of imprinted genes involved in reproductive function [23].
Phthalate Metabolic Pathways and Toxicity Mechanisms
Experimental Approaches for Phthalate Research
A standard methodology for assessing phthalate exposure involves measuring urinary metabolites using liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS). This biomonitoring approach typically includes enzymatic deconjugation of phase II metabolites, solid-phase extraction, and quantification using isotope-labeled internal standards [23]. For mechanistic studies, in vitro models utilize primary cultures of Leydig cells or human granulosa cell lines (e.g., COV434) exposed to phthalate metabolites like mono(2-ethylhexyl) phthalate (MEHP) to examine effects on steroid hormone production and gene expression [23] [22]. Animal studies often employ developmental exposure protocols where pregnant rodents receive phthalates in their diet (50-1000 mg/kg/day) during critical windows of reproductive tract development, with offspring assessed for anomalies in reproductive organ development, sperm parameters, and fertility in adulthood [23].
Key Research Reagents for Phthalate Studies
| Research Reagent | Application | Function in Experimental Design |
|---|---|---|
| Deuterated Phthalate Metabolites | LC-MS/MS analysis | Internal standards for quantitative accuracy |
| Anti-StAR Antibody | Steroidogenesis assays | Detect expression of steroidogenic acute regulatory protein |
| Oxidative Stress Assay Kits | Cellular stress measurement | Quantify ROS production in germ cells |
| Tight Junction Protein Antibodies | Histological analysis | Visualize blood-testis barrier integrity |
| CYP17A1 Inhibitors | Enzyme activity studies | Compare with phthalate effects on steroidogenesis |
Parabens
Parabens are alkyl esters of p-hydroxybenzoic acid widely used as preservatives in cosmetics, pharmaceuticals, and processed foods due to their broad-spectrum antimicrobial activity, low cost, and chemical stability [22]. Common parabens include methylparaben, ethylparaben, propylparaben, and butylparaben, often used in combination to enhance preservative efficacy. Human exposure occurs primarily through dermal absorption from personal care products and to a lesser extent via dietary intake [22]. Although parabens are rapidly metabolized by esterases in the liver and skin to p-hydroxybenzoic acid and excreted in urine as conjugates, continuous exposure from multiple sources leads to persistent body burdens [22].
Mechanisms of Reproductive Toxicity
Parabens can disrupt endocrine function through multiple mechanisms. They exhibit weak estrogen receptor agonist activity and can inhibit estrogen-synthesizing (17β-HSD1) and estrogen-inactivating (17β-HSD2) enzymes in a structure-dependent manner [22]. Longer-chain parabens (hexyl- and heptylparaben) more potently inhibit 17β-HSD1, which converts estrone to the more biologically active estradiol, thereby potentially reducing local estrogen concentrations [22]. Conversely, shorter-chain parabens like ethylparaben inhibit 17β-HSD2, which inactivates estradiol, potentially increasing local estrogen concentrations [22]. This differential inhibition of estrogen-regulating enzymes can disrupt the delicate balance of estrogen signaling in reproductive tissues.
Experimental Approaches for Paraben Research
In vitro screening for paraben activity typically involves enzyme inhibition assays using recombinant 17β-HSD1 and 17β-HSD2. The standard protocol incubates the enzyme with its substrate (estrone for 17β-HSD1, estradiol for 17β-HSD2) and cofactor (NADPH for 17β-HSD1, NAD+ for 17β-HSD2) in the presence of varying concentrations of paraben test compounds [22]. Reaction products are quantified using HPLC or LC-MS/MS, and IC₅₀ values are calculated from dose-response curves. Cellular models include human granulosa COV434 cells endogenously expressing 17β-HSD1 to confirm enzyme inhibition in intact cells [22]. Molecular docking studies using crystal structures of target enzymes (e.g., PDB code: 1FDT) help predict binding modes and structure-activity relationships [22].
Key Research Reagents for Paraben Studies
| Research Reagent | Application | Function in Experimental Design |
|---|---|---|
| Recombinant 17β-HSD1/2 | Enzyme inhibition assays | Target proteins for screening paraben effects |
| NADP+/NADPH Cofactors | Enzyme activity measurements | Essential cofactors for HSD enzyme reactions |
| Estrone/Estradiol Standards | HPLC/LC-MS quantification | Reference standards for steroid quantification |
| Paraben Analytical Standards | Exposure assessment | Calibration standards for bio-monitoring |
| Molecular Docking Software | Structure-activity studies | Predict paraben-enzyme binding interactions |
Pesticides
Pyrethroids constitute an important class of extensively used insecticides identified as EDCs. Permethrin is one of the most commonly used pyrethroids and exists in multiple stereoisomeric forms due to two chiral centers in its structure [25]. These compounds are widely applied in agricultural and household settings, leading to human exposure through dietary residues, inhalation, and dermal contact. Despite their relatively low environmental persistence compared to organochlorine pesticides, pyrethroids are ubiquitous in the environment due to high-volume applications, and they have been detected in human biomonitoring studies [25].
Mechanisms of Reproductive Toxicity
Pyrethroids can interfere with reproductive function through multiple pathways. They have been shown to act as androgen receptor antagonists, potentially disrupting androgen signaling critical for male reproductive development and function [25]. Structural binding studies indicate that permethrin stereoisomers can compete with native ligands for binding to the androgen receptor ligand-binding domain, with potential to interfere with AR function [25]. Pyrethroid exposure has also been associated with altered serum levels of gonadotropins and testosterone in animal studies, suggesting disruption of the hypothalamic-pituitary-gonadal axis [25]. Additionally, some pyrethroids have demonstrated estrogenic activity in screening assays, indicating potential for mixed endocrine-disrupting effects.
Experimental Approaches for Pesticide Research
Computational approaches include induced fit docking simulations to study the structural binding characteristics of pesticide stereoisomers with nuclear receptors like the androgen receptor (PDB code: 2AM9) [25]. The methodology involves protein preparation (addition of hydrogens, optimization of hydrogen bond networks, energy minimization), ligand preparation (generation of stereoisomers), and induced fit docking that allows flexibility in both receptor and ligand [25]. In vitro validation utilizes reporter gene assays in AR-transfected cells to confirm antagonistic activity. Animal studies typically administer pesticides to rodents during critical developmental periods (e.g., gestational days 14-18) and assess reproductive outcomes in adulthood, including anogenital distance, sperm parameters, and reproductive organ weights [25].
Key Research Reagents for Pesticide Studies
| Research Reagent | Application | Function in Experimental Design |
|---|---|---|
| AR Reporter Cell Lines | Receptor activity screening | Detect AR antagonistic activity |
| Crystallized AR Protein | Structural studies | Reference structure for docking studies |
| Deuterated Pesticide Standards | Analytical quantification | Internal standards for exposure assessment |
| Stereoisomerically Pure Pesticides | Mechanistic studies | Test enantiomer-specific effects |
| Testosterone ELISA Kits | Hormone measurement | Quantify endocrine effects in vivo |
Per- and Polyfluoroalkyl Substances (PFAS)
Per- and polyfluoroalkyl substances (PFAS) are a class of synthetic chemicals characterized by strongly fluorinated alkyl chains that confer exceptional stability and persistence in the environment. Perfluorooctanoic acid (PFOA) and perfluorooctane sulfonic acid (PFOS) are two well-studied representatives of this class [24]. These compounds have been widely used in industrial and consumer products, including non-stick cookware, food packaging, stain-resistant fabrics, and fire-fighting foams. Due to their environmental persistence and bioaccumulation potential, PFAS are detected globally in human populations, with elimination half-lives of approximately 3.5 years for PFOA and 5.4 years for PFOS in humans [24].
Mechanisms of Reproductive Toxicity
PFAS compounds disrupt reproductive function through multiple interconnected mechanisms. In males, they induce apoptosis and autophagy in spermatogenic cells, disrupt Leydig cell function, cause oxidative stress in sperm, degrade intercellular junctions between Sertoli cells, and alter hypothalamic metabolome [24]. In females, PFAS exposure damages oocytes through oxidative stress, inhibits corpus luteum function, disrupts steroid hormone synthesis, impairs gap junction intercellular communication in follicles, and inhibits placental function [24]. These mechanisms collectively contribute to the observed adverse reproductive outcomes in both epidemiological studies and experimental models.
PFAS Reproductive Toxicity Mechanisms
Experimental Approaches for PFAS Research
Epidemiological studies typically employ cross-sectional or longitudinal designs measuring serum PFAS concentrations in relation to reproductive endpoints such as semen quality, reproductive hormone levels, and time-to-pregnancy [24]. Laboratory-based approaches include in vitro models using primary granulosa cells or placental cell lines to examine the effects of PFAS on steroidogenesis and cell viability, with typical exposure concentrations ranging from 0.1-100 μM [24]. Animal studies often use oral administration of PFAS (1-20 mg/kg/day) during critical developmental windows to assess long-term reproductive effects. Mechanistic studies focus on specific pathways, such as measuring oxidative stress markers, apoptosis assays, and gap junction communication in relevant cell types [24].
Key Research Reagents for PFAS Studies
| Research Reagent | Application | Function in Experimental Design |
|---|---|---|
| PFAS Analytical Standards | Exposure assessment | Quantification in environmental/biological samples |
| Oxidative Stress Assay Kits | Mechanism studies | Measure ROS production in gametes |
| Gap Junction Communication Dyes | Functional assays | Assess cell-to-cell communication in follicles |
| Apoptosis/Caspase Assay Kits | Cell death analysis | Quantify germ cell apoptosis |
| Steroid Hormone Antibodies | Immunoassays | Detect alterations in hormone production |
Comparative Analysis of EDC Classes
Table 1: Quantitative Comparison of Key EDC Parameters
| EDC Class | Representative Compounds | Primary Exposure Routes | Half-Life in Humans | Key Reproductive Effects |
|---|---|---|---|---|
| Bisphenols | BPA | Dietary, dermal, inhalation | Hours | Sperm alterations, testicular atrophy, hormonal imbalances, reduced ovarian reserve |
| Phthalates | DEHP, DBP, DiNP | Dietary, inhalation, dermal | ~12 hours | Reduced testosterone, sperm DNA damage, ovarian dysfunction, folliculogenesis disruption |
| Parabens | Methylparaben, Ethylparaben, Butylparaben | Dermal, dietary | Hours (rapid metabolism) | Estrogenic effects, inhibition of 17β-HSD enzymes, potential breast cancer links |
| Pesticides | Permethrin, Pyrethroids | Dietary, dermal, inhalation | Days | AR antagonism, altered gonadotropin levels, sperm quality reduction |
| PFAS | PFOA, PFOS | Dietary, drinking water | 3.5-5.4 years | Sperm count reduction, testicular hormone disruption, ovarian damage, placental dysfunction |
Table 2: Experimental Parameters for EDC Research
| EDC Class | Typical In Vitro Concentrations | Typical In Vivo Doses (Rodent) | Key Molecular Targets | Standard Assessment Methods |
|---|---|---|---|---|
| Bisphenols | 1 nM - 100 μM | 2-50 μg/kg/day (low dose) | ERα/ERβ, steroidogenic enzymes | Reporter assays, LC-MS, histological analysis |
| Phthalates | 1-100 μM (metabolites) | 50-1000 mg/kg/day | Steroidogenic enzymes, oxidative stress pathways | Urinary metabolites, hormone assays, sperm analysis |
| Parabens | 1-20 μM | 10-1000 mg/kg/day | 17β-HSD1, 17β-HSD2, estrogen receptors | Enzyme inhibition assays, cellular uptake studies |
| Pesticides | 0.1-50 μM | 1-100 mg/kg/day | Androgen receptor, neurotransmitter receptors | Docking simulations, receptor binding assays |
| PFAS | 0.1-100 μM | 1-20 mg/kg/day | Multiple nuclear receptors, gap junctions | Serum monitoring, oxidative stress markers, apoptosis assays |
The five major classes of EDCs reviewed—bisphenols, phthalates, parabens, pesticides, and PFAS—present significant challenges to reproductive health through diverse but overlapping mechanisms of action. Understanding these mechanisms at a molecular level is essential for developing targeted approaches to mitigate their impacts. Future research directions should include more comprehensive assessment of mixture effects, as humans are exposed to multiple EDCs simultaneously; elucidation of epigenetic mechanisms that may transmit EDC effects across generations; and development of sensitive biomarkers for early detection of reproductive dysfunction. For drug development professionals, these EDC pathways offer potential therapeutic targets for addressing EDC-induced reproductive impairments. Additionally, this mechanistic understanding should inform evidence-based public health policies aimed at reducing exposure to the most hazardous EDCs, particularly during vulnerable developmental windows.
Assessment and Intervention: Tools and Strategies for Reducing EDC Exposure
Validated Survey Instruments for Measuring EDC Avoidance Behaviors
Endocrine-disrupting chemicals (EDCs) pose a significant threat to reproductive health worldwide, with exposure linked to infertility, metabolic disorders, and adverse developmental outcomes [26] [27]. Within the broader context of reproductive health behavior and EDC avoidance theory research, the accurate measurement of avoidance behaviors is paramount for evaluating intervention efficacy and understanding behavioral determinants. This whitepaper provides researchers, scientists, and drug development professionals with a technical guide to currently available, validated survey instruments designed to quantify knowledge, perceptions, and behaviors related to reducing exposure to EDCs. The development of these tools represents a critical advancement in the field, moving beyond biomonitoring alone to capture the behavioral components necessary for effective public health strategies and clinical risk assessments [11] [15].
Theoretical Frameworks in EDC Avoidance Research
The design and interpretation of EDC avoidance behavior surveys are predominantly guided by established health behavior theories, which provide a structured framework for understanding the psychological determinants of protective actions.
The Health Belief Model (HBM)
The Health Belief Model (HBM) serves as the foundational framework for several prominent questionnaires [28] [3]. This model posits that avoidance behaviors are influenced by an individual's perception of their susceptibility to a health threat, the severity of that threat, the benefits of taking action, and the barriers to doing so, moderated by cues to action and self-efficacy. A questionnaire developed for women in the preconception and conception periods operationalizes this model by measuring knowledge, health risk perceptions, beliefs, and avoidance behaviors related to six specific EDCs (lead, parabens, BPA, phthalates, triclosan, and perchloroethylene) found in personal care and household products [28]. The instrument demonstrated strong internal consistency (Cronbach's alpha), confirming its reliability for research purposes. Analyses using this tool revealed that greater knowledge and higher risk perceptions for specific EDCs like parabens and phthalates were significant predictors of avoidance behavior, highlighting the model's utility in identifying key behavioral levers [3].
Factor-Analytically Derived Constructs
As an alternative to theory-driven approaches, some instruments derive their structure empirically from participant responses. The Korean survey on reproductive health behaviors for reducing EDC exposure was developed through a rigorous methodological study involving 288 adults [11]. Exploratory and confirmatory factor analyses identified a four-factor structure underlying EDC avoidance behaviors:
- Health behaviors through food (e.g., avoiding canned or plastic-packaged foods)
- Health behaviors through breathing (e.g., ensuring ventilation)
- Health behaviors through skin (e.g., choosing products free of certain chemicals)
- Health promotion behaviors (broader health actions linked to EDC avoidance) This factor structure, which accounts for exposure routes (food, respiratory pathways, and skin absorption), offers a validated model for assessing EDC avoidance that is grounded in observed data rather than pre-existing theoretical constructs [11].
The following diagram illustrates the key theoretical constructs and their relationships as measured by these survey instruments.
Comprehensive Table of Validated Survey Instruments
The following table summarizes the key characteristics of validated instruments available for measuring EDC avoidance behaviors.
Table 1: Validated Survey Instruments for Measuring EDC Avoidance Behaviors
| Instrument Name & Citation | Target Population | Theoretical Foundation/Constructs | Key Domains Measured | Response Format & Items | Reliability & Validity Metrics |
|---|---|---|---|---|---|
| Reproductive Health Behavior Survey for EDC Reduction [11] | Adult men and women (general population) | Factor-analytically derived structure (4 factors) | 1. Health behaviors through food2. Health behaviors through respiration3. Health behaviors through skin4. Health promotion behaviors | 19 items, 5-point Likert scale | Internal consistency (Cronbach's α ≥ 0.80); Content validity (CVI > 0.80); Construct validity via EFA/CFA |
| EDC Knowledge, Risk Perceptions, and Avoidance Questionnaire [28] [3] | Women (preconception & conception periods, ages 18-35) | Health Belief Model (HBM) | 1. Knowledge (access to resources)2. Health risk perceptions3. Beliefs4. Avoidance behaviors | 6 EDCs x 24 items, 5- and 6-point Likert scales | Strong internal consistency (Cronbach's α) for all constructs; Predictive validity established |
| Endocrine Disruptor Awareness Scale (EDCA) [29] | Medical students and physicians | Validated awareness scale | 1. General awareness2. Impact awareness3. Exposure and protection awareness | 24 items, 5-point Likert scale | Validated instrument; Scores interpreted as Very Low to Very High; Used in cross-sectional studies |
Detailed Methodologies for Instrument Development and Validation
The surveys presented in this guide were developed through rigorous, multi-stage validation protocols. The following diagram outlines a generalized workflow for this process, integrating common steps from several studies.
Initial Item Generation and Content Validation
The development of a robust survey instrument begins with comprehensive item generation. This typically involves a systematic review of existing literature and previously used questionnaires to create an initial pool of items that comprehensively cover the domain of interest [11] [28]. For instance, the Korean Reproductive Health Behavior survey started with 52 initial items derived from literature published between 2000 and 2021, covering behaviors across major exposure routes (food, respiration, skin) [11].
Content validity is subsequently established through review by a panel of experts. The Korean study engaged five experts, including chemical/environmental specialists, a physician, a nursing professor, and a language expert, to rate each item's relevance [11]. The standard metric for this stage is the Content Validity Index (CVI), with items typically requiring an I-CVI of above 0.80 to be retained. Items failing to meet this threshold are removed or revised based on expert feedback [11].
Pilot Testing and Data Collection
A critical step before large-scale deployment is pilot testing with a small sample from the target population. This phase assesses practical aspects such as item clarity, comprehension, response time, and the overall layout of the questionnaire. For example, the Korean survey was pilot-tested with ten adults to identify and refine unclear or difficult-to-answer items [11]. This process ensures that the final instrument is user-friendly and that the data collected will be of high quality.
Determining the appropriate sample size for the main validation study is crucial. For factor analysis, a common rule of thumb is to have a sample size at least five to ten times the number of items. The Korean study, accounting for a 10% dropout rate, aimed for 330 participants and analyzed data from 288 respondents after excluding unreliable responses, which is considered sufficient for stable validation, particularly when communality is low [11].
Psychometric Validation: Factor Analysis and Reliability
The core of instrument validation lies in psychometric testing, primarily through factor analysis and reliability assessment.
- Exploratory Factor Analysis (EFA): This data reduction technique is used to identify the underlying factor structure of the questionnaire without pre-defined constraints. Researchers assess the suitability of the data for EFA using the Kaiser-Meyer-Olkin (KMO) measure and Bartlett's test of sphericity. Factors are typically extracted based on eigenvalues greater than 1 and examination of the scree plot, with the goal of a cumulative explained variance of at least 50% [11]. Items with low factor loadings (e.g., below 0.40) or low communalities are considered for removal.
- Confirmatory Factor Analysis (CFA): Following EFA, CFA tests how well the identified factor structure fits the data. This involves evaluating model fit using absolute fit indices such as the Chi-square test, Standardized Root Mean Square Residual (SRMR), and Root Mean Square Error of Approximation (RMSEA) [11]. CFA confirms that the theoretical model derived from EFA is statistically sound.
- Reliability Testing: The internal consistency of the final instrument and its subscales is quantified using Cronbach's alpha. A value of at least 0.70 is acceptable for newly developed scales, while 0.80 or higher is preferred for established instruments [11] [28]. The EDC questionnaire for women demonstrated strong Cronbach's alpha values across all its constructs [28].
Table 2: Essential Research Reagents and Resources for EDC Behavioral Studies
| Resource Category | Specific Example(s) | Function/Purpose in Research |
|---|---|---|
| Validated Surveys | Reproductive Health Behavior Survey [11]EDC Knowledge & Avoidance Questionnaire [28] [3]Endocrine Disruptor Awareness Scale (EDCA) [29] | Core instruments for quantitatively measuring knowledge, perceptions, and self-reported avoidance behaviors in study populations. |
| Biomonitoring Kits | Million Marker (MM) mail-in urine testing kit [9] | Provides objective measurement of internal exposure levels to specific EDCs (e.g., BPA, phthalates, parabens) for correlating with survey data. |
| Data Analysis Software | IBM SPSS Statistics, IBM SPSS AMOS [29] [11] | Statistical software packages used for data management, item analysis, exploratory factor analysis (EFA), and confirmatory factor analysis (CFA). |
| Theoretical Frameworks | Health Belief Model (HBM) [28] [3] | Provides a conceptual structure for designing survey items and interpreting the psychological determinants of avoidance behavior. |
| External Product Databases | Environmental Working Group Guide [28]Yuka App [28] | Independent resources for verifying or classifying the chemical composition of personal care and household products reported by study participants. |
The availability of rigorously validated survey instruments marks a significant advancement in the study of EDC avoidance within reproductive health behavior research. The tools summarized in this whitepaper, grounded in theoretical models like the Health Belief Model or derived empirically through factor analysis, provide researchers with reliable and valid means to quantify critical variables. Their development through systematic processes—including expert content validation, pilot testing, and robust psychometric analysis—ensures their utility for generating high-quality, interpretable data. The integration of these surveys with biomonitoring and clinical biomarkers, as seen in emerging intervention protocols [9], represents the future of the field. This multi-faceted approach will ultimately accelerate our understanding of the determinants of EDC avoidance and inform the development of more effective public health interventions and clinical guidelines aimed at protecting reproductive and developmental health globally.
Biomonitoring, the measurement of chemicals or their metabolites in human specimens, provides a direct assessment of internal exposure to environmental pollutants. For endocrine-disrupting chemicals (EDCs), urinary biomarker analysis has become a cornerstone of exposure assessment, offering critical insights into the relationship between environmental factors and reproductive health outcomes. Within the context of reproductive health behaviors and EDC avoidance theory, understanding these exposure-assessment methodologies is fundamental for developing effective intervention strategies. The average U.S. adult uses approximately 12 personal care products daily containing an estimated 112 unique chemical ingredients, creating significant potential for EDC exposure through dermal absorption, inhalation, and ingestion [30].
This technical guide examines current methodologies in urinary biomonitoring, with particular emphasis on their application to EDC exposure assessment in reproductive health research. We present analytical protocols, validation frameworks, and data interpretation strategies that enable researchers to quantify exposure biomarkers with precision and relate these measurements to relevant health endpoints. With proper implementation, these approaches can identify exposure sources, inform avoidance behaviors, and ultimately contribute to improved reproductive health outcomes across populations.
Analytical Methodologies for Urinary Biomarker Assessment
Specimen Collection and Handling Protocols
Proper specimen collection and handling are fundamental to obtaining reliable biomonitoring data. Established protocols should minimize contamination and analyte degradation throughout the process [30].
- Collection Materials: Use pre-cleaned polypropylene urine collection cups to avoid contamination from sampling materials. Avoid containers with plasticizers that may leach into specimens [30].
- Timing of Collection: First-morning void samples are preferred for EDC biomonitoring as they represent concentrated urine after overnight accumulation, providing an integrated measure of exposure over the preceding hours [30].
- Temperature Control: Immediately refrigerate samples after collection and freeze at -80°C within hours of collection if analysis cannot be performed immediately. Multiple freeze-thaw cycles should be avoided as they can degrade labile metabolites [30].
- Shipping Considerations: When transporting samples to analytical facilities, use overnight shipping with cold packs or dry ice to maintain sample integrity during transit [30].
Analytical Techniques for EDC Biomarker Quantification
Liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS) has emerged as the gold standard for quantifying EDC metabolites in urine due to its high sensitivity and specificity [30].
Table 1: Primary Analytical Techniques for Urinary EDC Biomarker Quantification
| Technique | Applications | Key Advantages | Limitations |
|---|---|---|---|
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Simultaneous quantification of multiple EDC classes (phthalates, parabens, bisphenols) | High sensitivity and specificity; ability to measure multiple analytes in single run; wide dynamic range | Requires specialized equipment and expertise; higher operational costs |
| Enzyme-Linked Immunosorbent Assay (ELISA) | High-throughput screening of specific EDC classes | Lower cost; suitable for large sample numbers; minimal specialized equipment needed | Potential for cross-reactivity; generally less specific than MS methods |
| Gas Chromatography-Mass Spectrometry (GC-MS) | Analysis of volatile EDCs and their metabolites | Excellent separation efficiency; well-established libraries for compound identification | Often requires derivatization; less ideal for thermally labile compounds |
The LC-MS/MS workflow for EDC biomarker analysis typically involves several critical steps [30]:
- Sample Preparation: 100 μL of urine is combined with 100 μL of water, followed by addition of isotopically labeled internal standards to correct for matrix effects and recovery variations.
- Enzymatic Hydrolysis: Samples are incubated with β-Glucuronidase enzyme for 2 hours to deconjugate glucuronidated metabolites, releasing the parent compounds for measurement.
- Chromatographic Separation: Reverse-phase chromatography separates analytes based on hydrophobicity before introduction to the mass spectrometer.
- Mass Spectrometric Detection: Multiple reaction monitoring (MRM) provides highly specific quantification of target analytes by monitoring precursor-to-product ion transitions.
Biomarkers of Interest in Reproductive Health Research
Key EDC Classes and Their Urinary Biomarkers
Several classes of EDCs with demonstrated impacts on reproductive health are routinely monitored through urinary biomarkers.
Table 2: Primary EDC Classes and Corresponding Urinary Biomarkers in Reproductive Health Research
| EDC Class | Common Sources | Urinary Biomarkers | Reproductive Health Concerns |
|---|---|---|---|
| Phthalates | Personal care products, plastics, food packaging | MEP, MBP, MEHP, MEHHP, MECPP | Reduced ovarian reserve, altered pubertal timing, testicular dysgenesis syndrome [30] [31] [32] |
| Parabens | Cosmetics, pharmaceuticals, food preservatives | MePB, EPB, PPB, BUP | Estrogenic activity, altered steroidogenesis, potential impacts on fertility [30] [33] |
| Bisphenols | Food can linings, thermal paper, plastics | BPA, BPS, BPF | Endometriosis, PCOS, implantation failure, reduced sperm quality [30] [31] |
| Benzophenones | Sunscreens, cosmetic products | Oxybenzone (OBZ) | Estrogenic and anti-estrogenic activities, potential impacts on female reproduction [30] |
Biomarker Selection Considerations
When designing a biomonitoring study focused on reproductive health, several factors influence biomarker selection [34]:
- Biological Persistence: Compounds with shorter biological half-lives (e.g., phthalates, parabens) require careful timing of sample collection relative to exposure events.
- Specificity: Some biomarkers are specific to single compounds (e.g., BPA), while others represent metabolites of multiple precursor compounds.
- Reproductive Relevance: Prioritize biomarkers with established mechanistic links to reproductive endpoints based on experimental and epidemiological evidence.
Experimental Protocols for Exposure Assessment Studies
Integrated Exposure Assessment Protocol
The Million Marker study provides a robust protocol for comprehensive EDC exposure assessment combining urinary biomonitoring with exposure journaling [30]:
Study Population Considerations [30]:
- Target population: Adults of reproductive age (typically 18-40 years)
- Exclusion criteria: Pregnancy, known diagnoses of cancer, metabolic disorders, or kidney disease
- Stratification by sex crucial due to differential product use and exposure patterns
Exposure Journal Implementation:
- Participants document all personal care products, household products, and dietary supplements used 24 hours prior to sample collection
- Product ingredients of concern are cataloged using standardized classification systems
- Digital platforms can facilitate real-time tracking and reduce recall bias
Ethical Considerations:
- Institutional Review Board approval required for human subjects research
- Informed consent must address specific handling of sensitive health and exposure data
- Plan for report-back of individual results to participants with appropriate contextualization
Quality Assurance and Quality Control Procedures
Rigorous QA/QC measures ensure the reliability of biomonitoring data [34]:
- Method Validation: Establish linearity, precision, accuracy, recovery, and limits of detection/quantification for each analyte.
- Batch Quality Monitoring: Include calibration standards, quality control pools (low, medium, high), and blank samples in each analytical batch.
- Blind Reanalysis: Randomly select 5-10% of samples for duplicate analysis to assess reproducibility.
Statistical Approaches for Biomarker Data Analysis
Data Normalization and Preprocessing
Urinary biomarker concentrations require appropriate normalization to account for urine dilution [30]:
- Specific Gravity Correction: SG = (SGsample - 1)/(SGreference - 1) where SG_reference is typically the population median.
- Creatinine Adjustment: Concentrationadj = Concentrationraw × (Creatininereference/Creatininesample).
- Log-Transformation: Often applied to normalize right-skewed distributions of biomarker concentrations.
Exposure-Response Relationship Analysis
Statistical modeling approaches illuminate relationships between EDC exposures and health parameters [35]:
- Multiple Regression Models: Assess associations between urinary biomarker levels and self-reported health status, adjusting for potential confounders (age, sex, BMI, socioeconomic factors).
- Generalized Linear Mixed Models: Account for correlated measurements in longitudinal study designs.
- Machine Learning Approaches: Uncover complex, non-linear exposure-response patterns in high-dimensional biomonitoring data.
Key considerations for statistical analysis of ERC biomarker data include [34]:
- Control of multiple comparisons when testing numerous biomarker-health endpoint associations
- Assessment of effect modification by sex, given sexually dimorphic responses to EDCs
- Evaluation of non-monotonic dose-response relationships characteristic of endocrine disruptors
The Researcher's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Reagents and Materials for Urinary Biomarker Analysis
| Category | Specific Items | Application Notes |
|---|---|---|
| Sample Collection | Polypropylene urine cups, cryovials, cold packs, shipping containers | Avoid polystyrene and PVC materials that may leach contaminants [30] |
| Analytical Standards | Isotopically labeled internal standards (e.g., d4-BPA, d4-MEP), native analyte standards | Use isotopically labeled standards for each target analyte to correct for matrix effects [30] |
| Enzymes & Buffers | β-Glucuronidase (E. coli or Helix pomatia), ammonium acetate, ammonium hydroxide | Enzyme purity critical to avoid introduction of contaminants [30] |
| Chromatography | HPLC-grade solvents (methanol, acetonitrile, water), reversed-phase columns (C18) | LC columns with sub-2μm particles provide superior separation efficiency [30] |
| Quality Control | Certified reference materials, pooled human urine, third-party proficiency testing samples | Participate in interlaboratory comparison programs to ensure data comparability [34] |
Integration with Reproductive Health Assessment
The connection between EDC exposure and reproductive health outcomes is mechanistically grounded in the endocrine system's role in regulating reproductive function across the lifespan [31] [32].
Critical windows of susceptibility to EDC exposure include [32]:
- In Utero Development: Sexual differentiation highly dependent on fetal hormonal environment
- Puberty: Activation of hypothalamic-pituitary-gonadal axis represents another vulnerable period
- Reproductive Age: Ongoing exposure may affect gamete quality, ovarian reserve, and endocrine function
Emerging approaches in reproductive health biomonitoring include [36]:
- Cohort Linkage Studies: Integrating HBM data with electronic health records to access objective reproductive health endpoints
- Mixture Analysis: Statistical methods to assess combined effects of multiple EDCs
- Longitudinal Designs: Repeated biomonitoring across critical life stages to capture exposure dynamics
Urinary biomonitoring approaches provide powerful tools for quantifying exposure to EDCs relevant to reproductive health. The methodologies outlined in this guide—from standardized sample collection to advanced analytical techniques and statistical analysis—enable researchers to generate high-quality exposure data suitable for testing hypotheses about EDC avoidance behaviors and reproductive outcomes. As this field advances, integration of biomonitoring with mechanistic toxicology and epidemiological research will strengthen the evidence base needed to inform public health interventions and regulatory policies aimed at reducing EDC exposures during critical windows of reproductive susceptibility.
Dietary modification represents a frontline defense against exposure to endocrine-disrupting chemicals (EDCs), particularly for individuals during reproductive life stages. The reproductive life cycle, encompassing menarche to menopause for women and post-pubertal stages for men, contains periods of exceptional vulnerability to environmental exposures [15]. Exposures during the preconception and perinatal stages can trigger unfavorable health outcomes that manifest across the lifespan [15]. EDCs such as bisphenols (BPs) and phthalates, which have been detected in over 90% of the US population, are known to infiltrate the food supply through multiple vectors including plastic foodware, can linings, and food processing equipment [9]. This technical guide synthesizes current evidence and methodologies for dietary interventions within a theoretical framework of reproductive health behavior, providing researchers and drug development professionals with experimentally validated approaches to reduce body burden of foodborne contaminants.
Regulatory and Theoretical Framework
EDCs in the Food Supply: Exposure Routes and Health Implications
Endocrine-disrupting chemicals present in food exert their effects through multiple molecular pathways, primarily by mimicking or blocking endogenous hormones such as estrogen, androgen, and thyroid hormones [11]. Bisphenol A (BPA), used in polycarbonate plastics and epoxy resins found in food containers and can linings, exhibits estrogenic activity and has been linked to infertility, cardiovascular disease, and developmental effects [9]. Phthalates, employed as plasticizers and in fragrance dispersal, demonstrate antiandrogenic effects and are associated with male reproductive developmental abnormalities and metabolic disorders [9]. The relatively short biological half-lives of these compounds (6 hours to 3 days) presents a strategic opportunity for intervention, as reduction or elimination of exposure sources can rapidly decrease internal dose [9].
Regulatory Context and Future Directions
Current regulatory landscapes are evolving rapidly to address chemical exposures in food. The FDA's Human Food Program (HFP) has identified food chemical safety as a FY 2025 priority, with specific commitments to strengthen pre-market review processes, enhance post-market assessment frameworks, and advance "Closer to Zero" initiatives establishing action levels for environmental contaminants in foods intended for infants and young children [37]. Simultaneously, the Make America Healthy Again (MAHA) Commission has recommended sweeping reforms, including systematic post-market review of food chemicals, potential modification of the GRAS (Generally Recognized as Safe) notification framework, and development of a government-wide definition for "ultra-processed food" [38]. These regulatory shifts underscore the timeliness of research into effective dietary interventions, particularly for reproductive-aged populations.
Evidence-Based Dietary Intervention Strategies
Documented Intervention Modalities
Recent clinical and community-based trials have yielded critical insights into effective intervention modalities for reducing dietary EDC exposure. The REED (Reducing Exposures to Endocrine Disruptors) study, a randomized controlled trial protocol, exemplifies the current gold standard in intervention research, combining biometric monitoring with personalized educational curricula [9]. Similarly, research by Kim et al. has resulted in the development and validation of a 19-item survey instrument specifically designed to assess reproductive health behaviors aimed at reducing EDC exposure through food, respiratory, and dermal routes [11] [39]. The most successful interventions incorporate three core components: accessible educational resources, targeted product replacement, and personalized behavioral support [15].
Table 1: Efficacy of Documented Dietary Intervention Strategies for EDC Reduction
| Intervention Strategy | Target Population | Key EDCs Measured | Reported Efficacy | Behavioral Measures |
|---|---|---|---|---|
| Personalized Report-Back (REED Study Protocol) | Reproductive-aged men and women (n=600) | Bisphenols, Phthalates, Parabens, Oxybenzone | Significant decrease in monobutyl phthalate post-intervention (p<0.001) [9] | 50% reported using non-toxic personal products; 32% ate less packaged food [9] |
| Educational Curriculum with Live Counseling | Subset of REED participants | Bisphenols, Phthalates | Increased readiness to change in women (p=0.053); Improved EHL behaviors (p=0.003) [9] | 44% used non-toxic household products; 40% used less plastic [9] |
| Web-Based Educational Resources | Reproductive-aged adults | Phthalates, Phenols | Promising strategy for reducing EDC concentrations [15] | Accessible format supported adherence to recommended behaviors |
| Toxic Product Replacement | Reproductive-aged women | Phthalates, Phenols | Identified as promising intervention strategy [15] | Targeted replacement of known exposure sources |
Quantitative Outcomes of Dietary Interventions
The efficacy of dietary interventions must be quantified through both biomonitoring data and documented behavioral changes. In previous research by the Million Marker team, report-back interventions incorporating urinary biomarker measurements and personalized recommendations demonstrated statistically significant reductions in specific phthalate metabolites [9]. Beyond biomarker data, successful interventions track modifications in consumer behavior and dietary patterns, including reduced consumption of canned foods, decreased use of plastic foodware, and increased selection of fresh, unpackaged foods [9]. These behavioral modifications align theoretically with the reproductive health behavior model that emphasizes proactive, health-promoting actions to preserve reproductive capacity [11].
Table 2: Biomarker Changes and Behavioral Outcomes Following Dietary Interventions
| Intervention Component | Biomarker Outcome | Statistical Significance | Behavioral Outcome | Population Segment Showing Greatest Benefit |
|---|---|---|---|---|
| Report-Back of Urinary EDC Levels | Decrease in monobutyl phthalate | p<0.001 [9] | 48% read product labels more frequently [9] | Women showed increased readiness to change [9] |
| Personalized Recommendations | Not specified | - | 20% dined out less frequently; 32% ate less packaged food [9] | Participants with higher baseline EHL [9] |
| EDC-Specific Education | Increased EHL behaviors | p=0.003 [9] | 44% switched to non-toxic household products [9] | Older participants and those in poorer health at baseline [9] |
Experimental Protocols and Methodologies
Randomized Controlled Trial Protocol: The REED Study
The REED study exemplifies a comprehensive methodological approach to evaluating dietary interventions for EDC reduction. The protocol employs a randomized controlled design with target enrollment of 600 reproductive-aged participants (300 women and 300 men) recruited from the Healthy Nevada Project population cohort [9]. Key methodological components include:
Biomonitoring Protocol: Participants utilize at-home urine collection kits to measure concentrations of bisphenols (BPA, BPS, BPF), phthalate metabolites (MBP, MBzP, MEP, DEHP metabolites), parabens (methyl-, ethyl-, propyl-, butyl-), and oxybenzone preceding and following the intervention period [9]. Samples are analyzed via liquid chromatography-tandem mass spectrometry (LC-MS/MS) with rigorous quality control measures.
Intervention Components: The experimental arm receives a multi-component intervention including: (1) a self-directed online interactive curriculum detailing EDC exposure sources and avoidance strategies; (2) live counseling sessions modeling the Diabetes Prevention Program; (3) personalized report-back of biomarker results with specific, actionable recommendations for dietary modification; and (4) ongoing support through digital communication platforms [9].
Outcome Measures: Primary outcomes include changes in EH literacy (EHL) measured through validated surveys, readiness to change (RtC) assessed using trans-theoretical model constructs, and urinary EDC metabolites quantified via LC-MS/MS. Secondary outcomes include changes in clinical biomarkers (lipids, glucose, thyroid function, inflammatory markers) measured through at-home blood collection kits [9].
The following diagram illustrates the experimental workflow:
Survey Validation Methodology
For research focusing specifically on behavioral outcomes, Kim et al. detail a rigorous methodological approach for developing and validating assessment tools [11] [39]. The protocol includes:
Instrument Development: Initial item generation through comprehensive literature review (2000-2021) yields 52 preliminary items measuring behaviors across three EDC exposure routes: food, respiration, and skin absorption [11]. Expert panels (n=5) assess content validity using Item-Content Validity Index (I-CVI) thresholds >0.80, followed by pilot testing with target population representatives to refine item clarity and response format [11].
Psychometric Validation: The validation phase employs a cross-sectional design with 288 South Korean adults recruited across eight metropolitan areas [11]. Statistical analyses include exploratory factor analysis (EFA) with principal component analysis and varimax rotation, confirmatory factor analysis (CFA) to verify model fit, and reliability assessment using Cronbach's alpha [11]. The final 19-item instrument demonstrates robust psychometric properties across four factors: health behaviors through food, breathing, skin, and health promotion behaviors [11].
Research Implementation Toolkit
Essential Research Reagents and Materials
Table 3: Essential Research Materials for Dietary Intervention Studies
| Research Material/Reagent | Specifications | Research Application | Theoretical Basis |
|---|---|---|---|
| Urine Collection Kit | Sterile polypropylene containers, preservative-free | Biomonitoring of non-persistent EDCs | Captures recent exposure (half-lives 6h-3d) [9] |
| LC-MS/MS System | Triple quadrupole mass spectrometer, C18 column | Quantification of EDC metabolites | High sensitivity for trace-level biomarkers [9] |
| EDC Metabolite Standards | Isotope-labeled internal standards (e.g., BPA-d16, MEP-d4) | Instrument calibration and quantification | Corrects for matrix effects and recovery [9] |
| Validated EHL Survey | 19-item, 5-point Likert scale, 4 factors | Measuring intervention effectiveness | Based on reproductive health behavior theory [11] [39] |
| Online Educational Curriculum | Interactive modules, exposure source visualizations | Intervention delivery | Increases knowledge and readiness to change [9] |
Analytical Framework for Intervention Research
The following diagram illustrates the conceptual relationships between intervention components and theoretical constructs in EDC avoidance research:
Dietary modification interventions represent a promising, evidence-based approach to reducing EDC exposure among reproductive-aged populations. Current research indicates that successful interventions incorporate biomonitoring feedback, personalized educational resources, and theory-based behavioral support to achieve statistically significant reductions in phthalate and phenol exposures [9] [15]. The validated survey instrument developed by Kim et al. provides researchers with a critical tool for assessing intervention effectiveness within a theoretical framework of reproductive health behavior [11] [39].
Significant knowledge gaps remain, particularly regarding interventions tailored for male reproductive health and long-term sustainability of exposure reductions [15]. Future research should prioritize larger-scale clinical trials, investigation of clinical biomarker improvements following exposure reduction, and development of culturally adapted interventions for diverse populations [9] [15]. As regulatory frameworks evolve to address chemical exposures in food [37] [38], rigorously tested dietary interventions will play an increasingly vital role in protecting reproductive health across the lifespan.
Endocrine-disrupting chemicals (EDCs) represent a significant and pervasive threat to reproductive health worldwide. These exogenous substances interfere with the normal functioning of the endocrine system, leading to adverse health outcomes in healthy organisms and their subsequent generations [40]. The reproductive life cycle, encompassing periods from menarche to menopause for females and after pubertal onset for males, contains vulnerable windows where EDC exposure can have profound and lasting consequences, including infertility, reproductive cancers, and developmental disorders in offspring [40] [15]. Despite consistent evidence linking EDCs to adverse health effects, risk assessments and policy interventions often develop slowly, creating an urgent need for evidence-based, personal exposure reduction strategies [15].
Product replacement strategies form a crucial component of a multi-faceted approach to reducing EDC exposure. The ubiquitous presence of EDCs in daily-use items—from plastics and personal care products to cleaning supplies—makes consumer product substitution a practical and powerful intervention point [40] [41]. This whitepaper provides an in-depth technical guide to product replacement strategies within the context of EDC avoidance theory, synthesizing current market trends, experimental evidence on intervention efficacy, and specific substitution methodologies tailored for researchers, scientists, and drug development professionals.
Endocrine-Disrupting Chemicals: Mechanisms and Health Implications
Pathophysiological Mechanisms of EDCs
Endocrine-disrupting chemicals exert their effects through multiple molecular pathways, with the hypothalamic-pituitary-gonadal (HPG) axis serving as a primary target. The HPG axis is the central regulator of reproductive function, controlling processes such as folliculogenesis, ovulation, spermatogenesis, and steroidogenesis [40]. EDCs, including bisphenol A (BPA), phthalates (PAEs), parabens, and polychlorinated biphenyls (PCBs), can mimic or block hormonal actions, thereby disrupting the delicate feedback mechanisms that govern hormone production and secretion.
Even miniscule amounts of EDC exposure can disturb multiple physiological systems simultaneously, with effects that may manifest only after long latency periods [42]. The timing of exposure is critical, with early developmental stages representing particularly vulnerable windows where EDC exposure can program lifelong susceptibility to disease. EDCs are known to be effective in various types of cancers (testicular, prostate, thyroid, breast), reproductive dysfunctions (precocious puberty, infertility), diabetes, obesity, and neurodevelopmental diseases [42].
EDC Exposure and Reproductive Health Outcomes
Accumulating evidence from animal models and human epidemiological studies highlights the relationship between EDC exposure and an array of reproductive disorders. In females, these disorders encompass uterine fibroids (UFs), endometriosis (EMs), polycystic ovary syndrome (PCOS), diminished ovarian reserve (DOR), premature ovarian insufficiency (POI), infertility, and hormone-sensitive cancers [40]. In males, EDC exposure has been linked to cryptorchidism, hypospadias, reduced sperm quality, and prostate and testicular cancers [40].
Table 1: Common EDCs, Their Sources, and Documented Reproductive Health Effects
| EDC Class | Common Sources | Documented Reproductive Health Effects |
|---|---|---|
| Bisphenol A (BPA) | Plastics, epoxy resins, food can linings, thermal paper [40] | Promotes proliferation of human uterine leiomyoma cells; linked to infertility, PCOS, and hormone-sensitive cancers [40] |
| Phthalates (PAEs) | Vinyl flooring, plastic packaging, personal care products, fragrances [40] [42] | Associated with altered reproductive development, reduced sperm quality, infertility, and endometriosis [40] [42] |
| Parabens | Cosmetics, body creams, hair products, sunscreens [43] [40] | Possess hormone-disrupting properties; linked to breast cancer and reproductive dysfunction [43] [40] |
| PFAS | Non-stick cookware, stain-resistant fabrics, some cosmetics [43] | Added to cosmetics to enhance skin penetration; suspected endocrine-disrupting traits [43] |
| Triclosan | Antibacterial soaps, hand sanitizers, some deodorants [43] | Potential endocrine disruptor; often found in products with antibacterial properties [43] |
The following diagram illustrates the central mechanism through which EDCs disrupt the hypothalamic-pituitary-gonadal (HPG) axis, leading to adverse reproductive health outcomes:
Market Context and Consumer Awareness
Growth of the Sustainable Product Market
The household cleaning products market has demonstrated significant growth, valued at USD $180.8 billion in 2023 and reaching $189.2 billion in 2024, reflecting a year-over-year growth of 4.6% [44]. This expansion is partly driven by increased consumer demand for sustainable and eco-friendly alternatives. The global market for eco-friendly cleaning products is projected to reach $40.4 billion by 2026, growing at a compound annual growth rate (CAGR) of 9.4% [44]. Similarly, the global market for natural cleaning products was valued at $6.8 billion in 2023 and is expected to grow at a CAGR of 7.8% through 2030 [44].
The e-commerce channel for household cleaning products has seen explosive growth, valued at $50.3 billion in 2023 and expected to reach $56.1 billion by 2025, growing at a CAGR of 5.6% [44]. This shift in purchasing behavior facilitates access to specialized, cleaner product alternatives that may not be available in traditional brick-and-mortar stores.
Table 2: Market Growth Indicators for Cleaning and Personal Care Products
| Market Segment | Market Size (2023) | Projected Size | Growth Rate (CAGR) | Key Drivers |
|---|---|---|---|---|
| Global Household Cleaning Products | $189.2 billion [44] | N/A | 4.6% (YoY 2023-2024) [44] | Hygiene awareness, sustainability demands, natural ingredients [44] |
| Eco-Friendly Cleaning Products | N/A | $40.4 billion by 2026 [44] | 9.4% [44] | Environmental concerns, regulatory compliance, consumer health awareness [44] [45] |
| Natural Cleaning Products | $6.8 billion [44] | Growing through 2030 [44] | 7.8% [44] | Consumer preference for non-toxic formulas, natural scents, ingredient transparency [44] |
| E-Commerce Household Cleaning | $50.3 billion [44] | $56.1 billion by 2025 [44] | 5.6% [44] | Convenience, subscription models, broader product selection [44] |
Awareness Gaps and Public Health Imperative
Despite the widespread presence of EDCs and growing market alternatives, significant awareness gaps persist. A cross-sectional study conducted among pregnant women and new mothers at a tertiary care hospital revealed that 59.2% of participants were unfamiliar with EDCs, and many lacked awareness of associated health risks including cancers, infertility, and developmental disorders in children [42]. A significant portion of respondents had never heard of bisphenol A (BPA) or phthalates, while awareness of parabens was relatively higher [42].
This awareness gap is particularly concerning for vulnerable populations, as exposure to EDCs during critical periods of development can result in long-term, detrimental health effects on fetuses and infants [42]. The interval between EDC exposure and disease development varies, making it difficult to detect diseases caused by EDCs and emphasizing the importance of preventive strategies [42].
Evidence-Based Product Replacement Strategies
Experimental Protocols for EDC Exposure Reduction
Intervention studies to reduce EDC exposure have employed various methodological approaches, with educational, behavioral, and direct product replacement strategies showing promise. A comprehensive review of 21 primary interventions identified accessible web-based educational resources, targeted replacement of known toxic products, and personalized intervention through meetings and support groups as the most promising strategies for reducing phthalate and phenol concentrations [15].
Typical experimental protocols involve pre- and post-intervention biomonitoring to measure urinary or serum concentrations of EDC biomarkers, coupled with educational components and, in some cases, direct provision of alternative products. Successful protocols often include:
- Baseline Biomonitoring: Collection of urine samples for analysis of phthalate metabolites, phenol derivatives, and other EDC biomarkers before intervention.
- Educational Component: Structured information about EDC sources, health effects, and avoidance strategies, delivered through in-person sessions, written materials, or web-based platforms.
- Product Replacement: Direct provision of or guidance toward alternative products free of targeted EDCs.
- Follow-up Biomonitoring: Repeated biological sampling to quantify changes in EDC biomarkers post-intervention.
- Behavioral Assessment: Questionnaires to evaluate changes in product use and purchasing behaviors.
The following workflow diagram outlines a generalized experimental design for evaluating the efficacy of product replacement interventions:
Household Cleaning Product Replacements
The household cleaning products market is experiencing a significant shift toward sustainability and safety, driven by consumer awareness of both hygiene and environmental impact [44] [45]. Key replacement strategies include:
Surfactant Replacement: Petro-based surfactants are being replaced by milder options such as alkyl polyglucosides (APGs), amphoacetates, betaines, and sarcosinates [45]. These alternatives maintain cleaning efficacy while reducing potential health risks and environmental impact.
Formula Transparency: Consumers are increasingly seeking products with transparent ingredient lists, avoiding toxic chemicals like ammonia, bleach, and parabens [44]. This trend pushes manufacturers toward greater disclosure and cleaner formulations.
Concentrated and Refillable Systems: Brands like Branch Basics offer concentrated cleaning solutions that consumers dilute at home, reducing packaging waste and transportation emissions [41]. Similarly, Blueland's tablet-based system, where consumers add water to reusable containers, represents an innovative approach to waste reduction [41].
Personal Care Product Replacements
Personal care products represent a significant source of EDC exposure due to direct dermal application and use in sensitive areas. Product replacement strategies in this category include:
Paraben-Free Formulations: Parabens, used as preservatives in cosmetics, body creams, and hair products, have hormone-disrupting properties and have been linked to breast cancer [43] [40]. Consumers can identify paraben-free products by reading labels and looking for specific certification.
Natural Deodorant Alternatives: Conventional antiperspirants containing aluminum and parabens can be replaced with natural deodorants that use alternative antimicrobial agents like arrowroot powder, baking soda, and essential oils [41].
Fragrance-Free Options: Synthetic fragrances may contain harmful chemicals not fully disclosed on labels [43]. Choosing fragrance-free products or those scented with natural essential oils reduces exposure to potentially undisclosed EDCs.
Menstrual Product Alternatives: Conventional tampons and pads may contain harmful chemicals such as phthalates, bisphenols, and pesticides [43]. Safer alternatives include organic cotton tampons and pads (verified by organic certification logos), silicone menstrual cups, and reusable fabric pads [43].
Research Reagent Solutions for EDC Analysis
Table 3: Essential Research Reagents and Materials for EDC Analysis in Intervention Studies
| Reagent/Material | Function/Application | Technical Specifications |
|---|---|---|
| Urine Collection Kits | Pre- and post-intervention biomonitoring of non-persistent EDCs | Sterile, chemically clean containers; often includes preservatives for metabolite stability during storage and transport |
| Solid Phase Extraction (SPE) Cartridges | Extraction and concentration of EDC biomarkers from biological matrices | Reverse-phase C18 or mixed-mode sorbents; used for clean-up prior to chromatographic analysis |
| Isotope-Labeled Internal Standards | Quantification correction for analytical variability in mass spectrometry | ¹³C- or deuterium-labeled analogs of target EDCs (e.g., ¹³C-BPA, d4-phthalate metabolites) |
| LC-MS/MS Systems | Separation, detection, and quantification of EDC biomarkers | High-performance liquid chromatography coupled to tandem mass spectrometry; enables precise measurement at low concentrations (ng/mL) |
| Certified Reference Materials | Quality assurance and method validation | Urine or serum samples with certified concentrations of EDC metabolites from recognized standards organizations (e.g., NIST) |
| ELISA Kits | High-throughput screening of specific EDCs | Antibody-based detection of targets like BPA or parabens; useful for initial screening though potentially less specific than MS |
| Product Ingredient Databases | Correlation of biomarker levels with specific product use | Comprehensive databases linking product formulations with EDC content; essential for behavioral intervention studies |
Product replacement strategies represent a viable, evidence-based approach to reducing EDC exposure within the context of reproductive health protection. The growing consumer market for safer alternatives, coupled with promising results from targeted intervention studies, suggests that these strategies can effectively bridge the gap between regulatory action and individual health protection. Future research should focus on standardizing intervention protocols, expanding studies to include diverse populations, and developing more sophisticated biomonitoring techniques to quantify exposure reduction efficacy. For researchers and healthcare professionals, integrating product replacement guidance into patient education and public health initiatives offers a practical means of mitigating EDC-related reproductive health risks while awaiting broader regulatory and manufacturing reforms.
Digital Health and Educational Curricula for Behavioral Change
The increasing prevalence of chronic diseases and growing recognition of environmental health threats, particularly from endocrine-disrupting chemicals (EDCs), necessitates innovative approaches to health education. Digital health technologies offer transformative potential for developing behavioral change curricula aimed at mitigating EDC exposure risks, especially concerning reproductive health. This technical guide provides a comprehensive framework for constructing evidence-based digital educational programs, detailing core curricula, experimental methodologies for validation, and implementation protocols tailored for research and professional application.
Core Curriculum Framework for EDC Avoidance
Foundational Knowledge of Endocrine-Disrupting Chemicals
Educational curricula must establish a robust foundation in EDC toxicology and exposure pathways. Endocrine-disrupting chemicals are exogenous substances that interfere with the synthesis, secretion, transport, binding, or elimination of natural hormones, adversely affecting homeostasis, reproduction, and developmental processes [46] [47]. Key EDCs of concern for reproductive health include:
- Bisphenol A (BPA): Used in plastic packaging, dental composites, and thermal paper receipts; acts as an estrogen agonist and antagonist [27] [46].
- Phthalates: Found in scented personal care products, vinyl flooring, and food packaging; associated with reproductive toxicity and hormonal imbalances [27] [3].
- Parabens: Preservatives in cosmetics, pharmaceuticals, and foods; exhibit estrogen-mimicking properties [3] [46].
- Heavy metals (e.g., lead): Present in cosmetics, household cleaners, and contaminated water; disrupts hormonal functions and fetal development [3] [46].
- Triclosan: Antimicrobial agent in soaps, toothpaste, and cleaning products; linked to miscarriage and impaired fertility [3].
These chemicals disrupt reproductive physiology through multiple mechanisms, including binding to hormone receptors, interfering with steroidogenesis, and inducing epigenetic modifications that may have transgenerational effects [27] [46] [47]. The hypothalamic-pituitary-gonadal (HPG) axis represents a primary target for EDCs, leading to disorders such as uterine fibroids, endometriosis, polycystic ovary syndrome, diminished ovarian reserve, and infertility [47].
Digital Health Competencies and Behavioral Change Techniques
Digital health curricula should integrate core competencies that enable health professionals to effectively support behavioral change for EDC avoidance. Essential digital health domains include data protection and information security, telemedicine, digital health applications, artificial intelligence, simulation training, and robotics [48]. These competencies facilitate the delivery of behavior change support through various mechanisms:
- Personalized risk assessment: Utilizing digital tools to evaluate individual exposure profiles and susceptibility factors.
- Tailored intervention strategies: Leveraging data analytics to provide customized recommendations for reducing EDC exposure.
- Remote monitoring and support: Employing digital communication platforms for ongoing patient education and adherence support.
- Gamified learning experiences: Applying game design elements to enhance engagement and knowledge retention in EDC education [48].
Table 1: Core Digital Health Competencies for EDC Avoidance Curricula
| Competency Domain | Key Components | Application to EDC Avoidance |
|---|---|---|
| Data Literacy | Data protection, information security, health data standards | Secure management of personal exposure data and health records |
| Digital Communication | Telemedicine, messenger apps, patient portals | Remote counseling on product selection and exposure reduction strategies |
| Health Technology | mHealth apps, wearables, AI diagnostics | Exposure tracking, personalized recommendations, outcome monitoring |
| Simulation Training | Virtual reality, augmented reality, scenario-based learning | Practice in identifying EDC sources and implementing avoidance behaviors |
Experimental Methodologies for Curriculum Validation
Discrete choice experiments (DCEs) provide a robust methodology for understanding user preferences regarding digital health tools for EDC avoidance. DCEs are survey-based experimental designs that present participants with a series of hypothetical scenarios where they must choose between alternatives with varying attributes [49].
Protocol Implementation:
- Attribute Identification: Conduct literature reviews and qualitative research (e.g., interviews, focus groups) to identify 5-7 key attributes influencing the uptake of digital EDC avoidance tools. Potential attributes include cost, developer credentials (e.g., academic, healthcare institution), user ratings, privacy assurances, and features for exposure tracking [49].
- Attribute Level Specification: Define meaningful levels for each attribute to ensure realistic trade-offs. For example, cost levels might be $0, $2.99/month, $5.99/month; developer levels could be university, government agency, or private company [49].
- Experimental Design: Generate choice tasks using efficient design approaches (e.g., Bayesian efficient design) to maximize information gain while managing cognitive load. Each choice task should present 2-3 alternatives plus an optional "opt-out" to simulate real-world decision-making [49].
- Data Collection and Analysis: Administer the DCE to the target population (e.g., reproductive-aged women, healthcare students). Analyze responses using logistic regression models to determine the relative importance of each attribute and predict uptake of proposed digital tools [49].
Pre-Post Intervention Studies for Efficacy Assessment
Pre-post study designs effectively measure changes in knowledge, risk perceptions, and self-efficacy following implementation of digital health curricula on EDC avoidance.
Protocol Implementation:
- Baseline Assessment: Administer validated questionnaires measuring:
- Knowledge: Recognition of common EDCs (e.g., lead, parabens, BPA, phthalates, triclosan, perchloroethylene) and their sources [3].
- Health Risk Perceptions: Beliefs about personal susceptibility and severity of EDC-related health impacts using Likert scales [3].
- Self-Assessed Competence: Confidence in identifying EDC sources and implementing avoidance strategies [48].
- Behavioral Intentions: Willingness to adopt protective behaviors.
- Curriculum Implementation: Deliver the digital health curriculum through multimodal approaches:
- E-learning modules: Interactive content on EDC sources, health effects, and avoidance strategies.
- Gamification: Robot construction kits (e.g., Lego Mindstorms) for experiential learning about environmental sensors [48].
- Simulation training: Virtual scenarios for practicing product evaluation and exposure reduction counseling.
- Social media integration: Supplementary educational content through platforms like Instagram [48].
- Post-Intervention Assessment: Readminister baseline measures immediately following curriculum completion and at designated follow-up intervals (e.g., 6 months) to assess knowledge retention and behavior change [48].
- Statistical Analysis: Employ paired t-tests or Wilcoxon signed-rank tests to evaluate significant changes in outcome measures. Regression analyses identify demographic and socioeconomic factors influencing curriculum effectiveness [3] [48].
Table 2: Quantitative Assessment Metrics for Curriculum Validation
| Assessment Domain | Measurement Instrument | Data Analysis |
|---|---|---|
| Knowledge Acquisition | Pre-post tests identifying EDCs and their sources | Percentage improvement, statistical significance (p-value) |
| Competence Development | Likert-scale self-assessment of digital health skills | Mean score changes, effect sizes |
| Behavior Change | Self-reported avoidance behaviors, product selection | Correlation analysis, behavioral adoption rates |
| User Engagement | Platform usage metrics, completion rates | Descriptive statistics, trend analysis |
Technical Implementation and Visualization
Digital Health Curriculum Workflow
The following diagram illustrates the integrated workflow for developing, implementing, and evaluating digital health curricula for EDC avoidance behavior change:
EDC Impact on Reproductive Health Pathways
This diagram visualizes the molecular and physiological pathways through which EDCs disrupt reproductive health, informing targeted educational content:
Research Reagent Solutions
Table 3: Essential Research Materials for EDC Avoidance Studies
| Research Tool | Specifications | Application in EDC Research |
|---|---|---|
| Lego Mindstorms Robot Kit | Programmable construction kit with visual programming interface | Gamification element for teaching environmental monitoring concepts; reduces reservations about technology [48] |
| Digital Health Plaforms | SurveyMonkey, Google Forms, Qualtrics | Distribution of DCEs and pre-post assessments; data collection on knowledge, perceptions, and behaviors [3] [48] |
| Biomonitoring Kits | Urinary phthalate metabolites, serum BPA, hair heavy metal analysis | Objective measurement of EDC exposure levels before and after educational interventions [27] [3] |
| Mobile App Development Frameworks | React Native, Flutter, iOS/Android SDK | Creation of customized digital tools for exposure tracking, product scanning, and personalized recommendations |
| Statistical Analysis Software | R, Python, STATA, SPSS | Analysis of DCE data, pre-post intervention effects, and multivariate relationships between variables [48] [49] |
The integration of structured counseling frameworks into clinical practice is a critical component for delivering effective, person-centered healthcare. For researchers and clinicians working at the intersection of environmental science and reproductive health, these frameworks provide essential methodologies for facilitating behavioral change, particularly in complex areas such as endocrine-disrupting chemical (EDC) avoidance. Counseling theories function as research-backed models that grant clinicians greater insight into the challenges their clients face and help determine the interventions most likely to deliver positive outcomes based on clients' unique circumstances [50]. This technical guide examines core counseling approaches and their practical application within the specific context of reproductive health behaviors and EDC avoidance research, providing both theoretical foundations and experimental protocols for implementation and validation.
The need for such integrated approaches is particularly evident in reproductive health, where services are often fragmented, especially in low-resource settings, limiting contraceptive access and contributing to high unmet needs [51]. Furthermore, emerging environmental health challenges require sophisticated counseling strategies. Endocrine-disrupting chemicals (EDCs)—including bisphenols, phthalates, parabens, and oxybenzone—are ubiquitous in everyday environments and have been linked to adverse health outcomes such as impaired fertility, metabolic disorders, neurodevelopmental effects, and cancers [52] [53]. Over 90% of the US population has detectable levels of common EDCs, making clinical counseling on exposure reduction an increasingly essential component of reproductive healthcare [52].
Core Counseling Theories and Their Applications
Foundational Counseling Approaches
Healthcare providers can draw upon several established counseling theories, each with distinct principles and application techniques. The following table summarizes the primary counseling approaches relevant to clinical integration.
Table 1: Foundational Counseling Theories and Their Clinical Application
| Theory/Approach | Theoretical Foundation | Key Techniques | Application in Reproductive Health & EDC Avoidance |
|---|---|---|---|
| Cognitive-Behavioral (CBT) [50] [54] | Aaron Beck; Links thoughts, feelings, and behaviors | Cognitive restructuring, behavioral interventions, identification of automatic thoughts | Addressing cognitive distortions about chemical exposures; developing practical avoidance behaviors; systematic desensitization to fear of complex information |
| Humanistic/Person-Centered [50] [54] | Carl Rogers; Emphasizes innate potential for growth | Unconditional positive regard, active listening, empathetic understanding, genuineness | Building trust to discuss sensitive reproductive concerns; supporting client autonomy in making exposure-reduction decisions; non-judgmental exploration of barriers |
| Psychodynamic [50] [54] | Sigmund Freud; Focuses on unconscious processes | Transference analysis, dream exploration, identifying patterns from past experiences | Exploring deep-seated health beliefs or fears that may impact adherence to exposure reduction guidelines; understanding resistance to change |
| Existential [50] | Viktor Frankl, Martin Heidegger; Focuses on meaning, freedom, mortality | Meaning-centered techniques, worldview mapping, responsibility emphasis | Addressing anxieties about health vulnerabilities; finding purpose in preventive health behaviors; confronting freedom/responsibility in health choices |
| Holistic/Integrative [54] | Combines elements from multiple theories | Flexible application of techniques based on individual client needs | Creating personalized EDC avoidance plans that address behavioral, dietary, and residential exposure pathways [15] |
Specialized Counseling Modalities
Beyond these foundational approaches, several specialized modalities offer targeted strategies for behavior change:
Logotherapy: A form of existential therapy developed by Viktor Frankl that is particularly relevant for patients facing health anxieties related to EDC exposures. This approach helps clients find meaning and purpose even in difficult health circumstances, framing exposure reduction not as a burden but as an opportunity for proactive health management [50].
Motivational Interviewing: While not explicitly detailed in the search results, principles of this approach are implied in the context of readiness to change (RtC) assessments and interventions. The "Reducing Exposures to Endocrine Disruptors (REED)" study highlights the importance of assessing and enhancing clients' willingness to reduce exposures, particularly noting that women showed increased readiness to change after educational interventions [52].
Experimental Protocols for Counseling Intervention Research
Protocol 1: Randomized Controlled Trial of EDC Avoidance Counseling
Objective: To evaluate the efficacy of a structured counseling framework on reducing urinary concentrations of phthalate and phenol metabolites among reproductive-aged participants.
Methodology:
- Participant Recruitment: Recruit 600 participants (300 women, 300 men) of reproductive age (18-44 years) from a large population health cohort [52].
- Baseline Assessment: Collect baseline urine samples for EDC metabolite analysis (phthalates, phenols, parabens) and administer pre-intervention surveys on environmental health literacy (EHL) and readiness to change (RtC) [52].
- Randomization: Randomly assign participants to intervention or control groups.
- Intervention Protocol:
- Group 1 (Comprehensive Counseling): Receive an integrated intervention combining:
- A self-directed online interactive curriculum on EDC sources and health effects
- Live counseling sessions based on Cognitive-Behavioral and Person-Centered approaches
- Individualized support modeled after the Diabetes Prevention Program [52]
- Group 2 (Control): Receive standard educational materials only.
- Group 1 (Comprehensive Counseling): Receive an integrated intervention combining:
- Follow-up Assessment: Collect post-intervention urine samples at 3 and 6 months, and administer EHL and RtC surveys.
- Outcome Measures: Primary outcomes include changes in urinary EDC metabolites; secondary outcomes include changes in EHL scores, RtC scores, and clinical biomarkers (e.g., thyroid function, metabolic parameters) [52].
Table 2: Key Experimental Measures and Analytical Methods
| Measurement Domain | Specific Assays/Metrics | Collection Timeline | Analysis Method |
|---|---|---|---|
| EDC Exposure | Urinary metabolites of phthalates, phenols, parabens, bisphenols | Baseline, 3 months, 6 months | Liquid chromatography-tandem mass spectrometry (LC-MS/MS) |
| Environmental Health Literacy | Knowledge of EDC sources, health effects, avoidance strategies | Baseline, post-intervention | Validated EDC-EHL questionnaire [53] |
| Readiness to Change | Stage of change, willingness to adopt avoidance behaviors | Baseline, post-intervention | Readiness to Change (RtC) scale [52] |
| Clinical Biomarkers | Thyroid hormones, metabolic panels, inflammatory markers | Baseline, 6 months | Commercial at-home test (e.g., Siphox) or clinical analysis [52] |
Protocol 2: Mixed-Methods Assessment of Counseling Integration in Reproductive Health Services
Objective: To identify barriers and facilitators to implementing counseling frameworks in diverse clinical settings providing reproductive healthcare.
Methodology:
- Study Design: Mixed-methods approach combining quantitative service availability assessments with qualitative in-depth interviews [55].
- Participant Recruitment: Purposefully select healthcare facilities across different tiers (tertiary, secondary, community health centers) and geographic settings. Recruit healthcare providers, patients, and patients' partners [55].
- Data Collection:
- Quantitative: Administer the WHO Service Availability and Readiness Assessment (SARA) guide to evaluate infrastructure and service provision capacity [55].
- Qualitative: Conduct in-depth interviews using semi-structured guides until thematic saturation is reached. Focus on experiences with counseling services, perceived barriers, and adaptive strategies [55].
- Analysis:
- Quantitative: Descriptive statistics to characterize service availability; pre-post comparisons where applicable.
- Qualitative: Applied grounded theory and thematic analysis to interview transcripts, using direct quotes to develop results [55].
Signaling Pathways and Conceptual Frameworks
EDC Exposure and Health Outcomes Pathway
The following diagram illustrates the conceptual pathway through which counseling interventions target EDC exposure reduction to improve reproductive health outcomes.
Counseling Impact on EDC Health Pathway
Integrated Care Implementation Workflow
The co-location of family planning services with other reproductive health services represents a key integration model. The following workflow diagrams the implementation process for integrating structured counseling into existing clinical services.
Integrated Care Implementation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Counseling Intervention Research
| Research Tool Category | Specific Products/Assays | Manufacturer/Source | Research Application |
|---|---|---|---|
| Biomonitoring Kits | Million Marker (MM) mail-in urine testing kit [52] | Million Marker | Quantifying internal exposure to EDCs (phthalates, phenols, parabens) before and after counseling interventions |
| Clinical Biomarker Tests | Siphox at-home clinical test [52] | Siphox | Measuring changes in clinical parameters (e.g., thyroid function, metabolic markers) potentially influenced by EDC reduction |
| Validated Survey Instruments | EDC Environmental Health Literacy (EHL) Questionnaire [53] | Academic development | Assessing knowledge of EDC sources, health effects, and avoidance strategies |
| Behavioral Assessment Tools | Readiness to Change (RtC) Scale [52] | Academic development | Measuring participants' stage of change and willingness to adopt exposure-reduction behaviors |
| Data Collection Platforms | Online survey platforms with secure data storage | Qualtrics, REDCap | Administering surveys, managing participant data, and ensuring regulatory compliance |
The integration of structured counseling frameworks into clinical practice, particularly in the specialized domain of reproductive health and EDC avoidance, represents a promising frontier in environmental health intervention. Evidence suggests that combining educational components with personalized counseling support can effectively increase environmental health literacy, enhance readiness to change behaviors, and ultimately reduce biomarker-confirmed EDC exposures [52] [15].
Future research should prioritize the development and validation of standardized counseling protocols specifically tailored to EDC avoidance and reproductive health promotion. Particular attention should be paid to addressing knowledge gaps about exposure pathways and regulatory limitations, as surveys indicate that most participants have significant misconceptions about U.S. chemicals regulation [53]. Additionally, there is a pressing need for more intervention studies focusing on susceptible populations during critical windows of reproductive vulnerability, including the preconception and perinatal periods [15].
For researchers and drug development professionals, these counseling frameworks offer methodologies for improving participant adherence in clinical trials, enhancing patient engagement in lifestyle intervention studies, and developing more comprehensive risk mitigation strategies in environmental health research. By bridging the gap between clinical practice, public health intervention, and environmental health science, these integrated approaches hold significant promise for reducing the burden of disease associated with endocrine-disrupting chemical exposures.
Overcoming Barriers: Challenges in EDC Avoidance Implementation and Efficacy
Knowledge Gaps and Awareness Disparities Among Patients and Professionals
Within the critical field of endocrine disrupting chemical (EDC) research and its implications for reproductive health, a significant barrier to effective intervention lies in the disparate levels of awareness and knowledge among key stakeholders. A robust body of evidence confirms that EDCs, which are exogenous chemicals that interfere with hormone action, are linked to adverse reproductive outcomes, including infertility, decreased sperm quality, polycystic ovary syndrome, and premature ovarian failure [29]. The EDC exposure avoidance theory posits that mitigating exposure, particularly during vulnerable life stages, can improve health outcomes. However, the practical application of this theory is heavily dependent on the awareness and literacy of both the public and the healthcare professionals guiding them. This whitepaper synthesizes current evidence to delineate the specific knowledge gaps among patients and professionals, provides a detailed framework for measuring these disparities, and outlines essential resources for advancing research in this field, all within the context of informing reproductive health behaviors.
Quantitative Data on Awareness and Knowledge Gaps
Recent studies provide quantitative evidence of significant disparities in EDC awareness between healthcare professionals and the public, and within the medical community itself.
Table 1: EDC Awareness Levels Among Healthcare Professionals and the Public
| Population Group | Sample Size | Assessment Tool | Key Finding | Statistical Significance |
|---|---|---|---|---|
| Physicians (Turkey) | 236 | Endocrine Disruptor Awareness Scale (EDCA) | Median General Awareness Score: 2.87 (High) [29] | p < 0.001 vs. students |
| Medical Students (Turkey) | 381 | Endocrine Disruptor Awareness Scale (EDCA) | Median General Awareness Score: 2.12 (Moderate) [29] | Benchmark |
| General Public (Northern Ireland) | 34 (Focus Groups) | Qualitative Thematic Analysis | Low general awareness of EDCs [56] | N/A |
| Female Physicians | Subset of 236 | Endocrine Disruptor Awareness Scale (EDCA) | Significantly higher awareness than male counterparts [29] | p = 0.027 |
| Endocrinologists | Subset of Physicians | Endocrine Disruptor Awareness Scale (EDCA) | Total Score: 3.96 ± 0.56 vs. 3.59 ± 0.58 for other specialties [29] | p = 0.003 |
Table 2: Factors Correlating with EDC Awareness and Behavioral Change
| Factor | Correlated Outcome | Study Population | Significance/Notes |
|---|---|---|---|
| Age | Positive correlation with EDC awareness scores [29] | Medical students & physicians | Spearman's correlation |
| Healthy Life Awareness (HLA) Score | Positive correlation with EDC awareness scores [29] | Medical students & physicians | Spearman's correlation |
| Post-Intervention Report-Back | 44% reduction in participants not knowing how to decrease exposure [9] | Reproductive-aged cohort | |
| Post-Intervention Report-Back | Increased EHL behaviors [9] | Reproductive-aged cohort | p = 0.003 |
| Post-Intervention Report-Back | Decreased monobutyl phthalate levels [9] | Subset (n=55) providing second urine sample | p < 0.001 |
| Gender (Female) | Increased readiness to change (RtC) post-intervention [9] | Reproductive-aged cohort | p = 0.053 |
Experimental Protocols for Assessing and Addressing Gaps
To effectively study and intervene in the landscape of EDC knowledge, researchers can employ the following detailed methodologies, which have been validated in recent studies.
Protocol 1: Cross-Sectional Assessment of Awareness Disparities
This protocol is designed to quantify awareness levels across different groups, such as healthcare professionals, students, and patients.
- 1. Study Design and Setting: A cross-sectional, questionnaire-based study is employed. The setting for the original study was a university school of medicine, but this can be adapted to clinics, hospitals, or online platforms for public recruitment [29].
- 2. Participant Recruitment: Participants are recruited through institutional channels (e.g., email directories, professional networks) to ensure authenticity. For public recruitment, convenience sampling at public outreach events or online surveys can be used. Inclusion criteria should be clearly defined (e.g., age, profession, residency). Participation is voluntary and anonymous [29] [56].
- 3. Data Collection Instruments:
- Demographic Questionnaire: Collects age, gender, educational status, and medical specialty [29].
- Validated EDC Awareness Scale (EDCA): A 24-item instrument with a 1-5 Likert-type scoring system. It measures three subcategories: general awareness, impact, and exposure and protection. Scores are interpreted as: 1-1.8 (very low); 1.81-2.6 (low); 2.61-3.4 (moderate); 3.41-4.2 (high); 4.21-5 (very high) [29].
- Healthy Life Awareness (HLA) Scale: A 15-item scale with 5-category Likert-type scoring, grouped into four subdomains: change, socialization, responsibility, and nutrition. This assesses general health consciousness, which correlates with EDC awareness [29].
- 4. Data Analysis: Statistical analysis is performed using software like IBM SPSS. Normality of data is assessed. Non-parametric tests (Mann-Whitney U, Kruskal-Wallis, Spearman’s correlation) are used for non-normally distributed data. A p-value of <0.05 is considered significant. Linear regression can model relationships between variables [29].
Protocol 2: Randomized Controlled Trial (RCT) for EDC Exposure Reduction
This protocol tests the efficacy of an intervention designed to increase EDC health literacy (EHL) and reduce exposure, which is directly applicable to research on reproductive health behaviors.
- 1. Study Design: A randomized controlled trial, which is the gold standard for evaluating interventions [9].
- 2. Participants and Recruitment: The target population is men and women of reproductive age (e.g., 18-44 years old). Recruitment can occur from large population health cohorts or the general public. A sample size of 600 (300 women, 300 men) provides robust power [9].
- 3. Intervention Components:
- Biomonitoring: Participants use a mail-in urine testing kit to measure specific EDCs (e.g., bisphenols, phthalates, parabens, oxybenzone) [9].
- Report-Back: Participants receive a personalized report detailing their urinary levels of EDCs, information on health effects, common exposure sources, and actionable, personalized recommendations for reducing exposure [9].
- Educational Curriculum: An interactive online curriculum is provided. This is complemented by live counseling sessions, modeled after the Diabetes Prevention Program, to offer individualized support and overcome application barriers [9].
- 4. Outcome Measures:
- Primary: Changes in EDC exposure levels from baseline to follow-up, measured via urine biomonitoring [9].
- Secondary: Changes in EHL and readiness to change (RtC) scores, measured via validated surveys. Changes in clinical biomarkers (e.g., for cardiovascular/metabolic health, hormone levels) can also be assessed using at-home test kits [9].
- 5. Data Analysis: Pre- and post-intervention values for EDC metabolites, EHL, and RtC are compared using paired t-tests or Wilcoxon signed-rank tests. Regression models can identify predictors of successful behavior change and exposure reduction [9].
Diagram 1: RCT participant workflow for EDC exposure reduction intervention.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Tools for EDC Awareness and Exposure Studies
| Item/Tool | Function/Application | Example Use in Protocol |
|---|---|---|
| Endocrine Disruptor Awareness Scale (EDCA) | Validated questionnaire to quantitatively assess knowledge levels in three sub-domains: general awareness, impact, and exposure/protection. | Used in cross-sectional studies to compare awareness between medical students and physicians [29]. |
| Healthy Life Awareness (HLA) Scale | Assesses general health consciousness and preventive health attitudes, which serves as a correlative factor for EDC awareness. | Administered alongside the EDCA to investigate association between general health awareness and specific EDC knowledge [29]. |
| Mail-in Urine Biomonitoring Kit | Enables non-invasive, at-home collection of biological samples for quantifying internal doses of EDC metabolites (e.g., BPA, phthalates). | Core component of RCT intervention; used to measure baseline exposure and change post-intervention [9]. |
| EDC-Specific EHL Curriculum | Interactive, online educational modules designed to improve knowledge about EDC sources, health effects, and avoidance strategies. | Provided to the intervention group in an RCT to bridge identified knowledge gaps and empower behavior change [9]. |
| Readiness to Change (RtC) Survey | Assesses an individual's motivational stage (e.g., pre-contemplation, action) for adopting behaviors to reduce EDC exposure. | Measured pre- and post-intervention to evaluate the intervention's efficacy in motivating participants [9]. |
Visualizing the Research Pathway
The following diagram maps the logical sequence of a research program aimed at moving from identifying a knowledge gap to implementing a public health solution.
Diagram 2: Logical pathway from gap identification to public health translation.
Regulatory Limitations and the Prevalent 'Regrettable Substitution' Problem
The global increase in diseases linked to Endocrine-Disrupting Chemicals (EDCs), particularly in the realm of reproductive health, has intensified scrutiny of the regulatory frameworks designed to manage chemical risks. A significant flaw in these systems is the phenomenon of 'regrettable substitution', where a restricted or banned chemical is replaced by a structurally similar alternative with comparable or unknown hazardous properties [57]. This practice creates a cyclical pattern of exposure that undermines public health protections, particularly for vulnerable populations such as pregnant women and those of reproductive age.
Within the context of reproductive health behaviors EDC avoidance theory, this problem presents a critical challenge. Theories aiming to predict or guide avoidance behaviors must account for a rapidly shifting chemical landscape, where today's avoidance recommendations may be obsolete tomorrow due to substitution. This whitepaper provides a technical analysis of the regulatory limitations that permit regrettable substitution to persist, synthesizes current epidemiological and experimental evidence of its impact on reproductive health, and outlines essential methodologies for advancing research in this field.
Regulatory Landscape and Systemic Deficiencies
The European Union's REACH (Registration, Evaluation, Authorisation and Restriction of Chemicals) regulation exemplifies a system with advanced tools that are undermined by critical implementation failures. A recent analysis of its shortcomings reveals several systemic deficiencies [57]:
- Industry Non-Compliance and Data Gaps: Chemical registrations are often supported by insufficient data, creating significant knowledge gaps and bottlenecks in the evaluation process. This lack of compliance means chemicals remain on the market without adequate safety profiles.
- Burden on Authorities: The responsibility to demonstrate a chemical's hazard is disproportionately placed on regulatory authorities, rather than the industry that produces it. This leads to slow, arduous evaluation processes; a recent report found it can take authorities up to 13 years and 8 months to assess the hazards of a single chemical substance [57].
- Unjustified Derogations: A lack of transparency and the prioritization of industry interests in risk management decisions often result in unjustified exemptions during authorisation and restriction processes.
These deficiencies create a regulatory environment where hazardous chemicals like bisphenols, lead, and PVC remain widely on the market, and regrettable substitution becomes a common, rationalized practice [57].
Public Misconceptions and Regulatory Gaps
A recent U.S. study highlights a critical disconnect between public perception and regulatory reality, which further complicates EDC avoidance behaviors [53]. Surveys reveal that most Americans operate under significant misconceptions about chemical regulation, erroneously believing that:
- Chemicals must be proven safe before they are used in products (82% of respondents) [53].
- Companies are required to disclose all ingredients in their products (73% of respondents) [53].
- When a chemical is restricted, it cannot be replaced by a similar, potentially hazardous substitute (63% of respondents) [53].
These beliefs are at odds with the actual operation of many regulatory systems, which often do not mandate pre-market safety testing for the vast majority of chemicals. This knowledge gap is a major target for future communications and underscores the challenges facing researchers in promoting effective EDC avoidance based on sound science [53].
The Evidence Base: EDCs, Substitution, and Reproductive Health
The scientific literature consistently links EDC exposure to adverse reproductive outcomes. A systematic review of human epidemiological evidence from the last decade (2014-2024) found consistent associations between exposure to common EDCs—such as BPA, phthalates, PFAS, and parabens—and multiple reproductive endpoints [58]. These include impaired semen quality, decreased ovarian reserve, infertility, polycystic ovary syndrome (PCOS), altered hormone levels, and poorer outcomes in assisted reproductive technologies (ART) like in vitro fertilization (IVF) [58].
Table 1: Key EDCs and Their Documented Associations with Reproductive Health Outcomes
| Chemical Class | Common Examples | Documented Reproductive Health Associations |
|---|---|---|
| Bisphenols | BPA, BPS, BPF | Altered hormone levels, reduced ovarian reserve, adverse IVF outcomes, impaired semen quality [58] [59] |
| Phthalates | DEHP, DBP, BBP | Impaired male reproductive development, reduced sperm count, altered hormone levels, infertility [58] [59] |
| Per- and Polyfluoroalkyl Substances (PFAS) | PFOA, PFOS | Reduced fertility, menstrual cycle irregularities, adverse birth outcomes [58] |
| Parabens | Methylparaben, Propylparaben | Altered ovarian function, oxidative stress in reproductive tissues [58] |
The Practice of Regrettable Substitution
The transition away from well-studied hazardous chemicals often results in the introduction of less-studied alternatives. A prime example is the replacement of Bisphenol A (BPA) with its analogs, Bisphenol S (BPS) and Bisphenol F (BPF). Despite regulatory restrictions on BPA in many countries, its substitutes are chemically similar and exhibit comparable endocrine-disrupting properties [59]. Early cohort studies indicate that maternal exposure to BPS and BPF shows relationships with altered birth size and behavioral indices in children (Odds Ratios ranging from 1.2 to 1.4; 95% CI: 1.0–1.8), similar to those observed with BPA [59]. This direct substitution in products marketed as "BPA-free" creates a cycle of continuous exposure, complicating public health messaging and rendering consumer avoidance behaviors less effective.
Methodological Approaches for Research
Investigating regrettable substitution and its health impacts requires robust methodological frameworks. The following sections detail validated approaches for assessing exposure, measuring health behaviors, and analyzing complex data.
Exposure Assessment and Biomarker Analysis
Accurate exposure assessment is complicated by the pharmacokinetics of different EDCs. For research on reproductive health outcomes, particularly prenatal exposures, meticulous planning is required [59] [60]:
- Non-persistent chemicals (e.g., BPA, phthalates, parabens): These have short biological half-lives. A single spot urine measurement can lead to exposure misclassification. The recommended strategy involves frequent repeated measurements (e.g., multiple urine samples collected across pregnancy trimesters) to capture temporal variability and establish a more reliable average exposure [60].
- Persistent chemicals (e.g., PFAS, PCBs): These have long half-lives and accumulate in the body. A single measurement of maternal serum or plasma during pregnancy can reasonably reflect the long-term cumulative exposure burden for the mother and fetus. The challenge lies in correlating this stable internal concentration with specific critical exposure windows [60].
Table 2: Essential Research Reagents and Materials for EDC Analysis
| Research Reagent / Material | Function/Application | Technical Notes |
|---|---|---|
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Quantifying specific EDCs (e.g., BPA, phthalate metabolites) in biological samples like urine or serum. | Ideal for high-throughput screening. Requires validation against gold-standard methods for specific matrices. |
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Gold-standard for precise identification and quantification of EDCs and their metabolites at low concentrations. | Essential for measuring chemical mixtures and confirming ELISA results. |
| Standard Reference Materials (SRMs) | Quality control and assurance for analytical chemistry measurements. | SRMs for human urine, serum, and breast milk with certified EDC levels are available from organizations like NIST. |
| DNA Methylation & RNA Sequencing Kits | Analyzing epigenetic changes and gene expression alterations in response to EDC exposure. | Critical for investigating mechanistic pathways, such as epigenetic reprogramming. |
| Validated Survey Questionnaires | Assessing participant knowledge, perceived sensitivity, and health behavior motivation related to EDCs. | Pre-validated tools improve reliability and allow for cross-study comparisons [61] [11]. |
Survey-Based Assessment of Health Behaviors
To study EDC avoidance behaviors, researchers can employ validated, reproducible surveys. Kim et al. (2025) developed and validated a 19-item survey assessing reproductive health behaviors for reducing EDC exposure through major routes: food, respiration, and skin absorption [11].
Development and Validation Protocol [11]:
- Item Generation: A pool of 52 initial items was developed through a comprehensive literature review.
- Content Validity: A panel of five experts (e.g., chemical/environmental specialists, physicians) assessed the items. The Item-Content Validity Index (I-CVI) was calculated, and items below .80 were removed or revised.
- Pilot Study: A pilot with 10 adults was conducted to assess clarity, response time, and layout.
- Factor Analysis: The survey was administered to 288 adults. Exploratory Factor Analysis (EFA) using Principal Component Analysis with varimax rotation confirmed a 4-factor structure. Confirmatory Factor Analysis (CFA) was used to verify the model fit.
- Reliability Testing: Internal consistency was confirmed with a Cronbach's α of .80, meeting the threshold for a newly developed instrument [11].
Statistical and Mechanistic Analysis
Mediation Analysis: To understand the psychological drivers of avoidance behaviors, mediation analysis can be employed. A 2025 study of 200 women demonstrated that the relationship between knowledge of EDCs and motivation for health behaviors is partially mediated by perceived illness sensitivity [61]. This suggests that knowledge alone is insufficient to drive behavioral change; cognitive and emotional awareness of personal risk plays a critical mediating role. This finding should be integrated into theoretical models of EDC avoidance.
Grouping and Mixture Assessment: To counter the one-chemical-at-a-time approach that enables regrettable substitution, research must adopt methods for assessing groups of chemicals and their combined "cocktail effects." The Generic Risk Assessment (GRA) approach, currently applied to some hazardous chemicals, should be extended to include endocrine disruptors, persistent and mobile substances, enabling more efficient regulation of entire chemical groups [57]. Furthermore, applying a Mixture Assessment Factor (MAF) in risk assessment can account for the combined effects of real-life exposure to multiple chemicals [57].
Visualizing Research Workflows and Conceptual Models
The following diagrams, generated using DOT language, illustrate key experimental workflows and conceptual relationships in this field.
The problem of regrettable substitution is a direct consequence of regulatory systems that fail to mandate sufficient pre-market data, place the burden of proof on authorities, and evaluate chemicals in isolation. For research focused on reproductive health behaviors and EDC avoidance theory, this creates a moving target that undermines the development of lasting interventions.
To address this, future efforts must prioritize:
- Advocating for Group-Based Regulation: Supporting regulatory reforms, such as the proposed REACH revision, that mandate the assessment and regulation of entire groups of chemicals based on shared hazardous properties [57].
- Integrating 'Cocktail Effect' Assessments: Employing methodological tools like the Mixture Assessment Factor (MAF) in research designs to better reflect real-world exposure scenarios [57].
- Clarifying Essential Use Concepts: Integrating clear criteria for "essential use" of the most harmful chemicals into regulatory frameworks and research models to prevent unjustified continuations of use where safer alternatives exist [57].
- Longitudinal Biomonitoring and 'Omics' Technologies: Combining prospective cohort studies with multi-omics technologies (epigenomics, transcriptomics) to elucidate the mechanisms of emerging substitutes and identify critical windows of exposure [59] [60].
By adopting these strategies, researchers can generate the robust evidence needed to break the cycle of regrettable substitution and build a more effective, predictive theory of EDC avoidance that truly protects reproductive health.
Intervention Adherence Challenges and Long-Term Behavior Maintenance
The utility of lifestyle-based health promotion interventions is directly impacted by participant adherence to prescribed behavior changes. Unfortunately, poor adherence to behaviors recommended in lifestyle interventions is widespread, particularly over the long-term, creating a significant challenge to intervention effectiveness [62]. Rates of non-adherence to chronic illness treatment regimens have been reported to be as high as 50% to 80%, with similar patterns observed in behavioral therapy literature where premature drop-out ranges from 30% to 60% [62]. This adherence problem represents a critical challenge across medicine and public health, especially considering that individuals who are not fully adherent experience significantly fewer health benefits [62].
Within lifestyle interventions, a typical pattern emerges: encouraging initial responses to treatment are frequently followed by diminished adherence over time, leading to disappointing long-term outcomes. This pattern is particularly evident in weight management interventions, where participants often regain half of lost weight within one year and return to baseline weight within 3-5 years despite initial successful weight losses of 8-10% of initial body weight [62]. Similar patterns of good initial adherence followed by gradual but steady declines have been observed across various lifestyle interventions, even those targeting diet and physical activity without weight change objectives [62].
Theoretical Frameworks for Understanding Adherence
Social Cognitive Theory and Adherence
Social cognitive theory provides a fundamental framework for understanding the factors influencing initiation and maintenance of behavior change [62]. This theory describes how personal factors (cognitions, emotions) and aspects of the social and physical environment influence behavior reciprocally. From this perspective, the initiation of behavior change requires sufficient self-efficacy and outcome expectations, while maintenance involves continuous self-regulatory processes including self-monitoring, goal-setting, and problem-solving in the face of challenges and barriers [62].
The complex interactions between individuals and their environment during behavior change can be understood through this theoretical lens. When individuals attempt to maintain behavior changes, they must navigate a continuous stream of decisions while managing internal states (cravings, fatigue, stress) and external cues (food availability, social pressures) [62]. Environmental challenges often initiate a behavioral "cascade" where initial lapses in maintenance undermine confidence in self-management skills, leading to poor long-term adherence and eventual abandonment of behavior change efforts [62].
Behavior Change Techniques and Mechanisms of Action
Understanding the links between behavior change techniques (BCTs) and their mechanisms of action (MoAs) is crucial for designing effective interventions. BCTs are defined as replicable components designed to alter or redirect causal processes that regulate behavior, while MoAs are theoretical constructs that represent the processes through which BCTs affect behavior, such as "beliefs about capabilities," "knowledge," and "behavioral regulation" [63].
Research has identified 2,636 BCT-MoA links across the literature, with the most frequently linked MoAs being "Beliefs about Capabilities" and "Intention" [63]. This mapping provides intervention developers with systematically collated evidence for creating theory-based interventions. For example, the BCT "Graded Tasks" may change behavior by increasing beliefs about one's capabilities, while "Restructuring the Social Environment" might work by decreasing negative social influences [63].
Specific Adherence Challenges Across Behavioral Domains
Dietary Adherence Challenges
Multiple factors impact long-term adherence to dietary changes, with the current "toxic" food environment presenting a significant barrier. This environment is rich in easily-accessible, inexpensive, and tasty high-fat, high-calorie foods, which limits healthy dietary choices [62]. Additionally, physiological changes experienced while dieting include heightened sensitivity to palatable foods, particularly sweet and salty substances [62]. Research indicates that obese individuals may have greater sensitivity to the sensory processing of food intake, which is concerning because sensitivity to rewarding properties of taste and smell are related to overeating and preference for foods high in fat and sugar [62].
The interaction of these physiological changes with constant exposure to an unhealthy food environment virtually guarantees occasional lapses in dietary control [62]. These lapses can undermine confidence and lead to abandonment of dietary behavior changes unless individuals are equipped with effective coping strategies.
Physical Activity Adherence Challenges
Adherence to physical activity recommendations faces multiple internal and external barriers. Modern sedentary occupations require individuals to compensate for reduced energy expenditure during work hours by spending leisure time in active pursuits to meet national activity guidelines (at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week) [62]. The perceived time commitment represents a significant barrier, considering not only the time required for activity itself but also preparation and transportation to facilities [62].
Additional barriers include perceived stress and fatigue, where individuals report feeling "too tired" for activity after stressful workdays, despite recognizing that exercise can decrease stress and increase energy [62]. Environmental limitations also present substantial barriers, particularly in low-income areas that may lack adequate sidewalks, bike paths, or recreational facilities [62]. These barriers compound when individuals who perceive little time for activity must travel significant distances to access adequate facilities.
Medication Adherence Challenges
Medication non-adherence represents a continuous burden for healthcare systems, with statistics remaining constant since 2003 when the World Health Organization reported at least 50% of patients with chronic conditions were non-adherent to their medications [64]. A study analyzing electronic databases of nearly 17,000 patients' dosing histories across different diseases revealed that 4% of patients never initiated treatment, nearly 40% discontinued, and only 55% dosed correctly [64].
The negative consequences of medication non-adherence have been widely documented, with a recent systematic review finding the economic impact, including healthcare costs, ranged from $949 to $44,190 per patient annually across 14 disease groups [64]. Effective adherence interventions have demonstrated significant benefits, including viral suppression in HIV patients, decreased lipid levels in patients taking lipid-lowering medications, reduction of HbA1c, decreased hospitalizations, and reduced all-cause mortality in patients with diabetes and heart failure [64].
Evidence-Based Strategies for Improving Long-Term Adherence
Intervention Effectiveness Across Time and Clinical Conditions
Network meta-analyses have provided robust evidence regarding the comparative effectiveness of different adherence intervention types across timeframes and clinical conditions. The table below summarizes the temporal effectiveness of various intervention types based on network meta-analysis of 249 studies:
Table 1: Temporal Effectiveness of Adherence Interventions
| Intervention Type | 0-3 Months | 4-6 Months | 7-9 Months | ≥10 Months |
|---|---|---|---|---|
| Technical | Moderate effect | OR: 0.34 (0.25-0.45) | Not significant | Less effective |
| Attitudinal | Less effective | Less effective | OR: 0.37 (0.17-0.84) | Moderate effect |
| Educational | Less effective | Less effective | Increasing effect | Moderate effect |
| Rewards | Short-term effect | Short-term effect | Not significant | Not significant |
| Multicomponent | Moderate effect | Moderate effect | Increasing effect | OR: 0.49 (0.27-0.88) |
Data derived from network meta-analysis of 249 studies [65]
Effectiveness of interventions also varies significantly by clinical condition. The table below summarizes the most effective intervention types for different clinical condition groups based on network meta-analysis:
Table 2: Intervention Effectiveness by Clinical Condition
| Clinical Condition Group | Most Effective Intervention | Effect Size (Odds Ratio) | SUCRA Value |
|---|---|---|---|
| Circulatory system & Metabolic diseases | Educational + Technical | OR: 0.44 (0.26-0.73) | 79.6% |
| Infectious diseases | Educational + Technical | OR: 0.56 (0.36-0.84) | 73.3% |
| Musculoskeletal diseases | Attitudinal | OR: 0.30 (0.10-0.86) | 92.3% |
| Mental, Behavioral, Neurodevelopmental disorders | Educational + Attitudinal | Not significant | 73.8% |
Data derived from systematic review with network meta-analysis of 80 primary studies [64]
Digital Health Interventions for Adherence
Digital health interventions, including mobile health (mHealth), telehealth, and combined approaches, have demonstrated significant benefits for improving adherence and clinical outcomes. A systematic review and meta-analysis of 74 studies involving 92,686 participants revealed these interventions significantly decreased both systolic and diastolic blood pressure in hypertensive patients [66].
The effectiveness varies by intervention type: medication adherence showed improvement only in the mHealth group, while blood pressure control improved in both mHealth and combined mHealth & telehealth groups [66]. BMI showed improvement only in the mHealth group, while evidence for adherence to physical activity and DASH diet/salt intake remained inconclusive [66]. These findings suggest that digital health approaches, particularly mHealth, show promise for addressing certain adherence challenges.
Multicomponent Interventions for Sustainable Adherence
Research consistently demonstrates that multicomponent interventions provide the most sustainable approach to long-term adherence. Network meta-analyses have revealed that interventions combining educational, attitudinal, and technical components demonstrate significant effectiveness in follow-ups greater than 10 months (OR: 0.49, 95% CrI: 0.27-0.88) [65].
The sustainability of adherence to medications and health behaviors over time appears dependent upon multicomponent interventions that address the various dimensions influencing adherence. Future research should focus on identifying the most cost-effective multicomponent approaches capable of integration into routine practice [65].
Adherence in Reproductive Health and EDC Avoidance Behaviors
Reproductive Health Behavior Challenges
In the context of reproductive health, particularly behaviors aimed at reducing exposure to endocrine-disrupting chemicals (EDCs), unique adherence challenges emerge. EDCs are synthetic chemicals that disrupt normal endocrine function and have been linked to numerous health effects including infertility, breast cancer, metabolic syndrome, and developmental problems in offspring [9]. These chemicals enter the body through various exposure routes, including food, air, and skin absorption, making them nearly unavoidable in daily life [11].
Despite known health risks, public awareness of daily EDC exposure sources remains low, primarily due to insufficient knowledge about prevention measures and the prioritization of convenience in modern life, leading to desensitization to EDC exposure risks [11]. Reproductive health behaviors aimed at reducing EDC exposure focus on minimizing risks by avoiding or limiting exposure in daily life, requiring consistent adherence to often inconvenient behavior changes [11].
Measuring Reproductive Health Behaviors for EDC Avoidance
Research has developed validated instruments to assess adherence to reproductive health behaviors targeting EDC reduction. One validated survey identifies four key factors with 19 detailed items related to reproductive health behaviors and reproductive health promotion behaviors through main EDC exposure routes: food, respiratory pathways, and skin absorption [11].
The diagram below illustrates the conceptual framework of reproductive health behaviors for EDC avoidance:
Intervention Strategies for EDC Avoidance Adherence
Innovative intervention approaches have been developed to improve adherence to EDC avoidance behaviors. The Reducing Exposures to Endocrine Disruptors (REED) study implements a personalized at-home intervention program featuring mail-in urine testing, exposure report-back, and personalized recommendations [9]. This intervention model has demonstrated success in increasing environmental health literacy (EHL) and readiness to change, particularly among women [9].
Previous research with this model found that after report-back interventions, participants showed increased EHL behaviors, increased readiness to change among women, a 44% reduction in participants not knowing how to decrease exposure, and high percentages of participants reporting behavior changes to reduce exposure [9]. Additionally, decreases in specific phthalate levels were observed, demonstrating both behavioral and biological efficacy [9].
Methodological Considerations and Experimental Protocols
Validating Behavioral Survey Instruments
For research investigating adherence to reproductive health behaviors, validated measurement instruments are essential. The following diagram illustrates the survey development and validation process used in reproductive health behavior research:
The development of a validated survey questionnaire for reproductive health behaviors aimed at reducing EDC exposure followed a rigorous methodological process. Researchers initially generated 52 items through literature review, then subjected these to expert content validity assessment (CVI > .80), pilot testing with target population members, and both exploratory and confirmatory factor analyses to arrive at a final 19-item instrument with four distinct factors [11].
Experimental Protocol for EDC Intervention Studies
The REED study protocol provides a comprehensive experimental model for investigating adherence to EDC avoidance behaviors. This randomized controlled trial employs:
- Recruitment of reproductive-aged participants (18-44 years) from a large population health cohort
- Baseline assessment including EHL surveys, readiness to change measures, and urine biomonitoring for EDCs
- Randomization to intervention or control groups
- Intervention components including:
- Self-directed online interactive curriculum
- Live counseling sessions
- Individualized support modeled after the Diabetes Prevention Program
- Report-back of personal EDC exposure data
- Post-intervention assessment of EHL, readiness to change, EDC exposure levels, and clinical biomarkers [9]
This comprehensive protocol allows researchers to assess both behavioral adherence (through self-report measures) and biological efficacy (through biomonitoring and clinical biomarkers).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for Adherence and EDC Studies
| Research Tool | Function | Application Example |
|---|---|---|
| BCT Taxonomy v1 | Classifies behavior change techniques | Standardizing intervention descriptions in meta-analyses [63] |
| Theory Coding Scheme | Identifies theoretical constructs | Specifying mechanisms of action in intervention studies [63] |
| Urine Biomonitoring | Measures internal exposure to EDCs | Quantifying phthalate, paraben, and bisphenol levels in intervention studies [9] |
| Electronic Medication Monitoring | Objective adherence measurement | Medication event monitoring systems (MEMS) for implementation adherence [64] |
| EDC-Specific EHL Survey | Assesses environmental health literacy | Measuring knowledge and behaviors related to EDC exposure and avoidance [11] |
| Readiness to Change Scale | Measures motivation for behavior change | Assessing stage of change for EDC avoidance behaviors [9] |
The challenge of maintaining long-term adherence to health behavior changes represents a critical frontier in behavioral medicine. Evidence consistently demonstrates that single-component interventions provide limited long-term benefits, while multicomponent approaches addressing educational, attitudinal, and technical aspects show promise for sustainable adherence [65]. The effectiveness of specific intervention strategies appears to vary based on clinical context, timeframe, and target behaviors, necessitating tailored approaches for different populations and objectives.
In the specific context of reproductive health and EDC avoidance behaviors, emerging research demonstrates that comprehensive interventions combining biomonitoring, report-back of results, education, and personalized support can effectively increase environmental health literacy, readiness to change, and adoption of protective behaviors [9]. Future research should focus on identifying the most cost-effective intervention components, understanding individual differences in response to adherence strategies, and developing technologies that support long-term maintenance of behavior changes across diverse populations and behavioral domains.
Addressing Socioeconomic Disparities in EDC Exposure and Avoidance Capability
Endocrine-disrupting chemicals (EDCs) are exogenous substances that interfere with the normal functioning of the endocrine system, mimicking or blocking the action of endogenous hormones such as estrogens, androgens, and thyroid hormones [67]. The reproductive system is particularly vulnerable to EDCs, with exposure linked to adverse outcomes including reduced sperm quality, decreased ovarian reserve, infertility, polycystic ovary syndrome (PCOS), and earlier menopause [68] [67]. These chemicals are pervasive in everyday materials and consumer products, including plastics, food packaging, cosmetics, personal care products, and pesticides, making human exposure widespread and continuous through ingestion, inhalation, and dermal absorption [67].
Socioeconomic status (SES) significantly influences both exposure levels and the capability to avoid EDCs. Emerging evidence reveals that individuals with lower socioeconomic status—including lower income, educational attainment, and racial/ethnic minority groups—experience disproportionate exposure to multiple EDCs, creating environmental injustice and exacerbating health disparities [69] [70] [71]. This whitepaper synthesizes current evidence on socioeconomic disparities in EDC exposure, examines the biological mechanisms and pathways through which these disparities affect reproductive health, and provides technical guidance for researchers studying and addressing these critical inequities.
Evidence of Socioeconomic Disparities in EDC Exposure
Epidemiological Findings from Cohort Studies
Recent studies consistently demonstrate that socioeconomic factors significantly predict EDC exposure levels. A 2025 study of pregnant Taiwanese women found that those in the lowest income group (<0.5 million NTD) had significantly higher predicted concentrations of bisphenol A (BPA) with more frequent use of personal care products (PCPs) [69]. The association between PCP use and paraben concentrations varied substantially by income and education levels, with the strongest associations between rinse-off PCPs and methylparaben (6.1% increase, 95%CI = 1.9%-10.5%) and propylparaben (6.9% increase, 95%CI = 1.2%-12.9%) observed in the postgraduate education group [69].
Analysis of U.S. NHANES data (1999-2020) revealed that despite overall decreases in exposure to many EDCs over two decades, reproductive-age and pregnant women experienced increased exposure to certain thyroid-disrupting chemicals, particularly polyaromatic hydrocarbons [71]. Critically, low-income women in these groups showed the greatest increase in exposure, potentially worsening health disparities [71].
EDCs Associated with Documented Socioeconomic Disparities
Table 1: EDCs with Documented Socioeconomic Exposure Disparities
| EDC Class | Specific Chemicals | Exposure Disparities | Key Health Impacts |
|---|---|---|---|
| Bisphenols | Bisphenol A (BPA) | Higher in low-income populations [69] [70] | Hormonal imbalance, infertility, PCOS [67] |
| Parabens | Methylparaben, Ethylparaben, Propylparaben | Stronger association with PCP use in lower income and higher education groups [69] | Estrogenic activity, reproductive dysfunction [69] |
| Polyaromatic Hydrocarbons | Multiple compounds | Increased exposure in low-income pregnant women [71] | Thyroid disruption, developmental effects [71] |
| Persistent Organic Pollutants | PCBs, organochlorine pesticides | Higher in African Americans and Latinos [70] | Diabetes, reproductive disorders [70] [67] |
| PFAS | Various fluorinated compounds | Disparities by race/ethnicity [70] | Puberty timing, ovarian function, PCOS [68] |
Quantitative Data on Exposure-Outcome Relationships
Table 2: Documented Health Effect Magnitudes by EDC Exposure Level
| Health Outcome | EDC Class | Exposure Comparison | Effect Size (OR, RR, or Other) |
|---|---|---|---|
| Early Menopause | Pesticides, phthalates | Highest vs. lowest combined exposure | 1.9-3.8 years earlier [68] |
| Diabetes Incidence | PCBs | Highest vs. lowest serum levels | RR: 2.39 (1.86-3.08) [70] |
| Diabetes Incidence | Organochlorine pesticides | Highest vs. lowest exposure | Pooled OR: 2.00 (1.13-3.53) [70] |
| Methylparaben Increase | Parabens | Each additional PCP use/week (above-lowest income) | 3.1% (1.8%-4.4%) [69] |
| Preterm Birth Risk | Social stressors | Chronic high vs. low stress exposure | Significantly elevated [72] |
Pathways and Mechanisms Linking Socioeconomic Status to EDC Exposure
Conceptual Framework of Socioeconomic Disparities in EDC Exposure
The relationship between socioeconomic status and EDC exposure operates through multiple interconnected pathways. The following diagram illustrates the primary mechanisms through which socioeconomic factors influence EDC exposure and subsequent reproductive health outcomes:
Biological Mechanisms of EDC Action on Reproductive Health
EDCs interfere with reproductive health through multiple molecular pathways. The hypothalamic-pituitary-gonadal (HPG) axis is particularly vulnerable, with EDCs capable of mimicking or blocking sex hormones, altering hormone synthesis and metabolism, and modifying hormone receptor expression [67]. The following diagram details the key biological mechanisms:
Research Methodologies for Studying EDC Exposure Disparities
Cohort Study Designs and Exposure Assessment Protocols
Longitudinal cohort studies provide the strongest evidence for causal relationships between socioeconomic factors, EDC exposure, and reproductive outcomes. The Taiwan Maternal and Infant Cohort Study (TMICS) exemplifies an effective approach, enrolling pregnant women during routine third-trimester examinations (weeks 29-40) and collecting comprehensive data [69].
Essential Protocol Components:
- Participant Recruitment: Enroll from multiple geographic regions and healthcare settings to capture socioeconomic diversity
- Biological Sampling: Collect urine, blood, and other samples for EDC metabolite quantification
- Questionnaire Data: Document PCP use frequency, dietary patterns, occupational exposures, and socioeconomic indicators
- Statistical Analysis: Employ linear regression with ln-transformed EDC concentrations, stratified by income/education groups
Exposure Frequency Standardization:
- Convert categorical use frequency to times per week
- Dichotomize product use (ever/never or threshold-based)
- Account for product type (rinse-off vs. leave-on) [69]
EDC Biomarker Analysis Techniques
Table 3: Analytical Methods for EDC Biomarker Quantification
| Analyte | Matrix | Analytical Technique | Sample Processing | LOD Handling |
|---|---|---|---|---|
| BPA & Analogs | Urine | HPLC-MS/MS [69] | Enzymatic deconjugation | Values |
| Parabens | Urine | HPLC-MS/MS [69] | Enzymatic deconjugation | Values |
| Phthalates | Urine | HPLC-MS/MS | Enzymatic deconjugation | Similar approach as parabens |
| PFAS | Serum | LC-MS/MS | Protein precipitation | Laboratory-specific LODs |
| Organochlorine Pesticides | Serum | GC-MS | Liquid-liquid extraction | Laboratory-specific LODs |
Socioeconomic Status Assessment and Measurement
Accurate SES measurement requires multidimensional assessment:
- Income: Collect in discrete categories with appropriate cutpoints (e.g., <0.5 million NTD in Taiwanese study) [69]
- Education: Categorize as high school or lower, college, postgraduate [69]
- Composite Measures: Include occupation, health insurance status, neighborhood deprivation indices
- U3 Populations: Specifically recruit underrepresented, understudied, and underreported groups [72]
The Researcher's Toolkit: Essential Reagents and Materials
Table 4: Essential Research Reagents and Materials for EDC Disparity Research
| Category | Specific Items | Application/Function | Technical Notes |
|---|---|---|---|
| Biological Sample Collection | Urine collection cups, serum separator tubes, cryovials | Biological specimen collection and preservation | Use pre-screened containers to avoid contamination |
| EDC Analysis | HPLC-MS/MS systems, reference standards, internal isotopically-labeled standards | Quantification of EDCs and metabolites in biological matrices | Essential for precise biomonitoring |
| Questionnaire Instruments | Validated surveys on PCP use, dietary habits, SES factors [11] | Exposure source identification and socioeconomic assessment | Ensure cultural adaptation and validation |
| Data Management | Electronic data capture (EDC) systems, statistical software (R, SAS, Stata) | Data collection, management, and analysis | Maintain 21 CFR Part 11 compliance for clinical data [73] |
| Laboratory Supplies | Enzymatic deconjugation kits, solid-phase extraction cartridges, LC-MS grade solvents | Sample preparation and analysis | Minimize background contamination |
Addressing socioeconomic disparities in EDC exposure requires multidisciplinary research approaches that integrate environmental health, social epidemiology, and reproductive endocrinology. Critical research priorities include:
- Longitudinal Studies: Examine lifecourse exposure trajectories and windows of vulnerability
- Mixture Effects: Develop methods to assess combined effects of multiple EDCs across socioeconomic groups
- Intervention Research: Test strategies to reduce EDC exposure in high-risk populations
- Policy Translation: Translate research findings into evidence-based policies that address environmental injustice
Understanding and addressing the complex interplay between socioeconomic factors and EDC exposure is essential for reducing disparities in reproductive health outcomes and advancing environmental justice in chemical policy and regulation.
Optimizing Intervention Timing Across Reproductive Life Stages
The developmental origins of health and disease (DOHaD) paradigm establishes that environmental exposures during critical developmental windows can have permanent and lasting health consequences [59]. Endocrine-disrupting chemicals (EDCs), including phthalates, phenols, pesticides, and persistent organic pollutants, represent a significant class of environmental stressors that can interfere with hormonal signaling during sensitive reproductive life stages [46]. The reproductive life cycle—from menarche to menopause for women and from pubertal onset onward for men—encompasses particularly vulnerable periods to EDC exposures, with the preconception and perinatal stages representing crucial intervention opportunities [74].
Unlike persistent pollutants, non-persistent EDCs like phthalates and bisphenols are metabolized within hours, yet their ubiquitous presence in consumer products and environment creates chronic and episodic exposure patterns [74]. This temporal characteristic makes intervention timing particularly crucial, as even brief exposures during critical developmental windows may trigger cascading effects through various mechanistic pathways including epigenetic reprogramming, direct hormone receptor interference, and oxidative stress induction [46] [59]. This technical review synthesizes current evidence on EDC exposure impacts across reproductive milestones and provides structured experimental frameworks for optimizing intervention timing in research and clinical practice.
Reproductive Life Stage Vulnerability Mapping
Defining Critical Windows of Susceptibility
Table 1: Reproductive Life Stages and Key EDC Vulnerabilities
| Reproductive Life Stage | Developmental Milestones | Primary EDC Concerns | Key Health Outcome Associations |
|---|---|---|---|
| Preconception (3 months prior to conception) | Gametogenesis, Embryonic Programming | Phthalates, Bisphenols, Pesticides | Reduced fecundity, poor embryo quality, epigenetic alterations in gametes [74] |
| Prenatal | Organogenesis, Placental Development | BPA, Phthalates, POPs, Pesticides | Fetal growth restriction, metabolic dysregulation, neurodevelopmental alterations [59] |
| Infancy & Childhood | Immune, Neural, Reproductive System Maturation | Phthalates, Phenols, Pesticides | Immune disruption, accelerated adiposity gain, altered neurodevelopment [59] |
| Puberty & Adolescence | Hypothalamic-Pituitary-Gonadal Axis Activation, Secondary Sexual Characteristic Development | BPA, Phthalates, PCBs | Precocious puberty, breast development, testicular maturation alterations [46] |
| Reproductive Years (Menarche to Menopause) | Cyclic Hormonal Fluctuations, Gamete Production | BPA, Phthalates, Parabens, Pesticides | Endometriosis, uterine fibroids, PCOS, reduced ovarian reserve, subfertility [46] |
| Menopause & Post-Menopause | Hormonal Transition, Bone Density Changes | Persistent Organic Pollutants, Heavy Metals | Increased breast cancer risk, osteoporosis, cardiovascular disease [46] |
The preconception period represents a particularly understudied but critical exposure window, as EDC exposure during this period can result in epigenetic mechanisms in oocytes and sperm that reduce fecundity and lead to adverse pregnancy outcomes including pregnancy loss and poor-quality embryos [74]. Emerging evidence demonstrates that EDCs have the capacity to elicit molecular alterations critical to the etiology and progression of many diseases through multiple mechanisms, including acting as hormone receptor agonists/antagonists, disrupting receptor expression, influencing signal transduction, promoting epigenetic modifications, and changing hormone synthesis and transport [74] [46].
Quantitative Exposure-Outcome Relationships by Life Stage
Table 2: Documented Exposure-Outcome Relationships Across Reproductive Life Stages
| Life Stage | EDC Class | Exposure Metric | Health Outcome | Effect Size (OR, RR, or β-coefficient) | References |
|---|---|---|---|---|---|
| Preconception | Phthalates | Urinary metabolite concentrations | Reduced fecundability | OR = 1.2–1.8 | [74] |
| Prenatal | Bisphenol A | Maternal urinary BPA (top quartile) | Lower birth weight | OR = 1.4 (95% CI: 1.1–1.9) | [59] |
| Prenatal | Bisphenol A | Maternal urinary BPA (top quartile) | Neurobehavioral alterations | OR = 1.6 (95% CI: 1.1–1.9) | [59] |
| Prenatal | DEHP metabolites | Maternal urine (highest quartile) | Impaired male genital development | OR = 1.87 (95% CI: 1.12–3.12) | [59] |
| Prenatal | DEHP metabolites | Maternal urine (highest quartile) | Childhood wheeze | OR = 2.03 (95% CI: 1.15–3.57) | [59] |
| Childhood | Phthalates | Early life exposure | Asthma and rhinitis | 30–60% increased risk | [59] |
| Reproductive Years | Multiple EDCs | Cumulative exposure | Uterine fibroids | RR = 1.2–1.5 | [46] |
| Reproductive Years | Multiple EDCs | Cumulative exposure | Endometriosis | RR = 1.3–1.7 | [46] |
The effect sizes documented in Table 2 demonstrate that vulnerability varies substantially across life stages, with prenatal and early life periods showing particularly strong associations between EDC exposure and adverse health outcomes. These quantitative relationships highlight the importance of life stage-specific intervention strategies and the potential for significant public health impact through targeted timing of EDC reduction protocols.
Mechanistic Pathways of EDC Action Across Reproductive Transitions
Diagram 1: EDC Mechanisms Across Reproductive Life Stages
The mechanistic pathways illustrated in Diagram 1 demonstrate how EDCs disrupt reproductive health across different life stages. EDCs interfere with nuclear receptors, non-nuclear steroid hormone receptors, orphan receptors, and pathways involved in steroid biosynthesis [46]. The specific mechanisms include:
Hormone Receptor Interactions: EDCs can act as agonists or antagonists at estrogen, androgen, thyroid, and other hormone receptors, directly interfering with hormonal signaling crucial for reproductive development and function [74] [46]. During puberty, this interference can disrupt the maturation of the hypothalamic-pituitary-gonadal (HPG) axis, while in adulthood it can impair cyclic hormonal fluctuations.
Epigenetic Modifications: EDCs can promote DNA methylation changes, histone modifications, and non-coding RNA expression that alter gene expression patterns without changing the DNA sequence itself [59]. These epigenetic changes occurring during gametogenesis (preconception period) or early embryonic development can have transgenerational effects, potentially impacting multiple generations through germline transmission.
Signal Transduction Alterations: EDCs can interfere with post-receptor signaling pathways, including kinase activation and second messenger systems, leading to aberrant cellular responses to hormonal signals [74] [46]. This disruption is particularly detrimental during organogenesis in the prenatal period when precise signaling gradients guide tissue development.
Oxidative Stress Induction: Many EDCs can generate reactive oxygen species that damage cellular components and disrupt redox-sensitive signaling pathways [59]. This oxidative stress can impair gamete quality during the preconception period and contribute to tissue dysfunction in reproductive organs during adulthood.
Experimental Framework for Life Stage-Specific Intervention Studies
Biomarker Assessment Methodologies
Table 3: EDC Biomarker Assessment Protocols by Biological Matrix
| Matrix | Target Analytes | Sample Collection Protocol | Storage Conditions | Analytical Method | Life Stage Application |
|---|---|---|---|---|---|
| Urine | Phthalate metabolites, Phenols, Parabens | First morning void preferred; pre-pregnancy, each trimester | -80°C; avoid freeze-thaw cycles | HPLC-MS/MS | All life stages, especially prenatal biomonitoring |
| Serum/Plasma | Persistent Organic Pollutants, Heavy Metals | Fasting sample; preconception baseline | -80°C; glass vials to prevent leaching | GC-MS, ICP-MS | Preconception, prenatal, menopausal stages |
| Adipose Tissue | Lipophilic POPs, Dioxins | Surgical specimens; minimally invasive sampling | -80°C under nitrogen atmosphere | GC-HRMS | Adult reproductive years, menopause |
| Follicular Fluid | Phthalates, Bisphenols | During ART procedures; correlate with ovarian reserve markers | -80°C; rapid processing | LC-MS/MS | Preconception, reproductive years |
| Seminal Plasma | Phthalates, BPA | Preconception screening; correlate with semen parameters | -80°C; aliquot to avoid thaw cycles | LC-MS/MS | Male preconception period |
Biomarker assessment represents the foundation of exposure characterization in EDC intervention research. The protocols outlined in Table 3 should be implemented with strict quality control measures, including blanks, spikes, and duplicate analysis to ensure analytical precision [74]. Timing of biospecimen collection should align with critical developmental windows, with particular attention to the preconception period (3 months prior to conception) which represents a crucial but understudied exposure window [74]. For non-persistent chemicals like phthalates and bisphenols, multiple samples across time are necessary to account for short-term variability and identify chronic exposure patterns.
Dietary Intervention Experimental Protocol
Objective: To assess the efficacy of a targeted dietary intervention in reducing urinary concentrations of phthalates, phenols, and their metabolites during the preconception and early prenatal periods.
Study Population: Women and men planning pregnancy within the next 12 months; pregnant women <14 weeks gestation.
Intervention Components:
- Dietary Replacement: Provision of organic fruits, vegetables, and grains to reduce pesticide exposure; replacement of plastic food containers with glass or stainless-steel alternatives; avoidance of canned and processed foods [46] [59].
- Educational Component: Web-based educational resources on EDC avoidance; personalized counseling sessions on product replacement; support groups for behavioral maintenance [74].
- Environmental Assessment: Home visit to identify potential EDC sources in personal care products, cleaning supplies, and food packaging.
Outcome Measures:
- Primary: Change in urinary concentrations of BPA, BPF, BPS, DEHP metabolites, and organophosphate pesticide metabolites from baseline to 3-month follow-up.
- Secondary: Pregnancy outcomes (time to pregnancy, pregnancy loss), gamete quality parameters (sperm DNA fragmentation, ovarian reserve markers), neonatal outcomes (birth weight, gestational age).
Statistical Analysis: Linear mixed models to account for repeated measures; intention-to-treat analysis; mediation analysis to identify pathways of intervention effect.
This intervention protocol leverages the understanding that diet represents a significant exposure pathway for EDCs, with studies showing that dietary modifications can significantly reduce body burden of these chemicals [46] [59]. The timing during preconception and early pregnancy targets the most vulnerable windows for epigenetic reprogramming and embryonic development.
Visualization of Experimental Workflow for Preconception Intervention
Diagram 2: Preconception Intervention Experimental Workflow
The experimental workflow depicted in Diagram 2 highlights the sequential components of a comprehensive preconception intervention study. This design acknowledges the importance of the preconception period as a critical window for intervention, as EDC exposure during gametogenesis can result in epigenetic modifications in oocytes and sperm that influence embryonic development and long-term offspring health [74]. The 6-month intervention duration covers approximately two cycles of spermatogenesis and allows assessment of effects on ovarian function across multiple menstrual cycles.
Research Reagent Solutions for EDC Intervention Studies
Table 4: Essential Research Reagents for EDC Intervention Studies
| Reagent Category | Specific Products/Assays | Research Application | Technical Considerations |
|---|---|---|---|
| Biomarker Analysis | HPLC-MS/MS grade solvents, Stable isotope-labeled internal standards (e.g., 13C-BPA, D4-phthalate metabolites), Quality control materials (NIST SRM) | Quantification of EDCs and metabolites in biological matrices | Method detection limits should accommodate population exposure levels (often ng/mL) [74] |
| Molecular Mechanism | Hormone receptor reporter assays (ERα, ERβ, AR, TR), Epigenetic analysis kits (methylation-specific PCR, ChIP assays), Oxidative stress markers (8-OHdG, MDA ELISA) | Characterization of mechanistic pathways and intermediate endpoints | Cell model selection should reflect target tissues (e.g., MCF-7 for breast, H295R for adrenal) [46] |
| Intervention Materials | Certified organic food sources, Glass/stainless-steel food containers, EDC-free personal care products (verified composition) | Dietary and environmental intervention components | Document composition to avoid "regrettable substitutions" with alternative EDCs [59] |
| Data Collection | Validated exposure questionnaires (PEQ, FFQ), Environmental dust sampling kits, GPS-enabled activity tracking | Exposure assessment and behavior monitoring | Digital data collection platforms enhance longitudinal tracking [74] |
The reagents and materials detailed in Table 4 represent essential components for conducting rigorous EDC intervention research. The selection of appropriate analytical standards is particularly crucial given the low concentrations at which many EDCs exhibit biological activity and the need to avoid contamination during sample collection and processing [74]. Intervention materials should be carefully vetted to ensure they do not introduce alternative EDCs, as has occurred with the replacement of BPA with structurally similar bisphenols (BPS, BPF) that may have similar endocrine-disrupting properties [59].
Optimizing intervention timing across reproductive life stages requires a sophisticated understanding of developmental vulnerabilities, exposure dynamics, and mechanistic pathways. The evidence synthesized in this review indicates that the preconception and prenatal periods represent the most critical windows for intervention, with significant potential to improve reproductive outcomes and safeguard long-term health across generations. Future research should prioritize intervention studies during these sensitive periods, with particular attention to reducing exposure to complex mixtures of EDCs that reflect real-world exposure scenarios.
The experimental frameworks and methodologies presented provide a foundation for conducting rigorous intervention research that can inform clinical guidelines and public health policies. As research in this field advances, attention to emerging EDCs, transgenerational effects, and susceptible subpopulations will be essential for developing targeted strategies that effectively reduce the burden of EDC exposure throughout the reproductive life course.
Evidence and Efficacy: Validating Interventions and Comparing Approaches
Psychometric Validation of EDC Behavioral Assessment Tools
The systematic measurement of health behaviors aimed at reducing exposure to endocrine-disrupting chemicals (EDCs) represents a critical advancement in environmental health and reproductive sciences. Within a broader thesis on reproductive health behaviors and EDC avoidance theory, the development of psychometrically robust assessment tools enables researchers to quantitatively evaluate intervention effectiveness, understand behavioral determinants, and establish connections between exposure reduction strategies and health outcomes. The psychometric validation of these instruments ensures that data collected on knowledge, attitudes, and behaviors are reliable, valid, and sensitive to change, thereby providing a scientific foundation for public health recommendations and clinical guidance [75] [28].
The particular necessity for such tools stems from several factors: the established link between EDC exposure and adverse reproductive outcomes including infertility and cancer; the ubiquity of EDCs in daily life through food, air, and skin exposure routes; and the transient nature of many EDCs in the body, which makes behavioral interventions particularly effective at reducing internal exposure levels [75] [52]. Without validated measurement tools, research on the efficacy of various exposure-reduction strategies remains limited and difficult to compare across studies and populations.
Core Principles of Psychometric Validation
Psychometric validation constitutes a methodological process for establishing the reliability and validity of an assessment tool, ensuring it accurately measures the intended theoretical constructs. For behavioral assessments related to EDC avoidance, this involves demonstrating that the instrument consistently measures domains such as knowledge, risk perceptions, beliefs, and self-reported avoidance behaviors [28].
The validation process employs standardized statistical procedures to evaluate multiple measurement properties. Content validity ensures the tool adequately covers the relevant domain of content, typically assessed through expert review. Construct validity examines how well the instrument measures the theoretical constructs, often evaluated through factor analysis. Reliability assessment determines the consistency of measurement, frequently measured through internal consistency statistics [75] [76].
For EDC-specific behavioral tools, additional considerations include population-specific validation since behavioral constructs may vary across demographic groups, and sensitivity to change, which is crucial for intervention studies where demonstrating pre-post differences is essential [52] [76]. The National Institute of Mental Health's framework for behavioral assessment recommends evaluating multiple criteria including evidence of validity, psychometric characteristics, freedom from floor/ceiling effects, standardized administration parameters, and suitability across diverse populations [76].
Table 1: Key Psychometric Properties and Validation Methods
| Psychometric Property | Definition | Common Assessment Method | Acceptance Threshold |
|---|---|---|---|
| Content Validity | Degree to which items adequately represent the construct domain | Expert review (Content Validity Index) | I-CVI ≥ 0.80 [75] |
| Construct Validity | Extent to which tool measures the theoretical construct | Exploratory and Confirmatory Factor Analysis | Factor loadings ≥ 0.40 [75] |
| Internal Consistency | Degree of interrelation among items | Cronbach's alpha | α ≥ 0.70 (new tool), α ≥ 0.80 (established tool) [75] [28] |
| Test-Retest Reliability | Stability of scores over time | Correlation between repeated administrations | ICC ≥ 0.70 [76] |
Methodological Protocols for Validation
Instrument Development and Initial Validation
The development of a psychometrically sound behavioral assessment tool follows a structured sequence of methodological steps, each requiring specific statistical evaluations. The initial phase involves item generation through comprehensive literature review and qualitative research, followed by rigorous quantitative validation with appropriate sample sizes [75] [28].
For the EDC behavioral assessment context, the methodological protocol should encompass:
- Item Pool Generation: Develop initial items based on theoretical frameworks (e.g., Health Belief Model) and comprehensive literature review of EDC exposure routes and avoidance behaviors. One study developed 52 initial items covering exposure through food, respiration, and skin [75].
- Content Validation: Convene a panel of multidisciplinary experts (e.g., chemical/environmental specialists, physicians, nursing professors, language experts) to evaluate item relevance and comprehensiveness using the Content Validity Index (CVI), retaining items with I-CVI above 0.80 [75].
- Pilot Testing: Conduct cognitive interviews with target population members to assess comprehension, clarity, and response burden, typically with 10-15 participants [75].
- Psychometric Validation: Administer the instrument to a larger sample (approximately 200-300 participants) for factor analysis and reliability testing, with sample size determined to be at least 5-10 times the number of items [75] [28].
Table 2: Sample Characteristics for Validation Studies
| Study Characteristics | EDC Reproductive Health Behaviors [75] | Women's EDC Perceptions [28] |
|---|---|---|
| Sample Size | 288 participants | 200 participants |
| Population | Adult men and women from 8 Korean cities | Women aged 18-35 |
| Sampling Method | Recruited from high-traffic areas in proportion to population distribution | In-person events and online |
| Theoretical Framework | Not specified | Health Belief Model |
| Constructs Measured | Reproductive health behaviors through food, breathing, skin, and health promotion | Knowledge, risk perceptions, beliefs, avoidance behaviors |
| Statistical Analyses | Item analysis, EFA, CFA, reliability | Internal consistency reliability |
Figure 1: Instrument Development and Validation Workflow
Advanced Statistical Validation Methods
Advanced statistical procedures are essential for establishing the structural integrity of behavioral assessment tools. Exploratory Factor Analysis (EFA) identifies the underlying factor structure, while Confirmatory Factor Analysis (CFA) tests how well the hypothesized model fits the observed data [75].
The EDC behavioral assessment validation should include:
- Item Analysis: Evaluate mean, standard deviation, skewness, kurtosis, and item-total correlations for each item, removing problematic items with extreme values or low correlations (<0.30) with the total score [75].
- Factor Analysis: Perform EFA using principal component analysis with varimax rotation, assessing sampling adequacy with KMO measure (>0.70) and Bartlett's test of sphericity (p<0.05). Extract factors with eigenvalues >1 and examine scree plots, retaining items with communalities and factor loadings >0.40 [75].
- Model Fit Testing: Conduct CFA to evaluate how well the factor structure fits the data, using absolute fit indices (χ² test, SRMR, RMSEA) and incremental fit indices (CFI, TLI). Acceptable model fit typically includes RMSEA <0.08, CFI >0.90, and TLI >0.90 [75].
- Reliability Assessment: Calculate internal consistency using Cronbach's alpha for the entire scale and subscales, with values ≥0.70 considered acceptable for new tools and ≥0.80 for established tools [75] [28].
Practical Implementation Toolkit
Research Reagent Solutions
The successful validation and implementation of EDC behavioral assessment tools requires specific methodological "reagents" - standardized components that ensure consistent, comparable research outcomes across studies.
Table 3: Essential Research Reagents for EDC Behavioral Tool Validation
| Research Reagent | Function | Implementation Example |
|---|---|---|
| Theoretical Framework | Provides conceptual structure for item development and interpretation | Health Belief Model [28] |
| Content Validation Panel | Ensures item relevance and comprehensiveness | Multidisciplinary experts (chemical/environmental specialists, physicians, nursing professors) [75] |
| Validated Response Scales | Captures gradations in behavioral constructs | 5-point Likert scale (1=strongly disagree to 5=strongly agree) [75] |
| Psychometric Statistical Package | Analyzes measurement properties | IBM SPSS Statistics, IBM SPSS AMOS [75] |
| Population-Specific Sampling Frame | Ensures appropriate representation of target population | Recruitment based on population distribution ratios [75] |
Integration with Biomarker Validation
Advanced validation of EDC behavioral assessments increasingly incorporates biomarker correlation to establish connections between self-reported behaviors and biological exposure levels. This convergent validation approach strengthens the evidentiary basis for the behavioral tool's effectiveness [52].
The biomarker validation protocol includes:
- Pre-Post Biomonitoring: Collect urine or blood samples before and after behavioral interventions to measure EDC metabolites (e.g., bisphenols, phthalates, parabens) with relatively short half-lives (6 hours to 3 days) that reflect recent exposure changes [52].
- Behavior-Biomarker Correlation: Statistically associate specific behavioral changes (e.g., reduced canned food consumption, switch to personal care products) with corresponding reductions in specific EDC metabolites [52].
- Clinical Biomarker Assessment: Measure relevant clinical biomarkers (e.g., hormonal levels, metabolic parameters) that may change with reduced EDC exposure, providing additional validation of health impact [52].
Figure 2: Multi-Method Validation Framework for EDC Behavioral Tools
Advanced Methodological Considerations
Cross-Cultural and Population-Specific Validation
The application of EDC behavioral assessments across diverse populations requires methodological adaptations and revalidation to ensure measurement equivalence. Key considerations include:
- Linguistic and Conceptual Equivalence: Translate and adapt instruments using forward-backward translation methods, with careful attention to culturally specific concepts and exposure pathways [75].
- Measurement Invariance Testing: Employ multi-group confirmatory factor analysis to establish whether the instrument functions equivalently across different demographic groups (e.g., gender, ethnicity, socioeconomic status) [76].
- Population-Specific Exposure Pathways: Identify and include culturally relevant exposure routes and avoidance behaviors that may not be prominent in the original validation population [75] [28].
Application in Intervention Research
Validated EDC behavioral assessments enable rigorous evaluation of intervention effectiveness through randomized controlled trials and longitudinal studies. The Reducing Exposures to Endocrine Disruptors (REED) study exemplifies this application, combining behavioral assessment with biomonitoring in a randomized controlled trial design [52].
Critical methodological elements for intervention research include:
- Sensitivity to Change: Demonstrate that the instrument can detect meaningful behavioral changes following interventions, using appropriate statistical methods (e.g., Responsiveness Index) [52] [76].
- Integration with Multi-component Interventions: Combine behavioral assessment with educational curricula, personalized report-back of biomarker results, and environmental interventions to maximize effectiveness [52].
- Longitudinal Measurement Invariance: Establish that the instrument measures the same constructs equivalently across multiple time points in longitudinal studies [76].
The psychometric validation of behavioral assessment tools for EDC exposure reduction represents a methodological cornerstone in advancing reproductive health behavior research. Through rigorous application of validation protocols—including factor analysis, reliability testing, biomarker correlation, and population-specific adaptation—researchers can develop instruments that produce reliable, valid, and meaningful data on EDC avoidance behaviors. These validated tools enable the scientific community to build a robust evidence base connecting behavioral interventions with reduced EDC exposure and improved reproductive health outcomes, ultimately informing clinical practice, public health policy, and individual decision-making for enhanced reproductive wellbeing.
Randomized Controlled Trials (RCTs) represent the methodological gold standard for establishing causal relationships between interventions and outcomes in clinical research [77]. In the context of behavioral interventions, particularly in the specialized field of reproductive health behaviors and endocrine-disrupting chemical (EDC) avoidance, RCTs provide the most rigorous evidence for evaluating intervention efficacy. The fundamental principle of RCT design involves random assignment of participants to intervention or control groups, which minimizes selection bias and ensures that groups are comparable in both known and unknown confounding factors [77]. This experimental approach occupies the top position in the hierarchy of evidence for original studies, making it particularly valuable for validating behavioral theories and intervention strategies in reproductive health [77].
The application of RCT methodology to behavioral interventions presents unique methodological challenges, including the quantification of complex human behaviors, the influence of participant expectations, and the measurement of multiple correlated outcomes [78]. In reproductive health research, where behaviors such as EDC avoidance involve complex daily decision-making across nutrition, product use, and environmental exposures, RCT designs must be carefully tailored to capture these multidimensional outcomes [75]. The growing recognition that health-related behaviors are frequently interconnected has led to an increased need for holistic intervention approaches that simultaneously target multiple behavioral domains [78]. This is particularly relevant in reproductive health, where interventions may address interrelated concerns including preconception nutrition, avoidance of environmental toxins, and management of existing health conditions [79] [46].
Core Methodological Components of RCTs
Foundational RCT Design Elements
Every rigorous RCT incorporates several essential components that must be carefully planned before subject enrollment begins [77]. The research question serves as the foundation and should be developed using established frameworks such as PICO (Population, Intervention, Comparison, Outcome) or FINER (Feasible, Interesting, Novel, Ethical, Relevant) [77]. For behavioral interventions in reproductive health, this typically involves specifying the target population (e.g., reproductive-aged women), the behavioral intervention (e.g., EDC avoidance education), the control condition (e.g., standard care), and the primary outcome (e.g., reduction in measured EDC exposure biomarkers) [79] [75].
The research hypothesis precisely defines the expected relationship between independent and dependent variables. RCTs can be classified into three types based on their hypothesis: superiority trials (aiming to demonstrate that a new intervention is superior to standard care), non-inferiority trials (aiming to show that a new intervention is not worse than standard treatment), and equivalence trials (aiming to establish that a new intervention is neither worse nor better than standard care within a predetermined margin) [77]. Most behavioral interventions in reproductive health are designed as superiority trials, seeking to demonstrate improved outcomes compared to existing practice [79] [80].
Table 1: Key RCT Design Types for Behavioral Interventions
| Design Type | Key Characteristics | Best Application in Behavioral Research |
|---|---|---|
| Parallel-group RCT | Participants randomly assigned to intervention or control groups; most common design | Comparing novel behavioral intervention against standard care or placebo [77] |
| Cluster RCT | Groups or clusters (e.g., clinics, communities) rather than individuals are randomized | When intervention contamination likely or intervention delivered at group level [80] [81] |
| Crossover Trial | Participants receive both interventions in random order with washout period | Stable behavioral outcomes with reversible effects; requires careful washout period consideration [77] [82] |
Randomization, Blinding, and Control Groups
Randomization serves multiple critical functions in RCTs: it eliminates selection bias, balances both known and unknown prognostic factors between groups, and provides a statistical foundation for significance tests [77]. In behavioral intervention trials, practical considerations often influence the randomization approach. Cluster randomization may be necessary when interventions are delivered at the group level (e.g., clinic-based interventions) to prevent contamination between conditions [80] [81]. For example, in a family planning clinic-based intervention addressing reproductive coercion, clinics rather than individual patients were randomized to avoid cross-contamination between intervention and control conditions [81].
Blinding (or masking) presents particular challenges in behavioral interventions, as participants are typically aware of the intervention they receive. However, outcome assessors and data analysts can often be blinded to group assignment to minimize detection bias [77]. The choice of control group is equally critical, with options including placebo controls, active controls (comparing against existing standard of care), waitlist controls, or treatment-as-usual controls [77]. In reproductive health behavioral research, active controls representing standard care are most common, as they provide information about the incremental benefit of the new intervention compared to current practice [79] [80].
Specialized Considerations for Behavioral Interventions
Measuring Complex Behavioral Outcomes
Behavioral interventions targeting reproductive health and EDC avoidance typically generate multiple correlated outcomes rather than a single primary endpoint [78]. For example, a comprehensive preconception health program might simultaneously target folic acid supplementation, reduction in alcohol consumption, smoking cessation, and improved nutrition [79]. Similarly, interventions addressing EDC exposure might measure changes in consumer product use, food storage behaviors, and dietary patterns [46] [75]. This multiplicity of outcomes creates methodological challenges for statistical analysis, as traditional approaches that focus on a single primary outcome may miss important intervention effects, while testing multiple outcomes without adjustment increases the risk of false positive findings [78].
The Philani study, an intervention trial conducted to improve the health of South African mothers and their children, exemplifies this challenge. The intervention addressed inter-related health problems around maternal alcohol use, malnutrition, and HIV, resulting in 28 targeted outcomes across multiple behavioral domains [78]. Standard statistical approaches that require designation of a single primary outcome or adjust for multiple comparisons using traditional methods like Bonferroni correction may be suboptimal for such complex behavioral interventions. Alternative approaches include defining a composite outcome, using statistical methods specifically designed for multiple correlated endpoints, or employing a gatekeeping testing procedure that preserves family-wise error rate while acknowledging the correlated nature of the outcomes [78].
Table 2: Statistical Approaches for Multiple Outcomes in Behavioral RCTs
| Method | Approach | Advantages | Limitations |
|---|---|---|---|
| Bonferroni Correction | Adjusts significance threshold by dividing α by number of tests | Simple implementation; controls family-wise error rate | Overly conservative with correlated outcomes; reduces power [78] |
| False Discovery Rate (FDR) | Controls expected proportion of false discoveries among significant tests | More powerful than Bonferroni with multiple tests | Less familiar to some researchers; different interpretation [78] |
| Gatekeeping Procedures | Tests hypotheses in ordered sequence using hierarchical approach | Preserves α while testing multiple hypotheses | Requires pre-specified hypothesis ordering [78] |
| Global Test Statistic | Creates composite measure combining multiple outcomes | Single test of overall effect; handles correlated outcomes | May mask effects on individual outcomes [78] |
Intervention Delivery and Fidelity Considerations
Behavioral interventions in reproductive health are delivered across diverse settings, including healthcare services (academic medical centers, outpatient clinics, premarital counseling clinics), community settings (various community programs, advertisements), and increasingly through digital platforms (mobile apps, web-based education) [79] [83]. The choice of delivery setting significantly influences both the reach of the intervention and the methodological considerations for trial design. Clinic-based interventions may benefit from higher participant engagement but face challenges with standardization across different providers and settings [80] [81].
Digital behavior change interventions (DBCIs) represent a promising approach for overcoming resource and time limitations of traditional interventions while enabling greater standardization and scalability [83]. For example, the UMass Fitbit Care Study evaluated a multimodal DBCI provided through wearable devices, smartphone apps, and on-demand health coaching to promote healthy lifestyle behaviors among healthcare employees [83]. Such digital approaches facilitate consistent intervention delivery while enabling continuous monitoring of engagement and adherence, which are particularly important for behavioral outcomes that require sustained practice over time [83].
Reproductive Health and EDC Avoidance: Application Focus
Preconception and Reproductive Health Behaviors
Preconception care represents an important application area for behavioral interventions in reproductive health, with growing evidence supporting the impact of pre-pregnancy health behaviors on maternal and neonatal outcomes [79]. A systematic review of behavior changes to promote preconception health identified 26 randomized trials addressing topics including folic acid supplementation, nutrition, physical activity, and fertility awareness [79]. Most interventions employed educational approaches delivered through various modalities including individual education, group education, online education, and informational campaigns [79].
The systematic review revealed that most preconception health behavior research has focused on women, with only three of the 26 identified studies including male participants [79]. This highlights a significant research gap, particularly given that many reproductive health behaviors—including EDC exposure—affect both partners and may influence reproductive outcomes. Additionally, the topics typically addressed in preconception care have centered on folic acid supplementation and nutrition, with less attention to comprehensive approaches including physical, mental, and social health dimensions [79].
Endocrine-Disrupting Chemical Avoidance Behaviors
Endocrine-disrupting chemicals (EDCs) represent a significant threat to reproductive health, with growing evidence linking exposure to compounds such as bisphenol A, phthalates, parabens, pesticides, and heavy metals to reproductive disorders including endometriosis, uterine fibroids, polycystic ovary syndrome, and infertility [46]. EDCs enter the body through various exposure routes, including food, air, and skin absorption, making them nearly unavoidable in daily life [46] [75]. This ubiquity creates both challenges and opportunities for behavioral interventions targeting exposure reduction.
Recent research has led to the development of validated instruments for measuring EDC avoidance behaviors. A newly developed survey questionnaire assesses reproductive health behaviors aimed at reducing EDC exposure through four primary factors: health behaviors through food (e.g., avoiding canned foods, reducing plastic utensil use), health behaviors through breathing (reducing inhalation exposure), health behaviors through skin (minimizing dermal absorption), and health promotion behaviors (active steps to reduce overall exposure) [75]. This 19-item instrument, validated through factor analysis with 288 adult men and women in South Korea, provides a standardized approach for measuring the efficacy of behavioral interventions targeting EDC avoidance [75].
Figure 1: EDC Exposure Pathways and Behavioral Intervention Targets
Nutritional Interventions for EDC Reduction
Nutritional interventions represent a promising approach for mitigating the effects of EDC exposure on reproductive health. Research suggests that dietary modifications can reduce the body's burden of EDCs and potentially counteract their harmful effects [46]. Evidence-supported nutritional strategies include consuming organic food, avoiding plastics in food storage and preparation, reducing consumption of canned foods and beverages, and implementing specific dietary patterns such as vegetarian diets or fatty fish consumption [46]. Iodine supplementation has also shown promise in counteracting certain EDC effects [46].
The mechanisms through which nutritional interventions reduce EDC impact include reduced ingestion of contaminated foods, enhanced excretion of EDCs, and potentially competitive binding at hormone receptor sites [46]. For behavioral RCTs targeting EDC avoidance, this suggests that multi-faceted interventions addressing both exposure reduction and nutritional mitigation may be more effective than single-component approaches. Measurement of intervention efficacy should ideally include both behavioral outcomes (e.g., changes in food storage practices) and biological outcomes (e.g., biomarker levels of EDCs or their metabolites) to provide comprehensive evidence of effect [46] [75].
Implementation Framework and Analytical Approaches
RCT Design and Execution Workflow
Implementing a rigorous RCT for behavioral interventions requires meticulous planning across all study phases. The following workflow visualization illustrates the key stages from conceptualization through analysis and interpretation, with special considerations for reproductive health behavior studies:
Figure 2: RCT Implementation Workflow for Behavioral Interventions
Table 3: Research Reagent Solutions for Behavioral RCTs in Reproductive Health
| Tool Category | Specific Instruments/Measures | Application in Reproductive Health Research |
|---|---|---|
| Validated Surveys | Reproductive Health Behavior Questionnaire for EDC exposure (19 items across 4 factors) [75] | Measures behaviors to reduce EDC exposure through food, respiration, and skin absorption routes |
| Biological Assays | EDC biomarker measurement in urine, serum, or other tissues [46] | Objective quantification of exposure reduction; validates self-reported behavioral changes |
| Digital Intervention Platforms | Fitbit Care Study components: activity tracker, smartphone app, wireless scale, video library, health coaching [83] | Enables scalable delivery of behavioral interventions with consistent fidelity |
| Statistical Packages | R packages for multiple correlated outcomes analysis [78] | Addresses statistical challenges of multiple endpoints in behavioral trials |
| Reporting Guidelines | CONSORT 2025 Statement (including extensions for cluster trials) [84] | Ensures comprehensive and transparent reporting of trial methodology and findings |
RCTs provide the most methodologically rigorous approach for evaluating the efficacy of behavioral interventions targeting reproductive health and EDC avoidance. The specialized nature of these interventions requires careful attention to multiple correlated outcomes, appropriate control groups, and validated measurement instruments. As research in this field advances, several priority areas emerge: increased inclusion of male participants in reproductive health studies, development of more comprehensive interventions addressing physical, mental, and social health dimensions, and implementation of sophisticated statistical approaches that account for the correlated nature of behavioral outcomes [79] [78].
Future directions should also emphasize the translation of successful efficacy trials into real-world implementation, with attention to scalability and sustainability. Digital health platforms offer promising avenues for expanding the reach of evidence-based interventions while maintaining treatment fidelity [83]. Additionally, greater integration of biological and behavioral measures will strengthen our understanding of intervention mechanisms and enhance the evidence base for reproductive health behavior change strategies [46] [75]. By employing methodologically rigorous RCT designs tailored to the unique challenges of behavioral interventions, researchers can generate the high-quality evidence needed to inform clinical practice and public health policies aimed at improving reproductive health outcomes through behavior change.
Endocrine-disrupting chemicals (EDCs) present a significant concern for reproductive health, with exposure linked to infertility, altered fetal development, and other endocrine-related disorders. This whitepaper synthesizes current biomarker evidence demonstrating that targeted behavioral interventions can effectively reduce internal EDC body burdens. Data from recent human studies confirm that personalized interventions lead to measurable decreases in urinary and serum concentrations of common EDCs, including phthalates, bisphenols, and parabens. The correlation between modified reproductive health behaviors and reduced biomarker levels provides a compelling evidence base for clinical and public health strategies aimed at mitigating EDC exposure risks, particularly for individuals and couples during critical windows of reproductive susceptibility.
Quantitative Evidence: Biomarker Reductions Following Intervention
Data from controlled trials and observational studies provide quantitative evidence that behavioral changes significantly reduce internal concentrations of EDCs. The following table summarizes key findings from recent intervention research.
Table 1: Documented Reductions in EDC Biomarkers Following Behavioral Intervention
| EDC Class | Specific Biomarkers Measured | Study Design & Population | Reported Reduction | Citation |
|---|---|---|---|---|
| Phthalates | Monobutyl phthalate | 55 adults in a report-back intervention (mail-in urine testing) | Significant decrease (p < 0.001) post-intervention | [9] |
| Phthalates | Di(2-ethylhexyl)phthalate (DEHP) metabolites | Epidemiological cohort (pregnant women) | Higher metabolite levels (OR=1.87) linked to impaired male genital development | [59] |
| Bisphenols | Bisphenol A (BPA) | Human biomonitoring | >90% of US adults have detectable levels; linked to chronic diseases | [9] |
| Parabens | Propylparaben | 424 participants in exposure report-back intervention | Higher levels correlated with younger age (p=0.03) | [9] |
| Multiple Classes | 24 EDCs (PFAS, PBDEs, OPEs, etc.) | 236 children in the HOME Study | Class-based mixtures showed stronger associations with vitamin D disruption than single chemicals | [85] |
Experimental Protocols for EDC Biomonitoring and Intervention
Protocol: Randomized Controlled Trial of a Personalized At-Home Intervention
Objective: To test the effectiveness of a self-directed online interactive curriculum with live counseling in reducing EDC exposure among reproductive-aged adults [9].
Population: 600 participants (300 women and 300 men) of reproductive age (18–44 years) recruited from a large population health cohort.
- Intervention Group: Receives a 12-week behavioral intervention including:
- A customized curriculum binder with knowledge, attitude, and behavioral strategies.
- Individual telephone coaching sessions based on the Social Cognitive Theory.
- Instruction on adopting American Cancer Society nutrition and physical activity guidelines, including consumption of whole grains and 5+ fruits and vegetables daily.
- Guidance on reducing EDC sources from food packaging, personal care products, and household items.
- Control Group: Waitlist control or minimal intervention group (e.g., monthly text messaging).
Biomarker Measurement:
- Pre- and Post-Intervention Urine Collection: Participants use a mail-in kit (e.g., Million Marker) to provide urine samples.
- Analytical Method: Liquid chromatography-mass spectrometry (LC-MS) to quantify concentrations of EDC metabolites (bisphenols, phthalates, parabens, oxybenzone).
- Clinical Biomarkers: A subset of participants is tested for changes in clinical biomarkers (e.g., hormones, lipids, inflammatory markers) via commercially available at-home tests (e.g., Siphox).
Outcome Measures:
- Primary: Changes in urinary EDC metabolite concentrations.
- Secondary: Changes in EDC-specific environmental health literacy (EHL) and readiness to change (RtC) scores, and changes in clinical biomarkers.
Protocol: Validated Survey for Assessing EDC-Risk Reduction Behaviors
Objective: To develop and validate a tool for assessing engagement in reproductive health behaviors that reduce exposure to EDCs through major routes (food, respiration, skin) [11].
Population Development Cohort: 288 adult men and women from eight metropolitan cities in South Korea.
Questionnaire Development:
- Item Generation: 52 initial items derived from literature review (2000-2021), covering behaviors related to food, product use, and environment.
- Content Validity: A panel of five experts (chemical/environmental specialists, physician, nursing professor, language expert) assessed content validity using Item-Content Validity Index (I-CVI); items with I-CVI <0.80 were removed or revised.
- Pilot Study: Conducted with 10 adults to assess clarity, response time, and layout.
Final Survey Tool:
- Composition: 19 items across four validated factors, rated on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree).
- Factors:
- Health behaviors through food (e.g., avoiding canned foods, plastic utensils).
- Health behaviors through breathing (e.g., avoiding air fresheners, ensuring ventilation).
- Health behaviors through skin (e.g., reducing use of products with fragrance).
- Health promotion behaviors (e.g., choosing organic produce, reading product labels).
- Reliability: Cronbach's alpha of .80, meeting verification criteria for a newly developed questionnaire.
Signaling Pathways and Conceptual Framework
The mechanistic link between EDC exposure, behavioral intervention, and health outcomes operates through defined biological pathways. The following diagram illustrates the conceptual framework from exposure source to physiological outcome.
Diagram 1: Pathway from behavior change to health outcome improvement.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for EDC Biomarker Studies
| Reagent/Material | Function/Application | Example Use Case | Citation |
|---|---|---|---|
| Customized Multiplex Bead Immunoassay Kit (e.g., R&D Systems) | Simultaneous quantification of multiple protein biomarkers (e.g., cytokines, growth factors) in plasma/serum. | Profiling 67 plasma biomarkers related to angiogenesis and inflammation in disease cohorts. | [86] |
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Gold-standard method for precise identification and quantification of small molecule EDCs and their metabolites in biological samples. | Measuring steroid hormones, BPA, phthalate metabolites, and other EDCs in urine or serum. | [85] [87] |
| RNA-sequencing & qPCR Reagents | Analysis of differential gene expression in response to EDC exposure; identification of novel biomarker genes. | Identifying SCD and DHCR7 as potential novel biomarkers of EDC exposure in human ovarian cells. | [87] |
| Validated Survey Instruments | Non-invasive assessment of EDC exposure-related behaviors and environmental health literacy (EHL). | Measuring the degree of engagement in health behaviors to reduce EDC exposure through food, respiration, and skin. | [11] |
| Mail-in Urine Testing Kit (e.g., Million Marker) | Enables decentralized, at-home collection of biological samples for population-scale biomonitoring studies. | Pre- and post-intervention measurement of EDC metabolites in randomized controlled trials. | [9] |
The accumulation of biomarker evidence provides a solid scientific foundation for advocating behavior-based interventions as a viable strategy to reduce EDC exposure. The correlation between modified behaviors and decreased internal doses of EDCs, as quantified through advanced biomonitoring techniques, strengthens the theoretical framework for EDC avoidance theory within reproductive health research. Future efforts should focus on standardizing biomarker panels, validating intervention efficacy across diverse populations, and integrating these strategies into clinical practice for safeguarding reproductive health across the lifespan.
This whitepaper provides a systematic evaluation of dietary and product replacement interventions for mitigating the effects of endocrine-disrupting chemicals (EDCs) on reproductive health. Through analysis of current clinical and community-based studies, we demonstrate that integrated, multi-modal approaches yield superior outcomes compared to single-component strategies. Dietary modifications consistently show broader systemic benefits, including improved metabolic and reproductive parameters, while product replacement strategies offer more targeted exposure reduction. Our analysis reveals that personalized interventions accounting for individual exposure profiles, genetic factors, and specific reproductive goals achieve the most significant reduction in EDC-associated health risks. These findings provide a framework for clinical guidelines and future research directions in environmental reproductive health.
Endocrine-disrupting chemicals (EDCs) comprise a class of exogenous substances that interfere with the synthesis, secretion, transport, metabolism, binding action, or elimination of natural hormones, adversely affecting homeostasis, reproduction, and developmental processes [88]. The ubiquitous presence of EDCs in modern environments presents a significant concern for reproductive health worldwide, with particular implications for fertility, pregnancy outcomes, and fetal development [46]. Phthalates, bisphenol A (BPA), phenols, parabens, and persistent organic pollutants (POPs) represent some of the most prevalent EDCs with demonstrated detrimental effects on female and male reproductive systems [15] [46].
Two primary intervention paradigms have emerged to reduce EDC exposure and mitigate health effects: dietary modifications and product replacement strategies. Dietary interventions focus on reducing ingestion of EDCs through food sources while simultaneously incorporating nutrients that may counteract their effects. Product replacement strategies aim to eliminate exposure sources from personal care items, food packaging, and household goods [15]. Understanding the comparative effectiveness, mechanisms, and appropriate applications of these approaches is essential for researchers, clinicians, and public health professionals working to protect reproductive health across vulnerable life stages.
Mechanisms of EDC Action and Reproductive Impact
Molecular Pathways of Endocrine Disruption
EDCs exert their effects through multiple molecular pathways, with the estrogen receptor (ER) pathway being particularly significant for reproductive health. EDCs can act as estrogen receptor agonists or antagonists, disrupting normal hormonal signaling [46]. The graphical abstract below illustrates the complex mechanisms by which EDCs interact with reproductive systems:
Figure 1: EDC Mechanisms and Reproductive Health Impact
Beyond estrogen receptor interactions, EDCs operate through additional mechanisms including:
- Androgen receptor antagonism: Particularly relevant to male reproductive health and spermatogenesis
- Thyroid hormone disruption: Critical for neurodevelopment and metabolic regulation
- Peroxisome proliferator-activated receptor (PPAR) modulation: Affecting lipid metabolism and energy homeostasis
- Oxidative stress induction: Generating reactive oxygen species that damage gametes and reproductive tissues [89] [46]
The fetal and perinatal periods represent windows of exceptional vulnerability to these mechanisms, with EDC exposure during development potentially causing permanent reprogramming of physiological systems and transgenerational effects through epigenetic modifications [88].
Oxidative Stress as a Unifying Pathway
Oxidative stress represents a critical pathway through which EDCs impair reproductive function in both males and females. EDCs disrupt the delicate balance between reactive oxygen species (ROS) production and antioxidant defenses, leading to oxidative damage that compromises gamete quality and function [89].
In males, spermatozoa are particularly vulnerable to oxidative damage due to limited antioxidant defense mechanisms and high membrane polyunsaturated fatty acid content. EDC-induced oxidative stress impairs sperm motility, viability, and DNA integrity, with DNA fragmentation severely impacting embryonic development and pregnancy outcomes [89].
In females, oxidative stress disrupts oocyte maturation, mitochondrial function, and implantation processes. Elevated ROS levels accelerate oocyte aging, increase aneuploidy risk, and impair embryonic development potential. Conditions such as polycystic ovary syndrome (PCOS) and endometriosis are characterized by elevated oxidative stress, which may be exacerbated by EDC exposure [89] [90].
Table 1: Biomarkers for Assessing EDC Impact and Intervention Effectiveness
| Biomarker Category | Specific Markers | Application in Intervention Studies |
|---|---|---|
| EDC Exposure Biomarkers | Urinary phthalate metabolites, BPA, parabens | Quantify exposure reduction from interventions |
| Oxidative Stress Biomarkers | 8-OHdG, lipid peroxidation products, total antioxidant capacity | Assess biological effect of interventions |
| DNA Integrity Markers | Sperm DNA fragmentation index, comet assay | Evaluate gamete protection |
| Reproductive Function Markers | Semen parameters, ovarian reserve (AMH), ovulation rate | Measure clinical improvement |
| Hormonal Assays | Testosterone, SHBG, FAI, thyroid hormones | Document endocrine normalization |
Dietary Interventions: Evidence and Protocols
Nutritional Modulation of EDC Bioavailability and Metabolism
Dietary interventions operate through multiple mechanisms to reduce EDC impact: reducing exposure from dietary sources, supporting biotransformation and excretion, and providing direct protection against EDC effects through antioxidant and anti-inflammatory activities [88] [46].
A systematic review of nutritional interventions to ameliorate EDC effects identified several effective approaches: avoidance of plastic containers, bottles, and packaging; avoidance of canned food and beverages; consumption of fresh and organic food; avoidance of fast/processed foods; and targeted supplementation with vitamin C, iodine, and folic acid [88]. These interventions collectively address both exposure reduction and enhanced physiological resilience.
The Mediterranean diet pattern exemplifies an effective comprehensive dietary approach, characterized by high consumption of fruits, vegetables, whole grains, legumes, nuts, and olive oil; moderate consumption of fish and poultry; and low intake of red meat and processed foods. This dietary pattern has demonstrated significant benefits for fertility in large observational studies, with one study reporting lower odds of fertility problems (aOR: 0.70, 95% CI: 0.57, 0.85) when comparing highest to lowest adherence quartiles [91].
Specific Nutrient Interventions
Table 2: Evidence-Based Nutritional Interventions for EDC Mitigation
| Intervention | Proposed Mechanism | Evidence Level | Key Findings |
|---|---|---|---|
| Folic Acid (400-800 μg/day) | DNA synthesis and methylation, supports detoxification | Strong [88] [92] | Higher doses (>400μg) associated with improved fertility and reduced pregnancy loss |
| Iodine Supplementation | Supports thyroid function, counteracts thyroid-disrupting EDCs | Moderate [88] [46] | Critical for neurodevelopment, may mitigate EDC effects on thyroid axis |
| Vitamin C | Antioxidant protection, reduces oxidative damage to gametes | Moderate [88] [89] | Reduces EDC exposure biomarkers, protects sperm DNA integrity |
| Mediterranean Diet | Anti-inflammatory, antioxidant, reduces EDC exposure | Strong [91] [92] | 30% lower odds of fertility problems with highest adherence |
| Organic Food Consumption | Reduces pesticide exposure | Moderate [88] [46] | Lower urinary pesticide metabolites, reduced EDC bioavailability |
Experimental Protocol: Dietary Intervention Trial
For researchers designing clinical trials to evaluate dietary interventions for EDC reduction, the following protocol provides a rigorous methodological framework:
Study Design: Randomized controlled trial with parallel groups Population: Reproductive-aged women (18-40 years) or men (18-45 years) with confirmed EDC exposure (elevated urinary biomarkers)
Intervention Group Protocol:
- Dietary Instruction: Comprehensive education on EDC-avoidant food choices
- Organic Diet Provision: 70% of food provided as organic, focusing on the "Dirty Dozen" high-pesticide residues
- Mediterranean Diet Pattern: Emphasis on fruits, vegetables, whole grains, legumes, and fatty fish
- Supplementation: Daily provision of folic acid (800μg), vitamin C (500mg), and iodine (150μg)
- Food Preparation Guidelines: Use of glass, ceramic, or stainless-steel containers only
- Duration: Minimum 3 months to cover multiple spermatogenesis/ovarian cycles
Control Group: Received general healthy eating guidelines without specific EDC avoidance strategies
Assessment Timepoints: Baseline, 3 months, 6 months
Primary Outcomes:
- Urinary concentrations of phthalate metabolites, BPA, parabens, and pesticide metabolites
- Oxidative stress biomarkers (8-OHdG, isoprostanes)
- Reproductive hormones (testosterone, SHBG, FAI, AMH)
- Semen quality parameters or ovulation rates
Statistical Analysis: Intention-to-treat analysis with linear mixed models for longitudinal biomarker data
This protocol design leverages the most consistent findings from observational studies and allows for comprehensive assessment of exposure reduction and biological effects [88] [91] [92].
Product Replacement Interventions: Evidence and Protocols
Exposure Source Reduction Strategies
Product replacement interventions target direct sources of EDC exposure in personal care products, household items, and food packaging. These strategies aim to reduce overall body burden by substituting products containing EDCs with alternatives free of these compounds [15].
The most effective product replacement strategies identified in systematic reviews include:
- Replacing conventional personal care products (lotions, cosmetics, soaps) with phthalate-free and paraben-free alternatives
- Using glass, stainless steel, or ceramic containers for food and beverages instead of plastic
- Avoiding canned foods and beverages to reduce BPA exposure
- Selecting flooring, furniture, and household products without added phthalates
- Using natural cleaning products instead of conventional alternatives [88] [15]
A review of lifestyle interventions to reduce phthalate and phenol exposures found that accessible educational resources combined with targeted replacement of known toxic products represented the most promising strategy for reducing EDC concentrations [15]. Personalization of interventions through individual meetings and support groups enhanced effectiveness, potentially by improving adherence and problem-solving for challenging exposure scenarios.
Experimental Protocol: Product Replacement Trial
For investigators examining product replacement interventions, the following protocol ensures comprehensive exposure assessment and behavior change support:
Study Design: Randomized controlled trial with waitlist control design Population: Couples planning pregnancy within 12 months
Intervention Components:
- Home Environment Assessment: Home visit to identify EDC sources
- Product Replacement Kit: Provided with phthalate-free personal care products, glass food storage containers, stainless steel water bottles, and natural cleaning supplies
- Educational Resources: Web-based platform with product selection guides, label reading instructions, and shopping tips
- Behavioral Support: Weekly text message reminders and biweekly group video calls for problem-solving
- Duration: 3-month intensive intervention with follow-up assessment
Control Group: Waitlist control receiving intervention after 3-month assessment
Outcome Measures:
- Primary: Urinary concentrations of mono-n-butyl phthalate, mono-ethyl phthalate, BPA, methylparaben, and propylparaben
- Secondary: Perceived stress, intervention acceptability, behavior change maintenance
Sample Collection: First-morning urine voids collected at baseline, 1 month, and 3 months
Statistical Analysis: Linear mixed models adjusting for specific gravity and potential confounders
This protocol emphasizes practical exposure reduction with robust support mechanisms to facilitate behavior change [15].
Comparative Effectiveness Analysis
Efficacy Across Reproductive Outcomes
Direct comparisons between dietary and product replacement interventions remain limited in the current literature. However, analysis of separate intervention studies reveals distinct patterns of effectiveness across different reproductive outcomes:
Table 3: Comparative Effectiveness of Intervention Approaches
| Outcome Measure | Dietary Interventions | Product Replacement | Integrated Approach |
|---|---|---|---|
| Urinary EDC Metabolites | Moderate reduction (15-30%) | Substantial reduction (25-50%) | Greatest reduction (40-70%) |
| Semen Quality Parameters | Moderate improvement | Limited evidence | Significant improvement |
| Ovulation Rates | Significant improvement | No direct effect | Substantial improvement |
| Pregnancy Rates | Moderate improvement | No evidence | Greatest improvement |
| Oxidative Stress Biomarkers | Significant reduction | Moderate reduction | Maximal reduction |
| Intervention Sustainability | Variable adherence | High adherence with provision | Enhanced long-term maintenance |
Dietary interventions demonstrate broader systemic benefits beyond exposure reduction, including improvements in metabolic parameters that indirectly support reproductive function. In women with PCOS, dietary modifications significantly improved fertility outcomes, including increased clinical pregnancy rates (RR: 1.68, 95% CI: 1.16-2.44) and ovulation rates (RR: 1.56, 95% CI: 1.18-2.06), while reducing miscarriage rates (RR: 0.44, 95% CI: 0.24-0.79) [90]. These benefits were particularly pronounced with low-carbohydrate dietary approaches and interventions of longer duration (>6 months).
Product replacement interventions show more targeted effects, with substantial reductions in specific EDC metabolites but less documented impact on ultimate reproductive endpoints. The focused nature of these interventions makes them particularly valuable for addressing known high-exposure sources but may miss opportunities for comprehensive health improvement [15].
Biomarker Reduction Efficacy
The following workflow illustrates the comparative effectiveness of interventions across the exposure-disease continuum:
Figure 2: Intervention Impact Across Exposure-Disease Continuum
Integrated Intervention Framework
Synergistic Application of Combined Strategies
The most effective approach to EDC reduction and reproductive health protection involves integrating dietary and product replacement strategies within a comprehensive framework. Combined interventions leverage synergistic mechanisms:
- Product replacement directly reduces incoming EDC load
- Dietary modifications enhance biotransformation and excretion of unavoidable exposures
- Specific nutrients provide direct protection against residual EDC effects
- Healthy dietary patterns improve overall physiological resilience
This integrated approach addresses the multi-factorial nature of EDC exposure while supporting overall reproductive health through multiple pathways. Research indicates that nutritional status can modify susceptibility to EDCs, with adequate folate, iodine, and antioxidant status potentially buffering against adverse effects [88] [46].
Personalization Factors for Optimal Intervention
Intervention effectiveness varies based on individual characteristics and circumstances. Key personalization factors include:
Genetic Factors: Polymorphisms in detoxification enzymes (e.g., GST, NAT) may influence response to interventions Baseline Exposure Profile: Individuals with higher initial exposures may show greater absolute reduction Reproductive Status: Preconception, pregnancy, and specific infertility diagnoses warrant tailored approaches Socioeconomic Considerations: Practical constraints may influence intervention feasibility and sustainability Motivational Factors: Readiness for change and self-efficacy impact adherence and outcomes
Future research should prioritize understanding these effect modifiers to enable precision environmental health interventions.
Research Gaps and Future Directions
Despite growing evidence regarding EDC interventions, significant knowledge gaps remain. Few studies have directly compared dietary and product replacement approaches in the same population, and most existing research has focused on women, with limited attention to male reproductive health [15]. Additionally, studies examining effects on ultimate reproductive outcomes (live birth rates, child health) remain scarce.
Priority areas for future research include:
- Head-to-head trials comparing intervention strategies
- Mechanistic studies elucidating nutrient-EDC interactions
- Development of validated exposure reduction biomarkers
- Investigation of critical exposure windows and susceptibility periods
- Economic evaluations of intervention cost-effectiveness
- Translation of research findings into clinical guidelines
The research reagent table below outlines essential materials for conducting intervention studies in this field:
Table 4: Research Reagent Solutions for EDC Intervention Studies
| Reagent/Material | Specifications | Research Application |
|---|---|---|
| Urine Collection Kits | BPA-free containers, preservatives | Biomarker assessment in clinical trials |
| LC-MS/MS Standards | Isotope-labeled phthalates, phenols, parabens | Quantification of EDC metabolites |
| Antioxidant Assay Kits | Commercial kits for 8-OHdG, isoprostanes | Oxidative stress biomarker measurement |
| Hormone Assay Kits | ELISA for testosterone, SHBG, AMH | Reproductive endocrine assessment |
| Organic Food Provisions | Certified organic, diverse food categories | Dietary intervention implementation |
| EDC-Free Product Kits | Phthalate-free, paraben-free alternatives | Product replacement interventions |
| DNA Integrity Assays | Sperm chromatin structure, comet assay | Gamete quality assessment |
Both dietary and product replacement interventions demonstrate efficacy in reducing EDC exposure and mitigating reproductive health impacts. Dietary interventions offer broader systemic benefits and address multiple EDC sources simultaneously, while product replacement strategies provide more targeted exposure reduction from specific sources. The integrated application of both approaches within personalized frameworks represents the most promising strategy for protecting reproductive health across susceptible populations.
Future research should prioritize direct comparison of intervention strategies, examination of effects on clinical reproductive outcomes, and development of implementation protocols for clinical and public health practice. As evidence continues to accumulate, these interventions hold significant potential for reducing the burden of EDC-related reproductive dysfunction and improving outcomes for couples across the reproductive lifespan.
Endocrine-disrupting chemicals (EDCs) present a significant threat to reproductive health worldwide. However, exposure sources, risk perceptions, and intervention effectiveness are not uniform across populations. A one-size-fits-all approach to public health intervention fails to account for critical demographic, socioeconomic, and life-stage factors that significantly influence both exposure patterns and behavioral responses. This technical guide synthesizes current evidence on population-specific considerations for EDC avoidance, focusing on gender, life stage, and occupational variables within the broader context of reproductive health behavior research. The content provides researchers, scientists, and drug development professionals with structured data, validated methodologies, and conceptual frameworks to advance targeted intervention strategies in EDC avoidance theory.
Gender-Specific Exposure Patterns and Interventions
Disproportionate Exposure Burdens in Women
Women face significantly higher exposure to EDCs from personal care and household products (PCHPs) compared to men. Epidemiological studies indicate women are exposed to an estimated 168 different chemicals daily through their product use patterns, creating a substantially higher cumulative burden [3]. This disparity is particularly pronounced among Black women, who report using a greater number of hair care and intimate care products compared to other demographic groups, with these products often containing numerous EDCs [93].
The health consequences of these exposure patterns are profound. Black women experience higher rates of hormone-mediated conditions including uterine fibroids, infertility, and aggressive forms of breast, ovarian, and endometrial cancers—conditions potentially linked to consumer product exposures [93]. This disparity underscores the critical need for gender-informed intervention strategies.
Gender-Based Behavioral Interventions
Recent research has demonstrated the efficacy of tailored interventions for specific female populations. A study leveraging strategic social media influencer (SMI) communication to reach Black women with EDC information showed significant improvements in knowledge and behavioral intentions [93]. After exposure to culturally tailored content:
- 80% of follow-up survey respondents reported they would always consider a company's chemical policy when shopping (compared to 26.8% at baseline)
- 80% would always consider product ingredients (compared to 46.9% at baseline)
- Significant increases were observed in intentions to avoid specific EDCs including parabens (32.7% vs 15.3%), BPA (24.8% vs 14.9%), and PFAS (16.8% vs 3.5%) [93]
Table 1: Gender-Specific Intervention Outcomes
| Intervention Approach | Target Population | Key Outcomes | Effect Size |
|---|---|---|---|
| Strategic SMI Communication | Black Women | Increased chemical policy consideration | 53.2% increase |
| SMI Content Engagement | Black Women | Increased ingredient awareness | 33.1% increase |
| Report-back Intervention [9] | Reproductive-aged Women | Increased readiness to change | 72% planning behavior change |
| HBM-based Questionnaire [3] | Canadian Women (18-35) | Product avoidance linked to knowledge | Higher knowledge predicted avoidance |
For reproductive-aged women, the Health Belief Model (HBM) has proven effective in framing interventions. Research in Toronto demonstrated that greater knowledge of specific EDCs (lead, parabens, BPA, and phthalates) significantly predicted chemical avoidance in PCHPs, with higher risk perceptions of parabens and phthalates also predicting greater avoidance [3]. Women with higher education and chemical sensitivities were more likely to avoid lead, highlighting how demographic factors intersect with gender in determining protective behaviors.
Life Stage Considerations in EDC Exposure and Avoidance
Critical Windows of Vulnerability
The impact of EDC exposure varies significantly across the lifespan, with particular vulnerability during developmentally sensitive periods. A comprehensive literature review synthesizing epidemiological studies, animal experiments, and mechanistic investigations documents how EDCs interfere with multiple stages of female reproduction, from fetal development to premature menopause [68].
Exposure begins in utero, where EDCs such as PFAS and phthalates cross the placental barrier, interfering with fetal development. This exposure continues postpartum through breast milk, with EDCs detected in both biological matrices [68]. The consequences of early life exposure manifest across the lifespan:
- Earlier puberty: Girls are entering breast development and attaining menarche earlier, linked to increased risk of PCOS, obesity, type 2 diabetes, and hormone-dependent cancers [68]
- Reproductive impacts: Rising prevalence of polycystic ovary syndrome (PCOS) affecting up to 20% in some regions [68]
- Shortened reproductive lifespan: Women with the highest combined exposure to pesticides and phthalates experience menopause 1.9–3.8 years sooner [68]
Table 2: Life Stage-Specific Vulnerabilities and Manifestations
| Life Stage | Key Exposure Sources | Primary Health Impacts | Research Evidence |
|---|---|---|---|
| In utero | Placental transfer, maternal product use | Fetal developmental disruption, programming effects | EDCs detected in cord blood, follicular fluid [68] |
| Childhood/Adolescence | Food, household dust, personal care products | Altered pubertal timing, neurodevelopmental effects | Earlier breast development linked to EDC exposure [68] |
| Reproductive years | Personal care products, occupational exposures, food packaging | Infertility, PCOS, endometriosis, fibroids | BPA levels in canned beverages exceed EFSA guidelines by up to 2000-fold [94] |
| Perimenopause/Menopause | Cumulative body burden, ongoing product use | Earlier menopause, hormone-sensitive cancers | High combined EDC exposure associated with 3.8-year earlier menopause [68] |
Life Stage-Tailored Research Methodologies
Research on life stage-specific vulnerabilities requires tailored methodological approaches. The "Reducing Exposures to Endocrine Disruptors (REED)" study protocol targets men and women of reproductive age (18-44 years), recognizing this as a critical window for intervention to protect future reproductive outcomes [9]. This randomized controlled trial employs:
- Pre- and post-intervention biomonitoring of EDC metabolites in urine
- EDC-specific environmental health literacy (EHL) curriculum
- Readiness to change (RtC) assessments
- Clinical biomarker tracking (via Siphox at-home test) to correlate exposure reduction with health outcomes [9]
For the preconception and conception periods, research conducted in Toronto focused specifically on women aged 18-35, aligning with Canadian fertility patterns where women typically have their first child between 25-35 [3]. This precise targeting ensures research findings are relevant to the most vulnerable life stages.
Occupational and Regional Exposure Considerations
Occupational Exposure Disparities
Occupational settings represent significant sources of EDC exposure, particularly for agricultural workers. The review published in Nature Reviews Endocrinology highlights that pesticide exposure is often occupational, "especially for women farmworkers" [68]. These occupational exposures contribute to cumulative toxic burden that disrupts reproductive health across the lifespan.
Beyond agricultural settings, occupational exposures occur through:
- Dry cleaning professionals: Exposure to perchloroethylene (PERC), classified as a probable human carcinogen (IARC Group 2A) and reproductive toxicant [3]
- Hair and beauty professionals: Regular exposure to phthalates, parabens, and other EDCs in scented and cosmetic products [3]
- Industrial manufacturing workers: Exposure to BPA, phthalates, and other plasticizers in production processes
Regional and Cultural Variations in Exposure
Exposure profiles vary significantly across geographic and cultural contexts, necessitating regionally tailored research approaches. A Korean study developed and validated a survey instrument specifically for the Korean population, accounting for unique exposure sources, cultural practices, and product use patterns [11]. The resulting questionnaire identified four primary exposure pathways:
- Health behaviors through food
- Health behaviors through breathing
- Health behaviors through skin
- Health promotion behaviors [11]
This culturally adapted instrument demonstrated reliability (Cronbach's alpha = .80) through rigorous validation with 288 Korean adults [11] [75]. The study highlights the importance of developing population-specific assessment tools rather than simply translating Western instruments.
Research Methodologies and Experimental Protocols
Validated Survey Instruments for Population Research
Research into population-specific EDC avoidance behaviors requires rigorously validated assessment tools. The Korean research team developed their survey through a systematic process:
- Initial item generation: 52 items derived from literature review (2000-2021)
- Content validity verification: Expert panel assessment (CVI > .80)
- Pilot testing: 10 adults to assess clarity and response time
- Psychometric validation: Item analysis, exploratory factor analysis (EFA), and confirmatory factor analysis (CFA) with 288 participants [11] [75]
The final 19-item instrument uses a 5-point Likert scale and assesses behaviors across four domains corresponding to primary exposure routes [11]. This methodological approach provides a template for developing culturally adapted EDC assessment tools for other specific populations.
The Toronto study utilized a researcher-designed questionnaire based on the Health Belief Model, comprising dedicated sections for each of six EDCs (lead, parabens, phthalates, BPA, triclosan, and PERC) [3]. For each chemical, four scales measured:
- Knowledge (6 items, 6-point Likert)
- Health risk perceptions (7 items, 6-point Likert)
- Beliefs (5 items, 6-point Likert)
- Avoidance behaviors (6 items, 5-point Likert) [3]
This granular approach allowed researchers to identify chemical-specific knowledge gaps and behavioral determinants.
Intervention Study Protocols
The REED study protocol provides a comprehensive framework for testing EDC exposure reduction interventions [9]. Key methodological elements include:
- Study design: Randomized controlled trial
- Participants: 600 reproductive-aged men and women (18-44 years)
- Intervention components:
- Self-directed online interactive curriculum
- Live counseling sessions
- Individualized support modeled after the Diabetes Prevention Program
- Outcome measures:
- EDC-specific environmental health literacy (EHL)
- Readiness to change (RtC) surveys
- Biomonitoring of EDC metabolites before and after intervention
- Clinical biomarkers via at-home testing (Siphox) [9]
This protocol represents a significant advancement in intervention research through its incorporation of both behavioral and clinical outcome measures, addressing a critical gap in EDC intervention literature.
Conceptual Frameworks and Signaling Pathways
Strategic Social Media Influencer Communication Framework
The POWER project successfully applied a conceptual model for strategic communication through social media influencers, adapting Borchers and Enke's framework with community health worker principles [93]. The implementation workflow is structured as follows:
SMI Communication Workflow
Population-Specific EDC Research Methodology
Research into population-specific EDC avoidance behaviors requires a systematic approach that accounts for demographic and environmental variables. The following workflow visualizes the integrated methodological approach:
EDC Research Methodology
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Methods for Population-Specific EDC Studies
| Research Tool | Function/Application | Example Implementation |
|---|---|---|
| Validated Survey Instruments | Assess knowledge, risk perceptions, and avoidance behaviors | 19-item reproductive health behavior questionnaire (Cronbach's α=.80) [11] |
| Biomonitoring Kits | Quantify internal EDC exposure concentrations | Mail-in urine testing for phthalates, parabens, BPA, and other EDCs [9] |
| Product Chemical Analysis | Identify exposure sources in commonly used products | LC-MS/MS analysis of beverages for PFAS, bisphenols, parabens [94] |
| Environmental Health Literacy Curricula | Standardized educational interventions | Online interactive curriculum with live counseling sessions [9] |
| Readiness to Change Assessments | Measure behavioral intention stages | Pre- and post-intervention surveys assessing motivation for EDC avoidance [9] |
| Cultural Adaptation Frameworks | Tailor instruments and interventions to specific populations | Expert panels for content validity, pilot testing for cultural appropriateness [11] |
Population-specific approaches to EDC avoidance are essential for effective public health intervention. Significant disparities in exposure patterns, risk perceptions, and intervention effectiveness exist across gender, life stage, occupational, and cultural dimensions. Women—particularly Black women and those of reproductive age—face disproportionate exposure burdens from personal care products, necessitating targeted educational and behavioral interventions. Life stage considerations are equally critical, with vulnerability extending from in utero development through reproductive years and menopause. Occupational exposures compound these risks for agricultural and industrial workers. Future research must continue to develop and validate culturally adapted assessment tools and account for the complex interplay of demographic variables in EDC exposure and avoidance behaviors. The methodological frameworks, validated instruments, and intervention protocols outlined in this guide provide researchers with essential tools to advance this field and develop increasingly targeted, effective strategies for reducing EDC exposure across diverse populations.
Conclusion
The growing body of evidence unequivocally demonstrates that behavioral interventions targeting EDC avoidance represent a crucial component of comprehensive reproductive health protection. Validated assessment tools and targeted behavioral strategies show significant promise in reducing internal EDC concentrations and mitigating associated health risks. Future research must prioritize the development of more sensitive biomarkers, longer-term intervention studies, personalized approaches based on genetic susceptibility, and systematic integration of environmental health education into clinical practice and medical curricula. For biomedical and pharmaceutical research, understanding EDC exposure reduction creates opportunities for novel therapeutic approaches that account for environmental determinants of reproductive health, while regulatory science must advance to better evaluate cumulative exposure risks and protect vulnerable populations throughout their reproductive lifespans.
References
- 1. The impact, mechanisms and prevention strategies of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12520972/]
- 2. Global research on endocrine disruptors as emerging hazards ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12240779/]
- 3. Analysis of Women's Knowledge, Health Risk Perceptions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12116110/]
- 4. The potential endocrine-disrupting of fluorinated pesticides ... [https://www.sciencedirect.com/science/article/pii/S0147651324016919]
- 5. Early-life exposure to endocrine-disrupting chemicals may ... [https://www.endocrine.org/news-and-advocacy/news-room/endo-annual-meeting/endo-2025-press-releases/hilz-press-release]
- 6. New research method helps identify hormone-disrupting ... [https://news.ki.se/new-research-method-helps-identify-hormone-disrupting-chemicals]
- 7. Identifying a Window of Vulnerability during Fetal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3057971/]
- 8. Maternal air temperature exposure and risk of small ... [https://www.sciencedirect.com/science/article/pii/S0147651325010723]
- 9. Reducing Exposures to Endocrine Disruptors (REED) study, a ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-024-08627-3]
- 10. Analysis of Women's Knowledge, Health Risk Perceptions ... [https://pubmed.ncbi.nlm.nih.gov/40423493/]
- 11. Development and validation of a survey on reproductive ... [https://www.frontiersin.org/journals/reproductive-health/articles/10.3389/frph.2025.1519896/full]
- 12. Polycystic ovary syndrome [https://www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome]
- 13. POLYCYSTIC OVARY SYNDROME: ORIGINS AND ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12060724/]
- 14. Lifecycle of Polycystic Ovary Syndrome (PCOS) [https://pmc.ncbi.nlm.nih.gov/articles/PMC3849665/]
- 15. Lifestyle interventions to reduce endocrine-disrupting ... [https://www.sciencedirect.com/science/article/pii/S0160412022005037]
- 16. Two new studies show dual impact of family planning [https://www.guttmacher.org/news-release/2025/guttmacher-releases-most-comprehensive-evidence-date-global-family-planning-gaps]
- 17. The impact, mechanisms and prevention strategies of ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1573526/full]
- 18. The impact, mechanisms and prevention strategies of ... [https://pubmed.ncbi.nlm.nih.gov/41103656/]
- 19. Endocrine-disrupting chemicals and female reproductive ... [https://www.nature.com/articles/s41574-025-01131-x]
- 20. Endocrine disruptors and reproductive health - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/16781053/]
- 21. The impact of Bisphenol-A on human reproductive health [https://www.sciencedirect.com/science/article/pii/S2214750024001562]
- 22. Interference of Paraben Compounds with Estrogen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5618656/]
- 23. Phthalates and Their Impacts on Human Health - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8157593/]
- 24. Reproductive toxicity of PFOA, PFOS and their substitutes [https://www.sciencedirect.com/science/article/abs/pii/S001393512400389X]
- 25. Structural Aspects of Potential Endocrine-Disrupting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7918290/]
- 26. Consensus on the key characteristics of endocrine ... [https://www.nature.com/articles/s41574-019-0273-8]
- 27. Endocrine-Disrupting Chemicals & Reproductive Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC6701840/]
- 28. The Development and Reliability Testing of a Tool to ... [https://www.mdpi.com/2076-3298/12/5/138]
- 29. Awareness of endocrine-disrupting chemicals among medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12636539/]
- 30. Associations Between Daily-Use Products and Urinary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11764522/]
- 31. Role of personal care products as endocrine disruptors ... [https://www.frontiersin.org/journals/reproductive-health/articles/10.3389/frph.2025.1514060/full]
- 32. Endocrine-disrupting chemicals and reproductive health [https://www.sciencedirect.com/science/article/pii/S0003426625001064]
- 33. Associations Between Daily-Use Products and Urinary ... [https://pubmed.ncbi.nlm.nih.gov/39857552/]
- 34. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 35. Establishing Good Practices for Exposure–Response Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4625861/]
- 36. Integrating human biomonitoring exposure data into a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11700452/]
- 37. Human Food Program (HFP) FY 2025 Priority Deliverables [https://www.fda.gov/about-fda/human-foods-program/human-food-program-hfp-fy-2025-priority-deliverables]
- 38. MAHA Commission Strategy Report Outlines Sweeping ... [https://www.bdlaw.com/publications/maha-commission-strategy-report-outlines-sweeping-federal-actions-on-chemicals-in-food-and-the-environment/]
- 39. Development and validation of a survey on reproductive ... [https://pubmed.ncbi.nlm.nih.gov/40162030/]
- 40. The adverse role of endocrine disrupting chemicals in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10832042/]
- 41. 10 Healthy Swaps to make in 2025 [https://www.urbanapronblog.com/home/2025/1/3/10-health-swaps-to-make-in-2025]
- 42. Awareness and Knowledge of Endocrine-Disrupting ... [https://www.mdpi.com/2305-6304/12/12/890]
- 43. Avoiding endocrine disruptors in toiletries, cosmetics and ... [https://chemtrust.org/cosmetics/]
- 44. 2025 Key Drivers Behind the Growth of the Household ... [https://finicecleaning.com/key-drivers-behind-the-growth-of-the-household-cleaning-products-market/]
- 45. Five Consumer Behavior Trends In HI&I Cleaning ... [https://klinegroup.com/chemicals/five-consumer-behavior-trends-in-hii-cleaning-ingredients-for-2025/]
- 46. Endocrine disruptors: Unravelling the link between ... [https://www.sciencedirect.com/science/article/abs/pii/S0013935123021898]
- 47. The adverse role of endocrine disrupting chemicals in ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1324993/full]
- 48. Impact of a “Digital Health” Curriculum on Students ... [https://formative.jmir.org/2025/1/e58940]
- 49. Understanding Uptake of Digital Health Products [https://www.jmir.org/2021/10/e32365/]
- 50. Counseling Theories and Approaches [https://www.keiseruniversity.edu/counseling-theories-and-approaches-understanding-different-modalities/]
- 51. The Process of Integrating Family Planning Services with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12227082/]
- 52. Reducing Exposures to Endocrine Disruptors (REED) study, a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11587698/]
- 53. What do people need to know about endocrine disrupting ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-025-25561-4]
- 54. Five Counseling Theories and Approaches [https://counseling.northwestern.edu/blog/five-counseling-theories-and-approaches/]
- 55. Evaluating health system barriers to sexual and reproductive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12455775/]
- 56. Public Awareness and Risk Perceptions of Endocrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7660691/]
- 57. Health-focused REACH reform [https://www.env-health.org/health-focused-reform-of-reach-2025/]
- 58. Associations Between Endocrine-Disrupting Chemical ... [https://pubmed.ncbi.nlm.nih.gov/40724496/]
- 59. Prenatal Dietary Exposure to Endocrine Disruptors and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568251/]
- 60. Prenatal exposure to endocrine-disrupting chemicals and ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1681214/full]
- 61. The influence of knowledge about endocrine-disrupting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12499794/]
- 62. Long-Term Adherence to Health Behavior Change - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4988401/]
- 63. Behavior Change Techniques and Their Mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6636886/]
- 64. A Systematic Review With Network Meta-Analysis [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2018.01454/full]
- 65. Temporal effectiveness of interventions to improve medication adherence: A network meta-analysis | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0213432]
- 66. Effectiveness of digital health interventions on adherence ... [https://pubmed.ncbi.nlm.nih.gov/38973553/]
- 67. Associations Between Endocrine-Disrupting Chemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299029/]
- 68. Endocrine Disrupting Chemicals' Effects on Reproductive ... [https://beyondpesticides.org/dailynewsblog/2025/07/endocrine-disruptors-effects-on-reproductive-health/]
- 69. Socioeconomic status in the association between use of ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1537669/full]
- 70. Disparities in Environmental Exposures to Endocrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5741159/]
- 71. Low socioeconomic status raises pregnant women's risk of ... [https://www.endocrine.org/news-and-advocacy/news-room/2024/endo-2024-press-han]
- 72. Social determinants of health in pregnant individuals from ... [https://equityhealthj.biomedcentral.com/articles/10.1186/s12939-023-01963-x]
- 73. EDC 101: What is Electronic Data Capture in Clinical Trials? [https://www.medidata.com/en/life-science-resources/medidata-blog/edc-clinical-trials-electronic-data-capture/]
- 74. Lifestyle interventions to reduce endocrine-disrupting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9890927/]
- 75. Development and validation of a survey on reproductive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11949970/]
- 76. Behavioral Assessment Methods for RDoC Constructs [https://www.nimh.nih.gov/about/advisory-boards-and-groups/namhc/reports/behavioral-assessment-methods-for-rdoc-constructs]
- 77. How to Conduct a Randomized Controlled Trial - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10753608/]
- 78. A test of intervention effect in HIV behavioral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5627604/]
- 79. Behavior changes to promote preconception health: a systematic review | BMC Women's Health | Full Text [https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-024-03544-8]
- 80. A family planning clinic-based intervention to address reproductive coercion: a cluster randomized controlled trial - PubMed [https://pubmed.ncbi.nlm.nih.gov/26892333/]
- 81. A family planning clinic-based intervention to address reproductive coercion: A cluster randomized controlled trial - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4884549/]
- 82. A Decision Tree for Controlled Trials [https://sportsci.org/jour/05/wghamb.htm]
- 83. Efficacy of a Multimodal Digital Behavior Change ... [https://www.researchprotocols.org/2024/1/e50378/]
- 84. CONSORT 2025 Statement - Reporting guideline [https://www.equator-network.org/reporting-guidelines/consort/]
- 85. Associations of endocrine disrupting chemical biomarkers ... [https://www.sciencedirect.com/science/article/pii/S0013935125025691]
- 86. Plasma biomarkers in patients with familial cavernous ... [https://www.nature.com/articles/s41598-025-91141-6]
- 87. Identification of biomarkers and outcomes of endocrine ... [https://www.sciencedirect.com/science/article/pii/S0300483X23000100]
- 88. Nutritional interventions to ameliorate the effect of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9305939/]
- 89. Dietary and Lifestyle Interventions to Mitigate Oxidative Stress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12195172/]
- 90. Dietary Modification for Reproductive Health in Women With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8591222/]
- 91. Diet and female fertility: a population-based study re ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12586016/]
- 92. Diet and Fertility: A Review - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5826784/]
- 93. The Power of Strategic Social Media Influencer ... [https://www.jmir.org/2025/1/e66128]
- 94. Exposure to endocrine disrupting chemicals from beverage ... [https://www.sciencedirect.com/science/article/pii/S0304389423025980]