A Comprehensive Protocol for Developing and Validating Reproductive Health Behavior Questionnaires
This article provides a detailed, step-by-step protocol for developing and validating robust reproductive health behavior questionnaires.
A Comprehensive Protocol for Developing and Validating Reproductive Health Behavior Questionnaires
Abstract
This article provides a detailed, step-by-step protocol for developing and validating robust reproductive health behavior questionnaires. Aimed at researchers and clinical professionals, it synthesizes current methodologies from foundational qualitative research and item generation to advanced psychometric validation and intervention optimization. The protocol covers essential stages including defining conceptual frameworks, conducting cognitive interviews, applying rigorous scale development techniques like exploratory and confirmatory factor analysis, and utilizing modern optimization frameworks such as the Multiphase Optimization Strategy (MOST). It also addresses troubleshooting common pitfalls and emphasizes the critical role of cross-cultural validation to ensure tools are reliable, valid, and applicable for diverse populations in both research and clinical settings.
Laying the Groundwork: Conceptual Frameworks and Initial Item Generation
Defining the Construct and Target Population
The initial phase of developing a reproductive health behavior questionnaire is foundational, setting the trajectory for all subsequent research and instrument validation. This stage involves the precise definition of the construct to be measured and the explicit specification of the target population from which data will be collected. A meticulously executed definition process ensures the questionnaire's content validity, guaranteeing that the instrument comprehensively captures the full spectrum of the reproductive health behaviors it intends to measure [1]. Within the broader thesis on questionnaire development protocol, this phase dictates the appropriateness of all future psychometric evaluations and the ultimate utility of the tool in research or clinical settings.
Framing the construct within a recognized theoretical model of health behavior is paramount. Furthermore, the definition must be culturally contextualized, reflecting the specific beliefs, norms, and healthcare access realities of the intended population, as a construct valid in one cultural setting may not hold in another [2]. This document outlines detailed application notes and experimental protocols for systematically defining the construct and target population for a reproductive health behavior questionnaire.
Conceptual Foundations and Literature Review
The Importance of a Clear Construct
In psychometrics, a "construct" refers to the abstract concept, theme, or behavior that the questionnaire aims to measure. A well-defined construct provides a clear framework for item generation and ensures that all questions are relevant to the research objective. For reproductive health, this is particularly critical due to the multifaceted nature of the field, which encompasses physical, mental, and social well-being [2] [3].
A shift from a deficit-based perspective to a well-being-focused framework is emerging in the field. Traditional metrics often focus on adverse outcomes like unintended pregnancy or disease rates. In contrast, a construct centered on Sexual and Reproductive Well-Being (SRWB) aims to capture whether people are living the sexual and reproductive lives they wish to, aligning with reproductive justice and human rights frameworks [3]. This positive, person-centered approach should be considered when defining the construct for a new questionnaire.
Core Components of a Reproductive Health Behavior Construct
The table below summarizes potential domains and their behavioral indicators relevant to defining a reproductive health behavior construct, synthesized from existing literature.
Table 1: Potential Domains and Behavioral Indicators for a Reproductive Health Construct
| Domain | Description | Example Behavioral Indicators |
|---|---|---|
| Preventive Health-Seeking | Behaviors related to seeking information and services to maintain reproductive health. | Frequency of health check-ups; online health information-seeking [4]; contraceptive counseling uptake. |
| Risk Reduction & Management | Actions taken to minimize the risk of adverse reproductive health outcomes. | Consistent contraceptive use; STI testing behaviors; smoking or alcohol cessation during pregnancy [2]. |
| Fertility and Parenthood Behaviors | Behaviors related to achieving or avoiding pregnancy, and parenting. | Pregnancy planning activities; fertility treatment-seeking; prenatal care adherence [5]. |
| Partner and Sexual Communication | Interpersonal behaviors concerning sexual and reproductive health. | Communication with partners about sexual history, contraception, or reproductive desires [2]. |
| Health Literacy and Self-Care | Daily practices and knowledge application for self-management of reproductive health. | Adherence to medical regimens; engagement in healthy diet/exercise [2]; correct use of health products. |
Operational Definitions and Methodological Protocols
Protocol 1: Construct Elucidation via Qualitative Exploration
1. Objective: To explore and define the nuanced dimensions of the reproductive health behavior construct from the perspective of the target population.
2. Materials and Reagents:
- Audio recording equipment
- Semi-structured interview guide
- Transcribed interview transcripts
- Qualitative data analysis software (e.g., NVivo, MAXQDA)
3. Experimental Workflow: This protocol employs a qualitative study design, typically using contractual or conventional content analysis, to generate items from the ground up [2] [5].
4. Data Analysis: Data are analyzed inductively to identify meaning units, which are condensed into codes, grouped into subcategories, and finally organized into main themes or dimensions representing the construct [5]. The trustworthiness of data is ensured through credibility, dependability, confirmability, and transferability [5].
Protocol 2: Systematic Literature Review for Construct Dimension Identification
1. Objective: To systematically identify established and theoretically-grounded dimensions of reproductive health behavior to inform and complement the qualitative findings.
2. Materials and Reagents:
- Access to scientific databases (e.g., PubMed, Scopus, Web of Science)
- Reference management software (e.g., EndNote, Zotero)
- Data extraction forms
3. Experimental Workflow: This protocol involves a systematic search of national and international literature to map the existing knowledge and tools related to the construct [6].
4. Data Analysis: Findings from the literature review are integrated with the results from the qualitative phase (Protocol 1). The goal is to create a comprehensive and comparative list of items and dimensions, ensuring the preliminary instrument is both culturally relevant (from qualitative data) and scientifically grounded (from literature) [2] [6].
Protocol 3: Operational Definition of the Target Population
1. Objective: To establish clear and justified inclusion and exclusion criteria for the target population.
2. Key Defining Parameters: The target population must be defined with precision to ensure the instrument's validity and future generalizability. The following parameters must be specified:
- Demographics: Age range, gender, socioeconomic status, education level, and ethnicity [2] [4].
- Clinical/Reproductive Status: Specific reproductive health experiences (e.g., women with premature ovarian insufficiency [6], women shift workers [5], men in reproductive age).
- Contextual Factors: Geographical location (urban vs. rural) [4], occupation, and cultural or religious background [2].
3. Justification: The rationale for each parameter must be documented. For example, studying women shift workers specifically is justified because shift work has documented effects on menstruation, sexual relationships, and pregnancy outcomes, requiring a tailored instrument [5].
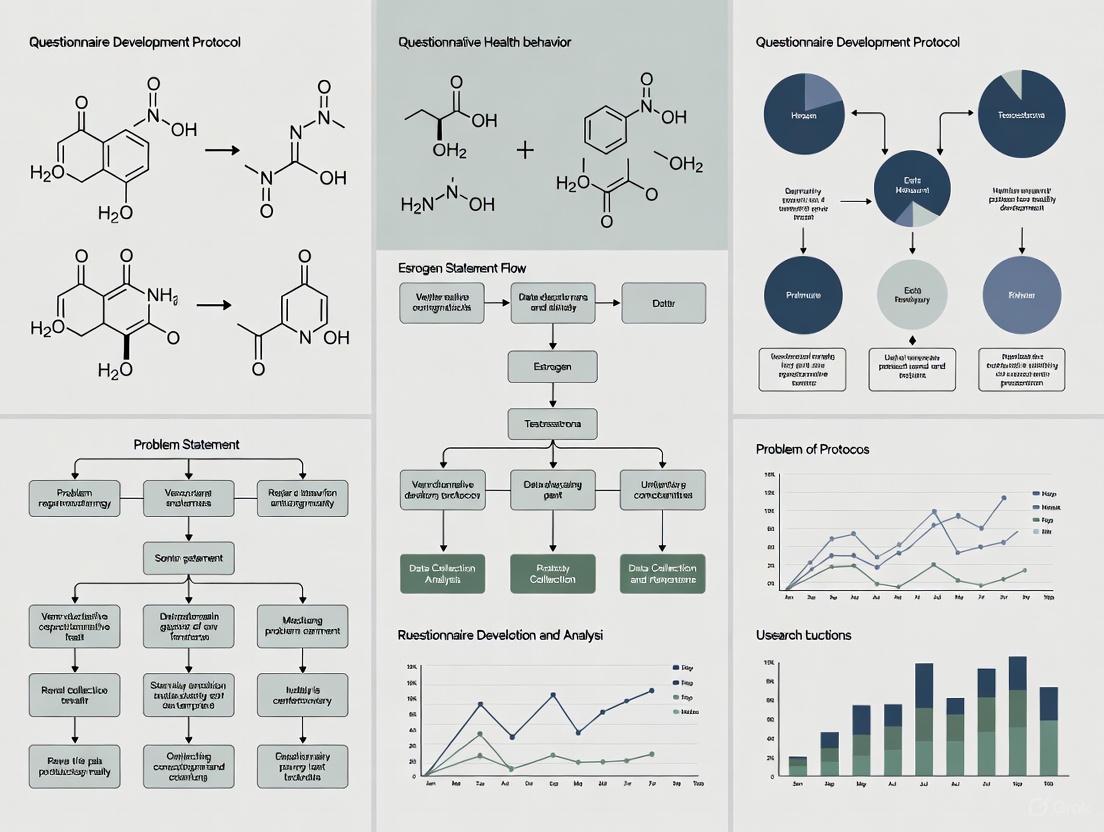
Diagram 1: Workflow for defining the construct and target population, integrating qualitative and literature-based methods.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Defining Construct and Population
| Research Reagent / Material | Function/Application in Protocol |
|---|---|
| Semi-Structured Interview Guide | A flexible protocol to ensure key topics are covered while allowing participants to express their views freely, generating rich qualitative data [2] [5]. |
| Qualitative Data Analysis Software (e.g., NVivo) | Facilitates the organization, coding, and thematic analysis of large volumes of textual interview data [5]. |
| Literature Search Strategy & Boolean Operators | A pre-defined, reproducible plan for searching scientific databases to ensure a comprehensive and unbiased literature review [6]. |
| Expert Panel | A group of specialists (e.g., in reproductive health, gynecology, psychology) who provide input on the relevance and comprehensiveness of the constructed dimensions, establishing content validity [5]. |
| Data Saturation Log | Documentation to track when no new information or themes are observed in qualitative data collection, signaling an adequate sample size [2]. |
Data Synthesis and Preliminary Validation
Integrating Findings into a Working Definition
The final output of this phase is a detailed, operational definition of the construct and the target population. The construct definition should clearly list the identified dimensions (e.g., motherhood, sexual relationships, general health) and their components [5]. The population definition should include finalized inclusion and exclusion criteria.
Logical Workflow for Population Stratification: The following diagram outlines the decision process for defining and stratifying the target population, which is crucial for ensuring the instrument's relevance and for planning subsequent psychometric testing.
Diagram 2: Logic flow for applying criteria to define and stratify the target population.
Output for the Next Phase
The conclusive deliverables from this stage form the direct input for the next phase of questionnaire development: Item Generation.
- A formal written Construct Definition.
- A finalized Target Population Profile with explicit criteria.
- A comprehensive list of Dimensions and Sub-Dimensions of the reproductive health behavior construct, ready to be translated into a pool of specific questionnaire items.
Conducting Formative Qualitative Research
Application Notes: The Role of Formative Qualitative Research in Questionnaire Development
Formative qualitative research is an indispensable preliminary phase in developing robust, contextually-grounded research instruments, particularly for complex fields like reproductive health. This exploratory process leverages in-depth qualitative methods to gain a nuanced understanding of the population's knowledge, attitudes, experiences, and vocabulary surrounding a health issue. These insights directly inform the content, structure, and language of subsequent quantitative survey instruments, ensuring they are comprehensive, culturally appropriate, and cognitively accessible to the target population.
Within a broader thesis on reproductive health behavior questionnaire development, formative research ensures that the final instrument accurately captures the salient beliefs, behaviors, and barriers specific to the population of interest. This methodology is especially critical when researching sensitive topics or working with diverse cultural groups, where researcher assumptions may not align with local realities. The application of these methods ensures the final questionnaire has high content validity and face validity, forming a solid foundation for psychometric testing and eventual deployment in larger-scale studies.
Experimental Protocols for Formative Qualitative Research
This section provides a detailed methodological framework for conducting formative qualitative research to inform a reproductive health behavior questionnaire.
Protocol Phase 1: Foundational Scoping
Objective: To define the core domains of inquiry and develop a preliminary understanding of the research landscape.
Detailed Methodology:
- Systematic Literature Review: Conduct a structured review of peer-reviewed literature and existing instruments to conceptualize key dimensions. As demonstrated in the development of an integrated oral, mental, and sexual reproductive health tool for adolescents, this involves defining dimensions a priori (e.g., sexual practices, health outcomes) and systematically searching databases like PubMed and ScienceDirect to identify relevant conceptualizations and measurement items [7].
- Domain Identification: Thematically analyze retrieved articles to extract information on relevant domains and subscales. The goal is to identify constructs that are statistically or conceptually associated with your core research interest [7].
- Expert Consultation: Engage a multi-disciplinary panel of experts (e.g., subject matter specialists, clinical professionals, language experts) to verify the identified domains and assess the content validity of initial concepts. The Content Validity Index (CVI) can be used quantitatively to retain items meeting a predefined threshold (e.g., I-CVI > 0.80) [8].
Protocol Phase 2: Primary Qualitative Data Collection
Objective: To gather rich, contextual data directly from the target population and key stakeholders.
Detailed Methodology: Adopt a qualitative research design guided by grounded theory principles, aiming to develop a theory or deep understanding characterized by the population's own perspectives and experiences [9]. Data collection should involve multiple activities to triangulate findings.
In-Depth Interviews (IDIs):
- Participant Selection: Purposively select participants to reflect a range of characteristics (e.g., gender, age, location, socioeconomic status) known to affect the delivery and experience of the health issue [9].
- Procedure: Conduct semi-structured interviews using a pre-tested interview guide. The guide should explore perceptions, experiences, unmet needs, and the acceptability of potential interventions or measurement approaches. For a study on digital diabetes solutions, interviews explored how digital solutions may improve care and assessed digital readiness [9]. All interviews should be audio-recorded, transcribed verbatim, and, if necessary, translated.
Contextual and Clinical Observations:
- Procedure: Have trained researchers shadow practitioners in their care environment for a full shift. One researcher (a trained clinician) can observe clinical competencies using a validated tool, while a second researcher observes the environment, duties, and interpersonal interactions [9]. This method provides insight into real-world practices and how the care environment influences service delivery.
- Data Recording: Use a structured observation guide to record detailed field notes. A brief semi-structured interview with the practitioner can follow the observation session to clarify observations [9].
Structured Workshops:
- Procedure: Conduct separate workshops with different stakeholder groups (e.g., practitioners, patients, family members). The aim is to collaboratively identify and prioritize advantages, challenges, and practical recommendations for the intervention or, in this context, the questionnaire's design and implementation [9].
- Facilitation: Use facilitation techniques to encourage open discussion and consensus-building on key design considerations.
Table 1: Data Collection Methods for Formative Qualitative Research
| Method | Primary Objective | Participant Profile | Key Outcomes |
|---|---|---|---|
| In-Depth Interviews (IDIs) | Explore individual experiences, perceptions, and beliefs in depth. | Patients, family members, healthcare providers. | Rich, narrative data on personal views and lived experiences. |
| Contextual Observations | Understand behaviors and practices within their natural setting. | Healthcare providers in clinical settings. | Insights into real-world workflows, environmental constraints, and unspoken practices. |
| Structured Workshops | Generate consensus and gather diverse perspectives on specific topics. | Separate groups of practitioners, patients, and family members. | Prioritized list of needs, design requirements, and potential implementation challenges. |
Protocol Phase 3: Qualitative Analysis and Item Generation
Objective: To analyze qualitative data and translate findings into a draft questionnaire.
Detailed Methodology:
- Qualitative Data Analysis: Employ a thematic analysis approach. This involves a progression from (a) identifying surface-level codes to (b) grouping similar codes to develop themes.
- Coding: Systematically code transcript excerpts and field notes to label key concepts.
- Theme Development: Examine codes for commonalities and group them into meaningful themes that answer the research questions. Qualitative analysis software (e.g., NVivo, MAXQDA) provides organizational tools for this process, though the analysis itself remains a human, interpretive task [10].
- Item Generation: Use a deductive method, or logical partitioning, to generate questionnaire items based on the defined constructs and themes identified from the literature and primary data [7].
- Source Material: Derive measurement items from validated tools and the unique themes from your qualitative data. Most items should retain their original response scales, though some can be adjusted for clarity and cultural appropriateness [7].
- Compilation: Draft a preliminary questionnaire by organizing items into logical sections (e.g., socio-demographics, knowledge, attitudes, behaviors, service utilization) [7].
Table 2: Translating Qualitative Findings into Questionnaire Items
| Qualitative Data Source | Analytic Activity | Output for Questionnaire Development |
|---|---|---|
| Interview & Workshop Transcripts | Thematic Analysis -> Initial Coding | List of emergent codes (e.g., "fear of judgment," "prioritization of convenience"). |
| Grouped Codes | Thematic Analysis -> Theme Development | Overarching themes and subthemes (e.g., "Barriers to Service Access," "Sources of Health Information"). |
| Established Themes & Constructs | Deductive Item Generation [7] | Draft survey items measuring each theme. E.g., the theme "Stigma" generates items about comfort discussing reproductive health. |
| Validated Tools & Literature | Item Compilation & Adaptation [7] | Pool of validated questions, rephrased for context, integrated with newly generated items. |
Workflow Diagram
The following diagram visualizes the end-to-end protocol for using formative qualitative research in questionnaire development.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Essential Reagents and Materials for Formative Qualitative Research
| Item / Solution | Function / Application in Protocol |
|---|---|
| Semi-Structured Interview Guides | A predefined set of open-ended questions and prompts that ensure key topics are covered across all interviews while allowing flexibility to explore participant-specific issues in depth [9]. |
| Structured Observation Guides | A tool used during contextual observations to systematically record data on practitioner competencies, environmental factors, workflows, and interactions, ensuring consistency across different observers and settings [9]. |
| Digital Audio Recorders | Essential for capturing verbatim accounts of in-depth interviews and workshop discussions for accurate transcription and analysis. |
| Qualitative Data Analysis Software (e.g., NVivo, MAXQDA) | Software that provides organizational tools to manage, code, and retrieve qualitative data efficiently. It aids in the coding process and visualization of relationships in the data but does not perform the analysis itself [10]. |
| Participant Information Sheets & Consent Forms | Ethically mandatory documents that clearly explain the study's purpose, procedures, risks, benefits, and confidentiality measures in language accessible to the participant, ensuring informed consent is obtained. |
| Workshop Facilitation Kits | Materials including agendas, prompts, large writing surfaces (whiteboards/flipcharts), and note-taking materials to structure group discussions and effectively capture collective insights [9]. |
| Validated Cognitive Testing Protocols | A set of procedures (e.g., "think-aloud" techniques, verbal probing) used in pilot testing to evaluate if the draft questionnaire items are understood as intended by the target population. This is a critical step for refining items before validation [11]. |
Developing a Conceptual Model and Initial Domains
The development of a robust reproductive health behavior questionnaire is a critical step in addressing nuanced public health challenges. Such tools enable researchers to gather standardized, quantifiable, and comparable data on the factors that influence health behaviors and outcomes. The process is methodologically rigorous, requiring a structured approach to ensure the instrument is both valid—meaning it measures what it intends to—and reliable—meaning it produces consistent results [12]. This document outlines a detailed protocol for the initial stages of questionnaire development: establishing a conceptual model and defining the initial domains, framed within a broader research context. The guidance provided is designed for researchers, scientists, and professionals engaged in health instrument development, with a specific focus on reproductive health.
Establishing the Conceptual Foundation
A strong conceptual model provides the theoretical backbone for the questionnaire, guiding item generation and ensuring that the final instrument comprehensively addresses the constructs of interest.
Theoretical Frameworks for Behavioral Questionnaires
A well-defined theoretical framework helps in hypothesizing relationships between variables and provides a structure for organizing questionnaire domains. Several established models are applicable to reproductive health behavior research.
The Theory of Planned Behavior (TPB) is a prominent framework used in reproductive health research. It posits that behavioral intention, the most immediate predictor of behavior, is influenced by three factors: Attitude (the individual's positive or negative evaluation of performing the behavior), Subjective Norms (the perceived social pressure from important others to perform or not perform the behavior), and Perceived Behavioral Control (the perceived ease or difficulty of performing the behavior, which can also directly influence the behavior itself) [13]. This model effectively predicts intention and can be extended by integrating distal variables such as demographic factors or parental control, providing a robust structure for a conceptual model [13].
A Mixed-Methods Approach to model development, which combines qualitative and quantitative data, is highly recommended for ensuring cultural and contextual relevance. This approach involves two key phases [14] [5]:
- Qualitative Exploration: In-depth understanding of the concept is achieved through interviews and focus group discussions with the target population until data saturation is reached. For instance, one study conducted 21 interviews with women shift workers to explore the concept of reproductive health in their specific context [5]. This phase ensures the model is grounded in the lived experiences of the population.
- Item Generation: The qualitative data are analyzed (e.g., using conventional content analysis) to identify key themes and components. These components are then used to generate an initial pool of questionnaire items, often supplemented by a review of existing literature and instruments [14] [5].
Defining Initial Domains and Constructs
Domains are the broad conceptual categories that the questionnaire aims to measure. Based on the theoretical framework and qualitative research, initial domains can be defined. The table below summarizes example domains identified in relevant reproductive health questionnaire studies.
Table 1: Example Domains from Reproductive Health Questionnaire Studies
| Domain / Factor Name | Description | Source Study Population |
|---|---|---|
| Attitude towards reproductive health behavior | The individual's evaluation (positive or negative) of behaviors that preserve reproductive health. | Female adolescents in Iran [13] |
| Subjective Norms | The perceived social pressure from important people (e.g., parents, peers) regarding reproductive health. | Female adolescents in Iran [13] |
| Perceived Behavioral Control | The individual's perception of their ability to perform reproductive health behaviors. | Female adolescents in Iran [13] |
| Disease-related Concerns | Worries and anxieties specific to living with a health condition that affects reproductive choices. | HIV-positive women [14] |
| Sexual Relationships | Aspects related to sexual function, satisfaction, and behaviors within partnerships. | Women shift workers [5] |
| Motherhood | Issues pertaining to pregnancy, breastfeeding, and maternal health. | Women shift workers [5] |
| Menstruation | Health and regularity of the menstrual cycle. | Women shift workers [5] |
| Need for Self-Management Support | The perceived need for external help or resources to manage one's health condition. | HIV-positive women [14] |
The following diagram illustrates the logical workflow for establishing the conceptual model and initial domains, integrating both theoretical and empirical elements.
Figure 1: Workflow for developing a conceptual model and initial domains.
Experimental Protocols for Domain Validation
Once an initial item pool is generated from the conceptual model, rigorous quantitative protocols are employed to validate the proposed domain structure.
Protocol for Assessing Content Validity
Objective: To ensure the questionnaire's items are relevant, clear, and comprehensive for the intended construct and population. Materials: Preliminary item pool, panel of experts (typically 10-13), standardized rating forms. Method:
- Convene Expert Panel: Assemble a multidisciplinary panel of experts in relevant fields (e.g., reproductive health, psychology, instrument development) [13] [5].
- Quantitative Assessment:
- Content Validity Ratio (CVR): Experts rate each item on its essentiality to the construct using a 3-point scale (e.g., "essential," "useful but not essential," "not essential"). The CVR is calculated for each item, and items falling below a critical value (e.g., 0.62 for 10 experts) are removed [13] [14].
- Content Validity Index (CVI): Experts rate each item on relevance, clarity, and simplicity using a 4-point scale. The CVI is calculated, and items with a value below 0.79 should be revised or eliminated [13] [14].
- Qualitative Assessment: Experts provide open-ended feedback on grammar, wording, item allocation, and scaling, which is used to refine the items [13] [5].
- Pilot with Target Population: A small sample from the target population completes the questionnaire and is interviewed to identify any difficulties with interpretation, wording, or phrasing, establishing face validity [13] [5].
Protocol for Assessing Construct Validity via Exploratory Factor Analysis (EFA)
Objective: To empirically uncover the underlying factor structure (domains) of the questionnaire and assess how well items load onto their intended constructs. Materials: Refined item pool from content validity, statistical software (e.g., SPSS, R), a sample of participants from the target population (minimum N=300 is a common rule of thumb) [5]. Method:
- Data Collection: Administer the refined questionnaire to a sufficiently large sample.
- Data Suitability Checks: Before performing EFA, check the suitability of the data using:
- Factor Extraction: Use maximum likelihood or principal axis factoring to extract factors. The number of factors to retain can be determined by eigenvalues (>1.0) and scree plots [13] [12].
- Factor Rotation: Apply a rotation method (e.g., Varimax) to simplify the factor structure and enhance interpretability.
- Interpretation: Examine the factor loadings for each item. Loadings equal to or greater than |0.3| are typically considered acceptable for retaining an item within a factor [13] [14]. The factors are then named based on the themes of the items that load onto them.
Table 2: Key Psychometric Properties from Sample Validation Studies
| Psychometric Property | Target Value | Example from Literature |
|---|---|---|
| Content Validity | ||
| Content Validity Ratio (CVR) | > 0.62 (for 10 experts) | Mean CVR of 0.64 [13] |
| Content Validity Index (CVI) | > 0.79 per item | 104 items had CVI ≥ 0.79 [13] |
| Construct Validity | ||
| KMO Measure | > 0.8 | KMO value was acceptable [13] |
| Total Variance Explained | > 50% | Six factors accounted for 67% of variance [13] |
| Reliability | ||
| Cronbach's Alpha (Internal Consistency) | > 0.7 | Alpha = 0.92 [13]; Alpha = 0.713 [14] |
| Intraclass Correlation Coefficient (ICC) - Test-Retest | > 0.7 (Good) | ICC = 0.86 (Total Scale) [13]; ICC = 0.952 [14] |
The Scientist's Toolkit: Research Reagents and Essential Materials
This section details key resources required for the experimental protocols described in this document.
Table 3: Essential Materials for Questionnaire Development and Validation
| Item / Solution | Function in Protocol | Specifications / Notes |
|---|---|---|
| Expert Panel | To provide qualitative and quantitative assessments of content validity. | Should include 10-13 multidisciplinary experts in relevant fields (e.g., health education, reproductive health, psychology) [13] [5]. |
| Target Population Sample | To participate in qualitative phases and pilot testing for face validity. | Participants should meet specific inclusion criteria (e.g., age, health status, experience) relevant to the research objective [14] [5]. |
| Statistical Software | To perform data management, Exploratory Factor Analysis (EFA), and reliability analysis. | Common platforms include SPSS, R (with packages like 'psych' for EFA and 'irr' for ICC), and AMOS for Confirmatory Factor Analysis [13] [15]. |
| Standardized Rating Forms | To collect structured feedback from experts during content validity assessment. | Forms should be designed for 3-point (CVR) and 4-point (CVI) Likert scales as per established guidelines [13] [14]. |
| Semi-Structured Interview Guide | To conduct in-depth qualitative exploration of the research concept. | Includes open-ended questions and probes to explore participants' experiences and perceptions until data saturation is achieved [5]. |
Generating the Preliminary Item Pool
This application note details the methodology for generating a preliminary item pool, a critical first step in developing a valid and reliable reproductive health behavior questionnaire. The process outlined below employs a sequential exploratory mixed-method design, which integrates qualitative and literature-driven approaches to ensure the item pool is both comprehensive and grounded in the lived experiences of the target population [2] [5] [14].
Detailed Experimental Protocols
Protocol 1: Qualitative Item Generation via Thematic Analysis
This protocol aims to generate novel items directly from the target population's narratives and experiences [2] [5].
1.1 Participant Recruitment and Sampling:
- Sampling Method: Employ purposive sampling with maximum variation to capture a wide spectrum of experiences. Key demographic and experiential characteristics for stratification include age, socioeconomic status, educational level, and clinical history (e.g., work schedule for shift workers, HIV status, or years since diagnosis) [5] [14].
- Sample Size: Recruitment continues until data saturation is achieved, typically involving 20-30 participants [5] [14].
- Inclusion Criteria: Criteria are population-specific. For a women's shift worker questionnaire, for example, participants may be required to be married, aged 18–45, with work experience exceeding two years [5].
1.2 Data Collection:
- Method: Conduct semi-structured, in-depth, individual interviews in a private setting [2] [5].
- Interview Guide: Use open-ended questions to explore perceptions and behaviors. Example prompts include:
- Data Management: Audio-record interviews and transcribe them verbatim for analysis [14].
1.3 Data Analysis:
- Method: Utilize conventional content analysis as described by Graneheim and Lundman [5].
- Process:
- Repeatedly read transcripts to achieve immersion and obtain a sense of the whole.
- Identify meaning units (words, sentences, or paragraphs related to the research aim).
- Condense meaning units into codes.
- Group similar codes into subcategories and categories based on their relationships and hidden meanings.
- Formulate themes that describe the phenomenon under study [5] [14].
- Software: Use qualitative data analysis software (e.g., MAXQDA) to manage and retrieve coded data [14].
1.4 Item Formulation:
- Convert the identified codes, subcategories, and categories into a series of preliminary questionnaire items. This represents the inductive component of the item pool [2] [14].
Protocol 2: Item Generation via Systematic Literature Review
This protocol supplements qualitative findings by identifying established concepts and existing items from prior research [5] [8].
2.1 Search Strategy:
- Databases: Search relevant scientific databases (e.g., PubMed, Scopus, Web of Science).
- Keywords: Use a combination of keywords related to the target population (e.g., "men," "HIV-positive women," "shift workers"), "reproductive health," and "questionnaire" or "instrument."
- Time Frame: Review literature from a defined period, often the past 10-20 years, to ensure contemporary relevance [8].
2.2 Data Extraction and Synthesis:
- Objective: Identify constructs, domains, and specific items from validated reproductive health assessment tools [16] [17].
- Process: Systematically extract all items from relevant questionnaires. Commonly used toolkits include the Reproductive Health Assessment Toolkit for Conflict-Affected Women (CDC) and the Adolescent Sexual and Reproductive Health Toolkit for Humanitarian Settings (UNFPA/Save the Children) [16] [17].
- Outcome: This process generates a list of deductive items for potential inclusion [5].
2.3 Finalizing the Preliminary Item Pool:
- Action: Combine items derived from the qualitative analysis (Protocol 1) with those gathered from the literature review (Protocol 2).
- Refinement: Hold research team meetings to review all items, merging overlapping items and removing duplicates to form the initial preliminary item pool [14].
The following workflow summarizes this two-pronged protocol.
The Scientist's Toolkit: Research Reagent Solutions
The table below lists essential materials and their functions for executing the protocols.
| Item Name | Function/Application in Protocol | Specific Examples from Literature |
|---|---|---|
| Semi-Structured Interview Guide | Ensures consistent exploration of key topics across all participants while allowing flexibility to probe unique experiences [5]. | Questions: "What are the effects of shift work on reproductive health?" "What factors affect reproductive health?" [5] |
| Audio Recording Equipment | Captures participant interviews verbatim for accurate transcription and data analysis [14]. | - |
| Qualitative Data Analysis Software | Aids in organizing, managing, and coding large volumes of textual data efficiently [14]. | MAXQDA software [14]. |
| Validated Reference Toolkits | Provides a foundation of pre-existing, psychometrically tested items and constructs for the literature review [16] [17]. | - Reproductive Health Assessment Toolkit for Conflict-Affected Women (CDC) [16] [17].- Adolescent Sexual and Reproductive Health Toolkit for Humanitarian Settings (UNFPA/Save the Children) [16] [17]. |
| Expert Panel | Provides qualitative assessment of content validity, checking grammar, wording, item allocation, and scaling of the initial item pool [5] [13]. | Panel of 10-12 experts in fields like reproductive health, midwifery, gynecology, and occupational health [5]. |
Key Methodological Considerations
Successful execution of this phase requires careful attention to several factors:
- Theoretical Framework: In some studies, the entire process is guided by a theoretical framework (e.g., the Theory of Planned Behavior), which shapes the interview questions and literature search strategy [13].
- Data Trustworthiness (Qualitative Phase): Ensure the credibility, dependability, confirmability, and transferability of qualitative data through techniques like member checking, peer debriefing, and maintaining an audit trail [5].
- Pilot Testing: Conduct a pilot of the interview guide and the initial merged item pool with a small sample from the target population to assess comprehension, clarity, and relevance [8] [13].
By rigorously adhering to this mixed-method protocol, researchers can generate a robust and culturally relevant preliminary item pool, establishing a solid foundation for subsequent phases of psychometric validation, including face, content, and construct validity assessment.
Establishing Content and Face Validity
Within the rigorous process of reproductive health behavior questionnaire development, establishing content and face validity forms the foundational pillar ensuring a tool's credibility and usefulness. For researchers and drug development professionals, these initial validation stages guarantee that an instrument accurately measures the constructs it intends to measure and is perceived as relevant by its target audience. In the context of reproductive health, where topics are often sensitive and constructs complex—ranging from behaviors to reduce exposure to endocrine-disrupting chemicals (EDCs) to sexual practices and contraceptive use—methodologically sound validity establishment is not merely beneficial but essential for generating reliable data [8] [11]. This protocol provides detailed application notes for systematically establishing content and face validity, framed within a comprehensive questionnaire development framework.
Conceptual Foundations: Content and Face Validity
Content validity refers to the degree to which elements of an assessment instrument are relevant to and representative of the targeted construct for a particular assessment purpose. It is not a statistical property but is established qualitatively through structured expert judgment. The goal is to ensure the item pool comprehensively covers the entire domain of the construct without contamination from irrelevant content [8].
Face validity, often considered a superficial form of validity, assesses whether the instrument appears to measure what it is supposed to measure from the perspective of the end respondent. While not sufficient on its own, strong face validity improves participant engagement, reduces measurement error, and increases response rates, particularly for sensitive topics in reproductive health where respondent buy-in is critical [18].
The following table differentiates these key concepts:
Table 1: Distinguishing Content and Face Validity
| Aspect | Content Validity | Face Validity |
|---|---|---|
| Primary Focus | Relevance and representativeness of content to the construct | Appearance of relevance to the respondent |
| Evaluation Method | Expert judgment (quantified via CVI) | Target population feedback |
| Key Question | "Does this item validly measure part of the construct?" | "Does this item seem relevant and clear to the respondent?" |
| Outcome Metric | Content Validity Index (CVI) | Thematic analysis of feedback on relevance and comprehension |
Experimental Protocol for Establishing Content Validity
Stage 1: Defining the Construct and Generating Items
The initial stage involves a precise operational definition of the reproductive health construct to be measured.
Procedure:
- Construct Delineation: Conduct a comprehensive literature review of the construct (e.g., "behaviors to reduce exposure to EDCs in daily life") to define its boundaries and key dimensions [8].
- Item Generation: Develop a large, inclusive pool of initial items based on the literature, existing instruments, and theoretical frameworks. For a reproductive health behavior questionnaire, this may involve generating items related to specific exposure routes (food, respiration, skin) and health promotion behaviors [8].
- Item Formulation: Write clear, unambiguous, and simple items. Avoid jargon, double-barreled questions, and leading language. For sensitive topics, use neutral and non-judgmental phrasing [11].
Stage 2: Assembling the Expert Panel
The selection of a multidisciplinary expert panel is critical for robust content validity assessment.
Procedure:
- Panel Composition: Recruit 5-10 experts with diverse backgrounds relevant to the construct. For a reproductive health questionnaire, this may include clinical specialists (e.g., physicians, nurses), research methodologies, and subject-matter experts (e.g., environmental scientists, psychologists) [8].
- Expert Credentials: Ensure experts have recognized expertise in the field, evidenced by publications, clinical experience, or professional qualifications.
- Briefing: Provide experts with a clear briefing document detailing the construct definition, target population, and the purpose of the instrument.
Stage 3: Expert Rating and Quantitative Analysis
Experts systematically rate each item on its relevance to the defined construct.
Procedure:
- Rating Scale: Provide experts with a 3- or 4-point rating scale (e.g., 1 = not relevant, 2 = somewhat relevant, 3 = quite relevant, 4 = highly relevant) [8].
- Data Collection: Use a structured survey to collect expert ratings for all items.
- Calculate Content Validity Indices (CVI):
- Item-level CVI (I-CVI): The proportion of experts giving a rating of 3 or 4 for each item. An I-CVI of 0.78 or higher is considered excellent for a panel of 5-10 experts.
- Scale-level CVI (S-CVI): The average of all I-CVIs, representing the overall content validity of the scale. A target of 0.80 or higher is recommended for newly developed instruments [8].
- Qualitative Feedback: Solicit open-ended feedback from experts on item clarity, redundancy, and suggestions for new items.
The workflow for establishing content validity, from item generation to final item selection, is a structured, iterative process, as summarized below.
Experimental Protocol for Establishing Face Validity
Stage 1: Developing the Pilot Instrument
Procedure:
- Instrument Formatting: Compile the items that have passed the content validity stage into a draft questionnaire. Use a clear layout, intuitive navigation instructions, and a consistent response scale.
- Cognitive Interview Guide: Develop a semi-structured interview guide to probe participants' understanding of items, instructions, and response options.
Stage 2: Recruiting the Target Population
Procedure:
- Participant Sampling: Recruit a small but diverse sample (e.g., n=10-15) from the instrument's intended target population [8] [18]. For a reproductive health questionnaire, ensure diversity in age, gender, socioeconomic status, and relevant health experiences.
- Informed Consent: Obtain informed consent, clearly explaining the purpose of the pilot test and the voluntary nature of participation, following IRB-approved protocols [19] [18].
Stage 3: Conducting Cognitive Interviews and Thematic Analysis
Procedure:
- Think-Aloud Protocol: Ask participants to complete the questionnaire while verbalizing their thought process. Prompt them to explain what they think each question is asking and how they decided on their answer.
- Probing Questions: After completion, use the interview guide to ask specific probes (e.g., "Can you explain that question in your own words?", "Was any wording confusing or offensive?", "How did you find the response options?").
- Data Analysis: Transcribe interviews and analyze the data using thematic analysis. Identify recurring themes related to comprehension difficulties, ambiguous terms, irrelevant content, and layout issues [18].
- Questionnaire Revision: Systematically revise the questionnaire based on the thematic analysis to improve clarity, relevance, and acceptability.
The process of establishing face validity is participatory and iterative, centering on the end-user's perspective, as shown in the following workflow.
Data Presentation and Analysis
Quantitative Data from Expert Review
The following table provides a template for presenting and analyzing quantitative results from the expert content validity review, using hypothetical data from a reproductive health behavior questionnaire.
Table 2: Exemplar Content Validity Analysis for a Reproductive Health Questionnaire
| Item Number | Item Description | Expert 1 | Expert 2 | Expert 3 | Expert 4 | Expert 5 | I-CVI | Action |
|---|---|---|---|---|---|---|---|---|
| 1 | I check product labels for "BPA-free" before purchasing. | 4 | 3 | 4 | 4 | 3 | 1.00 | Retain |
| 2 | I avoid consuming food from plastic containers when possible. | 4 | 4 | 4 | 3 | 4 | 1.00 | Retain |
| 3 | I use public transportation daily. | 2 | 1 | 3 | 2 | 1 | 0.20 | Discard |
| 4 | I choose personal care products labeled "paraben-free." | 3 | 4 | 4 | 4 | 3 | 1.00 | Retain |
| 5 | I air out my home to reduce indoor chemical exposure. | 4 | 3 | 4 | 3 | 4 | 1.00 | Retain |
| ... | ... | ... | ... | ... | ... | ... | ... | ... |
| S-CVI/Ave | 0.90 |
Thematic Analysis from Target Population Review
The following table demonstrates how to synthesize qualitative feedback from cognitive interviews to establish face validity.
Table 3: Exemplar Thematic Analysis of Face Validity Feedback
| Theme | Illustrative Quotation | Identified Issue | Recommended Revision |
|---|---|---|---|
| Jargon | "I don't know what 'endocrine-disrupting' means. It sounds scary." | Technical term not understood by laypersons. | Replace with simpler language: "chemicals that can harm your health". |
| Ambiguous Wording | " 'Often'... what does that mean? Once a week? Once a month?" | Vague frequency term. | Use specific timeframes: "In the past month, how many times...". |
| Sensitive Language | "The question about my sex life felt too direct and judgmental." | Question perceived as intrusive or offensive. | Rephrase to be more neutral and normalize the behavior. |
| Response Option Clarity | "I wanted an option between 'agree' and 'disagree'." | Limited response options force inaccurate answers. | Expand from a 4-point to a 5-point Likert scale to include "Neutral". |
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential methodological components for establishing content and face validity.
Table 4: Essential Methodological Components for Validity Establishment
| Tool or Resource | Function in Validity Establishment | Application Notes |
|---|---|---|
| Multidisciplinary Expert Panel | Provides authoritative judgment on item relevance and representativeness (content validity). | Include 5-10 experts from clinical, research, and subject-matter backgrounds. Document expertise credentials [8]. |
| Content Validity Index (CVI) | Quantifies the degree of expert consensus on item relevance. | Calculate I-CVI (per item) and S-CVI/Ave (for the scale). Use thresholds of 0.78 and 0.80, respectively [8]. |
| Cognitive Interviewing | Elicits evidence of how the target population comprehends and responds to items (face validity). | Use "think-aloud" and verbal probing techniques. Focus on identifying misinterpretation and sources of response error [18]. |
| Structured Rating Survey | Systematically collects expert ratings for CVI calculation. | Should include the construct definition, rating scale, and items. Administer via platforms like REDCap or Qualtrics for efficiency [20]. |
| Thematic Analysis Framework | Analyzes qualitative feedback from cognitive interviews to identify recurring usability issues. | Use inductive and deductive coding to systematically categorize feedback into themes like clarity, relevance, and sensitivity [21]. |
| Pilot Questionnaire | A draft version of the instrument used for face validity testing with the target population. | Should mirror the final format, including all instructions, items, and response layouts to test the full user experience [8]. |
From Items to Instrument: Scale Development and Quantitative Evaluation
Survey Administration and Sample Size Determination
Within reproductive health research, the development of validated questionnaires is fundamental for translating complex behavioral, attitudinal, and clinical observations into reliable quantitative data. This process is critical for assessing constructs such as behaviors to reduce exposure to endocrine-disrupting chemicals (EDCs) or the impact of shift work on female reproductive health [8] [22]. The administration of these surveys and the determination of an adequate sample size are not mere procedural steps; they are foundational to the statistical validity and overall scientific rigor of a study. This document provides detailed application notes and protocols for these key methodological areas, framed within the context of reproductive health behavior questionnaire development.
Core Concepts and Definitions
Key Validity and Reliability Concepts for Questionnaires
For a research questionnaire to yield meaningful data, its validity and reliability must be established. Validity refers to the accuracy of a tool—whether it measures what it intends to measure. Reliability refers to the consistency of the measure over time and across different observers [1]. The table below summarizes the primary types of validity and reliability researchers must assess.
Table 1: Key Types of Questionnaire Validity and Reliability
| Type | Brief Description | Common Assessment Method |
|---|---|---|
| Face Validity | A subjective assessment of whether the questionnaire appears to measure what it claims to. | Review by non-experts from the target audience for clarity and appropriateness. |
| Content Validity | The degree to which a tool covers all aspects of the construct it aims to investigate. | Review by a panel of subject matter experts; calculated using a Content Validity Index (CVI). |
| Construct Validity | The extent to which the tool actually measures the theoretical construct. | Exploratory Factor Analysis (EFA) and Confirmatory Factor Analysis (CFA). |
| Criterion Validity | How well the tool agrees with an existing gold-standard assessment. | Correlation analysis with the validated criterion measure. |
| Internal Consistency | The extent of intercorrelations among all items within the questionnaire. | Cronbach's alpha coefficient (α); value of 0.7 or higher is typically acceptable. |
| Test-Retest Reliability | The stability of the measure over time when the characteristic is assumed to be unchanged. | Administering the same test to the same individuals after a set time interval. |
| Inter-rater Reliability | The consistency of the measure when used by different assessors. | Cohen’s kappa statistic to evaluate agreement between multiple raters. |
Fundamentals of Sample Size Determination
Sample size calculation is essential to ensure a study has a high probability of detecting a true effect if one exists, while balancing ethical and resource constraints. An inappropriately small sample size may lead to false negatives, while an excessively large one can identify statistically significant but clinically trivial effects [23]. The following elements are crucial for sample size calculation:
- Statistical Analysis Plan: The intended statistical tests (e.g., t-test, ANOVA, regression) dictate the sample size formula [23].
- Effect Size: The magnitude of the difference or relationship the study aims to detect. This is often the most challenging parameter to set and can be determined from prior literature, pilot studies, or by using conventional values (e.g., small=0.2, medium=0.5, large=0.8) [23].
- Study Power: The probability that the test will correctly reject a false null hypothesis. A power of 80% or 90% is standard [23].
- Significance Level (Alpha): The threshold for statistical significance, typically set at 0.05 [23].
- Margin of Error (Precision): Particularly for descriptive studies estimating a proportion, this defines the acceptable plus-or-minus range around the estimated value [24].
Experimental Protocols
Protocol for Questionnaire Development and Validation
The following workflow outlines the sequential steps for creating a psychometrically sound questionnaire, exemplified by studies developing reproductive health instruments [8] [22].
Diagram 1: Questionnaire Development Workflow
Phase 1: Qualitative Item Pool Development
- Objective: To define the concept and generate an initial pool of questionnaire items [22].
- Procedure:
- Data Collection: Conduct semi-structured interviews with individuals from the target population (e.g., female shift workers, couples concerned about EDC exposure) until data saturation is reached. Perform a comprehensive literature review [22].
- Data Analysis: Transcribe interviews and analyze using conventional content analysis. Identify meaning units, code them, and group codes into subcategories and main categories that represent the dimensions of the construct [22].
- Item Generation: Convert the identified categories and codes into a preliminary set of questionnaire items. Wording should be clear and precise [8].
Phase 2: Quantitative Psychometric Validation
- Objective: To refine the item pool and validate the questionnaire's psychometric properties [8] [22].
- Procedure:
- Face Validity Assessment:
- Qualitative: Ask members of the target population to evaluate items for difficulty, appropriateness, and clarity.
- Quantitative: Use the "item impact" method, where participants rate the importance of each item. Retain items with an impact score above 1.5 [22].
- Content Validity Assessment:
- Qualitative: A panel of experts (e.g., in instrument development, reproductive health) reviews the items for wording and scaling.
- Quantitative: Experts rate each item on relevance. Calculate the Item-Level Content Validity Index (I-CVI); items with an I-CVI above 0.78 are typically retained [8] [1].
- Pilot Study: Administer the questionnaire to a small sample (e.g., n=10) to identify any practical issues with administration, comprehension, or time [8].
- Construct Validity Assessment:
- Exploratory Factor Analysis (EFA): Administer the questionnaire to a larger sample (e.g., n=288). Use EFA (e.g., Principal Component Analysis with varimax rotation) to identify the underlying factor structure. Retain items with factor loadings >0.4 [8].
- Confirmatory Factor Analysis (CFA): Test the model derived from EFA on a separate sample or the same sample to confirm the factor structure. Use fit indices (e.g., RMSEA, SRMR) to evaluate model fit [8].
- Reliability Assessment:
- Internal Consistency: Calculate Cronbach's alpha for the entire scale and each subscale. A value of 0.7 or higher is acceptable for a new tool [8] [1].
- Stability (Test-Retest): Administer the questionnaire to the same participants after a suitable time interval (e.g., 2-3 weeks). Assess concordance using Pearson's correlation or similar methods [1].
- Face Validity Assessment:
Protocol for Sample Size Determination
The process for determining an adequate sample size varies based on the primary study design. The following workflow outlines the key steps and considerations.
Diagram 2: Sample Size Determination Workflow
A. For Descriptive Studies (e.g., Cross-Sectional Prevalence Studies)
- Objective: To estimate a population parameter (e.g., proportion, mean) with a specified level of precision [23].
- Parameters:
- Confidence Level: Typically 95%.
- Margin of Error (MoE): The acceptable deviation from the true population value (e.g., ±5%).
- Estimated Proportion (p): The expected proportion. If unknown, use 0.5 (50%) to maximize the required sample size and ensure adequacy [23].
- Calculation Formula (for a proportion):
n = (Z^2 * p * (1-p)) / e^2WhereZis the z-score for the confidence level (1.96 for 95%),pis the estimated proportion, andeis the margin of error. - Example: To estimate a prevalence with 95% confidence, a 5% MoE, and an assumed proportion of 0.5, the required sample size is
(1.96^2 * 0.5 * 0.5) / 0.05^2 = 385.
B. For Comparative Studies (e.g., Group Differences, Intervention Effects)
- Objective: To detect a specified effect size with adequate power [23].
- Parameters:
- Effect Size: The minimum difference of practical/clinical importance. This can be a standardized effect size (e.g., Cohen's d of 0.2, 0.5, 0.8 for small, medium, large effects) [23].
- Power (1-β): Usually 80% or 90%.
- Alpha (α): Usually 0.05.
- Calculation Method: Use statistical software (e.g., G*Power, OpenEpi, PS Power) and select the test corresponding to the primary analysis (e.g., t-test, chi-square test) [23].
- Example: For an independent samples t-test comparing two groups to detect a medium effect size (d=0.5) with 80% power and α=0.05, the required total sample size is 128 (64 per group) [23].
C. Adjustments and Considerations
- Dropout Rate: Inflate the calculated sample size to account for potential participant attrition. For example, if the calculated
nis 300 and a 10% dropout rate is anticipated, the final sample size should be300 / (1 - 0.10) = 334[8]. - Complex Analyses: For advanced analyses like Factor Analysis, sample size is often guided by rules of thumb, such as 5-10 participants per questionnaire item or a minimum of 300-500 participants [8] [23].
Table 2: Sample Size Requirements for Common Statistical Tests (Power=80%, α=0.05)
| Statistical Test | Effect Size | Total Sample Size | Key Parameters |
|---|---|---|---|
| Independent t-test | Small (d = 0.2) | 788 | Two groups, continuous outcome. |
| Medium (d = 0.5) | 128 | ||
| Large (d = 0.8) | 52 | ||
| Chi-square test | Small (w = 0.1) | 964 | Two groups, categorical outcome (e.g., 2x2 table). |
| Medium (w = 0.3) | 88 | ||
| Large (w = 0.5) | 32 | ||
| Correlation (Pearson's r) | Small (r = 0.1) | 782 | Tests the strength of a linear relationship. |
| Medium (r = 0.3) | 85 | ||
| Large (r = 0.5) | 29 |
Essential Research Reagents and Tools
Table 3: Key Research Reagent Solutions for Questionnaire Development and Validation
| Item/Tool | Function/Brief Explanation | Example Use in Protocol |
|---|---|---|
| Expert Panel | A multi-disciplinary group of subject matter experts to assess content validity. | Evaluating the relevance and clarity of initial items for a reproductive health questionnaire [8] [22]. |
| Statistical Software (e.g., IBM SPSS, AMOS, R) | Software packages used for comprehensive psychometric and statistical analysis. | Conducting Exploratory Factor Analysis (EFA), Confirmatory Factor Analysis (CFA), and calculating Cronbach's alpha [8]. |
| Sample Size Calculation Software (e.g., G*Power, OpenEpi) | Free, specialized tools for computing sample size requirements for various study designs. | Determining the minimum number of participants needed for a study comparing two groups with sufficient power [23]. |
| Pilot Sample | A small, representative subset of the target population used for preliminary testing. | Identifying ambiguous questions, estimating response time, and testing administrative procedures before full-scale deployment [8]. |
| Validated Gold-Standard Questionnaire | An existing, well-validated instrument measuring a related construct. | Assessing criterion validity by correlating scores from the new questionnaire with those from the established tool [1]. |
Psychometric Analysis and Factor Structure Identification
The development of robust, reliable, and valid questionnaires is fundamental to advancing research in sexual and reproductive health (SRH). Without rigorously validated instruments, researchers cannot accurately measure constructs, assess interventions, or compare outcomes across populations and studies. This protocol details comprehensive methodologies for the psychometric analysis and factor structure identification of SRH behavior questionnaires, providing researchers with a structured framework for measurement development and validation. The guidelines presented here are framed within a broader thesis on reproductive health questionnaire development, emphasizing standardized, evidence-based approaches that enhance measurement precision and facilitate cross-study comparisons.
The critical importance of psychometric validation is highlighted by a rapid review of sexual health knowledge tools for adolescents, which found that among sixteen identified Patient-Reported Outcome Measures (PROMs), the overall methodological quality was often "Inadequate" according to COSMIN (COnsensus-based Standards for the selection of health Measurement Instruments) standards. This review revealed inconsistent coverage of criterion validity, responsiveness, and interpretability across existing instruments [25]. Similarly, the development of a questionnaire for assessing SRH needs of married adolescent women addressed a significant gap, as no valid and reliable instrument previously existed specifically for this population [26]. This protocol aims to address these methodological shortcomings by providing detailed, standardized approaches for psychometric validation.
Theoretical Foundations: Factor Analysis vs. Cluster Analysis
A fundamental step in psychometric analysis involves understanding the appropriate application of different statistical techniques for dimension reduction. Factor analysis and cluster analysis serve distinct purposes and answer different research questions, yet they are frequently confused in multiple behavior research [27].
Factor Analysis is a variable-centered approach that identifies latent constructs (factors) that explain patterns of covariance among observed variables. It reduces many measured variables into fewer underlying factors and assesses how well these factors explain the observed data structure. This technique is ideal when researchers aim to understand the dimensional structure of a construct or identify groups of interrelated behaviors that may share a common underlying mechanism [27].
Cluster Analysis is a person-centered approach that classifies individuals into homogeneous subgroups (clusters) based on their similarity across multiple variables. It reduces a large number of individuals into a smaller set of clusters where individuals within clusters are more similar to each other than to those in other clusters. This method is appropriate for identifying typologies or subpopulations based on specific behavioral patterns [27].
Table 1: Comparison of Factor Analysis and Cluster Analysis
| Feature | Factor Analysis | Cluster Analysis |
|---|---|---|
| Primary Goal | Identify latent variables that explain patterns among observed variables | Classify individuals into homogeneous subgroups |
| Focus | Variable relationships | Individual similarities |
| Research Question | "What underlying constructs explain the patterns in our data?" | "What subgroups exist in our population based on their response patterns?" |
| Data Reduction | Reduces number of variables | Reduces number of individuals |
| Outcome | Factors or components | Clusters or groups of people |
| Example Application | Identifying domains of reproductive autonomy [28] | Identifying clusters of sleep and physical activity patterns in pregnant women [29] |
The choice between these techniques has significant implications for both analysis and subsequent interventions. As demonstrated in a study of co-occurring risk behaviors, cluster analysis identified three distinct clusters of individuals: a poor diet cluster, a high-risk cluster, and a low-risk cluster. In contrast, factor analysis of the same data revealed two latent factors: substance use and unhealthy diet, demonstrating how the same dataset can yield different insights based on the analytical approach selected [27].
Phase 1: Questionnaire Development and Initial Validation
Item Generation and Content Validity
The initial phase of questionnaire development requires comprehensive item generation and rigorous content validation. The protocol for developing a questionnaire for married adolescent women's SRH needs exemplifies this process, beginning with in-depth interviews with 34 married adolescent women and four key informants, complemented by a comprehensive literature review. This qualitative phase generated 137 initial items encompassing the full spectrum of SRH needs [26].
Content validity assessment involves evaluating the relevance, comprehensiveness, and appropriateness of each item for the target construct and population. Expert review panels should assess each item for clarity, specificity, and conceptual alignment with the theoretical framework. In the married adolescent women questionnaire development, this process resulted in the refinement of the initial 137 items to a 108-item preliminary questionnaire through several modifications based on expert feedback and conceptual overlap assessment [26].
Face validity assessment ensures the questionnaire appears to measure the intended constructs from the perspective of the target population. Cognitive interviewing techniques, where participants verbalize their thought process while responding to items, are particularly valuable for identifying problematic wording, confusing response options, or sensitive items that may cause discomfort or non-response. The World Health Organization's development of the Sexual Health Assessment of Practices and Experiences (SHAPE) questionnaire employed a comprehensive multi-country cognitive interviewing study across 19 countries to refine questions and ensure cross-cultural applicability [11].
Instrument Selection and Adaptation
For researchers adapting existing instruments rather than developing new ones, careful evaluation of measurement properties is essential. The COSMIN (COnsensus-based Standards for the selection of health Measurement Instruments) checklist provides a standardized framework for evaluating the methodological quality of existing PROMs [25]. When evaluating instruments, researchers should consider:
- Conceptual alignment with the target construct and population
- Measurement properties including reliability, validity, and responsiveness
- Linguistic and cultural appropriateness for the intended population
- Administrative feasibility in terms of length, format, and scoring requirements
The Reproductive Health Literacy Scale development demonstrates this adaptive approach, where researchers combined domains from multiple existing validated instruments: the HLS-EU-Q6 for general health literacy, eHEALS for digital health literacy, and items from the C-CLAT and a postpartum literacy scale for reproductive health-specific literacy [30].
Table 2: Selected Validated Instruments for Sexual and Reproductive Health Research
| Instrument Name | Construct Measured | Factors/ Domains | Reliability (Cronbach's α) | Sample Items/Format |
|---|---|---|---|---|
| Questionnaire for SRH Needs of Married Adolescent Women [26] | SRH needs of married adolescents | 9 domains including sexual quality of life, self-care, self-efficacy, knowledge | 0.878 (whole scale) | 74 items using Likert-scale responses |
| Reproductive Autonomy Scale (RAS) [28] | Reproductive autonomy | 3 factors: Freedom from coercion, Communication, Decision-making | 0.75 (UK validation) | Items rated on agreement scale; 3-factor structure confirmed |
| Sexual Health Questionnaire (SHQ) [25] | Sexual health knowledge | Not specified | 0.90 | Distinguished by robust construct validity (68.25% variance explained) |
| WHO SHAPE Questionnaire [11] | Sexual practices, behaviors, and health outcomes | Multiple modules including sexual problems | Implementation tested | Combination of interviewer-administered and self-administered modules |
| Reproductive Health Literacy Scale [30] | Health literacy in refugee women | 3 domains: General, digital, and reproductive health literacy | >0.7 (all domains) | Adapted from multiple validated tools; translated into multiple languages |
Phase 2: Psychometric Validation Protocol
Factor Structure Identification
Sample Size Considerations
Adequate sample size is critical for stable factor solutions. While rules of thumb vary, a minimum of 10 participants per item is often recommended for exploratory factor analysis (EFA). For confirmatory factor analysis (CFA), sample sizes of 200+ are generally recommended, though larger samples provide more stable parameter estimates. The married adolescent women questionnaire development utilized an exploratory sequential mixed methods design, with the quantitative phase including a sufficient sample size for stable factor analysis [26].
Exploratory Factor Analysis (EFA) Protocol
Data Preparation: Screen data for missing values, outliers, and assess normality of distributions. Use appropriate missing data techniques (e.g., multiple imputation) if necessary.
Factorability Assessment: Examine the correlation matrix for sufficient correlations (≥0.30) between items. Calculate the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy (values >0.60 acceptable, >0.80 good) and Bartlett's test of sphericity (should be significant, p<0.05).
Factor Extraction: Principal axis factoring or maximum likelihood estimation are commonly used. Determine the number of factors to retain using multiple criteria:
- Kaiser criterion (eigenvalues >1)
- Scree test (visual examination of the scree plot)
- Parallel analysis (comparing eigenvalues to those from random data)
Factor Rotation: Apply oblique rotation (e.g., promax) when factors are expected to correlate, or orthogonal rotation (e.g., varimax) when theoretical independence is assumed.
Interpretation and Refinement: Retain items with factor loadings ≥0.40 on primary factor and minimal cross-loadings (<0.32 on secondary factors). The married adolescent women questionnaire development removed 11 items during EFA based on these criteria, resulting in a final 74-item questionnaire categorized into nine factors [26].
The following workflow diagram illustrates the comprehensive factor analysis process:
Confirmatory Factor Analysis (CFA) Protocol
Model Specification: Define the theoretical model based on EFA results or existing literature, specifying which items load on which factors.
Parameter Estimation: Use maximum likelihood estimation or robust alternatives for non-normal data.
Model Fit Assessment: Evaluate multiple fit indices:
- χ²/df ratio (<3 acceptable, <2 good)
- Comparative Fit Index (CFI >0.90 acceptable, >0.95 good)
- Tucker-Lewis Index (TLI >0.90 acceptable, >0.95 good)
- Root Mean Square Error of Approximation (RMSEA <0.08 acceptable, <0.05 good)
- Standardized Root Mean Square Residual (SRMR <0.08 acceptable)
Model Modification: Use modification indices cautiously to improve model fit, with strong theoretical justification for any changes.
In the validation of the Reproductive Autonomy Scale for use in the UK, confirmatory factor analysis confirmed the three-factor structure of the scale originally identified in the US version, demonstrating cross-cultural stability of the measurement model [28].
Reliability Assessment
Reliability refers to the consistency and stability of measurement. This protocol assesses multiple forms of reliability:
Internal Consistency
Calculate Cronbach's alpha coefficient for the total scale and each subscale. Values ≥0.70 are generally acceptable for group comparisons, while ≥0.90 is preferable for individual clinical assessment. The married adolescent women questionnaire demonstrated excellent internal consistency with a Cronbach's alpha of 0.878 for the whole scale [26]. For the Reproductive Health Literacy Scale, internal consistency was maintained across multiple language versions with alpha coefficients above 0.7 for all domains [30].
Test-Retest Reliability
Administer the same questionnaire to the same participants after a sufficient time interval (typically 2-4 weeks) to assess temporal stability. Calculate the intraclass correlation coefficient (ICC), with values ≥0.70 indicating acceptable stability. The married adolescent women questionnaire demonstrated exceptional test-retest reliability with an ICC of 0.99 for the whole scale [26], while the Reproductive Autonomy Scale validation in the UK showed fair-good test-retest reliability with an ICC of 0.67 over a 3-month interval [28].
Additional Validity Evidence
Construct Validity
Assess relationships with other measures through hypothesis testing. For example, in the UK validation of the Reproductive Autonomy Scale, researchers tested the hypothesis that among women who want to avoid pregnancy, those with higher reproductive autonomy would be more likely to use contraception, which was supported by the data [28].
Criterion Validity
When possible, compare scores with a "gold standard" measure of the same construct. However, this is often challenging in SRH research where well-established criteria may not exist. The rapid review of sexual health knowledge tools noted that criterion validity was often neglected in existing PROMs [25].
Advanced Applications: Cluster Analysis in SRH Research
While factor analysis identifies latent constructs, cluster analysis classifies individuals based on their response patterns. This approach is particularly valuable for identifying subpopulations with distinct behavioral profiles that may require tailored interventions.
Cluster Analysis Protocol
Variable Selection: Choose variables that theoretically relate to the clustering objective. A study of sleep and physical activity patterns in pregnant women used the Pittsburgh Sleep Quality Index and International Physical Activity Questionnaire as clustering variables [29].
Data Standardization: Standardize variables to comparable scales using z-scores or other normalization techniques.
Similarity Measure Selection: Select appropriate distance measures (e.g., Euclidean, Squared Euclidean, Manhattan distance) based on variable types.
Clustering Algorithm Selection: Choose between:
- Hierarchical clustering (agglomerative or divisive)
- Partitioning methods (e.g., k-means clustering)
- Model-based methods (e.g., latent profile analysis)
Determining Number of Clusters: Use multiple criteria:
- Theoretical justification
- Dendrogram inspection (for hierarchical clustering)
- Statistical indices (e.g., elbow method, silhouette width, Bayesian Information Criterion)
Cluster Validation and Interpretation: Validate clusters through:
- Internal validation (within-cluster homogeneity, between-cluster separation)
- External validation (relationship with variables not used in clustering)
- Replication in split samples or independent datasets
In a study of Korean pregnant women, cluster analysis identified three distinct clusters: 'good sleeper' (63.4%), 'poor sleeper' (24.6%), and 'low activity' (12.0%). These clusters demonstrated differential associations with demographic factors and psychological outcomes, with the good-sleeper cluster associated with higher education and income levels, and the poor-sleeper and low-activity clusters associated with higher depressive symptoms and pregnancy stress [29].
The following diagram illustrates the cluster analysis methodology:
Comparative Analysis of Clustering Applications
Table 3: Applications of Cluster Analysis in Health Behavior Research
| Study/Application | Clustering Variables | Identified Clusters | Key Associations |
|---|---|---|---|
| Sleep & Activity in Pregnancy [29] | Sleep quality, sleep duration, physical activity | 1. Good sleeper (63.4%)2. Poor sleeper (24.6%)3. Low activity (12.0%) | Good sleepers: higher education/income, healthier behaviorsPoor sleepers/low activity: higher depression/stress |
| Multiple Health Behaviors [27] | Alcohol, smoking, drug use, physical inactivity, diet | 1. Poor diet cluster2. High risk cluster3. Low risk cluster | Different demographic and psychological profiles per cluster |
| Canadian Longitudinal Study on Aging [31] | Physical inactivity, unhealthy eating, smoking, alcohol use | Proposed analysis of how behaviors cluster in adults 45-85+ | Aim to inform tailored interventions for subpopulations |
Implementation Considerations and Reporting Standards
Cross-Cultural Adaptation
When adapting instruments for cross-cultural use or specific populations, additional steps are necessary:
- Forward and Back Translation: Use independent translators followed by reconciliation of discrepancies.
- Cognitive Interviewing: Conduct interviews with target population members to assess comprehension, cultural relevance, and acceptability.
- Psychometric Re-validation: Conduct full psychometric validation in the new cultural context or population.
The Reproductive Health Literacy Scale development exemplified this approach through translation into Dari, Arabic, and Pashto, followed by validation with refugee women from different linguistic backgrounds [30]. Similarly, the UK validation of the Reproductive Autonomy Scale confirmed that the instrument maintained its measurement properties despite cultural differences [28].
Administration Modalities
Questionnaire administration methods can impact data quality and participant responses:
- Computer-Assisted Self-Interviewing (CASI): Enh privacy for sensitive topics, reduces social desirability bias.
- Computer-Assisted Personal Interviewing (CAPI): Allows clarification but may increase social desirability bias for sensitive topics.
- Mixed-Mode Administration: The WHO SHAPE questionnaire uses a combination of CAPI and CASI to balance advantages of both approaches [11].
Implementation of the SHAPE questionnaire in Portugal demonstrated feasibility across different administration modalities, with an overall response rate of 30.9% (79.5% online, 12.4% by telephone) and 94% of responses deemed valid. The average completion time was 17.7 minutes for the core questionnaire [32].
Sample Size Planning for Psychometric Studies
Adequate sample sizes are essential for stable parameter estimates in psychometric analyses:
- Exploratory Factor Analysis: Minimum 10 participants per item, with larger samples preferred
- Confirmatory Factor Analysis: Minimum 200 participants, with larger samples for complex models
- Test-Retest Reliability: Minimum 50 participants for stability assessment
- Cluster Analysis: Larger samples (n>300) provide more stable cluster solutions
Table 4: Research Reagent Solutions for Psychometric Analysis
| Tool/Resource | Function/Purpose | Application Context | Key Features |
|---|---|---|---|
| COSMIN Checklist [25] | Assess methodological quality of Patient-Reported Outcome Measures | Systematic evaluation of existing instruments | Standardized framework for evaluating reliability, validity, responsiveness |
| WHO SHAPE Questionnaire [11] | Assess sexual practices, behaviors, and health outcomes | Global population-based studies | Cross-culturally validated; combination of CAPI and CASI administration |
| Reproductive Autonomy Scale [28] | Measure control over contraceptive use and reproductive decisions | Clinical practice, intervention research | Three-factor structure: coercion, communication, decision-making |
| Health Literacy Tool Shed [30] | Database of health literacy measurement instruments | Identifying existing validated measures | Searchable repository with instrument characteristics |
| REDCap/XLSForm Versions of SHAPE [11] | Electronic implementation of questionnaires | Multi-site studies, global research | Facilitates standardized data collection across settings |
Robust psychometric analysis and factor structure identification are essential components of questionnaire development in reproductive health research. This protocol provides a comprehensive framework for developing, adapting, and validating SRH measures, with specific methodologies for both factor analysis and cluster analysis approaches. By following these standardized procedures, researchers can enhance the methodological rigor of measurement development, facilitate cross-study comparisons, and ultimately contribute to more valid assessment of sexual and reproductive health outcomes across diverse populations.
The field would benefit from increased attention to often-neglected psychometric properties such as criterion validity, responsiveness, and interpretability, as well as greater application of advanced psychometric methods such as Item Response Theory and Computerized Adaptive Testing. Furthermore, increased focus on cross-cultural validation and measurement invariance testing will enhance our ability to compare SRH outcomes across diverse populations and settings.
Conducting Exploratory and Confirmatory Factor Analyses
Factor analysis is a family of multivariate statistical techniques essential for developing and validating questionnaires in reproductive health research. These methods help researchers identify the underlying constructs (latent variables) that give rise to observed responses on questionnaires and ensure these instruments measure what they intend to measure accurately and reliably [33]. In the context of reproductive health behavior questionnaire development, factor analysis serves critical functions including theory development, psychometric instrument validation, and data reduction to identify core constructs from numerous potential items [33].
The two main approaches—Exploratory Factor Analysis (EFA) and Confirmatory Factor Analysis (CFA)—serve complementary purposes in the questionnaire development process. EFA is typically employed in early stages when researchers lack a well-defined expectation about the underlying structure of a reproductive health construct, allowing the data to reveal the number and nature of latent factors [34] [35]. In contrast, CFA is used when researchers have a theoretically-grounded prediction about the number of specific factors and which questionnaire items are influenced by which factors, enabling statistical testing of how well a pre-specified model fits the collected data [34]. A promising integrated approach, Exploratory Structural Equation Modeling (ESEM), has recently emerged, incorporating the best elements of both EFA and CFA to overcome limitations of traditional methods [36] [37].
Theoretical Foundations and Key Concepts
Fundamental Principles
Factor analysis operates on the premise that measured variables (questionnaire items) are influenced by latent constructs that cannot be directly observed [33]. In reproductive health research, these might include constructs such as "contraceptive self-efficacy," "reproductive health knowledge," or "pregnancy intentions." The covariance between observed variables is explained by their common relationships with these underlying factors [33]. The factor analysis model partitions the variance of each observed variable into common variance (shared with other variables through common factors), specific variance (unique to the variable but reliable), and error variance (random measurement error) [33].
Key terminology essential for understanding factor analysis includes: latent variables (unobserved constructs inferred from measured variables), observed variables (directly measured items or indicators), factor loadings (strength of relationship between observed variables and latent factors), eigenvalues (amount of variance explained by each factor), and communality (proportion of a variable's variance explained by the common factors) [33]. Understanding these concepts is fundamental to appropriately applying factor analysis techniques in reproductive health questionnaire development.
Comparison of Factor Analysis Approaches
Table 1: Key Characteristics of Factor Analysis Approaches
| Feature | Exploratory Factor Analysis (EFA) | Confirmatory Factor Analysis (CFA) | Exploratory Structural Equation Modeling (ESEM) |
|---|---|---|---|
| Primary Purpose | Explore underlying structure without strong prior hypotheses | Test theoretically-derived factor structures | Combine exploratory and confirmatory approaches |
| Factor Loading Patterns | Cross-loadings permitted | Cross-loadings constrained to zero | Targeted cross-loadings permitted |
| Theoretical Basis | Data-driven | Theory-driven | Integrates theory with data exploration |
| Model Specifications | Minimal a priori specifications | Strong a priori specifications | Flexible specifications with some constraints |
| Typical Application Stage | Early instrument development | Advanced validation | Comprehensive validation across groups/cultures |
Methodological Protocols
Study Design and Sample Considerations
Appropriate study design is crucial for valid factor analysis in reproductive health research. Sample size requirements vary by method, with general guidelines suggesting at least 20 observations per variable, though larger samples increase stability of parameter estimates [33]. For the Surveys of Women reproductive health study, a target of 2000 completed surveys per state was established to ensure adequate power for complex analyses [19]. Sampling methods should ensure representation of the target population; address-based sampling enhanced with age-targeted lists was employed in the Surveys of Women to maximize coverage of women aged 18-44 years [19].
Data collection protocols must account for the specific requirements of reproductive health research. The Surveys of Women implemented a multimode design (web survey and hard copy questionnaire) with rigorous scheduling of various prompts to maximize response rates [19]. All materials should undergo ethical review, with informed consent procedures that clearly explain the voluntary nature of participation, confidentiality protections, and potential risks specific to reproductive health topics [19].
Protocol for Exploratory Factor Analysis
Step 1: Preparation and Assumptions Checking
Begin by examining the correlation matrix to assess factorability of the data. Compute the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy (values >0.8 are desirable) and Bartlett's test of sphericity (should be significant) to determine if variables share common variance sufficient for factor analysis [5]. Check assumptions of linearity, normality, and absence of influential outliers that might distort results [33].
Step 2: Factor Extraction
Select an appropriate extraction method. Principal axis factoring or maximum likelihood estimation are recommended for common factor analysis in reproductive health research, as they distinguish between common and unique variance [35]. Avoid principal components analysis unless the goal is purely data reduction rather than identifying latent constructs [34]. Determine the number of factors to retain using multiple criteria: eigenvalues greater than 1, scree plot inspection, and parallel analysis [5] [34].
Step 3: Factor Rotation and Interpretation
Apply rotation to achieve a simpler, more interpretable structure. Orthogonal rotation (varimax) is appropriate when factors are theoretically independent, while oblique rotation (promax, oblimin) is more realistic for reproductive health constructs that are likely correlated [35]. Interpret the pattern matrix, considering loadings above 0.3 as meaningful, though higher thresholds (e.g., 0.4 or 0.5) may enhance interpretability [5]. Label factors based on the conceptual themes of items with strong loadings.
Step 4: Refinement and Score Calculation
Refine the factor solution by considering removing items with weak loadings (<0.3) or complex cross-loadings (loading highly on multiple factors with similar magnitude). Calculate factor scores for use in subsequent analyses, noting the various methods available (e.g., regression, Bartlett, Anderson-Rubin) and their different properties [35].
Protocol for Confirmatory Factor Analysis
Step 1: Model Specification
Based on theoretical foundations and/or prior EFA results, specify the hypothesized factor model. This includes defining which observed variables (questionnaire items) load on which latent constructs, and determining whether factors will be correlated or uncorrelated. For example, in developing the Women Shift Workers' Reproductive Health Questionnaire, a five-factor model (motherhood, general health, sexual relationships, menstruation, and delivery) was specified based on prior qualitative and quantitative work [5].
Step 2: Model Identification
Ensure the model is statistically identified by having sufficient degrees of freedom. This typically requires setting the metric of latent variables by either fixing one factor loading per factor to 1 or fixing the factor variance to 1 [38]. For a one-factor model with n indicators, the number of known parameters (variances and covariances) must exceed the number of parameters to be estimated.
Step 3: Model Estimation
Select an appropriate estimation method based on data characteristics. Maximum likelihood is most common for continuous normally distributed data, while weighted least squares or robust diagonally weighted least squares are preferable for categorical or non-normal data [39]. For reproductive health measures often using Likert-type scales, the latter methods may be more appropriate.
Step 4: Model Evaluation
Assess model fit using multiple indices: Chi-square statistic (non-significant values indicate good fit, but sensitive to sample size), RMSEA (values <0.08 acceptable, <0.05 good), CFI and TLI (values >0.90 acceptable, >0.95 good), and SRMR (values <0.08 good) [38] [5]. For the Women Shift Workers' Reproductive Health Questionnaire, CFI, GFI, AGFI, NFI, and PNFI indices all confirmed adequate fit for the five-factor model [5].
Step 5: Model Modification
If initial model fit is inadequate, consider theoretically-justified modifications such as allowing correlated residuals between items with similar content or wording. Use modification indices cautiously to avoid capitalizing on chance characteristics of the sample. Cross-validate any modifications in a new sample when possible.
Advanced Integrative Approaches
Exploratory Structural Equation Modeling (ESEM)
ESEM represents an integrative approach that incorporates the best elements of both EFA and CFA [36] [37]. Unlike traditional CFA that constrains all cross-loadings to zero, ESEM allows targeted cross-loadings, which is particularly valuable for reproductive health constructs that often have conceptual overlap [36]. ESEM is especially useful for establishing measurement invariance across cultural groups, as demonstrated with the Mental Health Continuum-Short Form where psychological and social well-being factors were more closely related in collectivistic cultures [36] [37].
The ESEM framework involves specifying a measurement model with cross-loadings estimated rather than constrained, followed by structural relationships between factors. This approach can be implemented using specialized syntax generators for programs like Mplus, making it more accessible to researchers [36].
Data Analysis and Interpretation
Quantitative Guidelines for Interpretation
Table 2: Key Metrics for Evaluating Factor Analysis Results
| Metric | Threshold for Adequacy | Interpretation |
|---|---|---|
| Kaiser-Meyer-Olkin (KMO) | >0.8 desirable | Measures sampling adequacy; higher values indicate better factorability |
| Bartlett's Test of Sphericity | p<0.05 | Indicates whether correlation matrix is factorable |
| Factor Loadings | >0.3 minimal, >0.4 fair, >0.5 good | Strength of relationship between item and factor |
| Communalities | >0.4 | Proportion of item variance explained by factors |
| Eigenvalues | >1.0 (Kaiser criterion) | Amount of variance explained by each factor |
| Cronbach's Alpha | >0.7 | Internal consistency reliability |
| Average Variance Extracted (AVE) | >0.5 | Convergent validity |
| RMSEA | <0.08 acceptable, <0.05 good | Model fit in CFA |
| CFI/TLI | >0.90 acceptable, >0.95 good | Comparative model fit |
Workflow Visualization
Research Reagent Solutions
Table 3: Essential Tools for Factor Analysis in Reproductive Health Research
| Tool Category | Specific Solutions | Application in Reproductive Health Research |
|---|---|---|
| Statistical Software | Mplus, R (psych, lavaan packages), SPSS, FACTOR, Jamovi | Implementation of EFA, CFA, and ESEM models; Mplus is particularly strong for categorical data common in reproductive health questionnaires [36] [34] [39] |
| Syntax Generators | De Beer and Van Zyl ESEM Syntax Generator | Simplifies complex ESEM model specification in Mplus for reproductive health instrument validation [36] |
| Data Collection Platforms | Web surveys, ABS multimode approaches | Address-based sampling with multimodal design (web + mail) as used in Surveys of Women improves coverage and response rates [19] |
| Reliability Assessment Tools | Cronbach's alpha, composite reliability, test-retest | Essential for establishing internal consistency and stability of reproductive health constructs; composite reliability >0.7 recommended [5] |
| Validity Assessment Tools | AVE, MSV, HTMT, multi-group invariance testing | Critical for establishing convergent, discriminant, and cross-group validity of reproductive health measures across diverse populations [5] |
Application to Reproductive Health Behavior Questionnaire Development
The development of the Women Shift Workers' Reproductive Health Questionnaire (WSW-RHQ) exemplifies the rigorous application of factor analysis protocols in reproductive health research [5]. The sequential mixed-methods approach began with qualitative item generation through interviews with 21 women shift workers, followed by systematic psychometric evaluation [5]. The process reduced an initial pool of 88 items to a final 34-item instrument across five factors: motherhood, general health, sexual relationships, menstruation, and delivery [5].
Factor analysis in reproductive health research requires special consideration of cultural appropriateness and contextual relevance of constructs. As demonstrated in validation of the Mental Health Continuum-Short Form across cultures, factor structures may vary significantly between populations, necessitating careful examination of measurement invariance [36] [37]. For reproductive health behaviors, this is particularly important as constructs like sexual relationships, motherhood, and reproductive decision-making may manifest differently across cultural contexts.
The integration of ESEM approaches offers particular promise for reproductive health questionnaire development, as it accommodates the complex nature of psychological and health constructs that often include meaningful cross-loadings not captured by traditional CFA [36] [37]. This flexibility enables more accurate modeling of the "dynamic interactions" between related reproductive health constructs that may be theoretically distinct but empirically related in specific populations.
Application Notes: Core Principles for Scale Refinement
The refinement of a scale through item reduction and subscale formation is a critical psychometric process that enhances the feasibility, reliability, and validity of a research instrument. In the context of reproductive health behavior questionnaire development, this process ensures that the final tool efficiently captures the essential latent constructs—such as knowledge, attitudes, and practices regarding endocrine-disrupting chemicals (EDCs) or contraceptive care—without unnecessary respondent burden [8] [40].
Key Objectives of Scale Refinement:
- Reduce Participant Burden: Shorter questionnaires are associated with higher response rates and less random error caused by fatigue or lack of motivation [41].
- Improve Reliability: Removing redundant or poorly performing items increases the internal consistency of the scale, as measured by metrics like Cronbach's alpha [42].
- Enhance Validity: The process helps confirm that the remaining items accurately measure the intended theoretical constructs, such as health behaviors through food, respiration, and skin absorption in EDC research [8].
- Identify Underlying Structure: Exploratory Factor Analysis (EFA) is central to uncovering the latent subscales (factors) that exist within a larger pool of items, grouping questions that tap into the same underlying dimension of reproductive health [8] [43].
Experimental Protocols for Item Reduction and Subscale Formation
The following protocols provide a detailed, sequential methodology for refining a reproductive health behavior questionnaire.
Protocol 1: Sequential Mixed-Methods Design for Comprehensive Scale Development
This protocol outlines the overarching framework, integrating qualitative and quantitative phases to ensure the item pool is both comprehensive and psychometrically sound [22].
Protocol 2: Statistical Validation Workflow for Item Reduction
This protocol details the quantitative steps for analyzing data collected from a large-scale survey to statistically identify the best-performing items and the underlying factor structure [8] [42].
Data Presentation: Quantitative Metrics for Item Evaluation
The following tables summarize the key quantitative criteria and benchmarks used to make decisions about item retention or removal during the statistical validation protocol.
Table 1: Key Statistical Criteria for Item Reduction Decisions
| Method | Key Metric | Acceptance Threshold | Rationale for Removal |
|---|---|---|---|
| Item Analysis | Item-Total Correlation | ≥ 0.30 - 0.50 [42] | Item does not correlate well with the overall scale score. |
| Skewness & Kurtosis | Within ±2 [8] | Indicates severe deviation from normal distribution. | |
| Internal Reliability | Change in Cronbach's Alpha if Item Deleted | Alpha decreases or remains stable [42] | Removal of the item increases the scale's internal consistency. |
| Content Validity | Content Validity Index (CVI) | I-CVI ≥ 0.78 [43] | Experts rate the item as not essential or not representative. |
| Factor Analysis | Factor Loading | ≥ 0.40 - 0.50 [8] | Item has a weak association with the underlying factor. |
| Communality | ≥ 0.40 [8] | The factor explains a low amount of the item's variance. | |
| Cross-loading | Loads ≥ 0.40 on multiple factors [43] | Item is ambiguous and does not cleanly measure a single construct. |
Table 2: Comparative Results of Item Reduction Methods from a Lifestyle Questionnaire Study
| Question Frequency | Variance Inflation Factor (VIF) Results | Factor Analysis (FA) Results | Conclusion |
|---|---|---|---|
| Daily Questions | Suggested larger item reduction. | Suggested more conservative item reduction. | VIF was more aggressive than FA for daily items. |
| Weekly Questions | Suggested fewer reductions. | Suggested more reductions. | FA identified more redundancies than VIF for weekly items. |
| Monthly Questions | Identified redundancies in stress-related items. | Identified redundancies in stress-related items. | Both methods converged on the same construct (stress) for monthly items. |
| Overall Implication | Using multiple statistical methods for item reduction is critical, as results can vary [41]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Software for Questionnaire Development and Validation
| Item / Solution | Function / Application in Protocol |
|---|---|
| Statistical Software (IBM SPSS Statistics with AMOS module, R, Python) | Performs all statistical analyses, including descriptive statistics, reliability analysis, Exploratory Factor Analysis (EFA), and Confirmatory Factor Analysis (CFA) [8] [41]. |
| Expert Panel (5-15 members) | Provides qualitative and quantitative assessment of content validity (CVI). Panel should include methodologies, content experts, and end-user representatives [43]. |
| Target Population Participants (Pilot Group, n=10-30) | Engages in cognitive debriefing during pilot testing to identify ambiguous items, difficult wording, and feasibility issues [8] [44]. |
| Digital Survey Platform (Qualtrics, REDCap) | Administers the final survey for large-scale data collection, ensures data integrity, and facilitates data export to statistical software [45]. |
| Data Visualization Software (Tableau, Graphviz) | Creates artistic representations of data findings and generates workflow diagrams for research protocols, aiding in the distillation and presentation of results [46]. |
Applying Frameworks like the Multiphase Optimization Strategy (MOST)
The Multiphase Optimization Strategy (MOST) is an innovative framework for developing and optimizing behavioral interventions, drawing heavily from principles in engineering, statistics, and behavioral science [47] [48]. Unlike traditional randomized controlled trials (RCTs) that evaluate interventions as bundled packages, MOST employs a systematic process to empirically identify which individual components contribute meaningfully to desired outcomes [48] [49]. This approach is particularly valuable for complex interventions consisting of multiple components that can be delivered simultaneously, sequentially, or through various methods [47]. The framework is conceived as an alternative to the conventional cycle of intervention development, which typically involves constructing an intervention a priori, evaluating it in an RCT, conducting post-hoc analyses to inform revisions, and then testing again in a new RCT—a process that often leads slowly, if at all, to an optimized intervention [48].
MOST is especially relevant for developing and optimizing reproductive health behavior questionnaires and interventions, where understanding the active components and their optimal delivery is crucial for effectiveness and scalability [47] [49]. The framework follows a resource management principle, advocating for careful management of research resources to yield maximal information from a given experimental design [50]. This makes MOST particularly suitable for research areas like reproductive health, where resources may be limited and the need for efficient, evidence-based tools is high [5] [2].
Core Principles and Phases of MOST
The MOST framework consists of three distinct phases: Preparation, Optimization, and Evaluation [47] [48]. Each phase addresses specific questions about the intervention and employs rigorous methodologies, including randomized experimentation, to build a cumulative evidence base for intervention optimization.
The Three Phases of MOST
Table 1: The Three Phases of the Multiphase Optimization Strategy
| Phase | Primary Objective | Key Activities | Outcomes |
|---|---|---|---|
| Preparation | Develop conceptual foundation and identify candidate components | Develop conceptual model; pilot test; identify core components; determine optimization criteria | Conceptual model; pilot-tested components; specification of optimization criteria (e.g., effectiveness, efficiency, cost) |
| Optimization | Test individual components and identify optimal combination | Randomized factorial experiment of specific components; assess performance against pre-specified criteria | Empirical data on component performance; identification of active/inactive components; optimized "final draft" intervention |
| Evaluation | Validate the optimized intervention package | Standard RCT comparing optimized intervention against suitable control | Evidence of efficacy for the optimized intervention package; preparation for implementation |
The Preparation Phase involves establishing a conceptual model for the intervention, conducting pilot testing, identifying potential core components, and determining what outcomes should be optimized (e.g., effectiveness, efficiency, cost) [47] [48]. In reproductive health behavior questionnaire development, this might include qualitative exploration of the construct, literature review, and initial item generation [5] [2].
The Optimization Phase uses efficient experimental designs, particularly factorial designs, to test the performance of individual intervention components [47]. This phase addresses critical questions about which components are active and should be retained, which are inactive and should be discarded, and what are the optimal doses of the active components [48]. For questionnaire development, this could involve testing different formatting, wording, or scaling options to maximize psychometric properties.
The Confirming Phase (also called Evaluation Phase) consists of a standard RCT to evaluate the optimized intervention package developed in the previous phases [47] [48]. This phase answers questions about whether the optimized intervention, as a complete package, is efficacious and whether its effects are substantial enough to warrant implementation [48].
MOST Workflow Diagram
Graphical Representation of the MOST Framework
Application of MOST in Reproductive Health Questionnaire Development
The development of reproductive health behavior questionnaires represents a promising application for the MOST framework, particularly through sequential exploratory mixed-methods designs [5] [2]. These designs typically involve an initial qualitative phase for item generation followed by a quantitative phase for psychometric evaluation, aligning well with the phased approach of MOST.
Integrating MOST with Mixed-Methods Questionnaire Development
Table 2: Application of MOST to Reproductive Health Questionnaire Development
| MOST Phase | Mixed-Methods Research Component | Specific Activities in Reproductive Health Context |
|---|---|---|
| Preparation | Qualitative Phase | In-depth interviews with target population; literature review; conceptual analysis; initial item pool generation |
| Optimization | Quantitative Phase - Psychometric Evaluation | Face, content, and construct validity assessment; reliability testing; factor analysis; item reduction |
| Evaluation | Final Validation | Confirmatory factor analysis; criterion validity assessment; test-retest reliability; establishment of scoring norms |
In the context of reproductive health behavior questionnaire development, the Preparation Phase would involve exploring the concept of reproductive health behavior through qualitative methods such as interviews with the target population [2]. For instance, a study developing a women's shift workers' reproductive health questionnaire conducted 21 interviews with women shift workers to explore dimensions of reproductive health affected by shift work [5]. Similarly, a protocol for developing a male reproductive health behavior questionnaire includes a qualitative study with a contractual content analysis approach to understand men's perceptions of reproductive health-related behavior [2].
The Optimization Phase in questionnaire development focuses on psychometric evaluation, assessing face validity, content validity, construct validity, and reliability [5]. This phase employs quantitative methods to refine and optimize the questionnaire. For example, in the women shift workers' reproductive health questionnaire study, researchers used both exploratory and confirmatory factor analyses with 620 participants to identify a five-factor structure with 34 items, explaining 56.50% of the total variance [5].
The Evaluation Phase involves final validation of the optimized questionnaire, establishing its psychometric properties across different populations and contexts [5] [2]. This might include multi-site studies to establish population norms and demonstrate the questionnaire's utility in clinical or public health settings.
Questionnaire Development Workflow
Questionnaire Development within MOST Framework
Experimental Protocols for MOST Implementation
Factorial Designs in Optimization Trials
Factorial designs are the cornerstone of the Optimization Phase in MOST, allowing researchers to efficiently test multiple intervention components simultaneously [47] [48]. In a factorial design, several independent variables (factors) are investigated at once, with each level of every variable combined with each level of all other variables [48]. This design enables isolation of the effects of individual components and their interactions.
For example, in a study applying MOST to Family Navigation (FN) for child behavioral health services, researchers employed a 2×2×2×2 factorial design to test four different FN delivery strategies simultaneously [47]. This created 16 experimental conditions ranging from the most basic (core FN) to the most intensive combination of all enhanced strategies [47]. Similarly, a protocol for adapting Cognitive Processing Therapy (CPT) for PTSD using MOST describes a 16-condition fractional factorial experiment to test the effectiveness of five CPT components and their two-way interactions [50].
Sample Size Considerations
The sample size for optimization trials depends on the specific experimental design and the effects of interest. The Family Navigation study planned to enroll 304 children and their families randomized to one of 16 possible combinations of FN delivery strategies [47]. The CPT adaptation study plans to enroll 270 veterans across 16 experimental conditions [50]. For questionnaire development, the women shift workers' reproductive health questionnaire study recruited 620 participants for factor analysis [5], following the rule of thumb of at least 300 participants for factor analysis [5].
Data Collection and Analysis
Data collection in MOST studies typically includes both outcome measures and implementation data. The Family Navigation study collects data on the primary outcome (achieving family-centered behavioral health goals) as well as implementation outcomes including fidelity, acceptability, feasibility, and cost [47]. Similarly, in questionnaire development, researchers collect data on multiple psychometric properties including face validity, content validity, construct validity, and reliability [5] [2].
Analysis approaches include analysis of variance (ANOVA) for factorial experiments [48] and factor analysis for questionnaire development [5]. In the Optimization Phase, decisions about which components to retain are based on the main effect and interaction estimates obtained from the ANOVA, using criteria such as statistical significance, effect size thresholds, or cost-effectiveness considerations [48].
Research Reagent Solutions for MOST Implementation
Table 3: Essential Research Reagents for Implementing MOST in Reproductive Health Research
| Research Reagent | Function in MOST Application | Specific Examples in Reproductive Health |
|---|---|---|
| Validated Screening Instruments | Detection of at-risk populations for intervention targeting | Preschool Pediatric Symptom Checklist (PPSC), Pediatric Symptom Checklist-17 (PSC-17) [47] |
| Qualitative Interview Guides | Exploration of construct dimensions and item generation in Preparation Phase | Semi-structured interviews on reproductive health perceptions [5] [2] |
| Psychometric Evaluation Tools | Assessment of validity and reliability in Optimization Phase | Content Validity Index (CVI), Content Validity Ratio (CVR), Factor Analysis [5] |
| Factorial Experimental Designs | Efficient testing of multiple intervention components | 2×2×2×2 factorial design for FN delivery strategies [47] |
| Outcome Measurement Tools | Assessment of primary and secondary outcomes in Evaluation Phase | Clinical outcome measures, implementation outcomes (fidelity, acceptability, feasibility) [47] |
Case Study: Application to Reproductive Health Behavior Questionnaire Development
A specific application of MOST in reproductive health behavior questionnaire development can be illustrated through a hypothetical study based on existing protocols [5] [2]. The study would aim to develop an optimized questionnaire for assessing reproductive health behaviors in a specific population (e.g., male reproductive health or women shift workers).
In the Preparation Phase, researchers would conduct in-depth interviews with the target population to explore perceptions and experiences related to reproductive health behaviors [2]. For instance, in developing a male reproductive health behavior questionnaire, researchers would conduct semi-structured interviews with men to understand their perceptions of reproductive health-related behavior, including knowledge, attitudes, and practices [2]. This qualitative exploration would be supplemented by a comprehensive literature review to identify existing measures and theoretical frameworks.
The Optimization Phase would involve developing an initial item pool based on the qualitative findings and literature review, followed by systematic psychometric evaluation [5]. This would include face validity assessment through cognitive interviewing with target population members, content validity assessment through expert panels (calculating CVI and CVR), and construct validity assessment through factor analysis [5]. The optimization might also involve testing different response formats, question orderings, or scaling options using factorial experiments to determine the optimal configuration for maximizing reliability and validity.
The Evaluation Phase would involve a final validation study with a larger sample to establish the questionnaire's psychometric properties, including test-retest reliability, convergent and discriminant validity, and criterion validity [5] [2]. The optimized questionnaire would then be ready for implementation in clinical or public health settings to assess reproductive health behaviors and evaluate interventions.
This systematic approach to questionnaire development, guided by the MOST framework, ensures the resulting instrument is not only theoretically grounded but empirically optimized for its intended purpose and population.
Navigating Challenges and Enhancing Questionnaire Efficacy
Addressing Common Pitfalls in Item Wording and Scaling
Within the specialized field of reproductive health behavior research, the validity and reliability of collected data fundamentally depend on the precision of survey instruments. Questionnaire development protocols require meticulous attention to item construction and scaling techniques, as even minor wording or formatting flaws can systematically skew data, potentially compromising research conclusions and subsequent intervention strategies [51] [52]. For researchers and drug development professionals, understanding these pitfalls is not merely methodological but ethical, ensuring that findings accurately reflect the reproductive health behaviors, attitudes, and needs of the populations studied. This document outlines common pitfalls and provides standardized protocols to enhance the rigor of reproductive health questionnaire development.
A Systematic Catalog of Item Wording Pitfalls and Solutions
The language used in survey items can significantly influence participant responses. The table below summarizes common wording biases, their impact on data quality, and corrective strategies, with particular attention to reproductive health contexts.
Table 1: Common Item Wording Pitfalls and Corrective Strategies
| Pitfall Type | Description & Example | Impact on Data | Corrective Strategy |
|---|---|---|---|
| Leading Questions [53] [51] | Phrasing that suggests a desired answer. Example:"Do you agree that the new reproductive health service, which provides vital care to underserved women, is effective?" | Skews responses toward agreement, inflating positive perceptions. | Use neutral language.Improved: "How effective or ineffective do you find the new reproductive health service?" |
| Double-Barreled Items [51] | A single question addressing two distinct concepts.Example:"Do you find the clinic staff to be knowledgeable and courteous?" | Ambiguous responses; cannot discern if the respondent agrees with one, both, or neither concept. | Split into separate items.Improved: "How knowledgeable is the clinic staff?" and "How courteous is the clinic staff?" |
| Technical Jargon [51] | Using specialized terms not universally understood.Example:"What was your age at menarche?" | Confusion and inaccurate responses from participants unfamiliar with the term. | Use common, accessible language.Improved: "How old were you when you had your first menstrual period?" |
| Ambiguous Questions [51] | Wording that can be interpreted in multiple ways.Example:"Do you regularly get checked?" | Varying interpretations of "regularly" and "checked" lead to non-comparable data. | Define terms precisely.Improved: "In the past 12 months, how many times have you had a gynecological examination?" |
| Vague Quantifiers [52] | Using unanchored, subjective terms.Example:Response scale: "Never, Sometimes, Often, Always" | Words like "sometimes" mean different things to different people, creating noise in the data. | Use specific behavioral frequencies or fully labeled scales.Improved: "Never, Once a month or less, 2-3 times a month, Once a week or more" |
Experimental Protocol: Qualitative Validation for Item Wording
Objective: To identify and rectify ambiguous, leading, or unclear item wordings in a draft reproductive health questionnaire before quantitative pilot testing [13] [54].
Methodology:
- Participant Recruitment: Recruit 10-15 participants from the target population (e.g., female adolescents, women living with HIV) using purposive sampling [13] [14].
- Cognitive Interviewing: Conduct one-on-one sessions where participants are presented with the draft questionnaire. Employ the "think-aloud" technique, prompting them to verbalize their thought process as they interpret each question and decide on an answer [55].
- Probing: Follow up with specific probes to uncover hidden interpretations (e.g., "What does the word 'regularly' mean to you in this context?" or "Can you paraphrase that question in your own words?") [54].
- Expert Panel Review: Convene a panel of 8-12 experts in health education, reproductive health, and psychometrics [13] [14]. They will quantitatively assess each item using:
- Content Validity Ratio (CVR): Rates the essentiality of each item on a 3-point scale. Items scoring below a threshold (e.g., 0.54 for 10 experts) are removed [13].
- Content Validity Index (CVI): Rates items on relevance, clarity, and simplicity on a 4-point scale. Items with a CVI ≥ 0.79 are retained [13] [14].
Deliverable: A revised questionnaire with item wording refined based on participant comprehension and expert validation.
Figure 1: Workflow for the qualitative validation of item wording, integrating feedback from both target populations and expert panels.
Optimizing Scale and Response Option Design
The design of response scales is as critical as item wording. Poorly constructed scales can introduce measurement error by failing to align with respondents' cognitive processes [52].
Table 2: Guidelines for Selecting and Designing Response Scales
| Scale Aspect | Pitfall | Evidence-Based Best Practice | Application in Reproductive Health |
|---|---|---|---|
| Number of Points | Using too few (loses nuance) or too many (increases cognitive load) points [52]. | 5-point scales offer a good balance for satisfaction/frequency [52].7-point scales are superior for capturing attitudinal intensity [52]. | Use a 5-point scale from "Never" to "Always" for frequency of contraceptive use. |
| Labeling | Using only endpoint labels or vague quantifiers (e.g., "Sometimes") [52]. | Fully label all scale points to ensure consistent interpretation [52]. | For a stress scale: "Not at all stressed," "Slightly stressed," "Moderately stressed," "Very stressed," "Extremely stressed." |
| Acquiescence Bias | Using only positively framed statements, leading to agreement bias [56]. | Balance item valence by including both positively and negatively worded statements [56]. | Instead of only "I feel confident managing my reproductive health," add "I often feel unsure about how to manage my reproductive health." (Reverse-scored) |
| Forced Choice | Not providing a "Not Applicable" or "Don't Know" option [51]. | Include explicit escape options to prevent forced, inaccurate responses [51]. | A question about "partner's attitude" should include "Not Applicable" for respondents without a partner. |
Experimental Protocol: Psychometric Evaluation of Scales
Objective: To establish the construct validity and reliability of the scaled questionnaire within a specific reproductive health population [13] [14] [57].
Methodology:
- Pilot Testing & Sampling: Administer the refined questionnaire to a large, representative sample of the target population. A common rule of thumb is 10-20 participants per item (e.g., n=289 for a 28-item scale) [13] [57].
- Construct Validity - Exploratory Factor Analysis (EFA):
- Assess sampling adequacy using the Kaiser-Meyer-Olkin (KMO) index (should be >0.6) and Bartlett's Test of Sphericity (should be significant, p<.05) [13] [14].
- Use principal component analysis with Varimax rotation to identify latent factor structures.
- Retain factors with eigenvalues >1 and items with factor loadings ≥ 0.3-0.4 on their primary factor [13] [14].
- Reliability Analysis:
- Internal Consistency: Calculate Cronbach's alpha coefficient for the entire scale and its subscales. A value of α ≥ 0.70 is generally considered acceptable, with α ≥ 0.90 indicating excellent consistency for high-stakes decisions [13] [14].
- Test-Retest Reliability: Administer the same questionnaire to a sub-sample (e.g., n=45) after a 2-week interval. Calculate the Intra-class Correlation Coefficient (ICC); values above 0.7 indicate good stability [13] [14].
Deliverable: A psychometrically robust scale with demonstrated factorial structure, internal consistency, and temporal stability for use in reproductive health research.
Figure 2: Workflow for the quantitative psychometric evaluation of a scale, establishing its construct validity and reliability.
The Scientist's Toolkit: Essential Reagents for Questionnaire Development
The following table details key methodological "reagents" required for rigorous scale development in reproductive health research.
Table 3: Essential Reagents for Reproductive Health Questionnaire Development
| Research Reagent | Function and Specification | Application Example |
|---|---|---|
| Target Population Sample | Participants who represent the demographic and clinical characteristics of the group under study. Requires careful sampling (random, cluster) and power calculation [13] [14]. | Recruiting 289 female students aged 12-15 via multi-stage random cluster sampling in schools to validate an adolescent reproductive health scale [13]. |
| Expert Panel | A multidisciplinary group (8-12 members) including specialists in reproductive health, psychometrics, and qualitative methods to assess content validity [13] [14]. | Panelists rate each item's relevance (CVI) and essentiality (CVR) to ensure the scale adequately covers reproductive health constructs like knowledge, attitude, and behavior [13]. |
| Validated Gold-Standard Measures | Existing scales with established psychometric properties used for testing convergent validity [57]. | Correlating scores on a new "Reproductive Health Self-Efficacy" scale with an existing, validated general self-efficacy scale to demonstrate convergent validity. |
| Statistical Software Packages | Tools for conducting advanced psychometric analyses (EFA, CFA, Reliability Analysis). | Using SPSS with the AMOS plugin or R with the psych and lavaan packages to perform factor analysis and calculate Cronbach's alpha [13]. |
| Pilot Testing Protocol | A structured procedure for administering the draft questionnaire to a small sample to identify logistical problems, timing, and general participant reaction before full-scale deployment [52] [55]. | Conducting a pilot with 30-50 HIV-positive women to ensure questions about sexual behavior are understood and not overly distressing, refining the protocol accordingly [14]. |
Adherence to rigorous protocols for item wording and scale design is non-negotiable in reproductive health behavior research. By systematically addressing common pitfalls through qualitative pre-testing, quantitative psychometric validation, and the application of evidence-based scaling guidelines, researchers can produce data of the highest quality. This methodological rigor ensures that subsequent analyses, intervention designs, and policy recommendations are built upon a foundation of valid and reliable measurement, ultimately contributing to more effective outcomes in reproductive health.
Utilizing Cognitive Interviews to Improve Comprehension
Within the framework of reproductive health behavior questionnaire development, ensuring that respondents accurately comprehend and interpret survey questions is paramount for data validity. Cognitive interviewing is a qualitative, participant-centered method specifically designed to identify and rectify potential problems in survey instruments by understanding the cognitive processes respondents use to answer questions [58] [59]. In sensitive fields like reproductive health, where terminology and concepts can be misunderstood, stigmatized, or vary culturally, this method is indispensable for developing protocols that yield reliable and comparable data across diverse populations [59] [60]. This document provides detailed application notes and experimental protocols for integrating cognitive interviews into reproductive health research, supporting a broader thesis on robust questionnaire development.
Theoretical Foundations and Key Concepts
Cognitive interviewing is grounded in cognitive theory, which breaks down the survey response process into several stages. The methodology assesses three key components derived from Tourangeau's model: comprehension, relevance, and acceptability [58].
- Comprehension: This measures whether the respondent understands both the intent of the question and the specific meaning of the words and phrases used. It probes the respondent's ability to use the provided information to answer questions correctly [58].
- Relevance (Response Mapping): This assesses whether the respondent finds the information personally applicable and useful for their own situation and decision-making [58].
- Acceptability (Sensitivity): This evaluates whether the information or questions seem truthful, credible, and inoffensive to the respondent, which is crucial for topics that may be stigmatized [58].
The ultimate goal is to refine the survey instrument so that its language is clear, it addresses the informational needs of the target audience, and it minimizes measurement error [58] [59].
Experimental Protocol: A Step-by-Step Guide
This protocol is adapted from established methods used in sexual and reproductive health research [58] [59] [60].
Pre-Interview Phase: Preparation and Localization
- Define Objectives and Recruit Participants: Clearly articulate the aspects of the questionnaire to be evaluated. Use purposive sampling to recruit participants who represent the diversity of the target population in terms of key characteristics such as age, race/ethnicity, socioeconomic status, reproductive history, and health literacy [58]. For a global instrument, aim for participants from a variety of geographic and cultural settings [59].
- Localize the Instrument: Translate the core questionnaire from the source language into the target language using forward- and back-translation processes. This ensures conceptual equivalence, not just literal translation [59].
- Develop the Interview Protocol: Create a semi-structured interview guide that includes:
- A "think-aloud" section where participants verbalize their thoughts as they read and answer each survey question [58] [61].
- Scripted probing questions to explore cognitive processes further after the think-aloud exercise. Probes should target comprehension (e.g., "What does the term 'contraceptive effectiveness' mean to you in your own words?"), recall ("How did you remember the number of sexual partners you've had?"), and sensitivity ("How did you feel about answering that question?") [58] [60].
Interview Phase: Execution and Data Collection
- Conduct the Interviews: Interviews are typically conducted in person or via secure virtual methods. The process involves:
- Obtaining Informed Consent: Explain the study purpose and procedures, emphasizing that the survey itself is being tested, not the participant.
- Think-Aloud Practice: Give participants a simple practice task to familiarize them with the think-aloud technique.
- Administer the Questionnaire: Present the survey instrument. For comparative designs (e.g., testing a new patient-centered tool against an existing one), present materials in alternating order to control for bias [58].
- Employ Probing Techniques: Use concurrent probing (during the survey) and/or retrospective debriefing (after the survey) to delve deeper into the participant's thought process [58] [62]. Techniques from "The Scientist's Toolkit" (see Section 6) can be applied here.
- Audio-Record and Transcribe: Record the interviews with permission and have them transcribed verbatim for rigorous analysis. For multi-country studies, transcripts should be translated into a common language for cross-site analysis [61] [59].
Post-Interview Phase: Analysis and Iteration
- Code the Transcripts: Use a pre-developed coding framework based on the key measures: comprehension, relevance, acceptability, and design [58]. Employ qualitative data analysis software (e.g., NVivo, Dedoose) to manage the data.
- Analyze for Patterns and Issues: Identify recurring problems, misunderstandings, or suggestions for improvement. Create an overview report documenting each issue, the number of participants who mentioned it, and direct quotes [58].
- Revise the Instrument: Use the analysis to make informed revisions to the questionnaire. This may involve rephrasing questions, changing the order, modifying response options, or altering the design layout.
- Iterate until Saturation: Conduct multiple rounds (or "waves") of interviews. After each round, revise the instrument. The process stops when a new round of interviews produces no new substantive issues warranting modification—a state known as saturation [58] [59]. A typical workflow is visualized below.
Data Presentation and Analysis
Data from cognitive interviews is primarily qualitative, but quantifying the frequency of specific issues can help prioritize revisions. The following table summarizes quantitative data from a published study that used cognitive interviews to refine a contraceptive effectiveness poster, demonstrating how participant feedback can be systematically assessed [58].
Table 1: Quantitative Results from Cognitive Interviews on a Patient-Centered Contraceptive Poster (Final Round, N=7) [58]
| Metric | Patient-Centered Poster Preference | CDC Poster Preference |
|---|---|---|
| Overall Preference | 83% | 17% |
| Comprehension | 86% | 14% |
| Relevance | 86% | 14% |
| Design | 100% | 0% |
Table 2: Analysis of Categorical and Quantitative Data in Cognitive Interviewing
| Data Type | Role in Cognitive Interviewing | Analysis Methods |
|---|---|---|
| Categorical Data (e.g., participant demographics, types of comprehension errors) [63] [64] | Used to describe participant characteristics and classify different types of issues (e.g., "terminology misunderstanding," "layout confusion"). | Frequency counts, thematic analysis. Used to ensure a diverse sample and to categorize problems. |
| Quantitative Data (e.g., preference rates, numeracy scores, number of participants reporting an issue) [58] [63] | Used to measure the prevalence of identified issues and to quantify participant preferences between different instrument versions. | Descriptive statistics (percentages, means). Helps prioritize which issues affect the most users. |
The analysis involves summarizing qualitative data into a structured matrix to guide revisions. The following diagram illustrates the logical flow from raw data to final insights.
Application in Reproductive Health Research
Cognitive interviewing has proven critical in reproductive health for improving the accuracy of self-reported data on sensitive behaviors. Key applications include:
- Improving Reporting of Sensitive Behaviors: A study aimed at reducing abortion underreporting tested new question formulations. Findings suggested that including abortion in a list of other sexual health services, asking a simple yes/no lifetime experience question, and using a less intrusive introduction improved the accuracy of reports [60].
- Developing Patient-Centered Educational Materials: Researchers used cognitive interviews to compare a patient-centered contraceptive effectiveness poster with a standard CDC poster. Through iterative rounds of testing and revision, they identified unanticipated issues and refined the material to be more comprehensible, relevant, and acceptable to the target audience [58].
- Validating Global Survey Instruments: The World Health Organization (WHO) employs cognitive interviewing across multiple countries to ensure that questions on sexual practices and behaviors are comprehensible and applicable in diverse cultural and linguistic contexts. This process is essential for creating a standardized instrument that allows for valid cross-national comparisons [59].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Essential Materials for Conducting Cognitive Interviews
| Item/Reagent | Function in the Protocol |
|---|---|
| Semi-Structured Interview Protocol | A flexible guide containing the survey questions, think-aloud instructions, and planned probe questions. Ensures consistency across interviews while allowing for exploration of emergent topics [58] [59]. |
| Purposive Sampling Framework | A predefined plan for recruiting participants with a range of characteristics (e.g., age, literacy, reproductive history) to capture diverse perspectives and ensure the findings are relevant to the entire target population [58]. |
| Audio Recording Equipment | To capture the interview verbatim. High-quality recording is essential for accurate transcription and analysis. |
| Qualitative Data Analysis Software (e.g., NVivo, Dedoose) | Software used to manage, code, and analyze interview transcripts systematically. It facilitates the organization of data into themes and calculates inter-coder reliability [58] [61]. |
| Translation & Back-Translation Services | For multi-lingual studies, professional services ensure the conceptual meaning of questions is retained across languages, which is critical for comparative research [59]. |
| Informed Consent Documents | Documents that clearly explain the study purpose, procedures, risks, benefits, and participant rights. Ethical review and consent are foundational to research involving human subjects [59]. |
Optimizing Intervention Delivery and Component Selection
Application Notes: Quantitative Data on Intervention Effectiveness
This section synthesizes key quantitative findings from recent studies on reproductive health interventions, focusing on component effectiveness and measurement tools.
Table 1: Key Findings from Recent Reproductive Health Intervention Studies
| Study Focus / Population | Sample Size & Design | Key Quantitative Findings | Implication for Intervention Design |
|---|---|---|---|
| Parent-Teen Sexual Health Communication [65] | 522 parent-teen dyads; Cross-sectional, nationally representative US survey | Frequent communication associated with higher teen self-efficacy only when parents felt informed (β=0.11, p=0.01) and comfortable (β=0.11, p=0.03). When parents lacked these, frequent communication was associated with lower teen self-efficacy. | Intervention success is contingent on parent readiness. Components must target parental knowledge and comfort, not just communication frequency. |
| Reproductive Health Literacy for Refugee Women [30] | 184 refugee women (67 Dari, 53 Arabic, 64 Pashto speakers); Survey post-RHL training | The developed RHL scale showed strong inter-item reliability across all three language groups (Cronbach's α > 0.7 for all domains: general health literacy, digital health literacy, and reproductive health literacy). | Validated, translated tools are critical for measuring intervention impact in multicultural populations. The RHL scale is a reliable metric. |
| Caesarean Section Reduction Interventions [66] | 21 intervention studies; Qualitative Comparative Analysis (QCA) | Identified five components triggering success: 1) provider training, 2) active dissemination of CS indications, 3) actionable recommendations, 4) multidisciplinary collaboration, and 5) provider willingness to change. | A combination of these components is sufficient for success. If one or more are absent, a "dictated" (enforced) intervention nature may be needed. |
| Sexual & Reproductive Health Questionnaire Validation [67] | 90 students; Psychometric validation study | The knowledge section of the validated questionnaire demonstrated good internal consistency (Kuder-Richardson score > 0.7). Discrimination index varied, identifying specific knowledge gaps. | The tool is valid for evaluating intervention effectiveness and pinpointing precise topics for educational sessions. |
Experimental Protocols
This section provides detailed methodological workflows for key experimental approaches cited in the application notes.
Protocol 1: Development and Validation of a Reproductive Health Literacy Scale
Objective: To create a culturally and linguistically appropriate instrument for measuring reproductive health literacy among refugee women [30].
Procedure:
- Domain and Item Identification: Conduct a systematic literature review to identify existing health literacy tools and establish conceptual domains. The core domains should align with the Health People 2030 definition and include a) General Health Literacy, b) Digital Health Literacy, and c) Reproductive Health Literacy (e.g., cervical cancer, family planning, postpartum care) [30].
- Scale Selection and Adaptation: Select validated scales for each domain. For example:
- General Health Literacy: Use the 6-item European Health Literacy Survey Questionnaire (HLS-EU-Q6), which has a known reliability of α = 0.803 [30].
- Digital Health Literacy: Use the eHealth Literacy Scale (eHEALS), an 8-item scale with an alpha coefficient of 0.88 [30].
- Reproductive Health Literacy: Create a composite scale using items from validated tools like the Cervical Cancer Literacy Assessment Tool (C-CLAT) and postpartum literacy scales. Maintain original 4-point Likert response options where validated [30].
- Content and Face Validity: Assemble a panel of content experts (e.g., international medical graduates, subject matter experts) to qualitatively assess the relevance, appropriateness, and representativeness of each item. Revise the scale based on feedback [30] [67].
- Translation and Cultural Adaptation: Employ bilingual and bicultural translators to perform forward- and back-translation of the final English scale into target languages (e.g., Dari, Arabic, Pashto). Pilot the translated versions with bilingual volunteers and refugee women for understandability and accuracy [30].
- Psychometric Validation: Administer the translated scale to the target population (e.g., after a health literacy training session).
- Internal Consistency: Calculate Cronbach's alpha (α) for each domain and the overall scale. A value above 0.7 is generally considered acceptable [30] [67].
- Construct Validity: Use exploratory factor analysis (EFA) to validate the underlying factor structure. Assess the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy (should be >0.6) and Bartlett's Test of Sphericity (should be significant, p<0.05) [67] [68].
Protocol 2: Qualitative Comparative Analysis (QCA) for Intervention Optimization
Objective: To identify critical intervention components and their combinations that lead to successful implementation of programs aimed at reducing caesarean sections [66].
Procedure:
- Develop a Logic Model: Construct a preliminary logic model based on existing qualitative and quantitative evidence syntheses. This model outlines the hypothesized pathways and components (e.g., provider training, audit & feedback) leading to the desired outcome (e.g., optimized CS use) [66].
- Case Selection and Data Sourcing: Identify a set of "cases" (individual intervention studies) from systematic reviews that meet the inclusion criteria (e.g., interventions targeting healthcare providers to reduce CS). Both successful and unsuccessful cases are required for comparison [66].
- Define and Code Conditions: Identify potential "conditions" (intervention features) from the logic model and literature. Code each case for the presence or absence of these conditions using a binary crisp-set (csQCA: 1=present, 0=absent) or an ordinal fuzzy-set (fsQCA: values between 0 and 1) system. Example conditions include [66]:
- Provision of training
- Use of audit and feedback
- Multidisciplinary collaboration
- Providers' willingness to change
- Code the Outcome: Code the outcome of each case (e.g., 1="successful" if a significant reduction in CS rates was reported, 0="unsuccessful" if not) [66].
- Analyze for Sufficiency: Use QCA software (e.g., the QCA package in R) to analyze the data. The analysis identifies which combinations of conditions are sufficient (but not necessarily necessary) for achieving the successful outcome. This is reported as a consistency score, which measures how frequently a condition or combination is present when the outcome is achieved [66].
- Interpret Solutions: Interpret the resulting combinatorial pathways. For example, the solution might show that "training AND multidisciplinary collaboration AND provider willingness" is a sufficient pathway for success, while another pathway might be "dictated intervention guidelines" in the absence of other components [66].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools and Instruments for Reproductive Health Behavior Research
| Item / Tool Name | Type | Primary Function in Research | Exemplar Use Case |
|---|---|---|---|
| Reproductive Health Literacy (RHL) Scale [30] | Validated Survey Instrument | Measures the ability to find, understand, and use information for health-related decisions in reproductive health. | Evaluating the effectiveness of health literacy training interventions for refugee and migrant populations. |
| eHEALS (eHealth Literacy Scale) [30] | Validated Survey Instrument | Assesses an individual's ability to seek, find, understand, and appraise health information from electronic sources. | Gauging participants' digital health literacy as a component of broader health literacy, crucial for digital interventions. |
| HLS-EU-Q6 [30] | Validated Survey Instrument | A short 6-item tool to measure general, subjective health literacy across clinical and population settings. | Providing a brief, reliable assessment of general health literacy within a larger reproductive health battery. |
| Cervical Cancer Literacy Assessment Tool (C-CLAT) [30] | Validated Survey Instrument | Specifically assesses literacy and knowledge related to cervical cancer prevention and screening. | Measuring knowledge outcomes in interventions focused on cervical cancer awareness. |
| Parent-Teen Sexual Health Communication Scale [65] | Validated Survey Instrument | A 7-item scale measuring the frequency of communication on specific SRH topics between parents and teens. | Investigating the relationship between communication patterns and teen SRH self-efficacy and outcomes. |
| Sexual & Reproductive Health (SRH) Knowledge Questionnaire [67] | Validated Knowledge Assessment | Multiple-choice questions to assess specific knowledge gaps in sexual and reproductive health. | Objectively measuring knowledge gains in school-based or community SRH education interventions. |
| SRH-POI Scale [68] | Condition-Specific Patient-Reported Outcome Measure | A 30-item tool to assess the sexual and reproductive health status of women with Premature Ovarian Insufficiency. | Capturing the multidimensional impact of a specific reproductive health condition in clinical trials or cohort studies. |
| CDC Surveillance Systems (e.g., PRAMS, NASS) [69] | Population-Level Data Systems | Provide ongoing, systematic collection and analysis of maternal and infant health data at a national level. | Providing benchmark data, understanding population trends, and evaluating large-scale public health interventions. |
Ensuring Inclusivity Across Genders and Cultural Contexts
Inclusive research instrument design is critical for generating valid, reliable, and generalizable data in sexual and reproductive health (SRH) research. The development of questionnaires that accurately capture experiences across gender identities and cultural contexts remains methodologically challenging. This protocol outlines evidence-based approaches for creating SRH behavior questionnaires that are inclusive across genders and cultural contexts, supporting equitable research practices in global health studies.
Application Notes: Theoretical Framework and Considerations
Conceptualizing Gender Inclusivity in SRH Questionnaires
Gender inclusivity in SRH research extends beyond binary male-female categorizations to encompass diverse gender identities and expressions. Research indicates that gender-specific SRH instruments often overlook the unique needs of gender-diverse populations and fail to account for intersecting factors that influence health behaviors. A study developing a reproductive health behavior questionnaire in South Korea focused specifically on exposure to endocrine-disrupting chemicals but limited its participant recruitment to "adult men and women," potentially excluding gender-diverse individuals [8]. Similarly, the sexual and reproductive health assessment scale for women with premature ovarian insufficiency (SRH-POI) was designed specifically for cisgender women, demonstrating how some instruments must remain condition-specific while still acknowledging gender diversity within research populations [68].
Key considerations for gender-inclusive design:
- Terminology and language: Use inclusive terminology that acknowledges diverse gender identities and sexual orientations.
- Participant recruitment: Implement stratified sampling strategies that ensure representation across gender spectrum.
- Item development: Create items that are relevant to diverse gendered experiences without reinforcing stereotypes.
Cultural Contexts in SRH Instrument Development
Cultural contexts significantly shape how individuals perceive, experience, and report on SRH behaviors. A qualitative study in Sanandaj, Western Iran, demonstrated how customs, traditions, and socio-cultural norms directly influence women's sexual and reproductive health literacy [70]. Researchers identified three primary socio-cultural factors affecting SRH literacy: (1) customs and traditions (including marriage customs, importance of virginity, and gender roles), (2) socio-cultural norms and beliefs (including perceptions of sexual behavior), and (3) economic conditions that impact access to SRH information and services [70].
The WHO-led development of the Sexual Health Assessment of Practices and Experiences (SHAPE) questionnaire represents a significant advancement in cross-cultural SRH instrument development. As the first global survey to assess sexual practices and behaviors impacting health, SHAPE was implemented in Portugal with a nationally representative sample, demonstrating feasibility across different administration modes (online and telephone) while maintaining data quality [32].
Experimental Protocols and Methodologies
Protocol for Cross-Cultural Questionnaire Adaptation
Objective: To adapt SRH questionnaires for different cultural contexts while maintaining conceptual equivalence and psychometric properties.
Methodology:
- Forward-translation: Two independent bilingual translators translate the original instrument into the target language.
- Back-translation: Two different translators blind to the original instrument back-translate to the source language.
- Expert committee review: A panel including translators, methodologists, and content experts compares original and back-translated versions and develops a pre-final version.
- Cognitive interviewing: Conduct think-aloud interviews with 10-15 target population members to assess comprehension, cultural relevance, and acceptability.
- Psychometric validation: Administer to a larger sample (n=200-300) for factor analysis and reliability testing.
The development and validation of the SRH assessment scale for women with premature ovarian insufficiency (SRH-POI) followed a rigorous methodological sequence including item generation through literature review and qualitative study, content validation, pilot testing, construct validation through factor analysis, and reliability assessment [68].
Protocol for Gender-Inclusive Questionnaire Development
Objective: To develop SRH questionnaires that are inclusive across gender identities.
Methodology:
- Stakeholder engagement: Establish advisory boards comprising diverse gender identities, including transgender, non-binary, and gender-diverse individuals.
- Item pool generation: Develop items through systematic literature review and qualitative methods (focus groups, interviews) with gender-diverse populations.
- Content validity assessment: Convene expert panels including gender diversity specialists to evaluate item relevance, clarity, and inclusivity using content validity indices (CVI).
- Cognitive testing: Conduct interviews with participants across gender spectrum to assess comprehension and relevance.
- Psychometric validation: Administer to a large, diverse sample to establish factor structure, measurement invariance, and reliability.
A protocol for a mobile health app (Health-E You/Salud iTu) for male adolescents demonstrates gender-considerate approaches by specifically addressing the research gap in SRH interventions for male populations while employing gender-diverse design team advisory groups (DTAGs) to inform content development [18].
Table 1: Quantitative Data from SRH Questionnaire Validation Studies
| Study/Questionnaire | Sample Size | Number of Items | Validation Method | Reliability (Cronbach's α) | Response Rate |
|---|---|---|---|---|---|
| EDC Reproductive Health Behaviors (Korea) [8] | 288 | 19 | EFA, CFA | 0.80 | Not specified |
| SHAPE Questionnaire (Portugal) [32] | 2,010 | Not specified | Not specified | Not specified | 30.9% (79.5% online, 12.4% telephone) |
| SRH-POI Scale [68] | Not specified | 30 (final from 84 initial) | EFA, content validity | 0.884 | Not specified |
| Health-E You/Salud iTu mHealth App [18] | 2,752 (planned) | Not specified | RCT protocol | Not applicable | Not applicable |
Table 2: Cross-Cultural Adaptation Challenges and Mitigation Strategies
| Challenge | Impact on Questionnaire Validity | Mitigation Strategy |
|---|---|---|
| Language nuances and idioms | Conceptual nonequivalence | Use of bilingual translators with cultural context knowledge |
| Cultural taboos around SRH topics | Reduced response accuracy | Cognitive interviewing to identify sensitive topics; alternative phrasing |
| Differing health literacy levels | Variable comprehension | Plain language summaries; multiple response formats |
| Varied healthcare system experiences | Differential item functioning | Contextual priming questions; local examples |
| Stigma around gender diversity | Underrepresentation | Community engagement; trusted data collectors |
Visualization of Research Workflows
Gender-Inclusive Questionnaire Development Workflow
Cross-Cultural Adaptation Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Reagents and Materials for Inclusive SRH Questionnaire Development
| Item/Resource | Function/Application | Implementation Example |
|---|---|---|
| Content Validity Index (CVI) | Quantifies expert agreement on item relevance and clarity | Used in SRH-POI scale development with S-CVI of 0.926 [68] |
| Cognitive Interviewing Protocols | Identifies comprehension problems, sensitive topics, and cultural barriers | Employed in Iranian SRH literacy study to understand cultural contexts [70] |
| WHO SHAPE Questionnaire | Global standard for assessing sexual practices and experiences | Implemented in Portugal with 2,010 participants; 17.7 min average completion [32] |
| Digital Data Collection Platforms | Enables multi-modal data collection (online, telephone) | SHAPE questionnaire used both online (79.5%) and telephone (12.4%) modalities [32] |
| Exploratory/Confirmatory Factor Analysis | Establishes construct validity and measurement invariance | EDC reproductive health behavior questionnaire used EFA and CFA for validation [8] |
| Mixed-Methods Research Designs | Combines qualitative and quantitative approaches for comprehensive understanding | SRH-POI scale development used sequential exploratory mixed-methods design [68] |
| Gender-Diverse Advisory Boards | Ensures inclusive language and relevant content | Health-E You/Salud iTu app utilized Design Team Advisory Groups (DTAGs) [18] |
| Cross-Cultural Translation Protocols | Maintains conceptual equivalence across languages | Standardized forward/back-translation methods used in global studies |
Discussion and Implementation Guidelines
The protocols and application notes outlined provide a framework for developing SRH questionnaires that are inclusive across genders and cultural contexts. Successful implementation requires ongoing community engagement, iterative refinement, and commitment to addressing power imbalances in research relationships. Future directions should focus on developing standardized measures for assessing inclusivity and establishing benchmarks for representative sampling across diverse populations.
Researchers should consider the ethical implications of SRH questionnaire development, particularly regarding privacy and confidentiality for marginalized populations. The study in Iran highlighted how economic conditions and financial constraints significantly impact access to SRH information and services, reminding researchers to consider structural barriers to participation [70]. Similarly, digital data collection methods, while increasing accessibility, must be implemented with attention to digital literacy and access disparities.
By adopting these evidence-based protocols and utilizing the provided toolkit, researchers can advance the field of SRH research through more inclusive, valid, and culturally responsive measurement approaches that generate findings representative of diverse global populations.
Balancing Comprehensiveness with Participant Burden
In reproductive health research, a fundamental challenge exists between collecting sufficiently comprehensive data to draw valid conclusions and minimizing participant burden to ensure high-quality responses and strong participation rates [8]. This balance is critical, as excessively long or intrusive questionnaires can lead to respondent fatigue, poor data quality, and low completion rates, particularly when addressing sensitive topics such as sexual practices and endocrine-disrupting chemical (EDC) exposure [8] [11]. This protocol outlines evidence-based strategies for developing reproductive health behavior questionnaires that maintain scientific rigor while respecting participant constraints, drawing from recent methodological advances in survey design, validation techniques, and technology-enabled administration.
Theoretical Framework and Key Concepts
Defining Comprehensiveness and Burden
In questionnaire development, comprehensiveness refers to the adequate coverage of all constructs relevant to the research objectives, including knowledge, behaviors, attitudes, and outcomes. For reproductive health, this may encompass sensitive topics such as sexual practices, contraceptive use, exposure to environmental chemicals, and healthcare-seeking behaviors [8] [11].
Participant burden encompasses multiple dimensions: cognitive load (mental effort required), temporal demands (completion time), psychological discomfort (especially with sensitive topics), and logistical barriers [21]. The relationship between these constructs is often inverse—increasing comprehensiveness typically elevates burden, necessitating strategic trade-offs.
Reproductive Health Specific Considerations
Reproductive health questionnaires present unique challenges due to the personal nature of the topics. Participants may experience survey fatigue when asked to recount detailed sexual behaviors or reproductive histories [11]. Additionally, complex biomedical concepts (e.g., endocrine-disrupting chemicals, contraceptive mechanisms) require careful explanation without overwhelming respondents [8] [18]. Cultural and linguistic appropriateness is particularly crucial in global contexts, where concepts of sexual health and reproductive behaviors vary significantly [11].
Methodological Approaches and Experimental Protocols
Iterative Questionnaire Development Protocol
The following structured protocol outlines a comprehensive approach for developing reproductive health questionnaires that balance data needs with participant experience:
Questionnaire Development Workflow
Define Research Objectives and Conceptual Framework
Clearly articulate the core constructs to be measured, distinguishing essential from supplementary domains. For reproductive health behavior research, this involves specifying whether primary outcomes include knowledge (e.g., EDC exposure routes), behaviors (e.g., condom use, product consumption), clinical outcomes (e.g., pregnancy, STI incidence), or attitudes [8] [18]. Establish theoretical frameworks guiding questionnaire structure, such as health behavior models or socio-ecological frameworks.
Conduct Comprehensive Literature Review
Systematically identify existing validated instruments to avoid redundant development. For example, the WHO Sexual Health Assessment of Practices and Experiences (SHAPE) questionnaire provides a validated foundation for sexual behavior research [11]. Similarly, Kim et al.'s reproductive health behaviors survey for EDC exposure offers a structured approach to chemical exposure assessment [8]. Adapt rather than create new items when possible to enhance comparability across studies.
Draft Initial Item Pool (Over-inclusive)
Generate items comprehensively covering all identified constructs, using multiple item formats:
- Closed-ended questions with categorical responses for straightforward behaviors and demographics
- Likert scales for attitudes and perceptions (e.g., 5-point agreement scales)
- Open-ended questions for nuanced experiences unanticipated by researchers [21] Kim et al. began with 52 initial items covering EDC exposure through food, respiration, and skin absorption before refinement [8].
Expert Panel Review (Content Validity)
Convene multidisciplinary experts (e.g., clinical specialists, methodologists, community representatives) to evaluate item relevance, clarity, and completeness. Calculate Content Validity Index (CVI) for each item, retaining those meeting threshold values (typically I-CVI ≥ 0.80). Kim et al. used a panel including chemical/environmental specialists, a physician, a nursing professor, and a language expert [8].
Cognitive Testing with Target Population
Conduct think-aloud interviews or verbal probing with representatives from the target population to identify problematic items, misinterpretations, or sensitive questions. The WHO SHAPE questionnaire underwent cognitive testing in 19 countries to ensure cross-cultural appropriateness [11]. This phase is critical for identifying and mitigating burden from confusing items.
Pilot Testing (Exploratory Factor Analysis and Reliability)
Administer the refined questionnaire to a sample large enough for psychometric analysis (typically 5-10 participants per item). Kim et al. recruited 288 participants for their validation study, conducting exploratory factor analysis to identify underlying factor structure and eliminate redundant items [8]. Calculate internal consistency reliability (Cronbach's alpha) for multi-item scales.
Finalize Instrument (Confirmatory Factor Analysis and Validation)
Conduct confirmatory factor analysis on a separate sample to verify the factor structure. Establish convergent, discriminant, and criterion validity as appropriate. Kim et al. used this approach to finalize their 19-item instrument across four factors [8].
Sampling and Administration Protocols
The "Surveys of Women" study implemented an address-based sampling (ABS) multimodal approach to reduce participation barriers while maintaining representative sampling [71]. The protocol combines:
- Cross-sectional baseline survey with random household selection
- Multiple follow-up surveys with an opt-in panel
- Multimode design (web and paper questionnaires)
- Strategic prompting schedule with modest monetary incentives
This approach accommodates participant preferences while collecting longitudinal data, demonstrating how flexible administration can mitigate burden without sacrificing data collection goals [71].
Technology-Enabled Administration Protocols
Mobile health applications offer innovative approaches to reduce burden while collecting comprehensive data. The Health-E You/Salud iTu randomized controlled trial protocol demonstrates how technology can enhance reproductive health assessment [18]:
- Pre-visit administration: Patients complete assessments before clinical visits, distributing time commitment
- Interactive design: Tailored content based on previous responses avoids irrelevant questions
- Clinical integration: Automated summary reports for clinicians reduce duplicate data collection
- Adaptive questioning: Branching logic eliminates unnecessary items based on individual characteristics
Quantitative Data and Validation Metrics
Item Reduction Statistics from Validation Studies
Table 1: Item Reduction Metrics from Reproductive Health Questionnaire Validation Studies
| Study | Initial Items | Final Items | Reduction Rate | Primary Reduction Method | Sample Size | Reliability (α) |
|---|---|---|---|---|---|---|
| Kim et al. (2025) EDC Reproductive Health Behaviors [8] | 52 | 19 | 63.5% | Expert review (CVI) + EFA/CFA | 288 | 0.80 |
| WHO SHAPE Questionnaire (2025) [11] | Not specified | Priority question set | Not specified | Global Delphi consultation + cognitive testing | 19 countries | Not specified |
Factor Structures of Validated Instruments
Table 2: Factor Analysis Results from Reproductive Health Behavior Instruments
| Questionnaire | Identified Factors/Domains | Variance Explained | Example Items | Response Format |
|---|---|---|---|---|
| EDC Reproductive Health Behaviors [8] | 1. Health behaviors through food2. Health behaviors through breathing3. Health behaviors through skin4. Health promotion behaviors | Not specified | "I often eat canned tuna""I use plastic water bottles""I frequently dye or bleach my hair" | 5-point Likert scale (1=strongly disagree to 5=strongly agree) |
| WHO SHAPE Questionnaire [11] | Combination of interviewer-administered and self-administered modules covering sexual practices, behaviors, and health-related outcomes | Not specified | Priority questions comprehensible to general population across diverse global contexts | Mixed methods (CAPI/CASI) |
Data Visualization Strategies for Mixed-Methods Data
Reproductive health questionnaires often generate both quantitative (closed-ended) and qualitative (open-ended) data. Effective visualization strategies enhance comprehension while minimizing analytical burden for researchers:
Open-Ended Response Visualization Protocol
Qualitative Data Analysis Workflow
Rouder et al. (2021) outline specific visualization techniques for open-ended survey responses based on Gestalt principles [21]:
- Color and shape: Highlight commonalities among respondents using heat maps or spectrum displays
- Weight or size: Display importance or frequency using packed bubble diagrams (superior to word clouds)
- Proximity and connection: Show interrelationships using process charts or Venn diagrams
These approaches transform qualitative data into accessible visual formats that complement quantitative findings, supporting more nuanced interpretation of mixed-methods results in reproductive health research [21].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Reproductive Health Questionnaire Development and Testing
| Resource Category | Specific Tools/Solutions | Function/Application | Example Use Cases |
|---|---|---|---|
| Survey Platforms | REDCap, XLSForm [11] | Enable computer-assisted personal interviewing (CAPI) and computer-assisted self-interviewing (CASI) | WHO SHAPE questionnaire implementation; multimodal data collection |
| Statistical Analysis Software | IBM SPSS Statistics, IBM SPSS AMOS, R Programming [8] [72] | Conduct exploratory and confirmatory factor analysis; reliability testing; advanced statistical modeling | Psychometric validation; item reduction; scale refinement |
| Mobile Health Platforms | Health-E You/Salud iTu mobile web app [18] | Pre-visit assessment with tailored content and clinical summary generation | Sexual and reproductive health care delivery in clinical settings |
| Sampling Frameworks | Address-Based Sampling (ABS) multimodal design [71] | Representative household sampling with web and mail response options | Population-based surveys of women across multiple states |
| Qualitative Analysis Tools | Microsoft Office Suite (Excel, PowerPoint) with advanced visualization capabilities [21] | Thematic coding and visualization of open-ended responses | Transforming qualitative feedback into compelling data stories |
| Validation Metrics | Content Validity Index (CVI), Cronbach's alpha, EFA/CFA fit indices [8] | Quantify instrument validity and reliability | Establishing measurement properties during questionnaire development |
Balancing comprehensiveness with participant burden requires methodical approaches throughout questionnaire development. The protocols outlined—iterative item reduction, multimodal administration, technology integration, and strategic visualization—provide reproductive health researchers with evidence-based strategies to optimize this balance. By applying these structured methodologies, researchers can develop instruments that yield comprehensive, valid data while respecting participants' time and cognitive resources, ultimately enhancing scientific rigor and response quality in reproductive health behavior research.
Establishing Rigor: Reliability, Validity, and Cross-Cultural Adaptation
Robust psychometric validation is a fundamental prerequisite for any instrument intended for use in reproductive health research and clinical practice. The assessment of reliability, defined as the consistency and stability of a measurement tool, provides critical evidence that a questionnaire produces trustworthy data. Within the context of a broader thesis on reproductive health behavior questionnaire development, this document details application notes and protocols for establishing two core types of reliability: internal consistency, which measures the interrelatedness of items within a scale, and test-retest reliability, which assesses the stability of measurements over time. These metrics are indispensable for researchers, scientists, and drug development professionals who require validated tools to accurately measure patient-reported outcomes, evaluate interventional efficacy, and inform clinical decision-making.
Data from recent validation studies on reproductive health questionnaires reveal a range of acceptable to excellent reliability metrics. The table below summarizes key quantitative findings, which serve as benchmarks for instrument development.
Table 1: Reliability Metrics from Recent Reproductive Health Questionnaire Validation Studies
| Questionnaire / Instrument Name | Study Population | Internal Consistency (Cronbach’s α) | Test-Retest Reliability | Retest Interval | Citation |
|---|---|---|---|---|---|
| SRH Service Seeking Scale (SRHSSS) | 458 young adults | 0.90 | Performed (n=220) | 1 month | [73] |
| Reproductive Health Literacy Questionnaire | 1587 Chinese unmarried youth | 0.919 | Correlation = 0.720 (n=60) | 2 weeks | [74] [75] |
| Sexual Health Questionnaire (SHQ) | Adolescents (Rapid Review) | 0.90 | Reliable results (Wilcoxon test) | 7 weeks | [25] |
| Rheuma Reproductive Behavior Questionnaire | 165 female rheumatic disease patients | Not Specified | 34/41 items perfect correlation | Not Specified | [76] |
| Sexual Behavior History Questionnaire | Urbanized Nigerian Women | Not Applicable | ICC: 0.7 - 0.9 | 6 months | [77] |
These findings highlight that excellent internal consistency (α ≥ 0.9) is an achievable standard for reproductive health tools [73] [74] [25]. For test-retest reliability, the specific statistical measures used—including correlation coefficients, Intraclass Correlation Coefficients (ICC), and simple percent agreement—vary based on the nature of the data (continuous or categorical) [77]. The retest interval is a critical variable, with studies employing periods from two weeks to one month to balance the mitigation of memory effects against the assumption of trait stability [73] [74] [25].
Experimental Protocols for Reliability Assessment
Protocol for Establishing Internal Consistency
Principle: Internal consistency evaluates whether all items in a scale or subscale measure the same underlying construct. This is typically measured using Cronbach's alpha coefficient.
Table 2: Key Research Reagents and Materials for Internal Consistency Analysis
| Item / Solution | Function / Explanation |
|---|---|
| Finalized Draft Questionnaire | The instrument with a fixed set of items and response scales to be tested. |
| Target Population Sample | A representative sample from the intended study population. |
| Statistical Software (e.g., R, SPSS, SAS) | To compute Cronbach's alpha and item-total statistics. |
Step-by-Step Procedure:
- Administration: Administer the finalized draft questionnaire to a sufficient sample size from the target population. A sample of over 150 participants is generally recommended for stable estimates [73].
- Data Preparation: Code and clean the response data. Reverse-score any negatively phrased items as per the instrument's design.
- Statistical Analysis: Use statistical software to calculate the overall Cronbach's alpha for the scale. A value of ≥ 0.70 is generally considered acceptable for group-level analysis, while ≥ 0.90 is desirable for high-stakes clinical decision-making [73] [25].
- Item Analysis: Examine the "alpha if item deleted" statistic. This helps identify items that, if removed, would increase the overall alpha, suggesting they may not be measuring the same construct and should be considered for removal.
- Reporting: Report the final Cronbach's alpha value, the number of items in the scale, and the sample size used for the calculation.
Protocol for Establishing Test-Retest Reliability
Principle: Test-retest reliability assesses the stability of a measurement instrument when administered to the same participants on two separate occasions, under the assumption that the underlying construct being measured has not changed.
Table 3: Key Research Reagents and Materials for Test-Retest Analysis
| Item / Solution | Function / Explanation |
|---|---|
| Validated Interviewers/Platform | To ensure consistent administration; reduces interviewer-induced variability. |
| Stable Participant Cohort | Participants whose underlying health status/behavior is not expected to change. |
| Statistical Software (e.g., R, SPSS, SAS) | To calculate ICC, Kappa, or correlation coefficients with confidence intervals. |
Step-by-Step Procedure:
- Initial Test (T1): Administer the questionnaire to a subset of the study population under standardized conditions.
- Retest Interval: Determine an appropriate time interval before the second administration. The interval must be short enough to ensure the construct of interest is stable, yet long enough to prevent recall bias. Based on successful studies, an interval of two weeks to one month is often optimal [73] [74] [78]. Document this interval precisely.
- Second Test (T2): Re-administer the identical questionnaire to the same participants under the same conditions as T1.
- Statistical Analysis:
- For continuous or ordinal data (e.g., Likert scales, scores), calculate the Intraclass Correlation Coefficient (ICC). A two-way mixed-effects model is commonly used. Values above 0.75 are generally considered excellent, while 0.60 to 0.74 are good [77] [78].
- For categorical data, calculate the Kappa statistic (κ). According to Landis and Koch, values from 0.61–0.80 indicate substantial agreement, and 0.81–1.00 indicate almost perfect agreement [77].
- Reporting: Report the reliability coefficient (ICC or Kappa), its 95% confidence interval, the retest interval, and the sample size used for the analysis.
Rigorous assessment of internal consistency and test-retest reliability forms the bedrock of developing valid and scientifically credible reproductive health behavior questionnaires. The protocols outlined herein, supported by contemporary validation studies, provide a clear methodological pathway. Adherence to these standards ensures that resulting data are stable, consistent, and fit-for-purpose, thereby enabling robust measurement in both research and clinical contexts, from epidemiological studies to drug development programs.
Establishing Construct and Convergent Validity
Within the framework of reproductive health behavior questionnaire development, establishing robust psychometric properties is paramount for ensuring that research instruments accurately measure the intended constructs. Construct validity examines whether a tool truly measures the theoretical construct it purports to measure, while convergent validity assesses the extent to which the instrument correlates with other measures of the same or similar constructs [79]. For researchers and pharmaceutical developers working in reproductive health, rigorously validated questionnaires provide reliable endpoints for clinical trials, intervention studies, and health outcomes research. This protocol outlines standardized methodologies for establishing construct and convergent validity within reproductive health questionnaire development, drawing upon validated approaches from recent studies in the field.
Theoretical Foundations and Key Concepts
The development of a valid reproductive health assessment tool must be grounded in a clear conceptual framework that defines the target constructs. Reproductive health encompasses multidimensional constructs including physical, emotional, mental, and social well-being in all matters relating to the reproductive system [80]. Recent instrument development studies have emphasized the importance of adapting theoretical models to specific cultural contexts and population characteristics. For instance, the concept of sexual and reproductive empowerment for adolescents and young adults reflects the expansion of an individual's ability to make strategic life choices in contexts where this ability was previously denied [80]. Similarly, condition-specific reproductive health profiles for populations such as women with type-1 diabetes or premature ovarian insufficiency require conceptual models that capture unique health experiences and challenges [68] [81].
Methodological Protocols for Establishing Construct Validity
Factor Analysis Procedures
Factor analysis represents the cornerstone methodology for establishing construct validity, comprising both exploratory (EFA) and confirmatory (CFA) approaches.
Exploratory Factor Analysis (EFA) Protocol
Sample Requirements: Recruitment should target 5-10 participants per questionnaire item, with a minimum sample size of 300 subjects [80]. For the Women Shift Workers' Reproductive Health Questionnaire, researchers recruited 620 participants to ensure adequate power for factor analysis [5].
Data Collection: Administer the preliminary instrument to the target population using appropriate sampling methods (e.g., convenience, stratified, or random sampling). Ensure demographic diversity representative of the intended population.
Analytical Procedure:
- Assess Factorability: Calculate Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy (acceptable value ≥0.8) and Bartlett's test of sphericity (significant at p<0.05) [5].
- Factor Extraction: Utilize maximum likelihood estimation with equimax rotation and Horn's parallel analysis to extract latent factors.
- Factor Retention: Apply Kaiser's criterion (eigenvalues >1) and examine scree plots to determine the optimal number of factors.
- Item Assignment: Retain items with factor loadings ≥0.3, with cross-loading differences >0.2 [5].
Table 1: Exemplar EFA Results from Reproductive Health Questionnaire Studies
| Questionnaire | Sample Size | KMO Value | Variance Explained | Factor Structure | Citation |
|---|---|---|---|---|---|
| Sexual & Reproductive Empowerment Scale | 581 | 0.83 | Not specified | 6 factors, 21 items | [80] |
| Women Shift Workers' Reproductive Health Questionnaire | 620 | >0.8 | 56.50% | 5 factors, 34 items | [5] |
| SRH Profile of Women with T1DM | 365 | Not specified | 49.44% | 3 components | [81] |
Confirmatory Factor Analysis (CFA) Protocol
Sample Requirements: Utilize an independent sample from the EFA population, maintaining the 5-10 participants per item guideline.
Analytical Procedure:
- Model Specification: Test the factor structure identified through EFA.
- Model Estimation: Employ maximum likelihood estimation.
- Fit Indices Assessment: Evaluate multiple goodness-of-fit indices:
- Comparative Fit Index (CFI) ≥0.90
- Goodness of Fit Index (GFI) ≥0.90
- Root Mean Square Error of Approximation (RMSEA) ≤0.07
- Standardized Root Mean Square Residual (SRMR) ≤0.07 [80]
- Model Modification: If needed, apply theoretically justified modifications based on modification indices and standardized residual covariance matrix.
Table 2: Exemplar CFA Fit Indices from Validation Studies
| Questionnaire | CFI | GFI | RMSEA | SRMR/RMR | Citation |
|---|---|---|---|---|---|
| C-SRES | 0.91 | 0.90 | 0.07 | 0.07 | [80] |
| Evidence-Based Practice Questionnaire | 0.95 | 0.91 | 0.066 | 0.033 | [79] |
Diagram: Construct Validation Workflow
Methodological Protocols for Establishing Convergent Validity
Statistical Assessment Procedures
Convergent validity evaluates the degree to which an instrument correlates with other measures that theoretically should be related.
Average Variance Extracted (AVE) Protocol
Procedure:
- Calculate AVE for each construct using the formula: AVE = (Σ standardized factor loadings²) / number of items
- Interpret results: AVE ≥ 0.5 indicates adequate convergent validity [79]
- For the Evidence-Based Practice Questionnaire, AVE values ranged from 0.5-0.7 across domains, supporting convergent validity [79]
Correlation Analysis Protocol
Procedure:
- Administer the new instrument alongside established measures of similar constructs
- Calculate Pearson or Spearman correlation coefficients between the target instrument and validation measures
- Interpret results: Correlation coefficients ≥ 0.5 indicate strong convergent validity, with 0.3-0.5 representing moderate relationships
Fornell-Larcker Criterion Protocol
Procedure:
- Calculate the square root of AVE for each construct
- Compare this value with the correlations between that construct and all other constructs
- Interpret results: The square root of AVE should be greater than inter-construct correlations, demonstrating the construct shares more variance with its indicators than with other constructs [5]
Diagram: Convergent Validity Assessment Framework
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Methodological Components for Validity Assessment
| Research Component | Function/Application | Exemplar Implementation |
|---|---|---|
| Statistical Software (R, SPSS, AMOS, Mplus) | Conducting factor analyses and calculating validity coefficients | R packages: lavaan, psych; SPSS FACTOR procedure |
| Content Validity Panel | Evaluating item relevance and comprehensiveness | 7-12 experts in relevant fields (e.g., obstetrician-gynecologists, reproductive health specialists) [80] [5] |
| Target Population Sample | Providing data for psychometric analysis | Representative sample of 300+ participants from target population [80] |
| Validated Comparator Instruments | Establishing convergent validity | Established measures of related constructs (e.g., FSFI for sexual function, WHOQoL for quality of life) [81] |
| Cultural Adaptation Framework | Ensuring contextual appropriateness | Brislin translation model for cross-cultural adaptation [80] |
| Reliability Assessment Tools | Establishing instrument stability | Internal consistency (Cronbach's α ≥ 0.7), test-retest reliability (ICC ≥ 0.7) [80] [81] |
Application Notes for Specific Reproductive Health Contexts
Cultural Adaptation Protocols
When adapting existing reproductive health questionnaires for new cultural contexts, specific validity procedures are required:
- Translation and Back-Translation: Follow the Brislin translation model with independent forward and back-translation by bilingual experts [80]
- Cultural Expert Review: Engage cultural and clinical experts to review item appropriateness and relevance
- Cognitive Interviewing: Conduct interviews with target population members to assess comprehension and cultural acceptability
- Psychometric Revalidation: Completely reestablish construct and convergent validity in the new cultural context, as cultural factors may alter factor structures
Condition-Specific Adaptation
For reproductive health questionnaires targeting specific medical conditions:
- Clinical Expert Involvement: Include specialist clinicians in content validity assessment (e.g., endocrinologists for diabetes-related reproductive health) [81]
- Population-Specific Domains: Ensure factor structure reflects condition-specific concerns (e.g., reproductive concerns specific to premature ovarian insufficiency) [68]
- Clinical Validation: Correlate questionnaire scores with clinical indicators where possible to establish clinical relevance
Establishing robust construct and convergent validity is methodologically demanding but essential for developing scientifically sound reproductive health behavior questionnaires. The protocols outlined herein provide researchers with standardized methodologies for ensuring their instruments accurately capture the theoretical constructs they purport to measure. By adhering to these rigorous validation procedures, researchers can generate reliable data that advances both scientific understanding and clinical practice in reproductive health. Future methodological developments should focus on integrating modern psychometric approaches, such as item response theory, alongside traditional validity assessment methods to further enhance measurement precision in this critically important field.
Comparing Scoring Approaches and Indicator Formulations
Within reproductive health research, the development of precise and valid assessment tools is fundamental to advancing scientific understanding and improving clinical outcomes. The integrity of data collected on health behaviors, service-seeking patterns, and literacy is critically dependent on the methodological rigor applied in questionnaire development and the strategic selection of scoring approaches [82]. A well-defined protocol for creating these instruments ensures that they are reliable, valid, and capable of detecting meaningful changes or differences in target populations. This document, framed within a broader thesis on reproductive health behavior questionnaire development, outlines standardized protocols and application notes for comparing scoring methodologies and indicator formulations. It is designed to equip researchers, scientists, and drug development professionals with the experimental frameworks necessary to construct and evaluate robust data collection tools in this specialized field.
Application Notes: Core Concepts and Scoring Frameworks
Foundational Principles of Indicator Formulation
The formulation of indicators is a deliberate process that translates abstract theoretical constructs into measurable variables. In reproductive health, this often involves defining specific, observable, and quantifiable elements that reflect complex states like "reproductive health literacy" or "pro-health behaviors." A recent scoping review on global population policies categorized reproductive health indicators into nine key domains, providing a structured framework for researchers [83] [84]. These domains, along with the most frequent indicator, are summarized in Table 1.
Table 1: Categorized Reproductive Health Indicators for Policy and Research
| Category | Description & Example Indicators |
|---|---|
| Fertility | Tracks population-level reproduction metrics. • Total fertility rate (Most frequent indicator) • Age-specific fertility rates |
| Marriage & Divorce | Monitors societal structures supporting childbearing. • Age of first marriage • Divorce prevalence |
| Childcare | Assesses support systems for parents. • Access to government childcare centers • Parental leave policies |
| Household Economics | Measures financial capacity for child-rearing. • Family financial support programs • Income security |
| Contraception & Abortion | Evaluates access to family planning services. • Right to access contraceptive methods • Safe abortion availability |
Comparative Analysis of Scoring Approaches
Different research questions and constructs demand distinct scoring methodologies. The choice of approach directly impacts how data is interpreted and what conclusions can be drawn. Below is a comparative analysis of common scoring methods, synthesized from various validation studies.
Table 2: Comparison of Scoring Methods for Reproductive Health Questionnaires
| Scoring Method | Description | Best Use Cases | Example from Literature |
|---|---|---|---|
| Simple Summative Scoring | Responses to individual items (e.g., on a Likert scale) are summed to create a total score. This total is often interpreted against pre-defined ranges (e.g., Low, Medium, High). | Assessing overall levels of a broad construct, such as general health behaviors. | The Scale of Health Behaviors of Women During the Reproductive Period used 16 items. A score of 0-5 was "low," 6-10 "medium," and 11-16 "high" [82]. |
| Multi-Domain Factor Scoring | Exploratory Factor Analysis (EFA) and Confirmatory Factor Analysis (CFA) are used to group items into underlying domains (factors). Scores are calculated for each domain separately. | When a construct is multi-dimensional and nuanced understanding is needed. | The Women Shift Workers’ Reproductive Health Questionnaire identified 5 factors (e.g., motherhood, sexual relationships). Scoring per subscale provides specific insights [5]. |
| Composite & Combined Scoring | Combines results from different scoring methods or components of a tool (e.g., symptom scores plus impairment scores) to create a more comprehensive classification. | Identifying complex cases where multiple aspects of a condition must be met. | The SDQ can classify based on: 1) Total Difficulties Score, 2) Parent-defined difficulties, or 3) A combination of any method. This increases sensitivity [85]. |
| Cut-off Based Classification | A single score or a combination of scores is compared against a validated threshold to classify individuals into categories (e.g., "clinical" vs. "non-clinical"). | Screening and identification of individuals at risk or in need of services. | The Strengths and Difficulties Questionnaire (SDQ) uses a cut-off on the Total Difficulties Score to identify children with psychosocial problems [85]. |
Experimental Protocols
This section provides a detailed, step-by-step protocol for the development and validation of a reproductive health questionnaire, integrating the scoring approaches discussed above.
Protocol: Questionnaire Development and Validation
Objective: To develop a valid and reliable instrument for measuring a defined reproductive health construct (e.g., health literacy, service-seeking barriers, specific health behaviors) and to establish a psychometrically sound scoring system.
Phase 1: Qualitative Item Generation and Content Validation
- Define the Construct: Operationally define the reproductive health concept to be measured (e.g., "reproductive health literacy" as "the ability to find, understand, and use information for health-related decisions") [30].
- Generate Item Pool:
- Conduct a comprehensive literature review of existing tools and relevant studies [5] [8].
- Perform qualitative research (e.g., focus groups, semi-structured interviews) with the target population to explore the concept in context [73] [5]. Example: Hold 75-minute focus groups with audio recording and verbatim transcription [73].
- Draft an initial set of items based on the synthesized information.
- Assess Content Validity:
- Convene a panel of experts (e.g., in reproductive health, methodology, target population culture) [5] [8].
- Experts evaluate each item for relevance and clarity, typically on a 4-point scale.
- Calculate the Content Validity Index (CVI) both for individual items (I-CVI) and the entire scale (S-CVI). An I-CVI of >0.78 and S-CVI of >0.90 are considered excellent [5] [8].
- Revise or remove items based on expert feedback and CVI results.
Phase 2: Quantitative Psychometric Evaluation
- Pilot Testing:
- Main Study Sampling:
- Determine sample size. A common rule is 10 participants per questionnaire item, or a minimum of 300-500 for factor analysis [8].
- Recruit a large, representative sample using appropriate sampling techniques (e.g., convenience, stratified).
- Assess Construct Validity via Factor Analysis:
- Exploratory Factor Analysis (EFA): Use Principal Component Analysis with Varimax rotation on a half of the dataset.
- Check sampling adequacy with the Kaiser-Meyer-Olkin (KMO) measure (should be >0.8) and Bartlett's Test of Sphericity (should be significant, p<0.05) [5] [8].
- Extract factors with eigenvalues greater than 1. Retain items with factor loadings >0.4 on their primary factor and with cross-loadings <0.2 on other factors [8].
- Confirmatory Factor Analysis (CFA): Use the second half of the dataset to test the model fit of the factor structure identified in the EFA.
- Use model fit indices to assess goodness-of-fit: CFI >0.90, GFI >0.90, RMSEA <0.08, and CMIN/DF <5.0 [5].
- Exploratory Factor Analysis (EFA): Use Principal Component Analysis with Varimax rotation on a half of the dataset.
- Assess Reliability:
- Internal Consistency: Calculate Cronbach's alpha for the total scale and for each identified subscale. A value of 0.7-0.9 is generally considered acceptable to good [73] [5] [8].
- Test-Retest Reliability: Administer the questionnaire to the same participants after a suitable interval (e.g., 2-4 weeks). Calculate the Intraclass Correlation Coefficient (ICC); a value >0.7 indicates good stability [73].
Phase 3: Finalizing the Scoring System
- Based on the factor analysis results, finalize the questionnaire's structure (total score and/or subscale scores).
- Define the precise scoring algorithm (e.g., simple sum of item scores, average of subscale scores).
- If applicable, establish and validate cut-off scores using Receiver Operating Characteristic (ROC) curve analysis against a clinical gold standard [85].
The following workflow diagram visualizes this multi-phase protocol:
Protocol: Comparing Scoring Methods for a Single Instrument
Objective: To empirically compare the performance and outcomes of different scoring methods applied to the same dataset from a reproductive health questionnaire.
- Data Collection: Administer the questionnaire of interest to a sufficiently large sample (N > 300 recommended).
- Apply Different Scoring Methods: Calculate scores for each participant using each of the pre-defined methods to be compared (e.g., Method A: Simple Summative; Method B: Multi-Domain Factor; Method C: Composite) [85].
- Define Validation Criteria: Choose one or more external criteria to validate the scoring methods against. This could be:
- A clinical diagnosis or status (e.g., presence of sexual dysfunction).
- Scores from a previously validated "gold standard" instrument (e.g., the CBCL for the SDQ) [85].
- Current treatment status for the condition.
- Statistical Comparison:
- For categorical outcomes, create contingency tables and calculate Cohen's Kappa to assess agreement between different scoring methods and the validation criterion. Kappa values can be interpreted as: 0.01-0.20 = slight, 0.21-0.40 = fair, 0.41-0.60 = moderate, 0.61-0.80 = substantial, 0.81-0.99 = almost perfect [85].
- Calculate the sensitivity, specificity, and area under the curve (AUC) for each scoring method against the gold standard.
- Use correlation analysis (e.g., Spearman's rank correlation) to compare continuous scores from different methods.
- Interpretation and Selection: The optimal scoring method is typically the one that best balances sensitivity and specificity for identification purposes, or demonstrates the strongest correlation with the validation criterion for measurement purposes. Bourdon et al. found that while different SDQ scoring methods identified varying percentages of children, a simple classification based on the Total Difficulties Score yielded results similar to more complex methods [85].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and resources essential for executing the experimental protocols described above.
Table 3: Essential Reagents and Resources for Questionnaire Development Research
| Item / Resource | Function / Application in Research |
|---|---|
| Statistical Software (e.g., IBM SPSS AMOS, R, Mplus) | To perform complex statistical analyses including EFA, CFA, reliability analysis, ROC curve analysis, and calculation of model fit indices. Essential for Phases 2 and 3 of the development protocol [5] [8]. |
| Digital Recorder & Transcription Software | To accurately capture qualitative data from focus groups and semi-structured interviews during the initial item generation phase (Phase 1). Ensures data integrity for content analysis [73] [5]. |
| Validated "Gold Standard" Instruments | To serve as an external criterion for establishing concurrent or criterion validity when comparing scoring methods. Examples include the Child Behaviour Checklist (CBCL) or the Female Sexual Function Index (FSFI) [85] [86]. |
| Health Literacy Tool Shed (Online Database) | A curated database of health literacy measures. Used during the literature review phase to identify, compare, and select existing instruments for adaptation or to avoid duplication of effort [30]. |
| Expert Panel | A multidisciplinary group of content and methodology experts (e.g., reproductive health clinicians, psychometricians, cultural and linguistic experts) to assess content validity and provide critical feedback on item wording and relevance [5] [8]. |
The rigorous development of reproductive health questionnaires and the deliberate comparison of scoring approaches are non-negotiable for generating high-quality, actionable scientific evidence. The protocols and application notes detailed herein provide a roadmap for creating instruments that are not only statistically sound but also contextually relevant to diverse populations, from shift workers [5] to refugee women [30]. By adhering to a structured methodology that integrates both qualitative insights and quantitative validation, researchers can ensure that their tools accurately capture the complexities of reproductive health behaviors and constructs. The choice of a scoring system should be a deliberate one, informed by the research question and validated against meaningful criteria. As the field advances, these standardized protocols will be crucial for enabling valid cross-population comparisons and reliably measuring the impact of public health interventions and therapeutic developments.
Validating Against Behavioral and Clinical Outcomes
Within the protocol for reproductive health behavior questionnaire development, validation against behavioral and clinical outcomes represents the pivotal step that transforms a collection of items into a scientifically rigorous instrument. This process moves beyond internal psychometric properties to establish whether questionnaire scores correspond meaningfully to tangible, real-world health indicators [87]. For reproductive health research, this connection is paramount, as it ensures that assessments of health behaviors—such as those aimed at reducing exposure to endocrine-disrupting chemicals (EDCs)—accurately reflect an individual's actual health status and risks [8] [88].
The landscape of validation is evolving. Contemporary measurement theory emphasizes that clinical outcome assessments (COAs) are never definitively "validated" in a complete sense, but rather accumulate evidence of validity for a specific context of use [88]. This is particularly relevant for reproductive health behaviors, where the connection between self-reported actions and clinical endpoints like fertility status, pregnancy complications, or cancer incidence must be carefully established and documented.
Theoretical Foundation: From Concept to Clinical Endpoint
The Validation Hierarchy
A robust validation strategy requires a clear understanding of the pathway from the abstract concept being measured (e.g., "reproductive health behavior") to the ultimate clinical outcome. This pathway can be conceptualized as follows:
- Concept of Interest (COI): The foundational construct the questionnaire aims to measure, such as "engagement in behaviors to reduce EDC exposure" [87] [8].
- Questionnaire Score: The quantitative output from the administered instrument, which serves as a proxy for the COI [87].
- Behavioral Outcome: An objective, measurable behavior related to the COI (e.g., verified purchase of BPA-free products, dietary changes documented through food diaries) [8].
- Clinical Outcome: A direct measure of health status (e.g., biomarker levels, diagnosis of infertility, time to pregnancy) [8] [87].
The strength of a questionnaire's validity is demonstrated by the consistent, theorized relationships between these levels.
Defining "Treatment Benefit" in a Validation Context
In therapeutic development, a "treatment benefit" is a favorable effect on a meaningful aspect of how a patient feels or functions. This concept can be adapted for validation: a questionnaire demonstrates validity if its scores correlate with meaningful aspects of reproductive health status that matter to patients [87]. For instance, a higher score on a "EDC avoidance behavior" scale should correlate with improved clinical markers of reproductive function or a reduced risk of negative reproductive outcomes [8].
Table 1: Types of Clinical and Behavioral Outcomes for Validation
| Outcome Category | Definition | Examples in Reproductive Health |
|---|---|---|
| Biomarker Outcomes | Objective physiological or molecular measurements | Sperm count/motility, hormone levels (e.g., FSH, AMH), urinary or serum levels of EDCs [8] |
| Clinical Endpoints | Direct measures of disease or health status | Diagnosis of infertility, polycystic ovary syndrome (PCOS), endometriosis, time to conception [8] |
| Behavioral Outcomes | Objectively verified health-related actions | Verified use of prenatal supplements, adherence to medical regimens, documented attendance at wellness visits [89] |
| Patient-Reported Outcomes (PROs) | Reports of health status coming directly from the patient | Standardized quality of life scores, pain diaries, symptom tracking [90] |
Practical Validation Approaches and Protocols
Correlational Studies with Biomarkers and Clinical Records
The most direct method for validation involves collecting questionnaire data alongside objective clinical measures within a cohort study.
Protocol: Concurrent Validation with Clinical Biomarkers
- Participant Recruitment: Recruit a cohort that represents the target population for the questionnaire (e.g., couples trying to conceive, adolescents, women of reproductive age) [8] [89].
- Questionnaire Administration: Administer the reproductive health behavior questionnaire using a standardized protocol (e.g., self-completed electronically in a clinic setting to ensure confidentiality and consistent conditions) [89].
- Biospecimen Collection & Clinical Assessment: Collect biospecimens (blood, urine, saliva) for analysis of relevant biomarkers (e.g., EDC metabolites, reproductive hormones) concurrently with questionnaire completion [8]. Obtain relevant clinical data from medical records (e.g., semen analysis results, ovulatory status, diagnosis codes) with appropriate consent.
- Data Analysis: Conduct statistical analyses to test pre-specified hypotheses about the relationship between questionnaire scores and clinical measures. This typically involves correlation analysis (e.g., Pearson's r), regression models controlling for potential confounders (e.g., age, BMI), or comparing questionnaire scores across known groups (e.g., fertile vs. infertile) [8] [43].
Predictive Validation Studies
This robust design assesses the questionnaire's ability to predict future health states or events.
Protocol: Longitudinal Predictive Validation
- Baseline Assessment: Administer the questionnaire to a cohort at baseline.
- Follow-up Period: Follow the cohort over a clinically relevant time period (e.g., 12 months for couples trying to conceive).
- Outcome Ascertainment: Document the occurrence of key clinical events during follow-up (e.g., clinical pregnancy, live birth, onset of a reproductive condition).
- Data Analysis: Use survival analysis (e.g., Cox proportional hazards models) or logistic regression to determine if baseline questionnaire scores predict the likelihood of the outcome, again controlling for relevant covariates.
Integration with Existing Clinical Outcome Assessments (COAs)
Linking a new questionnaire to established COAs can provide strong evidence of validity.
Protocol: Convergence with Standardized Measures
- Selection of Comparator COAs: Identify well-validated, disorder-specific severity measures or cross-cutting symptom measures relevant to reproductive health. Examples include the PHQ-9 for depression or the DSM-5 Level 1 Cross-Cutting Symptom Measure [90].
- Concurrent Administration: Administer the new reproductive health questionnaire and the established COA(s) to the same participant group.
- Analysis of Convergence: Analyze the degree to which scores on the new questionnaire correlate with related domains on the established measures. This provides evidence for convergent validity. For example, one might hypothesize that poor reproductive health behaviors correlate with higher scores on anxiety or depression scales [90].
Table 2: Experimental Designs for Clinical Validation
| Design | Key Strength | Key Limitation | Statistical Methods |
|---|---|---|---|
| Concurrent Correlational | Efficient, provides initial evidence of relationship with clinical state | Cannot establish temporal sequence or causation | Correlation coefficients, multiple regression, ANOVA |
| Longitudinal Predictive | Establishes temporal precedence and predictive utility | Time-consuming, costly, potential for participant attrition | Cox regression, logistic regression, survival analysis |
| Known-Groups Validation | Intuitively clear evidence of discriminative ability | Requires pre-defined and accurately diagnosed groups | t-tests, Mann-Whitney U test, ANOVA |
| Intervention-Responsive | Demonstrates that scores change with expected clinical improvement | Requires a successful clinical trial or intervention | Paired t-tests, repeated measures ANOVA |
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Validation Studies
| Reagent/Material | Function in Validation | Example Application |
|---|---|---|
| Validated Clinical Outcome Assessments (COAs) | Serves as a gold-standard or comparator instrument to test convergent validity [90] | Using the PHQ-9 to validate a new questionnaire's correlation with mental health in infertility patients [89] [90] |
| Biomarker Assay Kits | Provides objective, quantitative physiological data for correlational analysis [8] | ELISA kits for measuring reproductive hormones (e.g., Estradiol, Testosterone) or EDC metabolites in urine/serum [8] |
| Electronic Data Capture (EDC) System | Standardizes questionnaire administration, ensures data integrity, and facilitates confidential data collection preferred by participants [89] | Using secure, HIPAA-compliant tablet-based surveys in clinic waiting rooms to administer questionnaires [89] |
| Statistical Analysis Software (with specific modules) | Enables performance of advanced psychometric and correlational analyses | Using IBM SPSS AMOS for Confirmatory Factor Analysis or R with lavaan package for structural equation modeling linking scores to outcomes [8] |
Workflow for Validation Against Behavioral and Clinical Outcomes
The following diagram illustrates the sequential, iterative process of validating a questionnaire against clinical and behavioral outcomes.
Integrating validation against behavioral and clinical outcomes is not an optional final step but a fundamental component of a rigorous reproductive health behavior questionnaire development protocol. This process grounds the instrument in biological and clinical reality, ensuring that the data it generates are not just statistically sound but also clinically meaningful. By systematically employing correlational, predictive, and known-groups designs, and by clearly linking questionnaire scores to biomarkers, clinical endpoints, and established COAs, researchers can build a compelling case for the utility of their instrument. This, in turn, empowers clinicians and public health professionals to reliably identify at-risk populations, evaluate the impact of interventions, and ultimately improve reproductive health outcomes.
Cross-Cultural Validation and Cognitive Testing in Multiple Countries
The development of reproducible and valid research instruments is paramount in reproductive health research. Cross-cultural validation ensures that questionnaires function as intended across diverse populations, while cognitive testing provides critical insights into how participants interpret and respond to items. This protocol outlines a standardized approach for the cross-cultural validation and cognitive testing of reproductive health questionnaires, drawing upon rigorous methodologies employed in recent global health research. Adherence to this protocol ensures that resulting data are comparable across settings and that instruments accurately capture the constructs they are designed to measure.
Core Principles and Foundational Knowledge
Cross-cultural validation is the process of establishing the equivalence and appropriateness of a research instrument when used in a cultural or linguistic context different from the one in which it was originally developed [91]. It addresses the challenge that psychological and health constructs may be expressed, understood, or valued differently across cultures. Without this process, measurements can be biased, leading to inaccurate findings and potentially ineffective interventions [91].
Cognitive testing is a qualitative method used to understand the response process of participants completing a survey. It investigates whether respondents understand items as intended, can retrieve relevant information, form judgments, and select responses that accurately reflect their situation [59] [92]. This is particularly critical for sensitive topics like reproductive health, where terminology and social norms can significantly influence responses.
Integrating these two processes is essential for developing a "global standard instrument" that is both comprehensible and acceptable to general populations in diverse global contexts, from high-income to low- and middle-income settings [59] [92].
Experimental Protocols
Protocol for Cross-Cultural Validation of a Reproductive Health Questionnaire
The following workflow outlines the multi-stage process for the cross-cultural validation of a questionnaire. This structured approach ensures linguistic, semantic, and conceptual equivalence between the original and adapted instruments.
Figure 1. Workflow for the cross-cultural adaptation of a questionnaire, based on established models like the Brislin method [80].
3.1.1 Step-by-Step Methodology:
- Forward Translation: The original instrument is translated into the target language by at least two independent bilingual translators with expertise in the relevant field (e.g., reproductive health). The goal is to produce a translation that is conceptually accurate, not just literally correct [80].
- Synthesis of Translations: The two translated versions are reviewed by a panel (often including the original translators and a coordinator) to resolve discrepancies and create a single consensus version.
- Back-Translation: The synthesized translated version is independently back-translated into the original language by one or more translators who were not involved in the initial forward translation and are blinded to the original instrument. This step helps identify potential misunderstandings or conceptual deviations introduced during the forward translation [80].
- Expert Panel Review: A multidisciplinary panel (e.g., including clinicians, methodologists, and language experts) reviews all versions of the questionnaire (original, translated, back-translated) and documentation. They evaluate equivalence across several dimensions [91]:
- Semantic Equivalence: Whether words and phrases have the same meaning.
- Idiomatic Equivalence: Whether colloquialisms and idioms are appropriately adapted.
- Experiential Equivalence: Whether the described situations are relevant and familiar in the target culture.
- Conceptual Equivalence: Whether the underlying construct is measured the same way in both cultures. The panel uses a content validity index (CVI) to quantitatively assess each item, typically retaining items with an item-level CVI (I-CVI) above 0.80 [8].
- Pilot Testing: The pre-final version of the questionnaire is administered to a small sample from the target population (e.g., 10-20 individuals) to assess comprehension, acceptability, and the time required for completion. Feedback on clarity and layout is incorporated [8].
- Final Version: The final adapted questionnaire is prepared for full psychometric validation.
Protocol for Cognitive Testing of a Reproductive Health Questionnaire
Cognitive interviewing is the core method for testing and refining a questionnaire. The following workflow details the iterative process of conducting and analyzing these interviews to improve question performance.
Figure 2. Iterative workflow for cognitive testing, based on the WHO Multi-Country Study protocol [59] [92].
3.2.1 Step-by-Step Methodology:
- Developing a Field Guide: Create a semi-structured interview guide that includes prompts for the interviewer. This includes concurrent probes (asked during the survey administration) and retrospective probes (asked after completion) to explore specific questions in depth [59] [92].
- Participant Recruitment and Sampling: Recruit a diverse sample of 15-30 participants per study site, purposively selected to represent variations in age, gender, education, geography (urban/rural), and other relevant demographics. Inclusion criteria should ensure participants are able and willing to provide informed consent and articulate their thought process [59] [93].
- Conducting the Interviews: Trained interviewers administer the draft questionnaire while employing cognitive interviewing techniques:
- Think-Aloud: Participants are instructed to verbalize their thoughts as they read each question, consider their answer, and select a response.
- Verbal Probing: Interviewers ask targeted follow-up questions to understand the participant's interpretation, such as "What does the term 'reproductive health' mean to you in your own words?" or "How did you arrive at that answer?" [59].
- Data Analysis: After each interview, researchers complete a standardized analysis matrix to document issues for every question. Analysis focuses on identifying:
- Cross-Site Analysis and Revision: Sites within a data collection "wave" (e.g., 5+ countries) hold joint analysis meetings to review findings and identify consistent "question failures." This collaborative process distinguishes local issues from those requiring universal revisions to the core instrument [59]. Revisions may involve re-wording, changing the order of questions, adding explanatory preambles, or removing items with limited cultural applicability.
Data Presentation and Analysis
The table below synthesizes key quantitative outcomes from recent validation and cognitive testing studies in reproductive health, demonstrating the application of the protocols described above.
Table 1: Psychometric and Cognitive Testing Outcomes from Select Reproductive Health Studies
| Study / Instrument Focus | Country / Region | Sample Size | Key Quantitative Findings | Primary Outcome |
|---|---|---|---|---|
| WHO Sexual Health Assessment of Practices and Experiences (SHAPE) [92] | 19 Countries | 645 cognitive interviews | Identified issues affecting acceptability, knowledge barriers, and interpretation. Willingness to answer sensitive items was high across sites. | A refined, globally comprehensible survey instrument. |
| Reproductive Health Behaviors for EDC Reduction [8] | South Korea | 288 adults | 4 factors, 19 items. Internal consistency (Cronbach's α = 0.80). All items met content validity index (CVI) > 0.80. | A reliable and valid 19-item questionnaire. |
| Sexual and Reproductive Empowerment Scale (SRE) Adaptation [80] | China | 581 nursing students | Cronbach's α = 0.89; Test-retest reliability (ICC) = 0.89; Scale-CVI = 0.96. Good model fit (CFI=0.91, RMSEA=0.07). | A culturally adapted, valid 21-item scale (C-SRES). |
| "AprendeLact" Questionnaire on Breastfeeding Knowledge [94] | Portugal | 57 nursing students | High internal consistency (KR-20 = 0.87). Excellent test-retest reliability (ICC = 0.899). | A valid and reliable Portuguese tool for assessing breastfeeding knowledge. |
| Female College Students' Reproductive Health [93] | Xinjiang, China | 625 students | 26.6% had menstrual disorders; 51.8% had dysmenorrhea; only 12.8% had undergone gynecological exams. Medical students had better knowledge (OR: 1.912). | Identified disparities in knowledge and health status, underscoring need for targeted education. |
Psychometric Parameters for Validation Studies
When performing cross-cultural validation, researchers must assess a suite of psychometric properties to ensure the instrument's robustness.
Table 2: Essential Psychometric Properties for Questionnaire Validation
| Property | Description | Standard/Benchmark | Common Assessment Method |
|---|---|---|---|
| Reliability | The consistency and stability of the measure. | ||
| Internal Consistency | The extent to which items measuring the same construct are interrelated. | Cronbach's α ≥ 0.70 (new tool) / ≥ 0.80 (established) [8] | Cronbach's Alpha |
| Test-Retest Reliability | The stability of scores over time when no change is expected. | Intraclass Correlation Coefficient (ICC) ≥ 0.70 [80] | Correlation between scores from the same participants at two time points. |
| Validity | The extent to which an instrument measures what it is intended to measure. | ||
| Content Validity | The degree to which an instrument adequately covers the thematic content of the construct. | Item-level CVI (I-CVI) ≥ 0.80; Scale-level CVI (S-CVI) ≥ 0.90 [8] [80] | Expert Panel Review |
| Construct Validity | The extent to which the instrument measures the theoretical construct. | ||
| • Convergent | Items within the same factor are highly correlated. | Factor loadings ≥ 0.40 - 0.50 [8] | Exploratory Factor Analysis (EFA) |
| • Discriminant | Items from different factors are not highly correlated. | Confirmatory Factor Analysis (CFA) | |
| • Model Fit | How well the factor structure fits the observed data. | CFI/GFI/IFI > 0.90; RMSEA < 0.08 [80] | Confirmatory Factor Analysis (CFA) |
The Scientist's Toolkit: Research Reagent Solutions
This section catalogs key methodological "reagents" — the essential tools and techniques — required for executing the protocols of cross-cultural validation and cognitive testing.
Table 3: Essential Research Reagents for Cross-Cultural Validation and Cognitive Testing
| Item / Solution | Function / Application in Protocol | Specific Examples / Notes |
|---|---|---|
| Brislin Translation Model | A formal protocol for forward-translation, back-translation, and reconciliation to achieve semantic equivalence [80]. | Fundamental first step for any cross-cultural adaptation. |
| Semi-Structured Field Guide | The interview protocol for cognitive testing, containing the survey and standardized verbal probes [59] [92]. | Ensures consistency and coverage across all interviewers. |
| Analysis Framework Matrix | A standardized data extraction sheet to systematically document findings from each cognitive interview [59]. | Allows for structured qualitative analysis and comparison across sites. |
| Content Validity Index (CVI) | A quantitative metric to assess the relevance of each item and the overall scale as rated by expert panels [8]. | I-CVI and S-CVI provide objective criteria for item retention. |
| Statistical Software Packages | For conducting psychometric analysis, including factor analysis and reliability testing. | IBM SPSS Statistics, IBM SPSS AMOS, R packages (e.g., 'lavaan', 'psych'). |
| Cognitive Interviewing Techniques | The specific methods used to elicit participants' thought processes. | "Think-aloud" and verbal probing (both concurrent and retrospective). |
Conclusion
The development of a rigorous reproductive health behavior questionnaire is a multi-stage, iterative process that integrates qualitative insight with quantitative rigor. A protocol grounded in a clear conceptual framework, validated through robust psychometric analysis, and refined using modern optimization strategies is paramount for creating tools that yield reliable and meaningful data. Future efforts must prioritize cross-cultural adaptation to ensure global applicability and embrace adaptive intervention designs, such as those facilitated by the MOST framework, to enhance the real-world impact of reproductive health research. By adhering to this comprehensive protocol, researchers can generate high-quality evidence to inform clinical practice, public health policy, and ultimately improve sexual and reproductive health outcomes across diverse populations.
References
- 1. Designing and validating a research questionnaire - Part 2 [https://pmc.ncbi.nlm.nih.gov/articles/PMC10810057/]
- 2. Designing and psychometric of reproductive health related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7398262/]
- 3. Advancing a Measure of Sexual and Reproductive Well-Being ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12332293/]
- 4. Online Health Information–Seeking Behaviors Among the ... [https://formative.jmir.org/2025/1/e56028]
- 5. Development and psychometric evaluation of the women shift ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-020-00994-9]
- 6. Sexual and reproductive health assessment scale in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12228241/]
- 7. Development of the oral, mental, and sexual reproductive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611828/]
- 8. Development and validation of a survey on reproductive ... [https://www.frontiersin.org/journals/reproductive-health/articles/10.3389/frph.2025.1519896/full]
- 9. Formative qualitative research on the potential for digital ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11216042/]
- 10. Presenting Your Qualitative Analysis Findings: Tables to ... [https://precisionconsultingblog.com/presenting-your-qualitative-analysis-findings-tables-to-include-in-chapter-4/]
- 11. Asking about sexual practices and experiences [https://www.who.int/teams/sexual-and-reproductive-health-and-research-(srh)/areas-of-work/sexual-health/asking-about-sexual-practices-and-experiences]
- 12. A statistical approach to quantitative data validation focused ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3795879/]
- 13. Developmental and Psychometric Properties of a Belief ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6123591/]
- 14. Development and Psychometric Evaluation of a ... [https://brieflands.com/journals/semj/articles/20464]
- 15. Reproducibility of Age at Menarche Gathered From Mail ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527403/]
- 16. A Cross-Sectional Quantitative Study on Sexual and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8471977/]
- 17. A cross-sectional mixed-methods study of sexual and ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-019-0698-5]
- 18. A Previsit Mobile Health App (Health-E You/Salud iTu) for ... [https://www.researchprotocols.org/2025/1/e77780]
- 19. Design and Implementation of the Surveys of Women [https://www.researchprotocols.org/2023/1/e40675/]
- 20. Standardizing Survey Data Collection to Enhance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299943/]
- 21. What to Do With All Those Open-Ended Responses? Data ... [https://www.surveypractice.org/article/25699-what-to-do-with-all-those-open-ended-responses-data-visualization-techniques-for-survey-researchers]
- 22. and psychometric evaluation of a women shift workers... Development [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-018-0456-0]
- 23. Sample size determination: A practical guide for health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000262/]
- 24. Sample Size Calculator [https://www.qualtrics.com/articles/strategy-research/calculating-sample-size/]
- 25. Quality and measurement properties of sexual health ... [https://www.sciencedirect.com/science/article/pii/S0738399124000405]
- 26. Design and psychometric properties of a questionnaire for ... [https://pubmed.ncbi.nlm.nih.gov/35980622/]
- 27. Review A primer on the use of cluster analysis or factor ... [https://www.sciencedirect.com/science/article/abs/pii/S0091743514002485]
- 28. Evaluation of the psychometric properties ... [https://pubmed.ncbi.nlm.nih.gov/36657958/]
- 29. Cluster Analysis of the Combined Association of Sleep and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7926961/]
- 30. Reproductive health literacy scale: a tool to measure the ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-025-01959-6]
- 31. Clustering of Unhealthy Behaviors: Protocol for a Multiple ... [https://www.researchprotocols.org/2021/6/e24887/]
- 32. Shaping the WHO Sexual Health Assessment of Practices ... [https://pubmed.ncbi.nlm.nih.gov/40888305/]
- 33. Exploratory Factor Analysis [https://www.publichealth.columbia.edu/research/population-health-methods/exploratory-factor-analysis]
- 34. Best Practices for Your Exploratory Factor Analysis [https://www.redalyc.org/journal/840/84072128005/html/]
- 35. A Practical Introduction to Factor Analysis - OARC Stats - UCLA [https://stats.oarc.ucla.edu/spss/seminars/introduction-to-factor-analysis/]
- 36. Exploratory Structural Equation Modeling [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2021.795672/full]
- 37. Exploratory Structural Equation Modeling: Practical Guidelines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8779472/]
- 38. Structural Equation Modeling: A Complete Guide [https://www.digitalocean.com/community/tutorials/structural-equation-modeling-complete-guide]
- 39. Structural equation modeling (SEM) in L2 writing research [https://www.sciencedirect.com/science/article/pii/S2772766125000230]
- 40. Reproductive Health Impact Study [https://www.guttmacher.org/reproductive-health-impact-study]
- 41. Statistical Methods for Item Reduction in a Representative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8976253/]
- 42. How to Know Which Items to Remove in a Questionnaire [https://measuringu.com/remove-items/]
- 43. Practical Guidelines to Develop and Evaluate a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8088187/]
- 44. A Step-By-Step Guide to Developing Effective Questionnaires ... [https://njaes.rutgers.edu/fs995/]
- 45. Survey Analysis of Quantitative and Qualitative Menstrual ... [https://pubmed.ncbi.nlm.nih.gov/37763628/]
- 46. How To Tell Stories with Data: 5 Tips [https://graduate.northeastern.edu/knowledge-hub/blog-how-to-tell-stories-with-data/]
- 47. Using the Multiphase Optimization Strategy (MOST ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6915979/]
- 48. The Multiphase Optimization Strategy (MOST) and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2062525/]
- 49. Applying the Multiphase Optimization Strategy for ... [https://www.sciencedirect.com/science/article/pii/S0885392420308861]
- 50. Using the multiphase optimization strategy to adapt cognitive ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-023-07669-3]
- 51. A Catalog of Biases in Questionnaires - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC1323316/]
- 52. How to choose and use scales in surveys [https://www.enalyzer.com/articles/how-to-choose-and-use-scales-in-surveys]
- 53. Wording Bias: What it is with Examples [https://www.questionpro.com/blog/wording-bias/]
- 54. Designing and validation of a reproductive health need ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-022-01342-9]
- 55. Writing Survey Questions [https://www.pewresearch.org/writing-survey-questions/]
- 56. Why Scale questions in surveys suck | by Christina Teklina [https://medium.com/design-bootcamp/why-scale-questions-in-surveys-suck-9574e97595f7]
- 57. Scale development: ten main limitations and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6966966/]
- 58. Cognitive interviews to improve a patient-centered ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6478498/]
- 59. Cognitive testing of a survey instrument to assess sexual ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-021-01301-w]
- 60. Improving abortion underreporting in the USA: a cognitive ... [https://www.guttmacher.org/article/2022/08/improving-abortion-underreporting-usa-cognitive-interview-study]
- 61. Comparison of Evaluation Methods for Improving the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10923187/]
- 62. The Efficiency of Conducting Concurrent Cognitive ... [https://www.surveypractice.org/article/2887-the-efficiency-of-conducting-concurrent-cognitive-interviewing-and-usability-testing-on-an-interviewer-administered-survey]
- 63. Categorical vs. Quantitative Data: The Difference [https://www.fullstory.com/blog/categorical-vs-quantitative-data/]
- 64. Categorical vs quantitative data: which holds more insights? [https://contentsquare.com/blog/categorical-vs-quantitative-data/]
- 65. Parent-Teen Sexual Health Communication and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590298/]
- 66. Interventions targeting healthcare providers to optimise use of ... [https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-022-08783-9]
- 67. Validation of a Questionnaire on Sexual and Reproductive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10469261/]
- 68. Sexual and reproductive health assessment scale in women ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-025-02061-7]
- 69. Data and Statistics | Reproductive Health [https://www.cdc.gov/reproductive-health/data-statistics/index.html]
- 70. The sociocultural context of sexual and reproductive health ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-025-02155-2]
- 71. Protocol for an Address-Based Sampling Multimodal Study [https://pubmed.ncbi.nlm.nih.gov/36920469/]
- 72. Top 6 Visualizations for Quantitative Data Analysis Methods [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 73. Sexual and Reproductive Health Service Seeking Scale ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10837854/]
- 74. Development and validation of the reproductive health literacy ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-021-01278-6]
- 75. Development and validation of the reproductive health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8590315/]
- 76. Construction and validation of a reproductive behavior ... [https://pubmed.ncbi.nlm.nih.gov/37335407/]
- 77. Test–Retest Reliability of Self-Reported Sexual Behavior ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2017.00172/full]
- 78. Reproducibility of an extensive self-report questionnaire ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5405837/]
- 79. The Internal Reliability and Construct Validity of ... [https://www.mdpi.com/2227-9032/11/15/2168]
- 80. Sexual and reproductive empowerment scale for adolescents ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619207/]
- 81. Development and psychometric assessment of the sexual ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-022-14400-5]
- 82. A Questionnaire-Based Study to Evaluate Health-Related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8725340/]
- 83. Identifying the reproductive health indicators for population ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-025-02000-6]
- 84. Identifying the reproductive health indicators for population ... [https://pubmed.ncbi.nlm.nih.gov/40537789/]
- 85. A comparison of four scoring methods based on the parent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2359742/]
- 86. study protocol for a randomized controlled trial | Reproductive ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-024-01867-1]
- 87. Clinical Outcome Assessments: Conceptual Foundation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4610138/]
- 88. Clinical Outcome Assessments Are Never “Validated” [https://www.sciencedirect.com/science/article/abs/pii/S1098301524027876]
- 89. A Validation Study of the Total Teen Assessment - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12329912/]
- 90. DSM-5-TR Online Assessment Measures [https://www.psychiatry.org/psychiatrists/practice/dsm/educational-resources/assessment-measures]
- 91. The Cross-Cultural Validation of Neuropsychological ... [https://www.mdpi.com/1660-4601/21/8/1110]
- 92. Cognitive testing in 19 countries to refine WHO's Sexual ... [https://pubmed.ncbi.nlm.nih.gov/39611192/]
- 93. Comparative analysis of reproductive health knowledge ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12334665/]
- 94. CROSS-CULTURAL ADAPTATION AND VALIDATION OF ... [https://www.sciencedirect.com/science/article/pii/S0266613825003389]