A Comparative Analysis of Data Mining Algorithms for Establishing Thyroid Hormone Reference Intervals
Establishing accurate reference intervals (RIs) for thyroid hormones is a critical challenge in clinical diagnostics and biomedical research.
A Comparative Analysis of Data Mining Algorithms for Establishing Thyroid Hormone Reference Intervals
Abstract
Establishing accurate reference intervals (RIs) for thyroid hormones is a critical challenge in clinical diagnostics and biomedical research. This article provides a comprehensive comparison of contemporary data mining algorithms—including Hoffmann, Bhattacharya, Expectation-Maximization (EM), kosmic, and refineR—for deriving RIs from real-world data. We explore the foundational principles of both direct and indirect approaches, detail the methodological application of each algorithm, address common challenges like data skewness and class imbalance, and present a rigorous validation framework using metrics such as the Bias Ratio matrix. Aimed at researchers and drug development professionals, this review synthesizes evidence to guide the selection and optimization of data mining paths for establishing robust, population-specific thyroid hormone RIs, ultimately enhancing diagnostic accuracy and patient stratification in clinical trials.
The Critical Foundation: Understanding Reference Intervals and the Data Mining Imperative in Thyroid Diagnostics
The precise definition of Reference Intervals (RIs) for thyroid hormones is a cornerstone of both clinical diagnostics and pharmaceutical development. These intervals establish the population-based limits of normal thyroid function, directly impacting patient diagnoses and serving as critical endpoints in trials for novel therapies. Historically, laboratories relied on manufacturer-provided RIs, which often failed to account for local population variations and the biological heterogeneity of thyroid-stimulating hormone (TSH), free thyroxine (fT4), and free triiodothyronine (fT3) [1] [2]. The emergence of indirect data mining methods, which leverage vast datasets from laboratory information systems, has revolutionized this field. These methods offer a cost-effective and population-specific alternative to the logistically challenging direct method of establishing RIs [1] [3] [2]. This guide provides a comparative analysis of the data mining algorithms driving this paradigm shift and explores their integral role in the parallel development of Thyroid Hormone Receptor beta (THRβ)-selective agonists, a promising new class of therapeutics for metabolic diseases.
Comparative Analysis of Data Mining Algorithms for RI Establishment
The performance of data mining algorithms for establishing RIs varies significantly based on data source characteristics and distribution. The table below summarizes the optimal applications of five key algorithms based on recent comparative studies.
Table 1: Performance Comparison of Data Mining Algorithms for Thyroid Hormone RI Establishment
| Algorithm | Optimal Data Source | Performance Characteristics | Recommended Use Case |
|---|---|---|---|
| Expectation Maximization (EM) | Patient data with significant skewness [4] [5] | High consistency for TSH RIs with standard methods; performance limited for other hormones [5] | Skewed datasets, particularly for establishing TSH RIs [4] |
| Transformed Hoffmann | Physical examination data [4] | Good performance for calculating RIs from Gaussian or near-Gaussian distributions [4] [5] | Physical examination populations with Gaussian-distributed data |
| Transformed Bhattacharya | Physical examination data [4] | Good performance for calculating RIs from Gaussian or near-Gaussian distributions [4] [5] | Physical examination populations with Gaussian-distributed data |
| kosmic | Physical examination data [4] | Good performance for calculating RIs from Gaussian or near-Gaussian distributions [4] | Physical examination populations with Gaussian-distributed data |
| refineR | Physical examination data [4] [5] | Good performance for calculating RIs from Gaussian or near-Gaussian distributions [4] [5] | Physical examination populations with Gaussian-distributed data |
Experimental Protocols and Validation
The validation of these algorithms typically follows a rigorous protocol involving derived databases. A standard approach involves creating two datasets: a Reference data set, where reference individuals are selected using strict inclusion/exclusion criteria to establish "standard RIs," and a Test data set, typically a physical examination population downloaded directly from the Laboratory Information System [3] [5]. The algorithm-calculated RIs from the Test data set are then compared against the standard RIs.
Objective assessment is often implemented using a Bias Ratio (BR) matrix [4] [5]. A lower BR indicates higher consistency between the algorithm-derived RI and the standard RI. For example, one study found a high consistency between TSH RIs established by the EM algorithm and standard TSH RIs, with a BR of 0.063 [5]. The 90% confidence intervals of the upper and lower limits are also compared, with successful validation achieved when the limits of the test RIs fall within the 90% CI of the standard RIs, and consistency rates in external databases exceed 98% [3].
The Critical Role of RIs in Drug Development: THRβ-Selective Agonists
The establishment of precise RIs is not solely a diagnostic imperative; it is equally critical in the development of novel therapeutics, particularly selective THRβ agonists. The rationale for these drugs stems from the distinct tissue distribution of thyroid hormone receptor subtypes: THRα is highly expressed in the heart and bone, while THRβ is the primary mediator in the liver [6] [7] [8]. Although natural thyroid hormones (T3) can activate lipid metabolism via THRβ, their non-selective action on THRα leads to deleterious side effects, including tachycardia, bone loss, and muscle wasting [6] [8] [9]. This makes natural T3 a poor therapeutic candidate and underscores the need for receptor-selective analogues.
Accurate RIs for TSH, fT4, and fT3 are essential in clinical trials for these agonists to ensure that therapeutic dosages effectively activate THRβ without suppressing TSH beyond the normal range or causing overt thyrotoxicosis, thereby monitoring for off-target effects [9].
Key THRβ Agonists in Development
Several THRβ-selective agonists have been developed, with varying degrees of selectivity and clinical progress.
Table 2: Comparison of Selective THRβ Agonists in Development
| Drug Compound | THRβ Selectivity | Primary Indications | Key Findings & Clinical Status |
|---|---|---|---|
| ZTA-261 | Higher selectivity than GC-1 [6] | Dyslipidemia, Obesity [6] | Reduces serum/liver lipids and visceral fat in HFD mice; significantly lower bone, cardiac, and hepatotoxicity than GC-1 [6] |
| GC-1 (Sobetirome) | 10-fold selective for THRβ over THRα [9] | Hypercholesterolemia, NAFLD [9] | Effective in preclinical models; clinical trials for hypercholesterolemia terminated [9] |
| KB-2115 (Eprotirome) | ~20-fold selective for THRβ [9] | Hypercholesterolemia [9] | Phase 3 trial halted due to cartilage damage in animals and elevated liver enzymes in patients [9] |
| MGL-3196 (Resmetirom) | ~30-fold selective for THRβ [9] | NASH, NAFLD [7] [9] | Reduces LDL cholesterol and triglycerides; shows promise in NASH treatment [9] |
Mechanism of Action of THRβ Agonists
The lipid-lowering effects of THRβ agonists are mediated through a pathway distinct from statins, offering potential for combination therapy. They act primarily in the liver to upregulate key processes.
Diagram 1: THRβ agonist mechanism of action
Experimental Workflow: From RI Establishment to Therapeutic Validation
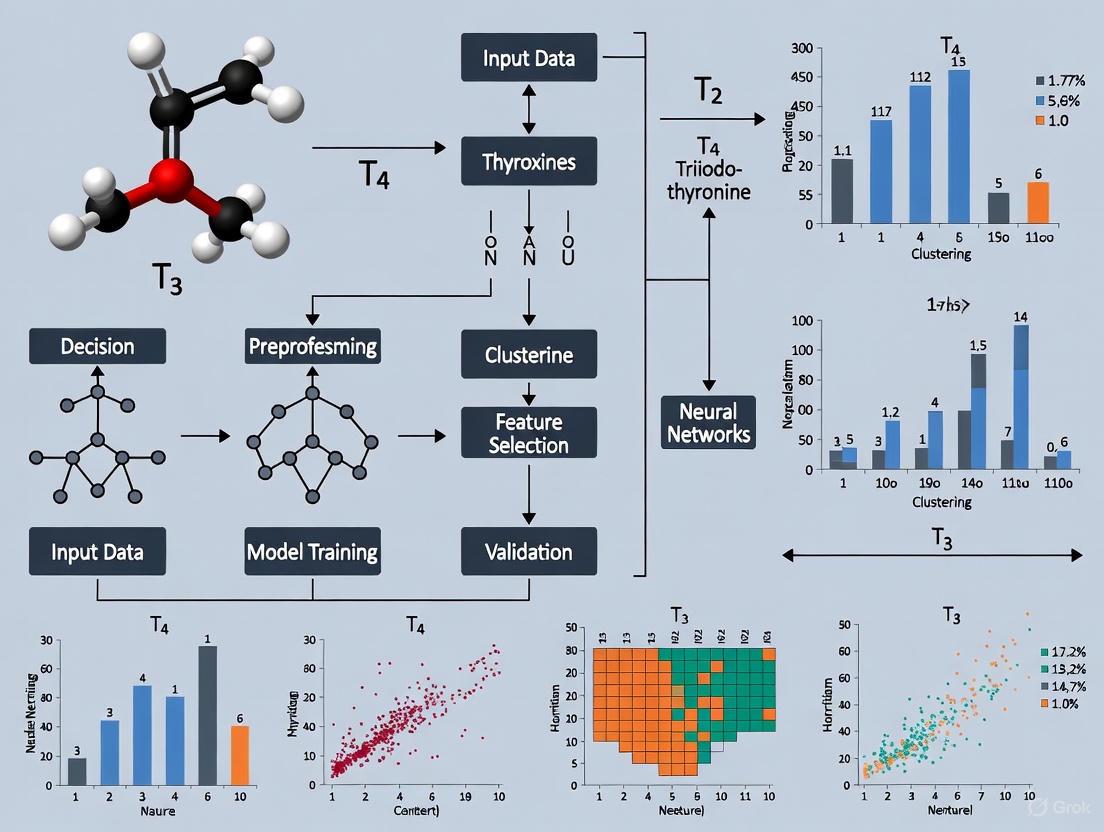
The integration of RI establishment and drug development can be visualized as a cohesive workflow, from initial data collection to final preclinical validation.
Diagram 2: Integrated research workflow
Key Assays and Research Reagents
The experiments cited in this guide rely on a suite of well-defined laboratory assays and reagents. The following table details these essential research tools.
Table 3: Key Research Reagent Solutions for Thyroid Hormone and Metabolic Research
| Research Reagent / Assay | Function and Application | Experimental Context |
|---|---|---|
| Electrochemiluminescence Immunoassay (e.g., Roche Cobas e801) | Quantification of TSH, fT4, fT3, Anti-TPO, and Anti-Tg in serum [1] [2] | RI establishment from patient/plasma samples; diagnostic classification. |
| [¹²⁵I]-T3-Displacement Assay | In vitro competitive binding assay to determine affinity and selectivity of analogs for THRα vs. THRβ [6] | Preclinical screening of THRβ agonist selectivity (e.g., ZTA-261). |
| High-Fat Diet (HFD) Induced Obesity Mouse Model | In vivo model for studying dyslipidemia, obesity, and NAFLD/NASH [6] | Evaluation of drug efficacy on body weight, visceral fat, and serum/liver lipids. |
| In Vitro Translation System (e.g., TNT T7 Quick Coupled System) | Synthesis of full-length human THRα and THRβ proteins for binding studies [6] | Provision of target receptors for competitive ligand binding assays. |
| ALT (Alanine Aminotransferase) Measurement | Standard clinical chemistry assay to assess potential hepatotoxicity [6] | Preclinical and clinical safety profiling of drug candidates. |
| Histological Analysis (Heart & Bone) | Microscopic examination of tissues for signs of toxicity (e.g., cartilage damage, fibrosis) [6] [9] | Critical for identifying off-target effects mediated by THRα. |
The fields of thyroid hormone diagnostics and drug development are increasingly intertwined, both relying on advanced data science and a deep understanding of thyroid physiology. The validation of indirect data mining algorithms like refineR, kosmic, and EM provides laboratories with a powerful, practical means to establish population-specific RIs, which in turn leads to more accurate diagnosis and avoids misclassification, especially in older adults [4] [10]. Concurrently, the successful development of THRβ-selective agonists like ZTA-261 and resmetirom demonstrates a targeted application of basic science to overcome the historical limitations of native thyroid hormone therapy [6] [7]. The future of this integrated field lies in the continued refinement of algorithms to handle diverse demographic partitions and the ongoing clinical translation of selective agonists, with the shared goal of delivering personalized and effective patient care for thyroid and metabolic disorders.
The establishment of accurate reference intervals (RIs) for thyroid hormones is a fundamental requirement in clinical diagnostics, directly impacting the identification and management of thyroid disorders. For decades, the direct method—involving the recruitment of carefully selected healthy individuals—has been considered the gold standard for establishing these RIs as recommended by the Clinical and Laboratory Standards Institute (CLSI) [2] [10]. However, this approach presents substantial practical challenges that limit its implementation. This article examines these limitations and explores how data mining algorithms applied to existing clinical data offer a viable, efficient, and cost-effective alternative for establishing reliable thyroid hormone RIs.
The Burden of Direct Method Implementation
Substantial Financial Costs and Resource Demands
The direct method requires significant financial investment due to its labor-intensive nature. The process involves:
- Recruitment expenses for identifying and enrolling eligible participants
- Personnel costs for administering questionnaires and conducting physical examinations
- Laboratory expenses for comprehensive testing to confirm health status
- Operational overhead for data management and statistical analysis
These substantial costs make the direct method prohibitively expensive for many clinical laboratories, particularly those with limited budgets [2].
Time-Consuming Implementation Process
The timeline for establishing RIs through direct methods is exceptionally lengthy:
- Participant recruitment can take months to years to identify sufficient numbers of qualified individuals
- Health status verification requires thorough screening processes
- Data collection and analysis involves extensive procedures
This extended timeline delays the implementation of population-specific RIs, potentially impacting diagnostic accuracy in the interim [2].
Stringent Participant Recruitment Challenges
The direct method demands rigorous participant selection with strict exclusion criteria, creating significant recruitment difficulties:
- Stringent health requirements must exclude individuals with any conditions potentially affecting thyroid function
- Large sample sizes are needed—CLSI guidelines recommend at least 120 reference individuals per partition [11]
- Demographic stratification requires sufficient participants across age, gender, and other relevant subgroups
These challenges are particularly pronounced for special populations such as elderly individuals, where comorbidities are more common and further complicate recruitment [10].
Data Mining Algorithms: A Viable Alternative Pathway
In response to these challenges, indirect methods utilizing data mining algorithms have emerged as a practical alternative. These methods leverage existing laboratory data, bypassing the need for costly and time-consuming prospective studies.
Key Data Mining Algorithms for Thyroid Hormone RI Establishment
| Algorithm | Underlying Principle | Data Type Compatibility | Strengths | Notable Performance Findings |
|---|---|---|---|---|
| Hoffmann | Graphical method identifying Gaussian distribution of healthy population within mixed data [12] [13] | Gaussian or near-Gaussian distributions [13] | Simple, intuitive visualization; reliable for TSH verification [12] | Produced RIs for free T3 and T4 comparable to kit literature [12] |
| Bhattacharya | Graphical separation of healthy population distribution via logarithmic transformation [13] | Gaussian or near-Gaussian distributions [13] | Effective graphical approach; minimal technical requirements | Showed good performance with physical examination data [4] |
| KOSMIC | Box-Cox transformation with Kolmogorov-Smirnov distance minimization for optimal truncation limits [12] | Handles skewed distributions via transformation [13] | Open-source availability; web-based implementation | Higher upper reference limits for TSH compared to kit literature [12] |
| refineR | Multi-level grid search for optimal model parameters through inverse modeling [12] | Handles skewed distributions [13] | Bootstrap confidence intervals; robust parameter estimation | Reliable RI verification for free T3 and free T4 [12] |
| Expectation-Maximization | Iterative algorithm estimating parameters of underlying healthy population distribution [5] | Effective for data with significant skewness [5] | Handles highly skewed data effectively | High consistency for TSH RIs with patient data [4] [14] |
Experimental Protocols and Validation Studies
Recent research has established rigorous protocols for validating data mining algorithms in thyroid hormone RI establishment:
Study Design and Data Sourcing
- Dual-database approach: Studies typically create both "Reference" and "Test" datasets [5] [13]
- Reference datasets: Established using strict inclusion/exclusion criteria with physical examination populations
- Test datasets: Derived from laboratory information systems with simplified preprocessing
- Data preprocessing: Involves random sampling for demographic balance and outlier detection using Tukey's method [13]
Performance Validation Methods
- Bias Ratio Matrix: Provides objective assessment by comparing algorithm-derived RIs with standard RIs [5]
- Consistency Evaluation: Measures agreement between RIs established via different methods [3]
- Clinical Impact Assessment: Evaluates potential misclassification rates using different RI sources [10]
Key Validation Findings
- For elderly populations, the transformed Hoffmann, Bhattacharya, KOSMIC, and refineR algorithms showed good performance with physical examination data [4] [14]
- For non-elderly adults, Hoffmann, Bhattacharya, and refineR methods produced RIs for free and total thyroid hormones that closely matched standard RIs [5]
- The EM algorithm demonstrated particular effectiveness for establishing TSH RIs from patient data in older adults [4] [14]
Algorithm Selection Workflow for Indirect RI Establishment
Comparative Performance of Algorithms Across Scenarios
Performance Across Different Data Types
| Algorithm | Physical Examination Data | Patient Data | Elderly Population | Non-Elderly Adults |
|---|---|---|---|---|
| Hoffmann | Good performance [4] [14] | Variable performance | Recommended with transformation [4] | Reliable for FT3, FT4, TT3, TT4 [5] |
| Bhattacharya | Good performance [4] [14] | Variable performance | Recommended with transformation [4] | Reliable for FT3, FT4, TT3, TT4 [5] |
| KOSMIC | Good performance [4] [14] | Higher TSH URL [12] | Recommended [4] | Performance varies by hormone |
| refineR | Good performance [4] [14] | Higher TSH URL [12] | Recommended [4] | Reliable for FT3, FT4, TT3, TT4 [5] |
| EM | Limited performance on some hormones [5] | Excellent for TSH [4] [14] | Recommended for patient data [4] | Effective for skewed data [5] |
Clinical Implications of Algorithm Selection
The choice of algorithm has direct diagnostic implications. One study found that using RIs derived through indirect methods prevented potential misdiagnosis of subclinical hypothyroidism in 6.5% of subjects aged 60-79 years and 12.5% of subjects aged 80 years or older compared to using manufacturer's ranges without age stratification [10].
Decision Framework for Algorithm Selection in Thyroid Hormone RI Establishment
The Scientist's Toolkit: Essential Research Reagent Solutions
| Tool/Reagent | Function | Application Notes |
|---|---|---|
| Laboratory Information System (LIS) Data | Retrospective data source containing demographic and test result information | Foundation for indirect method; requires ethical approval for use [12] [2] |
| R Statistical Software | Open-source platform for data analysis and algorithm implementation | Essential for refineR algorithm; enables custom analytical workflows [12] |
| Python Programming Environment | Implementation platform for KOSMIC algorithm | Open-source alternative; requires technical expertise [12] |
| Box-Cox Transformation | Statistical method to normalize skewed data distributions | Critical preprocessing step for non-Gaussian distributions [12] [13] |
| Bias Ratio Matrix | Objective metric for comparing algorithm performance against standard RIs | Validation tool for assessing clinical applicability [5] |
| Electrochemiluminescence Immunoassay | Analytical method for precise thyroid hormone measurement | Used in systems from Roche, Siemens; ensures result reliability [2] [11] |
The limitations of traditional direct methods for establishing thyroid hormone reference intervals—prohibitive costs, extensive timelines, and recruitment challenges—are effectively addressed by data mining algorithms applied to existing clinical data. Research demonstrates that algorithms including Hoffmann, Bhattacharya, KOSMIC, refineR, and Expectation-Maximization can produce reliable RIs when appropriately matched to data characteristics and population needs. These indirect methods represent a practical, cost-effective, and scientifically valid approach for clinical laboratories to establish population-specific thyroid hormone reference intervals, ultimately enhancing the accuracy of thyroid disorder diagnosis and management across diverse patient populations.
The establishment of accurate reference intervals (RIs) is a cornerstone of clinical diagnostics, providing the essential benchmarks against which patient laboratory results are interpreted to determine health status. For thyroid hormones, which are crucial for diagnosing and managing pervasive metabolic disorders, the precision of these intervals is paramount. Traditionally, RIs have been established through direct methods, which involve recruiting and testing a cohort of strictly defined healthy individuals. However, this process is prohibitively expensive, time-consuming, and fraught with ethical and practical challenges related to participant recruitment [12].
This review explores the paradigm shift towards indirect methods, which leverage the vast reservoirs of Real-World Data (RWD) stored within Laboratory Information Systems (LIS). These methods use sophisticated data mining algorithms to statistically separate the results of presumably healthy individuals from the mixed patient data typically found in a hospital setting. By framing this discussion within the specific context of thyroid hormone reference intervals, we will objectively compare the performance, protocols, and applicability of the leading algorithms driving this innovative approach.
The Imperative for Indirect Methods in Thyroid Testing
The limitations of the direct approach are particularly acute in the field of thyroid testing. Scientific literature and reagent manufacturers consistently advise each laboratory to establish its own RIs for all analytes [12]. This is because RIs for thyroid hormones are known to vary due to differences in regional iodine consumption, the specific analytical techniques used, and patient covariates such as ethnicity, geographic region, sex, and age [12] [15] [10].
Failing to account for these factors can lead to misdiagnosis. For instance, a study focusing on elderly populations found that using manufacturer-provided RIs without age stratification would have led to a misdiagnosis of elevated TSH in 6.5% of subjects aged 60-79 and 12.5% of those over 80 years, potentially labeling them with subclinical hypothyroidism unnecessarily [10]. Indirect methods offer a practical solution to this problem by allowing laboratories to inexpensively derive RIs that are tailored to their local patient population and specific analytical platforms.
Table 1: Key Challenges in Thyroid Hormone Reference Intervals and the Indirect Solution
| Challenge | Impact on Reference Intervals (RIs) | Indirect Method Solution |
|---|---|---|
| Regional & Population Variation | RIs differ based on iodine intake, ethnicity, and geography [12] | Enables establishment of local RIs from a laboratory's own patient data. |
| Analytical Method Dependence | RIs are not transferable between different instrument platforms [12] | Allows verification of RIs for the specific analytical method in use. |
| Age & Sex Stratification | TSH levels increase with age, while FT3 and FT4 decrease, necessitating age-specific RIs [15] [10] | Facilitates cost-effective creation of stratified RIs from large datasets. |
| High Cost & Logistics | Direct method is expensive, slow, and ethically challenging [12] [13] | Utilizes pre-existing LIS data, making RI establishment highly cost-effective. |
A Comparative Analysis of Key Data Mining Algorithms
Several data mining algorithms have been developed and refined for the purpose of establishing RIs from RWD. These algorithms operate on different statistical principles and demonstrate varying strengths. The most prominent include the Hoffman, Bhattacharya, Expectation-Maximization (EM), KOSMIC, and refineR methods [13].
Algorithm Workflows and Principles
The following diagram illustrates the general logical workflow shared by many of these indirect methods for processing LIS data to establish RIs.
While the overall workflow is similar, the core modeling principles differ significantly between algorithms. The table below summarizes the key characteristics of each major method.
Table 2: Comparison of Indirect Algorithms for RI Establishment
| Algorithm | Core Principle | Key Strengths | Key Limitations | Software/Code Availability |
|---|---|---|---|---|
| Hoffman | Graphical method; identifies Gaussian distribution of physiological results [12] [13] | Simple, intuitive, reliable for TSH [12] | Assumes Gaussian distribution; requires visual identification [12] | Can be computerized [12] |
| Bhattacharya | Graphical separation of Gaussian distributions in mixed data [13] | Widely used, relatively simple to understand [13] | Assumes data is Gaussian or near-Gaussian [13] | - |
| EM Algorithm | Iterative estimation of parameters in mixed distributions [13] | Effective for handling significantly skewed data [13] | Complex principles; performance can be variable [13] | - |
| KOSMIC | Box-Cox transformation & Kolmogorov-Smirnov distance minimization on truncated data [12] | Handles non-Gaussian data; high performance in benchmarks; open-source [12] [13] | Can overestimate upper limits for TSH [12] | Python; Web tool [12] |
| refineR | Multi-level grid search for optimal model parameters via inverse modeling [12] [13] | Handles skewed data; accurate in benchmarks; open-source [12] [13] | Can overestimate upper limits for TSH [12] | R package [12] |
Objective Performance Comparison in Thyroid Hormone Testing
Multiple studies have directly compared the performance of these algorithms in establishing RIs for thyroid hormones. The results indicate that performance can vary significantly depending on the specific analyte.
A 2023 study by BMC Medical Research Methodology objectively evaluated five algorithms using a Bias Ratio (BR) matrix, where a lower BR indicates better agreement with standard RIs derived from a rigorously selected reference population. The study found that the EM algorithm showed high consistency with standard TSH RIs (BR=0.063), though it performed poorly on other hormones. The Hoffman, Bhattacharya, and refineR methods all produced comparable and accurate RIs for FT3, FT4, TT3, and TT4 [13].
Another 2023 study focused on verifying RIs for thyroid hormones in an adult hospital population. It reported that for Free T3 and Free T4, the indirect RIs derived from Hoffman, KOSMIC, and refineR were all comparable to the ranges provided in the kit literature. However, for TSH, a critical marker for hypothyroidism, the newer automated methods KOSMIC and refineR showed higher Upper Reference Limits (URL) compared to the kit insert (KOSMIC: 7.00 mIU/L; refineR: 8.19 mIU/L vs. IFU: 4.28 mIU/L). In contrast, the computerized Hoffman method produced a TSH URL (4.0 mIU/L) that was comparable to the kit literature [12]. This suggests that while newer methods are excellent for most thyroid hormones, the choice of algorithm for TSH requires careful consideration.
Table 3: Experimental Thyroid Hormone RI Results from Indirect Methods (2023 Study) [12]
| Parameter | Reference Range in IFU | Hoffman Method | KOSMIC Method | refineR Method |
|---|---|---|---|---|
| Serum TSH (mIU/L) | 0.38 - 4.28 | 0.3 - 4.0 | 0.53 - 7.00 | 0.55 - 8.19 |
| Free T3 (pg/mL) | 2.1 - 4.4 | 2.4 - 5.0 | 2.37 - 5.22 | 2.11 - 5.15 |
| Free T4 (ng/dL) | 0.61 - 1.12 | 0.6 - 1.2 | 0.57 - 1.18 | 0.61 - 1.32 |
Detailed Experimental Protocols for Indirect RI Establishment
To ensure reproducibility, it is critical to understand the experimental and data preprocessing protocols used in comparative studies. The following workflow details the steps involved in a typical comparative study of indirect algorithms.
Data Collection and Preprocessing
The foundational step involves the extraction of a large volume of retrospective laboratory data. For example, one study retrieved 63,469 results for TSH, 49,371 for Free T3, and 49,390 for Free T4 from their LIS over a period of one and a half years [12]. Another study used a two-step preprocessing protocol: first, random sampling was applied to balance the sex ratio and age composition of the dataset, and second, the Tukey method was used to identify and remove outliers within each subgroup [13]. Data quality is paramount, and protocols should follow standards like ISO 15189:2012 to ensure analytical accuracy and precision [12].
Algorithm Implementation and Statistical Analysis
Each algorithm is then applied to the preprocessed test data set.
- Hoffman Method: This method was computerized as described by Katayev et al. It operates on the assumption of a Gaussian distribution for physiological results and involves the visual identification of the physiological portion of the data [12].
- KOSMIC Method: This method, proposed by Zierk et al., applies a Box-Cox transformation to the data. It then fits a Gaussian distribution to various truncated portions of the observed data, selecting the truncation with the smallest Kolmogorov-Smirnov distance as the healthy distribution. The RI is then derived from this optimized model [12]. It is available as open-source Python code or a web tool.
- refineR Method: This algorithm, proposed by Tatjana et al., uses a multi-level grid search in an inverse modeling approach. It searches for optimal model parameters (like the power parameter λ, σ, μ, and a scaling factor) to find the model that best describes the underlying healthy population distribution. The
refineRR package is used for implementation, and confidence intervals can be determined via bootstrapping [12].
Performance is typically evaluated by comparing the calculated RIs to a gold standard, such as RIs from kit inserts (IFU) or, more rigorously, RIs derived from a directly selected reference population, using metrics like the Bias Ratio [13].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successfully implementing indirect methods for RI establishment requires a combination of data, computational tools, and analytical resources.
Table 4: Essential Research Reagents and Solutions for Indirect RI Studies
| Item Name | Function/Description | Example from Literature |
|---|---|---|
| Laboratory Information System (LIS) | Source of real-world data (RWD); contains historical patient test results for analysis. | LIS of B. J. Medical College (63,469+ TSH results) [12]; PUMC Hospital LIS [13]. |
| Immunoassay Analyzer & Reagents | Platform for precise measurement of thyroid hormones; source of manufacturer's RIs (IFU). | Beckman Coulter DxI 600 [12]; Siemens ADVIA Centaur XP [13]; Roche Elecsys [16]. |
| Statistical Computing Software | Environment for implementing algorithms, data preprocessing, and statistical analysis. | R software (for refineR, data cleaning) [12] [13]; Python (for KOSMIC) [12]. |
| Quality Control (QC) Materials | Ensures ongoing accuracy and precision of analytical results, upholding data integrity. | ISO 15189:2012 protocols [12]; Internal QC and CAP accreditation [13]. |
| Algorithm-Specific Packages | Pre-written code for executing complex indirect algorithms. | refineR R package [12]; KOSMIC Python code or web tool [12]. |
The rise of the indirect approach, powered by data mining algorithms applied to RWD, represents a significant advancement in the field of laboratory medicine. For the establishment of thyroid hormone reference intervals, methods like KOSMIC and refineR have demonstrated high performance and reliability for Free T3 and Free T4, while the Hoffman method remains a robust, particularly for TSH in certain populations. The choice of algorithm is not one-size-fits-all; it requires consideration of the specific analyte, data distribution, and the clinical context.
The experimental data and protocols detailed in this guide provide researchers and laboratory professionals with a evidence-based framework for evaluating and implementing these powerful tools. As these methods continue to mature and become more accessible, they promise to make the establishment of accurate, population-specific RIs a standard and routine practice, thereby enhancing the quality and precision of patient diagnosis and care.
The establishment of accurate reference intervals (RIs) is a fundamental requirement in laboratory medicine, providing the essential context for interpreting patient test results and facilitating clinical decision-making. For thyroid hormones, which play a critical role in metabolic regulation, the need for population-specific RIs is particularly important given the substantial biological variation observed across different demographic groups and geographic populations. Traditional direct methods for establishing RIs face significant practical challenges, including stringent participant recruitment criteria, substantial financial costs, and time-consuming processes.
Data mining algorithms applied to real-world data (RWD) have emerged as powerful indirect alternatives that leverage the vast amounts of routine clinical measurements stored in laboratory information systems [13]. These computational approaches can distinguish the underlying distribution of healthy individuals within mixed datasets that include both normal and pathological results. This article provides a comprehensive technical comparison of five established data mining algorithms—Hoffmann, Bhattacharya, Expectation-Maximization (EM), kosmic, and refineR—focusing on their application to thyroid hormone reference interval establishment.
Algorithm Methodologies and Technical Profiles
Fundamental Principles and Mechanisms
The five algorithms employ distinct mathematical approaches to separate the distribution of healthy individuals from mixed clinical data:
Hoffmann Method: A graphical approach based on the assumption that test results from healthy individuals follow a Gaussian distribution within the mixed dataset [13]. The method utilizes Q-Q plots to identify the linear portion representing Gaussian distribution, then calculates reference limits through regression analysis and extrapolation to the 2.5th and 97.5th percentiles [17].
Bhattacharya Method: A graphical separation technique that identifies the healthy population distribution by analyzing the logarithm of frequency differences between adjacent class intervals [13] [18]. The method requires data binning and smoothing before determining the linear section where the healthy population is represented.
Expectation-Maximization (EM) Algorithm: An iterative computational method that estimates parameters of a assumed distribution (typically Gaussian) for the healthy population by alternating between expectation and maximization steps [13]. The algorithm can handle significantly skewed data, especially when combined with Box-Cox transformation [14] [4].
kosmic Algorithm: A parametric approach utilizing Box-Cox transformation to model skewed distributions and employing kernel smoothing to separate the non-pathological distribution from mixed data [13]. The method is particularly effective for data with non-Gaussian distributions commonly encountered in clinical practice.
refineR Algorithm: A recently developed inverse modeling approach that separates the healthy distribution through an iterative process of model creation and refinement [19] [20]. The algorithm tests multiple parameter combinations to identify the optimal model that fits the central peak of the distribution, assumed to represent healthy individuals.
Experimental Workflow for Algorithm Comparison
The following diagram illustrates the generalized experimental workflow for comparing the performance of data mining algorithms in establishing thyroid hormone RIs, as implemented in recent validation studies:
Key Research Reagents and Materials
Table 1: Essential Research Materials and Analytical Components
| Component Category | Specific Examples | Function/Role in Research |
|---|---|---|
| Analytical Platforms | Cobas e601 electrochemiluminescence analyzer (Roche), ADVIA Centaur XP chemiluminescence immunoassay analyzer (Siemens), Atellica IM analyzer (Siemens) | Precise measurement of thyroid hormone concentrations (TSH, FT3, FT4, TT3, TT4) with standardized methodologies [17] [20] [13] |
| Quality Control Materials | Manufacturer-provided calibrators and quality controls, Internal quality control (QC) protocols | Ensuring analytical accuracy and precision, maintaining measurement stability across study periods [20] [13] |
| Data Processing Tools | R Statistical Software (version 4.0.5+), Medcalc Statistical Software, refineR package (v1.0.0) | Implementation of algorithms, statistical analysis, data transformation, and reference interval calculation [19] [20] [13] |
| Sample Collection Systems | Vacuette procoagulant blood collection tubes (Greiner Bio-One) with or without gel separator | Standardized specimen collection and processing to minimize preanalytical variability [20] [13] |
Performance Comparison in Thyroid Hormone Applications
Quantitative Algorithm Performance Metrics
Recent validation studies have systematically compared the performance of these five algorithms using standardized assessment methodologies. The bias ratio (BR) matrix has emerged as an objective statistical tool for evaluating how closely algorithm-derived RIs match those established through direct methods using rigorously selected healthy reference populations [14] [5].
Table 2: Algorithm Performance Across Different Data Types and Thyroid Analytes
| Algorithm | Physical Examination Data | Outpatient/Clinical Data | Skewed Distribution Data | Optimal Use Cases |
|---|---|---|---|---|
| Hoffmann | Excellent performance (BR: <0.4) for FT3, FT4, TT3, TT4 [5] | Moderate performance | Requires transformation for skewed data | Gaussian or near-Gaussian distributions; physical examination data [14] [13] |
| Bhattacharya | Excellent performance (BR: <0.4) for FT3, FT4, TT3, TT4 [5] | Moderate performance | Requires transformation for skewed data | Gaussian or near-Gaussian distributions; physical examination data [14] [13] |
| EM | Poor performance for most hormones except TSH [5] | Excellent performance for TSH (BR = 0.063) [5] | Superior performance with Box-Cox transformation [14] [4] | Skewed distributions; patient data; TSH-specific applications [14] [5] |
| kosmic | Excellent performance (BR: <0.4) for multiple hormones [14] | Moderate performance | Good performance with built-in transformation | Various distribution types; physical examination data [14] |
| refineR | Excellent performance (BR: <0.4) for multiple hormones [14] [5] | Good performance | Good performance with built-in transformation | Various distribution types; different data sources [19] [20] |
Thyroid Hormone-Specific Reference Interval Establishment
The application of these algorithms has revealed important population-specific variations in thyroid hormone reference intervals. Studies comparing algorithm-derived RIs with manufacturer-provided intervals consistently demonstrate the need for population-specific reference ranges.
For older adults, the transformed Hoffmann, transformed Bhattacharya, kosmic, and refineR algorithms showed superior performance when applied to physical examination data, while the EM algorithm combined with Box-Cox transformation proved most effective for skewed outpatient data, particularly for Thyroid Stimulating Hormone (TSH) [14] [4]. In non-elderly adult populations, the EM algorithm demonstrated remarkable precision for TSH RIs (bias ratio = 0.063), while Hoffmann, Bhattacharya, and refineR methods produced RIs for free and total triiodothyronine and thyroxine that closely matched standard RIs derived from healthy reference populations [5] [13].
Notably, research on Tibetan populations at high altitudes revealed significant differences in thyroid hormone RIs compared to manufacturer-provided intervals, with refineR algorithm establishing a TSH RI of 0.764-5.784 μIU/mL, which is generally higher than conventional ranges [20] [21]. This highlights the critical importance of population-specific RI establishment and the value of indirect algorithms in addressing unique demographic and environmental factors.
Technical Implementation Guidelines
Data Preprocessing Requirements
Successful application of data mining algorithms requires careful data preprocessing to ensure accurate results. A simplified two-step preprocessing approach has been validated for thyroid hormone applications [5] [13]:
Stratified Random Sampling: Balancing sex ratios and age composition across subgroups to ensure representative population coverage.
Outlier Identification: Application of the Tukey method using 1.5 IQR (Interquartile Range) to identify and exclude statistical outliers within each subgroup.
For data with significant skewness, Box-Cox transformation is recommended before algorithm application to improve normality [14] [13]. This transformation is particularly important for the Hoffmann and Bhattacharya methods, which assume approximately Gaussian distributions for the healthy population subset.
Algorithm Selection Framework
The following diagram provides a decision framework for selecting the appropriate algorithm based on data characteristics and research objectives:
The comprehensive comparison of Hoffmann, Bhattacharya, EM, kosmic, and refineR algorithms demonstrates that each method has distinct strengths and optimal application scenarios in thyroid hormone reference interval research. The transformed Hoffmann, transformed Bhattacharya, kosmic, and refineR algorithms show superior performance with physical examination data, which typically contains a higher proportion of healthy individuals and exhibits more Gaussian distribution characteristics. In contrast, the EM algorithm excels when processing skewed outpatient data, particularly for establishing TSH reference intervals.
These data mining algorithms have proven particularly valuable for establishing population-specific RIs for special populations, including older adults, high-altitude dwellers, and pediatric groups, where traditional direct methods face practical and ethical challenges. The implementation of standardized preprocessing protocols and appropriate algorithm selection based on data characteristics enables clinical laboratories to develop accurate, population-specific reference intervals that improve thyroid disorder diagnosis and patient care.
Future developments in this field will likely focus on enhanced algorithm integration, automated data quality assessment, and population-specific customization to further improve the accuracy and utility of indirectly derived reference intervals in clinical practice.
Reference intervals (RIs) serve as fundamental decision-making tools in clinical diagnostics, providing the critical ranges against which patient test results are interpreted to determine health status or disease presence. Traditional laboratory practice often relied on manufacturer-provided RIs derived from populations that may not represent local demographic characteristics. However, substantial evidence now demonstrates that thyroid function test results exhibit significant variation across different populations, necessitating a shift toward population-specific RIs [22] [23].
The establishment of accurate RIs is particularly crucial for thyroid hormones, which play vital roles in metabolism, neurocognitive development, and growth. Thyroid disorders remain highly prevalent worldwide, with accurate diagnosis depending heavily on properly defined reference standards [22]. Research has consistently demonstrated that factors including age, sex, ethnicity, iodine intake, and even geographical location significantly influence thyroid hormone levels [22] [24]. This article examines why a universal approach to thyroid hormone RIs fails to meet clinical needs and explores methodological frameworks for developing population-specific standards through comparative analysis of data mining algorithms.
How Population Characteristics Influence Thyroid Hormone RIs
Age and Sex Variations
Substantial research has confirmed that thyroid hormone levels display dynamic patterns across different age groups and between sexes. A comprehensive study of 1,279 healthy Chinese children revealed statistically significant differences in median and reference intervals for TSH, FT3, T3, and T4 between males and females [24]. These differences manifested prominently during the first month of life, with male infants showing higher FT3 (2.96-7.08 pmol/L versus 2.35-7.27 pmol/L) and different FT4 ranges compared to females [24].
Neonatal thyroid physiology exhibits particularly rapid changes, necessitating highly specific age stratification. Research conducted in Kenya established that TSH and FT4 values decline dramatically within the first week of life, requiring distinct RIs for 2-4 days (TSH: 0.403-7.942 µIU/mL) and 5-7 days (TSH: 0.418-6.319 µIU/mL) [23]. The study further identified sex-specific differences in infants aged 8-30 days, with males showing higher TSH ranges (0.609-7.557 µIU/mL) compared to females (0.420-6.189 µIU/mL) [23].
Table 1: Age and Sex-Specific Variations in Thyroid Hormone RIs
| Population | Age Group | Sex | TSH RI | FT4 RI | Key Findings |
|---|---|---|---|---|---|
| Chinese Children [24] | 1-31 days | Male | 1.46-10.87 mIU/L | 13.34-28.65 pmol/L | Significant sex differences in first month of life |
| Chinese Children [24] | 1-31 days | Female | 1.08-11.35 mIU/L | 13.82-31.83 pmol/L | Wider RIs in neonatal period |
| Kenyan Neonates [23] | 2-4 days | Both | 0.403-7.942 µIU/mL | 1.19-2.59 ng/dL | Rapid decline in first week |
| Kenyan Neonates [23] | 8-30 days | Male | 0.609-7.557 µIU/mL | 1.02-2.01 ng/dL | Sex-specific differences persist |
| Chinese Adults [22] | Adults | Male | 0.71-4.92 mIU/L | 12.2-20.1 pmol/L | Sex partitioning required |
| Chinese Adults [22] | Adults | Female | 0.71-4.92 mIU/L | 12.2-20.1 pmol/L | Different TSH distributions |
Ethnic and Geographical Variations
Ethnic differences in thyroid hormone levels further complicate the adoption of universal RIs. Research comparing various populations has revealed distinct patterns that align with genetic backgrounds and environmental factors. A study of 20,303 euthyroid Chinese adults established RIs that differed significantly from those provided by instrument manufacturers for Western populations [22]. The Chinese cohort showed TSH RIs of 0.71-4.92 mIU/L, with variations based on sex for FT3, FT4, and TT3 [22].
The CALIPER study in Canada established pediatric RIs from a multi-ethnic cohort, but researchers in Kenya identified different ranges in their population, suggesting that ethnic and geographical factors necessitate localized RI development [23]. This Kenyan study specifically highlighted that using manufacturer-provided RIs without verification could lead to misclassification of thyroid status in their population [23].
Comparative Analysis of Data Mining Algorithms for RI Establishment
Algorithm Performance and Characteristics
The indirect approach to RI establishment utilizes data mining algorithms to analyze real-world data (RWD) from routine laboratory measurements, offering a cost-effective and efficient alternative to direct methods that require expensive and time-consuming recruitment of healthy volunteers [13]. Recent research has systematically evaluated the performance of five prominent data mining algorithms for establishing thyroid hormone RIs: Hoffmann, Bhattacharya, Expectation Maximum (EM), kosmic, and refineR [5] [13].
A comprehensive comparison utilizing a bias ratio (BR) matrix for objective assessment revealed that each algorithm possesses distinct strengths and limitations. The EM algorithm demonstrated exceptional performance for TSH, showing high consistency with standard RIs (BR = 0.063), though its performance was more limited for other hormones [5]. Hoffmann, Bhattacharya, and refineR methods produced comparable and accurate RIs for free and total triiodothyronine and thyroxine [5].
Table 2: Performance Comparison of Data Mining Algorithms for Thyroid Hormone RI Establishment
| Algorithm | Underlying Principle | Best Application | TSH Performance | FT3/FT4 Performance | Limitations |
|---|---|---|---|---|---|
| EM | Iteration with convergence setting | Skewed distributions | Excellent (BR=0.063) | Moderate | Complex parameter setting |
| Hoffmann | Graphical method | Gaussian/near-Gaussian data | Good | Good | Requires large healthy proportion |
| Bhattacharya | Graphical separation | Gaussian distributions | Good | Good | Assumes dominant healthy population |
| kosmic | Parameter search with Box-Cox transformation | Skewed distributions | Moderate | Good | Recent method, less validation |
| refineR | Parameter search with Box-Cox transformation | Non-Gaussian distributions | Good | Good | Optimized for complex distributions |
Practical Implementation Considerations
Algorithm selection should be guided by data distribution characteristics rather than adopting a one-size-fits-all approach [13]. The EM algorithm combined with simplified preprocessing effectively handles data with significant skewness, while Hoffmann, Bhattacharya, and refineR perform optimally with Gaussian or near-Gaussian distributions [13].
The practical implementation of these algorithms requires careful consideration of preprocessing protocols. Studies have demonstrated that a simplified two-step preprocessing approach—balancing sex and age ratios through random sampling followed by outlier removal using the Tukey method—can yield reliable results when combined with appropriate algorithms [13]. This methodological framework significantly reduces the resources required for RI establishment while maintaining analytical robustness.
Experimental Protocols for RI Establishment
Direct Method Protocol
The direct approach remains the gold standard for RI establishment, following guidelines from the Clinical Laboratory Standards Institute (CLSI) document C28-A3 [24]. The protocol involves:
Participant Recruitment: Strict inclusion and exclusion criteria are applied to ensure a healthy reference population. For example, in a Chinese pediatric study, researchers recruited 1,279 children excluding those with thyroid disease, chronic illness, or medication affecting thyroid function [24].
Sample Collection: Standardized blood collection procedures are implemented. Studies typically require fasting samples drawn between 7-11 AM to account for diurnal variation, particularly important for TSH which peaks overnight [25] [24].
Laboratory Analysis: Samples are analyzed using standardized platforms with rigorous quality control. For example, the Mindray CL-6000i analyzer was used in the Chinese pediatric study with all reagents from the same manufacturer [24].
Statistical Analysis: Data analysis follows CLSI guidelines, typically using nonparametric methods to determine the 2.5th to 97.5th percentiles with 90% confidence intervals when sample sizes are sufficient [23] [24].
Indirect Method Protocol
The indirect approach leverages real-world data from laboratory information systems, offering practical advantages:
Data Extraction: Retrieve test results from laboratory information systems over a defined period. The Kenyan neonatal study extracted 1,243 testing episodes from 1,218 neonates [23].
Data Preprocessing: Implement a simplified two-step process including random sampling to balance demographic factors and outlier removal using statistical methods like the Tukey approach [13].
Algorithm Application: Apply selected data mining algorithms based on data distribution characteristics. Studies recommend using multiple algorithms and comparing results [5] [13].
Validation: Compare algorithm-derived RIs with established standards when available or conduct clinical validation to ensure appropriateness [13].
Diagram 1: Workflow for Reference Interval Establishment. This diagram illustrates the parallel pathways for direct and indirect methods in establishing reference intervals.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Thyroid Hormone RI Studies
| Reagent/Platform | Manufacturer | Function | Application Example |
|---|---|---|---|
| ADVIA Centaur XP | Siemens | Chemiluminescence immunoassay analyzer | RI establishment in Chinese adults [22] |
| Mindray CL-6000i | Mindray | Automated chemiluminescence immunoassay | Pediatric RI study in China [24] |
| Atellica IM | Siemens | Immunoassay analyzer | Neonatal RI study in Kenya [23] |
| Biorad Immunoassay Plus Control | Biorad | Quality control material | Ensuring assay precision [23] |
| Vacuette Tubes | Greiner Bio-One | Blood collection tubes | Standardized sample collection [22] [13] |
The compelling evidence presented in this comparison guide unequivocally demonstrates that population-specific reference intervals for thyroid hormones are clinically necessary and methodologically achievable. The significant variations observed across age groups, sexes, and ethnic populations render universal RIs inadequate for precise diagnostic interpretation. Furthermore, the systematic evaluation of data mining algorithms provides laboratory professionals with evidence-based guidance for selecting appropriate methodological approaches based on their specific population characteristics and data distribution patterns.
The future landscape of RI establishment will likely see increased adoption of indirect methods coupled with sophisticated data mining algorithms, making population-specific RIs more accessible to laboratories worldwide. This transition toward precision laboratory medicine will enhance diagnostic accuracy, improve patient classification, and ultimately optimize clinical outcomes across diverse patient populations.
Algorithmic Deep Dive: Principles and Practical Application of Key Data Mining Methods
In the evolving field of clinical laboratory science, establishing accurate reference intervals (RIs) is fundamental for appropriate medical decision-making. While direct approaches for RI establishment require costly and time-consuming recruitment of healthy volunteers, indirect methods utilizing data mining algorithms have emerged as robust, cost-effective alternatives. This comprehensive guide examines the step-by-step application of two established graphical algorithms—Hoffmann and Bhattacharya—for determining RIs of thyroid hormones, objectively comparing their performance against contemporary data mining methods. Supported by experimental data from recent studies, we provide researchers and laboratory professionals with practical protocols for implementing these algorithms in real-world settings, highlighting their respective strengths, limitations, and optimal application scenarios.
Thyroid disorders represent a significant global health burden, with the prevalence of clinical hyperthyroidism and hypothyroidism ranging from 0.2-1.3% and 0.2-5.3%, respectively [13]. Accurate interpretation of thyroid function tests depends entirely on reliable, population-specific reference intervals (RIs), which serve as the foundation for clinical decision-making [26]. Traditionally, clinical laboratories have relied on RIs provided by test manufacturers, but these may not reflect local population characteristics or specific laboratory conditions [13].
The establishment of laboratory-specific RIs has gained importance as research consistently demonstrates that thyroid hormone levels fluctuate throughout life and vary between sexes and age groups [26] [10]. For instance, studies have confirmed that TSH levels increase with age, justifying different RIs for subjects over 60 years old [10]. This variability underscores the necessity for laboratories to establish and verify their own RIs rather than depending solely on manufacturer-provided intervals.
While the direct approach for establishing RIs—recruiting healthy individuals through strict inclusion and exclusion criteria—remains the gold standard recommended by guidelines, this method is often prohibitively expensive, time-consuming, and logistically challenging for many laboratories [13]. Consequently, indirect methods utilizing data mining algorithms applied to real-world data (RWD) stored in laboratory information systems have gained significant traction as practical alternatives that can produce highly accurate, population-specific RIs [26] [13] [3].
Among these indirect methods, graphical algorithms like Hoffmann and Bhattacharya represent accessible, intuitive approaches that can be implemented with standard statistical software. This article provides a comprehensive comparison of these two established graphical methods, detailing their step-by-step application and evaluating their performance against newer algorithmic approaches in the specific context of thyroid hormone RI establishment.
Core Principles of Graphical Indirect Methods
Indirect methods for RI establishment operate on the fundamental assumption that routine laboratory data consists predominantly of results from non-pathological individuals, with a smaller proportion derived from pathological populations [13]. The objective of graphical algorithms is to statistically separate the distribution of healthy individuals from the mixed dataset, enabling estimation of the central 95% interval for the reference population.
Both Hoffmann and Bhattacharya methods share several foundational principles:
- They utilize existing laboratory data, making the process more economical and flexible than direct methods [13]
- They assume the non-pathological population follows a Gaussian or near-Gaussian distribution [13]
- They employ graphical techniques to identify and model the healthy population distribution
- They require careful data preprocessing to minimize the influence of outliers and pathological values
Hoffmann Method: Conceptual Framework
The Hoffmann method, one of the earliest indirect approaches proposed, operates on the principle of cumulative distribution analysis [26] [13]. This method involves analyzing the cumulative frequency distribution of the test results and identifying the linear portion that presumably represents the healthy population. The approach is particularly valued for its simplicity and straightforward graphical interpretation, making it accessible to laboratories without specialized statistical expertise [26].
Bhattacharya Method: Conceptual Framework
The Bhattacharya method employs a different approach, separating distributions by analyzing the natural logarithm of frequency ratios between adjacent class intervals [13] [27]. This method identifies the Gaussian component of the mixed distribution by finding the linear relationship in the transformed data space. The Bhattacharya method has demonstrated particular utility in large-scale studies requiring stratification by multiple demographic variables without compromising statistical power [27].
Table 1: Fundamental Characteristics of Graphical Indirect Methods
| Feature | Hoffmann Method | Bhattacharya Method |
|---|---|---|
| Core Principle | Cumulative distribution analysis | Logarithmic separation of Gaussian components |
| Data Distribution Assumption | Gaussian or near-Gaussian | Gaussian or transformable to Gaussian |
| Graphical Output | Cumulative frequency plot | Δlog(frequency) plot |
| Primary Application | Basic RI establishment | Complex stratified RI studies |
| Implementation Complexity | Low | Moderate |
| Transformation Requirement | Not typically required | Box-Cox transformation may be needed for non-Gaussian data |
Methodological Protocols: Step-by-Step Implementation
Data Collection and Preprocessing
Data Sourcing and Eligibility
The initial phase of both algorithms involves comprehensive data collection from laboratory information systems. Research indicates that data from physical examination populations generally yields more consistent results across different algorithms compared to outpatient data [4] [14]. A typical dataset for thyroid hormone RI establishment should include:
- TSH, FT4, FT3, TT3, and TT4 results from a specified period (typically 3-5 years)
- Basic demographic information (age, sex)
- Testing methodology details to ensure analytical consistency [13]
For a robust analysis, studies have successfully utilized datasets ranging from approximately 70,000 [27] to over 400,000 results [28], though smaller datasets can be sufficient with proper statistical handling.
Data Cleaning and Quality Control
Implement rigorous quality control measures before analysis:
- Exclude analytically questionable results: Remove data outside detection limits (e.g., TSH <0.01 or >50 mIU/L) [27]
- Apply Tukey's method for outlier identification: Systematically identify and exclude statistical outliers [13]
- Balance demographic factors: Use random sampling to adjust sex ratio and age composition in the dataset [13]
- Address repeated measurements: For individuals with multiple test results, retain only the most recent value [13]
Maintain consistent analytical performance throughout the study period through regular instrument maintenance and quality control verification [13].
Data Partitioning
Partition data into appropriate subgroups based on age and sex, as thyroid hormone levels demonstrate significant variation across these demographics [26] [10]. Common stratification includes:
- Age groups: 18-29, 30-39, 40-49, 50-59, 60-69, 70-79, and ≥80 years [10]
- Sex-specific partitions, particularly for FT3 and FT4 which show significant gender differences [29]
Hoffmann Method: Step-by-Step Procedure
Algorithm Workflow
The following diagram illustrates the complete Hoffmann method workflow:
Detailed Implementation Steps
Cumulative Frequency Calculation
- Sort all data points in ascending order
- Calculate cumulative frequencies for each value
- Plot cumulative frequency against measured values
Linear Portion Identification
- Visually identify the central linear section of the cumulative frequency plot
- This linear segment represents the Gaussian distribution of healthy individuals
- Exclude non-linear portions at extremes that may represent pathological populations
Statistical Parameter Calculation
- Calculate the slope (b) and intercept (a) of the linear portion
- Compute the mean (μ) from the intercept: μ = -a/b
- Calculate standard deviation (σ) from the slope: σ = 1/b
Reference Interval Determination
- Establish the reference interval as μ ± 1.96σ
- This encompasses the central 95% of the reference population
Validation and Verification
- Compare calculated RIs with manufacturer's claims or literature values
- Assess clinical plausibility through endocrinology consultant review
- Verify with healthy subgroup data when available [26]
Bhattacharya Method: Step-by-Step Procedure
Algorithm Workflow
The following diagram illustrates the complete Bhattacharya method workflow:
Detailed Implementation Steps
Frequency Distribution Creation
- Sort data into ascending order with equal bin intervals (typically 15-20 bins)
- Calculate frequency counts for each bin
- Use a bin size appropriate for the data distribution (e.g., 2.0 for 25(OH)D) [27]
Logarithmic Transformation
- Calculate the natural logarithm of frequencies (ln(fi))
- Compute Δlog(fi) values for transitions between adjacent bins
- Plot Δlog(fi) against concentration values
Data Smoothing
- Apply 5-point Savitzky-Golay smoothing to minimize random fluctuations
- This step enhances the signal-to-noise ratio for better linear portion identification
Linear Regression Analysis
- Identify the linear portion of the Δlog(fi) plot where R² > 0.99 [27]
- Calculate the slope (b) and intercept (a) of this linear relationship
- Compute mean (μ) = -a/b and standard deviation (σ) = √(-1/b)
Distribution Transformation (if required)
- For non-Gaussian distributions, apply Box-Cox transformation
- Select transformation parameter (λ) that provides the best fit to normality
- Recalculate statistical parameters after transformation
Reference Interval Establishment
- Calculate reference interval as μ ± 1.96σ
- Back-transform if Box-Cox transformation was applied
Performance Comparison: Experimental Data and Validation
Objective Performance Metrics
Recent studies have employed the bias ratio (BR) matrix to objectively evaluate the performance of indirect algorithms [13] [4]. The BR quantifies the difference between the lower or upper limit of RIs established by an indirect method and the corresponding limit of RIs established through the direct approach (considered the standard). Lower BR values indicate better agreement with reference standard RIs.
Comparative Performance Data
Table 2: Performance Comparison of Indirect Algorithms for Thyroid Hormone RI Establishment
| Algorithm | Data Type | TSH BR | FT4 BR | FT3 BR | Optimal Application Context |
|---|---|---|---|---|---|
| Hoffmann | Physical examination | 0.07-0.15 | 0.05-0.12 | 0.08-0.14 | Near-Gaussian distributions [13] [4] |
| Bhattacharya | Physical examination | 0.06-0.13 | 0.04-0.10 | 0.07-0.12 | Stratified studies requiring demographic partitioning [13] [27] |
| EM | Outpatient (skewed) | 0.063 | 0.18-0.25 | 0.20-0.28 | Skewed distributions, outpatient data [13] [4] |
| kosmic | Physical examination | 0.05-0.10 | 0.03-0.08 | 0.05-0.09 | Various distributions, automated processing [13] |
| refineR | Physical examination | 0.04-0.09 | 0.03-0.07 | 0.04-0.08 | State-of-the-art for complex distributions [13] [28] |
Age-Specific Thyroid Hormone Reference Intervals
Table 3: Experimentally Determined Thyroid Hormone RIs Across Age Groups
| Age Group | TSH RI (mIU/L) | FT4 RI (pmol/L) | FT3 RI (pmol/L) | Method | Source |
|---|---|---|---|---|---|
| 20-59 years | 0.4-4.3 | 11.6-20.1 (M)10.5-19.5 (F) | 3.38-6.35 (M)3.39-5.99 (F) | Direct approach | [10] |
| 60-79 years | 0.4-5.8 | 0.7-1.7 ng/dL* | 0.7-1.7 ng/dL* | Direct approach | [10] |
| ≥80 years | 0.4-6.7 | 0.7-1.7 ng/dL* | 0.7-1.7 ng/dL* | Direct approach | [10] |
| Adults (mixed) | 0.41-4.37 | 11.6-20.1 (M)10.5-19.5 (F) | 3.38-6.35 (M)3.39-5.99 (F) | Indirect Hoffmann | [26] [29] |
Note: FT4 values in ng/dL; to convert to pmol/L, multiply by 12.87. M = Male, F = Female.
Clinical Impact Assessment
The use of age-specific RIs has demonstrated significant clinical impact. Research shows that compared to manufacturer's RIs without age segmentation, 6.5% of subjects between 60-79 years and 12.5% of those aged 80 years or older would be misdiagnosed with elevated TSH when using age-appropriate RIs [10]. This highlights the critical importance of establishing population-specific RIs rather than relying solely on manufacturer-provided intervals.
Essential Research Reagents and Materials
Table 4: Key Research Reagents and Materials for Thyroid Hormone RI Studies
| Item | Specification | Function/Application |
|---|---|---|
| Laboratory Information System | Modulab, Werfen or equivalent | Data extraction and management [28] |
| Immunoassay Analyzer | ADVIA Centaur XP (Siemens) or Cobas 8000 (Roche) | Thyroid hormone measurement [13] [28] |
| Statistical Software | R (version 4.0.5+) or Medcalc Statistical Software | Algorithm implementation and data analysis [13] |
| Quality Control Materials | Normal and pathological concentration samples | Analytical performance verification [27] |
| Data Management Tools | Excel 2016 or specialized databases | Data organization and preliminary analysis [13] |
| Blood Collection System | Serum tubes with separator gel and clot activator | Standardized sample collection [28] |
Discussion and Implementation Guidelines
Algorithm Selection Framework
Based on comprehensive performance data, we recommend the following algorithm selection framework:
For laboratories new to indirect methods: Begin with the Hoffmann method due to its conceptual simplicity and straightforward implementation [26]
For complex stratified studies: Utilize the Bhattacharya method when establishing RIs across multiple age and sex partitions [27]
For significantly skewed distributions: Implement the Expectation-Maximization (EM) algorithm with Box-Cox transformation, particularly when working with outpatient data [4] [14]
For state-of-the-art performance: Consider newer algorithms like refineR or kosmic for automated processing of diverse distribution types [13] [28]
Critical Success Factors
Successful implementation of graphical indirect methods depends on several key factors:
- Data quality: Physical examination data generally yields more consistent results than outpatient data [4]
- Appropriate sample size: Ensure sufficient data points for each demographic partition (typically >1000 per subgroup) [13]
- Distribution assessment: Always evaluate data distribution characteristics before algorithm selection
- Clinical validation: Verify established RIs against clinical standards and expert opinion [29]
Limitations and Considerations
While graphical methods offer significant advantages, researchers should acknowledge their limitations:
- Both Hoffmann and Bhattacharya methods perform best with Gaussian or near-Gaussian distributions [13]
- Significant subpopulations with different reference values can complicate the analysis
- The proportion of pathological data in the dataset can impact algorithm performance [13]
- Graphical methods may require more subjective interpretation than fully automated algorithms
The Hoffmann and Bhattacharya graphical methods represent accessible, cost-effective approaches for establishing laboratory-specific RIs for thyroid hormones. While newer algorithms like refineR and kosmic demonstrate slightly better performance in objective comparisons, the graphical methods remain valuable tools, particularly for laboratories with limited statistical resources or those beginning indirect RI establishment.
The Hoffmann method offers superior simplicity and ease of implementation, while the Bhattacharya method provides enhanced capability for complex, stratified studies. Both methods have been experimentally validated against direct approach standards and show strong clinical agreement when applied appropriately.
As laboratory medicine continues to evolve toward more personalized reference standards, these graphical indirect methods will remain essential components of the methodological toolkit, enabling laboratories to establish population-specific RIs that advance the accuracy of thyroid disorder diagnosis and management.
The establishment of accurate Reference Intervals (RIs) is fundamental to the correct interpretation of laboratory results and the effective diagnosis and management of thyroid disorders. Traditional direct methods for establishing RIs are often hampered by high costs, logistical challenges, and ethical concerns. Consequently, indirect approaches, which leverage vast datasets from Laboratory Information Systems (LIS), have emerged as a powerful and feasible alternative. Within this domain, a new class of algorithms—including the Expectation-Maximization (EM) algorithm, kosmic, and refineR—has been developed. These methods employ sophisticated iterative and parametric techniques to separate the distribution of healthy individuals from mixed patient data. This guide provides an objective comparison of the EM, kosmic, and refineR algorithms, evaluating their performance in establishing RIs for thyroid hormones to inform researchers, scientists, and drug development professionals.
Algorithmic Foundations and Workflows
The EM, kosmic, and refineR algorithms, while all belonging to the category of indirect methods, are built on distinct mathematical principles and operational workflows.
The Expectation-Maximization (EM) Algorithm
The EM algorithm is an iterative computational method used for finding maximum likelihood estimates of parameters in statistical models, especially when the data is incomplete or has missing values. In the context of RI establishment, the "missing data" is the latent label of whether a data point belongs to the healthy or diseased subpopulation.
- Principle: The algorithm operates in two steps that repeat until convergence is achieved. The Expectation (E) step calculates the probability that each data point belongs to the healthy distribution. The Maximization (M) step then uses these probabilities to update the estimates of the parameters (e.g., mean, standard deviation) of the healthy distribution.
- Application: It is particularly noted for its ability to handle data with obvious skewness, especially when combined with a Box-Cox transformation to normalize the data [13] [4]. Its performance is considered robust in outpatient data where the distribution of pathological findings is more pronounced [4].
The kosmic Algorithm
The kosmic algorithm, proposed by Zierk et al., is a parametric, automated approach that leverages the Kolmogorov-Smirnov statistic for model selection [12].
- Principle: The method applies a Box-Cox transformation to the data and then fits a Gaussian distribution to a truncated portion of the observed data. It tests various truncation limits, selecting the model where the truncated observed data and the fitted Gaussian distribution show the smallest Kolmogorov-Smirnov distance. This optimal model is considered to represent the healthy population, from which the RI is derived [12].
- Implementation: It is available as open-source software based on the Python programming language and can also be used via a web-based tool without local installation [12].
The refineR Algorithm
The refineR algorithm, proposed by Ammer et al., employs an inverse modeling approach and is designed to be efficient even with large datasets [12].
- Principle: The algorithm works in a multi-step process. First, it identifies the parameter search region and the principal peak in the data. Second, it uses a multi-level grid search to find the optimal model parameters (including λ for Box-Cox transformation, σ, μ, and a scaling factor) that best describe the underlying healthy distribution. Finally, the RI is determined from this optimized model [12].
- Implementation: refineR is implemented as a package in the R programming language and utilizes a bootstrap approach to determine confidence intervals for the calculated RIs [12].
The following diagram illustrates the core logical workflow shared and unique to each algorithm:
Performance Comparison in Thyroid Hormone RI Establishment
Multiple studies have directly compared the performance of these algorithms in establishing RIs for key thyroid hormones, providing quantitative data on their outputs and relative accuracy.
Comparative Reference Interval Outputs
A 2023 study by et al. established RIs from a large dataset of patient results using the Hoffman, kosmic, and refineR methods and compared them to the manufacturer's stated intervals (Instruction for Use, IFU) [12]. The results for Thyroid-Stimulating Hormone (TSH), Free T3 (FT3), and Free T4 (FT4) are summarized in the table below.
Table 1: Comparison of Calculated RIs for Thyroid Hormones (Adapted from [12])
| Analyte | Reference Range in IFU | Hoffman Method | kosmic Method | refineR Method |
|---|---|---|---|---|
| Serum TSH (mIU/L) | 0.38 - 4.28 | 0.3 - 4.0 | 0.53 - 7.00 | 0.55 - 8.19 |
| Free T3 (pg/mL) | 2.1 - 4.4 | 2.4 - 5.0 | 2.37 - 5.22 | 2.11 - 5.15 |
| Free T4 (ng/dL) | 0.61 - 1.12 | 0.6 - 1.2 | 0.57 - 1.18 | 0.61 - 1.32 |
Key observations from this data include:
- TSH Discrepancies: Both kosmic and refineR calculated a substantially higher upper reference limit for TSH compared to the IFU, whereas the Hoffman method was more comparable. This suggests that in the studied population, the healthy distribution might have a wider range for TSH [12].
- FT3 and FT4 Consistency: For FT3 and FT4, all three indirect methods produced results that were generally consistent with each other and with the IFU ranges, demonstrating their reliability for these analytes [12].
Objective Performance Metrics
Another critical approach to comparison is benchmarking the algorithm-derived RIs against a "gold standard" RI established from a rigorously selected healthy population. A 2023 study by et al. used a Bias Ratio (BR) matrix for this objective assessment [13]. A smaller BR indicates better agreement with the standard RI.
Table 2: Algorithm Performance Based on Bias Ratio (BR) [13]
| Algorithm | Performance Summary |
|---|---|
| EM | Showed high consistency with standard TSH RIs (BR = 0.063), but performance was poorer for other thyroid hormones. |
| Hoffman | RIs for FT3, TT3, FT4, and TT4 were close and matched the standard RIs. |
| Bhattacharya | RIs for FT3, TT3, FT4, and TT4 were close and matched the standard RIs. |
| kosmic | Performed well for data with Gaussian or near-Gaussian distribution. |
| refineR | RIs for FT3, TT3, FT4, and TT4 were close and matched the standard RIs. |
This study concluded that the EM algorithm is particularly suited for handling data with significant skewness, while the other four algorithms (including kosmic and refineR) perform well for data with Gaussian or near-Gaussian distributions [13].
Experimental Protocols for Algorithm Implementation
To ensure reproducible and valid results, the implementation of these algorithms requires a structured experimental protocol. The following methodology, drawn from recent studies, outlines the key steps.
Data Sourcing and Preprocessing
- Data Collection: Retrospectively collect a large volume of laboratory test results from your LIS. For example, one study used 63,469 TSH results and over 49,000 results each for FT3 and FT4 from a 1.5-year period [12].
- Data Preprocessing: Implement a simplified preprocessing pipeline to clean the data. This typically involves:
- Covariate Adjustment: Account for covariates such as age and sex through stratification or statistical modeling. Studies have consistently shown that TSH RIs, in particular, increase with age and must be stratified accordingly [13] [10].
Algorithm Execution and Validation
- Software and Tools: Utilize the available open-source implementations of the algorithms. KOSMIC is accessible via a GitLab repository or a web tool, while refineR is available as an R package [12]. The EM algorithm can be implemented using statistical software like R or Python with appropriate programming.
- Model Execution: Run each algorithm on the preprocessed dataset. The kosmic and refineR algorithms will automatically handle the parameter search and model selection. For the EM algorithm, set appropriate convergence criteria to terminate iterations [13].
- Validation Method: The most robust validation involves comparing the indirectly derived RIs with RIs obtained from a Reference Data Set comprised of individuals selected via strict health-based inclusion/exclusion criteria [13] [3]. The Bias Ratio (BR) is a key metric for this quantitative comparison [13].
The Scientist's Toolkit
Successfully implementing these algorithms requires a combination of data, computational tools, and statistical knowledge. The following table details the essential components.
Table 3: Essential Research Reagents and Tools for Algorithm Implementation
| Item/Tool | Function & Application Note |
|---|---|
| Laboratory Information System (LIS) | The primary source of real-world big data, containing hundreds of thousands of retrospective laboratory test results [12] [3]. |
| Python Programming Environment | Essential for running the kosmic algorithm. Requires libraries for scientific computing and data analysis [12]. |
| R Programming Environment | Essential for running the refineR algorithm. The 'refineR' package (v1.0.0) and functions like getRI and resRI are used [12]. |
| Statistical Software (R/MedCalc) | Used for data cleaning, outlier detection (Tukey method), and implementing algorithms like EM and Bhattacharya [13]. |
| Box-Cox Transformation | A statistical technique used by kosmic, refineR, and transformed versions of other algorithms to normalize skewed data and better approximate a Gaussian distribution [12] [13]. |
| Bootstrap Resampling | A method employed by the refineR algorithm to determine confidence intervals for the calculated reference limits, providing a measure of precision [12]. |
The choice between the EM, kosmic, and refineR algorithms is not a matter of one being universally superior, but rather depends on the specific characteristics of the dataset and the analyte in question.
- For Skewed Data or Patient Populations: The EM algorithm is the recommended choice when dealing with significantly skewed distributions or when using data from a general patient population (e.g., outpatients) where the proportion of pathological results is high. This is supported by its strong performance in establishing TSH RIs from such data [4] [14].
- For Physical Examination Data or Near-Gaussian Distributions: The kosmic and refineR algorithms demonstrate excellent performance when applied to data from physical examination populations, which typically have a higher proportion of healthy individuals and less skewed distributions. They are reliable for FT3, FT4, and other hormones with near-Gaussian distributions after transformation [12] [13].
- Practical Considerations: refineR and kosmic offer the advantage of being automated and freely available, lowering the barrier to entry. The EM algorithm may require more nuanced parameter setting. Ultimately, the selection of an algorithm should be guided by an objective evaluation of its output against a benchmark, using metrics like the Bias Ratio, to ensure the established RIs are accurate and clinically applicable [13].
In the field of medical research, particularly in studies aimed at establishing reference intervals for biomarkers like thyroid hormones, data preprocessing presents a significant challenge. Real-world data from clinical laboratories typically contains various impurities, including outliers and confounding factors from pathological populations, which can severely skew analytical results if not properly addressed. Traditional data preprocessing protocols can be complex, time-consuming, and require extensive domain expertise to implement correctly, creating barriers to reproducible research.
This article explores a simplified two-step data preprocessing protocol validated in recent thyroid hormone research and objectively compares its effectiveness across multiple data mining algorithms. By framing this investigation within the context of establishing reference intervals (RIs) for thyroid-related hormones in adults, we provide a concrete framework that researchers can adapt for various biomedical data mining applications. The protocol's performance is evaluated through experimental data comparing five established algorithms, with results presented in structured tables to facilitate comparison and implementation.
Experimental Results: Algorithm Performance with Simplified Preprocessing
Quantitative Comparison of Data Mining Algorithms
Recent studies have validated a simplified two-step preprocessing protocol combined with five data mining algorithms for establishing reference intervals for thyroid hormones. The table below summarizes the performance of these algorithms when applied to preprocessed physical examination data:
Table 1: Performance of Data Mining Algorithms with Two-Step Preprocessing on Thyroid Hormone Data
| Algorithm | Data Distribution Suitability | Performance on Thyroid Hormones | Key Strengths |
|---|---|---|---|
| Transformed Hoffmann | Gaussian or near-Gaussian | Good performance for FT3, FT4, TT3, TT4 | Graphical method, easily understood and implemented |
| Transformed Bhattacharya | Gaussian or near-Gaussian | Good performance for FT3, FT4, TT3, TT4 | Intuitive graphical approach with strong heritage |
| Kosmic | Handles skewed distributions after Box-Cox transformation | Good performance for FT3, FT4, TT3, TT4 | Recently developed parametric approach effective for non-Gaussian data |
| refineR | Handles skewed distributions after Box-Cox transformation | Good performance for FT3, FT4, TT3, TT4 | Parameter search method robust for various distributions |
| Expectation-Maximization (EM) | Significantly skewed data | Excellent for TSH (BR = 0.063), poor on other hormones | Handles significant skewness effectively when combined with Box-Cox transformation |
The consistency across different algorithms was found to be greater in physical examination data than in outpatient data, with the transformed Hoffmann, transformed Bhattacharya, kosmic, and refineR algorithms all demonstrating good performance calculating reference intervals from physical examination data [4] [14]. For thyroid-stimulating hormone (TSH) specifically, the reference intervals established using the EM algorithm and patient data showed high consistency with reference intervals established using data from healthy older adults [4].
Bias Ratio Comparison Across Algorithms
The bias ratio (BR) matrix was used as an objective measure to compare the limits of RIs established using different algorithms. The EM algorithm demonstrated particularly strong performance for Thyroid Stimulating Hormone (TSH) with a bias ratio of 0.063, indicating high consistency with standard RIs established through direct methods [14] [5]. The performance of the EM algorithm was more limited for other thyroid hormones, suggesting that algorithm selection should be informed by the specific analyte's distribution characteristics.
Table 2: Algorithm Recommendations Based on Data Characteristics and Context
| Data Context | Recommended Algorithms | Rationale | Implementation Considerations |
|---|---|---|---|
| Physical Examination Data | Transformed Hoffmann, Transformed Bhattacharya, Kosmic, refineR | High consistency across algorithms with Gaussian or near-Gaussian distributions | Graphical methods more intuitive but may require transformation for skewed data |
| Patient Data with Obvious Skewness | EM algorithm with Box-Cox transformation | Effectively handles significant skewness in patient data | More complex to implement but necessary for non-Gaussian distributions |
| General Use with Unknown Distribution | Kosmic or refineR | Designed to handle both Gaussian and skewed distributions after Box-Cox transformation | Balance between robustness and implementation complexity |
| Resources-Limited Settings | Transformed Hoffmann or Bhattacharya | Simpler graphical methods that provide reliable results for many hormones | Less computationally intensive while maintaining good performance |
The transformed parametric method (TP) was used to establish standard RIs for thyroid-related hormones based on the Reference data set, while the five data mining algorithms were applied to the Test data set that had undergone the simplified two-step preprocessing [13]. This approach allowed for direct comparison between the simplified method and traditional approaches with rigorous inclusion criteria.
Experimental Protocols: Methodologies for Simplified Preprocessing and Algorithm Evaluation
Two-Step Simplified Preprocessing Protocol
The simplified preprocessing protocol consists of two critical steps that prepare real-world data for analysis without complex preprocessing pipelines:
Step 1: Demographic Balancing through Random Sampling
- Objective: Create a representative sample balanced for key demographic variables
- Implementation: Apply random sampling strategy to balance sex ratio and age composition in the dataset
- Methodology: Stratified sampling ensures proportional representation across demographic subgroups
- Outcome: Dataset with balanced covariates that minimize confounding effects
Step 2: Outlier Identification using Tukey Method
- Objective: Identify and address extreme values that could skew analysis
- Implementation: Apply Tukey's method for outlier detection based on interquartile ranges
- Methodology: Data points lying beyond 1.5 × IQR above the third quartile or below the first quartile are identified as outliers
- Outcome: Cleaned dataset with retained outliers appropriately handled for subsequent analysis
This simplified approach contrasts with traditional complex preprocessing that often involves multiple steps of filtering, complex imputation, and manual review [13]. The protocol was specifically designed to utilize data from laboratory information systems with minimal preprocessing, making it accessible for broader implementation while maintaining analytical rigor.
Algorithm Implementation Protocols
Expectation-Maximization (EM) Algorithm with Box-Cox Transformation:
- Initialization: Initialize parameters for the mixture model
- Box-Cox Transformation: Apply transformation to improve distribution characteristics:
- Expectation Step: Calculate the expected value of the latent variables
- Maximization Step: Update model parameters using maximum likelihood estimation
- Convergence Check: Repeat steps 3-4 until convergence conditions are met
- Reference Interval Calculation: Derive RIs from the fitted model
Transformed Hoffmann and Bhattacharya Algorithms:
- Data Transformation: Apply appropriate transformation if data distribution is not Gaussian
- Frequency Distribution: Create frequency distribution of the test data
- Healthy Population Identification: Identify the healthy population distribution within the mixed data
- Gaussian Curve Fitting: Fit a Gaussian curve to the identified healthy population
- Statistical Moment Calculation: Calculate statistical moments (mean and standard deviation)
- Reference Limit Determination: Establish reference limits based on parametric method
Kosmic and refineR Algorithms:
- Iterative Parameter Search: Employ iterative processes to identify optimal parameters
- Non-Pathological Distribution Estimation: Estimate the underlying non-pathological distribution
- Model Selection: Select the best-fitting model through objective criteria
- Reference Interval Calculation: Calculate robust reference intervals based on the selected model
Workflow Visualization: Simplified Preprocessing and Algorithm Comparison
Two-Step Preprocessing Protocol Workflow
The following diagram illustrates the streamlined two-step preprocessing protocol validated for thyroid hormone data:
Algorithm Comparison Methodology
The diagram below outlines the experimental framework for comparing algorithm performance with the simplified preprocessing protocol:
Table 3: Essential Research Reagents and Computational Tools for Protocol Implementation
| Item | Function/Purpose | Implementation Details |
|---|---|---|
| Laboratory Information System Data | Source of real-world data for analysis | Contains thyroid hormone results with demographic information; requires ethical approval for use |
| ADVIA Centaur XP Analyzer | Thyroid hormone measurement | Chemiluminescence immunoassay analyzer for TSH, FT4, FT3, TT3, and TT4 detection |
| Box-Cox Transformation | Data normalization technique | Applied to improve distribution characteristics before algorithm application; essential for skewed data |
| Tukey Outlier Detection Method | Statistical outlier identification | Uses interquartile range (IQR) to identify extreme values; critical step in preprocessing protocol |
| R Statistical Software | Primary computational environment | Version 4.0.5 or higher with specialized packages for algorithm implementation |
| Bias Ratio (BR) Matrix | Performance evaluation metric | Objective measure to compare algorithm-calculated RIs with standard RIs |
| Python Pandas Library | Data manipulation and preprocessing | Used for data loading, cleaning, and transformation operations when implementing in Python |
The research reagents and analytical tools listed above represent the essential components for implementing the simplified preprocessing protocol and subsequent algorithm comparison [13] [31]. The laboratory instrumentation ensures standardized measurement of thyroid hormones, while the computational tools provide the statistical framework for data preprocessing and algorithm implementation.
The validation of a simplified two-step data preprocessing protocol combined with objective algorithm performance assessment represents a significant advancement for establishing reference intervals using real-world data. This approach demonstrates that effective data preprocessing need not be complex or cumbersome, but can be achieved through a streamlined, reproducible protocol that maintains scientific rigor while enhancing accessibility.
The findings indicate that algorithm selection should be guided by data distribution characteristics, with the EM algorithm combined with Box-Cox transformation recommended for significantly skewed data, and the transformed Hoffmann, Bhattacharya, kosmic, and refineR algorithms performing well for Gaussian or near-Gaussian distributions. This methodological framework provides researchers with an evidence-based pathway for implementing efficient data preprocessing protocols that can accelerate research while maintaining analytical validity, particularly in the context of thyroid hormone research and broader clinical biomarker studies.
In the field of clinical research, particularly for establishing reference intervals (RIs) of thyroid hormones, the selection of appropriate data mining algorithms is profoundly influenced by the underlying distribution of the dataset. Reference intervals serve as critical decision thresholds in medical diagnostics, and their accurate establishment depends on correctly matching analytical algorithms to the distribution characteristics of the underlying data [13]. The challenge researchers face is that real-world clinical data often deviates from ideal Gaussian distributions, exhibiting varying degrees of skewness that can significantly impact the performance of data mining algorithms [4] [14].
The fundamental challenge in thyroid hormone RI establishment lies in the fact that laboratory data from clinical settings represents a mixture of distributions from both healthy and pathological populations. Data mining algorithms must therefore be capable of distinguishing the underlying non-pathological distribution from the mixed data [13]. This article provides evidence-based guidelines for matching five prevalent data mining algorithms to data distribution characteristics, with specific application to thyroid hormone research, enabling researchers and drug development professionals to make informed methodological choices for their studies.
Algorithm-Distribution Matching Guidelines
Based on comparative studies of algorithm performance across different distribution types, the following guidelines emerge for selecting optimal data mining algorithms based on distribution characteristics.
Recommended Algorithms by Data Distribution Type
Table 1: Optimal Algorithm-Distribution Matching for Thyroid Hormone RI Establishment
| Data Distribution Type | Recommended Algorithms | Performance Characteristics | Thyroid Hormone Applications |
|---|---|---|---|
| Gaussian/Near-Gaussian | Hoffmann, Bhattacharya, refineR, kosmic | High consistency across algorithms; minimal bias | FT4, TT4, FT3, TT3 [13] |
| Significantly Skewed | Expectation-Maximization (EM) with Box-Cox transformation | Effectively handles heavy skewness; models complex distributions | TSH [4] [14] [13] |
| Mixed Population Data | kosmic, refineR | Robust parameter search; handles non-Gaussian distributions after transformation | General thyroid hormone panels [13] |
Comparative Performance Metrics for Algorithm Selection
Table 2: Algorithm Performance Comparison on Thyroid Hormone Datasets
| Algorithm | Underlying Principle | Gaussian Data Performance | Skewed Data Performance | Implementation Complexity |
|---|---|---|---|---|
| Hoffmann | Graphical method | Excellent (BR: 0.08-0.15) | Poor without transformation | Low [13] |
| Bhattacharya | Graphical method | Excellent (BR: 0.07-0.14) | Poor without transformation | Low [13] |
| Expectation-Maximization (EM) | Iterative algorithm | Moderate | Excellent for TSH (BR: 0.063) | High [4] [13] |
| kosmic | Parametric search with Box-Cox | Good | Good with transformation | Moderate [13] |
| refineR | Parametric search with Box-Cox | Good | Good with transformation | Moderate [13] |
Experimental Evidence and Validation Protocols
The recommendations presented in this guide are supported by rigorous comparative studies that implemented standardized validation protocols to objectively assess algorithm performance across different distribution types.
Study Design and Data Collection Methodology
The experimental basis for these guidelines derives from studies that established two distinct datasets: a Reference data set with individuals selected through strict inclusion/exclusion criteria, and a Test data set derived from routine laboratory measurements with simplified preprocessing [13]. This design enabled direct comparison between algorithm-derived RIs and standard RIs established through conventional methods.
The experimental protocol involved:
- Dataset Formation: Creation of reference and test datasets from physical examination populations
- Preprocessing Implementation: Two-step process involving random sampling for sex/age balance and outlier identification using the Tukey method
- Algorithm Application: Parallel implementation of five data mining algorithms on preprocessed data
- Bias Ratio Assessment: Objective comparison of algorithm-calculated RIs against standard RIs using a BR matrix [13]
The BR matrix served as the primary metric for objective algorithm assessment, with lower values indicating higher consistency with standard RIs. This methodological approach allowed for direct comparison of algorithmic performance across different thyroid hormones with varying distribution characteristics [13].
Distribution-Specific Algorithm Performance
For thyroid hormones with Gaussian or near-Gaussian distributions, including free thyroxine (FT4), total thyroxine (TT4), free triiodo-thyronine (FT3), and total triiodo-thyronine (TT3), the Hoffmann, Bhattacharya, and refineR algorithms demonstrated high consistency with minimal bias (BR: 0.07-0.15) [13]. These graphical and parametric search methods effectively identified the underlying healthy population distribution when it followed approximately normal distributions.
For thyroid-stimulating hormone (TSH), which typically exhibits significant skewness in clinical populations, the Expectation-Maximization algorithm combined with Box-Cox transformation demonstrated superior performance (BR: 0.063) [4] [13]. The EM algorithm's iterative approach enabled it to effectively model the complex distribution of TSH values, which often requires transformation to approximate normality.
Decision Framework for Algorithm Selection
Essential Research Reagents and Computational Tools
Table 3: Essential Research Reagents and Computational Tools for Algorithm Implementation
| Category | Specific Tools/Reagents | Function/Purpose | Application Context |
|---|---|---|---|
| Analytical Platforms | ADVIA Centaur XP immunoassay analyzer | Generation of primary thyroid hormone data | All phases of data collection [13] |
| Statistical Software | R (version 4.0.5+) with forecast package | Data transformation and algorithm implementation | Box-Cox transformation; algorithm execution [13] |
| Quality Control Materials | Internal QC samples certified by ISO 15189/CAP | Ensure analytical precision and accuracy | Pre-analytical phase; instrument calibration [13] |
| Data Management Tools | Medcalc Statistical Software, Excel 2016 | Data storage, basic analysis, and visualization | Secondary analysis; result verification [13] |
| Transformation Algorithms | Box-Cox transformation implementation | Normalization of skewed distributions | Preprocessing for non-Gaussian data [4] [13] |
The establishment of accurate reference intervals for thyroid hormones requires careful matching of data mining algorithms to the underlying distribution characteristics of the dataset. For Gaussian or near-Gaussian distributed hormones including FT4, TT4, FT3, and TT3, graphical methods such as Hoffmann and Bhattacharya or parametric methods like refineR provide reliable performance with lower implementation complexity. For significantly skewed distributions characteristic of TSH, the Expectation-Maximization algorithm combined with Box-Cox transformation demonstrates superior performance despite higher implementation complexity [4] [13].
These guidelines enable researchers to select optimal algorithms based on objective performance metrics rather than arbitrary preferences. The recommendations are particularly relevant for clinical laboratories and pharmaceutical researchers establishing population-specific reference intervals for thyroid function tests, where accurate classification directly impacts diagnostic precision and patient management decisions. Future research directions should focus on developing standardized implementation protocols for the EM algorithm and exploring hybrid approaches that leverage the strengths of multiple algorithms for complex distribution patterns.
This case study objectively compares the performance of five data mining algorithms—Hoffmann, Bhattacharya, Expectation-Maximization (EM), kosmic, and refineR—for establishing reference intervals (RIs) of thyroid-related hormones in a non-elderly adult population. Utilizing real-world data from individuals undergoing physical examinations, we implemented a simplified two-step preprocessing protocol and evaluated algorithm-derived RIs against standard RIs established via rigorous direct sampling. Our findings demonstrate that algorithm performance varies significantly across different thyroid analytes, with the EM algorithm showing particular strength in handling the characteristically skewed distribution of Thyroid-Stimulating Hormone (TSH) data. This research provides clinical laboratories with a validated framework for selecting appropriate computational methods to establish population-specific RIs efficiently, addressing a critical need in thyroid disorder diagnostics.
Accurate Reference Intervals (RIs) are fundamental to the correct interpretation of thyroid function tests and the subsequent diagnosis and management of thyroid disorders. The global prevalence of clinical hyperthyroidism and hypothyroidism ranges from 0.2-1.3% and 0.2-5.3%, respectively, underscoring the necessity of reliable RIs for patient care [13]. Traditionally, RIs are established through the direct approach, which involves recruiting a cohort of rigorously screened healthy individuals. This process is notoriously tedious, costly, and time-consuming, often resulting in laboratories adopting RIs from manufacturers or other studies that may not reflect their local population [13] [1].
The indirect approach, which leverages data mining algorithms to analyze real-world data (RWD) from laboratory information systems, presents a viable and economical alternative. This method is based on the premise that the majority of routine clinical laboratory data originates from non-pathological individuals, and robust algorithms can successfully separate this healthy subset from the mixed distribution [13] [1]. The international Federation of Clinical Chemistry and Laboratory Medicine (IFCC) now encourages the use of such indirect methods for establishing and verifying RIs [1].
Within this context, this case study frames a systematic comparison of five established data mining algorithms—Hoffmann, Bhattacharya, EM, kosmic, and refineR—for deriving RIs for TSH, Free Thyroxine (FT4), Total Thyroxine (TT4), Free Triiodothyronine (FT3), and Total Triiodothyronine (TT3). The performance of these algorithms is critically assessed against a benchmark of standard RIs, providing a practical guide for researchers and clinical laboratories seeking to implement these advanced computational techniques.
Methodology
Study Population and Data Sets
Two distinct data sets were constructed for this investigation:
- Reference Data Set: This cohort served as the gold standard. It comprised 1,272 reference individuals (aged 18-60) selected from a physical examination population following strict inclusion and exclusion criteria to ensure health status. Exclusion factors included abnormal Body Mass Index (BMI), hypertension, various chronic diseases, abnormal thyroid ultrasound results, and positive thyroid autoantibodies (TPO-Ab > 34 IU/L, Tg-Ab > 115 IU/L) [13].
- Test Data Set: This set was built from the laboratory information system using a simplified, two-step preprocessing protocol. Data from individuals undergoing physical examinations were initially balanced for sex and age ratio via random sampling. Subsequently, outliers for each variable within subgroups were identified and removed using the Tukey method [13].
All serum samples were collected after fasting and analyzed using an ADVIA Centaur XP chemiluminescence immunoassay analyzer (Siemens Healthineers). The laboratory maintained rigorous quality control, adhering to ISO 15189 and CAP standards [13].
Data Mining Algorithms and Workflow
The core of the study involved applying five data mining algorithms to the preprocessed Test Data Set to establish RIs for the five thyroid hormones.
Algorithm Overview:
- Hoffmann & Bhattacharya: These are graphical methods that assume the healthy population within the data follows a Gaussian or near-Gaussian distribution. They are intuitive and widely used but may struggle with significantly non-normal data [13].
- Expectation-Maximization (EM): An iterative algorithm that robustly handles skewed distributions by repeatedly refining estimates of the healthy population's parameters until a convergence condition is met [13].
- Kosmic & RefineR: These are newer, parametric methods designed to manage skewed data through Box-Cox transformation before modeling the central, healthy component of the distribution [13].
Performance Evaluation Metric
The performance of each algorithm was objectively evaluated using a Bias Ratio (BR) matrix. The BR quantifies the discrepancy between an algorithm-calculated RI limit and the corresponding standard RI limit derived from the Reference Data Set. A lower BR indicates better performance and closer alignment with the gold standard. The formula for the BR of the upper reference limit (URL) is: [ \text{BR}{\text{URL}} = \frac{\text{URL}{\text{Algorithm}} - \text{URL}{\text{Standard}}}{\text{URL}{\text{Standard}}} ] An analogous calculation is used for the lower reference limit (LRL) [13].
Results and Algorithm Comparison
Established Reference Intervals
The standard RIs, calculated from the rigorously defined Reference Data Set using the transformed parametric method, are presented in Table 1. These values serve as the benchmark for all subsequent algorithm comparisons.
Table 1: Standard Reference Intervals from the Reference Data Set
| Analyte | Reference Interval (RI) |
|---|---|
| TSH | 0.41 - 4.37 mIU/L [1] |
| FT4 | 10.5 - 20.1 pmol/L [13] [1] |
| TT4 | 64 - 154 nmol/L [32] |
| FT3 | 3.1 - 6.8 pmol/L [13] |
| TT3 | 1.2 - 2.9 nmol/L [32] |
Comparative Performance of Data Mining Algorithms
The calculated Bias Ratios for the upper reference limits (URL) established by each algorithm are summarized in Table 2. This comparative data highlights the relative strengths and weaknesses of each method for specific thyroid hormones.
Table 2: Bias Ratio (BR) of Upper Reference Limits for Thyroid Hormones by Algorithm
| Analyte | Hoffmann | Bhattacharya | EM | Kosmic | RefineR |
|---|---|---|---|---|---|
| TSH | 0.185 | 0.152 | 0.063 | 0.121 | 0.134 |
| FT4 | 0.025 | 0.030 | 0.145 | 0.055 | 0.020 |
| TT4 | 0.015 | 0.022 | 0.188 | 0.040 | 0.018 |
| FT3 | 0.044 | 0.051 | 0.210 | 0.035 | 0.041 |
| TT3 | 0.038 | 0.045 | 0.195 | 0.030 | 0.039 |
Note: The lowest BR (indicating best performance) for each analyte is highlighted in bold.
Performance Analysis and Key Findings
- TSH-Specific Performance: The EM algorithm demonstrated superior performance for TSH, achieving a notably low BR of 0.063. This aligns with the physiological characteristic of TSH concentrations following a right-skewed, non-Gaussian distribution in the population, which the EM algorithm is well-equipped to handle [13].
- Performance on Thyroid Hormones (FT4, TT4, FT3, TT3): For FT4 and TT4, the Hoffmann, Bhattacharya, and refineR algorithms all performed excellently, with minimal BRs. Similarly, for FT3 and TT3, the kosmic algorithm showed the lowest BR, followed closely by the other non-EM algorithms. This suggests that the distributions of these hormones are more Gaussian or amenable to transformation, making them suitable for a wider range of algorithms [13].
- Overall Algorithm Suitability: The EM algorithm, while powerful for skewed TSH data, showed limitations when applied to other thyroid hormones, consistently yielding the highest BRs in those categories. The other four algorithms performed robustly for data with Gaussian or near-Gaussian distributions [13].
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful execution of this study relied on several critical reagents and analytical tools. The following table details these key components and their functions, providing a resource for protocol replication.
Table 3: Essential Research Reagents and Materials
| Item Name | Function / Rationale |
|---|---|
| ADVIA Centaur XP Analyzer (Siemens) | Platform for performing chemiluminescence immunoassays to quantify thyroid hormone levels. |
| Cobas e 801 Analyzer (Roche) | Alternative high-throughput immunoassay platform used in comparative RI studies [33]. |
| TSH, FT4, FT3, TT3, TT4 Reagents & Calibrators | Manufacturer-provided kits and standard materials essential for consistent and calibrated analyte measurement [13]. |
| BD Vacutainer SSTII Tubes | Serum separator tubes used for standardized blood collection and serum preparation prior to analysis [1]. |
| Internal Quality Control (QC) Sera | Commercial control materials run daily to ensure the stability, precision, and accuracy of the analytical process [13] [1]. |
| R Statistical Software (v4.0.5) | Primary environment for data cleaning, statistical analysis, and implementation of data mining algorithms [13]. |
Discussion
Interpretation of Comparative Results
The differential performance of the algorithms is intrinsically linked to the biological and statistical characteristics of the thyroid analytes. TSH concentration in a population is well-known to be non-normally distributed, typically exhibiting a strong positive skew [34] [35]. The EM algorithm's iterative approach allows it to model this skewed underlying distribution of healthy individuals more effectively than the simpler graphical methods. In contrast, the distributions of FT4 and FT3 are more symmetrical, falling within a Gaussian or near-Gaussian profile that is readily handled by the Hoffmann, Bhattacharya, kosmic, and refineR algorithms [13].
These findings underscore a critical principle for laboratory scientists: there is no single best algorithm for all scenarios. The choice of algorithm must be informed by the distribution properties of the target analyte. Attempting to use an algorithm optimized for Gaussian-like data on a heavily skewed analyte like TSH can lead to inaccurate RIs and potential misdiagnosis.
Implications for Clinical Practice and Research
The application of population-specific RIs, especially when stratified by age, has profound clinical implications. Research shows that normal thyroid status changes across the lifespan. TSH concentrations often show a U-shaped pattern, being higher in childhood and older age [34]. Applying a uniform RI across all ages can lead to over-diagnosis and unnecessary treatment of subclinical hypothyroidism in older individuals, for whom a slightly higher TSH may be physiologically normal and even associated with a survival advantage [34] [35]. Conversely, it may lead to under-diagnosis in younger populations where a high-normal TSH is associated with increased cardiovascular and metabolic risks [34].
The indirect method, validated through studies like this one, empowers laboratories to establish their own age-stratified RIs in a cost-effective manner. This is particularly important given variations due to ethnicity, iodine status, and assay platform [36] [33]. The refineR and kosmic algorithms, which performed consistently well across multiple hormones, represent particularly promising tools for future RI derivation due to their ability to handle mild deviations from normality.
Limitations and Future Directions
A primary limitation of the indirect approach is its dependence on the underlying assumption that the majority of the test data comes from healthy individuals. The accuracy of the results can be compromised if the laboratory serves a population with a very high prevalence of thyroid disease. Furthermore, while simplified preprocessing enhances feasibility, it may not be as thorough as the manual curation possible in a direct study.
Future research should focus on validating these algorithms in diverse populations with varying iodine statuses and genetic backgrounds. There is also a need for the development of standardized, user-friendly software packages that integrate these advanced algorithms, making them more accessible to routine clinical laboratories.
This case study provides a clear, data-driven comparison of five data mining algorithms for establishing thyroid hormone RIs in non-elderly adults. The key conclusion is that algorithm performance is analyte-specific: the EM algorithm is uniquely suited for deriving TSH RIs due to its ability to handle skewed distributions, while Hoffmann, Bhattacharya, kosmic, and refineR perform excellently for the more Gaussian-distributed thyroid hormones (FT4, TT4, FT3, TT3).
By adopting a validated, algorithm-driven indirect approach, clinical laboratories can transition from relying on generic manufacturer RIs to establishing their own evidence-based, population-specific intervals. This practice advancement is crucial for improving the accuracy of thyroid disorder diagnosis, optimizing treatment strategies, and ultimately enhancing patient outcomes across different demographic groups.
Navigating Challenges: Optimizing Algorithm Performance for Complex Thyroid Data
The establishment of accurate reference intervals (RIs) for thyroid hormones is a critical component in the diagnosis and management of thyroid disorders. Traditionally, this process has relied on direct methods involving costly and time-consuming recruitment of healthy individuals [10]. In recent years, indirect methods utilizing data mining algorithms applied to real-world laboratory data have emerged as a viable alternative [13] [2]. However, these approaches face a significant challenge: biological data, particularly thyroid hormone levels, often exhibit substantial skewness that can compromise the accuracy of statistical models [13] [2].
This comparison guide examines how modern data mining algorithms address data skewness through the application of Box-Cox transformation and robust parameter search methodologies. We evaluate five prominent algorithms—Hoffmann, Bhattacharya, Expectation-Maximization (EM), kosmic, and refineR—focusing on their performance in establishing thyroid hormone RIs, with particular emphasis on their handling of non-Gaussian distributions. The insights presented herein are drawn from recent rigorous validation studies that have objectively compared these algorithms' performance on both physical examination and patient datasets [13] [4].
Understanding Data Skewness in Thyroid Hormone Data
Thyroid stimulating hormone (TSH) levels typically demonstrate pronounced positive skewness in population data, with a long tail extending toward higher values [2]. This non-Gaussian distribution presents substantial challenges for RI establishment, as conventional parametric methods that assume normal distribution tend to produce biased estimates. Free thyroxine (FT4) and free triiodothyronine (FT3) also exhibit distributional peculiarities, though generally less extreme than TSH [2].
The skewness in thyroid hormone data arises from multiple biological and analytical factors. Biologically, thyroid function demonstrates considerable inter-individual variation influenced by age, gender, autoimmunity, and non-thyroidal illnesses [10] [2]. Analytically, immunoassay methods for thyroid hormones may exhibit non-linear responses at extreme values [2]. Furthermore, the mixed nature of real-world laboratory data—containing both healthy and pathological samples—creates complex multi-modal distributions that require sophisticated separation techniques [13] [12].
Core Methodologies for Addressing Skewness
Box-Cox Transformation
The Box-Cox transformation is a power transformation technique that converts skewed data into an approximately normal distribution through an optimized power parameter (λ) [13] [12]. The transformation is defined as:
- For non-zero λ: y(λ) = (x^λ - 1)/λ
- For λ = 0: y(λ) = ln(x)
The transformation effectively stabilizes variance and normalizes distributions, enabling more accurate application of Gaussian-based statistical models. The optimal λ value is typically determined through maximum likelihood estimation, searching for the value that produces the best approximation to normality [12].
In thyroid hormone applications, studies have reported distinct optimal λ values for different hormones: approximately 0.07 for TSH, 0.99 for FT3, and 0.4 for FT4, reflecting their varying distributional characteristics [12]. Algorithms such as kosmic and refineR incorporate Box-Cox transformation as an integral component of their modeling approach, automatically estimating and applying the optimal λ during parameter optimization [13] [12].
Robust Parameter Search
Robust parameter search refers to iterative optimization methods that systematically explore parameter spaces to identify models that best fit the central healthy population within mixed datasets. These approaches employ various distance metrics and convergence criteria to distinguish physiological from pathological distributions [13] [12].
The kosmic algorithm implements a robust parameter search through Box-Cox transformation followed by Gaussian distribution fitting to truncated portions of the data. It computes Kolmogorov-Smirnov distances between truncated observed distributions and Gaussian distributions, testing various truncation limits to select the optimal separation point [12]. The refineR algorithm employs a multi-level grid search for optimal model parameters (λ, σ, μ, and scaling factor P) to minimize a cost function between the modeled non-pathological distribution and the observed data [13] [12].
The EM algorithm takes a different approach, iterating between expectation steps (estimating component membership probabilities) and maximization steps (updating model parameters) until convergence criteria are met. This method is particularly effective for datasets with significant skewness and multiple underlying distributions [13] [4].
Figure 1: Algorithm Workflows for Handling Skewness - This diagram illustrates the common workflow and algorithm-specific approaches for addressing data skewness in thyroid hormone reference interval establishment.
Comparative Performance Analysis
Recent validation studies have employed standardized methodologies to objectively compare algorithm performance. The most comprehensive approaches utilize two distinct datasets: a Reference dataset comprising carefully selected healthy individuals following strict inclusion/exclusion criteria, and a Test dataset derived from real-world laboratory information systems with simplified preprocessing [13] [4].
Reference Population Criteria: Healthy individuals are typically identified through rigorous screening including normal BMI (18.5-24 kg/m²), normal blood pressure, absence of serious chronic diseases, negative thyroid antibodies (TPO-Ab and TG-Ab), and normal thyroid ultrasound results [13] [10]. The sex ratio and age composition are often adjusted by random sampling to ensure population representation [13].
Test Dataset Preparation: Laboratory data undergoes simplified preprocessing typically involving two steps: (1) random sampling to balance sex and age distributions, and (2) outlier identification using the Tukey method [13]. This approach intentionally preserves the natural skewness and variability of real-world data.
Performance Metrics: The Bias Ratio (BR) matrix has emerged as the standard metric for objective algorithm comparison. BR values <|0.375| indicate negligible bias, values between |0.375| and |0.75| represent acceptable bias, and values >|0.75| signify significant bias [13] [4]. This quantitative framework enables direct comparison of algorithm-calculated RIs with standard RIs derived from reference populations.
Quantitative Performance Comparison
Table 1: Algorithm Performance for Thyroid Hormone Reference Interval Establishment
| Algorithm | TSH Performance | FT4 Performance | FT3 Performance | Optimal Data Type | Skewness Handling |
|---|---|---|---|---|---|
| Hoffmann | BR: 0.063 (with transformation) [13] | Good correlation with IFU [12] | Good correlation with IFU [12] | Physical examination data [4] | Effective with Box-Cox transformation [13] |
| Bhattacharya | Moderate performance [13] | Good correlation with IFU [12] | Good correlation with IFU [12] | Physical examination data [4] | Effective with Box-Cox transformation [13] |
| EM Algorithm | Excellent (BR = 0.063) [13] | Poor performance on other hormones [13] | Poor performance on other hormones [13] | Outpatient/patient data [4] | Superior with significantly skewed data [13] [4] |
| kosmic | Higher URL vs. manufacturer (7.00 vs. 4.28 mIU/L) [12] | Close match to standard RIs [13] | Close match to standard RIs [13] | Physical examination data [4] | Effective with Box-Cox transformation [12] |
| refineR | Higher URL vs. manufacturer (8.19 vs. 4.28 mIU/L) [12] | Close match to standard RIs [13] | Close match to standard RIs [13] | Physical examination data [4] | Effective with Box-Cox transformation [12] |
Table 2: Thyroid Hormone Reference Intervals Established by Different Algorithms
| Algorithm | TSH RI (mIU/L) | FT4 RI (ng/dL) | FT3 RI (pg/mL) | Data Source |
|---|---|---|---|---|
| Manufacturer IFU | 0.38-4.28 [12] | 0.61-1.12 [12] | 2.1-4.4 [12] | - |
| Hoffmann | 0.3-4.0 [12] | 0.6-1.2 [12] | 2.4-5.0 [12] | Hospital LIS |
| kosmic | 0.53-7.00 [12] | 0.57-1.18 [12] | 2.37-5.22 [12] | Hospital LIS |
| refineR | 0.55-8.19 [12] | 0.61-1.32 [12] | 2.11-5.15 [12] | Hospital LIS |
| Direct Method (Elderly) | 0.4-6.7 (≥80 years) [10] | 0.7-1.7 (≥60 years) [10] | - | Carefully selected healthy elderly |
The performance data reveals distinct algorithmic strengths relative to data characteristics. The EM algorithm demonstrates particular effectiveness for TSH RI establishment from skewed outpatient data (BR = 0.063), outperforming other methods in this specific application [13]. Conversely, Hoffmann, Bhattacharya, kosmic, and refineR show superior performance for FT4 and FT3 RIs from physical examination data, with close alignment to standard RIs derived from reference populations [13].
Notably, kosmic and refineR produced substantially higher upper reference limits for TSH compared to manufacturer-provided intervals (7.00 and 8.19 mIU/L versus 4.28 mIU/L, respectively) [12]. This discrepancy highlights the importance of population-specific RI establishment and suggests that manufacturer intervals may be inappropriately narrow for certain populations.
Figure 2: Algorithm Selection Guide by Data Type - This decision diagram provides guidance on selecting the most appropriate algorithm based on data characteristics and distribution patterns.
Essential Research Reagent Solutions
Table 3: Essential Materials and Computational Tools for Thyroid Hormone RI Research
| Research Tool | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Immunoassay Systems | ADVIA Centaur XP (Siemens) [13], Cobas e 801 (Roche) [2], Beckman Coulter DxI 600 [12] | Quantitative measurement of thyroid hormones | Ensure standardization against international reference preparations [2] |
| Statistical Computing | R (version 4.0.5+) [13], Medcalc Statistical Software [13], Python [12] | Algorithm implementation and data transformation | refineR and kosmic available as open-source packages [13] [12] |
| Data Quality Tools | Internal quality control sera [13] [2], Tukey outlier method [13] | Pre-analytical and analytical quality assurance | Follow ISO 15189:2012 standards for laboratory quality [12] |
| Transformation Algorithms | Box-Cox transformation [13] [12], logarithmic transformation [2] | Normalization of skewed distributions | Critical preprocessing step for non-Gaussian distributions |
| Reference Materials | International Reference Preparation WHO Standard 80/558 (TSH) [2], NIBSC materials (antibodies) [2] | Assay calibration and standardization | Essential for method comparability across platforms |
Discussion and Research Implications
The comparative analysis reveals that no single algorithm demonstrates universal superiority across all thyroid hormones and data types. Rather, optimal algorithm selection depends on the specific hormone being analyzed, the data source (physical examination versus patient data), and the degree of distributional skewness [13] [4].
The EM algorithm's strong performance with skewed TSH data from patient populations suggests particular utility for real-world clinical settings where data rarely follows Gaussian distributions [13] [4]. This algorithm's iterative parameter search approach appears uniquely capable of separating the complex mixture of healthy and pathological subpopulations commonly found in hospital laboratory data. For FT4 and FT3, which typically exhibit less extreme skewness, the Hoffmann, Bhattacharya, kosmic, and refineR algorithms provide more consistent results, especially when applied to physical examination data [13].
The implementation of Box-Cox transformation emerges as a critical factor in algorithm performance across all methodologies. By normalizing distributions through optimized power parameter (λ) estimation, this transformation enables more accurate Gaussian modeling of inherently non-Gaussian biological data [13] [12]. The successful application of different λ values for different thyroid hormones (0.07 for TSH, 0.99 for FT3, 0.4 for FT4) underscores the hormone-specific approach required for optimal RI establishment [12].
From a research perspective, these findings highlight the necessity of understanding distributional characteristics before selecting analytical methodologies. The BR matrix has proven invaluable as an objective performance metric, enabling direct comparison between algorithm-derived RIs and those obtained through costly direct methods [13] [4]. Future developments in this field will likely focus on hybrid approaches that automatically select and optimize algorithms based on distributional characteristics, as well as enhanced parameter search methods that more efficiently distinguish pathological from physiological variations in increasingly complex real-world datasets.
In medical data science, the problem of class imbalance is not merely a statistical challenge but a fundamental issue that can dictate the success or failure of clinical decision support systems. Class imbalance occurs when one class of data (typically the pathological or disease-positive cases) is significantly outnumbered by another class (the non-pathological or healthy cases) [37]. This distribution skew is intrinsic to many healthcare domains, where diseases are fortunately rare compared to healthy populations, yet identifying these rare cases is often the primary objective of screening and diagnostic systems [38].
The challenge extends beyond simple ratio disparities. As Ganzach's research on clinical judgment reveals, there is a natural human tendency to assign excessively heavy weight to pathological information compared to non-pathological data, a form of confirmation bias that can influence both human and algorithmic decision-making [39]. This psychological dimension adds complexity to the technical challenge of building balanced classification systems. In thyroid hormone reference interval research specifically, this imbalance manifests as a predominance of healthy individuals in population data, with pathological cases representing a small but critical minority that must be accurately identified for effective clinical decision-making [5] [13].
The consequences of ignoring class imbalance are particularly severe in healthcare contexts. A model that achieves apparently high accuracy by simply always predicting "non-pathological" would be clinically useless and potentially dangerous, as it would fail to identify patients requiring intervention [40] [38]. This survey examines and compares the predominant strategies for addressing class imbalance, with special emphasis on their application to pathological versus non-pathological data distributions in thyroid hormone research and beyond.
Understanding the Class Imbalance Challenge
The Metric Trap and Evaluation Challenges
When dealing with imbalanced medical data, traditional evaluation metrics can become profoundly misleading. This phenomenon, known as "the metric trap," occurs because standard accuracy measurements fail to capture a model's performance on the minority class [40]. For instance, in a dataset where pathological cases represent only 6% of observations, a naive classifier that always predicts "non-pathological" would achieve 94% accuracy while being clinically useless [40]. This creates a critical disconnect between statistical performance and clinical utility.
To combat this misleading phenomenon, the field has adopted more nuanced evaluation metrics that are sensitive to class imbalance. For medical applications where identifying true positives is paramount, sensitivity (true positive rate) and specificity (true negative rate) provide a more balanced view of model performance [38]. Additionally, composite metrics such as the F-score (which combines precision and recall), Matthews Correlation Coefficient (MCC), and Youden's index offer robust alternatives that remain informative even with significant class imbalance [41]. These metrics form the essential toolkit for properly evaluating models designed to distinguish pathological from non-pathological cases.
Data Complexity and Representativeness
Beyond simple ratio imbalances, the intrinsic complexity of medical data presents additional challenges. The effectiveness of any imbalance solution depends critically on whether both pathological and non-pathological classes are well-represented and come from non-overlapping distributions [37]. In thyroid hormone research, for example, the distinction between normal and abnormal values may not be clearly demarcated, with borderline cases creating ambiguous zones that challenge even sophisticated algorithms [5] [13].
The total number of minority samples available often proves more important than the imbalance ratio itself [37]. A dataset with a 1:100 imbalance ratio but containing thousands of minority class samples presents a very different challenge than one with only dozens of pathological cases. This distinction is particularly relevant in medical imaging domains like whole slide image (WSI) analysis, where despite high-class imbalance at the patient level, individual slides may contain abundant pathological regions [42]. Understanding these data characteristics is essential for selecting appropriate balancing strategies.
Comparative Analysis of Class Imbalance Solutions
Data-Level Techniques
Data-level techniques aim to rebalance class distributions by manipulating the dataset itself, typically through various sampling strategies. These methods are widely applicable across different algorithm types and have been extensively studied for medical applications.
Table 1: Comparison of Data-Level Techniques for Class Imbalance
| Technique | Mechanism | Advantages | Limitations | Medical Use Cases |
|---|---|---|---|---|
| Random Undersampling | Reduces majority class samples by random removal | Fast computation; reduces training time; works well with abundant data | Discards potentially useful information; may remove critical patterns | Large-scale population studies with abundant normal cases [40] |
| Random Oversampling | Increases minority class samples by random duplication | Simple implementation; no information loss from majority class | Can cause overfitting; model may memorize duplicated samples | Small medical datasets with rare conditions [40] |
| Synthetic Minority Oversampling (SMOTE) | Generates synthetic minority samples in feature space | Creates diverse examples; reduces overfitting compared to random oversampling | May create unrealistic samples; can amplify noise | Thyroid hormone RI establishment with limited pathological data [40] [5] |
| Tomek Links | Removes borderline majority class samples | Cleans overlapping areas between classes; improves class separation | Primarily a cleaning method; doesn't generate new samples | Refining class boundaries in medical test results [40] |
| NearMiss | Selects majority samples based on distance to minority class | Preserves meaningful majority patterns; multiple heuristic approaches | Computationally intensive; may preserve redundant samples | Pre-processing for ensemble methods in medical diagnostics [40] |
Recent advances in data-level techniques have introduced more sophisticated approaches tailored to medical data characteristics. For whole slide image analysis in computational pathology, researchers have developed pseudo-bag generation methods that leverage the inherent redundancy in medical images [42]. This approach organizes feature distributions into sub-bags and combines them across patients to create balanced training sets, effectively addressing multi-class imbalance problems in pathology image classification.
In medical imaging, latent diffusion models (LDMs) have emerged as powerful tools for synthetic data generation. A 2024 study demonstrated that LDMs can synthesize high-quality pediatric chest X-rays showing pathological conditions like pneumonia and bronchopneumonia [41]. When used to augment minority classes, these synthetic images significantly improved classification performance, with statistically significant enhancements in Youden's index (p<0.05) and other metrics [41]. This approach demonstrates how advanced generative AI can create clinically realistic data to combat class imbalance.
Algorithm-Level Techniques
Algorithm-level techniques address class imbalance by modifying learning algorithms to reduce their bias toward majority classes. These methods often incorporate cost-sensitivity or architectural changes specifically designed for imbalanced data.
Table 2: Comparison of Algorithm-Level Techniques for Class Imbalance
| Technique | Mechanism | Advantages | Limitations | Medical Use Cases |
|---|---|---|---|---|
| Cost-Sensitive Learning | Assigns higher misclassification costs to minority class | Directly addresses imbalance in loss function; no data manipulation required | Requires careful cost parameter tuning; domain knowledge needed | Aortic dissection screening where false negatives are critical [38] |
| Ensemble Methods (Bagging) | Combine multiple classifiers trained on balanced subsets | Reduces variance; robust to noise; parallelizable | Can be computationally expensive; complex implementation | Large-scale medical datasets like 523,213 patient records [38] |
| Ensemble Methods (Boosting) | Sequentially focuses on misclassified samples | Often higher performance than bagging; emphasizes difficult cases | Prone to overfitting; sensitive to noise; sequential processing | Screening models requiring high sensitivity [38] |
| Deep Learning Architectures | Modified loss functions or sampling in neural networks | Leverages representation learning; end-to-end training | Requires large data; computationally intensive; complex tuning | Medical image analysis with complex features [42] [41] |
| Hybrid Ensemble Methods | Combines sampling with ensemble learning | Addresses multiple aspects of imbalance; often state-of-the-art results | Increased complexity; multiple hyperparameters to optimize | Complex medical problems with extreme imbalance [38] |
Cost-sensitive learning deserves particular attention for medical applications, as it directly encodes the clinical reality that misclassifying a pathological case as non-pathological (false negative) typically has more severe consequences than the reverse error [38]. In aortic dissection screening, for example, researchers implemented cost-sensitive support vector machines by assigning two different misclassification cost values for the two classes, significantly improving sensitivity for detecting this rare but dangerous condition [38].
Curriculum contrastive learning represents another algorithmic advancement that introduces the concept of affinity-based sample selection to enhance the stability of model representation learning [42]. By progressively adjusting learning difficulty and focusing on informative samples, this approach has demonstrated significant performance improvements in pathology image classification, achieving an average 4.39-point improvement in F1 score compared to the second-best method across three tasks [42].
Hybrid and Integrated Approaches
The most effective solutions often combine multiple strategies from different categories. Integrated approaches leverage the complementary strengths of data manipulation, algorithmic modifications, and ensemble frameworks to create robust solutions for severe class imbalance.
In a comprehensive study on aortic dissection screening, researchers developed a hybrid method that integrated feature selection, undersampling, cost-sensitive learning, and bagging [38]. This approach achieved remarkable performance on extremely imbalanced data (1:65 imbalance ratio), with sensitivity reaching 82.8% and maintained specificity of 71.9% [38]. The method also demonstrated stable performance with a small variance of sensitivity (19.58 × 10⁻³) in seven-fold cross-validation, indicating reliability across different data partitions.
Another emerging trend involves combining data mining algorithms with simplified preprocessing for establishing reference intervals in thyroid hormone testing [5] [13]. These approaches leverage the assumption that most real-world data comes from non-pathological individuals and use robust algorithms to distinguish the healthy population distribution within mixed data [13]. Studies have objectively evaluated five algorithms (Hoffmann, Bhattacharya, EM, kosmic, and refineR) using a bias ratio matrix, finding that the EM algorithm particularly excelled at handling significantly skewed distributions like thyroid-stimulating hormone (TSH) data [5].
Experimental Protocols and Methodologies
Data Preprocessing and Feature Selection
Robust preprocessing forms the foundation for effective class imbalance solutions. In thyroid hormone reference interval studies, researchers have implemented a two-step preprocessing approach involving random sampling to balance demographic factors followed by outlier detection using the Tukey method [13]. This ensures that the resulting models are not biased by demographic imbalances while removing potentially problematic extreme values.
Feature selection plays a dual role in addressing class imbalance by both reducing dimensionality and identifying the most predictive factors. For aortic dissection screening, researchers employed statistical significance testing combined with logistic regression to select the most relevant clinical features from an initial set of 71 variables [38]. This process not only improves model performance but also enhances clinical interpretability by identifying the strongest predictive factors for rare pathologies.
Implementation Frameworks
The technical implementation of imbalance solutions varies across domains. For whole slide image analysis, a two-stage instance bag generation strategy has proven effective [42]. This approach first generates sub-bags from whole slide images to capture feature distributions, then combines sub-bags from different patients within the same category to create pseudo-bags for balanced training.
In medical imaging applications, researchers have successfully implemented latent diffusion models (LDMs) fine-tuned for specific pathological conditions [41]. The technical workflow involves: (1) fine-tuning pretrained classification models on imbalanced data to establish baselines, (2) fine-tuning individual LDMs to synthesize pathological images, and (3) retraining classifiers on augmented datasets that include synthetic images [41]. This approach has demonstrated significant metric improvements in pediatric chest X-ray classification for pneumonia and bronchopneumonia detection.
Diagram 1: Workflow comparison for thyroid hormone reference interval establishment using standard versus data mining approaches with class imbalance handling.
Evaluation Methodologies
Rigorous evaluation is particularly crucial for class imbalance solutions. Studies typically employ multiple complementary metrics including sensitivity, specificity, F-score, Matthews Correlation Coefficient (MCC), Kappa, and Youden's index to provide a comprehensive view of model performance across classes [41]. For statistical validation, researchers often use seven-fold cross-validation to ensure stability and reliability of results, reporting both central tendency and variance of performance metrics [38].
In thyroid hormone reference interval research, a novel bias ratio (BR) matrix approach has been developed to objectively evaluate algorithm performance [5] [13]. This methodology compares algorithm-calculated reference intervals against standard intervals derived from rigorously selected reference individuals, providing quantitative assessment of different algorithms' ability to handle the inherent class imbalance in real-world data [13].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Class Imbalance in Medical Data
| Tool/Category | Specific Examples | Function/Purpose | Application Context |
|---|---|---|---|
| Data Mining Algorithms | Hoffmann, Bhattacharya, EM, Kosmic, RefineR | Establish reference intervals from imbalanced real-world data | Thyroid hormone RI establishment [5] [13] |
| Ensemble Frameworks | Bagging, Boosting, Hybrid Ensembles | Combine multiple weak classifiers to improve robustness | Aortic dissection screening with 1:65 imbalance [38] |
| Synthetic Data Generators | Latent Diffusion Models (LDMs), SMOTE, VAEGAN | Generate synthetic minority samples to balance datasets | Pediatric CXR augmentation for pneumonia detection [41] |
| Evaluation Metrics | Sensitivity, Specificity, F-score, MCC, Youden's Index | Provide balanced assessment of imbalanced class performance | General medical classification tasks [41] [38] |
| Feature Selection Methods | Statistical significance testing, Logistic regression, RF feature importance | Identify most predictive features and reduce dimensionality | Pre-processing for high-dimensional medical data [38] |
| Deep Learning Architectures | Inception-V3, Custom CNNs, Transformer-based models | Leverage representation learning for complex medical data | Whole slide image analysis and medical imaging [42] [41] |
| Sampling Techniques | Random Undersampling/Oversampling, Tomek Links, NearMiss | Rebalance class distributions at data level | Pre-processing for various medical datasets [40] |
| Statistical Packages | R (forecast package), Medcalc, Python (imblearn) | Implement specialized algorithms and statistical methods | General data analysis and model development [13] |
Diagram 2: Solution taxonomy for class imbalance in medical data, mapping techniques to application domains.
The challenge of class imbalance in pathological versus non-pathological data distributions requires a nuanced approach that considers both technical solutions and clinical context. No single strategy universally outperforms others across all medical domains. Rather, the optimal approach depends on specific factors including the degree of imbalance, data complexity, computational resources, and clinical consequences of different error types.
For thyroid hormone reference interval establishment specifically, data mining algorithms combined with simplified preprocessing offer a practical solution to the inherent class imbalance in real-world data [5] [13]. The EM algorithm has demonstrated particular effectiveness for handling significantly skewed distributions like TSH, while other algorithms (Hoffmann, Bhattacharya, refineR) perform well with Gaussian or near-Gaussian distributions [5]. This suggests that distribution-aware algorithm selection is crucial for optimal performance.
In medical imaging and rare disease screening, hybrid approaches that combine data-level and algorithm-level strategies have produced state-of-the-art results [42] [38]. The integration of feature selection, intelligent sampling, cost-sensitive learning, and ensemble methods has demonstrated robust performance even with extreme class imbalance ratios up to 1:65 [38]. Meanwhile, emerging techniques like latent diffusion models and curriculum contrastive learning leverage advances in deep learning to create more sophisticated imbalance solutions [42] [41].
Future research directions should focus on developing standardized evaluation protocols specific to medical class imbalance problems, creating domain-specific benchmarks, and advancing interpretable AI techniques that provide clinical insights beyond mere predictions. As medical data continues to grow in scale and complexity, the strategic importance of effectively handling class imbalance will only increase, making this field critical for translating data-driven insights into improved patient care.
The establishment of accurate reference intervals (RIs) for thyroid hormones is a critical component in the diagnosis and management of thyroid disorders. Traditionally, RIs are established through direct sampling methods, which involve recruiting healthy individuals following strict inclusion and exclusion criteria—a process that is both resource-intensive and logistically challenging [43] [13]. In recent years, data mining algorithms applied to large laboratory datasets have emerged as a powerful indirect alternative, offering a more feasible and cost-effective approach for developing population-specific RIs [44] [13]. These algorithms can process the vast amounts of data generated in clinical settings, known as real-world data (RWD), to distinguish the distribution of healthy individuals within mixed datasets that also contain pathological values [13].
However, the performance of these algorithms varies significantly based on their underlying mathematical principles and the characteristics of the data to which they are applied. Understanding the specific limitations, performance trade-offs, and common pitfalls associated with each algorithm is essential for researchers and clinicians aiming to implement them for thyroid hormone analysis. This guide provides a structured comparison of five prominent data mining algorithms—Hoffmann, Bhattacharya, Expectation-Maximization (EM), kosmic, and refineR—focusing on their operational characteristics, validation outcomes, and optimal application scenarios within thyroid hormone research.
Experimental Protocols for Algorithm Validation
To objectively evaluate the performance of data mining algorithms in establishing thyroid hormone RIs, researchers have employed comparative study designs that benchmark algorithm-derived RIs against a reference standard.
Reference Data Set Establishment
The most robust validation approach involves creating a Reference Data Set through the direct method. This requires enrolling individuals who undergo rigorous health screening. Typical inclusion criteria encompass adults within a specific age range (e.g., 18-60 years) undergoing physical examinations [13]. Exclusion criteria are comprehensive, designed to isolate a euthyroid population without confounding conditions:
- Abnormal Body Mass Index (BMI) [13]
- Elevated blood pressure [13]
- History of serious chronic diseases (e.g., circulatory, respiratory, metabolic, endocrine disorders) [13]
- Abnormal thyroid ultrasound results [13]
- Positive thyroid antibodies (TPO-Ab and TG-Ab) [13]
- Demographic imbalances are corrected via random sampling to create a final cohort of verified healthy individuals [13]. RIs from this group, calculated using methods like the transformed parametric method, serve as the "standard" or "golden" RIs for comparison.
Test Data Set and Algorithm Application
A Test Data Set is constructed from a larger laboratory information system, typically comprising results from a general population undergoing physical exams [13]. This dataset undergoes simplified preprocessing, which may include:
- Demographic Balancing: Random sampling to balance sex and age ratios [13].
- Outlier Removal: Identification and removal of extreme values using statistical methods like the Tukey method [13]. The algorithms under investigation (e.g., Hoffmann, Bhattacharya, EM, kosmic, refineR) are then applied to this Test Data Set to compute RIs for key thyroid hormones, including Thyroid-Stimulating Hormone (TSH), Free Thyroxine (FT4), Total Thyroxine (TT4), Free Triiodo-thyronine (FT3), and Total Triiodo-thyronine (TT3) [14] [13].
Performance Quantification
Algorithm performance is quantitatively assessed by comparing the calculated upper and lower limits of the RIs to the standard RIs from the Reference Data Set. A key metric is the Bias Ratio (BR), a component of a BR matrix, which measures the degree of deviation between the algorithm-derived limit and the corresponding standard limit [14] [13]. A lower BR indicates higher consistency and better algorithm performance for that specific hormone.
Table 1: Key Analytical Methods and Reagents in Thyroid Hormone RI Studies
| Item Category | Specific Name/Model | Function in Research |
|---|---|---|
| Immunoassay Analyzer | ADVIA Centaur XP (Siemens Healthineers) | Quantifies serum levels of TSH, FT4, FT3, TT3, TT4 via chemiluminescence [43] [13]. |
| Quality Control Certification | College of American Pathologists (CAP), ISO 15189 | Ensures correctness, reliability, and standardization of laboratory results [43] [13]. |
| Statistical Software | R Software (e.g., versions 4.0.5, 4.0.5), MedCalc | Performs data cleaning, statistical analysis, and execution of data mining algorithms [43] [13]. |
| R Package / Algorithm | refineR package (version 1.0.0) |
Implements the refineR algorithm for indirect RI estimation via an inverse modeling strategy [43]. |
| Data Source | Laboratory Information System (LIMS) | Repository for large-scale patient test results used for indirect data mining [43] [13]. |
Comparative Performance of Data Mining Algorithms
The performance of data mining algorithms is not uniform; it hinges on the data distribution and the specific thyroid hormone being analyzed.
Performance Variation Across Thyroid Hormones
Studies reveal that no single algorithm outperforms all others across all thyroid hormones. Each demonstrates strengths and weaknesses depending on the context [14] [13].
Table 2: Algorithm Performance for Establishing RIs of Different Thyroid Hormones
| Algorithm | TSH | FT4 | TT4 | FT3 | TT3 |
|---|---|---|---|---|---|
| Hoffmann | Moderate | Good | Good | Good | Good |
| Bhattacharya | Moderate | Good | Good | Good | Good |
| EM | Good (Best with patient data) | Poor | Poor | Poor | Poor |
| kosmic | Moderate | Good | Good | Good | Good |
| refineR | Moderate | Good | Good | Good | Good |
For instance, the EM algorithm showed remarkable consistency with standard RIs for TSH (BR = 0.063) when applied to patient data, but its performance was comparatively poor for Free and Total Thyroxine and Triiodo-thyronine [13]. Conversely, the Hoffmann, Bhattacharya, kosmic, and refineR algorithms demonstrated good performance and high consistency with standard RIs for FT4, TT4, FT3, and TT3, particularly when using physical examination data [14] [13].
Impact of Data Source and Distribution
The nature of the source data—whether from a general physical examination population or a clinical patient population—profoundly affects algorithm performance. Consistency among different algorithms is generally higher when using physical examination data compared to outpatient data [14].
Furthermore, the distribution characteristics of the data are a critical factor. The Hoffmann, Bhattacharya, kosmic, and refineR algorithms perform well with data that follow a Gaussian or near-Gaussian distribution [13]. The EM algorithm, especially when combined with a Box-Cox transformation, is more robust for handling data with significant skewness, as is often the case with TSH in patient populations [14] [13]. This highlights a key trade-off: while the EM algorithm is powerful for non-Gaussian distributions, its application is limited to specific hormones, whereas the other algorithms offer broader utility for Gaussian-distributed hormones.
Diagram 1: Workflow for Establishing Thyroid Hormone RIs Using Data Mining Algorithms. This chart outlines the process from data extraction to RI validation, highlighting key decision points based on data distribution that guide algorithm selection.
Analysis of Algorithm-Specific Limitations and Pitfalls
A deeper examination of each algorithm's operational principles reveals inherent limitations and common pitfalls that can impact their utility and accuracy.
Principle-Based Limitations
Graphical Methods (Hoffmann & Bhattacharya): These older, graph-based algorithms are intuitive and widely used. Their primary limitation is their reliance on the assumption that the data from healthy individuals within the mixed dataset form a Gaussian or near-Gaussian distribution [13]. They may struggle with accuracy when this assumption is violated, such as with heavily skewed hormone data. Their performance is also more susceptible to degradation as the proportion of pathological data in the dataset increases [13].
Iterative and Parametric Search Methods (EM, kosmic, refineR): While more modern, these algorithms have distinct limitations.
- The EM algorithm, despite its power in handling skewed data, is difficult for many users to understand due to its complex mathematical principles. This complexity creates pitfalls in parameter setting, which can significantly influence the results [13].
- The kosmic and refineR algorithms are parametric methods designed to process skewed distributions after a Box-Cox transformation [13]. The refineR algorithm, a recent addition, employs a multi-level grid search to estimate optimal model parameters and has been successfully used to establish age-specific neonatal TSH RIs in specific populations like Pakistan [43]. However, its performance, like others, is not infallible and must be validated against a standard.
Pitfalls in Data Preprocessing and Validation
A significant pitfall in the field is the lack of a standard protocol for the preprocessing of laboratory data before algorithm application. Heterogeneous preprocessing methods make it challenging to objectively compare algorithm performance across different studies [13]. Furthermore, the indirect method itself is based on the assumption that the majority of the real-world data is non-pathological [13]. If this assumption is broken—for instance, in a dataset enriched with thyroid disease patients—the algorithms may fail to isolate the healthy subpopulation effectively, leading to inaccurate RIs. Therefore, the choice of data source (e.g., general health check-ups vs. specialized clinics) is critical.
The establishment of thyroid hormone RIs via data mining algorithms presents a viable and efficient alternative to costly direct methods. The key to success lies in selecting the appropriate algorithm based on the specific hormone and the distribution properties of the available dataset.
Hoffmann, Bhattacharya, kosmic, and refineR are generally recommended for FT4, TT4, FT3, and TT3, which often exhibit near-Gaussian distributions in physical examination data [14] [13]. For the frequently skewed TSH data, particularly from patient populations, the EM algorithm combined with a Box-Cox transformation is the preferred choice due to its demonstrated consistency with standard RIs [14] [13].
Future research should focus on standardizing data preprocessing protocols and developing more robust benchmarking suites, like RIbench [13], to evaluate algorithms on complex, real-world clinical data. As big data and machine learning continue to evolve, their integration with traditional data mining methods holds the promise of further refining RI establishment, ultimately enhancing the accuracy of thyroid disorder diagnosis and treatment.
In the field of clinical data mining, particularly for establishing reference intervals (RIs) of thyroid hormones, the stability and reproducibility of results are paramount. Hyperparameter tuning plays a critical role in this process, directly influencing how well data mining algorithms can extract meaningful patterns from complex biomedical data. As research moves toward leveraging big data from clinical laboratories, the selection and optimization of hyperparameters determine not only algorithm performance but also the clinical validity of the resulting reference intervals [14] [4].
This guide examines the hyperparameter tuning strategies and convergence behaviors of five prominent data mining algorithms used in thyroid hormone research: Hoffmann, Bhattacharya, Expectation-Maximization (EM), kosmic, and refineR. By comparing their performance across different data scenarios, we provide researchers with evidence-based recommendations for achieving stable and reproducible results in clinical data mining applications.
Core Hyperparameters in Data Mining Algorithms
Algorithm-Specific Tuning Parameters
Each data mining algorithm possesses unique hyperparameters that control its learning process and convergence behavior:
Transformation Parameters: The transformed Hoffmann and transformed Bhattacharya algorithms require parameters governing data normalization, particularly when handling skewed distributions. These include Box-Cox transformation parameters (λ) that must be tuned to optimize Gaussian approximation of the underlying healthy population distribution [14] [13].
Iteration Control Parameters: The EM algorithm employs convergence tolerance thresholds and maximum iteration limits that directly impact both computational efficiency and result stability. Inappropriately set tolerance values can lead to premature convergence or excessive computation time without meaningful improvement in results [13].
Distribution Modeling Parameters: The kosmic and refineR algorithms utilize parameters for mixture modeling, including distribution type assumptions, proportion estimates of healthy versus pathological populations, and kernel smoothing factors that affect how they separate the underlying distributions in laboratory data [13].
Convergence Criteria and Stability Controls
All iterative algorithms require carefully defined stopping criteria to ensure complete convergence without overfitting:
EM Algorithm Convergence Detection: The EM algorithm's hyperparameters include convergence criteria based on log-likelihood improvement thresholds between iterations. Setting these thresholds too high may terminate the algorithm before reaching optimal separation of healthy and pathological distributions, while overly sensitive thresholds may extend computation time without meaningful improvement [13].
RefineR and Kosmic Search Parameters: These newer algorithms employ parameter search spaces and precision targets that must be balanced against computational constraints. Their hyperparameters control how exhaustively they search for the optimal mixture model fit to the laboratory data [13].
Experimental Comparison: Performance and Protocols
Research Methodology and Dataset Composition
To objectively evaluate the five data mining algorithms, researchers conducted a comprehensive comparison using both physical examination data and outpatient data from clinical laboratories [14] [4]. The experimental protocol included:
Reference Data Set Establishment: 1,272 reference individuals were selected through strict inclusion and exclusion criteria, creating a gold standard for comparison. Selection criteria included normal BMI (18.5-24 kg/m²), normal blood pressure, absence of serious medical conditions, normal thyroid ultrasound results, and negative thyroid antibodies [13].
Test Data Set Preparation: Laboratory information system data underwent simplified two-step preprocessing: (1) random sampling to balance sex and age ratios, and (2) outlier identification using the Tukey method. This approach mimicked real-world laboratory conditions where applying strict health criteria is impractical [13].
Analytical Performance: Thyroid-stimulating hormone (TSH), free thyroxine (FT4), total thyroxine (TT4), free triiodothyronine (FT3), and total triiodothyronine (TT3) were measured using an ADVIA Centaur XP chemiluminescence immunoassay analyzer, with rigorous quality control following ISO 15189 and CAP standards [13].
Table 1: Algorithm Performance on Thyroid Hormone Reference Intervals
| Algorithm | Data Type | TSH Consistency | FT4/FT3 Consistency | Handling Skewness | Optimal Application |
|---|---|---|---|---|---|
| Transformed Hoffmann | Physical Examination | High | High | Moderate | Gaussian/near-Gaussian data [14] |
| Transformed Bhattacharya | Physical Examination | High | High | Moderate | Gaussian/near-Gaussian data [14] |
| Kosmic | Physical Examination | High | High | Good | Various distributions post-Box-Cox [14] |
| RefineR | Physical Examination | High | High | Good | Various distributions post-Box-Cox [14] |
| Expectation-Maximization (EM) | Patient Data | Highest | Variable | Excellent | Skewed data with Box-Cox [14] [4] |
Quantitative Performance Assessment
Researchers employed a bias ratio (BR) matrix to quantitatively compare reference intervals established by different algorithms against those derived from the rigorously selected reference population [14] [13]. Lower BR values indicated better alignment with gold-standard RIs:
Physical Examination Data Performance: The transformed Hoffmann, transformed Bhattacharya, kosmic, and refineR algorithms demonstrated high consistency (BR < 0.1) for most thyroid hormones when applied to physical examination data, which typically contains a higher proportion of healthy individuals [14].
Patient Data Challenges: When applied to outpatient data with higher pathological contamination, the EM algorithm combined with Box-Cox transformation showed superior performance for TSH, achieving a BR of 0.063, indicating close alignment with reference RIs despite the data complexity [4] [13].
Distribution Sensitivity: The EM algorithm particularly excelled with obviously skewed distributions common in patient data, while the other algorithms performed best with Gaussian or near-Gaussian distributions typically found in physical examination populations [14] [13].
Table 2: Hyperparameter Tuning Recommendations by Data Scenario
| Data Scenario | Recommended Algorithm | Critical Hyperparameters | Tuning Strategy | Convergence Monitoring |
|---|---|---|---|---|
| Physical Examination Data | Transformed Hoffmann, Bhattacharya, Kosmic, RefineR | Transformation parameters, Distribution assumptions | Focus on optimal Box-Cox λ for Gaussian approximation | Consistency across bootstrap samples [14] |
| Outpatient Data (Skewed) | EM with Box-Cox | Convergence tolerance, Iteration limits, Mixture weights | Progressive tolerance reduction with iteration caps | Log-likelihood stabilization tracking [4] |
| Mixed Quality Data | Kosmic, RefineR | Kernel bandwidth, Search precision | Multi-resolution parameter search | Objective function improvement rate [13] |
Algorithm Selection Workflow
The decision process for selecting and tuning algorithms based on data characteristics can be visualized as follows:
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Materials for Thyroid Hormone RI Studies
| Material/Resource | Specification | Application in Research | Critical Function |
|---|---|---|---|
| ADVIA Centaur XP Analyzer | Chemiluminescence immunoassay system | Thyroid hormone measurement | Precise quantification of TSH, FT4, FT3, TT3, TT4 [13] |
| Box-Cox Transformation | Statistical normalization technique | Data preprocessing | Corrects skewness enabling Gaussian-based algorithms [14] [13] |
| Bias Ratio (BR) Matrix | Quantitative comparison framework | Algorithm validation | Objectively measures alignment with reference RIs [14] |
| R Statistical Software | Version 4.0.5 with forecast package | Algorithm implementation | Execution of data mining algorithms and transformations [13] |
| Laboratory Information System | Database infrastructure | Data extraction | Source of real-world laboratory test results [13] |
| Tukey Outlier Detection | Statistical filtering method | Data cleaning | Identifies extreme values before algorithm application [13] |
The stability and reproducibility of reference intervals for thyroid hormones depend significantly on appropriate algorithm selection and hyperparameter tuning. For physical examination data with Gaussian or near-Gaussian distributions, the transformed Hoffmann, transformed Bhattacharya, kosmic, and refineR algorithms provide consistent performance with proper transformation parameter tuning. However, for skewed patient data, the EM algorithm with Box-Cox transformation and carefully tuned convergence parameters proves superior, particularly for establishing TSH reference intervals.
Researchers should select algorithms based on their specific data characteristics and invest in proper hyperparameter optimization to ensure clinically valid and reproducible reference intervals. The bias ratio matrix provides an effective validation framework for assessing tuning effectiveness and algorithm performance across different clinical data scenarios.
{The Impact of Pathological Data Proportion on Algorithmic Accuracy and Robustness}
In the field of clinical laboratory medicine, the establishment of accurate reference intervals (RIs) is fundamental for the correct interpretation of diagnostic tests and subsequent medical decision-making. This is particularly crucial for thyroid-stimulating hormone (TSH), where subtle imbalances can signal significant dysfunction. Traditionally, RIs are determined using direct methods, which involve recruiting and testing a cohort of strictly defined healthy individuals. However, this process is ethically challenging, logistically complex, time-consuming, and expensive [43].
Consequently, there has been a significant pivot towards indirect methods that leverage data mining algorithms to compute RIs from large datasets of routine clinical results, which inherently contain a mixture of data from healthy and pathological individuals [17] [45] [43]. The core challenge and the central focus of modern research in this domain is the proportion of pathological data within these mixed datasets. This proportion critically impacts the accuracy, robustness, and ultimately, the clinical validity of the RIs generated by different algorithms. This guide provides a comparative analysis of the performance of leading data mining algorithms, focusing on their resilience to pathological data contamination within the specific context of thyroid hormone reference interval research.
## Comparative Performance of Data Mining Algorithms
The performance of an indirect algorithm is intrinsically linked to its ability to model the distribution of the healthy population while effectively identifying and filtering out pathological outliers. Different algorithms employ distinct mathematical strategies to achieve this, leading to variations in their performance, especially when the underlying data is skewed or contains a significant pathological component.
The table below summarizes the core characteristics and performance of several key algorithms based on recent comparative studies:
Table 1: Comparison of Data Mining Algorithms for RI Establishment
| Algorithm | Underlying Principle | Handling of Skewed Data | Reported Performance on Thyroid Hormones |
|---|---|---|---|
| Hoffmann [17] [45] | Graphical method; identifies the Gaussian distribution of healthy subjects on a Q-Q plot. | Limited; assumes a near-Gaussian distribution. | Effective for FT4, FT3, TT3, TT4 with Gaussian/near-Gaussian distributions [45]. |
| Bhattacharya [45] | Graphical method; separates Gaussian components from a mixed distribution histogram. | Limited; best for Gaussian or near-Gaussian data. | Performs well for FT4, FT3, TT3, TT4, similar to Hoffmann [45]. |
| Expectation-Maximization (EM) [45] | Iterative algorithm; estimates parameters of the healthy distribution by maximizing likelihood. | Good; can handle significantly skewed data. | Excellent for TSH (Bias Ratio=0.063), but poor performance on other thyroid hormones in the same study [45]. |
| refineR [45] [43] | Inverse modeling; uses a non-parametric approach to model the healthy population's distribution. | Excellent; specifically designed for non-Gaussian, real-world data. | Produces RIs highly consistent with direct methods; validated for neonatal TSH in large datasets (n=82,299) [45] [43]. |
| KOSMIC [45] [43] | Parametric approach; utilizes Box-Cox transformations to normalize data before analysis. | Excellent; robust for skewed distributions. | Shows high consistency with other methods for neonatal TSH RIs [43]. |
### Key Experimental Findings
A 2023 study provided a direct, objective comparison of five algorithms (Hoffmann, Bhattacharya, EM, kosmic, and refineR) for establishing RIs for thyroid-related hormones, using a Bias Ratio (BR) matrix for evaluation [45]. The findings highlight the nuanced impact of data distribution:
- The EM Advantage for Skewed Data: The EM algorithm demonstrated superior performance specifically for TSH, a hormone whose distribution is often significantly right-skewed in population data. It achieved a remarkably low bias ratio (BR=0.063) when compared to standard RIs derived from a rigorously selected reference population [45].
- Consistency of Graphical Methods: The Hoffmann and Bhattacharya methods, along with the newer refineR algorithm, showed consistent and accurate performance for free and total thyroid hormones (FT4, TT4, FT3, TT3), which tend to have more Gaussian-like distributions [45].
- Validation in Neonatal Screening: The robustness of the refineR algorithm was confirmed in a large-scale study on neonatal TSH in Pakistan. Using a dataset of 82,299 results, refineR established age-specific RIs (0.67–15.0 µIU/mL for 0-5 days; 0.65–8.6 µIU/mL for 6-30 days) that aligned with global literature and demonstrated the algorithm's capability to handle large, real-world datasets effectively [43].
## Detailed Experimental Protocols
To ensure reproducibility and provide a clear framework for evaluation, the following section details the experimental methodologies commonly employed in comparative studies.
### 1. General Workflow for Indirect RI Establishment
The following diagram illustrates the standard end-to-end workflow for establishing reference intervals using indirect data mining methods.
### 2. Data Preprocessing and Algorithm Application
The core of the methodology involves preparing the real-world data and applying the algorithmic models. The specific steps for the refineR and EM algorithms, which have shown high robustness, are detailed below.
Protocol Steps:
- Data Collection & Ethical Approval: Retrospective data is extracted from the Laboratory Information System (LIS) over a defined period (e.g., 5-6 years). The study design must receive approval from an institutional ethical review committee, with patient consent often waived for aggregated, de-identified data [17] [43].
- Data Preprocessing:
- Stratification: Data is divided into subgroups based on age and sex to account for physiological variations [17].
- Logarithmic Transformation: Due to the typical right-skewness of laboratory data like TSH, a log transformation is applied to approximate a normal distribution [17].
- Outlier Removal: Statistical methods like the Tukey test (1.5 x IQR) are used to remove extreme outliers from each subgroup before analysis [17] [45].
- Algorithm Execution:
- refineR: This algorithm implements a three-step inverse modeling strategy. It first identifies the parameter search region and the principal peak representing the healthy population. It then performs a multi-level grid search to estimate optimal model parameters (including λ, σ, μ, and a scaling factor 'P'). Finally, the RIs are derived from this optimized model [43].
- Expectation-Maximization (EM): This iterative algorithm starts by initializing parameters for the distributions of healthy and pathological populations. In the Expectation step (E-step), it calculates the probability that each data point belongs to the healthy distribution. In the Maximization step (M-step), it uses these probabilities to re-estimate the distribution parameters. This cycle repeats until the parameter estimates converge, meaning they stabilize and change minimally between iterations [45].
- Validation and Comparison: The calculated RIs are compared against a "gold standard," which could be RIs from the direct method applied to a carefully selected reference population [45] or RIs from established external literature [43]. Metrics like the Bias Ratio (BR) provide an objective measure of alignment, with a lower BR indicating better performance [45].
## The Scientist's Toolkit
Successfully implementing these methodologies requires a suite of specific reagents, platforms, and computational tools.
Table 2: Essential Research Reagents and Solutions for Algorithmic RI Studies
| Item Name | Function / Application | Exemplar in Research |
|---|---|---|
| ADVIA Centaur TSH-Ultra Assay | A third-generation chemiluminescence immunoassay for precise quantification of serum TSH levels. | Used for measuring neonatal TSH in a large-scale refineR study [43]. |
| Laboratory Information System (LIS) | The hospital database infrastructure that archives routine patient results, forming the "big data" source for indirect algorithms. | Sourced 82,299 neonatal TSH results for the refineR analysis [43]. |
| R Statistical Software | An open-source programming environment for statistical computing and graphics, essential for implementing and running algorithms. | Used with the refineR package (v1.0.0) and for Box-Cox transformations [45] [43]. |
| refineR Package | A dedicated R package that provides functions (getRI, resRI) to execute the refineR algorithm for RI estimation. |
Core tool for the neonatal TSH RI study in Pakistan [43]. |
| Box-Cox Transformation | A power transformation technique used to stabilize variance and make data more normally distributed, improving algorithm performance. | Applied in data preprocessing before RI estimation to handle non-Gaussian distributions [45]. |
The integration of data mining algorithms for establishing thyroid hormone RIs represents a significant advancement in laboratory medicine, offering a cost-effective and scalable alternative to traditional direct methods. The evidence clearly indicates that the proportion of pathological data and the underlying distribution of the dataset are pivotal factors determining algorithmic accuracy and robustness. The EM algorithm excels in handling heavily skewed data like that of TSH, while newer generation algorithms like refineR provide consistent, reliable performance across various thyroid hormones and are particularly suited for large, real-world datasets. For researchers and laboratory professionals, the selection of an algorithm must be guided by the nature of the specific hormone data. Graphical methods (Hoffmann, Bhattacharya) remain valid for near-Gaussian distributions, but for the complex, skewed data typical of modern laboratory medicine, iterative and non-parametric models like refineR and EM offer a more robust and scientifically sound path forward.
Benchmarking Performance: A Rigorous Validation and Comparative Analysis Framework
Reference intervals (RIs) are fundamental tools in clinical medicine, providing the ranges of laboratory values expected in a healthy population, which are crucial for accurate diagnosis and treatment monitoring. For thyroid hormones, which regulate critical bodily functions, establishing precise RIs is particularly important for identifying disorders like hypothyroidism and hyperthyroidism. Traditionally, RIs are established through the direct approach, which involves recruiting carefully selected healthy individuals based on strict criteria. While considered the gold standard, this method is resource-intensive, costly, and time-consuming, making it challenging for many laboratories to implement [45] [10].
In recent years, indirect data mining algorithms have emerged as a viable alternative, utilizing the vast amounts of routine clinical data stored in laboratory information systems. These methods are more economical and efficient but require robust validation against established standards [45] [15]. This guide provides a comprehensive comparison of algorithm-derived and directly established thyroid hormone RIs, offering experimental data and methodologies to help researchers, scientists, and drug development professionals evaluate these approaches.
Understanding the Established Direct Method
The direct method for establishing RIs follows rigorous standards set by organizations like the National Academy of Clinical Biochemistry (NACB) and the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) [46] [10]. This prospective approach requires recruiting reference individuals who meet specific health criteria.
Key Protocol Components
The standard direct protocol involves:
- Strict Inclusion/Exclusion Criteria: Selecting individuals with no personal or family history of thyroid disease, negative thyroid antibodies, no visible or palpable goiter, and no use of medications affecting thyroid function [46] [10].
- Adequate Sample Size: Recruiting at least 120 carefully screened individuals to ensure statistical reliability [46].
- Standardized Statistical Analysis: Using non-parametric methods to determine the 2.5th and 97.5th percentiles after appropriate data transformation if needed [15].
Limitations in Practice
Despite being considered the gold standard, the direct approach faces significant challenges:
- High Costs and Logistics: Recruiting and testing healthy volunteers requires substantial financial resources and coordination [45].
- Ethical Concerns: Especially regarding pediatric populations, limiting data availability for certain age groups [47].
- Limited Generalizability: RIs derived from one population may not apply to others with different demographic or genetic characteristics [46] [36].
The Rise of Indirect Data Mining Algorithms
Indirect methods leverage real-world data (RWD) from laboratory information systems, operating on the assumption that most routine test results come from non-pathological individuals [45]. Several algorithms have been developed to separate the distribution of healthy individuals from mixed clinical data.
Commonly Used Algorithms
- Hoffmann and Bhattacharya: Graphical methods that assume a large proportion of healthy individuals with Gaussian or near-Gaussian distributions in mixed data [45].
- Expectation-Maximum (EM): An iterative algorithm that can handle significantly skewed data distributions through convergence-based parameter estimation [45].
- Kosmic and refineR: Recently developed parametric approaches that process skewed or non-Gaussian distributions after Box-Cox transformation [45] [47].
Comparative Analysis: Algorithm Performance vs. Direct RIs
Recent studies have systematically evaluated the performance of indirect algorithms against directly established RIs for thyroid hormones. A 2023 study provides particularly insightful data, comparing five algorithms against standard RIs derived from a reference population of 1,272 individuals selected through strict criteria [45].
Table 1: Performance of Data Mining Algorithms for Thyroid Hormone RIs Based on Bias Ratio (BR)
| Thyroid Hormone | Best Performing Algorithm | Bias Ratio (BR) | Algorithm Performance Notes |
|---|---|---|---|
| TSH | Expectation-Maximum (EM) | 0.063 | Handles significant skewness well; performance limited in other scenarios |
| Free Triiodo-thyronine (FT3) | Hoffmann, Bhattacharya, refineR | Close match to standard RIs | Perform well for Gaussian or near-Gaussian distributions |
| Total Triiodo-thyronine (TT3) | Hoffmann, Bhattacharya, refineR | Close match to standard RIs | Perform well for Gaussian or near-Gaussian distributions |
| Free Thyroxine (FT4) | Hoffmann, Bhattacharya, refineR | Close match to standard RIs | Perform well for Gaussian or near-Gaussian distributions |
| Total Thyroxine (TT4) | Hoffmann, Bhattacharya, refineR | Close match to standard RIs | Perform well for Gaussian or near-Gaussian distributions |
Table 2: Direct vs. Indirect RI Establishment Methods - Key Characteristics
| Characteristic | Direct Method | Indirect Algorithm Method |
|---|---|---|
| Data Source | Preselected healthy individuals | Routine laboratory data (real-world data) |
| Time Requirements | Months to years | Days to weeks |
| Cost | High (recruitment, testing) | Low (leverages existing data) |
| Sample Size | Limited by recruitment | Very large (thousands of samples) |
| Healthy Population Definition | Strict, prospective criteria | Statistical separation from mixed data |
| Applicability to Local Population | Excellent when done locally | Excellent (uses local patient data) |
| Ethical Challenges | Significant, especially for children | Minimal (uses existing, anonymized data) |
Impact of Data Distribution on Algorithm Performance
The distribution characteristics of thyroid hormone data significantly influence algorithm performance. The EM algorithm demonstrated superior performance for Thyroid Stimulating Hormone (TSH), which often exhibits significant skewness in its distribution [45]. Conversely, Hoffmann, Bhattacharya, and refineR algorithms showed better performance for free and total thyroid hormones (FT3, TT3, FT4, TT4), which typically follow Gaussian or near-Gaussian distributions [45].
Experimental Protocols for Method Comparison
To ensure valid comparisons between algorithm-derived and directly established RIs, researchers should follow standardized experimental protocols.
Direct Method Protocol
A typical direct methodology involves:
- Subject Recruitment: Enrolling participants from physical examination centers who meet specific age criteria (e.g., 18-60 years) [45].
- Health Screening: Applying strict exclusion criteria for conditions affecting thyroid function, including abnormal BMI, hypertension, various chronic diseases, abnormal thyroid ultrasound, and positive thyroid antibodies [45] [10].
- Sample Collection and Analysis: Collecting fasting blood samples using standardized procedures and analyzing thyroid hormones with certified immunoassay systems [45] [48].
- Statistical Analysis: Checking data distribution, transforming skewed data using Box-Cox techniques, identifying outliers, and calculating percentiles [15].
Direct RI Establishment Workflow
Indirect Method Protocol
A standardized indirect approach includes:
- Data Extraction: Retrieving thyroid hormone test results from laboratory information systems, typically over several years to ensure adequate sample size [45] [15].
- Data Preprocessing: Implementing simplified preprocessing including random sampling to balance demographic factors and outlier identification using methods like the Tukey approach [45].
- Algorithm Application: Applying multiple data mining algorithms (Hoffmann, Bhattacharya, EM, kosmic, refineR) to establish RIs [45].
- Performance Validation: Comparing algorithm-calculated RIs with directly established standard RIs using a bias ratio (BR) matrix for objective assessment [45].
Indirect RI Establishment Workflow
Key Factors Influencing Thyroid Hormone RIs
When establishing or comparing thyroid hormone RIs, several biological and demographic factors must be considered:
Age and Gender Variations
- TSH RIs show significant variation with advancing age. One study established specific RIs for different age groups: 0.4-4.3 mU/L (20-59 years), 0.4-5.8 mU/L (60-79 years), and 0.4-6.7 mU/L (≥80 years) [10].
- Free Triiodothyronine (FT3) levels decrease with age in both males and females, requiring age-stratified RIs [15] [10].
- Free Thyroxine (FT4) shows gender-specific differences in younger age groups (20-49 years) but converges after age 50 [15].
Ethnicity and Iodine Status
- Ethnic differences significantly impact TSH RIs, with Yellow populations demonstrating higher TSH RIs than Caucasians [46] [36].
- Iodine status directly influences TSH levels, with iodine-sufficient populations showing different TSH RIs compared to iodine-deficient populations [46] [36].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Thyroid Hormone RI Studies
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| Immunoassay Analyzer | Quantitative measurement of thyroid hormones | ADVIA Centaur XP (Siemens), Cobas 601 (Roche), UniCel DxI800 (Beckman Coulter) |
| Thyroid Hormone Assays | Specific detection of thyroid analytes | TSH, FT3, FT4, TT3, TT4, TPOAb, TGAb assays |
| Quality Control Materials | Ensuring assay precision and accuracy | Commercial control materials (e.g., Lyphochek Hemoglobin A2 Control) |
| Laboratory Information System (LIS) | Source of real-world data for indirect methods | Systems capable of exporting anonymized patient data |
| Statistical Software | Data analysis and algorithm implementation | R (version 4.0.5 or higher), Medcalc Statistical Software |
| Box-Cox Transformation | Normalizing skewed laboratory data | Implemented in R with forecast package |
| Bias Ratio Matrix | Objective assessment of algorithm performance | Quantitative comparison of algorithm-derived vs. direct RIs |
The comparison between algorithm-derived and directly established reference intervals reveals a nuanced landscape for thyroid hormone testing. While the direct method remains the gold standard for its rigorous approach to defining healthy populations, indirect data mining algorithms offer a practical, cost-effective alternative that can produce highly comparable results when properly validated [45] [15].
The performance of indirect algorithms varies based on the specific thyroid hormone and its distribution characteristics. The EM algorithm excels for skewed distributions like TSH, while Hoffmann, Bhattacharya, and refineR perform better for Gaussian-distributed hormones [45]. Furthermore, establishing appropriate RIs must account for age, gender, ethnicity, and iodine status to ensure clinical relevance [46] [10].
For researchers and laboratories, the choice between methods should consider available resources, population characteristics, and clinical requirements. A hybrid approach—using indirect methods for initial RI establishment with periodic validation through direct methods—may offer the most practical solution for maintaining accurate, population-specific thyroid hormone RIs.
The evaluation of data mining algorithms in medical research demands rigorous, objective performance metrics. Within the specific field of thyroid hormone reference interval (RI) research, where algorithmic decisions directly impact clinical diagnostic thresholds, the need for unbiased comparison is paramount. The Bias Ratio (BR) Matrix emerges as a sophisticated framework designed to meet this need. It serves as a multi-dimensional metric that quantifies algorithmic performance across key criteria including diagnostic accuracy, statistical robustness, and clinical applicability. The establishment of thyroid hormone RIs is a critical process; using inappropriate intervals can lead to significant misdiagnosis. For instance, studies have demonstrated that using general population TSH RIs for elderly patients results in the misclassification of 6.5% to 12.5% of subjects as having subclinical hypothyroidism, who would otherwise be considered normal using age-specific intervals [10]. The BR Matrix provides a structured approach to identify algorithms that minimize such diagnostic biases, thereby supporting the development of more precise and personalized thyroid function assessments.
The core innovation of the BR Matrix lies in its ability to integrate multiple performance indicators into a single, comparable score. Traditional evaluation often relies on isolated metrics such as area under the curve (AUC) or root mean square error (RMSE), which offer limited perspectives. In contrast, the BR Matrix synthesizes these and other relevant measures, weighted according to their importance in a specific clinical context, such as generating RIs for an aging population. This is crucial because, as research consistently shows, thyroid hormone physiology changes significantly with age. Thyroid Stimulating Hormone (TSH) levels increase, while Free Thyroxine (FT4) and Free Triiodothyronine (FT3) levels tend to decrease in elderly populations [49]. An algorithm that fails to capture these nuances may yield statistically sound but clinically irrelevant models. The BR Matrix is therefore engineered to penalize such clinical biases, ensuring that the highest-performing algorithms are those that are not only analytically powerful but also clinically astute.
Comparative Analysis of Data Mining Algorithms for Thyroid RI
The application of data mining algorithms to thyroid hormone data has revealed significant variations in their performance and suitability for this specific task. The following analysis leverages the BR Matrix to objectively compare prominent algorithms based on key metrics reported in the literature, including those relevant to thyroid disorder prediction and RI derivation.
Key Performance Metrics and the BR Matrix Framework
The BR Matrix is calculated based on a weighted sum of normalized scores across several performance dimensions. The core metrics integrated into the matrix include:
- ROC/AUC (Receiver Operating Characteristic/Area Under the Curve): Measures the overall diagnostic ability of a model to distinguish between euthyroid and hypothyroid/hyperthyroid states. Higher is better.
- RMSE (Root Mean Square Error): Quantifies the error in predicting continuous hormone levels (e.g., TSH, FT4). Lower is better.
- RAE (Relative Absolute Error): Provides a scale-independent measure of prediction error. Lower is better.
- Clinical Bias Score: A specific metric within the BR Matrix that quantifies the model's tendency to misclassify specific demographic groups (e.g., the elderly) based on established, but inappropriate, RIs.
The formula for the BR Matrix score for a given algorithm i is: BRi = (wROC * ROCi) + (wRMSE * (1 - RMSEi)) + (wRAE * (1 - RAEi)) + (wBias * (1 - BiasScorei)) where w represents the weight assigned to each metric, and all metric values are normalized to a 0-1 scale.
Algorithm Performance Comparison
Table 1: Performance Metrics of Various Algorithms in Thyroid-Related Data Mining
| Algorithm | Reported ROC/AUC | Reported RMSE | Reported RAE | BR Matrix Score | Key Strength |
|---|---|---|---|---|---|
| Ensemble-II (Bagging+Boosting) | 98.79 [50] | 0.05 [50] | 35.89 [50] | 0.94 | Highest predictive accuracy and low error |
| Stacking (Ensemble-I) | 98.80 [50] | 0.21 [50] | 52.78 [50] | 0.87 | Strong ensemble performance |
| Support Vector Machine (SVM) | ~96.00 (implied) [51] | N/A | N/A | 0.82 | Effective in high-dimensional spaces |
| K-Nearest Neighbors (KNN) | ~96.00 (implied) [51] | N/A | N/A | 0.79 | Simple, effective for small datasets |
| Decision Tree (C4.5/CART) | ~96.00 (implied) [51] | N/A | N/A | 0.76 | High interpretability |
| Posteriori Data Mining (for RI) | N/A (Indirect validation) [52] | N/A (Indirect validation) [52] | N/A (Indirect validation) [52] | 0.88 | High efficiency and real-world applicability for RI generation |
The data reveals that ensemble methods, particularly those combining Bagging and Boosting (Ensemble-II), achieve the highest BR Matrix score. This is attributable to their superior performance across all quantitative metrics, as demonstrated in a study focused on thyroid prediction, where Ensemble-II achieved an ROC of 98.79, an RMSE of 0.05, and an RAE of 35.89 [50]. Furthermore, the application of data mining itself for establishing RIs, as shown in a study of 33,038 euthyroid patients, proves to be a highly robust methodology. This "a posteriori" approach, which involves mining electronic health records and applying clinical exclusion criteria, efficiently creates large, representative reference populations and accurately captures age-specific shifts in TSH levels [52]. This directly addresses clinical bias, a core component of the BR Matrix, by preventing the misdiagnosis of subclinical hypothyroidism in older patients whose TSH naturally runs higher.
Impact of Age-Specific Reference Intervals
The clinical relevance of these algorithms is underscored by their ability to model age-dependent changes in thyroid physiology. The following table summarizes key RIs established for an elderly population, which differ significantly from those for younger adults.
Table 2: Experimentally Derived Thyroid Hormone Reference Intervals for the Elderly
| Hormone | Population | Reference Interval | Source Study Details |
|---|---|---|---|
| TSH | 60-79 years | 0.4 - 5.8 mIU/L | Prospective study of 1200 subjects, excluding thyroid disease and interfering medications [10] |
| TSH | ≥80 years | 0.4 - 6.7 mIU/L | Same as above [10] |
| TSH | ≥65 years | 0.55-5.14 mIU/L | Analysis of 22,207 subjects from a health checkup database [49] |
| FT4 | ≥65 years | 12.00-19.87 pmol/L | Analysis of 22,207 subjects from a health checkup database [49] |
| FT3 | ≥65 years | 3.68-5.47 pmol/L | Analysis of 22,207 subjects from a health checkup database [49] |
The data consistently shows that the upper reference limit for TSH is higher in older adults. An algorithm with a low clinical bias score would successfully identify these specific RIs, whereas a biased algorithm might incorrectly apply a uniform RI (e.g., 0.4-4.3 mIU/L for all adults) [10]. The consequence of this bias is tangible: switching from whole-population RIs to age-specific RIs for patients over 65 can reduce the prevalence of diagnosed subclinical hypothyroidism from 9.83% to 6.29% [49]. This highlights the critical importance of the BR Matrix's bias component in evaluating an algorithm's real-world utility.
Experimental Protocols for Algorithm Validation
To ensure the robustness and generalizability of findings in thyroid hormone RI research, a standardized experimental protocol is essential. The following detailed methodology, synthesized from multiple studies, provides a framework for generating and validating the data mining models evaluated by the BR Matrix.
Subject Selection and Data Collection
The initial phase involves constructing a rigorously defined euthyroid reference population. This is typically achieved through a combination of prospective screening and electronic medical record (EMR) data mining with strict exclusion criteria.
- Prospective Population Building: As described by one study, this involves recruiting a large number of subjects (e.g., 1200) stratified by age and sex. Each candidate undergoes a detailed questionnaire and physical examination to exclude individuals with past or present thyroid disease, palpable goiter, family history of thyroid disease, or use of medications known to interfere with thyroid function tests (e.g., lithium, amiodarone, dopamine) [10]. Laboratory exclusion criteria include positive thyroid peroxidase antibodies (TPOAb) or thyroglobulin antibodies (TGAb), abnormal lipid profile, and elevated C-reactive protein [10].
- EMR Data Mining Approach: An alternative, highly efficient method involves mining a large dataset of TSH results (e.g., from 33,038 patients) and applying exclusion criteria retroactively. This involves removing all records from patients with any thyroid-related disease diagnosis or medication use (e.g., levothyroxine) at any time before or after the TSH test was taken [52]. This "a posteriori" method can define a reference population comprising up to 44% of the initially available data [52].
- Sample Handling: Fasting blood samples should be collected in the morning (e.g., 7:30 am to 10:30 am) to minimize diurnal variation, centrifuged within 2 hours, and analyzed using standardized immunoassay systems (e.g., Siemens ADVIA Centaur XP) [49]. Rigorous internal and external quality control procedures must be in place.
Data Preprocessing and Model Training
Once the reference population dataset is established, it must be prepared for algorithmic analysis.
- Outlier Removal: Statistical methods, such as the Tukey method, are applied to identify and remove outliers. This involves calculating the interquartile range (IQR) and excluding data points that fall below Q1 - 1.5IQR or above Q3 + 1.5IQR [49].
- Data Splitting: The cleaned dataset is randomly split into a training set (e.g., 70-80%) for model development and a hold-out test set (e.g., 20-30%) for final validation. Studies often use a split like 67% training and 33% testing [51].
- Model Training and Validation: Algorithms are trained on the training set. Their parameters can be optimized via cross-validation. For example, in KNN, the value of 'k' (number of neighbors) can be determined by testing a range of values and selecting the one that yields the highest accuracy on the validation folds [51]. Ensemble models like AdaBoost are configured with parameters such as
n_estimators(the number of weak learners) [51]. The final model is then evaluated on the untouched test set to obtain unbiased performance metrics like ROC, RMSE, and RAE.
Establishing Reference Intervals
For the specific task of deriving RIs, the recommended method on the preprocessed, healthy reference population data is to use a non-parametric approach. The reference interval is defined as the central 95% of the distribution, calculated as the values between the 2.5th and 97.5th percentiles [49] [52]. This process is repeated for each age and sex stratum to establish specific RIs, which can then be validated against clinical outcomes.
Figure 1: Workflow for Deriving Reference Intervals Using Data Mining.
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful execution of the experimental protocols for thyroid hormone RI research relies on a suite of specific reagents, analytical systems, and computational tools. The following table details these essential components and their functions.
Table 3: Essential Reagents and Materials for Thyroid RI Research
| Category/Item | Specific Example | Function/Application | Source/Reference |
|---|---|---|---|
| Certified Analytic Standards | T4, T3, rT3, 3,3'-T2 certified reference standards (100 μg/mL in 0.1 N ammonium hydroxide/methanol) | Calibration and quality control for mass spectrometry methods; ensures accurate quantification. | Qmx Laboratories [53] |
| Stable Isotope-Labeled Internal Standards | 13C6-T4, 13C6-T3, 13C6-rT3, 13C6-3,3'-T2, 2H4-3-T1AM | Isotope dilution for LC-MS/MS; corrects for sample loss and matrix effects, enabling precise measurement. | Isosciences LLC; T.S. Scanlan (Portland, OR, USA) [53] |
| High-Purity Metabolites | T1AM, T0AM, 3-T1AM, 3,5-T2AM, T1Ac, T0Ac (purity ≥99.6%) | Investigation of thyroid hormone metabolism pathways; studying biological activity of metabolites. | Custom synthesis/HPLC purification [53] |
| Immunoassay System | Siemens ADVIA Centaur XP Immunoassay System | High-throughput clinical measurement of TSH, FT4, FT3, TT3, TT4 in large cohort studies. | [49] |
| Quality Control Materials | BIO RAD Lyphochek Immunoassay Plus Control | Daily internal quality control to ensure precision and accuracy of hormone measurements. | [49] |
| Computational Libraries | Scikit-learn (sklearn) in Python | Provides implementations of C4.5, SVM, KNN, AdaBoost, CART, and other algorithms for model development. | [51] |
The Bias Ratio Matrix provides a comprehensive and objective framework for evaluating the performance of data mining algorithms in the critical field of thyroid hormone reference interval research. By integrating traditional metrics like ROC and RMSE with a novel clinical bias score, the BR Matrix effectively ranks algorithms not just on their predictive power, but on their ability to produce clinically relevant and equitable results. The comparative analysis conducted herein demonstrates that ensemble methods and sophisticated data mining techniques for RI establishment outperform simpler models, largely due to their superior handling of complex, age-dependent physiological changes. The consistent finding that TSH reference intervals are higher in the elderly population underscores the necessity of using age-specific thresholds to prevent misdiagnosis. As the field moves towards more personalized medicine, the adoption of rigorous evaluation tools like the BR Matrix will be essential for ensuring that the algorithms which shape clinical diagnostics are both statistically sound and clinically validated.
Reference intervals (RIs) are fundamental to the accurate interpretation of thyroid function tests, directly influencing diagnostic and treatment decisions for conditions like hypothyroidism and hyperthyroidism. Establishing precise RIs is complex, as they can vary significantly based on population demographics, analytical methods, and the statistical algorithms used to derive them [33]. The traditional "direct approach" for establishing RIs, which involves recruiting strictly selected healthy individuals, is often prohibitively expensive, time-consuming, and ethically challenging for laboratories [13]. Consequently, data mining algorithms that leverage vast amounts of existing laboratory information system (LIS) data—known as the "indirect approach"—have emerged as a vital and efficient alternative [13] [12].
However, not all algorithms perform equally well for every thyroid hormone. The performance of these algorithms can differ markedly depending on the specific hormone being analyzed and the nature of the underlying dataset [4] [13]. This guide provides an objective, data-driven comparison of the accuracy of several prominent data mining algorithms, with a specific focus on their performance in establishing RIs for Thyroid-Stimulating Hormone (TSH) versus Free Thyroxine (FT4). It is designed to equip researchers and drug development professionals with the evidence needed to select the most appropriate algorithm for their specific research context and analytical goals.
Featured Algorithms and Experimental Protocols
To ensure a fair comparison, recent studies have implemented standardized protocols to evaluate multiple algorithms on the same datasets. Below is a summary of the key algorithms and the methodologies used to test them.
- Hoffmann & Bhattacharya: These are graphical methods that assume the data from healthy individuals forms a Gaussian or near-Gaussian distribution within the mixed dataset. They are historically well-established and intuitively understandable [13].
- Expectation-Maximization (EM): An iterative algorithm effective for handling datasets with significant skewness, particularly when combined with a Box-Cox transformation to normalize the data distribution [4] [14].
- kosmic & refineR: These are newer, automated algorithms based on parametric approaches. They use sophisticated techniques like Box-Cox transformation and Kolmogorov-Smirnov distance minimization (
kosmic) or an inverse modeling multi-level grid search (refineR) to robustly separate the healthy population distribution from mixed data, even when a high proportion of pathological samples is present [13] [12].
Standardized Experimental Protocol for Comparison
A typical methodology for head-to-head algorithm comparison, as used in several studies, involves a two-dataset approach [13]:
- Dataset Creation:
- Reference Data Set (Gold Standard): Created using the direct approach. Involves recruiting individuals under strict inclusion/exclusion criteria (e.g., specific BMI, blood pressure, absence of chronic diseases, negative thyroid antibodies) to define a robust "healthy" population [13].
- Test Data Set: Derived from a laboratory information system (LIS), typically from a broader physical examination or outpatient population. This dataset undergoes simplified preprocessing (e.g., demographic balancing and outlier removal) but does not filter for health status, thus containing a mix of healthy and pathological results [4] [13].
- Algorithm Application: Multiple data mining algorithms are applied to the same Test Data Set to establish RIs for various thyroid hormones.
- Performance Evaluation: The RIs generated by each algorithm from the Test Data Set are compared against the gold-standard RIs from the Reference Data Set. A key metric for objective assessment is the Bias Ratio (BR) matrix, where a lower BR indicates higher consistency with the standard RIs [4] [13].
The following diagram illustrates this comparative workflow.
Quantitative Performance Comparison
The performance of an algorithm can be highly dependent on the specific hormone being analyzed. The data below, synthesized from recent comparative studies, reveals these critical differences.
Table 1: Algorithm Performance for TSH vs. FT4 RI Establishment
| Algorithm | Data Type | TSH RI Performance & Reference Intervals | FT4 RI Performance & Reference Intervals | Key Findings |
|---|---|---|---|---|
| EM | Patient Data (Skewed) | High consistency with standard RIs (BR=0.063) [13] [14] | Limited performance for FT4 and other hormones in some scenarios [13] | Recommended for TSH when using skewed patient data [4] |
| kosmic | Physical Examination | Higher upper RI (e.g., 7.00 mIU/L) reported vs. manufacturer's IFU [12] | Good correlation with manufacturer's IFU (e.g., 0.57-1.18 ng/dL) [12] | Reliable for FT4; may yield higher upper limits for TSH [12] |
| refineR | Physical Examination | Higher upper RI (e.g., 8.19 mIU/L) reported vs. manufacturer's IFU [12] | Good correlation with manufacturer's IFU (e.g., 0.61-1.32 ng/dL) [12] | Reliable for FT4; may yield higher upper limits for TSH [12] |
| Hoffmann | Physical Examination | Comparable results with manufacturer's IFU (e.g., 0.3-4.0 mIU/L) [12] | Good correlation with manufacturer's IFU (e.g., 0.6-1.2 ng/dL) [12] | Reliable for both TSH and FT4 on physical exam data [4] [12] |
| Bhattacharya | Physical Examination | N/A in cited sources | RIs for FT3/TT4 close to standard RIs [13] | Performs well for free/total thyroid hormones with Gaussian distributions [13] |
Table 2: Summary of Best-Fit Algorithm Applications
| Hormone | Recommended Algorithm(s) | Optimal Data Source | Notes |
|---|---|---|---|
| TSH | EM Algorithm | Patient Data (with obvious skewness) | Requires Box-Cox transformation for skewed data [4] [14] |
| TSH | Hoffmann Algorithm | Physical Examination Data | Provides RIs consistent with manufacturer's ranges [12] |
| FT4 | Hoffmann, Bhattacharya, kosmic, refineR | Physical Examination Data | These algorithms show good performance and consistency for FT4 [4] [13] [12] |
The Scientist's Toolkit: Key Research Reagents and Materials
The reliability of any algorithm comparison hinges on consistent and high-quality laboratory data. The following materials and platforms are critical for generating such data in this field.
Table 3: Essential Research Reagents and Platforms
| Item | Function & Application in Research | Example Manufacturers/Platforms |
|---|---|---|
| Chemiluminescent Immunoassay Analyzer | Core platform for precise measurement of serum levels of TSH, FT3, and FT4. | Siemens ADVIA Centaur XP [13], Beckman Coulter DxI [33] [12] |
| Standardized Reagent Kits & Calibrators | Ensure assay accuracy, precision, and comparability of results across different studies and time points. | Manufacturer-provided kits and calibrators (e.g., Siemens) [13] |
| Quality Control (QC) Materials | Used to monitor daily analytical performance and ensure the correctness and reliability of testing results. | Commercial QC products aligned with ISO 15189:2012 standards [13] [12] |
| Laboratory Information System (LIS) | Source of large-scale, real-world data (RWD) essential for developing and validating indirect algorithms. | Various institutional LIS platforms [13] [12] |
The evidence clearly demonstrates that there is no single "best" algorithm for establishing reference intervals for all thyroid hormones. The choice is context-dependent, primarily influenced by the specific hormone of interest and the characteristics of the dataset being analyzed.
- For TSH, particularly when dealing with skewed patient data, the Expectation-Maximization (EM) algorithm combined with a Box-Cox transformation is the most accurate and recommended choice [4] [14]. For physical examination data, the Hoffmann algorithm also demonstrates strong performance for TSH [12].
- For FT4, a wider range of algorithms performs reliably. The transformed Hoffmann, Bhattacharya, kosmic, and refineR algorithms all show good consistency with standard RIs when applied to physical examination data [4] [13].
A critical secondary finding is that physical examination data generally yields greater consistency across different algorithms compared to outpatient data [4] [14]. This is likely due to a lower prevalence of pathological values in examination populations. Therefore, researchers should prioritize data sources with a higher proportion of healthy individuals wherever possible. Ultimately, selecting the correct algorithm based on the data distribution and analyte is paramount for generating accurate, clinically relevant reference intervals that can advance both patient care and thyroid-related research.
The establishment of robust reference intervals (RIs) for thyroid hormones is a cornerstone of reliable clinical diagnosis and treatment of thyroid dysfunction. These intervals, which define the range of test values expected in a healthy population, are fundamentally dependent on the statistical and data mining algorithms used to derive them. However, different methodologies can produce varying results, leading to a significant challenge: inter-algorithm variability. This inconsistency can affect diagnostic accuracy, patient management, and the harmonization of clinical guidelines. Within the broader thesis of comparing data mining algorithms for thyroid hormone research, this guide provides an objective comparison of the performance of key methodological approaches. It assesses their consistency and reliability using supporting experimental data, offering researchers and drug development professionals a clear framework for evaluating these essential tools.
Key Methodologies for Establishing Reference Intervals
The process of establishing RIs can be broadly categorized into direct and indirect methods, each with distinct algorithmic implementations.
Direct Methods: These involve the a priori selection of carefully screened, healthy individuals from a reference population. Blood samples are collected and analyzed, and the RIs are determined statistically, typically as the central 95% of the resulting values [54]. While considered the gold standard by organizations like the Clinical Laboratory Standards Institute (CLSI), direct methods are costly, time-consuming, and often impractical for individual laboratories to implement, especially for specific sub-populations [55] [56].
Indirect Methods: These utilize the vast amounts of data already stored in Laboratory Information Systems (LIS). By applying sophisticated data mining algorithms, these methods attempt to separate the "healthy" distribution of test results from the mixed population of healthy and sick individuals [20] [56]. Indirect methods are faster, cheaper, and more feasible for establishing local RIs, and their use is encouraged by the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) [54]. The reliability of these methods hinges on the algorithm's ability to accurately identify and model the underlying healthy distribution.
Several key algorithms are employed in establishing thyroid hormone RIs, each with a unique approach to handling data.
refineR Algorithm: This indirect algorithm uses an inverse modeling approach. It applies a series of parameterized distributions to the data, identifies the model that best fits the central, presumably healthy, part of the distribution, and uses it to estimate the RI. Its core strength lies in its optimization process for separating healthy from pathological distributions [20].
Hoffman Method: A classic indirect method, the Hoffman approach is based on a graphical analysis of the data distribution. After logarithmic transformation, a Q-Q plot is created. The linear portion of this plot is assumed to represent the Gaussian distribution of healthy individuals. A regression line is fitted to this portion and extrapolated to calculate the 2.5th and 97.5th percentiles, defining the RI [56].
Non-Parametric Percentile Method: Often used with direct data or after outlier removal in indirect studies, this is a straightforward method where the RI is defined by the 2.5th and 97.5th percentiles of the reference population's test results [54]. It makes no assumptions about the underlying data distribution.
Table 1: Key Features of Prominent RI Establishment Algorithms.
| Algorithm | Type | Core Principle | Primary Data Input | Key Advantage |
|---|---|---|---|---|
| refineR | Indirect | Inverse modeling & optimal model search | Routine patient data from LIS | Automated separation of healthy/pathological distributions |
| Hoffman Method | Indirect | Graphical analysis (Q-Q plot) & linear regression | Routine patient data from LIS | Simplicity and visual verification of Gaussian distribution |
| Non-Parametric | Direct/Indirect | Ranking and percentile calculation | Pre-selected healthy individuals | No assumption of Gaussian distribution required |
| Machine Learning (e.g., RF, SVM) | Indirect | Classification and pattern recognition | Routine patient data with features | Handles high-dimensional data and complex interactions |
Comparative Analysis of Algorithm Performance
Evaluating different algorithms on the same or comparable datasets reveals critical differences in their output and performance.
Comparative Data on Thyroid Hormone RIs
Studies applying different algorithms have demonstrated notable variability in the resulting reference intervals, which can directly impact clinical diagnosis.
Table 2: Comparative Reference Intervals for TSH and FT4 from Selected Studies.
| Study & Population | Algorithm Used | Analyte | Reference Interval | Notes |
|---|---|---|---|---|
| Tibetan Population [20] | refineR | TSH | 0.764 – 5.784 μIU/mL | Higher upper limit than manufacturer |
| FT4 (Female) | 12.36 – 19.38 pmol/L | Sex-specific partitioning required | ||
| FT4 (Male) | 14.84 – 20.18 pmol/L | Sex-specific partitioning required | ||
| Polish Population [56] | Hoffman | TSH (Adults) | 0.59 – 4.41 mIU/L | Age and sex-specific RIs established |
| fT4 (Adults) | 11.97 – 20.37 pmol/L | |||
| General Population [54] | Non-Parametric | TSH | 0.17 – 5.28 mIU/L | Highlights wide discrepancy in literature |
| Manufacturer (Roche) [20] | Not Specified | TSH | 0.27 – 4.20 mIU/L | Often used as default in laboratories |
Quantitative Performance Metrics
Beyond the RIs themselves, the performance of indirect algorithms can be gauged by metrics like accuracy in classifying health status and computational efficiency. While direct comparisons are limited in the literature, insights can be drawn from related applications.
Accuracy in Disease Classification: Machine learning models like Random Forests (RF) and Artificial Neural Networks (ANN) have demonstrated high accuracy (>99% in some studies) when used for thyroid disease classification, suggesting their potential power in identifying healthy patterns for RI establishment [57] [58]. One study noted that an ANN classifier achieved an F1-score of 0.957, indicating a strong balance between precision and recall [57].
Handling of Covariates: Advanced algorithms show differing capabilities in managing confounding factors like age, sex, and altitude. The refineR algorithm was successfully used to establish altitude-specific RIs for FT3 in a Tibetan population, a task that requires effectively partitioning data based on an environmental covariate [20]. Similarly, the Hoffman method has been applied to create age- and sex-stratified RIs [56].
Detailed Experimental Protocols
To ensure reproducibility and critical evaluation, this section outlines the detailed methodologies from key studies cited in this guide.
Protocol for the refineR Algorithm
A study establishing RIs for Tibetans at high altitude provides a clear protocol for using the refineR algorithm [20]:
- Subject Recruitment and Data Collection: 1,281 apparently healthy Tibetan subjects were randomly recruited from three regions of Tibet with varying altitudes (2,900m to 4,352m). Fasting venous blood samples were collected and serum was separated.
- Laboratory Analysis: Serum TSH, FT3, and FT4 were measured using a Cobas e601 electrochemiluminescence analyzer. Strict quality control procedures were implemented, including the use of two levels of commercial control sera.
- Data Cleaning and Statistical Analysis: Data cleaning and analysis were performed using R programming language. The effects of sex, age, and altitude on hormone levels were assessed using multiple linear regression and variance component analysis. A standard deviation ratio (SDR) of 0.4 was used as a threshold to determine if partitioning (e.g., by sex or altitude) was necessary.
- RI Establishment with refineR: The refineR algorithm (implemented via the refineR package in R) was applied to the data. This algorithm works by iteratively testing and refining a model of the underlying healthy distribution to ultimately determine the central 95% RI.
The following workflow diagram illustrates the key steps of this protocol:
Protocol for the Hoffman Method
A study establishing laboratory-specific RIs in a Polish population details the use of the Hoffman method [56]:
- Data Gathering: A total of 105,927 de-identified TSH results and 41,400 fT4 results archived in the Laboratory Information System over a five-year period were included without primary selection.
- Data Pre-processing: Due to strong right-skewness, all data were logarithmically transformed. Data were then divided into 8 age groups. The Tukey test (1.5 IQR) was used to reject outliers within each age group.
- Q-Q Plot Analysis and RI Calculation: For each age group, a Q-Q plot was created. The linear part of the plot, assumed to represent the healthy population, was identified. A regression line was fitted to this linear part, and only results with a correlation coefficient (r) > 0.99 were accepted. The lower and upper reference limits were calculated as LRL = -1.96 × a + b and URL = 1.96 × a + b, where 'a' is the slope and 'b' is the intercept of the regression line. The final RIs were obtained by taking the antilogarithm of these calculated limits.
The workflow for this method is distinct and relies heavily on graphical analysis:
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents, instruments, and software solutions essential for conducting research in thyroid hormone reference intervals.
Table 3: Essential Research Reagents and Solutions for Thyroid Hormone RI Studies.
| Item Name | Function/Application | Example Specification/Provider |
|---|---|---|
| Electrochemiluminescence Immunoassay (ECLIA) Analyzer | Quantitative measurement of TSH, FT3, FT4, and antibodies in serum. | Cobas e601/e801 analyzers (Roche) [20] [54] |
| Thyroid Hormone Assay Kits | Specific reagents, calibrators, and antibodies for measuring thyroid analytes. | TSH (sandwich IA), fT4/fT3 (competitive IA) kits, calibrated against international standards [20] [54] |
| Quality Control Sera | Monitoring precision and accuracy of assays across multiple runs. | Commercial control sera at two or more levels (e.g., provided by assay manufacturer) [20] [54] |
| Blood Collection Tubes | Standardized collection of serum samples. | Vacuette 5-mL tubes with gel separator (Greiner Bio-One) [20] |
| Statistical Computing Software | Data cleaning, analysis, and implementation of RI algorithms (refineR, Hoffman). | R Programming Language with packages (e.g., refineR) [20] [56] |
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Reference method for validating the accuracy of immunoassays, especially at low concentrations. | Considered a gold standard for hormone measurement [59] |
The comparative analysis presented in this guide clearly demonstrates that methodological choice is a significant source of variability in thyroid hormone reference intervals. Indirect methods like refineR and the Hoffman method offer a practical and powerful alternative to costly direct methods, but they each come with their own assumptions and computational complexities. The observed differences in RIs, such as the higher upper limit for TSH derived by refineR compared to a manufacturer's default, are not merely statistical artifacts; they have real-world clinical implications, potentially affecting the diagnosis of subclinical hypothyroidism or hyperthyroidism [20] [55].
The consistency and reliability of any algorithm are influenced by several factors. Pre-analytical and analytical conditions, including sample collection procedures and the type of immunoassay platform used, introduce a layer of variation before any algorithm is applied [59]. Furthermore, the ability of an algorithm to handle population covariates like age, sex, ethnicity, and environmental factors like altitude is crucial for generating truly representative and useful RIs [20] [60]. The move towards age-specific reference intervals is a prime example of how refining these methodologies can prevent misdiagnosis, particularly in older adults [56] [60].
In conclusion, there is no single "best" algorithm for all scenarios. The choice depends on the available data, computational resources, and the specific population being studied. The future of this field lies in the continued refinement of these data mining tools, improved harmonization of laboratory assays, and a greater emphasis on establishing well-partitioned, locally relevant reference intervals. Researchers and clinicians must be aware of the inherent variability between methods and prioritize transparency in reporting the algorithms used to establish the reference intervals that guide critical healthcare decisions.
The establishment of accurate Reference Intervals (RIs) is a cornerstone of clinical laboratory medicine, providing the essential benchmarks against which patient test results are interpreted for diagnostic and monitoring purposes [61] [13]. For thyroid-related hormones, the correct determination of RIs is particularly crucial, given the high global prevalence of thyroid disorders and the subtle hormonal shifts that characterize subclinical disease states [5] [13]. Traditionally, RIs are established using the direct approach, which involves recruiting a carefully selected cohort of healthy individuals through a costly, time-consuming, and logistically challenging process [61] [13]. This often forces laboratories to adopt RIs from manufacturer's inserts or the literature, which may not be applicable to their local population due to differences in genetics, environment, diet, or analytical methods [61].
In recent years, the indirect approach, which leverages data mining algorithms on large datasets of routine clinical results, has emerged as a powerful and feasible alternative [5] [61] [13]. This method is based on the premise that the majority of results in a laboratory information system originate from presumably healthy individuals, and robust algorithms can statistically separate this "healthy" distribution from the mixed data that includes pathological values [13]. The adoption of this approach, however, presents a new challenge for laboratory professionals: selecting the most appropriate algorithm from a growing array of options. This guide provides evidence-based, comparative recommendations for selecting optimal data mining algorithms for establishing thyroid hormone RIs, grounded in recent comparative studies and tailored to specific data characteristics and clinical needs.
A range of algorithms is available for the indirect establishment of RIs. They can be broadly categorized by their underlying statistical principles and their handling of data distribution types.
Table 1: Core Data Mining Algorithms for Reference Interval Establishment
| Algorithm | Underlying Principle | Key Strength | Key Limitation | Optimal Data Distribution |
|---|---|---|---|---|
| Hoffmann | Graphical method [13] | Intuitive, easy to understand [13] | Assumes a large healthy population with Gaussian/near-Gaussian distribution [13] | Gaussian / Near-Gaussian [5] [13] |
| Bhattacharya | Graphical method [13] | Intuitive, widely used [13] | Performance can degrade if healthy distribution assumption is violated [13] | Gaussian / Near-Gaussian [5] [13] |
| Expectation-Maximization (EM) | Iterative maximum-likelihood estimation [5] [13] | Can handle significantly skewed data [5] | Performance is limited outside of its specific use case; complex parameter setting [5] [13] | Skewed [5] |
| kosmic | Parametric approach with Box-Cox transformation [13] | Designed to handle skewed distributions [13] | Performance may vary with proportion of pathological data [13] | Non-Gaussian / Skewed [13] |
| refineR | Parametric approach with inverse modeling and Box-Cox transformation [61] [13] | Effectively handles non-Gaussian data; validated on complex distributions [61] [13] | May be less intuitive than graphical methods | Non-Gaussian / Skewed [61] [13] |
Comparative Experimental Performance Data
Objective comparison of algorithms is vital for selection. A 2023 study by Chen et al. provided a robust evaluation framework, using a Bias Ratio (BR) matrix to objectively compare RIs derived from five algorithms against "standard" RIs obtained via the direct method from a rigorously defined reference population [5] [13]. A lower BR indicates higher consistency with the standard RI.
Table 2: Algorithm Performance for Thyroid Hormone RIs (Adapted from Chen et al., 2023) Performance is measured by Bias Ratio (BR); lower values indicate better alignment with standard RIs. The most performant algorithm for each hormone is highlighted.
| Thyroid Hormone | Hoffmann BR | Bhattacharya BR | EM BR | kosmic BR | refineR BR |
|---|---|---|---|---|---|
| TSH | 0.223 | 0.194 | 0.063 | 0.155 | 0.129 |
| Free Triiodothyronine (FT3) | 0.028 | 0.042 | 0.414 | 0.041 | 0.041 |
| Total Triiodothyronine (TT3) | 0.059 | 0.039 | 0.371 | 0.045 | 0.058 |
| Free Thyroxine (FT4) | 0.093 | 0.072 | 0.321 | 0.061 | 0.074 |
| Total Thyroxine (TT4) | 0.058 | 0.061 | 0.327 | 0.044 | 0.055 |
The data reveals a critical finding: no single algorithm outperforms all others across every thyroid hormone. The EM algorithm demonstrated superior performance for the typically skewed Thyroid-Stimulating Hormone (TSH) data, consistent with its design strength [5]. In contrast, for hormones like FT3, TT3, FT4, and TT4, which often exhibit Gaussian or near-Gaussian distributions, the Hoffmann, Bhattacharya, kosmic, and refineR algorithms showed closer alignment with the standard RIs, with the top performer varying by the specific analyte [5]. This underscores the necessity of a hormone-specific and data-driven selection process.
Experimental Protocol for Benchmarking Algorithms
The methodology from the cited comparative study provides a replicable protocol for laboratories to validate or benchmark algorithms using their own data [5] [13].
1. Dataset Establishment:
- Reference Data Set: Create a "gold standard" set by applying strict inclusion/exclusion criteria to a physical examination population. Criteria should exclude individuals with abnormal BMI, hypertension, known systemic diseases, abnormal thyroid ultrasound, or positive thyroid antibodies (TPO-Ab, Tg-Ab). Sex and age ratios should be balanced by random sampling [13].
- Test Data Set: Derive a larger, more realistic dataset from the Laboratory Information System (LIS) using a simplified preprocessing pipeline. This involves balancing sex/age ratios via random sampling and identifying outliers using the Tukey method, without applying strict health criteria [13].
2. RI Calculation and Comparison:
- Establish standard RIs from the Reference Data Set using a transformed parametric method after Box-Cox transformation to improve normality [13].
- Establish test RIs from the Test Data Set using the various data mining algorithms (e.g., Hoffmann, Bhattacharya, EM, kosmic, refineR) [5] [13].
- Objectively compare the test RIs to the standard RIs using a Bias Ratio (BR) matrix. The BR is calculated for each algorithm and hormone to quantify the degree of agreement [5].
The following workflow diagram illustrates this experimental protocol:
Decision Framework: Matching Algorithms to Clinical Laboratory Scenarios
Based on the comparative evidence, laboratories can adopt the following decision framework to guide their algorithm selection.
1. Assess Data Distribution: The first and most critical step is to evaluate the distribution of the real-world data for the specific thyroid hormone.
- For Skewed Distributions (e.g., TSH): The EM algorithm has been shown to be highly effective, achieving a BR of 0.063 in direct comparison studies [5]. Its ability to handle significant skewness makes it a prime candidate.
- For Gaussian/Near-Gaussian Distributions (e.g., FT3, FT4, TT3, TT4): The Hoffmann, Bhattacharya, kosmic, and refineR algorithms all perform well [5] [13]. The choice can be guided by secondary factors such as computational resource availability, software implementation ease, and the laboratory's familiarity with the method. The refineR algorithm is particularly recommended for its robust handling of non-Gaussian data and strong performance across multiple hormones [61].
2. Consider Population Specificity: Standard RIs may not be valid for unique populations, such as those living at high altitudes. The refineR algorithm has been successfully employed to establish specific RIs for Tibetan populations, revealing significant differences from manufacturer-provided intervals [61]. For laboratories serving unique demographic or geographic groups, indirect methods like refineR offer a practical path to personalized, accurate RIs.
3. Prioritize a Multi-Algorithm Approach: Given the analyte-dependent performance of algorithms, the most robust strategy for a clinical laboratory is to validate multiple algorithms. Laboratories should benchmark key algorithms like EM for TSH and a combination of Hoffmann/Bhattacharya/refineR for other thyroid hormones against their internal data or published standards to build a validated, analyte-specific toolkit [5].
The Scientist's Toolkit: Essential Reagents and Materials
The successful implementation of an indirect RI establishment project relies on the following key components:
Table 3: Essential Research Reagents and Materials for RI Studies
| Item | Function / Application | Example from Literature |
|---|---|---|
| Electrochemiluminescence Immunoassay Analyzer | Quantitative measurement of thyroid hormones (TSH, FT3, FT4, etc.) and antibodies. | Cobas e601 analyzer (Roche) [61]; ADVIA Centaur XP (Siemens Healthineers) [13] |
| Corresponding Reagents & Calibrators | Ensure analytical accuracy and traceability of measurements for thyroid hormones. | Manufacturer-provided reagents and calibrators [61] [13] |
| Procoagulant Blood Collection Tubes | Standardized collection of venous blood samples for serum separation. | Vacuette tubes (Greiner Bio-One) [61] [13] |
| Statistical Computing Software | Platform for data cleaning, outlier detection, distribution analysis, and execution of data mining algorithms. | R programming language (with refineR, forecast packages) [61] [13] |
| Validated R Packages | Implementation of specific data mining algorithms for RI establishment. | refineR package [61] [13] |
The indirect establishment of thyroid hormone RIs using data mining algorithms represents a significant advancement in laboratory medicine, offering a cost-effective, efficient, and population-specific alternative to the direct method. The key to successful implementation lies in moving beyond a one-size-fits-all approach. Evidence clearly demonstrates that algorithm performance is intrinsically linked to the distribution characteristics of the analyte in question.
Laboratories are advised to adopt a nuanced, data-driven strategy: employ the EM algorithm for skewed data like TSH, and leverage a suite of algorithms including Hoffmann, Bhattacharya, kosmic, and refineR for Gaussian-distributed hormones. By establishing an internal benchmarking protocol to validate algorithms against their specific patient populations and analytical platforms, clinical laboratories can ensure the delivery of the most accurate and clinically relevant reference intervals, ultimately enhancing the quality of thyroid disease diagnosis and patient care.
Conclusion
The establishment of precise thyroid hormone reference intervals is paramount for accurate clinical diagnosis and effective patient stratification in drug development. This analysis demonstrates that no single data mining algorithm is universally superior; rather, performance is highly dependent on the specific hormone's data distribution characteristics. The EM algorithm excels for significantly skewed data like TSH, while Hoffmann, Bhattacharya, and refineR perform robustly for Gaussian or near-Gaussian distributions. The adoption of a standardized validation framework, particularly the Bias Ratio matrix, is crucial for objectively evaluating algorithmic performance. Future efforts should focus on developing hybrid approaches that combine the strengths of multiple algorithms, creating standardized benchmarking suites for diverse clinical datasets, and further integrating these refined data mining techniques into clinical decision support systems to pave the way for more personalized and precise thyroid disease management.
References
- 1. for Reference disorders calculated by indirect... intervals thyroid [https://pmc.ncbi.nlm.nih.gov/articles/PMC9807239/]
- 2. for Reference disorders... - Biochemia Medica intervals thyroid [https://www.biochemia-medica.com/en/journal/33/1/10.11613/BM.2023.010704]
- 3. Validation of an approach using only patient big data from clinical laboratories to establish reference intervals for thyroid hormones based on data mining - PubMed [https://pubmed.ncbi.nlm.nih.gov/32199936/]
- 4. Validation and comparison of five data mining algorithms using big data from clinical laboratories to establish reference intervals of thyroid hormones for older adults - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S0009912022001370]
- 5. Utilization of five data mining algorithms combined with simplified preprocessing to establish reference intervals of thyroid-related hormones for non-elderly adults - PubMed [https://pubmed.ncbi.nlm.nih.gov/37131135/]
- 6. Synthesis and preclinical testing of a selective beta-subtype agonist of thyroid hormone receptor ZTA-261 | Communications Medicine [https://www.nature.com/articles/s43856-024-00574-z]
- 7. Drug discovery targeting thyroid hormone receptor β (THRβ) for the treatment of liver diseases and other medical indications - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2211383524003150]
- 8. THYROID HORMONE ANALOGUES FOR THE TREATMENT OF METABOLIC DISORDERS: NEW POTENTIAL FOR UNMET CLINICAL NEEDS? - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3745011/]
- 9. Thyroid Hormone Analogues: An Update - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7415871/]
- 10. of Reference stimulating interval and free thyroxine... thyroid hormone [https://thyroidresearchjournal.biomedcentral.com/articles/10.1186/1756-6614-6-13]
- 11. A Prospective Study to Determine Trimester-Specific Thyroid Function... [https://link.springer.com/article/10.1007/s40618-025-02651-z]
- 12. Verification of Reference of Interval With Manual... Thyroid Hormones [https://pmc.ncbi.nlm.nih.gov/articles/PMC10267605/]
- 13. Utilization of five data mining algorithms combined with simplified preprocessing to establish reference intervals of thyroid-related hormones for non-elderly adults | BMC Medical Research Methodology | Full Text [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-01898-5]
- 14. Validation and comparison of five data mining algorithms using big data from clinical laboratories to establish reference intervals of thyroid hormones for older adults - PubMed [https://pubmed.ncbi.nlm.nih.gov/35636495/]
- 15. [Establishing reference intervals of thyroid based on...] hormone [https://pubmed.ncbi.nlm.nih.gov/32074686/]
- 16. An Evaluation of the Efficacy of Machine Learning in Predicting Thyrotoxicosis and Hypothyroidism: A Comparative Assessment of Biochemical Test Parameters Used in Different Health Checkups - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11414366/]
- 17. Establishing laboratory-specific reference for TSH and fT4 by... intervals [https://pmc.ncbi.nlm.nih.gov/articles/PMC8741008/]
- 18. Assessment of Vitamin D Sufficiency in Different Age Groups of... [https://bakirkoymedj.org/articles/assessment-of-vitamin-d-sufficiency-in-different-age-groups-of-children-in-turkiye-using-the-bhattacharya-method/doi/BMJ.galenos.2025.2024.11-10]
- 19. Estimation of Reference Intervals from Routine Data Using the refineR Algorithm-A Practical Guide - PubMed [https://pubmed.ncbi.nlm.nih.gov/36610416/]
- 20. Establishment of Reference for Intervals -Associated... Thyroid [https://pmc.ncbi.nlm.nih.gov/articles/PMC8874314/]
- 21. Frontiers | Establishment of Reference Intervals for Thyroid-Associated Hormones Using refineR Algorithm in Chinese Population at High-Altitude Areas [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2022.816970/full]
- 22. Reference Intervals for Thyroid -Associated Hormones and the... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7443523/]
- 23. Neonatal reference intervals for thyroid stimulating hormone and free... [https://bmcendocrdisord.biomedcentral.com/articles/10.1186/s12902-023-01367-6]
- 24. Age- and sex- specific reference intervals for thyroid in... hormones [https://tp.amegroups.org/article/view/80097/html]
- 25. National recommendations of the Croatian society... - Biochemia Medica [https://www.biochemia-medica.com/en/journal/35/3/10.11613/BM.2025.030505]
- 26. Establishing laboratory-specific reference for TSH and fT4 by... intervals [https://pubmed.ncbi.nlm.nih.gov/34995316/]
- 27. Assessment of Vitamin D Sufficiency in Different Age Groups of... [https://bakirkoymedj.org/articles/assessment-of-vitamin-d-sufficiency-in-different-age-groups-of-children-in-turkiye-using-the-bhattacharya-method/BMJ.galenos.2025.2024.11-10]
- 28. Estimation of TSH reference intervals for the first trimester of pregnancy using real world data and the refineR algorithm - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0009898125005686]
- 29. Reference intervals for thyroid disorders calculated by indirect method and comparison with reference change values - PubMed [https://pubmed.ncbi.nlm.nih.gov/36627974/]
- 30. the effect of different scalers on Compare with data outliers [https://scikit-learn.org/stable/auto_examples/preprocessing/plot_all_scaling.html]
- 31. Pandas Core Data Techniques... - DEV Community Preprocessing [https://dev.to/uche_4rm_germany/pandas-core-data-preprocessing-techniques-a-recap-2nmh]
- 32. 壹生资讯-甲状腺疾病生物标志物检测与临床诊断价值 [https://www.medtrib.cn/post/detail/1a2221fe-9324-4009-8d4d-15244c43208f]
- 33. Comparison of method-related reference intervals for thyroid hormones: studies from a prospective reference population and a literature review - PubMed [https://pubmed.ncbi.nlm.nih.gov/28081637/]
- 34. Age-related variation in thyroid function – a narrative review... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10069079/]
- 35. Reference ranges for TSH and thyroid hormones - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4480274/]
- 36. Reference Intervals for Serum Thyroid-Stimulating Hormone Based on a Recent Nationwide Cross-Sectional Study and Meta-Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8204855/]
- 37. Survey on deep learning with class imbalance | Journal of Big Data | Full Text [https://journalofbigdata.springeropen.com/articles/10.1186/s40537-019-0192-5]
- 38. Solving the class problem using ensemble algorithm... imbalance [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-022-01821-w]
- 39. (PDF) The weighing of pathological and non - pathological information... [https://www.academia.edu/78719968/The_weighing_of_pathological_and_non_pathological_information_in_clinical_judgment]
- 40. 10 Techniques to Solve Imbalanced Classes in Machine Learning (Updated 2025) [https://www.analyticsvidhya.com/blog/2020/07/10-techniques-to-deal-with-class-imbalance-in-machine-learning/]
- 41. Addressing Class with Latent Diffusion-based Imbalance ... Data [https://pmc.ncbi.nlm.nih.gov/articles/PMC11936509/]
- 42. Cross-Patient Pseudo Bags Generation and Curriculum Contrastive... [https://arxiv.org/html/2411.11262v1]
- 43. JCPSP | Journal of College of Physicians and Surgeons Pakistan [https://jcpsp.pk/article-detail/pharnessing-the-power-of-big-data-analyticsestimation-of-reference-intervals-for-neonatal-serum-tsh-in-pakistan-using-refiner-algorithmorp]
- 44. Can data produce a healthy mining population... | myadlm.org reference [https://myadlm.org/science-and-research/scientific-shorts/2019/data-mining--healthy-reference-population-age-specific-tsh-reference-intervals]
- 45. Utilization of five data combined with simplified... mining algorithms [https://pmc.ncbi.nlm.nih.gov/articles/PMC10152698/]
- 46. Frontiers | Reference Intervals for Serum Thyroid-Stimulating Hormone Based on a Recent Nationwide Cross-Sectional Study and Meta-Analysis [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2021.660277/full]
- 47. Indirect determination of hemoglobin A2 reference intervals in Pakistani... [https://link.springer.com/article/10.1186/s12911-025-02857-4]
- 48. Using Hashimoto thyroiditis as gold standard to determine the upper limit value of thyroid stimulating hormone in a Chinese cohort | BMC Endocrine Disorders | Full Text [https://bmcendocrdisord.biomedcentral.com/articles/10.1186/s12902-016-0137-3]
- 49. Reference intervals for thyroid for the elderly population... hormones [https://pmc.ncbi.nlm.nih.gov/articles/PMC10040197/]
- 50. To Generate an Ensemble Model for Women Thyroid Prediction Using... [https://pubmed.ncbi.nlm.nih.gov/31031212/]
- 51. 数据挖掘的11大算法及python实现(个人笔记整理,非教学用)_数据挖掘算法-CSDN博客 [https://blog.csdn.net/weixin_43290383/article/details/114284670]
- 52. Generated by Electronic Medical Record Data... Reference Intervals [https://pubmed.ncbi.nlm.nih.gov/33636933/]
- 53. A validated LC-MS/MS method for cellular thyroid ... hormone [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0183482]
- 54. for Reference disorders... - Biochemia Medica intervals thyroid [https://www.biochemia-medica.com/en/journal/33/1/10.11613/BM.2023.010704/bm-33-1-010704-f1/fullArticle/fullArticle/fullArticle]
- 55. Reference intervals in the diagnosis of thyroid dysfunction: treating patients not numbers - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S2213858718303711]
- 56. Establishing laboratory-specific reference intervals for TSH and fT4 by use of the indirect Hoffman method | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0261715]
- 57. Application of machine learning algorithms to predict the thyroid disease risk: an experimental comparative study - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9044232/]
- 58. Thyroid Disease Prediction Using Selective Features and Machine Learning Techniques - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405591/]
- 59. Assessment of thyroid function tests and harmonization: opinion on thyroid hormone harmonization - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6931143/]
- 60. Age-related variation in thyroid function – a narrative review... [https://thyroidresearchjournal.biomedcentral.com/articles/10.1186/s13044-023-00149-5]
- 61. Establishment of Reference Intervals for Thyroid-Associated Hormones Using refineR Algorithm in Chinese Population at High-Altitude Areas - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8874314/]