Measuring What Matters: A Guide to the Psychometric Properties of Reproductive Health Surveys
This article provides a comprehensive guide for researchers and drug development professionals on the critical psychometric properties of reproductive health assessment tools.
Measuring What Matters: A Guide to the Psychometric Properties of Reproductive Health Surveys
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the critical psychometric properties of reproductive health assessment tools. It explores the foundational concepts of validity and reliability, details the methodological steps for scale development and application, addresses common challenges in optimization, and establishes standards for rigorous validation and cross-cultural comparison. By synthesizing current methodologies and evidence from recent studies, this resource aims to equip scientists with the knowledge to select, develop, and implement robust, culturally-sensitive instruments that yield reliable data for clinical research and intervention development.
Core Principles: Understanding Validity and Reliability in Reproductive Health Metrics
In the field of sexual and reproductive health (SRH) research, the quality of data and the robustness of findings are paramount. Our clinical reasoning, intervention strategies, and research conclusions can only be as strong as the tools we use for measurement [1]. Psychometrics—the field concerned with the statistical description of instrumental data and the relationships between variables—provides the foundation for ensuring that our measurement instruments are scientifically sound [1]. For researchers, scientists, and drug development professionals working in SRH, understanding the core psychometric properties of validity, reliability, and responsiveness is essential for developing rigorous surveys and assessment tools that yield trustworthy, actionable data. This technical guide examines these properties within the specific context of SRH research, where measuring sensitive constructs such as contraceptive needs, service-seeking behaviors, and health outcomes requires particularly meticulous methodological approaches.
Core Psychometric Properties
Psychometric properties represent the methodological qualities of assessment tools, questionnaires, outcome measures, scales, or clinical tests [1]. In SRH research, these properties ensure that instruments developed for specific populations—such as adolescents, young adults, or specific cultural groups—generate data that accurately reflects the constructs being studied.
Validity
Validity refers to a tool's ability to measure what it is intended to measure [1]. In SRH research, this extends beyond simple face validity to encompass whether an instrument truly captures complex, multi-faceted constructs such as "contraceptive need," "service-seeking behavior," or "reproductive autonomy."
The following table summarizes the key types of validity and their application in SRH research:
Table 1: Types of Validity and Their Applications in SRH Research
| Validity Type | Definition | SRH Research Application | Quantitative Metrics |
|---|---|---|---|
| Content Validity | Degree to which tool content reflects the construct of interest [1] | Ensuring SRH surveys cover all relevant topics (contraception, STIs, abortion, etc.) | Expert consensus ratings |
| Face Validity | Whether the tool appears to adequately reflect what it is supposed to measure [1] | Initial perception that SRH questions are appropriate and relevant | Stakeholder feedback |
| Construct Validity | Degree to which scores align with hypotheses based on abstract concepts [1] | Testing theoretical relationships between SRH knowledge and service utilization | Factor analysis fit indices [2] |
| Criterion Validity | How well tool measurements correlate with an established reference standard [1] | Comparing new contraceptive need measures against established indicators [3] | Correlation coefficients (r): Large ≥0.5, Moderate 0.3-0.5, Small 0.1-0.29 [2] |
| Cross-cultural Validity | Degree to which a culturally adapted tool is equivalent to the original [1] | Adapting SRH instruments for different cultural contexts while maintaining measurement properties | Measurement invariance statistics |
Recent innovations in SRH measurement highlight the evolving nature of validity. The Guttmacher Institute's "Adding It Up 2024" report introduces a new "unmet demand" measure for contraception that better aligns with rights-based, person-centered approaches by incorporating women's expressed intentions to use contraception, moving beyond assumptions based solely on pregnancy desires [3].
Reliability
Reliability refers to the extent to which a measurement is consistent and free from error [1]. In SRH research, this ensures that instruments yield stable results across different administrators, time points, and population subgroups. Reliability is not a fixed property but varies based on the instrument's application context and population [1].
Table 2: Reliability Types and Assessment Methods in SRH Research
| Reliability Type | Definition | Assessment Method | Interpretation Guidelines |
|---|---|---|---|
| Internal Consistency | Degree of inter-relatedness among items | Cronbach's Alpha | Excellent ≥0.80, Adequate 0.60-0.79, Poor <0.60 [2] |
| Test-Retest | Stability of scores when patients self-evaluate at two separate occasions [1] | Intraclass Correlation Coefficient (ICC) | Excellent ≥0.80, Good 0.60-0.79, Poor <0.60 [2] |
| Inter-rater | Agreement between different evaluators at the same time [1] | ICC or Kappa for categorical data | Excellent ≥0.80, Good 0.60-0.79, Poor <0.60 [2] |
| Intra-rater | Consistency of the same evaluator over time [1] | ICC or Kappa for categorical data | Excellent ≥0.80, Good 0.60-0.79, Poor <0.60 [2] |
The Total Teen Assessment validation study exemplifies comprehensive reliability testing in SRH research, employing a three-phase psychometric development process that included factor analysis to establish internal consistency across sexual health, mental health, and substance use domains [4].
Responsiveness
Responsiveness, also known as sensitivity to change, is an instrument's ability to detect clinically important changes over time, particularly in response to effective therapeutic interventions [1]. In SRH research, this property is crucial for evaluating whether interventions (such as educational programs or service delivery improvements) actually produce meaningful changes in knowledge, attitudes, or behaviors.
A tool is considered sensitive to change if it can precisely measure increases and decreases in the construct measured following an intervention [1]. Common indices of responsiveness include:
- Effect size with pooled or baseline standard deviation
- Standardized response mean
- Guyatt responsiveness index
- Receiver operating characteristic (ROC) curves [2]
The relationship between different measurement precision concepts can be visualized as follows:
Experimental Protocols for Psychometric Validation
Robust psychometric validation requires structured methodological approaches. The following protocols outline key processes for establishing instrument validity and reliability in SRH research.
Scale Development and Validation Protocol
The development of the Sexual and Reproductive Health Service Seeking Scale (SRHSSS) exemplifies a comprehensive validation methodology [5]:
Phase 1: Conceptualization and Item Development
- Conduct literature review to define construct boundaries
- Administer preliminary questionnaires to target population (n=98 in SRHSSS development)
- Conduct focus group interviews (n=8) to identify relevant themes and terminology
- Draft initial item pool with attention to including both positive and negative statements
- Ensure each item contains only one judgment/thought
Phase 2: Content Validation
- Engage expert evaluation (e.g., psychiatric nursing, obstetrics/gynecology nursing specialists)
- Assess content validity through structured expert ratings
- Obtain language expert review to ensure clarity and appropriateness
- Conduct pre-test with target population (n=15) to assess comprehensibility
- Refine items based on cognitive interviewing feedback
Phase 3: Psychometric Testing
- Administer scale to large sample (n=458 in SRHSSS study)
- Perform exploratory factor analysis to examine construct validity
- Calculate variance explained by extracted factors (89.45% in SRHSSS)
- Assess factor loadings (0.78-0.97 in SRHSSS)
- Establish reliability through Cronbach's alpha (α=0.90 in SRHSSS)
- Conduct test-retest reliability with sub-sample (n=220) at one-month interval
Electronic Assessment Implementation Protocol
The Total Teen Assessment validation study demonstrates specialized protocols for electronic SRH assessment [4]:
Workflow Integration
- Implement tablet-based administration to ensure confidentiality
- Utilize skip logic to display relevant questions based on responses
- Automatically generate scores in youth-friendly format immediately after completion
- Classify patients into no-to-low or moderate-to-high need categories for clinical intervention
Stakeholder Engagement
- Conduct focus groups with youth (n=8) via Zoom to gather feedback on assessment
- Ensure representation across diverse demographics (ages 12-17, multiple states)
- Facilitate discussion of content coverage, format, verbiage, clarity, and length
- Collaborate iteratively with healthcare professionals serving adolescents
- Incorporate feedback from project advisory committee including youth representatives
Successful psychometric validation in SRH research requires specific methodological resources and approaches.
Table 3: Essential Research Reagents for Psychometric Validation
| Resource Category | Specific Tools/Techniques | Application in SRH Research |
|---|---|---|
| Statistical Software | R, SPSS, Mplus | Conduct factor analysis, ICC calculations, reliability testing |
| Reliability Analysis | Intraclass Correlation Coefficient (ICC), Cronbach's Alpha, Kappa Statistics | Quantify measurement consistency across raters and time [1] [2] |
| Validity Assessment | Exploratory/Confirmatory Factor Analysis, Principal Component Analysis | Establish construct validity, examine dimensionality [2] [5] |
| Participant Engagement | Financial incentives (e.g., $25 gift cards), Multiple contact methods, Trusted adult contacts | Maintain high response rates in longitudinal SRH studies [6] |
| Cross-cultural Adaptation | Translation/back-translation, Cognitive interviewing, Measurement invariance testing | Ensure equivalence of SRH instruments across cultural contexts [1] |
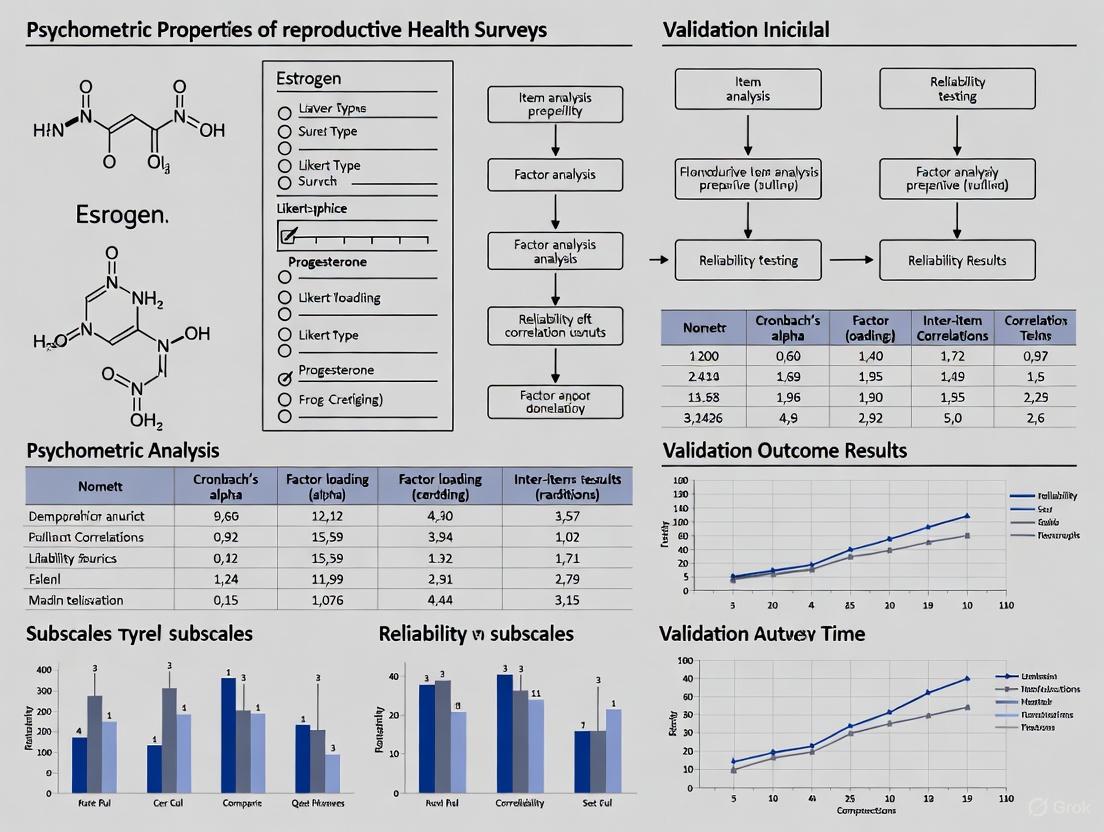
The following diagram illustrates the comprehensive workflow for developing and validating SRH instruments:
In reproductive health survey research, rigorous attention to psychometric properties is not merely methodological refinement but an ethical imperative. The sensitive nature of SRH data, coupled with the profound implications for policy and clinical practice, demands instruments of the highest scientific quality. As the field evolves toward more person-centered measurement approaches—exemplified by innovations such as the "unmet demand" contraceptive need metric—the fundamental requirements for validity, reliability, and responsiveness remain cornerstones of scientific rigor [3]. By adhering to comprehensive validation protocols, employing appropriate statistical methodologies, and actively engaging target populations throughout the development process, SRH researchers can ensure their measurement tools generate the trustworthy evidence necessary to advance sexual and reproductive health and rights globally.
This technical guide provides researchers and drug development professionals with an in-depth analysis of three fundamental psychometric indicators—Cronbach's alpha, Intraclass Correlation Coefficient (ICC), and Factor Analysis—within the context of reproductive health survey research. Ensuring the reliability and validity of assessment tools is paramount in producing scientifically rigorous and clinically meaningful data. This whitepaper delineates the theoretical underpinnings, calculation methodologies, interpretation guidelines, and application protocols for each indicator, supported by contemporary research examples and standardized data presentation tables to facilitate implementation in psychometric validation studies.
Reproductive health surveys are critical instruments for assessing sensitive constructs such as reproductive autonomy, sexual health, and patient-reported outcomes in clinical trials and public health interventions. The validity of conclusions drawn from these tools hinges on their psychometric properties, primarily reliability (consistency of measurement) and validity (accuracy in measuring the intended construct) [7] [8]. Within this framework, Cronbach's alpha serves as a key metric for internal consistency, the Intraclass Correlation Coefficient (ICC) evaluates score stability over time or across raters, and factor analysis provides evidence for the underlying structural validity. These indicators are not standalone metrics but interconnected components of a comprehensive validation strategy, particularly crucial when adapting existing scales for new populations or developing novel instruments for specific clinical groups, such as women with premature ovarian insufficiency or other reproductive health conditions [9] [10].
Cronbach's Alpha: Assessing Internal Consistency
Theoretical Foundation and Calculation
Cronbach's alpha (α) is a coefficient of internal consistency that estimates how closely related a set of items are as a group [11] [12]. It is founded on the concept that items designed to measure the same underlying construct should produce similar scores. The coefficient is calculated as a function of the number of test items and the average inter-correlation among these items.
The standard formula for Cronbach's alpha is: [ \alpha = \frac{N \bar{c}}{\bar{v} + (N-1) \bar{c}} ] Where:
- ( N ) = number of items
- ( \bar{c} ) = average inter-item covariance
- ( \bar{v} ) = average variance [11]
Alpha can also be conceptualized as the average of all possible split-half reliabilities within an instrument [13]. Higher alpha values indicate greater internal consistency, with values closer to 1.0 suggesting that the items reliably measure the same underlying construct.
Interpretation Guidelines and Application
Established benchmarks for interpreting Cronbach's alpha are detailed in Table 1. These thresholds provide researchers with standardized criteria for evaluating the internal consistency of their instruments.
Table 1: Interpretation Guidelines for Cronbach's Alpha
| Alpha Value Range | Interpretation | Recommendation |
|---|---|---|
| < 0.50 | Unacceptable | Revise or discard the scale |
| 0.51 - 0.60 | Poor | Substantial revision needed |
| 0.61 - 0.70 | Questionable | May require item modification |
| 0.71 - 0.80 | Acceptable | Appropriate for research use |
| 0.81 - 0.90 | Good | Good internal consistency |
| 0.91 - 0.95 | Excellent | Possible item redundancy |
| > 0.95 | Potentially problematic | Likely item redundancy [7] [8] |
In reproductive health research, Cronbach's alpha has been successfully employed to validate key instruments. For instance, the Reproductive Autonomy Scale (RAS) demonstrated good internal consistency with a Cronbach's α of 0.75 in a UK validation study [9]. Similarly, the Sexual and Reproductive Health Assessment Scale for women with Premature Ovarian Insufficiency (SRH-POI) showed strong internal consistency with α = 0.884 [10].
Experimental Protocol for Assessing Internal Consistency
Objective: To determine the internal consistency of a multi-item reproductive health survey instrument.
Materials and Software Requirements:
- Dataset containing respondent scores for all items
- Statistical software (e.g., SPSS, R, Stata)
- Documentation of the instrument's theoretical construct
Procedure:
- Data Preparation: Compile respondent data in a structured format with rows representing participants and columns representing item scores.
- Preliminary Checks: Ensure all items are measured on the same scale and coded consistently.
- Software Analysis:
- In SPSS: Navigate to
Analyze > Scale > Reliability Analysis - Select all target items for the scale
- In the
Statisticsdialog, selectInter-item Correlations[7]
- In SPSS: Navigate to
- Output Interpretation:
- Record the overall Cronbach's alpha value
- Examine "alpha if item deleted" statistics to identify problematic items
- Review inter-item correlation matrix (optimal range: 0.15-0.50) [12]
Troubleshooting:
- If alpha is unacceptably low (<0.70), examine items with low item-total correlations (<0.30) for potential revision or removal
- If alpha is excessively high (>0.95), check for redundant items with nearly identical wording or content
Figure 1: Cronbach's Alpha Assessment Workflow
Limitations and Considerations
While Cronbach's alpha is widely used, several limitations warrant consideration:
- Sensitivity to Scale Length: Alpha tends to increase with more items, potentially inflating reliability estimates for longer scales [8]
- Dimensionality Assumption: Alpha assumes unidimensionality but cannot confirm it; high alpha doesn't guarantee the scale measures a single construct [8]
- Tau-Equivalence: Alpha requires items to measure the same construct on the same scale; violations can lead to reliability underestimation [8]
Intraclass Correlation Coefficient (ICC): Evaluating Reliability
Theoretical Foundations and ICC Forms
The Intraclass Correlation Coefficient (ICC) is a versatile reliability statistic used to assess consistency or agreement between measurements, particularly in test-retest, inter-rater, and intra-rater reliability analyses [14] [7]. Unlike Pearson's correlation, which only measures linear relationship, ICC incorporates both correlation and agreement, making it more appropriate for reliability assessment [14].
ICC calculations are based on variance components derived from analysis of variance (ANOVA): [ ICC = \frac{\sigma{\alpha}^{2}}{\sigma{\alpha}^{2} + \sigma_{\varepsilon}^{2}} ] Where:
- (\sigma_{\alpha}^{2}) = variance between subjects (true variance)
- (\sigma_{\varepsilon}^{2}) = variance within subjects (error variance) [15]
McGraw and Wong defined 10 forms of ICC based on three key considerations, outlined in Table 2.
Table 2: Selection Framework for ICC Forms
| Selection Factor | Options | Appropriate ICC Form |
|---|---|---|
| Model | One-way random effects | Different raters for each subject |
| Two-way random effects | Raters randomly selected from population | |
| Two-way mixed effects | Specific raters of interest only | |
| Type | Single rater/measurement | Reliability of typical single rater |
| Mean of k raters/measurements | Reliability of averaged ratings | |
| Definition | Consistency | Relative agreement allowing additive differences |
| Absolute agreement | Exact score agreement required [14] |
Interpretation Guidelines and Application
ICC values are interpreted using standardized benchmarks that indicate the degree of reliability, as shown in Table 3.
Table 3: ICC Interpretation Guidelines
| ICC Value Range | Interpretation | Application Context |
|---|---|---|
| < 0.50 | Poor | Unacceptable for clinical or research use |
| 0.50 - 0.75 | Moderate | Acceptable for group-level comparisons |
| 0.76 - 0.90 | Good | Suitable for individual-level assessment |
| > 0.90 | Excellent | Ideal for high-stakes clinical decision making [14] [7] |
In reproductive health research, ICC has been effectively implemented for test-retest reliability assessment. The UK validation of the Reproductive Autonomy Scale reported "fair-good" test-retest reliability with an ICC of 0.67 [9]. The SRH-POI instrument demonstrated excellent temporal stability with an ICC of 0.95 for the entire scale [10].
Experimental Protocol for Test-Retest Reliability Using ICC
Objective: To evaluate the stability of a reproductive health survey instrument over time.
Materials and Software Requirements:
- Validated survey instrument
- Participant cohort representative of target population
- Statistical software with ANOVA and ICC capabilities
Procedure:
- Study Design:
- Administer the instrument to participants at time point 1 (T1)
- Schedule follow-up administration at time point 2 (T2)
- Determine appropriate interval based on construct stability (typically 1-4 weeks for reproductive health attitudes) [7]
- Data Collection:
- Ensure consistent administration conditions
- Maintain identical instrument format and instructions
- Statistical Analysis:
- In SPSS:
Analyze > Scale > Reliability Analysis - Select both time points as items
- In
Statistics, selectIntraclass Correlation Coefficient - Choose appropriate model based on study design [7]
- In SPSS:
- Model Selection Guidance:
- For test-retest: Two-way mixed effects, absolute agreement, single rater (ICC(3,1))
- For inter-rater with random raters: Two-way random effects, absolute agreement, single rater (ICC(2,1))
Reporting Standards:
- Specify the ICC model, type, and definition used
- Report 95% confidence intervals for ICC estimates
- Include both single-measure and average-measure ICC when appropriate
Figure 2: ICC Assessment Workflow for Test-Retest Reliability
Common Pitfalls and Solutions
- Inappropriate Time Interval: Too short may introduce memory effects; too long may capture genuine construct change
- Incorrect Model Selection: Carefully consider whether raters are random or fixed effects based on research question
- Ignoring Context: Clinical decision-making requires higher ICC thresholds (>0.90) than group-level research (>0.70)
Factor Analysis: Establishing Structural Validity
Theoretical Foundations and Types
Factor analysis is a multivariate statistical method used to identify the latent constructs (factors) that explain the pattern of correlations within a set of observed variables [16]. In scale development, it serves to verify the hypothesized structure of an instrument and provide evidence for construct validity.
The fundamental factor analysis model represents each observed variable as a linear combination of underlying factors: [ Xi = \lambda{i1}F1 + \lambda{i2}F2 + ... + \lambda{im}Fm + \varepsiloni ] Where:
- ( X_i ) = observed variable i
- ( \lambda_{ij} ) = factor loading of variable i on factor j
- ( F_j ) = latent factor j
- ( \varepsilon_i ) = unique variance (measurement error) [16]
Two primary approaches to factor analysis are employed in psychometric validation:
- Exploratory Factor Analysis (EFA): Used when the underlying factor structure is unknown or not well-established
- Confirmatory Factor Analysis (CFA): Used to test a pre-specified factor structure based on theory or previous research [16]
Key Concepts and Interpretation
Factor Loadings: Correlation coefficients between observed variables and latent factors, with absolute values >0.4 generally considered meaningful [16]
Eigenvalues: Represent the amount of variance explained by each factor, with values >1.0 indicating factors that explain more variance than a single observed variable (Kaiser's criterion) [16]
Kaiser-Meyer-Olkin (KMO) Measure: Assesses sampling adequacy, with values >0.80 considered meritorious for factor analysis
In reproductive health research, factor analysis has been instrumental in validating instrument structure. The SRH-POI scale development employed EFA, reporting KMO=0.83 and a significant Bartlett's test of sphericity, ultimately confirming a 4-factor structure with 30 items [10].
Experimental Protocol for Confirmatory Factor Analysis
Objective: To verify the hypothesized factor structure of a reproductive health measurement instrument.
Materials and Software Requirements:
- Complete dataset from instrument administration
- Statistical software with CFA capabilities (e.g., SPSS Amos, R lavaan, Mplus)
- A priori hypothesized factor model based on theory or EFA
Procedure:
- Data Screening:
- Check for multivariate normality and outliers
- Assess missing data patterns
- Verify adequate sample size (minimum 10:1 participant to variable ratio) [16]
- Model Specification:
- Define latent factors based on theoretical constructs
- Specify which items load on which factors
- Allow correlation between factors unless theoretical justification exists for orthogonality
- Model Estimation:
- Use Maximum Likelihood estimation for continuous data
- Assess model fit using multiple indices (see Table 4)
- Model Evaluation and Modification:
- Examine factor loadings for statistical and practical significance
- Review modification indices for potential model improvements
- Test alternative nested models if theoretically justified
Table 4: CFA Model Fit Indices and Interpretation
| Fit Index | Excellent Fit | Acceptable Fit | Calculation/Notes |
|---|---|---|---|
| χ²/df | < 2 | < 3 | Sensitive to sample size |
| CFI | > 0.95 | > 0.90 | Compares to null model |
| TLI | > 0.95 | > 0.90 | Less sensitive to model complexity |
| RMSEA | < 0.05 | < 0.08 | Penalizes model complexity |
| SRMR | < 0.05 | < 0.08 | Standardized residual mean |
Application in Reproductive Health Research
The three-factor structure of the Reproductive Autonomy Scale was confirmed using CFA in its UK validation, providing robust evidence for its structural validity [9]. Similarly, the SRH-POI instrument development employed factor analysis to refine an initial 84-item pool down to a concise 30-item scale with clear factor structure [10].
Figure 3: Factor Analysis Decision Workflow
Integrated Application in Reproductive Health Research
Sequential Validation Framework
A comprehensive psychometric validation follows a logical sequence where each indicator informs the next, creating a robust chain of evidence for instrument quality. Figure 4 illustrates this integrated approach.
Figure 4: Sequential Psychometric Validation Framework
Table 5: Essential Methodological Components for Psychometric Validation
| Component | Function | Implementation Example |
|---|---|---|
| Statistical Software | Data analysis and psychometric calculations | SPSS Reliability Analysis module for Cronbach's alpha and ICC [11] [7] |
| Participant Cohort | Source of response data for validation | Representative sample of target population (e.g., women of reproductive age for RAS validation) [9] |
| Validated Reference Instruments | Establishing convergent validity | Well-validated measures of related constructs for correlation analysis |
| Documentation Protocol | Ensuring methodological transparency | Detailed recording of model specifications, ICC forms, and factor rotation methods |
Case Example: Reproductive Autonomy Scale Validation
The UK validation of the Reproductive Autonomy Scale exemplifies the integrated application of these psychometric indicators [9]:
- Internal Consistency: Cronbach's α = 0.75 demonstrated acceptable reliability
- Factor Structure: Confirmatory factor analysis confirmed the hypothesized three-factor structure
- Test-Retest Reliability: ICC = 0.67 indicated fair-good temporal stability
- Construct Validity: Hypothesis testing confirmed that women wanting to avoid pregnancy with higher reproductive autonomy scores were more likely to use contraception
This comprehensive validation approach supported the RAS as a scientifically sound tool for research, clinical practice, and policy development in reproductive health.
Cronbach's alpha, ICC, and factor analysis constitute essential indicators of a robust psychometric instrument in reproductive health research. When applied systematically and interpreted according to established guidelines, these statistical tools provide compelling evidence for the reliability and validity of assessment instruments. The integrated application of these methods, as demonstrated in contemporary reproductive health research, ensures that resulting data are scientifically rigorous and clinically meaningful. Future directions in psychometric validation may incorporate more advanced statistical approaches, but these fundamental indicators will continue to form the cornerstone of instrument validation in reproductive health survey research.
The Critical Role of Content Validity in Culturally-Sensitive Contexts
In the field of reproductive health research, the psychometric properties of survey instruments fundamentally determine the quality and applicability of collected data. Among these properties, content validity—the degree to which an instrument adequately covers the target construct—is paramount, particularly when researching culturally diverse populations. Without strong content validity, even statistically reliable measures may fail to capture culturally-specific manifestations of health phenomena, leading to flawed conclusions and ineffective interventions. This technical guide examines the critical role of content validity within culturally-sensitive research contexts, providing methodological frameworks and experimental protocols essential for researchers, scientists, and drug development professionals working in global reproductive health.
The development of the MatCODE and MatER tools for assessing Spanish women's knowledge of healthcare rights and perception of resource scarcity during maternity exemplifies rigorous content validation. These instruments underwent systematic expert evaluation using Aiken's V coefficient and content validity index (CVI), achieving values >0.80, thus establishing robust content validity before field implementation [17]. Similarly, when adapting the Cultural Formulation Interview (CFI) for Iranian populations, researchers identified varying content validity ratios across cultural domains, with particularly challenging items in "cultural perception of the context" and "cultural factors affecting help-seeking" [18]. These cases underscore how cultural context directly influences what constitutes valid content across different populations.
Conceptual Foundations of Content Validity in Cultural Contexts
Defining Content Validity Beyond Linguistic Translation
Content validity in culturally-sensitive research extends far beyond simple linguistic translation of instruments. It requires conceptual equivalence—ensuring that constructs hold similar meaning and relevance across cultural contexts. For reproductive health surveys, concepts like "family planning," "sexual health," or "maternal well-being" may manifest differently across cultural frameworks, necessitating deep conceptual validation rather than superficial translation.
The cultural adaptation of the Cultural Awareness Scale (CAS) for Polish nursing students illustrates this comprehensive approach. Researchers followed WHO guidelines for cultural and linguistic adaptation, which included not just translation but also evaluation of conceptual relevance to the Polish healthcare context [19]. This process recognized that cultural competence components might carry different weights and manifestations in Poland's specific multicultural landscape, particularly following increased migration from Ukraine and other countries.
Theoretical Frameworks for Cultural Validity
Several theoretical frameworks inform content validation in culturally-sensitive research. The Campinha-Bacote model of cultural competence, which conceptualizes cultural awareness, knowledge, skills, encounters, and desire as interconnected components, provided the theoretical foundation for the Cultural Awareness Scale [19]. This model emphasizes that content validity must address multiple dimensions of cultural experience rather than treating culture as a monolithic variable.
Similarly, the person-centered maternity care framework underpinning the MatCODE instrument recognizes that women's participation and evaluation of their needs are essential components of maternity care quality [17]. This framework necessitated including items that captured culturally-specific expressions of autonomy and rights within Spanish healthcare settings, demonstrating how theoretical orientation directly shapes content validity requirements.
Methodological Protocols for Establishing Content Validity
Expert Panel Evaluation Protocols
Systematic expert evaluation constitutes the cornerstone of establishing content validity in culturally-sensitive instruments. The following table summarizes quantitative benchmarks from recent reproductive health validation studies:
Table 1: Content Validity Benchmarks in Reproductive Health Instrument Development
| Instrument | Cultural Context | Validation Metric | Result | Reference Standard |
|---|---|---|---|---|
| MatCODE/MatER | Spanish maternity care | Aiken's V | >0.80 | Excellent validity [17] |
| WSW-RHQ | Iranian shift workers | CVR | >0.64 | Acceptable [20] |
| Fertility Knowledge Inventories | Iranian couples | CVI | 0.90-0.95 | Excellent [21] |
| Cultural Formulation Interview | Iranian population | CVI | 0.51 | Requires improvement [18] |
| Sexual Health Questionnaire | Adolescents | Construct Validity | 68.25% variance | Robust [22] |
Expert Recruitment and Composition
Expert panels must demonstrate both methodological expertise and cultural representativeness. The validation of the Women Shift Workers' Reproductive Health Questionnaire involved twelve experts from midwifery, gynecology, and occupational health, ensuring multidisciplinary perspective on reproductive health content [20]. Similarly, the Cultural Formulation Interview validation employed a diverse panel including psychiatrists, psychologists, sociologists, social workers, and even patients to capture multiple dimensions of cultural validity [18].
The composition of expert panels should reflect the cultural ecosystems in which instruments will be deployed. For the Polish Cultural Awareness Scale adaptation, experts needed understanding of both nursing education standards and Poland's specific multicultural context, particularly regarding Ukrainian migrant populations [19].
Quantitative Evaluation Procedures
The content validity index (CVI) calculation follows specific methodological protocols. For each item, experts rate relevance on a 4-point scale (1=not relevant, 4=highly relevant). The CVI is calculated as the number of experts rating the item 3 or 4, divided by the total number of experts. The universal agreement CVI (UA-CVI) calculates the proportion of items rated 3 or 4 by all experts [17].
Aiken's V coefficient provides another quantitative approach, particularly useful for smaller expert panels. This statistic quantifies the agreement among experts regarding an item's relevance, clarity, and coherence, with values >0.80 indicating strong content validity [17].
Table 2: Experimental Parameters for Content Validity Assessment
| Parameter | Calculation Method | Interpretation Threshold | Application Context |
|---|---|---|---|
| Content Validity Index (CVI) | Proportion of experts giving rating ≥3 | ≥0.78 per item; ≥0.90 overall | Item-level relevance assessment |
| Aiken's V | V = (Σ(r - lo)/(n(c - lo)) | >0.80 acceptable | Small expert panels (3-5 experts) |
| Content Validity Ratio (CVR) | CVR = (ne - N/2)/(N/2) | ≥0.62 for 10 experts | Essentiality assessment |
| Kappa Coefficient | (I-CVI - pc)/(1 - pc) | >0.74 excellent | Chance-corrected agreement |
Target Population Engagement Protocols
Content validity requires participant feedback on instrument comprehensibility, relevance, and cultural appropriateness. The MatCODE validation employed a pilot cohort of 27 women who assessed the understandability of questionnaires using the INFLESZ scale, a validated Spanish tool for evaluating text readability [17]. This demonstrated semantic understanding at the target population level before full-scale deployment.
The development of a sexual and reproductive health needs assessment for married adolescent women in Iran involved in-depth interviews with 34 married adolescent women and four key informants during item generation [23]. This qualitative exploration ensured that items reflected the lived experiences and specific needs of this unique population, whose SRH needs differ from both adult women and unmarried adolescents.
Experimental Workflow for Cultural Validation
The following diagram illustrates the comprehensive workflow for establishing content validity in culturally-sensitive instruments:
The Researcher's Toolkit: Essential Methodological Reagents
Table 3: Research Reagent Solutions for Content Validation Studies
| Reagent Category | Specific Tools | Primary Function | Application Example |
|---|---|---|---|
| Expert Assessment Tools | Aiken's V Calculator, CVI Spreadsheet | Quantifying expert agreement on item relevance | MatCODE validation achieving Aiken's V >0.80 [17] |
| Readability Instruments | INFLESZ Scale, Flesch-Kincaid Tests | Assessing comprehensibility for target population | Spanish maternity tool testing with INFLESZ [17] |
| Qualitative Analysis Frameworks | Thematic Analysis, Content Analysis | Identifying culturally-specific constructs | Married adolescent women SRH needs assessment [23] |
| Psychometric Validation Software | R psych package, SPSS FACTOR, Mplus | Conducting factor analysis and reliability testing | Female Fertility Knowledge Inventory validation [21] |
| Cross-Cultural Adaptation Guidelines | WHO Translation Guidelines, COSMIN Checklist | Standardizing cultural adaptation process | Polish CAS adaptation following WHO protocols [19] |
Advanced Considerations in Cultural Validation
Addressing Measurement Invariances
Advanced content validation must consider measurement invariance—whether instruments function equivalently across cultural subgroups. The rapid review of sexual health knowledge tools for adolescents found inconsistent attention to measurement invariance, with only 5 of 14 studies addressing hypothesis testing about group differences [22] [24]. Establishing content validity prerequisites subsequent tests of measurement invariance through multi-group confirmatory factor analysis.
Navigating Cultural Paradoxes in Instrument Design
Cultural validation sometimes reveals paradoxical requirements where instruments must balance seemingly contradictory attributes. The Cultural Sensibility Scale for Nursing (CUSNUR) needed to assess both universal nursing competencies and culture-specific adaptations, requiring items that captured this nuanced balance [25]. Similarly, reproductive health surveys must often navigate tensions between standardized measurement (enabling cross-cultural comparison) and cultural specificity (ensuring local relevance).
Content validity represents the foundational psychometric property without which other measurement properties become irrelevant, particularly in culturally-sensitive reproductive health research. The methodologies and protocols outlined in this technical guide provide researchers with evidence-based approaches for establishing robust content validity across cultural contexts. As global reproductive health challenges require increasingly sophisticated measurement approaches, the rigorous cultural validation of research instruments will remain essential for generating meaningful data, developing effective interventions, and advancing equitable health outcomes across diverse populations. Future directions should emphasize mixed-methods validation approaches that integrate quantitative metrics with qualitative insights, and dynamic validation frameworks that recognize cultural contexts as evolving rather than static.
Within the critical field of reproductive health research, the development and validation of robust measurement instruments are foundational to generating reliable evidence. This technical guide provides researchers and drug development professionals with a comprehensive framework for establishing construct validity—a core psychometric property. Grounded in the context of reproductive health survey research, this whitepaper delineates a systematic pathway from theoretical conceptualization to quantitative measurement validation. Through detailed protocols, structured data presentation, and visual workflows, we equip scientists with practical methodologies to ensure their instruments accurately capture the complex, latent constructs inherent to sexual and reproductive health.
Theoretical Foundations of Construct Validity
In psychometrics, a construct is an abstract concept, characteristic, or variable that cannot be directly observed but is measured through indicators and manifestations [26]. In reproductive health research, quintessential constructs include reproductive autonomy, sexual assertiveness, and health service-seeking behavior.
Construct validity is the degree to which an instrument truly measures the theoretical construct it purports to measure [26] [27] [28]. It is not a single test but an ongoing process of accumulating evidence to support the inference that a test score accurately represents the intended construct. This is paramount in reproductive health, where constructs are often sensitive, multi-faceted, and heavily influenced by socio-cultural norms. For instance, measuring "reproductive autonomy" requires ensuring a scale captures a person's control over contraceptive use and childbearing, rather than their general assertiveness or knowledge [9].
Within a broader validation framework, construct validity is supported by other validity types, each providing a unique form of evidence (See Table 1).
Table 1: Types of Validity Evidence in Psychometric Research
| Validity Type | Definition | Key Question | Common Assessment Method |
|---|---|---|---|
| Construct Validity | The extent to which a test measures the theoretical construct it is intended to measure [26]. | Does this test measure the concept of interest? | Hypothesis testing, Factor Analysis [9] [29]. |
| Content Validity | The degree to which a test is systematically representative of the entire domain of the construct [26] [27]. | Does the test fully cover all relevant aspects of the construct? | Expert panel review (CVI, CVR) [29] [20]. |
| Face Validity | A subjective judgment of whether the test appears to measure what it claims to [26] [27]. | Does the test look like it measures the construct? | Informal review by target population or experts. |
| Criterion Validity | The extent to which test scores correlate with an external "gold standard" measure of the same construct [26] [28]. | Do the results correspond to a known standard? | Correlation analysis (e.g., Pearson's r) with a benchmark. |
Methodological Pathways for Establishing Construct Validity
Establishing construct validity is a multi-stage process that integrates qualitative and quantitative methodologies. The following workflow and subsequent protocols outline a comprehensive approach.
Figure 1: A Sequential Workflow for Establishing Construct Validity in Instrument Development.
Phase 1: Content and Face Validity Assessment
Objective: To ensure the initial item pool is relevant, representative, and clear to the target population.
Experimental Protocol:
Expert Panel Review (Content Validity):
- Participants: Assemble a panel of 8-12 experts in the field (e.g., reproductive health, psychometrics, clinical medicine) [20].
- Procedure: Experts evaluate each item for relevance, clarity, and comprehensiveness using a structured form.
- Quantitative Metrics:
- Content Validity Ratio (CVR): Assesses the essentiality of each item. Lawshe's table provides minimum values (e.g., 0.62 for 10 experts) [29].
- Content Validity Index (CVI): Measures the proportion of experts agreeing on an item's relevance. An item-level CVI (I-CVI) ≥ 0.78 is acceptable, and the scale-level average (S-CVI) should be ≥ 0.90 [29] [20].
- Outcome: Items with poor metrics are revised or discarded.
Target Population Review (Face Validity):
- Participants: A small sample (e.g., n=10) from the intended study population [30] [20].
- Procedure: Participants complete the draft scale and are interviewed about the clarity, difficulty, and appropriateness of each item.
- Quantitative Metric: Item Impact Score is calculated to identify items with low perceived importance [29] [20].
- Outcome: Wording is refined for clarity and cultural appropriateness.
Phase 2: Pilot Testing and Item Analysis
Objective: To refine the scale using statistical methods on a preliminary dataset.
Protocol:
- Sample: Administer the scale to a small but sufficient sample (typically 50-100 participants) [20].
- Analysis: Conduct item analysis to calculate:
- Item-Total Correlation: The correlation between each item and the total scale score. Values below 0.3 may indicate the item is not measuring the same construct [20].
- Inter-Item Correlation: The average correlation among all items.
- Cronbach's Alpha: A preliminary measure of internal consistency. A value > 0.7 is generally desired for group-level analysis [20].
Phase 3: Construct Validity Assessment via Factor Analysis
This is the core quantitative phase for evaluating construct validity.
Protocol 1: Exploratory Factor Analysis (EFA)
- Objective: To uncover the underlying factor structure of the scale without pre-defined constraints.
- Sample Size: A minimum of 5-10 participants per item is a common rule of thumb [20].
- Procedure:
- Sampling Adequacy: Check the Kaiser-Meyer-Olkin (KMO) measure; a value > 0.8 is good [20]. Bartlett's Test of Sphericity should be significant (p < .05).
- Factor Extraction: Use Principal Component Analysis or Maximum Likelihood estimation.
- Factor Retention: Determine the number of factors using eigenvalues > 1.0 and scree plot inspection.
- Rotation: Apply an orthogonal (e.g., Varimax) or oblique (e.g., Promax) rotation to simplify the factor structure and enhance interpretability.
- Interpretation: Items with factor loadings > |0.4|–|0.5| are typically considered to load significantly on a factor. The resulting factors should align with the theoretical dimensions of the construct.
Protocol 2: Confirmatory Factor Analysis (CFA)
- Objective: To statistically test how well the pre-specified factor structure (e.g., from EFA or theory) fits the observed data.
- Sample: A new, independent sample is ideal.
- Procedure: The hypothesized model is tested using structural equation modeling.
- Model Fit Indices: Assess fit using multiple indices [20]:
- Chi-Square/df (CMIN/DF): < 3.0 indicates good fit.
- Comparative Fit Index (CFI): > 0.90 (preferably > 0.95).
- Root Mean Square Error of Approximation (RMSEA): < 0.08 (preferably < 0.06).
- Outcome: A well-fitting model provides strong evidence for the construct validity of the proposed factor structure.
Phase 4: Reliability and Stability Assessment
Objective: To establish the consistency and reproducibility of the scale scores.
Protocol:
- Internal Consistency: Calculate Cronbach's alpha for the total scale and its subscales. A value between 0.70 and 0.95 is generally considered acceptable, indicating that the items are consistently measuring the same construct [31] [27] [28].
- Test-Retest Reliability:
Applied Case Studies in Reproductive Health Research
The following table summarizes how the aforementioned protocols have been successfully implemented to establish construct validity in recent reproductive health research.
Table 2: Case Studies of Construct Validity Establishment in Reproductive Health Instrument Development
| Instrument / Study | Target Population | Factor Analysis Method & Results | Reliability Metrics | Key Validity Evidence |
|---|---|---|---|---|
| Reproductive Autonomy Scale (RAS) for use in the UK [9] | Women of reproductive age, UK | Confirmatory Factor Analysis (CFA): Confirmed the original 3-factor structure from the US version. | Cronbach's α: 0.75Test-Retest ICC: 0.67 | Hypothesis Testing: Confirmed that women wanting to avoid pregnancy but with higher RAS scores were more likely to use contraception. |
| Women Shift Workers’ Reproductive Health Questionnaire (WSW-RHQ) [20] | Women shift workers, Iran | EFA & CFA: EFA revealed a 5-factor structure (34 items) explaining 56.5% of variance. CFA confirmed the model fit (CFI, RMSEA, etc.). | Cronbach's α: > 0.70Composite Reliability: > 0.70 | Content and face validity were rigorously established via expert panels and target population interviews. |
| Reproductive Health Needs of Violated Women Scale [30] | Women subjected to domestic violence, Iran | Exploratory Factor Analysis (EFA): Revealed a 4-factor structure (39 items) explaining 47.62% of total variance. | Cronbach's α: 0.94 (total scale)ICC: 0.98 (total scale) | Item generation was informed by a prior qualitative study, ensuring grounding in lived experience. |
| Sexual and Reproductive Health Service Seeking Scale (SRHSSS) [5] | Young adults, Turkey | Exploratory Factor Analysis (EFA): A 4-factor structure (23 items) was obtained, explaining 89.45% of the variance. | Cronbach's α: 0.90 | The scale development included focus group interviews and expert evaluation to ensure content validity. |
The Scientist's Toolkit: Essential Reagents for Validation
Table 3: Key Methodological and Analytical Tools for Construct Validation
| Tool / Reagent | Function in Validation Process | Application Notes |
|---|---|---|
| Expert Panel | To provide evidence for content validity by judging item relevance and representativeness. | Should include methodologies and subject-matter experts (e.g., clinicians, community health experts) [20]. |
| Target Population Sample | To assess face validity, ensure cultural appropriateness, and pilot test the instrument. | Crucial for ensuring questions are understood and relevant to those with lived experience [30]. |
| Statistical Software (e.g., R, SPSS, Mplus) | To perform quantitative psychometric analyses (EFA, CFA, reliability). | R and Mplus offer advanced SEM/CFA capabilities. SPSS is common for EFA and basic reliability analysis. |
| Kaiser-Meyer-Olkin (KMO) Measure | To sample adequacy for factor analysis; confirms the data is suitable for EFA/CFA. | Values > 0.8 are desirable; below 0.5 indicates inadequacy [20]. |
| Cronbach's Alpha (α) | To measure the internal consistency reliability of the scale and its subscales. | A necessary but insufficient condition for validity; values of 0.7-0.9 are typically targeted [31] [27]. |
| Intraclass Correlation Coefficient (ICC) | To quantify test-retest reliability and the stability of measurements over time. | Preferred over simple correlation for continuous data as it accounts for systematic bias [9]. |
Establishing construct validity is an iterative and evidence-driven process that bridges theoretical frameworks with empirical measurement. In reproductive health research, where constructs are complex and measurements have direct implications for clinical care and policy, rigorous validation is not merely methodological but an ethical imperative. By adhering to the sequential workflow—from theoretical definition and content validation through factor analysis and reliability testing—researchers can develop instruments that yield trustworthy and meaningful data. This, in turn, fortifies the scientific foundation upon which advancements in reproductive health outcomes are built.
The development of validated, population-specific assessment tools is a critical component of advancing sexual and reproductive health (SRH) research. Generic health measurement instruments often fail to capture the unique experiences and challenges faced by distinct patient populations, potentially overlooking critical aspects of their health status and quality of life. Within psychometric research, there is growing recognition that condition-specific and population-specific instruments provide more sensitive and clinically relevant measurements [10].
Recent methodological advances have demonstrated the importance of creating tailored instruments for vulnerable populations and those with specific health conditions. The psychometric properties of these tools—including validity, reliability, and sensitivity—are paramount for ensuring they produce scientifically sound data capable of detecting meaningful clinical changes and informing evidence-based interventions [10] [32] [29].
This technical guide examines the development and validation of reproductive health assessment scales across diverse populations, with particular focus on their psychometric properties and methodological considerations for researchers and drug development professionals.
Methodological Framework for Scale Development
The development of robust reproductive health assessment scales typically follows a structured mixed-methods approach that integrates both qualitative and quantitative research phases. The sequential exploratory design has emerged as a particularly effective methodology for this purpose, as implemented in recent studies developing scales for women with premature ovarian insufficiency (POI) and HIV-positive women [10] [29].
Core Development Phases
The instrument development process typically progresses through five methodical phases:
- Item Generation: Comprehensive literature review and qualitative studies (interviews, focus groups) to identify relevant concepts and create initial item pools [10] [29]
- Content and Face Validity Assessment: Expert evaluation and participant feedback to refine items for relevance, clarity, and appropriateness [10] [29]
- Pilot Testing and Item Analysis: Administration to a preliminary sample to identify problematic items and assess preliminary psychometric properties [10]
- Construct Validation: Statistical analyses, particularly exploratory factor analysis (EFA), to identify underlying dimensions and scale structure [10] [32] [29]
- Reliability Assessment: Evaluation of internal consistency and test-retest stability [10] [29]
Psychometric Evaluation Metrics
Rigorous psychometric evaluation employs standardized metrics to establish measurement quality. The following table summarizes key psychometric parameters and their acceptable thresholds based on recent scale development studies:
Table 1: Key Psychometric Properties and Standards in Scale Development
| Psychometric Property | Assessment Method | Acceptable Threshold | Exemplary Findings |
|---|---|---|---|
| Content Validity | Content Validity Index (CVI) | ≥0.79 | CVI of 0.926 for SRH-POI scale [10] |
| Content Validity | Content Validity Ratio (CVR) | ≥0.62 (for 10 experts) | CVR based on Lawshe's table [29] |
| Face Validity | Impact Score | ≥1.5 | Qualitative assessment of difficulty, appropriateness, ambiguity [10] |
| Internal Consistency | Cronbach's Alpha | 0.70-0.95 | 0.884 for SRH-POI; 0.713 for HIV-specific scale [10] [29] |
| Test-Retest Reliability | Intraclass Correlation (ICC) | ≥0.70 | ICC of 0.95 for SRH-POI; 0.952 for HIV-specific scale [10] [29] |
| Sampling Adequacy | KMO Measure | ≥0.60 | KMO of 0.83 for SRH-POI factor analysis [10] |
| Construct Validity | Factor Loadings | ≥0.30 | Varimax rotation with loadings >0.3 considered acceptable [29] |
Population-Specific Scale Development: Case Studies
Reproductive Health Scale for Women with Premature Ovarian Insufficiency (POI)
The Sexual and Reproductive Health Assessment Scale for Women with POI (SRH-POI) exemplifies the rigorous development of a condition-specific instrument. POI affects 1-3% of women under 40 and presents significant physical, psychological, and sexual challenges that generic quality-of-life instruments fail to adequately capture [10].
Methodology: The development employed a sequential exploratory mixed-method design between 2019-2021. The initial phase generated an 84-item pool through literature review and qualitative studies. After face and content validity assessment, the pool was reduced to 41 items, with exploratory factor analysis finally yielding a 30-item instrument with a four-factor structure [10].
Psychometric Properties: The scale demonstrated excellent reliability (Cronbach's alpha = 0.884, ICC = 0.95) and strong content validity (S-CVI = 0.926). The factor analysis revealed a coherent structure accounting for significant variance in SRH experiences, with KMO sampling adequacy of 0.83 and Bartlett's test of sphericity confirming sufficient correlation between items for factor analysis [10].
Reproductive Health Assessment for HIV-Positive Women
The reproductive health scale for HIV-positive women addresses the unique challenges faced by this population, including disease-related concerns, life instability, coping with illness, disclosure status, responsible sexual behaviors, and need for self-management support [29].
Methodology: This study also employed an exploratory mixed-methods design with three phases: qualitative data collection through semi-structured interviews and focus groups (n=25), item pool generation, and psychometric evaluation. The initial 48-item pool was refined to a 36-item scale with six factors through content validity assessment and exploratory factor analysis [29].
Psychometric Properties: The instrument demonstrated good internal consistency (Cronbach's alpha = 0.713) and excellent test-retest reliability (ICC = 0.952). Content validity was established through both qualitative expert review and quantitative assessment (CVI, CVR) [29].
Mental Health Literacy Scale for Reproductive-Age Women
The Women's Reproductive Ages Mental Health Literacy Scale (WoRA-MHL) represents another application of these methodological principles, focusing on mental health literacy rather than direct health assessment [32].
Methodology: Following a similar mixed-method approach, the final 30-item instrument was organized across four themes: "Accessing and Obtaining Mental Health Information," "Understanding Mental Health Information," "Maintaining Mental Health," and "Adapting to the Challenges of Women's Lives." These factors collectively accounted for 54.42% of the total variance [32].
Psychometric Properties: Confirmatory factor analysis validated a satisfactory model fit, with reliability assessments showing strong internal consistency (Cronbach's alpha = 0.889) and excellent test-retest reliability (ICC = 0.966) [32].
Experimental Protocols and Methodological Workflows
The development of reproductive health scales follows standardized experimental protocols that ensure scientific rigor and reproducibility. The workflow below visualizes the key stages from conceptualization to final validation.
Diagram 1: Scale Development Workflow
Sample Recruitment and Data Collection Protocols
Robust sampling strategies are essential for developing valid assessment tools. Recent studies have employed various approaches:
- Targeted Sampling: For condition-specific scales (e.g., POI, HIV), participants are typically recruited from clinical settings or specialized patient registries to ensure the sample represents the target population [10] [29].
- Snowball Sampling: For hard-to-reach populations (e.g., refugees), snowball sampling with multiple starting points helps access diverse participants while acknowledging potential limitations in generalizability [33].
- Sample Size Considerations: Appropriate sample sizes are determined through power analysis, with typical participant numbers ranging from 25-50 for qualitative phases to several hundred for quantitative validation [10] [33] [29].
Data collection procedures emphasize standardized administration, private settings for sensitive topics, and trained interviewers who share language and cultural backgrounds with participants when working with vulnerable populations [33].
Quantitative Assessment in Diverse Populations
Specialized Applications in Vulnerable Groups
Assessment tools must be adapted for vulnerable populations with specific accessibility needs. Research with Syrian refugee young women in Lebanon demonstrates approaches to SRH assessment in humanitarian settings [33].
Methodology: A cross-sectional survey of 297 Syrian Arab and Kurdish participants aged 18-30 assessed SRH knowledge and access to services. The questionnaire was developed from validated tools (CDC Reproductive Health Assessment Toolkit, UNFPA Adolescent SRH Toolkit) and administered electronically in Arabic [33].
Findings: The study revealed significant knowledge gaps, with only 49.8% of participants aware of SRH service facilities in their area. Higher education and urban origin were associated with better SRH knowledge. The research developed an unweighted knowledge score assessing STIs, contraceptive methods, and pregnancy danger signs [33].
Advanced Statistical Modeling for Population Health Assessment
Statistical innovation enables estimation of reproductive health indicators when direct measurement is impractical. Recent research has developed modeling approaches for the Demand for Family Planning Satisfied (DFPS) indicator [34].
Methodological Approach: Using survey data from 1,099 subnational regions across 103 countries, researchers fitted least-squares regression models predicting DFPS based on contraceptive prevalence rates. A fractional polynomial approach accounted for non-linear relationships, with model performance evaluated through 5-fold cross-validation [34].
Statistical Models: The analysis produced two primary equations for DFPS by any method (DFPSany) and by modern methods (DFPSm). The models explained over 97% of variability, with minimal bias (approximately 0.1) in cross-validated samples [34].
Table 2: Statistical Models for Family Planning Indicators
| Indicator | Model Equation | Predictors | Variance Explained |
|---|---|---|---|
| DFPSany (Demand for Family Planning Satisfied by any method) | ( logit(DFPSany) = 1.05 + (log(CPRany)0.93) + (CPRany^22.49) + (cpdiff*0.70) ) | CPRany, Difference between CPRany and CPRm | >97% |
| DFPSm (Demand for Family Planning Satisfied by modern methods) | ( logit(DFPSm) = 1.12 + (log(CPRm)0.97) + (CPRm^22.13) + (cpdiff*-1.43) ) | CPRm, Difference between CPRany and CPRm | >97% |
The Researcher's Toolkit: Essential Methodological Components
The development and validation of reproductive health assessment scales requires specific methodological components that function as essential "research reagents" in the instrument development process.
Table 3: Essential Methodological Components for Scale Development
| Component | Function | Application Examples |
|---|---|---|
| Exploratory Factor Analysis (EFA) | Identifies underlying factor structure and reduces items to coherent domains | KMO=0.83 and Bartlett's significant test in POI scale [10] |
| Content Validity Index (CVI) | Quantifies expert agreement on item relevance and clarity | S-CVI of 0.926 for SRH-POI scale [10] |
| Content Validity Ratio (CVR) | Assesses essentiality of items based on expert panel evaluation | Lawshe's table minimum CVR of 0.62 for 10 experts [29] |
| Cronbach's Alpha | Measures internal consistency and inter-item correlation | α=0.884 for SRH-POI; α=0.713 for HIV-specific scale [10] [29] |
| Intraclass Correlation (ICC) | Evaluates test-retest reliability and temporal stability | ICC=0.95 for SRH-POI over 2-week interval [10] |
| Impact Score | Assesses item clarity and importance from participant perspective | Score ≥1.5 considered acceptable for item retention [10] |
| Varimax Rotation | Simplifies factor structure by maximizing variance of loadings | Orthogonal rotation with factor loadings >0.3 [29] |
The development of population-specific reproductive health assessment scales represents a methodological advancement in health services research and clinical trial design. The rigorous psychometric frameworks demonstrated across these case studies provide researchers with validated protocols for creating sensitive, reliable measurement tools.
The consistent finding across all studies is that condition-specific and population-specific instruments capture unique aspects of health experiences that generic tools miss. The strong psychometric properties of these scales—including high reliability coefficients, robust factor structures, and excellent content validity—support their utility in both clinical research and intervention evaluation.
Future directions in this field include cross-cultural validation of existing instruments, development of computerized adaptive testing versions to reduce respondent burden, and integration of these scales as endpoints in clinical trials of therapeutic interventions for reproductive health conditions.
From Theory to Practice: A Step-by-Step Guide to Scale Development and Deployment
Item generation is the foundational phase in creating a valid and reliable psychometric instrument. It involves the systematic creation of a comprehensive pool of questionnaire items that represent the entire theoretical domain of the construct being measured [35]. In reproductive health survey research, this process ensures the assessment tool adequately captures the multifaceted nature of sexual and reproductive health experiences, behaviors, and attitudes. The quality of this initial phase directly impacts all subsequent psychometric evaluations, including validity and reliability testing [10]. Without a robust item generation process, even sophisticated statistical analyses cannot compensate for content gaps or conceptual misalignment in the final instrument.
Within the broader context of psychometric property evaluation, item generation establishes the content validity foundation upon which other measurement properties (construct validity, criterion validity, internal consistency, and test-retest reliability) are later built [35] [36]. For reproductive health research specifically, this process must account for culturally sensitive topics, diverse population needs, and complex behavioral determinants that influence health outcomes [37] [38].
Methodological Approaches to Item Generation
Comprehensive Literature Review
A systematic literature review forms the scholarly foundation for item generation by identifying established constructs, measurement gaps, and existing terminology relevant to the target domain.
Protocol Implementation:
- Search Strategy Development: Define comprehensive search terms encompassing relevant reproductive health concepts (e.g., "reproductive autonomy," "contraceptive access," "sexual health communication") across multiple databases [10]. The SRH-POI scale development team searched SID, Scopus, PubMed, Google Scholar, and other databases spanning publications from 1950 to 2021 [10].
- Existing Instrument Analysis: Identify and evaluate previously developed instruments for potentially adaptable items while ensuring copyright compliance. For the Reproductive Autonomy Scale (RAS) adaptation in the UK, researchers analyzed the original US scale to maintain conceptual equivalence while ensuring cultural appropriateness [9].
- Conceptual Mapping: Synthesize findings into a conceptual framework that identifies core domains and subdomains of the construct. The SRH-POI scale development identified multiple dimensions through literature review before qualitative investigation [10].
Table 1: Literature Review Documentation Protocol
| Review Component | Documentation Element | Application Example |
|---|---|---|
| Search Parameters | Databases searched, date ranges, search terms | PubMed, Scopus, Web of Science (2010-2025) |
| Inclusion/Exclusion Criteria | Systematic criteria for source selection | Peer-reviewed articles, validated instruments, specific populations |
| Extracted Concepts | Thematic organization of findings | Reproductive decision-making, service access barriers, communication autonomy |
| Existing Items | Catalog of adaptable questionnaire items | 84-item pool generated for SRH-POI scale [10] |
Qualitative Research Methods
Qualitative research provides the lived-experience context that literature alone cannot capture, ensuring the item pool reflects the actual concerns, language, and conceptual frameworks of the target population.
Protocol Implementation:
- Participant Recruitment: Employ purposive sampling to ensure diverse representation across relevant demographics (age, socioeconomic status, geographic location, reproductive experiences) [38]. In a study exploring SRH service use in Ethiopia, researchers selected participants based on "age, educational level, and relationship status" to capture varied perspectives [38].
- Data Collection Techniques: Implement semi-structured interviews, focus group discussions, or observational methods to explore the construct domain. The DHS Program utilizes "focus group discussions, in-depth interviews, and personal narratives" to understand social and cultural contexts of reproductive health [39].
- Thematic Analysis: Employ systematic coding procedures to identify emergent themes and concepts using established qualitative methodology. Braun and Clarke's thematic analysis framework has been applied in reproductive health literature reviews to identify key themes across studies [37].
Implementation Considerations:
- Saturation Principle: Continue data collection until no new themes emerge from subsequent interviews or focus groups. In the Ethiopian SRH study, researchers used "data saturation" to determine when sufficient interviews had been conducted [38].
- Stakeholder Inclusion: Engage multiple perspectives, including healthcare providers and diverse patient populations, to capture comprehensive conceptualization. A study in Ethiopia included both adolescents (service users) and health professionals (service providers) to understand SRH service use from multiple angles [38].
Integration and Initial Item Pool Development
The integration phase synthesizes findings from both literature review and qualitative research to create a comprehensive preliminary item pool.
Concept Synthesis and Domain Specification
Systematically map identified concepts from both sources into coherent domains and subdomains that collectively represent the entire construct space. The Reproductive Autonomy Scale was structured around a confirmed "three-factor structure" identified through this synthetic process [9].
Protocol Implementation:
- Conceptual Matrix Development: Create a cross-walking framework that aligns literature-derived constructs with qualitative themes to identify coverage gaps and redundancies.
- Domain Specification: Define clear operational definitions for each domain to guide item creation. Reproductive health research often identifies domains such as "contraceptive use, childbearing preferences, and healthcare decision-making" [9].
- Item Conceptualization: Develop items that precisely map to each domain while using language and conceptual frameworks identified in qualitative research.
Table 2: Integration Framework for Reproductive Health Constructs
| Domain Identified | Literature Support | Qualitative Validation | Sample Item Stem |
|---|---|---|---|
| Contraceptive Decision-Making | Previous scales measuring reproductive autonomy [9] | Young women's reported experiences with provider interactions [38] | "I decide what contraceptive method to use..." |
| Healthcare Access Barriers | Documented structural barriers in marginalized populations [37] | Experiences of stigma and discrimination reported in interviews [38] | "I can get reproductive healthcare when..." |
| Relationship Communication | Sexual Assertiveness Scale items [9] | Partner dynamics described in focus groups [39] | "I feel comfortable discussing contraception with my partner..." |
| Service Provider Interactions | Power dynamics in clinical settings [9] | Youth reports of judgmental provider attitudes [38] | "My healthcare provider listens to my concerns about..." |
Item Formulation and Documentation
Transform identified concepts into preliminary questionnaire items using established item-writing principles to minimize bias and enhance comprehension.
Protocol Implementation:
- Item Writing: Develop clear, unambiguous items using appropriate response formats (e.g., Likert scales, frequency scales, binary responses). The SRH-POI scale used a "5-part Likert scale" for response options [10].
- Language Appropriation: Utilize terminology and phrasing identified during qualitative research to enhance cultural and contextual relevance. Research with underserved groups highlights the importance of using "accessible language" that reflects how participants conceptualize their experiences [37].
- Comprehensive Documentation: Maintain detailed records of each item's conceptual origin, development rationale, and corresponding domain.
Table 3: Research Reagent Solutions for Qualitative Item Generation
| Research 'Reagent' | Function in Item Generation | Application Example |
|---|---|---|
| Semi-Structured Interview Guides | Ensure systematic exploration of domain-relevant topics while allowing emergent themes | Guides with open-ended questions about reproductive healthcare experiences [38] |
| Focus Group Protocols | Facilitate group interaction to identify shared conceptual frameworks and terminology | Discussions exploring community norms around contraceptive use [39] |
| Digital Recorders & Transcription Services | Create verbatim records of qualitative data for systematic analysis | Audio recording of interviews with adolescents about SRH services [38] |
| Qualitative Data Analysis Software | Facilitite systematic coding and thematic analysis (e.g., NVivo, MAXQDA) | Software used to identify emergent themes across multiple interviews [37] |
| Conceptual Mapping Tools | Visualize relationships between concepts and domains during analysis | Diagrams linking themes like "stigma," "access," and "autonomy" in reproductive health |
| Systematic Review Databases | Identify established constructs and existing measures | PubMed, Scopus, PsycINFO searches for reproductive autonomy measures [9] [10] |
Quality Assurance in Item Generation
Implement systematic quality checks throughout the item generation process to ensure comprehensive content coverage and minimal construct-irrelevant variance.
Protocol Implementation:
- Expert Consultation: Engage content experts and methodological specialists to review the conceptual framework and item-domain alignment. The SRH-POI scale development involved asking "10 researchers and reproductive health experts" to provide input on the preliminary tool [10].
- Pilot Cognitive Testing: Conduct preliminary testing with target population members to assess item comprehensibility, sensitivity, and relevance. This process helps identify terminology that may be misunderstood or culturally inappropriate.
- Documentation Audit: Verify thorough documentation of all methodological decisions and item rationales to create an audit trail for subsequent validation phases.
The item generation phase culminates in a comprehensive item pool ready for formal content validation, where items undergo systematic evaluation by stakeholders and experts for relevance, comprehensiveness, and appropriateness before proceeding to quantitative psychometric evaluation. This rigorous approach to initial scale development establishes the foundation for instruments with strong content validity, enabling accurate measurement of complex reproductive health constructs across diverse populations [9] [10].
In the development of reproductive health surveys, establishing robust psychometric properties is paramount to ensuring that research data is valid, reliable, and actionable. Within this framework, content and face validity represent foundational validation stages that determine whether an instrument adequately measures the constructs it purports to measure. Content validity assesses the degree to which a scale's items comprehensively represent the target domain, while face validity evaluates whether the items appear appropriate to end users. For reproductive health research—where constructs like empowerment, coercion, and health behaviors are complex and multidimensional—these validation phases require systematic methodological approaches employing expert panels to leverage collective scientific judgment [40] [41].
The rigorous development of reproductive health scales, such as the Reproductive Autonomy Scale [9], the Reproductive Coercion Scale [41], and the Sexual and Reproductive Health Assessment Scale for women with Premature Ovarian Insufficiency [10], demonstrates that structured validity assessment is critical for producing instruments that yield scientifically sound results. This technical guide provides researchers with comprehensive methodologies for establishing content and face validity through expert panels, framed within the broader context of psychometric validation for reproductive health surveys.
Theoretical Foundation: Content and Face Validity in Context
Content and face validity represent distinct but complementary forms of measurement validity. Content validity provides objective evidence that a scale's content is representative, relevant, and comprehensive for the construct being measured, while face validity offers subjective evidence that the items appear meaningful and appropriate to respondents and practitioners [10] [29]. In reproductive health research, where sensitive topics including coercion, sexual behavior, and contraceptive use are frequently assessed, both forms of validity are essential for ensuring that instruments are both scientifically rigorous and acceptable to target populations.
The theoretical importance of content validation is evident across multiple reproductive health scale development studies. For instance, when developing the Reproductive Health Assessment Scale for HIV-Positive Women, researchers emphasized that "addressing the sexual and reproductive health needs of infected women can help them to gain self-confidence in having control over own sexual life that leads to improved participation in public health" [29]. This underscores how content relevance directly impacts both measurement quality and potential health outcomes. Similarly, a systematic review of women empowerment measures in reproductive health found that scales applying literature reviews, expert panels, or empirical methods to develop item pools produced more valid and reliable instruments [40].
Methodological Framework: Implementing Expert Panels
Expert Panel Composition and Recruitment
Constructing an appropriate expert panel requires strategic consideration of both domain expertise and stakeholder representation. The panel should include multidisciplinary specialists who collectively cover the full scope of the construct being measured.
Table 1: Recommended Expert Panel Composition for Reproductive Health Surveys
| Expertise Domain | Recommended Background | Primary Contribution | Example from Literature |
|---|---|---|---|
| Clinical/Medical | Obstetrician-gynecologists, reproductive endocrinologists, family planning clinicians | Ensure medical accuracy and clinical relevance | HIV specialists in reproductive health scale development [29] |
| Research Methodologists | Psychometricians, epidemiologists, survey methodologists | Address measurement properties and study design | Researchers with psychometric expertise in scale validation [40] |
| Content Specialists | Public health researchers, behavioral scientists, sociologists | Verify theoretical alignment and construct coverage | Chemical/environmental specialists in EDC reproductive health behavior survey [42] |
| Practice Experts | Counselors, patient advocates, community health workers | Assess practical utility and contextual appropriateness | Domestic violence advocates in Reproductive Coercion Scale refinement [41] |
| Target Population Representatives | Patients, community members with lived experience | Ensure relevance, comprehension, and cultural appropriateness | HIV-positive women in face validity assessment [29] |
Research indicates that panels of approximately 5-10 experts typically provide sufficient diversity of perspective while maintaining practical manageability. For example, in developing a reproductive health behavior survey for endocrine-disrupting chemicals, researchers engaged "five experts—including two chemical/environmental specialists, a physician, a nursing professor, and a Korean language expert" [42]. Similarly, in content validation of the Sexual and Reproductive Health Assessment Scale for women with Premature Ovarian Insufficiency (SRH-POI), ten experts were recruited to evaluate content validity [10].
Implementation Protocols for Content Validity Assessment
The content validation process employs both qualitative and quantitative methods to systematically evaluate each item's relevance and representation of the target construct.
Qualitative Content Validation Protocol
The qualitative assessment involves comprehensive expert evaluation of item clarity, relevance, and comprehensiveness through structured feedback mechanisms:
Structured Evaluation Framework: Provide experts with the conceptual definition of the construct and operational definitions of each domain, then ask them to evaluate:
- Relevance: Whether each item accurately reflects the construct domain it intends to measure
- Clarity: Whether item wording is unambiguous and easily understood
- Comprehensiveness: Whether the item set fully covers all aspects of the theoretical construct
- Cultural appropriateness: Whether items are sensitive to cultural norms and values
Systematic Feedback Collection: Utilize structured forms that allow experts to provide specific suggestions for item modification, addition, or deletion. In the development of the SRH-POI scale, researchers "asked 10 researchers and reproductive health experts, some of whom had a history of research and activity in the field of reproductive health of women suffering from POI, after carefully studying the tool, about observing the grammar, appropriateness of words, allocation of items in their proper place and appropriate scoring" [10].
Quantitative Content Validation Protocol
The quantitative assessment employs standardized metrics to statistically evaluate expert consensus on item relevance:
Content Validity Ratio (CVR): Assesses the essentiality of each item using Lawshe's formula:
- Procedure: Experts rate each item on a 3-point scale: "essential," "useful but not essential," or "not necessary"
- Calculation: CVR = (nₑ - N/2)/(N/2), where nₑ is the number of experts rating the item as "essential," and N is the total number of experts
- Threshold: The minimum acceptable CVR value depends on the number of experts (e.g., 0.62 for 10 experts) [10] [29]
Content Validity Index (CVI): Evaluases item quality in terms of clarity and relevance:
- Procedure: Experts rate each item on a 4-point Likert scale for simplicity, specificity, and clarity
- Item-CVI Calculation: The proportion of experts giving a rating of 3 or 4 for each item
- Scale-CVI Calculation: The average of I-CVI scores across all items
- Threshold: I-CVI > 0.79 is appropriate; 0.70-0.79 needs revision; <0.70 should be eliminated [29]
Table 2: Quantitative Content Validity Standards and Thresholds
| Metric | Calculation Method | Acceptability Threshold | Application in Reproductive Health Research |
|---|---|---|---|
| Content Validity Ratio (CVR) | CVR = (nₑ - N/2)/(N/2) where nₑ = essential ratings, N = total experts | Minimum value depends on panel size (0.62 for 10 experts) | Used in HIV-Positive Women Reproductive Health Scale [29] |
| Item-Level Content Validity Index (I-CVI) | Proportion of experts giving relevance rating of 3-4 on 4-point scale | >0.79 acceptable; 0.70-0.79 requires revision | Applied in Premature Ovarian Insufficiency SRH scale development [10] |
| Scale-Level Content Validity Index (S-CVI) | Average of I-CVI scores across all items | ≥0.90 indicates excellent content validity | Achieved 0.926 in SRH-POI scale development [10] |
In the development of a reproductive health survey for endocrine-disrupting chemicals, researchers reported that "the content validity index (CVI) for the 52 items was above .80, meeting the standard criteria. Four items were removed for failing to meet the required validity threshold, and others were revised based on expert feedback" [42].
Implementation Protocols for Face Validity Assessment
Face validity assessment ensures that the survey items appear relevant, appropriate, and acceptable to the end users, which is particularly crucial for sensitive reproductive health topics.
Qualitative Face Validation Protocol
The qualitative approach involves gathering in-depth feedback from target population representatives:
Cognitive Interviewing: Engage participants from the target population to complete the survey while verbalizing their thought process, interpretations, and reactions to each item.
Structured Debriefing: Conduct focused discussions after survey completion to assess:
- Interpretation clarity: Whether items are understood as intended
- Sensitivity comfort: Whether items feel intrusive or uncomfortable
- Response process: Whether response options align with experiences
- Time burden: Whether completion time is acceptable
In developing the reproductive health scale for HIV-positive women, researchers distributed the tool to 10 HIV-infected women and "asked to identify any difficulties with interpretations of the words and questions (understanding phrases, expressions, and words)" [29].
Quantitative Face Validation Protocol
The quantitative approach employs impact scores to numerically evaluate item relevance:
Impact Score Calculation:
- Procedure: Target population representatives rate each item on a 5-point importance scale (1 = not at all important to 5 = extremely important)
- Calculation: Impact Score = Frequency (%) × Importance, where Frequency is the percentage of respondents rating the item 4 or 5, and Importance is the mean importance rating
- Threshold: Impact score ≥1.5 indicates adequate face validity [29]
Comprehension Testing:
- Participants rate each item for clarity on a categorical scale (e.g., "very easy to understand," "somewhat easy," "difficult")
- Items receiving "difficult" ratings from more than 20% of participants should be revised
Data Analysis and Interpretation Framework
Quantitative Data Analysis Procedures
Analysis of expert panel data requires both statistical computations and qualitative synthesis:
Content Validity Metrics Calculation:
- Compute CVR, I-CVI, and S-CVI using formulas previously described
- Determine inter-rater agreement using modified kappa statistics to account for chance agreement
- Calculate descriptive statistics (means, standard deviations) for importance ratings
Decision Rules for Item Modification:
- Retain: Items meeting all quantitative thresholds (CVR, I-CVI) and receiving no substantive negative qualitative feedback
- Revise: Items approaching thresholds (e.g., I-CVI 0.70-0.79) or receiving consistent qualitative suggestions for improvement
- Eliminate: Items failing to meet quantitative thresholds or receiving consistent negative feedback regarding relevance or appropriateness
In the SRH-POI scale development, researchers used both quantitative and qualitative methods during content validation: "During the stages of face and content validity was reduced to 41 items but finally after factor analysis 30 items with four factors gained" [10].
Qualitative Data Synthesis Approach
Thematic analysis of qualitative expert feedback provides critical context for statistical findings:
- Systematic Coding: Categorize expert comments into thematic areas (e.g., wording issues, conceptual misalignment, missing content)
- Pattern Identification: Identify recurring suggestions across multiple experts that indicate systematic issues
- Triangulation: Integrate qualitative findings with quantitative metrics to make informed revision decisions
Integration with Broader Psychometric Validation
Content and face validity represent initial but critical components within a comprehensive validation framework. Subsequent validation stages must build upon these foundations:
Construct Validity: After establishing content validity, reproductive health scales typically proceed to factor analysis to assess structural validity. For example, in validating the Reproductive Autonomy Scale for use in the UK, researchers performed confirmatory factor analysis that "found the scale to be valid based on our hypothesis that among women who want to avoid pregnancy, those with higher reproductive autonomy will be more likely to use contraception" [9].
Reliability Assessment: Internal consistency and test-retest reliability should be evaluated following content validation. In the Reproductive Autonomy Scale validation, "internal consistency was good, with a Cronbach's α of 0.75. Test-retest reliability was fair-good with an intraclass correlation coefficient of 0.67" [9].
Criterion Validity: Establish relationships between scale scores and relevant outcomes. For instance, in reproductive coercion research, the refined Reproductive Coercion Scale demonstrated that "recent reproductive coercion was reported by 6.7% and 6.3% of the sample with the full and short-form RCS, respectively" [41].
Visualization of Methodological Workflows
Content Validity Assessment Workflow
Face Validity Assessment Workflow
Research Reagent Solutions: Methodological Tools
Table 3: Essential Methodological Tools for Content and Face Validity Assessment
| Tool Category | Specific Instrument/Software | Primary Function in Validation | Application Example |
|---|---|---|---|
| Expert Recruitment Framework | Multidisciplinary panel selection protocol | Ensure comprehensive content coverage | Combining clinical, research, and community expertise [42] [29] |
| Quantitative Validity Metrics | CVR and CVI calculation templates | Statistical assessment of expert consensus | Lawshe's table for minimum CVR values [10] [29] |
| Qualitative Data Collection | Structured feedback forms, cognitive interview guides | Gather in-depth expert and participant insights | "Grammar, appropriateness of words, allocation of items" evaluation [10] |
| Data Analysis Tools | Statistical software (SPSS, R), qualitative analysis software (NVIVO) | Analyze quantitative metrics and qualitative themes | Using IBM SPSS Statistics for factor analysis [42] |
| Reporting Frameworks | Standards for reporting psychometric studies (COSMIN) | Ensure comprehensive documentation of methods | Following systematic validation protocols [40] |
Establishing content and face validity through systematic expert panel methodology provides the foundational evidence necessary for developing psychometrically sound reproductive health surveys. The structured protocols outlined in this guide—encompassing expert recruitment, qualitative and quantitative assessment methods, data analysis procedures, and integration with broader validation frameworks—enable researchers to create instruments that accurately measure complex reproductive health constructs.
As the field of reproductive health research continues to evolve, with emerging focus areas such as reproductive coercion [41], endocrine-disrupting chemical exposure [42], and condition-specific sexual and reproductive health assessments [10] [29], the rigorous application of these validation methodologies becomes increasingly critical. By employing these standardized approaches, researchers can contribute to the advancement of reproductive health measurement, ultimately supporting more valid and reliable research findings that inform clinical practice, public health interventions, and policy development.
In the specialized field of reproductive health survey research, establishing robust psychometric properties is paramount to ensuring that assessment tools accurately capture the complex, often latent, constructs they intend to measure. Construct validity evidence confirms that a survey instrument adequately represents the theoretical construct it was designed to assess. Within this framework, factor analysis serves as a powerful statistical method for investigating the underlying structure of a set of observed variables. It operates on the premise that observed variables (e.g., survey item responses) are influenced by a smaller number of underlying, unobservable traits known as latent factors. For instance, in developing the Sexual and Reproductive Health Scale for Women with Premature Ovarian Insufficiency (SRH-POI), researchers used factor analysis to validate that groups of items correctly measured distinct dimensions of health, such as psychological well-being or sexual function [10].
The process of establishing construct validity typically involves two sequential and complementary phases: Exploratory Factor Analysis (EFA) and Confirmatory Factor Analysis (CFA). EFA is an inductive, data-driven approach used in the early stages of scale development to explore the data and identify the number and nature of the underlying factors. In contrast, CFA is a deductive, hypothesis-testing approach used to confirm a pre-specified factor structure, often based on theory or prior EFA results [43] [44]. In reproductive health research, where constructs like "mental health literacy" or "sexual and reproductive health" are multifaceted, this two-phase approach provides a rigorous methodology for ensuring that surveys are both comprehensive and scientifically sound [32] [10].
Foundational Concepts and Terminology
A clear understanding of key terminology is essential for implementing and interpreting factor analysis correctly.
- Latent Construct/Variable: A variable that cannot be directly observed or measured but is inferred from other observed variables. In reproductive health, examples include "quality of life," "menstrual health literacy," or "contraceptive self-efficacy."
- Observed Variable/Indicator/Item: A directly measured variable, such as an individual's response to a specific survey question, that is presumed to be influenced by a latent construct.
- Factor Loading: A statistic, analogous to a standardized regression coefficient, that represents the correlation between an observed variable and a latent factor. Higher loadings (typically ≥ 0.7) indicate a stronger relationship [44].
- Communality: The proportion of an observed variable's variance that is explained by the extracted factors. High communality indicates that the variable is well-represented by the factor structure.
- Eigenvalue: Represents the amount of variance in all the observed variables that is accounted for by a given factor. Factors with eigenvalues greater than 1.0 are generally considered meaningful and are retained for interpretation [43].
- Model Fit: A set of statistics that quantify how well the hypothesized factor model reproduces the observed covariance matrix. Key indices include the Chi-square test, RMSEA, CFI, and TLI [44].
Table 1: Key Differences Between Exploratory and Confirmatory Factor Analysis
| Aspect | Exploratory Factor Analysis (EFA) | Confirmatory Factor Analysis (CFA) |
|---|---|---|
| Purpose | To explore the underlying structure of a set of variables and identify the number and nature of factors. | To test a pre-specified model of the relationships between observed variables and latent constructs [43]. |
| Theoretical Basis | Data-driven; no strong a priori hypothesis about the number of factors or the pattern of loadings. | Theory-driven; a specific model is hypothesized a priori based on theory or previous research [44]. |
| Number of Factors | Determined by the data using criteria like eigenvalues, scree plots, and parallel analysis [43]. | Specified by the researcher in the model before analysis begins [43]. |
| Factor Loadings | All variables are typically allowed to load on all factors, and the analysis estimates all loadings [43]. | The researcher specifies which variables load on which factors; other loadings are restricted to zero [44]. |
| Model Fit Assessment | Not a primary focus, as the goal is exploration. | A primary focus; statistical tests and fit indices are used to evaluate the hypothesized model's acceptability [44]. |
Phase 3a: Exploratory Factor Analysis (EFA) - Experimental Protocol
Objective and Applications
The primary objective of EFA is to uncover the underlying, latent factor structure of a set of observed variables without imposing a pre-defined structure. In reproductive health research, EFA is indispensable during the initial development of a new survey instrument. For example, when creating the Mental Health Literacy Scale for Women of Reproductive Age (WoRA-MHL), researchers used EFA to discover that 30 items naturally grouped into four distinct themes: "Accessing and Obtaining Mental Health Information," "Understanding Mental Health Information," "Maintaining Mental Health," and "Adapting to the Challenges of Women's Lives" [32]. This discovery phase is critical for ensuring the survey comprehensively covers the different dimensions of the complex construct being measured.
Step-by-Step EFA Protocol
Step 1: Data Preparation and Assumption Checking Begin by ensuring your dataset is suitable for EFA. The minimum sample size is a subject of debate, but a common rule of thumb is at least 10 observations per observed variable, with an absolute minimum of 200 participants [43]. Check the correlation matrix for the presence of sufficient correlations (e.g., multiple coefficients > |0.3|) among the variables. Two statistical tests are crucial:
- Kaiser-Meyer-Olkin (KMO) Measure of Sampling Adequacy: Values closer to 1.0 indicate that patterns of correlations are compact, thus suitable for factor analysis. A KMO value of 0.83, as reported in the SRH-POI scale development, is considered good [10].
- Bartlett's Test of Sphericity: A statistically significant test (p < 0.05) indicates that the correlation matrix is not an identity matrix, meaning there are sufficient correlations to proceed with factor analysis [10].
Step 2: Factor Extraction This step determines how many latent factors are needed to adequately represent the observed data. The most common method is Principal Axis Factoring, which estimates factors based on shared variance. To determine the number of factors to retain, use a combination of:
- Kaiser's Criterion: Retain factors with eigenvalues greater than 1.0.
- Scree Plot: Visual inspection of the plot of eigenvalues, looking for the "elbow" point where the slope of the curve flattens out.
- Parallel Analysis: A robust method where the eigenvalues from your data are compared to those from a random dataset; factors from your data that exceed those from the random data are retained.
Step 3: Factor Rotation Rotation simplifies the factor structure to make it more interpretable. It resolves ambiguous loadings by maximizing high loadings and minimizing low ones.
- Orthogonal Rotation (Varimax): Assumes factors are uncorrelated. This is simpler and results in more easily interpretable factors.
- Oblique Rotation (Promax): Allows factors to be correlated. This is often more realistic in social and health sciences, where constructs like reproductive health dimensions are often interrelated.
Step 4: Interpreting the Rotated Solution Interpret the factor structure by examining the pattern matrix (for oblique rotation) or the rotated factor matrix (for orthogonal rotation). Assign each variable to the factor on which it has the highest loading, provided that loading is meaningful (typically ≥ 0.4 or 0.5). A clear structure is achieved when most variables have high loadings on one factor and low loadings on others. Finally, the researcher examines the groups of variables loading on each factor to conceptually label or name the underlying latent construct.
EFA Workflow Visualization
Phase 3b: Confirmatory Factor Analysis (CFA) - Experimental Protocol
Objective and Applications
CFA shifts from exploration to confirmation. Its objective is to rigorously test a pre-specified factor structure—derived from theory, prior research, or a previous EFA—against empirical data. In reproductive health research, CFA provides strong evidence for the validity of a survey's structure. For instance, after developing the WoRA-MHL scale through EFA, the researchers used CFA to confirm that the four-factor model indeed provided a satisfactory fit to the data [32]. This step is crucial before a survey is deployed in clinical trials or epidemiological studies, as it confirms that the instrument measures what it purports to measure in the way researchers intend.
Step-by-Step CFA Protocol
Step 1: Model Specification This is the most critical step, where the researcher formally defines the hypothesized model. This includes:
- Specifying the number of latent factors (constructs).
- Defining which observed variables (items) load on which factors.
- Typically, each item is allowed to load on only one factor (this is the "primary loading").
- Specifying which factors are allowed to correlate (if using an oblique model).
- Fixing the scale of the latent factors, usually by setting the factor variance to 1 or by fixing one factor loading per factor to 1.
Step 2: Model Identification Ensure the model is "identified," meaning there is enough information in the data to estimate all model parameters. A necessary condition is that the number of parameters to be estimated must be less than or equal to the number of unique elements in the covariance matrix (i.e., the number of unique variances and covariances). A common rule of thumb is to have at least three indicators per factor for a model to be identified.
Step 3: Model Estimation The specified model is fitted to the observed data from the sample. The most common estimation method is Maximum Likelihood (ML), which assumes multivariate normality. For data that violates this assumption, alternative estimators like Robust Maximum Likelihood (MLR) or Weighted Least Squares (WLS) can be used.
Step 4: Model Fit Evaluation Assess how well the hypothesized model reproduces the observed covariance matrix. This is done by examining a suite of fit indices, as no single index is sufficient. The following table summarizes the key indices and their commonly accepted thresholds for a "good" fit.
Table 2: Key Model Fit Indices for CFA and Their Target Values
| Fit Index | Description | Target Value for Good Fit | Citation |
|---|---|---|---|
| χ²/df (Chi-square/df) | Adjusts the model chi-square for model complexity. | < 3.0 | [44] |
| CFI (Comparative Fit Index) | Compares the fit of the model to a null model. | ≥ 0.95 | [44] |
| TLI (Tucker-Lewis Index) | Another comparative fit index that penalizes model complexity. | ≥ 0.95 | [44] |
| RMSEA (Root Mean Square Error of Approximation) | Measures approximate fit in the population, accounting for model complexity. | < 0.06 | [44] |
| SRMR (Standardized Root Mean Square Residual) | The average difference between the observed and model-implied correlations. | < 0.08 | [44] |
Step 5: Model Respecification (if needed) If the initial model fit is inadequate, the model may need to be respecified. This should be done cautiously and with strong theoretical justification. Guidance can be taken from modification indices (MI), which estimate the improvement in model chi-square if a fixed parameter (e.g., a cross-loading or error covariance) were freed. However, freeing parameters based solely on statistical grounds can capitalize on chance and should be avoided unless it makes substantive sense.
CFA Workflow Visualization
The Researcher's Toolkit for Factor Analysis
Successfully conducting EFA and CFA requires a suite of statistical software and a clear understanding of key analytical concepts. The following table outlines essential "research reagents" for this process.
Table 3: Essential Research Reagents for Factor Analysis
| Tool Category | Specific Example | Function in Factor Analysis |
|---|---|---|
| Statistical Software | R (with packages psych, lavaan, GPArotation) |
A free, open-source environment. The psych package is excellent for EFA (e.g., fa()), and lavaan is the standard for CFA (cfa()). [45] |
| Statistical Software | Mplus, SPSS, Stata | Commercial software packages with robust procedures for both EFA and CFA. |
| Data Screening Protocol | Tests for Normality, Multicollinearity, Sample Size | Ensures data meets the assumptions of factor analysis (e.g., multivariate normality, absence of perfect multicollinearity). [43] |
| Factor Retention Method | Parallel Analysis | A robust method for determining the number of factors to retain in EFA by comparing data eigenvalues to those from random data. [43] |
| Model Fit Indices | CFI, TLI, RMSEA, SRMR | A suite of indices used in CFA to quantitatively assess how well the hypothesized model fits the observed data. [44] |
Integration with Broader Psychometric Validation
Factor analysis, while central to establishing construct validity, is one component of a comprehensive psychometric validation framework. In reproductive health survey research, this framework also includes:
- Reliability Assessment: Demonstrating that the instrument produces consistent results. This is typically measured using Cronbach's alpha for internal consistency (e.g., a value of 0.889 for the WoRA-MHL scale is considered good) [32] and the intraclass correlation coefficient (ICC) for test-retest reliability (e.g., an ICC of 0.95 for the SRH-POI scale indicates excellent stability) [10].
- Other Forms of Validity: This includes content validity, ensured through expert review and qualitative studies with the target population [10], and criterion validity, which examines the relationship between the survey scores and an external gold standard measure.
The sequential application of EFA and CFA, embedded within this broader validation framework, provides a powerful and defensible methodology for developing and validating reproductive health surveys. This rigorous approach ensures that these critical tools are scientifically sound, reliable, and capable of producing valid evidence to inform clinical practice and public health policy.
In the context of reproductive health survey research, establishing reliability is fundamental to ensuring that measurement instruments produce stable, consistent, and error-free results. Reliability assessment verifies that a scale measures a construct consistently across time, items, and researchers. This phase focuses on two core methodological approaches: internal consistency, which evaluates the extent to which items within a scale measure the same underlying construct, and test-retest reliability, which assesses the stability of measurements over time. For researchers and drug development professionals, these metrics provide critical evidence that a reproductive health survey will perform reliably in both research and clinical applications, ensuring that observed changes in outcomes reflect true variation rather than measurement error.
Core Concepts and Measurement Frameworks
Theoretical Foundations of Reliability
Reliability in psychometrics refers to the degree to which an instrument is free from random measurement error, thus yielding consistent results under consistent conditions. In reproductive health research, where constructs such as sexual empowerment, autonomy, and health knowledge are often latent variables (not directly observable), establishing robust reliability is particularly crucial. High reliability indicates that the instrument's items are homogeneous and that scores remain stable over short time periods when the underlying construct being measured has not changed.
The consensus-based standards for the selection of health measurement instruments (COSMIN) initiative provides a rigorous framework for evaluating psychometric properties, including reliability parameters [24]. Adherence to these standards ensures methodological rigor in the validation of patient-reported outcome measures (PROMs), which are extensively used in reproductive health research to capture sensitive and subjective experiences.
Key Reliability Metrics and Their Interpretation
The following table summarizes the primary reliability metrics used in reproductive health survey validation:
Table 1: Key Reliability Metrics in Psychometric Validation
| Metric | Definition | Interpretation Guidelines | Common Applications in Reproductive Health Research |
|---|---|---|---|
| Cronbach's Alpha (α) | Measures extent to which items in a scale correlate with each other | α ≥ 0.9: Excellent0.7 ≤ α < 0.9: Good0.6 ≤ α < 0.7: Acceptableα < 0.6: Poor | Widely used for multi-item scales measuring constructs like reproductive autonomy, sexual empowerment, and health knowledge |
| Intraclass Correlation Coefficient (ICC) | Assesses agreement between repeated measurements | ICC ≥ 0.9: Excellent0.75 ≤ ICC < 0.9: Good0.5 ≤ ICC < 0.75: ModerateICC < 0.5: Poor | Preferred for test-retest reliability of continuous scores; used in pelvic pain, reproductive autonomy scales |
| McDonald's Omega (Ω) | Alternative to alpha, less sensitive to number of items | Similar interpretation to Cronbach's alpha | Increasingly used in modern validation studies as a robust measure of internal consistency |
| Split-half Reliability | Correlates scores from two halves of a test | Values > 0.7 generally acceptable | Less commonly reported than alpha in contemporary reproductive health literature |
Experimental Protocols for Reliability Testing
Protocol 1: Assessing Internal Consistency
Purpose: To evaluate the extent to which all items in a scale measure the same underlying construct.
Materials and Equipment:
- Finalized survey instrument after content validation
- Statistical software package (SPSS, R, STATA, or similar)
- Target population sample (minimum n=100-200 recommended)
Procedure:
- Administer the survey to a representative sample of the target population. Sample size should be sufficient, typically 5-10 participants per survey item.
- Code and clean the data, ensuring no missing values for included items.
- Calculate Cronbach's alpha coefficient using statistical software:
- The formula for alpha is: α = (k / (k-1)) * (1 - (Σσ²item / σ²total))
- Where k = number of items, σ²item = variance of each item, σ²total = total variance of the scale
- Calculate item-total correlations to identify poorly performing items:
- Correlations < 0.3 may indicate items not well-aligned with the overall construct
- Compute alpha if item deleted statistics to determine if removing any item would substantially improve overall reliability
- Report results including the overall alpha coefficient, subscale alphas if applicable, and item-total correlations
Quality Control Considerations:
- Ensure unidimensionality of the scale through exploratory factor analysis before assessing internal consistency
- Check for skewness in item responses that might artificially inflate or deflate alpha values
- For multidimensional scales, calculate separate alpha coefficients for each subscale
Exemplar Application: In the validation of the Sexual and Reproductive Empowerment Scale for Chinese adolescents, researchers reported a Cronbach's alpha of 0.89, indicating excellent internal consistency among the 21 items measuring the empowerment construct [46].
Protocol 2: Determining Test-Retest Reliability
Purpose: To assess the stability of measurements over time, assuming the underlying construct being measured has not changed.
Materials and Equipment:
- Validated survey instrument
- Statistical software capable of calculating ICC and correlation coefficients
- Participant tracking system for follow-up
Procedure:
- Administer the survey (Time 1) to a subset of participants from the main validation study
- Determine appropriate retest interval based on construct stability:
- Typically 2-4 weeks for most reproductive health constructs
- Short enough that the construct shouldn't have changed substantially
- Long enough that participants are unlikely to recall their previous answers
- Readminister the survey (Time 2) to the same participants using identical procedures and conditions
- Calculate intraclass correlation coefficients (ICC):
- Use two-way mixed effects model for consistency
- Report both single measures and average measures ICC when appropriate
- Compute correlation between Time 1 and Time 2 scores:
- Pearson's r for normally distributed continuous data
- Spearman's rho for ordinal data or non-normal distributions
- Assess systematic changes between time points using paired t-tests or Wilcoxon signed-rank tests
Quality Control Considerations:
- Document and report participant attrition between test and retest
- Monitor for external events that might actually change the construct being measured
- Assess potential practice effects where prior exposure might influence subsequent responses
Exemplar Application: In the validation of the Pelvic Pain Impact Questionnaire, researchers demonstrated excellent test-retest reliability with an ICC of 0.977 (95% CI: 0.955-0.988) over an appropriate retest interval [47].
Data Analysis and Interpretation Framework
Quantitative Benchmarks from Reproductive Health Studies
The table below summarizes reliability coefficients reported in recent reproductive health instrument validation studies:
Table 2: Reliability Coefficients from Recent Reproductive Health Validation Studies
| Instrument | Population | Internal Consistency (α) | Test-Retest Reliability (ICC) | Citation |
|---|---|---|---|---|
| Sexual and Reproductive Empowerment Scale (Chinese version) | Chinese nursing students (n=581) | 0.89 | 0.89 | [46] |
| Reproductive Health Scale for HIV-Positive Women | Iranian women with HIV (n=25 qualitative, larger quantitative) | 0.713 | 0.952 | [29] |
| Reproductive Autonomy Scale (UK validation) | UK women of reproductive age (n=826) | 0.75 | 0.67 | [48] |
| Pelvic Pain Impact Questionnaire (Hungarian version) | Hungarian women with endometriosis (n=240) | 0.881 (α) / 0.885 (Ω) | 0.977 | [47] |
| Sexual and Reproductive Health Scale for Premature Ovarian Insufficiency | Women with POI (development phase) | 0.884 | 0.95 | [10] |
Interpretation Guidelines for Different Contexts
The acceptable thresholds for reliability coefficients vary based on research context and application:
For research purposes:
- Cronbach's alpha ≥ 0.70 is generally acceptable for group-level comparisons
- Test-retest ICC ≥ 0.70 indicates adequate stability for most research applications
For clinical decision-making:
- Cronbach's alpha ≥ 0.90 is preferred for individual-level assessment
- Test-retest ICC ≥ 0.80 provides greater confidence in score stability
For high-stakes applications (e.g., drug development endpoints):
- Cronbach's alpha ≥ 0.90 is essential
- Test-retest ICC ≥ 0.85 demonstrates robust measurement stability
In the UK validation of the Reproductive Autonomy Scale, researchers reported a Cronbach's alpha of 0.75 and test-retest ICC of 0.67, which they characterized as "good" and "fair-good" respectively for research purposes [48]. Similarly, the Chinese Sexual and Reproductive Empowerment Scale demonstrated excellent reliability with both internal consistency (α=0.89) and test-retest reliability (ICC=0.89) exceeding recommended thresholds for research applications [46].
Methodological Visualization
Figure 1: Workflow for Assessing Reliability in Survey Validation
Essential Research Reagent Solutions
Table 3: Essential Methodological Tools for Reliability Assessment
| Research Tool | Specific Function | Application in Reliability Testing |
|---|---|---|
| Statistical Software (SPSS, R, STATA) | Data analysis and psychometric calculation | Computing Cronbach's alpha, ICC, item-total correlations, and other reliability metrics |
| Participant Tracking System | Managing longitudinal data collection | Maintaining contact with participants for test-retest assessments and minimizing attrition |
| Electronic Data Capture (REDCap) | Survey administration and data management | Ensuring consistent presentation of surveys across test and retest occasions |
| COSMIN Checklist | Methodological quality assessment | Ensuring comprehensive evaluation of reliability and other measurement properties [24] |
| Quality of Life/Health Measurement Databases | Reference for comparison | Providing benchmark values for reliability coefficients from similar instruments |
Advanced Considerations and Methodological Challenges
Addressing Common Methodological Issues
Sample Size Requirements: Adequate sample size is critical for precise reliability estimation. For internal consistency, a minimum of 100 participants is recommended, though larger samples (200+) provide more stable estimates. For test-retest reliability, a subset of 50-100 participants is typically sufficient, though this depends on the expected ICC magnitude and desired precision.
Interval Selection for Test-Retest: The optimal retest interval balances recall effects against true construct change. For most reproductive health constructs, 2-4 weeks is appropriate. Shorter intervals risk inflation of reliability estimates due to memory effects, while longer intervals increase the likelihood that the underlying construct has actually changed.
Multidimensional Instruments: For scales with subscales, reliability should be calculated separately for each dimension. The overall scale reliability may be misleading if subscales measure distinct constructs. The Reproductive Autonomy Scale, for example, demonstrates this approach with its three subscales: Decision Making, Freedom from Coercion, and Communication [48].
Emerging Methodological Innovations
Modern psychometric approaches are increasingly incorporating additional reliability indices beyond traditional metrics. McDonald's Omega is gaining prominence as a less biased alternative to Cronbach's alpha, particularly when tau-equivalence (equal factor loadings) cannot be assumed. The Hungarian validation of the Pelvic Pain Impact Questionnaire appropriately reported both Cronbach's alpha (0.881) and McDonald's Omega (0.885), providing a more comprehensive assessment of internal consistency [47].
Additionally, item response theory (IRT) approaches offer sophisticated methods for examining item-level reliability across different levels of the underlying trait, though these require larger sample sizes and more complex analytic approaches.
Surveys are a fundamental research approach for collecting subjective opinions and reported experiences from a sample of subjects, serving as a critical tool for generating evidence in clinical research [49]. In the specific context of reproductive health research, rigorously developed surveys allow investigators to measure complex constructs such as patient knowledge, attitudes, and experiences related to sexual and reproductive health services, including sensitive topics like contraception and abortion [50]. The integrity of this research hinges on the seamless integration of the survey methodology into the overall study protocol. A well-defined protocol outlines the proposed research idea, including the research question, study design, data collection, and analysis methods, and is typically submitted to funding agencies, institutions, or journals for approval [51]. This guide provides a detailed framework for incorporating survey-based studies into clinical research protocols, with an emphasis on establishing robust psychometric properties.
Foundational Survey Design and Typology
The first step in protocol development is to define the survey's purpose and design. Surveys in clinical research can be broadly categorized by their primary objective, which dictates their overall design and the types of conclusions they can support [49].
- Exploratory Surveys: These are qualitative investigations used to understand a topic without predetermined notions. They often employ open-ended questions to understand the "why" and "how" of participant experiences.
- Descriptive Surveys: These quantitative studies aim to describe respondent perceptions, attitudes, or behaviors and their association with other characteristics. They primarily use descriptive statistics to summarize data, for example, reporting the frequency distribution of Likert-scale responses.
- Explanatory Surveys: These quantitative studies test hypotheses about relationships between variables. They employ inferential statistics, such as regression analysis, to explain or predict how certain respondent characteristics might lead to specific outcomes.
Furthermore, the temporal design must be specified. A cross-sectional design collects data at a single point in time, providing a snapshot of the population. In contrast, a longitudinal design collects data from the same or similar groups at two or more time points to detect changes over time [49]. For instance, the Youth Reproductive Health Access (YouR HeAlth) Survey employs a repeated, cross-sectional design to examine trends annually [50].
Table 1: Key Survey Design Options in Clinical Research
| Design Feature | Options | Description and Application |
|---|---|---|
| Primary Purpose | Exploratory | Investigates little-understood topics; uses open-ended questions [49]. |
| Descriptive | Describes perceptions/behaviors and associations; uses descriptive statistics [49]. | |
| Explanatory | Tests hypotheses and predicts outcomes; uses inferential statistics [49]. | |
| Time Period | Cross-sectional | Single data collection point; provides a population snapshot [49]. |
| Longitudinal | Multiple data collection points; measures change over time [49]. | |
| Respondent Group | Single Cohort | Surveys one group of subjects [49]. |
| Multiple Cohorts | Surveys different groups (e.g., users vs. non-users) for comparison [49]. | |
| Data Collection Mode | Self-administered | Questionnaires via mail, email, or online platforms [49]. |
| Interviewer-administered | Interviews conducted in-person or by phone [49]. |
Methodological Considerations for Survey Integration
Population, Sampling, and Bias Mitigation
A protocol must precisely define the study population and the strategy for selecting a representative sample. The two primary sampling strategies are probability and non-probability sampling [49]. Probability sampling (e.g., simple random, stratified) is used in descriptive and explanatory surveys to allow for statistical inference to the broader population, with the sample size determined by the desired confidence level and margin of error. Non-probability sampling (e.g., convenience, purposeful) is often used in exploratory surveys to include individuals with specific experiences relevant to the research topic.
The protocol must also address potential sources of bias and how they will be minimized [49]:
- Coverage bias: Occurs when the sampling frame is not representative of the population.
- Sampling bias: Arises from the sampling method itself.
- Non-response bias: Happens when respondents differ systematically from non-respondents.
- Measurement error: Stems from poorly worded questions or problematic data collection procedures.
Mitigation strategies include using multiple recruitment sources, employing rigorous sampling methods, and implementing follow-up reminders to improve response rates [49].
Survey Instrument Development and Validation
The heart of a survey study is the instrument itself. The protocol must detail the development process and provide evidence of the instrument's validity and reliability—its psychometric properties [49].
The development process should be multi-faceted, drawing from a literature review, existing validated surveys, and qualitative research (e.g., focus groups, site visits) to ensure content is relevant and comprehensive [52]. Subsequent cognitive interviews with individuals from the target population are crucial for assessing item comprehension, relevance, and ease of response, allowing researchers to refine the survey before full-scale administration [52].
Establishing validity is a core psychometric requirement. The following types of validity should be considered and assessed [49]:
- Face Validity: A qualitative assessment by non-experts of the instrument's clarity and comprehensibility.
- Content Validity: A formal assessment by subject matter experts to ensure the items adequately cover the domain of interest.
- Criterion Validity: The instrument's correlation with another reputable test (concurrent validity) or with future outcomes (predictive validity).
- Construct Validity: The degree to which the instrument measures the theoretical construct it purports to measure. This can be demonstrated by showing the survey distinguishes between known groups (discriminative validity) or correlates with other measures as expected (concurrent validity) [53].
Establishing reliability is equally important. Key assessments include [49]:
- Test-Retest Reliability: The correlation between results from the same survey administered to the same respondents at two different times.
- Internal Consistency Reliability: The extent to which different items measuring the same construct produce similar scores, often measured with Cronbach's alpha.
Figure 1: Survey Instrument Development and Validation Workflow
Experimental Protocols for Psychometric Validation
The research protocol should treat psychometric testing as a critical experiment within the larger study. The following provides a detailed methodology for key validation steps.
Protocol for Assessing Discriminative Validity
Objective: To test whether the survey instrument can reliably distinguish between known groups that theoretically should score differently on the measured construct [53].
Methodology:
- Participant Recruitment: Recruit a sufficient sample of participants from the target population (e.g., patients who have received healthcare in the last year).
- Group Allocation: Use a between-subjects design. Participants are randomized to be exposed to different simulated healthcare scenarios (e.g., via written vignettes or audio clips) that depict clearly "good," "mixed," or "poor" integration of care [53].
- Data Collection: After exposure to the scenario, participants are asked to imagine themselves as the patient in the scenario and complete the survey instrument (e.g., IntegRATE).
- Analysis: Compare the mean survey scores across the different experimental conditions using analysis of variance (ANOVA). A statistically significant difference in scores between the "good" and "poor" integration groups supports the instrument's discriminative validity [53].
Protocol for Assessing Test-Retest Reliability
Objective: To evaluate the stability of the survey instrument over a short period of time when no real change in the construct is expected [53].
Methodology:
- Participant Recruitment: A subset of participants from the main study (e.g., those in the "good" or "poor" integration conditions) is recontacted.
- Time Interval: The follow-up survey (Time 2) is administered 1 to 3 weeks after the initial administration (Time 1). This interval is short enough that perceptions of the static scenario should not change, but long enough to minimize recall bias [53].
- Data Collection: Participants complete the same survey instrument under the same conditions at Time 2.
- Analysis: Calculate the correlation (e.g., intraclass correlation coefficient) between the Time 1 and Time 2 scores for each participant. A high correlation coefficient indicates good test-retest reliability [53] [49].
Table 2: Core Psychometric Properties and Assessment Methods
| Psychometric Property | Assessment Method | Interpretation |
|---|---|---|
| Discriminative Validity | Administer survey to groups known to differ on the construct; compare scores with ANOVA [53]. | A significant difference (p < 0.05) in scores between known groups supports validity. |
| Test-Retest Reliability | Administer the same survey to the same respondents at two time points; calculate correlation [53] [49]. | A correlation coefficient > 0.70 is generally considered acceptable stability. |
| Internal Consistency | Calculate Cronbach's alpha based on responses to all items in a multi-item scale [49] [52]. | Alpha between 0.70 and 0.95 is considered acceptable to good internal consistency. |
| Content Validity | Expert panel review of survey items for relevance and comprehensiveness [49]. | A high rating (e.g., > 80%) from experts confirms items are appropriate. |
The Scientist's Toolkit: Essential Reagents for Survey Research
Beyond theoretical design, successful survey implementation relies on a suite of practical "research reagents"—standardized tools and methods that ensure quality and consistency.
Table 3: Essential Research Reagents for Survey Studies
| Tool or Solution | Function in Survey Research |
|---|---|
| Cognitive Interview Guide | A semi-structured protocol used to pretest draft survey items, assessing comprehension, relevance, and ease of response from the target population's perspective [52]. |
| Validated Reference Instrument | An existing survey with established psychometric properties, used to assess criterion validity by correlating scores from the new instrument with this "gold standard" [49]. |
| Probability-Based Online Panel | A pre-recruited pool of respondents (e.g., Ipsos KnowledgePanel) that provides a representative sample, enhancing the generalizability of findings beyond convenience samples [50] [49]. |
| Structured Scenario/Vignette | A standardized, fictional narrative (e.g., a letter describing a healthcare experience) used to experimentally manipulate the construct being measured for validity testing [53]. |
| Multi-Mode Data Collection System | Integrated platforms for administering surveys via mail, web, or telephone with follow-up reminders, which helps to maximize response rates and reduce non-response bias [52]. |
Figure 2: Survey Integration and Execution Workflow within a Research Protocol
Ethical Considerations and Reporting
Ethical conduct is paramount. The protocol must outline how informed consent will be obtained, how confidentiality and anonymity will be maintained, and what compensation, if any, will be offered to participants [54]. Even though surveys are often considered low-risk, they can pose informational harms (e.g., from data breaches) or psychological harms (e.g., anxiety from sensitive questions). Therefore, obtaining formal ethics review or an exemption from an Institutional Review Board (IRB) is mandatory [54] [51].
For transparency and reproducibility, researchers should adhere to reporting guidelines such as the Consensus-based Checklist for Reporting of Survey Studies (CROSS) or the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) [54]. The protocol should also detail the plan for disseminating results to participants, the scientific community, and other relevant stakeholders [51].
By meticulously addressing each of these components—from foundational design and rigorous psychometric validation to ethical implementation and transparent reporting—researchers can robustly integrate surveys into clinical research protocols. This ensures the collection of high-quality, meaningful data capable of advancing understanding in complex fields like reproductive health.
Navigating Challenges: Strategies for Refining and Enhancing Survey Instruments
Addressing Common Pitfalls in Scale Development and Item Wording
The psychometric properties of a measurement scale are fundamental to building robust scientific knowledge in reproductive health research. A well-developed instrument ensures that researchers, clinicians, and drug development professionals can accurately capture complex, latent constructs such as reproductive autonomy, mental health literacy, and sexual health functioning. The development process is critical, as methodological weaknesses at any stage can compromise the validity of research findings and their subsequent application in clinical practice and intervention design [55] [56]. Within the specific context of reproductive health surveys, where topics are often sensitive and multidimensional, a rigorous approach to scale development and item wording is not merely a methodological preference but a scientific necessity. This guide addresses common pitfalls in this process and provides evidence-based recommendations to enhance the quality of measurement in this field.
Foundational Principles of Scale Development
Scale development is a systematic process that transforms abstract theoretical constructs into measurable variables. It involves complex procedures requiring both theoretical and methodological rigor [55] [56]. The process is typically conceptualized in three fundamental phases, each with distinct objectives and activities.
Table 1: The Three Core Phases of Scale Development
| Phase | Primary Objective | Key Activities | Common Outputs |
|---|---|---|---|
| Item Development | To generate and refine a comprehensive pool of items | Domain identification, item generation, content validity assessment | Conceptual definition, initial item pool |
| Scale Development | To construct a coherent measurement instrument | Pre-testing, survey administration, item reduction, factor extraction | Refined item set, preliminary factor structure |
| Scale Evaluation | To rigorously assess the instrument's psychometric quality | Tests of dimensionality, reliability, and validity | Final scale with documented psychometric properties [57] |
A well-defined construct domain provides the foundational theory for the scale, specifying its boundaries and ensuring that generated items are relevant to the target phenomenon [57]. Failure to adequately define the construct domain is a frequently cited limitation that weakens all subsequent development steps [55]. In reproductive health research, constructs like "reproductive autonomy" or "sexual and reproductive health" must be precisely delineated, often through a combination of literature review and qualitative exploration with the target population [9] [10].
The Critical Role of Item Wording
The phrasing of individual items is a critical determinant of a scale's quality. Items must be worded simply and unambiguously to ensure they are consistently understood by all respondents [57]. Fowler's five essential characteristics for high-quality items provide a useful framework: consistent understanding, consistent administration, clear communication of adequate answers, respondent access to required information, and respondent willingness to provide accurate answers [57]. In reproductive health surveys, where questions may involve sensitive topics, adherence to these principles is paramount to minimize measurement error and social desirability bias [55].
Common Pitfalls and Limitations
A systematic review of 105 scale development studies published between 1976 and 2015 identified ten main types of limitations frequently reported by researchers. Understanding these pitfalls is the first step toward mitigating them in future research [55] [56].
Table 2: Common Limitations in Scale Development Processes
| Category of Limitation | Description | Impact on Psychometric Quality |
|---|---|---|
| Sample Characteristics | Non-representative samples, small sample sizes | Limits generalizability and statistical power for analysis |
| Methodological Limitations | Weaknesses in study design or procedure | Threatens internal and external validity |
| Psychometric Limitations | Inadequate evidence for validity or reliability | Undermines confidence in scale scores |
| Qualitative Research Limitations | Insufficient foundational qualitative work | Compromises content validity and relevance of items |
| Missing Data | High rates of non-response or incomplete data | Introduces potential bias and reduces analytic sample |
| Social Desirability Bias | Respondents answering in socially acceptable ways | Distorts scores, particularly for sensitive topics |
| Item Limitations | Poorly worded, complex, or ambiguous items | Increases measurement error |
| Brevity of the Scale | Too few items to adequately capture the construct | Reduces reliability and content coverage |
| Uncontrolled Variables | Inability to control for confounding factors | Introduces extraneous variance |
| Lack of Manual/Instructions | No standardized administration guidelines | Leads to inconsistent use and scoring |
One of the most prevalent issues is inadequate sample size. Approximately 50.4% of studies in the systematic review used sample sizes smaller than the commonly recommended rule of thumb, which is at least 10 participants per scale item, with an ideal ratio of 15:1 or 20:1 [55] [56]. Insufficient sample power can lead to unstable factor solutions and overfitted models, ultimately limiting the generalizability of the scale.
Another critical pitfall is the underutilization of qualitative methods during the item generation phase. The systematic review found that only 7.6% of studies used exclusively inductive (qualitative) methods, while 35.2% relied solely on deductive methods (e.g., literature review) without input from the target population [55]. For reproductive health surveys, failing to incorporate the lived experiences and terminology of the target population through interviews or focus groups can result in items that lack cultural relevance or fail to capture important nuances of the construct [10] [29].
Methodological Recommendations and Best Practices
Item Generation and Content Validation
A combined deductive-inductive approach is considered best practice for item generation [57]. This involves:
- Deductive Methods: Conducting an extensive literature review and analyzing pre-existing scales to build a theoretical foundation for the construct [55].
- Inductive Methods: Gathering qualitative information from the target population through focus groups, interviews, and expert panels to ensure items reflect the lived experience of the construct [55] [58].
For example, in developing the Sexual and Reproductive Health Scale for women with Premature Ovarian Insufficiency (SRH-POI), researchers created an initial pool of 84 items through literature review and a qualitative study, which was then refined by the research team [10]. Similarly, the development of the Mental Health Literacy Scale for reproductive-age women (WoRA-MHL) involved semi-structured interviews with 14 women and 6 key informants to ensure comprehensive coverage of the domain [58].
The initial item pool should be broader than the final desired scale. Recommendations suggest the initial pool should be at least twice as long as the intended final instrument, providing a sufficient margin to select an optimal combination of items [57].
To assess content validity, seek opinions from both expert judges (subject matter experts) and target population judges (potential scale users) [55]. Quantitatively, this can be evaluated using:
- Content Validity Ratio (CVR): Assesses the essentiality of each item. The minimum acceptable value depends on the number of experts, typically 0.62 for 10 experts [10] [29].
- Content Validity Index (CVI): Measures the relevance, simplicity, and clarity of items on a scale of 1-4. Items with a CVI >0.79 are acceptable, 0.70-0.79 need revision, and <0.70 should be omitted [10] [29].
The SRH-POI scale development reported a Scale-CVI of 0.926, indicating excellent content validity [10].
Psychometric Validation
Construct validity should be assessed using both Exploratory Factor Analysis (EFA) and Confirmatory Factor Analysis (CFA) [55]. EFA helps identify the underlying factor structure, while CFA tests how well the hypothesized structure fits the data. For example, in the development of the Reproductive Health Assessment Scale for HIV-Positive Women, researchers used EFA with Varimax rotation, retaining factors with eigenvalues greater than 1 and items with factor loadings greater than 0.3 [29]. The Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy and Bartlett's test of sphericity should be used to ensure the data are suitable for factor analysis [10] [29].
Reliability should be evaluated through multiple methods:
- Internal Consistency: Typically measured by Cronbach's alpha, with values above 0.70 generally considered acceptable [10] [29]. The WoRA-MHL scale reported a Cronbach's alpha of 0.889 [58].
- Test-Retest Reliability: Assesses stability over time using intraclass correlation coefficients (ICC). The Reproductive Autonomy Scale validation for the UK reported an ICC of 0.67, indicating fair-good reliability [9].
- Split-Half Reliability: Correlates scores from two halves of the test [58].
Scale Development Workflow
Addressing Social Desirability Bias in Reproductive Health Surveys
Social desirability bias is particularly problematic in reproductive health research due to the sensitive nature of many topics [55]. To mitigate this:
- Use neutral wording that does not imply judgment.
- Ensure confidentiality and anonymity in administration.
- Consider incorporating social desirability scales to identify and statistically control for this bias.
- Employ self-administered formats rather than interviewer-administered surveys for sensitive items.
Essential Research Reagents and Tools
Table 3: Essential Methodological Tools for Scale Development
| Tool Category | Specific Technique/Index | Primary Function | Interpretation Guidelines |
|---|---|---|---|
| Content Validity | Content Validity Ratio (CVR) | Quantifies expert consensus on item essentiality | Value >0.62 (for 10 experts) indicates essential item [29] |
| Content Validity | Content Validity Index (CVI) | Measures relevance, clarity, and simplicity of items | I-CVI >0.79 acceptable; S-CVI >0.90 excellent [10] |
| Factor Analysis | Kaiser-Meyer-Olkin (KMO) | Assesses sampling adequacy for factor analysis | >0.8 meritorious; >0.9 marvelous [29] |
| Factor Analysis | Bartlett's Test of Sphericity | Tests if correlation matrix is an identity matrix | Significant p-value (<0.05) supports factorability |
| Factor Analysis | Factor Loadings | Indicates strength of relationship between item and factor | >0.3 minimal; >0.5 practically significant [29] |
| Reliability Analysis | Cronbach's Alpha | Measures internal consistency | 0.7-0.9 acceptable; >0.9 may indicate redundancy [29] |
| Reliability Analysis | Intraclass Correlation (ICC) | Assesses test-retest reliability | <0.5 poor; 0.5-0.75 moderate; >0.75 good [9] [58] |
| Qualitative Validation | Cognitive Interviews | Identifies problems in item interpretation | Uncovers issues with comprehension and recall |
Construct Operationalization Process
Robust scale development is fundamental to advancing research on reproductive health. By systematically addressing common pitfalls—particularly through adequate sample sizes, mixed-method item generation, rigorous content validation, and comprehensive psychometric testing—researchers can create instruments that yield valid and reliable data. The field benefits from standardized approaches that facilitate cross-cultural comparisons and longitudinal assessments of reproductive health outcomes. As scale development methodologies continue to evolve, their thoughtful application within reproductive health survey research will enhance both scientific understanding and clinical application in this critically important domain.
Optimizing Questionnaires for Specific Subpopulations and Clinical Settings
The validity and reliability of clinical trial data are fundamentally dependent on the quality of the instruments used to collect patient-reported outcomes. Questionnaire optimization for specific subpopulations and clinical settings represents a critical methodological challenge in clinical research, particularly in sensitive domains such as reproductive health. A well-designed questionnaire minimizes bias, maximizes precision in treatment effect estimates, and ensures that collected data accurately reflects the experiences of diverse patient populations [59]. Within reproductive health research, where conditions like HIV, premature ovarian insufficiency (POI), and shift work present unique challenges, developing population-specific instruments is not merely advantageous but essential for capturing clinically relevant outcomes [29] [10] [20].
The regulatory framework governing clinical trials emphasizes that forms and content of collected data should be established in advance and focus on information necessary to implement planned analyses [59]. Ignoring population heterogeneity can substantially impact medical practice, as treatments may work well in some patients but not in others, potentially exposing non-responding groups to harmful side effects without benefit [60]. Furthermore, the International Conference on Harmonisation (ICH) guidelines warn against collecting excessive data that will not be analyzed, as this wastes resources, reduces recruitment rates, and increases losses to follow-up [59].
Foundational Principles of Questionnaire Design and Validation
Psychometric Properties and Validation Frameworks
The development of validated questionnaires requires rigorous methodology to ensure they measure what they intend to measure consistently and accurately. The psychometric evaluation process typically assesses both validity (whether the instrument measures the intended construct) and reliability (whether it produces consistent results) [29] [10] [20].
Table 1: Core Psychometric Properties in Questionnaire Validation
| Property | Description | Assessment Methods | Acceptability Thresholds |
|---|---|---|---|
| Content Validity | Degree to which items adequately reflect the full domain of interest | Content Validity Index (CVI), Content Validity Ratio (CVR) | CVI > 0.79; CVR > 0.62 (for 10 experts) [29] [10] |
| Face Validity | Whether the questionnaire appears to measure what it claims to | Qualitative feedback from target population | Impact score ≥ 1.5 [10] [20] |
| Construct Validity | Extent to which the instrument measures the theoretical construct | Exploratory Factor Analysis (EFA), Confirmatory Factor Analysis (CFA) | KMO > 0.6; significant Bartlett's test [29] [20] |
| Internal Consistency | Degree of interrelation among items | Cronbach's alpha | α ≥ 0.7 [29] [20] |
| Test-Retest Reliability | Stability of measurements over time | Intraclass Correlation Coefficient (ICC) | ICC > 0.7 [29] [20] |
The questionnaire design taxonomy identifies six distinct methods, each optimizing different psychometric aspects: rational method (face validity), prototypical method (process validity), internal method (homogeneity), external method (criterion validity), construct method (construct validity), and facet method (content validity) [61]. Selection among these methods involves trade-offs, as optimizing one psychometric aspect may cause others to be suboptimal [61].
Methodological Approaches to Questionnaire Development
The sequential exploratory mixed-methods design has emerged as a robust framework for developing population-specific questionnaires, particularly in complex reproductive health contexts [29] [10] [20]. This approach integrates qualitative and quantitative phases to ensure instruments are both conceptually grounded and psychometrically sound.
Table 2: Phases of Sequential Exploratory Mixed-Methods Design
| Phase | Primary Objective | Key Activities | Outputs |
|---|---|---|---|
| Qualitative Phase | Concept exploration and item generation | In-depth interviews, focus groups, literature review | Preliminary item pool, Conceptual framework |
| Quantitative Phase | Psychometric validation | Face/content validity assessment, Factor analysis, Reliability testing | Refined questionnaire with documented psychometric properties |
The qualitative phase typically involves in-depth interviews and focus groups with the target population to ensure the conceptual framework reflects their lived experiences. For example, in developing the Women Shift Workers' Reproductive Health Questionnaire, researchers conducted 21 interviews with women shift workers to identify relevant domains [20]. Similarly, development of the Reproductive Health Assessment Scale for HIV-Positive Women included semi-structured interviews with 25 HIV-positive women to capture disease-specific concerns [29].
The quantitative phase employs statistical methods to refine and validate the instrument. Factor analysis (both exploratory and confirmatory) helps identify the underlying structure of the questionnaire, while reliability assessments ensure consistency of measurements [29] [20]. This phase typically results in item reduction and scale refinement, as seen in the development of the Sexual and Reproductive Health Assessment Scale for women with POI, where the initial 84-item pool was reduced to a 30-item final instrument [10].
Specialized Methodologies for Subpopulation Assessment
Addressing Heterogeneity in Clinical Trials
Population heterogeneity presents significant challenges in clinical trials, as variations in clinical background, environmental factors, and genetic profiles can lead to differential treatment responses [60]. This heterogeneity is particularly relevant in reproductive health, where conditions manifest differently across populations. To address this, researchers have developed specialized designs that allow for subpopulation selection during trials [60].
The single-stage design with one biomarker tests null hypotheses for both the full population and predefined subgroups simultaneously [60]. This approach is typically used for exploratory subgroup analysis in phase II trials or confirmatory analysis in phase III. More complex multistage designs incorporate adaptive elements, allowing researchers to refine the population to either the whole population or specific subgroups at interim analyses [60]. These designs can include early stopping rules for both benefit and lack of benefit.
A critical consideration in these designs is estimator performance, as bias can be introduced when selecting subgroups based on observed data. The maximum likelihood estimator in these settings can be substantially biased, with the degree of bias influenced by subgroup prevalence [60]. Recent methodological advances have focused on bias-adjusted estimators and confidence intervals to address this challenge [60].
Advanced Statistical Approaches for Subpopulation Analysis
Distributionally Robust Optimization (DRO) has emerged as a promising approach for improving worst-case model performance across predefined subpopulations [62]. Unlike methods that aim to equalize performance across groups, DRO seeks to maximize minimum performance, representing a form of minimax fairness [62]. This approach is particularly valuable when predictive models for clinical outcomes perform well on average but drastically underperform for specific subpopulations.
In empirical comparisons of methods to improve disaggregated and worst-case performance, researchers have found that with relatively few exceptions, no approach consistently outperforms standard empirical risk minimization applied to the entire training dataset [62]. This suggests that when improved performance for specific subpopulations is necessary, it may require data collection techniques that increase effective sample size or reduce noise rather than algorithmic solutions alone.
Domain-Specific Applications in Reproductive Health Research
Representative Questionnaire Development Initiatives
Reproductive health research has seen significant advances in population-specific questionnaire development, with several rigorously validated instruments emerging in recent years:
The Reproductive Health Assessment Scale for HIV-Positive Women was developed through a sequential exploratory mixed-methods design [29]. The final 36-item instrument covers six factors: disease-related concerns, life instability, coping with the illness, disclosure status, responsible sexual behaviors, and need for self-management support. The scale demonstrated strong psychometric properties with Cronbach's alpha of 0.713 and test-retest intraclass correlation of 0.952 [29].
The Women Shift Workers' Reproductive Health Questionnaire (WSW-RHQ) addresses the unique challenges faced by this population [20]. Through interviews with 21 women shift workers and subsequent psychometric validation with 620 participants, researchers developed a 34-item instrument covering five domains: motherhood, general health, sexual relationships, menstruation, and delivery. The final questionnaire showed excellent reliability with Cronbach's alpha exceeding 0.7 and composite reliability values above the threshold [20].
The Sexual and Reproductive Health Assessment Scale for Women with Premature Ovarian Insufficiency (SRH-POI) filled a critical measurement gap for this population [10]. Beginning with an 84-item pool, the development process yielded a 30-item instrument with four factors. The scale demonstrated strong internal consistency (Cronbach's alpha = 0.884) and excellent test-retest reliability (ICC = 0.95) [10].
The Reproductive Autonomy Scale (RAS) validation for use in the UK demonstrated the importance of cross-cultural adaptation [9]. The study confirmed the scale's three-factor structure and found good internal consistency (Cronbach's alpha = 0.75) and fair-to-good test-retest reliability (ICC = 0.67) [9].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Methodological Components for Questionnaire Development
| Component | Function | Application Examples |
|---|---|---|
| Expert Panels | Provide qualitative content validation and ensure domain coverage | 10-12 experts assessing content validity ratio and index [10] [20] |
| Target Population Representatives | Ensure face validity and relevance of items | 10+ participants from subpopulation providing feedback on difficulty, appropriateness, ambiguity [20] |
| Statistical Software (EFA/CFA) | Conduct exploratory and confirmatory factor analysis | SPSS, R, or Mplus for factor analysis and reliability testing [29] [20] |
| Reliability Assessment Tools | Measure internal consistency and stability | Cronbach's alpha for internal consistency, ICC for test-retest reliability [29] [10] |
| Validity Assessment Metrics | Quantify content and construct validity | CVR/CVI for content validity, KMO and Bartlett's test for construct validity [29] [10] |
Experimental Protocols for Questionnaire Validation
Protocol for Content Validity Assessment
Objective: To ensure questionnaire items adequately cover the construct domain and are relevant to the target population.
Procedure:
- Expert Panel Recruitment: Convene 10-12 experts with relevant expertise (clinicians, researchers, and content specialists) [10] [20].
- Content Validity Ratio (CVR) Assessment:
- Present experts with each item and ask them to rate its essentiality using a 3-point scale: "essential," "useful but not essential," or "not necessary" [10].
- Calculate CVR using the formula: CVR = (nₑ - N/2)/(N/2), where nₑ is the number of experts rating the item as "essential" and N is the total number of experts.
- Retain items meeting the minimum CVR threshold (0.62 for 10 experts) [10].
- Content Validity Index (CVI) Assessment:
- Ask experts to rate the relevance of each item on a 4-point scale (1 = not relevant, 4 = highly relevant).
- Calculate I-CVI (item-level CVI) as the number of experts giving a rating of 3 or 4 divided by the total number of experts.
- Calculate S-CVI (scale-level CVI) as the average of I-CVIs for all items.
- Retain items with I-CVI ≥ 0.78 and aim for S-CVI ≥ 0.90 [10].
Protocol for Construct Validity via Factor Analysis
Objective: To verify the underlying factor structure of the questionnaire and assess how well items load on theoretical constructs.
Procedure:
- Sample Size Determination: Recruit a minimum of 300 participants based on the rule of thumb for factor analysis [20].
- Sampling Adequacy Assessment:
- Factor Extraction:
- Item Retention Criteria:
- Keep items with factor loadings ≥ 0.3 [20].
- Consider cross-loading items and remove those loading significantly on multiple factors.
- Confirmatory Factor Analysis:
- Conduct CFA on a separate sample to confirm the factor structure identified through EFA.
- Assess model fit using indices: RMSEA (< 0.08 acceptable, < 0.05 good), CFI (> 0.90 acceptable, > 0.95 good), GFI (> 0.90) [20].
Optimizing questionnaires for specific subpopulations and clinical settings requires methodologically rigorous approaches that balance psychometric excellence with practical utility. The sequential mixed-methods design has proven particularly valuable in reproductive health research, where understanding lived experiences is essential for developing relevant instruments. As research in this field advances, several areas warrant continued attention: improving statistical methods for subgroup analysis in clinical trials, developing more sophisticated approaches for cross-cultural adaptation of instruments, and establishing standardized methodologies for assessing measurement invariance across diverse populations.
The development of population-specific questionnaires remains both a scientific and ethical imperative. Without instruments capable of capturing the unique experiences and outcomes of diverse subpopulations, clinical research risks generating incomplete or misleading evidence, potentially exacerbating health disparities. The methodologies and frameworks presented in this review provide a foundation for developing questionnaires that yield valid, reliable, and clinically meaningful data across the spectrum of reproductive health contexts and patient populations.
Techniques for Improving Response Rates and Data Quality
High response rates and superior data quality are fundamental to the validity of reproductive health research. In psychometric studies, where the goal is to develop and validate robust measurement instruments, nonresponse bias and measurement error can severely compromise the reliability and construct validity of scales. This technical guide synthesizes evidence-based methodologies to optimize participation and ensure data integrity, with specific application to the specialized field of reproductive health surveys.
Strategies for Enhancing Response Rates
Participant Outreach and Tracking Protocols
Systematic and persistent outreach is critical for engaging hard-to-reach populations. Evidence from a long-term evaluation of a sex education program, which achieved an 89% response rate on a 9-month follow-up survey, highlights several effective protocols [6].
- Multi-Modal Contact Strategies: Researchers should collect multiple forms of contact information from participants at the outset, including phone numbers and email addresses. Furthermore, obtaining contact details for two trusted adults or friends can facilitate reconnection if a participant's primary contact information becomes invalid. This information must be updated regularly [6].
- Scheduled Persistence: Approved by an Institutional Review Board, contact attempts can include in-person visits, texts, and phone calls, occurring up to 10 times over 4-6 weeks. Initial contact should be made via an in-person survey session, followed by text messages for those unable to attend. Sending reminders at different times of day accommodates varied schedules. If there is no response after multiple texts, the protocol should switch to phone calls [6].
- Identity and Trust Building: Participants are more likely to respond when they remember the study and trust the messenger. Facilitators should inform youth about future follow-ups during initial programming, highlighting incentives. Subsequent text messages should include program-specific details, such as a facilitator's name, to jog memory and build trust [6].
Incentive Structures
Financial incentives demonstrate tangible appreciation for participants' time and can significantly boost participation, particularly among demographic groups that are typically harder to engage.
Table 1: Impact of Conditional Monetary Incentives on Response Rates
| Incentive Value | Baseline Response Rate (18-22 yrs) | Response Rate with Incentive | Relative Response Rate (95% CI) |
|---|---|---|---|
| None | 3.4% | (Control) | (Reference) |
| £10 (∼$12.5) | 8.1% | 2.4 (2.0–2.9) | |
| £20 (∼$25.0) | 11.9% | 3.5 (3.0–4.2) | |
| £30 (∼$37.5) | 18.2% | 5.4 (4.4–6.7) |
Source: Adapted from REACT-1 Study [63]
As shown in Table 1, monetary incentives had a dose-response effect, with the largest increases observed among the lowest responders, such as teenagers and young adults. This strategy can improve sample representativeness by engaging typically under-represented groups [63]. However, a study in primary care settings found that a non-financial, unconditional incentive (an origami paper with a seed) did not significantly improve completion rates, suggesting that the context and nature of the incentive matter [64].
Survey Administration and Mixed-Mode Approaches
The method of survey administration directly influences participation and completion. A cluster-randomized study in primary care waiting rooms demonstrated that while mixed-mode options (paper or web-based via tablet/QR code) offered logistical advantages, they did not enhance participation or completion rates compared to paper-only versions administered with research assistant support [64].
Crucially, completion rates were significantly higher in the paper-only group (99.8%) compared to the mixed-mode groups (96.8% for tablet; 93.3% for QR code) [64]. This underscores the value of direct, in-person support for ensuring data completeness, though web-based methods remain valuable for broader reach.
Ensuring Data Quality and Psychometric Integrity
Survey Design to Minimize Burden
Reducing participant burden is a key strategy for minimizing attrition and improving data quality. Researchers should design follow-up surveys to be "as short as possible" [6]. Furthermore, for longer web-based surveys, providing a return code allows participants to complete the survey in multiple sittings, which has been shown to reduce the number of incomplete responses [6]. Cognitive interviews during the development phase ensure survey content is easy to understand and appropriate for the target population, such as youth ages 15-19 [6].
Psychometric Validation Workflow
For research focused on developing reproductive health assessment scales, adhering to a rigorous psychometric validation workflow is non-negotiable for ensuring data quality and instrument reliability.
Diagram 1: Psychometric Validation Workflow for Instrument Development. This diagram outlines the sequential stages of developing and validating a robust research instrument, such as a reproductive health scale. CVR: Content Validity Ratio; CVI: Content Validity Index; EFA: Exploratory Factor Analysis; CFA: Confirmatory Factor Analysis [10].
The development and validation of the Sexual and Reproductive Health Assessment Scale in women with Premature Ovarian Insufficiency (SRH-POI) exemplifies this workflow [10]:
- Item Generation: An initial pool of 84 items was generated through a literature review and a qualitative study.
- Face and Content Validity: The tool was reduced to 41 items after expert and participant review. Quantitative content validity was confirmed with a Scale-Level Content Validity Index (S-CVI) of 0.926 [10].
- Construct Validation: Exploratory Factor Analysis yielded a final 30-item instrument with a 4-factor structure (KMO=0.83; Bartlett's test was significant) [10].
- Reliability Assessment: The scale demonstrated excellent internal consistency (Cronbach’s α = 0.884) and test-retest reliability (ICC = 0.95) [10].
Similarly, the Reproductive Autonomy Scale (RAS) was validated for use in the UK, showing good internal consistency (Cronbach’s α of 0.75), fair-to-good test-retest reliability (ICC of 0.67), and confirmed construct validity and a three-factor structure [9].
The Scientist's Toolkit: Essential Reagents for Survey Research
Table 2: Essential Research Reagents for Survey-Based Psychometric Studies
| Reagent / Tool | Function in Research Protocol |
|---|---|
| Participant Tracking System | Manages multiple contact points and schedules persistent outreach to reduce attrition [6]. |
| Conditional Monetary Incentives | Financial tokens used to boost response rates and improve sample representativeness, particularly among hard-to-reach groups [63]. |
| Cognitive Interview Protocol | A structured guide for testing survey items with individuals from the target population to identify and rectify problems with question wording, structure, and comprehension [6]. |
| Content Validity Index (CVI) | A quantitative metric for evaluating the relevance and representativeness of survey items as rated by a panel of subject matter experts [10]. |
| Statistical Software (e.g., R, SPSS) | Platform for conducting key psychometric analyses, including Factor Analysis (EFA/CFA) and calculating reliability coefficients (Cronbach's α, ICC) [9] [10]. |
Integrated Participant Engagement Strategy
A truly effective protocol integrates outreach, design, and validation into a cohesive strategy. The following diagram maps this comprehensive approach, connecting specific actions to their ultimate impact on data quality.
Diagram 2: Integrated Strategy Linking Engagement to Data Quality. This diagram illustrates how pre-survey preparation, deployment tactics, and active follow-up drive high response rates, while rigorous psychometric validation of the collected data ensures high quality, forming the two pillars of a successful study.
Achieving high response rates and impeccable data quality in reproductive health survey research requires a meticulous, multi-faceted methodology. Key techniques include systematic and persistent multi-modal outreach, the strategic use of conditional monetary incentives to enhance representativeness, and minimizing participant burden through concise survey design. For psychometric instrument development, a rigorous validation workflow—encompassing face, content, and construct validity, alongside reliability testing—is essential. By integrating these robust engagement strategies with rigorous scientific validation, researchers can generate reliable, valid, and generalizable data that advances the field of reproductive health.
In the realm of global health research, particularly in studies concerning reproductive health, the ability to accurately measure constructs across different populations is paramount. The process of translating and culturally validating research instruments ensures that data collected from diverse cultural and linguistic groups is comparable, valid, and reliable. Within the specific context of reproductive health surveys, where cultural norms, values, and practices significantly influence both the constructs being measured and how respondents interpret questions, rigorous cross-cultural adaptation becomes not merely methodological refinement but an ethical imperative [10] [29]. This technical guide outlines the systematic processes required to adapt tools for cross-cultural research, with a specific focus on maintaining the psychometric integrity of instruments designed to assess reproductive health outcomes.
The consequences of poorly adapted instruments are profound, ranging from measurement bias to erroneous conclusions about health disparities and intervention effectiveness [65]. For instance, research on women with Premature Ovarian Insufficiency (POI) or HIV-positive women has demonstrated that their reproductive health experiences are deeply embedded in cultural contexts, necessitating tools that are not merely linguistically translated but conceptually aligned with their lived realities [10] [29]. This guide synthesizes current methodologies to provide researchers, scientists, and drug development professionals with a robust framework for the cross-cultural adaptation of surveys, ensuring that the psychometric properties—such as validity and reliability—are preserved or appropriately recalibrated for the target population.
Foundational Concepts and Equivalence
Cross-cultural adaptation extends beyond simple translation to encompass the comprehensive process of ensuring an instrument is appropriate, comprehensible, and conceptually equivalent in a new cultural context. Key to this process is understanding and achieving different types of equivalence between the source instrument (original version) and the target instrument (adapted version) [65].
Core Types of Equivalence in Cross-Cultural Adaptation:
- Conceptual Equivalence: Ensures that the theoretical constructs (e.g., "reproductive health," "quality of work life") being measured have the same meaning and relevance in the target culture as in the source culture [65].
- Semantic/Linguistic Equivalence: Achieved when the translated items have the same intended meaning, connotation, and readability as the original items, avoiding literal translations that may distort meaning [65].
- Item Equivalence: Confirms that the specific questions or items are applicable and appropriate for the target culture. Some items may need modification or replacement to reflect culturally specific manifestations of a construct [65].
- Operational Equivalence: Ensures that the method of administration (e.g., self-completion, interviewer-led), format, and measurement scales (e.g., Likert scales) are suitable and function similarly in the new context [65].
- Measurement Equivalence: The final goal, establishing that the psychometric properties of the instrument, including its factor structure, reliability, and validity, are consistent across cultures [65].
A critical challenge in this process is mitigating cultural biases, which can be categorized as construct bias (the construct is not equivalent across cultures), method bias (problems with sampling or instrument administration), and item bias (poor item translation or inappropriate item content) [65]. Strategies to minimize these biases include using forward and back-translation techniques, involving cultural experts, and conducting rigorous pilot testing with the target population.
Methodological Framework: An Eight-Step Guide
A rigorous, multi-stage process is fundamental to successful cross-cultural adaptation. The following eight-step guideline, synthesized from established methodological frameworks, provides a structured approach for researchers [65].
Forward Translation
The initial translation of the instrument from the source language to the target language is performed by at least two independent bilingual translators. Ideally, one translator should be knowledgeable about the health constructs being measured, while the other should be a naive translator to capture natural language use. This dual approach helps identify jargon and complex phrasing [66] [65].
Synthesis of Translations
The forward translations are reconciled into a single, consensus-based version (T3). The project team and translators review all versions, discussing and resolving discrepancies in wording, conceptual meaning, and cultural relevance to create a preliminary adapted version [66] [65].
Back Translation
The synthesized target language version is independently translated back into the source language by two translators who are blinded to the original instrument. This step is not for a literal match but to identify unintended deviations in meaning or conceptual gaps between the original and the adapted version [66] [65].
Harmonization
An expert committee—typically comprising methodologies, linguists, health professionals, and the translators—reviews the entire process. They compare the original instrument, the forward translations, the synthesized version, and the back-translations. The committee makes final decisions on any disputed items to ensure all forms of equivalence (conceptual, semantic, etc.) have been achieved. This step also includes a formal assessment of content validity, often quantified using a Content Validity Index (CVI) [66] [10] [29].
Pre-Testing
The harmonized version is tested with a small sample from the target population. Cognitive debriefing techniques, such as "think-aloud" interviews, are used to assess participants' understanding of each item, the clarity of instructions, and the appropriateness of response options. This qualitative feedback is crucial for identifying lingering problems [65] [67].
Field Testing
The revised instrument is administered to a larger, representative sample to gather data for quantitative psychometric evaluation. Sample size requirements vary, but studies in reproductive health have utilized samples ranging from approximately 110 to over 650 participants [66] [68] [29].
Psychometric Validation
The data from the field test is analyzed to establish the instrument's psychometric properties in the new cultural context. Key analyses include:
- Construct Validity: Assessed via Exploratory Factor Analysis (EFA) and/or Confirmatory Factor Analysis (CFA) to verify the underlying factor structure.
- Reliability: Evaluated through internal consistency (Cronbach's α, McDonald's ω) and test-retest reliability (Intraclass Correlation Coefficient - ICC).
- Other Validities: Convergent, discriminant, and criterion validity are also examined [66] [10] [68].
Documentation and Reporting
The final step involves compiling a detailed report of the entire adaptation process, including all decisions, modifications, and full psychometric results. This transparency allows other researchers to evaluate the quality of the adapted instrument [65].
The workflow below illustrates the sequential and iterative nature of this process.
Experimental Protocols and Psychometric Evaluation
This section details the core experimental and analytical protocols referenced in the cross-cultural validation literature.
Assessing Content Validity
Content validity confirms that the instrument's items adequately cover and are relevant to the construct being measured.
- Protocol: A panel of subject matter experts (e.g., clinicians, researchers) rates each item on a scale (e.g., 1-4) for relevance, clarity, and simplicity.
- Quantitative Analysis:
- Content Validity Index (CVI): Calculated at the item level (I-CVI) and scale level (S-CVI). I-CVI is the proportion of experts giving a rating of 3 or 4. An I-CVI > 0.78 is generally acceptable. S-CVI is the average of all I-CVIs or the proportion of items rated 3 or 4 by all experts (S-CVI/UA), with a target of 0.8 or higher [10] [29].
- Content Validity Ratio (CVR): Assesses the essentiality of an item. The minimum acceptable value depends on the number of experts; for 10 experts, the CVR must be > 0.62 [10] [29].
Assessing Construct Validity via Factor Analysis
Factor analysis is used to evaluate the underlying dimensional structure of the instrument.
- Preliminary Checks: Before factor analysis, researchers check the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy (values > 0.8 are good) and Bartlett's test of sphericity (which should be significant, p < .05) [10] [29].
- Exploratory Factor Analysis (EFA): Used when the factor structure in the target culture is unknown or needs verification. EFA helps identify the number of underlying factors and which items load onto them. Items with factor loadings above 0.4 or 0.5 are typically retained. For example, the development of the SRH-POI scale used EFA to reduce 41 items to a final 30 items across four factors [10].
- Confirmatory Factor Analysis (CFA): Used to statistically test how well the pre-specified factor structure (e.g., the 4-factor model of the Health-ITUES) fits the new data. Model fit is assessed using indices such as the Comparative Fit Index (CFI > 0.90), Tucker-Lewis Index (TLI > 0.90), and Root Mean Square Error of Approximation (RMSEA < 0.08) [66].
Assessing Reliability
Reliability evaluates the consistency and stability of the instrument.
- Internal Consistency: Measured using Cronbach's alpha or McDonald's omega. A value above 0.7 is acceptable for group comparisons, while values above 0.8 or 0.9 are preferred for clinical applications [66] [68] [29]. For example, the Portuguese SALI validation reported a Cronbach's alpha of 0.95 for the total scale [68].
- Test-Retest Reliability: Assesses stability over time. The instrument is administered twice to the same participants within a short interval (e.g., 2 weeks). The agreement between scores is calculated using the Intraclass Correlation Coefficient (ICC), where values above 0.7 indicate good stability [10] [29]. One study on a reproductive health scale for HIV-positive women reported an excellent ICC of 0.95 [29].
The table below summarizes key psychometric data from several validation studies, illustrating the typical outcomes of this process.
Table 1: Psychometric Properties from Exemplar Cross-Cultural Validation Studies
| Study & Instrument | Sample Size | Content Validity (CVI/S-CVI) | Construct Validity Method | Reliability (Cronbach's α) |
|---|---|---|---|---|
| Health-ITUES (Chinese) [66] | 234 total (110 older adults, 124 nurses) | S-CVI: 0.99 | Confirmatory Factor Analysis (CFA) | α > 0.80 (overall); > 0.75 (subscales) |
| SRH-POI Scale [10] | Information in source | S-CVI: 0.926 | Exploratory Factor Analysis (EFA) | α = 0.884 |
| Self-Assessment Leadership Instrument (Portuguese) [68] | 656 nursing students | Ensured in translation/adaptation stages | Factor Analysis (EFA/CFA) | α = 0.95 (total scale) |
| Reproductive Health Scale for HIV+ Women [29] | 25 (qual.) + Psychometric testing | CVI calculated | Exploratory Factor Analysis (EFA) | α = 0.713 |
| Mental Health Literacy Scale (WoRA-MHL) [32] | Information in source | Information in source | EFA & CFA | α = 0.889 |
The Scientist's Toolkit: Essential Reagents for Cross-Cultural Validation
Successful cross-cultural validation requires both methodological rigor and specific "research reagents" or tools. The following table details essential components for executing a robust validation study.
Table 2: Essential Research Reagents and Resources for Cross-Cultural Validation
| Tool/Reagent | Function & Application | Exemplars & Specifications |
|---|---|---|
| Bilingual Translators | Perform forward and back-translation; ensure linguistic and conceptual equivalence. | Native speakers fluent in both source and target languages; ideally one content-expert and one naive translator [66] [65]. |
| Expert Review Panel | Provides qualitative and quantitative assessment of content validity (CVI/CVR). | A multidisciplinary panel (e.g., 10+ experts) including methodologies, clinical specialists in the field (e.g., reproductive health), and linguists [10] [29] [65]. |
| Target Population Participants | Participate in pre-testing (cognitive interviews) and field testing. | Representative samples from the specific population of interest (e.g., women with POI, HIV-positive women, nursing students) [66] [10] [29]. |
| Statistical Software Packages | Used for comprehensive psychometric analysis. | Software like SPSS, R, Mplus, or STATA for conducting EFA, CFA, and calculating reliability coefficients (Cronbach's α, ICC) [66] [10] [68]. |
| Validated Concurrent Measures | Instruments measuring related constructs to assess criterion validity. | Used to establish convergent/discriminant validity by calculating Pearson correlations (e.g., Health-ITUES-R correlated with a mobile health acceptance questionnaire) [66]. |
The cross-cultural adaptation of research instruments is a meticulous and essential process that underpins the validity of international and multicultural health research. For fields like reproductive health, where constructs are deeply intertwined with cultural norms, skipping or shortening this process jeopardizes the very foundation of the research. The rigorous eight-step framework—encompassing translation, harmonization, pre-testing, and psychometric validation—provides a roadmap for developing instruments that are not only linguistically accurate but also conceptually and metrically sound.
The resulting adapted tools, such as the Chinese Health-ITUES or the SRH-POI scale, enable researchers to make valid comparisons across populations and accurately identify needs, ultimately leading to more effective, culturally-sensitive interventions and drug development programs. By adhering to these detailed methodologies and utilizing the essential "research reagents," scientists can ensure that their findings are robust, reliable, and truly representative of the diverse populations they aim to serve.
Overcoming Methodological Limitations in Complex Health Domains
Research in complex health domains, particularly those involving sensitive and multifaceted concepts like reproductive health, faces significant methodological challenges. These limitations can compromise the validity, reliability, and overall utility of the findings. The development and validation of psychometric instruments—tools designed to measure subjective, latent constructs such as quality of life, health status, or patient-reported outcomes—are especially vulnerable to these methodological issues. Within reproductive health, where conditions like Premature Ovarian Insufficiency (POI) and HIV intersect with profound psychological, social, and physical dimensions, the need for robust, scientifically sound measurement tools is paramount. This guide provides an in-depth technical framework for identifying and overcoming common methodological limitations, with a specific focus on ensuring the psychometric rigor of reproductive health surveys.
Identifying Key Methodological Limitations
A critical first step is recognizing the common methodological shortcomings in the field. A meta-epidemiologic study of reproductive endocrinology and infertility (REI) articles revealed significant gaps in transparent and reproducible research practices [69] [70]. The table below quantifies these issues, providing a baseline for improvement.
Table 1: Prevalence of Reproducible Research Practices in Reproductive Endocrinology and Infertility (REI) Research (n=222 articles)
| Research Practice | REI Journal Articles (2013) | REI Journal Articles (2018) | High-Impact Journal Articles (2013-2018) |
|---|---|---|---|
| Studies Prospectively Registered | Information Missing | Information Missing | More likely than REI articles |
| Protocol Available | 15 total across all groups | 15 total across all groups | More likely than REI articles |
| Explicitly Willing to Share Raw Data | 2 total across all groups | 2 total across all groups | Information Missing |
| Explicitly Described as a Replication | 2 total across all groups | 2 total across all groups | Information Missing |
Furthermore, the measurement of retrospective data, such as age at menarche, introduces another layer of methodological complexity. A study on the reproducibility of this measure found only moderate reliability overall (Intraclass Correlation Coefficient, ICC = 0.72), with significant variation depending on the respondent type [71]. This highlights how data collection methods can directly impact data quality and introduces measurement error.
Advanced Psychometric Validation Frameworks
To overcome these limitations, a rigorous, multi-stage psychometric validation process is essential. The following experimental protocols, derived from successful scale development studies in women with HIV and POI, provide a template for ensuring the structural integrity and validity of reproductive health surveys [29] [10].
Experimental Protocol 1: Comprehensive Scale Development and Validation
This protocol outlines the sequential stages for creating a new psychometric instrument from scratch.
Objective: To develop and validate a reliable, valid, and disease-specific reproductive health scale for a target population (e.g., women with POI or HIV).
Methodology: A sequential exploratory mixed-methods design is recommended, comprising qualitative and quantitative phases [10].
Item Generation:
- Qualitative Data Collection: Conduct in-depth, semi-structured interviews and focus group discussions with members of the target population until data saturation is achieved. For example, a study with HIV-positive women conducted 25 interviews [29].
- Literature Review: Perform a comprehensive review of existing literature and instruments to identify potential items and theoretical frameworks.
- Item Pool Creation: Synthesize findings from the qualitative phase and literature review to generate an initial pool of items.
Face and Content Validity:
- Qualitative Face Validity: Have 10-15 target participants review the items for clarity, difficulty, and ambiguity [10].
- Quantitative Face Validity: Calculate an Impact Score for each item using a 5-point Likert scale. Retain items with a score ≥ 1.5 [29]. The formula is:
Impact Score = Frequency (%) * Importance - Qualitative Content Validity: Convene a panel of 10+ experts (e.g., researchers, clinicians) to evaluate the items for grammar, wording, and appropriateness [29] [10].
- Quantitative Content Validity:
- Calculate the Content Validity Ratio (CVR) to assess the essentiality of each item. Based on Lawshe's table, with 10 experts, the minimum acceptable CVR is 0.62 [29] [10].
- Calculate the Content Validity Index (CVI) to assess item clarity, simplicity, and relevance. The Item-CVI (I-CVI) should be ≥ 0.78, and the Scale-CVI (S-CVI/Ave), an average of all I-CVIs, should be ≥ 0.90 [10].
Pilot Study and Construct Validity:
- Pilot the Questionnaire: Administer the refined scale to a larger sample from the target population.
- Assess Sampling Adequacy: Check the suitability of the data for factor analysis using the Kaiser-Meyer-Olkin (KMO) measure (should be ≥ 0.6, ideally ≥ 0.8) and Bartlett’s Test of Sphericity (should be significant, p < 0.05) [29] [10].
- Exploratory Factor Analysis (EFA): Use EFA to identify the underlying factor structure. Employ a Varimax rotation and retain factors with an eigenvalue > 1.0. Items with a factor loading > 0.3 are typically considered acceptable for retention in the scale [29].
Reliability Assessment:
- Internal Consistency: Calculate Cronbach's Alpha for the entire scale and its subscales. A value between 0.70 and 0.95 is generally considered to indicate good internal consistency [29] [10].
- Stability (Test-Retest Reliability): Administer the scale to the same participants after a 2-4 week interval. Calculate the Intraclass Correlation Coefficient (ICC). An ICC value > 0.70 indicates good external reliability and stability [29] [10].
The following workflow diagram visualizes this multi-stage protocol.
Experimental Protocol 2: Assessing Reproducibility of Retrospective Data
This protocol is crucial for evaluating and improving the quality of self-reported or proxy-reported historical data, a common limitation in long-term health studies.
Objective: To evaluate the reproducibility (reliability and agreement) of a self-reported or proxy-reported measure, such as age at menarche, collected at two different time points.
Methodology: A reproducibility study analyzing paired data from longitudinal surveys [71].
Data Collection:
- Collect data on the target variable (e.g., age at menarche) at two different time points (e.g., 1969 and 1978 surveys).
- Record the type of respondent (self or proxy) and, for proxies, their relationship to the participant (e.g., spouse, parent, child).
Statistical Analysis:
- Agreement Analysis: Use Bland-Altman's method to calculate the 95% limits of agreement. This quantifies the range within which 95% of the differences between the two measurements are expected to lie. Visually inspect the Bland-Altman plot for any systematic bias [71].
- Reliability Analysis: Calculate the Intraclass Correlation Coefficient (ICC) using a two-way mixed-effects model (for consistency). Interpret the ICC value as follows [71]:
- < 0.50: Poor
- 0.50 - 0.75: Moderate
- 0.75 - 0.90: Good
- ≥ 0.90: Excellent
- Stratified Analysis: Conduct the above analyses stratified by key variables such as the type of respondent and the participant's age at the time of the first survey to identify sources of variability.
Table 2: Results from a Reproducibility Study of Age at Menarche Reporting (9-year interval)
| Respondent Type | Sample Size (N) | 95% Limits of Agreement (Years) | Intraclass Correlation Coefficient (ICC) | Interpretation |
|---|---|---|---|---|
| All Participants | 9,043 | -2.3 to 2.4 | 0.72 (0.71 - 0.73) | Moderate |
| Self-Respondents (Both Surveys) | 6,664 | Information Missing | Information Missing | Moderate |
| Proxy Respondents (Varies) | Information Missing | Information Missing | Lower than self-respondents | Varies |
| Spouse Proxy | Information Missing | Information Missing | Highest among proxies | Information Missing |
| Parent Proxy | Information Missing | Information Missing | Lowest among proxies | Information Missing |
The Scientist's Toolkit: Essential Reagents & Materials
Beyond statistical methods, robust research requires specific "reagents" and tools. The following table details key resources for conducting high-quality psychometric and reproducible research.
Table 3: Essential Research Reagents and Tools for Psychometric and Reproducible Research
| Item Name | Function/Application | Technical Specifications / Examples |
|---|---|---|
| Qualitative Data Analysis Software | Aids in organizing, coding, and analyzing qualitative data from interviews and focus groups. | MAXQDA, NVivo. Used for retrieving encoded data and managing qualitative datasets [29]. |
| Statistical Software Suite | Performs essential psychometric statistical analyses, including factor analysis and reliability testing. | IBM SPSS, JASP, R (with irr package for ICC). Used for EFA, Cronbach's alpha, and ICC calculations [29] [71] [72]. |
| Data Visualization & Dashboard Tools | Creates interactive dashboards and visualizations to present healthcare data trends and patterns effectively. | Microsoft Excel, ParaView, Gephi, Tableau. Used for building analytical and strategic dashboards for data presentation [72]. |
| Cloud-Based Collaboration Platforms | Facilitates scientific reproducibility by hosting graphics, sharing underlying data, and enabling discussion among collaborators. | Platforms like Gephi and ParaView can serve this function, ensuring transparency and teamwork [70] [72]. |
| Standardized Psychometric Protocols | Provides a methodological framework for establishing the validity and reliability of a newly developed scale. | Includes defined procedures for assessing Content Validity Ratio (CVR), Content Validity Index (CVI), and conducting Exploratory Factor Analysis (EFA) [29] [10]. |
Visualization and Data Transparency Protocols
Effectively communicating complex data and methodologies is a critical part of overcoming limitations. Data visualization techniques are not merely illustrative; they are analytical tools that can simplify complex information, reveal patterns, and facilitate shared understanding among diverse stakeholders [72].
Implementation Strategies:
- Interactive Dashboards: Develop dashboards that provide real-time data (active), display trends over time (strategic), or present advanced analytics. These were crucial for monitoring parameters like oxygen saturation during the COVID-19 pandemic and can be adapted for tracking recruitment or data quality in large-scale studies [72].
- Standardized Workflow Diagrams: Use clear, standardized diagrams to map out complex research workflows, such as the psychometric validation process outlined in Section 3.1. This enhances reproducibility and clarity.
- Adherence to Accessibility Standards: When creating visualizations, ensure sufficient color contrast between foreground elements (text, lines) and their backgrounds. For standard text, a contrast ratio of at least 7:1 is recommended, and for large text, at least 4.5:1 [73] [74]. This ensures accessibility for all readers, including those with visual impairments.
The following diagram synthesizes the core strategies discussed in this guide into a unified framework for robust research.
Establishing Rigor: Validation Standards and Comparative Tool Analysis
Benchmarks for Psychometric Excellence in Health Measurement
Psychometrics provides the scientific foundation for developing and evaluating measurement instruments in health research. In the specific context of reproductive health surveys, rigorous psychometric validation is essential to ensure that researchers, clinicians, and policymakers obtain accurate, reliable, and meaningful data about women's health status, needs, and outcomes. The fundamental goal of psychometric evaluation is to demonstrate that an instrument consistently measures what it claims to measure across diverse populations and settings. Without proper validation, reproductive health surveys risk producing misleading results that could negatively impact clinical care, resource allocation, and policy decisions.
The development of reproductive health instruments has evolved significantly, with recent studies emphasizing culturally-specific adaptations and population-targeted approaches. For instance, researchers have developed specialized instruments for women with premature ovarian insufficiency, married adolescent women, and female shift workers, recognizing that each group experiences unique reproductive health challenges [10] [23] [20]. This specialization reflects a growing understanding that reproductive health is multidimensional, encompassing physical, psychological, social, and environmental factors that cannot be adequately captured with generic instruments. The field continues to advance through the application of sophisticated statistical methods and rigorous validation protocols that establish the credibility and utility of health measurement tools.
Core Psychometric Properties and Their Quantitative Benchmarks
Psychometric excellence is demonstrated through multiple validation phases, each with specific quantitative benchmarks and statistical thresholds. The following table summarizes the essential psychometric properties with their corresponding excellence benchmarks:
Table 1: Essential Psychometric Properties and Excellence Benchmarks
| Psychometric Property | Statistical Measures | Benchmarks for Excellence | Interpretation |
|---|---|---|---|
| Reliability | Cronbach's alpha | ≥ 0.7 (Acceptable), ≥ 0.8 (Good), ≥ 0.9 (Excellent) [10] [32] [20] | Internal consistency of items |
| Intraclass Correlation Coefficient (ICC) | 0.5-0.75 (Moderate), 0.76-0.9 (Good), >0.9 (Excellent) [48] | Test-retest stability | |
| Validity | Content Validity Index (CVI) | ≥ 0.78 per item, ≥ 0.90 overall [10] [17] | Item relevance assessment |
| Content Validity Ratio (CVR) | ≥ 0.62 (for 10 experts) [10] [20] | Item essentiality | |
| Aiken's V Coefficient | > 0.80 [17] | Expert agreement on items | |
| Construct Validity | KMO Measure | ≥ 0.8 [10] [48] | Sampling adequacy for factor analysis |
| Factor Loadings | ≥ 0.3 (Minimum), ≥ 0.4 (Important), ≥ 0.5 (Significant) [20] | Item-factor relationships | |
| RMSEA | < 0.08 (Acceptable), < 0.05 (Good) [17] | Model fit in confirmatory analysis |
Advanced Quantitative Standards
Beyond the fundamental thresholds, advanced psychometric evaluations employ more sophisticated statistical approaches. Item Response Theory (IRT) and Rasch analysis provide granular insights into item-level performance and measurement precision [17]. For example, the MatCODE and MatER questionnaires demonstrated excellent fit values in Rasch analysis (RMSEA = 0.113 and 0.067 respectively), confirming their unidimensionality [17]. Similarly, exploratory factor analysis should explain a substantial proportion of total variance, with studies in reproductive health research typically achieving 54-56% of variance explained through identified factors [32] [20].
The standard error of measurement (SEM) provides crucial information about the precision of individual scores. In the Mental Health Literacy Scale for reproductive-age women, researchers reported an SEM of 4.68, which helps establish the confidence interval around obtained scores [32]. For known-groups validity, effect size metrics such as Cohen's d (0.2 = small, 0.5 = medium, 0.8 = large) and eta squared (η²) determine the instrument's ability to discriminate between clinically distinct groups [75].
Methodological Protocols for Psychometric Validation
Instrument Development and Content Validation
The initial phase of scale development requires systematic item generation and content validation through structured protocols:
Item Generation: Develop preliminary item pools through comprehensive literature reviews (e.g., reviewing sources from 1950-2021 across multiple databases) [10] and qualitative explorations (e.g., in-depth interviews with 21-34 target population members) [23] [20]. Transcribe and analyze interviews using conventional content analysis to identify key domains and concepts [20].
Content Validation: Convene a panel of 10-12 experts with complementary expertise (e.g., reproductive health, midwifery, gynecology, occupational health) [20]. Experts evaluate items using structured rating scales for clarity, relevance, and essentiality. Calculate CVI and CVR for each item, retaining only those meeting excellence benchmarks [10] [20].
Cognitive Interviewing: Conduct interviews with 16-27 target population members to assess comprehension, interpretation, and acceptability of items [17] [48]. Revise problematic items based on feedback to enhance face validity and cultural appropriateness.
Construct Validation and Reliability Assessment
The subsequent phase employs quantitative methods to empirically verify the theoretical construct and establish reliability:
Factor Analysis Protocol: Administer the preliminary instrument to 300-620 participants, ensuring a minimum ratio of 15 observations per item [17] [20]. Perform exploratory factor analysis using maximum likelihood estimation with equimax rotation [20]. Determine factor retention through parallel analysis, scree plots, and eigenvalues >1. Confirm the factor structure through confirmatory factor analysis in a separate validation sample, reporting multiple fit indices (CFI, GFI, RMSEA, CMIN/DF) [20].
Reliability Testing Protocol: Assess internal consistency by calculating Cronbach's alpha for the total scale and each subscale [10] [20]. Establish test-retest reliability by readministering the instrument to a subset of participants after 2-4 weeks [23] or 3 months [48]. Calculate ICC using two-way mixed effects models with absolute agreement [32] [48].
The Researcher's Toolkit: Essential Methodological Reagents
Table 2: Essential Methodological Reagents for Psychometric Validation
| Research Reagent | Function | Exemplary Application |
|---|---|---|
| Expert Panel | Evaluate content relevance, comprehensiveness, and representativeness | 10-12 multidisciplinary experts assessing item essentiality via CVR [20] |
| Target Population Sample | Provide data for psychometric analysis and ensure ecological validity | 620 women shift workers for factor analysis [20]; 185 women for maternal health tool validation [17] |
| Validated Comparator Instruments | Establish convergent and discriminant validity | Using Resilience Scale (RS-14), PANAS, and Maternity Beliefs Scale for divergent validity [17] |
| Statistical Software Packages | Perform advanced psychometric analyses | STATA for confirmatory factor analysis [48]; specialized software for Rasch analysis [17] |
| Cognitive Interview Protocol | Identify problems with comprehension, recall, and sensitivity | 16 women evaluating Reproductive Autonomy Scale items for understanding [48] |
Emerging Paradigms: Beyond Traditional Benchmarking
Contemporary psychometric science recognizes the limitations of overreliance on traditional benchmarking approaches. Benchmark-based evaluation often suffers from inadequate explanatory and predictive power, failing to explain how or why measurement instruments might fail in specific circumstances [76]. This is particularly problematic in reproductive health, where cultural contexts, relationship dynamics, and socioeconomic factors significantly influence measurement accuracy.
The emerging paradigm of construct-oriented evaluation addresses these limitations by focusing on underlying constructs rather than performance on specific benchmark tasks [76]. This approach employs modern psychometric techniques like factor analysis to identify core constructs that account for variance in performance. For example, Burnell et al. extracted three factors (reasoning, comprehension, and core language modeling) that accounted for 82% of variance in LLM performance across 27 cognitive tasks [76]. Similarly, reproductive health research can identify fundamental constructs that transcend specific populations or settings.
Alternative assessment formats including practical, observational, situational, and interactive assessments provide complementary approaches to traditional self-report measures [76]. For instance, empathy—a crucial component of patient-centered reproductive care—can be assessed through simulated clinical conversations rather than knowledge examinations [76]. These approaches are less susceptible to data contamination and may better capture real-world competencies essential for quality healthcare.
Psychometric excellence in reproductive health measurement requires meticulous attention to established benchmarks across multiple validation domains. By adhering to rigorous methodological protocols, employing appropriate statistical reagents, and embracing emerging paradigms that address the limitations of traditional benchmarking, researchers can develop instruments that generate valid, reliable, and meaningful data. Such rigorously validated tools are essential for advancing reproductive health research, improving clinical care, informing policy decisions, and ultimately enhancing health outcomes for diverse populations of women across the reproductive lifespan.
Comparative Analysis of Existing Reproductive Health Scales
Reproductive health (RH) is a critical component of overall well-being, encompassing physical, emotional, mental, and social aspects related to the reproductive system. The accurate assessment of reproductive health status, needs, and outcomes relies heavily on validated measurement instruments. Within the context of psychometric properties research, this technical guide provides a comprehensive comparative analysis of existing reproductive health scales, examining their development methodologies, psychometric properties, and applications across diverse populations. The increasing recognition that reproductive health extends beyond mere biological functioning to include empowerment, autonomy, and literacy has driven the development of specialized instruments tailored to specific populations and constructs. This analysis synthesizes current research on reproductive health scales, focusing on their quantitative measurement properties and methodological frameworks to guide researchers, scientists, and drug development professionals in selecting, adapting, and implementing appropriate assessment tools.
Methodology of Scale Identification and Analysis
Search Strategy and Selection Criteria
The comparative analysis incorporated a systematic approach to identify relevant reproductive health scales. The search strategy focused on peer-reviewed literature published across multiple databases including PubMed, Scopus, Google Scholar, and specialized journals such as Reproductive Health and BMJ Sexual & Reproductive Health. Search terms included combinations of "reproductive health," "scale," "instrument," "questionnaire," "psychometric properties," "validation," "reliability," and specific constructs such as "autonomy," "empowerment," "literacy," and "satisfaction." Articles were included if they: (1) described the development or validation of a reproductive health scale; (2) reported psychometric properties including reliability and validity metrics; (3) were published in English; and (4) provided sufficient methodological detail for comparative analysis.
Analytical Framework
The analysis employed a structured framework to evaluate each scale across multiple dimensions: (1) Conceptual Foundation - theoretical underpinnings and construct definition; (2) Development Methodology - procedures for item generation, refinement, and validation; (3) Psychometric Properties - reliability indices (internal consistency, test-retest) and validity evidence (content, construct, criterion); (4) Population Applicability - target populations and cultural adaptations; and (5) Practical Utility - administration characteristics, scoring procedures, and implementation requirements. This multidimensional framework enabled systematic comparison across diverse instruments and identification of strengths and limitations specific to research contexts.
Comprehensive Comparison of Reproductive Health Scales
Table 1: Comparative Analysis of Reproductive Health Scale Psychometric Properties
| Scale Name | Target Population | Item Number (Final) | Factor Structure | Reliability (Cronbach's α) | Validity Evidence |
|---|---|---|---|---|---|
| SRH-POI [10] | Women with Premature Ovarian Insufficiency | 30 | 4 factors | 0.884 | Content validity (S-CVI: 0.926), Construct validity (EFA: KMO=0.83) |
| Reproductive Health Literacy Scale [77] | Refugee women | Domain-specific | 3 domains: General, Digital, and RH literacy | >0.7 (all domains) | Content validity, Face validity, Criterion validity |
| SRE Scale for AYAs (Chinese version) [46] | Chinese adolescents and young adults | 21 | 6 dimensions | 0.89 | Content validity (S-CVI: 0.96), Construct validity (CFA: CFI=0.91, RMSEA=0.07) |
| Reproductive Autonomy Scale (UK version) [9] | Women of reproductive age (UK) | Not specified | 3 factors (confirmed) | 0.75 | Construct validity (CFA), Criterion validity |
| RH Assessment Scale for HIV+ Women [29] | HIV-positive women | 36 | 6 factors | 0.713 | Content validity (CVR, CVI), Construct validity (EFA) |
| QD-BES Scale [78] | Postpartum women (LMICs) | 10 | 3 dimensions: Emotional satisfaction, Support/respect, Communication | 0.70-0.90 | Construct validity (EFA, CFA: CFI=0.95) |
| WoRA-MHL Scale [32] | Women of reproductive age | 30 | 4 themes: Accessing information, Understanding information, Maintaining health, Adapting to challenges | 0.889 | Content validity, Construct validity (EFA, CFA) |
Table 2: Scale Development Methodologies and Administration Characteristics
| Scale Name | Development Approach | Item Generation Methods | Response Format | Administration Mode | Cultural Adaptations |
|---|---|---|---|---|---|
| SRH-POI [10] | Sequential exploratory mixed-method | Literature review (1950-2021), Qualitative study | 5-point Likert scale | Self-administered | Developed specifically for POI population |
| Reproductive Health Literacy Scale [77] | Domain aggregation and adaptation | Literature review, Existing scale adaptation | 4-point Likert scale | Interviewer-administered | Translated to Dari, Arabic, Pashto; culturally adapted for refugees |
| SRE Scale for AYAs (Chinese version) [46] | Cross-cultural translation and adaptation | Brislin translation model, Expert consultation | Not specified | Self-administered | Extensive cultural adaptation for Chinese context |
| Reproductive Autonomy Scale (UK version) [9] | Cross-cultural validation | Original US scale adaptation | Not specified | Online survey | Validated for UK population |
| RH Assessment Scale for HIV+ Women [29] | Exploratory mixed-methods design | Semi-structured interviews, Focus groups, Literature review | 5-point Likert scale | Interviewer-administered | Developed for HIV-positive women in Iranian context |
| QD-BES Scale [78] | Systematic tool development | Existing tool identification and assessment | Not specified | Postpartum exit survey | Validated in 4 LMICs (Argentina, Burkina Faso, Thailand, Vietnam) |
| WoRA-MHL Scale [32] | Mixed method study | Qualitative studies, Literature review, Systematic item generation | Not specified | Self-administered | Developed for reproductive-age women |
Scale Development Methodologies
The analyzed scales demonstrate diverse methodological approaches to development and validation. The SRH-POI Scale employed a sequential exploratory mixed-method design, beginning with comprehensive literature review (sources from 1950-2021) and qualitative components to develop preliminary items, followed by psychometric evaluation including exploratory factor analysis [10]. Similarly, the RH Assessment Scale for HIV+ Women utilized an exploratory mixed-methods design with an initial qualitative phase involving semi-structured interviews and focus groups to determine components of sexual and reproductive health, followed by quantitative psychometric analysis [29].
The Reproductive Health Literacy Scale took a distinctive approach by aggregating and adapting existing validated instruments across three domains: general health literacy (HLS-EU-Q6), digital health literacy (eHEALS), and reproductive health literacy (C-CLAT and ReproNet postpartum literacy scale) [77]. This methodology leveraged previously validated instruments while creating a comprehensive tool specific to refugee populations.
Cross-cultural adaptation methodologies are exemplified by the SRE Scale for AYAs (Chinese version), which employed the Brislin translation model with forward and back-translation, expert consultation, and cultural adaptation to ensure relevance and appropriateness for Chinese adolescents and young adults [46]. The Reproductive Autonomy Scale (UK version) followed a similar cross-cultural validation approach, adapting the original US-developed scale for the UK context while maintaining the original three-factor structure [9].
Psychometric Property Evaluation
The psychometric properties of the scales demonstrate generally strong reliability and validity metrics, though with variation across instruments. The SRH-POI Scale showed excellent internal consistency (Cronbach's α = 0.884) and content validity (S-CVI = 0.926), with construct validity supported by exploratory factor analysis (KMO = 0.83) [10]. The SRE Scale for AYAs (Chinese version) also demonstrated high reliability (Cronbach's α = 0.89) and strong content validity (S-CVI = 0.96), with confirmatory factor analysis supporting the theoretical structure (CFI = 0.91, RMSEA = 0.07) [46].
The Reproductive Autonomy Scale (UK version) showed good internal consistency (Cronbach's α = 0.75) and fair-good test-retest reliability (ICC = 0.67), with construct validity confirmed through hypothesis testing and confirmatory factor analysis [9]. The QD-BES Scale demonstrated variable internal consistency across subscales (α = 0.70-0.90) and good model fit on confirmatory factor analysis (CFI = 0.95), supporting its use in LMIC settings [78].
The WoRA-MHL Scale showed high reliability (Cronbach's α = 0.889, ICC = 0.966) and satisfactory model fit on confirmatory factor analysis, supporting its use for assessing mental health literacy in reproductive-age women [32].
Conceptual Relationships in Reproductive Health Measurement
Diagram 1: Conceptual Framework of Reproductive Health Measurement Tools. This diagram illustrates the relationships between measurement constructs, target populations, and specific assessment scales in reproductive health research.
Experimental Protocols for Scale Development and Validation
Protocol 1: Comprehensive Scale Development with Mixed Methods
Purpose: To develop a novel reproductive health scale when no existing instrument adequately measures the construct in the target population, as exemplified by the SRH-POI Scale [10] and RH Assessment Scale for HIV+ Women [29].
Phase 1: Item Generation
- Conduct systematic literature review across multiple databases (PubMed, Scopus, Google Scholar, etc.) using structured search terms
- Perform qualitative data collection through semi-structured interviews and focus group discussions with target population until saturation achieved
- Transcribe and analyze qualitative data using content analysis methods
- Generate preliminary item pool combining literature-derived and qualitative-derived items
- Conduct research team reviews to eliminate overlapping or similar items
Phase 2: Content and Face Validation
- Assemble expert panel (minimum 10 specialists in relevant field) for content validity assessment
- Calculate Content Validity Ratio (CVR) using Lawshe's table with minimum acceptable values (0.62 for 10 experts)
- Compute Content Validity Index (CVI) for individual items and entire scale (acceptable >0.79)
- Conduct qualitative face validity assessment with target population (n=10) to assess difficulty, appropriateness, and ambiguity
- Perform quantitative face validity using impact score method (items with impact score ≥1.5 retained)
Phase 3: Psychometric Validation
- Administer preliminary scale to larger sample (minimum 5-10 participants per item)
- Conduct Exploratory Factor Analysis (EFA) with Kaiser-Meyer-Olkin (KMO) measure (>0.6 acceptable) and Bartlett's test of sphericity
- Determine factor structure using eigenvalue >1 criterion and scree plot examination
- Perform Varimax rotation for factor simplification and clarity
- Assess internal consistency using Cronbach's alpha (>0.7 acceptable)
- Evaluate test-retest reliability with intraclass correlation coefficients (ICC >0.7 good stability)
Protocol 2: Cross-Cultural Scale Adaptation
Purpose: To adapt an existing reproductive health scale for a different cultural context or language, as demonstrated by the SRE Scale for AYAs (Chinese version) [46] and Reproductive Autonomy Scale (UK version) [9].
Phase 1: Translation and Cultural Adaptation
- Obtain authorization from original scale developers
- Conduct forward translation by two independent bilingual experts
- Review forward translations for linguistic appropriateness by monolingual experts
- Perform back-translation by bilingual experts with medical backgrounds
- Compare back-translated version with original scale for semantic consistency
- Conduct expert reviews (7+ specialists) for cultural relevance and appropriateness
Phase 2: Psychometric Validation in Target Culture
- Administer adapted scale to target population sample (minimum 300 participants)
- Conduct both Exploratory Factor Analysis (EFA) and Confirmatory Factor Analysis (CFA)
- Assess model fit using multiple indices (CFI >0.90, GFI >0.90, RMSEA <0.08, RMR <0.08)
- Evaluate reliability through Cronbach's alpha, split-half reliability, and test-retest methods
- Establish construct validity through hypothesis testing and correlation with related measures
Protocol 3: Domain-Based Scale Aggregation
Purpose: To create a comprehensive scale by aggregating validated existing instruments measuring related domains, as implemented in the Reproductive Health Literacy Scale [77].
Phase 1: Domain Identification and Instrument Selection
- Conduct systematic literature review to identify existing tools measuring target domains
- Apply selection criteria: address training/content topics, align with theoretical framework, report robust psychometrics, validated in similar populations
- Select instruments for each domain: general health literacy (HLS-EU-Q6), digital health literacy (eHEALS), reproductive health literacy (C-CLAT, postpartum literacy scale)
- Maintain original response formats of selected instruments where possible
Phase 2: Integration and Cultural Adaptation
- Assemble selected instruments into single survey with consistent formatting
- Translate complete survey into target languages using bilingual translators
- Pilot survey with bilingual volunteers and target population for understandability
- Assess content validity and face validity of integrated scale
Phase 3: Validation in Target Population
- Administer integrated scale to participants from target population
- Calculate reliability coefficients for each domain separately
- Compare scores across different language/cultural groups within target population
- Establish criterion validity through correlations with relevant outcomes
Essential Research Reagents and Methodological Components
Table 3: Essential Methodological Components for Reproductive Health Scale Development
| Component Category | Specific Element | Function/Application | Exemplary Implementation |
|---|---|---|---|
| Validity Assessment Tools | Content Validity Ratio (CVR) | Evaluates necessity of items from expert perspective | Lawshe's table with minimum acceptable values (0.62 for 10 experts) [10] [29] |
| Content Validity Index (CVI) | Assesses item design quality (simplicity, specificity, clarity) | Items with CVI >0.79 retained; 0.70-0.79 revised; <0.70 eliminated [10] [29] | |
| Impact Score | Quantitative face validity measure | Impact Score = Frequency (%) * Importance; items with score ≥1.5 retained [10] [29] | |
| Statistical Analysis Tools | Kaiser-Meyer-Olkin (KMO) Measure | Sampling adequacy for factor analysis | KMO >0.6 acceptable; 0.83 in SRH-POI Scale development [10] |
| Bartlett's Test of Sphericity | Tests correlation among variables for factor analysis | Significant result indicates sufficient correlation between items [10] | |
| Varimax Rotation | Simplifies and clarifies factor structures in EFA | Orthogonal rotation method used in multiple scale developments [29] | |
| Reliability Assessment Methods | Cronbach's Alpha | Measures internal consistency of scale | α >0.7 acceptable; 0.884 for SRH-POI Scale [10] |
| Intraclass Correlation Coefficient (ICC) | Evaluates test-retest reliability | ICC >0.7 indicates good stability; 0.95 for SRH-POI Scale [10] | |
| Cross-Cultural Adaptation Tools | Brislin Translation Model | Systematic approach to scale translation and back-translation | Used in Chinese adaptation of SRE Scale for AYAs [46] |
| Expert Review Panels | Assess cultural relevance and appropriateness | 7+ experts in medical specialties for SRE Scale adaptation [46] |
This comparative analysis demonstrates significant advancements in reproductive health scale development, with sophisticated methodologies employed to ensure psychometric robustness across diverse populations. The evaluated instruments address a spectrum of constructs from condition-specific health status (SRH-POI, HIV-specific RH) to cross-cutting concepts of autonomy, empowerment, and literacy. The methodological protocols provide structured approaches for developing new instruments, adapting existing ones, and creating comprehensive tools through domain aggregation. Future scale development should emphasize cross-cultural validation, digital administration modalities, and integration with emerging technologies while maintaining rigorous psychometric standards. The continued refinement and appropriate application of these measurement tools will enhance research quality, intervention effectiveness, and ultimately reproductive health outcomes across diverse global populations.
Assessing Measurement Invariance Across Diverse Demographic Groups
Within the specific domain of reproductive health surveys, ensuring that research instruments function equivalently across different demographic groups is a critical prerequisite for valid scientific comparison. Measurement Invariance (MI) testing provides the methodological framework to verify that a scale measures the same underlying construct in the same way across various populations, such as different ethnicities, age groups, or clinical statuses [79] [80]. Without establishing MI, observed score differences between groups may reflect biases in the instrument itself rather than true differences in the latent construct, potentially leading to flawed conclusions in psychometric research and subsequent drug development efforts [81] [82].
This guide provides an in-depth technical protocol for assessing MI, contextualized within reproductive health research. It is designed to equip researchers and scientists with the advanced statistical knowledge required to rigorously validate their instruments, ensuring that comparisons across diverse demographic groups are both meaningful and scientifically sound.
Conceptual Foundations of Measurement Invariance
The Hierarchical Nature of Invariance Testing
Measurement invariance is not an all-or-nothing property but exists on a continuum of increasingly strict statistical constraints. The analysis proceeds sequentially through a series of nested models, where each step imposes additional equality restrictions across groups [81] [83].
- Configural Invariance: This is the most basic level of invariance and establishes that the same factor structure exists across groups. It requires that the same items load onto the same latent factors in all groups, serving as the foundational model for all subsequent tests [81] [84].
- Metric Invariance: Also known as weak invariance, this level tests whether the factor loadings (the strengths of the relationships between items and the latent factor) are equivalent across groups. Establishing metric invariance allows researchers to conclude that participants from different groups attribute the same meaning to the latent construct and that the scale's unit of measurement is equivalent [81] [80].
- Scalar Invariance: Also known as strong invariance, this level tests for the equivalence of item intercepts (the origins of the measurement scales). Without scalar invariance, group differences on the latent construct's mean cannot be meaningfully interpreted, as observed score differences could be contaminated by differential response styles or other biases [81] [82].
- Strict Invariance: This is the most stringent level, requiring that item residuals (unique variances) are equal across groups. Meeting this criterion indicates that the reliability of the items is equivalent across groups. In practice, achieving the first three levels is often considered sufficient for meaningful group comparisons [81].
Consequences of Non-Invariance
Failure to establish measurement invariance has serious implications for reproductive health research. If a survey instrument used to assess sexual distress or attitudes toward reproductive health research functions differently for, say, cancer patients versus non-clinical populations [80], or across different racialized groups [79], then:
- Group mean comparisons become uninterpretable, as differences may stem from measurement artifact rather than true disparity.
- Associations with other variables may be misestimated, potentially biasing models that predict health outcomes or test intervention efficacy.
- Longitudinal comparisons may be invalid, as changes over time could be confounded with measurement instability across subgroups.
Methodological Protocols for Testing Measurement Invariance
Prerequisite: Confirmatory Factor Analysis
A well-fitting measurement model is a mandatory prerequisite for MI testing. This is established via Confirmatory Factor Analysis (CFA) to confirm the hypothesized factor structure within each group separately or in a combined sample [79] [83].
Core Protocol: Baseline CFA Specification The CFA model is specified as follows:
- Model Formulation: The relationship between manifest variables and latent factors is pre-specified, unlike the data-driven approach of Exploratory Factor Analysis (EFA) [81].
- Model Identification: The scale of each latent factor is typically set by fixing one factor loading to 1 (the "marker variable" method) or by fixing the factor variance to 1 [83].
- Fit Assessment: Model fit is evaluated using multiple indices, as the chi-square statistic is overly sensitive to large sample sizes common in this research area [79].
Table 1: Key Model Fit Indices and Their Interpretation
| Fit Index | Abbreviation | Excellent Fit | Acceptable Fit | Primary Interpretation |
|---|---|---|---|---|
| Comparative Fit Index | CFI | > 0.95 | > 0.90 | Compares model to a null model of no covariance |
| Tucker-Lewis Index | TLI | > 0.95 | > 0.90 | A non-normed version of CFI |
| Root Mean Square Error of Approximation | RMSEA | < 0.05 | < 0.08 | Measures misfit per degree of freedom |
| Standardized Root Mean Square Residual | SRMR | < 0.05 | < 0.08 | Average difference between observed and predicted correlations |
Core Workflow: Multi-Group Confirmatory Factor Analysis (MG-CFA)
The primary method for testing MI is Multi-Group Confirmatory Factor Analysis (MG-CFA), which involves estimating and comparing a series of nested models [81].
Figure 1: The Sequential Workflow for Testing Measurement Invariance. Models are tested in order, with increasing constraints. A significant deterioration in fit (ΔFit is Sig) at any step indicates a lack of invariance and may necessitate investigation into partial invariance.
Experimental Protocol for MG-CFA:
Model Specification:
- Define the baseline CFA model using the same factor structure for all groups.
- For example, a model for the 7-item Research Attitudes Questionnaire (RAQ) would be specified as a one-factor model in all groups [79].
Sequential Model Testing:
- Step 1: Test Configural Invariance. Estimate a model where the pattern of fixed and free loadings is identical across groups, but all parameters are free to be estimated. A good fit here indicates the same basic factor structure holds for all groups [79] [84].
- Step 2: Test Metric Invariance. Add constraints so that all factor loadings are equal across groups. Compare this model to the configural model. A non-significant degradation in fit supports metric invariance [81] [80].
- Step 3: Test Scalar Invariance. Add constraints so that all item intercepts are equal across groups. Compare this model to the metric model. A non-significant degradation in fit supports scalar invariance, allowing for valid comparison of latent means [81] [82].
- Step 4: Test Strict Invariance. Add constraints so that all item residual variances are equal across groups. Compare this model to the scalar model. This final step tests for homogeneity of item-level measurement error [81].
Model Comparison and Decision Making:
- The chi-square difference test (Δχ²) is a traditional method for comparing nested models. However, it is highly sensitive to sample size.
- In large samples typical of psychometric studies, reliance on changes in approximate fit indices is recommended [79]. A ΔCFI ≤ -0.010 supplemented by a ΔRMSEA ≥ 0.015 often suggests non-invariance [79].
Handling Partial Measurement Invariance
It is common to find that some, but not all, parameters are invariant. In such cases, partial invariance can be established.
Protocol for Establishing Partial Invariance:
- Identification of Non-Invariant Parameters: After a model shows significant misfit, use modification indices or expected parameter change statistics to identify which specific parameters (loadings or intercepts) are non-invariant.
- Sequential Freeing: Free the parameter with the largest modification index and re-test the model. Repeat this process until the model fit is acceptable.
- Interpretation: If only a small number of parameters are non-invariant, partial invariance is achieved. Comparisons can still be made, but with caution, acknowledging the specific items that function differently across groups [79] [85]. For instance, a study on the Research Attitudes Questionnaire found evidence for partial scalar invariance, which still supported its use for cross-group comparisons [79].
Practical Implementation and Technical Toolkit
Implementation in R withlavaan
The lavaan package in R is a flexible and widely used tool for conducting MG-CFA. The following code block demonstrates the core syntax for testing MI.
Key lavaan Syntax Notes:
group = "group_variable": Specifies the categorical variable that defines the groups for comparison.group.equal: This argument is used to specify which parameters to constrain across groups. The testing sequence requires adding constraints sequentially: first"loadings", then"intercepts".estimator = "WLSMV": This is the recommended estimator for ordinal data (e.g., Likert-scale items commonly used in surveys) [81].
The Researcher's Toolkit for MI Analysis
Table 2: Essential Reagents and Resources for Measurement Invariance Analysis
| Tool Category | Specific Tool/Resource | Function/Purpose | Considerations for Reproductive Health Surveys |
|---|---|---|---|
| Statistical Software | R with lavaan & semTools packages [81] [83] |
Provides a flexible environment for specifying, estimating, and comparing MG-CFA models. | Open-source; allows for complex model specification needed for adapted health scales. |
| Data Management | Qualtrics, REDCap | Used for survey administration and data collection integrity (e.g., catch questions, reverse-scored items) [79]. | Ensures high-quality, clean data; critical for managing multi-site or international studies. |
| Model Specification | Pre-established factor structure from prior validation studies | The theoretical model linking survey items to latent constructs (e.g., sexual distress, research attitudes) [79] [80]. | Must be robust. For new populations, preliminary EFAs may be needed. |
| Instrument | Translated and culturally adapted survey (e.g., SaRDS, RAQ) [79] [80] | The actual measure being validated. Requires transcultural adaptation if used in new linguistic contexts. | Follow WHO translation/adaptation guidelines (e.g., TRAPD model) to minimize non-invariance from linguistic issues [80] [86]. |
Application in Reproductive Health Survey Research
The principles of MI are critically applied in reproductive health research to ensure the validity of instruments across diverse populations.
Exemplar Study 1: Validation of the Sexual and Relationship Distress Scale (SaRDS)
- Context: The SaRDS was translated into Chinese and validated for use among both colorectal cancer (CRC) patients and a nonclinical general population of reproductive-age adults [80].
- MI Analysis: Researchers tested invariance across population groups (CRC vs. nonclinical) and across gender (male vs. female).
- Outcome: The study successfully demonstrated that the factor structure, factor loadings, and item intercepts were invariant across both types of groups. This provides empirical evidence that differences in SaRDS scores between these groups reflect true differences in sexual and relationship distress, rather than measurement bias [80]. This is crucial for accurately assessing the impact of cancer treatment on sexual health.
Exemplar Study 2: Cross-Cultural Application of the Research Attitudes Questionnaire (RAQ)
- Context: The RAQ, used to predict willingness to participate in biomedical research (e.g., Alzheimer's disease studies), was administered to younger and older adults from African American, American Indian/Alaska Native, and non-Hispanic White backgrounds [79].
- MI Analysis: A series of cross-sample invariance tests constrained factor loadings, means, and residuals.
- Outcome: The study found evidence for configural, metric, and partial scalar invariance. This supports the suitability of the RAQ for making meaningful cross-cultural and age-group comparisons regarding attitudes toward research, which is fundamental for addressing disparities in recruitment for clinical trials and biomarker studies [79].
Figure 2: Conceptual Diagram of a Multi-Group CFA Model. The same latent construct is measured by the same items in two groups. Measurement invariance testing examines whether the loadings (λ) and intercepts are equivalent across groups. A non-invariant item (Item 4, in red) would have different statistical properties in Group A versus Group B.
Rigorous assessment of measurement invariance is a fundamental step in the psychometric validation of reproductive health surveys, especially when research aims to compare outcomes across diverse demographic subgroups. The multi-group confirmatory factor analysis framework provides a robust and systematic methodology for this purpose. By adhering to the detailed protocols outlined in this guide—from establishing a baseline model and sequential testing to handling partial invariance—researchers and drug development professionals can produce more valid, reliable, and interpretable findings. This, in turn, strengthens the scientific foundation for understanding health disparities, evaluating interventions, and ensuring that research instruments are equitable and applicable to all populations they intend to serve.
Evaluating Responsiveness and Interpretability of Outcome Measures
In the realm of psychometric validation, responsiveness and interpretability are critical properties that determine whether an outcome measure is suitable for use in clinical research and practice. Within reproductive health research, where accurately capturing patient experiences and changes in health status is paramount, these properties ensure that surveys and instruments produce meaningful, actionable data.
Responsiveness is defined as the ability of an outcome measure to detect change over time in the construct being measured. It evaluates whether an instrument can capture clinically important changes, even if those changes are small. This property is particularly crucial in intervention studies and clinical trials where demonstrating treatment efficacy depends on sensitive measurement tools.
Interpretability refers to the degree to which one can assign qualitative meaning to an instrument's quantitative scores. It involves understanding what a specific score or change in score means in clinical practice, often through metrics like the minimal important change (MIC), which represents the smallest change in score that patients perceive as important. Proper interpretability allows researchers and clinicians to distinguish between statistical significance and clinical relevance [87].
Methodological Frameworks for Evaluation
Established Evaluation Criteria
The Consensus-based Standards for the selection of health Measurement Instruments (COSMIN) methodology provides a rigorous framework for evaluating measurement properties, including responsiveness and interpretability. This systematic approach assesses instruments against defined criteria for construct validity, reliability, measurement error, and responsiveness [88].
When applying the COSMIN criteria to reproductive health surveys, researchers should evaluate:
- Hypothesis testing: Pre-specifying how scores should change following interventions or clinical events
- Longitudinal validity: Assessing relationships between change scores and changes in other measures
- Area under the curve (AUC) analysis: Using receiver operating characteristic curves to distinguish between improved and stable groups
- Minimal Important Change (MIC) determination: Establishing thresholds for clinically meaningful change through anchor-based methods
Experimental Protocols for Assessment
Protocol 1: Responsiveness Evaluation in Intervention Studies
- Participant Recruitment: Include study participants representing the target population (e.g., women using reproductive health services)
- Baseline Assessment: Administer the outcome measure at study initiation
- Follow-up Assessment: Re-administer the measure after a clinically relevant time interval or following a known-effective intervention
- External Criterion Collection: Collect global rating of change scales from patients and clinicians
- Statistical Analysis:
- Calculate correlation between change scores and external criteria
- Perform AUC analysis to determine the instrument's ability to discriminate between changed and unchanged patients
- Compute effect sizes (standardized response means) for change scores
Protocol 2: Establishing Minimal Important Change (MIC)
- Anchor Selection: Identify an appropriate external indicator of meaningful change (e.g., patient global impression of change scales)
- Data Collection: Administer both the outcome measure and anchor questionnaire at baseline and follow-up
- Respondent Categorization: Classify patients as "changed" or "unchanged" based on anchor responses
- MIC Calculation:
- Use receiver operating characteristic (ROC) curve analysis to identify the change score that best distinguishes between "changed" and "unchanged" patients
- Calculate the optimal cut-off point that maximizes both sensitivity and specificity
- Report the MIC value with its associated sensitivity and specificity metrics [87]
Quantitative Standards and Data Presentation
Psychometric Standards for Reproductive Health Measures
Table 1: Quantitative Standards for Responsiveness and Interpretability Evaluation
| Psychometric Property | Statistical Method | Threshold for Sufficiency | Application in Reproductive Health |
|---|---|---|---|
| Responsiveness | Area Under Curve (AUC) | AUC > 0.7 indicates adequate responsiveness | The Reproductive Autonomy Scale demonstrated sufficient responsiveness for detecting changes in contraceptive use autonomy [9] |
| Internal Consistency | Cronbach's Alpha | α ≥ 0.7 indicates acceptable consistency | The SRH-POI scale showed excellent internal consistency with α = 0.884 [10] |
| Test-Retest Reliability | Intraclass Correlation | ICC ≥ 0.7 indicates adequate stability | The Reproductive Autonomy Scale demonstrated fair-good test-retest reliability with ICC = 0.67 [9] |
| Minimal Important Change | ROC Curve Analysis | MIC should exceed measurement error | The DEMMI mobility index established population-specific MIC values to interpret meaningful change [87] |
| Floor/Ceiling Effects | Percentage at extremes | <15% of respondents at minimum/maximum scores | The KOOS-PF patellofemoral scale demonstrated 0% floor and ceiling effects, supporting its interpretability [88] |
Data Interpretation Guidelines
Table 2: Framework for Evaluating Responsiveness Evidence
| Evidence Level | Statistical Criteria | Interpretation in Clinical Studies |
|---|---|---|
| Strong Evidence | AUC ≥ 0.8 AND correlation with anchor ≥ 0.5 | Instrument is highly recommended for detecting change in clinical trials |
| Moderate Evidence | AUC 0.7-0.79 OR correlation with anchor 0.3-0.49 | Instrument shows acceptable responsiveness for group-level measurement |
| Limited Evidence | AUC < 0.7 AND correlation with anchor < 0.3 | Instrument has insufficient responsiveness for clinical application |
| Conflicting Evidence | Mixed results across different methods | Requires further validation in specific populations |
Application in Reproductive Health Research
Case Study: Reproductive Autonomy Scale
The evaluation of the Reproductive Autonomy Scale (RAS) for use in the UK demonstrates comprehensive assessment of psychometric properties. Researchers assessed responsiveness through hypothesis testing, confirming that women who wanted to avoid pregnancy and had higher reproductive autonomy scores were more likely to use contraception. The scale demonstrated acceptable internal consistency (Cronbach's α = 0.75) and test-retest reliability (ICC = 0.67) [9].
The RAS evaluation followed a rigorous methodology:
- Participant Recruitment: 826 women of reproductive age completed the survey
- Longitudinal Assessment: Sub-sample retested after 3 months for reliability
- Construct Validation: Confirmatory factor analysis confirmed the three-factor structure
- Responsiveness Testing: Hypothesis testing confirmed expected relationships with contraceptive use
Case Study: Sexual and Reproductive Health Scale for Premature Ovarian Insufficiency (SRH-POI)
The development of the SRH-POI scale exemplifies robust instrument validation for a specific reproductive health population. Researchers employed a sequential exploratory mixed-method design with both qualitative and quantitative phases. The final 30-item instrument demonstrated excellent psychometric properties, including high internal consistency (Cronbach's α = 0.884) and strong test-retest reliability (ICC = 0.95) [10].
The validation process included:
- Item Generation: Comprehensive literature review and qualitative interviews produced 84 initial items
- Content Validation: Expert panels evaluated content validity (CVI = 0.926)
- Factor Analysis: Exploratory factor analysis reduced items to 30 across four factors
- Reliability Testing: Excellent internal consistency and test-retest reliability established
Assessment Workflow and Methodological Integration
Psychometric Assessment Workflow
Research Reagent Solutions for Outcome Validation
Table 3: Essential Methodological Components for Responsiveness Assessment
| Research Component | Function in Evaluation | Implementation Example |
|---|---|---|
| Global Rating of Change Scales | Serves as external criterion for assessing meaningful change | Patients rate their change in condition on a 7-point scale from "much worse" to "much better" to anchor MIC calculations [87] |
| Structured Intervention | Provides known-effective treatment to create expected change | Contraceptive counseling intervention for evaluating reproductive autonomy measures [9] |
| Retest Interval Protocol | Establishes appropriate timeframe for reliability assessment | 3-month retest interval used for Reproductive Autonomy Scale to evaluate stability [9] |
| ROC Curve Analysis | Determines optimal cut-points for minimal important change | Used to establish DEMMI mobility index MIC values in older patients [87] |
| Cognitive Interviewing | Ensures respondents understand items as intended | Identifies problematic items in reproductive health surveys before quantitative validation [10] |
Implications for Reproductive Health Research
The rigorous evaluation of responsiveness and interpretability is particularly crucial in reproductive health research due to several field-specific considerations:
- Sensitivity to Change: Reproductive health outcomes often change gradually, requiring instruments sensitive to small but clinically important differences
- Patient-Centered Care: Reproductive autonomy and patient preferences are central to care decisions, necessitating measures that capture these constructs meaningfully
- Legal and Policy Implications: With evolving reproductive health legislation, valid measures are needed to assess the impact of policy changes on health outcomes [89]
Future directions in reproductive health survey development should emphasize:
- Digital Administration: Ensuring responsiveness and interpretability are maintained in electronic and mobile formats
- Cross-Cultural Validation: Establishing measurement invariance across diverse populations
- Integration with Clinical Outcomes: Linking patient-reported outcomes with clinical biomarkers and health records
- Dynamic Assessment: Developing computerized adaptive testing to improve precision and reduce respondent burden
By adhering to rigorous methodological standards for evaluating responsiveness and interpretability, researchers can ensure that reproductive health surveys generate valid, meaningful data to inform clinical practice, policy decisions, and further research.
Implementing COSMIN Standards for Comprehensive Psychometric Assessment
The Consensus-based Standards for the selection of health Measurement Instruments (COSMIN) initiative provides a standardized framework for developing and evaluating patient-reported outcome measures (PROMs), addressing a critical need for methodological rigor in health measurement [90]. In the specialized field of reproductive health survey research, where constructs like sexual function, reproductive autonomy, and fertility concerns are complex and multidimensional, implementing COSMIN standards ensures that measurement instruments possess robust psychometric properties. This technical guide examines the application of COSMIN methodology within reproductive health research, providing researchers with evidence-based protocols for developing and validating instruments that yield reliable, valid, and interpretable data.
The necessity for COSMIN-implemented instruments is particularly pronounced in reproductive health, where a systematic review of sexual and reproductive health knowledge tools for adolescents found the overall methodological quality "Inadequate" per COSMIN standards [22]. Similarly, a review of tools for women with type 1 diabetes mellitus identified 14 psychometrically valid instruments, yet none possessed all features noted in COSMIN, and all lacked interpretability and accountability [91]. These deficiencies highlight the imperative for standardized methodology in field-specific instrument development.
Core COSMIN Methodology and Framework
The COSMIN Framework Structure
The COSMIN initiative employs a structured approach to evaluate measurement instruments across multiple psychometric domains, with particular emphasis on content validity as the most crucial property [92]. The framework systematically assesses: (1) structural validity, (2) internal consistency, (3) cross-cultural validity, (4) reliability, (5) measurement error, (6) criterion validity, (7) construct validity, and (8) responsiveness [92]. This comprehensive coverage ensures that instruments measure what they intend to measure accurately and consistently across diverse populations and settings.
A key innovation of the COSMIN approach is its Risk of Bias checklist, which enables standardized quality assessment of development studies [92]. According to COSMIN methodology, evaluation begins with assessing the quality of instrument development using COSMIN Box 3, followed by evaluation of content validity studies using COSMIN Box 2, before the content validity itself is evaluated [92]. This sequential, systematic approach ensures that fundamental development processes are rigorously examined before other measurement properties.
Application to Reproductive Health Constructs
In reproductive health research, COSMIN standards help address field-specific challenges, including culturally sensitive topics, varying health literacy levels, and the need for gender-responsive approaches. The framework's emphasis on target population involvement during content validity assessment is particularly valuable for ensuring reproductive health instruments reflect the lived experiences and priorities of affected individuals. Studies developing reproductive health scales for HIV-positive women [29], women with premature ovarian insufficiency [10], and women shift workers [20] have demonstrated the adaptability of COSMIN methodology to diverse reproductive health contexts.
Figure 1: COSMIN Systematic Review Process for Reproductive Health Instruments
Implementing COSMIN Standards: Methodological Protocols
Content Validity Assessment Protocol
Objective: To ensure the instrument adequately reflects the construct of interest and is comprehensive for the target population.
Procedure:
- Item Generation: Combine qualitative approaches (interviews, focus groups) with literature review to develop preliminary items [29] [10]. For reproductive health scales, conduct semi-structured interviews with affected individuals until data saturation is achieved [20] [93].
- Target Population Involvement: Recourse participants representing the diversity of the intended population. In studies developing reproductive health scales, include 10-25 participants with the health condition [29] [20].
- Expert Evaluation: Convene a panel of 10-16 content experts to evaluate item relevance using Content Validity Ratio (CVR) and Content Validity Index (CVI) [29] [20] [93].
- Cognitive Interviewing: Conduct interviews with target population members to assess comprehensibility, comprehensiveness, and relevance of items.
Quality Metrics:
- CVR: According to Lawshe's table, minimum acceptable values are 0.62 for 10 experts [29] and 0.64 for 10 experts in other studies [20].
- CVI: Item-level CVI > 0.79 is acceptable; between 0.70-0.79 requires revision; below 0.70 necessitates removal [29] [93].
- Scale-level CVI: Average of I-CVIs, with 0.90+ indicating excellent content validity [10].
Structural Validity and Internal Consistency Protocol
Objective: To verify the hypothesized factor structure and evaluate how well items measure the same construct.
Procedure:
- Sample Size Determination: Recruit approximately 10 participants per item for exploratory factor analysis [93], with minimum samples of 300-620 participants as used in reproductive health scale development [20] [93].
- Factor Analysis Suitability: Assess using Kaiser-Meyer-Olkin (KMO) measure (>0.8 acceptable) [20] and Bartlett's test of sphericity (significant at p<0.05).
- Factor Extraction: Employ principal component analysis with varimax rotation [93] or maximum likelihood estimation with equimax rotation [20].
- Factor Retention: Use eigenvalue >1 criterion combined with parallel analysis and scree plot examination.
- Internal Consistency Assessment: Calculate Cronbach's alpha for the total scale and subscales.
Quality Metrics:
- Factor loadings: >0.3 considered acceptable [20] [93]; >0.4 preferred.
- Total variance explained: >50% considered adequate [93].
- Cronbach's alpha: >0.7 acceptable [29] [20]; 0.8-0.9 preferred.
Reliability and Measurement Error Protocol
Objective: To evaluate the instrument's stability and precision over time.
Procedure:
- Test-Retest Reliability: Administer the same instrument to the same participants under similar conditions with a 2-week interval [29] [93].
- Statistical Analysis: Calculate Intraclass Correlation Coefficient (ICC) for continuous measures.
- Interpretation: ICC values >0.7 indicate acceptable stability [29]; >0.8 considered excellent [93].
Quality Metrics:
- ICC values: >0.7 good stability; 0.5-0.75 average; <0.5 poor [29].
- Measurement error: Assessed through standard error of measurement or limits of agreement.
Table 1: Psychometric Standards for Reproductive Health Measurement Instruments
| Measurement Property | COSMIN Standard | Application in Reproductive Health | Statistical Thresholds |
|---|---|---|---|
| Content Validity | Comprehensive assessment of relevance, comprehensiveness, and comprehensibility | Mixed-methods approach with target population interviews [29] [10] [20] | CVI > 0.79 [29]; CVR > 0.62 [29]; Impact score ≥ 1.5 [10] |
| Structural Validity | Factor analysis demonstrating hypothesized structure | EFA/CFA with reproductive health populations [20] [93] | KMO > 0.8 [20]; Factor loadings > 0.3 [20]; Variance explained > 50% [93] |
| Internal Consistency | Items measuring same construct | Cronbach's alpha calculation for reproductive health domains [29] [20] [93] | α > 0.7 acceptable [29]; α > 0.8 preferred [29] |
| Reliability | Stability over time | Test-retest in reproductive health populations with 2-week interval [29] [93] | ICC > 0.7 good [29]; ICC > 0.8 excellent [93] |
| Construct Validity | Relationships with other measures as hypothesized | Hypothesis testing (e.g., contraceptive use with reproductive autonomy) [94] | Correlation coefficients supporting hypotheses [94] |
Experimental Applications in Reproductive Health Research
Case Example: Reproductive Health Scale for HIV-Positive Women
A sequential exploratory mixed-methods study developed and validated a reproductive health assessment scale for HIV-positive women, demonstrating comprehensive COSMIN implementation [29]. The instrument development phase included 25 HIV-positive women in semi-structured interviews and focus group discussions. Psychometric evaluation yielded a 36-item scale with six factors: disease-related concerns, life instability, coping with the illness, disclosure status, responsible sexual behaviors, and need for self-management support [29].
Psychometric performance demonstrated strong results with Cronbach's alpha of 0.713 and test-retest intraclass correlation of 0.952 [29]. The methodological rigor included assessment of face validity, content validity (CVR, CVI), and construct validity through exploratory factor analysis with KMO index adequacy testing [29]. This case exemplifies appropriate application of COSMIN standards for a vulnerable population with specific reproductive health concerns.
Case Example: Women Shift Workers' Reproductive Health Questionnaire
This study developed a comprehensive reproductive health assessment tool for women shift workers using COSMIN-informed methodology [20]. The qualitative phase included 21 interviews with women shift workers until data saturation, followed by psychometric evaluation with 620 participants. Exploratory factor analysis revealed five factors explaining 56.50% of total variance: motherhood, general health, sexual relationships, menstruation, and delivery [20].
The reliability assessment demonstrated strong internal consistency (Cronbach's alpha > 0.7) and composite reliability values exceeding 0.7 [20]. The study employed advanced statistical validation including confirmatory factor analysis with multiple goodness-of-fit indices (RMSEA, CFI, GFI, etc.), convergent validity through average variance extracted, and discriminant validity assessment [20]. This represents a sophisticated application of COSMIN standards for an occupational health population with unique reproductive health considerations.
Figure 2: Content Validity Assessment Workflow for Reproductive Health Instruments
Research Reagent Solutions: Methodological Tools
Table 2: Essential Methodological Reagents for COSMIN-Implemented Studies
| Research Reagent | Function | Application Example | Quality Threshold |
|---|---|---|---|
| Target Population Participants | Provide lived experience for content validity | 21 women shift workers [20]; 25 HIV-positive women [29] | Data saturation; maximum variation sampling |
| Expert Panel | Evaluate content relevance and comprehensiveness | 10-16 reproductive health specialists [20] [93] | Multidisciplinary representation; >10 years experience |
| COSMIN Risk of Bias Checklist | Standardized quality assessment of measurement properties | Systematic review of sexual health literacy measures [92] | Comprehensive evaluation across 8 measurement properties |
| Statistical Software (EFA/CFA) | Factor analysis for structural validity | Exploratory factor analysis with Varimax rotation [20] [93] | KMO >0.8; significant Bartlett's test; factor loadings >0.3 |
| Reliability Assessment Package | Internal consistency and stability analysis | Cronbach's alpha and test-retest ICC [29] [20] [93] | α >0.7; ICC >0.7 |
Discussion and Future Directions
The implementation of COSMIN standards in reproductive health survey research addresses significant methodological gaps identified in current literature. A systematic review of sexual health literacy self-report measures for adolescents found that despite 83 studies examining 68 different outcome measurement instruments, development quality was generally "inadequate or doubtful" [92]. Common deficiencies included insufficient involvement of target populations and inadequate piloting processes [92]. Similarly, a rapid review of sexual health knowledge tools for adolescents found only one instrument, the Sexual Health Questionnaire (SHQ), demonstrated robustness in multiple areas including construct validity (explaining 68.25% of variance) and internal consistency (Cronbach's alpha: 0.90) [22].
Future development of reproductive health measurement instruments should prioritize comprehensive content validity assessment with substantive target population involvement, longitudinal validation to establish responsiveness to change, and cross-cultural adaptation for global applicability. The COSMIN methodology provides the rigorous framework necessary to advance reproductive health measurement, ultimately strengthening the evidence base for interventions and policies affecting diverse populations across the reproductive lifespan.
As reproductive health research continues to evolve, implementation of COSMIN standards will ensure that measurement instruments meet methodological rigor sufficient for clinical trials, public health monitoring, and drug development applications where precise measurement of complex constructs is paramount.
Conclusion
The development and validation of reproductive health surveys with strong psychometric properties are fundamental to advancing women's health research and drug development. A rigorous, multi-phase methodology—encompassing comprehensive validity and reliability testing—is essential for creating tools that yield precise, meaningful, and actionable data. Future efforts must focus on refining existing instruments, establishing cross-cultural validity for global research, and enhancing the responsiveness of scales to measure intervention effects accurately. By adhering to high psychometric standards, researchers can generate robust evidence to inform clinical practice, shape health policy, and ultimately improve reproductive health outcomes across diverse populations.
References
- 1. Psychometric Properties [https://www.physio-pedia.com/Psychometric_Properties]
- 2. Table 2, Metrics for evaluation of reliability, validity, and ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK531518/table/ch3.tab1/]
- 3. It Is Time to Take a New Approach to Measuring ... [https://www.guttmacher.org/2025/10/adding-it-up-person-centered-approach-to-measuring-contraceptive-need]
- 4. A Validation Study of the Total Teen Assessment - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12329912/]
- 5. Sexual and Reproductive Health Service Seeking Scale ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-17867-6]
- 6. Strategies to Increase Survey Response Rates From Youth [https://www.childtrends.org/publications/strategies-increase-survey-response-rates-youth]
- 7. A primer on reliability testing of a rating scale - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12331005/]
- 8. Making sense of Cronbach's alpha - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4205511/]
- 9. Evaluation of the psychometric properties ... [https://pubmed.ncbi.nlm.nih.gov/36657958/]
- 10. Sexual and reproductive health assessment scale in women ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-025-02061-7]
- 11. What does Cronbach's alpha mean? | SPSS FAQ - OARC Stats [https://stats.oarc.ucla.edu/spss/faq/what-does-cronbachs-alpha-mean/]
- 12. Cronbach's Alpha: Definition, Calculations & Example [https://statisticsbyjim.com/basics/cronbachs-alpha/]
- 13. Cronbach Alpha Coefficient - an overview [https://www.sciencedirect.com/topics/nursing-and-health-professions/cronbach-alpha-coefficient]
- 14. A Guideline of Selecting and Reporting Intraclass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4913118/]
- 15. Intraclass correlation [https://en.wikipedia.org/wiki/Intraclass_correlation]
- 16. and How It Simplifies Factor Findings Analysis Research [https://www.qualtrics.com/articles/strategy-research/factor-analysis/]
- 17. Psychometric Evaluation of Women's Knowledge of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11508016/]
- 18. The Content Validity of the Cultural Formulation Interview ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6304484/]
- 19. Cultural awareness scale: psychometric properties and ... [https://bmcnurs.biomedcentral.com/articles/10.1186/s12912-025-03181-y]
- 20. Development and psychometric evaluation of the women shift ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-020-00994-9]
- 21. Validation and measurement properties of the Male and ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-024-01795-0]
- 22. Quality and measurement properties of sexual health ... [https://pubmed.ncbi.nlm.nih.gov/38335768/]
- 23. Design and psychometric properties of a questionnaire for ... [https://pubmed.ncbi.nlm.nih.gov/35980622/]
- 24. Quality and measurement properties of sexual health ... [https://www.sciencedirect.com/science/article/pii/S0738399124000405]
- 25. A valid and reliable scale to assess cultural sensibility in ... [https://www.sciencedirect.com/science/article/pii/S0260691721002586]
- 26. The 4 Types of Validity in Research | Definitions & Examples [https://www.scribbr.com/methodology/types-of-validity/]
- 27. Validity, reliability and generalisability [https://www.healthknowledge.org.uk/content/validity-reliability-and-generalisability]
- 28. Reliability vs Validity in Research [https://www.simplypsychology.org/reliability-or-validity.html]
- 29. Development and Psychometric Evaluation of a ... [https://brieflands.com/journals/semj/articles/20464]
- 30. Designing and validation of a reproductive health need ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8800275/]
- 31. Maths and Stats - Reliability, Validity and Reproducibility [https://library.soton.ac.uk/reliability-validity-reproducibility]
- 32. Development and Psychometric Properties of the Mental ... [https://pubmed.ncbi.nlm.nih.gov/40970108/]
- 33. A Cross-Sectional Quantitative Study on Sexual and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8471977/]
- 34. Deriving national and disaggregated estimates for the ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-025-02187-8]
- 35. Psychometric properties in instruments evaluation of ... [https://pubmed.ncbi.nlm.nih.gov/28977189/]
- 36. Reliability and Validity [https://www.testpartnership.com/academy/reliability-validity.html]
- 37. Review Underserved groups access to reproductive services [https://www.sciencedirect.com/science/article/pii/S1877575625000643]
- 38. Exploring the perceptions of health service providers and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10798077/]
- 39. The DHS Program - Qualitative Research [https://dhsprogram.com/What-We-Do/Survey-Types/Qualitative-Research.cfm]
- 40. Women empowerment in reproductive health: a systematic ... [https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-021-01566-0]
- 41. Psychometric properties and refinement of the ... [https://www.sciencedirect.com/science/article/abs/pii/S0010782416304127]
- 42. Development and validation of a survey on reproductive ... [https://www.frontiersin.org/journals/reproductive-health/articles/10.3389/frph.2025.1519896/full]
- 43. A Primer on Factor Analysis in Research using ... [https://rstudio-pubs-static.s3.amazonaws.com/1064415_4457273740634e8b81901636e1371c29.html]
- 44. Confirmatory Factor Analysis (CFA): A Detailed Overview [https://www.statisticssolutions.com/free-resources/directory-of-statistical-analyses/confirmatory-factor-analysis/]
- 45. Factor Analysis | R Programming for Psychometrics [https://bookdown.org/sz_psyc490/r4psychometics/factor-analysis.html]
- 46. Sexual and reproductive empowerment scale for adolescents ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619207/]
- 47. Validity and reliability testing of the Pelvic Pain Impact ... [https://www.nature.com/articles/s41598-025-18269-3]
- 48. Evaluation of the psychometric properties ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10359515/]
- 49. Chapter 13 Methods for Survey Studies - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK481602/]
- 50. Youth Reproductive Health Access Survey 2025 [https://powertodecide.org/yourhealthsurvey]
- 51. Tips from an expert panel on the development of a clinical ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02315-1]
- 52. Development and psychometric properties of surveys to ... [https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-021-06766-w]
- 53. Measuring Patient Experiences of Integration in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8205402/]
- 54. Designing, Conducting, and Reporting Survey Studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC10713437/]
- 55. Scale development: ten main limitations and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6966966/]
- 56. Scale development: ten main limitations and ... [https://prc.springeropen.com/articles/10.1186/s41155-016-0057-1]
- 57. Best Practices for Developing and Validating Scales ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2018.00149/full]
- 58. Development and Psychometric Properties of the Mental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12440801/]
- 59. Questionnaires in clinical trials: guidelines for optimal design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2823735/]
- 60. Design and estimation in clinical trials with subpopulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6282861/]
- 61. Methods for questionnaire design: a taxonomy linking ... [https://link.springer.com/article/10.1007/s11136-019-02209-6]
- 62. A comparison of approaches to improve worst-case ... [https://www.nature.com/articles/s41598-022-07167-7]
- 63. Strategies to Increase Response Rate and Reduce ... [https://publichealth.jmir.org/2025/1/e60022]
- 64. Increasing Participation and Completion Rates in ... [https://www.i-jmr.org/2025/1/e67981/]
- 65. , Translation - Cross Adaptation, and Cultural of... Validation [https://www.dovepress.com/translation-cross-cultural-adaptation-and-validation-of-measurement-in-peer-reviewed-fulltext-article-JMDH]
- 66. Journal of Medical Internet Research - Translation , Cross - Cultural ... [https://www.jmir.org/2025/1/e67948]
- 67. Dutch translation and cross - cultural of the Adult Social... validation [https://research.vu.nl/en/publications/dutch-translation-and-cross-cultural-validation-of-the-adult-soci]
- 68. Translation and Validation of the Self-Assessment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537816/]
- 69. Reproducible research practices and transparency in ... [https://pubmed.ncbi.nlm.nih.gov/32771255/]
- 70. Reproducible research practices and transparency in ... [https://www.sciencedirect.com/science/article/pii/S0015028220305069]
- 71. Reproducibility of Age at Menarche Gathered From Mail ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527403/]
- 72. Visualization Techniques in Healthcare Applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC9741729/]
- 73. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 74. Text has enhanced contrast - Rules - Siteimprove [https://alfa.siteimprove.com/rules/sia-r66]
- 75. The Psychometric Performance of the EQ Health and ... [https://www.sciencedirect.com/science/article/pii/S1098301525023368]
- 76. Beyond Benchmarks: Evaluating Generalist Medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12129431/]
- 77. Reproductive health literacy scale: a tool to measure the ... [https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-025-01959-6]
- 78. Development and validation of a measurement scale for ... [https://pubmed.ncbi.nlm.nih.gov/40424400/]
- 79. Measurement invariance of the Research Attitudes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317168/]
- 80. Psychometric evaluation and measurement invariance of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12128924/]
- 81. Testing for Measurement Invariance using Lavaan (in R) [https://dlab.berkeley.edu/news/testing-measurement-invariance-using-lavaan-r]
- 82. Psychometric Properties and Measurement Invariance of ... [https://www.mdpi.com/2254-9625/14/6/113]
- 83. Latent Growth Models (LGM) and Measurement Invariance ... [https://stats.oarc.ucla.edu/r/seminars/lgm/]
- 84. Assessing Measurement Invariance in Neighborhood ... [https://link.springer.com/article/10.1007/s11524-025-01020-8]
- 85. Measurement invariance and psychometric properties of ... [https://www.sciencedirect.com/science/article/abs/pii/S1740144521001534]
- 86. A cross-sectional study of demographic variation in health ... [https://bmcglobalpublichealth.biomedcentral.com/articles/10.1186/s44263-025-00190-6]
- 87. Responsiveness and interpretability of commonly used ... [https://hqlo.biomedcentral.com/articles/10.1186/s12955-021-01690-3]
- 88. Patient-Reported Outcome Measures for Adults and ... [https://pubmed.ncbi.nlm.nih.gov/37339377/]
- 89. Revisiting restricted reproductive rights in 2025: what do ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11986880/]
- 90. COSMIN - Improving the selection of outcome measurement ... [https://www.cosmin.nl/]
- 91. Assessing sexual and reproductive health dimensions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7774613/]
- 92. A COSMIN Systematic Review of Sexual Health Literacy ... [https://link.springer.com/article/10.1007/s10508-025-03142-1]
- 93. Developing and Psychometric Evaluation of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8262531/]
- 94. Evaluation of the psychometric properties of the Reproductive ... [https://researchportal.ukhsa.gov.uk/en/publications/evaluation-of-the-psychometric-properties-of-the-reproductive-aut/]